- 1College of Nursing Science, Kyung Hee University, Seoul, Republic of Korea
- 2East-West Nursing Research Institute, Kyung Hee University, Seoul, Republic of Korea
- 3Department of Nursing, Graduate School, Kyung Hee University, Seoul, Republic of Korea
Introduction: Long-term care hospitals (LTCHs) faced challenges beyond the scope of their previous practice in response to the pandemic. However, not much is known about LTCHs' responses and business continuity plans (BCPs) during the pandemic. We investigated attempts by LTCHs to maintain continuity of operation during COVID-19 in order to gain insight on how to support them in future crises.
Methods: A mixed-method design was used, comprising a survey and individual interviews, to understand the responses and measures taken to address the pandemic.
Results: For LTCHs, inpatient ward operations were identified as an essential function. Following the government's recommendation, most (85.7%) confirmed having BCPs, but over half felt that the operational effectiveness of BCPs was inadequate. Only 9.5% formed teams dedicated to infectious disease emergency preparedness and response before COVID-19. Qualitative analysis identified six main themes that explained the efforts of the LTCHs: workplace culture and leadership, communication, human resources, safety, continuity of essential services, and financial and supply management. The themes explained the reasons for operational effectiveness and provided examples and context on how staff responded in small and medium-sized LTCHs during the pandemic, considering elements in health service continuity planning.
Conclusion: Management of significant changes forced by the pandemic necessitates preparing a response that considers key components beforehand, particularly for vulnerable healthcare facilities. To address unexpected crises, LTCHs should develop, implement, and practice well-thought-out plans to enhance organizational resiliency and ensure continued hospital functioning.
1 Introduction
The COVID-19 pandemic has posed unprecedented challenges to healthcare systems worldwide, with long-term care facilities being among the most critically affected (1). In long-term care settings, such an infection can rapidly spread by human-to-human transmission through direct contact or droplets (2, 3). As major long-term care facilities, long-term care hospitals (LTCHs) in Korea are hospitals that provide medical services to patients requiring extended care, primarily those with advanced age and a range of chronic underlying conditions (4, 5). These long-term care recipients are highly susceptible to the emerging infectious disease; 94.7% of LTCHs reported experiencing an outbreak in 2022 (6, 7). LTCHs across Korea have become focal points for COVID-19 outbreaks, reporting higher fatality rates (12%) than the domestic COVID-19 fatality rate (1.75%) during the first year since the initial case in Korea (8).
Given LTCHs' significant role in this era of aging, it is necessary to ensure that LTCHs respond appropriately when faced with various risks pertaining to calamities, such as infectious disease outbreaks (9). Managing the spread of the COVID-19 and changes within LTCHs entailed complex challenges that extended beyond standard healthcare practices, including testing all contacts and setting cohorts (10–12). According to an existing review (13) and the related literature (14), some actions taken to adapt to external/internal demand during the pandemic by resilient hospitals were beneficial based on preparedness, whereas measures implemented by other hospitals revealed vulnerabilities.
As such, the pandemic has highlighted the importance of building hospital resilience. Hospital resilience refers to a system's capacity to promptly and effectively withstand, absorb, adapt to, and recover from the impacts of hazards (15, 16). Several studies have found indicators to assess disaster-resilient hospitals, including leadership, in-hospital business continuity plan (BCP), and hospital management for disaster risk reduction (17–19). Importantly, pandemic plans as part of BCP focus on enabling critical hospital functions and strengthening preparedness for a disaster (20, 21). Healthcare facilities need to prepare for and respond to crises by considering these factors.
Concerning biological hazards, hospital resilience during COVID-19 has been explored in the literature, but it is still relatively limited, including the actual participation of frontline hospitals (16, 22). There is a need for further research to enhance hospital resilience in resource-constrained and fragile settings and to offer practical guidance (16). From empirical works, a study explored hospital resilience throughout the COVID-19 recovery in the Eastern Mediterranean Region, and the need for service continuity planning was highlighted as one of the hospital roles (23). Another paper conducted in the Eastern Mediterranean Region emphasized the necessity of preventive and proactive contingency planning and strengthening preparedness capacities for such planning (24). Moreover, a recent study of hospital resilience factors in China (22) mentioned a demand for adjustment and optimization of response plans during a pandemic. However, prior studies had some drawbacks in guiding effective future actions. There was no limitation on the type or size of the healthcare facilities covered in the studies, and they did not give enough attention to the pandemic responses, considering the extent to which BCPs had been prepared in reality.
Existing research shows a wide range of aspects regarding pandemic responses, including lessons learned from experience on hospital resilience to the pandemic (24–26). An existing qualitative literature review on healthcare professionals' adaptation to COVID-19 (13), focusing on clinical settings for physical conditions, identified themes including an intensified need for individual and team capacity to handle changes in working conditions, as well as shifts in healthcare organizations to address the challenges of the pandemic. While a qualitative study focused on outbreak management by frontline workers and leaders during the pandemic in long-term care in Canada (11), many others examined psychological burdens and challenges in this setting (27, 28). To the best of our knowledge, studies considering the components of hospital resilience in vulnerable settings, especially small and medium-sized private LTCHs, during the pandemic are scarce. How these LTCHs should have navigated hospital operations rapidly in the face of limited resources during COVID-19 remains unclear. To foster LTCHs' preparedness and organizational resilience, it is important to understand how LTCHs respond to disruptions, and continue providing quality care and functioning during such unexpected crises. Addressing these research gaps, this study uses mixed methods to investigate LTCHs' perceptions of and practical responses to upholding hospital business continuity during the pandemic, considering key elements related to hospital emergency response.
2 Methods
2.1 Design
We study adopted a mixed methods approach (29) to explore LTCHs' responses considering hospital business continuity during COVID-19. This study was conducted during the COVID-19 pandemic, from August to November 2022 with cohorts of HCWs who manage the pandemic in LTCHs in South Korea. In the first phase, quantitative research was conducted via an online survey of healthcare workers (HCWs) in LTCHs in accordance with the aims of this study (Phase 1). This was followed by a second phase of qualitative data collection through semi-structured interviews with HCWs in selected hospitals to further explore in-depth views on responding to the pandemic in LTCHs (Phase 2). The researchers followed the STROBE and COREQ checklists to report this study.
2.2 Data collection and sampling
2.2.1 Quantitative
In the quantitative phase, we conducted a cross-sectional and exploratory study. The participants in the online survey were HCWs, specifically infection control professionals (ICPs) of LTCHs. HCWs were eligible to participate if they were designated to perform infection control duties and were working in small and medium-sized LTCHs for at least the prior 6 months. Those who did not work during the pandemic were excluded. This sample considered ICPs as representatives from LTCHs, given their pivotal role in emergency preparedness, responses, and decision-making (30, 31). Using a recruitment flier, the link to the survey was distributed to LTCHs and professional associations, including the Korean Small and Medium Hospital Association (KSMHA), and the Korean Association of Infection Control Nurses (KAICN). These associations shared the link through their social networks/websites, where participants could complete the surveys. All the questionnaires were completed anonymously.
2.2.2 Survey development and administration
The survey was developed with the aim of understanding LTCHs' response status to ensure continuity of operation during the pandemic. Survey questions were developed based on a review of relevant sources, including the BCP checklists provided by the Ministry of Employment and Labor (32), the World Health Organization's (WHO) hospital emergency response checklist (33), and guidelines from the Central Disaster Management Headquarters (34). The questionnaire covered domains related to business continuity planning, governance and control, communication, and resource management, including human resources and finance. For an assessment of face validity, clarity, and completeness of the survey, the questionnaire was reviewed, commented on, and revised by six experts in the field, and pilot-tested by HCWs before being implemented in the study. Following this, consensus on a final version of the survey was achieved.
2.2.3 Qualitative
Semi-structured, key informant interviews were utilized to collect data. Based on an extensive literature review, an interview guide was developed to provide a general outline of the interviews and to understand the perceived and actual responses to the pandemic in LTCHs based on the findings of the quantitative phase (see Supplementary Table 1). The guide questions were devised to capture the participants' professional experiences and their hospitals' responses to the pandemic, piloted with HCWs to gather feedback on content, flow, and cohesion, and refined for contextual relevance. The guide included aspects regarding general response experience, and experiences related to disruption threats and BCP during COVID-19. For this phase, key informants were defined as HCWs, who are leaders involved in outbreak management in LTCHs; they represented HCWs in LTCHs to provide the best explanations of the pandemic responses. Purposive sampling supplemented by snowball sampling was employed to obtain a sample of HCWs, especially various team leaders with direct experience in LTCHs, including physicians, nurses, and administrators, each of with at least 6 months of experience in their respective roles. The sample size was decided considering saturation and literature (35).
2.3 Data analysis
2.3.1 Quantitative
The statistical software package SPSS version 25 (IBM Corp., Armonk, NY, USA) was used for quantitative analysis. Descriptive statistics, including means and standard deviations, were used to summarize the responses to the questionnaires.
2.3.2 Qualitative
All recorded interviews were transcribed into text, and thematic analysis was employed to analyze responses following the framework of Braun and Clark (36). The method includes six steps: familiarizing with the transcribed text; generating initial codes; collecting codes for potential themes; checking if the themes align with the coded segments; refining each theme; and writing a report with examples and quotations. Once two researchers read transcripts of all interviews, initial codes were independently created to capture recurring themes across responses. Codes were reviewed and analyzed collaboratively by three researchers (two of whom were nursing researchers; the other had methodology expertise) considering components of the WHO hospital emergency response checklist (33). Themes were reviewed and discussed by the research team. To ensure trustworthiness and validity of the findings (37), team members collaborated through several research team meetings to reach an agreement on emerging patterns, themes, and sample quotes until no new themes were identified. Coding and qualitative analyses were performed using NVivo14 (QRS International, Melbourne Australia). We used a coding framework and member checking for the credibility of this study. Peer debriefing in the research process was conducted to minimize researcher bias.
2.4 Ethical considerations
This study was approved by the Institutional Review Board of Kyung Hee University (No. KHSIRB-22-380).
3 Results
3.1 Quantitative findings
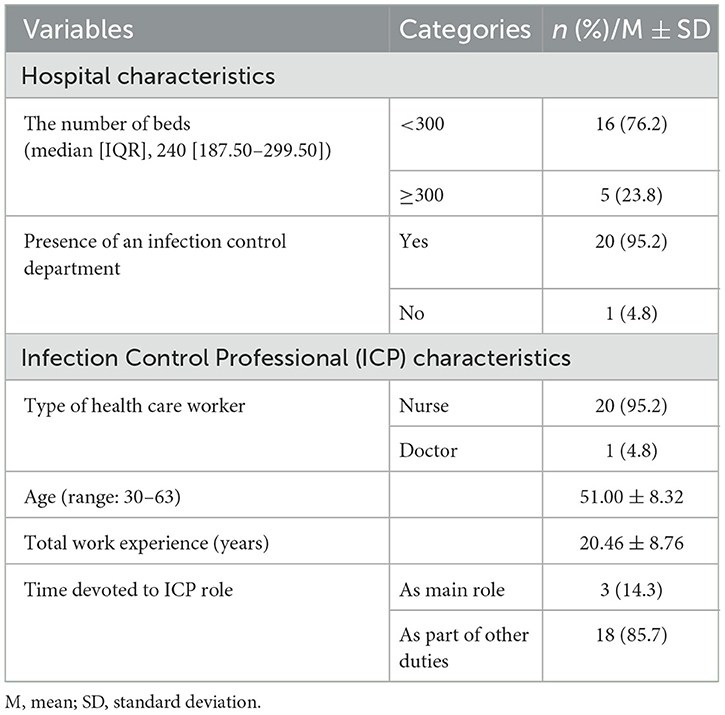
Table 1 summarizes the characteristics of the HCWs and affiliated LTCHs. Most LTCHs (76.2%) were small and medium-sized hospitals with fewer than 300 beds, and 95.2% had an Infection Control Department. Participants were Infection Control Professionals (ICPs) representing 21 private LTCHs. Almost all ICPs were nurses (95.2%), and more than 80% reported concurrently holding responsibilities for additional roles. The mean age of the sample was 51.00 years (SD = 8.32), and the mean years of total clinical experience was 20.46 (SD = 8.76).
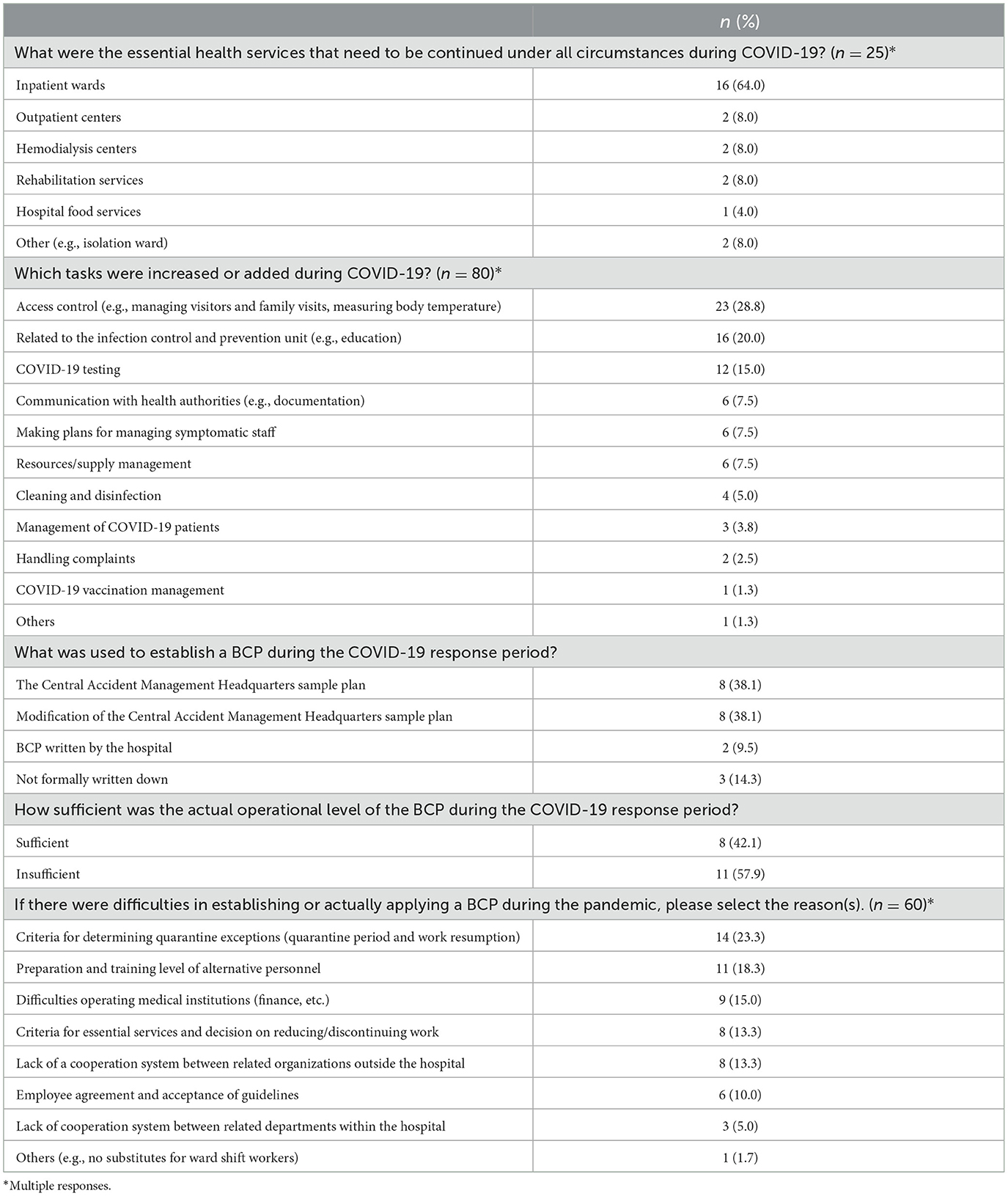
3.1.1 Hospital business continuity planning
Most hospitals (85.7%) reported that they developed BCPs following government recommendations (see Table 2). Of those that had established BCPs, almost all utilized the government-provided plans by either adopting it as is or modifying it. However, 57.9% of the respondents believed that the operational status of BCPs during COVID-19 was insufficient. The reasons for difficulties in establishing/applying a BCP during the pandemic included challenges in determining the criteria for quarantine exclusion, difficulties preparing alternative staff to perform tasks, and financial issues with operating medical institutions.
3.1.1.1 Critical operations that needed to be continued
When asked about the essential functions of LTCHs, inpatient ward operations (64%), including patient admission and care, were the most frequently reported. Some respondents also mentioned outpatient services, hemodialysis centers, rehabilitation services, and hospital food services (8%, 8%, 8%, and 4%, respectively).
3.1.1.2 New/intensified operations in response to COVID-19
Regarding the new/intensified operations necessary after the onset of COVID-19, access control (28.8%), including measuring body temperature and managing visitors and family visits, was the most frequently mentioned. This was followed by tasks associated with the Infection Control and Prevention Unit (20%) and COVID-19 testing (15%).
3.1.2 Responses based on key components
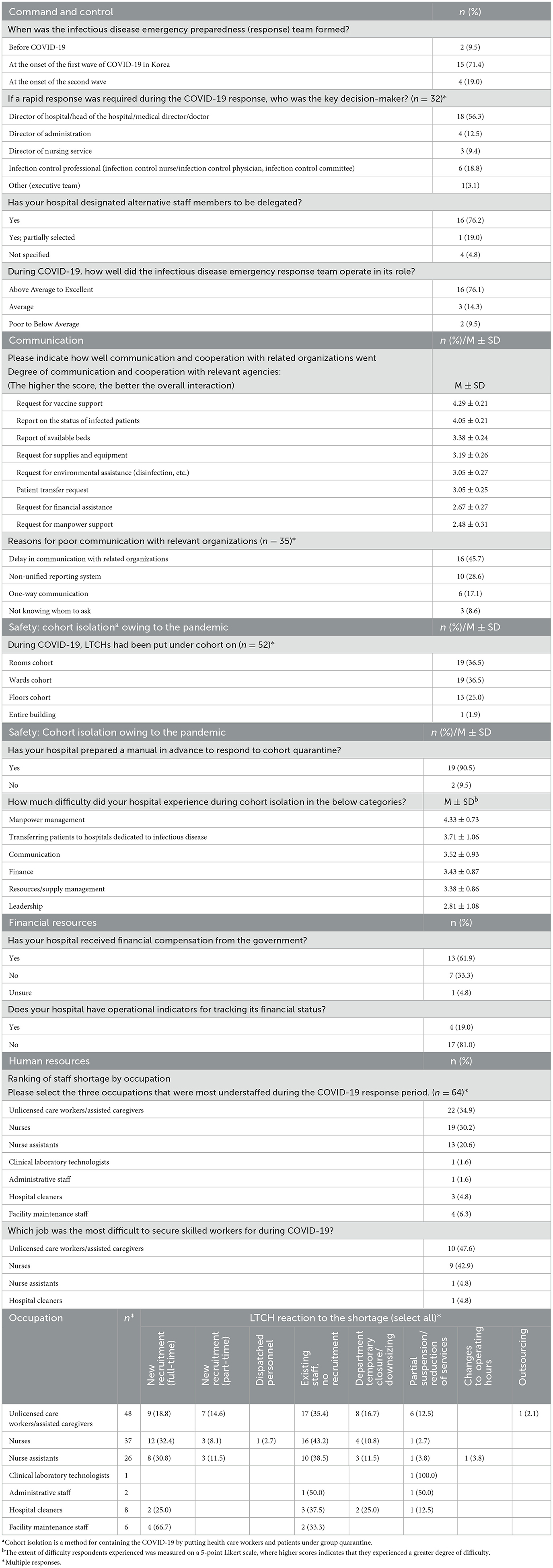
3.1.2.1 Command and control
Following the onset of the first wave of COVID-19, 71.4% of the respondents established a team responsible for infectious disease emergency preparedness and response as shown in Table 3. Only 9.5% of respondents had formed such a team before the pandemic. Regarding key decision-makers within the team, most respondents (56.3%) identified the hospital director. Over 70% reported having alternatives in the case of absent team members. Regarding operational effectiveness, 76.1% rated the team's operations as above average to excellent in fulfilling its roles.
3.1.2.2 Communication
Between LTCHs and relevant agencies during COVID-19, the most effective communication was related to requests for vaccine support (4.29 ± 0.21), while the least was related to requests for manpower support (2.48 ± 0.31) and financial assistance (2.67 ± 0.27). Reasons cited for poor communication with relevant agencies (such as public health centers and local governments) included communication delays, non-unified reporting systems, and one-way communication.
3.1.2.3 Cohort isolation
All respondents reported that their hospitals implemented some form of cohort isolation (including types of isolation at the room and ward levels, floor level, and the entire building) during COVID-19. Although a substantial number of LTCHs (90.5%) had prepared manuals for implementing cohort isolation, they encountered several challenges. The most difficult one was managing manpower (4.33 ± 0.73), followed by transferring COVID-19 patients to hospitals dedicated to managing infectious diseases (3.71 ± 1.06).
3.1.2.4 Human resources
Considering the rankings individually, staff shortage was most severe among nurses, then among unlicensed hospital-based care workers (ganbyeongin)/care assistants, and then among nursing assistants. Furthermore, when combining the shortfalls in staffing for the three highest ranks, LTCHs experienced staff shortages, with unlicensed care workers (ganbyeongin)/care assistants (34.9%) being the most frequently reported, followed by nurses (30.3%) and nurse assistants (21.2%). Additionally, the jobs that were most difficult to find skilled individuals for during COVID-19 were nurses and unlicensed care workers/care assistants. In response to staff shortages, most LTCHs explored various options, including operating with existing staff without recruitment, new recruits, and partial the suspension/reduction of services.
3.1.2.5 Financial resource
More than half of the LTCHs (61.9%) reported receiving financial compensation from the government to mitigate losses incurred due to COVID-19. Nevertheless, the majority (81%) did not monitor indicators that reflected their financial status.
3.2 Qualitative findings
Eleven semi-structured interviews were conducted. The participants were frontline leaders and middle managers responsible for leading staff, such as hospital directors, directors of nursing and food services, and other health care workers (e.g., nutritionists, physical therapists, and administrative staff). The mean age of the respondents in our qualitative sample was 48.91 years (SD = 9.35, range = 36–66), and the mean years of clinical experience was 16.64 years (SD = 10.88, range = 2–42); most were female (63%, n = 7). The participants' information and summary of responses to identified themes are presented in Supplementary Tables 2, 3.
Six main themes, with each theme having sub-themes were identified from the interviews regarding responses to COVID-19 to maintain LTCHs' operational continuity. The six themes were: workplace culture and leadership, communication, human resource, safety, continuity of essential service, and financial and supply resources. The following interpretations demonstrate the themes along with participants' statements.
3.2.1 Theme 1: workplace culture and leadership response
In LTCHs, workplace culture and leadership were considered forces alleviating the challenges of the pandemic in settings with scarce resources to plan and prepare. The efforts of the hospital staff members and the strong leadership structure centered around the hospital owner and director in small and medium-sized hospitals were related to this response.
3.2.1.1 Responding to the crisis based on the strong bond between staff members
Workplace culture response was manifest through strong cohesion and a culture of collective orientation, a mutual cooperative atmosphere, and employees' sense of responsibility. LTCHs in which pre-pandemic workplace culture was positive continued to benefit from these influences during the pandemic. This atmosphere helped the staff endure the circumstances by inspiring a sense of community and voluntary sacrifice. The following is an example:
“All the staff members had a sympathetic heart. They worked long hours and came to work to cover each other's duties. Even the director of nursing hadn't been home for almost two weeks and continued to take care of patients on the ward. Before the Omicron variant, the hospital was completely locked down and nobody could go home. It was not because they caught the virus, but because there were many people who volunteered to stay and do their work” (Director of nutrition services).
3.2.1.2 Dealing with the pandemic through hospital leadership
Crisis leadership was identified as an indispensable strategy to prevent the disruption of privately-owned LTCHs. As an important leadership response, hospital leaders' behavior described by participants included their high levels of consideration, ability to instill trust among their members, and attempts to be a good role model. Leaders with these attributes showing how to respond to crisis by example can become a source of endurance and a facilitator for their intense work together. One stated that:
“In any case, for the shifts to be covered, there needs to be a minimum staffing level... So, for those gaps, the nursing supervisor or doctors can just... I, as the hospital director, have had to come and go a bit at night without sleeping. As a director, I thought, ‘I really have to show that I'm willing to go through hell. I have to be the first to endure it.' Otherwise, it wouldn't work. So, it's literally like that. If the captain of a sinking ship is the first to run away, then everything just falls apart, right?” (Hospital director).
3.2.2 Theme 2: communication response
Multiple HCWs expressed how they responded to the situation by communicating with relevant stakeholders and neighboring LTCHs for decision-making and collaboration. They mobilized the communication channels they had been using in their personal sphere for their institutional response during the pandemic.
3.2.2.1 Expanding intra-organizational communication via social networking platforms
As 24-hour communication channels, mobile technology and social network services (SNS) helped provide better communication between HCWs in LTCHs. Participants stated that while larger tertiary hospitals tended to have their own internal intranet and communication channels, smaller providers relied on freely available SNS, just like they did. Participants also remarked how they communicated with each other using SNS/mobile apps to respond quickly, and share information with various departments inside the organization, including head nurses, administrative departments, and team leaders. This was reflected in responses such as, “Announcements about constantly changing responses... We use KakaoTalk.” (Director of Nursing) This facilitated communication, in turn, became possible to support LTCHs' communication with health authorities, including public health centers.
3.2.2.2 Expanding inter-organizational communication via social capital
Information about the pandemic, including practice guidelines for treatment and management that reflect real situations, was limited and not readily available. It was crucial to obtain and share the know-how for HCWs to respond to this newly emerging virus and its impact. Participants explained this interaction:
“For those with more severe conditions, I have heard Remdesivir works better. Since we began exchanging information with other LTCH directors, we also tailored treatments with dexamethasone when necessary. We do not just follow the guidelines from the Disease Control and Prevention Agency; our approach is grounded in our real, firsthand experiences. By acting on the collective experiences of directors, we have seen a significant reduction in patient severity” (Hospital director).
3.2.3 Theme 3: human resource response
The third theme, human resource response, captures a situation in which a large number of care staff is required in LTCHs due to the high number of long-term bedridden patients. Human resource responses were the most frequently reported. This theme encompassed utilizing short-term recruitment strategies for prompt response, division of duties among existing employees, efforts to retain staff through compensation and support, and multifaceted efforts to minimize employee exposure to infection risk.
3.2.3.1 Recruitment: utilizing short-term recruitment strategies for prompt response measures
Due to LTCHs' difficult working conditions and low wages, recruitment was cited as an ongoing challenge that existed before the pandemic, but worsened during the pandemic. In particular, for unlicensed care workers, LTCHs preferred to hire ethnic migrant workers mostly from China (Joseonjok) and Central Asia (Koryo Saram), because domestic care workers were hard to find and had higher wages even before the pandemic. Restrictions on traveling due to COVID-19 prevented them from returning to Korea, further exacerbating staffing levels. To address staffing issues, stopgap measures were taken, including hiring unlicensed care workers (ganbyeongin) by increasing daily wages, replacing nurses with nurse assistants, and checking the availability of temporary staff with contracts at other hospitals or with the government. Some quoted issues related to care workers and nurses.
“The director just called in external care workers (ganbyeongin) who had either tested positive for COVID-19 or had cared for COVID-19 patients. If they were paid around 100,000 won a day at other hospitals, we paid them 300,000 won, even if it meant spending more money. So, we tried to keep them for a few days. But these people don't have any attachment to our hospital.” (Director of nursing).
“Many RNs quit…so, I said that I would manage the hospital with the nurse staffing grade 1 (based on nursing staff-to-patient ratio) without nurses, only with our nursing assistants.” *Nursing staffing grades go from 1 to 7, with 1 being the highest nurse staffing level (as an indicator of the quality care) (Director of nursing).
3.2.3.2 Workforce arrangement: division of duties among existing employees
Deployment of existing health workers by changing the arrangement of staff and their duties was required due to the shortage of available HCWs. Division of duties among current staff included multitasking, modification of employee quarantine period depending on the situation, operation centered on middle managers (e.g., head nurses), patience of non-infected staff members until the quarantine period of the COVID-infected staff ends, working with adjusted schedules (e.g., double shifts, overtime, reduced break time, and solo night shift), and the handling additional tasks related to infection control. Many respondents described additional roles beyond their existing responsibilities (e.g., multitasking) in the care environment.
“Physical therapists supported others. Like... (in a soft voice) packing lunchboxes or something along those lines. For me, it was my first time dealing with COVID-19, and honestly, transporting COVID patients... We didn't have to usually do the disinfection in that way, because there is a company for that. But, because of COVID-19, we had to do all the disinfection ourselves” (Administrative staff).
“Actually, it was tough, but during that time, we had to work without enough staff, so all the staff ended up doing double shifts, and head nurses were deployed for night duties, and so on” (Infection control nurse).
3.2.3.3 Workforce retention: efforts to retain staff through compensation and support
It is vital to retain staff for operating hospitals and providing quality care. During the pandemic, compensation and support were frequently mentioned strategies, as the pandemic amplified HCWs' stress and turnover. Participants reported financial compensation as a motivational measure, as well as efforts to support and comfort employees (e.g., buying snacks or supporting staff by verbally motivating them).
“While there weren't salary increases or anything like that, we did provide a lot of snacks and engaged in a lot of conversations with the intention of saying we were all in this together, trying to overcome it collectively. Additionally, we have team leaders for care workers (ganbyeongin) now. We asked these team leaders to provide some extra care for them” (Administrative staff).
3.2.3.4 Minimization of employee exposure to infection risk
LTCHs took a multifaceted approach to prevent staff shortages due to staff infections and their isolation. These included encouraging more HCWs to receive COVID-19 vaccination, performing extra self-testing to avoid being the source of infection, minimizing non-essential interactions among current staff, limiting excursions to crowded places during time off, supplying PPE, and educating staff. Through these measures, they not only protected the workforce, but also ensured the continuity of hospital operations.
“Um... somewhat, (nervous laugh) in a slightly coercive manner, like taking pictures of each employee at around 8 or 9 in the evening to ensure they were at home. We implemented a bit of control, not exactly control, but more like monitoring, I guess” (Administrative staff).
“Other departments may follow guidelines, conducting PCR tests twice a week at the public health centers and self-testing with antigen kits three times a week. In our department, in addition to those guidelines, we perform self-testing with antigen kits every day before coming to work …Furthermore, we monitored temperature changes in the morning, afternoon, and evening” (Director of rehabilitation).
3.2.4 Theme 4: safety response
To reduce the number of infected patients and fatalities caused by COVID-19, safety measures were noted to be critical responses. These measures include changes in decisions regarding transfers and infection prevention for patients and visitors.
3.2.4.1 Changes in decisions regarding transfers
During the early stages, the rapid transfer of infected patients to designated hospitals was considered the first approach for controlling infection and caring for infected patients. Later, as transfer delays occurred due to the capacity limitations of designated hospitals, the participants reported associated concerns and changes in responses.
“At the very beginning, when beds were still available at the designated hospitals, they would admit the patients promptly. However, as time passed, the rooms for transferring COVID-19 patients did not become available. There was a time when we had to wait for up to three days. Initially, when it happened, we managed like that, but later on, the transfers were too delayed...Even when they were transferred to the designated hospitals, they (the designated hospitals) did not look after the patients as...(pauses) well as we did. They do not care as well; therefore, we decided to take care of them ourselves and provide proper treatment” (Infection control nurse).
3.2.4.2 Infection prevention for patients and visitors
Proactive activities related to preventing infection used by LCTHs involved organizing isolation areas, disinfecting environments, ventilation by opening windows, vaccinating patients, conducting mandatory preemptive PCR testing/comprehensive patient testing, strictly controlling outsider access (vendors, visitors). Amid the changing situation and evolving visitation guidelines announced by the government, the implementation of family visits was particularly important in LTCHs. Adjusting the visitation methods (e.g., contact-free visits and video calls) to fit the situation was necessary. For instance, one shared:
“We conduct (non-contact visits) every time. The patient's family makes a reservation in advance and brings a rapid test kit. (After conducting the COVID-19 rapid test), they then wear protective clothing like a PPE gown and gloves, and change their masks, before proceeding downstairs like that. (The family) meets the patient from outside the transparent barrier... For setting up non-contact visits, we tried everything…It took several tries to get it right” (Infection control nurse).
LTCHs had to address the vulnerability of physical spaces within LTCHs to accommodate the increase in infected patients and the remaining uninfected patients. HCWs described difficulties in securing designated pathways to separate clean and contaminated areas. One of the efforts to use a separate entrance/route was to avoid using the elevator; instead, stairs were used when transporting supplies.
“Since there was only one elevator, we had to bring down the waste. All the meals were provided to the ward in disposable containers, but the thought of putting those containers in the elevator made us feel like something might come out of it. Really. Even after disinfecting, we were still scared, so we carried everything up to the 4th floor using the stairs, every single meal. All the staff... We kept doing it throughout the entire cohort isolation period...” (Infection control nurse).
3.2.5 Theme 5: response to the continuity of essential services
Participants experienced the discontinuation of unnecessary functions and a lag in the development of the action plan for maintaining essential services.
3.2.5.1 Suspension of non-essential functions
Identifying priority functions in the context of the pandemic led to the closure of non-essential services. In addition to medical care, some respondents considered hospital food service operations, medical billing claim reviews, and personal care from non-licensed care workers (live-in care workers providing ongoing care) difficult to replace. HCWs described how prioritization could be applied.
“Everyone was still coming to work, but we had to close the rehabilitation room. That was the only place we could close. Patients from the second and third floors got mixed up [in the rehabilitation room]. Oh, there is one more place. Traditional Korean medicine treatment is also considered part of the supplementary services, you know...That is why we had to stop operations at those two places” (Director of nursing).
3.2.5.2 Shifting perceptions of response planning
Regarding the activation of hospital responses, efforts to devise operational plans assuming the impact of the COVID-19 were noted. Ad hoc planning after the occurrence of the infected patients was cited. HCWs experienced increased awareness of the severity and the need for action planning after the emergence of their own confirmed cases.
“From the time we got our first patient, we started making more specific plans. Before that, we had a bit of an attitude of 'it won't happen to us.' We hadn't had any cases for a long time, so we trusted that everyone was doing well and believed we wouldn't be affected. But after we had a case, we started making two-week plans continuously from that point on” (Administration staff).
3.2.6 Theme 6: response to financial and supply resources
Handling the loss of financial resources and maintaining essential supplies were important issues for the emergency response during the pandemic.
3.2.6.1 Bearing losses with constrained finances
LTCHs experienced a decline in patient admissions, which led to a decrease in revenue. The decline in patient admissions was due to the stigma of being seen as a hospital connected to the outbreak and to patients not returning after being transferred to designated hospitals. Importantly, insufficient contingency funding, which did not account for potential financial impacts/barriers in planning seemed to have had an unfavorable effect on the response capacity.
“The chaos caused by COVID-19 is almost unprecedented. This was the case across the country, and hospitals probably approached it with a mindset of accepting some level of loss and expense. [We] likely aimed to minimize this as much as possible. The reserve funds were only held to the extent required for achieving LTCHs accreditation. Since COVID-19 was rapidly spreading, we were in a position where we had to prevent it. As a result, we had to act quickly, which inevitably incurred costs” (Director of administration).
The government required accurate documentation and evidence of LTCHs' response activities, including waste disposal costs, which led to delays in receiving compensation or resulted in some LTCHs being unable to receive compensation or receiving only partial compensation. One described difficulty in proving their losses for reimbursement.
“We were only able to repay half (of the loan) due to the actual loss. The money we claimed from the public health center and the Health Insurance Review and Assessment Service—well, for waste disposal and so on—is difficult to prove… It was difficult to compare with the waste from before” (Infection control nurse).
3.2.6.2 Efforts to secure uninterrupted supplies
Some protective equipment was partially provided by the government. However, because it only served as a supplement, informants expended considerable effort on supplies by searching for available sources, such as via the Internet and public organizations, and spending a lot of money to maintain supply levels to manage situations. It was related to the lack of preparedness in identifying and securing suppliers for essential medical supplies.
“…Since the supplies were tightly managed, we also ordered a lot of motorcycle couriers (called quick service). When regular delivery was not possible, we paid extra and used lots of same-day delivery. Things like face shields are indispensable. Initially, we discarded them after use, but later, we wiped and reused them” (Infection control nurse).
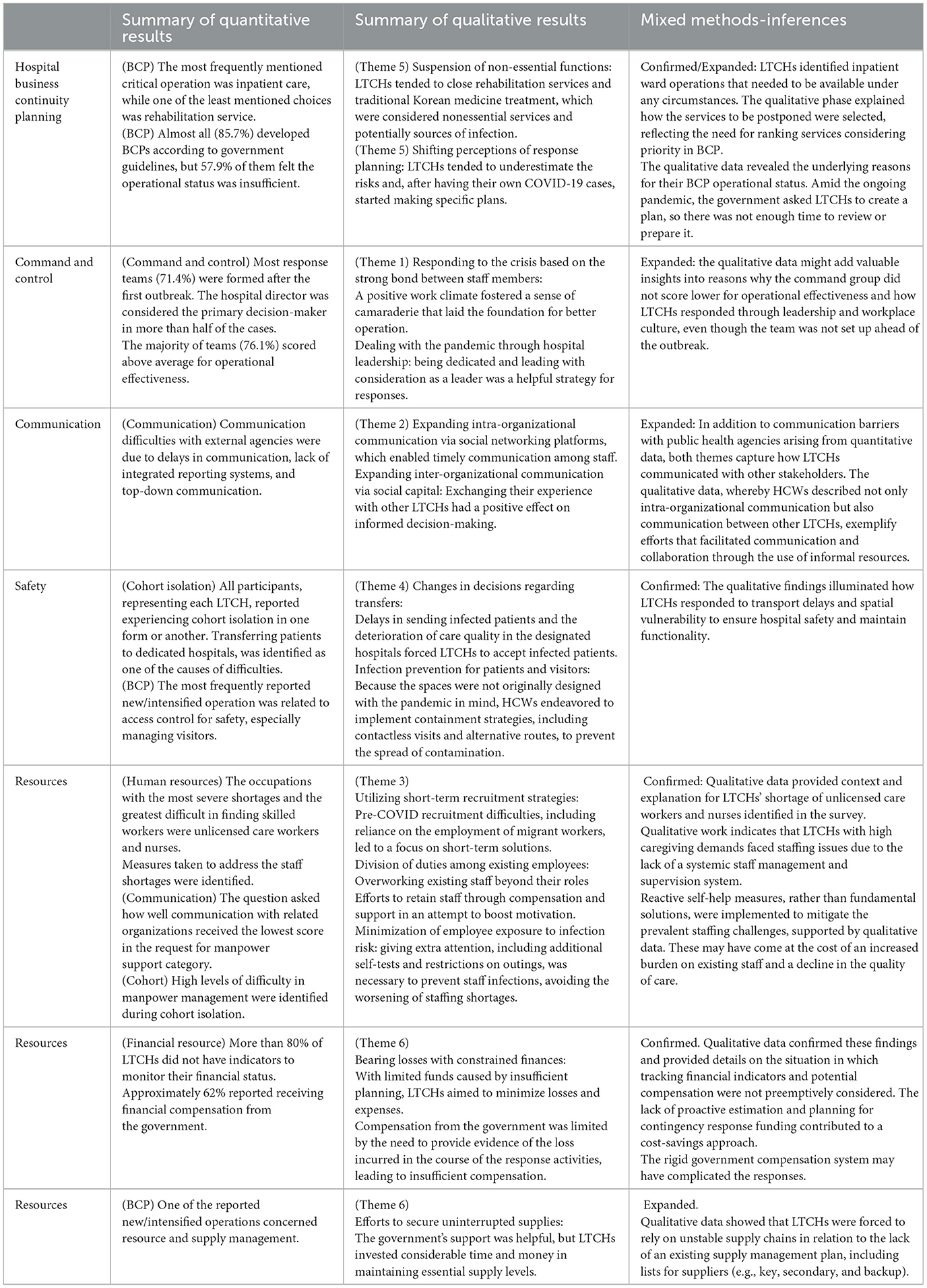
3.3 Integration of quantitative and qualitative findings
The integration of qualitative and quantitative data provided greater insights into LTCHs' responses for the continuity of healthcare services. The findings from the qualitative phase, providing contextual meaning and examples, confirmed and expanded the quantitative findings. Table 4 presents a joint display of the pandemic responses among LTCHs based on the integrated analysis.
4 Discussion
This study shows a range of pandemic responses among HCWs in LTCHs from a mixed perspective, considering both quantitative and qualitative data. This study applied qualitative data to gain more detailed information about responses in order to explain and complement the quantitative findings. This study can enhance our understanding of their circumstances and assess whether any components were left out in the responses.
Regarding BCP and response to the continuity of essential service, both quantitative and qualitative data indicate that in LTCHs, inpatient services were perceived as a critical function. However, they experienced some disruptions to rehabilitation services, which were deprioritized compared to other primary care services during the pandemic. Rehabilitation rooms were at risk of spreading the infection due to the need for direct patient contact and the high possibility of patients mixing together. The grounds for selecting operations in LTCHs were supported by qualitative data, which provided additional insights. Different from LTCHs in Korea, hospitals in Delhi (18) identified the emergency department as a critical function, as it is based on hospital type and specific circumstances. During the pandemic, a recent study showed that a hospital in Singapore identified orthopedic surgery as an essential service, reviewed and postponed non-urgent elective surgeries, and reduced outpatient visits to continue providing core musculoskeletal care (38). Further to this, during the pandemic, despite local differences in the choice of which specific services to maintain, hospitals prioritized essential services and canceled/postponed non-urgent care in countries in the WHO European region and Canada (39). In health service continuity planning as an ongoing and proactive process, identifying critical functions and recovery time objectives for each hospital based on its unique situation is necessary, and thus helps LTCHs reprioritize resources and efforts to continue their essential services (19, 40).
In addition, we found that many LTCHs quickly created BCPs using sample plans, but their operational status appeared to be unsatisfactory. The qualitative results, in which HCWs described their experiences of making action plans once they received their first confirmed case, help explain inefficient BCP implementation. The combined data showed that they may have experienced difficulties in building and implementing BCPs in situations with limited time and resources, including setting criteria for quarantine and essential services. While developing and testing BCPs tends to take several months, LTCHs in Korea had to create BCPs within just a few weeks for the first time because the government urged planning due to the pandemic. This has been criticized for mainly focusing on the reduction of isolation periods rather than properly reflecting the realities in each case (41, 42). Similarly, during the response to COVID-19, as their initial response, many countries focused on planning in hospitals; some countries determined the overall response, while others provided guidance, and left individual hospitals responsible for how they implemented the measures (39). Therefore, LTCHs should plan for a potential pandemic with a permanent BCP committee, taking the time to develop a BCP that covers all the critical components and periodically updating it (19, 20); in turn, their BCP would be effectively implemented during actual crises.
The WHO (33) emphasizes that well-functioning command-and-control systems are related to effective emergency management operations. In the quantitative data, LTCHs reported that response teams were mostly formed after the COVID-19 outbreak, but the operational effectiveness of most teams did not fall below average. Qualitative data provided further explanation of the response team's operation through workplace culture and leadership. Many HCWs reported that doctors who are owners/founders of hospitals were called directors/heads of the hospital. Due to this decision-making structure, implementation in an outbreak response can be made quickly without the approval of other parties. Global studies in the COVID-19 era corroborate that, because crisis management depends on hospital leadership, leaders should be trained to improve their inadequate leadership skills and serve as a champion (23, 43, 44). Consistent with our findings, a previous study (24) found that strong leadership with a clear vision can help push a hospital through the pandemic; the leadership of middle management also needs to be equipped to improve hospital outbreak response, since middle management is responsible for executing much of the day-day work (24). Moreover, during the pandemic, respectful organizational culture focusing on team-based approaches also fostered resilience for outbreak response, which is consistent with a previous study in long-term care (11). This implies that workplace culture and organizational leadership may hold a significant portion of the key continuity strategies and resources of private LTCHs.
In terms of communication, quantitative data showed that LTCHs reported a lack of smooth and effective risk communication between LTCHs and local health authorities. Meanwhile, qualitative data indicated that intra-hospital communication was relatively smooth when using smartphone technology, and sharing information with other LTCHs was beneficial for pandemic responses. The combined data highlighted a need to establish and activate a system with clear communication channels between authorities/stakeholders and LTCHs for real-time access, information exchange, and updates without delay or confusion. Some of these results echo the findings of a study that, through a multinational survey, pointed to increased use of virtual technologies for communication among health professionals, in parallel with changes during the pandemic, to keep staff connected and up to date with the ever-changing situation (45). Therefore, it is important to include information on communicating with stakeholders in BCP and provide support to address obstacles in order to ensure effective communication across and beyond hospitals during crises (40, 46).
Concerning the safety response, of the objectively measured new/intensified tasks, access control for safety accounted for the highest proportion. LTCHs reported implementing cohort isolation and experienced a high degree of difficulty in transferring patients during the process. The qualitative data confirmed these findings and revealed vulnerabilities and a process of trial and error in LTCHs. LTCHs in Korea lacked well-equipped isolation rooms and infection control specialists, so they had no choice but to follow the policy of transferring confirmed patients to hospitals dedicated to infectious diseases in the early phases, despite concerns over the quality of care in those hospitals (47). Later, a small number of designated hospitals with limited capacity were unable to admit confirmed patients, which led to transfer delays and the possibility of a surge in cluster infections in LTCHs (48). This is consistent with a study that found that several countries designated specific hospitals for the receiving and treatment of COVID-19 patients, but as case numbers increased, this arrangement was adapted, requiring other hospitals to admit confirmed cases as well (39). In addition to the lack of negative pressure isolation rooms, the lack of infection prevention and control (IPC) facilities, including single occupancy rooms for isolation, clear route separation, mandatory installation of ventilation systems, and a novel type of separate visiting area, further complicated the response to safety concerns (9, 49, 50). Taking this situation seriously, the government should provide financial and policy support to ensure the installation of IPC-related facilities, the activation of non-contact visits, and the proper layout of spaces in LTCHs, in preparation for future pandemics.
This study shows the pandemic placed a substantial burden on resource responses, pushing LTCHs to their limits, mirrored in other studies (11, 13, 20, 51). In particular, manpower issues throughout the pandemic response were frequently identified as the biggest challenge. The qualitative results in which HCWs described their experience of addressing human resources, largely confirmed and provided details on various self-help solutions. From this combined data, inferences emerged that pointed to desperate efforts to prevent staff shortages due to staff infections, as well as the impact of the pre-existing staffing issues of small and medium-sized LTCHs in Korea, including the absolute shortage of HCWs and instability in workforce quality, resulting in reduced care quality. Research involving hospitals in five countries (25) demonstrated comparable results; in terms of human resource management, during the pandemic, recruitment and retainment strategies were emphasized, including task-shifting with administrative staff assisting other services, recruitment of short-term contractors, moving staff within facilities, and simplifying recruitment, leading to hiring poorly qualified staff and less effective reinforcement in subsequent waves. This stresses the necessity for establishing a staff management and supervision system through collaboration between LTCHs and health authorities, including a human resources roster for infectious disease control and treatment, rather than counting on short-term solutions from individual LTCHs (25, 33). Considering the issues with care policies in Korea, improving the care worker system is also required, including the coverage of care worker costs through the National Health Insurance (48). Moreover, rewards for staff described during interviews, supporting and protecting staff can act as an important buffer against higher workload. Along with band-aid solutions for meeting immediate needs, better responses could be achieved through medium- to long-term strategies and planning, including needs assessment, ensuring an appropriate workload, and the development of incentive packages (52).
Quantitative results identified that in LTCHs, monitoring financial indicators was lacking in practice, and receiving compensation from the government was also difficult. Qualitative data provided more details insights into their limited financial responses. This meant that fiscally strained LTCHs, without a financial plan and plan evaluation, would not be able to provide adequate care to both infected patients and the remaining patients during the pandemic. The literature in this area stressed the need for increased fiscal autonomy for effective responses during the pandemic (24). Identifying funding sources as well as planning flexible contingency funds and reimbursement beforehand are foundations to meet additional demands for response (40). Also, additional financial compensation for hospitals' financial losses was a motive in other countries (53), so the government should develop payment systems to implement compensation for pandemic-related losses quickly, directly, and with great attention to distressed LTCHs.
How supply responses were made to address the continuity of the LTCHs' supply was provided by qualitative data. This may be related to the fact that the need of supplies was recognized without sufficient time to estimate or plan it in advance, consistent with previous research (47). Inconsistent assistance for PPE from the government and limited finances may also have an impact on supply management in LTCHs during the pandemic (28). This result aligns with earlier studies showing that tensions related to uncertainty about supplies were experienced due to a lack of diversity of supply channels, the absence of an inventory management tool, and shortages in the market, resulting in delivery delays and efforts to minimize unnecessary consumption and material waste, as well as efforts toward needs-based distribution (13, 24, 25). In this regard, evidence on hospital resilience has pointed to the importance of the government's proactive preparedness and comprehensive contingency planning, including the acquisition of supplies (23). Based on this lesson, it is important to plan for supply vulnerabilities at both the facility and national levels, including establishing a centralized supply system for the LTCHs through the health authority and alternative supply chains, maintaining reserves, and identifying storage space, to mitigate shortages of supplies (20).
Novel perspectives on LTCHs' BCP and responses to the pandemic in practice were gathered from HCWs, which contributes insights for developing and guiding preparedness plans and policies for vulnerable healthcare facilities in similar contexts, not only in Korea but also other countries, and provides evidence to enhance future responses. Similarly, studies suggest that small healthcare facilities should have BCPs to mitigate the impact of disasters, as damages (including preventable disaster death) occur in most hospitals with fewer beds, and patients cannot differentiate between the services available (18, 19, 54). It is thus imperative to be well prepared, including adaptive leadership, resilient staff, and established contingency funds for sustainable financing, regardless of hospital size (23, 55).
Nonetheless, its limitations should be acknowledged. First, our sample size was relatively small albeit focused on HCW representatives from LTCHs, restricting the conduct of additional inferential analyses. The low number of evaluated LTCHs in Korea also limits the generalizability of the results and findings; however, this indicates that this is an exploratory study, and further research is needed to gain a clearer understanding of responses in specific aspects and relevant factors in LTCHs. Moreover, this initial and exploratory study provides important information on this topic, but our study could be affected by the potential for selection bias. To obtain a representative sample for quantitative data, we attempted to recruit HCWs through professional associations/platforms used by small and medium-sized hospitals; however, recruitment was challenging during the pandemic, and self-selection bias cannot be prevented. While the selected small and medium-sized LTCHs are typical response cases in Korea, the interview participants may not represent the entirety of LTCHs. These may impact the generalizability and credibility of the findings. Future studies with more rigorous sampling methods, such as stratified random sampling, could be used to obtain more representative samples. Another limitation is related to the timing of data collection, which can lead to recall bias. In light of the persistence of the pandemic up to the Omicron period, HCWs were asked about their overall experiences while responding to the pandemic a few years after the initial outbreak. Additionally, a one-time survey of HCWs is limited in specifically capturing recovery phases and the changes across multiple waves of the COVID-19 pandemic, not the overall responses.
5 Conclusion
This study provides an opportunity to capture lessons learned by LTCHs that did not internalize BCPs when responding to crises. To protect vulnerable patients, ensuring the continuation of the LTCH operation is vital during a pandemic. The key lesson is that planning that fits the needs of the LTCHs and BCP implementation are critical to the LTCH's response and ultimately resilience. Considering BCP elements of planning within LTCHs is necessary to identify strong and weak points to prepare for and respond to future pandemics. To improve organizational resilience in LTCHs, there is a need for comprehensive continuity management strategies, including innovative platforms and policies, to support devising and implementing a realistic and effective contingency plan, and ensuring ongoing preparedness. At the same time, based on the findings, LTCHs need further adjustments and enhancements in their BCPs along with live, structured action plans, and should embed BCPs into the organization's culture.
Data availability statement
The data supporting the findings of this study will be made available by the corresponding author upon request.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Kyung Hee University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
EY: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing, Supervision. IL: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. SK: Conceptualization, Formal analysis, Methodology, Writing – review & editing. SH: Conceptualization, Formal analysis, Methodology, Writing – review & editing. HL: Conceptualization, Formal analysis, Methodology, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by a grant of the project for Infectious Disease Medical Safety, funded by the Ministry of Health and Welfare, Republic of Korea [grant number: RS-2022-KH125928(HG22C0051)].
Acknowledgments
We would like to thank Dr. In-Seo Son for advice and suggestions on the thematic analysis. We also would like to thank ISQua's 39th International Conference.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1518998/full#supplementary-material
References
1. Thompson DC, Barbu MG, Beiu C, Popa LG, Mihai MM, Berteanu M, et al. The impact of COVID-19 pandemic on long-term care facilities worldwide: An overview on international issues. BioMed Res Int. (2020) 2020:8870249. doi: 10.1155/2020/8870249
2. Lee MH Lee GA Lee SH Park YH A systematic review on the causes of the transmission and control measures of outbreaks in long-term care facilities: back to basics of infection control. PLoS One. (2020) 15:3. doi: 10.1371/journal.pone.0229911
3. Lai CC, Wang JH, Ko WC, Yen MY, Lu MC, Lee CM, et al. COVID-19 in long-term care facilities: an upcoming threat that cannot be ignored. J Microbiol Immunol Infect. (2020) 53:444–6. doi: 10.1016/j.jmii.2020.04.008
4. Ga H. Long-term care system in Korea. Ann Geriatr Med Res. (2020) 24:181. doi: 10.4235/agmr.20.0036
5. Park SK, Lee YJ. Categorization of long-term care hospital in Korea using cluster analysis. Public Health Aff. (2019) 3:71–81. doi: 10.29339/pha.3.1.71
6. Korean Disease Control and Prevention Agency. 2022 survey on the current status of infection control in domestic medical institutions. Seoul: Korean Disease Control and Prevention Agency. (2023) Available online at: https://www.kdca.go.kr/contents.es?mid=a20301080200 (accessed September 21, 2024).
7. Seon JY, Kim S, Lim MK, Oh IH. Increased risk of SARS-CoV-2 infection and COVID-19 death among older patients at long-term care hospitals in Korea. Front Public Health. (2023) 11:1235745. doi: 10.3389/fpubh.2023.1235745
8. Jang J, Kim Y, Kim YY, Yeom HS, Hwang IS, Park KS, et al. Coronavirus disease-19 (COVID-19) one-year outbreak major cluster infection report as of January 19, 2021, in the Republic of Korea. Public Health Wkly Rep. (2021) 14:482–95.
9. Kim T. Improving preparedness for and response to coronavirus disease 19 (COVID-19) in long-term care hospitals in Korea. Infect Chemother. (2020) 52:133. doi: 10.3947/ic.2020.52.2.133
10. Kim HJ, Kim J, Jang YS, Park H, Kim JM, Park YJ, et al. Early countermeasures to COVID-19 at long-term care facilities in Gwangju Metropolitan City, Republic of Korea. Osong Public Health Res Perspect. (2023) 14:59–65. doi: 10.24171/j.phrp.2022.0293
11. Yau B, Vijh R, Prairie J, McKee G, Schwandt M. Lived experiences of frontline workers and leaders during COVID-19 outbreaks in long-term care: a qualitative study. Am J Infect Control. (2021) 49:978–84. doi: 10.1016/j.ajic.2021.03.006
12. Rocard E, Sillitti P, Llena-Nozal A. COVID-19 in long-term care: impact, policy responses and challenges. OECD Health Working Papers, No 131 Paris: OECD Publishing. (2021).
13. Glette MK, Ludlow K, Wiig S, Bates DW, Austin EE. Resilience perspective on healthcare professionals' adaptations to changes and challenges resulting from the COVID-19 pandemic: a meta-synthesis. BMJ Open. (2023) 13:9. doi: 10.1136/bmjopen-2023-071828
14. Barbash IJ, Kahn JM. Fostering hospital resilience—lessons from COVID-19. JAMA. (2021) 326:693–4. doi: 10.1001/jama.2021.12484
15. United Nations Office for Disaster Risk Reduction (UNDRR). Report of the open-ended intergovernmental expert working group on indicators and terminology relating to disaster risk reduction. (2016). Available online at: https://www.undrr.org/publication/report-open-ended-intergovernmental-expert-working-group-indicators-and-terminology (accessed October 3, 2024).
16. Khalil M, Ravaghi H, Samhouri D, Abo J, Ali A, Sakr H, et al. What is “hospital resilience”? A scoping review on conceptualization, operationalization, and evaluation. Front Public Health. (2022) 10:1009400. doi: 10.3389/fpubh.2022.1009400
17. Ito H Aruga T A conceptual framework to assess hospitals for disaster risk reduction in the community. Int J Disaster Risk Reduct. (2022) 77:103032. doi: 10.1016/j.ijdrr.2022.103032
18. Jafar E, Taneja U. Business continuity planning—a survey of hospitals in Delhi. J Public Health. (2017) 25:699–709. doi: 10.1007/s10389-017-0830-3
19. Sasaki H, Maruya H, Abe Y, Fujita M, Furukawa H, Fuda M, et al. Scoping review of hospital business continuity plans to validate the improvement after the 2011 Great East Japan Earthquake and Tsunami. Tohoku J Exp Med. (2020) 251:147–59. doi: 10.1620/tjem.251.147
20. Koonin LM. Novel coronavirus disease (COVID-19) outbreak: now is the time to refresh pandemic plans. J Bus Contin Emerg Plan. (2020) 13:298–312. doi: 10.69554/GGFG5840
21. Jafar E, Taneja U. Determinants of business continuity management in hospitals. Int J Crit Infrastruct. (2017) 13:57–69. doi: 10.1504/IJCIS.2017.083640
22. Shi W, Chen R, Wang K, Wang Y, Gui L. Exploring hospital resilience protective or risk factors: lessons for future disaster response efforts. Front Public Health. (2024) 12:1378257. doi: 10.3389/fpubh.2024.1378257
23. Ravaghi H, Khalil M, Al-Badri J, Naidoo AV, Ardalan A, Khankeh H. Role of hospitals in recovery from COVID-19: reflections from hospital managers and frontliners in the Eastern Mediterranean Region on strengthening hospital resilience. Front Public Health. (2023) 10:1073809. doi: 10.3389/fpubh.2022.1073809
24. Khalil M, Mataria A, Ravaghi H. Building resilient hospitals in the Eastern Mediterranean Region: lessons from the COVID-19 pandemic. BMJ Glob Health. (2022) 7:e008754. doi: 10.1136/bmjgh-2022-008754
25. Dagenais C, Kielende M, Coulibaly A, Gautier L, David P-M, Peiffer-Smadja N, et al. Lessons learned from field experiences on hospitals' resilience to the COVID-19 pandemic: a systematic approach. Health Systems Reform. (2023) 9:2231644. doi: 10.1080/23288604.2023.2231644
26. Stennett J, Hou R, Traverson L, Ridde V, Zinszer K, Chabrol F. Lessons learned from the resilience of Chinese hospitals to the COVID-19 pandemic: scoping review. JMIRx Med. (2022) 3:e31272. doi: 10.2196/31272
27. Boamah SA, Weldrick R, Havaei F, Irshad A, Hutchinson A. Experiences of healthcare workers in long-term care during COVID-19: a scoping review. J Appl Gerontol. (2023) 42:1118. doi: 10.1177/07334648221146252
28. Park JY, Lee I. Healthcare workers' experiences in long-term care facilities during cohort quarantine for the COVID-19 pandemic in South Korea: a qualitative study. BMJ Open. (2024) 14:e089309. doi: 10.1136/bmjopen-2024-089309
29. Creswell JW, Creswell JD. Research design: qualitative, quantitative, and mixed methods approaches. Los Angeles: Sage Publications. (2017).
30. Mitchell BG, MacBeth D, Halton K, Gardner A, Hall L. Resourcing hospital infection prevention and control units in Australia: a discussion paper. Infect Dis Health. (2017) 22:83–8. doi: 10.1016/j.idh.2017.02.001
31. Wang J, Liu F, Zhou M, Lee YF. Will the status of infection prevention and control (IPC) professionals be improved in the context of COVID-19? Am J Infect Control. (2020) 48:729–30. doi: 10.1016/j.ajic.2020.04.003
32. Ministry Ministry of Employment and Labor, South Korea. Guidelines for developing a business continuity plan (BCP) for infectious disease outbreak preparedness. Seoul: Ministry of Employment and Labor. (2022) Available online at: https://www.moel.go.kr/local/gunsan/news/notice/noticeView.do?bbs_seq=20220101202 (accessed March 2, 2025).
33. World Health Organization. Hospital emergency response checklist. Geneva: World Health Organization. (2011) Available online at: https://www.who.int/publications/i/item/hospital-emergency-response-checklist (accessed October 3, 2024).
34. Central Disaster Management Headquarters. Guidelines for Business Continuity Plan (BCP) in Medical Institutions to Prepare for In-Hospital Healthcare Worker Infections. Ministry of Health and Welfare, Republic of Korea (2022).
35. Hennink M, Kaiser BN. Sample sizes for saturation in qualitative research: A systematic review of empirical tests. Soc Sci Med. (2022) 292:114523. doi: 10.1016/j.socscimed.2021.114523
37. Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods. (2017) 16:1609406917733847. doi: 10.1177/1609406917733847
38. Liow MHL, Tay KXK, Yeo NEM, Tay DKJ, Goh SK, Koh JSB, et al. Ensuring business continuity of musculoskeletal care during the COVID-19 pandemic: experience of a tertiary orthopaedic surgery department in Singapore. JBJS Open Access. (2020) 5:e0050. doi: 10.2106/JBJS.OA.20.00050
39. Webb E, Hernández-Quevedo C, Williams G, Scarpetti G, Reed S, Panteli D. Providing health services effectively during the first wave of COVID-19: a cross-country comparison on planning services, managing cases, and maintaining essential services. Health Policy. (2022) 126:382–90. doi: 10.1016/j.healthpol.2021.04.016
40. World Health Organization. Health service continuity planning for public health emergencies: a handbook for health facilities. Geneva: World Health Organization. (2021) Available online at: https://www.who.int/publications/i/item/9789240033337 (accessed October 3, 2024).
41. Song SY, Ko JM. Is K-quarantine maintained by ”overworking“ personnel? Focus on shortening isolation periods in BCP. Young Doctor. (2022) Available online at: https://www.docdocdoc.co.kr/news/articleView.html?idxno=2021313 (accessed October 3, 2024).
42. Kim JY. Communication with patients and medical staff needed, not unilateral BCP notification. Young Doctor. (2022) Available online at: https://www.docdocdoc.co.kr/news/articleView.html?idxno=2020253 (accessed October 3, 2024).
43. Abdi Z, Lega F, Ebeid N, Ravaghi H. Role of hospital leadership in combating the COVID-19 pandemic. Health Serv Manag Res. (2022) 35:2–6. doi: 10.1177/09514848211035620
44. Choflet A, Packard T, Stashower K. Rethinking organizational change in the COVID-19 era. J Hosp Manag Health Policy. (2021) 5:16. doi: 10.21037/jhmhp-21-11
45. Dunleavy L, Preston N, Bajwah S, Bradshaw A, Cripps R, Fraser LK, et al. “Necessity is the mother of invention”: Specialist palliative care service innovation and practice change in response to COVID-19. Results from a multinational survey (CovPall). Palliat Med. (2021) 35:814–29. doi: 10.1177/02692163211000660
46. Ow Yong LM, Xin X, Wee JML, Poopalalingam R, Kwek KYC, Thumboo J. Perception survey of crisis and emergency risk communication in an acute hospital in the management of COVID-19 pandemic in Singapore. BMC Public Health. (2020) 20:1–12. doi: 10.1186/s12889-020-10047-2
47. Kim EJ, Kang J, Byeon H. Coronavirus disease-2019 (COVID-19) outbreak in a long-term care hospital in Korea in early 2021. Infect Prev Pract. (2025) 7:100427. doi: 10.1016/j.infpip.2024.100427
48. Korean Convalescent Hospital Association. 2020 convalescent hospital white paper. Seoul: Korean Convalescent Hospital Association. (2021). Available online at: http://www.kagh.co.kr (accessed July 4, 2023).
49. Ok S, Yoo S, A. study on problems and improvement of cohort isolation for nursing hospitals and senior care facilities in Korea. Law Rev. (2021) 62:261–90. doi: 10.35275/pnulaw.2021.62.3.010
50. Capolongo S, Gola M, Brambilla A, Morganti A, Mosca EI, Barach P. COVID-19 and healthcare facilities: a decalogue of design strategies for resilient hospitals. Acta Biomed. (2020) 91:50–60. doi: 10.23750/abm.v91i9-S.10117
51. Behrens LL, Kitt-Lewis E, Boltz M, Calo WA, Lehman E, Whitaker J, et al. Leadership perspectives on nursing home operations from crisis to control: a mixed methods study. J Am Med Dir Assoc. (2024) 25:105145. doi: 10.1016/j.jamda.2024.105145
52. World Health Organization. Health workforce policy and management in the context of the COVID-19 pandemic response: interim guidance. (2020). Available online at: https://iris.who.int/handle/10665/337333 (accessed March 2, 2025).
53. Waitzberg R, Quentin W, Webb E, Glied S. The structure and financing of health care systems affected how providers coped with COVID-19. Milbank Q. (2021) 99:542–564. doi: 10.1111/1468-0009.12530
54. Yamanouchi S, Sasaki H, Kondo H, Mase T, Otomo Y, Koido Y, et al. Survey of preventable disaster deaths at medical institutions in areas affected by the Great East Japan Earthquake: retrospective survey of medical institutions in Miyagi Prefecture. Prehosp Disaster Med. (2017) 32:515–22. doi: 10.1017/S1049023X17006501
Keywords: long-term care, COVID-19 response, mixed methods, business continuity planning, healthcare workers, infection prevention and control, disaster preparedness
Citation: Yun EK, La IS, Kim S, Han S and Lee H (2025) Healthcare workers' views on the response to COVID-19 in long-term care hospitals in Korea: a mixed-method study. Front. Public Health 13:1518998. doi: 10.3389/fpubh.2025.1518998
Received: 29 October 2024; Accepted: 12 May 2025;
Published: 16 June 2025.
Edited by:
Faris Lami, University of Baghdad, IraqReviewed by:
Federica Pascale, Anglia Ruskin University, United KingdomKamal A. Kadhim, Ministry of Health, Iraq
Copyright © 2025 Yun, La, Kim, Han and Lee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: In Seo La, aW5zZW8ubGFAa2h1LmFjLmty
 Eun Kyoung Yun
Eun Kyoung Yun In Seo La
In Seo La Sunmi Kim
Sunmi Kim Seongyu Han
Seongyu Han Hyungran Lee
Hyungran Lee