- Department of Philosophy, University of Bergen, Bergen, Norway
Background: There are well-established literatures documenting the associations between mental disorders and unhealthy behaviors such as poor diet quality, sedentary behavior, and cannabis and tobacco use. Few studies have attempted to understand the respective findings in light of each other, however.
Objective: The purpose of this review was to assemble comparable data for each behavior-disorder association and assess the associations in terms of their overall strength. The review aimed to include a representative, but not exhaustive, range of studies that would allow for explorative comparisons.
Methods: Eligible studies were identified via Pubmed searches and citation searching, restricted to publications no older than 2015 written in English. To obtain comparable data, only studies that reported findings as odds ratios were included, and risk of bias related to study samples, behavioral measurement disparities, and control variables was assessed via sensitivity analyses. Findings for each disorder were compared on the basis of different measures of central tendency.
Results: From 3,682 records, 294 studies were included. The review found evidence of associations between each of the four unhealthy behaviors and psychosis, depression, anxiety, bipolar disorder, attention-deficit/hyperactivity disorder (ADHD), and post-traumatic stress disorder (PTSD), while personality disorder was only investigated in relation to cannabis and tobacco use. In overall comparison, the associations were generally of similar strength, and only the association between cannabis use and personality disorder was exceptional in terms of being significantly stronger than its counterparts across disorders and across behaviors. Analyses of bias risk identified some influence from behavioral measurement disparities and lack of adequate statistical control, but findings were generally robust across a range of sensitivity analyses.
Conclusion: This explorative and comparative review found that poor diet quality, sedentary behavior, and cannabis and tobacco use are about equally strongly associated with a range of different mental disorders. Given the general nature of these associations, we should probably understand them to reflect a general and shared etiology. However, the findings in this review should be regarded as tentative until confirmed by more comprehensive investigations.
Highlights
• In terms of mental disorder, moderate cannabis use appears to be about as harmful as moderate tobacco use.
• In terms of mental disorder, moderate cannabis use appears to be about as harmful as watching TV for more than 2–4 h per day or eating fast food and drinking sugary beverages every day.
• The association between cannabis use and psychosis is not stronger than the associations between cannabis use and other mental disorders.
• The association between psychosis and cannabis use is not stronger than the associations between psychosis and poor diet quality, sedentary behavior, or tobacco use.
Introduction
Associations between unhealthy behaviors and mental disorders are well established in research literature. This review considers four different unhealthy behaviors—cannabis use, tobacco use, sedentary behavior, and poor diet quality—and a range of mental disorders across the range from common mental disorders (CMDs) to serious mental illnesses (SMIs) and including both internalizing and externalizing disorders. Aiming for a broad but not exhaustive range of disorders that can provide a convincing basis for comparison, the seven disorders psychosis, depression, anxiety, bipolar disorder, personality disorder, attention deficit/hyperactivity disorder (ADHD), and post-traumatic stress disorder (PTSD) were included in the review.
Psychosis
Several recent reviews have confirmed an association between psychosis and cannabis use (1–6), while a few have failed to identify a statistically significant relationship (7, 8). The strength of associations identified in meta-analyses ranged from strong for the most severe cannabis users [(5): OR 3.90] to moderate [(8): OR 1.786; (3): RR 1.71; (4): OR 1.75 for abuse/dependence; (5): OR 1.97 for any use] or weak [(7): RR 1.11; (4): OR 1.14 for lifetime use]. Several recent reviews have also confirmed an association between psychosis and tobacco use (8–11), with the strength of the association ranging from moderate to strong in meta-analyses (respectively, OR 2.22, 3.04, 3.22/2.18 for case-control/prospective studies, and RR 1.99). One review did not find evidence of any significant association (12). Those reviews that have compared the strength of the relationship between cannabis and psychosis to that between tobacco and psychosis have found that the latter appears to be somewhat stronger (8, 13). The associations between psychosis and poor diet quality or sedentary behavior have not been extensively studied, although reviews have suggested that people with psychosis tend to have poor diet quality (14, 15) and low levels of physical activity (16, 17).
Depression
A number of recent review articles support an association between cannabis use and depression, although with some mixed results (12, 18–28), while one found that the relationship is unclear (29). The meta-analysis by Onaemo et al. (26) identified a strong association between cannabis use disorder and major depression (OR 3.22), while those by Esmaeelzadeh et al. (18) and Gobbi et al. (19) as well as an earlier meta-analysis by Lev-Ran et al. (30) identified a weak to moderate association (respectively, OR 1.29, 1.37 and 1.62) for overall cannabis use.
For tobacco, recent reviews by Weinberger et al. (31) and Fluharty et al. (32) confirmed that people with depression are more likely to smoke and to meet criteria for nicotine dependence, with the latter also indicating that smoking may lead to depression. A meta-analysis by Esmaeelzadeh et al. (18) found that the association between tobacco use and depression was moderately strong with an OR of 1.65, which was stronger than that for the corresponding association between cannabis use and depression. Another meta-analysis by Groenman et al. (33) found that childhood depression was a risk factor for subsequent nicotine use disorder (OR 2.56). Reviews by Zeng and Li (34) and Han et al. (35) also confirmed that secondhand smoking is associated with depression, with their meta-analyses obtaining ORs of 1.60 and 1.32, respectively. Furthermore, recent reviews have also indicated that e-cigarette use is associated with depression (36, 37).
There are also a number of reviews supporting associations between depression and sedentary behavior (17, 38–47) and poor diet quality (48–57), although with some mixed results. In meta-analyses, the associations were weak to moderate in strength, with RR 1.42 (47) and RR 1.25 (46) for overall sedentary behavior, OR 1.28 (45) and OR 1.12 (42) for screen time, RR 1.18 for TV viewing (41), OR 1.44 for ultra-processed food consumption (49), RR 1.25 (58) and RR 1.31 (48) for sugar-sweetened beverage consumption, OR 1.18 for western-style unhealthy dietary pattern (59), and OR 1.62 (52) and OR 1.11 (54) for fast/junk food.
Anxiety
Some reviews have identified an association between cannabis use and anxiety (18, 20, 26, 27, 60–62), although others have maintained that the relationship is unclear (19, 22, 28, 29, 63, 64). In meta-analyses, moderate to strong associations were identified between cannabis use disorder and anxiety [(60): OR 1.68; (26): OR 2.99], while the associations for overall use were generally weak [(18): OR 1.36; (19): OR 1.18; (60): OR 1.24; (61): OR 1.15; (62): OR 1.25]. Reviews have also identified an association between tobacco use and anxiety (12, 18, 65–67), although with some mixed results. A meta-analysis by Esmaeelzadeh et al. (18) found a strong association between tobacco use and anxiety with an OR of 2.21, which was stronger than that for the corresponding association between cannabis use and anxiety.
Reviews have also found evidence of an association between anxiety and sedentary behavior (68–71) and poor diet quality (49, 52). Associations in meta-analyses were of weak to moderate strength, with regular physical activity reducing the odds for anxiety [(72): OR 0.54; (70): OR 0.74] and sedentary behavior [(68): OR 1.48], ultra-processed food [(49): OR 1.48] and junk food [(52): OR 1.24] increasing the odds for anxiety.
Bipolar disorder
The relationship between cannabis use and bipolar disorder has not been intensively studied, but a number of reviews have suggested a positive association (20, 23, 25, 73–78). Meta-analyses by Gibbs et al. [(73): OR 2.97] and Hunt et al. [(74): OR 2.35] identified a strong association between cannabis use disorder and bipolar disorder. Some reviews have also suggested an association between tobacco use and bipolar disorder (75, 79), although the evidence is mixed (12). Nevertheless, the meta-analysis by Jackson et al. (79) identified a strong association with an OR of 3.5. Reviews have also identified tentative associations between bipolar disorder and sedentary behavior (17, 80, 81) and diet quality (82, 83), but there are few available studies.
Personality disorders
While the association between personality disorders and general substance use is well established, the evidence specifically for cannabis (20, 28, 84–86) and tobacco (12, 87) is quite limited. Similarly, the research into the relationships between personality disorders and sedentary behavior and diet quality is very limited (87, 88).
Attention-deficit/hyperactivity disorder
ADHD is commonly diagnosed in childhood, and most studies investigating the relationship between the disorder and substance use focus on ADHD as a risk factor for subsequent substance use. For cannabis, meta-analyses have found strong associations between childhood ADHD and regular [(89): OR 2.45] and lifetime use [(90): OR 2.78] as well as a moderate association for abuse or dependence [(90): OR 1.58]. For tobacco, meta-analyses similarly identified childhood ADHD as a strong risk factor both for subsequent nicotine use [(89) OR 2.16; (90): OR 2.08] and nicotine dependence or use disorder [(33): OR 2.52; (90): OR 2.82]. The evidence for e-cigarette use is very limited (36).
Reviews have also supported associations between ADHD and sedentary behavior (91–95) and diet quality (96–99). Meta-analyses of sedentary behavior found moderate to strong associations between electronic media use and ADHD [(91): OR 1.94; (92): 2.597], while meta-analyses of diet quality found weak to strong associations for sugar and soft drink consumption [(97): pooled effect size 1.22], junk food [(99): OR 1.51], and general unhealthy diets [(96): OR 1.41; (98): OR 2.24].
Post-traumatic stress disorder
Reviews have identified an association between cannabis use and PTSD (100, 101) and investigated the potential for therapeutic use (102–104). Reviews have also identified an association between tobacco use and PTSD (105–109), with one meta-analysis by van den Berk-Clark et al. (109) finding a strong association (OR 2.13) for unadjusted studies and a weak association (OR 1.22) for a single adjusted study. The evidence for e-cigarette use is very limited (36).
Furthermore, reviews have suggested that both sedentary behavior and poor diet quality are associated with PTSD, although with some mixed results (70, 109–111). In meta-analyses, high physical activity was moderately protective against PTSD [(70): OR 0.57], while PTSD in turn was a weak risk factor for low physical activity [(109): OR 0.91 for adjusted studies and OR 0.69 for unadjusted studies]. The meta-analysis by van den Berk-Clark et al. (109) on diet quality was somewhat unclear, as four unadjusted studies predicted a healthier diet (OR 1.25) while a single adjusted study predicted a less healthy diet (OR 0.95).
While these reviews indicate a broad range of associations between unhealthy behaviors and mental disorders, they also demonstrate that such associations have not often been understood in relation to each other across various behaviors and disorders, which would allow for both a calibration of their relative importance and a widened perspective on their etiology. Instead, individual associations are usually analyzed and discussed in isolation, which encourages the perspective that the association under scrutiny is unique and reflects a particular and individual etiology. Should it be true that the range of disorders here under scrutiny are generally associated with a range of unhealthy behaviors related to diet, exercise, and licit and illicit substance use, however, it might seem unlikely that these parallel associations are best understood in isolation from one another. If the association between a given behavior and a given mental disorder has parallels across a range of disorders and behaviors, its lack of specificity indicates that the association probably does not reflect a causal effect from the behavior itself (112). Instead, such a field of associations most likely point to general and shared dynamics. One such dynamic may involve underlying issues of social misery and psychological trauma that perhaps give rise to both unhealthy behaviors and to mental disorders. To take one example, long-term unemployment may entail poverty, boredom, and social isolation, which in turn may push a person into unhealthy behaviors as means of escapism and diversion and also contribute to a mounting sense of hopelessness and depression.
Indeed, there is strong evidence supporting a relationship between mental disorder and factors relating to misery and trauma. To take a few noteworthy examples, childhood abuse has been associated with psychosis at ORs of 7.3 (113) and 5.9 (8), with depression at ORs of 19.1 (114) and 4.2 (115), and with ADHD at ORs of 7.3 (91) and 3.3 (116), as well as with cannabis abuse at ORs of 5.8 (117), 2.7 (118), and 2.2 (119). Violence victimization has similarly been associated with psychosis at ORs of 5.9 (120), 4.0 (121), 2.2 (122), and 1.9 (123), with PTSD and depression at ORs of 32.4 and 5.4 (124), and with nicotine dependence at ORs of 22.4 (124) and 5.5 (125). Afifi et al. (118) for their part found that living in an unsafe community was associated with cannabis use at an OR of 5.0 and with tobacco use at an OR of 3.8. Comparable findings exist for childhood bullying victimization (120, 126), while poverty, low education, and unemployment have been associated with psychosis at ORs of 8.2 (127) and 3.0 (122), with depression at ORs of 9.1 (128), 5.0 (129), 3.4 (130), 3.2 (131), 2.8 (132), and 2.6 (133), with nicotine dependence at ORs of 37.0 (134), 2.4 (135), and 2.3 (125), and with cannabis use disorder at an OR of 2.5 (136). It should also be noted that factors relating to trauma and misery might accumulate in an individual and thereby increase risk. In a study by McMahon et al. (120), cumulative adverse life events were strongly associated with psychotic experiences, with four or more adverse life events incurring an OR of 16.8.
Thus, it seems possible that both unhealthy behaviors and mental disorders might be caused by underlying problems related to social misery and psychological trauma, and that the observed associations between those behaviors and disorders are largely spurious. As a basis for the discussion of the specificity of individual associations, this article will use the probably most discussed associations among those here under purview, namely that between cannabis use and psychosis, which is commonly taken to reflect a causal effect from cannabis use. A recent consensus paper by D'Souza et al. (1) pointed to a study by Starzer et al. (137) as evidence supporting the specificity of this association, and on this basis drew the inference that “[c]annabis is more likely to be associated with psychosis outcomes than other psychiatric diagnoses” (p. 732). This consensus paper also pointed to a somewhat broader range of evidence to support the specificity of the cannabis-psychosis association as compared to other forms of substance use, drawing the inference that “[t]he risk for a psychosis outcome is highest for cannabis relative to other drugs” (ibid.).
However, there is also evidence contradicting the consensus view presented in D'Souza et al. (1). As Ksir and Hart (138) pointed out, research has associated cannabis use with depression, which may challenge the specificity of the cannabis-psychosis association. Furthermore, a recent review by Johnstad (13) found that tobacco use tended to be at least as strongly associated with psychosis as is cannabis use. The cannabis-psychosis association may therefore lack specificity both across disorders and across behaviors, which would open for the perspective that the association may be spurious and reflective of a general etiology perhaps related to underlying psychological trauma and social misery.
This interpretation is supported by a study by Shakoor et al. (139) which found that in a sample of adolescent twins, “[e]nvironmental influences explained all of the covariation between cannabis use and paranoia, cognitive disorganization and parent-rated negative symptoms,” with a bivariate common environment of 69%−100% (p. 144). Cannabis use explained 2%−5% of variance in positive, cognitive, and negative psychotic experiences. Sideli et al. (140) for their part found that less than daily cannabis use was not associated with psychosis (OR 0.97, p = 0.92) unless it co-occurred with having experienced child abuse, in which case the association was strong (OR 2.51, p < 0.05), while Copeland et al. (141) found that cannabis use before the age of 16 was strongly associated with depression (OR 2.3) and anxiety (OR 2.9) in an analysis adjusted only for sex and race/ethnicity, but that the association disappeared with adjustment for childhood disorders and adversities (OR 0.6 for both depression and anxiety). A meta-analysis by Fusar-Poli et al. (8) similarly found that risk for psychosis was related to environmental risk factors such as childhood trauma and further accumulated by low education and unemployment, while finding no significant impact from cannabis use.
In sum, the worry that unhealthy behaviors such as cannabis use cause psychosis may be a case of projecting the social characteristics of the drug-using population onto the drug itself and understand these characteristics as pharmacological effects inherent to the drug use. This comparative review aimed to assemble data on a broad range of associations between unhealthy behaviors and mental disorders in order to compare their respective strengths and to gain insight into the influence of factors relating to trauma and misery by recording the inclusion of relevant control variables and subsequently running sensitivity tests on the dataset. It reviews recent (2015 through January 2023) research on associations between a range of unhealthy behaviors and mental disorders, using the much-debated association between cannabis use and psychosis as a basis for comparison. In order to obtain comparable figures, the review included only records that presented their findings as odds ratios, and attempted to account for variations in behavior intensity, sample generalizability, and covariates via subsequent sensitivity analyses. By thus gaining a comparative overview of the relationship between unhealthy behaviors and mental disorders, the review hoped to achieve three specific aims:
1. Understand individual associations between a given unhealthy behavior and a given mental disorder in relation to other such disorders.
2. Understand individual associations between a given unhealthy behavior and a given mental disorder in relation to other such behaviors.
3. Understand the association between unhealthy behaviors and mental disorders in relation to statistical control for covariates.
Methods
The pre-planned criteria for inclusion were that studies must investigate associations between any of the relevant behaviors and disorders and report their findings as odds ratios in a manner that allows for cross-study comparisons. In order to keep the number of included studies manageable, only recent studies (no older than 2015) would be included. Furthermore, the studies should be published in English, be available in the Pubmed database, and their sample size should be at least 100.
Two Pubmed searches were performed (February 3, 2023). The search related to cannabis and tobacco use was [(tobacco OR nicotine OR cigarette OR cannabis OR marijuana) AND (psychosis OR depression OR anxiety OR bipolar OR “personality disorder” OR adhd OR ptsd) AND associat* AND (use OR “use disorder” OR dependence OR abuse) AND (comorbid OR dual OR psychiatric)] while the search related to diet quality and sedentary behavior was [(“poor diet” OR “sedentary behavior” OR “fast food” OR soda OR “sugar-sweetened”) AND (psychosis OR depression OR anxiety OR bipolar OR “personality disorder” OR adhd OR ptsd) AND associat*]. The author assessed all records. Reported associations in included studies were classified as cross-sectional or longitudinal, with retrospective analyses being classified as longitudinal. In order to investigate directionality as openly as possible, longitudinal studies of both unhealthy behaviors leading to mental disorders and mental disorders leading to unhealthy behaviors were included. Study quality was assessed on the level of sample representativeness, behavioral measurement disparities, and the inclusion of control variables related to social misery and psychological trauma. Results are reported according to PRISMA guidelines (142).
The selection procedure is shown in the flow chart of Figure 1. Criteria related to language and publication date were implemented in the search itself. Four reports were excluded for having samples lower than n = 100, while 309 reports were excluded because they did not report any relevant odds ratios that allowed for comparisons. This was related to the following reasons:
1. The reports combined several types of drugs or disorders into a single construct (e.g., “substance use,” “psychological distress,” “internalizing disorders”).
2. The reports subdivided disorders into specific symptoms or symptom classes (e.g., auditory and visual hallucinations in psychosis).
3. Findings were reported in other terms than odds ratios (e.g., risk ratios, hazard ratios).
4. Some reports especially of sedentary behavior were also excluded because they reported ORs for continuous variables that were not readily comparable to the other studies included in the review.
5. A few reports utilizing Mendelian randomization methodology were excluded because they were not comparable to the cross-sectional or longitudinal studies included in the review and did not constitute a meaningful basis for comparison on their own.
Variables
The review focused on moderate cannabis and tobacco use as compared to high levels of sedentary behavior and poor diet quality. This approach was founded on the observation in Johnstad (13) that heavy substance use is very likely associated with underlying factors of social misery and psychological trauma, and that analyses of the heavy drug-using population are therefore at high risk of confusing the social characteristics of this population segment with the effects from the drug use itself. While heavy chronic drug use is commonly driven by coping motives related to underlying misery and trauma, moderate use is driven by a much broader range of motivations (143–145). In order to understand pharmacological effects from substance use in and of themselves, it therefore seems advisable to focus on moderate usage patterns.
In this review, moderate cannabis use was defined as one or two use occasions per week (146, 147). For tobacco, moderate use could be defined as daily use of about 10 cigarettes (148–150). When the studies included in this review reported effects related to several different usage patterns, the one most closely resembling a moderate pattern was selected. The review did not exclude any study on the basis of divergences in the usage pattern, however, and several included studies focused exclusively on use disorders or similarly problematic behavior. For sedentary behavior and diet quality, the review focused on high exposure represented by such measures as the worst quartile, daily consumption of soda or fast-food, not meeting physical activity guidelines, or more than 4–8 h of screen time per day. This approach was based on the observation that unlike cannabis and tobacco use, sedentary behavior and unhealthy food consumption are universal behaviors with which moderate levels of engagement are ubiquitous. When studies reported figures from several different multivariate models, the review included the figures from the final, most stringently adjusted model. Sensitivity analyses attempted to account for the inclusion of studies focusing on specialty samples and disordered behavior patterns.
Analyses
Across studies
The meta-analysis compared mean odds ratios for associations between behaviors and disorders across studies. To compare odds ratio means related to a given unhealthy behavior and a given mental disorder in relation to other such disorders, the data was restructured so as to combine odds ratios for different disorders into a single variable with different corresponding labels. T-tests were used for each pair of disorders for cross-sectional and longitudinal (behavior before disorder) studies. With 21 pairs of disorders, 4 behaviors, and 2 analytical approaches, a total of 168 different comparative analyses were performed. To compare odds ratio means between different unhealthy behaviors, findings for each disorder were compared for each pair of behaviors for cross-sectional and longitudinal (behavior before disorder) studies. With seven disorders, six pairs of behaviors, and two analytical approaches, a total of 84 different comparative analyses were performed between studies of different behaviors. It might be noted that none of these comparisons were Bonferroni corrected, which would probably have rendered them all non-significant.
Within studies
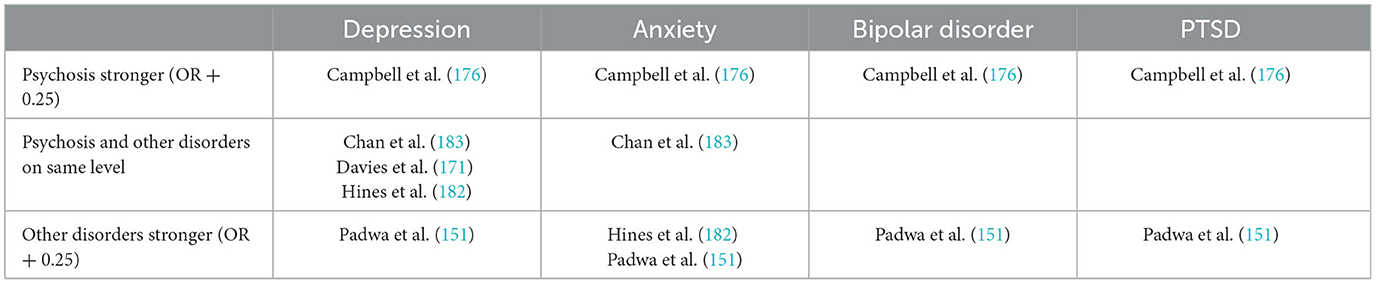
Some studies reported comparable odds ratios for several different disorders and/or behaviors. In studies of cannabis use that reported figures relating both to psychosis and to other disorders, the review compared the respective odds ratios and classified the figure for psychosis as stronger if it exceeded the other figure by 0.25, as weaker if the other figure exceeded the figure for psychosis by 0.25, and otherwise as being at the same level. Similarly, for studies that provided odds ratios relating to a given disorder for both cannabis/tobacco use and diet quality/sedentary behavior, the review classified either as stronger if it exceeded its counterpart by 0.25, and otherwise as being at the same level.
Sensitivity analyses
Sample groups
The studies included in the review analyzed participant samples ranging from representative samples of the nation's adult population to more narrowly defined groups such as children, older adults, male military conscripts, university students, and patient groups. In order to control for the possibility that narrow samples unduly impacted overall dataset analyses, dichotomous variables for “children” (samples below age 18), “older adults” (samples above age 60), “patient” (all patient or high-risk groups without controls), and “special” (samples consisting of university students or employees, all-male or all-female samples, military service members or veterans, and civil servants) were defined. Subsequently, these variables were combined into a single dichotomous indicator for specialty sample.
Behavioral measurement disparities
The studies included in the review spanned behaviors across the risk spectrum, from any (or ever) use of tobacco or weekly fast-food consumption to nicotine use disorder and binge eating disorder. In order to control for the possibility that the disordered behavior measured in some studies unduly impacted overall analyses, a dichotomous “problem behavior” indicator was defined to include behavioral variables including “binge eating disorder,” “emotional eating,” “maladaptive/pathological internet use,” “smartphone addiction,” “Facebook overuse,” “problematic gaming,” “internet addiction,” tobacco/cannabis problem use, abuse, dependence, use disorder, or high-risk use, and smoking during pregnancy. Especially for tobacco, however, it was not clear whether use measured in terms of daily smoking could be meaningfully differentiated from use measured in terms of abuse, dependence etc.
Control variables
The studies included in the review used a wide variety of control variables in their statistical analyses. In this review, systematic differences in association strengths related to statistical control for diet quality or sedentary behavior (for tobacco and cannabis analyses), tobacco use (for diet quality, sedentary behavior, or cannabis analyses), and cannabis use (for diet quality, sedentary behavior, or tobacco analyses) were controlled for by the application of dichotomous adjustment variables (0 = no control, 1 = control). Furthermore, dichotomous variables for adjustment for social misery (1 = inclusion of any control variable relating to poverty, education, or unemployment) and psychological trauma (1 = inclusion of any control variable relating to childhood abuse/neglect, bullying victimization, or violence victimization) were defined. Finally, a variable for studies that reported bivariate associations (1 = bivariate) was defined.
It should be noted, however, that some studies analyzed potential covariates on a bivariate basis and only included those that passed a significance threshold of p < 0.05 in the final model. This review accepted such variables as having been controlled for, although it should be clear that a covariate may exert meaningful influence on the outcome of a multivariate regression even if its bivariate correlation with the outcome variable is significant only at the 90% (p < 0.1) level, for instance.
Results
Overall findings
From 3,682 records, 294 were included. Some publications reported figures for several behaviors and methodological approaches (commonly, both cross-sectional and longitudinal), and counting these the review included 97 studies of cannabis use, 132 studies of tobacco use, 88 studies of sedentary behavior, and 47 studies of diet quality. The dataset included a total of 570 associations between behaviors (cannabis use, tobacco use, sedentary behavior, and diet quality) and disorders (psychosis, depression, anxiety, bipolar disorder, personality disorder, ADHD, and PTSD).
Sample groups
The review included 320 associations (out of 570) marked as relating to specialty samples. In the full dataset of cross-sectional and longitudinal associations, the specialty sample indicator was not significantly correlated with odds ratios for any disorder or behavior. Specialty samples were most commonly used in studies of diet quality and sedentary behavior (69%) and least commonly used in cannabis studies (44%). As a sensitivity test, the analyses reported below were repeated with studies using specialty samples removed from the dataset. This new set of analyses identified marginally significant differences (t = 2.30, df = 5.76, two-sided p = 0.06) for PTSD between cannabis use and tobacco use, with the former having higher ORs.
Behavioral measurement disparities
The review included 101 associations (out of 570) marked as relating to disordered or problematic behavior. In the full dataset of cross-sectional and longitudinal associations, the problem behavior indicator was significantly associated with odds ratios for depression (r = 0.15, p = 0.015, N = 251) and ADHD (r = 0.31, p = 0.021, N = 55). The inclusion of studies investigating problem behaviors may thus have served to increase association strengths for these disorders. Across disorders, the indicator for problem behavior was significantly correlated with the odds ratio strength in non-tobacco associations (r = 0.12, p = 0.021, N = 366) but not in associations with tobacco use (r = 0.08, p = 0.252, N = 204). This finding supports the notion that tobacco use measured in terms of daily smoking cannot necessarily be differentiated from use measured in terms of abuse or dependence. Problem behaviors were most commonly studied in relation to cannabis use (29%) and least commonly in relation to diet quality and sedentary behavior (10%). As a sensitivity test, the analyses reported below were repeated with studies investigating disordered or problematic behavior removed from the dataset. This new set of analyses identified significant differences (t = 2.31, df = 8.38, two-sided p < 0.05) for PTSD between cannabis use and tobacco use, as well as between cannabis use and sedentary behavior (t = 2.32, df = 8.13, two-sided p < 0.05), with ORs for cannabis in both cases being higher. Furthermore, these analyses identified marginally significant differences (t = 1.93, df = 32, two-sided p = 0.06) between cannabis-psychosis and cannabis-PTSD, with the latter having higher ORs. Finally, the review included a few studies that investigated the association between depression and secondhand smoking (N = 5) and e-cigarette use (N = 6). These studies did not diverge substantially from other tobacco studies in terms of their association strengths with mental disorders.
Control variables
Some studies reported bivariate associations (33 out of 570), generally because their main focus lay elsewhere and the relationships investigated in this review were only a secondary concern in their analysis. In the full dataset, the bivariate indicator was significantly associated with odds ratios for anxiety (r = 0.19, p = 0.043, N = 112) and ADHD (r = 0.33, p = 0.013, N = 55). The inclusion of studies reporting bivariate associations may thus have served to increase association strengths for these disorders. Across disorders and behaviors, the bivariate indicator was marginally correlated with odds ratios (r = 0.08, p = 0.064, N = 570). Bivariate findings were most commonly reported in tobacco studies (8%) and least commonly in studies of sedentary behavior and diet quality (4%). As a sensitivity test, the analyses reported below were repeated with studies reporting bivariate associations removed from the dataset. This new set of analyses identified marginally significant differences (t = 1.96, df = 18.57, two-sided p = 0.07) for PTSD between cannabis use and sedentary behavior, with the former having higher ORs.
Overall, 51 (out of 570) associations were adjusted for psychological trauma, and the indicator for trauma adjustment was marginally significant for psychosis (r = −0.25, p = 0.056, N = 61). Across disorders and behaviors, the indicator was marginally correlated with odds ratios (r = −0.07, p = 0.103, N = 570), and such adjustment was most commonly employed in cannabis studies (14%) and least commonly in studies of diet quality (2%). By contrast, 441 (out of 570) associations were adjusted for social misery, and such adjustment was most commonly employed in studies of diet quality (82%) and least in studies of cannabis and tobacco (76%). Across disorders and behaviors, the indicator for misery adjustment trended weakly in a negative direction (r = −0.06, p = 0.151, N = 570) but was marginally correlated with odds ratios in cannabis studies (r = −0.13, p = 0.093, N = 178).
Only 1% of cannabis studies and 14% of tobacco studies controlled for diet quality and/or sedentary behavior, while studies of the latter behaviors often controlled for tobacco (55%) but rarely for cannabis (8%). Furthermore, 35% of cannabis studies controlled for tobacco while 24% of tobacco studies controlled for cannabis. With regard to specific disorders, the indicator for cannabis adjustment was significant only in (non-cannabis) studies of psychosis (r = −0.55, p < 0.001, N = 32) while tobacco adjustment was significant in (non-tobacco) studies of anxiety (r = −0.24, p = 0.033, N = 80) and marginally of depression (r = −0.15, p = 0.059, N = 163). Across disorders, tobacco adjustment was significantly correlated with odds ratios in non-tobacco studies (r = −0.19, p < 0.001, N = 366) and cannabis adjustment was significantly correlated with odds ratios in non-cannabis studies (r = −0.13, p = 0.010, N = 392). The indicator for adjustment for diet quality and/or sedentary behavior was nowhere significant.
In exploratory linear regression analyses, the set of study quality variables (sample size, specialty sample, disordered behavior, and control variables) explained 2.7% of the variance in odds ratios in the overall dataset and 12.4% of the variance in longitudinal studies. For cross-sectional studies of individual behaviors, regression models explained between 9.0% (tobacco use) and 27.5% (poor diet quality) of the variance in odds ratios, and for individual disorders between 1.4% (personality disorder) and 37.5% (bipolar disorder). See Supplementary Appendix B for the specification of these models. In these models, disordered behavior commonly reached significance as a positive influence on odds ratios, indicating that studies investigating such behaviors tended to find higher risk for mental disorders. In the full dataset, higher sample size reduced odds ratios, indicating that large-N studies tended to obtain more moderate risks; this was an issue especially for longitudinal (behavior before disorder) studies. In studies of cannabis and tobacco use, adjustment for its counterpart was a highly significant negative influence on odds ratios.
Findings for individual disorders
Psychosis
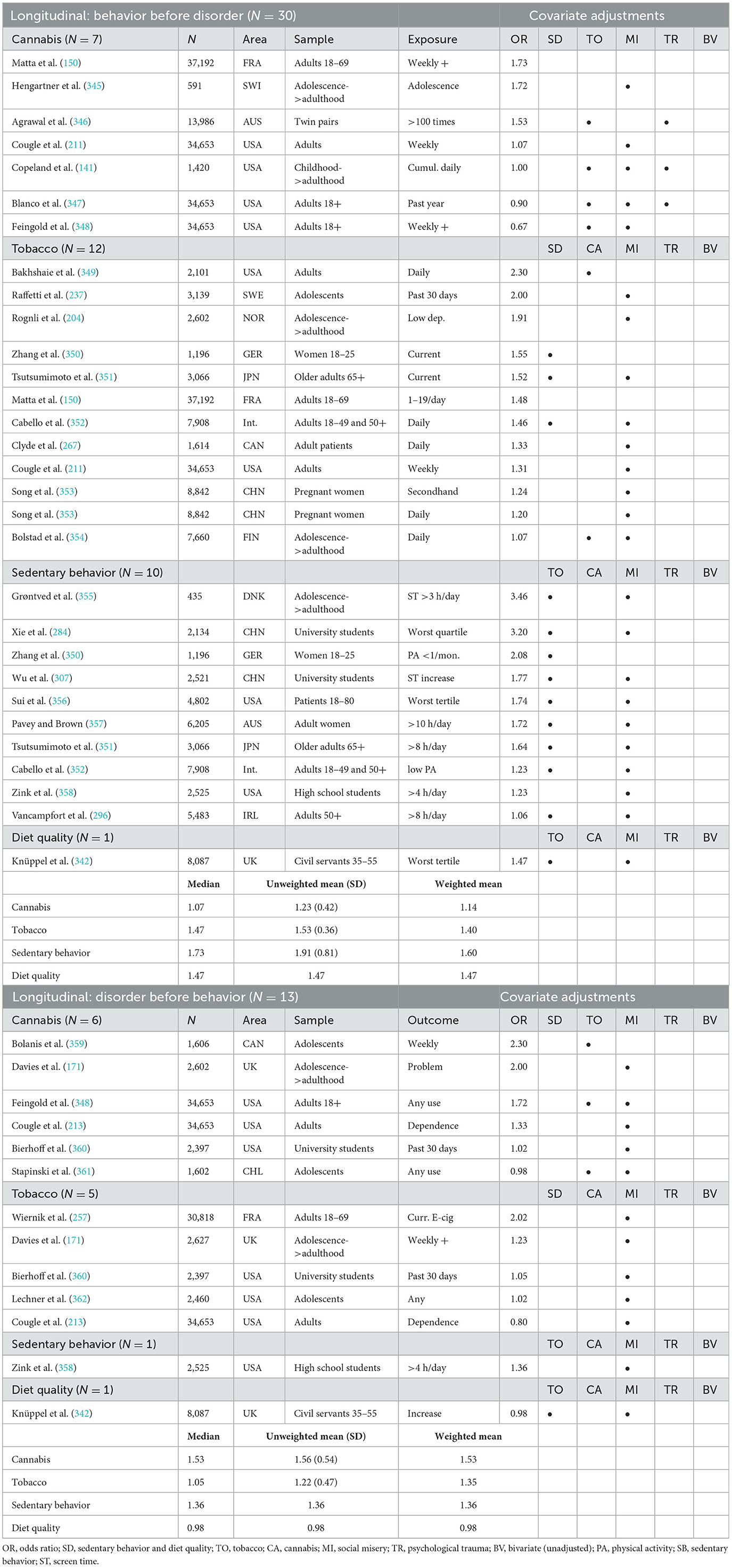
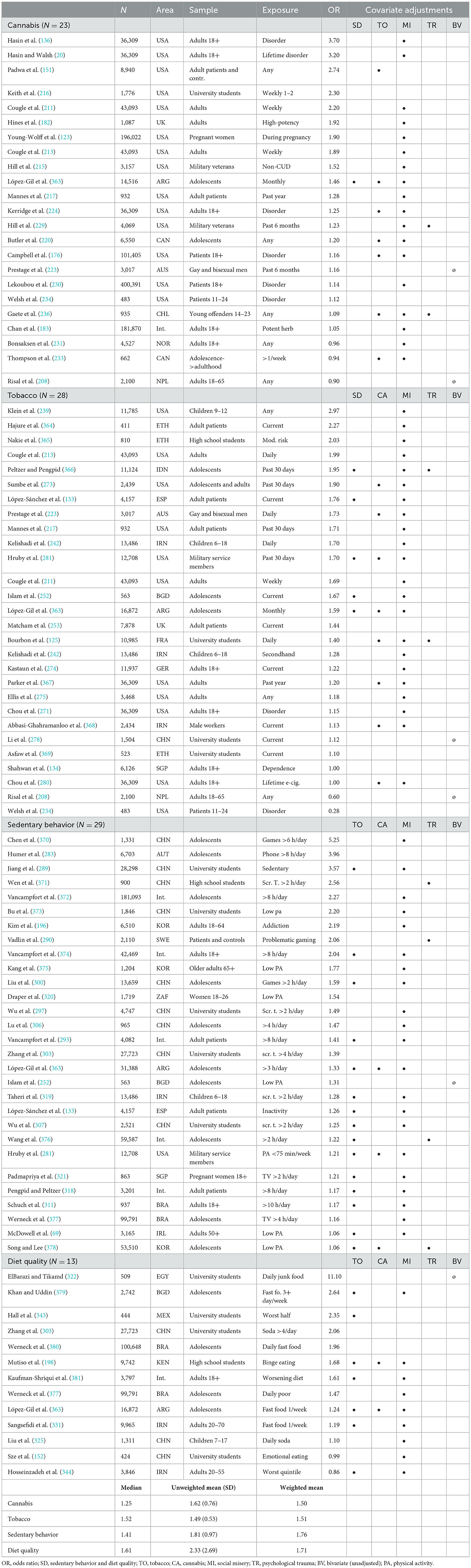
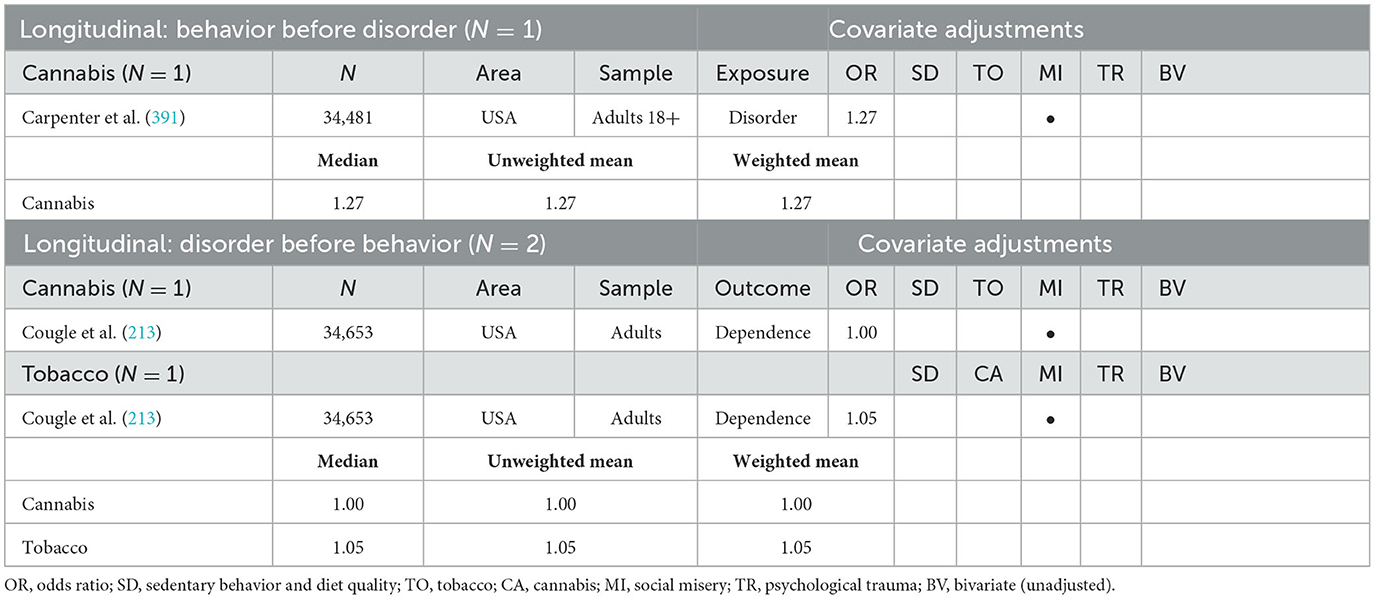
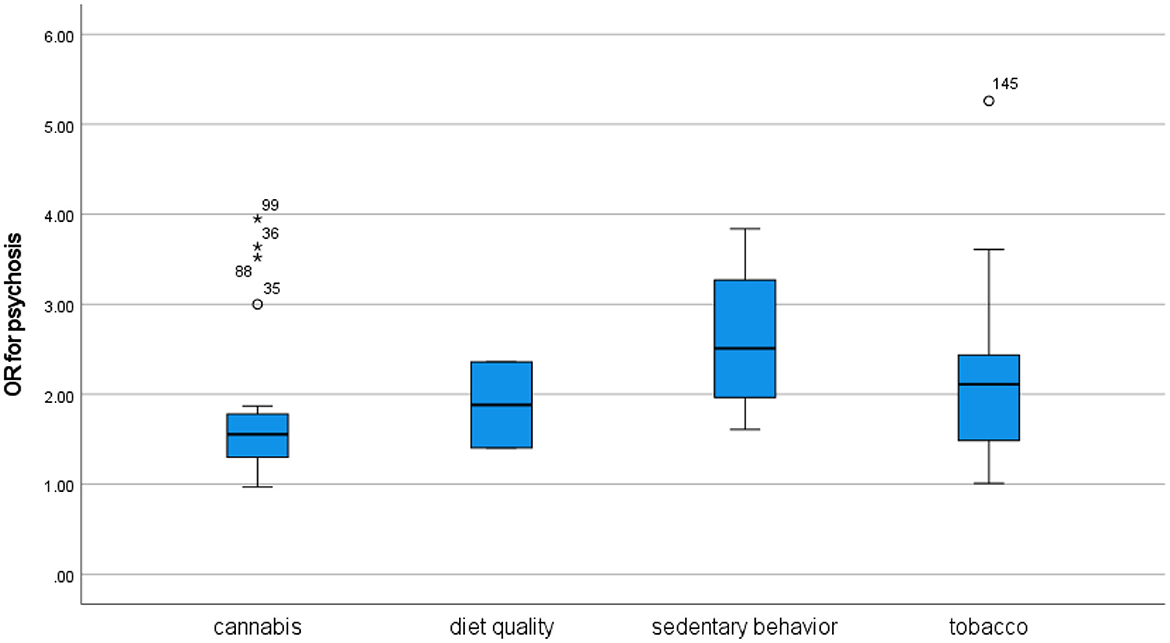
This review included 45 cross-sectional and 16 longitudinal figures for the association between unhealthy behaviors and psychosis (Tables 1a, 1b). The cross-sectional studies provide convincing evidence for associations between psychosis and cannabis and tobacco use and some evidence for associations with sedentary behavior and diet quality. The longitudinal studies provide some evidence that cannabis and tobacco use may lead to subsequent psychosis and more tenuous evidence that psychosis may lead to subsequent cannabis and tobacco use.
Depression
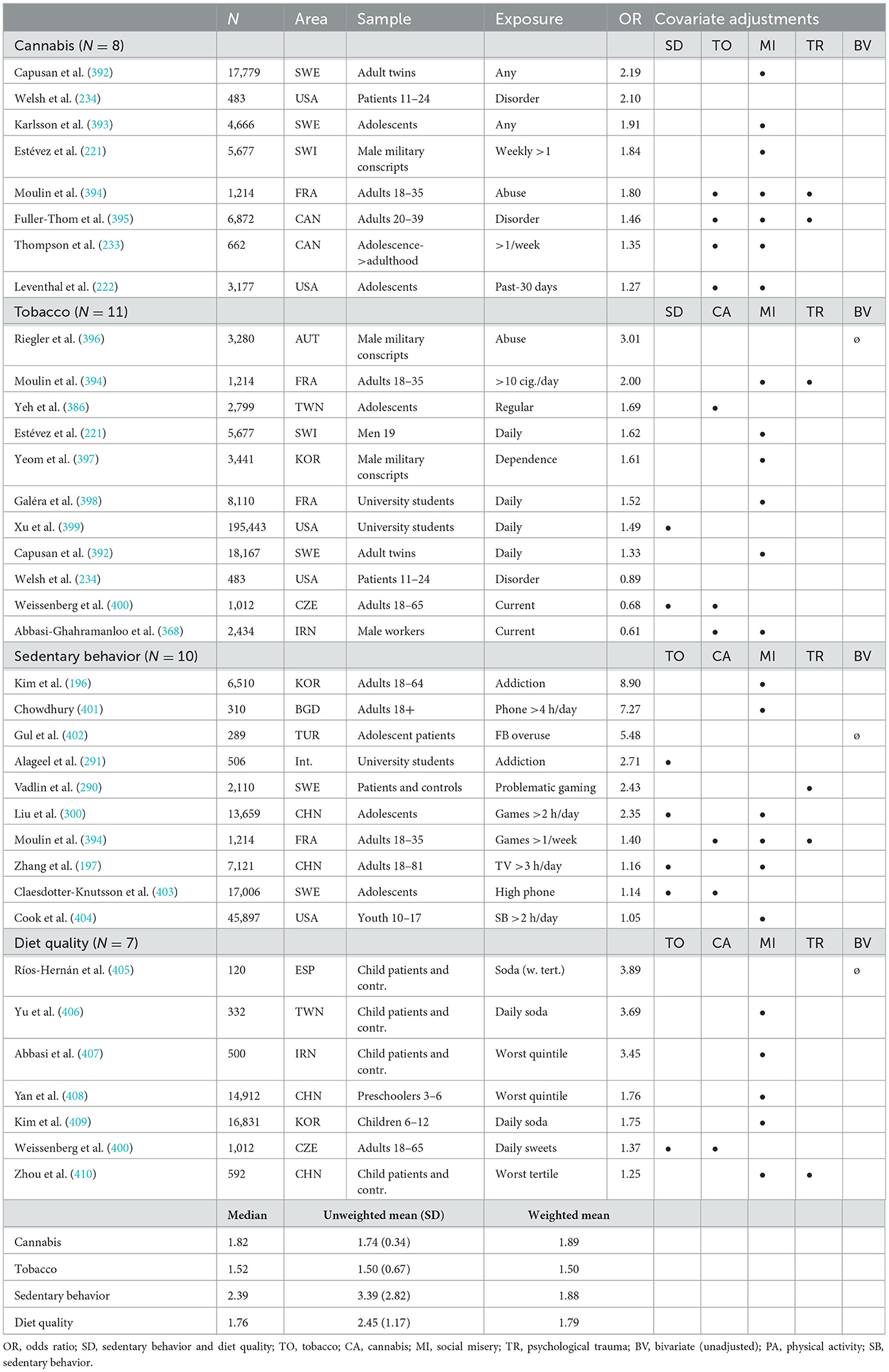
The present review included 208 cross-sectional and 43 longitudinal figures for the association between unhealthy behaviors and depression (Tables 2a, 2b). The cross-sectional studies provide convincing evidence for associations between depression and cannabis, tobacco, sedentary behavior, and diet quality. The longitudinal studies provide some evidence that sedentary behavior and use of cannabis and tobacco may lead to subsequent depression and that depression may lead to subsequent cannabis and tobacco use. There was very limited longitudinal evidence related to diet quality.
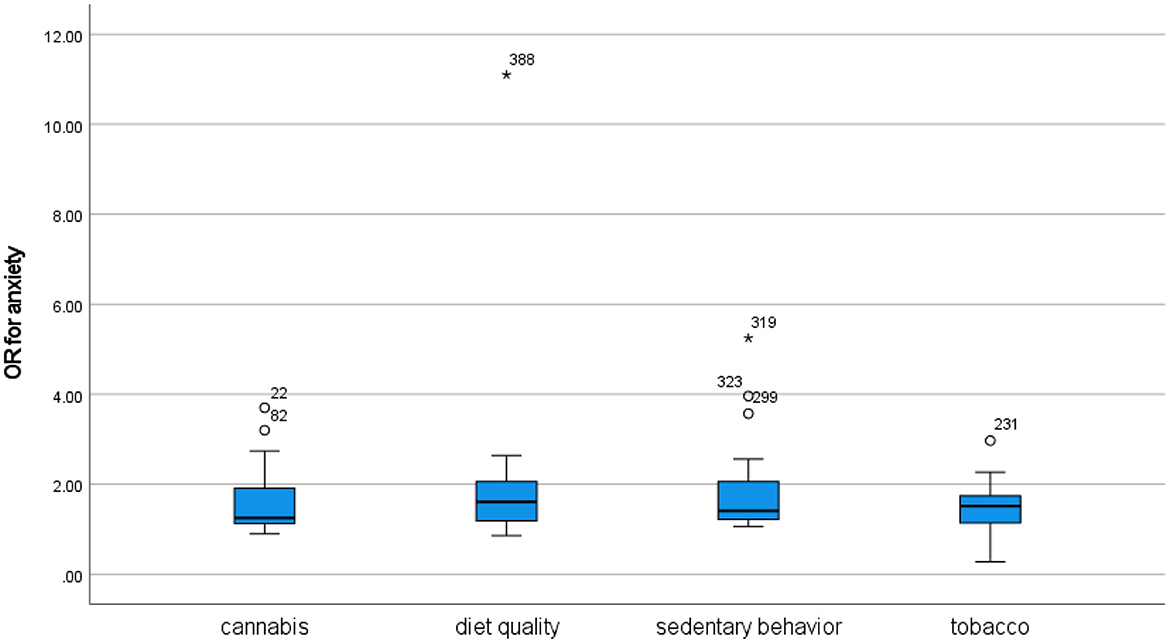
Anxiety
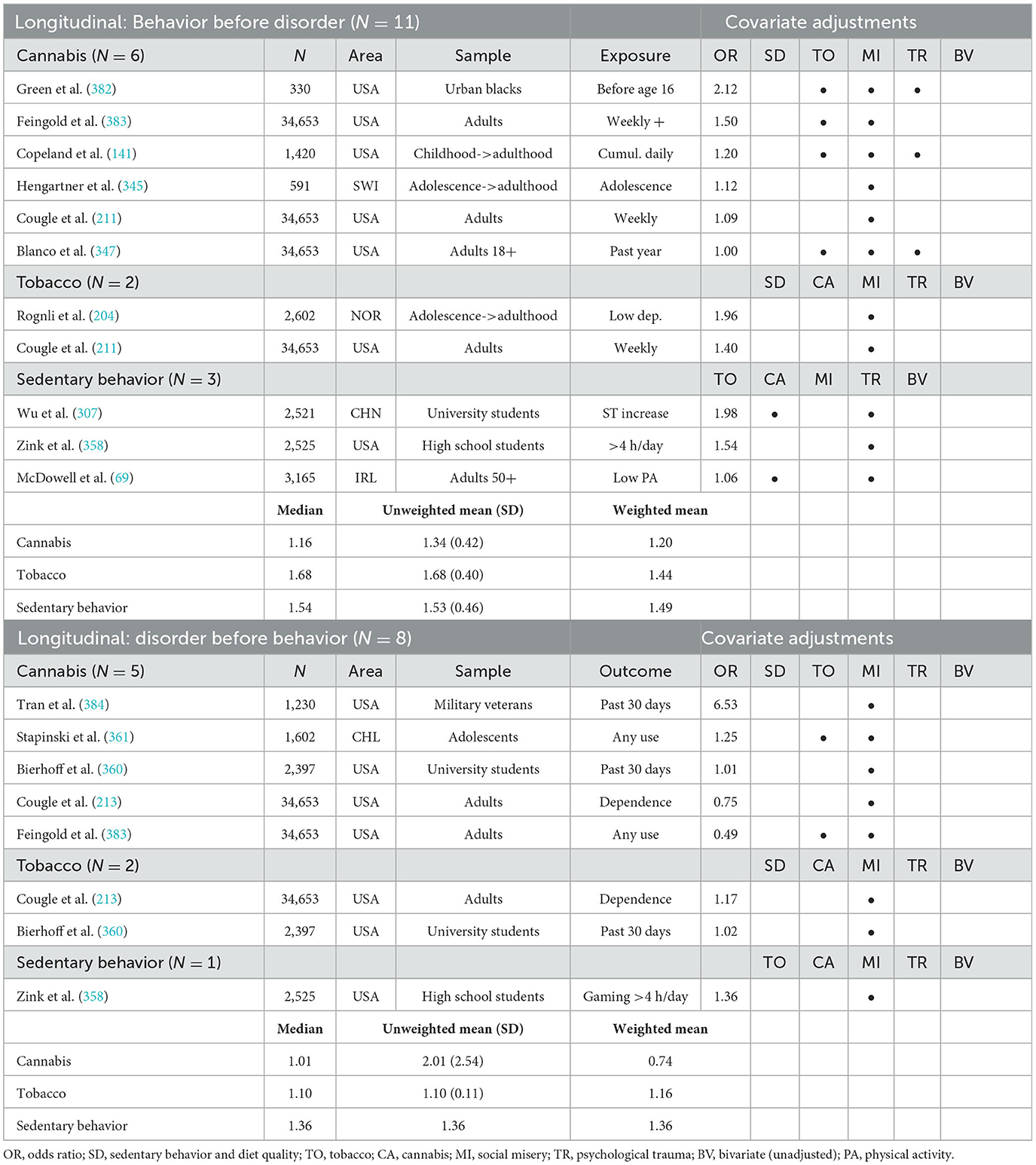
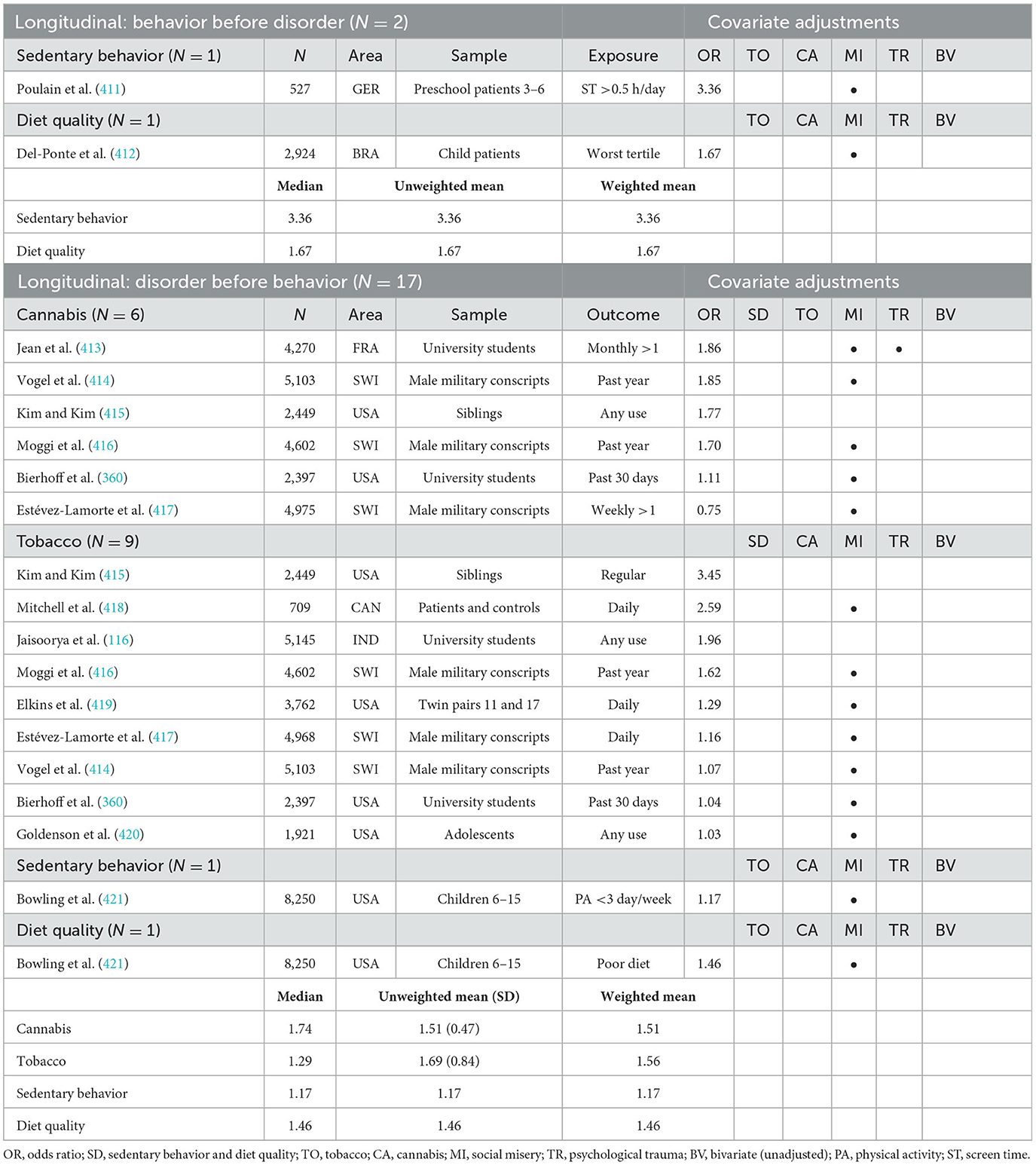
The review included 93 cross-sectional and 19 longitudinal figures for the association between unhealthy behaviors and anxiety (Tables 3a, 3b). The cross-sectional studies provide convincing evidence for associations between anxiety and cannabis, tobacco, sedentary behavior, and diet quality. The longitudinal studies provide some evidence that sedentary behavior and use of cannabis and tobacco may lead to subsequent anxiety and tenuous evidence that anxiety may lead to subsequent sedentary behavior and cannabis and tobacco use. No longitudinal evidence related to diet quality was included in this review.
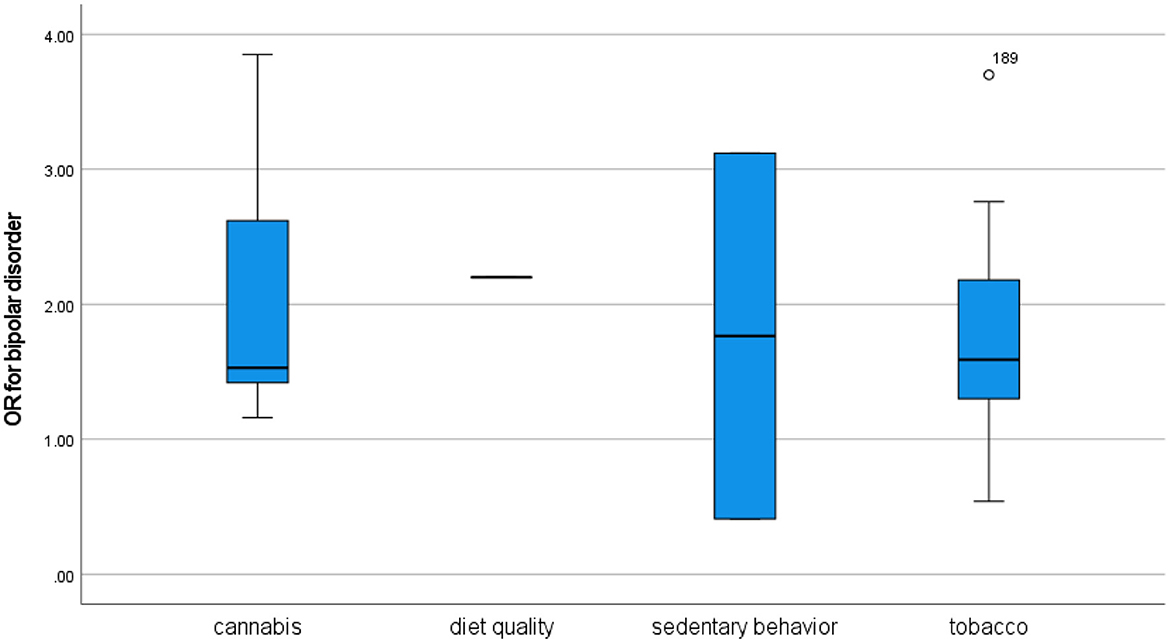
Bipolar disorder
This review confirms that there is limited research on the association between unhealthy behaviors and bipolar disorder. A total of 25 cross-sectional and 10 longitudinal figures were included in the review (Tables 4a, 4b), many of which were based on the same NESARC dataset. The cross-sectional studies provide convincing evidence for associations between bipolar disorder and cannabis and tobacco use and tenuous evidence for associations with sedentary behavior and diet quality. The longitudinal studies provide some evidence that the use of cannabis and tobacco may lead to subsequent bipolar disorder, but no evidence that bipolar disorder may lead to subsequent cannabis and tobacco use. No longitudinal evidence related to sedentary behavior and diet quality was included in this review.
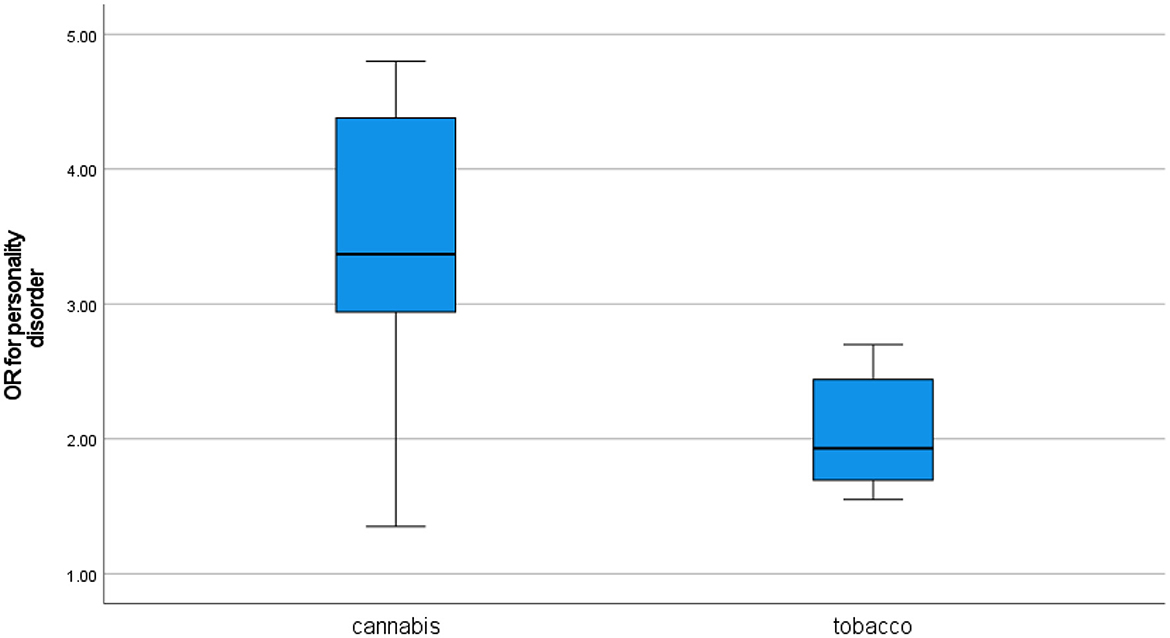
Personality disorders
The findings of this review confirm that the association between unhealthy behaviors and personality disorders has not been intensively studied. A total of 16 cross-sectional and three longitudinal figures were included in the review (Tables 5a, 5b), many of which were based on the same NESARC dataset. The cross-sectional studies provide convincing evidence for associations between personality disorder and cannabis and tobacco use, but no evidence related to sedentary behavior and diet quality was included in this review. Furthermore, no evidence indicating that unhealthy behaviors may lead to subsequent personality disorder and no evidence that personality disorder may lead to subsequent unhealthy behavior was included in this review.
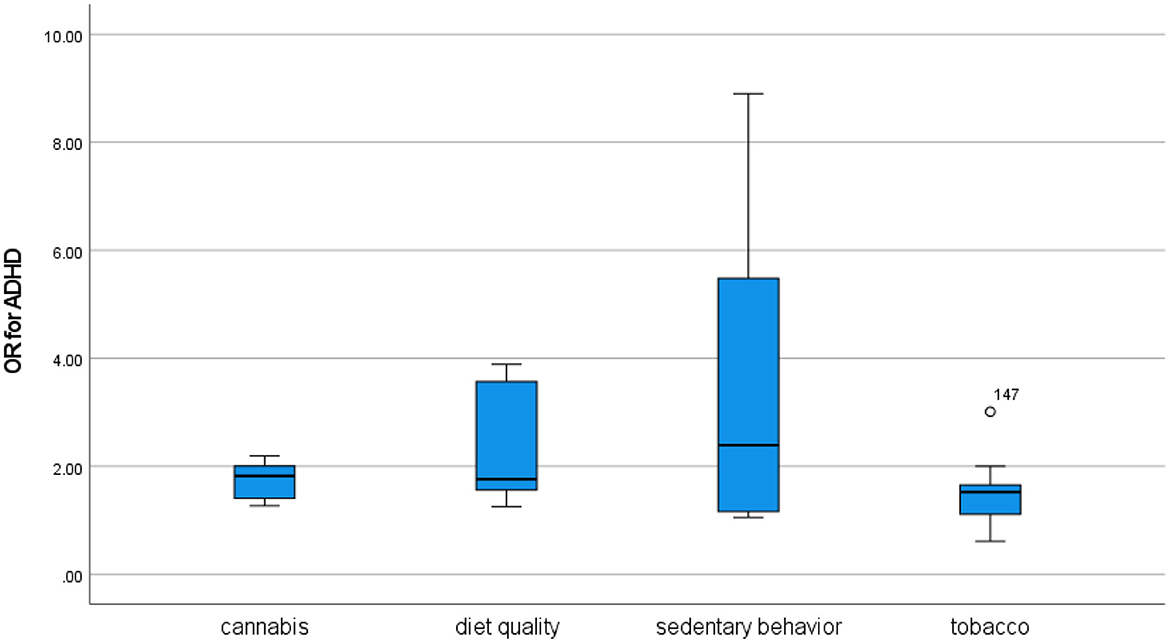
Attention-deficit/hyperactivity disorder
This review included 36 cross-sectional and 19 longitudinal figures for the association between unhealthy behaviors and ADHD (Tables 6a, 6b). The cross-sectional studies provide convincing evidence for associations between ADHD and cannabis use, tobacco use, sedentary behavior, and diet quality. The longitudinal studies focused for the most part on how the disorder may lead to unhealthy behavior, probably because ADHD is a disorder often diagnosed in childhood. As such, only single studies provide any evidence that sedentary behavior and poor diet quality may lead to subsequent ADHD, and no evidence at all was included for cannabis and tobacco use. However, there was some evidence that ADHD may lead to subsequent cannabis and tobacco use and single-study evidence that the disorder may lead to sedentary behavior and poor diet quality.
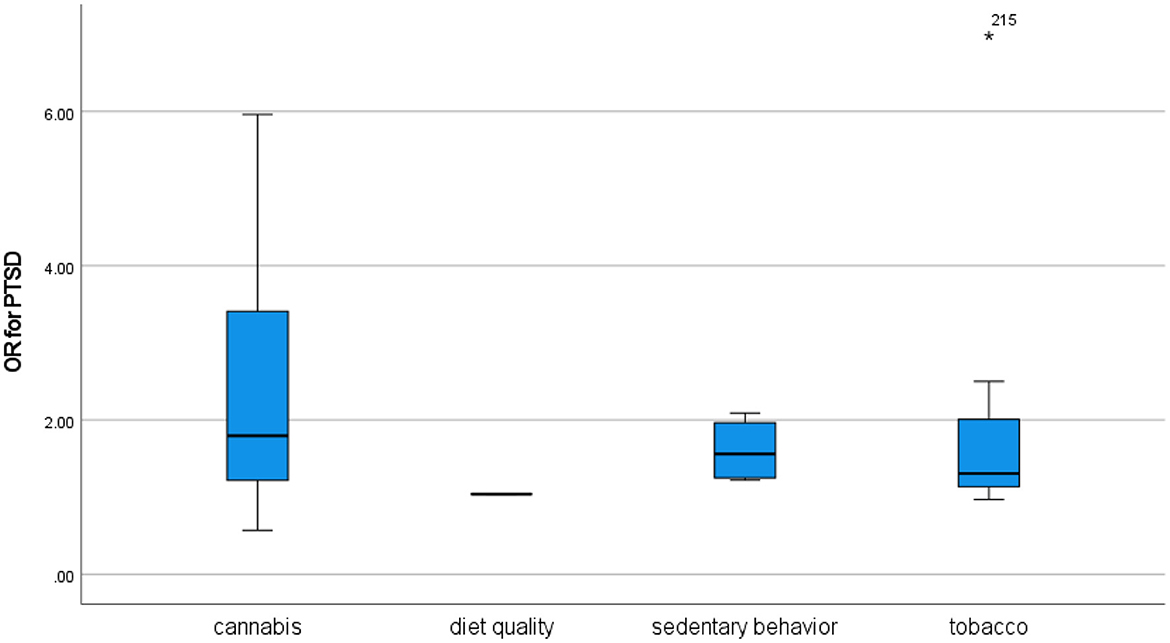
Post-traumatic stress disorder
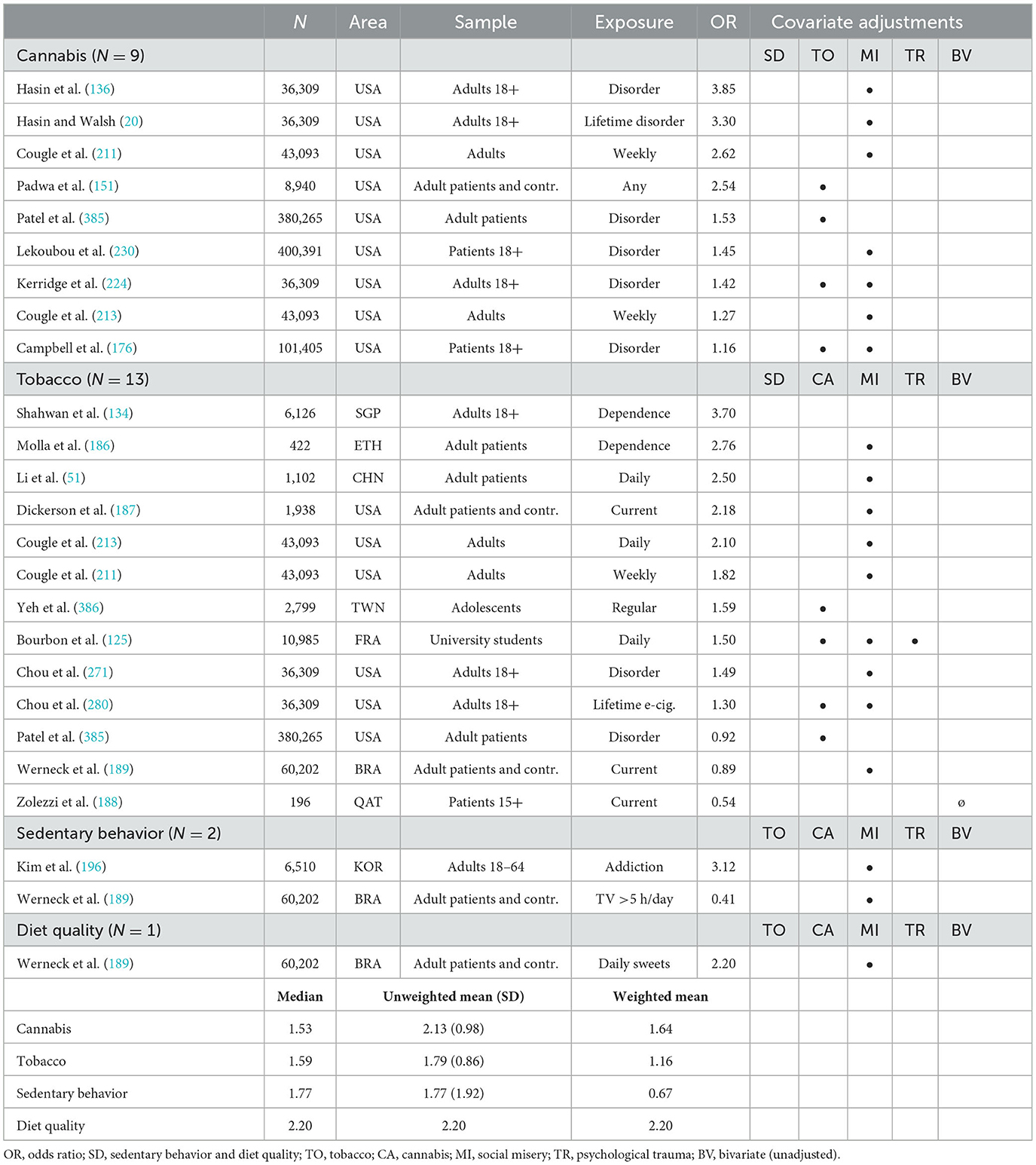
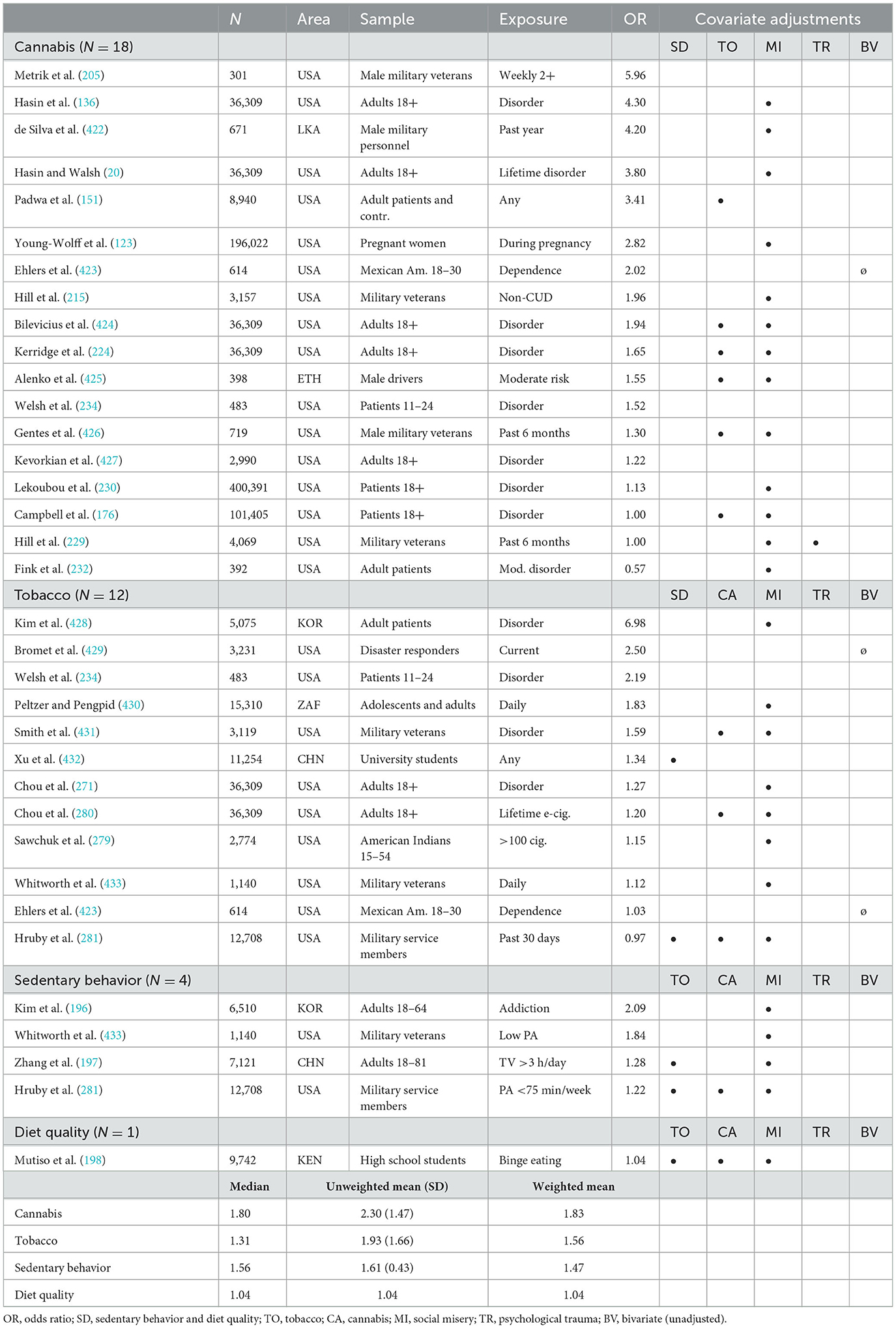
The review included 35 cross-sectional and only two longitudinal figures for the association between unhealthy behaviors and PTSD (Tables 7a, 7b). The cross-sectional studies provide convincing evidence for associations between PTSD and cannabis and tobacco use, as well as some evidence for an association with sedentary behavior, but none for diet quality. The longitudinal studies provide single-study evidence that the use of cannabis and tobacco may lead to subsequent PTSD. Nevertheless, it should be noted that sensitivity analyses for specialty samples, behavioral measurement disparities, and control variables introduced discrepancies related to the cannabis-PTSD relationship, indicating that these findings should be interpreted with extra carefulness.
Analyses
Aim 1: understand individual associations between a given unhealthy behavior and a given mental disorder in relation to other such disorders
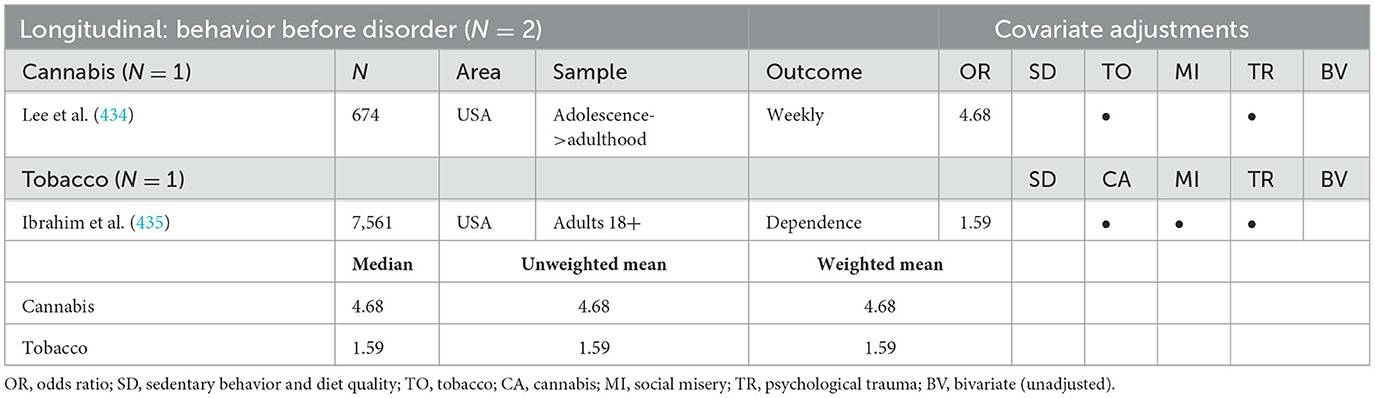
The general finding of this review was that associations between a given unhealthy behavior and mental disorders tended to resemble each other in terms of their strength (Figure 2 and Supplementary Figures A2a–A2d), although with some exceptions. In studies of tobacco use, associations with psychosis tended to be stronger than associations with other mental disorders, with the differences reaching statistical significance for cross-sectional studies in t-test comparisons with depression (t = 2.34, df = 88, two-sided p = 0.022), anxiety (t = 2.83, df = 24.07, two-sided p = 0.009), and ADHD (t = 2.09, df = 28, two-sided p = 0.046). Associations with anxiety for their part tended to be weaker than associations with other mental disorders, reaching statistical significance for cross-sectional studies in t-test comparisons with personality disorder (t = 2.61, df = 33, two-sided p = 0.014) and marginal significance (t = 1.86, df = 97, two-sided p = 0.066) with depression. In studies of sedentary behavior and diet quality, associations with PTSD tended to be weaker than associations with other mental disorders, although low numbers of studies for many disorders entailed that the differences reached marginal statistical significance only in cross-sectional t-test comparisons with psychosis (t = 2.03, df = 9, two-sided p = 0.07).
Because of constraints on space, it is not possible to report more detailed analyses for all the behaviors here reviewed. However, since the association between cannabis use and psychosis was previously noted as especially controversial, it will be analyzed in further detail. Two analyses compared the strength of the cannabis-psychosis association with that of associations between cannabis use and other mental disorders. The first such analysis compared the means and spreads for each disorder between different studies, with the boxplots of Figure 2 summing up this analysis for cross-sectional studies of cannabis use. These studies indicate that cannabis use was not more strongly associated with psychosis than with the other mental disorders here under purview. T-tests indicated that only the figures for personality disorder were significantly different from those for psychosis (t = 4.18, df = 27, two-sided p < 0.001), and indeed the figures for personality disorder were significantly higher than those for all other diagnoses (depression t = 4.33, df = 50, two-sided p < 0.001; anxiety t = 5.44, df = 30, two-sided p < 0.001; bipolar disorder t = 2.73, df = 16, two-sided p = 0.015; ADHD t = 4.44, df = 9.66, two-sided p < 0.001; PTSD t = 2.13, df = 25, two-sided p = 0.043). In addition, the association with anxiety was marginally weaker than the association with PTSD (t = 1.78, df = 24.05, two-sided p = 0.06). No differences were detected for longitudinal studies or specifically for longitudinal (behavior before disorder) studies (Supplementary Figures A2a, A2b), but there were not many such studies to compare.
As can be seen in Tables 1a–7a, furthermore, the weighted means of odds ratios for cross-sectional associations between cannabis use and the seven mental disorders tended to converge even more closely than the unweighted means to the area of 1.5–2.0, with the only exception relating to personality disorders. Longitudinal means (Tables 1b–7b) were somewhat more varied, but the weighted means for longitudinal (behavior before disorder) studies converged to the area of 1.0–2.0 except for ADHD, for which there was no evidence, and for a single high-OR PTSD study. Weighted means for the small number of longitudinal (disorder before behavior) studies for their part converged to the area of 0.5–1.5.
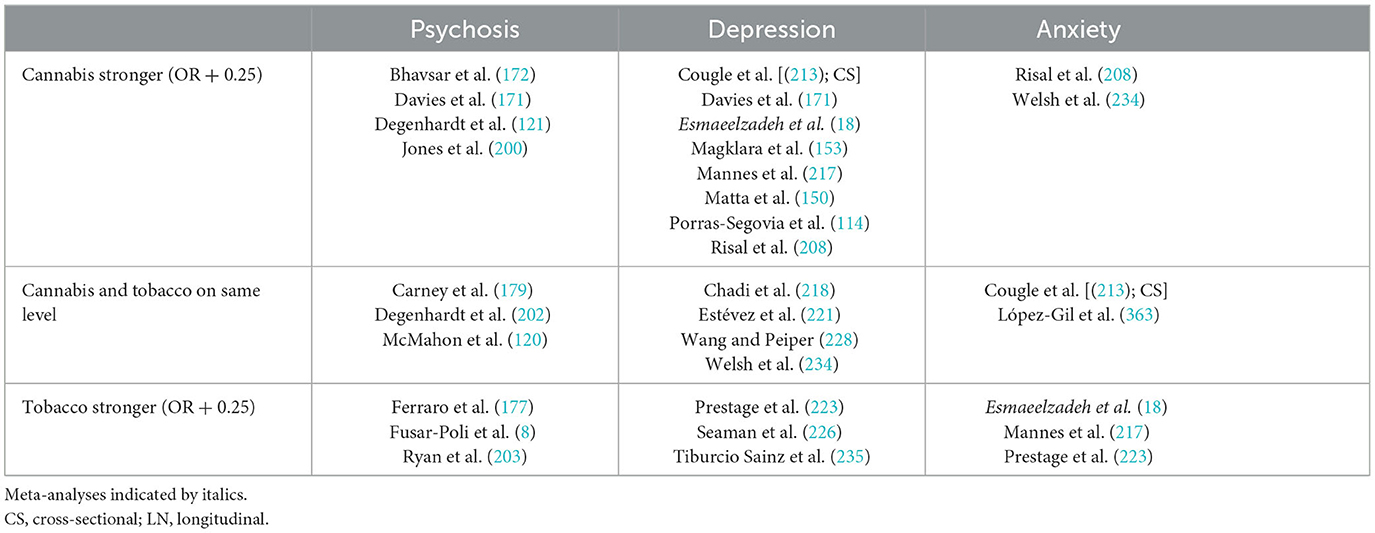
The second analysis focused on within-study comparisons. Some of the studies included in this review reported comparable figures for associations between cannabis use and psychosis as well as other disorders, and these figures are presented in Table 8 with an OR cut-off of 0.25. Longitudinal results related to having a mental disorder at baseline and subsequent initiation of cannabis or tobacco use have been ignored as they are not relevant for the comparison of putative harms resulting from the behavior. Unfortunately, only a few studies reported comparable figures, and there were no figures at all for ADHD and personality disorder. According to the available data, however, the strength of the association between cannabis use and psychosis seems to be at the same level as the strength of the associations between cannabis use and depression, anxiety, bipolar disorder, and PTSD. It appears that no reviews have investigated the associations between cannabis and psychosis as well as cannabis and other disorders at the same time.
It is worth mentioning that the study by Padwa et al. (151) found that cannabis use was also associated with a broad range of general medical disorders including circulatory system disease, digestive system disease, and musculoskeletal disease. The strength of these associations was broadly at the same level as the strength of the associations with mental disorders.
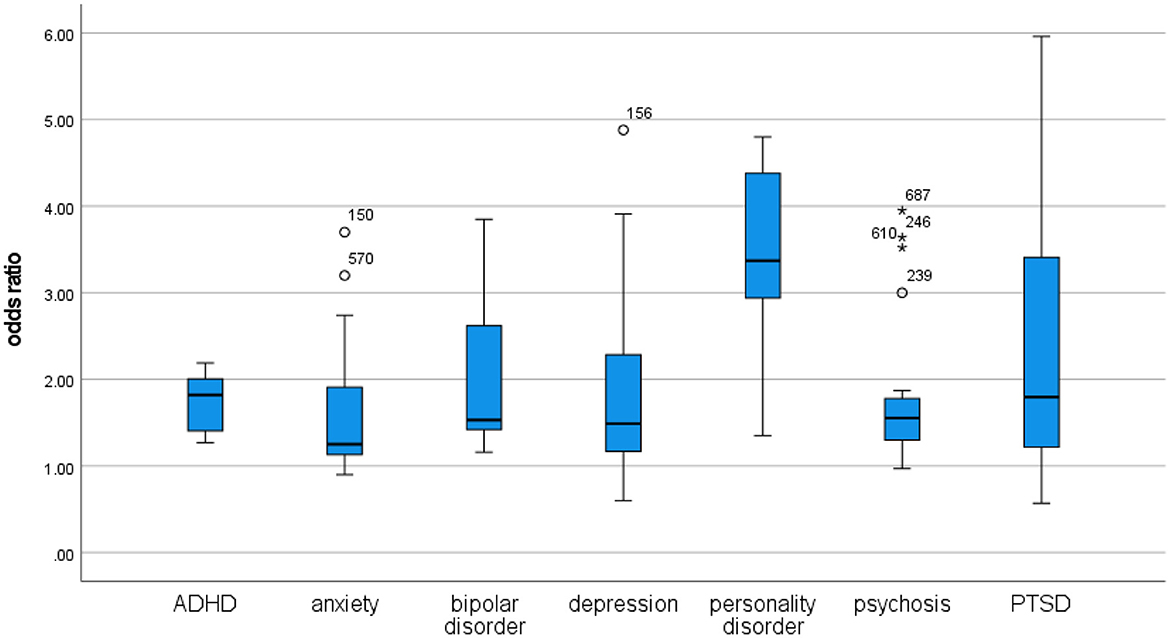
Aim 2: understand individual associations between a given unhealthy behavior and a given mental disorder in relation to other such behaviors
Two analyses compared the strength of associations between different unhealthy behaviors and a given mental disorder. The first such analysis compared the means and spreads for each disorder between different studies. The boxplots of Figures 3–9 sum up this analysis for each disorder in cross-sectional studies, while boxplots for longitudinal (behavior before disorder) studies are available in the Supplementary Figures A3–A6. Note that in order to improve the quality of presentation, one outlier study (152) with a very high OR of 28.19 has been removed from the figures for depression.
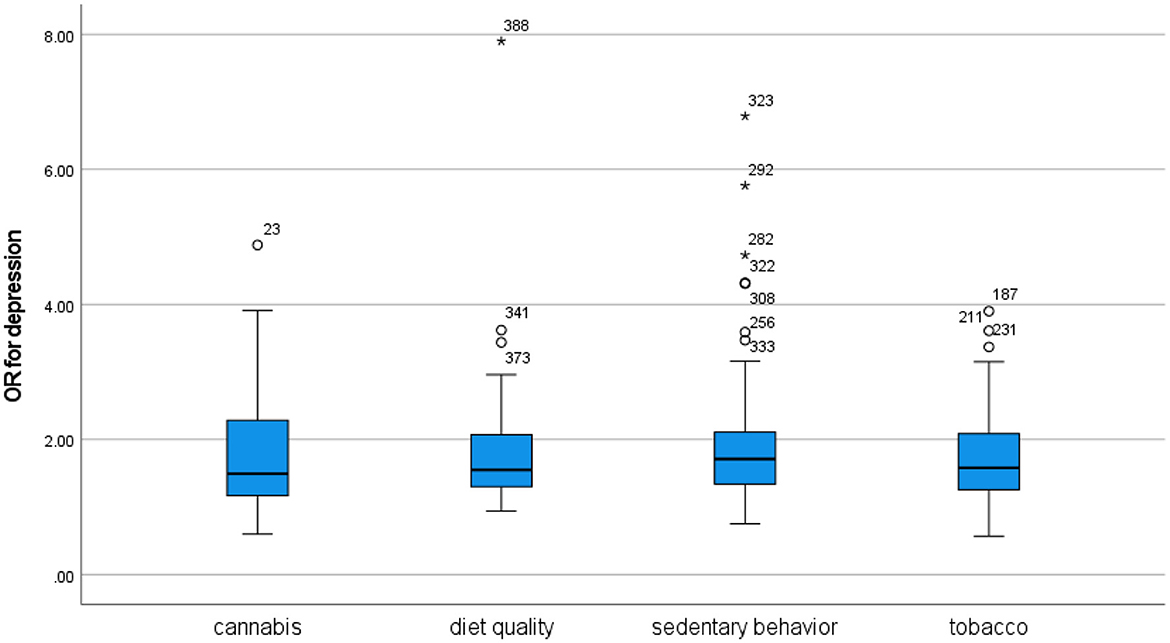
Figure 4. Odds ratios for depression in cross-sectional studies. In order to improve the quality of presentation, one outlier study (152) with a very high OR of 28.19 for diet quality and depression has been removed.
For the overall comparisons between cannabis and tobacco, t-tests indicated that only the figures for personality disorder were significantly different from each other (t = 3.13, df = 4, two-sided p = 0.007) in cross-sectional studies. There were no significant differences for longitudinal (behavior before disorder) findings. There were also no significant differences between cannabis and diet quality studies, although the number of studies available for each analysis was sometimes very small. For comparisons between cross-sectional studies of cannabis and sedentary behavior, t-tests indicated that the figures for ADHD (t = 1.83, df = 9.33, two-sided p = 0.099) were marginally significant. Tobacco use tended toward lower-strength associations with mental disorders than sedentary behavior and poor diet quality in cases where there were enough studies to make meaningful comparisons. These comparisons (with sedentary behavior and diet quality combined) reached significance for ADHD (t = 2.56, df = 19.94, two-sided p = 0.019). There were no significant differences between sedentary behavior and diet quality.
Weighted means gave emphasis to a single large-N, high-OR study of sedentary behavior and psychosis that made the cross-sectional association between sedentary behavior and psychosis appear to be substantially stronger especially than the association for cannabis. The weighing also gave emphasis to a single large-N study of sedentary behavior and bipolar disorder that made sedentary behavior seem protective against this disorder. Weighted means otherwise supported a difference between cannabis and tobacco with regard to personality disorder, but tended to mitigate the differences between cannabis use and sedentary behavior with regard to ADHD and PTSD. For longitudinal studies, weighing tended to reduce differences in odds ratio means between the different behaviors.
The second analysis focused on within-study comparisons. Some of the studies included in this review reported comparable figures for associations between different behaviors and a specific mental disorder, and these figures are presented in Table 9 with an OR cut-off of 0.25. In order to qualify as comparable, figures should reflect light, moderate or high use of both cannabis and tobacco, although exceptions were made for cases where differences in association strength were maintained despite a divergence in behavior intensity that presumably weakened the strongest association. In Magklara et al. (153), for instance, ever-use of cannabis incurred a higher OR for depression than daily use of tobacco, and this finding has been added to Table 9 despite the sub-moderate threshold for inclusion in the cannabis group. Longitudinal results related to having a mental disorder at baseline and subsequent initiation of cannabis or tobacco use have been ignored as they are not relevant for the comparison of putative harms resulting from the behavior.
We see in Table 9 that cannabis and tobacco appear to be associated with psychosis and anxiety at about the same level. For depression, the association for cannabis appears to be slightly stronger than that for tobacco. Other disorders were less commonly studied, but Supplementary Table A9 indicates that cannabis may be more strongly associated with personality disorder and perhaps ADHD than tobacco is, while the very limited evidence available indicates that their association with bipolar disorder and PTSD is about equally strong.
Table 10 compares diet quality and sedentary behavior to cannabis and (most commonly) tobacco use. Depression is fairly well-studied, and it appears that the association with diet quality and sedentary behavior is at the same level as the association with cannabis/tobacco use. Less evidence is available for psychosis and anxiety, but the evidence for psychosis seems to indicate that the association with diet quality and sedentary behavior is at least as strong as the association with cannabis/tobacco use, while the opposite may be true for anxiety. Very limited evidence for ADHD and PTSD indicates that the associations with diet quality and sedentary behavior are as strong or stronger than the associations with cannabis/tobacco use (Supplementary Table A10).
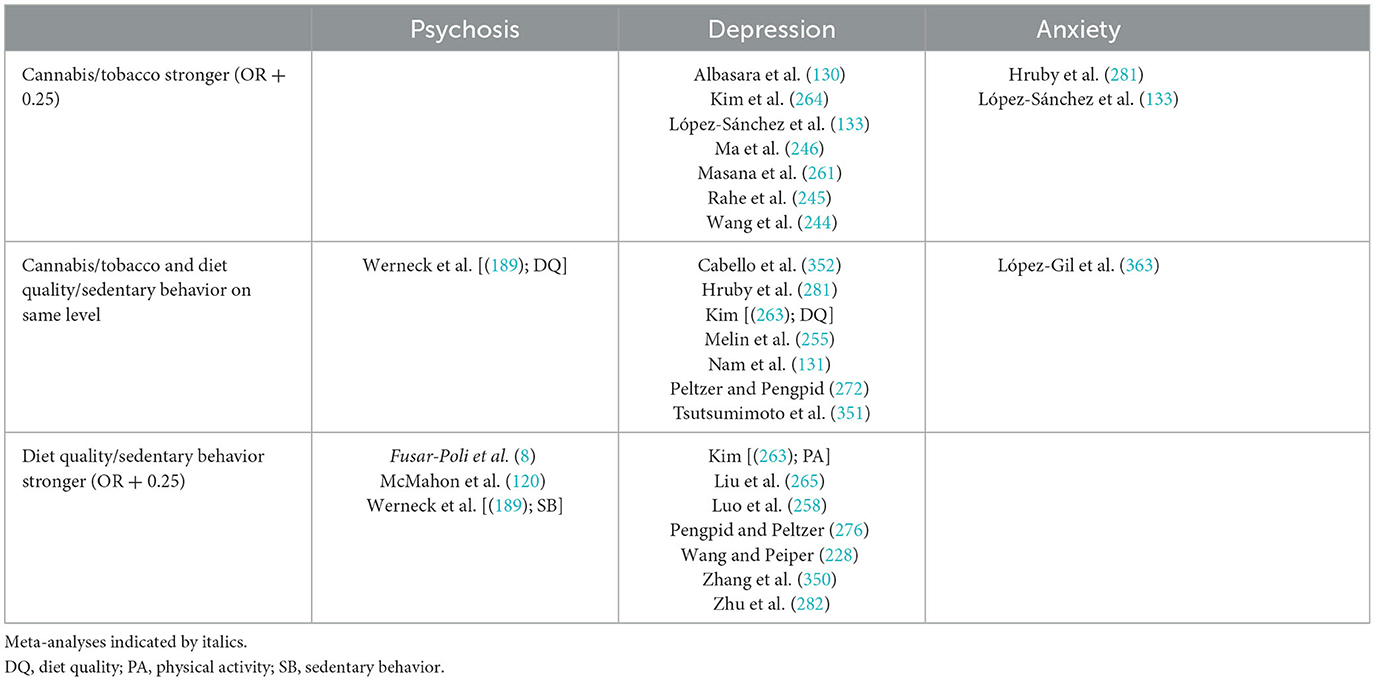
Table 10. Associations between cannabis/tobacco and psychiatric disorders compared to diet quality and sedentary behavior.
Discussion
Aim 1: understand individual associations between a given unhealthy behavior and a given mental disorder in relation to other such disorders
According to the findings of this comparative review, the association between a given behavior and a given disorder tended to resemble similar associations with other disorders. Some disorders distinguished themselves as particularly weakly or strongly associated with a given behavior, such as psychosis and anxiety for tobacco use and PTSD for sedentary behavior and diet quality, but even in these cases the differences were of moderate magnitude. Taking the cannabis-psychosis association as a basis for comparison, it appears that cannabis use is not more strongly associated with psychosis than with the other disorders. Comparisons across studies and within studies both supported this conclusion. However, personality disorder appeared to be more strongly associated with cannabis use than what is the case for psychosis and other disorders. Furthermore, in some of the sensitivity analyses that removed specific groups of studies from the dataset, cannabis use appeared to be more strongly associated with PTSD than with psychosis. Thus, in contrast to the consensus paper by D'Souza et al. (1), which used a single study by Starzer et al. (137) as the basis for inferring that “[c]annabis is more likely to be associated with psychosis outcomes than other psychiatric diagnoses” (p. 732), this review found that cannabis use is equally strongly associated with a range of different mental disorders, with only personality disorder (and perhaps PTSD) distinguishing themselves in terms of being especially strongly associated with cannabis use. D'Souza et al.'s (1) identification of the specificity of the cannabis-psychosis relationship as an indication that this relationship may reflect a causal effect from cannabis use, as per the classic criteria by Hill (112), is therefore unsupported by the present review.
This conclusion should not be especially susceptible to variation in behavior intensity, as moderate (weekly) cannabis use was emphasized in findings across different disorders. Nevertheless, sensitivity analyses did identify disparities related to sample groups, behavioral measurement, and control variables that may have impacted findings. Within-study analyses should be immune to such effects as the studies included in these analyses utilized the same participant samples and control variables, however.
Aim 2: understand individual associations between a given unhealthy behavior and a given mental disorder in relation to other such behaviors
The general finding from this review was that the association between a given behavior and a given disorder tended to resemble similar associations for other behaviors. Thus, it appears that moderate use of cannabis is about as strongly associated with mental disorders as is moderate use of tobacco and high use of fast food, sugary beverages, and television. In terms of their respective behavior intensity, conceptualized as the behavior related to the median-area odds ratio in cross-sectional studies, cannabis use ranging from any exposure via weekly or current use to use disorder appears to be about as harmful as tobacco use ranging from any exposure via daily, regular or current use to use disorder. Both of these, in turn, appear to be about as harmful as behavior ranging from 2 to 4 h of daily screen time, 4 to 10 h of daily inactivity, or daily ingestion of sweets, sodas, and fast food up to binge eating or the disordered use of computer games, Facebook or the internet. The only statistically significant divergence at the 0.05 level related to personality disorder, which was more strongly associated with moderate cannabis use than with moderate tobacco use.
Within-study comparisons generally supported this conclusion, although with some variation for depression and ADHD. Thus, in contrast to the consensus paper by D'Souza et al. (1) that drew the inference that “[t]he risk for a psychosis outcome is highest for cannabis relative to other drugs” (p. 732), this review found that the association between cannabis use and psychosis is about equally strong as the association between psychosis and tobacco use as well as the associations with sedentary behavior and poor diet quality. It should be acknowledged, however, that the latter two seem not to have been intensively studied, and that variation in behavior intensity may have affected overall findings. This review emphasized moderate cannabis and tobacco use, operationalized as weekly cannabis use and daily tobacco use of around 10 cigarettes, as compared to high levels of sedentary behavior and poor diet quality. If the review had instead focused on high levels of cannabis use, the comparison would probably have favored tobacco use, sedentary behavior, and poor diet quality as less harmful behaviors.
There are, however, several reasons to focus on moderate (weekly) rather than high (daily or more) cannabis use in harms assessments. Heavy use of intoxicants typically reflects motivations related to coping, and such motivations are normally related to underlying problems that are themselves associated with risk for mental disorder (13). Furthermore, the frequent use of intoxicants may exacerbate such underlying problems via social mechanisms that are not directly related to the pharmacological effects of the intoxicant itself. A person who engages in frequent daytime intoxicant use will incur a range of negative consequences in terms of employment and social relations irrespective of whether the intoxicant is cannabis, alcohol, or some other substance, and these negative consequences will often exacerbate the underlying problems that motivate the frequent intoxicant use in the first place. Studies of such behaviors will therefore tend to conflate negative consequences incurred via social mechanisms and negative consequences incurred via pharmacological mechanisms. In order to avoid such conflation of effects and constrain the measurement of consequences toward those that are of a pharmacological nature, it would be advisable to focus on moderate intoxicant use.
The findings of this review could be understood in relation to Nutt's (154) comparison of the harms related to MDMA use and horse riding. Both studies related the risks incurred by substance use to risks incurred by ordinary and socially acceptable activities, and found that despite their negative reputation, use of substances such as MDMA, cannabis, and tobacco do not appear to be more harmful than these ordinary activities.
Aim 3: understand the association between unhealthy behaviors and mental disorders in relation to statistical control for covariates
This review constructed dichotomous indicators for covariate adjustment in order to better understand the overall impact of such adjustment on studies of associations between unhealthy behaviors and mental disorders. The most influential of these adjustment indicators were those for cannabis and tobacco use, which reached significance at the 0.05 level in overall correlation with odds ratios across disorders in non-cannabis and non-tobacco studies, respectively. This finding allows for the conclusion that failing to control for cannabis and tobacco use, both of which tend toward collinearity both with each other and with other unhealthy behaviors as well as with a number of mental disorders, entails an exaggeration of the strength of the association under scrutiny. In other words, failing to control for cannabis and tobacco use in studies of unhealthy behaviors and mental disorders may amount to analytical malpractice. At a minimum, such studies should report comparable figures for cannabis and/or tobacco so that readers may calibrate the results presented for the unhealthy behavior under scrutiny in comparison to figures for cannabis and tobacco use.
The indicator for adjustment for diet quality and/or sedentary behavior was not correlated with odds ratios in cannabis and tobacco studies, but the inclusion of such adjustment was also so uncommon that the overall statistics of its impact may not be trustworthy. This applies especially to cannabis, as only 1% of cannabis studies controlled for diet quality and/or sedentary behavior and only 8% of studies of the latter behaviors controlled for cannabis use. It thus appears that researchers tend to understand cannabis use and poor diet quality/sedentary behavior as conceptually distinct, with cannabis use constituting a form of very harmful drug use whereas frequent consumption of fast food or television merely constitutes an unhealthy lifestyle choice. The findings of this review indicate that any such distinction, at least with regard to moderate cannabis use, is probably illusory, as weekly cannabis use appears to be about equally harmful as weekly to daily consumption of cheeseburgers.
Tobacco use appears to be positioned somewhat more closely to poor diet quality/sedentary behavior on a conceptual level. A majority (55%) of studies of the latter behaviors controlled for tobacco use, and the 14% of tobacco studies which controlled for diet quality and/or sedentary behavior at least outnumber the corresponding number of cannabis studies (1%) by a wide margin. Thus, there is some evidence of a tendency among researchers to understand tobacco use as a form of unhealthy behavior that is conceptually related to other unhealthy behaviors that do not involve substance use.
The indicator for bivariate analysis was also fairly influential on overall odds ratios, although perhaps not to the extent that one would expect. Only a small number of studies reported bivariate figures, and in comparative analyses with many included studies we would expect the influence from bivariate figures to cancel each other out on average. Sensitivity analyses that removed the studies with bivariate figures from the dataset introduced differences, albeit of marginal significance, relating to the association between cannabis use and PTSD. It would therefore appear that studies investigating the cannabis-PTSD relationship were especially impacted by figures lacking statistical control.
Indicators for trauma and misery adjustment had some influence on overall odds ratios and localized impact of a more substantial nature on findings related to specific disorders and behaviors. It is therefore true to say that the methods used to analyze the impact from trauma and misery on the studies included in this review did not identify a major impact on association strengths. Nevertheless, since this review focused on behaviors of moderate intensity for tobacco and cannabis use, the finding of a tentative or light influence could be said to reflect expectations. Moderate use was here conceptualized as use driven by a broad range of motivations, in contradistinction to the heavy use understood as being more often driven by coping motivations related to underlying trauma and misery. As such, one would expect that indicators for trauma and misery adjustment would have a more substantial impact on analyses of heavy substance use than what was the case in the present review.
It is important to note that if the association between substance use and mental disorder reflects, to some meaningful extent, an association between substance use and underlying factors of trauma and misery, then overall changes in the user population toward or away from more widespread use should be accompanied by corresponding changes to the strength of the association between the substance use and mental disorder. When the use of a given substance becomes more prevalent, at least in terms of large-scale changes, this normally reflects an acceptance of this substance among people who are driven primarily not by coping motives but by recreational, social, enhancement or expansion motives. Similarly, when the use of a previously prevalent substance is reduced, this normally reflects reduced acceptance of the given substance among people driven primarily by non-coping motives. In the western world, recent decades have seen reduced acceptance of tobacco use and increased acceptance of cannabis use, and we would therefore expect an increasing association between mental disorder and tobacco use along with a decreasing association for cannabis use.
These expectations are supported by research findings. Talati et al. (155) found that while overall tobacco use declined in the U.S. from the 1940s to 1980s, the proportion of smokers with nicotine dependence increased from 31% to 70% and the number of dependent smokers with depression, ADHD, bipolar disorder, and personality disorder increased significantly more than among non-smokers. In Canada, Yang and D'Arcy (156) similarly found that depression among older adults smokers increased substantially more than among non-smokers over the years 1994–2014. For cannabis, several studies have found increases in overall use without corresponding increases in cannabis use disorder (157–165), although there is also some conflicting evidence (166–168). Changes in associations with mental disorders have not been intensively explored, but one study by Livne et al. (169) found that “the association between cannabis use (but not CUDs) and dysthymia has weakened over time” (p. 327). If ongoing policy liberalization continues, the proportion of users with use disorder might be expected to further weaken, and the same could be said for the association between overall cannabis use and mental disorders.
Limitations
Beyond the classification of specialty samples, behavioral measurement disparities, and statistical control for social misery and psychological trauma, this review has not assessed the methodological validity of the studies included. In particular, their utilization of healthy controls for patient samples and their construction of samples putatively representing the general population have not been assessed. Relatedly, the review has not accounted for variation in the measurement of mental disorders, which is a possible confounder to the comparative analyses. It is also possible that the focus on studies presenting their findings in terms of odds ratios may constitute a source of bias, although there is no particular reason to believe that findings presented as odds ratios should be stronger or weaker than findings presented as hazard ratios or in some other way.
The dichotomous indicator variables for trauma and misery adjustment constructed in this review might be criticized for being overly simplistic. It is possible that a more complex set of adjustment indicators would have been more sensitive for nuanced variations in covariate regimes in the included studies. A high percentage of these studies controlled for education, but although education is correlated with poverty and unemployment, adjustment for this single variable by no means exhausts the impact from social misery on unhealthy behaviors and mental disorders. Adjustment for psychological trauma was far less common, making a single dichotomous indicator more appropriate.
This review was limited to records from the Pubmed database published in 2015 or later. Such a selection of recent studies registered in Pubmed may have served to introduce bias in overall findings, although the author is not aware of any reason to believe that the Pubmed database is systematically different from other databases. As such, the present selection of studies could arguably be regarded as representative of the full population of such studies. Nevertheless, the present findings should be regarded as tentative and explorative until confirmed by more comprehensive investigations.
Furthermore, this review has analyzed and compared included studies at the level of their published findings rather than in terms of their underlying data. While this approach arguably yielded noteworthy results, it would undoubtedly be interesting to perform a comparative meta-analysis of the datasets for the behaviors and disorders here under purview. Such a meta-analysis would probably have to limit its scope as compared to the present review, but would allow for a more comprehensive understanding of the tentative findings obtained here. It should also be noted that the author of the present review performed all the assessments and analyses singlehandedly, increasing the risk of bias. Inter-rater reliability therefore could not be established. Moreover, the comparisons reported in this review were not Bonferroni corrected, and because 252 separate analyses were performed it is unlikely that any association would have maintained statistical significance after such correction.
Publication bias should be assumed to have affected the results presented in this review. Indeed, it was not infrequently the case that studies which investigated several relationships between unhealthy behaviors and disorders only reported odds ratios for those relationships that were statistically significant. Unless there is reason to believe that such bias should have affected some relationships substantially more than others, however, the comparative perspective of this review probably entails that publication bias on each side of the comparison would tend to cancel each other out.
It must be acknowledged that this review compared a broad range of studies across different populations and participant samples, although the same is true for more narrow reviews examining only one of these behavior-disorder relationships (17). Variation related to specialty samples, behavioral measurement disparities, and control variables did not appear to have a major impact on overall findings, which were largely robust across relevant sensitivity analyses. The findings should nevertheless be regarded as explorative and interpreted with caution. While further research is necessary in order to confirm the results obtained in this review, the apparent convergence of the strength of associations between four different types of unhealthy behaviors and seven different mental disorders is a noteworthy if tentative basis for further investigations.
A useful extension to the comparisons in this review would be to include studies of alcohol. As an intoxicant, alcohol may constitute a closer parallel to cannabis than the other unhealthy behaviors under scrutiny in this review, and it seems possible to compare the two in terms of both moderate use and heavy chronic use. It would also be interesting to extend such comparisons to other illicit drugs, although the associations between such drug use and mental disorder may not yet have been studied to such an extent that it is meaningful to include them in a comparative review.
Conclusion
According to this review, the association between moderate cannabis use and mental disorder is about equally strong for psychosis, depression, anxiety, bipolar disorder, ADHD, and PTSD, while the less intensively studied association with personality disorder appears to be somewhat stronger than the others. Furthermore, these associations with cannabis use appear to be paralleled by associations with tobacco use, poor diet quality, and sedentary behavior at about the same strength, although once more with personality disorder as an exception. As such, the often-emphasized association between cannabis use and psychosis appears to lack specificity both across disorders and across behaviors.
When a broad range of different unhealthy behaviors appear to be about equally strongly associated with a broad range of mental disorders, we should probably understand them to reflect a general and shared etiology. The best candidate for a general explanation is arguably that this broad range of associations reflect underlying psychological trauma and social misery, which frequently appear together. Thus, the associations identified in this review may not represent a causal effect from the unhealthy behavior itself so much as a spurious relationship where both the behavior and the disorder are caused by underlying factors such as psychological trauma and social misery. Nevertheless, it should be noted that the analyses employed in the present review did not identify a major impact from variation in statistical control for such factors. Because of its exceptional strength, it is possible that the association between cannabis use and personality disorder constitutes an exception to this general explanation, although more research is required.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
PJ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing—original draft, Writing—review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1268339/full#supplementary-material
References
1. D'Souza DC, DiForti M, Ganesh S, George TP, Hall W, Hjorthøj C, et al. Consensus paper of the WFSBP task force on cannabis, cannabinoids and psychosis. World J Biol Psychiatry. (2022) 23:719–42. doi: 10.1080/15622975.2022.2038797
2. Gage SH, Hickman M, Zammit S. Association between cannabis and psychosis: epidemiologic evidence. Biol Psychiatry. (2016) 79:549–56. doi: 10.1016/j.biopsych.2015.08.001
3. Kiburi SK, Molebatsi K, Ntlantsana V, Lynskey MT. Cannabis use in adolescence and risk of psychosis: are there factors that moderate this relationship? A systematic review and meta-analysis. Subst Abuse. (2021) 42:527–42. doi: 10.1080/08897077.2021.1876200
4. Kraan T, Velthorst E, Koenders L, Zwaart K, Ising HK, van den Berg D, et al. Cannabis use and transition to psychosis in individuals at ultra-high risk: review and meta-analysis. Psychol Med. (2016) 46:673–81. doi: 10.1017/S0033291715002329
5. Marconi A, Di Forti M, Lewis CM, Murray RM, Vassos E. Meta-analysis of the association between the level of cannabis use and risk of psychosis. Schizophr Bull. (2016) 42:1262–9. doi: 10.1093/schbul/sbw003
6. Robinson T, Ali MU, Easterbrook B, Hall W, Jutras-Aswad D, Fischer B. Risk-thresholds for the association between frequency of cannabis use and the development of psychosis: a systematic review and meta-analysis. Psychol Med. (2023) 53:3858–68. doi: 10.1017/S0033291722000502
7. Farris MS, Shakeel MK, Addington J. Cannabis use in individuals at clinical high-risk for psychosis: a comprehensive review. Soc Psychiatry Psychiatr Epidemiol. (2020) 55:527–37. doi: 10.1007/s00127-019-01810-x
8. Fusar-Poli P, Tantardini M, De Simone S, Ramella-Cravaro V, Oliver D, Kingdon J, et al. Deconstructing vulnerability for psychosis: meta-analysis of environmental risk factors for psychosis in subjects at ultra high-risk. Eur Psychiatry. (2017) 40:65–75. doi: 10.1016/j.eurpsy.2016.09.003
9. De Micheli A, Provenzani U, Solmi M, Van Lawick Van Pabst A, Youssef E, McGuire P, et al. Prevalence of tobacco smoking in people at clinical high-risk for psychosis: systematic review and meta-analysis. Schizophr Res. (2023) 254:109–15. doi: 10.1016/j.schres.2023.02.008
10. Gurillo P, Jauhar S, Murray RM, MacCabe JH. Does tobacco use cause psychosis? Systematic review and meta-analysis. Lancet Psychiatry. (2015) 2:718–25. doi: 10.1016/S2215-0366(15)00152-2
11. Hunter A, Murray R, Asher L, Leonardi-Bee J. The effects of tobacco smoking, and prenatal tobacco smoke exposure, on risk of schizophrenia: a systematic review and meta-analysis. Nicotine Tob Res. (2020) 22:3–10. doi: 10.1093/ntr/nty160
12. Stevenson J, Miller CL, Martin K, Mohammadi L, Lawn S. Investigating the reciprocal temporal relationships between tobacco consumption and psychological disorders for youth: an international review. BMJ Open. (2022) 12:e055499. doi: 10.1136/bmjopen-2021-055499
13. Johnstad PG. Comparative harms assessments for cannabis, alcohol, and tobacco: risk for psychosis, cognitive impairment, and traffic accident. Drug Sci Policy Law. (2022) 8:1–20. doi: 10.1177/20503245221095228
14. Teasdale SB, Ward PB, Samaras K, Firth J, Stubbs B, Tripodi E, et al. Dietary intake of people with severe mental illness: systematic review and meta-analysis. Br J Psychiatry. (2019) 214:251–9. doi: 10.1192/bjp.2019.20
15. van Zonneveld SM, Haarman BCM, van den Oever EJ, Nuninga JO, Sommer IEC. Unhealthy diet in schizophrenia spectrum disorders. Curr Opin Psychiatry. (2022) 35:177–85. doi: 10.1097/YCO.0000000000000791
16. Brokmeier LL, Firth J, Vancampfort D, Smith L, Deenik J, Rosenbaum S, et al. Does physical activity reduce the risk of psychosis? A systematic review and meta-analysis of prospective studies. Psychiatry Res. (2020) 284:112675. doi: 10.1016/j.psychres.2019.112675
17. Vancampfort D, Firth J, Schuch FB, Rosenbaum S, Mugisha J, Hallgren M, et al. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: a global systematic review and meta-analysis. World Psychiatry. (2017) 16:308–15. doi: 10.1002/wps.20458
18. Esmaeelzadeh S, Moraros J, Thorpe L, Bird Y. Examining the association and directionality between mental health disorders and substance use among adolescents and young adults in the U.S. and Canada – a systematic review and meta-analysis. J Clin Med. (2018)7:543. doi: 10.3390/jcm7120543
19. Gobbi G, Atkin T, Zytynski T, Wang S, Askari S, Boruff J, et al. Association of cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood: a systematic review and meta-analysis. JAMA Psychiatry. (2019) 76:426–34. doi: 10.1001/jamapsychiatry.2018.4500
20. Hasin D, Walsh C. Cannabis use, cannabis use disorder, and comorbid psychiatric illness: a narrative review. J Clin Med. (2021) 10:15. doi: 10.3390/jcm10010015
21. Hunt GE, Malhi GS, Lai HMX, Cleary M. Prevalence of comorbid substance use in major depressive disorder in community and clinical settings, 1990-2019: systematic review and meta-analysis. J Affect Disord. (2020) 266:288–304. doi: 10.1016/j.jad.2020.01.141
22. Kaur N, Bastien G, Gagnon L, Graham J, Mongeau-Pérusse V, Bakouni H, et al. Variations of cannabis-related adverse mental health and addiction outcomes across adolescence and adulthood: a scoping review. Front Psychiatry. (2022) 13:973988. doi: 10.3389/fpsyt.2022.973988
23. Kuhns L, Kroon E, Colyer-Patel K, Cousijn J. Associations between cannabis use, cannabis use disorder, and mood disorders: longitudinal, genetic, and neurocognitive evidence. Psychopharmacology. (2022) 239:1231–49. doi: 10.1007/s00213-021-06001-8
24. Langlois C, Potvin S, Khullar A, Tourjman SV. Down and high: reflections regarding depression and cannabis. Front Psychiatry. (2021) 12:625158. doi: 10.3389/fpsyt.2021.625158
25. Lucatch AM, Coles AS, Hill KP, George TP. Cannabis and mood disorders. Curr Addict Rep. (2018) 5:336–45. doi: 10.1007/s40429-018-0214-y
26. Onaemo VN, Fawehinmi TO, D'Arcy C. Comorbid cannabis use disorder with major depression and generalized anxiety disorder: a systematic review with meta-analysis of nationally representative epidemiological surveys. J Affect Disord. (2021) 281:467–75. doi: 10.1016/j.jad.2020.12.043
27. Patten SB. Cannabis and non-psychotic mental disorders. Curr Opin Psychol. (2021) 38:61–6. doi: 10.1016/j.copsyc.2020.09.006
28. Urits I, Gress K, Charipova K, Li N, Berger AA, Cornett EM, et al. Cannabis use and its association with psychological disorders. Psychopharmacol Bull. (2020) 50:56–67.
29. Botsford SL, Yang S, George TP. Cannabis and cannabinoids in mood and anxiety disorders: impact on illness onset and course, and assessment of therapeutic potential. Am J Addict. (2020) 29:9–26. doi: 10.1111/ajad.12963
30. Lev-Ran S, Roerecke M, Le Foll B, George TP, McKenzie K, Rehm J. The association between cannabis use and depression: a systematic review and meta-analysis of longitudinal studies. Psychol Med. (2014) 44:797–810. doi: 10.1017/S0033291713001438
31. Weinberger AH, Kashan RS, Shpigel DM, Esan H, Taha F, Lee CJ, et al. Depression and cigarette smoking behavior: a critical review of population-based studies. Am J Drug Alcohol Abuse. (2017) 43:416–31. doi: 10.3109/00952990.2016.1171327
32. Fluharty M, Taylor AE, Grabski M, Munafò MR. The association of cigarette smoking with depression and anxiety: a systematic review. Nicotine Tob Res. (2017) 19:3–13. doi: 10.1093/ntr/ntw140
33. Groenman AP, Janssen TWP, Oosterlaan J. Childhood psychiatric disorders as risk factor for subsequent substance abuse: a meta-analysis. J Am Acad Child Adolesc Psychiatry. (2017) 56:556–69. doi: 10.1016/j.jaac.2017.05.004
34. Zeng YN, Li YM. Secondhand smoke exposure and mental health in adults: a meta-analysis of cross-sectional studies. Soc Psychiatry Psychiatr Epidemiol. (2016) 51:1339–48. doi: 10.1007/s00127-015-1164-5
35. Han C, Liu Y, Gong X, Ye X, Zhou J. Relationship between secondhand smoke exposure and depressive symptoms: a systematic review and dose–response meta-analysis. Int J Environ Res Public Health. (2019) 16:1356. doi: 10.3390/ijerph16081356
36. Becker TD, Arnold MK, Ro V, Martin L, Rice TR. Systematic review of electronic cigarette use (vaping) and mental health comorbidity among adolescents and young adults. Nicotine Tob Res. (2021) 23:415–25. doi: 10.1093/ntr/ntaa171
37. Livingston JA, Chen CH, Kwon M, Park E. Physical and mental health outcomes associated with adolescent E-cigarette use. J Pediatr Nurs. (2022) 64:1–17. doi: 10.1016/j.pedn.2022.01.006
38. González-Bueso V, Santamaría JJ, Fernández D, Merino L, Montero E, Ribas J. Association between internet gaming disorder or pathological video-game use and comorbid psychopathology: a comprehensive review. Int J Environ Res Public Health. (2018) 15:668. doi: 10.3390/ijerph15040668
39. Hallgren M, Dunstan DW, Owen N. Passive versus mentally active sedentary behaviors and depression. Exerc Sport Sci Rev. (2020) 48:20–7. doi: 10.1249/JES.0000000000000211
40. Hoare E, Milton K, Foster C, Allender S. The associations between sedentary behaviour and mental health among adolescents: a systematic review. Int J Behav Nutr Phys Act. (2016) 13:108. doi: 10.1186/s12966-016-0432-4
41. Huang Y, Li L, Gan Y, Wang C, Jiang H, Cao S, et al. Sedentary behaviors and risk of depression: a meta-analysis of prospective studies. Transl Psychiatry. (2020) 10:26. doi: 10.1038/s41398-020-0715-z
42. Liu M, Wu L, Yao S. Dose-response association of screen time-based sedentary behaviour in children and adolescents and depression: a meta-analysis of observational studies. Br J Sports Med. (2016) 50:1252–8. doi: 10.1136/bjsports-2015-095084
43. Ramalho A, Petrica J, Rosado A. Sedentary behaviors and psychological outcomes among older adults: a systematic review. Motricidade. (2018) 14:73–85. doi: 10.6063/motricidade.12223
44. Schuch FB, Vancampfort D, Firth J, Rosenbaum S, Ward PB, Silva ES, et al. Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am J Psychiatry. (2018) 175:631–48. doi: 10.1176/appi.ajp.2018.17111194
45. Wang X, Li Y, Fan H. The associations between screen time-based sedentary behavior and depression: a systematic review and meta-analysis. BMC Public Health. (2019) 19:1524. doi: 10.1186/s12889-019-7904-9
46. Zhai L, Zhang Y, Zhang D. Sedentary behaviour and the risk of depression: a meta-analysis. Br J Sports Med. (2015) 49:705–9. doi: 10.1136/bjsports-2014-093613
47. Zhou Q, Guo C, Yang X, He N. Dose-response association of total sedentary behaviour and television watching with risk of depression in adults: a systematic review and meta-analysis. J Affect Disord. (2023) 324:652–9. doi: 10.1016/j.jad.2022.12.098
48. Hu D, Cheng L, Jiang W. Sugar-sweetened beverages consumption and the risk of depression: a meta-analysis of observational studies. J Affect Disord. (2019) 245:348–55. doi: 10.1016/j.jad.2018.11.015
49. Lane MM, Gamage E, Travica N, Dissanayaka T, Ashtree DN, Gauci S, et al. Ultra-processed food consumption and mental health: a systematic review and meta-analysis of observational studies. Nutrients. (2022) 14:2568. doi: 10.3390/nu14132568
50. Lassale C, Batty GD, Baghdadli A, Jacka F, Sánchez-Villegas A, Kivimäki M, et al. Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol Psychiatry. (2019) 24:965–86. doi: 10.1038/s41380-018-0237-8
51. Li Y, Lv MR, Wei YJ, Sun L, Zhang JX, Zhang HG, et al. Dietary patterns and depression risk: a meta-analysis. Psychiatry Res. (2017) 253:373–82. doi: 10.1016/j.psychres.2017.04.020
52. Malmir H, Mahdavi FS, Ejtahed HS, Kazemian E, Chaharrahi A, Mohammadian Khonsari N, et al. Junk food consumption and psychological distress in children and adolescents: a systematic review and meta-analysis. Nutr Neurosci. (2023) 26:807–27. doi: 10.1080/1028415X.2022.2094856
53. Marx W, Moseley G, Berk M, Jacka F. Nutritional psychiatry: the present state of the evidence. Proc Nutr Soc. (2017) 76:427–36. doi: 10.1017/S0029665117002026
54. Molendijk M, Molero P, Ortuño Sánchez-Pedreño F, Van der Does W, Angel Martínez-González M. Diet quality and depression risk: a systematic review and dose-response meta-analysis of prospective studies. J Affect Disord. (2018) 226:346–54. doi: 10.1016/j.jad.2017.09.022
55. Nicolaou M, Colpo M, Vermeulen E, Elstgeest LEM, Cabout M, Gibson-Smith D, et al. Association of a priori dietary patterns with depressive symptoms: a harmonised meta-analysis of observational studies. Psychol Med. (2020) 50:1872–83. doi: 10.1017/S0033291719001958
56. Wang J, Li R, Zhang L, Gao X, Zhou M, Zhang X, et al. Associations between sedentary behaviour patterns and depression among people aged 60 and older in Hebei Province of China. BMC Public Health. (2022) 22:283. doi: 10.1186/s12889-022-12727-7
57. Wu PY, Chen KM, Belcastro F. Dietary patterns and depression risk in older adults: systematic review and meta-analysis. Nutr Rev. (2021) 79:976–87. doi: 10.1093/nutrit/nuaa118
58. Wang Y, Zhao R, Wang B, Zhao C, Zhu B, Tian X. The dose-response associations of sugar-sweetened beverage intake with the risk of stroke, depression, cancer, and cause-specific mortality: a systematic review and meta-analysis of prospective studies. Nutrients. (2022) 14:777. doi: 10.3390/nu14040777
59. Li XH, An FR, Ungvari GS, Ng CH, Chiu HFK, Wu PP, et al. Prevalence of smoking in patients with bipolar disorder, major depressive disorder and schizophrenia and their relationships with quality of life. Sci Rep. (2017) 7:8430. doi: 10.1038/s41598-017-07928-9
60. Kedzior KK, Laeber LT. A positive association between anxiety disorders and cannabis use or cannabis use disorders in the general population–a meta-analysis of 31 studies. BMC Psychiatry. (2014) 14:136. doi: 10.1186/1471-244X-14-136
61. Twomey CD. Association of cannabis use with the development of elevated anxiety symptoms in the general population: a meta-analysis. J Epidemiol Community Health. (2017) 71:811–6. doi: 10.1136/jech-2016-208145
62. Xue S, Husain MI, Zhao H, Ravindran AV. Cannabis use and prospective long-term association with anxiety: a systematic review and meta-analysis of longitudinal studies. Can J Psychiatry. (2021) 66:126–38. doi: 10.1177/0706743720952251
63. Shalit N, Lev-Ran S. Does cannabis use increase anxiety disorders? A literature review. Curr Opin Psychiatry. (2020) 33:8–13. doi: 10.1097/YCO.0000000000000560
64. Stiles-Shields C, Archer J, Zhang J, Burnside A, Draxler J, Potthoff LM, et al. A scoping review of associations between cannabis use and anxiety in adolescents and young adults. Child Psychiatry Hum Dev. (2021) 54:639–58. doi: 10.1007/s10578-021-01280-w
65. Moylan S, Jacka FN, Pasco JA, Berk M. Cigarette smoking, nicotine dependence and anxiety disorders: a systematic review of population-based, epidemiological studies. BMC Med. (2012) 10:123. doi: 10.1186/1741-7015-10-123
66. Vorspan F, Mehtelli W, Dupuy G, Bloch V, Lépine JP. Anxiety and substance use disorders: co-occurrence and clinical issues. Curr Psychiatry Rep. (2015) 17:4. doi: 10.1007/s11920-014-0544-y
67. Zimmermann M, Chong AK, Vechiu C, Papa A. Modifiable risk and protective factors for anxiety disorders among adults: a systematic review. Psychiatry Res. (2020) 285:112705. doi: 10.1016/j.psychres.2019.112705
68. Allen MS, Walter EE, Swann C. Sedentary behaviour and risk of anxiety: a systematic review and meta-analysis. J Affect Disord. (2019) 242:5–13. doi: 10.1016/j.jad.2018.08.081
69. McDowell CP, Gordon BR, Andrews KL, MacDonncha C, Herring MP. Associations of physical activity with anxiety symptoms and status: results from The Irish Longitudinal Study of Ageing. Epidemiol Psychiatr Sci. (2019) 28:436–45. doi: 10.1017/S204579601800001X
70. Schuch FB, Stubbs B, Meyer J, Heissel A, Zech P, Vancampfort D, et al. Physical activity protects from incident anxiety: a meta-analysis of prospective cohort studies. Depress Anxiety. (2019) 36:846–58. doi: 10.1002/da.22915
71. Teychenne M, Costigan SA, Parker K. The association between sedentary behaviour and risk of anxiety: a systematic review. BMC Public Health. (2015) 15:513. doi: 10.1186/s12889-015-1843-x
72. McDowell CP, Dishman RK, Gordon BR, Herring MP. Physical activity and anxiety: a systematic review and meta-analysis of prospective cohort studies. Am J Prev Med. (2019) 57:545–56. doi: 10.1016/j.amepre.2019.05.012
73. Gibbs M, Winsper C, Marwaha S, Gilbert E, Broome M, Singh SP. Cannabis use and mania symptoms: a systematic review and meta-analysis. J Affect Disord. (2015) 171:39–47. doi: 10.1016/j.jad.2014.09.016
74. Hunt GE, Malhi GS, Cleary M, Lai HM, Sitharthan T. Prevalence of comorbid bipolar and substance use disorders in clinical settings, 1990-2015: systematic review and meta-analysis. J Affect Disord. (2016) 206:331–49. doi: 10.1016/j.jad.2016.07.011
75. Lalli M, Brouillette K, Kapczinski F, de Azevedo Cardoso T. Substance use as a risk factor for bipolar disorder: a systematic review. J Psychiatr Res. (2021) 144:285–95. doi: 10.1016/j.jpsychires.2021.10.012
76. Marangoni C, Hernandez M, Faedda GL. The role of environmental exposures as risk factors for bipolar disorder: a systematic review of longitudinal studies. J Affect Disord. (2016) 193:165–74. doi: 10.1016/j.jad.2015.12.055
77. Pinto JV, Medeiros LS, Santana da Rosa G, Santana de Oliveira CE, Crippa JAS, Passos IC, et al. The prevalence and clinical correlates of cannabis use and cannabis use disorder among patients with bipolar disorder: a systematic review with meta-analysis and meta-regression. Neurosci Biobehav Rev. (2019) 101:78–84. doi: 10.1016/j.neubiorev.2019.04.004
78. Sideli L, Quigley H, La Cascia C, Murray RM. Cannabis use and the risk for psychosis and affective disorders. J Dual Diagn. (2020) 16:22–42. doi: 10.1080/15504263.2019.1674991
79. Jackson JG, Diaz FJ, Lopez L, de Leon J. A combined analysis of worldwide studies demonstrates an association between bipolar disorder and tobacco smoking behaviors in adults. Bipolar Disord. (2015) 17:575–97. doi: 10.1111/bdi.12319
80. Melo MCA, Daher EDF, Albuquerque SGC, de Bruin VMS. Exercise in bipolar patients: a systematic review. J Affect Disord. (2016) 198:32–8. doi: 10.1016/j.jad.2016.03.004
81. Vancampfort D, Firth J, Schuch F, Rosenbaum S, De Hert M, Mugisha J, et al. Physical activity and sedentary behavior in people with bipolar disorder: a systematic review and meta-analysis. J Affect Disord. (2016) 201:145–52. doi: 10.1016/j.jad.2016.05.020
82. Gabriel FC, Oliveira M, Martella BDM, Berk M, Brietzke E, Jacka FN, et al. Nutrition and bipolar disorder: a systematic review. Nutr Neurosci. (2023) 26:637–51. doi: 10.1080/1028415X.2022.2077031
83. Lopresti AL, Jacka FN. Diet and bipolar disorder: a review of its relationship and potential therapeutic mechanisms of action. J Altern Complement Med. (2015) 21:733–9. doi: 10.1089/acm.2015.0125
84. Köck P, Walter M. Personality disorder and substance use disorder—an update. Ment Health Prev. (2018) 12:82–9. doi: 10.1016/j.mhp.2018.10.003
85. Szoke A, Galliot AM, Richard JR, Ferchiou A, Baudin G, Leboyer M, et al. Association between cannabis use and schizotypal dimensions–a meta-analysis of cross-sectional studies. Psychiatry Res. (2014) 219:58–66. doi: 10.1016/j.psychres.2014.05.008
86. Trull TJ, Freeman LK, Vebares TJ, Choate AM, Helle AC, Wycoff AM. Borderline personality disorder and substance use disorders: an updated review. Borderline Pers Disord Emot Dysregul. (2018) 5:15. doi: 10.1186/s40479-018-0093-9
87. Castle DJ. The complexities of the borderline patient: how much more complex when considering physical health? Australas Psychiatry. (2019) 27:552–5. doi: 10.1177/1039856219848833
88. St-Amour S, Bérubé FA, Cailhol L, Le Corff C. Are physical activity and nutrition linked to personality disorders? Health habits and personality disorders: a scoping review. Pers Mental Health. (2023) 17:147–56. doi: 10.1002/pmh.1568
89. Erskine HE, Norman RE, Ferrari AJ, Chan GC, Copeland WE, Whiteford HA, et al. Long-term outcomes of attention-deficit/hyperactivity disorder and conduct disorder: a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. (2016) 55:841–50. doi: 10.1016/j.jaac.2016.06.016
90. Lee SS, Humphreys KL, Flory K, Liu R, Glass K. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: a meta-analytic review. Clin Psychol Rev. (2011) 31:328–41. doi: 10.1016/j.cpr.2011.01.006
91. Claussen AH, Holbrook JR, Hutchins HJ, Robinson LR, Bloomfield J, Meng L, et al. All in the family? A systematic review and meta-analysis of parenting and family environment as risk factors for attention-deficit/hyperactivity disorder (ADHD) in children. Prev Sci. (2022) 1–23. doi: 10.1007/s11121-022-01358-4. [Epub ahead of print].
92. Li B, Li J, Li Y. Overall media use and ADHD-related behaviors among children in China: a meta-analysis. J Contemp Educ Res. (2021) 5:176–82. doi: 10.26689/jcer.v5i12.2867
93. Lissak G. Adverse physiological and psychological effects of screen time on children and adolescents: literature review and case study. Environ Res. (2018) 164:149–57. doi: 10.1016/j.envres.2018.01.015
94. Suchert V, Hanewinkel R, Isensee B. Sedentary behavior and indicators of mental health in school-aged children and adolescents: a systematic review. Prev Med. (2015) 76:48–57. doi: 10.1016/j.ypmed.2015.03.026
95. Werling AM, Kuzhippallil S, Emery S, Walitza S, Drechsler R. Problematic use of digital media in children and adolescents with a diagnosis of attention-deficit/hyperactivity disorder compared to controls. A meta-analysis. J Behav Addict. (2022) 11:305–25. doi: 10.1556/2006.2022.00007
96. Del-Ponte B, Quinte GC, Cruz S, Grellert M, Santos IS. Dietary patterns and attention deficit/hyperactivity disorder (ADHD): a systematic review and meta-analysis. J Affect Disord. (2019) 252:160–73. doi: 10.1016/j.jad.2019.04.061
97. Farsad-Naeimi A, Asjodi F, Omidian M, Askari M, Nouri M, Pizarro AB, et al. Sugar consumption, sugar sweetened beverages and Attention Deficit Hyperactivity Disorder: a systematic review and meta-analysis. Complement Ther Med. (2020) 53:102512. doi: 10.1016/j.ctim.2020.102512
98. Papanastasiou G, Drigas A, Papanastasiou P. The association of diet quality and lifestyle factors in children and adults with ADHD: a systematic review and meta-analysis. Sci Electron Arch. (2021) 14. doi: 10.36560/14920211441
99. Shareghfarid E, Sangsefidi ZS, Salehi-Abargouei A, Hosseinzadeh M. Empirically derived dietary patterns and food groups intake in relation with Attention Deficit/Hyperactivity Disorder (ADHD): a systematic review and meta-analysis. Clin Nutr ESPEN. (2020) 36:28–35. doi: 10.1016/j.clnesp.2019.10.013
100. Hicks TA, Zaur AJ, Keeley JW, Amstadter AB. The association between recreational cannabis use and posttraumatic stress disorder: a systematic review and methodological critique of the literature. Drug Alcohol Depend. (2022) 240:109623. doi: 10.1016/j.drugalcdep.2022.109623
101. Lowe DJE, Sasiadek JD, Coles AS, George TP. Cannabis and mental illness: a review. Eur Arch Psychiatry Clin Neurosci. (2019) 269:107–20. doi: 10.1007/s00406-018-0970-7
102. Orsolini L, Chiappini S, Volpe U, De Berardis D, Latini R, Papanti GD, et al. Use of medicinal cannabis and synthetic cannabinoids in post-traumatic stress disorder (PTSD): a systematic review. Medicina. (2019) 55:525. doi: 10.3390/medicina55090525
103. Rehman Y, Saini A, Huang S, Sood E, Gill R, Yanikomeroglu S. Cannabis in the management of PTSD: a systematic review. AIMS Neurosc. (2021) 8:414–34. doi: 10.3934/Neuroscience.2021022
104. Stanciu CN, Brunette MF, Teja N, Budney AJ. Evidence for use of cannabinoids in mood disorders, anxiety disorders, and PTSD: a systematic review. Psychiatr Serv. (2021) 72:429–36. doi: 10.1176/appi.ps.202000189
105. Hall FS, Der-Avakian A, Gould TJ, Markou A, Shoaib M, Young JW. Negative affective states and cognitive impairments in nicotine dependence. Neurosci Biobehav Rev. (2015) 58:168–85. doi: 10.1016/j.neubiorev.2015.06.004
106. Kearns NT, Carl E, Stein AT, Vujanovic AA, Zvolensky MJ, Smits JAJ, et al. Posttraumatic stress disorder and cigarette smoking: a systematic review. Depress Anxiety. (2018) 35:1056–72. doi: 10.1002/da.22828
107. Mengin AC, Rolling J, Porche C, Durpoix A, Lalanne L. The intertwining of posttraumatic stress symptoms, alcohol, tobacco or nicotine use, and the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. (2022) 19:14546. doi: 10.3390/ijerph192114546
108. Pericot-Valverde I, Elliott RJ, Miller ME, Tidey JW, Gaalema DE. Posttraumatic stress disorder and tobacco use: a systematic review and meta-analysis. Addict Behav. (2018) 84:238–47. doi: 10.1016/j.addbeh.2018.04.024
109. van den Berk-Clark C, Secrest S, Walls J, Hallberg E, Lustman PJ, Schneider FD, et al. Association between posttraumatic stress disorder and lack of exercise, poor diet, obesity, and co-occuring smoking: a systematic review and meta-analysis. Health Psychol. (2018) 37:407–16. doi: 10.1037/hea0000593
110. Hall KS, Hoerster KD, Yancy WS Jr. Post-traumatic stress disorder, physical activity, and eating behaviors. Epidemiol Rev. (2015) 37:103–15. doi: 10.1093/epirev/mxu011
111. Vancampfort D, Stubbs B, Richards J, Ward PB, Firth J, Schuch FB, et al. Physical fitness in people with posttraumatic stress disorder: a systematic review. Disabil Rehabil. (2017) 39:2461–7. doi: 10.1080/09638288.2016.1226412
112. Hill AB. The environment and disease: association or causation? Proc R Soc Med. (1965) 58:295–300. doi: 10.1177/003591576505800503
113. Barrigón ML, Diaz FJ, Gurpegui M, Ferrin M, Salcedo MD, Moreno-Granados J, et al. Childhood trauma as a risk factor for psychosis: a sib-pair study. J Psychiatr Res. (2015) 70:130–6. doi: 10.1016/j.jpsychires.2015.08.017
114. Porras-Segovia A, Valmisa E, Gutiérrez B, Ruiz I, Rodríguez-Barranco M, Cervilla J. Prevalence and correlates of major depression in Granada, Spain: results from the GranadΣp study. Int J Soc Psychiatry. (2018) 64:450–8. doi: 10.1177/0020764018771405
115. Shah SM, Nowshad G, Dhaheri FA, Al-Shamsi MH, Al-Ketbi AM, Galadari A, et al. Child maltreatment and neglect in the United Arab Emirates and relationship with low self-esteem and symptoms of depression. Int Rev Psychiatry. (2021) 33:326–36. doi: 10.1080/09540261.2021.1895086
116. Jaisoorya TS, Desai G, Nair BS, Rani A, Menon PG, Thennarasu K. Association of childhood attention deficit hyperactivity disorder symptoms with academic and psychopathological outcomes in Indian college students: a retrospective survey. East Asian Arch Psychiatry. (2019) 29:124–8. doi: 10.12809/eaap1771
117. Werner KB, Grant JD, McCutcheon VV, Madden PA, Heath AC, Bucholz KK, et al. Differences in childhood physical abuse reporting and the association between CPA and alcohol use disorder in European American and African American women. Psychol Addict Behav. (2016) 30:423–33. doi: 10.1037/adb0000174
118. Afifi TO, Taillieu T, Salmon S, Davila IG, Stewart-Tufescu A, Fortier J, et al. Adverse childhood experiences (ACEs), peer victimization, and substance use among adolescents. Child Abuse Neglect. (2020) 106:104504. doi: 10.1016/j.chiabu.2020.104504
119. Hébert M, Amédée LM, Blais M, Gauthier-Duchesne A. Child sexual abuse among a representative sample of Quebec high school students: prevalence and association with mental health problems and health-risk behaviors. Can J Psychiatry. (2019) 64:846–54. doi: 10.1177/0706743719861387
120. McMahon EM, Corcoran P, Keeley H, Clarke M, Coughlan H, Wasserman D, et al. Risk and protective factors for psychotic experiences in adolescence: a population-based study. Psychol Med. (2021) 51:1220–8. doi: 10.1017/S0033291719004136
121. Degenhardt L, Coffey C, Hearps S, Kinner SA, Borschmann R, Moran P, et al. Associations between psychotic symptoms and substance use in young offenders. Drug Alcohol Rev. (2015) 34:673–82. doi: 10.1111/dar.12280
122. Chang WC, Wong CSM, Chen EYH, Lam LCW, Chan WC, Ng RMK, et al. Lifetime prevalence and correlates of schizophrenia-spectrum, affective, and other non-affective psychotic disorders in the Chinese adult population. Schizophr Bull. (2017) 43:1280–90. doi: 10.1093/schbul/sbx056
123. Young-Wolff KC, Sarovar V, Tucker LY, Goler NC, Alexeeff SE, Ridout KK, et al. Association of depression, anxiety, and trauma with cannabis use during pregnancy. JAMA Netw Open. (2020) 3:e1921333. doi: 10.1001/jamanetworkopen.2019.21333
124. An JH, Moon CS, Kim DE, Lee-Tauler SY, Jeon HJ, Cho SJ, et al. Prevalence of intimate partner violence victimization and its association with mental disorders in the Korean general population. Arch Womens Ment Health. (2019) 22:751–8. doi: 10.1007/s00737-019-00997-x
125. Bourbon A, Boyer L, Auquier P, Boucekine M, Barrow V, Lançon C, et al. Anxiolytic consumption is associated with tobacco smoking and severe nicotine dependence. Results from the national French medical students (BOURBON) study. Prog Neuro-Psychopharmacol Biol Psychiatry. (2019) 94:109645. doi: 10.1016/j.pnpbp.2019.109645
126. Woo J, Chang SM, Hong JP, Lee DW, Hahm BJ, Cho SJ, et al. The association of childhood experience of peer bullying with DSM-IV psychiatric disorders and suicidality in adults: results from a nationwide survey in Korea. J Korean Med Sci. (2019) 34:e295. doi: 10.3346/jkms.2019.34.e295
127. Jongsma HE, Gayer-Anderson C, Tarricone I, Velthorst E, van der Ven E, Quattrone D, et al. Social disadvantage, linguistic distance, ethnic minority status and first-episode psychosis: results from the EU-GEI case-control study. Psychol Med. (2021) 51:1536–48. doi: 10.1017/S003329172000029X
128. Mossie A, Kindu D, Negash A. Prevalence and severity of depression and its association with substance use in Jimma town, Southwest Ethiopia. Depress Res Treat. (2016) 2016:3460462. doi: 10.1155/2016/3460462
129. Islam MZ, Disu TR, Farjana S, Rahman MM. Malnutrition and other risk factors of geriatric depression: a community-based comparative cross-sectional study in older adults in rural Bangladesh. BMC Geriatr. (2021) 21:572. doi: 10.1186/s12877-021-02535-w
130. Albasara SA, Haneef MS, Zafar M, Moinuddin KG. Depression and associated risk factors among hypertensive patients in primary health care centers in Dammam, Kingdom of Saudi Arabia. Pan Afr Med J. (2021) 38:278. doi: 10.11604/pamj.2021.38.278.27133
131. Nam JY, Kim J, Cho KH, Choi J, Shin J, Park EC. The impact of sitting time and physical activity on major depressive disorder in South Korean adults: a cross-sectional study. BMC Psychiatry. (2017) 17:274. doi: 10.1186/s12888-017-1439-3
132. Madhav KC, Sherchand SP, Sherchan S. Association between screen time and depression among US adults. Prev Med Rep. (2017) 8:67–71. doi: 10.1016/j.pmedr.2017.08.005
133. López-Sánchez GF, Smith L, López-Bueno R, Pardhan S. Gender differences in the association between physical inactivity and mental-health conditions in people with vision or hearing impairment. Int J Environ Res Public Health. (2022) 19:3307. doi: 10.3390/ijerph19063307
134. Shahwan S, Abdin E, Shafie S, Chang S, Sambasivam R, Zhang Y, et al. Prevalence and correlates of smoking and nicotine dependence: results of a nationwide cross-sectional survey among Singapore residents. BMJ Open. (2019) 9:e032198. doi: 10.1136/bmjopen-2019-032198
135. Okunna N. A comparison of mental and behavioral health risks factors associated with current dual use of electronic cigarette and conventional tobacco cigarettes with exclusive tobacco cigarette use and nonuse among adults in the United States. Am J Addict. (2021) 30:138–46. doi: 10.1111/ajad.13110
136. Hasin DS, Kerridge BT, Saha TD, Huang B, Pickering R, Smith SM, et al. Prevalence and correlates of DSM-5 cannabis use disorder, 2012-2013: findings from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Am J Psychiatry. (2016) 173:588–99. doi: 10.1176/appi.ajp.2015.15070907
137. Starzer MSK, Nordentoft M, Hjorthøj C. Rates and predictors of conversion to schizophrenia or bipolar disorder following substance-induced psychosis. Am J Psychiatry. (2018) 175:343–50. doi: 10.1176/appi.ajp.2017.17020223
138. Ksir C, Hart CL. Cannabis and psychosis: a critical overview of the relationship. Curr Psychiatry Rep. (2016) 18:1–11. doi: 10.1007/s11920-015-0657-y
139. Shakoor S, Zavos HM, McGuire P, Cardno AG, Freeman D, Ronald A. Psychotic experiences are linked to cannabis use in adolescents in the community because of common underlying environmental risk factors. Psychiatry Res. (2015) 227:144–51. doi: 10.1016/j.psychres.2015.03.041
140. Sideli L, Fisher HL, Murray RM, Sallis H, Russo M, Stilo SA, et al. Interaction between cannabis consumption and childhood abuse in psychotic disorders: preliminary findings on the role of different patterns of cannabis use. Early Interv Psychiatry. (2018) 12:135–42. doi: 10.1111/eip.12285
141. Copeland WE, Hill SN, Shanahan L. Adult psychiatric, substance, and functional outcomes of different definitions of early cannabis use. J Am Acad Child Adolesc Psychiatry. (2022) 61:533–43. doi: 10.1016/j.jaac.2021.07.824
142. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
143. Johnstad PG. Cannabis as entheogen: survey and interview data on the spiritual use of cannabis. J Cannabis Res. (2020) 2:1–17. doi: 10.1186/s42238-020-00032-2
144. Johnstad PG. Entheogenic experience and spirituality. Method Theory Study Relig. (2021) 33:463–81. doi: 10.1163/15700682-12341512
145. Simons J, Correia CJ, Carey KB, Borsari BE. Validating a five-factor marijuana motives measure: relations with use, problems, and alcohol motives. J Couns Psychol. (1998) 45:265–73. doi: 10.1037/0022-0167.45.3.265
146. Ellingson JM, Ross JM, Winiger E, Stallings MC, Corley RP, Friedman NP, et al. Familial factors may not explain the effect of moderate-to-heavy cannabis use on cognitive functioning in adolescents: a sibling-comparison study. Addiction. (2021) 116:833–44. doi: 10.1111/add.15207
147. Watson CW, Campbell LM, Sun-Suslow N, Hong S, Umlauf A, Ellis RJ, et al. Daily cannabis use is associated with lower CNS inflammation in people with HIV. J Int Neuropsychol Soc. (2021) 27:661–72. doi: 10.1017/S1355617720001447
148. Boulos DN, Loffredo CA, El Setouhy M, Abdel-Aziz F, Israel E, Mohamed MK. Nondaily, light daily, and moderate-to-heavy cigarette smokers in a rural area of Egypt: a population-based survey. Nicot Tobacco Res. (2009) 11:134–8. doi: 10.1093/ntr/ntp016
149. Schane RE, Ling PM, Glantz SA. Health effects of light and intermittent smoking: a review. Circulation. (2010) 121:1518–22. doi: 10.1161/CIRCULATIONAHA.109.904235
150. Matta J, Hoertel N, Airagnes G, Wiernik E, Limosin F, Goldberg M, et al. Does substance use explain social differences in terms of depression? Findings from the Constances cohort. Compr Psychiatry. (2020) 102:152203. doi: 10.1016/j.comppsych.2020.152203
151. Padwa H, Huang D, Mooney L, Grella CE, Urada D, Bell DS, et al. Medical conditions of primary care patients with documented cannabis use and cannabis use disorder in electronic health records: a case control study from an academic health system in a medical marijuana state. Subst Abuse Treat Prev Policy. (2022) 17:36. doi: 10.1186/s13011-022-00467-1
152. Sze KYP, Lee EKP, Chan RHW, Kim JH. Prevalence of negative emotional eating and its associated psychosocial factors among urban Chinese undergraduates in Hong Kong: a cross-sectional study. BMC Public Health. (2021) 21:583. doi: 10.1186/s12889-021-10531-3
153. Magklara K, Bellos S, Niakas D, Stylianidis S, Kolaitis G, Mavreas V, et al. Depression in late adolescence: a cross-sectional study in senior high schools in Greece. BMC Psychiatry. (2015) 15:199. doi: 10.1186/s12888-015-0584-9
154. Nutt DJ. Equasy – an overlooked addiction with implications for the current debate on drug harms. J Psychopharmacol. (2009) 23:3–5. doi: 10.1177/0269881108099672
155. Talati A, Keyes KM, Hasin DS. Changing relationships between smoking and psychiatric disorders across twentieth century birth cohorts: clinical and research implications. Mol Psychiatry. (2016) 21:464–71. doi: 10.1038/mp.2015.224
156. Yang G, D'Arcy C. The changing relationship between health risk behaviors and depression among birth cohorts of canadians 65+, 1994-2014. Front Psychiatry. (2022) 13:1078161. doi: 10.3389/fpsyt.2022.1078161
157. Cabral TS. The 15th anniversary of the Portuguese drug policy: its history, its success and its future. Drug Sci Policy Law. (2017) 3:1–5. doi: 10.1177/2050324516683640
158. Compton WM, Han B, Jones CM, Blanco C, Hughes A. Marijuana use and use disorders in adults in the USA, 2002-14: analysis of annual cross-sectional surveys. Lancet Psychiatry. (2016) 3:954–64. doi: 10.1016/S2215-0366(16)30208-5
159. Fischer B, Lee A, Robinson T, Hall W. An overview of select cannabis use and supply indicators pre- and post-legalization in Canada. Subst Abuse Treat Prev Policy. (2021) 16:77. doi: 10.1186/s13011-021-00405-7
160. Hughes CE, Stevens A. A resounding success or a disastrous failure: re-examining the interpretation of evidence on the Portuguese decriminalisation of illicit drugs. Drug Alcohol Rev. (2012) 31:101–13. doi: 10.1111/j.1465-3362.2011.00383.x
161. Martins SS, Segura LE, Levy NS, Mauro PM, Mauro CM, Philbin MM, et al. Racial and ethnic differences in cannabis use following legalization in US states with medical cannabis laws. JAMA Netw Open. (2021) 4:e2127002. doi: 10.1001/jamanetworkopen.2021.27002
162. Mauro CM, Newswanger P, Santaella-Tenorio J, Mauro PM, Carliner H, Martins SS. Impact of medical marijuana laws on state-level marijuana use by age and gender, 2004-2013. Prev Sci. (2019) 20:205–14. doi: 10.1007/s11121-017-0848-3
163. Philbin MM, Mauro PM, Santaella-Tenorio J, Mauro CM, Kinnard EN, Cerdá M, et al. Associations between state-level policy liberalism, cannabis use, and cannabis use disorder from 2004 to 2012: looking beyond medical cannabis law status. Int J Drug Policy. (2019) 65:97–103. doi: 10.1016/j.drugpo.2018.10.010
164. Williams AR, Santaella-Tenorio J, Mauro CM, Levin FR, Martins SS. Loose regulation of medical marijuana programs associated with higher rates of adult marijuana use but not cannabis use disorder. Addiction. (2017) 112:1985–91. doi: 10.1111/add.13904
165. Zellers SM, Ross JM, Saunders GRB, Ellingson JM, Walvig T, Anderson JE, et al. Recreational cannabis legalization has had limited effects on a wide range of adult psychiatric and psychosocial outcomes. Psychol Med. (2023) 53:1–10. doi: 10.1017/S0033291722003762
166. Cerdá M, Mauro C, Hamilton A, Levy NS, Santaella-Tenorio J, Hasin D, et al. Association between recreational marijuana legalization in the United States and changes in marijuana use and cannabis use disorder from 2008 to 2016. JAMA Psychiatry. (2020) 77:165–71. doi: 10.1001/jamapsychiatry.2019.3254
167. Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, et al. Prevalence of marijuana use disorders in the United States between 2001-2002 and 2012-2013. JAMA Psychiatry. (2015) 72:1235–42. doi: 10.1001/jamapsychiatry.2015.1858
168. Wen H, Hockenberry JM, Cummings JR. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. J Health Econ. (2015) 42:64–80. doi: 10.1016/j.jhealeco.2015.03.007
169. Livne O, Razon L, Rehm J, Hasin DS, Lev-Ran S. The association between lifetime cannabis use and dysthymia across six birth decades. J Affect Disord. (2018) 234:327–34. doi: 10.1016/j.jad.2018.03.005
170. Livne O, Shmulewitz D, Sarvet AL, Wall MM, Hasin DS. Association of cannabis use-related predictor variables and self-reported psychotic disorders: U.S. adults, 2001-2002 and 2012-2013. Am J Psychiatry. (2022) 179:36–45. doi: 10.1176/appi.ajp.2021.21010073
171. Davies J, Sullivan S, Zammit S. Adverse life outcomes associated with adolescent psychotic experiences and depressive symptoms. Soc Psychiatry Psychiatr Epidemiol. (2018) 53:497–507. doi: 10.1007/s00127-018-1496-z
172. Bhavsar V, Jauhar S, Murray RM, Hotopf M, Hatch SL, McNeill A, et al. Tobacco smoking is associated with psychotic experiences in the general population of South London. Psychol Med. (2018) 48:123–31. doi: 10.1017/S0033291717001556
173. Bassir Nia A, Medrano B, Perkel C, Galynker I, Hurd YL. Psychiatric comorbidity associated with synthetic cannabinoid use compared to cannabis. J Psychopharmacol. (2016) 30:1321–30. doi: 10.1177/0269881116658990
174. Wainberg M, Jacobs GR, di Forti M, Tripathy SJ. Cannabis, schizophrenia genetic risk, and psychotic experiences: a cross-sectional study of 109,308 participants from the UK Biobank. Transl Psychiatry. (2021) 11:211. doi: 10.1038/s41398-021-01330-w
175. Pardo M, Matalí JL, Sivoli J, Regina VB, Butjosa A, Dolz M, et al. Early onset psychosis and cannabis use: prevalence, clinical presentation and influence of daily use. Asian J Psychiatr. (2021) 62:102714. doi: 10.1016/j.ajp.2021.102714
176. Campbell A, Bailey SR, Hoffman KA, Ponce-Terashima J, Fankhauser K, Marino M, et al. Associations between psychiatric disorders and cannabis-related disorders documented in electronic health records. J Psychoactive Drugs. (2020) 52:228–36. doi: 10.1080/02791072.2020.1747665
177. Ferraro L, La Cascia C, Quattrone D, Sideli L, Matranga D, Capuccio V, et al. Premorbid adjustment and IQ in patients with first-episode psychosis: a multisite case-control study of their relationship with cannabis use. Schizophr Bull. (2020) 46:517–29. doi: 10.1093/schbul/sbaa029.644
178. Corsi-Zuelli F, Marques L, da Roza DL, Loureiro CM, Shuhama R, Di Forti M, et al. The independent and combined effects of cannabis use and systemic inflammation during the early stages of psychosis: exploring the two-hit hypothesis. Psychol Med. (2021) 52:3874–84. doi: 10.1017/S0033291721000726
179. Carney R, Yung AR, Amminger GP, Bradshaw T, Glozier N, Hermens DF, et al. Substance use in youth at risk for psychosis. Schizophr Res. (2017) 181:23–9. doi: 10.1016/j.schres.2016.08.026
180. Di Forti M, Quattrone D, Freeman TP, Tripoli G, Gayer-Anderson C, Quigley H, et al. The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): a multicentre case-control study. Lancet Psychiatry. (2019) 6:427–36.
181. McGuckin T, Ferro MA, Hammond D, Stewart S, Maloney-Hall B, Madi N, et al. How high? Trends in cannabis use prior to first admission to inpatient psychiatry in Ontario, Canada, between 2007 and 2017. Can J Psychiatry. (2021) 66:1059–68. doi: 10.1177/0706743720984679
182. Hines LA, Freeman TP, Gage SH, Zammit S, Hickman M, Cannon M, et al. Association of high-potency cannabis use with mental health and substance use in adolescence. JAMA Psychiatry. (2020) 77:1044–51. doi: 10.1001/jamapsychiatry.2020.1035
183. Chan GCK, Hall W, Freeman TP, Ferris J, Kelly AB, Winstock A. User characteristics and effect profile of Butane Hash Oil: an extremely high-potency cannabis concentrate. Drug Alcohol Depend. (2017) 178:32–8. doi: 10.1016/j.drugalcdep.2017.04.014
184. Di Forti M, Marconi A, Carra E, Fraietta S, Trotta A, Bonomo M, et al. Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: a case-control study. Lancet Psychiatry. (2015) 2:233–8. doi: 10.1016/S2215-0366(14)00117-5
185. Bassir Nia A, Mann CL, Spriggs S, DeFrancisco DR, Carbonaro S, Parvez L, et al. The relevance of sex in the association of synthetic cannabinoid use with psychosis and agitation in an inpatient population. J Clin Psychiatry. (2019) 80:18m12539. doi: 10.4088/JCP.18m12539
186. Molla Z, Dube L, Krahl W, Soboka M. Tobacco dependence among people with mental illness: a facility-based cross sectional study from Southwest Ethiopia. BMC Res Notes. (2017) 10:289. doi: 10.1186/s13104-017-2608-7
187. Dickerson F, Schroeder J, Katsafanas E, Khushalani S, Origoni AE, Savage C, et al. Cigarette smoking by patients with serious mental illness, 1999-2016: an increasing disparity. Psychiatr Serv. (2018) 69:147–53. doi: 10.1176/appi.ps.201700118
188. Zolezzi M, Al-Rawi S, Eltorki Y. An exploration of smoking patterns among people with serious mental illness attending an outpatient clinic in Qatar. Neuropsychiatr Dis Treat. (2022) 18:2847–54. doi: 10.2147/NDT.S385970
189. Werneck AO, Vancampfort D, Oyeyemi AL, Szwarcwald CL, Stubbs B, Silva DR. Lifestyle behaviors among 4,343 Brazilian adults with severe mental illness and 55,859 general population controls: data from the Brazilian National Health Survey. Rev Bras Psiquiatr. (2020) 42:245–9. doi: 10.1590/1516-4446-2019-0621
190. Wolfe RM, Reeves LE, Gibson LE, Cooper S, Ellman LM. Attenuated positive psychotic symptoms in relation to cigarette smoking in a nonclinical population. Nicotine Tob Res. (2017) 19:124–8. doi: 10.1093/ntr/ntw240
191. Clark V, Conrad AM, Lewin TJ, Baker AL, Halpin SA, Sly KA, et al. Addiction vulnerability: exploring relationships among cigarette smoking, substance misuse, and early psychosis. J Dual Diagn. (2018) 14:78–88. doi: 10.1080/15504263.2017.1416436
192. Mustonen A, Niemelä S, Nordström T, Murray GK, Mäki P, Jääskeläinen E, et al. Adolescent cannabis use, baseline prodromal symptoms and the risk of psychosis. Br J Psychiatry. (2018) 212:227–33. doi: 10.1192/bjp.2017.52
193. Yilmaz Kafali H, Turan S, Akpinar S, Mutlu M, Özkaya Parlakay A, Çöp E, et al. Correlates of psychotic like experiences (PLEs) during pandemic: an online study investigating a possible link between the SARS-CoV-2 infection and PLEs among adolescents. Schizophr Res. (2022) 241:36–43. doi: 10.1016/j.schres.2021.12.049
194. Mallet J, Mazer N, Dubertret C, Le Strat Y. Tobacco smoking and psychotic-like experiences in a general population sample. J Clin Psychiatry. (2018) 79:17m11994. doi: 10.4088/JCP.17m11994
195. Fang Y, Wang W, Zhu C, Lin GN, Cheng Y, Zou J, et al. Use of tobacco in schizophrenia: a double-edged sword. Brain Behav. (2019) 9:e01433. doi: 10.1002/brb3.1433
196. Kim BS, Chang SM, Park JE, Seong SJ, Won SH, Cho MJ. Prevalence, correlates, psychiatric comorbidities, and suicidality in a community population with problematic Internet use. Psychiatry Res. (2016) 244:249–56. doi: 10.1016/j.psychres.2016.07.009
197. Zhang Y, Li Q, Hu W, Zhan N, Zou J, Wang J, et al. The relationships between screen time and mental health problems among Chinese adults. J Psychiatr Res. (2022) 146:279–85. doi: 10.1016/j.jpsychires.2021.11.017
198. Mutiso VN, Ndetei DM, Muia NE, Alietsi KR, Onsinyo L, Kameti F, et al. The prevalance of binge eating disorder and associated psychiatric and substance use disorders in a student population in Kenya - towards a public health approach. BMC Psychiatry. (2022) 22:122. doi: 10.1186/s12888-022-03761-1
199. van Os J, Pries LK, Ten Have M, de Graaf R, van Dorsselaer S, Bak M, et al. Schizophrenia and the environment: within-person analyses may be required to yield evidence of unconfounded and causal association-the example of cannabis and psychosis. Schizophr Bull. (2021) 47:594–603. doi: 10.1093/schbul/sbab019
200. Jones HJ, Gage SH, Heron J, Hickman M, Lewis G, Munafò MR, et al. Association of combined patterns of tobacco and cannabis use in adolescence with psychotic experiences. JAMA Psychiatry. (2018) 75:240–6. doi: 10.1001/jamapsychiatry.2017.4271
201. Bechtold J, Hipwell A, Lewis DA, Loeber R, Pardini D. Concurrent and sustained cumulative effects of adolescent marijuana use on subclinical psychotic symptoms. Am J Psychiatry. (2016) 173:781–9. doi: 10.1176/appi.ajp.2016.15070878
202. Degenhardt L, Saha S, Lim CCW, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, et al. The associations between psychotic experiences and substance use and substance use disorders: findings from the World Health Organization World Mental Health surveys. Addiction. (2018) 113:924–34. doi: 10.1111/add.14145
203. Ryan JE, Veliz P, McCabe SE, Stoddard SA, Boyd CJ. Association of early onset of cannabis, cigarette, other drug use and schizophrenia or psychosis. Schizophr Res. (2020) 215:482–4. doi: 10.1016/j.schres.2019.10.002
204. Rognli EB, Bramness JG, von Soest T. Smoking in early adulthood is prospectively associated with prescriptions of antipsychotics, mood stabilizers, antidepressants and anxiolytics. Psychol Med. (2022) 52:3241–50. doi: 10.1017/S0033291720005401
205. Metrik J, Jackson K, Bassett SS, Zvolensky MJ, Seal K, Borsari B. The mediating roles of coping, sleep, and anxiety motives in cannabis use and problems among returning veterans with PTSD and MDD. Psychol Addict Behav. (2016) 30:743–54. doi: 10.1037/adb0000210
206. Halladay JE, Boyle MH, Munn C, Jack SM, Georgiades K. Sex differences in the association between cannabis use and suicidal ideation and attempts, depression, and psychological distress among Canadians. Can J Psychiatry. (2019) 64:345–50. doi: 10.1177/0706743718804542
207. Wahby S, Karnik V, Brobbey A, Wiebe S, Sajobi T, Josephson CB. Cannabis use is both independently associated with and mediates worse psychosocial health in patients with epilepsy. J Neurol Neurosurg Psychiatry. (2019) 90:945–51. doi: 10.1136/jnnp-2018-319780
208. Risal A, Manandhar K, Linde M, Steiner TJ, Holen A. Anxiety and depression in Nepal: prevalence, comorbidity and associations. BMC Psychiatry. (2016) 16:102. doi: 10.1186/s12888-016-0810-0
209. Gorfinkel LR, Stohl M, Hasin D. Association of depression with past-month cannabis use among US adults aged 20 to 59 years, 2005 to 2016. JAMA Netw Open. (2020) 3:e2013802. doi: 10.1001/jamanetworkopen.2020.13802
210. Carrà G, Bartoli F, Crocamo C. Trends of major depressive episode among people with cannabis use: findings from the National Survey on Drug Use and Health 2006-2015. Subst Abuse. (2019) 40:178–84. doi: 10.1080/08897077.2018.1550464
211. Cougle JR, Hakes JK, Macatee RJ, Chavarria J, Zvolensky MJ. Quality of life and risk of psychiatric disorders among regular users of alcohol, nicotine, and cannabis: an analysis of the National Epidemiological Survey on Alcohol and Related Conditions (NESARC). J Psychiatr Res. (2015) 66–67:135–41. doi: 10.1016/j.jpsychires.2015.05.004
212. Pacek LR, Weinberger AH, Zhu J, Goodwin RD. Rapid increase in the prevalence of cannabis use among people with depression in the United States, 2005-17: the role of differentially changing risk perceptions. Addiction. (2020) 115:935–43. doi: 10.1111/add.14883
213. Cougle JR, Hakes JK, Macatee RJ, Zvolensky MJ, Chavarria J. Probability and correlates of dependence among regular users of alcohol, nicotine, cannabis, and cocaine: concurrent and prospective analyses of the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. (2016) 77:e444–50. doi: 10.4088/JCP.14m09469
214. Wu LT, Zhu H, Mannelli P, Swartz MS. Prevalence and correlates of treatment utilization among adults with cannabis use disorder in the United States. Drug Alcohol Depend. (2017) 177:153–62. doi: 10.1016/j.drugalcdep.2017.03.037
215. Hill ML, Nichter BM, Norman SB, Loflin M, Pietrzak RH. Burden of cannabis use and disorder in the U.S. veteran population: psychiatric comorbidity. suicidality, and service utilization. J Affect Disord. (2021) 278:528–35. doi: 10.1016/j.jad.2020.09.099
216. Keith DR, Hart CL, McNeil MP, Silver R, Goodwin RD. Frequent marijuana use, binge drinking and mental health problems among undergraduates. Am J Addict. (2015) 24:499–506. doi: 10.1111/ajad.12201
217. Mannes ZL, Dunne EM, Ferguson EG, Cook RL, Ennis N. Symptoms of generalized anxiety disorder as a risk factor for substance use among adults living with HIV. AIDS Care. (2021) 33:623–32. doi: 10.1080/09540121.2020.1808163
218. Chadi N, Li G, Cerda N, Weitzman ER. Depressive symptoms and suicidality in adolescents using e-cigarettes and marijuana: a secondary data analysis from the Youth Risk Behavior Survey. J Addict Med. (2019) 13:362–5. doi: 10.1097/ADM.0000000000000506
219. Halladay JE, Munn C, Boyle M, Jack SM, Georgiades K. Temporal changes in the cross-sectional associations between cannabis use, suicidal ideation, and depression in a nationally representative sample of Canadian adults in 2012 compared to 2002. Can J Psychiatry. (2020) 65:115–23. doi: 10.1177/0706743719854071
220. Butler A, Patte KA, Ferro MA, Leatherdale ST. Interrelationships among depression, anxiety, flourishing, and cannabis use in youth. Addict Behav. (2019) 89:206–15. doi: 10.1016/j.addbeh.2018.10.007
221. Estévez N, Dey M, Eich-Höchli D, Foster S, Gmel G, Mohler-Kuo M. Adult attention-deficit/hyperactivity disorder and its association with substance use and substance use disorders in young men. Epidemiol Psychiatr Sci. (2016) 25:255–66. doi: 10.1017/S2045796015000360
222. Leventhal AM, Bae D, Kechter A, Barrington-Trimis JL. Psychiatric comorbidity in adolescent use and poly-use of combustible, vaporized, and edible cannabis products. J Psychiatr Res. (2020) 124:91–8. doi: 10.1016/j.jpsychires.2020.02.021
223. Prestage G, Hammoud M, Jin F, Degenhardt L, Bourne A, Maher L. Mental health, drug use and sexual risk behavior among gay and bisexual men. Int J Drug Policy. (2018) 55:169–79. doi: 10.1016/j.drugpo.2018.01.020
224. Kerridge BT, Pickering R, Chou P, Saha TD, Hasin DS. DSM-5 cannabis use disorder in the National Epidemiologic Survey on Alcohol and Related Conditions-III: gender-specific profiles. Addict Behav. (2018) 76:52–60. doi: 10.1016/j.addbeh.2017.07.012
225. Rubenstein D, Aston ER, Nollen NL, Mayo MS, Brown AR, Ahluwalia JS. Factors associated with cannabis use among African American nondaily smokers. J Addict Med. (2020) 14:e170–4. doi: 10.1097/ADM.0000000000000652
226. Seaman EL, Green KM, Wang MQ, Quinn SC, Fryer CS. Examining prevalence and correlates of cigarette and marijuana co-use among young adults using ten years of NHANES data. Addict Behav. (2019) 96:140–7. doi: 10.1016/j.addbeh.2019.04.014
227. Gukasyan N, Strain EC. Relationship between cannabis use frequency and major depressive disorder in adolescents: findings from the National Survey on Drug Use and Health 2012-2017. Drug Alcohol Depend. (2020) 208:107867. doi: 10.1016/j.drugalcdep.2020.107867
228. Wang CH, Peiper N. Association between physical activity and sedentary behavior with depressive symptoms among US high school students, 2019. Prev Chronic Dis. (2022) 19:E76. doi: 10.5888/pcd19.220003
229. Hill ML, Loflin M, Nichter B, Norman SB, Pietrzak RH. Prevalence of cannabis use, disorder, and medical card possession in U.S. military veterans: results from the 2019-2020 National Health and Resilience in Veterans Study. Addict Behav. (2021) 120:106963. doi: 10.1016/j.addbeh.2021.106963
230. Lekoubou A, Fox J, Bishu KG, Ovbiagele B. Trends in documented cannabis use disorder among hospitalized adult epilepsy patients in the United States. Epilepsy Res. (2020) 163:106341. doi: 10.1016/j.eplepsyres.2020.106341
231. Bonsaksen T, Ekeberg Ø, Schou-Bredal I, Skogstad L, Heir T, Grimholt TK. Use of alcohol and addictive drugs during the COVID-19 outbreak in Norway: associations with mental health and pandemic-related problems. Front Public Health. (2021) 9:667729. doi: 10.3389/fpubh.2021.667729
232. Fink DS, Shmulewitz D, Mannes ZL, Stohl M, Livne O, Wall M, et al. Construct validity of DSM-5 cannabis use disorder diagnosis and severity levels in adults with problematic substance use. J Psychiatr Res. (2022) 155:387–94. doi: 10.1016/j.jpsychires.2022.09.016
233. Thompson K, Merrin GJ, Ames ME, Leadbeater B. Marijuana trajectories in Canadian youth: associations with substance use and mental health. Can J Behav Sci. (2018) 50:17–28. doi: 10.1037/cbs0000090
234. Welsh JW, Knight JR, Hou SS, Malowney M, Schram P, Sherritt L, et al. Association between substance use diagnoses and psychiatric disorders in an adolescent and young adult clinic-based population. J Adolesc Health. (2017) 60:648–52. doi: 10.1016/j.jadohealth.2016.12.018
235. Tiburcio Sainz M, Nagy G, Rosete Mohedano G, Martínez Vélez N, Carreño García S, Pérez Cisneros D, et al. The association between substance use and depressive symptomatology in nursing university students in Mexico. Nurse Educ Pract. (2019) 36:114–20. doi: 10.1016/j.nepr.2019.03.005
236. Gaete J, Labbé N, Del Villar P, Allende C, Araya R, Valenzuela E. Mental health and associated factors among young offenders in Chile: a cross-sectional study. Crim Behav Ment Health. (2018) 28:13–27. doi: 10.1002/cbm.2029
237. Raffetti E, Donato F, Forsell Y, Galanti MR. Longitudinal association between tobacco use and the onset of depressive symptoms among Swedish adolescents: the Kupol cohort study. Eur Child Adolesc Psychiatry. (2019) 28:695–704. doi: 10.1007/s00787-018-1237-6
238. Farrell KR, Karey E, Xu S, Gibbon G, Gordon T, Weitzman M. E-cigarette use, systemic inflammation, and depression. Int J Environ Res Public Health. (2021) 18:10402. doi: 10.3390/ijerph181910402
239. Klein RJ, Gyorda JA, Jacobson NC. Anxiety, depression, and substance experimentation in childhood. PLoS ONE. (2022) 17:e0265239. doi: 10.1371/journal.pone.0265239
240. Mohammadi AQ, Neyazi A, Rangelova V, Padhi BK, Odey GO, Ogbodum MU, et al. Depression and quality of life among Afghan healthcare workers: a cross-sectional survey study. BMC Psychol. (2023) 11:29. doi: 10.1186/s40359-023-01059-9
241. Conti CL, Barbosa WM, Simão JBP, Álvares-da-Silva AM. Pesticide exposure, tobacco use, poor self-perceived health and presence of chronic disease are determinants of depressive symptoms among coffee growers from Southeast Brazil. Psychiatry Res. (2018) 260:187–92. doi: 10.1016/j.psychres.2017.11.063
242. Kelishadi R, Babaki AE, Qorbani M, Ahadi Z, Heshmat R, Motlagh ME, et al. Joint association of active and passive smoking with psychiatric distress and violence behaviors in a representative sample of Iranian children and adolescents: the CASPIAN-IV study. Int J Behav Med. (2015) 22:652–61. doi: 10.1007/s12529-015-9462-6
243. Bernard C, Font H, Diallo Z, Ahonon R, Tine JM, N'guessan Abouo F, et al. Prevalence and factors associated with severe depressive symptoms in older west African people living with HIV. BMC Psychiatry. (2020) 20:442. doi: 10.1186/s12888-020-02837-0
244. Wang K, Zhao Y, Nie J, Xu H, Yu C, Wang S. Higher HEI-2015 score is associated with reduced risk of depression: result from NHANES 2005-2016. Nutrients. (2021) 13:348. doi: 10.3390/nu13020348
245. Rahe C, Khil L, Wellmann J, Baune BT, Arolt V, Berger K. Impact of major depressive disorder, distinct subtypes, and symptom severity on lifestyle in the BiDirect Study. Psychiatry Res. (2016) 245:164–71. doi: 10.1016/j.psychres.2016.08.035
246. Ma L, Hagquist C, Kleppang AL. Leisure time physical activity and depressive symptoms among adolescents in Sweden. BMC Public Health. (2020) 20:997. doi: 10.1186/s12889-020-09022-8
247. Weinberger AH, Gbedemah M, Wall MM, Hasin DS, Zvolensky MJ, Chaiton M, et al. Depression among non-daily smokers compared to daily smokers and never-smokers in the United States: an emerging problem. Nicotine Tob Res. (2017) 19:1062–72. doi: 10.1093/ntr/ntx009
248. van Binnendijk S, van Amsterdam JGC, Snijder MB, Schene AH, Derks EM, van den Brink W. Contribution of alcohol and nicotine dependence to the prevalence of depressed mood in different ethnic groups in the Netherlands: the HELIUS study. J Dual Diagn. (2020) 16:271–84. doi: 10.1080/15504263.2020.1772526
249. Chido-Amajuoyi OG, Mantey DS, Omega-Njemnobi O, Yu RK, Shete S. Association of dual and poly tobacco use with depressive symptoms and use of antidepressants. Addict Behav. (2021) 115:106790. doi: 10.1016/j.addbeh.2020.106790
250. Ye X, Li L, Gao Y, Zhou S, Yang Y, Chen S. Dose-response relations between second-hand smoke exposure and depressive symptoms among middle-aged women. Psychiatry Res. (2015) 229:533–8. doi: 10.1016/j.psychres.2015.06.008
251. Lee Y, Lee KS. Association of depression and suicidality with electronic and conventional cigarette use in South Korean adolescents. Subst Use Misuse. (2019) 54:934–43. doi: 10.1080/10826084.2018.1552301
252. Islam MS, Rahman ME, Moonajilin MS, van Os J. Prevalence of depression, anxiety and associated factors among school going adolescents in Bangladesh: findings from a cross-sectional study. PLoS ONE. (2021) 16:e0247898. doi: 10.1371/journal.pone.0247898
253. Matcham F, Carroll A, Chung N, Crawford V, Galloway J, Hames A, et al. Smoking and common mental disorders in patients with chronic conditions: an analysis of data collected via a web-based screening system. Gen Hosp Psychiatry. (2017) 45:12–8. doi: 10.1016/j.genhosppsych.2016.11.006
254. Gorfinkel L, Hasin D, Miech R, Keyes KM. The link between depressive symptoms and vaping nicotine in U.S. adolescents, 2017-2019. J Adolesc Health. (2022) 70:133–9. doi: 10.1016/j.jadohealth.2021.07.003
255. Melin EO, Wanby P, Neumark T, Holmberg S, Neumark AN, Johansson K, et al. Depression was associated with younger age, female sex, obesity, smoking, and physical inactivity, in 1027 patients with newly diagnosed type 2 diabetes: a Swedish multicentre cross-sectional study. BMC Endocr Disord. (2022) 22:273. doi: 10.1186/s12902-022-01184-3
256. Chen YL, Wu SC, Chen YT, Hsiao PC, Yu YH, Ting TT, et al. E-cigarette use in a country with prevalent tobacco smoking: a population-based study in Taiwan. J Epidemiol. (2019) 29:155–63. doi: 10.2188/jea.JE20170300
257. Wiernik E, Airagnes G, Lequy E, Gomajee R, Melchior M, Le Faou AL, et al. Electronic cigarette use is associated with depressive symptoms among smokers and former smokers: cross-sectional and longitudinal findings from the Constances cohort. Addict Behav. (2019) 90:85–91. doi: 10.1016/j.addbeh.2018.10.021
258. Luo Y, Li Y, Xie J, Duan Y, Gan G, Zhou Y, et al. Symptoms of depression are related to sedentary behavior and sleep duration in elderly individuals: a cross-sectional study of 49,317 older Chinese adults. J Affect Disord. (2022) 308:407–12. doi: 10.1016/j.jad.2022.04.102
259. Formagini TDB, Gomide HP, Perales J, Colugnati FAB. Prevalence and correlates of light and non-daily smoking in Brazil: results from a nationwide representative survey. Drug Alcohol Depend. (2017) 178:15–9. doi: 10.1016/j.drugalcdep.2017.04.018
260. Patanavanich R, Vityananan P, Neelapaichit N, Chariyalertsak S, Kessomboon P, Assanangkornchai S, et al. Association between electronic cigarette use and depression among Thai adolescents: the Thailand National Health Examination Survey 2019-2020. Tob Induc Dis. (2022) 20:103. doi: 10.18332/tid/155333
261. Masana MF, Haro JM, Mariolis A, Piscopo S, Valacchi G, Bountziouka V, et al. Mediterranean diet and depression among older individuals: the multinational MEDIS study. Exp Gerontol. (2018) 110:67–72. doi: 10.1016/j.exger.2018.05.012
262. Bandiera FC, Loukas A, Wilkinson AV, Perry CL. Associations between tobacco and nicotine product use and depressive symptoms among college students in Texas. Addict Behav. (2016) 63:19–22. doi: 10.1016/j.addbeh.2016.06.024
263. Kim S. The relationship between lifestyle risk factors and depression in Korean older adults: a moderating effect of gender. BMC Geriatr. (2022) 22:24. doi: 10.1186/s12877-021-02729-2
264. Kim J, Kim H, Jang SI, Park EC. Association between sedentary behavior and depression among South Korean adolescents. BMC Psychiatry. (2022) 22:622. doi: 10.1186/s12888-022-04262-x
265. Liu Y, Ozodiegwu ID, Yu Y, Hess R, Bie R. An association of health behaviors with depression and metabolic risks: data from 2007 to 2014 U.S. National Health and Nutrition Examination Survey. J Affect Disord. (2017) 217:190–6. doi: 10.1016/j.jad.2017.04.009
266. Patten SB, Williams JVA, Lavorato DH, Woolf B, Wang JL, Bulloch AGM, et al. Major depression and secondhand smoke exposure. J Affect Disord. (2018) 225:260–4. doi: 10.1016/j.jad.2017.08.006
267. Clyde M, Smith KJ, Gariépy G, Schmitz N. Assessing the longitudinal associations and stability of smoking and depression syndrome over a 4-year period in a community sample with type 2 diabetes 24. J Diabetes. (2015) 7:95–101. doi: 10.1111/1753-0407.12141
268. Chen CY, Chang CM, Lin HL, Chu CL. The association between exposure to second-hand smoke and major depressive disorder in perimenopausal women: results from a population-based study. Ann Med. (2018) 50:596–604. doi: 10.1080/07853890.2018.1534264
269. Liu Q, Leng P, Gu Y, Shang X, Zhou Y, Zhang H, et al. The dose-effect relationships of cigarette and alcohol consumption with depressive symptoms: a multiple-center, cross-sectional study in 5965 Chinese middle-aged and elderly men. BMC Psychiatry. (2022) 22:657. doi: 10.1186/s12888-022-04316-0
270. Salimi S, Terplan M, Cheng D, Chisolm MS. The relationship between postpartum depression and perinatal cigarette smoking: an analysis of PRAMS data. J Subst Abuse Treat. (2015) 56:34–8. doi: 10.1016/j.jsat.2015.03.004
271. Chou SP, Goldstein RB, Smith SM, Huang B, Ruan WJ, Zhang H, et al. The epidemiology of DSM-5 nicotine use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. J Clin Psychiatry. (2016) 77:1404–12. doi: 10.4088/JCP.15m10114
272. Peltzer K, Pengpid S. Depressive symptoms and social demographic, stress and health risk behaviour among university students in 26 low-, middle- and high-income countries. Int J Psychiatry Clin Pract. (2015) 19:259–65. doi: 10.3109/13651501.2015.1082598
273. Sumbe A, Wilkinson AV, Clendennen SL, Bataineh BS, Sterling KL, Chen B, et al. Association of tobacco and marijuana use with symptoms of depression and anxiety among adolescents and young adults in Texas. Tob Prev Cessation. (2022) 8:03. doi: 10.18332/tpc/144500
274. Kastaun S, Brose LS, Scholz E, Viechtbauer W, Kotz D. Mental health symptoms and associations with tobacco smoking, dependence, motivation, and attempts to quit: findings from a population survey in Germany (DEBRA study). Eur Addict Res. (2022) 28:287–96. doi: 10.1159/000523973
275. Ellis EM, Orom H, Giovino GA, Kiviniemi MT. Relations between negative affect and health behaviors by race/ethnicity: differential effects for symptoms of depression and anxiety. Health Psychol. (2015) 34:966–9. doi: 10.1037/hea0000197
276. Pengpid S, Peltzer K. High sedentary behavior is associated with depression among rural South Africans. Int J Environ Res Public Health. (2019) 16:1413. doi: 10.3390/ijerph16081413
277. Assari S, Smith JL, Zimmerman MA, Bazargan M. Cigarette smoking among economically disadvantaged African-American older adults in south Los Angeles: gender differences. Int J Environ Res Public Health. (2019) 16:1208. doi: 10.3390/ijerph16071208
278. Li M, Sun W, Wang Y, Qi C. Prevalence and differences of depression, anxiety, and substance use between Chinese college-age students studying in China and America during the coronavirus disease 2019 pandemic. Front Psychiatry. (2022) 13:805120. doi: 10.3389/fpsyt.2022.805120
279. Sawchuk CN, Roy-Byrne P, Noonan C, Bogart A, Goldberg J, Manson SM, et al. The association of panic disorder, posttraumatic stress disorder, and major depression with smoking in American Indians. Nicotine Tob Res. (2016) 18:259–66. doi: 10.1093/ntr/ntv071
280. Chou SP, Saha TD, Zhang H, Ruan WJ, Huang B, Grant BF, et al. Prevalence, correlates, comorbidity and treatment of electronic nicotine delivery system use in the United States. Drug Alcohol Depend. (2017) 178:296–301. doi: 10.1016/j.drugalcdep.2017.05.026
281. Hruby A, Lieberman HR, Smith TJ. Symptoms of depression, anxiety, and post-traumatic stress disorder and their relationship to health-related behaviors in over 12,000 US military personnel: bi-directional associations. J Affect Disord. (2021) 283:84–93. doi: 10.1016/j.jad.2021.01.029
282. Zhu Y, Yu X, Wu Y, Shi C, Zhang A, Jiang R, et al. Association of depression and unhealthy lifestyle behaviors in Chinese patients with acute coronary syndromes. J Cardiopulm Rehabil Prev. (2019) 39:E1–5. doi: 10.1097/HCR.0000000000000384
283. Humer E, Probst T, Wagner-Skacel J, Pieh C. Association of health behaviors with mental health problems in more than 7000 adolescents during COVID-19. Int J Environ Res Public Health. (2022) 19:9072. doi: 10.3390/ijerph19159072
284. Xie H, Tao S, Zhang Y, Tao F, Wu X. Impact of problematic mobile phone use and insufficient physical activity on depression symptoms: a college-based follow-up study. BMC Public Health. (2019) 19:1640. doi: 10.1186/s12889-019-7873-z
285. Zhu Y, Blumenthal JA, Shi C, Jiang R, Patel A, Zhang A, et al. Sedentary behavior and the risk of depression in patients with acute coronary syndromes. Am J Cardiol. (2018) 121:1456–60. doi: 10.1016/j.amjcard.2018.02.031
286. Galán-Arroyo C, Pereira-Payo D, Rojo-Ramos J, Hernández-Mocholí MA, Merellano-Navarro E, Pérez-Gómez J, et al. Increased odds for depression and antidepressant use in the inactive Spanish population. Int J Environ Res Public Health. (2022) 19:2829. doi: 10.3390/ijerph19052829
287. Xu Z, Xu Q, Wang Y, Zhang J, Liu J, Xu F. Association of sedentary behavior and depression among college students majoring in design. Int J Environ Res Public Health. (2020) 17:3545. doi: 10.3390/ijerph17103545
288. Adamson BC, Yang Y, Motl RW. Association between compliance with physical activity guidelines, sedentary behavior and depressive symptoms. Prev Med. (2016) 91:152–7. doi: 10.1016/j.ypmed.2016.08.020
289. Jiang L, Cao Y, Ni S, Chen X, Shen M, Lv H, et al. Association of sedentary behavior with anxiety, depression, and suicide ideation in college students. Front Psychiatry. (2020) 11:566098. doi: 10.3389/fpsyt.2020.566098
290. Vadlin S, Åslund C, Hellström C, Nilsson KW. Associations between problematic gaming and psychiatric symptoms among adolescents in two samples. Addict Behav. (2016) 61:8–15. doi: 10.1016/j.addbeh.2016.05.001
291. Alageel AA, Alyahya RA, Bahatheq AY, Alzunaydi NA, Alghamdi RA, Alrahili NM, et al. Smartphone addiction and associated factors among postgraduate students in an Arabic sample: a cross-sectional study. BMC Psychiatry. (2021) 21:302. doi: 10.1186/s12888-021-03285-0
292. Werneck AO, Oyeyemi AL, Szwarcwald CL, Vancampfort D, Silva DR. Associations between TV viewing and depressive symptoms among 60,202 Brazilian adults: the Brazilian National Health Survey. J Affect Disord. (2018) 236:23–30. doi: 10.1016/j.jad.2018.04.083
293. Vancampfort D, Stubbs B, Lara E, Vandenbulcke M, Swinnen N, Koyanagi A. Correlates of sedentary behavior in middle-aged and old age people with mild cognitive impairment: a multinational study. Int Psychogeriatr. (2019) 31:579–89. doi: 10.1017/S1041610218001163
294. Yu B, Gu Y, Bao X, Meng G, Wu H, Zhang Q, et al. Distinct associations of computer/mobile devices use and TV watching with depressive symptoms in adults: a large population study in China. Depress Anxiety. (2019) 36:879–86. doi: 10.1002/da.22932
295. Trinh L, Wong B, Faulkner GE. The independent and interactive associations of screen time and physical activity on mental health, school connectedness and academic achievement among a population-based sample of youth. J Can Acad Child Adolesc Psychiatry. (2015) 24:17–24.
296. Vancampfort D, Hallgren M, Schuch F, Stubbs B, Smith L, Rosenbaum S, et al. Sedentary behavior and depression among community-dwelling adults aged ≥50 years: results from the Irish Longitudinal Study on Ageing. J Affect Disord. (2020) 262:389–96. doi: 10.1016/j.jad.2019.11.066
297. Wu X, Tao S, Zhang Y, Zhang S, Tao F. Low physical activity and high screen time can increase the risks of mental health problems and poor sleep quality among Chinese college students. PLoS ONE. (2015) 10:e0119607. doi: 10.1371/journal.pone.0119607
298. da Costa ME, Cândido LM, de Avelar NCP, Danielewicz AL. How much time of sedentary behavior is associated with depressive symptoms in community-dwelling older adults in southern Brazil? Geriatr Nurs. (2023) 50:25–30. doi: 10.1016/j.gerinurse.2022.12.014
299. Lazarevich I, Irigoyen Camacho ME, Velázquez-Alva MC, Flores NL, Nájera Medina O, Zepeda Zepeda MA. Depression and food consumption in Mexican college students. Nutr Hosp. (2018) 35:620–6. doi: 10.20960/nh.1500
300. Liu M, Ming Q, Yi J, Wang X, Yao S. Screen time on school days and risks for psychiatric symptoms and self-harm in mainland Chinese adolescents. Front Psychol. (2016) 7:574. doi: 10.3389/fpsyg.2016.00574
301. Jensen-Otsu E, Austin GL. Antidepressant use is associated with increased energy intake and similar levels of physical activity. Nutrients. (2015) 7:9662–71. doi: 10.3390/nu7115489
302. Cho J, Jin Y, Kang H. Weight status, physical activity, and depression in Korean older adults. J Epidemiol. (2018) 28:292–9. doi: 10.2188/jea.JE20170083
303. Zhang Y, Tao S, Qu Y, Mou X, Gan H, Zhou P, et al. The correlation between lifestyle health behaviors, coping style, and mental health during the COVID-19 pandemic among college students: two rounds of a web-based study. Front Public Health. (2023) 10:1031560. doi: 10.3389/fpubh.2022.1031560
304. da Costa BGG, Chaput JP, Lopes MVV, Malheiros LEA, Silva KS. Movement behaviors and their association with depressive symptoms in Brazilian adolescents: a cross-sectional study. J Sport Health Sci. (2022) 11:252–9. doi: 10.1016/j.jshs.2020.08.003
305. Silva DR, Collings P, Araujo RHO, Barboza LL, Szwarcwald CL, Werneck AO. Correlates of screen-based behaviors among adults from the 2019 Brazilian National Health Survey. BMC Public Health. (2021) 21:2289. doi: 10.1186/s12889-021-12340-0
306. Lu C, Chi X, Liang K, Chen ST, Huang L, Guo T, et al. Moving more and sitting less as healthy lifestyle behaviors are protective factors for insomnia, depression, and anxiety among adolescents during the COVID-19 pandemic. Psychol Res Behav Manag. (2020) 13:1223–33. doi: 10.2147/PRBM.S284103
307. Wu X, Tao S, Zhang S, Zhang Y, Chen K, Yang Y, et al. Impact of screen time on mental health problems progression in youth: a 1-year follow-up study. BMJ Open. (2016) 6:e011533. doi: 10.1136/bmjopen-2016-011533
308. Zhou H, Dai X, Lou L, Zhou C, Zhang W. Association of sedentary behavior and physical activity with depression in sport university students. Int J Environ Res Public Health. (2021) 18:9881. doi: 10.3390/ijerph18189881
309. Vancampfort D, Stubbs B, Firth J, Van Damme T, Koyanagi A. Sedentary behavior and depressive symptoms among 67,077 adolescents aged 12-15 years from 30 low- and middle-income countries. Int J Behav Nutr Phys Act. (2018) 15:73. doi: 10.1186/s12966-018-0708-y
310. Hanna F, Daas RN, El-Shareif TJ, Al-Marridi HH, Al-Rojoub ZM, Adegboye OA. The relationship between sedentary behavior, back pain, and psychosocial correlates among university employees. Front Public Health. (2019) 7:80. doi: 10.3389/fpubh.2019.00080
311. Schuch FB, Bulzing RA, Meyer J, Vancampfort D, Firth J, Stubbs B, et al. Associations of moderate to vigorous physical activity and sedentary behavior with depressive and anxiety symptoms in self-isolating people during the COVID-19 pandemic: a cross-sectional survey in Brazil. Psychiatry Res. (2020) 292:113339. doi: 10.1016/j.psychres.2020.113339
312. Kim HR, Han MA. Associations between problematic smartphone use, unhealthy behaviors, and mental health status in Korean adolescents: based on data from the 13th Korea Youth Risk Behavior Survey (2017). Psychiatry Investig. (2020) 17:1216–25. doi: 10.30773/pi.2020.0007
313. Apriliyasari RW, Budi IS, Tan MP, Tsai PS. Physical activity and depression in Indonesian adults with stroke: a nationwide survey. J Nurs Scholarsh. (2023) 55:356–64. doi: 10.1111/jnu.12823
314. Carriedo A, Cecchini JA, Fernandez-Rio J, Méndez-Giménez A. COVID-19, psychological well-being and physical activity levels in older adults during the nationwide lockdown in Spain. Am J Geriatr Psychiatry. (2020) 28:1146–55. doi: 10.1016/j.jagp.2020.08.007
315. Souza AM, Fillenbaum GG, Blay SL. Prevalence and correlates of physical inactivity among older adults in Rio Grande do Sul, Brazil. PLoS ONE. (2015) 10:e0117060. doi: 10.1371/journal.pone.0117060
316. Liao Y, Shibata A, Ishii K, Oka K. Independent and combined associations of physical activity and sedentary behavior with depressive symptoms among Japanese adults. Int J Behav Med. (2016) 23:402–9. doi: 10.1007/s12529-015-9484-0
317. Pengpid S, Peltzer K. Prevalence and associated factors of physical inactivity among middle-aged and older adults in India: results of a national cross-sectional community survey. BMJ Open. (2022) 12:e058156. doi: 10.1136/bmjopen-2021-058156
318. Pengpid S, Peltzer K. High sedentary behaviour and low physical activity are associated with anxiety and depression in Myanmar and Vietnam. Int J Environ Res Public Health. (2019) 16:1251. doi: 10.3390/ijerph16071251
319. Taheri E, Heshmat R, Esmaeil Motlagh M, Ardalan G, Asayesh H, Qorbani M, et al. Association of physical activity and screen time with psychiatric distress in children and adolescents: CASPIAN-IV Study. J Trop Pediatr. (2019) 65:361–72. doi: 10.1093/tropej/fmy063
320. Draper CE, Cook CJ, Redinger S, Rochat T, Prioreschi A, Rae DE, et al. Cross-sectional associations between mental health indicators and social vulnerability, with physical activity, sedentary behaviour and sleep in urban African young women. Int J Behav Nutr Phys Act. (2022) 19:82. doi: 10.1186/s12966-022-01325-w
321. Padmapriya N, Bernard JY, Liang S, Loy SL, Shen Z, Kwek K, et al. Association of physical activity and sedentary behavior with depression and anxiety symptoms during pregnancy in a multiethnic cohort of Asian women. Arch Womens Ment Health. (2016) 19:1119–28. doi: 10.1007/s00737-016-0664-y
322. ElBarazi A, Tikamdas R. Association between university student junk food consumption and mental health. Nutr Health. (2023) 1–7. doi: 10.1177/02601060231151480. [Epub ahead of print].
323. Khosravi M, Sotoudeh G, Majdzadeh R, Nejati S, Darabi S, Raisi F, et al. Healthy and unhealthy dietary patterns are related to depression: a case-control study. Psychiatry Investig. (2015) 12:434–42. doi: 10.4306/pi.2015.12.4.434
324. Gomes AP, Oliveira Bierhals I, Gonçalves Soares AL, Hellwig N, Tomasi E, Formoso Assunção MC, et al. Interrelationship between diet quality and depressive symptoms in elderly. J Nutr Health Aging. (2018) 22:387–92. doi: 10.1007/s12603-017-0963-7
325. Liu J, Chen T, Chen M, Ma Y, Ma T, Gao D, et al. Sugar-sweetened beverages and depressive and social anxiety symptoms among children and adolescents aged 7-17 years, stratified by body composition. Front Nutr. (2022) 994:888671. doi: 10.3389/fnut.2022.888671
326. Hong SA, Peltzer K. Dietary behaviour, psychological well-being and mental distress among adolescents in Korea. Child Adolesc Psychiatry Ment Health. (2017) 11:56. doi: 10.1186/s13034-017-0194-z
327. Kim TH, Choi JY, Lee HH, Park Y. Associations between dietary pattern and depression in Korean adolescent girls. J Pediatr Adolesc Gynecol. (2015) 28:533–7. doi: 10.1016/j.jpag.2015.04.005
328. Yu B, He H, Zhang Q, Wu H, Du H, Liu L, et al. Soft drink consumption is associated with depressive symptoms among adults in China. J Affect Disord. (2015) 172:422–7. doi: 10.1016/j.jad.2014.10.026
329. Liu ZM, Ho SC, Xie YJ, Chen YJ, Chen YM, Chen B, et al. Associations between dietary patterns and psychological factors: a cross-sectional study among Chinese postmenopausal women. Menopause. (2016) 23:1294–302. doi: 10.1097/GME.0000000000000701
330. Vicente BM, Neto JV, Quaresma MVLDS, Vasconcelos JS, Espíndola Bauchiunas R, Dos Santos ECM, et al. Covid-19 social distancing, lifestyle and health outcomes among persons living with HIV (PLWH): a web-based survey. AIDS Behav. (2022) 26:4144–55. doi: 10.1007/s10461-022-03740-3
331. Sangsefidi ZS, Lorzadeh E, Hosseinzadeh M, Mirzaei M. Dietary habits and psychological disorders in a large sample of Iranian adults: a population-based study. Ann Gen Psychiatry. (2020) 19:8. doi: 10.1186/s12991-020-00263-w
332. Kim J, Hong C, Lee G. Association between sugar-sweetened beverage consumption and depression and suicidal ideation among Korean adults: a cross-sectional study from the 2014 and 2016 Korean National Health and Nutrition Examination Survey (KNHANES). Nutr Res Pract. (2022) 16:194–204. doi: 10.4162/nrp.2022.16.2.194
333. Kang M, Joo M, Hong H, Kang H. The relationship of lifestyle risk factors and depression in Korean adults: a moderating effect of overall nutritional adequacy. Nutrients. (2021) 13:2626. doi: 10.3390/nu13082626
334. Park S, Rim SJ, Lee JH. Associations between dietary behaviours and perceived physical and mental health status among Korean adolescents. Nutr Diet. (2018) 75:488–93. doi: 10.1111/1747-0080.12444
335. Ra JS. Consumption of sugar-sweetened beverages and fast foods deteriorates adolescents' mental health. Front Nutr. (2022) 9:1058190. doi: 10.3389/fnut.2022.1058190
336. Zheng L, Sun J, Yu X, Zhang D. Ultra-processed food is positively associated with depressive symptoms among United States adults. Front Nutr. (2020) 7:600449. doi: 10.3389/fnut.2020.600449
337. Xia Y, Wang N, Yu B, Zhang Q, Liu L, Meng G, et al. Dietary patterns are associated with depressive symptoms among Chinese adults: a case-control study with propensity score matching. Eur J Nutr. (2017) 56:2577–87. doi: 10.1007/s00394-016-1293-y
338. Tran A, Tran L, Geghre N, Darmon D, Rampal M, Brandone D, et al. Health assessment of French university students and risk factors associated with mental health disorders. PLoS ONE. (2017) 12:e0188187. doi: 10.1371/journal.pone.0188187
339. Miller C, Ettridge K, Wakefield M, Pettigrew S, Coveney J, Roder D, et al. Consumption of sugar-sweetened beverages, juice, artificially-sweetened soda and bottled water: an Australian population study. Nutrients. (2020) 12:817. doi: 10.3390/nu12030817
340. Nouri Saeidlou S, Kiani A, Ayremlou P. Association between dietary patterns and major depression in adult females: a case-control study. J Res Health Sci. (2021) 21:e00506. doi: 10.34172/jrhs.2021.37
341. Yim HR, Yun HJ, Lee JH. An investigation on Korean adolescents' dietary consumption: focused on sociodemographic characteristics, physical health, and mental health. Int J Environ Res Public Health. (2021) 18:9773. doi: 10.3390/ijerph18189773
342. Knüppel A, Shipley MJ, Llewellyn CH, Brunner EJ. Sugar intake from sweet food and beverages, common mental disorder and depression: prospective findings from the Whitehall II study. Sci Rep. (2017) 7:6287. doi: 10.1038/s41598-017-05649-7
343. Hall L, Tejada-Tayabas LM, Monárrez-Espino J. Breakfast skipping, anxiety, exercise, and soda consumption are associated with diet quality in Mexican college students. Ecol Food Nutr. (2017) 56:218–37. doi: 10.1080/03670244.2017.1299010
344. Hosseinzadeh M, Vafa M, Esmaillzadeh A, Feizi A, Majdzadeh R, Afshar H, et al. Empirically derived dietary patterns in relation to psychological disorders. Public Health Nutr. (2016) 19:204–17. doi: 10.1017/S136898001500172X
345. Hengartner MP, Angst J, Ajdacic-Gross V, Rössler W. Cannabis use during adolescence and the occurrence of depression, suicidality and anxiety disorder across adulthood: findings from a longitudinal cohort study over 30 years. J Affect Disord. (2020) 272:98–103. doi: 10.1016/j.jad.2020.03.126
346. Agrawal A, Nelson EC, Bucholz KK, Tillman R, Grucza RA, Statham DJ, et al. Major depressive disorder, suicidal thoughts and behaviours, and cannabis involvement in discordant twins: a retrospective cohort study. Lancet Psychiatry. (2017) 4:706–14. doi: 10.1016/S2215-0366(17)30280-8
347. Blanco C, Hasin DS, Wall MM, Flórez-Salamanca L, Hoertel N, Wang S, et al. Cannabis use and risk of psychiatric disorders: prospective evidence from a US national longitudinal study. JAMA Psychiatry. (2016) 73:388–95. doi: 10.1001/jamapsychiatry.2015.3229
348. Feingold D, Weiser M, Rehm J, Lev-Ran S. The association between cannabis use and mood disorders: a longitudinal study. J Affect Disord. (2015) 172:211–8. doi: 10.1016/j.jad.2014.10.006
349. Bakhshaie J, Zvolensky MJ, Goodwin RD. Cigarette smoking and the onset and persistence of depression among adults in the United States: 1994-2005. Compr Psychiatry. (2015) 60:142–8. doi: 10.1016/j.comppsych.2014.10.012
350. Zhang XC, Woud ML, Becker ES, Margraf J. Do health-related factors predict major depression? A longitudinal epidemiologic study. Clin Psychol Psychother. (2018) 25:378–87. doi: 10.1002/cpp.2171
351. Tsutsumimoto K, Makizako H, Doi T, Hotta R, Nakakubo S, Shimada H, et al. Prospective associations between sedentary behaviour and incident depressive symptoms in older people: a 15-month longitudinal cohort study. Int J Geriatr Psychiatry. (2017) 32:193–200. doi: 10.1002/gps.4461
352. Cabello M, Miret M, Caballero FF, Chatterji S, Naidoo N, Kowal P, et al. The role of unhealthy lifestyles in the incidence and persistence of depression: a longitudinal general population study in four emerging countries. Glob Health. (2017) 13:18. doi: 10.1186/s12992-017-0237-5
353. Song C, Li W, Leng J, Wang L, Li W, Shi F, et al. Passive smoking and postpartum depression among Chinese women: a prospective cohort study in Tianjin, China. Women Health. (2019) 59:281–93. doi: 10.1080/03630242.2018.1478365
354. Bolstad I, Alakokkare AE, Bramness JG, Rognli EB, Levola J, Mustonen A, et al. The relationships between use of alcohol, tobacco and coffee in adolescence and mood disorders in adulthood. Acta Psychiatr Scand. (2022) 146:594–603. doi: 10.1111/acps.13506
355. Grøntved A, Singhammer J, Froberg K, Møller NC, Pan A, Pfeiffer KA, et al. A prospective study of screen time in adolescence and depression symptoms in young adulthood. Prev Med. (2015) 81:108–13. doi: 10.1016/j.ypmed.2015.08.009
356. Sui X, Brown WJ, Lavie CJ, West DS, Pate RR, Payne JP, et al. Associations between television watching and car riding behaviors and development of depressive symptoms: a prospective study. Mayo Clin Proc. (2015) 90:184–93. doi: 10.1016/j.mayocp.2014.12.006
357. Pavey TG, Brown WJ. Sitting time and depression in young women over 12-years: the effect of physical activity. J Sci Med Sport. (2019) 22:1125–31. doi: 10.1016/j.jsams.2019.06.010
358. Zink J, Belcher BR, Kechter A, Stone MD, Leventhal AM. Reciprocal associations between screen time and emotional disorder symptoms during adolescence. Prev Med Rep. (2019) 13:281–8. doi: 10.1016/j.pmedr.2019.01.014
359. Bolanis D, Orri M, Castellanos-Ryan N, Renaud J, Montreuil T, Boivin M, et al. Cannabis use, depression and suicidal ideation in adolescence: direction of associations in a population based cohort. J Affect Disord. (2020) 274:1076–83. doi: 10.1016/j.jad.2020.05.136
360. Bierhoff J, Haardörfer R, Windle M, Berg CJ. Psychological risk factors for alcohol, cannabis, and various tobacco use among young adults: a longitudinal analysis. Subst Use Misuse. (2019) 54:1365–75. doi: 10.1080/10826084.2019.1581220
361. Stapinski LA, Montgomery AA, Araya R. Anxiety, depression and risk of cannabis use: examining the internalising pathway to use among Chilean adolescents. Drug Alcohol Depend. (2016) 166:109–15. doi: 10.1016/j.drugalcdep.2016.06.032
362. Lechner WV, Janssen T, Kahler CW, Audrain-McGovern J, Leventhal AM. Bi-directional associations of electronic and combustible cigarette use onset patterns with depressive symptoms in adolescents. Prev Med. (2017) 96:73–8. doi: 10.1016/j.ypmed.2016.12.034
363. López-Gil JF, Cavero-Redondo I, Tárraga López PJ, Jiménez-López E, González AD, Sequí-Domínguez I, et al. Anxiety-induced sleep disturbance and associated lifestyle behaviors according to sex in Argentine adolescents. Front Behav Neurosci. (2022) 16:860241. doi: 10.3389/fnbeh.2022.860241
364. Hajure M, Tariku M, Mohammedhussein M, Dule A. Depression, anxiety and associated factors among chronic medical patients amid COVID-19 pandemic in Mettu Karl Referral Hospital, Mettu, Ethiopia, 2020. Neuropsychiatr Dis Treat. (2020) 16:2511–8. doi: 10.2147/NDT.S281995
365. Nakie G, Segon T, Melkam M, Desalegn GT, Zeleke TA. Prevalence and associated factors of depression, anxiety, and stress among high school students in, Northwest Ethiopia, 2021. BMC Psychiatry. (2022) 22:739. doi: 10.1186/s12888-022-04393-1
366. Peltzer K, Pengpid S. Tobacco use and its association with mental morbidity and health compromising behaviours in adolescents in Indonesia. Asian Pac J Cancer Prev. (2021) 22:31–5. doi: 10.31557/APJCP.2021.22.1.31
367. Parker MA, Sigmon SC, Villanti AC. Higher smoking prevalence among United States adults with co-occurring affective and drug use diagnoses. Addict Behav. (2019) 99:106112. doi: 10.1016/j.addbeh.2019.106112
368. Abbasi-Ghahramanloo A, Janani L, Malakouti SK, Rabetian M, Rimaz S. Prevalence of cigarette smoking and its related factors among Iranian male workers. Med J Islam Repub Iran. (2020) 34:150. doi: 10.47176/mjiri.34.150
369. Asfaw H, Fekadu G, Tariku M, Oljira A. Anxiety and stress among undergraduate medical students of Haramaya University, Eastern Ethiopia. Neuropsychiatr Dis Treat. (2021) 17:139–46. doi: 10.2147/NDT.S290879
370. Chen S, Clark CCT, Ren Z. Different types of screen-based sedentary time and anxiety in adolescents: video games may be more important. Front Public Health. (2022) 10:918234. doi: 10.3389/fpubh.2022.918234
371. Wen X, Zhu F, Yuan Z, Mao Z. Relationship between physical activity, screen-related sedentary behaviors and anxiety among adolescents in less developed areas of China. Medicine. (2022) 101:e30848. doi: 10.1097/MD.0000000000030848
372. Vancampfort D, Van Damme T, Stubbs B, Smith L, Firth J, Hallgren M, et al. Sedentary behavior and anxiety-induced sleep disturbance among 181,093 adolescents from 67 countries: a global perspective. Sleep Med. (2019) 58:19–26. doi: 10.1016/j.sleep.2019.01.048
373. Bu H, He A, Gong N, Huang L, Liang K, Kastelic K, et al. Optimal movement behaviors: correlates and associations with anxiety symptoms among Chinese university students. BMC Public Health. (2021) 21:2052. doi: 10.1186/s12889-021-12116-6
374. Vancampfort D, Stubbs B, Herring MP, Hallgren M, Koyanagi A. Sedentary behavior and anxiety: association and influential factors among 42,469 community-dwelling adults in six low- and middle-income countries. Gen Hosp Psychiatry. (2018) 50:26–32. doi: 10.1016/j.genhosppsych.2017.09.006
375. Kang HJ, Bae KY, Kim SW, Shin IS, Yoon JS, Kim JM. Anxiety symptoms in Korean elderly individuals: a two-year longitudinal community study. Int Psychogeriatr. (2016) 28:423–33. doi: 10.1017/S1041610215001301
376. Wang MH, Xiao DM, Liu MW, Lu YA, He QQ. Relationship between sedentary behaviour and anxiety symptoms among youth in 24 low- and middle-income countries. PLoS ONE. (2020) 15:e0241303. doi: 10.1371/journal.pone.0241303
377. Werneck AO, Hoare E, Silva DR. Do TV viewing and frequency of ultra-processed food consumption share mediators in relation to adolescent anxiety-induced sleep disturbance? Public Health Nutr. (2021) 24:5491–7. doi: 10.1017/S1368980021000379
378. Song H, Lee K. Increased risk of generalized anxiety disorder according to frequent sedentary times based on the 16th Korea Youth Risk Behavior Web-based Survey. Children. (2022) 9:1548. doi: 10.3390/children9101548
379. Khan A, Uddin R. Is consumption of fast-food and carbonated soft drink associated with anxiety-induced sleep disturbance among adolescents? A population-based study. Clin Nutr ESPEN. (2020) 36:162–5. doi: 10.1016/j.clnesp.2020.01.011
380. Werneck AO, Vancampfort D, Oyeyemi AL, Stubbs B, Silva DR. Joint association of ultra-processed food and sedentary behavior with anxiety-induced sleep disturbance among Brazilian adolescents. J Affect Disord. (2020) 266:135–42. doi: 10.1016/j.jad.2020.01.104
381. Kaufman-Shriqui V, Navarro DA, Raz O, Boaz M. Dietary changes and anxiety during the coronavirus pandemic: a multinational survey. Eur J Clin Nutr. (2022) 76:84–92. doi: 10.1038/s41430-021-00897-3
382. Green KM, Doherty EE, Ensminger ME. Long-term consequences of adolescent cannabis use: examining intermediary processes. Am J Drug Alcohol Abuse. (2017) 43:567–75. doi: 10.1080/00952990.2016.1258706
383. Feingold D, Weiser M, Rehm J, Lev-Ran S. The association between cannabis use and anxiety disorders: results from a population-based representative sample. Eur Neuropsychopharmacol. (2016) 26:493–505. doi: 10.1016/j.euroneuro.2015.12.037
384. Tran DD, Fitzke RE, Wang J, Davis JP, Pedersen ER. Substance use, financial stress, employment disruptions, and anxiety among veterans during the COVID-19 pandemic. Psychol Rep. (2022) 126:1684–1700. doi: 10.1177/00332941221080413
385. Patel RS, Cheema Z, Singla A, Cornejo M, Verma G. Cannabis use is an independent risk factor for manic episode: a report from 380,265 bipolar inpatients. Subst Use Misuse. (2022) 57:344–9. doi: 10.1080/10826084.2021.2012690
386. Yeh TC, Wang SC, Chang YT, Yeh CB. Predictors of nicotine dependence in adolescents: symptoms of bipolar disorder and attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. (2017) 27:366–73. doi: 10.1089/cap.2016.0099
387. Marwaha S, Winsper C, Bebbington P, Smith D. Cannabis use and hypomania in young people: a prospective analysis. Schizophr Bull. (2018) 44:1267–74. doi: 10.1093/schbul/sbx158
388. Jemal M, Tessema W, Agenagnew L. Cluster B personality disorders and its associated factors among psychiatric outpatients in Southwest Ethiopia: institutional-based cross-sectional study. BMC Psychiatry. (2022) 22:500. doi: 10.1186/s12888-022-04143-3
389. Holzer KJ, Vaughn MG, Loux TM, Mancini MA, Fearn NE, Wallace CL. Prevalence and correlates of antisocial personality disorder in older adults. Aging Ment Health. (2022) 26:169–78. doi: 10.1080/13607863.2020.1839867
390. Goldstein RB, Chou SP, Saha TD, Smith SM, Jung J, Zhang H, et al. The epidemiology of antisocial behavioral syndromes in adulthood: results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. J Clin Psychiatry. (2017) 78:90–8. doi: 10.4088/JCP.15m10358
391. Carpenter RW, Wood PK, Trull TJ. Comorbidity of borderline personality disorder and lifetime substance use disorders in a nationally representative sample. J Pers Disord. (2016) 30:336–50. doi: 10.1521/pedi_2015_29_197
392. Capusan AJ, Bendtsen P, Marteinsdottir I, Larsson H. Comorbidity of adult ADHD and its subtypes with substance use disorder in a large population-based epidemiological study. J Atten Disord. (2019) 23:1416–26. doi: 10.1177/1087054715626511
393. Karlsson P, Ekendahl M, Raninen J. Exploring the link between ADHD and cannabis use in Swedish ninth graders: the role of conduct problems and sensation-seeking. Subst Use Misuse. (2022) 58:311–9. doi: 10.1080/10826084.2022.2155478
394. Moulin F, Chollet A, Ramos-Quiroga JA, Bouvard M, Melchior M, Galéra C. Prevalence and psychosocial correlates of ADHD symptoms in young adulthood: a French population-based study. J Atten Disord. (2018) 22:167–81. doi: 10.1177/1087054717706758
395. Fuller-Thomson E, Lewis DA, Agbeyaka S. Attention-deficit/hyperactivity disorder and alcohol and other substance use disorders in young adulthood: findings from a Canadian nationally representative survey. Alcohol Alcohol. (2022) 57:385–95. doi: 10.1093/alcalc/agab048
396. Riegler A, Völkl-Kernstock S, Lesch O, Walter H, Skala K. Attention deficit hyperactivity disorder and substance abuse: an investigation in young Austrian males. J Affect Disord. (2017) 217:60–5. doi: 10.1016/j.jad.2017.03.072
397. Yeom CW, Oh GH, Jung S, Moon JY, Son KL, Kim WH, et al. Prevalence and comorbidities of adult ADHD in male military conscripts in Korea: results of an epidemiological survey of mental health in Korean military service. Psychiatry Res. (2020) 293:113401. doi: 10.1016/j.psychres.2020.113401
398. Galéra C, Salla J, Montagni I, Hanne-Poujade S, Salamon R, Grondin O, et al. Stress, attention deficit hyperactivity disorder (ADHD) symptoms and tobacco smoking: the i-Share study. Eur Psychiatry. (2017) 45:221–6. doi: 10.1016/j.eurpsy.2017.07.007
399. Xu G, Snetselaar LG, Strathearn L, Ryckman K, Nothwehr F, Torner J. Association of attention-deficit/hyperactivity disorder with e-cigarette use. Am J Prev Med. (2021) 60:488–96. doi: 10.1016/j.amepre.2020.11.010
400. Weissenberger S, Ptacek R, Vnukova M, Raboch J, Klicperova-Baker M, Domkarova L, et al. ADHD and lifestyle habits in Czech adults, a national sample. Neuropsychiatr Dis Treat. (2018) 14:293–9. doi: 10.2147/NDT.S148921
401. Chowdhury S. Screen time and attention deficit hyperactive symptoms among young adults in Bangladesh: an online cross-sectional study during the COVID-19 pandemic. Found Univ J Psychol. (2023) 7:10–9.
402. Gul H, Yurumez Solmaz E, Gul A, Oner O. Facebook overuse and addiction among Turkish adolescents: are ADHD and ADHD-related problems risk factors? Psychiatr Clin Psychopharmacol. (2018) 28:80–90. doi: 10.1080/24750573.2017.1383706
403. Claesdotter-Knutsson E, André F, Fridh M, Delfin C, Hakansson A, Lindström M. Gender-based differences and associated factors surrounding excessive smartphone use among adolescents: cross-sectional study. JMIR Pediatr Parent. (2021) 4:e30889. doi: 10.2196/30889
404. Cook BG, Li D, Heinrich KM. Obesity, physical activity, and sedentary behavior of youth with learning disabilities and ADHD. J Learn Disabil. (2015) 48:563–76. doi: 10.1177/0022219413518582
405. Ríos-Hernández A, Alda JA, Farran-Codina A, Ferreira-García E, Izquierdo-Pulido M. The Mediterranean diet and ADHD in children and adolescents. Pediatrics. (2017) 139:e20162027. doi: 10.1542/peds.2016-2027
406. Yu CJ, Du JC, Chiou HC, Feng CC, Chung MY, Yang W, et al. Sugar-sweetened beverage consumption is adversely associated with childhood attention deficit/hyperactivity disorder. Int J Environ Res Public Health. (2016) 13:678. doi: 10.3390/ijerph13070678
407. Abbasi K, Beigrezai S, Ghiasvand R, Pourmasoumi M, Mahaki B. Dietary patterns and attention deficit hyperactivity disorder among Iranian children: a case-control study. J Am Coll Nutr. (2019) 38:76–83. doi: 10.1080/07315724.2018.1473819
408. Yan S, Cao H, Gu C, Ni L, Tao H, Shao T, et al. Dietary patterns are associated with attention-deficit/hyperactivity disorder (ADHD) symptoms among preschoolers in mainland China. Eur J Clin Nutr. (2018) 72:1517–23. doi: 10.1038/s41430-018-0131-0
409. Kim KM, Lim MH, Kwon HJ, Yoo SJ, Kim EJ, Kim JW, et al. Associations between attention-deficit/hyperactivity disorder symptoms and dietary habits in elementary school children. Appetite. (2018) 127:274–9. doi: 10.1016/j.appet.2018.05.004
410. Zhou F, Wu F, Zou S, Chen Y, Feng C, Fan G. Dietary, nutrient patterns and blood essential elements in Chinese children with ADHD. Nutrients. (2016) 8:352. doi: 10.3390/nu8060352
411. Poulain T, Vogel M, Neef M, Abicht F, Hilbert A, Genuneit J, et al. Reciprocal associations between electronic media use and behavioral difficulties in preschoolers. Int J Environ Res Public Health. (2018) 15:814. doi: 10.3390/ijerph15040814
412. Del-Ponte B, Anselmi L, Assunção MCF, Tovo-Rodrigues L, Munhoz TN, Matijasevich A, et al. Sugar consumption and attention-deficit/hyperactivity disorder (ADHD): a birth cohort study. J Affect Disord. (2019) 243:290–6. doi: 10.1016/j.jad.2018.09.051
413. Jean FAM, Arsandaux J, Montagni I, Collet O, Fatséas M, Auriacombe M, et al. Attention deficit hyperactivity disorder symptoms and cannabis use after one year among students of the i-Share cohort. Eur Psychiatry. (2022) 65:1–18. doi: 10.1192/j.eurpsy.2022.14
414. Vogel T, Dom G, van de Glind G, Studer J, Gmel G, Strik W, et al. Is attention deficit/hyperactivity disorder among men associated with initiation or escalation of substance use at 15-month follow-up? A longitudinal study involving young Swiss men. Addiction. (2016) 111:1867–78. doi: 10.1111/add.13422
415. Kim S, Kim D. Behavioral symptoms of child mental disorders and lifetime substance use in adolescence: a within-family comparison of US siblings. Drug Alcohol Depend. (2021) 219:108490. doi: 10.1016/j.drugalcdep.2020.108490
416. Moggi F, Schorno D, Soravia LM, Mohler-Kuo M, Estévez-Lamorte N, Studer J, et al. Screened attention deficit/hyperactivity disorder as a predictor of substance use initiation and escalation in early adulthood and the role of self-reported conduct disorder and sensation seeking: a 5-year longitudinal study with young adult Swiss men. Eur Addict Res. (2020) 26:233–44. doi: 10.1159/000508304
417. Estévez-Lamorte N, Foster S, Eich-Höchli D, Moggi F, Gmel G, Mohler-Kuo M. Adult attention-deficit/hyperactivity disorder, risky substance use and substance use disorders: a follow-up study among young men. Eur Arch Psychiatry Clin Neurosci. (2019) 269:667–79. doi: 10.1007/s00406-018-0958-3
418. Mitchell JT, Howard AL, Belendiuk KA, Kennedy TM, Stehli A, Swanson JM, et al. Cigarette smoking progression among young adults diagnosed with ADHD in childhood: a 16-year longitudinal study of children with and without ADHD. Nicotine Tob Res. (2019) 21:638–47. doi: 10.1093/ntr/nty045
419. Elkins IJ, Saunders GRB, Malone SM, Keyes MA, Samek DR, McGue M, et al. Increased risk of smoking in female adolescents who had childhood ADHD. Am J Psychiatry. (2018) 175:63–70. doi: 10.1176/appi.ajp.2017.17010009
420. Goldenson NI, Khoddam R, Stone MD, Leventhal AM. Associations of ADHD symptoms with smoking and alternative tobacco product use initiation during adolescence. J Pediatr Psychol. (2018) 43:613–24. doi: 10.1093/jpepsy/jsx153
421. Bowling A, Davison K, Haneuse S, Beardslee W, Miller DP. ADHD medication, dietary patterns, physical activity, and BMI in children: a longitudinal analysis of the ECLS-K study. Obesity. (2017) 25:1802–8. doi: 10.1002/oby.21949
422. de Silva VA, Jayasekera N, Hanwella R. Cannabis use among Navy personnel in Sri Lanka: a cross sectional study. BMC Res Notes. (2016) 9:174. doi: 10.1186/s13104-016-1988-4
423. Ehlers CL, Kim C, Gilder DA, Stouffer GM, Caetano R, Yehuda R. Lifetime history of traumatic events in a young adult Mexican American sample: relation to substance dependence, affective disorder, acculturation stress, and PTSD. J Psychiatr Res. (2016) 83:79–85. doi: 10.1016/j.jpsychires.2016.08.009
424. Bilevicius E, Sommer JL, Asmundson GJG, El-Gabalawy R. Associations of PTSD, chronic pain, and their comorbidity on cannabis use disorder: results from an American nationally representative study. Depress Anxiety. (2019) 36:1036–46. doi: 10.1002/da.22947
425. Alenko A, Berhanu H, Abera Tareke A, Reta W, Bariso M, Mulat E, et al. Posttraumatic stress disorder and associated factors among drivers surviving road traffic crashes in southwest Ethiopia. Neuropsychiatr Dis Treat. (2019) 15:3501–9. doi: 10.2147/NDT.S233976
426. Gentes EL, Schry AR, Hicks TA, Clancy CP, Collie CF, Kirby AC, et al. Prevalence and correlates of cannabis use in an outpatient VA posttraumatic stress disorder clinic. Psychol Addict Behav. (2016) 30:415–21. doi: 10.1037/adb0000154
427. Kevorkian S, Bonn-Miller MO, Belendiuk K, Carney DM, Roberson-Nay R, Berenz EC. Associations among trauma, posttraumatic stress disorder, cannabis use, and cannabis use disorder in a nationally representative epidemiologic sample. Psychol Addict Behav. (2015) 29:633–8. doi: 10.1037/adb0000110
428. Kim H, Lee J, Chang SM, Hong JP, Lee DW, Hahm BJ, et al. Prevalence of lifetime psychiatric disorders and suicidality in adults with subthreshold posttraumatic stress disorder: a population-based nationwide study in Korea. Psychol Trauma. (2021). doi: 10.1037/tra0001185
429. Bromet EJ, Hobbs MJ, Clouston SA, Gonzalez A, Kotov R, Luft BJ. DSM-IV post-traumatic stress disorder among World Trade Center responders 11-13 years after the disaster of 11 September 2001 (9/11). Psychol Med. (2016) 46:771–83. doi: 10.1017/S0033291715002184
430. Peltzer K, Pengpid S. Tobacco use and associated mental symptoms and health risk behaviours amongst individuals 15 years or older in South Africa. S Afr J Psychiatr. (2020) 26:1499. doi: 10.4102/sajpsychiatry.v26.i0.1499
431. Smith SM, Goldstein RB, Grant BF. The association between post-traumatic stress disorder and lifetime DSM-5 psychiatric disorders among veterans: data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). J Psychiatr Res. (2016) 82:16–22. doi: 10.1016/j.jpsychires.2016.06.022
432. Xu Y, Su S, Jiang Z, Guo S, Lu Q, Liu L, et al. Prevalence and risk factors of mental health symptoms and suicidal behavior among university students in Wuhan, China during the COVID-19 pandemic. Front Psychiatry. (2021) 12:695017. doi: 10.3389/fpsyt.2021.695017
433. Whitworth JW, Scioli ER, Keane TM, Marx BP. Physical inactivity, cigarette smoking, and psychiatric comorbidity among veterans with posttraumatic stress disorder. Health Psychol. (2022) 41:169–77. doi: 10.1037/hea0001174
434. Lee JY, Brook JS, Finch SJ, Brook DW. Trajectories of cannabis use beginning in adolescence associated with symptoms of posttraumatic stress disorder in the mid-thirties. Subst Abuse. (2018) 39:39–45. doi: 10.1080/08897077.2017.1363121
Keywords: cannabis, diet quality, sedentary behavior, tobacco, mental health, mental disorder
Citation: Johnstad PG (2024) Unhealthy behaviors associated with mental health disorders: a systematic comparative review of diet quality, sedentary behavior, and cannabis and tobacco use. Front. Public Health 11:1268339. doi: 10.3389/fpubh.2023.1268339
Received: 27 July 2023; Accepted: 14 November 2023;
Published: 05 January 2024.
Edited by:
Meryem Grabski, Frankfurt University of Applied Sciences, GermanyReviewed by:
Corine S. M. Wong, The University of Hong Kong, Hong Kong SAR, ChinaEzequiel Pinto, University of Algarve, Portugal
Copyright © 2024 Johnstad. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Petter Grahl Johnstad, cGV0dGVyLmdyYWhsLmpvaG5zdGFkQHZsZmsubm8=
 Petter Grahl Johnstad
Petter Grahl Johnstad