- 1Department of Epidemiology, University Medical Center Groningen, University of Groningen, Groningen, Netherlands
- 2Department of Health Sciences, Applied Health Research, University Medical Center Groningen, University of Groningen, Groningen, Netherlands
- 3Department of Health Sciences, Community and Occupational Medicine, University Medical Center Groningen, University of Groningen, Groningen, Netherlands
- 4Department of Public Health and Primary Care, Environment and Health, KU Leuven, Leuven, Belgium
Background: Low socioeconomic position (SEP) increases the risk of health inequalities. Understanding how to realize lifestyle improvements in groups with low SEP may offer routes to reduce these inequalities, and information from professionals involved in this target can support this. Our aims were to gain insight into the professionals’ perspectives on factors that influence the lifestyle of individuals with low SEP, and to identify promising approaches to reduce health inequalities.
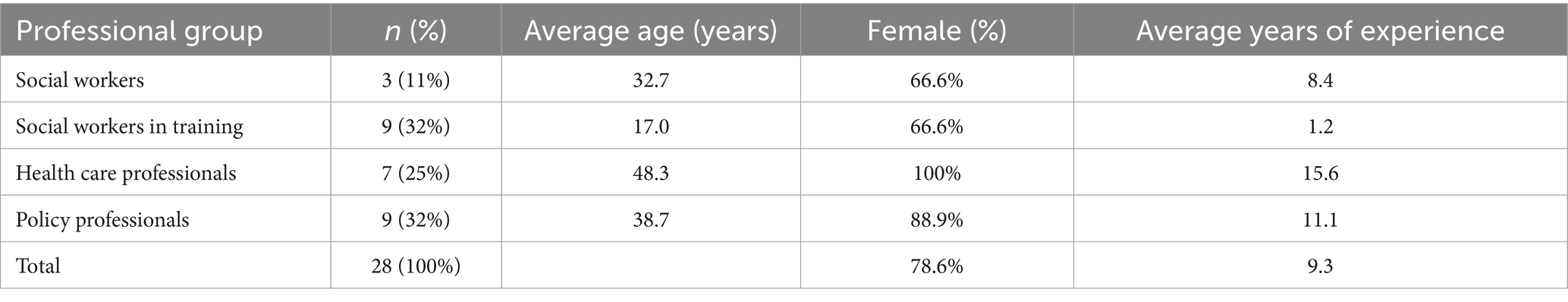
Methods: Focus group interviews and semi-structured interviews were conducted with 28 social workers (partially in training), health care and policy professionals. All interviews were audio recorded, transcribed verbatim, and analysed following thematic analysis.
Results: Four themes emerged from the data: individual factors, accumulating problems, social context and societal factors; for the second aim a fifth theme emerged: involvement of individuals with low SEP. Participants also indicated a hierarchy in these themes. Addressing accumulating multi-faceted issues such as poverty is imperative before a more healthy lifestyle can be adopted and individuals can focus on skills needed to achieve a healthy lifestyle. Additionally, the social context (e.g., parents or neighbours) can play a supportive role in lifestyle change, supported by government and with active involvement of low SEP individuals.
Conclusion: According to the professionals, to help individuals with low SEP to realize a healthier lifestyle, poverty, knowledge and skills, and the involvement of a person’s social context and society should be addressed.
Introduction
Socioeconomic inequalities in many health outcomes are large and persistent (1). Individuals with low socioeconomic position (SEP) often have a more unhealthy lifestyle than their higher SEP counterparts; they more often smoke, have an unhealthier diet, have worse sleeping habits, and are less physically active during leisure time (2, 3). An unhealthy lifestyle is in turn related to both adverse physical and mental health outcomes (4, 5). Given that lifestyle is potentially modifiable, it is important to understand how to improve lifestyle in individuals with low SEP in order to reduce SEP inequalities.
Several factors contribute to the unhealthy lifestyles of individuals with low SEP, including specific attitudes, non-supportive social norms, and insufficient self-efficacy, beliefs, and skills to maintain a healthy lifestyle (6–9). Low SEP individuals may feel less inclined to seek lifestyle advice due to challenges in their daily life, such as financial struggles and relationship issues (10–13). They also rely more on social support for making healthy choices (10). Upstream factors, like immediate crises related to their socioeconomic status, often take precedence over long-term health concerns (14). Understanding both upstream and downstream factors is crucial for addressing lifestyle changes in this group. Despite previous intervention efforts, reducing health inequalities has been challenging (15–17). Evidence from qualitative research may help to obtain a comprehensive understanding of why low SEP individuals lead unhealthier lives and how they can be supported in adopting healthier lifestyles.
The Social Determinants of Health model provides a framework for understanding the broader structural influences on lifestyle behaviors in individuals with a low SEP. The model highlights how factors such as income, education, employment, housing, and access to healthcare shape health outcomes and contribute to persistent health inequalities (18). Research has shown that these determinants influence lifestyle choices, as limited resources, adverse living conditions and health literacy can create barriers to healthy behaviors (19, 20). Addressing these determinants is pivotal for developing effective health promotion strategies that go beyond individual behavior change and incorporate systemic and policy-level interventions. (19, 20).
Reaching individuals with low SEP and supporting a healthier lifestyle may be more successful by tailored approaches (21). Several studies showed that, instead of following the standard principles of health promotion, attention should be paid to the capacities (e.g., abilities, resources and potential) of individuals with low SEP (12, 21–24). Furthermore, their social context should also be (more) involved to help them make lifestyle changes (8, 10, 11, 25–27). To achieve change it is important to understand which factors influence lifestyle, and how professionals closely involved with these individuals at neighbourhood level believe that change should be approached based on their personal experiences with the target group.
This study aims to explore professionals’ perspectives on implementing lifestyle promotion for low SEP individuals, on which evidence is scarce as yet. These professionals possess valuable expertise in this field. The qualitative study seeks insights from social workers, trainee social workers, healthcare, and policy professionals on (1) lifestyle influencers in low SEP individuals and (2) effective strategies for promoting healthy lifestyles in this group.
Methods
A qualitative exploratory research design, grounded in a constructivist paradigm (28), was used. This paradigm assumes that reality is socially constructed and shaped by interactions and experiences, making it suitable for exploring professionals’ perspectives on lifestyle promotion among low SEP individuals. In this qualitative study we used semi-structured interviews and focus group interviews to explore the views of professionals regarding factors influencing lifestyle, and potential preventive approaches to offer to individuals with low SEP. We used the Consolidated Criteria for Reporting Qualitative Health Research (COREQ) (29) (see Supplementary Table 1).
Study context
Our study was conducted in the Netherlands, where socioeconomic health inequalities remain a persistent challenge, despite a relatively well-developed social security system. Individuals with low SEP often experience multiple disadvantages, including financial instability, limited access to healthcare, and higher exposure to unhealthy living conditions (30). Dutch public health policies emphasize preventive care and lifestyle interventions, yet reaching and effectively supporting low SEP groups remains difficult (31–33). Professionals working in healthcare, social work, and policymaking play a role in bridging this gap by implementing tailored lifestyle interventions. Their perspectives provide valuable insights into the structural and behavioral challenges that low SEP individuals face, as well as effective strategies for promoting healthier lifestyles in this population (30–33).
Participants
We aimed at including professionals who work with low SEP individuals as proxy informants, considering the COVID-19 crisis during our recruitment period to block inclusion of low SEP individuals. These professionals have proximity to and insight in the target group and on top can also help bridge the gap between practice and research, making them key figures in translating insights from practice to science. Participants were recruited for one-time involvement through the networks of the Collaborative Research Center on Public Health in the Northern Netherlands, and through networks of the researchers involved in this study. To ensure rigor in participant selection, we employed a purposeful sample strategy, aiming for maximum variation in professional background, experience level, and roles in working with low SEP individuals. We included four types of professionals: social workers (n = 3), social workers in training, partially also coming from low SEP households themselves (n = 9), health care professionals (n = 7), and policy professionals (n = 9). Table 1 presents key characteristics of the participants. All included participants had work activities related to and contact with individuals with low SEP, often living in poverty. Ethical approval for the study was obtained from the Medical Ethics Committee of the University Medical Center Groningen. Participants received written information about the procedure and a short questionnaire on their age, sex, employer, occupation, and their low SEP target group (children, adolescents, adults, or the older adults). All recruited individuals participated in the study. We ensured ethical integrity by obtaining written informed consent from all participants, safeguarding confidentiality through anonymized data handling, and adhering to the Helsinki standards on health research. All participants gave written informed consent and received a gift voucher of 20 euros for their participation.
Data collection
We collected data in three phases using an iterative process, meaning that information from the previous phase was carried over into the next phase. First, we conducted a semi-structured interview with a policy professional, and a focus group interview with social workers in training. Second, we conducted focus group interviews with health care professionals and policy professionals. Third, we conducted semi-structured interviews with social workers to validate results from the previous phases.
We developed interview guides for the semi-structured interviews and focus group interviews based on results from quantitative analyses, which are elaborated upon in Appendix A. These analyses were conducted using data from the Lifelines Cohort and Biobank Study, a large multidisciplinary cohort study in the northern Netherlands that examines health and health-related behaviors across multiple generations (34). The quantitative analysis applied mediation techniques, i.e., the Karlson-Holm-Breen (KHB) method (35), to examine the role of lifestyle and psychosocial factors in explaining socioeconomic inequalities in health outcomes metabolic syndrome (MetS) and major depressive disorder (MDD).
The interview guides were further based on the Integrated Model for Behavioural Change (i-Change model) (36), and on the Social Determinants of Health model (18). According to the i-Change model, behavior is determined by an individual’s motivation and intention. The model integrates the ideas of the Social Cognitive Theory, the Health Belief Model, Theory of Planned Behavior, the Trans-Theoretical Model, and Goal Setting Theory (37–41). The model proposes that a person’s behavior is determined by awareness, knowledge, attitudes, subjective norms, self-efficacy, and intention (36). According to the Social Determinants of Health Model, an individual’s behavior and health are determined by economic stability, education access and quality, health care access and quality, neighbourhood and built environment, and social and community context (18). The interview guide as used in phase one – for the policy professional and social workers in training – focused on awareness, motivation and intentions to have a healthy lifestyle (Appendix B).
The interview guide as used in phase two – for the health care professionals and policy professionals – also contained questions regarding approaches toward encouraging individuals with low SEP to adopt a healthy lifestyle (Appendix C). The interviews in phase three, with social workers, were aimed to deepen the information from the previous phases (Appendix D). To enhance rigor, we ensured consistency in data collection through a structured protocol, as well as an iterative process of data collection and analysis, implying that the findings are credible, reproducible, and not unduly influenced by individual interviewer bias. The results of the quantitative analysis informed the development of the interview guides by identifying key explanatory factors, such as education, health literacy, and social contacts in health disparities. The qualitative study was then used to explore the mechanisms behind these associations in more depth, allowing for a richer understanding of the lived experiences and perspectives of the target populations. Data collection was continued until data saturation was reached.
All focus group interviews lasted 2 h; the semi-structured interviews lasted 1 to 1.5 h and took online place via Microsoft Teams due to COVID restrictions, except for the focus group interview with social workers in training, which took place face-to-face. An experienced qualitative researcher (JAL, female health scientist [PhD]) moderated the focus group interviews, and a PhD student (LAH, female health scientist [MSc]) observed the focus group interviews and conducted the semi-structured interviews. Researchers and participants had not met before the interviews took place. Some participants knew each other beforehand. All interviews were conducted between October 2021 and February 2022.
Data analysis
The interviews were audiotaped and transcribed verbatim. To ensure credibility, we maintained a reflexive logbook to document analytical decisions and enhance transparency. We used a thematic analysis approach as described by Braun and Clarke (42). To strengthen dependability and confirmability, we utilized investigator triangulation, with multiple researchers independently coding transcripts and discussing discrepancies. This process served as a form of cross-validation, ensuring that interpretations were not solely dependent on a single researcher’s perspective. First, two researchers (LAH and MAA, female health scientist [PhD]) read all transcripts individually and noted initial ideas. Second, we generated initial codes, performing systematic, line-by-line analysis of the transcripts, using Atlas.ti (version 9). Third, we organized these codes into preliminary themes related to influencing factors and approaches to decrease SEP lifestyle inequalities. Fourth, we reviewed themes in relation to the coded extracts and the entire data set, generating a ‘thematic map’. To ensure trustworthiness, we applied investigator triangulation by discussing emerging themes with multiple researchers involved in the study, incorporating diverse perspectives for cross-validation (42) To maximize dependability and reduce bias, we used an iterative team approach involving group discussion to group codes into themes (LAH, MAA, UB female health scientist [PhD], and MLAdK, female health scientist [MD, PhD]). Fifth, we refined and reviewed the initial coding framework and corresponding themes to ensure coding and theming were structured, and consistent with the research aims. Sixth, we reported and selected illustrative quotes, which were translated by a native speaker.
Results
Descriptive of the sample
The study included 28 professionals, with an average of 9.3 years of experience (Table 1). They were divided into four groups: social workers (11%), social workers in training (32%), health care professionals (25%), and policy professionals (32%). The average ages for these groups were 32.7, 17.0, 48.3, and 38.7, respectively. The majority of social workers and those in training were female (66.6%), while 88.9% of policy professionals and all health care professionals were female.
Realizing a healthy lifestyle in individuals with low SEP
The analysis revealed five themes: (1) Individual factors, (2) Accumulating problems, (3) Social context (parents, peers, neighbours), (4) Societal factors (government), and (5) Involvement of low-SEP individuals. Themes 1–4 address both influencing factors of an unhealthy lifestyle and approaches for a healthy one, while theme 5 pertains solely to approaches. All quotations referenced in brackets (e.g., Q1.1, Q2.3) refer to Table 2.
Theme 1: individual factors
Influencing factors
Participants emphasized various individual factors affecting the healthy lifestyle of low-SEP individuals, including awareness, knowledge, risk perception, habits, attitudes, self-efficacy, and skills. While low-SEP individuals possess basic knowledge about health and risks (Table 2, Q1.1), their attitudes toward a healthy lifestyle are often negative. They tend to prioritize immediate concerns over long-term health risks, like smoking and excessive drinking, which become ingrained habits (Q1.2). Many participants believed these individuals lacked determination, perseverance, self-efficacy, or discipline to adopt and maintain a healthy lifestyle (Q1.3). Additionally, these individuals often live day-to-day and have other priorities besides health risks (Q1.4).
Approaches
Regarding individual factors, participants stressed the need for education to enhance knowledge, awareness, risk perception, and self-efficacy in lifestyle choices. This education should cover healthy behavior and the risks of unhealthy choices, potentially starting in primary school (Q1.5). Some suggested beginning during adolescence when young individuals make their own choices. However, caution was advised against involving children in educating their parents, as it might lead to unhealthy compensatory behaviors (Q1.6).
Participants cautioned against assuming that adults with low SEP wish to become healthier or lack knowledge about healthy living. They advocated addressing other stressors like work, income, housing, and finances before promoting a healthy lifestyle. Emphasizing the consequences of an unhealthy lifestyle and the potential for change was deemed important (Q1.7).
Effective knowledge transfer to low-SEP individuals was emphasized. They often rely on others and social media for information. Brief, self-implemented knowledge transfer may not suffice; combining it with activities and repetition can help individuals apply knowledge and develop skills (Q1.8).
Theme 2: accumulating problems
Influencing factors
All participants acknowledged that various challenges hinder low-SEP individuals from leading healthy lives. These obstacles include low societal participation, unemployment, meagre income, poverty, addiction, mental health issues, and financial and housing-related stress (Q2.1). They stressed the importance of societal participation, which can provide income and a future outlook necessary for adopting a healthy lifestyle (Q2.2).
Poverty and financial stress negatively impact lifestyle choices, leading to avoidance of healthcare, smoking for relaxation, and purchasing less healthy food due to affordability (Q2.3). Furthermore, participants emphasized that parental poverty significantly affects children’s health, limiting their access to sports activities due to financial constraints (Q2.4). These issues often coexist and demand considerable effort to address, leaving individuals with little time or energy to improve their lifestyle.
Approaches
Participants stressed the need for an integrated approach to address the complex issues faced by low-SEP individuals, emphasizing coherence and cross-domain collaboration (Q2.5). They advocated prioritizing individuals’ life goals and providing a path to achieving them, aligning with the “positive health” approach (43) (Q2.6).
To tackle these accumulating problems, participants called for collaboration across different domains like social care and policy. Health care professionals should refer patients to social workers and local networks more frequently. They also recommended improving the knowledge of care providers about appropriate referrals for issues outside their domain. Government intervention to foster greater collaboration between domains was seen as essential for more impactful results (Q2.7).
Theme 3: social context
Influencing factors
Social influences shape an individual’s lifestyle from childhood. Parents play a pivotal role, positively or negatively impacting their children’s habits (Q3.1). As kids grow, peers become influential, sometimes positively, like warning against excessive alcohol or drug use.
In adulthood, partners have a significant impact on lifestyle. A negative view or the end of a relationship can lead to unhealthy behaviors like alcohol addiction (Q3.1). The social network in one’s neighbourhood or village is also crucial. It can combat loneliness, often linked to substance abuse (Q3.2).
Approaches
Participants stressed the importance of supporting parents in promoting a healthy lifestyle for their children. This could involve involving them in lifestyle-themed events at school or in the community centre. However, they cautioned against giving unsolicited advice, as it might backfire, causing parents to reject the health message (Q3.3).
To create a supportive social context for a healthy lifestyle, participants recommended connecting individuals through volunteer initiatives and role models within the community. Collaboration between the social, healthcare, and community sectors was seen as valuable. Additionally, organizers should actively invite individuals to neighbourhood activities (Q3.4).
Theme 4: societal factors
Influencing factors
Participants highlighted societal factors contributing to an unhealthy lifestyle among low-SEP individuals. In the Netherlands, policies emphasize individual initiative and responsibility, potentially widening inequality (Q4.1). Schools and professionals also influence lifestyles, although one participant, a social worker, believed healthy living should be the parents’ responsibility, not schools’ (Q4.2).
Approaches
Participants emphasized the societal responsibility to address the lifestyle and health of low-SEP individuals. They suggested several actions:
1. Assess available resources and best practices for improving their lifestyles (Q4.3).
2. Schools should regulate products, implement anti-smoking policies, provide information, model healthy behavior, and offer more physical activity opportunities (Q4.3).
3. Society should make healthy choices more accessible through measures like VAT reduction on fruits and vegetables and a “sugar tax.” Simplifying healthcare access is also crucial (Q4.4).
4. Municipalities should initiate efforts to reduce health disparities. However, participants noted challenges such as bureaucratic obstacles and limited financial resources (Q4.5).
Theme 5: involvement of individuals with low SEP
Approaches
Participants emphasized the importance of involving individuals in lifestyle change:
1. Tailor the message to each person, requiring professionals to be trained in working with low-SEP individuals (Q5.1).
2. Start involvement early, targeting adolescents who are receptive to change and breaking generational patterns (Q5.2).
3. Engage the target group in developing and implementing interventions to foster a sense of ownership (Q5.3).
4. Begin by understanding the individual’s priorities (Q5.4).
5. Ensure clear and understandable instructions in interventions, avoiding a pedantic approach. Allow more time for information processing and more frequent meetings (Q5.5).
Discussion
Using the i-Change model (36) and the Social Determinants of Health model (18) we identified several themes regarding the realization of a healthy lifestyle in individuals with low SEP at both individual and societal levels: individual factors, accumulating problems, social context, societal factors, and involvement of individuals with low SEP. By integrating these theoretical models, we provide a structured understanding of the complex interplay between personal, social, and structural determinants of health.
Individual factors
Our study shows that individuals with low SEP are influenced by various factors, including awareness, risk perception, self-efficacy, knowledge, attitudes, and habits, when it comes to leading a healthy lifestyle (9). This aligns with previous qualitative and quantitative research, which highlighted the impact of factors like lack of knowledge, risk perception, positive attitudes, negative personality traits, and low health literacy on their dietary and physical activity choices (44, 45).
Participants in our study, consistent with existing research, expressed concern regarding the motivation of individuals with low SEP to adopt a healthy lifestyle. They emphasized the importance of training professionals working with this population. This concern mirrors the broader sentiments of professionals working with disadvantaged communities (46). To address these issues, it is essential to move beyond individual behavioral approaches and incorporate structural interventions, such as regulatory policies on unhealthy food marketing, urban planning for accessible green spaces, or financial incentives for healthy lifestyles, that target social determinants of health (14). Such approaches can facilitate the connection between individual-level challenges, accumulating problems, and the social context. Furthermore, training should focus on tailoring healthy lifestyle messages to the specific needs of low SEP individuals (12, 22) and developing interventions that consider their knowledge, risk perception, and attitudes, allowing for more effective adaptation of interventions and health messages.
Accumulating problems
Accumulating problems, like low income, poor housing, and unemployment, are significant barriers to healthy lifestyle adoption. This aligns with prior research, which highlighted similar challenges including high costs, financial stress, and time constraints (10, 12, 13). Participants in our study also noted poor housing and working conditions (47), along with chronic stress related to relationships, finances, and work, in line with quantitative findings (47, 48).
A key implication of our findings is the necessity for integrated, community-based interventions that address multiple accumulating problems simultaneously. Policies aimed at improving housing, financial security, and employment opportunities should be seen as essential components of lifestyle interventions rather than separate domains. Participants emphasized an integrated approach involving collaboration between social, policy-making, and healthcare domains to address accumulating problems (49). This aligns with the concept of ‘positive health’ that encourages adaptability and self-management when working with individuals with low SEP (43).
Social context
The home environment, peers, partners, and neighbourhood significantly influence lifestyle habits and promotion in individuals with low SEP (9, 13). Qualitative studies have highlighted the positive impact of the social context on supporting a healthy lifestyle (10, 11, 27). However, a quantitative study revealed that low SEP individuals often experience isolation, emphasizing the importance of involving the neighbourhood’s social network (50).
Addressing the social context, it’s important to educate low SEP parents to encourage healthy lifestyles for their children (25, 26). Active parental involvement and considering parents’ personalities are key. Additionally, addressing isolation, a common issue among low SEP individuals, is essential (50). Community-driven interventions, including social support groups and peer mentorship programs, could enhance social cohesion and facilitate healthier behaviors in low SEP populations.
Societal factors
Participants highlighted societal barriers, including the lack of initiative, responsibility, and direction, contributing to unhealthy lifestyles among low SEP individuals. This aligns with prior research (9, 51). According to participants, government and policymakers should assume a more significant role in supporting low SEP individuals. In particular, urban health equity must be prioritized, ensuring that individuals in low SEP communities have equal access to green spaces, affordable healthy food options, low exposures to pollution, and safe recreational areas. For example, the Dutch government could take the lead in organizing care to promote lifestyle changes and implementing policies to encourage a healthy lifestyle (52). While existing policies on healthy lifestyles are in place, they are considered inadequate (53). Our findings suggest that health-promoting policies should extend beyond healthcare settings to include urban planning, education, and social services, fostering a comprehensive approach to health equity.
Involvement of individuals with low SEP
Participants emphasized the importance of tailored, well-considered health messages, early involvement, and personal guidance. This aligns with prior research, highlighting the need for comprehensive, culturally sensitive support, prioritizing goal-setting over mere information provision (12, 22, 23). Co-creation of interventions with individuals from low SEP backgrounds is important to ensure their relevance and effectiveness.
Strengths and limitations
A major strength of this study is that we explored not only factors influencing lifestyle choices among groups with low SEP, but also approaches by professionals closely involved with the target population for replacing unhealthy lifestyles with healthy ones. The credibility of the findings was enhanced by using an iterative process, different qualitative methods, and the use of a team approach for analysing the results. We were able to identify multidisciplinary perspectives by including different professionals, thereby increasing the robustness and transferability of the results. Furthermore, we reached data saturation, indicating that all major aspects are likely to have been identified. Our study also has some limitations. We cannot rule out the possibility of selection bias, as only the most interested participants may have participated in our study. These participants may also have been professionals very committed to the well-being of the individuals with low SEP, possibly feeling sorry for the individuals and making the issues worse. Information bias may also have occurred, with participants, themselves coming from a low SEP household, speaking from their own experience, and not just from that of the individuals they are currently working with.
Implications
Our results have practical, policy, and government implications. We’ve identified factors and approaches to enhance lifestyles for low SEP individuals from a multidisciplinary perspective. Collaboration among professionals in healthcare, policy-making, and social domains is crucial. In particular, our study highlights the need for stronger intersectoral policies that integrate health and social care services to create a more supportive environment for individuals with low SEP. Governments should allocate more resources to address fundamental low SEP issues, using measures like sugar taxes, VAT reductions on healthy foods, and anti-smoking zones. Cross-domain expertise can streamline the resolution of accumulating problems. Further research should prioritize quantitative approaches to assess the impact of previously unstudied factors, such as government regulations, on reducing SEP health inequalities. Moreover, while this study was in the Netherlands, its generalizability may vary in different contexts.
Conclusion
To our best knowledge this study is the first on the professionals’ views regarding lifestyle promotion in individuals with low SEP. Our findings indicate that professionals emphasize the need for a positive, integrated approach in addressing the accumulation of problems in this population. Additionally, the findings highlight the necessity for more elaborate governmental initiatives at both the individual and societal levels to support the adoption of a healthy lifestyle among individuals with low SEP. Moreover, individuals with low SEP should be involved more intensively in the development of interventions. Our findings also underscore the importance of urban health equity, particularly access to health-promoting environments, as a key priority for future interventions and policy measures. This study demonstrates that multiple factors must be addressed simultaneously to ensure the success of a healthy lifestyle intervention or strategy. Further research should explore the effectiveness of specific policy measures and intervention strategies to improve health outcomes in this population.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Medical Ethics Committee of University Medical Center Groningen. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LH: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. MA: Data curation, Formal analysis, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. JL-D: Writing – original draft, Writing – review & editing. NS: Writing – original draft, Writing – review & editing. SR: Writing – original draft, Writing – review & editing. UB: Writing – original draft, Writing – review & editing. MK: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Netherlands Organization for Health Research and Development (ZonMw) [grant number 531003011]. ZonMw had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1511317/full#supplementary-material
References
1. Mackenbach, JP, Stirbu, I, Roskam, AJR, Schaap, MM, Menvielle, G, Leinsalu, M, et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. (2008) 358:2468–81. doi: 10.1056/NEJMsa0707519
2. Coenen, P, Huysmans, MA, Holtermann, A, Troiano, R, Mork, PJ, Krokstad, S, et al. Can socioeconomic health differences be explained by physical activity at work and during leisure time? Rationale and protocol of the active worker individual participant meta-analysis. BMJ Open. (2018) 8:e023379. doi: 10.1136/bmjopen-2018-023379
3. Beenackers, MA, Kamphuis, CBM, Giskes, K, Brug, J, Kunst, AE, Burdorf, A, et al. Socioeconomic inequalities in occupational, leisure-time, and transport related physical activity among European adults: a systematic review. Int J Behav Nutr Phys Act. (2012) 9:116. doi: 10.1186/1479-5868-9-116
4. Barbaresko, J, Rienks, J, and Nöthlings, U. Lifestyle indices and cardiovascular disease risk: a Meta-analysis. Am J Prev Med. (2018) 55:555–64. doi: 10.1016/j.amepre.2018.04.046
5. Sarris, J, O’Neil, A, Coulson, CE, Schweitzer, I, and Berk, M. Lifestyle medicine for depression. BMC Psychiatry. (2014) 14:107. doi: 10.1186/1471-244X-14-107
6. Sheeran, P, Maki, A, Montanaro, E, Avishai-Yitshak, A, Bryan, A, Klein, WMP, et al. The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: a meta-analysis. Health Psychol. (2016) 35:1178–88. doi: 10.1037/hea0000387
7. Abel, T. Cultural capital and social inequality in health. J Epidemiol Community Health (1978). (2008) 62:e13–3. doi: 10.1136/jech.2007.066159
8. Romeike, K, Abidi, L, Lechner, L, de Vries, H, and Oenema, A. Similarities and differences in underlying beliefs of socio-cognitive factors related to diet and physical activity in lower-educated Dutch, Turkish, and Moroccan adults in the Netherlands: a focus group study. BMC Public Health. (2016) 16:813. doi: 10.1186/s12889-016-3480-4
9. Gillies, C, Super, S, te Molder, H, de Graaf, K, and Wagemakers, A. Healthy eating strategies for socioeconomically disadvantaged populations: a meta-ethnography. Int J Qual Stud Health Well-being. (2021) 16. doi: 10.1080/17482631.2021.1942416
10. Withall, J, Jago, R, and Fox, KR. Why some do but most don’t. Barriers and enablers to engaging low-income groups in physical activity programmes: a mixed methods study. BMC Public Health. (2011) 11:507.
11. Bukman, AJ, Teuscher, D, Feskens, EJM, van Baak, MA, Meershoek, A, and Renes, RJ. Perceptions on healthy eating, physical activity and lifestyle advice: opportunities for adapting lifestyle interventions to individuals with low socioeconomic status. BMC Public Health. (2014) 14:1036. doi: 10.1186/1471-2458-14-1036
12. Faber, JS, Al-Dhahir, I, Reijnders, T, Chavannes, NH, Evers, AWM, Kraal, JJ, et al. Attitudes toward health, healthcare, and eHealth of people with a low socioeconomic status: a community-based participatory approach. Front Digit Health. (2021) 3:3. doi: 10.3389/fdgth.2021.690182
13. van der Heijden, A, te Molder, H, Jager, G, and Mulder, BC. Healthy eating beliefs and the meaning of food in populations with a low socioeconomic position: a scoping review. Appetite. (2021) 161:105135. doi: 10.1016/j.appet.2021.105135
14. Ray, R, Lantz, PM, and Williams, D. Upstream policy changes to improve population health and health equity: a priority agenda. Milbank Q. (2023) 101:20–35. doi: 10.1111/1468-0009.12640
16. Wijtzes, AI, van de Gaar, VM, van Grieken, A, de Kroon, MLA, Mackenbach, JP, van Lenthe, FJ, et al. Effectiveness of interventions to improve lifestyle behaviors among socially disadvantaged children in Europe. Eur J Pub Health. (2017) 27:240–7. doi: 10.1093/eurpub/ckw136
17. Kornet-van der Aa, DA, Altenburg, TM, Randeraad-van, V, der Zee, CH, and MJM, C. The effectiveness and promising strategies of obesity prevention and treatment programmes among adolescents from disadvantaged backgrounds: a systematic review. Obes Rev. (2017) 18:581–93. doi: 10.1111/obr.12519
18. Office of Disease Prevention and Health Promotion. Healthy People 2030 Framework. Available online at: https://odphp.health.gov/healthypeople. (2018).
19. Marmot, M. Social determinants of health inequalities. Lancet. (2005) 365:1099–104. doi: 10.1016/S0140-6736(05)71146-6
20. Adler, NE, and Newman, K. Socioeconomic disparities in health: pathways and policies. Health Aff. (2002) 21:60–76. doi: 10.1377/hlthaff.21.2.60
21. Noar, SM, Benac, CN, and Harris, MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. (2007) 133:673–93. doi: 10.1037/0033-2909.133.4.673
22. Coveney, J. A qualitative study exploring socio-economic differences in parental lay knowledge of food and health: implications for public health nutrition. Public Health Nutr. (2005) 8:290–7.
23. Heikkinen, H, Patja, K, and Jallinoja, P. Smokers’ accounts on the health risks of smoking: why is smoking not dangerous for me? Soc Sci Med. (2010) 71:877–83. doi: 10.1016/j.socscimed.2010.05.036
24. Hawkins, RP, Kreuter, M, Resnicow, K, Fishbein, M, and Dijkstra, A. Understanding tailoring in communicating about health. Health Educ Res. (2008) 23:454–66. doi: 10.1093/her/cyn004
25. Norman, Å, Nyberg, G, Elinder, LS, and Berlin, A. Parental strategies for influencing the diet of their children – a qualitative study from disadvantaged areas. Appetite. (2018) 125:502–11. doi: 10.1016/j.appet.2018.03.002
26. Williams, LK, Veitch, J, and Ball, K. What helps children eat well? A qualitative exploration of resilience among disadvantaged families. Health Educ Res. (2011) 26:296–307. doi: 10.1093/her/cyr004
27. Teuscher, D, Bukman, AJ, van Baak, MA, Feskens, EJM, Renes, RJ, and Meershoek, A. Challenges of a healthy lifestyle for socially disadvantaged people of Dutch, Moroccan and Turkish origin in the Netherlands: a focus group study. Crit Public Health. (2015) 25:615–26. doi: 10.1080/09581596.2014.962013
29. Tong, A, Sainsbury, P, and Craig, J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
31. National Institute for Public Health and the Environment (RIVM). Desk for healthy living [in Dutch].
32. National Institute for Public Health and the Environment (RIVM). National Agreement on prevention [in Dutch]. Bilthoven: RIVM (2018).
33. Statistics Netherlands (CBS). Lifestyle and (preventive) health research; personal characteristics [in Dutch].
34. Scholtens, S, Smidt, N, Swertz, MA, Bakker, SJL, Dotinga, A, Vonk, JM, et al. Cohort profile: LifeLines, a three-generation cohort study and biobank. Int J Epidemiol. (2015) 44:1172–80. doi: 10.1093/ije/dyu229
35. Karlson, KB, Holm, A, and Breen, R. Comparing regression coefficients between same-sample nested models using logit and Probit: a new method. Sociol Methodol. (2012) 42:286–313. doi: 10.1177/0081175012444861
36. de Vries, H. An integrated approach for understanding health behavior; the I-change model as an example. Psychol Behav Sci Int J. (2017) 2:555–85. doi: 10.19080/PBSIJ.2017.02.555585
37. Bandura, A. Social foundations of thought and action: A social cognitive theory / Albert Bandura. New Jersey: Prentice-Hall (1986).
38. Rosenstock, IM. The health belief model and preventive health behavior. Health Educ Monogr. (1974) 2:354–86. doi: 10.1177/109019817400200405
39. Ajzen, I. The theory of planned behavior. Organ Behav Hum Decis Process. (1991) 50:179–211. doi: 10.1016/0749-5978(91)90020-T
40. Prochaska, JO, and DiClemente, CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. (1983) 51:390–5. doi: 10.1037/0022-006X.51.3.390
42. Braun, V, and Clarke, V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
43. van Wietmarschen, HA, Staps, S, Meijer, J, Flinterman, JF, and Jong, MC. The use of the Bolk model for positive health and living environment in the development of an integrated health promotion approach: a case study in a socioeconomically deprived neighborhood in the Netherlands. Int J Environ Res Public Health. (2022) 19:2478. doi: 10.3390/ijerph19042478
44. Park, CL, Cho, D, and Moore, PJ. How does education lead to healthier behaviours? Testing the mediational roles of perceived control, health literacy and social support. Psychol Health. (2018) 33:1416–29. doi: 10.1080/08870446.2018.1510932
45. van der Heide, I, Wang, J, Droomers, M, Spreeuwenberg, P, Rademakers, J, and Uiters, E. The relationship between health, education, and health literacy: results from the Dutch adult literacy and life skills survey. J Health Commun. (2013) 18:172–84. doi: 10.1080/10810730.2013.825668
46. Belak, A, Filakovska Bobakova, D, Madarasova Geckova, A, van Dijk, JP, and Reijneveld, SA. Why don’t health care frontline professionals do more for segregated Roma? Exploring mechanisms supporting unequal care practices. Soc Sci Med. (2019) 246:112739. doi: 10.1016/j.socscimed.2019.112739
47. Kristensen, TS, Borg, V, and Hannerz, H. Socioeconomic status and psychosocial work environment: results from a Danish national study. Scand J Public Health. (2002) 30:41–8. doi: 10.1177/14034948020300030701
48. Harkonen, J, and Dronkers, J. Stability and change in the educational gradient of divorce. A comparison of seventeen countries. Eur Sociol Rev. (2006) 22:501–17. doi: 10.1093/esr/jcl011
49. Husk, K, Blockley, K, Lovell, R, Bethel, A, Lang, I, Byng, R, et al. What approaches to social prescribing work, for whom, and in what circumstances? A realist review. Health Soc Care Community. (2020) 28:309–24. doi: 10.1111/hsc.12839
50. Ajrouch, KJ, Blandon, AY, and Antonucci, TC. Social networks among men and women: the effects of age and socioeconomic status. J Gerontol Series B. (2005) 60:S311–7. doi: 10.1093/geronb/60.6.S311
51. Tinner, L, Caldwell, D, Hickman, M, and Campbell, R. Understanding adolescent health risk behaviour and socioeconomic position: a grounded theory study of UK young adults. Sociol Health Illn. (2021) 43:528–44. doi: 10.1111/1467-9566.13240
52. Eykelenboom, M, Olthof, MR, van Stralen, MM, Djojosoeparto, SK, Poelman, MP, Kamphuis, CBM, et al. The effects of a sugar-sweetened beverage tax and a nutrient profiling tax based on Nutri-score on consumer food purchases in a virtual supermarket: a randomised controlled trial. Public Health Nutr. (2022) 25:1105–17. doi: 10.1017/S1368980021004547
Keywords: health promotion, socioeconomic factors, lifestyle, focus groups, semistructured interview
Citation: Hoveling LA, Alma MA, Landsman-Dijkstra JA, Smidt N, Reijneveld SA, Bültmann U and De Kroon MLA (2025) Healthy lifestyle in low-socioeconomic groups: expert views. Front. Public Health. 13:1511317. doi: 10.3389/fpubh.2025.1511317
Edited by:
Hilde Langseth, Cancer Registry of Norway, NorwayReviewed by:
Henrik Lerner, Marie Cederschiöld University, SwedenBerta Paz-Lourido, University of the Balearic Islands, Spain
Copyright © 2025 Hoveling, Alma, Landsman-Dijkstra, Smidt, Reijneveld, Bültmann and De Kroon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liza A. Hoveling, bC5hLmhvdmVsaW5nQHVtY2cubmw=
 Liza A. Hoveling
Liza A. Hoveling Manna A. Alma
Manna A. Alma Jeanet A. Landsman-Dijkstra
Jeanet A. Landsman-Dijkstra Nynke Smidt1
Nynke Smidt1 Sijmen A. Reijneveld
Sijmen A. Reijneveld