- 1Division of Population Studies and Prevention of Non-Communicable Diseases, Department of Population Health, Wrocław Medical University, Wrocław, Poland
- 2Division of Public Health, Department of Population Health, Wrocław Medical University, Wrocław, Poland
- 3Department of Applied Mathematics, Faculty of Environmental Engineering and Geodesy, Wrocław University of Environmental and Life Sciences, Wrocław, Poland
- 4Department of Angiology, Hypertension and Diabetology, Wroclaw Medical University, Wrocław, Poland
Introduction: Despite some improvement in awareness and treatment of hypertension, blood pressure control is still below expectations in Poland. The aim of the study was to analyze the secular trend of hypertension prevalence in the PURE Poland cohort study over 9 years of observation and to analyze factors associated with controlled HT.
Methods: The study group consisted of 1,598 participants enrolled in a Prospective Urban and Rural Epidemiological Study (PURE), who participated both in baseline (2007–2010) and 9-year follow-up (2016–2019). Hypertension was ascertained on the basis of (1) self-reported hypertension previously diagnosed by the physician, (2) self-reported anti-hypertensive medication, and/or (3) an average of two blood pressure measurements ≥140 mmHg systolic BP and/or ≥90 mmHg diastolic BP.
Results: The prevalence of hypertension increased from 69.4% at baseline to 85.9% at 9-year follow-up. The chance of HT was 8.6-fold higher in the oldest vs. the youngest age group [OR 8.55; CI 4.47–16.1]. Male sex increased the chance for hypertension over 3-fold [OR 3.23; CI 2.26–4.73]. Obesity, according to BMI, increased the chance of HT 8-fold [OR 8.01; CI 5.20–12.8] in comparison with normal body weight. Male sex decreased the chance of controlled HT after 9 years [OR 0.68; CI 0.50–0.92]. There was no statistically significant association between controlled HT and age or place of residence. Higher and secondary education increased the chance of controlled HT over 2-fold in comparison with primary education [OR 2.35; CI 1.27–4.34, OR 2.34; CI 1.33–4.11]. Obesity significantly decreased the chance of controlled HT after 9 years in comparison with normal body weight [OR 0.54; CI 0.35–0.83].
Conclusion: Factors significantly increasing the chance for controlled hypertension after 9 years were female sex, secondary and tertiary education, normal body weight, and avoiding alcohol drinking. Changes in lifestyle, with special emphasis on maintaining normal body weight, should be the basis of prevention and control of HT.
1. Introduction
According to the latest estimates, arterial hypertension (HT) affects 1.28 billion people worldwide—one in four men and one in five women are hypertensive (1). About half of the affected people are unaware of their condition. The prevalence of HT differs depending on the economic status of the country. It is estimated that two-third of HT patients live in countries with low or medium socio-economic status. HT is considered to be the main factor responsible for premature mortality. It affects the functioning of the whole cardiovascular system and other organs, e.g., kidneys and brain. HT risk factors can be divided into modifiable and non-modifiable. Non-modifiable risk factors include a family history of HT, age of over 65 years, and co-existing diseases such as diabetes or kidney disease. Modifiable risk factors include an unhealthy diet (excessive salt consumption (2), a diet high in saturated fat and trans fats, and low intake of fruits and vegetables), low physical inactivity, consumption of alcohol, and being overweight or obese (1). In 2019, the global prevalence of HT was 34% for men and 32% for women (3). On the contrary, the global analysis of HT prevalence included in the PURE study, which comprised countries from different socio-economic backgrounds, indicated that 40.8% of participants had elevated BP (4). There are still a lot of inequalities in BP prevalence and control between high- and low-income countries. In most high-income countries, HT prevalence decreased over time, whereas in low-income countries the opposite happened. In 2019, HT prevalence was the highest in central and eastern Europe, central Asia, Oceania, southern Africa, Latin America, and the Caribbean (3).
In Poland, according to the NATPOL survey in 2002, 29% of men and women aged 18 and older suffered from HT while 29% of survey participants had high normal blood pressure (5). The results of the WOBASZ study (2003–2005) and the NATPOL 2011 study indicated a high prevalence of HT as a high level of global risk within the population of adults in Poland (6, 7). NATPOL 2011 survey revealed a high prevalence of HT of 32%, and only in ~26% of all hypertensive patient's blood pressure was well-controlled (7). In another Polish survey, the PONS study revealed even higher HT prevalence of 67% in the Polish population in Kielce province (8). The Prospective Urban Rural Epidemiology (PURE) baseline study in Poland which was conducted between 2007 and 2010 showed that 60.28% of the studied population had HT. It was more prevalent among men than women (73.85% vs. 52.22%) (9). A recent nationwide cross-sectional study, LIPIDOGRAM 2015, showed that 49% of participants were hypertensive without significant differences between urban and rural settings (10). Analysis of cross-sectional data of the WOBASZ I and WOBASZ II study (2013–2016) revealed a 12% in HT prevalence between the first and second round of the study (11). Despite some improvement in treatment and BP control, they are still below expectations in the Polish population (12).
Studies on the prevalence of HT, lifetime trends, and BP control in Polish population are limited. The aim of the study was to analyze the secular trend of HT prevalence in the PURE Poland cohort study over 9 years of observation and to analyze factors associated with controlled HT.
2. Methods
2.1. Settings and participants
The study group consists of participants enrolled in the global Prospective Urban and Rural Epidemiological (PURE) study. The Polish cohort was established between 2007 and 2010, recruiting both urban and rural inhabitants from the Lower Silesia region in Poland. All participants were examined in accordance with the global PURE study protocol (13), which included a questionnaire study [individual health, household, family, food frequency questionnaire, and international physical activity questionnaire (IPAQ)], anthropometric measurements, blood pressure measurement, blood draw, ECG, and spirometry. The recruitment process of the Polish cohort and characteristics of the study group at the baseline were described by Zatońska et al. (14). The baseline cohort consisted of 2,036 adult participants (1,282 women and 754 men), aged 30–85 years (mean age: 54 years, SD ± 10). Participants have been repeatedly invited to the study center every 3 years and were examined with a consistent protocol. The study reports the results of 1,598 participants who took part in both the baseline study and 9-year follow-up (2016–2019).
2.2. Hypertension criteria
Hypertension was ascertained on the basis of (1) self-reported hypertension previously diagnosed by the physician, (2) self-reported anti-hypertensive medication, and/or (3) an average of two blood pressure measurements ≥140 mmHg systolic BP and/or ≥90 mmHg diastolic BP (9). Blood pressure measurements were carried out with an automated oscillometric device (Omron Corporation, Tokyo, Japan). The appropriate cuff size has been selected. Participants were advised to sit and rest for 5 min before consecutive blood pressure measurements. The same methodology was applied at the baseline and at 9-year follow-up. Hypertension was considered controlled after 9 years of observation if objectives of the ESH/ESC guidelines were met (BP < 140/90 mmHg).
2.3. Other variables
The following variables have been included in the analysis: sex, age, place of residence, education, marital status, attitudes toward tobacco smoking and alcohol consumption, body mass index (BMI), waist-to-hip ratio (WHR), and waist-to-height ratio (WHtR). Education was ascertained based on self-reported highest completed level, e.g., primary, vocational, secondary, and college/university.
The body mass of the participants was measured with the use of the Tanita Ironman Body Composition Monitor Model BC-554 with an accuracy of 0.1 kg. BMI was calculated as weight (kg) divided by height (m) squared. Participants were ascribed to four BMI categories according to the WHO guidelines: underweight (BMI < 18.5 kg/m2), normal weight (BMI 18.5–24.9 kg/m2), overweight (BMI 25.0–29.9 kg/m2), and obesity (BMI ≥ 30.0 kg/m2). The occurrence of abdominal obesity was assessed with the use of waist-to-hip ratio (WHR). Abdominal obesity was determined when WHR in men was ≥0.94 and in women was ≥0.80. Waist-to-height ratio (WHtR) has been assessed as waist circumference divided by body height expressed in the same units. Attitude toward tobacco smoking and alcohol consumption was self-reported by the participants. Participants could have chosen one of three possible answers regarding tobacco consumption: “formerly used tobacco products,” “currently use tobacco products,” and “never used tobacco products.” Regarding alcohol consumption, participants could have chosen between “formerly used alcohol products,” “currently use alcohol products,” and “never used alcohol products.”
2.4. Statistical methods
The normality of data was tested using the Shapiro–Wilk test and the assessment of the Q-Q plot. The significance of demographic and clinical data in the control and HT groups was tested using the chi square or Fisher's exact test depending on the number of expected observations. The relationship between 9-year controlled HT and BMI, WHR, and waist-to-height ratio was identified using Fisher's exact test. Analysis of chance for controlled HT after 9 years was performed using generalized linear mixed model analysis with patient ID as a random effect. Effect size is presented as odds ratio with 95% confidence intervals. The presented model is a full model adjusted for the following covariates: sex, age, residence, education, BMI, WHR, tobacco use, alcohol use, and blood pressure medications. Analysis was performed in R for Windows (version 4.0.3) (R Core Team, 2020). Differences were considered statistically significant if the p-value was lower than 0.05.
2.5. Ethics
The study has been reviewed and accepted by the Bioethics Committee of the Wrocław Medical University and has therefore been performed in accordance with the ethical standards laid down in an appropriate version of the 1964 Declaration of Helsinki (Positive opinion of The Bioethics Committee of the Wrocław Medical University nr KB- 443/2006).
3. Results
3.1. Prevalence of HT at the baseline
Baseline characteristics of the population considering the prevalence of HT and corresponding risk factors are presented in Table 1. At the baseline, HT was observed in 69.4% of participants. A total of 34.9% of the baseline population was not diagnosed with HT previously; however, BP measurement indicated HT. The occurrence of HT was significantly associated with age, sex, level of education, marital status, BMI, WHR, waist-to-height ratio, and attitude toward tobacco smoking. There was a gradual increase in HT prevalence along with age. HT was the most prevalent in the oldest age group >64 years of age (86.3%) in comparison with 42.8% in the youngest age group <45 years of age. The risk of HT was 8.7-fold higher in the oldest vs. the youngest age group [OR 8.73; CI 5.63–13.9].
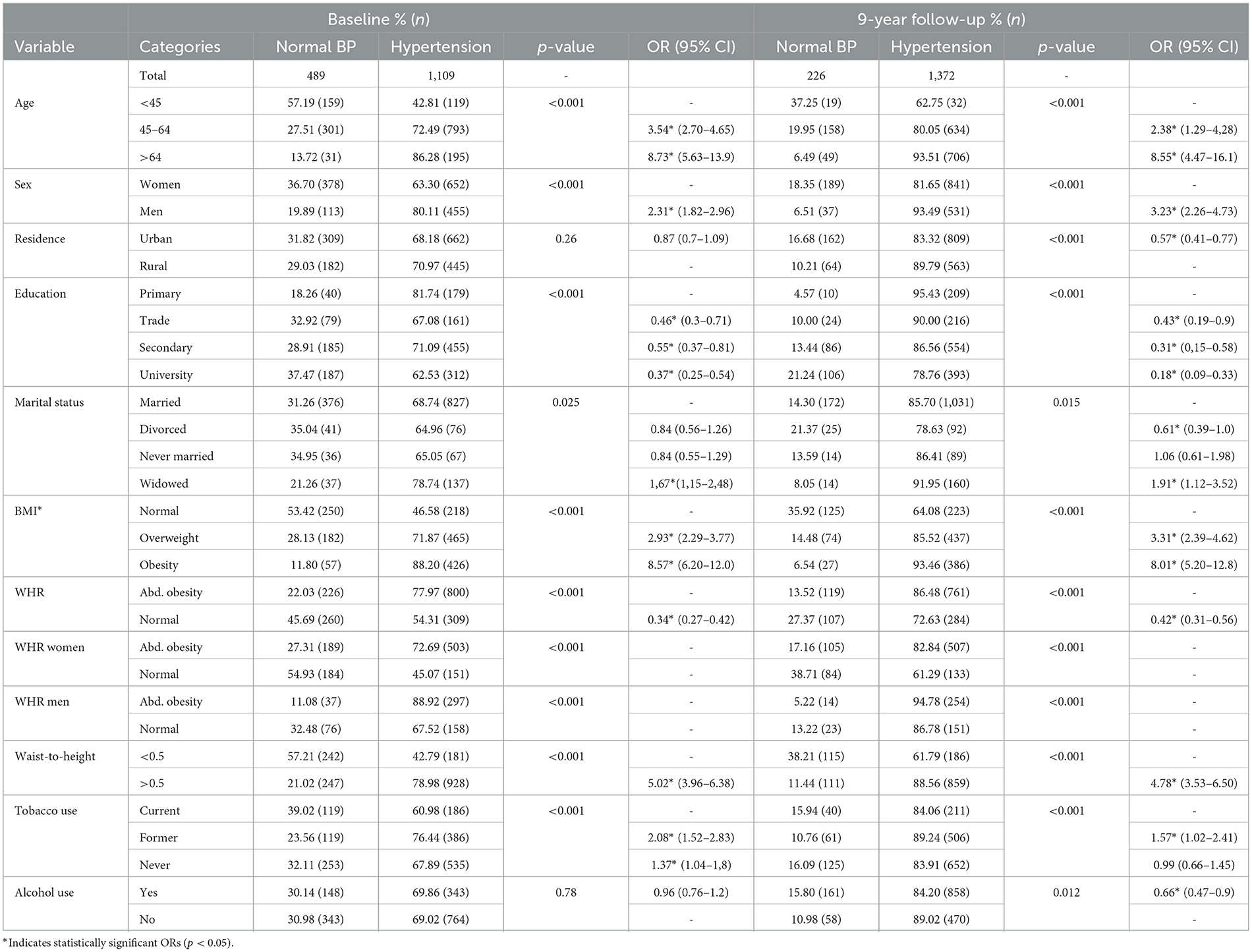
Table 1. Prevalence of hypertension at baseline and 9-year follow-up with corresponding sociodemographic factors.
HT was more prevalent in men than in women (80.1% vs. 63.3%). Male sex increased the chance of HT over 2-fold [OR 2.31; CI 1.82–2.96]. At the baseline, there was no statistically significant difference in HT prevalence between urban and rural inhabitants. Level of education was inversely associated with HT. Nearly 81.7% of participants with primary education was hypertensive in comparison with 62.5% of participants with higher education. Higher education was significantly associated with a lower chance of HT [OR 0.37, CI 0.25–0.54]. Widowhood increased the chance of HT over 1.5-fold [OR 1.67, CI 1.15–2.48] in comparison with being currently married.
The chance of HT increased along with the increase in BMI. Being overweight increased the chance of HT almost 3-fold [OR 2.93, CI 2.29–3.77], whereas obesity increased the chance of HT 8.6-fold [OR 8.57; CI 6.20–12.0] in comparison with normal body weight. A participant without abdominal obesity according to WHR also had a significantly lower chance of HT [OR 0.34; CI 0.27–0.42]. Waist-to-height ratio higher than 0.5 increased the chance of HT 5-fold [OR 5.02; CI 3.96–6.38]. Surprisingly, former smokers and never smokers had a higher chance of HT in comparison with current smokers. There was no significant difference in HT prevalence between alcohol drinkers and non-drinkers.
3.2. Prevalence of HT in 9-year follow-up
In the article, 9-year follow-up characteristics of the population are presented in Table 1. In the 9-year follow-up, HT was present in 85.9% of the study population. The occurrence of HT was significantly associated with age, sex, place of residence, level of education, marital status, BMI, WHR, waist-to-height ratio, and attitude toward tobacco smoking and alcohol use. Similarly as at the baseline, in the 9-year follow-up, the prevalence of HT was significantly associated with age. The chance of HT was 8.6-fold higher in the oldest vs. the youngest age group [OR 8.55; CI 4.47–16.1]. The male sex increased the chance of HT even more evidently than in the baseline [OR 3.23; CI 2.26–4.73]. In the 9-year follow-up, contrary to the baseline, the place of residence was a significant factor differentiating the prevalence of HT. The higher the level of education, the lower the chance of HT. Similarly to baseline, being widowed significantly increased the chance of HT in comparison with being currently married [OR 1.91; CI 1.12–3.52]. Additionally, in 9-year follow-up, being divorced significantly lowered the chance of HT [OR 0.61; CI 0.39–1.0].
Similarly to the baseline, obesity, according to BMI, increased the chance of HT 8-fold [OR 8.01; CI 5.20–12.8] in comparison with normal body weight. HT was significantly more prevalent in participants with abdominal obesity ascertained on the basis of WHR. In 9-year follow-up, the chance of HT was 1.6-fold higher in the former vs. current smokers [OR 1.57; CI 1.02–2.41]. Contrary to the baseline, where alcohol use was an insignificant factor associated with HT prevalence, in 9-year follow-up, current alcohol use was associated with a lower chance of HT [OR 0.66; CI 0.47–0.9].
3.3. Analysis of controlled HT in 9-year follow-up
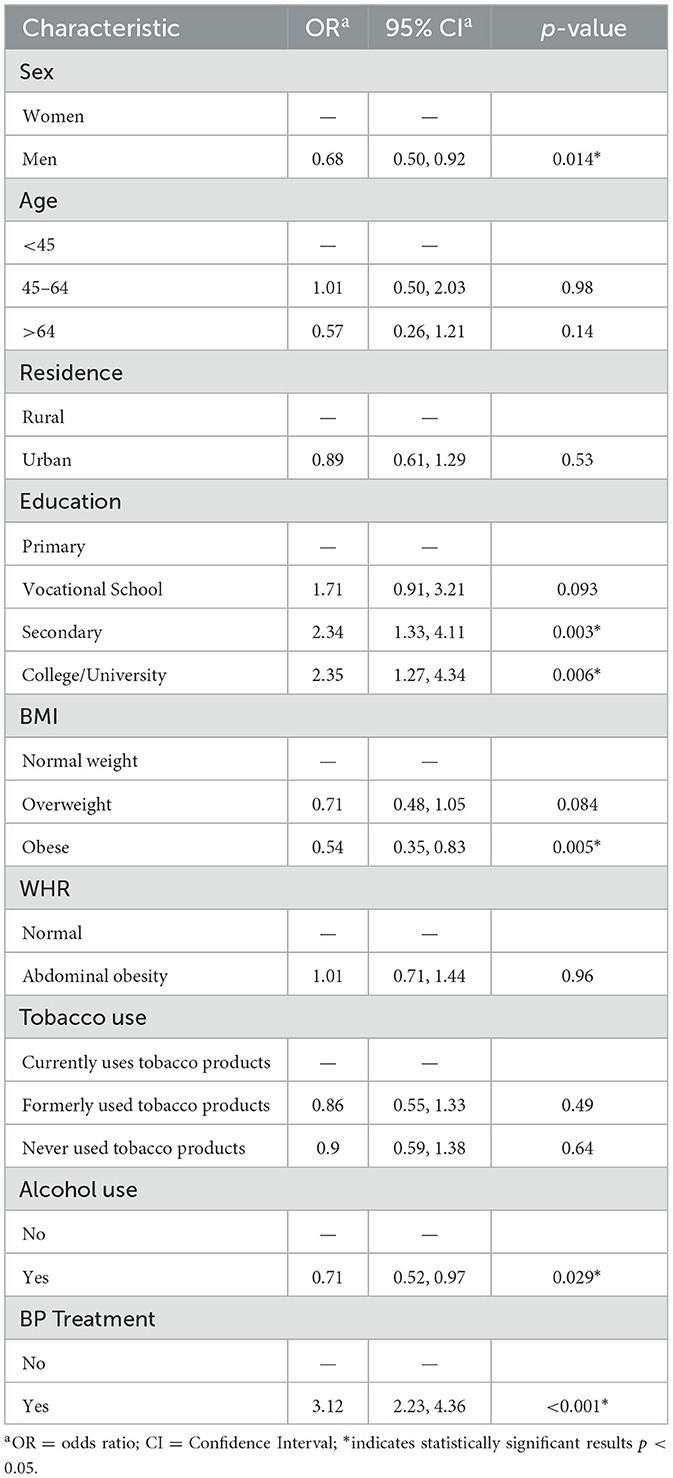
We have performed the analysis of control of HT in participants with HT diagnosed at the baseline. Factors associated with control of HT are presented in Table 2. Factors that significantly differentiated the control of HT in 9-year follow-up were sex, education, BMI, and use of alcohol and BP medication.
Male sex decreased the chance of controlled HT after 9 years [OR 0.68; CI 0.50–0.92]. There was no statistically significant association between controlled HT and age or place of residence. On the contrary, the chance of controlled HT increased significantly with an increasing level of education. Higher and secondary education increased the chance of controlled HT over 2-fold in comparison with primary education [OR 2.35; CI 1.27–4.34, OR 2.34; CI 1.33–4.11].
Obesity significantly decreased the chance of controlled HT after 9 years in comparison with normal body weight [OR 0.54; CI 0.35–0.83]. In this model, there was no statistical significance in the association between WHR and controlled HT. Alcohol use significantly decreased the chance of controlled HT [OR 0.71; CI 0.52–0.97].
3.4. ROC analyses of predicted HT in 9-year follow-up
We performed the ROC analyses, indicating the thresholds of BMI, WHR, and waist-to-height ratio above which the risk of HT after 9 years was significantly higher. All ROC analyses are presented in Figure 1.

Figure 1. Analysis of cutoff point of anthropometric indices for higher risk of hypertension in 9-year follow-up with the use of the ROC curve. (A) BMI cutoff point: 26.11 kg/m2. (B) WHR in women cutoff point: 0.83. (C) WHR in men cutoff point: 0.91. (D) Waist-to-height ratio cutoff point: 0.53.
The ROC analysis indicated the BMI cutoff point of 26.11 kg/m2, above which the risk of HT was significantly higher [AUC 0.738 (0.703, 0.773); sensitivity 0.70; specificity 0.67; PPV 0.91; NPV 0.33]. The cutoff point of WHR in women was 0.83 [AUC 0.709 (0.668, 0.749); sensitivity 0.66; specificity 0.66; PPV 0.87; NPV 0.36]. The cutoff point of WHR in men was 0.91 [AUC 0.682 (0.593, 0.771); sensitivity 0.77; specificity 0.54; PPV 0.95; NPV 0.18]. Analyzed cutoff points correspond to current criteria of abdominal obesity according to WHR. The cutoff point of waist-to-height ratio was 0.53 [AUC 0.773 (0.74, 0.805); sensitivity 0.71; specificity 0.75; PPV 0.93; NPV 0.36].
4. Discussion
In this article, we analyzed the prevalence and control of HT in 9 years of observation of the Polish cohort participating in the PURE study. The prevalence of HT was significantly associated with sex, age, place of residence, level of education, marital status, BMI, WHR, waist-to-height ratio, alcohol use, and attitudes toward tobacco smoking. We found that the control of HT in 9-year follow-up was significantly lower in men, participants currently drinking alcohol, participants with a lower level of education, and elevated BMI.
The worldwide prevalence of HT is high but is not always followed by adequate BP control (15, 16). Although in the late 1990's and early 2000's, there has been an improvement in global treatment and control of HT, the control rates have plateaued in the last decade at lower levels than expected (17). The cross-sectional analysis of epidemiological data obtained in WOBASZ I (2003–2005) and WOBASZ II (2013–2014) indicates that the prevalence of HT in Poland increased by 12% in that time (11). The prevalence of HT in our cohort increased by over 16% during 9 years of observation. The prevalence of HT in our cohort is high, which is partially explained by a higher average age than in the general Polish population. On the contrary, it has been previously reported that obesity, abdominal obesity, and HT are more prevalent in Poland than in North-Western European countries (18). Central and Eastern European countries, including Poland, are characterized by a higher prevalence of raised BP, especially in men (19). In comparison with other cohorts from countries of similar socio-economic status in the PURE study, Poland was characterized by a higher average systolic blood pressure and higher prevalence of HT (4).
In our cohort, the risk of HT was 2-fold higher at the baseline and 3-fold higher at 9-year follow-up in men than in women. A higher prevalence of HT in men than women is a widely observed phenomenon in most regions of the world (19). Interestingly, the difference in HT prevalence between men and women tends to be larger in high-income countries and in Central/Eastern Europe (19). On the contrary, the increment in HT prevalence in our cohort was higher in women than in men, which has been previously observed in US and UK cohort studies (20, 21).
We have analyzed factors associated with controlled hypertension (normal blood pressure in 9-year follow-up among previously hypertensive participants). In our cohort, men were less likely to control the HT after 9 years. This observation is similar to cross-sectional analysis of WOBASZ Senior and WOBASZ II studies, where women's awareness of HT and HT control and treatment was higher than that of men (12). In the same study, despite some improvement in BP control over 7 years of observations, 70% of older adult population had poorly controlled HT. In the analysis of the global PURE study data, women were also characterized by greater awareness of HT, higher adherence to treatment, and better BP control than men (4).
The chance for controlled HT in our study was also significantly lower with excessive body weight (especially in the case of obesity) and alcohol drinking. HT control in Poland among outpatients has been recently reported as unsatisfactory (22). The majority of patients with uncontrolled hypertension (>70%) were characterized by dyslipidemia and abdominal obesity (22). In the previously mentioned WOBASZ Senior/WOBASZ II analysis, it has been also observed that the parameters of physical activity, obesity, and dyslipidemia deteriorated between studies, which may furtherly contribute to poor HT control (12). In a study by Prejbisz et al. (23), elements of metabolic syndrome, especially obesity and dyslipidemia, were significantly more prevalent among patients with resistant HT.
Obesity is a well-established contributor to HT (24). Obesity influences the risk of HT, i.e., through activation of the renin–angiotensin–aldosterone (RAS) system, activation of mineralocorticoid receptors, and activation of the sympathetic nervous system (SNS) (24). Our analyses showed that BMI above 26 kg/m2, characteristic of being overweight, and abdominal obesity significantly increased the risk of HT. Excessive body weight remains one of the biggest challenges for public health worldwide as its prevalence increased significantly over the years. According to the National Health and Nutrition Examination Survey (NHANES), the prevalence of obesity in the USA between 2000 and 2018 increased in men from 27.5% to 43.0% and in women from 33.4% to 41.9% (25). Moreover, a significant increase in obesity prevalence has been observed in the population of children and adolescents (25). In the similar time period, the analysis of controlled HT in the USA performed by Muntner et al. (26) revealed that HT control increased between 1999 and 2008, then remained stable, and then significantly decreased from 48.5% in 2013/2014 to 43.7% in 2017/2018. The study concomitantly revealed the increase in HT prevalence between the study periods (26, 27).
In our cohort, the chance for controlled HT was over 2-fold higher in participants with secondary/university education vs. primary education. The link between socio-economic status and hypertension has been previously investigated, pointing toward better awareness, treatment, and control among higher-income households (28). In accordance with our results, the higher prevalence of HT and poorer HT control in participants with a lower level of education have been observed in the HAPPIE study (16). In the analysis of the global PURE study data, a higher level of education has been significantly associated with greater awareness of HT and treatment in men, but not in women, and with greater control regardless of sex (4).
Although the prevalence of tobacco smoking has significantly decreased in Poland since the 1980's (29), the consumption of alcohol is alarmingly high. Alcohol consumption, measured in liters of pure alcohol consumed per capita, has significantly increased in the last 20 years in Poland (30), causing an alarming increase in alcohol-related deaths (31). In our cohort, alcohol consumption was associated with a higher chance of uncontrolled HT. Similarly, a higher prevalence of HT and worse HT control have been also observed in the HAPPIE study (16). Recent studies indicate that even moderate consumption of alcohol can be associated with increased BP, especially in patients with a higher cardiovascular risk and diabetes (32). Alcohol consumption of up to 1–2 drinks per day has been significantly associated with an increased risk of HT in men, whereas consumption higher than two drinks per day was associated with a higher risk of HT regardless of sex (33). In our study, we assessed only the attitudes toward alcohol drinking, without taking into consideration the amount nor type of consumed alcohol.
A recently published study indicated that the lifetime risk of developing HT is as high as 75% (34). Since elevated BP has been observed also in the young population, the importance of primary prevention and early education about HT is strongly emphasized (34). Another factor pointing toward the need for early prevention is the higher cardiovascular risk in HT patients controlled with medication in comparison with people without HT (35). One of the largest screening campaigns conducted in Poland (May Measurement Month), indicated that one-third of participants were hypertensive and half of the participants with previously diagnosed HT and on BP medication were uncontrolled (36).
Our study has some limitations to discuss. First, we present the results from a cohort study, the population of which differs slightly from the overall Polish population (by the overrepresentation of women, urban residents, and participants with higher education). Having said that, to the best of our knowledge, this is one of the very few longitudinal cohort studies conducted with a consistent protocol for over a decade in Poland. Another strength is implementing repeated BP measurements conducted by a trained professional and not relying only on self-reported data.
5. Conclusion
Factors significantly increasing the chance for controlled hypertension after 9 years were female sex, secondary and tertiary education, normal body weight, and avoiding alcohol drinking. In addition to proper pharmacotherapy, changes in lifestyle, with special emphasis on maintaining normal body weight, should be the basis of the prevention and control of HT.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author: a2F0YXJ6eW5hLnphdG9uc2thQHVtdy5lZHUucGw=.
Ethics statement
The studies involving human participants were reviewed and approved by Positive opinion of The Bioethics Committee of the Wrocław Medical University nr KB-443/2006. The patients/participants provided their written informed consent to participate in this study.
Author contributions
KZ made contributions to the conception and design of the article, drafting the article, and revising it. AB-R made contribution to interpretation of data and drafting the article. KP-Z made contribution to analysis and interpretation of data and revision of the manuscript. DG-D made contributions to data analysis and drafting of the manuscript. MW made contribution to data acquisition. MK made contribution to data analysis and presentation of the results. AS made contributions to the conception and design of the article and revising the manuscript. All authors provided approval for publication of the content and agree to be accountable for all aspects of the article in ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved.
Funding
The main PURE study and its components are funded by the Population Health Research Institute, the Canadian Institute of Health Research, the Heart and Stroke Foundation of Ontario, and unrestricted grants from several pharmaceutical companies. The Poland cohort study is funded by Wroclaw Medical University (grant no. MR.C300.06.001). Additionally, the article was prepared within the framework of the topic “Zdrowie populacyjne w obliczu kryzysu - ocena czynników ryzyka wystepowania chorób przewlekłych oraz organizacji i zarzadzania w systemie ochrony zdrowia” (Population health in face of the crisis-assessment of risk factors of chronic diseases and organization and management of the health system) task recorded in the SIMPLE system: SUBZ.E260.23.023. We declare that the funding body had no role in the design of the study; the collection, analysis, or interpretation of data; and no role in writing the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Hypertension - key facts. (2021). Available online at: https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed January 19, 2023).
2. Mente A, O'Donnell M, Rangarajan S, McQueen M, Dagenais G, Wielgosz A, et al. Urinary sodium excretion, blood pressure, cardiovascular disease, and mortality: a community-level prospective epidemiological cohort study. Lancet. (2018) 392:496–506. doi: 10.1016/S0140-6736(18)31376-X
3. Zhou B, Carrillo-Larco RM, Danaei G, Riley LM, Paciorek CJ, Stevens GA, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. (2021) 398:957–80. doi: 10.1016/S0140-6736(21)01330-1
4. Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. (2013) 310:959–68. doi: 10.1001/JAMA.2013.184182
5. Zdrojewski T, Szpakowski P, Bandosz P, Pajak A, Wiecek A, Krupa-Wojciechowska B, et al. Arterial hypertension in Poland in 2002. J Hum Hypertens. (2004) 18:557–62. doi: 10.1038/SJ.JHH.1001739
6. Drygas W, Niklas AA, Piwońska A, et al. Multi-centre National Population Health Examination Survey (WOBASZ II study): assumptions, methods, and implementation. Kardiol Pol. (2016) 74:681–90. doi: 10.5603/KP.A2015.0235
7. Zdrojewski T, Bandosz P, Gaciong Z, et al. Rozpowszechnienie czynników ryzyka chorób układu sercowo-naczyniowego w Polsce w 2011 r. Zakres wieku 18-79 lat. NATPOL 2011 [Increase in cardiovascular diseases risk factors distribution in Poland in 2011. Age span 18-79. NATPOL 2011]. In: XV Miedzynarodowy Kongres PTK [XV Congress of Polish Cardiac Society (PTK)]. (2011.)
8. Szuba A, Martynowicz H, Zatońska K, Ilow R, Regulska-Ilow B, Rózańska D, et al. Prevalence of hypertension in a sample of Polish population—Baseline assessment from the prospective cohort ‘PONS' study. Ann Agric Environ Med. (2011) 18:260–4.
9. Szuba A, Martynowicz H, Zatońska K, et al. Prevalence of hypertension in Polish population of PURE Poland study. J Heal Inequalities. (2017) 2:157–62. doi: 10.5114/jhi.2016.65356
10. Studziński K, Tomasik T, Windak A, Banach M, Wójtowicz E, Mastej M, et al. The differences in the prevalence of cardiovascular disease, its risk factors, and achievement of therapeutic goals among urban and rural primary care patients in Poland: results from the LIPIDOGRAM 2015 study. J Clin Med. (2021) 10:5656. doi: 10.3390/JCM10235656/S1
11. Niklas A, Flotyńska A, Puch-Walczak A, et al. Prevalence, awareness, treatment and control of hypertension in the adult Polish population—multi-center national population health examination surveys—WOBASZ studies. Arch Med Sci. (2018) 14:951–61. doi: 10.5114/AOMS.2017.72423
12. Niklas AA, Flotyńska A, Zdrojewski T, Pajak A, Topór-Madry R, Nadrowski P, et al. Trends in hypertension prevalence, awareness, treatment, and control among Polish adults 75 years and older during 2007–2014. Cardiol J. (2018) 25:333–44. doi: 10.5603/CJ.A2018.0043
13. Teo K, Chow CK, Vaz M, Rangarajan S, Yusuf S, Group PI-W. The Prospective Urban Rural Epidemiology (PURE) study: Examining the impact of societal influences on chronic noncommunicable diseases in low-, middle-, and high-income countries. Am Heart J. (2009) 158:1–7. doi: 10.1016/j.ahj.2009.04.019
14. Zatońska K, Zatoński WA, Szuba A. Prospective urban and rural epidemiology Poland—study design. J Heal Inequalities. (2016) 2:136–41. doi: 10.5114/jhi.2016.65353
15. Ma S, Yang L, Zhao M, Magnussen CG, Xi B. Trends in hypertension prevalence, awareness, treatment and control rates among Chinese adults, 1991–2015. J Hypertens. (2021) 39:740–8. doi: 10.1097/HJH.0000000000002698
16. Lu W, Pikhart H, Tamosiunas A, et al. Prevalence, awareness, treatment and control of hypertension, diabetes and hypercholesterolemia, and associated risk factors in the Czech Republic, Russia, Poland and Lithuania: a cross-sectional study. BMC Public Health. (2022) 22:3. doi: 10.1186/S12889-022-13260-3
17. Zhou B, Danaei G, Stevens GA, et al. Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet. (2019) 394:639–51. doi: 10.1016/S0140-6736(19)31145-6
18. Chrostowska M, Szyndler A, Paczwa P, Narkiewicz K. Impact of abdominal obesity on the frequency of hypertension and cardiovascular disease in Poland - results from the IDEA study (international day for the evaluation of abdominal obesity). Blood Press. (2011) 20:145–52. doi: 10.3109/08037051.2010.538996
19. Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. (2021) 18:785–802. doi: 10.1038/s41569-021-00559-8
20. Ji H, Kim A, Ebinger JE, Niiranen TJ, Claggett BL, Merz CNB, et al. sex differences in blood pressure trajectories over the life course. JAMA Cardiol. (2020) 5:255–62. doi: 10.1001/JAMACARDIO.2019.5306
21. Wills AK, Lawlor DA, Matthews FE, Sayer AA, Bakra E, Ben-Shlomo Y, et al. Life course trajectories of systolic blood pressure using longitudinal data from eight UK cohorts. PLoS Med. (2011) 8:e1000440. doi: 10.1371/JOURNAL.PMED.1000440
22. Filipiak KJ, Tomaniak M, Płatek AE, Szymański FM, Tykarski A. Negative predictors of treatment success in outpatient therapy of arterial hypertension in Poland. Results of the CONTROL NT observational registry. Kardiol Pol. (2018) 76:353–61. doi: 10.5603/KP.A2017.0211
23. Prejbisz A, Klocek M, Gasowski J, Topór-Madry R, Leśniak W, Kabat M, et al. Factors associated with resistant hypertension in a large cohort of hypertensive patients: the Pol-Fokus study. Pol Arch Med Wewn. (2015) 125:249–59. doi: 10.20452/PAMW.2782
24. Hall JE, Do Carmo JM, Da Silva AA, et al. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. (2015) 116:991–1006. doi: 10.1161/CIRCRESAHA.116.305697
25. Ogden CL, Fryar CD, Martin CB, et al. Trends in obesity prevalence by race and hispanic origin−1999–2000 to 2017–2018. JAMA. (2020) 324:1208–10. doi: 10.1001/JAMA.2020.14590
26. Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, et al. Trends in blood pressure control among us adults with hypertension, 1999–2000 to 2017–2018. JAMA. (2020) 324:1190–200. doi: 10.1001/JAMA.2020.14545
27. Muntner P, Miles MA, Jaeger BC, Iii LH, Hardy ST, Ostchega Y, et al. Blood pressure control among US adults, 2009 to 2012 through 2017 to 2020. Hypertens. (2022) 79:1971–80. doi: 10.1161/HYPERTENSIONAHA.122.19222
28. Palafox B, McKee M, Balabanova D, AlHabib KF, Avezum AJ, Bahonar A, et al. Wealth and cardiovascular health: a cross-sectional study of wealth-related inequalities in the awareness, treatment and control of hypertension in high-, middle- and low-income countries. Int J Equity Health. (2016) 15:6. doi: 10.1186/S12939-016-0478-6
29. Zatoński WA, Zatoński M, Janik-Koncewicz K, et al. Hundred years of cigarette smoking in Poland: three phases of the tobacco epidemic. J Heal Inequalities. (2017) 3:118–22. doi: 10.5114/JHI.2017.74200
30. Zatoński WA, Janik-Koncewicz K, Zatoński M. Life expectancy and alcohol use health burden in Poland after 2002. J Heal Inequalities. (2022) 8:4–16. doi: 10.5114/JHI.2022.117977
31. Zatoński WA, Zatoński M, Janik-Koncewicz K, et al. Alcohol-related deaths in poland during a period of weakening alcohol control measures. JAMA. (2021) 325:1108–9. doi: 10.1001/JAMA.2020.25879
32. Mayl JJ, German CA, Bertoni AG, Upadhya B, Bhave PD, Yeboah J, et al. Association of alcohol intake with hypertension in type 2 diabetes mellitus: the accord trial. J Am Heart Assoc. (2020) 9:7334. doi: 10.1161/JAHA.120.017334
33. Roerecke M, Tobe SW, Kaczorowski J. Sex-specific associations between alcohol consumption and incidence of hypertension: a systematic review and meta-analysis of cohort studies. J Am Heart Assoc. (2018) 7:202. doi: 10.1161/JAHA.117.008202
34. Chen V, Ning H, Allen N, Kershaw K, Khan S, Lloyd-Jones DM, et al. Lifetime risks for hypertension by contemporary guidelines in African American and white men and women. JAMA Cardiol. (2019) 4:455–9. doi: 10.1001/JAMACARDIO.2019.0529
35. Liu K, Colangelo LA, Daviglus ML, Goff DC, Pletcher M, Schreiner PJ, et al. Can antihypertensive treatment restore the risk of cardiovascular disease to ideal levels? The coronary artery risk development in young adults (CARDIA) study and the multi-ethnic study of atherosclerosis (MESA). J Am Heart Assoc. (2015) 4:2275. doi: 10.1161/JAHA.115.002275
Keywords: hypertension, Poland, cohort, hypertension prevention and control, blood pressure-prevention and control
Citation: Zatońska K, Basiak-Rasała A, Połtyn-Zaradna K, Gaweł-Dąbrowska D, Wołyniec M, Karczewski M and Szuba A (2023) Sociodemographic and behavioral factors associated with controlled hypertension after 9 years of observation of a PURE Poland cohort study. Front. Public Health 11:1167515. doi: 10.3389/fpubh.2023.1167515
Received: 16 February 2023; Accepted: 28 March 2023;
Published: 21 April 2023.
Edited by:
Donald Lee Batisky, University of Cincinnati, United StatesReviewed by:
Ronny Westerman, Bundesinstitut für Bevölkerungsforschung, GermanyKrzysztof Kaczmarek, Medical University of Silesia, Poland
Copyright © 2023 Zatońska, Basiak-Rasała, Połtyn-Zaradna, Gaweł-Dąbrowska, Wołyniec, Karczewski and Szuba. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alicja Basiak-Rasała, YWxpY2phLmJhc2lhay1yYXNhbGFAdW13LmVkdS5wbA==
 Katarzyna Zatońska1
Katarzyna Zatońska1 Alicja Basiak-Rasała
Alicja Basiak-Rasała