- 1School of Economics, Peking University, Beijing, China
- 2China National Health Development Research Center, Beijing, China
Background: Falls place a heavy burden on older adults and families, and there was little research on the relationship between falls and depressive symptoms among older adults in China. This study is designed to examine the association between falls and depressive symptoms in Chinese older adults.
Methods: This study was based on 9,539 data sets from the China Health and Retirement Longitudinal Study (CHARLS) in 2018. The 10-item Center for Epidemiologic Studies-Depression Scale (CESD-10) was used to access depressive symptoms in older adults. A logistic regression model was used to calculate multivariate odds ratios (ORs) and 95% confidence intervals (CIs) for falls and depressive symptoms, adjusted for possible confounders. The Classification and regression tree (CART) demonstrates the prediction of the target variable values based on other variables.
Results: In this study, 9,539 older people were selected: 60–69 years old accounted for 63.0%, 70–79 years old accounted for 29.7%, and 80 years old and above accounted for 7.3%. Male accounted for 49.7% and female for 50.3%. The rate of falls among older adults was 21.4%, and the rate of depressive symptoms was 33.9%. Adjusted ORs (OR = 1.37, 95% CI: 1.23, 1.53) showed a significant association between falls and depressive symptoms among older adults. Subgroup analysis revealed that this association was statistically significant across male (OR = 1.29, 95% CI: 1.23, 1.53) and female (OR = 1.42, 95% CI: 1.23, 1.64), 60–69 aged (OR = 1.38, 95% CI: 1.19, 1.60) and 70–79 aged (OR =1.42, 95% CI: 1.16, 1.74), rural (OR = 1.42, 95% CI: 1.25, 1.61), <15,000 CNY (OR = 1.35, 95% CI: 1.19, 1.54) and more than 25,000 CNY (OR = 1.42, 95% CI: 1.09, 1.85). Additionally, The CART model showed that the probability (73.0%) of falls was highest among older adults with depressive symptoms who self-rated poor health and female gender.
Conclusions: This cross-sectional study demonstrated a significant association between falls and depressive symptoms in Chinese older adults. The findings provide some evidence and support for risk monitoring, screening for depressive symptoms, and early prevention in the high-risk older population.
1. Introduction
Falls are the leading cause of injury, disability and death among older adults, and are increasingly recognized as a severe public health problem among the older population (1, 2). It is estimated that nearly one-third of older adults have an accidental fall each year, and 50% of adults over 80 have an accidental fall (3, 4). Falls in older adults can lead to loss of function, including traumatic brain injury, hip fractures, and other moderate to severe injuries resulting in limited mobility, loss of autonomy, and death (5–7). As the most costly type of injury among older adults, falls place a heavy burden on individuals, their families, and society (8).
Depression is one of the most common mental health disorders in older adults, and it has become a severe health problem in both developed and developing countries around the world (9). Globally, 322 million people suffer from depression (10), accounting for 12.1% of total global disability life expectancy and 26.4% of total global disability-adjusted life expectancy (11). China has the largest older population in the world, and the challenge of depressive symptoms among older adults should be taken seriously enough.
Falls and depressive symptoms are both important older adult health issues. Although the findings were not entirely consistent, previous studies have shown that falls were associated with depressive symptoms, and the interaction of these two can lead to many health problems (12–14). In recent years, a series of studies in China have demonstrated that falls were associated with depressive symptoms using nationwide representative data from various perspectives, including age, gender, place of residence, and experience of falls (15–18). It should be noted that both depressive symptoms and falls are dynamic and undergo gradual change (19). It is significant to analyze and comprehend the current status, health characteristics, and association between falls and depressive symptoms among older Chinese adults to enrich the research in this area.
A better understanding of the relationship between falls and depressive symptoms will shed light on designing evidence-based prevention and interventions targeting this vulnerable population. We propose the hypothesis that there is an association between falls and depressive symptoms. We will draw profiles of falls and depressive symptoms among older adults in China using nationwide representative data from the China Health and Retirement Longitudinal Study (CHARLS). We will investigate the association between falls and depressive symptoms in older adults of different ages, gender, residence, and income through subgroup analyses while adjusting for various sociodemographic, lifestyle, disease, and health conditions. Subsequently, the Classification and regression tree (CART) demonstrates the prediction of the target variable values based on other variables. This study may expand our understanding of the relationship between falls and depressive symptoms in older adults in China and provide a valuable reference for related policy development.
2. Materials and methods
2.1. Design and study population
The data for this study were based on the third wave of the China Health and Retirement Longitudinal Study (CHARLS) conducted by Peking University in 2018, and the respondents of CHARLS were selected using a multistage stratified probability-proportional to size sampling (PPS) technique, which is a nationally representative community-based population survey (20). The project sampling covered 150 county-level units on the Chinese Mainland (scattered in 28 provincial units across the country), 450 village -level units, and about 10,000 households. A household survey was conducted among residents aged 45 and above. CHARLS carried out three national follow-up surveys in 2013, 2015, and 2018, of which 19,816 individual questionnaires for those aged 45 and over were successfully completed in 2018. The 2018 wave of CHARLS data is the most recent data available. In addition, the data is based on a national sample survey, which makes it a large and representative sample. Survey data and detailed information about the CHARLS can be accessed through its official website (charls.cer.edu.cn/en).
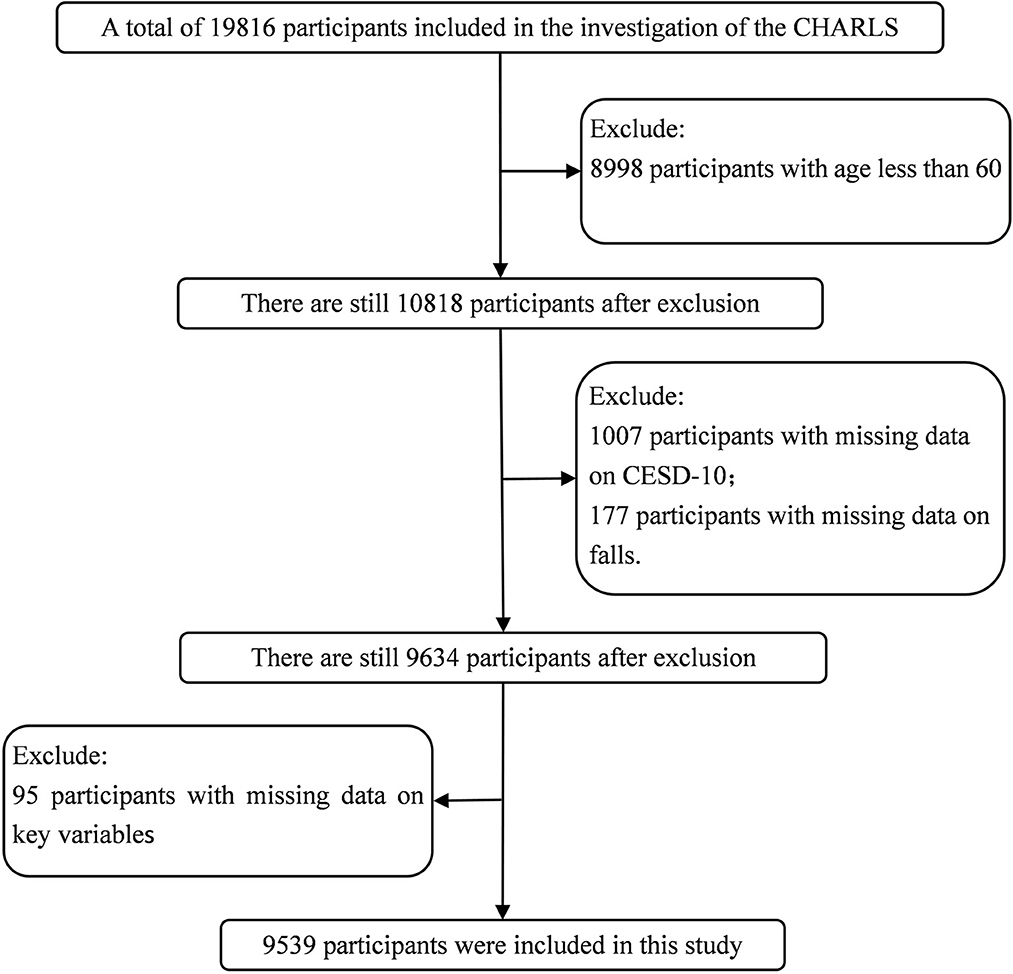
Based on a large population-based study, the current study excluded participants if they were younger than 60 years old, missing CESD-10 date, missing falls date, and missing values in main variables. A total of 19,816 participants completed the CHARLS in 2018, 8,998 participants < 60 years old were excluded, 1,007 participants missing CESD-10 data were excluded, 177 participants were excluded for missing falls data, 95 participants missing values in main variables were excluded. After the above screening, 9,539 participants were finally included in our analysis (for the sample screening process, see Figure 1).
2.2. Depressive symptoms assessment
Our study measured depressive symptoms using the 10-item Center for Epidemiological Studies Depression Scale (CESD), the scale was presented in the first part of the Supplementary material. Survey respondents were asked about the number of days of relevant experience in the past week. Each item was rated on a four-point Likert scale: 0 (rarely or none of the time; < 1 day), 1 (some of the time; 1–2 days), 2 (much or a moderate amount of the time; 3–4 days), or 3 (most or all of the time; 5–7 days). The scale has a maximum score of 30 and a minimum score of 0, with higher scores indicating higher levels of depressive symptoms. A previous survey showed that the cut-off point of 10 had high levels of sensitivity (0.85) and specificity (0.80) in Chinese older adults (21), and the cut-off points of 10 used in CESD-10 have been validated in numerous studies of the older adults in China (22, 23). Thus, we used 10 as the cut-off point to generate the binary depression symptoms variable.
2.3. Falls assessment
Falls were evaluated based on the following single item, “Have you ever fallen during the past 2 years?” In this study, falls were dichotomized as no falls vs. ≥1 falls. Then we used a question to assess the condition of fall injury “how many times have you fallen down seriously enough to need medical treatment?”
2.4. Covariates
Our covariates included sex, age, marital status, education level, personal annual income (CNY), residence, health insurance, self-rated health, self-rated eyesight, medication use, smoking, drinking, number of Non-Communicable Diseases (NCDs), sleep time, Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL).
Sex was divided into male and female. Age was divided into three groups: 60–69, 70–79, ≥80. Marital status was divided into two groups: married, others (merged with single, divorced, widowed). Education level was divided into four groups: illiterate, primary, middle, college or higher (Primary: primary school and junior high school; Middle: high school, technical secondary school, vocational school; College or higher: some college, junior college, college or higher.). Personal annual income was categorized into 0–15,000, 15,001–25,000, and >25,000 CNY (equals to 0–2,268, 2,269–3,781, >3782 US dollars in 2018). The residence was divided into rural and urban. Health insurance was divided into two groups: yes, no.
Self-rated health and self-rated eyesight were divided into good, fair, and poor. Smoking and drinking were categorized as current, former, and never. Medication use included antidepressants or tranquilizers and sleeping pills divided into two groups: yes and no. The number of Non-Communicable Diseases for each respondent was categorized as none, 1, 2, and ≥3 (Chronic diseases including hypertension, dyslipidemia, diabetes, cancer, chronic lung diseases, liver or gallbladder disease, heart disease, stroke, kidney disease, stomach or other digestive diseases, emotional, nervous, or psychiatric problems, memory-related disease, rheumatism or arthritis, asthma). People with depressive symptoms have a high prevalence of sleep disorders, while most falls occur during sleep (24). In this study, sleep time was assessed based on one question: “During the past month, how many hours of actual sleep did you get at night (average hours for one night, this may be shorter than the number of hours you spend in bed.)?” The ADL included six activities: dressing, bathing/showering, eating, getting in and out of bed, using the toilet, and bladder and bowel control (25, 26). The IADL included six activities: doing household chores, preparing meals, shopping, making phone calls, managing money, and taking medications (27, 28). For both ADL and IADL, answers were categorized as a four-point Likert scale: 1 (do not have any difficulty), 2 (have difficulty but can still do it), 3 (have difficulty and need help), or 4 (can not do it). ADL and IADL scores ranged from 6 to 24, from lowest to highest dependency.
2.5. Data analysis
Descriptive statistic methods were used to analyze the participants' characteristics; Chi-square test and student's t-test were used to compare the difference in categorical and continuous variables. Then, multivariate logistic regression was used to assess the association between falls and depressive symptoms among older adults, and the results were expressed as adjusted odds ratios (OR-adjusted) and their 95% confidence intervals (95% CI).
A classification and regression tree model was used to explore further the interactions between falls and depressive symptoms in older adults. The CHAID (chi-squared automatic interaction detector) algorithm was selected for the filter variables for the metric setting of the classification and regression tree model. The CHAID algorithm decided to branch on the data based on the p-value in the node chi-square test, selecting the independent variable that interacted most strongly with the dependent variable at each step and merging the categories of each independent variable if they were not statistically different from the dependent variable. This analysis method can intuitively reflect the sample characteristics and the proportion of different results occurring and find the optimal classification variables and results by comparing numerous classification rules. It provided a reference basis for subsequent covariate mergers and divisions, reduced the influence of human subjective factors, and also reflected the existence of interactions between covariates (29–32). Decision tree models were pruned by setting the number of layers and minimum sample size of parent and child nodes. In this study, the maximum growth depth of the decision tree was set to three layers according to the research needs. In order to prevent the number of samples on a tree node from being too small, the minimum sample size on the parent node was specified to be 400 in advance, the minimum sample size on the child node was specified to be 200, and if the number of samples on the node did not meet this requirement, this node was the terminal node, and no further splitting was performed.
All statistical analyses were performed using SPSS version 26.0 (SPSS, Chicago, Illinois, USA). The level of significance was set at P-values < 0.05.
3. Results
3.1. Basic information of the participants
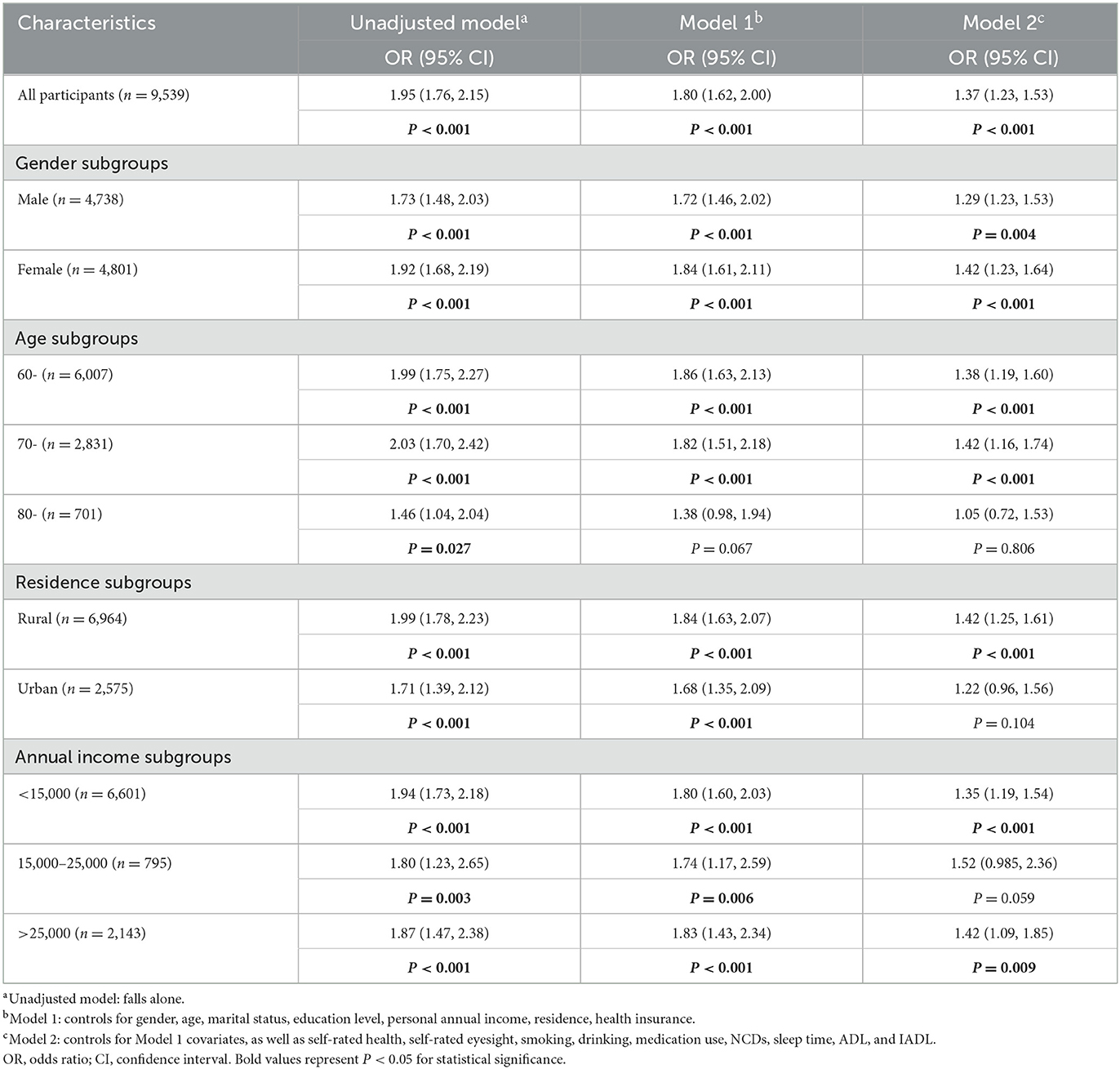
Table 1 provides the general characteristics of the participants in this study. Of the 9,539 participants, 3,235 had depressive symptoms, accounting for 33.9%. Generally speaking, the majority of older adults were female (50.3%), at the age of 60–69 (63.0%), married (80.3%), an illiterate education level (51.7%), personal annual income < 15,000 CNY (69.2%), residence in the rural (73.0%), with health insurance (97.2%), fair self-rated health (48.4%), bad self-rated eyesight (66.8%), never smoking (54.0%), never drinking (63.6%), no medication use (98.9%), no non-communicable chronic disease (52.9%), the average sleep time was 6.19 ± 2.05 h, ADL and IADL scores were 8.01 ± 2.70 and 7.58 ± 3.06, respectively. Among the participants, older adults were more likely to have depressive symptoms (all P < 0.05) if they were female (41.01%), marital status was other (41.44%), illiterate education level (40.91%), personal annual income < 15,000 CNY (38.33%), residence in rural areas (36.72%), without health insurance (40.98%), bad self-rated health (53.02%), bad self-rated eyesight (38.77%), never smoking (38.34%), former drinking (37.92%), used medication (83.7%), and had 3 or more chronic diseases (47.67%). Participants who were male (73.62%), married (67.93%), college or higher education level (88.18%), personal annual income more than 25,000 CNY (78.11%), residence in urban area (73.67%), with health insurance (66.29%), good self-rated health (81.96%), good self-rated eyesight (82.09%), current smoking (71.41%), current drinking (73.13%), no medication use (66.6%), no non-communicable chronic disease (71.29%) were less likely to have depressive symptoms (all P < 0.05). In addition, older adults with less sleep time (SD = 5.62 ± 2.17), lower ADL (SD = 7.85 ± 2.60), and higher IADL (8.61 ± 3.77) were more likely to have depressive symptoms (all P < 0.05).
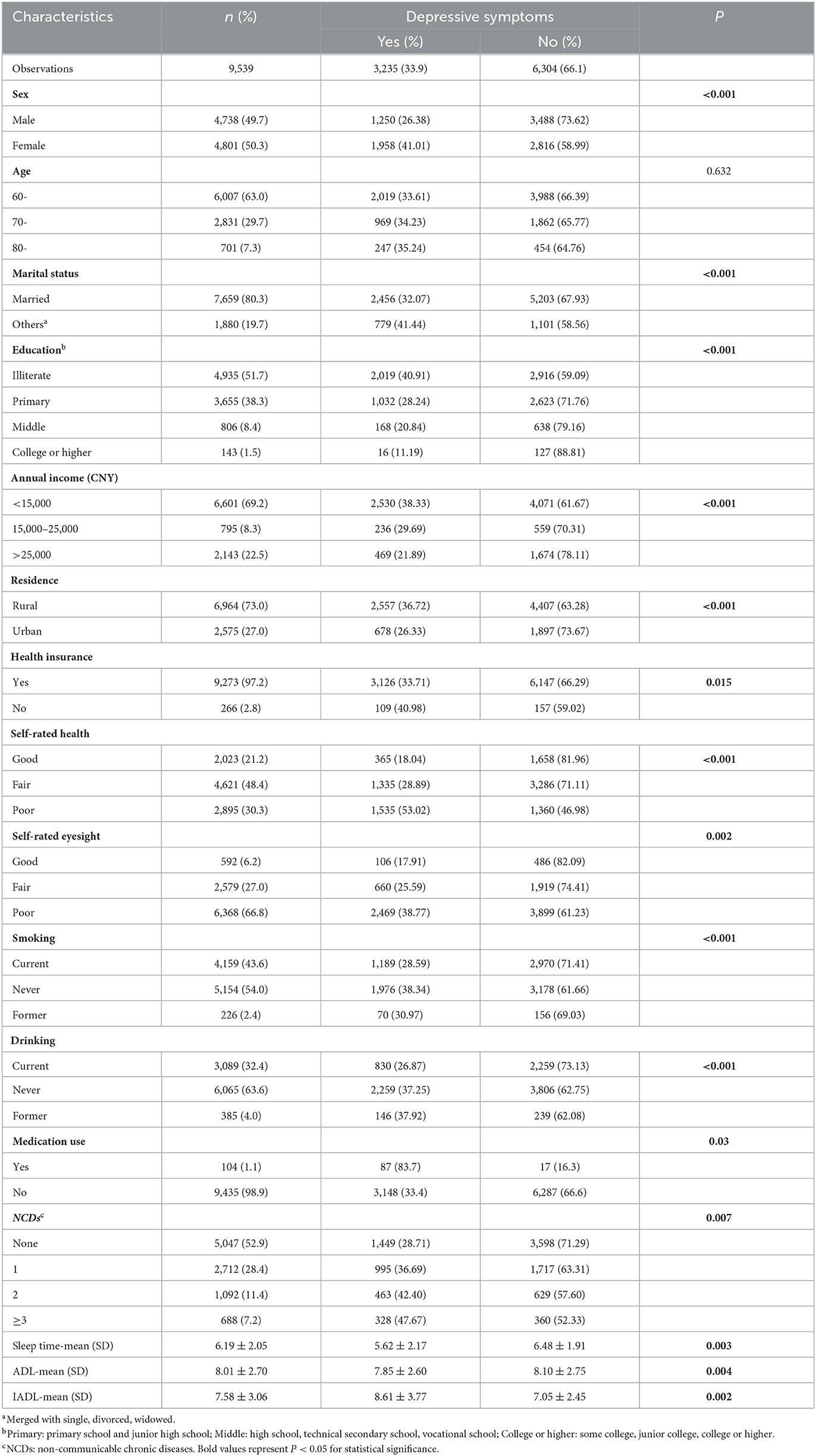
Table 1. Comparison of sample characteristics between depressive and non-depressive among older adults.
3.2. Prevalence of falls and medical treatment
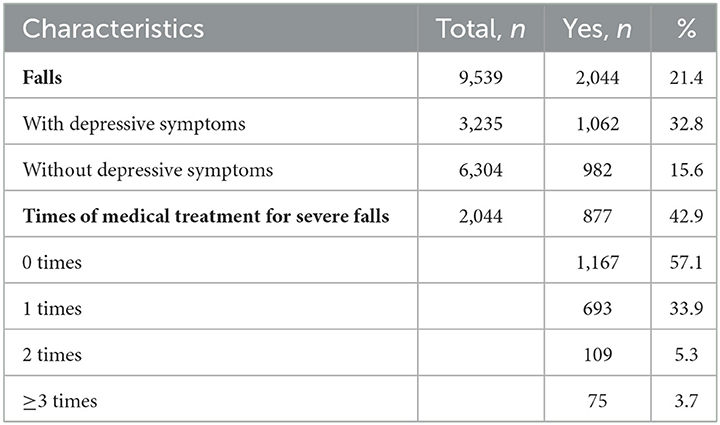
Table 2 illustrates the prevalence of falls and medical treatment. About the 9,539 participants, 2,044 participants have experienced falls, accounting for 21.4%. The falls prevalence of participants with and without depressive symptoms was 32.8 and 15.6%, respectively. Among older adults who had experienced falls, 42.9% had been medically treated for severe fall, with the percentages of 1 time, 2 times, and ≥3 times was 33.9, 5.3, and 3.7%, respectively.
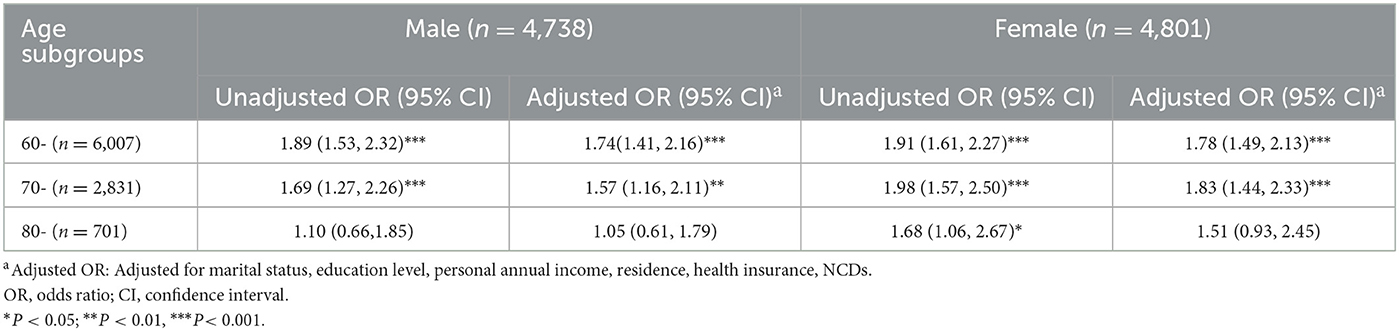
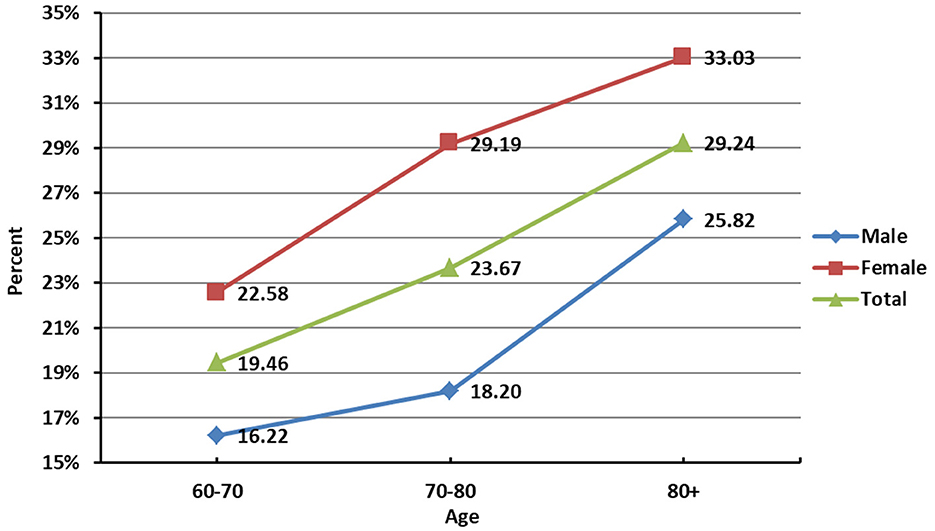
We found that older adults with depressive symptoms have higher rates of falls than those without depressive symptoms, the difference was statistically significant (P < 0.001). Further, the association between depressive symptoms and falls in older adults of different ages and genders subgroups was analyzed (Table 3), and significant associations were found in male at age 60- (OR = 1.74, 95% CI: 1.41, 2.16), 70- (OR = 1.57, 95% CI: 1.16, 2.11), and female at age 60- (OR = 1.78, 95% CI: 1.49, 2.13), 70- (OR = 1.83, 95% CI: 1.44, 2.33). As shown in Figure 2 increases with age, and the fall rate of females was higher than that of males in the same age group.
3.3. Falls and depressive symptoms
In Table 4, we used three sets of logistic regression models (unadjusted model, model 1, and model 2) to examine the associations between falls and depressive symptoms, more detailed results of the logistic regression analysis were presented in the second part of the Supplementary material. After being adjusted with gender, age, marital status, education level, personal annual income, residence, and health insurance (model 1), the result shows that falls (OR = 1.80, 95% CI: 1.62, 2.00) were associated with depressive symptoms. In Model 2, although the OR value (OR = 1.37, 95% CI: 1.23, 1.53) becomes lower after being adjusted with all of the covariates, the existence of the association between falls and depressive symptoms can still be shown.
Regarding the subgroups divided according to gender, significant associations were found for both male (OR = 1.29, 95% CI: 1.23, 1.53) and female (OR = 1.42, 95% CI: 1.23, 1.64) subgroups. Moreover, the ORs of female subgroup were higher than that of the male in all models; The OR value of the age subgroup of the 70–79 (OR = 1.42, 95% CI: 1.16, 1.74) people was higher than that of the 60–69 (OR = 1.38, 95% CI: 1.19, 1.60) people in all models, but the OR value in ≥80 people did not show a significant association; Also, the OR values of the subgroups by place of residence showed that only the rural (OR = 1.42, 95% CI: 1.25, 1.61) had statistically significant ORs; In the subgroup of annual income, personal annual income < 15,000 CNY (OR = 1.35, 95% CI: 1.19, 1.54) and more than 25,000 CNY (OR = 1.42, 95% CI: 1.09, 1.85) showed a statistically significant association.
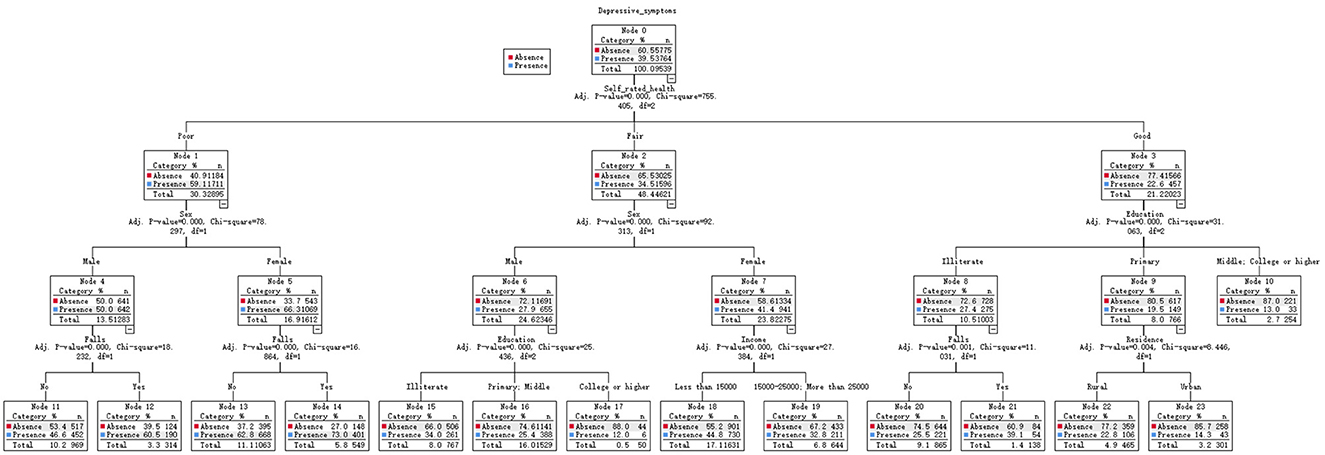
3.4. CART model analysis
As shown in Figure 3, the interaction between falls and depressive symptoms in older adults was analyzed using the CATR model, which contains 3 depths, 23 nodes, and 12 terminal nodes, the p-values of the chi-square test for all nodes met the criteria (P < 0.001). The CART model analysis found that depressive symptoms in older adults were mainly related to falls, gender, education, annual income, residence, and self-rated health. In this model, self-rated health was the first split factor, the second level was split at gender and education, and the end nodes of the model were falls, education, income, and residence. For those older adults with depressive symptoms, self-rated good health (node 3) and degree of illiterate (node 8), the possibility (39.1%) of falls (node 21) was lowest. Conversely, for those with poor self-rated health (node 1), female gender (node 5), the possibility (73.0%) of falls (node 14) was the highest.
4. Discussion
This study aimed to explicitly investigate the association between falls and depressive symptoms in the older adults in China while focusing on whether an interaction exists between falls, depressive symptoms, and demographic characteristics based on the nationally representative sample of the older adults in China. When we adjusted for possible confounders, the associations between falls and depressive symptoms remained, although the strength of the association was reduced. Further subgroup analysis found statistically significant associations between falls and depressive symptoms among males, female, 60–69 aged, 70–79 aged, <15,000 CNY, and more than 25,000 CNY in the personal annual income subgroups.
This study found that the prevalence of falls in older adults was 21.4%, lower than those found in other studies focusing on other countries' older adults, such as 31% in the United States (33), 25.6% in Australia (34), 20–30% in Canada (35) and 27.6% in Brazil (36). This difference may be related to the age grouping and the time frame of the measurement. We also found that the rate of falls in older adults increased with age, with females having a higher rate of falls than males in the same age group, consistent with previous research findings (37, 38). The prevalence of depressive symptoms among older adults in this study was 33.9%, which was higher than that in the United States (23.97%) (4), South Korea (16.08%) (5), and Singapore (7.8%) (6). Due to different cultural backgrounds, environment and application measures, and methodological differences (including the screening scale used and the cut-off point adopted), differences in depressive symptoms between countries should be compared with caution.
Several studies have analyzed the relationship between falls and depressive symptoms, and our findings further confirm this result (39–41). A cross-sectional analysis of 1,261 community-dwelling older adults showed a significant association between depressive symptoms and falls (42). In several prospective studies, depressive symptoms have been identified as a risk factor for falls (14, 43, 44). A meta-analysis of 20 prospective studies found that depressive symptoms in older adults were a risk factor for falls, regardless of how depressive symptoms and falls were measured, as well as different follow-up times and statistical methods (45). A 2-year follow-up cohort study showed that depressive symptoms significantly increased the risk of unexplained falls and the association with accidental falls was only close to borderline significance (12). Despite this, the mechanism for this relationship remains unclear. One possible mechanism is that depressive symptoms are often associated with greater physical impairment and cognitive deficits (46, 47). Another possible mechanism is that antidepressants affect attention, gait, balance, and blood pressure regulation (48). Besides, fear of falling is another critical factor in the case of older adults. Fear of falling has been related to anxiety and symptoms of depression, which may mediate the relationship between physical and cognitive factors, depressive symptoms, and falls (49, 50).
In our study, we found a significant association between depressive symptoms and falls among the Chinese older adults population, as well as specific subgroups. This finding may indicated a potential association between falls and depressive symptoms among the older adults. Subgroup analysis showed an association between falls and depressive symptoms in 60–69, 70–79 aged, while this association was not significant in those over 80 aged. One possible reason for this is the reduced mobility and physical activity of older adults with increasing age, reducing the chances of falls (51–53). Interestingly, after controlling for health-related factors, subgroups by place of residence showed no statistically significant association for urban older adults, with only those living in rural areas confirming the association. In China, medical conditions, economic conditions and living facilities in rural areas are inferior to those in urban areas. Compared to rural older adults, urban older adults have access to high-quality and timely preventive care and medical services when needed, and these differences may have a direct or indirect effect on falls and depressive symptoms in older adults (54–56). Besides, in a subgroup analysis of income, we found a statistically significant relationship between falls and depressive symptoms in older adults with annual incomes < 15,000 CNY and >25,000 CNY, while the relationship approached borderline significance for those in the 15,000–25,000 CNY income subgroup. It has been argued that financial income makes older adults feel more secure in their financial independence, reduces poverty-related stress, and trades off health-generating resources such as health care and better housing conditions (57, 58). More and more evidence suggests that older adults with low socioeconomic status are vulnerable to developing falls and depressive symptoms (59, 60). Since cross-sectional data were used, our analysis cannot examine causality and more research needs to be conducted further to analyze the relationship between income levels and them.
Our study investigated the association between falls and depressive symptoms and related demographic characteristics in an older Chinese population based on a national sample. The CART model was used to explore further the interactions between falls and depressive symptoms and its demographic variables. This study found that older adults with depressive symptoms, self-rated good health and degree of illiterate, the possibility of falls was lowest. Meanwhile, for those with poor self-rated health, female gender, the possibility of falls was the highest. The CART model can analyze non-linear and highly correlated data without pre-processing, it can visualize the importance of early warning indicators and their interactions, which is represented in the form of a tree diagram. By using the CART model, we conducted a more in-depth analysis of the data results on the relationship between depressive symptoms and falls in older adults, identifying people at risk for different characteristics by percentage. This study further explored the relationship between falls and depressive symptoms in older adults using data from a large sample. Further subgroup analyses found that the association between falls and depressive symptoms did not hold for older adults over 80 years and residents in urban after controlling for relevant covariates. The CART analysis found that older adults with depressive symptoms, poor self-rated health, and females had the highest probability of falling. This study enriched related studies and have some clinical and research implications. Furthermore, the findings related to falls and depressive symptoms in older adults may provide some rationale and support for implementing measures such as risk monitoring, screening for depressive symptoms, and early prevention in high-risk older adult populations.
This study has several limitations as follows. Firstly, study data were obtained through participant self-reports, which are inevitably biased. Secondly, this study is an analysis based on cross-sectional data, and we can only demonstrate an association between falls and depressive symptoms in older adults. The conclusion of causality needs to be proven by further studies. Thirdly, we control for relevant covariates in our analysis, but there is still a portion of unknown factors that we cannot exclude. Although we adjusted for the use of the medication, information regarding the dose, dosing schedule, adherence and start of treatment was not available, which may have led to some bias.
5. Conclusion
This cross-sectional study provides evidence of the significant association between falls and depressive symptoms in older Chinese adults, and subgroup analyses further demonstrated differences in the relationship across age, residence, and income groups. The probability of falls was highest among older adults with depressive symptoms who self-rated poor health and female gender. The findings provide some evidence and support for risk monitoring, screening for depressive symptoms, and early prevention in the high-risk older population.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://charls.charlsdata.com/pages/Data/2018-charls-wave4/en.html.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ZF and XH: conceptualization, methodology, and writing—review and editing. ZF and QC: software, formal analysis, resources, data curation, and writing—original draft preparation. ZF, YL, and ZX: validation and investigation. XH: supervision, project administration, and funding acquisition. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the National Natural Science Foundation of China (71774034) and National Key Research and Development Program of China (2018YFC2002600).
Acknowledgments
The authors are grateful to the National School of Development of Peking University for providing the data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1248551/full#supplementary-material
References
1. Tinetti ME. Preventing falls in elderly persons — NEJM. N Engl J Med. (2003) 348:1816–8. doi: 10.1056/NEJM200305013481819
2. Stel VS, Smit JH, Pluijm SM, Lips P. Consequences of falling in older men and women and risk factors for health service use and functional decline. Age Ageing. (2004) 33:58–65. doi: 10.1093/ageing/afh028
3. Soriano TA, DeCherrie LV, Thomas DC. Falls in the community-dwelling older adult: a review for primary-care providers. Clin Interv Aging. (2007) 2:545–54. doi: 10.2147/CIA.S1080
4. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. (2013) 75:51–61. doi: 10.1016/j.maturitas.2013.02.009
5. Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. (1997) 337:1279–84. doi: 10.1056/NEJM199710303371806
6. Tinetti ME, Williams CS. The effect of falls and fall injuries on functioning in community-dwelling older persons. J Gerontol A Biol Sci Med Sci. (1998) 53:M112–9. doi: 10.1093/gerona/53A.2.M112
7. Kannus P, Parkkari J, Koskinen S, Niemi S, Palvanen M, Järvinen M, et al. Fall-induced injuries and deaths among older adults. JAMA. (1999) 281:1895–9. doi: 10.1001/jama.281.20.1895
8. Rizzo JA, Friedkin R, Williams CS, Nabors J, Acampora D, Tinetti ME. Health care utilization and costs in a Medicare population by fall status. Med Care. (1998) 36:1174–88. doi: 10.1097/00005650-199808000-00006
9. Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet. (2007) 369:1302–13. doi: 10.1016/S0140-6736(07)60368-7
10. Depression W. Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization (2017). p. 1–24.
11. Ustün TB, Ayuso-Mateos JL, Chatterji S, Mathers C, Murray CJ. Global burden of depressive disorders in the year 2000. Br J Psychiatry. (2004) 184:386-92. doi: 10.1192/bjp.184.5.386
12. Briggs R, Kennelly SP, Kenny RA. Does baseline depression increase the risk of unexplained and accidental falls in a cohort of community-dwelling older people? Data from The Irish Longitudinal Study on Ageing (TILDA). Int J Geriatr Psychiatry. (2018) 33:e205–11. doi: 10.1002/gps.4770
13. Eggermont LHP, Penninx BWJH, Jones RN, Leveille SG. Depressive symptoms, chronic pain, and falls in older community-dwelling adults: the MOBILIZE Boston Study. J Am Geriatr Soc. (2012) 60:230–7. doi: 10.1111/j.1532-5415.2011.03829.x
14. Kvelde T, Lord SR, Close JCT, Reppermund S, Kochan NA, Sachdev P, et al. Depressive symptoms increase fall risk in older people, independent of antidepressant use, and reduced executive and physical functioning. Arch Gerontol Geriatr. (2015) 60:190–5. doi: 10.1016/j.archger.2014.09.003
15. Chen X, Lin S, Zheng Y, He L, Fang Y. Long-term trajectories of depressive symptoms and machine learning techniques for fall prediction in older adults: Evidence from the China Health and Retirement Longitudinal Study (CHARLS). Arch Gerontol Geriatr. (2023) 111:105012. doi: 10.1016/j.archger.2023.105012
16. Song J, Wu X, Zhang Y, Song P, Zhao Y. Association between changes in depressive symptoms and falls: the China health and retirement longitudinal study (CHARLS). J Affect Disord. (2023) 341:393–400. doi: 10.1016/j.jad.2023.09.004
17. Zhang Y, Zhang L, Zhang X, Sun J, Wang D, Chen G. Fall injuries and depressive symptoms among older adults and the mediating effects of social participation - China, 2011-2018. China CDC Wkly. (2021) 3:837–41. doi: 10.46234/ccdcw2021.207
18. Wang J, Li S, Hu Y, Ren L, Yang R, Jiang Y, et al. The moderating role of psychological resilience in the relationship between falls, anxiety and depressive symptoms J Affect Disord. (2023) 341:211–8. doi: 10.1016/j.jad.2023.08.060
19. Ouyang P, Sun W. The association between depressive symptoms and fall accidents among middle-aged and elderly people in China. Environ Health Prev Med. (2018) 23:42. doi: 10.1186/s12199-018-0735-y
20. Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
21. Boey KW. Cross-validation of a short form of the CES-D in Chinese elderly. Int J Geriatr Psychiatry. (1999) 14:608–17. doi: 10.1002/(SICI)1099-1166(199908)14:8<608::AID-GPS991>3.0.CO;2-Z
22. Cheng HG, Chen S, McBride O, Phillips MR. Prospective relationship of depressive symptoms, drinking, and tobacco smoking among middle-aged and elderly community-dwelling adults: results from the China Health and Retirement Longitudinal Study (CHARLS). J Affect Disord. (2016) 195:136–43. doi: 10.1016/j.jad.2016.02.023
23. Li LW, Liu J, Zhang Z, Xu H. Late-life depression in Rural China: Do village infrastructure and availability of community resources matter? Int J Geriatr Psychiatry. (2015) 30:729–36. doi: 10.1002/gps.4217
24. Chang KJ, Son SJ, Lee Y, Back JH, Lee KS, Lee SJ, et al. Perceived sleep quality is associated with depression in a Korean elderly population. Arch Gerontol Geriatr. (2014) 59:468–73. doi: 10.1016/j.archger.2014.04.007
25. Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged the index of ADL: a standardized measure of biological and psychosocial function. JAMA. (1963) 185:914–9. doi: 10.1001/jama.1963.03060120024016
26. Qiao Y, Liu S, Li G, Lu Y, Wu Y, Shen Y, et al. Longitudinal follow-up studies on the bidirectional association between ADL/IADL disability and multimorbidity: results from two national sample cohorts of middle-aged and elderly adults. Gerontology. (2021) 67:563–71. doi: 10.1159/000513930
27. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. (1969) 9:179–86. doi: 10.1093/geront/9.3_Part_1.179
28. Qian J, Ren X. Association between comorbid conditions and BADL/IADL disability in hypertension patients over age 45: based on the China health and retirement longitudinal study (CHARLS). Medicine. (2016) 95:e4536. doi: 10.1097/MD.0000000000004536
29. Song YY, Lu Y. Decision tree methods: applications for classification and prediction. Shanghai Arch Psychiatry. (2015) 27:130–5.
30. Atieh MA, Pang JK, Lian K, Wong S, Tawse-Smith A, Ma S, et al. Predicting peri-implant disease: chi-square automatic interaction detection (CHAID) decision tree analysis of risk indicators. J Periodontol. (2019) 90:834–46. doi: 10.1002/JPER.17-0501
31. Díaz-Pérez FM, García-González CG, Fyall A. The use of the CHAID algorithm for determining tourism segmentation: a purposeful outcome. Heliyon. (2020) 6:e04256. doi: 10.1016/j.heliyon.2020.e04256
32. Gunduz M, Lutfi HM. Go/no-go decision model for owners using exhaustive CHAID and QUEST decision tree algorithms. Sustainability. (2021) 13:815. doi: 10.3390/su13020815
33. Stevens JA, Mack KA, Paulozzi LJ. Self-reported falls MF and fall-related injuries among persons aged? 65 years-United States, 2006. J Safety Res. (2008) 39:345–9. doi: 10.1016/j.jsr.2008.05.002
34. Milat AJ, Watson WL, Monger C, Barr M, Giffin M, Reid M. Prevalence, circumstances and consequences of falls among community-dwelling older people: results of the 2009 NSW Falls Prevention Baseline Survey. NSW Public Health Bull. (2011) 22:43–8. doi: 10.1071/NB10065
35. Stinchcombe A, Kuran N, Powell S. Report summary. Seniors' falls in Canada: second report: key highlights. Chronic Dis Inj Can. (2014) 34:171–4. doi: 10.24095/hpcdp.34.2/3.13
36. Siqueira FV, Facchini LA, da Silveira DS, Piccini RX, Tomasi E, Thumé E, et al. Prevalence of falls in elderly in Brazil: a countrywide analysis. Cad Saude Publica. (2011) 27:1819–26. doi: 10.1590/S0102-311X2011000900015
37. Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj Prev. (2006) 12:290–5. doi: 10.1136/ip.2005.011015
38. Wu H, Ouyang P. Fall prevalence, time trend and its related risk factors among elderly people in China. Arch Gerontol Geriatr. (2017) 73:294–9. doi: 10.1016/j.archger.2017.08.009
39. Launay C, De Decker L, Annweiler C, Kabeshova A, Fantino B, Beauchet O. Association of depressive symptoms with recurrent falls: a cross-sectional elderly population based study and a systematic review. J Nutr Health Aging. (2013) 17:152–7. doi: 10.1007/s12603-012-0370-z
40. Brito TA, Coqueiro Rda S, Fernandes MH, de Jesus CS. Determinants of falls in community-dwelling elderly: hierarchical analysis. Public Health Nurs. (2014) 31:290–7. doi: 10.1111/phn.12126
41. Grenier S, Payette M-C, Langlois F, Vu TTM, Bherer L. Depressive symptoms are independently associated with recurrent falls in community-dwelling older adults. Int Psychogeriatr. (2014) 26:1511–9. doi: 10.1017/S104161021400074X
42. Wada T, Ishine M, Ishimoto Y, Hirosaki M, Kimura Y, Kasahara Y, et al. Community-dwelling elderly fallers in Japan are older, more disabled, and more depressed than nonfallers, J Am Geriatr Soc. (2008) 56:1570–1. doi: 10.1111/j.1532-5415.2008.01762.x
43. Quach L, Yang FM, Berry SD, Newton E, Jones RN, Burr JA, et al. Depression, antidepressants, and falls among community-dwelling elderly people: the MOBILIZE Boston study. J Gerontol A Biol Sci Med Sci. (2013) 68:1575–81. doi: 10.1093/gerona/glt084
44. Stubbs B, Stubbs J, Gnanaraj SD, Soundy A. Falls in older adults with major depressive disorder (MDD): a systematic review and exploratory meta-analysis of prospective studies. Int Psychogeriatr. (2016) 28:23–9. doi: 10.1017/S104161021500126X
45. Kvelde T, McVeigh C, Toson B, Greenaway M, Lord SR, Delbaere K, et al. Depressive symptomatology as a risk factor for falls in older people: systematic review and meta-analysis. J Am Geriatr Soc. (2013) 61:694–706. doi: 10.1111/jgs.12209
46. Kerse N, Flicker L, Pfaff JJ, Draper B, Lautenschlager NT, Sim M, et al. Falls, depression and antidepressants in later life: a large primary care appraisal. PLoS ONE. (2008) 3:e2423. doi: 10.1371/journal.pone.0002423
47. Zhao D, Li J, Fu P, Hao W, Yuan Y, Yu C, et al. What role does activity engagement play in the association between cognitive frailty and falls among older adults? Evidence from Rural Shandong, China. Gerontology. (2020) 66:593–602. doi: 10.1159/000510639
48. Darowski A, Chambers SA, Chambers DJ. Antidepressants and falls in the elderly. Drugs Aging. (2009) 26:381–94. doi: 10.2165/00002512-200926050-00002
49. Delbaere K, Crombez G, Vanderstraeten G, Willems T, Cambier D. Fear-related avoidance of activities, falls and physical frailty A prospective community-based cohort study. Age Ageing. (2004) 33:368–73. doi: 10.1093/ageing/afh106
50. van Haastregt JC, Zijlstra GA, van Rossum E, van Eijk JT, Kempen GI. Feelings of anxiety and symptoms of depression in community-living older persons who avoid activity for fear of falling Am J Geriatr Psychiatry. (2008) 16:186–93. doi: 10.1097/JGP.0b013e3181591c1e
51. Buchman AS, Wilson RS, Yu L, James BD, Boyle PA, Bennett DA. Total daily activity declines more rapidly with increasing age in older adults. Arch Gerontol Geriatr. (2014) 58:74–9. doi: 10.1016/j.archger.2013.08.001
52. Lin SF, Beck AN, Finch BK, Hummer RA, Masters RK. Trends in US older adult disability: exploring age, period, and cohort effects. Am J Public Health. (2012) 102:2157–63. doi: 10.2105/AJPH.2011.300602
53. Lopes PB, Rodacki ALF, Wolf R, Fisher K, Bento PCB, Pereira G. Can age influence functional tests differently to predict falls in nursing home and community-dwelling older adults? Exp Aging Res. (2021) 47:192–202. doi: 10.1080/0361073X.2020.1871277
54. Zhang X, Dupre ME, Qiu L, Zhou W, Zhao Y, Gu D. Urban-rural differences in the association between access to healthcare and health outcomes among older adults in China. BMC Geriatr. (2017) 17:151. doi: 10.1186/s12877-017-0538-9
55. Koyanagi A, Moneta MV, Garin N, Olaya B, Ayuso-Mateos JL, Chatterji S, et al. The association between obesity and severe disability among adults aged 50 or over in nine high-income, middle-income and low-income countries: a cross-sectional study. BMJ Open. (2015) 5:e007313. doi: 10.1136/bmjopen-2014-007313
56. You X, Zhang Y, Zeng J, Wang C, Sun H, Ma Q, et al. Disparity of the Chinese elderly's health-related quality of life between urban and rural areas: a mediation analysis. BMJ Open. (2019) 9:e024080. doi: 10.1136/bmjopen-2018-024080
57. Anderson NB, Armstead CA. Toward understanding the association of socioeconomic status and health: a new challenge for the biopsychosocial approach. Psychosom Med. (1995) 57:213–25. doi: 10.1097/00006842-199505000-00003
58. Liu M, Zhang Q, Lu M, Kwon C-S, Quan H. Rural and urban disparity in health services utilization in China. Med Care. (2007) 45:767–74. doi: 10.1097/MLR.0b013e3180618b9a
59. Trujillo AJ, Puvanachandra P, Hyder AA. Individual income and falls among the elderly in Latin America. Geriatr Gerontol Int. (2011) 11:180–90. doi: 10.1111/j.1447-0594.2010.00662.x
Keywords: depressive symptoms, falls, older adults, China, CART
Citation: Feng Z, Chen Q, Li Y, Xue Z and Hao X (2023) The association between falls and depressive symptoms among older adults: evidence from the China Health and Retirement Longitudinal Study. Front. Public Health 11:1248551. doi: 10.3389/fpubh.2023.1248551
Received: 27 June 2023; Accepted: 10 October 2023;
Published: 30 October 2023.
Edited by:
Madia Lozupone, University of Bari Aldo Moro, ItalyCopyright © 2023 Feng, Chen, Li, Xue and Hao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoning Hao, eG5oYW81NDIxQDE2My5jb20=
 Zhiqiang Feng1,2
Zhiqiang Feng1,2 Xiaoning Hao
Xiaoning Hao