- 1College of Geography and Planning, Chengdu University of Technology, Chengdu, China
- 2Qilu Hospital, Shandong University, Jinan, China
Introduction: Green spaces have been recognized for their ecological services, including air purification and biodiversity protection, which contribute to the enhancement of life quality and well-being. However, despite the surge in research evaluating the impact of blue-green spaces on health outcomes, we still lack a definitive understanding of how green and blue spaces affect human health outcomes. To assess the impact of blue-green spaces on human health outcomes, we systematically summarized and evaluated the relationship between green and blue spaces and human health through an umbrella review of epidemiological meta-analyses up to the year 2024.
Methods: The study follows the PRISMA guidelines and includes meta analyses from PubMed, Embase, and Cochrane databases, focusing on evidence and methodological improvements. Inclusion criteria encompass studies on human populations, exposure to green and blue spaces, and health outcomes such as mortality, disease risk, and physiological indicators. Data extraction and quality assessment of evidence and methods are conducted using the GRADE system and AMSTAR 2 tool.
Results: We find that green space exposure is associated with reduced all-cause mortality, mortality from cardiovascular diseases, incidence of diabetes and metabolic syndrome, low birth weight, and mental health improvements. Blue spaces also show positive associations with beneficial health outcomes, including reduced obesity rates and improved psychological well-being. However, the evidence regarding green space exposure and specific health outcomes such as cancer, asthma, and allergic rhinitis remains heterogeneous and unclear.
Discussion: Green and blue spaces clearly have some impact on health. For some outcomes, the effects are robust. This article emphasizes the importance of improving residents’ health through urban planning in public health strategies.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/, identifier [CRD42024533346].
1 Introduction
As an essential component of the human living ecosystem, green spaces have increasingly drawn attention for their impact on human health (1). Green spaces not only provide recreational areas but also offer various ecological services such as air purification, mitigation of the heat island effect, and biodiversity protection (2). These services play a crucial role in enhancing residents’ quality of life and physical and mental well-being. Numerous studies in recent years have confirmed the positive association between green spaces and human health, including promoting physical activity (3), reducing mortality rates (4), lowering the risk of cardiovascular diseases (5), and improving mental health (6).
Although a systematic review of this field was conducted in 2021 (7), significant advancements in the study of the relationship between green spaces and human health have been made over the past 3 years due to continuous improvements in research methodologies and the emergence of new scientific evidence. These advancements include identifying and confirming more health outcomes associated with green spaces, such as the risks of type 2 diabetes (8, 9) and obesity (101, 102). Correspondingly, new literature reviews and meta-analyses have increased not only in quantity but also in the depth and breadth of research. These studies cover various aspects, from the impact of green spaces on specific health outcomes to how green space characteristics (10), frequency of exposure (11), and socioeconomic factors modulate this relationship (12). There are also articles where no relationship is found or a negative relationship in some results. Some studies have even presented contradictory results. We are drowning in a sea of evidence, yet we still lack a definitive understanding of the impact of green spaces on human health outcomes.
This study aims to systematically summarize and evaluate all meta-analyses on the relationship between green spaces and human health up to 2024. 5 through an umbrella review of evidence provided by epidemiological studies (13). Compared to the 2021 study, we focus on new evidence, improvements in research methods, potential differences, and controversies to supplement and update the existing knowledge system. We conduct relatively more rigorous semi-quantitative analyses using advanced methodological tools (e.g., AMSTAR2, GRADE) to obtain updated and more reliable evidence. Additionally, we will update the assessment of another important system in the living environment: the impact of blue spaces on human health, specifically, it refers to the living environment and water-related environment, such as lakes, rivers, wetlands, coasts, and other water bodies (14). Like green spaces, blue spaces provide opportunities for recreation and relaxation, and emerging research suggests that they can also have significant effects on mental health, physical well-being, and social interactions (15). We aim to provide the latest scientific evidence for public health decision-makers, urban planners, and environmental protection policymakers, guiding them in formulating more effective strategies to promote the protection and utilization of green spaces, thereby improving the health and quality of life of urban residents, and to anticipate future research directions.
2 Methods
We conducted a systematic umbrella review of the meta-analyses following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (16) (Supplementary Table S1). The protocol for this umbrella review has been registered in the International Prospective Register of Systematic Reviews (Prospero), ID: CRD42024533346.
2.1 Inclusion criteria and searches
We systematically searched three international electronic databases: PubMed, Embase, and Cochrane. Our search strategy used terms related to green spaces (“urban forest,” “green area,” “open space,” “greenness,” “greenspace,” “greenery,” “urban park,” “green infrastructure,” “urban vegetation,” “green land,” and greenspace and land type indicators: “normalized difference vegetation index, (NDVI),” “Soil Adjusted Vegetation Index,” “Enhanced Vegetation Index,” and “Leaf area index”), blue spaces, gardening, forest bathing, and exposure to natural environments, as well as systematic reviews and meta-analyses (“systematic review” or “meta-analysis”) (Supplementary Table S2). The data included studies published up to May 30, 2024. We restricted our search to research articles. We manually cross-checked the results of the title and abstract searches to remove duplicates and extended the search to papers and reports cited in the literature but not in the above databases.
Two researchers (W.X. and F.B.) independently screened the titles and abstracts to determine study inclusion. Discrepancies were resolved through discussion with a third author (W.J.). Our inclusion criteria were as follows: (1) Population—studies on human populations regardless of age, gender, race, geographic region, and health status; (2) Exposure—studies on exposure to green and blue spaces, including residential green spaces (assessed using vegetation indices, proportion of green space, proximity to green spaces, or the amount of green space in a specific area), activities conducted in natural environments (e.g., exercising in nature, gardening) and exposure to blue spaces; (3) Comparison—studies comparing health impacts of different levels of green space exposure; (4) Outcomes—studies investigating any health outcomes, such as mortality, disease risk, prevalence, incidence, and physiological indicators. We applied no specific design limitations to the primary studies under consideration. However, we deliberately excluded studies not written in English, not involving human subjects, and conference abstracts from our review.
2.2 Data extraction
Two authors (W.X. and F.B.) independently extracted the data, with discrepancies resolved through discussion with a third author (W.J.). For every systematic review that met eligibility criteria, we extracted key details, including the authorship, the year of publication, the type of study design—be it observational or interventional—the principal findings, and the defining traits of the encompassed primary studies. These characteristics included age range, sample size, methods of assessing green/blue spaces, health outcomes, effect sizes, 95% confidence intervals, and statistical significance.
2.3 Credibility and quality assessment of evidence and methods
The quality of included meta-analyses was evaluated by using AMSTAR 2 (A Measurement Tool to Assess Systematic Reviews—second edition) (17). Two authors independently assessed each item of the tool, and any discrepancies were discussed with a third author. According to AMSTAR2 checklist, items 2, 4, 7, 9, 11, 13, and 15 were identified as critical domains, as a basis for evaluate the characteristics of systematic reviews included in the umbrella review (Supplementary Table S3).
We used the GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) system to assess the quality of evidence for each outcome in each meta-analysis, categorizing them as “high,” “moderate,” “low,” or “very low” (18). According to GRADE standards, all observational studies are considered low-quality evidence. The GRADE method includes eight criteria, five of which can lower confidence in the accuracy of effect estimates, resulting in downgrading: risk of bias, inconsistency of results, indirectness of evidence, imprecision, and publication bias. Additionally, three criteria can increase or enhance confidence: a large magnitude of effect with no plausible confounders, a dose–response gradient, and a study where all plausible residual confounders would reduce the effect or suggest a spurious effect if not controlled. Two authors independently assessed each item based on the content of the articles. Heterogeneity was primarily evaluated using the I2 value: we defined 0–30% as low, 30–70% as moderate, and above 70% as high heterogeneity. If high heterogeneity was observed, the evidence score was downgraded.
2.4 Data synthesis
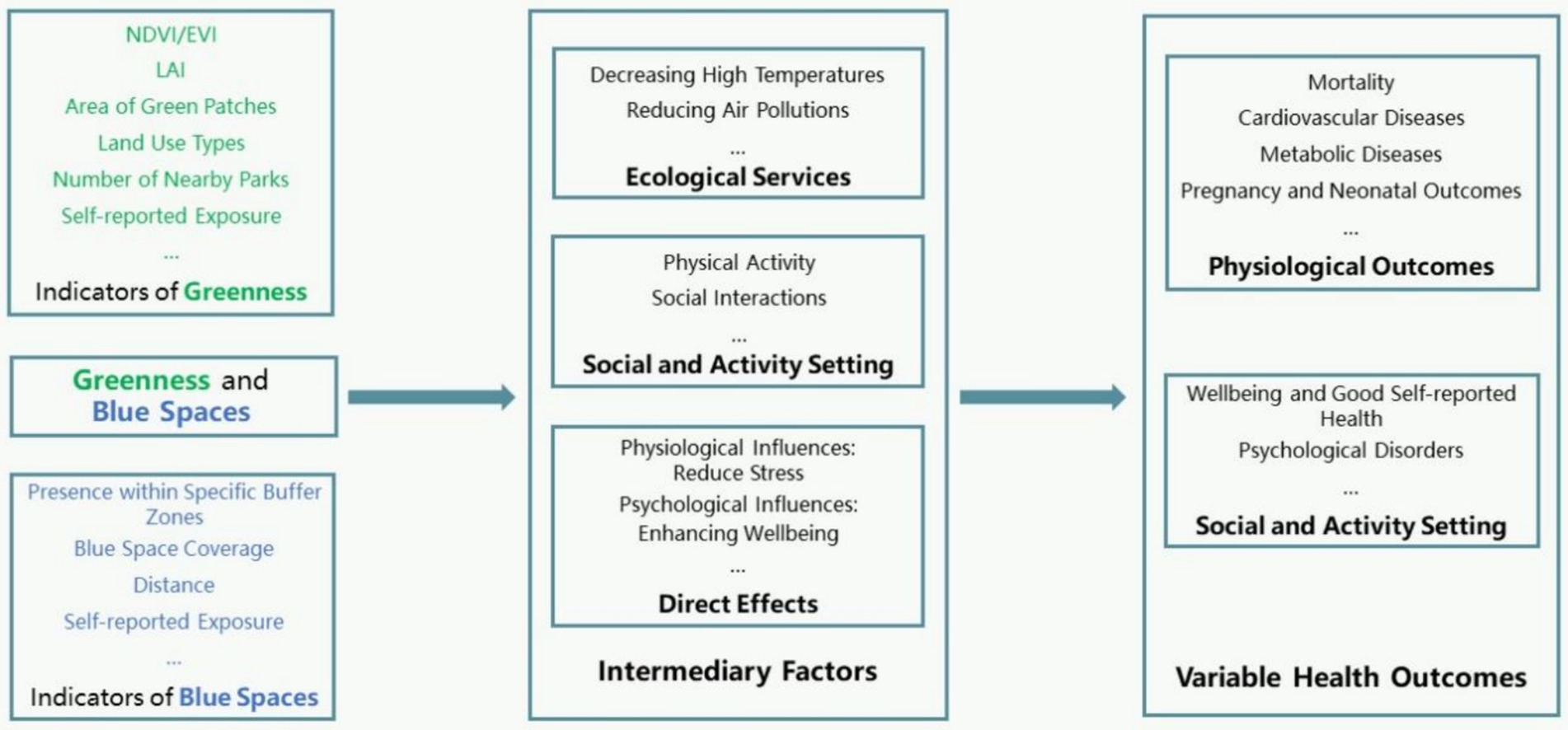
We conducted data synthesis in a semi-quantitative manner. We graded each health outcome in the included studies using the GRADE system and assessed their statistical significance. If for the same or similar outcomes, there was consistent statistical significance across all studies, we considered the result to be robust. This would indicate that green (or blue) is a protective factor for health. Conversely, we might not be able to confirm the consistency of the research, or for some outcomes, the studies show inconsistency, making it difficult to determine the association (Figure 1; Table 1; Supplementary Table S4). All the meta-analyses referenced in the results section are included in the umbrella review.
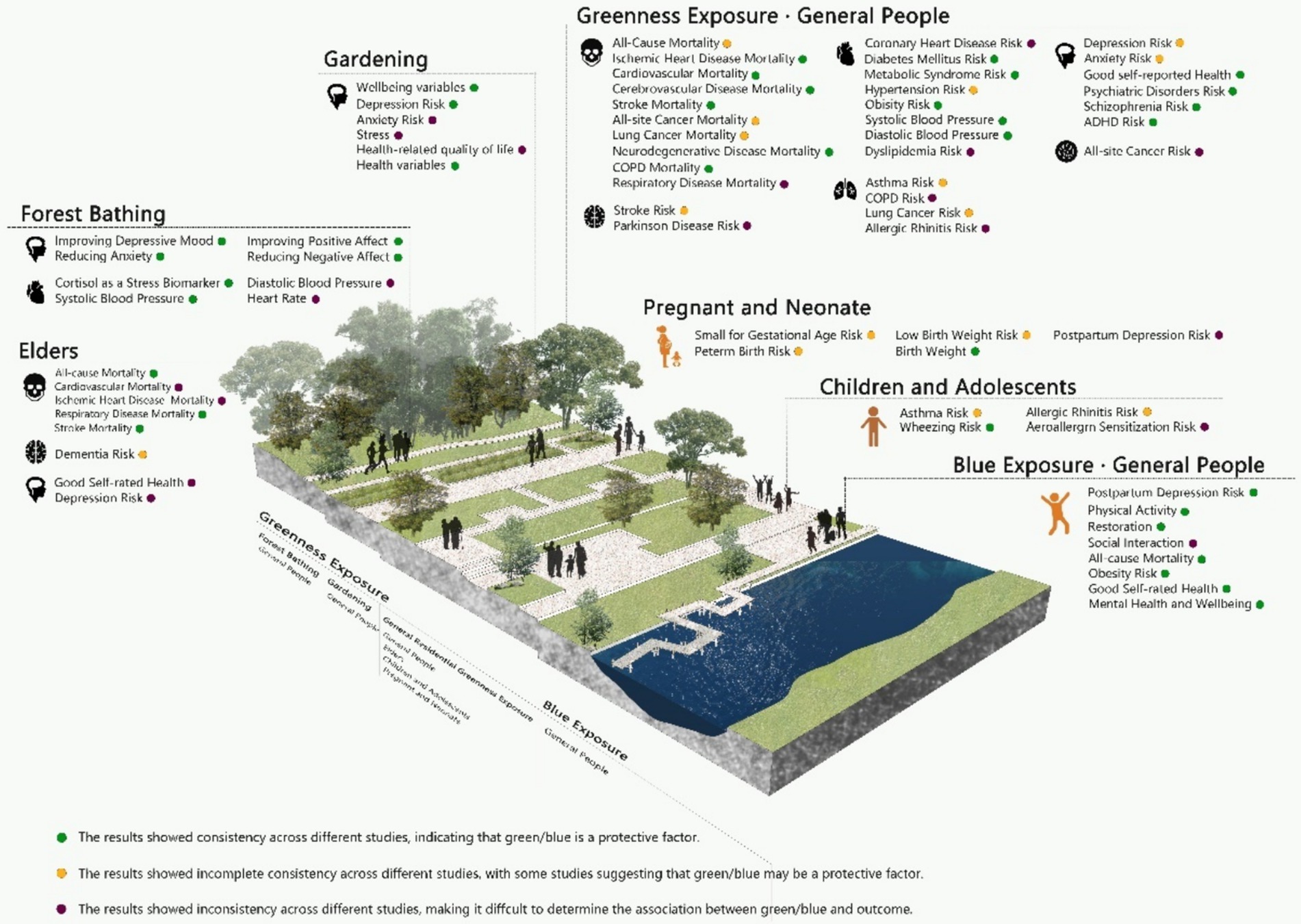
Figure 1. The association between green/blue spaces and human health outcomes. COPD, Chronic Obstructive Pulmonary Disease; ADHD, Attention Deficit Hyperactivity Disorder.
Key details are extracted, including author, year of publication, type of study design (observational or interventional), key findings, and defining features of the major studies included. These features include age range, sample size, methods for assessing green/blue spaces, health outcomes, effect size, 95% confidence intervals, and statistical significance. Heterogeneity was also included in the statistics, and was mainly assessed using an I2 value: where 0–30% was defined as low heterogeneity, 30–70% as moderate heterogeneity, and more than 70% as high heterogeneity. If high heterogeneity is observed, the confidence with the evidence is reduced.
3 Results
3.1 Systematic review retrieval
The initial search identified 4,475 records. After removing duplicates, 4,214 titles and abstracts of systematic reviews were assessed, and 4,125 articles were excluded during the title and abstract screening, 89 articles were subjected to full-text review. A total of 34 articles were further eliminated as they were irrelevant to the topic or focused on other priorities. Two articles (19, 20) were excluded due to unavailability of full text or being conference abstracts, and 6 articles (21–26) were excluded for not being quantitative analyses. Finally, 47 meta-analyses were included in the umbrella review (Figure 2).
3.2 Characteristics of systematic reviews included in the umbrella review
The umbrella review included 47 systematic reviews with meta-analyses. Most of these articles were published between 2021 and 2024, with 34 articles (approximately 72%) published after 2021. The number of primary studies included in the meta-analyses for each health outcome ranged from 2 to 76. Most of the primary studies incorporated were observational, with experimental or interventional studies in the minority. Our research spanned a wide demographic range, encompassing individuals from infancy to old age, and was predominantly centered on regions known for their capacity to execute extensive cohort studies, including North America, Europe, and China.
3.3 Green/blue spaces exposure measures
Of the 47 studies, 45 were related to green spaces. The remaining two assessed blue spaces. Various metrics have been used to assess green space exposure. Objective parameters include the Normalized Difference Vegetation Index (NDVI) (29/45), Leaf Area Index (LAI) (1/46), area of green patches (6/45), distance to the nearest green space (2/45), and the number of nearby parks (1/45). One quantitative review analyzing the health impacts of residential building characteristics included descriptions of land use types (1/45). Subjective parameters included self-reported exposure and visits to natural environments (8/45). We separately assessed activities conducted in natural environments, such as forest bathing (2/45) and gardening (4/45). Blue space exposure assessments included distance, the presence of blue spaces within specific buffer zones, blue space coverage, and self-reported frequency of use.
3.4 Health outcomes
We categorized the health outcomes related to green space exposure into several sections: outcomes associated with green space exposure include mortality, neurological disorders and cognitive function, cardiovascular and metabolic diseases (including cardiovascular diseases, diabetes, metabolic syndrome, overweight and obesity, metabolic indicators), cancer, allergic diseases (mainly affecting children and adolescents), pregnancy outcomes, and mental health. Additionally, we conducted a separate review of blue space outcomes. These health outcomes were measured using various methods, including physician diagnosis, questionnaire surveys, records from hospitals or other health-related departments, self-reported health status, and laboratory tests.
3.5 Methodological quality
Many of the included systematic reviews did not meet all seven key domains of the AMSTAR2 checklist above (Table 2). 25 out of 47 reviews (53%) developed a protocol for this review. 46 out of 47 reviews (98%) conducted a comprehensive literature search or pre-specified specific cohorts. Of the 47 reviews, 11 (23%) offered a rationale for excluding studies, while 46 (98%) employed suitable meta-analysis techniques. A strong majority, 42 (89%), considered the potential bias in the primary studies during their discussions. Nevertheless, only 32 (68%) of the reviews evaluated the risk of publication bias due to small sample sizes in the primary research. We used GRADE grading to assess each study’s evidence level for each health outcome (N = 154). Most of the evidence from studies ranged from “very low” to “low” quality (Table 3).
3.6 Associations between green spaces exposure and health outcomes
The final confidence rating was evaluated using a stepped upgrade/downgrade scale: intervention studies had a high initial quality rating, while all observational studies were considered low-quality evidence. The following items lead to a downgrade: Risk of bias, Inconsistent results, Indirect evidence, and Imprecision. The Dose–response gradient is an independent escalation criterion.
3.6.1 Mortality outcome
Several systematic reviews and meta-analyses have shown a significant association between green space exposure and reduced all-cause mortality. For the general population, an increase of 0.1 unit in NDVI around residential areas is associated with a 4 to 7% reduction in all-cause mortality risk (27, 28). Among the older adult population, each 0.1 unit increase in NDVI is linked to a 1% reduction in all-cause mortality risk (29). Additionally, green space exposure may reduce disease-specific mortality rates by providing a healthier living environment. For instance, every 0.1 unit increase in NDVI is associated with a 2–3% reduction in mortality from cardiovascular disease (CVD), ischemic heart disease (IHD), and cerebrovascular disease (CBVD) (30–32). Other quantitative analyses found beneficial associations between green space and mortality rates related to neurodegenerative diseases (33) and chronic obstructive pulmonary disease (34). For the older adult, each 0.1 unit increase in NDVI corresponds to a 23 to 33% lower risk of stroke mortality (29). Two studies explored potential associations between green space exposure and mortality from cancer, with quantitative analyses suggesting potentially beneficial associations with mortality from lung cancer and prostate cancer (35, 36). These studies consistently provide evidence demonstrating the beneficial effects of green space exposure on overall health risks in the general population, particularly regarding cardiovascular diseases. However, studies on mortality risks related to other diseases currently lack quantitative data, and the evidence quality is very low, necessitating cautious interpretation of the study results.
3.6.2 Neurological disorders and cognitive function
Recent studies have highlighted the association between green space exposure and neurological system diseases (NSD), which is a significant concern in public health. A meta-analysis covering 15 studies investigated the relationship between greenness exposure and NSD outcomes, including cerebrovascular diseases, stroke, and neurodegenerative diseases (33). The analysis found a significant negative correlation between greenness exposure and the risk of NSD mortality or incidence/prevalence.
Specifically, two studies observed that green space exposure could be a protective factor against dementia among various environmental exposures in residential settings (37, 38). However, a dose–response study separately examined the association between greenness and dementia. It found a slight negative correlation at moderate levels of greenness exposure but no association at high levels (39).
While evidence remains limited, factors related to climate-related exposures, including air pollution (40), short-term extreme heat (41), and climate change (42), may exacerbate symptoms of Alzheimer’s disease and related dementias (ADRD) and Parkinson’s disease (PD), and disproportionately affect them. Exposure to green spaces, vegetation, or parks may mitigate the impacts of these exposures. However, existing studies are limited and inconsistent, suggesting very low levels of evidence.
Commonly used green space metrics may not capture specific outdoor green space utilization, and less investigation into policy-related and socio-economic protective characteristics, such as economic development status and education level, remains. These overlooked features could be crucial factors influencing how green space exposure mediates neurological and cognitive function.
3.6.3 Cardiovascular and metabolic diseases
The relationship between green space exposure and cardiovascular diseases and metabolic health has garnered considerable attention. Previous studies indicate that meta-analyses consistently show that green space exposure reduces mortality rates associated with ischemic heart disease and cerebrovascular diseases, though evidence regarding disease incidence is inconsistent. Research suggests that green spaces can lower the risk of cerebrovascular diseases (33), but evidence regarding the impact on cardiovascular disease risk is limited (32).
Regarding type 2 diabetes mellitus, different studies indicate that greater exposure to green spaces is associated with reduced diabetes risk (32, 43, 44), potentially linked to higher community walkability (43). Multiple systematic reviews and meta-analyses have explored the relationship between green space and metabolic health factors, including obesity (45), body mass index (BMI), hypertension (HTN) (46), blood glucose (BG), and lipid profiles (44). Studies indicate that greater exposure to green spaces is associated with lower odds of hypertension, obesity, and diabetes. Normalized Difference Vegetation Index (NDVI) in residential areas is negatively correlated with the incidence of metabolic syndrome (47).
Considering the clear evidence of green spaces and mortality from CVD, there is conflicting evidence regarding the impact of green space on mortality of cardiovascular diseases and risk. Despite heterogeneous study results and low evidence levels, it appears that residential green space exposure has a latent beneficial effect on metabolic health, warranting further prospective and mechanistic research.
3.6.4 Tumors
Research on green space and cancer primarily focuses on lung cancer, while studies on other cancers (breast, prostate, and skin) suggest green spaces may be protective factors, but overall evidence is very limited due to small cohort sizes (35, 36). Additionally, green space may have different impacts on cancer mortality rates for urban and rural residents, with urban residents potentially benefiting more from green spaces (35). The quality of evidence in most current studies is rated as “very low,” indicating the need for higher-quality research to establish the exact relationship between green space and cancer. Given the unclear and highly complex etiology of cancer, along with numerous confounding factors, establishing causation is challenging; thus, future research needs to assess environmental exposure factors and investigate biological mechanisms more precisely.
3.6.5 Respiratory and allergic diseases
As previously mentioned, green space exposure may serve as a protective factor against lung cancer. For other chronic non-communicable respiratory diseases, only one study categorized the impact of green space on asthma incidence and COPD incidence and mortality rates for the general population. The results indicated a significant association where an increase of 0.1 in NDVI was linked to reduced asthma incidence, lung cancer incidence, and mortality risk for chronic obstructive pulmonary disease (34). Additionally, multiple studies have explored the effects of residential green spaces, including vegetation and parks, on allergic respiratory diseases such as childhood asthma and allergic rhinitis. However, these studies have produced inconsistent results (32, 48–52). Variations in measurement methods of residential green spaces, disease diagnoses, and adjustment for confounding factors across included studies may influence the outcomes. Furthermore, seasonal changes in residential green spaces and their impact on allergens have not been fully considered. Another study involving nine European cohorts suggested an association between residential green spaces and increased childhood asthma and allergic rhinitis, emphasized that different types of green spaces, such as coniferous forests, may be associated with increased respiratory disease risks (51).
Collectively, studies examining the impact of green space exposure on respiratory health outcomes indicate inconclusive evidence regarding whether green spaces act as protective factors. The complex interactions between green spaces and respiratory system health may vary across different geographical regions and climatic conditions (53). Given the distinct mechanisms underlying chronic non-communicable respiratory diseases, respiratory infections, and allergic diseases, future research should categorically explore these diseases and consider the influence of vegetation types.
The association between residential green spaces and allergic diseases in children and adolescents is an active area of environmental health research. Simultaneously, “child-friendliness” is a focal point in landscape design studies. Certain plant species may act as allergens (54); therefore, in relevant planning and design, careful consideration should be given to the selection of vegetation that could potentially trigger allergic diseases.
3.6.6 Pregnancy and neonatal outcomes
According to meta-analysis results, an increase of 0.1 unit in Normalized Difference Vegetation Index (NDVI) is associated with higher birth weight (55–59). Additionally, exposure to green spaces is linked to reduced risk of low birth weight (LBW) (55–57, 59). While the association between green space exposure and preterm birth (PTB) or small-for-gestational-age (SGA) varies across studies (32, 56–59), these studies also indicate a positive trend in reducing these risks. Some studies suggest a non-linear relationship between green space exposure and birth weight, indicating that moderate levels of green space may be more beneficial than extremely high or low levels (59). The heterogeneity of these research findings suggests the presence of other factors influencing the relationship between green space exposure and pregnancy outcomes, such as socioeconomic variables, other environmental factors, and residential conditions.
3.6.7 Mental health outcomes
Residential green spaces are considered a unique and potentially modifiable exposure that can reduce physiological stress and improve mental health (60). The relationship between green spaces and mental health is a multidimensional and complex research area that has garnered increasing attention in recent years. The exact impact of green space exposure on improving mental health outcomes in adults, such as reducing depression (37, 61, 62) and anxiety symptoms, shows high heterogeneity among studies (37, 61). Although short-term exposure to natural environments exhibits significant heterogeneity, minor effects suggest a decrease in depressive mood following exposure to natural environments, whereas the increase in green spaces within residential areas alone has limited effects on enhancing positive emotions (63). However, greener residential environments correspond to higher self-rated health assessments (32). For specific populations like postpartum depression, the relationship with green spaces is less significant, whereas blue spaces may pose potential risk factors (64). Nevertheless, due to high-risk bias and low-quality studies, the credibility of these results is limited. Future research should aim to reduce biases, enhance study quality, and adhere to reporting guidelines.
Some studies further support the positive impact of green spaces on mental health. Nature-based interventions (NBIs) such as gardening, green exercise, and nature-based therapies have been effective in improving mental health outcomes for adults, including those with existing mental health issues. These interventions include promoting overall mental health through gardening activities (65–68) and alleviating depression (65). Physical activities in forests have shown improvements in depression (69–71), reduction in anxiety (69, 71), enhancement of positive emotions (69, 71), reduction of anxiety symptoms (69, 71), and have been associated with lower cortisol levels (72) and systolic blood pressure reduction (70). The most effective intervention durations range from 8 to 12 weeks, with optimal dosages varying from 20 to 90 min (69). However, interventional studies may introduce additional placebo effect, which is a significant factor limiting the credibility of the results. A policy review emphasizes the importance of creating psychologically supportive urban environments for adolescents and young adults. It suggests that while cities offer opportunities for medical, educational, and economic benefits, urban environments often pose challenges to mental health. Implementing nature-based solutions within cities through parks and urban green spaces is crucial for enhancing the mental health and well-being of urban residents (73).
3.7 Associations between blue exposure and health outcomes
Blue Spaces refer to all forms of natural and artificial surface water bodies, which are essential components of urban environments. There is currently only two retrieved quantitative analysis of evidence regarding the association between Blue Spaces and health outcomes. The studies found that urban Blue Spaces are positively associated with decreased obesity rates, lower all-cause mortality, overall health status, and self-reported psychological health and well-being (74). Blue Spaces facilitate physical activity and play a significant role in providing restorative environments. The impact of Blue Spaces, including coastlines, on human health in residential environments appears promising, but more evidence is still needed (75). In addition to this, some studies have shown that blue spaces help enhance health through their environmental benefits (76). Wetlands and lakes play a role in air purification, reducing air pollutants, and mitigating the urban heat island effect. Water bodies can regulate local climates, lower temperatures, and provide moisture through evaporation, helping to alleviate the adverse health effects of urban heat on residents (77). Some studies suggest that exposure to blue spaces seemed to reduce the risk of certain diseases, particularly those related to environmental pollution. For example, populations living near blue spaces generally show lower rates of cardiovascular diseases (78) compared to those residing in city centers or industrial areas.
4 Discussion
4.1 Key findings
This review encompassed a total of 47 meta-analyses. The majority of these meta-analyses were observational and evaluated green space exposure using both objective and subjective parameters, although significant variations existed between studies. Overall, exposure to green spaces showed protective effects on all-cause and cardiovascular disease mortality, overall cardiovascular disease incidence, diabetes and metabolic syndrome, low birth weight, and mental illnesses. Contact with natural environments, including gardening activities, facilitated reductions in depression, anxiety, stress, and cortisol levels. Exposure to blue spaces was positively correlated with reduced all-cause mortality, overall health status, and self-reported psychological health and well-being.
In contrast, within the included systematic reviews, evidence regarding green space exposure and disease-specific mortality, cancer, asthma, and allergic rhinitis was heterogeneous and remains unclear. AMSTAR2 assessments indicated that most included systematic reviews and meta-analyses had one or more methodological limitations, potentially introducing credibility biases into the synthesized evidence.
4.2 Discussion of high heterogeneity in the results
In this review, we encountered significant heterogeneity across several outcomes, as indicated by high I2 values and Q statistics. High levels of heterogeneity can challenge the interpretation of pooled data, as they suggest that the studies may not be directly comparable. To manage this heterogeneity, we followed the GRADE guidelines to perform a detailed heterogeneity assessment for each outcome, considering heterogeneity as a factor for downgrading the strength of evidence in our statistical analysis.
Despite these efforts, we observed that for some outcomes, particularly those with highly divergent results or even contradictory findings, it was necessary to retain all studies in the synthesis, as excluding them would risk omitting valuable data. This approach allowed us to provide a more comprehensive overview, but we acknowledge that it may have introduced further complexity into the interpretation of the results.
High heterogeneity could, in part, stem from the use of different measurement methods for the same health outcomes across studies. Variability in how outcomes are assessed—whether through different scales, questionnaires, or clinical measures—can exacerbate heterogeneity and lead to less consistent results. To address this issue in future studies, we suggest that standardization of outcome measurement tools be considered, particularly for commonly assessed health outcomes. This would enhance the comparability of results and potentially reduce heterogeneity in systematic reviews.
4.3 Potential mechanisms underlying green space and health
Green spaces and their effect on health outcomes involve potential mediating factors, which we categorize into three aspects for discussion.
Firstly, green spaces provide ecological services themselves (2). They are part of residential environments and influence other environmental factors such as heat exposure, air pollution levels, and noise (79), which are causally linked to various health outcomes. For instance, (1) High temperatures affect thermoregulation in humans, leading to heat-related illnesses such as heatstroke, heat fatigue, and heat cramps. Long-term exposure to high temperatures increases the risk of cardiovascular diseases (80). (2) Air pollutants like particulate matter (PM2.5 and PM10), nitrogen dioxide, sulfur dioxide, and ozone contribute to respiratory diseases such as asthma, COPD, and lung cancer (81), and are associated with increased incidence and hospitalization rates for cardiovascular diseases (82). (3) Noise can cause increased psychological stress (83, 84) and elevated risk of cardiovascular diseases (85). Environmental factors impact health in multiple ways, through direct physiological effects and by influencing behaviors and mental health. Therefore, reducing exposure to these environmental risk factors is crucial for protecting public health.
Secondly, green spaces benefit residents’ health by providing social and activity settings (86). (1) Green (and blue) spaces serve as platforms that promote physical activity and social interaction (87, 88), encouraging outdoor activities such as walking, exercising, leisure, and socializing. These activities not only promote physical health but also enhance social interactions, improving mental well-being. Exercise improves cardiorespiratory function (89), prevents and manages chronic diseases (90), enhances bone health (91), and boosts cognitive function (92); (2) Social interactions provide emotional support, reduce loneliness, and help alleviate stress and anxiety (73). Green spaces offer high-quality settings for socializing and activities, which are crucial for their impact on human health. The relationship between urban design with people behavior, and health outcomes is complex, further studies are needed to explore how different urban designs and green spaces specifically impact physical activity and health outcomes.
Additionally, based on our literature review, contact with green (and blue) spaces may have direct effects on residents’ physical health. Activities in green environments can reduce stress and anxiety, improve mood, and enhance psychological well-being (69, 71). Moreover, natural elements in green environments such as trees, water bodies, and vegetation can positively impact physiological indicators like blood pressure (70).
We propose a model (Figure 3) illustrating the role of green and blue spaces in influencing human health. In this model, green spaces and blue spaces positively impact residents’ health through their different service functions, acting as “bridges” between blue/green spaces and human health. These service functions include various aspects of green spaces, such as area, quantity, distribution uniformity, accessibility, biodiversity, vegetation coverage, which reflect different service functions of green spaces. Some studies have suggested positive psychological effects of green spaces, such as biodiversity and landscape composition (93). Future research could further explore the impact and the mechanism of internal characteristics of on resident well-being, as well as regional variations in the relationship between green space service functions and resident health across different socio-economic and cultural backgrounds.
Future research should pay attention to several important issues. First, there is a risk of information loss when converting and indirectly coupling different green space indicators. Current literature reviews mostly rely on cross-sectional surveys based on NDVI/EVI indices. Therefore, future studies should not be limited to NDVI/EVI but should utilize various indicators reflecting green space. It is essential to enhance the quantitative coupling between green space indicators and ecological functions to deepen our understanding of green space ecological benefits. For example, a recent study using AI-based Google Street View assessed neighborhood features related to coronary heart disease prevalence, highlighting associations between the amount and quality of green spaces, forests, and lower CHD incidence (94). For blue spaces, further research is needed to establish standardized measures of exposure that account for aspects such as accessibility, quality, and type of water bodies (e.g., lakes, rivers, coastlines). Consistent definitions and metrics will allow for more reliable comparisons across studies and enable researchers to assess how these variables influence health outcomes. Furthermore, it is essential to explore green and blue spaces across diverse geographic and cultural contexts to verify whether the health benefits observed in one region are applicable globally.
Secondly, longitudinal studies are essential to track the long-term health effects of exposure to green and blue spaces, as cross-sectional studies cannot establish causality. These studies will identify lasting benefits and help understand how exposure across different life stages (e.g., childhood, adolescence, old age) influences health outcomes over time. Geospatial tracking can further refine this by combining environmental data with individual health trajectories. During our understanding of the interaction between health and environmental factors, it is crucial to distinguish between mediating and confounding factors. Mediating factors are part of the causal chain, acting as intermediate steps between the causal variable (green space) and the outcome variable (health). Confounding factors, on the other hand, are variables correlated with both the cause and the effect, potentially obscuring, or masking the true relationships. Factors such as gender, age, education level, regional economic status, and other environmental factors unrelated to green space should be thoroughly analyzed in layers when discussing these confounding factors to clarify causality. Many mediating factors themselves directly influence health independently of the presence of green space. It is important to further clarify the mediating effects reflected by different indicators on various health outcomes and assess their robustness to avoid biases and heterogeneity, thus guiding real-world urban design and landscape planning practices.
Thirdly, a promising direction for future research is to investigate the synergistic effects of green and blue spaces. While both types of spaces have individually been shown to benefit human health, little is known about how they may interact to enhance well-being when combined. For instance, neighborhoods that integrate both green parks and blue water features could provide cumulative health benefits beyond those offered by either type of space alone. Exploring these combined effects could inform urban planning strategies that optimize public health outcomes by integrating both green and blue spaces into urban environments.
Lastly, pure environmental ecological studies can only assess associations and mediating factors but cannot evaluate the physiological reasons behind causal relationships. Future research should integrate knowledge and techniques from multiple fields such as biology, ecology, genetics, molecular biology, and computer science under interdisciplinary backgrounds to delve into the complex mechanisms of human-environment interactions in urban living environments.
4.4 Strengths and limitations
Based on our comprehension, this is the second comprehensive review of evidence linking green spaces and human health, summarizing, and evaluating the evidence using systematic reviews and meta-analyses. It also represents the first systematic summary of quantitative evidence from literature that analyzes the relationship between green or blue spaces and human health in a tertiary review. This tertiary-level research surpasses primary and secondary studies in terms of evidence hierarchy. The authors thoroughly searched three international databases for relevant systematic reviews, and the two authors independently selected studies and extracted data. We strictly adhered to PRISMA guidelines and use the AMSTAR2 checklist to assess the methodological quality of the included articles. The GRADE grading system was introduced to evaluate the level of evidence in the literature. This rigorous process was able to uncover gaps and limitations in the current literature and set the stage for making recommendations to enhance future systematic reviews. Compared to the initial umbrella review in 2021, we observed progress and standardization in evidence assessment, including improved definitions of health outcomes, enhanced consideration of evidence grading, and expanded evaluation of blue spaces (7). Particularly, detailed discussions on mediating factors were added to provide guidance for future green space planning and development.
However, there are several issues to note: AMSTAR2 assessments indicated methodological limitations in most included meta-analyses, potentially undermining the credibility of synthesized evidence. Umbrella reviews can only synthesize associations between green spaces and health outcomes reported in published systematic reviews, potentially missing or underestimating associations not encompassed in these reviews. We recognize that high-quality individual studies and non-meta-analytic reviews can offer valuable insights that are not always captured in pooled analyses. Single studies with rigorous designs may highlight the nuances of green space exposure in specific populations, geographic regions, or under particular environmental conditions, which might not be well-represented in a generalized meta-analysis. Non-meta-analytic reviews often discuss theoretical frameworks or investigate specific pathways through which green space exposure affects human health, which are essential for understanding the mechanisms behind these associations. Although such studies may not provide the statistical power of meta-analyses, their qualitative contributions are indispensable for guiding future research directions and deepening our understanding of this complex relationship. The exclusion of these studies from our umbrella review represents a limitation, as it may omit important findings or perspective, such as the interaction between green space and specific socioeconomic factors (95), or the role of cultural perceptions of nature in health outcomes (96). Future researches are encouraged to integrate both meta-analytic and non-meta-analytic approaches to enrich the evidence base and provide a more holistic view of green space exposure and human health.
The green space indicators covered in this study are as previously described. Most observational studies use objective green space indicators such as NDVI as statistical metrics, which provide convenience in computing statistical measures. Linking residents’ green space exposure to NDVI using satellite imagery has become a research paradigm (97). However, this approach has limitations for many health outcomes. For example, NDVI may overlook information such as vegetation types, health conditions, and biomass within areas, and satellite-derived information is also limited by resolution (98). NDVI values are highly influenced by seasonal changes, and using NDVI values from a single time point may not accurately reflect year-round green space exposure (99). Despite the introduction of averages, this could introduce significant bias in assessing certain diseases such as cardiovascular diseases (32) and allergic diseases (32, 48–52), such as increased cardiovascular disease rates in winter and allergic diseases in spring. Other objective green space indicators, such as proximity to the nearest green space or green space ratio, also suffer from similar information losses. Although some landscape indicators that take into account heterogeneity have been proposed, they have not been widely used (100). The use of subjective assessments, such as residents’ access to green spaces, may introduce subjective biases. The quality of evidence provided by observational studies is much lower than that of intervention studies, indicating the need for more mixed-method and intervention research in the future. There remains considerable heterogeneity in health outcome assessments among studies, and pure environmental ecology alone cannot account for the sources of this heterogeneity.
We limited our review to studies published in English. English-language articles are more readily accessible and manageable for systematic review, and this allowed for a more efficient and consistent review process. This choice may introduce language bias and potentially exclude valuable international studies.
5 Conclusion
Overall, preliminary evidence is observed that exposure to green spaces exerts a protective influence on all-cause mortality and cardiovascular disease mortality, cardiovascular disease incidence, diabetes and metabolic syndrome, low birth weight, and mental disorders. Contact with natural environments, including gardening activities, facilitates the reduction of depression, anxiety, stress, and cortisol levels; exposure to blue spaces is positively correlated with reduced all-cause mortality, improved overall health status, and self-reported psychological well-being and happiness. However, the impact on other health outcomes is limited or uncertain. Nevertheless, these findings mainly stem from heterogeneous cross-sectional studies. Therefore, there is a necessity for longitudinal or intervention study designs to examine causality; there is a demand for more accurate quantitative assessments targeting mediating factors. For instance, dynamic assessments of green exposure using big data technologies should be implemented, considering residents’ utilization of green facilities. Studies should include more populations from low and middle-income countries. Moreover, adherence to standard guidelines in future systematic reviews is essential to bolster their methodological quality.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
XW: Visualization, Writing – original draft. BF: Investigation, Supervision, Writing – review & editing. JW: Funding acquisition, Methodology, Resources, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1505292/full#supplementary-material
References
1. Taylor, L, and Hochuli, DF. Defining greenspace: multiple uses across multiple disciplines. Landsc Urban Plan. (2017) 158:25–38. doi: 10.1016/j.landurbplan.2016.09.024
2. Kumar, A, Ekka, P, Upreti, M, Shilky, S, and Saikia, P. Urban green spaces for environmental sustainability and climate resilience In: S Nautiyal, AK Gupta, M Goswami, and YD Imran Khan, editors. The Palgrave handbook of socio-ecological resilience in the face of climate change: Contexts from a developing country. Singapore: Springer Nature Singapore (2023). 389–409.
3. McMorris, O, Villeneuve, PJ, Su, J, and Jerrett, M. Urban greenness and physical activity in a national survey of Canadians. Environ Res. (2015) 137:94–100. doi: 10.1016/j.envres.2014.11.010
4. Ji, JS, Zhu, A, Bai, C, Wu, C-D, Yan, L, Tang, S, et al. Residential greenness and mortality in oldest-old women and men in China: a longitudinal cohort study. The Lancet Planetary Health. (2019) 3:e17–25. doi: 10.1016/S2542-5196(18)30264-X
5. Pereira, G, Foster, S, Martin, K, Christian, H, Boruff, BJ, Knuiman, M, et al. The association between neighborhood greenness and cardiovascular disease: an observational study. BMC Public Health. (2012) 12:1–9. doi: 10.1186/1471-2458-12-466
6. Wang, J, Ma, Y, Tang, L, Li, D, Xie, J, Hu, Y, et al. Long-term exposure to residential greenness and decreased risk of depression and anxiety. Nature Mental Health. (2024) 2:525–34. doi: 10.1038/s44220-024-00227-z
7. Yang, B-Y, Zhao, T, Hu, L-X, Browning, MH, Heinrich, J, Dharmage, SC, et al. Greenspace and human health: an umbrella review. Innovation. (2021) 2:100164. doi: 10.1016/j.xinn.2021.100164
8. Tsai, H-J, Li, C-Y, Pan, W-C, Yao, T-C, Su, H-J, Wu, C-D, et al. The effect of surrounding greenness on type 2 diabetes mellitus: a nationwide population-based cohort in Taiwan. Int J Environ Res Public Health. (2021) 18:267. doi: 10.3390/ijerph18010267
9. Yu, L, Li, T, Yang, Z, Zhang, X, Xu, L, Wu, Y, et al. Long-term exposure to residential surrounding greenness and incidence of diabetes: a prospective cohort study. Environ Pollut. (2022) 310:119821. doi: 10.1016/j.envpol.2022.119821
10. Wang, H, and Tassinary, LG. Association between greenspace morphology and prevalence of non-communicable diseases mediated by air pollution and physical activity. Landsc Urban Plan. (2024) 242:104934. doi: 10.1016/j.landurbplan.2023.104934
11. Xia, T, Zhao, B, Yu, J, Gao, Y, Wang, X, Mao, Y, et al. Making residential green space exposure evaluation more accurate: a composite assessment framework that integrates objective and subjective indicators. Urban For Urban Green. (2024) 95:128290. doi: 10.1016/j.ufug.2024.128290
12. Jamalishahni, T, Turrell, G, Foster, S, Davern, M, and Villanueva, K. Neighbourhood socio-economic disadvantage and loneliness: the contribution of green space quantity and quality. BMC Public Health. (2023) 23:598. doi: 10.1186/s12889-023-15433-0
13. Choi, GJ, and Kang, H. Introduction to umbrella reviews as a useful evidence-based practice. J Lipid Atheroscler. (2023) 12:3–11. doi: 10.12997/jla.2023.12.1.3
14. World Health Organization. Setting global research priorities for urban health. Geneva: World Health Organization (2022).
15. Hunter, RF, Nieuwenhuijsen, M, Fabian, C, Murphy, N, O'Hara, K, Rappe, E, et al. Advancing urban green and blue space contributions to public health. Lancet Public Health. (2023) 8:e735–42. doi: 10.1016/S2468-2667(23)00156-1
16. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
17. Shea, BJ, Reeves, BC, Wells, G, Thuku, M, Hamel, C, Moran, J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. (2017) 358:j4008. doi: 10.1136/bmj.j4008
18. Guyatt, GH, Oxman, AD, Schünemann, HJ, Tugwell, P, and Knottnerus, A. GRADE guidelines: a new series of articles in the journal of clinical epidemiology. J Clin Epidemiol. (2011) 64:380–2. doi: 10.1016/j.jclinepi.2010.09.011
19. Jia, P, Shi, Y, Jiang, Q, Dai, S, Yu, B, Yang, S, et al. Environmental determinants of childhood obesity: a meta-analysis. Lancet Glob Health. (2023) 11:S7. doi: 10.1016/S2214-109X(23)00092-X
20. Patwary, MM, Dzhambov, A, Disha, AS, Bardhan, M, Haque, MZ, Rahman, MA, et al. Exposure to nature during the COVID-19 pandemic and the associated effect on mental health: a systematic review with meta-analysis. The Lancet Planetary Health. (2022) 6:S20. doi: 10.1016/S2542-5196(22)00282-0
21. Annesi-Maesano, I, Cecchi, L, Biagioni, B, Chung, KF, Clot, B, Collaud Coen, M, et al. Is exposure to pollen a risk factor for moderate and severe asthma exacerbations? Allergy. (2023) 78:2121–47. doi: 10.1111/all.15724
22. Gascon, M, Triguero-Mas, M, Martínez, D, Dadvand, P, Rojas-Rueda, D, Plasència, A, et al. Residential green spaces and mortality: a systematic review. Environ Int. (2016) 86:60–7. doi: 10.1016/j.envint.2015.10.013
23. Lambert, A, Vlaar, J, Herrington, S, and Brussoni, M. What is the relationship between the neighbourhood built environment and time spent in outdoor play? A systematic review. Int J Environ Res Public Health. (2019) 16:3840. doi: 10.3390/ijerph16203840
24. Liu, M, Meijer, P, Lam, TM, Timmermans, EJ, Grobbee, DE, Beulens, JW, et al. The built environment and cardiovascular disease: an umbrella review and meta-meta-analysis. Eur J Prev Cardiol. (2023) 30:1801–27. doi: 10.1093/eurjpc/zwad241
25. Moore, TH, Kesten, JM, López-López, JA, Ijaz, S, McAleenan, A, Richards, A, et al. The effects of changes to the built environment on the mental health and well-being of adults: systematic review. Health Place. (2018) 53:237–57. doi: 10.1016/j.healthplace.2018.07.012
26. Ye, T, Yu, P, Wen, B, Yang, Z, Huang, W, Guo, Y, et al. Greenspace and health outcomes in children and adolescents: a systematic review. Environ Pollut. (2022) 314:120193. doi: 10.1016/j.envpol.2022.120193
27. Bertrand, C, Pascal, M, and Médina, S. Do we know enough to quantify the impact of urban green spaces on mortality? An analysis of the current knowledge. Public Health. (2021) 200:91–8. doi: 10.1016/j.puhe.2021.09.015
28. Rojas-Rueda, D, Nieuwenhuijsen, MJ, Gascon, M, Perez-Leon, D, and Mudu, P. Green spaces and mortality: a systematic review and meta-analysis of cohort studies. The Lancet Planetary Health. (2019) 3:e469–77. doi: 10.1016/S2542-5196(19)30215-3
29. Yuan, Y, Huang, F, Lin, F, Zhu, P, and Zhu, P. Green space exposure on mortality and cardiovascular outcomes in older adults: a systematic review and meta-analysis of observational studies. Aging Clin Exp Res. (2021) 33:1783–97. doi: 10.1007/s40520-020-01710-0
30. Bianconi, A, Longo, G, Coa, AA, Fiore, M, and Gori, D. Impacts of urban green on cardiovascular and cerebrovascular diseases—a systematic review and Meta-analysis. Int J Environ Res Public Health. (2023) 20:5966. doi: 10.3390/ijerph20115966
31. Liu, X-X, Ma, X-L, Huang, W-Z, Luo, Y-N, He, C-J, Zhong, X-M, et al. Green space and cardiovascular disease: a systematic review with meta-analysis. Environ Pollut. (2022) 301:118990. doi: 10.1016/j.envpol.2022.118990
32. Twohig-Bennett, C, and Jones, A. The health benefits of the great outdoors: a systematic review and meta-analysis of greenspace exposure and health outcomes. Environ Res. (2018) 166:628–37. doi: 10.1016/j.envres.2018.06.030
33. Li, F, Liu, W, Hu, C, Tang, M, Zhang, Y, Ho, HC, et al. Global association of greenness exposure with risk of nervous system disease: a systematic review and meta-analysis. Sci Total Environ. (2023) 877:162773. doi: 10.1016/j.scitotenv.2023.162773
34. Tang, M, Liu, W, Li, H, and Li, F. Greenness and chronic respiratory health issues: a systematic review and meta-analysis. Front Public Health. (2023) 11:1279322. doi: 10.3389/fpubh.2023.1279322
35. Li, J, Xie, Y, Xu, J, Zhang, C, Wang, H, Huang, D, et al. Association between greenspace and cancer: evidence from a systematic review and meta-analysis of multiple large cohort studies. Environ Sci Pollut Res. (2023) 30:91140–57. doi: 10.1007/s11356-023-28461-5
36. Sakhvidi, MJZ, Yang, J, Mehrparvar, AH, Dzhambov, AM, Ebrahimi, A, Dadvand, P, et al. Exposure to greenspace and cancer incidence, prevalence, and mortality: a systematic review and meta-analyses. Sci Total Environ. (2022) 838:156180. doi: 10.1016/j.scitotenv.2022.156180
37. Zhang, Y, Wu, T, Yu, H, Fu, J, Xu, J, Liu, L, et al. Green spaces exposure and the risk of common psychiatric disorders: a meta-analysis. SSM-Popul Health. (2024) 25:101630. doi: 10.1016/j.ssmph.2024.101630
38. Zhao, Y-L, Qu, Y, Ou, Y-N, Zhang, Y-R, Tan, L, and Yu, J-T. Environmental factors and risks of cognitive impairment and dementia: a systematic review and meta-analysis. Ageing Res Rev. (2021) 72:101504. doi: 10.1016/j.arr.2021.101504
39. Zagnoli, F, Filippini, T, Jimenez, MP, Wise, LA, Hatch, EE, and Vinceti, M. Is greenness associated with dementia? A systematic review and dose–response Meta-analysis. Curr Environ Health Rep. (2022) 9:574–90. doi: 10.1007/s40572-022-00365-5
40. Dong, S., Braun, D., Wu, X., Yitshak Sade, M., Blacker, D., Kioumourtzoglou, M. A., et al. (2021). The impact of air pollution on mortality risk in the older adults with Alzheimer's disease and related dementias (ADRD). Paper presented at the ISEE Conference Abstracts, 2021.
41. Zhang, Y, Ebelt, ST, Shi, L, Scovronick, NC, D'Souza, RR, Steenland, K, et al. Short-term associations between warm-season ambient temperature and emergency department visits for Alzheimer's disease and related dementia in five US states. Environ Res. (2023) 220:115176. doi: 10.1016/j.envres.2022.115176
42. Bongioanni, P, Del Carratore, R, Corbianco, S, Diana, A, Cavallini, G, Masciandaro, SM, et al. Climate change and neurodegenerative diseases. Environ Res. (2021) 201:111511. doi: 10.1016/j.envres.2021.111511
43. Den Braver, N, Lakerveld, J, Rutters, F, Schoonmade, L, Brug, J, and Beulens, J. Built environmental characteristics and diabetes: a systematic review and meta-analysis. BMC Med. (2018) 16:1–26. doi: 10.1186/s12916-017-0997-z
44. Sharifi, Y, Sobhani, S, Ramezanghorbani, N, Payab, M, Ghoreshi, B, Djalalinia, S, et al. Association of greenspaces exposure with cardiometabolic risk factors: a systematic review and meta-analysis. BMC Cardiovasc Disord. (2024) 24:170. doi: 10.1186/s12872-024-03830-1
45. Luo, YN, Huang, WZ, Liu, XX, Markevych, I, Bloom, MS, Zhao, T, et al. Greenspace with overweight and obesity: a systematic review and meta-analysis of epidemiological studies up to 2020. Obes Rev. (2020) 21:e13078. doi: 10.1111/obr.13078
46. Bu, Y, Zhang, X, Song, S, Su, H, Yu, Z, and Guo, Y. Association of greenspace with hypertension in adult: a systematic review and meta-analysis of epidemiological studies. Int J Environ Health Res. (2024) 34:2556–77. doi: 10.1080/09603123.2023.2259817
47. Patwary, MM, Sakhvidi, MJZ, Ashraf, S, Dadvand, P, Browning, MH, Alam, MA, et al. Impact of green space and built environment on metabolic syndrome: a systematic review with meta-analysis. Sci Total Environ. (2024) 923:170977. doi: 10.1016/j.scitotenv.2024.170977
48. Cao, N-W, Zhou, H-Y, Du, Y-J, Li, X-B, Chu, X-J, and Li, B-Z. The effect of greenness on allergic rhinitis outcomes in children and adolescents: a systematic review and meta-analysis. Sci Total Environ. (2023) 859:160244. doi: 10.1016/j.scitotenv.2022.160244
49. Fuertes, E, Markevych, I, Bowatte, G, Gruzieva, O, Gehring, U, Becker, A, et al. Residential greenness is differentially associated with childhood allergic rhinitis and aeroallergen sensitization in seven birth cohorts. Allergy. (2016) 71:1461–71. doi: 10.1111/all.12915
50. Lambert, K, Bowatte, G, Tham, R, Lodge, C, Prendergast, L, Heinrich, J, et al. Residential greenness and allergic respiratory diseases in children and adolescents–a systematic review and meta-analysis. Environ Res. (2017) 159:212–21. doi: 10.1016/j.envres.2017.08.002
51. Parmes, E, Pesce, G, Sabel, CE, Baldacci, S, Bono, R, Brescianini, S, et al. Influence of residential land cover on childhood allergic and respiratory symptoms and diseases: evidence from 9 European cohorts. Environ Res. (2020) 183:108953. doi: 10.1016/j.envres.2019.108953
52. Wang, X, Zhou, N, and Zhi, Y. Association between exposure to greenness and atopic march in children and adults—a systematic review and meta-analysis. Front Public Health. (2023) 10:1097486. doi: 10.3389/fpubh.2022.1097486
53. Squillacioti, G, Fasola, S, Ghelli, F, Colombi, N, Pandolfo, A, La Grutta, S, et al. Different greenness exposure in Europe and respiratory outcomes in youths. A systematic review and meta-analysis. Environ Res. (2024) 247:118166. doi: 10.1016/j.envres.2024.118166
54. Oh, J-W. Pollen allergy in a changing planetary environment. Allergy Asthma Immunol Res. (2022) 14:168–81. doi: 10.4168/aair.2022.14.2.168
55. Ahmer, Z, Atif, M, Zaheer, S, Adil, O, Shaikh, S, and Shafique, K. Association between residential green spaces and pregnancy outcomes: a systematic review and meta-analysis. Int J Environ Health Res. (2024) 34:3188–205. doi: 10.1080/09603123.2023.2299242
56. Akaraci, S, Feng, X, Suesse, T, Jalaludin, B, and Astell-Burt, T. A systematic review and meta-analysis of associations between green and blue spaces and birth outcomes. Int J Environ Res Public Health. (2020) 17:2949. doi: 10.3390/ijerph17082949
57. Hu, C-Y, Yang, X-J, Gui, S-Y, Ding, K, Huang, K, Fang, Y, et al. Residential greenness and birth outcomes: a systematic review and meta-analysis of observational studies. Environ Res. (2021) 193:110599. doi: 10.1016/j.envres.2020.110599
58. Lee, KJ, Moon, H, Yun, HR, Park, EL, Park, AR, Choi, H, et al. Greenness, civil environment, and pregnancy outcomes: perspectives with a systematic review and meta-analysis. Environ Health. (2020) 19:1–15. doi: 10.1186/s12940-020-00649-z
59. Zhan, Y, Liu, J, Lu, Z, Yue, H, Zhang, J, and Jiang, Y. Influence of residential greenness on adverse pregnancy outcomes: a systematic review and dose-response meta-analysis. Sci Total Environ. (2020) 718:137420. doi: 10.1016/j.scitotenv.2020.137420
60. Bratman, GN, Hamilton, JP, and Daily, GC. The impacts of nature experience on human cognitive function and mental health. Ann N Y Acad Sci. (2012) 1249:118–36. doi: 10.1111/j.1749-6632.2011.06400.x
61. Liu, Z, Chen, X, Cui, H, Ma, Y, Gao, N, Li, X, et al. Green space exposure on depression and anxiety outcomes: a meta-analysis. Environ Res. (2023) 231:116303. doi: 10.1016/j.envres.2023.116303
62. Roberts, H, van Lissa, C, Hagedoorn, P, Kellar, I, and Helbich, M. The effect of short-term exposure to the natural environment on depressive mood: a systematic review and meta-analysis. Environ Res. (2019) 177:108606. doi: 10.1016/j.envres.2019.108606
63. Yao, W, Chen, F, Wang, S, and Zhang, X. Impact of exposure to natural and built environments on positive and negative affect: a systematic review and meta-analysis. Front Public Health. (2021) 9:758457. doi: 10.3389/fpubh.2021.758457
64. Cadman, T, Strandberg-Larsen, K, Calas, L, Christiansen, M, Culpin, I, Dadvand, P, et al. Urban environment in pregnancy and postpartum depression: an individual participant data meta-analysis of 12 European birth cohorts. Environ Int. (2024) 185:108453. doi: 10.1016/j.envint.2024.108453
65. Briggs, R, Morris, PG, and Rees, K. The effectiveness of group-based gardening interventions for improving wellbeing and reducing symptoms of mental ill-health in adults: a systematic review and meta-analysis. J Ment Health. (2023) 32:787–804. doi: 10.1080/09638237.2022.2118687
66. Panțiru, I, Ronaldson, A, Sima, N, Dregan, A, and Sima, R. The impact of gardening on well-being, mental health, and quality of life: an umbrella review and meta-analysis. Syst Rev. (2024) 13:45. doi: 10.1186/s13643-024-02457-9
67. Soga, M, Gaston, KJ, and Yamaura, Y. Gardening is beneficial for health: a meta-analysis. Prev Med Rep. (2017) 5:92–9. doi: 10.1016/j.pmedr.2016.11.007
68. Spano, G, D’Este, M, Giannico, V, Carrus, G, Elia, M, Lafortezza, R, et al. Are community gardening and horticultural interventions beneficial for psychosocial well-being? A meta-analysis. Int J Environ Res Public Health. (2020) 17:3584. doi: 10.3390/ijerph17103584
69. Coventry, PA, Brown, JE, Pervin, J, Brabyn, S, Pateman, R, Breedvelt, J, et al. Nature-based outdoor activities for mental and physical health: systematic review and meta-analysis. SSM-Population Health. (2021) 16:100934. doi: 10.1016/j.ssmph.2021.100934
70. Siah, CJR, Goh, YS, Lee, J, Poon, SN, Ow Yong, JQY, and Tam, WSW. The effects of forest bathing on psychological well-being: a systematic review and meta-analysis. Int J Ment Health Nurs. (2023) 32:1038–54. doi: 10.1111/inm.13131
71. Song, S, Tu, R, Lu, Y, Yin, S, Lin, H, and Xiao, Y. Restorative effects from green exposure: a systematic review and meta-analysis of randomized control trials. Int J Environ Res Public Health. (2022) 19:14506. doi: 10.3390/ijerph192114506
72. Antonelli, M, Barbieri, G, and Donelli, D. Effects of forest bathing (shinrin-yoku) on levels of cortisol as a stress biomarker: a systematic review and meta-analysis. Int J Biometeorol. (2019) 63:1117–34. doi: 10.1007/s00484-019-01717-x
73. Collins, PY, Sinha, M, Concepcion, T, Patton, G, Way, T, McCay, L, et al. Making cities mental health friendly for adolescents and young adults. Nature. (2024) 627:137–48. doi: 10.1038/s41586-023-07005-4
74. Smith, N, Georgiou, M, King, AC, Tieges, Z, Webb, S, and Chastin, S. Urban blue spaces and human health: a systematic review and meta-analysis of quantitative studies. Cities. (2021) 119:103413. doi: 10.1016/j.cities.2021.103413
75. Georgiou, M, Morison, G, Smith, N, Tieges, Z, and Chastin, S. Mechanisms of impact of blue spaces on human health: a systematic literature review and meta-analysis. Int J Environ Res Public Health. (2021) 18:2486. doi: 10.3390/ijerph18052486
76. Ampatzidis, P, and Kershaw, T. A review of the impact of blue space on the urban microclimate. Sci Total Environ. (2020) 730:139068. doi: 10.1016/j.scitotenv.2020.139068
77. Gunawardena, KR, Wells, MJ, and Kershaw, T. Utilising green and bluespace to mitigate urban heat island intensity. Sci Total Environ. (2017) 584-585:1040–55. doi: 10.1016/j.scitotenv.2017.01.158
78. Li, Y, Zhang, J, Schipperijn, J, Tuffier, S, Hyman, S, Bergmann, M, et al. Long-term exposure to green and blue space and incidence of cardiovascular disease: a Danish nurse cohort study. Int J Hyg Environ Health. (2025) 263:114465. doi: 10.1016/j.ijheh.2024.114465
79. Yao, X, Lin, T, Sun, S, Zhang, G, Zhou, H, Jones, L, et al. Greenspace’s value orientations of ecosystem service and socioeconomic service in China. Ecosyst Health Sustain. (2022) 8:2078225. doi: 10.1080/20964129.2022.2078225
80. Ebi, KL, Capon, A, Berry, P, Broderick, C, de Dear, R, Havenith, G, et al. Hot weather and heat extremes: health risks. Lancet. (2021) 398:698–708. doi: 10.1016/S0140-6736(21)01208-3
81. Hoek, G, Krishnan, RM, Beelen, R, Peters, A, Ostro, B, Brunekreef, B, et al. Long-term air pollution exposure and cardio-respiratory mortality: a review. Environ Health. (2013) 12:1–16. doi: 10.1186/1476-069X-12-43
82. Langrish, J, Bosson, J, Unosson, J, Muala, A, Newby, D, Mills, N, et al. Cardiovascular effects of particulate air pollution exposure: time course and underlying mechanisms. J Intern Med. (2012) 272:224–39. doi: 10.1111/j.1365-2796.2012.02566.x
83. Stansfeld, S, Haines, M, Burr, M, Berry, B, and Lercher, P. A review of environmental noise and mental health. Noise Health. (2000) 2:1–8. Avilable at: https://journals.lww.com/nohe/fulltext/2000/02080/a_review_of_environmental_noise_and_mental_health.1.aspx
84. Zaman, M, Muslim, M, and Jehangir, A. Environmental noise-induced cardiovascular, metabolic and mental health disorders: a brief review. Environ Sci Pollut Res. (2022) 29:76485–500. doi: 10.1007/s11356-022-22351-y
85. Münzel, T, Sørensen, M, and Daiber, A. Transportation noise pollution and cardiovascular disease. Nat Rev Cardiol. (2021) 18:619–36. doi: 10.1038/s41569-021-00532-5
86. Coombes, E, Jones, AP, and Hillsdon, M. The relationship of physical activity and overweight to objectively measured green space accessibility and use. Soc Sci Med. (2010) 70:816–22. doi: 10.1016/j.socscimed.2009.11.020
87. Astell-Burt, T, Hartig, T, Eckermann, S, Nieuwenhuijsen, M, McMunn, A, Frumkin, H, et al. More green, less lonely? A longitudinal cohort study. Int J Epidemiol. (2022) 51:99–110. doi: 10.1093/ije/dyab089
88. Gascon, M, Zijlema, W, Vert, C, White, MP, and Nieuwenhuijsen, MJ. Outdoor blue spaces, human health and well-being: a systematic review of quantitative studies. Int J Hyg Environ Health. (2017) 220:1207–21. doi: 10.1016/j.ijheh.2017.08.004
89. Tucker, WJ, Fegers-Wustrow, I, Halle, M, Haykowsky, MJ, Chung, EH, and Kovacic, JC. Exercise for primary and secondary prevention of cardiovascular disease: JACC focus seminar 1/4. J Am Coll Cardiol. (2022) 80:1091–106. doi: 10.1016/j.jacc.2022.07.004
90. Booth, FW, Roberts, CK, and Laye, MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. (2012) 2:1143–211. doi: 10.1002/j.2040-4603.2012.tb00425.x
91. Chang, X, Xu, S, and Zhang, H. Regulation of bone health through physical exercise: mechanisms and types. Front Endocrinol. (2022) 13:1029475. doi: 10.3389/fendo.2022.1029475
92. Sewell, KR, Erickson, KI, Rainey-Smith, SR, Peiffer, JJ, Sohrabi, HR, and Brown, BM. Relationships between physical activity, sleep and cognitive function: a narrative review. Neurosci Biobehav Rev. (2021) 130:369–78. doi: 10.1016/j.neubiorev.2021.09.003
93. Fuller, RA, Irvine, KN, Devine-Wright, P, Warren, PH, and Gaston, KJ. Psychological benefits of greenspace increase with biodiversity. Biol Lett. (2007) 3:390–4. doi: 10.1098/rsbl.2007.0149
94. Chen, Z, Dazard, J-E, Khalifa, Y, Motairek, I, Al-Kindi, S, and Rajagopalan, S. Artificial intelligence–based assessment of built environment from Google street view and coronary artery disease prevalence. Eur Heart J. (2024) 45:1540–9. doi: 10.1093/eurheartj/ehae158
95. Kabisch, N. The influence of socio-economic and socio-demographic factors in the association between urban green space and health In: Biodiversity and health in the face of climate change. Editors. M Marselle, J Stadler, H Korn, K Irvine, and A Bonn. Cham: Springer (2019). 91–119. doi: 10.1007/978-3-030-02318-8_5
96. Gavrilidis, AA, Zakerhaghighi, K, Popa, AM, Akbarian, SZ, Onose, DA, Grădinaru, SR, et al. Perceptions of cultural ecosystem services provision by small public urban green spaces: perspectives from different cultural backgrounds. Urban Ecosyst. (2024) 27:699–716. doi: 10.1007/s11252-023-01480-3
97. De La Iglesia Martinez, A, and Labib, S. Demystifying normalized difference vegetation index (NDVI) for greenness exposure assessments and policy interventions in urban greening. Environ Res. (2023) 220:115155. doi: 10.1016/j.envres.2022.115155
98. Jimenez, RB, Lane, KJ, Hutyra, LR, and Fabian, MP. Spatial resolution of normalized difference vegetation index and greenness exposure misclassification in an urban cohort. J Expo Sci Environ Epidemiol. (2022) 32:213–22. doi: 10.1038/s41370-022-00409-w
99. Holland, I, DeVille, NV, Browning, MH, Buehler, RM, Hart, JE, Hipp, JA, et al. Measuring nature contact: a narrative review. Int J Environ Res Public Health. (2021) 18:4092. doi: 10.3390/ijerph18084092
100. Cadenasso, ML, Pickett, ST, and Schwarz, K. Spatial heterogeneity in urban ecosystems: reconceptualizing land cover and a framework for classification. Front Ecol Environ. (2007) 5:80–8. doi: 10.1890/1540-9295(2007)5[80:SHIUER]2.0.CO;2
101. Fan, S, Feng, W, Zhou, Z, Guo, Y, Xue, Z, Yuan, J, et al. (2022). Association between residential greenness and overweight/obesity among rural adults in northwestern China. Environmental research, 204:112358.
Keywords: green spaces, blue spaces, human health, human settlements, umbrella review
Citation: Wang X, Feng B and Wang J (2025) Green spaces, blue spaces and human health: an updated umbrella review of epidemiological meta-analyses. Front. Public Health. 13:1505292. doi: 10.3389/fpubh.2025.1505292
Edited by:
Paolo Vineis, Imperial College London, United KingdomReviewed by:
Amelie Y. Davis, United States Air Force Academy, United StatesAbdullah Addas, King Abdulaziz University, Saudi Arabia
Mian Yang, Sichuan Tourism University, China
Copyright © 2025 Wang, Feng and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Juan Wang, d2FuZ2p1YW5AY2R1dC5lZHUuY24=
†These authors have contributed equally to this work
 XiaoWen Wang1†
XiaoWen Wang1† Bowen Feng
Bowen Feng