- 1Graduate School of Harbin Sport University, Harbin, Heilongjiang, China
- 2College of Physical Education, Zhangjiakou University, Zhangjiakou, Hebei, China
Objective: This study aims to investigate the impact of various combinations of exercise prescription variables—namely type, duration, frequency, and period—on improving chronic low back pain (CLBP) in adults. The goal is to provide evidence to inform the development of exercise prescriptions for CLBP interventions.
Methods: Data sources were obtained from EBSCO, PubMed, Web of Science, Embase, and Cochrane, with the search conducted up to June 30, 2024. Two independent reviewers screened the literature, extracted data, and assessed the risk of bias in the included studies. A network meta-analysis (NMA) was performed using Stata 17.0 software, and the surface under the cumulative ranking (SUCRA) was utilized to rank the effectiveness of the exercise prescription variables.
Results: Significant effects were observed for durations of 15–30 min [SMD = −1.62, 95% CI (−2.32, −0.92)] and ≥60 min [SMD = −0.81, 95% CI (−1.58, −0.03)] when compared to the control group. Intervention periods of 4 weeks [SMD = −1.82, 95% CI (−3.37, −0.28)], 12 weeks [SMD = −1.18, 95% CI (−1.85, −0.51)], and ≥16 weeks [SMD = −2.75, 95% CI (−4.26, −1.24)] also resulted in significantly better outcomes compared to the control group. The intervention effect for durations of ≥16 weeks was significantly greater than that for 12 weeks [SMD = −2.17, 95% CI (−3.58, −0.47)] and 6 weeks [SMD = −2.18, 95% CI (−3.85, −0.45)]. A frequency of three sessions per week [SMD = −1.44, 95% CI (−2.09, −0.78)] demonstrated significantly superior outcomes compared to the control group. An intervention duration of 15 to 30 min (SUCRA = 94.6), three sessions per week (SUCRA = 87), an intervention period of ≥16 weeks (SUCRA = 95.4), and Tai Chi exercise (SUCRA = 77.4) may be the most effective approaches for improving chronic low back pain in adults.
Conclusion: Tai Chi exercise, lasting 15 to 30 min per session, performed three times a week over an intervention period of at least 16 weeks, may represent the most effective intervention for alleviating chronic low back pain in adults. However, due to the limited number of studies included, further research is necessary to provide stronger evidence.
1 Introduction
Chronic low back pain is characterized by persistent discomfort in the lower back, lumbosacral, and sacroiliac regions lasting more than three months. This pain may radiate to the buttocks or lower limbs, with or without accompanying radiating pain (1, 2). The condition significantly affects both the physical and mental health of patients, limiting daily activities, reducing sleep quality, and potentially leading to a substantial psychological burden, often manifested as anxiety, depression, and other emotional disorders (3). The high prevalence of chronic low back pain increases the strain on healthcare resources, as patients frequently seek medical attention and incur considerable treatment costs (4, 5). Furthermore, its effect on work performance can result in indirect economic losses, ultimately placing significant economic and social pressures on individuals, families, and society at large (6–8).
In recent years, the continuous advancement of health science research has led to an increased focus on non-pharmacological treatment approaches. Compared to traditional pharmacological treatments, exercise interventions, as a form of non-pharmacological therapy, present potential advantages, including reduced drug dependency, lower risk of side effects, and enhanced overall health (9). Numerous studies have demonstrated that appropriate exercise can strengthen lumbar muscles, improve spinal stability, and promote local blood circulation, effectively alleviating symptoms of chronic low back pain (10, 11). These exercise interventions encompass core stability training, yoga, Pilates, and Tai Chi, among others (12–15). While these studies provide robust evidence for the effectiveness of exercise in managing chronic low back pain (16–18), the optimal combination of exercise prescription—specifically, type, duration, frequency, and period—remains unclear for achieving the most effective intervention in adults with chronic low back pain.
The advantage of network meta-analysis lies in its ability to indirectly compare the effects of various interventions through their effects as intermediaries, even in the absence of direct comparison evidence. This approach overcomes the limitations of traditional meta-analysis, which can only handle direct comparisons between two interventions, thereby enhancing the precision of the analysis (19). Currently, treatment protocols for chronic low back pain in adults still require further exploration, particularly in determining the most effective types of exercise interventions, including their duration, frequency, and period, to develop more targeted exercise prescriptions (20–22). Therefore, this study aims to conduct a network meta-analysis of randomized controlled trials on exercise interventions for chronic low back pain in adults, providing specific recommendations for alleviating low back pain symptoms.
2 Data and methods
This systematic review was conducted by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (23) and prospectively registered on the PROSPERO platform, with registration number CRD42024595808 (24). Additionally, the study protocol has been published, and the results are reported by the PRISMA Extension for Network Meta-Analysis (PRISMA-NMA) guidelines (refer to the PRISMA-NMA checklist in Supplementary material) (25).
2.1 Literature search strategy
The following databases were searched: EBSCO, PubMed, Web of Science, Embase, and Cochrane databases. The search was conducted until June 30, 2024, for each respective database. The search terms used included: ① exercise, strength training, physical exercise, physical activity, Pilates, sports, fitness, functional training, cardio training, yoga, exercise therapy; ② adult, mature, grown-up, adulthood, middle-aged, older adult, senior, full-grown, professional, independent, mature individual, established person; ③ CLBP, chronic back pain, lumbar pain, low backache, chronic lumbago, persistent backache, recurring low back pain, chronic lumbar dysfunction, persistent lumbosacral pain, musculoskeletal pain, disc degeneration, sacroiliac joint dysfunction, RCT, experiment, trial. Boolean operator “AND” was used to connect the three sets of terms. Furthermore, relevant studies were identified by tracing articles from published systematic reviews and meta-analyses to ensure comprehensive coverage of the literature. For instance, the search strategy for Web of Science was as follows: TS = (exercise OR “Strength Training” OR “physical exercise” OR “physical activity” OR Pilates OR sports OR fitness OR “Functional Training” OR “Cardio Training” OR Yoga OR “Exercise Therapy”) AND TS = (Adult OR Mature OR “Grown-up” OR Adulthood OR “Middle-aged” OR Older adult OR Senior OR “Full-grown” OR Professional OR Independent OR “Mature Individual” OR “Established Person”) AND TI = (CLBP OR “Chronic Back Pain” OR “Lumbar Pain” OR “Low Backache” OR “Chronic Lumbago” OR “Persistent Backache” OR “Recurring Low Back Pain” OR “Chronic Lumbar Dysfunction” OR “Persistent Lumbosacral Pain” OR “Musculoskeletal Pain” OR “Disc Degeneration” OR “Sacroiliac Joint Dysfunction” OR RCT OR experiment OR trial).
2.2 Inclusion and exclusion criteria
The inclusion and exclusion criteria were defined according to the PICOS framework (26). Duplicate records from the retrieved literature were eliminated using EndNote 20 software (27). Two independent reviewers performed the screening process in a double-blind manner, adhering to the inclusion and exclusion criteria. The reviewers first conducted a preliminary reading of titles and abstracts to identify potentially eligible studies. Full-text articles of studies that appeared to meet the inclusion criteria were then retrieved and further assessed, with final inclusion decisions made according to the criteria. The inclusion criteria were as follows: (1) Population: Adults aged 18 years and older with chronic low back pain (CLBP) lasting more than 3 months, specifically non-specific chronic low back pain. (2) Interventions: Studies including any form of exercise intervention were eligible. No mandatory requirements were specified for the type, duration, or frequency of exercise, but the intervention period was required to last at least 4 weeks. (3) Control: Studies including a control group receiving usual care, such as routine daily activities, health education, or conventional nursing. (4) Outcomes: The Visual Analog Scale (VAS) was used to measure treatment outcomes. (5) Study Design: Randomized controlled trials (RCTs). The exclusion criteria were as follows: (1) Cross-sectional studies, case–control studies, and other descriptive research designs. (2) Reviews, abstracts, letters, and commentaries lacking a clear description of the study design. (3) Articles with incomplete data that could not be obtained from alternative sources. (4) Studies involving structural issues, such as osteoporosis, scoliosis, fractures, or inflammatory conditions causing low back pain.
2.3 Data extraction
Two members of the research team, both trained in evidence-based methodology and possessing extensive experience in the field of chronic low back pain in adults, independently conducted the literature screening and data extraction. In cases where discrepancies arose during the screening or extraction process, a third team member, possessing significant expertise in the treatment of chronic low back pain in adults, was consulted to provide guidance. The final decision was made through discussion and consensus. The data extraction primarily focused on the following key information: first author’s name, publication year, the country where the study was conducted, sample size of adult participants, type of intervention implemented, duration of the intervention, frequency of the intervention, intervention period, and primary outcome measures used to assess the effectiveness of the intervention.
2.4 Bias risk assessment
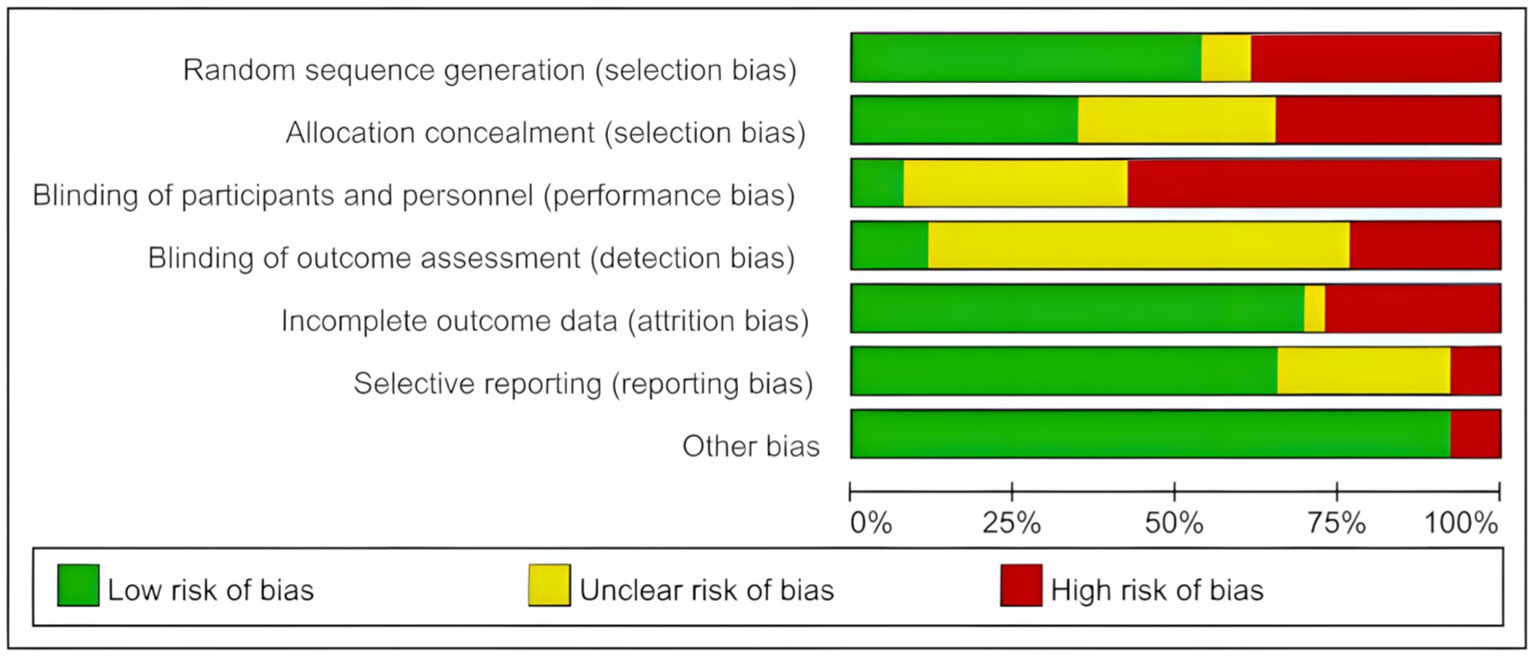
In this study, an independent bias risk assessment was conducted for all included studies using the Cochrane Risk of Bias Tool, by the PROSPERO registration statement (28). This assessment framework comprehensively addresses seven key dimensions: the validity of the randomization method, the implementation of blinding for trial participants and personnel, the blinding status of outcome assessors, the concealment of the allocation process, the completeness and accuracy of outcome data, the presence of selective reporting of outcomes, and the potential for other biases. The quality risk of each study was categorized into three levels: low risk, high risk, and unclear risk. In the case of discrepancies in the bias risk assessment, the reviewers reached a consensus through discussion. If a consensus could not be reached, the corresponding author made the final decision based on their judgment, considering the opinions of the majority of reviewers.
2.5 Statistical methods
In this study, global inconsistency was tested, and the test result showed a p-value of 0.520, which is greater than 0.05, indicating good global consistency. Further testing for consistency within each closed loop revealed that the inconsistency factor was closer to zero, suggesting better consistency. The results showed that the lower limits of the inconsistency factors included zero, suggesting no significant inconsistency between direct and indirect comparisons. Subsequently, the analysis was performed using Stata 17.0 software (29). Given that the outcome measures were continuous data and that different studies used varying assessment tools and measurement units, the standardized mean difference (SMD) was selected as the effect size measure to ensure consistency and comparability across studies, allowing precise calculation of the combined effect size. Network meta-analysis is a method that integrates both direct and indirect evidence, allowing comparisons of more than two interventions simultaneously. In the network plot, each node represents an intervention, with the size of the node reflecting the sample size, while the thickness of the connecting lines indicates the number of studies included. To further compare the efficacy of different interventions, the SUCRA (Surface Under the Cumulative Ranking Curve) method was used to rank the interventions. SUCRA is a statistical method based on network meta-analysis, employed to quantify the relative efficacy of each intervention among all possible interventions. The value ranges from 0 to 100, with higher values indicating better relative efficacy in improving chronic non-specific low back pain. Specifically, the standardized mean difference (SMD) and its 95% confidence interval were first calculated for each intervention, followed by the estimation of the cumulative ranking curves of each intervention through the network meta-analysis model, and ultimately ranking all interventions based on the SUCRA values. A higher SUCRA value indicates a greater likelihood that the intervention is the best treatment (30).
2.6 Evidence certainty assessment
In this study, the GRADE system assessment tool was used to evaluate the quality of evidence for all outcome indicators, and the results showed that there were 2 high-level evidence, 17 moderate-level evidence, 5 low-level evidence, and 2 very low-level evidence (see Table 1). Among the downgrading factors, limitations were the main downgrading factor, 24 were downgraded because of limitations, most of the literature only mentioned randomization without describing the method of generating random numbers, most of the literature did not use blinding and allocation concealment, and only a few of the literature described the process of single or double blinding and allocation concealment.
3 Results
3.1 Literature search results
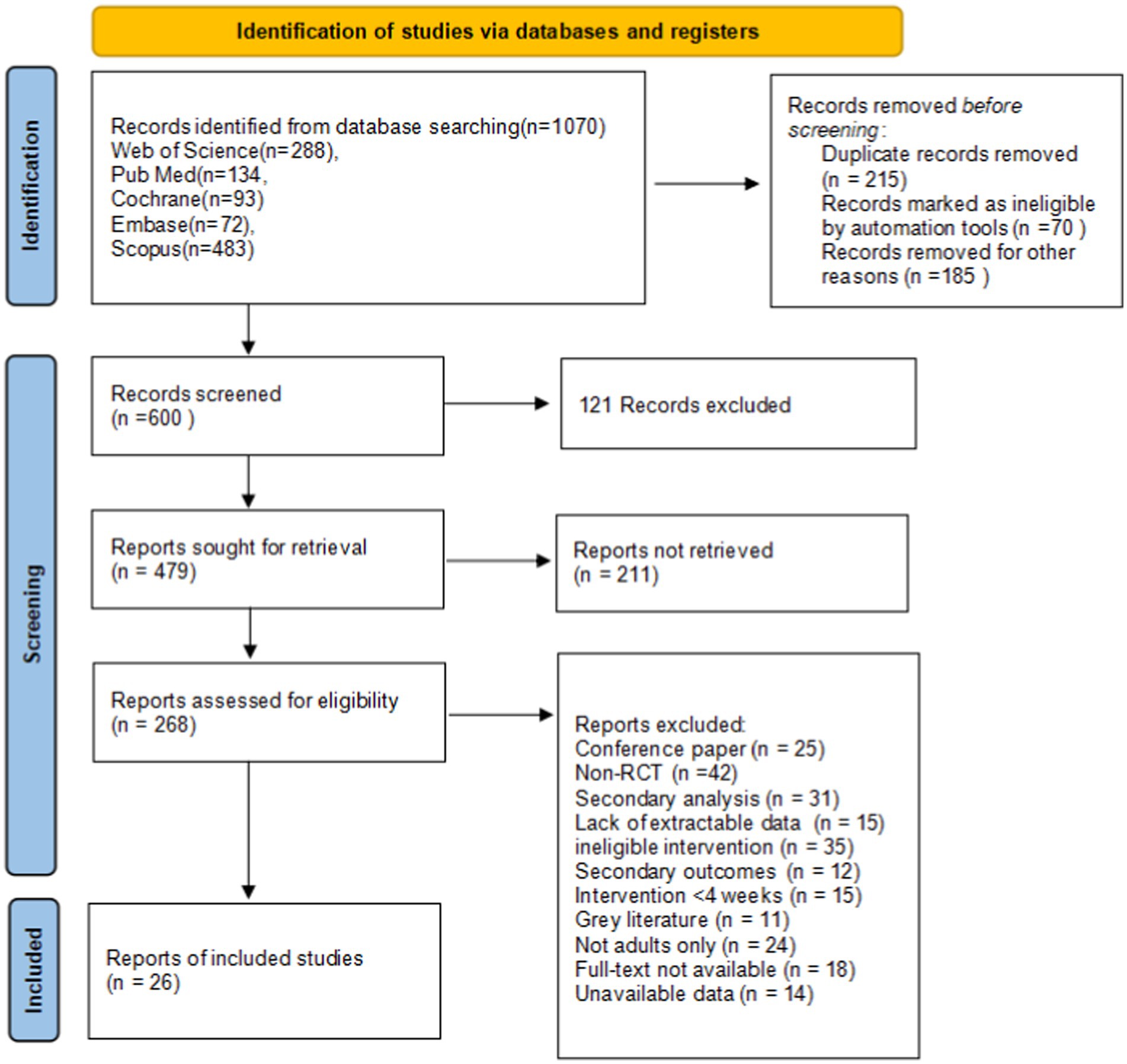
A total of 1,070 articles were identified from various databases and additional sources. After duplicates were removed, 215 articles were excluded, leaving 855 articles for further screening. Ultimately, 26 studies were included in the analysis, with a total of 1,507 participants. The screening process is shown in Figure 1.
3.2 Basic characteristics of included studies
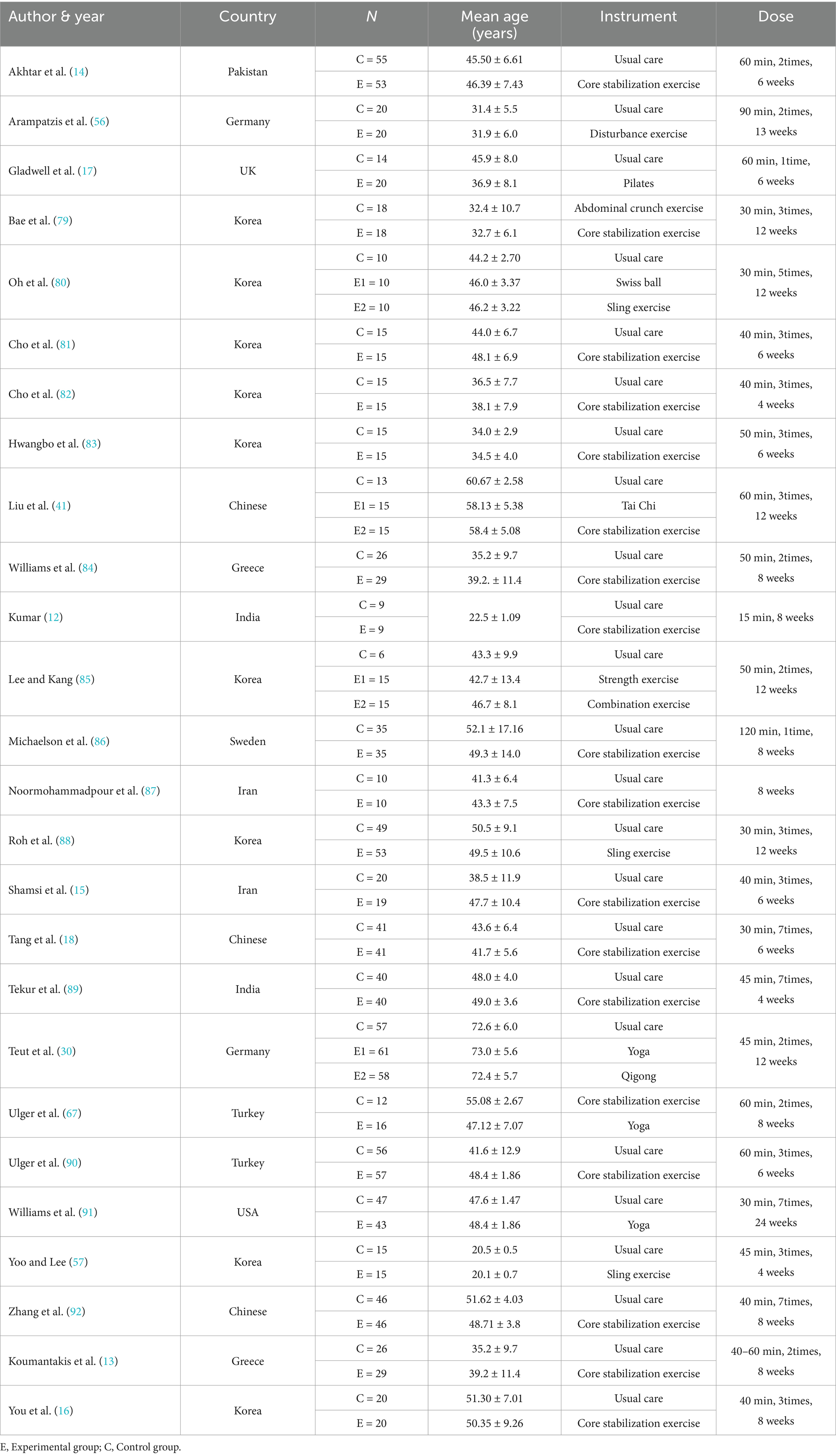
Among the 26 studies included, the exercise interventions in the experimental groups primarily involved core stability training, combined training, Pilates, yoga, qigong, suspension training, Swiss ball exercises, strength training, perturbation therapy, sit-up exercises, and tai chi. The intervention durations varied, ranging from 4, 6, 8, 12, 13, and ≥16 weeks. The frequency of interventions ranged from 1–2 sessions, 3 sessions, 5 sessions, to 7 sessions per week. Intervention durations ranged from 15–30 min, 40 min, 45 min, 50 min, to ≥60 min. The detailed characteristics of the included studies are presented in Table 2.
3.3 Quality assessment of included studies
The quality of the included studies was comprehensively evaluated using RevMan 5.4 software and the Cochrane risk of bias assessment tool (4, 31). The Cochrane risk of bias results for each study are shown in Figure 2, while Figure 3 presents a visual representation of the overall distribution of bias risk. Studies that employed randomization for allocation were classified as having a low risk of selection bias. In contrast, studies that either did not employ randomization or did not report the randomization process were classified as having a high risk of bias. Due to the inclusion of multiple exercise interventions and the inability of participants to remain blinded to treatment allocation, the majority of studies were classified as having a high risk of bias for patient blinding. The detailed risk of bias assessments for each study are provided in Table 3.
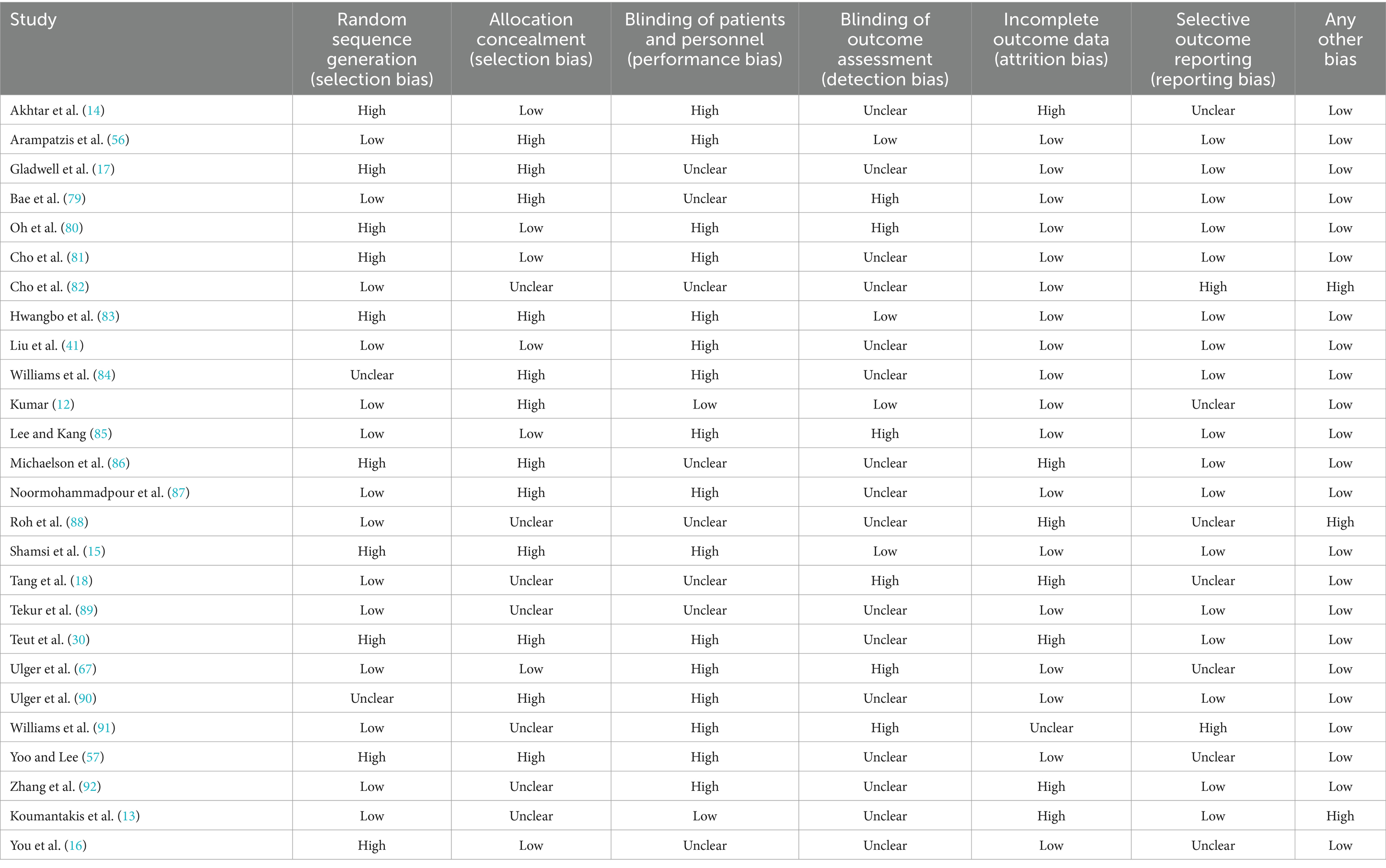
Table 3. Risk of bias assessment of included studies (n = 26) examining the efficacy of exercise training in patients with nonspecific chronic low back pain.
3.4 Network meta-analysis results
3.4.1 Network plot
A network plot is used to illustrate the direct and indirect comparative relationships among multiple interventions. In this plot, the connecting lines represent the direct comparisons between two interventions based on the original studies. The size of each node (i.e., point) corresponds to the sample size of the respective intervention in the study; larger sample sizes are represented by larger nodes. The thickness of the connecting lines reflects the amount of evidence for the direct comparison between the two interventions; thicker lines indicate a greater number of studies making direct comparisons between the two interventions. The specific network plot is presented in Figure 4. (Note: When an element refers to a range, the lower limit of the range is used).
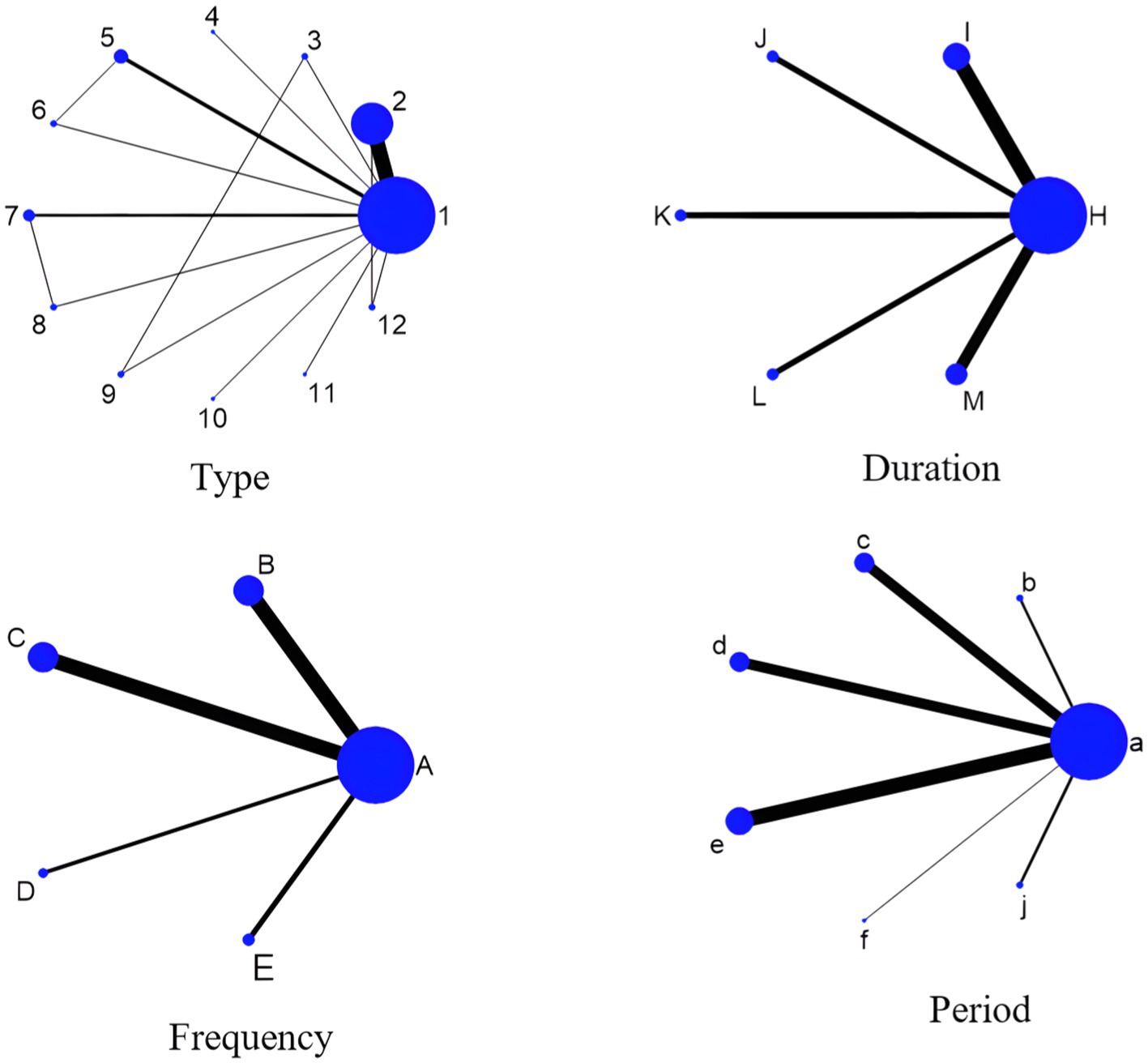
Figure 4. Network plot of the impact of exercise prescription elements on chronic low back pain control in adults. 1, con; 2, Core stabilization exercise; 3, Combination exercise; 4, Pilates; 5, Yoga; 6, Qigong; 7, Sling exercise; 8, Swiss ball; 9, Strength exercise; 10, Disturbance exercise; 11, Abdominal crunch exercise A; 12, Taichi; A, con; B, 1–2 times; C, 3 times; D, 5 times; E, 7 times; H, con; I, 15–30 min; J, 40 min; K, 45 min; L,50 min; M, ≥60 min; a, con; b, 4 weeks; c, 6 weeks; d, 8 weeks; e, 12 weeks; f, 13 weeks; j, ≥16weeks.
3.4.2 Results of pairwise comparisons of elements of exercise prescription
According to the data presented in Figure 5, both Yoga (SMD = −1.71, 95% CI: −2.93 to −0.49, p < 0.05) and Core Stability Training (SMD = −0.81, 95% CI: −1.44 to −0.18, p < 0.05) demonstrated significant improvement compared to the control group, showing substantial effects on pain intensity reduction. Data from Figure 6 indicate that intervention durations of 15–30 min (SMD = −1.62, 95% CI: −2.33 to −0.92) and ≥60 min (SMD = −0.81, 95% CI: −1.58 to −0.03) also significantly outperformed the control group. As shown in Figure 7, an intervention frequency of 3 times per week (SMD = −1.44, 95% CI: −2.09 to −0.78) demonstrated significantly better outcomes than the control group. Figure 8 presents data indicating that intervention periods of 4 weeks (SMD = −1.82, 95% CI: −3.37 to −0.28), 12 weeks (SMD = −1.18, 95% CI: −1.85 to −0.51), and ≥16 weeks (SMD = −2.75, 95% CI: −4.26 to −1.24) demonstrated significantly superior effects compared to the control group. Furthermore, interventions lasting ≥16 weeks also significantly outperformed those of 12 weeks (SMD = −2.17, 95% CI: −3.58 to −0.47) and 6 weeks (SMD = −2.18, 95% CI: −3.85 to −0.45). No significant differences were found in other pairwise comparisons.
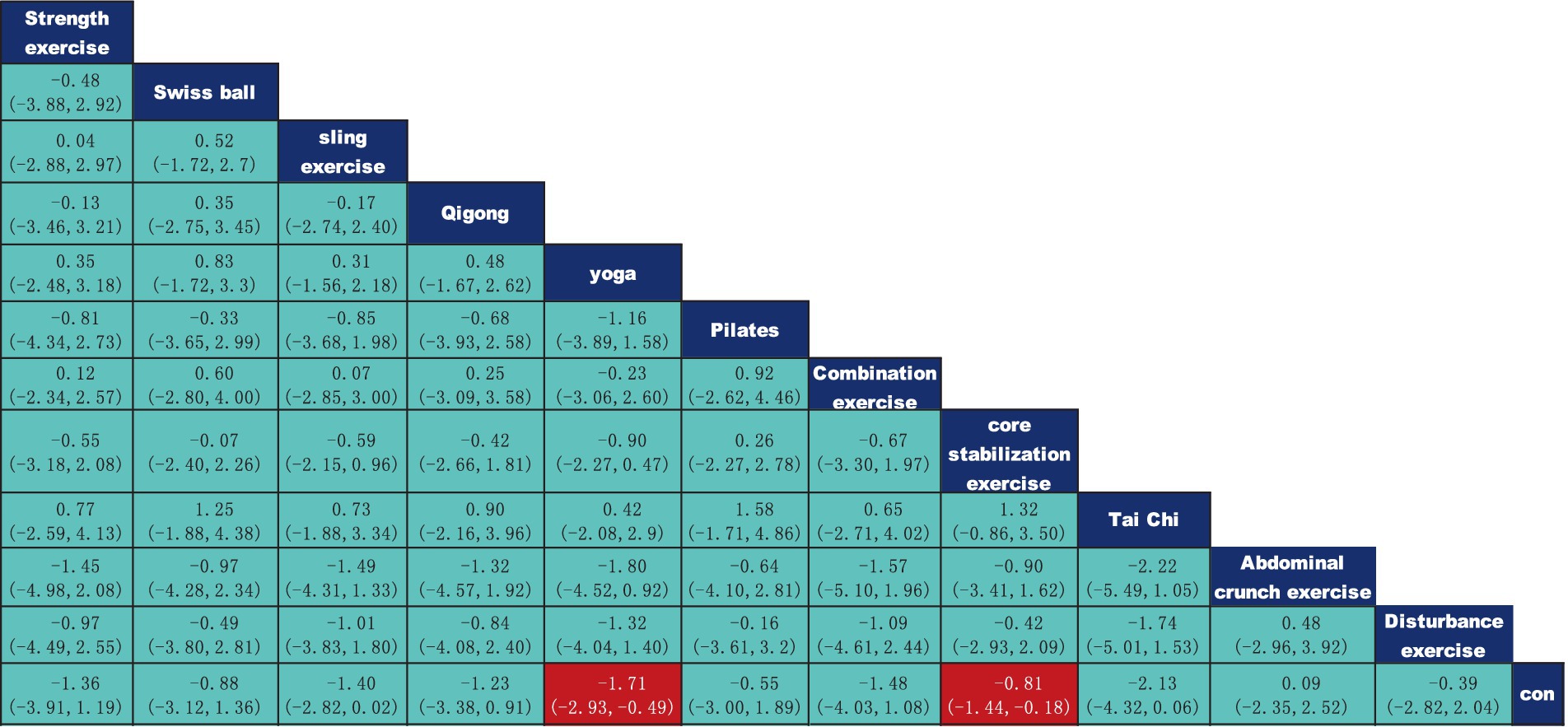
Figure 5. League table of pairwise comparisons of intervention effects for different elements of exercise types.
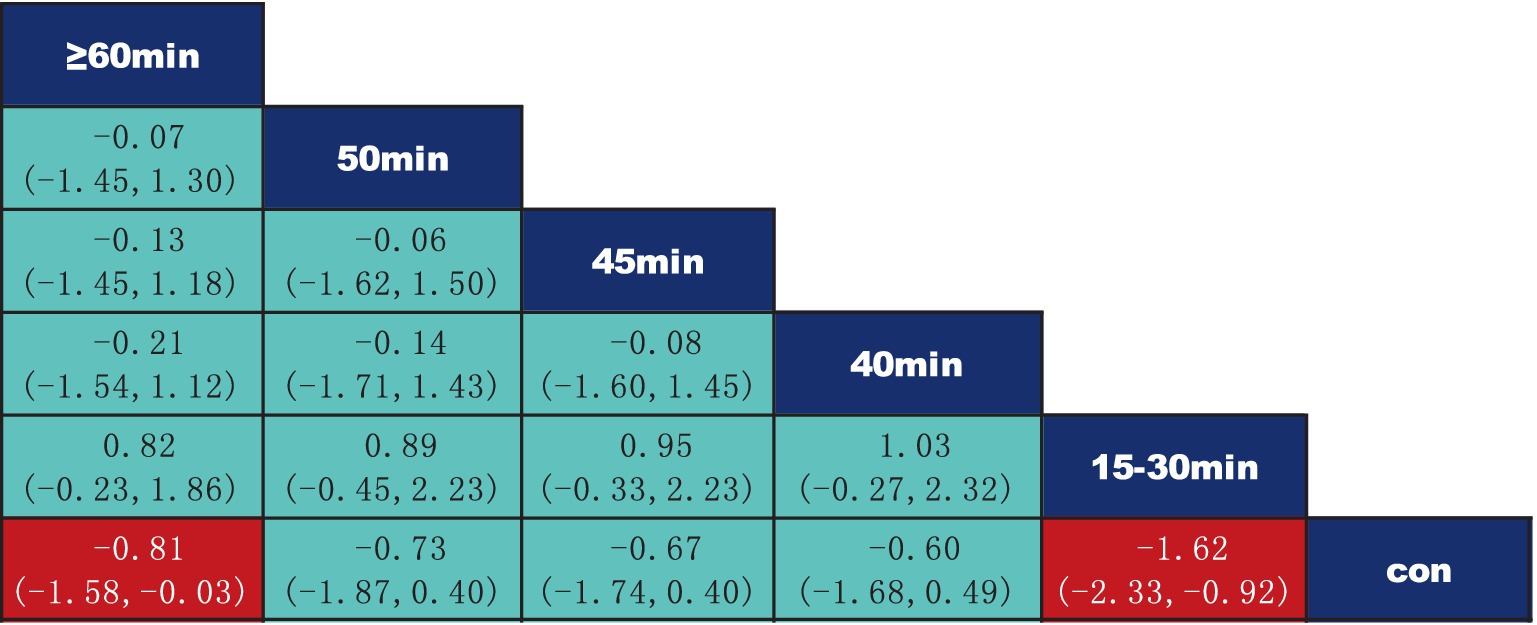
Figure 6. League table of pairwise comparisons of intervention effects for different elements of exercise duration.
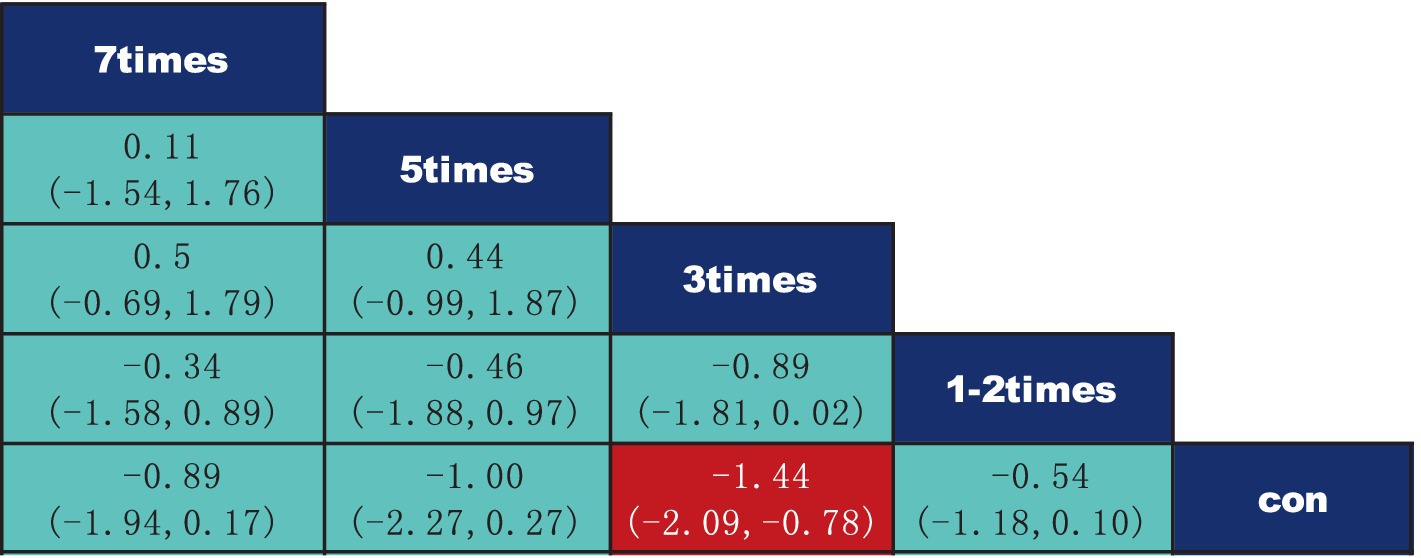
Figure 7. League table of pairwise comparisons of intervention effects for different elements of exercise frequency.
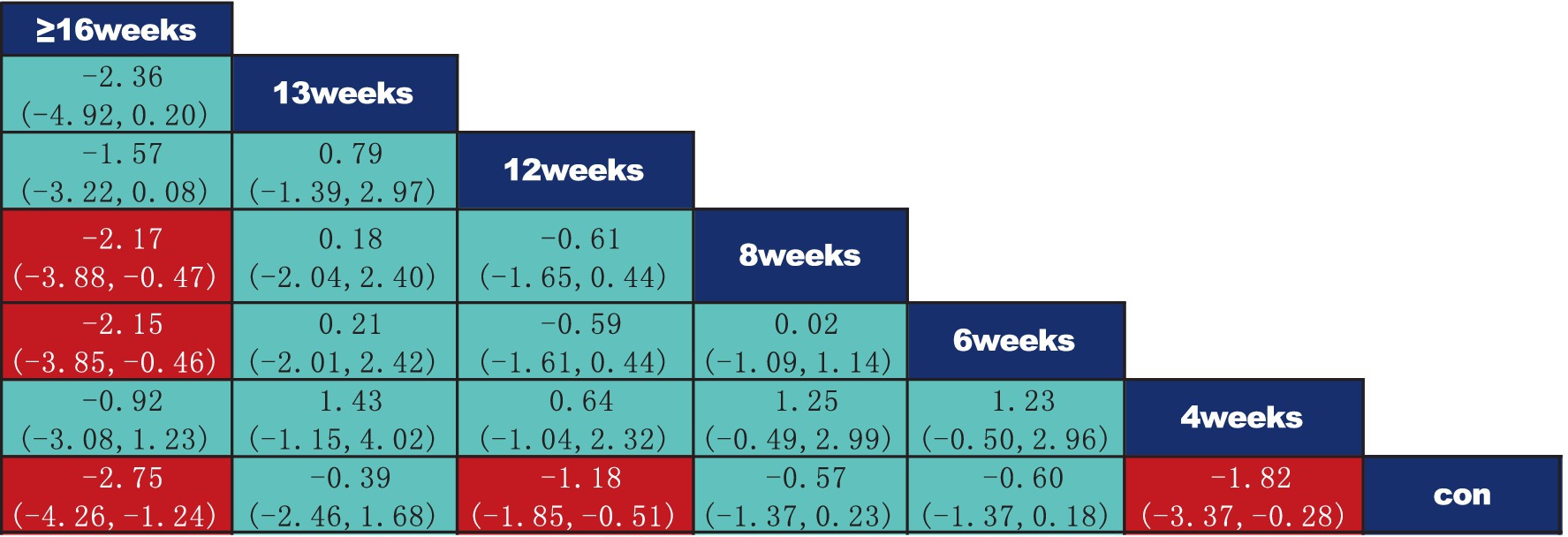
Figure 8. League table of pairwise comparisons of intervention effects for different elements of exercise period. The red numbers are statistically significant.
3.4.3 Probability ranking of the most effective interventions for elements of exercise prescription
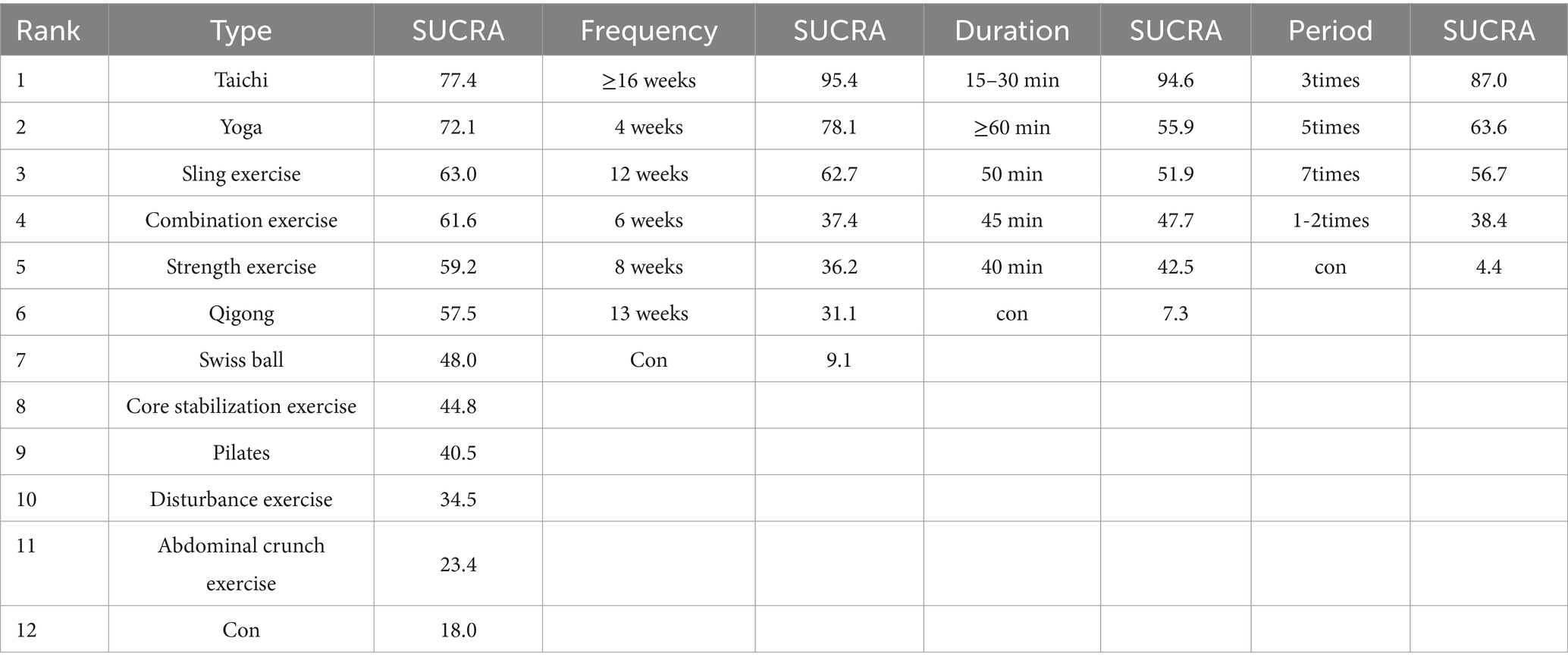
Based on the SUCRA values presented in Table 4 and Figure 9, the ranking of different exercise intervention types according to their effectiveness in improving chronic low back pain in adults is as follows: Tai Chi (SUCRA = 77.4) > Yoga (SUCRA = 72.1) > Sling Exercise (SUCRA = 63) > Combination Exercise (SUCRA = 61.6) > Strength Exercise (SUCRA = 59.2) > Qigong (SUCRA = 57.5) > Swiss Ball (SUCRA = 48) > Core Stabilization Exercise (SUCRA = 44.8) > Pilates (SUCRA = 40.5) > Disturbance Exercise (SUCRA = 34.5) > Abdominal Crunch Exercise (SUCRA = 23.4). In terms of intervention duration, the ranking of effectiveness for improving chronic low back pain in adults is as follows: 15–30 min (SUCRA = 94.6) > ≥60 min (SUCRA = 55.9) > 50 min (SUCRA = 51.9) > 45 min (SUCRA = 47.7) > 40 min (SUCRA = 42.5). The ranking of the effects of different intervention frequencies on the improvement of chronic low back pain in adults is as follows: 3 times per week (SUCRA = 87) > 5 times per week (SUCRA = 63.6) > 7 times per week (SUCRA = 56.7) > 1–2 times per week (SUCRA = 38.4). The ranking of intervention duration effectiveness is as follows: ≥16 weeks (SUCRA = 95.4) > 4 weeks (SUCRA = 78.1) > 12 weeks (SUCRA = 62.7) > 6 weeks (SUCRA = 37.4) > 8 weeks (SUCRA = 36.2) > 13 weeks (SUCRA = 31.1).
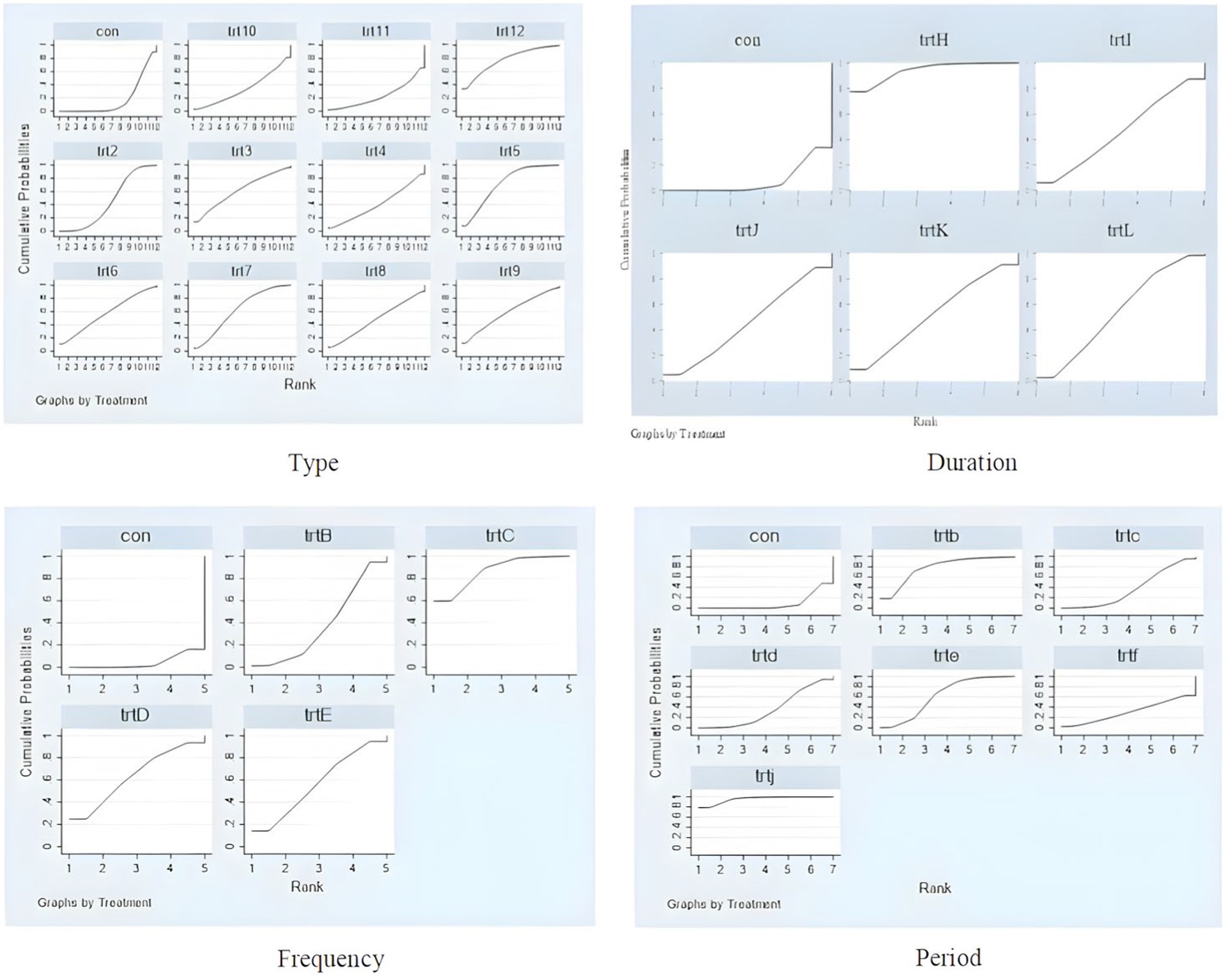
Figure 9. Probability ranking chart of intervention effects for different elements of exercise prescription dose. Type, con; trt2, Core stabilization exercise; trt3, Combination exercise; trt4, Pilates; trt5, Yoga; trt6, Qigong; trt7, Sling exercise; trt8, Swiss ball; trt9, Strength exercise; trt10, Disturbance exercise; trt11, Abdominal crunch exercise; trt12, Taichi; Duration, con; trtH, 15–30 min; trtI, 40 min; trtJ, 45 min; trtK, 45 min; trtL, ≥60 min; Frequency, con; trtB, 1–2 times; trtC, 3 times; trtD, 5 times; trtE, 7 times; Period, con; trtb, 4 weeks; trtc, 6 weeks; trtd, 8 weeks; trte, 12 weeks; trtf, 13 weeks; trtj, ≥16 weeks.
3.4.4 Sensitivity analysis
A leave-one-out sensitivity analysis was performed to assess the robustness of the results. The analysis demonstrated that, after removing any individual study, the pooled effect size fluctuated within the range of −1.059 to −0.845. This indicates that the exclusion of any individual study had a minimal impact on the overall pooled effect, confirming the stability and robustness of the findings in this analysis (Table 5).
3.4.5 Publication bias assessment
As shown in Figure 10, the funnel plots for all indicators were nearly symmetrical, with the majority of points located in the upper part of the funnel and only a few points falling outside the funnel. This suggests that the likelihood of publication bias in this study is low. Furthermore, Egger’s test for publication bias yielded a p-value of 0.161, indicating no significant evidence of publication bias. However, caution is advised when interpreting these results, and further studies may be needed to confirm the findings.
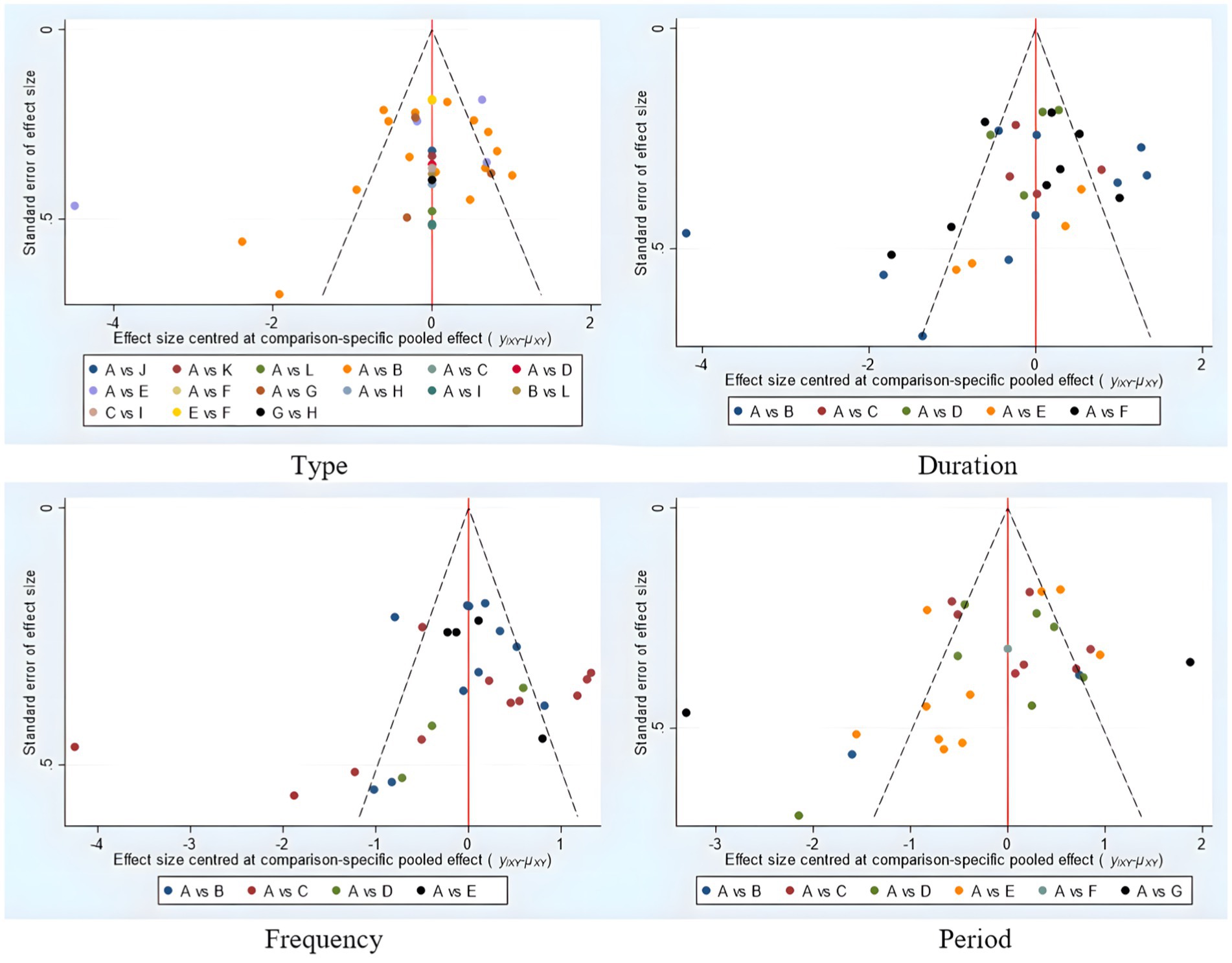
Figure 10. Funnel plot of intervention effects for different elements of exercise prescription dose. Type: A, con; B, Core stabilization exercise; C, Combination exercise; D, Pilates; E, Yoga; F, Qigong; G, Sling exercise; H, Swiss ball; I, Strength exercise; J, Disturbance exercise; K, Abdominal crunch exercise; L, Taichi; Duration: A, con; B, 15–30 min; C, 40 min; D, 45 min; E, 50 min, E, ≥60 min; Frequency: A, con; B, 1–2 times; C, 3 times; D, 5 times; E, 7 times; Period: A, con; B, 4 weeks; C, 6 weeks; D, 8 weeks; E, 12 weeks; F, 13 weeks; G ≥16 weeks.
4 Discussion
Despite the existence of several recent systematic reviews and meta-analyses discussing the effects of exercise interventions on chronic low back pain (CLBP) in adults, our network meta-analysis is the first to investigate the effects of exercise prescription components on CLBP outcomes (32–35). Additionally, we ranked the impact of different exercise types, frequencies, durations, and periods on adult chronic low back pain, which will aid in identifying the most effective exercise interventions for this population. This information is crucial for formulating the most appropriate and beneficial intervention strategies.
Our network meta-analysis identified that the most effective exercise for alleviating chronic low back pain in adults may be Tai Chi. The optimal intervention duration is likely 15–30 min, the best frequency is 3 times per week, and the most beneficial intervention period is likely ≥16 weeks.
Firstly, our findings suggest that Tai Chi is an effective exercise intervention that can significantly improve symptoms of CLBP in adults (36, 37). However, this contradicts existing research findings. Existing meta-analysis results suggest that Pilates, aerobic exercise, and resistance training may be the best interventions for adult chronic low back pain (38–40). The superiority of Tai Chi in our analysis may be attributed to its unique exercise approach. Tai Chi is a slow, continuous, and mindful form of exercise that helps regulate muscle tension, effectively alleviating the tension-type pain associated with chronic low back pain. Furthermore, Tai Chi emphasizes core stability, body posture, muscle coordination, strength, joint flexibility, and breathing regulation. By training these physical components in an integrated manner, Tai Chi enhances overall body function and comfort, contributing to the relief of chronic low back pain (37). The smooth, flowing, and coordinated movements of Tai Chi, coupled with its emphasis on controlled breathing and mental focus, are thought to improve core stability and lumbar proprioception (41–43). Furthermore, the circular and spiral movements in Tai Chi are thought to gently stretch and strengthen the lumbar muscles and connective tissues, addressing muscle imbalances and stiffness associated with CLBP (44).
Tai Chi, as a traditional mind–body exercise, demonstrated a high efficacy score in this study. During the bias risk assessment for Tai Chi, we found that the randomization method was well-implemented, with both random sequence generation and allocation concealment assessed as low risk. This indicates that the study adhered to rigorous standards for randomization and allocation control. However, there was a higher risk associated with the blinding of trial participants and operators, which may have influenced the evaluation of the intervention’s effectiveness. Additionally, the blinding status of the assessors is unclear, which may introduce subjectivity into the evaluation results. In terms of data completeness and accuracy, there was minimal missing data, leading to a low-risk assessment for these factors. Furthermore, there was no selective reporting of outcomes in the study, contributing to the overall low risk of bias. Other potential sources of bias were also evaluated as low-risk. Overall, the study’s risk of bias was relatively low. While the insufficient blinding of participants and operators may have influenced the evaluation of treatment effects, sensitivity analyses excluding high-risk bias studies indicated that the efficacy of Tai Chi remained stable, further confirming its effectiveness.
Nevertheless, caution should be exercised when promoting Tai Chi as a therapeutic intervention, particularly considering that other forms of exercise, such as Pilates, core stability training, and yoga, also demonstrate significant therapeutic effects and have been recommended in several clinical guidelines (45). Each type of exercise has advantages and is worth trying in therapy. However, our study found that although the effect of tai chi seems to be good, it may be due to factors such as cultural background and exercise habits, which affect the results of the overall analysis. Therefore, when choosing exercises for patients with chronic low back pain, we should not only look at the ranking of exercise effectiveness, but also consider the patients themselves, such as whether they can do it, whether they like it, and whether they can stick to it. Only by combining these factors with the exercise rankings can we find exercises that are both effective and easy to adhere to, and ultimately achieve the best treatment results.
Secondly, the results of this study suggest that the optimal intervention duration for improving chronic low back pain in adults is 15–30 min, consistent with previous studies (46). This duration ensures sufficient stimulation to promote muscle relaxation, enhance core muscle strength, and improve joint flexibility, while avoiding muscle fatigue or discomfort that may arise from prolonged duration, thus effectively alleviating back pain symptoms and promoting recovery (47, 48). This phenomenon can be reasonably explained from multiple theoretical perspectives. According to the “Supercompensation Theory,” the body undergoes a recovery phase after moderate stimulation, eventually surpassing its previous level (49). In this study, despite the relatively short total intervention duration, this precise stimulation enabled the body to quickly adapt and recover, avoiding fatigue and injury associated with prolonged exercise. Through deep breathing and gentle movements, participants could further relax their bodies and consolidate the benefits of the practice (50–52). Furthermore, the ‘Adaptation Efficiency Hypothesis’ offers another perspective. This hypothesis posits that, within a given time frame, the body adapts most effectively to stimuli that best promote its overall function (53). In this study, the 15-30-min intervention duration may represent the optimal time window for triggering the body’s adaptive mechanism and promoting recovery (54, 55).
The study also found that a three-times-per-week intervention schedule significantly improved chronic low back pain (CLBP) in adults, consistent with existing studies (56–58). Further analysis reveals why a three-times-per-week intervention schedule has been shown to be more effective from several perspectives. From a physiological adaptation standpoint, the body requires time to recover after exercise stimulation to reach a supercompensation state before the next session (59–61). Excessively frequent interventions may lead to overuse of muscles and joints, increasing the risk of injury and potentially inhibiting the body’s natural recovery process (62). In contrast, a three-times-per-week schedule provides adequate stimulation to promote recovery while offering necessary recovery time, allowing the body to reach its optimal state before the next intervention (61). From a behavioral compliance perspective, a three-times-per-week schedule may be more acceptable and easier for patients to adhere to (63). An overly frequent training program may bring more stress to patients’ lives, thus reducing their motivation to participate in training and their willingness to adhere to it in the long term (64). On the contrary, moderate training frequency not only reduces patients’ psychological burden, but also enhances their confidence in treatment (65). In addition, a study of patients with chronic low back pain showed that patients who performed core stability training 3 times per week performed well in terms of pain relief and functional improvement, with no significant difference in outcomes compared with patients who trained 7 times per week (66). This result emphasizes the importance of moderate interventions and suggests that we do not have to overdo the high frequency of training to achieve good therapeutic results when developing a training program.
Finally, the results of this study indicate that an intervention period exceeding 16 weeks is optimal for improving chronic low back pain in adults (67). This contrasts with previous findings, which suggest that an intervention period of ≤8 weeks is the most effective for treating chronic low back pain in adults (68). However, chronic low back pain is often accompanied by long-term pathological changes, such as muscle imbalances, ligament laxity, and intervertebral disc degeneration, which cannot be fully reversed within a short time frame (69). Therefore, a longer intervention period provides the body with sufficient time to adapt and produce sustained therapeutic effects (49). As the intervention period lengthens, the body gradually attains a new state of balance, leading to more stable pain relief and functional recovery (53). Long-term interventions not only address physical symptoms but also promote the development of healthy lifestyle and exercise habits (70). Through consistent Tai Chi practice, patients can gradually integrate exercise into their daily routines, establishing positive health behavior patterns. This behavioral change not only alleviates chronic low back pain symptoms but also plays a crucial role in preventing relapse (71). During long-term intervention, patients benefit not only from physical improvements but also from psychological support provided by coaches and peers (72). This behavior is very helpful in improving patients’ negative emotions and can significantly improve their quality of life (73). Therefore, this study concludes that intervention cycles longer than 16 weeks are more effective than short-term interventions. This is because a longer intervention period can provide enough time for full physical recovery.
5 Limitations
Firstly, because most of the included studies did not adequately implement blinding, bias may have been introduced, potentially compromising the objectivity and reliability of the findings. Secondly, due to resource and time constraints, this study did not incorporate registered but unpublished clinical trial data, which may have resulted in incomplete data. Moreover, the studies included were predominantly focused on the Asian region, which may limit the generalizability of the findings and their applicability to broader populations. Despite these limitations, this study provides valuable insights, and future research should aim to include data from a greater number of randomized controlled trials to improve the comprehensiveness and reliability of the conclusions.
6 Implications for research
In the 2017 guidelines, the American College of Physicians (ACP) recommended exercise as the first-line non-pharmacological treatment for chronic non-specific or radicular low back pain. Specifically, the ACP endorsed Tai Chi, yoga, spinal manipulation, massage, and acupuncture as effective therapeutic methods (74). The National Institute for Health and Care Excellence (NICE), in its 2010 guidelines, also recommended moderate exercise as the first choice for treating chronic low back pain. The guidelines emphasized that patients should be encouraged to remain active, avoid prolonged bed rest, and engage in moderate exercises, such as walking, swimming, or yoga (75). Although the specific recommendations of these two guidelines vary, our findings largely align with the recommended interventions. Notably, the NICE guidelines stress the importance of considering the patient’s individual needs, preferences, and abilities when selecting the type of exercise, and our results align with the low-intensity exercise interventions (such as Tai Chi and yoga) recommended by both the ACP and NICE. We found that Tai Chi, as a low-risk, low-intensity exercise, is highly effective in alleviating chronic low back pain, supporting the recommendations of these clinical guidelines (76).
However, despite the consistency of our study with the ACP and NICE guidelines, there are notable differences in some aspects. For instance, the NICE guidelines highlight the importance of multidisciplinary interventions and individualized treatment plans, while our study focuses primarily on Tai Chi as a sole intervention. Another difference is that the ACP guidelines emphasize short-term effects, while our study provides an evaluation of long-term interventions lasting more than 16 weeks, emphasizing the importance of sustained exercise. Furthermore, the World Health Organization (WHO) guidelines published in 2020 also explicitly recommend exercise interventions as the first-line treatment for chronic low back pain, advocating for aerobic and stretching exercises aimed at strengthening muscles, improving function, and reducing pain (77). Additionally, the Australian Commission on Safety and Quality in Health Care (ACSQHC) emphasized in its 2017 guidelines that exercise interventions are crucial for treating low back pain, recommending moderate exercise to alleviate pain symptoms (78).
7 Implications for clinical practice
Our study suggests that exercise interventions, particularly Tai Chi, may be among the most effective methods for alleviating pain in patients with chronic low back pain (LBP). Tai Chi, as a low-intensity, low-risk exercise, not only helps strengthen and improve the flexibility of the lumbar muscles but also effectively reduces pain through mind–body relaxation techniques. Long-term commitment to exercise is crucial, with an optimal intervention period potentially exceeding 16 weeks to achieve more significant therapeutic effects. Although we provide exercise prescription recommendations for public health, many chronic LBP patients still require personalized exercise plans tailored to individual differences. Therefore, we recommend improving the pre-exercise health assessment system, which should comprehensively evaluate a patient’s physical abilities, potential risks, health status, exercise goals, and preferences. Based on these assessments, personalized exercise plans should be developed. Furthermore, regular evaluation of exercise outcomes, along with adjustments based on the latest research evidence, will ensure the ongoing effectiveness of the exercise prescription. Additionally, regular evaluations of exercise effectiveness should be conducted, with adjustments made based on the latest research evidence to ensure the ongoing effectiveness of the exercise prescription and further reduce patients’ reliance on medication and surgical treatments.
8 Conclusion
This study included 26 studies and performed a network meta-analysis to compare the effects of different exercise prescriptions on improving chronic low back pain (CLBP) in adults. Limited evidence suggests that an exercise prescription with a duration of 15–30 min, a frequency of three times per week, a duration exceeding 16 weeks, and Tai Chi as the intervention type may be the most effective for improving chronic low back pain in adults. This finding is an important guide to help adults choose the most appropriate exercise intervention program. However, due to the small number of studies included in this study and the fact that most of the studies focused on the Asian region, we still need to remain cautious in interpreting these results. Future studies need to increase the number of studies and work to address current limitations to improve the comprehensiveness and reliability of the evidence.
Author contributions
KZ: Writing – original draft. PZ: Writing – review & editing. HL: Writing – review & editing. LL: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors would like to express sincere gratitude to those who provided data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1512450/full#supplementary-material
References
1. Hayden, JA, Ellis, J, Ogilvie, R, Malmivaara, A, and van Tulder, MW. Exercise therapy for chronic low back pain. Cochrane Database Syst Rev. (2021) 2021:9. doi: 10.1002/14651858.CD009790.pub2
2. Tagliaferri, SD, Miller, CT, Owen, PJ, Mitchell, UH, Brisby, H, Fitzgibbon, B, et al. Domains of chronic low back pain and assessing treatment effectiveness: a clinical perspective. Pain Pract. (2020) 20:211–25. doi: 10.1111/papr.12846
3. Kalso, E, Edwards, JE, Moore, RA, and McQuay, HJ. Opioids in chronic non-cancer pain: systematic review of efficacy and safety. Pain. (2004) 112:372–80. doi: 10.1016/j.pain.2004.09.019
4. Tantry, TP, Karanth, H, Shetty, PK, and Kadam, D. Self-learning software tools for data analysis in meta-analysis. Korean J Anesthesiol. (2021) 74:459–61. doi: 10.4097/kja.21080
5. Chou, R, Qaseem, A, Owens, DK, and Shekelle, P. Diagnostic imaging for low back pain: advice for high-value health care from the American College of Physicians. Ann Intern Med. (2011) 154:181–9. doi: 10.7326/0003-4819-154-3-201102010-00008
6. Cui, Y, Guo, J, Lu, Y, Hu, M, Zhou, H, Zhang, W, et al. Genome-wide Mendelian randomization identifies potential drug targets for Dorsopathies. medRxiv (2024). medRxiv:2024.01.24306675.
7. Warburton, DE, Nicol, CW, and Bredin, SS. Health benefits of physical activity: the evidence. CMAJ. (2006) 174:801–9. doi: 10.1503/cmaj.051351
8. Blumenthal, JA, Babyak, MA, Doraiswamy, PM, Watkins, L, Hoffman, BM, Barbour, KA, et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med. (2007) 69:587–96. doi: 10.1097/PSY.0b013e318148c19a
9. Sallis, R. Exercise is medicine and physicians need to prescribe it! Br J Sports Med. (2009) 43:3–4. doi: 10.1136/bjsm.2008.054825
10. Deodato, M, Saponaro, S, Šimunič, B, Martini, M, Murena, L, and Buoite, SA. Trunk muscles’ characteristics in adolescent gymnasts with low back pain: a pilot study on the effects of a physiotherapy intervention including a postural reeducation program. J Manual Manipul Ther. (2024) 32:310–24. doi: 10.1080/10669817.2023.2252202
11. Paolucci, T, Attanasi, C, Cecchini, W, Marazzi, A, Capobianco, SV, and Santilli, V. Chronic low back pain and postural rehabilitation exercise: a literature review. J Pain Res. (2018) 12:95–107. doi: 10.2147/JPR.S171729
12. Kumar, SP. Efficacy of segmental stabilization exercise for lumbar segmental instability in patients with mechanical low back pain: a randomized placebo controlled crossover study. N Am J Med Sci. (2011) 3:456–61. doi: 10.4297/najms.2011.3456
13. Koumantakis, GA, Watson, PJ, and Oldham, JA. Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent low back pain. Phys Ther. (2005) 85:209–25. doi: 10.1093/ptj/85.3.209
14. Akhtar, MW, Karimi, H, and Gilani, SA. Effectiveness of core stabilization exercises and routine exercise therapy in management of pain in chronic nonspecific low back pain: a randomized controlled clinical trial. Pak J Med Sci. (2017) 33:1002. doi: 10.12669/pjms.334.12664
15. Shamsi, MB, Sarrafzadeh, J, and Jamshidi, A. Comparing core stability and traditional trunk exercise on chronic low back pain patients using three functional lumbopelvic stability tests. Physiother Theory Pract. (2015) 31:89–98. doi: 10.3109/09593985.2014.959144
16. You, JH, Kim, S-Y, Oh, D-W, and Chon, S-C. The effect of a novel core stabilization technique on managing patients with chronic low back pain: a randomized, controlled, experimenter-blinded study. Clin Rehabil. (2014) 28:460–9. doi: 10.1177/0269215513506231
17. Gladwell, V, Head, S, Haggar, M, and Beneke, R. Does a program of Pilates improve chronic non-specific low back pain? J Sport Rehabil. (2006) 15:338–50. doi: 10.1123/jsr.15.4.338
18. Tang, S, Qian, X, Zhang, Y, and Liu, Y. Treating low back pain resulted from lumbar degenerative instability using Chinese Tuina combined with core stability exercises: a randomized controlled trial. Complement Ther Med. (2016) 25:45–50. doi: 10.1016/j.ctim.2016.01.001
19. Mavridis, D. Network meta-analysis in a nutshell. BMJ Ment Health. (2019) 22:100–1. doi: 10.1136/ebmental-2019-300104
20. Cipriani, A, Higgins, JP, Geddes, JR, and Salanti, G. Conceptual and technical challenges in network meta-analysis. Ann Intern Med. (2013) 159:130–7. doi: 10.7326/0003-4819-159-2-201307160-00008
21. Dias, S, Sutton, AJ, Welton, NJ, and Ades, A. Evidence synthesis for decision making 3: heterogeneity—subgroups, meta-regression, bias, and bias-adjustment. Med Decis Mak. (2013) 33:618–40. doi: 10.1177/0272989X13485157
22. Mills, EJ, Thorlund, K, and Ioannidis, JP. Demystifying trial networks and network meta-analysis. BMJ. (2013) 346:346. doi: 10.1136/bmj.f2914
23. Moher, D, Shamseer, L, Clarke, M, Ghersi, D, Liberati, A, Petticrew, M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1–9. doi: 10.1186/2046-4053-4-1
24. Gianola, S, Castellini, G, Andreano, A, Corbetta, D, Frigerio, P, Pecoraro, V, et al. Effectiveness of treatments for acute and sub-acute mechanical non-specific low back pain: protocol for a systematic review and network meta-analysis. Syst Rev. (2019) 8:1–8. doi: 10.1186/s13643-019-1116-3
25. Hutton, B, Salanti, G, Caldwell, DM, Chaimani, A, Schmid, CH, Cameron, C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. (2015) 162:777–84. doi: 10.7326/M14-2385
26. Munn, Z, Stern, C, Aromataris, E, Lockwood, C, and Jordan, Z. What kind of systematic review should I conduct? A proposed typology and guidance for systematic reviewers in the medical and health sciences. BMC Med Res Methodol. (2018) 18:1–9. doi: 10.1186/s12874-017-0468-4
27. Idris, SA, Qureshi, AG, Elkhair, IS, Idris, TA, Adam, AM, and Mohammed, NK. Usefulness of EndNote software for writing scientific manuscripts: a comparative study. Health Res. (2019) 11:6–10. doi: 10.5958/2456-9399.2022.00012
28. Sterne, JA, Savović, J, Page, MJ, Elbers, RG, Blencowe, NS, Boutron, I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019):l4898. doi: 10.1136/bmj.l4898
29. Shim, S, Yoon, B-H, Shin, I-S, and Bae, J-M. Network meta-analysis: application and practice using Stata. Epidemiol Health. (2017) 39:e2017047. doi: 10.4178/epih.e2017047
30. Teut, M, Knilli, J, Daus, D, Roll, S, and Witt, CM. Qigong or yoga versus no intervention in older adults with chronic low back pain—a randomized controlled trial. J Pain. (2016) 17:796–805. doi: 10.1016/j.jpain.2016.03.003
31. Higgins, JP, and Thompson, SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
32. Chou, R, Deyo, R, Friedly, J, Skelly, A, Hashimoto, R, Weimer, M, et al. Nonpharmacologic therapies for low back pain: a systematic review for an American College of Physicians clinical practice guideline. Ann Intern Med. (2017) 166:493–505. doi: 10.7326/M16-2459
33. Enthoven, WT, Roelofs, PD, Deyo, RA, van Tulder, MW, Koes, BW, Back, C, et al. Non-steroidal anti-inflammatory drugs for chronic low back pain. Cochrane Database Syst Rev. (1996) 2016:2087. doi: 10.1002/14651858.CD012087
34. Hildebrandt, V, Bongers, P, Dul, J, Van Dijk, F, and Kemper, H. The relationship between leisure time, physical activities and musculoskeletal symptoms and disability in worker populations. Int Arch Occup Environ Health. (2000) 73:507–18. doi: 10.1007/s004200000167
35. Saragiotto, BT, Maher, CG, Yamato, TP, Costa, LO, Menezes Costa, LC, Ostelo, RW, et al. Motor control exercise for chronic non-specific low-back pain. Cochrane Database Syst Rev. (1996) 2016:CD012004. doi: 10.1002/14651858.CD012004
36. Qin, J, Zhang, Y, Wu, L, He, Z, Huang, J, Tao, J, et al. Effect of tai chi alone or as additional therapy on low back pain: systematic review and meta-analysis of randomized controlled trials. Medicine. (2019) 98:e17099. doi: 10.1097/MD.0000000000017099
37. Hall, A, Copsey, B, Richmond, H, Thompson, J, Ferreira, M, Latimer, J, et al. Effectiveness of tai chi for chronic musculoskeletal pain conditions: updated systematic review and meta-analysis. Phys Ther. (2017) 97:227–38. doi: 10.2522/ptj.20160246
38. Yu, Z, Yin, Y, Wang, J, Zhang, X, Cai, H, and Peng, F. Efficacy of Pilates on pain, functional disorders and quality of life in patients with chronic low back pain: a systematic review and meta-analysis. Int J Environ Res Public Health. (2023) 20:2850. doi: 10.3390/ijerph20042850
39. Searle, A, Spink, M, Ho, A, and Chuter, V. Exercise interventions for the treatment of chronic low back pain: a systematic review and meta-analysis of randomised controlled trials. Clin Rehabil. (2015) 29:1155–67. doi: 10.1177/0269215515570379
40. Owen, PJ, Miller, CT, Mundell, NL, Verswijveren, SJ, Tagliaferri, SD, Brisby, H, et al. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br J Sports Med. (2020) 54:1279–87. doi: 10.1136/bjsports-2019-100886
41. Liu, J, Yeung, A, Xiao, T, Tian, X, Kong, Z, Zou, L, et al. Chen-style tai chi for individuals (aged 50 years old or above) with chronic non-specific low back pain: a randomized controlled trial. Int J Environ Res Public Health. (2019) 16:517. doi: 10.3390/ijerph16030517
42. Weifen, W, Muheremu, A, and Chaohui, C. Effectiveness of tai chi practice for non-specific chronic low back pain on retired athletes: a randomized controlled study. J Musculoskel Pain. (2013) 21:37–45. doi: 10.3109/10582452.2013.763394
43. Hall, A, Maher, C, Latimer, J, and Ferreira, M. The effectiveness of tai chi for chronic musculoskeletal pain conditions: a systematic review and meta-analysis. Arthr Care Res. (2009) 61:717–24. doi: 10.1002/art.24515
44. Kong, LJ, Lauche, R, Klose, P, Bu, JH, Yang, XC, Guo, CQ, et al. Tai chi for chronic pain conditions: a systematic review and meta-analysis of randomized controlled trials. Sci Rep. (2016) 6:25325. doi: 10.1038/srep25325
45. Fernández-Rodríguez, R, Álvarez-Bueno, C, Cavero-Redondo, I, Torres-Costoso, A, Pozuelo-Carrascosa, DP, Reina-Gutiérrez, S, et al. Best exercise options for reducing pain and disability in adults with chronic low back pain: Pilates, strength, core-based, and mind-body. A network meta-analysis. J Orthop Sports Phys Ther. (2022) 52:505–21. doi: 10.2519/jospt.2022.10671
46. Rainville, J, Hartigan, C, Martinez, E, Limke, J, Jouve, C, and Finno, M. Exercise as a treatment for chronic low back pain. Spine J. (2004) 4:106–15. doi: 10.1016/S1529-9430(03)00174-8
47. Louw, A, Puentedura, EJ, Zimney, K, and Schmidt, S. Know pain, know gain? A perspective on pain neuroscience education in physical therapy. J Orthop Sports Phys Ther. (2016) 46:131–4. doi: 10.2519/jospt.2016.0602
48. Louw, A, Zimney, K, Puentedura, EJ, and Diener, I. The efficacy of pain neuroscience education on musculoskeletal pain: a systematic review of the literature. Physiother Theory Pract. (2016) 32:332–55. doi: 10.1080/09593985.2016.1194646
49. Lo, AW. The adaptive markets hypothesis: market efficiency from an evolutionary perspective. J Portfolio Manage. (2004) 30:15–29. doi: 10.3905/jpm.2004.442611
50. Davis, MC, Zautra, AJ, Wolf, LD, Tennen, H, and Yeung, EW. Mindfulness and cognitive–behavioral interventions for chronic pain: differential effects on daily pain reactivity and stress reactivity. J Consult Clin Psychol. (2015) 83:24–35. doi: 10.1037/a0038200
51. Holtzman, S, and Beggs, RT. Yoga for chronic low back pain: a meta-analysis of randomized controlled trials. Pain Res Manage. (2013) 18:267–72. doi: 10.1155/2013/105919
52. Friedman, NP, and Robbins, TW. The role of prefrontal cortex in cognitive control and executive function. Neuropsychopharmacology. (2022) 47:72–89. doi: 10.1038/s41386-021-01132-0
53. Mayer, JM, Mooney, V, Matheson, LN, Erasala, GN, Verna, JL, Udermann, BE, et al. Continuous low-level heat wrap therapy for the prevention and early phase treatment of delayed-onset muscle soreness of the low back: a randomized controlled trial. Arch Phys Med Rehabil. (2006) 87:1310–7. doi: 10.1016/j.apmr.2006.07.259
54. Busso, T. Variable dose-response relationship between exercise training and performance. Med Sci Sports Exerc. (2003) 35:1188–95. doi: 10.1249/01.MSS.0000074465.13621.37
55. Luiggi-Hernandez, JG, Woo, J, Hamm, M, Greco, CM, Weiner, DK, and Morone, NE. Mindfulness for chronic low back pain: a qualitative analysis. Pain Med. (2018) 19:2138–45. doi: 10.1093/pm/pnx197
56. Arampatzis, A, Schroll, A, Catalá, MM, Laube, G, Schüler, S, and Dreinhofer, K. A random-perturbation therapy in chronic non-specific low-back pain patients: a randomised controlled trial. Eur J Appl Physiol. (2017) 117:2547–60. doi: 10.1007/s00421-017-3742-6
57. Yoo, Y-D, and Lee, Y-S. The effect of core stabilization exercises using a sling on pain and muscle strength of patientswith chronic low back pain. J Phys Ther Sci. (2012) 24:671–4. doi: 10.1589/jpts.24.671
58. Ijzelenberg, W, Oosterhuis, T, Hayden, JA, Koes, BW, Van Tulder, MW, Rubinstein, SM, et al. Exercise therapy for treatment of acute non-specific low back pain: a Cochrane systematic review and meta-analysis of randomised controlled trials. Arch Phys Med Rehabil. (2024) 2023. doi: 10.1002/14651858.CD009365.pub2
59. Williams, D, Consalvo, M, Caplan, S, and Yee, N. Looking for gender: Gender roles and behaviors among online gamers. J Commun. (2009) 59:700–25. doi: 10.1111/j.1460-2466.2009.01453.x
60. Linke, SE, and Ussher, M. Exercise-based treatments for substance use disorders: evidence, theory, and practicality. Am J Drug Alcohol Abuse. (2015) 41:7–15. doi: 10.3109/00952990.2014.976708
61. Côté, S, House, J, and Willer, R. High economic inequality leads higher-income individuals to be less generous. Proc Natl Acad Sci. (2015) 112:15838–43. doi: 10.1073/pnas.1511536112
62. Ne, M. Mindfulness meditation for the treatment of chronic low back pain in older adults: a randomized controlled pilot study. Pain. (2008) 134:310–9. doi: 10.1016/j.pain.2007.04.038
63. Cadmus-Bertram, L, Irwin, M, Alfano, C, Campbell, K, Duggan, C, Foster-Schubert, K, et al. Predicting adherence of adults to a 12-month exercise intervention. J Phys Act Health. (2014) 11:1304–12. doi: 10.1123/jpah.2012-0258
64. Rigsby, MO, Rosen, MI, Beauvais, JE, Cramer, JA, Rainey, PM, O’Malley, SS, et al. Cue-dose training with monetary reinforcement: pilot study of an antiretroviral adherence intervention. J Gen Intern Med. (2000) 15:841–7. doi: 10.1046/j.1525-1497.2000.00127.x
65. Saida, TGRH, Sørensen, TJ, and Langberg, H. Long-term exercise adherence after public health training in at-risk adults. Ann Phys Rehabil Med. (2017) 60:237–43. doi: 10.1016/j.rehab.2017.02.006
66. Robergs, RA. A critical review of the history of low-to moderate-intensity steady-state VO 2 kinetics. Sports Med. (2014) 44:641–53. doi: 10.1007/s40279-014-0161-2
67. Ulger, O, Oz, M, and Asliyuce, YO. The effects of yoga and stabilization exercises in patients with chronic low Back pain: a randomized crossover study. Holist Nurs Pract. (2023) 37:E59–68. doi: 10.1097/HNP.0000000000000593
68. López, CB, Fritz, NB, Campillo, RR, and Sánchez, JCC. Water-based exercise in patients with nonspecific chronic low-Back pain: a systematic review with Meta-analysis. J Strength Cond Res. (2024) 38:216–9. doi: 10.1519/JSC.0000000000004635
69. O'Sullivan, P. It's time for change with the management of non-specific chronic low back pain. BMJ Publishing Group Ltd and British Association of Sport and Exercise Medicine; (2012). p. 224–227.
70. Oliveira, VC, Ferreira, PH, Maher, CG, Pinto, RZ, Refshauge, KM, and Ferreira, ML. Effectiveness of self-management of low back pain: systematic review with meta-analysis. Arthritis Care Res. (2012) 64:1739–48. doi: 10.1002/acr.21737
71. Hsu, W-L, Chen, C-Y, Tsauo, J-Y, and Yang, R-S. Balance control in elderly people with osteoporosis. J Formos Med Assoc. (2014) 113:334–9. doi: 10.1016/j.jfma.2014.02.006
72. Ghorbani Saeedian, R, Nagyova, I, Krokavcova, M, Skorvanek, M, Rosenberger, J, Gdovinova, Z, et al. The role of social support in anxiety and depression among Parkinson’s disease patients. Disabil Rehabil. (2014) 36:2044–9. doi: 10.3109/09638288.2014.886727
73. Gerontoukou, E-I, Michaelidoy, S, Rekleiti, M, Saridi, M, and Souliotis, K. Investigation of anxiety and depression in patients with chronic diseases. Health Psychol Res. (2015) 3:2123. doi: 10.4081/hpr.2015.2123
74. Qaseem, A, Wilt, TJ, McLean, RM, and Forciea, MA. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. (2017) 166:514–30. doi: 10.7326/M16-2367
75. Kirkwood, G, Rampes, H, Tuffrey, V, Richardson, J, and Pilkington, K. Yoga for anxiety: a systematic review of the research evidence. Br J Sports Med. (2005) 39:884–91. doi: 10.1136/bjsm.2005.018069
76. Littlejohns, P, Chalkidou, K, Culyer, AJ, Weale, A, Rid, A, Kieslich, K, et al. National Institute for health and care excellence, social values and healthcare priority setting. J R Soc Med. (2019) 112:173–9. doi: 10.1177/0141076819842846
77. Krenn, C, Horvath, K, Jeitler, K, Zipp, C, Siebenhofer-Kroitzsch, A, and Semlitsch, T. Management of non-specific low back pain in primary care–a systematic overview of recommendations from international evidence-based guidelines. Prim Health Care Res Dev. (2020) 21:e64. doi: 10.1017/S1463423620000626
78. Ranganathan, H, and Singh, DKA. A review of clinical practice guidelines for physiotherapy Management of Patients with non-specific low Back pain. Natl J Commun Med. (2024) 15:405–15. doi: 10.55489/njcm.150520243849
79. Bae, C-R, Jin, Y, Yoon, B-C, Kim, N-H, Park, K-W, and Lee, S-H. Effects of assisted sit-up exercise compared to core stabilization exercise on patients with non-specific low back pain: a randomized controlled trial. J Back Musculoskelet Rehabil. (2018) 31:871–80. doi: 10.3233/BMR-170997
80. Oh, B-H, Kim, H-H, Kim, C-Y, and Nam, C-W. Comparison of physical function according to the lumbar movement method of stabilizing a patient with chronic low back pain. J Phys Ther Sci. (2015) 27:3655–8. doi: 10.1589/jpts.27.3655
81. Cho, I, Jeon, C, Lee, S, Lee, D, and Hwangbo, G. Effects of lumbar stabilization exercise on functional disability and lumbar lordosis angle in patients with chronic low back pain. J Phys Ther Sci. (2015) 27:1983–5. doi: 10.1589/jpts.27.1983
82. Cho, H-y, Kim, E-h, and Kim, J. Effects of the CORE exercise program on pain and active range of motion in patients with chronic low back pain. J Phys Ther Sci. (2014) 26:1237–40. doi: 10.1589/jpts.26.1237
83. Hwangbo, G, Lee, C-W, Kim, S-G, and Kim, H-S. The effects of trunk stability exercise and a combined exercise program on pain, flexibility, and static balance in chronic low back pain patients. J Phys Ther Sci. (2015) 27:1153–5. doi: 10.1589/jpts.27.1153
84. Williams, KA, Petronis, J, Smith, D, Goodrich, D, Wu, J, Ravi, N, et al. Effect of Iyengar yoga therapy for chronic low back pain. Pain. (2005) 115:107–17. doi: 10.1016/j.pain.2005.02.016
85. Lee, J-S, and Kang, S-J. The effects of strength exercise and walking on lumbar function, pain level, and body composition in chronic back pain patients. J Exerc Rehabil. (2016) 12:463–70. doi: 10.12965/jer.1632650.325
86. Michaelson, P, Holmberg, D, Aasa, B, and Aasa, U. High load lifting exercise and low load motor control exercises as interventions for patients with mechanical low back pain: a randomized controlled trial with 24-month follow-up. J Rehabil Med. (2016) 48:456–63. doi: 10.2340/16501977-2091
87. Noormohammadpour, P, Kordi, M, Mansournia, MA, Akbari-Fakhrabadi, M, and Kordi, R. The role of a multi-step core stability exercise program in the treatment of nurses with chronic low back pain: a single-blinded randomized controlled trial. Asian Spine J. (2018) 12:490–502. doi: 10.4184/asj.2018.12.3.490
88. Roh, HS, Cho, WJ, Ryu, WJ, Park, SJ, and An, CS. The change of pain and lumbosacral sagittal alignment after sling exercise therapy for patients with chronic low back pain. J Phys Ther Sci. (2016) 28:2789–92. doi: 10.1589/jpts.28.2789
89. Tekur, P, Nagarathna, R, Chametcha, S, Hankey, A, and Nagendra, H. A comprehensive yoga programs improves pain, anxiety and depression in chronic low back pain patients more than exercise: an RCT. Complement Ther Med. (2012) 20:107–18. doi: 10.1016/j.ctim.2011.12.009
90. Ulger, O, Demirel, A, Oz, M, and Tamer, S. The effect of manual therapy and exercise in patients with chronic low back pain: double blind randomized controlled trial. J Back Musculoskelet Rehabil. (2017) 30:1303–9. doi: 10.3233/BMR-169673
91. Williams, K, Abildso, C, Steinberg, L, Doyle, E, Epstein, B, Smith, D, et al. Evaluation of the effectiveness and efficacy of Iyengar yoga therapy on chronic low back pain. Spine. (2009) 34:2066–76. doi: 10.1097/BRS.0b013e3181b315cc
Keywords: chronic low back pain, exercise prescription, network meta-analysis, Tai Chi, intervention effectiveness
Citation: Zhao K, Zhang P, Li H and Li L (2025) Exercise prescription for improving chronic low back pain in adults: a network meta-analysis. Front. Public Health. 13:1512450. doi: 10.3389/fpubh.2025.1512450
Edited by:
Eleuterio A. Sánchez Romero, Hospital Universitario Puerta de Hierro Majadahonda, SpainReviewed by:
Manuela Deodato, University of Trieste, ItalyPaul Silvian, King Khalid University, Saudi Arabia
Copyright © 2025 Zhao, Zhang, Li and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ping Zhang, emhhbmdwaW5nQGhyYmlwZS5lZHUuY24=
 Ke Zhao
Ke Zhao Ping Zhang
Ping Zhang Hua Li
Hua Li Li Li
Li Li