- 1School of Healthcare Technology, Dalian Neusoft University of Information, Dalian, China
- 2Advanced Institute for Medical Sciences, Dalian Medical University, Dalian, China
- 3Department of Thoracic Surgery, Zhongshan Hospital Affiliated to Dalian University, Dalian, China
- 4School of Information and Business Management, Dalian Neusoft University of Information, Dalian, China
The pollution posed by medical waste complicate the procedures of medical waste logistics (MWL), and the increasingly frequent occurrence of public health emergencies has magnified the risks posed by it. In this study, the authors established an index of the factors influencing the risks posed by MWL along five dimensions: the logistics business, emergency capacity, equipment, personnel, and management. The best-worst case method was used to identify the critical risk-related factors and rank them by importance. Following this, we assessed the risk posed by MWL in four major cities in China as an example and propose the corresponding measures of risk control. The results showed that the linking of business processes was the most important factor influencing the risk posed by MWL. The other critical risk-related factors included the location of the storage site, the capacity for emergency transportation, measures to manage emergencies, and the safety of packaging. Of the cities considered, Beijing was found to be a high-risk city, and its MWL needed to be improved as soon as possible in light of the relevant critical risks. Shanghai, Guangzhou, and Shenzhen were evaluated as general-risk cities, which meant that the risks of MWL were not a priority in these areas, and the other goals of urban development should be comprehensively considered during the long-term planning for MWL in these municipalities.
1 Introduction
Medical waste refers to waste containing infectious materials that is generated by institutions engaged in medical services, such as medical treatment, prevention, and healthcare (1). Past studies have shown that medical waste contains infectious pathogens, chemicals, and even radioactive substances. Medical waste contains dozens, and even hundreds, of times more germs that ordinary household garbage that can readily harm human health. For example, the WHO reported that abandoned needles cause about 1.6 million people to be infected with hepatitis B, 0.31 million people to be infected with hepatitis C and 0.03 million people to be infected with AIDS virus every year. Moreover, the packaging and containers used for medical waste contain a large amount of plastic, glass, and metal shards that are highly resistant to degradation. The long-time exposure of these materials to the environment has negative effects on the air, water, and soil. Furthermore, there are many kinds of medical waste, the methods of disposal of which are significantly different and complicated such that they require skilled professionals (2). The safe disposal of medical waste has attracted attention in research since the 1950s. The relevant theoretical work has helped refine the definition of medical waste, technologies for its disposal, and specifications of the disposal process (3). Many countries have also implemented special regulations on medical waste management and established disposal centers to ensure that medical waste is appropriately separated from domestic waste. The frequency, duration, and impact of global public health emergencies have increased in the past two decades (4). Such emergencies can cause a sharp increase in the medical waste generated in a short time, where this poses a daunting challenge to urban public health.
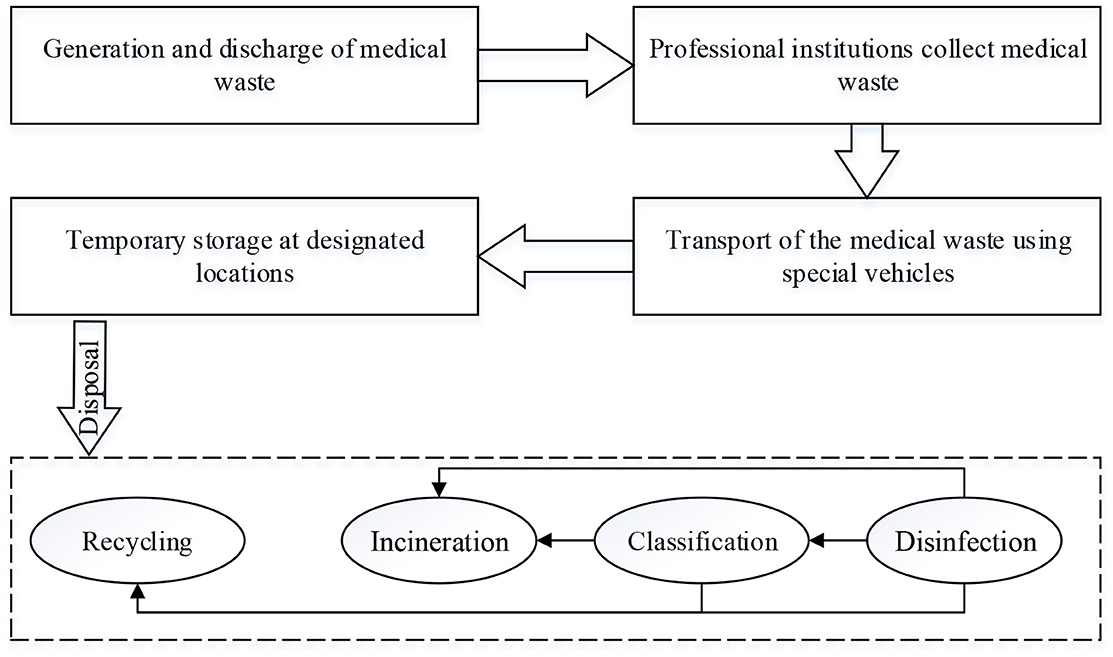
The process of disposal of medical waste is shown in Figure 1. First, the medical waste is discharged, packaged and placed in temporary storage sites. Second, the waste is transferred to special disposal centers in designated vehicles. Finally, it is subjected to high temperature incineration, steam disinfection, and chemical disinfection for disposal. The process of disposal of medical waste must be completed within 12 h. This process is thus complex, and needs to be quickly carried out. It is also likely that a large amount of newly generated medical waste cannot be disposed of in time when public health emergencies occur. Figure 1 shows the medical waste logistics (MWL) involves many participants, and accidents or disruptions in any one link of MWL can cause the entire system to collapse (5). For example, inappropriate packaging can cause contamination of vehicles, leading to the spread of pollution. An obstructed logistics network can lead to excessive inventory of medical waste. Insufficient logistics equipment will be unable to cope with the sudden increase in medical waste in public health emergencies. Therefore, managing the risk posed by MWL in case of public health emergencies is an important issue that requires further examination.
Researchers have investigated the disposal of medical waste generated in case of public health emergencies. Given the low capacity for the disposal of such waste, Xueyun studied the construction of temporary facilities and the requisitioning of domestic waste incineration centers (6). Joneghani et al. (7) analyzed the risk posed by medical waste to public safety, the urgency of its disposal, and the cost of its disinfection, and used this information to optimize the location of sites of the waste disposal network to increase its efficiency (7). Mohamed Faizal et al. (8) examined optimizing the path of the network to reduce congestion in the transportation network used to dispose of medical waste generated in case of public health emergencies. Researchers have also studied the responses to and aftercare plans in light of the risks posed by medical waste generated during public health emergencies (5). The above shows that a considerable amount of research has been conducted on the classification, collection, transportation, storage, and disposal of medical waste in case of public health emergencies, but little work has been reported on managing the risk in this case based on a systematic perspective. Because of the public benefit provided by MWL, its coordination and implementation cannot be left to the mercy of the market mechanism. This article identifies and controls key risk factors in urban MWL from the perspective of government macroeconomic regulation based on the theory of integrated supply chain management.
This study seeks to answer the following questions: how do we ensure that only a limited amount of resources can be used to control the critical risks posed by MWL by identifying them? How do we evaluate the risk of MWL in areas in which public health emergencies have occurred based on a system of risk-related factors? How do we design effective measure of risk control based on these factors? Answering these questions can help urban health management departments to reasonably integrate their resources and improve MWL, and to design mechanisms of coordination for the participants of MWL. This can in turn improve the capacity of the city's response to public health emergencies, and protect the urban environment as well as public health. We assume here that the relevant decisions need to be made under limited resources, the relevance and importance of different types of risk-related factors need to be assessed, and the available information needs to be used to evaluate the alternatives at hand. This is a typical multi-criteria decision-making (MCDM) problem. We used the best-worst method (BWM) to identify the risk-related factors. We also evaluated the risk of MWL in four first-tier cities of China.
The remainder of this paper is organized as follows: Section 2 reviews the literature on identifying, assessing, and controlling risks in MWL, and Section 3 introduces the proposed method. Section 4 considers four cities in China as an example of how to establish a system of indicators of risks posed by MWL, measure the weights of the key risk-related factors, and evaluate the overall risk. Section 6 provides a discussion of the results and the conclusions of this study.
2 Literature review
For a literature review, this study implemented four steps processes as prescribed under the qualitative content analysis method: material collection, descriptive analysis, category selection and finally, material evaluation (9). Firstly, keywords such as “medical waste,” “medical waste logistics,” “risk factor of medical waste logistics,” “factor identification,” “factor evaluation” and “risk control” were used in the Scopus (www.scopus.com), and Web of Science (WoS) databases to collect materials. Secondly, the collected materials should be analyzed by year and journal to ensure the quality of the literature. Then, the collected materials should be classified into different research categories. Finally, all necessary information should be recorded, evaluated and organized into the literature review.
2.1 The importance of MWL
In recent years, frequent public health emergencies have led to an increase of medical waste, putting enormous pressure on the waste management system (10). Medical wastes cause infectious diseases (11). According to the statistics, approximately 15 % of medical waste contains infectious, toxic, or radioactive substances (12). Improper disposal of waste generated by healthcare facilities can have a direct impact on human health and the environment (13). WHO recommends that medical waste be collected, stored, and disposed of separately from domestic and industrial wastes by accounting for its risks and threats (14). Medical waste management is actually a reverse logistics management problem. When we examine MWL practices, it is clear that MWL problems have not been solved in many developing countries yet. improper MWL procedures can aggravate the problem, leading to more severe risks to the sustainability of the environment and public health (11), such as mutagenic and carcinogenic problems, respiratory injuries, complications of the central nervous system, and reproductive system damage (15).
Therefore, research on MWL is crucial. By designing a reverse logistics network for medical waste, potential risks, including virus transmission, can be reduced. By utilizing risk control measures, the city's ability to respond to public health emergencies can be effectively improved, protecting the urban environment and human health.
2.2 Risk factors' identification and evaluation of MWL
The logistical process of the removal of medical waste includes its collection, storage, transportation, and treatment. Because medical waste may be highly spatially infectious, latent, and viral, many risks are involved in its logistics. Many scholars have studied risk-related factors in the process of MWL. Makajic-Nikolic et al. (16) studied the risks associated with the probability of generation of medical waste during diagnosis and treatment as well as during its transportation (internal and external) (16). Tushar et al. (2) studied the risks posed by medical waste from four perspectives: operation, technology, government, and management (2). Tang et al. (17) used the characteristics of transportation of medical waste combined with past research to propose 16 risk-related factors, including poor safety awareness among employees, incorrect operation by them, improper disinfection of transportation tools, unsafe transportation tools, and unreasonable storage locations. However, they did not classify these risk-related factors. Niyongabo et al. (18) studied risk-related factors involved in the generation and storage of medical waste in 12 healthcare facilities in Bujumbura, Burundi, and concluded that the risk posed by the storage process was the highest (18). The application of advanced technologies to MWL has also gradually been attended to in research. Celik et al. (19) claimed that the failure to use such new technologies as big data, the blockchain, and novel and reliable software will introduce risks to the process of MWL (19). The above literature shows that not many studies have been devoted to investigating and classifying the risk-related factors of MWL, where this can help control and reduce risks.
Identifying and evaluating risk-related factors in MWL is the key to managing the risk, and is important for improving medical waste management. Many scholars have studied risk identification and evaluation (16, 17, 19), but few have specifically focused on MWL. And the identification and evaluation of risk is a typical MCDM problem. The technology for multi-standard analysis can help decision-makers evaluate and control risks (20). Karuppiah et al. (21) used MCDM to establish a Framework for improving supply chain sustainability (21). Many scholars have used MCDM to examine the problem of risk management in different fields. Koohathongsumrit et al. (22) integrated the fuzzy risk assessment model (FRAM) and the best–worst method (BWM) to select the best transportation route in a multi-modal supply chain (22). Aydin et al. (23) proposed a framework for risk assessment based on the failure mode and effect analysis (FMEA), the best–worst method (BWM), and image fuzzy multi-attribute boundary approximation area comparison (PF-MABAC) to prioritize the risks of fires and explosions in the oil and gas industry (23). Celik et al. (24) combined the BWM and MARCOS to identify and analyze risks to the safety of dams (24), Zheng et al. (25) used the G-DEMATEL-AHP to study the risk of urban flooding (25), and Ghorui et al. (26) used the HFS and TOPSIS to identify major risk-related factors involved in the transmission of COVID-19 (26). The MCDM method has also been widely used in research on medical waste management, particularly in studies on techniques of management, and methods and sites of disposal (27–29).
The above shows that a diversity of methods to identify and assess risks have been developed. MCDM is a classic method of risk identification and assessment, and the BWM has been applied to manufacturing, transportation, and supply chain management (30–33). It is frequently used to derive the weights of the decision-related criteria in MCDM problems. Therefore, BWM is suitable for use in research on the risk management of MWL.
2.3 Research on risk control of MWL
With increasing public awareness of the impact of green development, disposing of medical waste in a safe and environmentally friendly manner has become a popular subject of research in recent years (19). Medical waste mainly affects healthcare workers, patients and their companions, cleaning personnel, and personnel engaged in the transportation and disposal of medical waste. It can also affect the environment, soil, water, and air. Therefore, managing and controlling the risks posed by it have attracted worldwide academic attention. Some researchers have designed logistics networks that can select the location of storage and treatment sites, and have planned and designed transportation routes to reduce the risks posed by MWL (34–37). The facilities and equipment used for MWL are crucial. Many studies have pointed out that the safety of the packaging and transportation of medical waste are key factors influencing its leakage (17). The operator is also important in MWL. Any non-compliance incurs unexpected risks. Some scholars have studied risk management in MWL from the perspective of the operators. For example, Makajic-Nikolic et al. (16) examined the risks caused by operators and their probability of occurrence, and concluded that better training of the personnel engaged in MWL and improving their awareness of safety can reduce risks (16). Moreover, the role of managers in MWL cannot be ignored (2). Some scholars have also studied the risk management of MWL in the context of public health emergencies in recent years. Chen et al. (38) used Wuhan, China as an example to study the management and control of the risks posed by the generation, transportation, and treatment of medical waste in emergencies, and their results showed that the emergency capacity needs to be improved (38). Liu et al. (39) claimed that the explosive growth in the volume of medical waste leads to risks due to limitations on the disposal facilities of hospitals when medical institutions respond to public health emergencies. It is thus crucial to design a reverse supply chain network of medical waste (39). Celik et al. (19) aimed to determine the hospital in Erzurum that carries out medical waste management the most effectively and efficiently by IFMCDM methods. Shanshan (40) summarized and analyzed methods of managing the risk of medical waste in China to reduce the risks posed by logistics (40). Nimita Jebaranjitham et al. (41) studied the impact of governmental policies on managing the risk of MWL, and concluded that Asian countries need to allocate more funds for the treatment of medical waste (41).
To sum-up, the process of risk control of MWL mainly involves the design of the reverse logistics network, management of the logistics operator and the equipment, formulation and supervision of a management system, and risk management in case of public health emergencies. Management based on the above perspectives can help control the risks posed by MWL.
2.4 Prototype decision-making structure
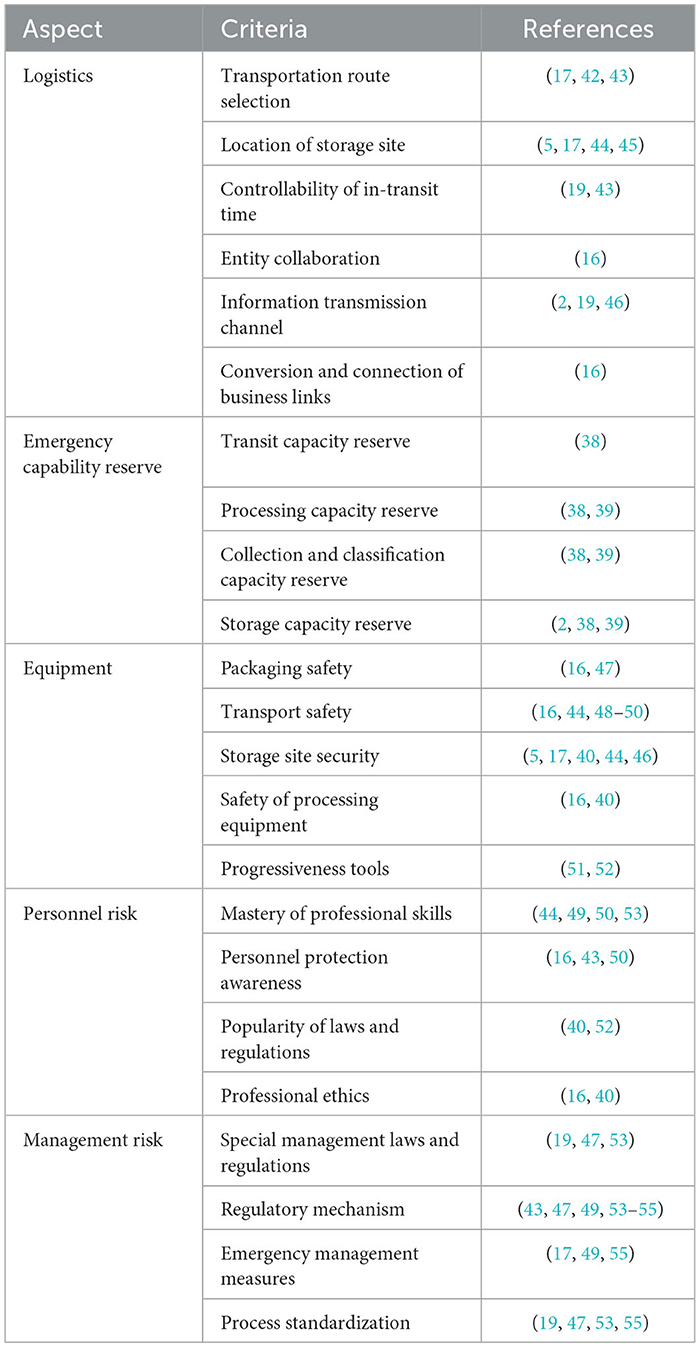
We chose and integrated the risk-related factors involved in MWL based on the above literature review and classified them into different aspects. We then eliminated factors that had the same meaning. We thus developed a prototype of a decision-making structure consisting of five aspects: (i) logistics, (ii) reserve for emergency capability, (iii) equipment, (iv) personnel-related risk, and (v) management-related risk. A detailed description of each category is provided in Table 1.
3 Methodology
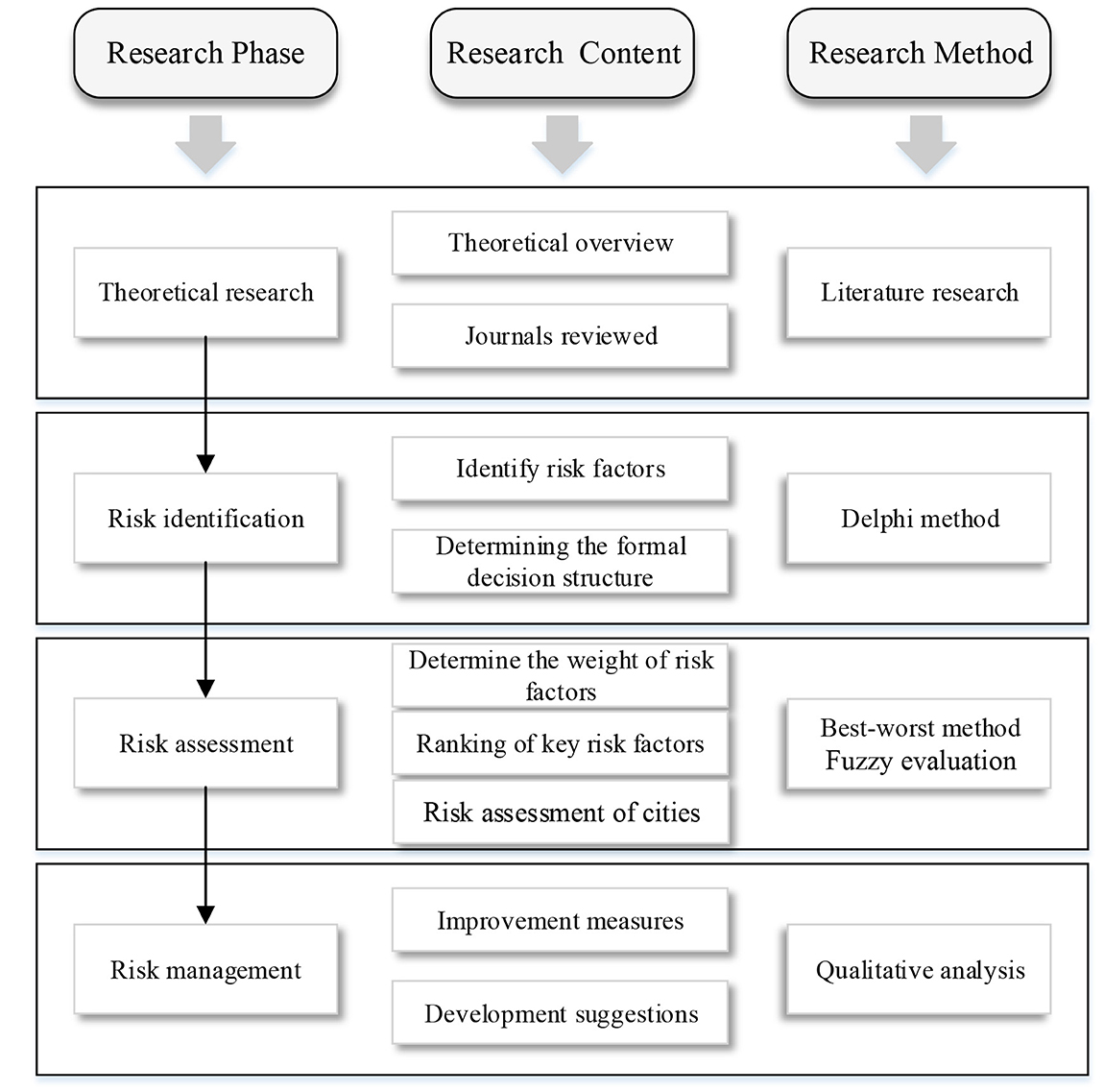
Based on theoretical research, expand according to the logic of risk identification, risk assessment, and risk management. In Risk identification, the Delphi method is used to obtain the formal decision structure. In Risk assessment, BWM is used to calculate the weights of each criterion, and key factors are determined by ranking them based on the weights. Then, a Fuzzy evaluation was used to evaluate the performance of the four cities and obtain the final results. In risk management, based on the research results, propose management suggestions and directions. The description of the methodological framework is shown in Figure 2.
3.1 Prototype decision-making structure
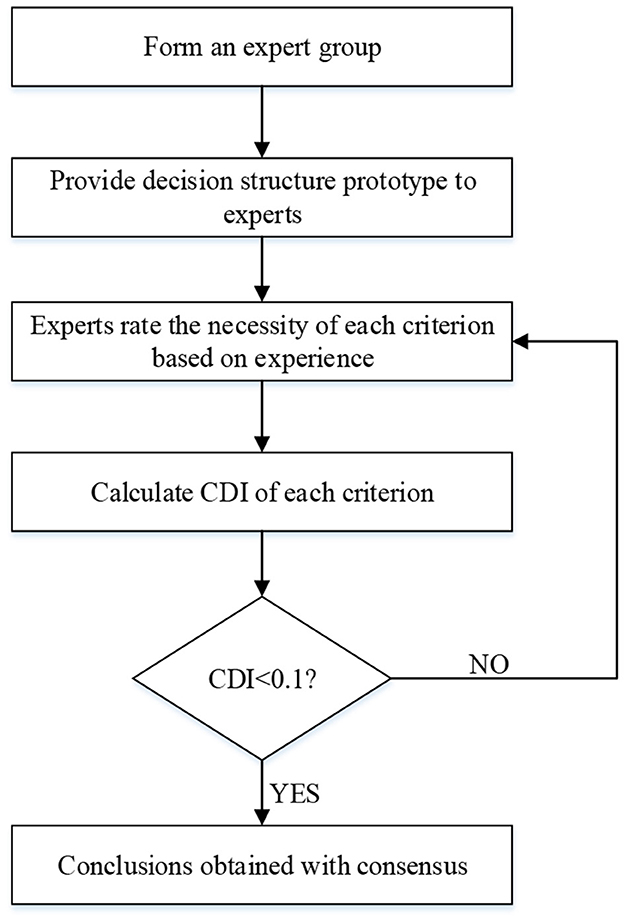
The Delphi technique was proposed by the RAND Corporation (56). Also known as the expert opinion method, it uses back-to-back communication to solicit the predictive opinions of members of an expert group. It is a management technology used to deal with problems involving complex tasks. We use the consensus deviation index (CDI), namely, the mean divided by the variance, to determine consensus in this study.
Step One. Each expert was invited to fill in an open questionnaire according to the prototype decision-making structure above. The experts judged whether the criteria in the decision-making structure were suitable for medical waste logistics, and checked whether the definitions of the criteria were clear based on their knowledge and experience.
Step Two. The experts rated the criteria on a scale of 0–10. The scale indicates the degree of necessity, where a score of “0” indicates that the corresponding factor is absolutely unnecessary and a score of “10” indicates that it is absolutely necessary. We used the CDI to calculate the degree of consensus of the expert group (57).
Step Three. The average values and standard deviations of the scores assigned by all experts to each criterion were calculated. Experts who assigned scores higher than the average ± one standard deviation were asked to explain their reasoning for their scoring before they were allowed to assign new scores.
If the experts disagreed with one another after the second step, a third step was conducted, and so on until they had reached a consensus. The threshold of the CDI is 0.1. A value higher than 0.1 indicates significant differences in the opinions of experts, and means that further steps of scoring are needed until all the CDI values are lower than 0.1 (58). The procedures involved in the Delphi method are shown in Figure 3.
3.2 Best-worst method
The best-worst method (BWM) is an MCDM method developed by Rezaei (59). It can obtain consistent results by using a small amount of information. The BWM has been used to solve many MCDM problems in business, economy, engineering, education, and agriculture, and can be used to determine the weights of factors and select alternatives. Its main steps are as follows:
Step 1: Determine a set of decision criteria.
The decision-maker considers the criteria {c1, c2, c3...cn} that should be used to arrive at a decision.
Step 2: Determine the best (e.g., the most important) and the worst (e.g., the least important) criteria.
The decision-maker identifies the best and the worst criteria. No comparisons are made at this stage.
Step 3: Determine the preference of the best criterion over all the other criteria, and represent it by using a number from 1 to 9. The resulting best-to-others (BO) vector is:
where aBj indicates the preference of the best criterion B over criterion j. It is clear that aBB = 1.
Step 4: Determine the preference of all the criteria over the worst criterion and represent it by using a number from 1 to 9. The resulting others-to-worst (OW) vector is:
where ajW indicates the preference of criterion j over the worst criterion W. It is clear that aWW = 1.
Step 5: Calculate the optimal relative weights .
The aim is to determine the optimal weights of the criteria such that the maximum absolute differences and for all j are minimized. This can translate into the following min–max model:
According to literature (60), we minimize the maximum value in the set {|wB − aBjwj|, |wj − ajwww|}, instead of minimizing the maximum value in .
Model (1) can be transferred into the following linear programming model (2) :
In this model, ξL can be directly considered to be indicator of the consistency of comparisons (we do not use the consistency index here). Values of ξL close to zero reflect a high level of consistency.
Step 6: Find the composite weights .
Once the relative weights of the indicators have been determined, the calculation of the composite weight of the corresponding criterion is simple:
Wi refers to the composite weight of criterion i and wi is its relative weight. Nj refers to the weight of criterion i relative to the corresponding aspect j.
3.3 Fuzzy evaluation
The fuzzy evaluation method is a comprehensive method of assessment based on fuzzy mathematics (61). It transforms qualitative evaluation into quantitative evaluation based on the membership theory in fuzzy mathematics. It provides clear results, is highly systematic, can be used to solve fuzzy and difficult-to-quantify problems (62), and is thus suitable for a variety of problems involving uncertainty. We use fuzzy vagueness here. The procedure of this method is as follows:
Step 1: Determine the set of factors and their weights.
We construct a set of risk-related factors and calculate their weights. The set can be expressed as:
Step 2: Determine the set of comments.
We use the literature on the transportation and storage of medical waste to classify the risks posed by it. The comment set V is thus formed:
Step 3: Construct a matrix of comprehensive evaluation.
We used questionnaires for each risk-related factor according to the comment set, collected the responses, and processed them to form a matrix of comprehensive evaluation R:
where rnm represents the result of evaluation of factor n based on comment m.
Step 4: Perform matrix synthesis to obtain the comprehensive set of fuzzy evaluations.
The weighted average operator is a method for performing the synthesis operation. Qian and Xueping (63) used it on seven commonly used synthesis operators (63). We combine the matrix of weights Z and the matrix of comprehensive evaluation R according to the weighted average operator to obtain the comprehensive set of fuzzy evaluations B:
Step 5: Normalize the comprehensive set of fuzzy evaluations.
B is normalized. If B = (b1, b2, ⋯bn), then
Step 6: Perform comprehensive evaluation.
We use the principle of the maximum degree of membership, and choose the corresponding grade vj of the largest in the fuzzy set of comprehensive evaluation as the result.
4 Empirical study
4.1 Problem statement
Global public health emergencies have begun emerging more frequently in recent years (64). As major cities in China and hubs of international commerce, Beijing, Shanghai, Guangzhou, and Shenzhen have large populations and rich medical resources at all levels, and thus generate large amounts of daily medical waste that requires quick and efficient treatment (65). However, the current number of medical waste disposal enterprises in first-tier cities is small, and all aspects of reverse logistics are not optimal. The management and disposal of MWL in the face of public health emergencies is complex, and needs to be comprehensively improved. We used Beijing, Shanghai, Guangzhou, and Shenzhen as examples in this paper, and examined their capacities for the reverse logistics of medical waste in terms of risk identification, evaluation, and management in case of public health emergencies. The aim is to help government departments in making the correct decisions, protecting people's lives and health, and thus ensuring the healthy development of the urban economy.
4.2 Determining the formal decision structure
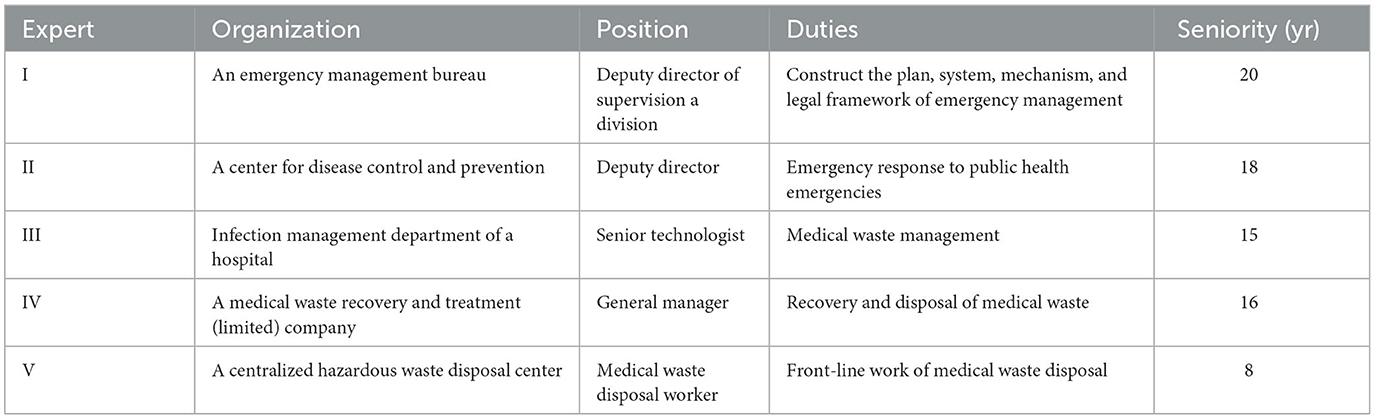
As is shown in Table 2, we used five experts with rich experience as well as a strong theoretical background in medical waste management, reverse logistics, and emergency management for this case study.
The preliminary decision structure obtained from the literature review (Table 1) was distributed to the expert group in the first step and their opinions were sought. They were asked to opine whether the classification of each criterion was appropriate and its definition clear.
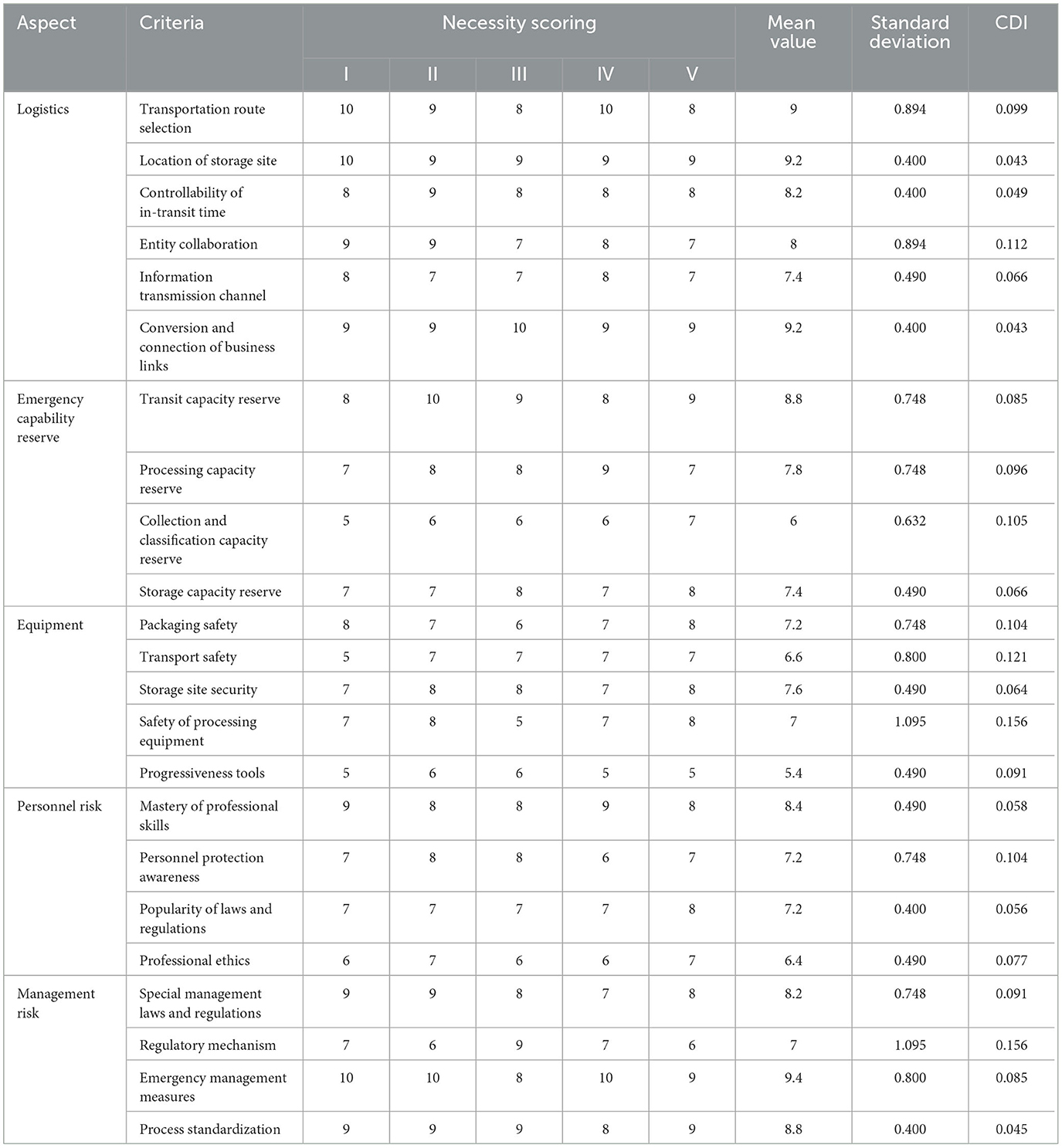
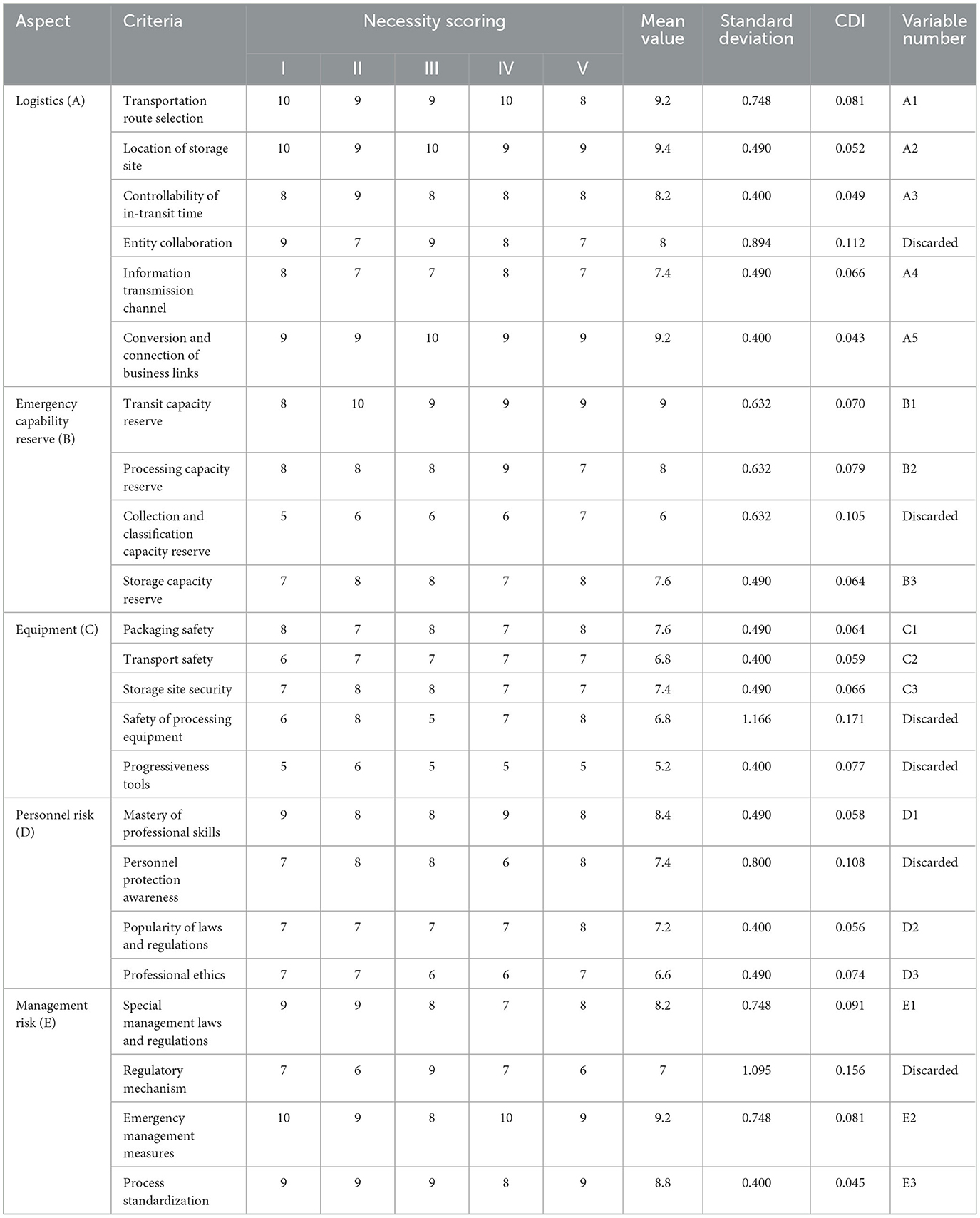
The experts were asked to rate the necessity of each criterion by assigning it a score from 1 to 10 in the second step. The higher the score of a criterion was, the greater was its necessity/importance. The mean value, variance, and CDI of each criterion were calculated, and the results are shown in Table 3. The CDI values of some standards was >0.1, which means that the expert group had not reached a consensus regarding them and a third step was required.
The mean value, variance, and CDI of each criterion calculated in the second step were fed back in the third step to the experts, who were asked to explain their scoring of items that exhibited large deviations. After the third step of scoring, the CDI value of each criterion was lower than 0.1, which means that the expert group had reached an agreement regarding all items. In further discussion, the expert group claimed some indicators had a relatively limited impact on the object of research, and thus that indicators with average values smaller than 6 should be discarded. The formal decision-making structure is shown in Table 4.
4.3 Identifying key risk-related factors
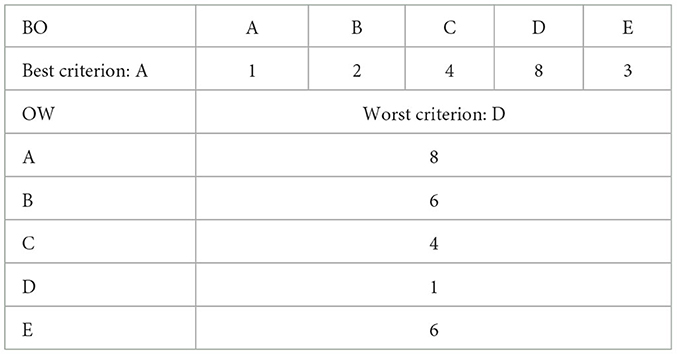
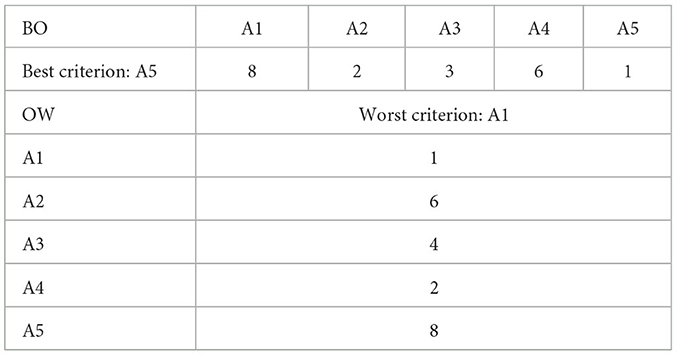
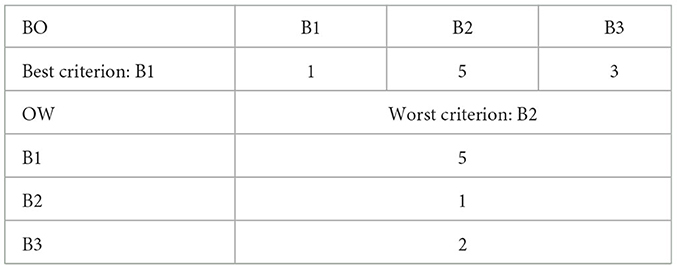
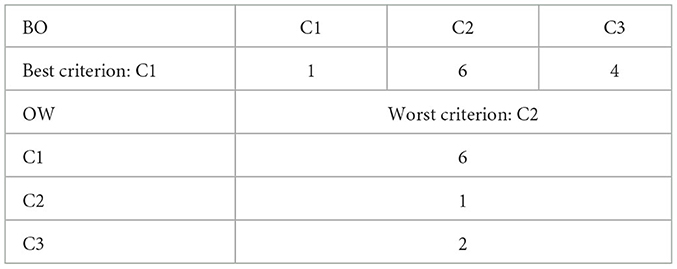
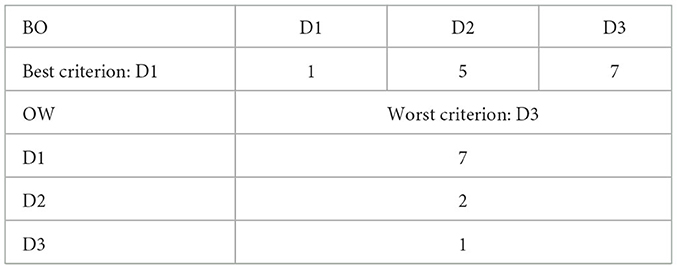
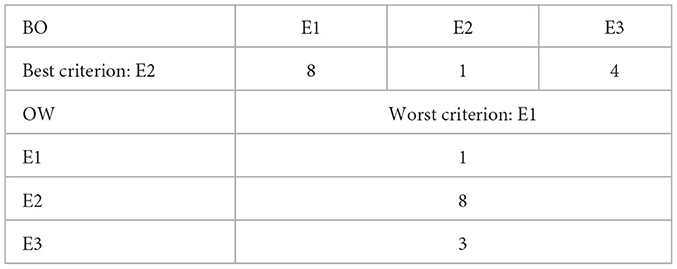
To identify the key factors influencing MWL and determine the importance of each, we asked the five experts to calculate the absolute weight of each criterion according to the BWM methodology. As an example, we give the procedure used by expert I to perform the above task.
First, expert I selected the most and least important of five aspects—logistics (A), emergency reserve capacity (B) , equipment (C) , personnel-related risk, (D) and management-related risk (E), and assigned scores to them on a scale of 1–9. The results are shown in Table 5.
Second, expert I selected the most and least important indicators for each of the above five factors. They chose five influential factors, A1, A2, A3, A4, and A5, at the second level for logistics (A), three factors, B1, B2 and B3, for the emergency reserve capacity (B), three influential factors, C1, C2, and C3, for equipment (C), three factors, D1, D2, and D3, for personnel-related risk (D), and three influential factors, E1, E2, and E3, for management-related risk (E), and scored them on a scale of 1–9. The results are shown in Tables 6–10.
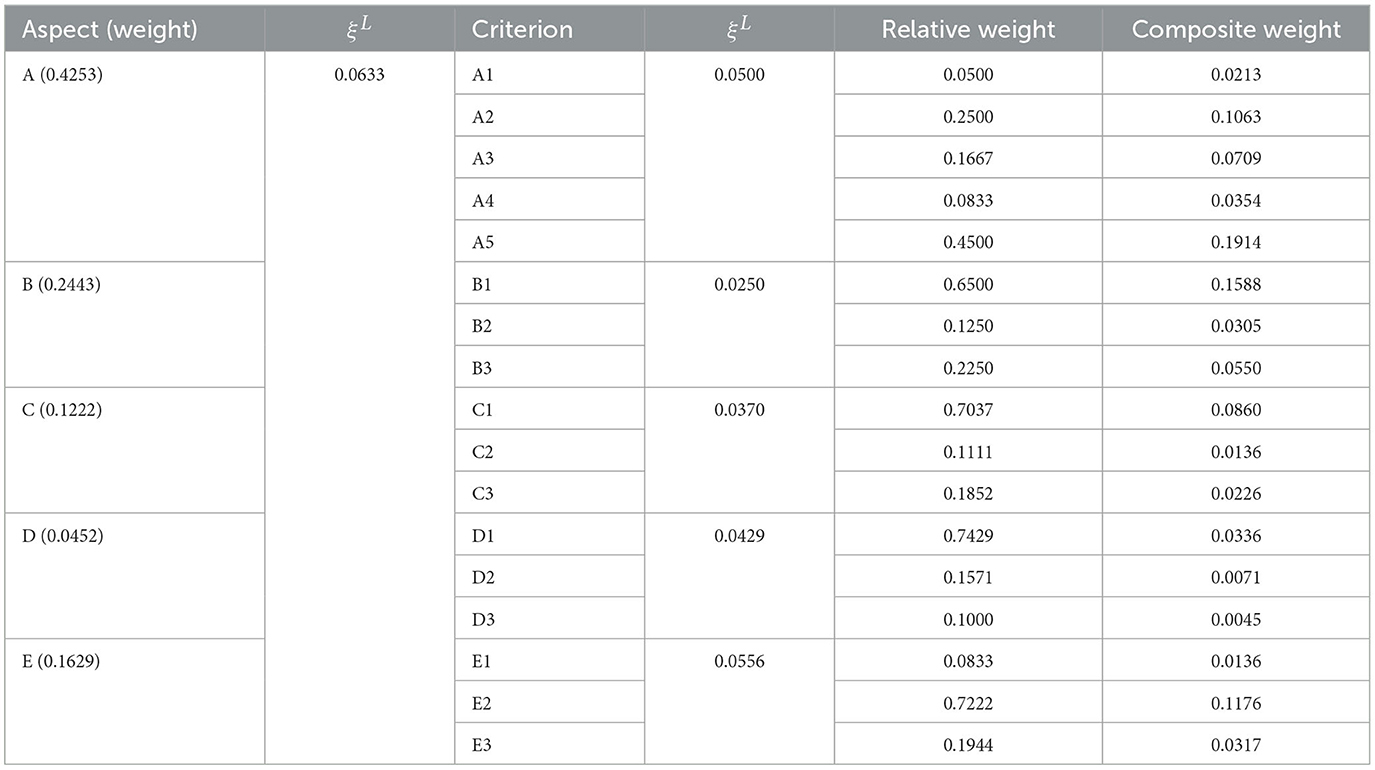
Finally, the expert used a programming solution in Excel to calculate the relative weights and target values of the above. The closer the target value was to zero, the higher was the consistency among the factors. Their absolute weight is shown in Table 11.
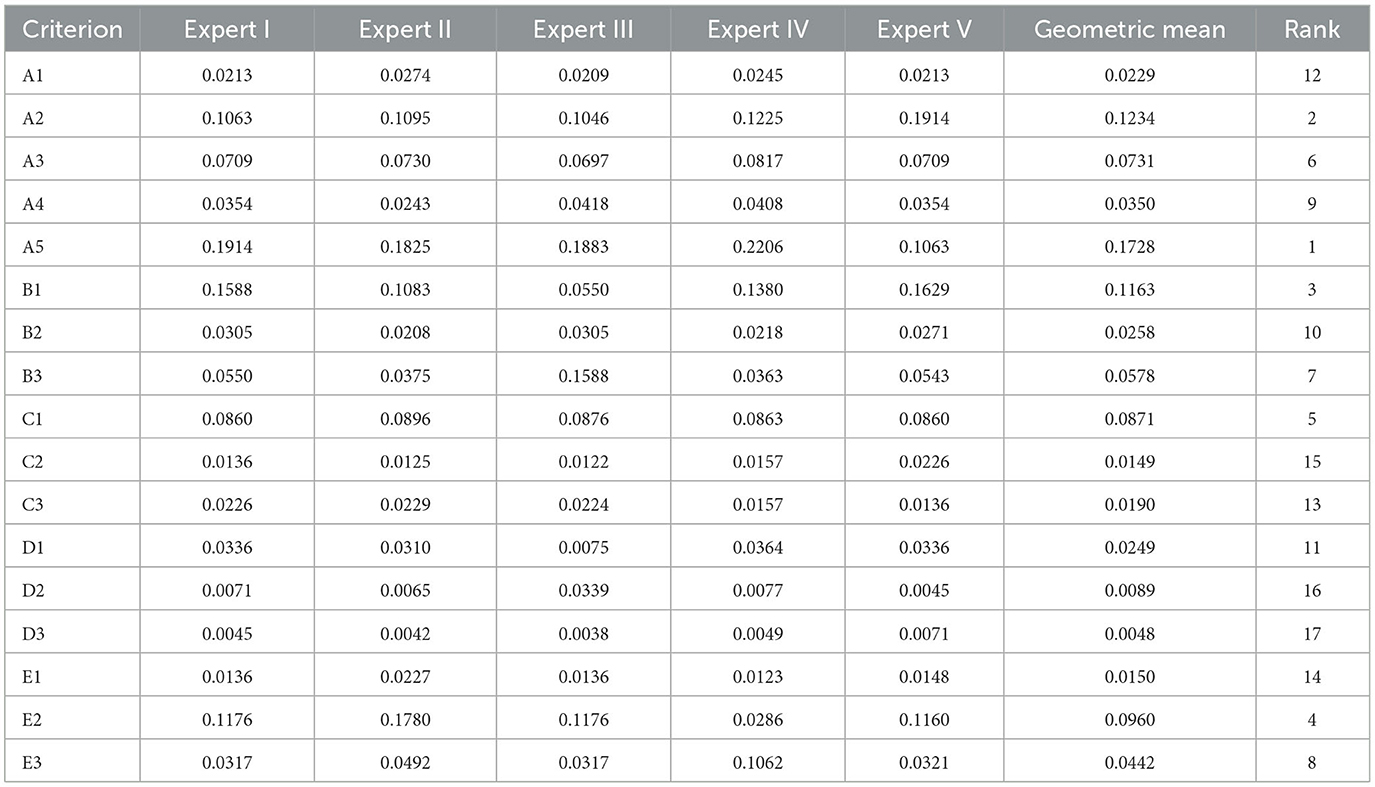
The results of scores assigned by experts II, III, IV, and V were collected and calculated by using the same steps as above (see Appendix A), and the final weights were obtained by using the geometric mean as shown in Table 12.
Table 12 lists the weights of the criteria according to the index to assess medical waste logistics. For example, the weight of A1 was 0.0229. We ranked all the criteria in descending order of weight to obtain their importance. The results showed that the first eight items were critical factors: A5, A2, B1, E2, C1, A3, B3, and E3.
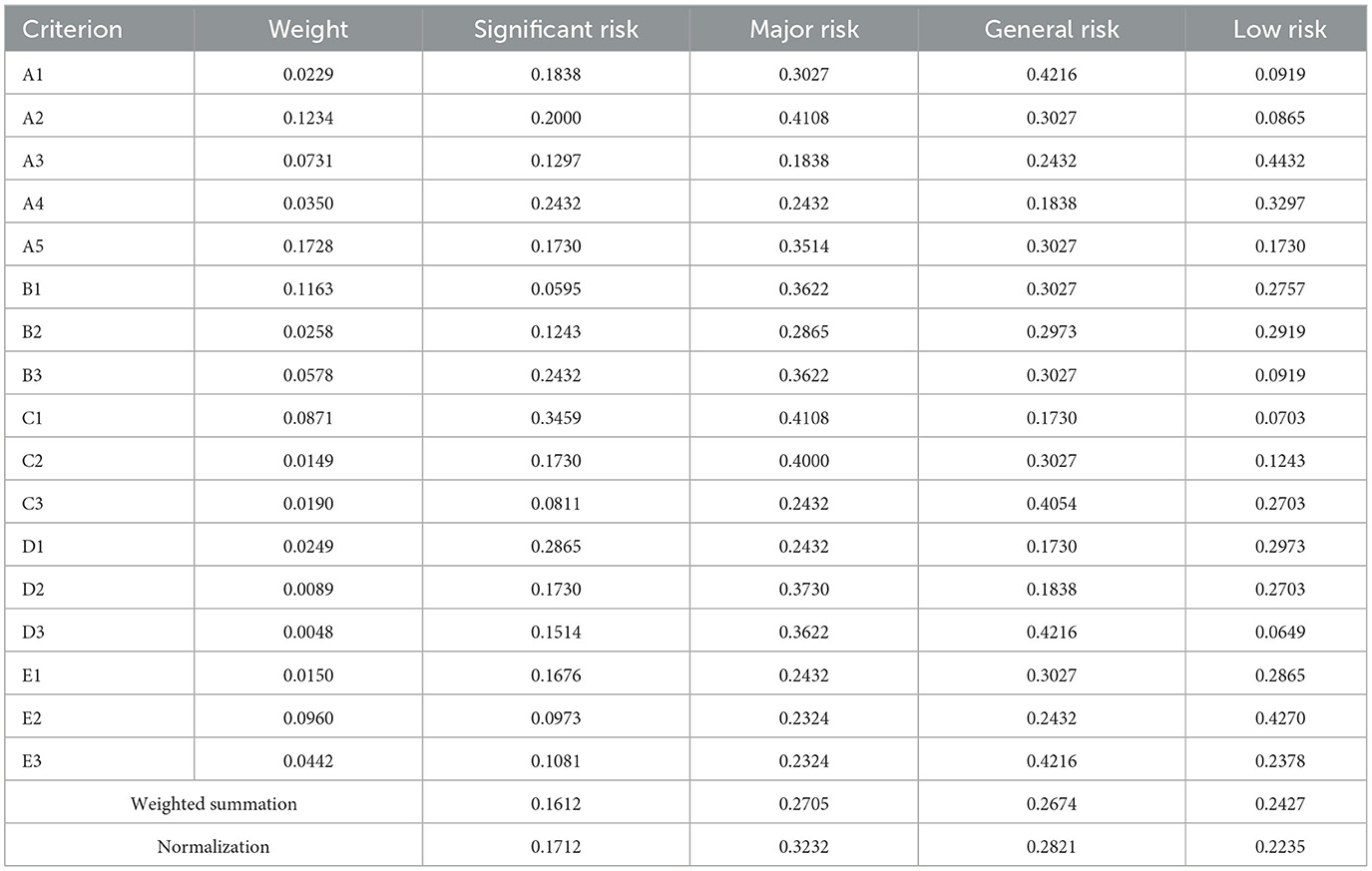
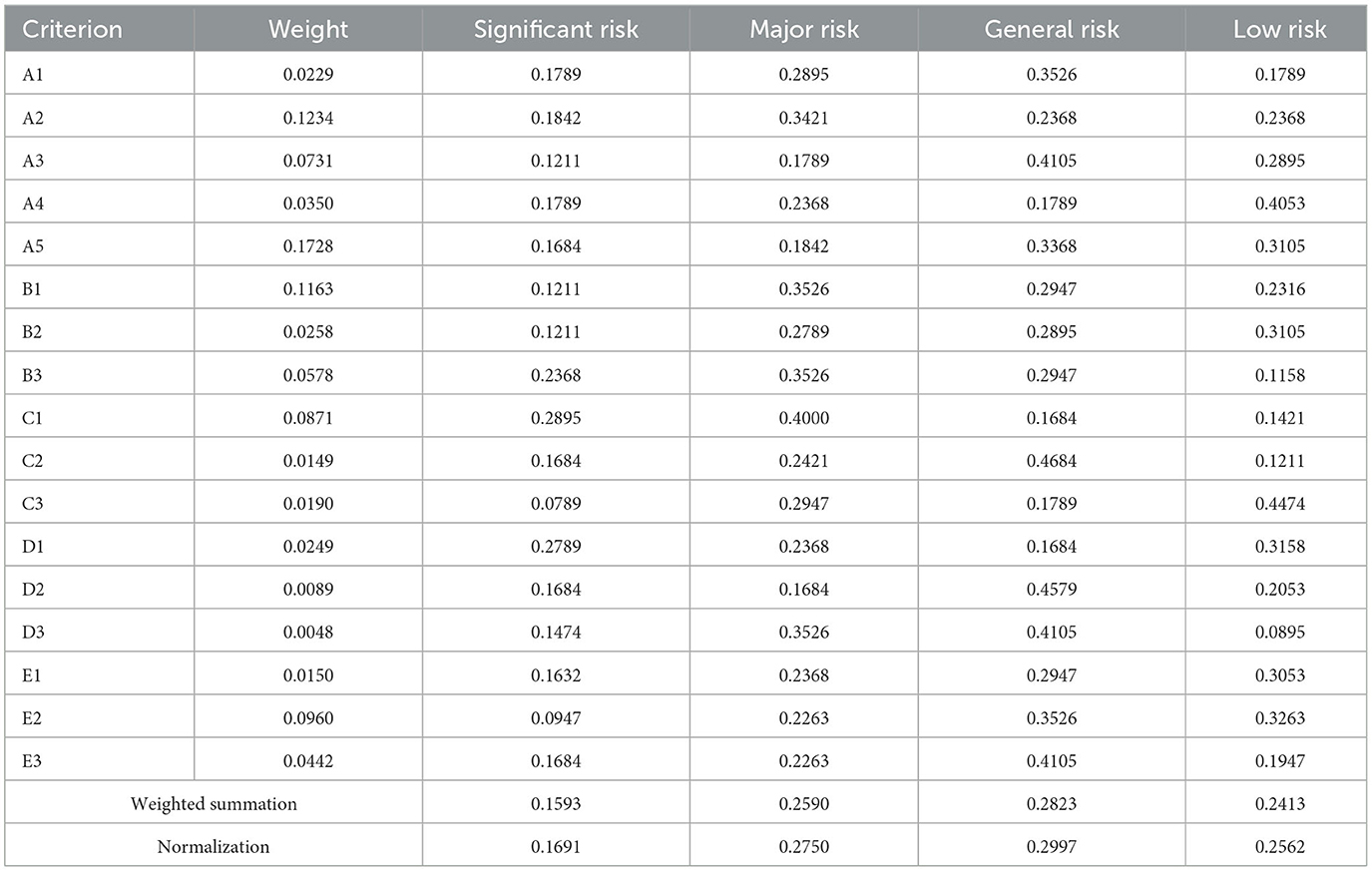
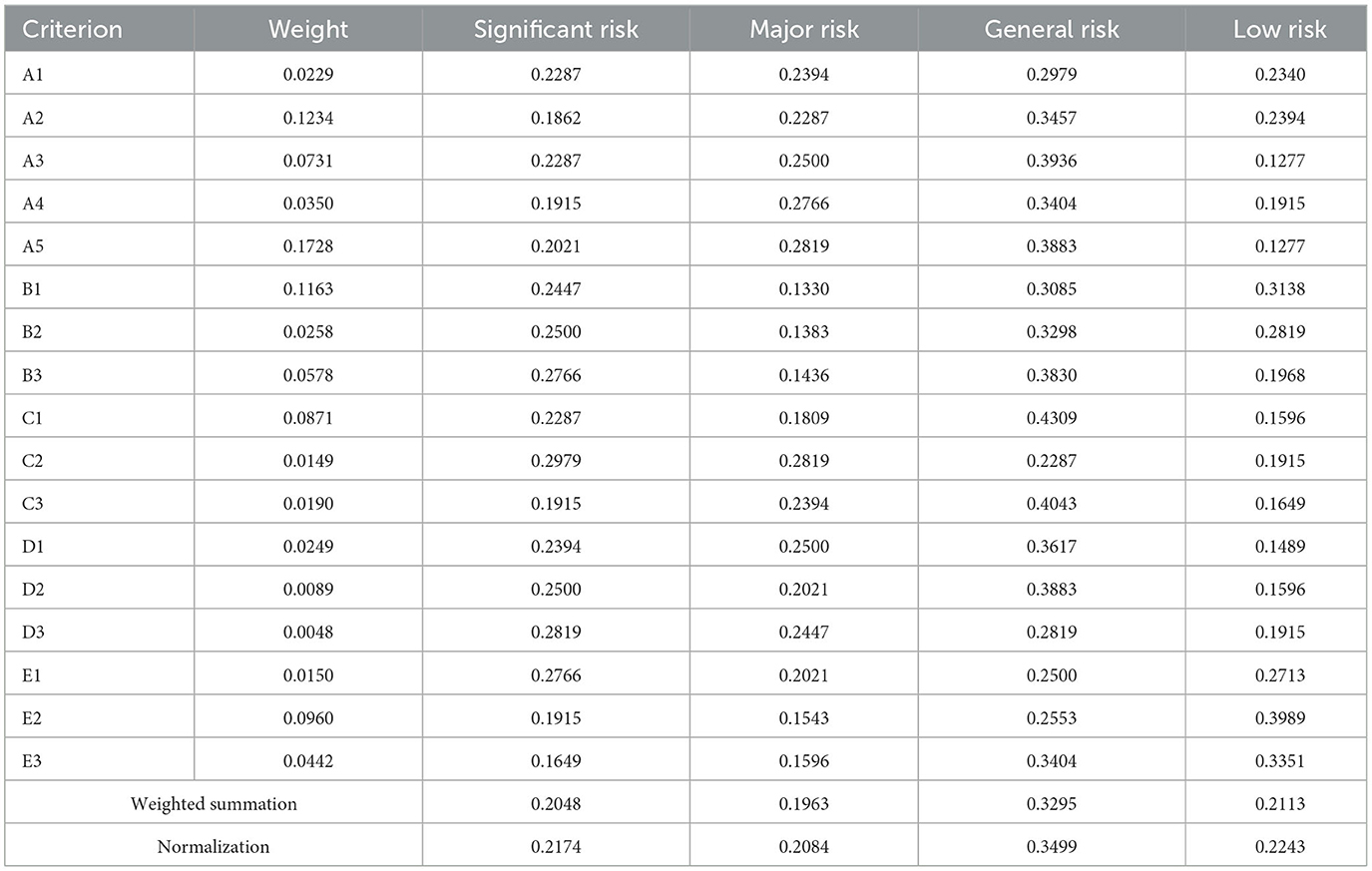
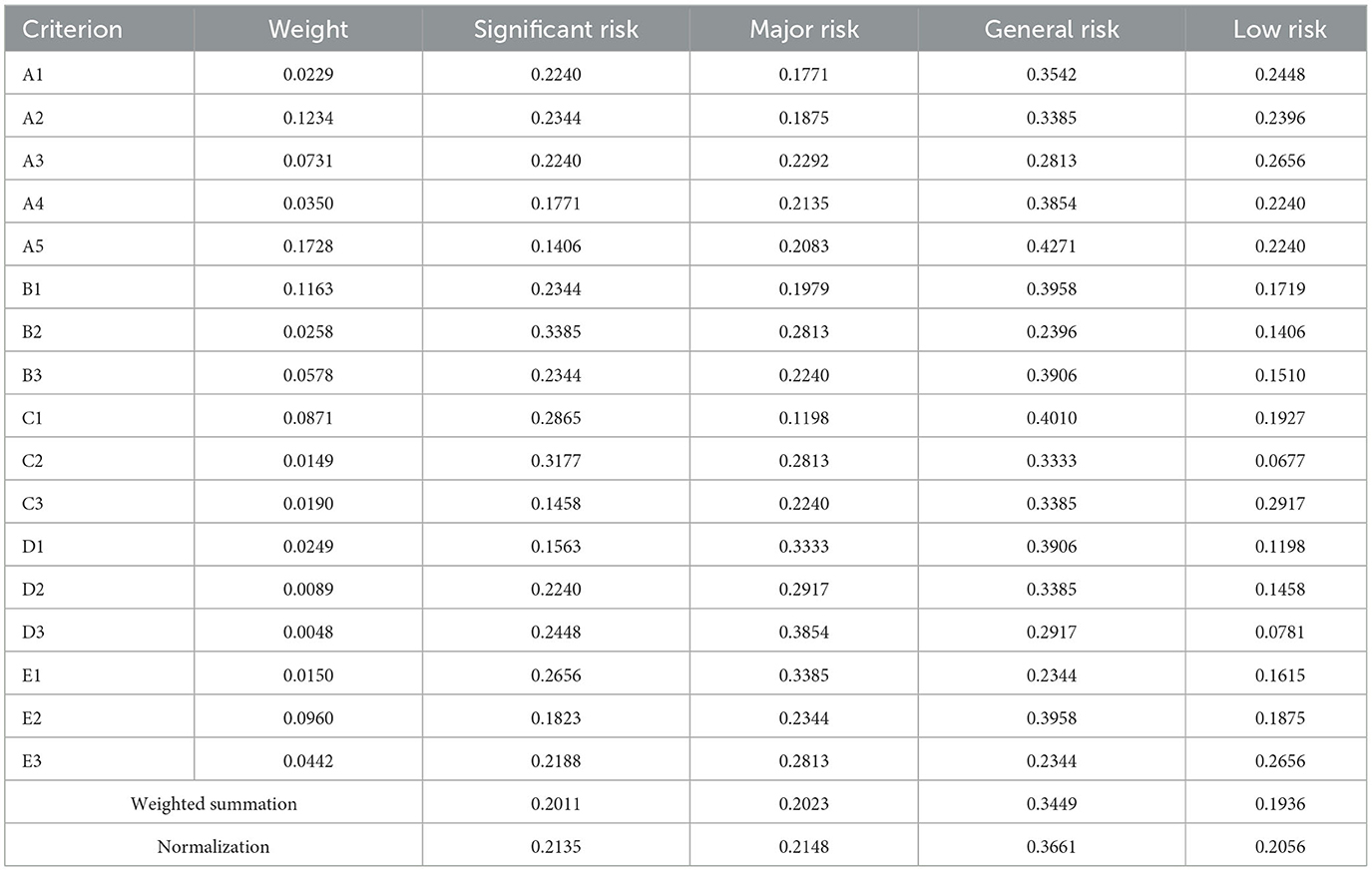
4.4 Assessing the risk to cities
The level of risk of reverse logistics is generally divided into four levels in the literature: significant risk, major risk, general risk, and low risk (59). We distributed 200 questionnaires to stakeholders in MWL in Beijing, Shanghai, Guangzhou, and Shenzhen to investigate this issue further. We collected 185 valid responses from Beijing, 190 from Shanghai, 188 from Guangzhou, and 192 from Shenzhen. We divided the total number of distributed questionnaires by the number of valid questionnaires for statistical processing. For example, Table 13 shows that of the 185 valid respondents from Beijing, 34 claimed that the choice of the transportation route (A1) posed a significant risk to MWL, 56 claimed that it posed a major risk, 78 chose it as a general risk, and 17 determined that it incurred only a low risk. We then divided 34, 56, 78, and 17 by 185 to obtain 0.1838, 0.3027, 0.4216, and 0.0919. This questionnaire was thus convenient and practical, and could adequately reflect the opinions of the respondents. We performed a weighted summation of the results of all questionnaires from all four cities to obtain the final results, and then normalized them as shown in Tables 14–16.
The results in the above tables show that MWL posed a major risk in Beijing and a general risk in Shanghai, Guangzhou, and Shenzhen. Both general and low levels of risks are generally considered acceptable while significant and major levels of risk are deemed unacceptable.
5 Discussion and conclusions
5.1 Discussion
We identified the risks of MWL in case of public health emergencies and ranked the risk-related factors according to their importance in this study. The results showed that linking business processes is the most critical risk in the above context. Previous studies have claimed that the most critical risk posed by MWL lies in transportation and storage (5). The results of this study are different from this. According to historical data on accidents involving medical waste in Beijing in recent years, 40% of them occurred during business handover while only < 10% occurred during transportation and storage. The results of our study differ from those of past work because the latter was based on older data. The technological capabilities and skills of management of enterprises involved in MWL have improved with awareness of it. However, the participants of MWL include hospitals, transportation companies, disposal institutions, and other organizations. Some of them are public institutions and others are profit-making enterprises. Their operational objectives are thus different such that they are usually responsible only for achieving their own goals, and have little incentive to cooperate with one another. The handing and taking over of activities in the process may also involve personnel who are not adept at the task.
The location of storage sites is related to efficiency and security in the MWL network. While many studies have investigated site selection (45), a number of factors need to be considered in this vein. When the constraints of time, cost, and service satisfaction cannot be simultaneously met, the importance-based ranking of the risk-related factors can help arrive at a satisfactory solution. The capacity for emergency transportation is also an important risk-related factor. Zhihao et al. (66) recognized its important role (66) but did not consider it to be a key risk. Our survey here showed that the frequency of transportation increases significantly in case of public health emergencies, and the path of transportation of waste changes often based on the available equipment, temporary storage sites, and disposal locations. Flexibility in the capacity for emergency transportation is thus necessary. It plays a critical in the stability of MWL as a bridge among collection, storage, and disposal.
Due to advances in packaging technology, some researchers have claimed that the safety of packaging equipment is no longer a key risk (6). We disagree. There is great deal of uncertainty in the type and quantity of medical waste that is generated when public health emergencies arise. Different types of medical waste require different packaging, and this may lead to a mismatch between the available packaging and the medical waste that needs to be sealed. In addition, the packaging operation usually occurs at the source of waste discharge, but the workers at these facilities are usually not skilled in packaging operations. This is one reason for why packaging remains a risk in MWL.
Our work here has shown that management-related and personnel-related risks are not key in MWL. While management and personnel training are important for daily MWL, their roles are not significant when public health emergencies are considered. This is because establishing the standards of management and personnel training requires a certain lead time, that is, emergency drills are more important than temporary responses.
5.2 Risk control measures
According to the importance of the risk-related factors calculated above, we propose the following measures to control the risk posed by MWL:
(1) The linking of the relevant business processes must be prioritized because the risk posed by it directly affects the basic operation of MWL, and public health emergencies can amplify its impacts. The government should help the participants in the MWL process to cooperate by integrating the supply chain. First, the government should specify the division of responsibilities of each participant to MWL and set the standards of operation for them. Second, it is necessary to help build information-sharing platforms for them. When a public health emergency occurs, all participants of MWL should communicate with one another about the problems encountered, share the risks, and jointly propose solutions.
(2) The risk posed by the location of waste storage sites can be mitigated through coordination between the government and the relevant private enterprises. It is difficult for enterprises to resolve the conflict between cost and efficiency without the support of the government. In addition, the government needs to plan for temporary locations for storage sites in advance, and to conduct regular mock tests of the overall operation to prepare for public health emergencies.
(3) The government needs to plan for its capacity for emergency transportation in advance, and to encourage enterprises to transform non-specialized medical waste equipment and train an appropriate number of personnel to account for emergencies based on subsidies and other incentives. This can help ensure that the requisite resources can be quickly mobilized in case of public health emergencies.
(4) The risk posed by the safety of packaging should also be considered. Transportation enterprises need to acquire the relevant knowledge on medical waste while hospitals need to learn the appropriate packaging and classification of medical waste. In addition, the government needs to support scientific research institutions in developing safer packaging to help hospitals conveniently deal with medical waste.
(5) Personnel need to be trained in emergency preparedness and a plan for emergency management needs to be formulated in advance. A scientific warning mechanism can also buy more preparation time for the relevant departments in case of public health emergencies.
5.3 Conclusions
This article considers the impact of public health emergencies on MWL and researches risk identification and control of MWL from the perspective of systemic coordination. This article combines multiple disciplines, such as environmental science, public health, and logistics management, to provide practical cases for interdisciplinary research. By analyzing and controlling the risks in the logistics process of medical waste, the development of risk management theory can be promoted, especially in high-risk and highly sensitive fields. This article helps to improve relevant policies and regulations, providing a scientific basis for policymakers.
We used the BWM to obtain the weights and ranked importance of risk-related factors in MWL and found that linking the relevant business processes, location of storage sites, capacity for emergency transportation, emergency management measures, and safety of packaging are the key risk-related factors in MWL. The used four first-tier cities in China as examples, and assessed the risk posed to them by MWL. Their final ranking in terms of risk was Beijing > Shanghai > Guangzhou > Shenzhen. Such results are useful for the construction of MWL. Effective risk control measures include integrating supply chain management, emergency training for personnel, training in waste packaging, and an early warning mechanism for public health emergencies.
The disposal standards and processes about medical waste vary in different countries, so the risks posed by MWL are also different. The prototype for decision making structure in this paper sorted and classified the risks posed by MWL in public health emergencies, and it was of high universality. By expanding the number of experts to clarify the selection criteria, the formal decision-making structure can be better matched with the regional characteristics of the evaluation object. In addition, this paper took Beijing as an example and proposed risk control measures for key risks. However, in practice, further consideration needs to be given to the implementation costs of the measures, while also taking into account the coordination effect between different measures. In addition, early risk control is also a future research direction. By combining key risk factors with data analysis techniques to design an MWL risk warning model and developing response strategies based on different risk scenarios, the resilience of MWL in major health and safety incidents can be further enhanced.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
XW: Conceptualization, Writing – original draft. LL: Data curation, Writing – review & editing. LW: Data curation, Writing – original draft, Writing – review & editing. WC: Resources, Supervision, Writing – original draft. DG: Methodology, Validation.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was partially supported by the Humanities and Social Sciences Foundation of the Ministry of Education of China (no. 20YJC630127).
Acknowledgments
The authors would like to thank the editor and reviewers for their valuable comments.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1331679/full#supplementary-material
References
1. Kumar V, Gaurav G, Khan V, Choudhary S, Dangayach GS. Life cycle assessment and its application in medical waste disposal. Materials Today Pro. (2023). doi: 10.1016/j.matpr.2022.12.255
2. Tushar SR, Alam MFB, Bari ABMM, Karmaker CL. Assessing the challenges to medical waste management during the COVID-19 pandemic: Implications for the environmental sustainability in the emerging economies. Socioecon Plann Sci. (2023) 87:101513. doi: 10.1016/j.seps.2023.101513
3. Zhao HL, Wang L, Liu F, Liu HQ, Zhang N, Zhu YW, et al. Energy, environment and economy assessment of medical waste disposal technologies in China. Sci Total Environ. (2021) 796:148964. doi: 10.1016/j.scitotenv.2021.148964
4. An M, Liu M, An H, Ramsey TS. Systematic evaluation of emergency management capacity for rural public health emergencies. Int J Disaster Risk Reduc. (2023) 85:103493. doi: 10.1016/j.ijdrr.2022.103493
5. Taslimi M, Batta R, Kwon C. Medical waste collection considering transportation and storage risk. Comput Oper Res. (2020) 120:104966. doi: 10.1016/j.cor.2020.104966
6. Xueyun M. Optimisation of Emergency Reverse Logistics Network for Medical Waste Under the COVID-19 Pandemic [Master thesis]. Shanghai: Shanghai Polytechnic University (2022).
7. Joneghani NM, Zarrinpoor N, Eghtesadifard M. A mathematical model for designing a network of sustainable medical waste management under uncertainty. Comput Ind Eng. (2022) 171:108372. doi: 10.1016/j.cie.2022.108372
8. Mohamed Faizal U, Jayachitra R, Vijayakumar P, Rajasekar M. Optimization of inbound vehicle routes in the collection of bio-medical wastes. Materials Today Proc. (2021) 45:692–9. doi: 10.1016/j.matpr.2020.02.741
9. Islam MT, Huda N. Reverse logistics and closed-loop supply chain of Waste Electrical and Electronic Equipment (WEEE)/E-waste: a comprehensive literature review. Resour Conserv Recycl. (2018) 137:48–75. doi: 10.1016/j.resconrec.2018.05.026
10. Yaspal B, Jauhar SK, Kamble S, Belhadi A, Tiwari S. A data-driven digital transformation approach for reverse logistics optimization in a medical waste management system. J Clean Prod. (2023) 430:139703. doi: 10.1016/j.jclepro.2023.139703
11. Görçün F, Aytekin A, Selçuk K, Tirkolaee EB. Evaluating and selecting sustainable logistics service providers for medical waste disposal treatment in the healthcare industry. J Clean Prod. (2023) 408:137194. doi: 10.1016/j.jclepro.2023.137194
12. Wang N, Cui W, Zhang M, Jiang Q. Routing optimization for medical waste collection considering infectious risk and multiple disposal centers. Expert Syst Appl. (2023) 234:121035. doi: 10.1016/j.eswa.2023.121035
13. Leal Filho W, Lisovska T, Fedoruk M, Taser D. Medical waste management and the UN sustainable development goals in Ukraine: an assessment of solutions to support post-war recovery efforts. Environ Challenges. (2023) 13:100763. doi: 10.1016/j.envc.2023.100763
14. Liu HC, You JX, Lu C, Shan MM. Application of interval 2-tuple linguistic MULTIMOORA method for health-care waste treatment technology evaluation and selection. Waste Management. (2014) 34:2355–64. doi: 10.1016/j.wasman.2014.07.016
15. Kalhor R, Kiaei MZ, Mohebbifar R, Bahrami ES, Azmal M. Prioritizing the options for health-care waste management in Qazvin: using a multi-criteria decision making approach. Genetics Millennium. (2016). doi: 10.15412/J.JBTW.01050603
16. Makajic-Nikolic D, Petrovic N, Belic A, Rokvic M, Radakovic JA, Tubic V, et al. The fault tree analysis of infectious medical waste management. J Clean Prod. (2016) 113:365–73. doi: 10.1016/j.jclepro.2015.11.022
17. Tang J, Liu X, Wang W. COVID-19 medical waste transportation risk evaluation integrating type-2 fuzzy total interpretive structural modeling and Bayesian network. Expert Syst Appl. (2023) 213:118885. doi: 10.1016/j.eswa.2022.118885
18. Niyongabo E, Jang YC, Kang D, Sung K. Generation, management practices and rapid risk assessment of solid medical wastes: a case study in Burundi. J Mat Cycles Waste Manage. (2019) 21:950–61. doi: 10.1007/s10163-019-00854-0
19. Celik S, Peker I, Gök-Kisa AC, Büyüközkan G. Multi-criteria evaluation of medical waste management process under intuitionistic fuzzy environment: a case study on hospitals in Turkey. Socioecon Plann Sci. (2023) 86:101499. doi: 10.1016/j.seps.2022.101499
20. Chai N, Zhou W. Evaluating operational risk for train control system using a revised risk matrix and FD-FAHP-Cloud model: a case in China. Eng Fail Anal. (2022) 137:106268. doi: 10.1016/j.engfailanal.2022.106268
21. Karuppiah K, Sankaranarayanan B, Ali SM. A novel quality function deployment based integrated framework for improving supply chain. Sustainability. (2023) 35:285–98. doi: 10.1080/10429247.2022.2097575
22. Koohathongsumrit N, Chankham W. Route selection in multimodal supply chains: a fuzzy risk assessment model-BWM-MARCOS framework. Appl Soft Comput. (2023) 137:110167. doi: 10.1016/j.asoc.2023.110167
23. Aydin N, Seker S, Sen C. A new risk assessment framework for safety in oil and gas industry: application of FMEA and BWM based picture fuzzy MABAC. J Petr Sci Eng. (2022) 219:111059. doi: 10.1016/j.petrol.2022.111059
24. Celik E, Gul M. Hazard identification, risk assessment and control for dam construction safety using an integrated BWM and MARCOS approach under interval type-2 fuzzy sets environment. Autom Constr. (2021) 127:103699. doi: 10.1016/j.autcon.2021.103699
25. Zheng Q, Shen SL, Zhou A, Lyu HM. Inundation risk assessment based on G-DEMATEL-AHP and its application to Zhengzhou flooding disaster. Sust Cities Soc. (2022) 86:104138. doi: 10.1016/j.scs.2022.104138
26. Ghorui N, Ghosh A, Mondal SP, Bajuri MY, Ahmadian A, Salahshour S, et al. Identification of dominant risk factor involved in spread of COVID-19 using hesitant fuzzy MCDM methodology. Results Phys. (2021) 21:103811. doi: 10.1016/j.rinp.2020.103811
27. Xiao F. A novel multi-criteria decision making method for assessing health-care waste treatment technologies based on D numbers. Eng Appl Artif Intell. (2018) 71:216–25. doi: 10.1016/j.engappai.2018.03.002
28. Aung TS, Luan S, Xu Q. Application of multi-criteria-decision approach for the analysis of medical waste management systems in Myanmar. J Clean Prod. (2019) 222:733–45. doi: 10.1016/j.jclepro.2019.03.049
29. Narayanamoorthy S, Annapoorani V, Kang D, Baleanu D, Jeon J, Kureethara JV, et al. A novel assessment of bio-medical waste disposal methods using integrating weighting approach and hesitant fuzzy MOOSRA. J Clean Prod. (2020) 275:122587. doi: 10.1016/j.jclepro.2020.122587
30. Chang TW, Lo HW, Chen KY, Liou JJ. A novel FMEA model based on rough BWM and rough TOPSIS-AL for risk assessment. Mathematics. (2019) 7:874. doi: 10.3390/math7100874
31. Ketabchi R, Ghaeli MR. An application of fuzzy BWM for risk assessment in offshore oil projects. J Proj Manage. (2019) 4:233–40. doi: 10.5267/j.jpm.2019.3.001
32. Gül M, Ak MF. Assessment of occupational risks from human health and environmental perspectives: a new integrated approach and its application using fuzzy BWM and fuzzy MAIRCA. Stochastic Environ Res Risk Assess. (2020) 34:1231–62. doi: 10.1007/s00477-020-01816-x
33. Moslem S, Gul M, Farooq D, Celik E, Ghorbanzadeh O, Blaschke T, et al. An integrated approach of best-worst method (BWM) and triangular fuzzy sets for evaluating driver behavior factors related to road safety. Mathematics. (2020) 8:414. doi: 10.3390/math8030414
34. Torkayesh AE, Hashemkhani Zolfani S, Kahvand M, Khazaelpour P. Landfill location selection for healthcare waste of urban areas using hybrid BWM-grey MARCOS model based on GIS. Sust Cities Soc. (2021) 67:102712. doi: 10.1016/j.scs.2021.102712
35. Erdem M. Designing a sustainable logistics network for hazardous medical waste collection a case study in COVID-19 pandemic. J Clean Prod. (2022) 376:134192. doi: 10.1016/j.jclepro.2022.134192
36. Govindan K, Nosrati-Abarghooee S, Nasiri MM, Jolai F. Green reverse logistics network design for medical waste management: A circular economy transition through case approach. J Environ Manage. (2022) 322:115888. doi: 10.1016/j.jenvman.2022.115888
37. Cao C, Xie Y, Liu Y, Liu J, Zhang F. Two-phase COVID-19 medical waste transport optimisation considering sustainability and infection probability. J Clean Prod. (2023) 389:135985. doi: 10.1016/j.jclepro.2023.135985
38. Chen C, Chen J, Fang R, Ye F, Yang Z, Wang Z, et al. What medical waste management system may cope With COVID-19 pandemic: Lessons from Wuhan. Resource, Conserv Recycl. (2021) 170:105600. doi: 10.1016/j.resconrec.2021.105600
39. Liu S, Zhang J, Niu B, Liu L, He X. A novel hybrid multi-criteria group decision-making approach with intuitionistic fuzzy sets to design reverse supply chains for COVID-19 medical waste recycling channels. Comput Ind Eng. (2022) 169:108228. doi: 10.1016/j.cie.2022.108228
40. Shanshan S. Research on Safety Risk Evaluation System of Medical Waste Logistic [Master thesis]. Beijing: Capital University of Economics and Business (2010).
41. Nimita Jebaranjitham J, Selvan Christyraj JD, Prasannan A, Rajagopalan K, Chelladurai KS, Gnanaraja JKJS, et al. Current scenario of solid waste management techniques and challenges in COVID-19 – A review. Heliyon. (2022) 8:e09855. doi: 10.1016/j.heliyon.2022.e09855
42. Zografos KG, Samara S. Combined location-routing model for hazardous waste transportation and disposal. Transp Res Record J Transp Res Board. (1989) 1245:52–9.
43. Ouyang L, Zhu Y, Zheng W, Yan L. An information fusion FMEA method to assess the risk of healthcare waste. J Manage Sci Eng. (2021) 6:111–24. doi: 10.1016/j.jmse.2021.01.001
44. Kumar A, Duggal S, Gur R, Rongpharpi SR, Sagar S, Rani M, et al. Safe transportation of biomedical waste in a health care institution. Indian J Med Microbiol. (2015) 33:383–6. doi: 10.4103/0255-0857.158559
45. Karimi H, Herki BMA, Gardi SQ, Galali S, Pirsaheb M. Site selection and environmental risks assessment of medical solid waste landfill for the City of Kermanshah-Iran. Int J Environ Health Res. (2020) 30:13. doi: 10.1080/09603123.2020.1742876
46. Mihai FC. Assessment of COVID-19 waste flows during the emergency state in Romania and related public health and environmental concerns. Int J Environ Res Public Health. (2020) 17:5439. doi: 10.3390/ijerph17155439
47. Tabrizi JS, Rezapour R, Saadati M, Seifi S, Amini B, Varmazyar F, et al. Medical waste management in community health centers. Iran J Public Health. (2018) 47:286–91.
48. Akpieyi A, Tudor TL, Dutra C. The utilisation of risk-based frameworks for managing healthcare waste: a case study of the national health service in London. Saf Sci. (2015) 72:127–32. doi: 10.1016/j.ssci.2014.08.014
49. Huang W, Zhang Y, Kou X, Yin D, Mi R, Li L, et al. Railway dangerous goods transportation system risk analysis: an interpretive structural modeling and Bayesian network combining approach. Reliab Eng Syst Safety. (2020) 204:107220. doi: 10.1016/j.ress.2020.107220
50. Manupati VK, Ramkumar M, Baba V, Agarwal A. Selection of the best healthcare waste disposal techniques during and post COVID-19 pandemic era. J Clean Prod. (2021) 281:125175. doi: 10.1016/j.jclepro.2020.125175
51. Al-Emad AA. Assessment of medical waste management in the main hospitals in Yemen. Eastern Mediter Health J. (2011) 17:730–7. doi: 10.26719/2011.17.10.730
52. Wei-Juan WU. Existing problems in medical waste management and countermeasures. Chin J Nosocomiol. (2011).
53. Yong Z, Gang X, Guanxing W, Tao Z, Dawei J. Medical waste management in China: a case study of Nanjing. Waste Manage. (2009) 29:1376–82. doi: 10.1016/j.wasman.2008.10.023
54. Song W, Li J, Li H, Ming X. Human factors risk assessment: an integrated method for improving safety in clinical use of medical devices. Appl Soft Comput. (2020) 86:105918. doi: 10.1016/j.asoc.2019.105918
55. Makan A, Fadili A. Sustainability assessment of healthcare waste treatment systems using surrogate weights and PROMETHEE method. Waste Manage Res. (2021) 39:73–82. doi: 10.1177/0734242X20947162
56. Schmidt RC. Managing Delphi Surveys Using Nonparametric Statistical Techniques. London: Blackwell Publishing Ltd. (1997). 763–74.
57. Zhang CL, Zhang J, Yang Q. identifying critical risk factors in green product certification using hybrid multiple-criteria decision-making. Sustainability. (2022) 14:1–12. doi: 10.3390/su14084513
58. Deng ZY. Multi Criteria Decision Analysis Method and Application. Shanghai: Dingmao Book Publishing Co. Ltd (2012).
60. Rezaei J. Best-worst multi-criteria decision-making method: Some properties and a linear model. Omega. (2016) 64:126–30. doi: 10.1016/j.omega.2015.12.001
61. Chen CT, Lin CT, Huang SF. A fuzzy approach for supplier evaluation and selection in supply chain management. Int J Prod Econ. (2006) 102:289–301. doi: 10.1016/j.ijpe.2005.03.009
62. Mardani A, Jusoh A, Zavadskas EK. Fuzzy multiple criteria decision-making techniques and applications - Two decades review from 1994 to 2014. Expert Syst Appl. (2015) 42:4126–48. doi: 10.1016/j.eswa.2015.01.003
63. Qian Z, Xueping W. The comparision of some fuzzy operators used in fuzzy comprehensive evaluation models. Fuzzy Syst Math. (2016) 30:165–71.
64. Khorram-Manesh A, Goniewicz K, Burkle FM. Unleashing the global potential of public health: a framework for future pandemic response. J Infect Pub Health. (2024) 17:82–95. doi: 10.1016/j.jiph.2023.10.038
65. Hou Y, Jia L, Ma W, Hao JL. Analysing the factors affecting medical waste generation in China. Sust Chem Pharm. (2023) 32:100975. doi: 10.1016/j.scp.2023.100975
Keywords: medical waste logistics, public health emergencies, risk identification, risk assessment, best-worst method
Citation: Wang X, Liu L, Wang L, Cao W and Guo D (2024) An application of BWM for risk control in reverse logistics of medical waste. Front. Public Health 12:1331679. doi: 10.3389/fpubh.2024.1331679
Received: 06 November 2023; Accepted: 08 January 2024;
Published: 26 January 2024.
Edited by:
Ciro Fernando Bustillo LeCompte, Toronto Metropolitan University, CanadaReviewed by:
Karuppiah Koppiahraj, Saveetha University, IndiaPradeep Nair, Central University of Himachal Pradesh, India
Copyright © 2024 Wang, Liu, Wang, Cao and Guo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenjun Cao, Y2Fvd2VuanVuQGRsdS5lZHUuY24=
 Xiaozhu Wang1
Xiaozhu Wang1 Wenjun Cao
Wenjun Cao