- 1Zhuhai Center for Disease Control and Prevention, Zhuhai, Guangdong, China
- 2University of North Carolina Project-China, Guangzhou, China
- 3Department of Health Law, Policy and Management, Boston University School of Public Health, Boston, MA, United States
- 4Zhuhai Xutong Voluntary Services Center, Zhuhai, China
- 5Department of Strategic Communication, University of Miami, Coral Gables, FL, United States
- 6Department of Public Health and Preventive Medicine, School of Medicine, Jinan University, Guangzhou, China
- 7Dermatology Hospital of South Medical University, Guangzhou, China
- 8Faculty of Medicine, Macau University of Science and Technology, Macau, Macao SAR, China
Background: Support from peers is a commonly employed behavioral prevention approach aimed at key populations to enhance HIV prevention efforts. Internet-based HIV self-testing (HIVST) has been widely used among men who have sex with men (MSM) across China over the past few years.
Objective: We aimed to analyze the occurrence of Internet-based peer support and high-risk behaviors during the process of distributing HIVST kits among MSM.
Methods: The single-arm prospective cohort study was conducted among MSM in Zhuhai, China. The study utilized an HIVST online ordering system based on WeChat, which was developed by Xutong. MSM who ordered HIVST kits and distributed them to people in their network for self-testing were defined as index participants. People who received the kits from the index participants and provided testing results were defined as alters. Chi-squared tests were used to compare baseline and follow-up characteristics of the participants. Cramer’s V was used to quantify the level of association between the Internet-based HIVST and condomless anal sexual behaviors among index participants. Logistic regression analysis was used to evaluate factors associated with peer support among alter participants. A p-value <0.05 was regarded as statistically significant.
Results: A total of 288 index participants were included in the study, and they distributed HIVST kits to 478 alters. In the study, 84.0% (242/288) of the index participants reported that they provided peer support to their alters, and 87.4% (418/478) of the alters reported receiving peer support from the index participants. As for the alters, 19.9% (95/478) had sex with index participants on the day of HIVST. Among them, 24.2% (23/95) had sex after the HIVST and 72.6% (69/95) used a condom during sex. Index participants who had been asked for advice about HIV and other sexually transmitted infections were more likely to provide peer support to alters (OR: 1.85, 95% CI: 1.01–3.37).
Conclusion: This study has enhanced our understanding of the occurrence of peer support and high-risk behaviors during the process of HIVST kits secondary distribution and provided evidence that Internet-based HIVST appears to be a promising approach for behaviors interventions among MSM.
Introduction
In China, sexual transmission is the primary route of human immunodeficiency virus (HIV) transmission (1). A report by the Chinese Ministry of Health estimated that approximately 1.05 million people were living with HIV/AIDS in China in 2020, and 23.3% of the newly identified HIV/AIDS cases were attributable to male-to-male sexual contact (1, 2). Behavioral prevention remains central to the effort to reduce HIV transmission. Peer-supported intervention is a widely used behavioral prevention strategy targeting key populations to promote HIV prevention (3–5). A peer-based intervention program conducted among MSM in China has proven that peer support can be used to improve HIV testing and linkage to care (6). A meta-analysis of 15 studies also found that peer-led HIV interventions might reduce overall unprotected anal intercourse among HIV-negative MSM (7). Another meta-analysis published on JMIR recently also found that Internet/digital-based interventions are now most commonly used to promote and facilitate HIV testing among MSM (8). A program carried out in Brazil has also proven that E-testing proved highly feasible and acceptable, supporting scale-up to additional centers for MSM (9). Support for the use of peers in a wide variety of HIV care settings is likely based on their perceived availability and accessibility (10).
HIV self-testing (HIVST) has been shown as a cost-effective approach to supplement HIV testing services and reach individuals who have avoided facility-based testing (11). A systematic review and meta-analysis conducted in China showed that HIVST has become a valuable tool for HIV prevention in China and is widely spread (12). A national cross-sectional study in China has proven that distributing HIVST application links among the MSM population via Internet-based social media is feasible (13). A previous study by our team showed that peer-based secondary distribution of HIVST kits holds promise to increase HIV testing coverage and case identification among MSM (14). HIVST secondary distribution encourages MSM to apply multiple HIVST kits (index) and distribute them to people within their social networks, including sexual partners and friends (alters) (15). A program data analysis carried out in Côte d’Ivoire, West Africa, showed that enhanced peer outreach was effective, even in reaching female sex workers for HIV prevention and treatment (16). As a result, peers have access to a broader network of MSM than researchers and traditional medical clinics.
In addition, counseling and information provided through HIV testing services may provide opportunities to influence subsequent sexual behaviors, particularly in terms of reducing the number of sexual partners and increasing condom-protected sex among HIV-positive individuals. This, in turn, can impact HIV transmission and prevention (17–19). These changes in behaviors may be attributable to supportive information provided at the time of HIV testing, testing behaviors, or knowledge of HIV serostatus. However, few studies have assessed whether the individuals (referred to as “alters”) received peer support (i.e., messages on HIV, what HIVST is, and how to conduct HIVST) during the process of HIVST distribution by index participants; a big part of whom never tested for HIV before and may have higher-risk behaviors compared to other MSM.
Therefore, this study aimed to analyze the occurrence of peer support and high-risk behaviors between index participants and alters during the process of HIVST kits distribution.
Methods
Study design and participants
This single-arm prospective cohort study was carried out in Zhuhai, a city located in southern China, where an estimated 17,000 MSM reside. This study was conducted jointly by the University of North Carolina at Chapel Hill Project-China, Zhuhai Center for Diseases Control and Prevention (CDC), and Zhuhai Xutong Voluntary Services Center (Xutong). Xutong is a gay-friendly community-based organization in Zhuhai, providing HIV prevention services (e.g., condoms, testing, and linkage to treatment) to men who have had sex with men for many years. The study utilized an HIVST online ordering system developed by Xutong. The ordering system was hosted and managed using WeChat, China’s largest social networking platform. Based on the pilot study’s results and the characteristics of single-arm prospective cohort studies, we set the index’s transmission proportion at 1.2, with an alpha level of 0.05, a power of 0.90, and a 20% dropout rate. We estimated the sample size for the index group to be 208 individuals of index participants and 249 for alters. In this study, we collected data from two groups of population: (1) the Index group, who applied HIVST kits and distributed them to people within their social networks, including sexual partners and friends; (2) the Alter group, who received HIVST kits from the index participants. To observe the peer support, we only selected all index participants who distributed HIVST and alters who received HIVST from one of the index participants and provided feedback on testing results. Index participants did not receive any training on how to distribute HIVST.
The inclusion criteria of the index participants were as follows: (1) assigned male at birth; (2) aged 18 years or older; (3) ever had male-to-male sex; (4) ordered HIVST kits through the online platform; and (5) be consented to take baseline and follow-up surveys online. All index participants and alters agreed to sign informed consent forms before the online baseline survey. The inclusion criteria of the alter participants were as follows: (1) assigned male at birth; (2) aged 18 years or older; (3) received HIVST kits through index; and (4) consented to take follow-up surveys online.
Procedures
MSM were able to apply for HIVST kits for free using Xutong’s public WeChat account. HIVST kits were mailed to index men after they paid the deposit (US$15 per kit) and provided shipping information. Upon receiving a photographed test result and verified by a Xutong staff member trained in HIV testing, the deposit was immediately refunded to index men through WeChat. The index group completed the baseline survey and ordered HIVST kits (SD Bioline, South Korea) through the online system. The SD BIOLINE HIV/syphilis duo test kits (Standard Diagnostics Inc.) were utilized in this study. Each index participant could conduct self-tests or distribute the HIVST kits to alters. After testing, all testers scanned the QR code in a returning card in each HIVST kit to submit photographs of their test results and reported whether they were HIVST kit index participants or alters. Alters completed and submitted the baseline survey when they received HIVST kits from index participants and subsequently submitted their test results. In the second phase of the study, we used an additional monetary incentive to increase the number of HIVST kit applications and distribution from the index participants. In this phase, in addition to the fixed monetary incentive, both the index participants who distributed HIVST to the alter and the alters who returned the test results received an additional 20 RMB (≈3 USD) as monetary incentive. Individuals with positive test results for HIV were referred for confirmatory testing at the local CDC and provided other counseling and linkage to care services by volunteers. Trained staff of Xutong ensured the confidentiality of all the test results. Three months after the HIVST kits application, the index participants completed a follow-up survey to assess their risk behaviors and whether they provided peer support to the alters. More details was shown in (Figure 1).

Figure 1. Study flow diagram of the internet-based HIVST kits secondary distribution among MSM in Zhuhai, China.
Outcomes
The primary outcomes of our study encompassed the proportion of peer support and the occurrence of high-risk behaviors during the HIV self-testing (HIVST) distribution process. We separately delineated index participants who self-reported providing peer support and those who did not provide peer support to the alters. Peer support was defined as index participants providing all of the following four items to the alters: (1) HIV-related knowledge, (2) HIV testing relevant knowledge, (3) how to conduct HIVST, and (4) how to read the results of HIVST. Each item was assessed as a dichotomous response (yes or no). We summed the scores for these four items and created a binary variable indicating whether alters had received comprehensive peer support, covering all assessed aspects. Peer sexual behaviors on the day of HIVST kits distribution were related to the four items, which were also assessed dichotomously: (1) use HIVST at the same time with index participants, (2) had sex with index participants on the day of the test, (3) had sex with index participants before or after the test, and (4) condom use during the sex with index participants. High-risk behaviors were related to the following items: (1) disclosed sexual orientation, (2) had anal sex with men, (3) frequency of condom use during anal sex, (4) condom use during last sexual activity with a male partner, and (5) role in the sex (see Supplementary File). Our analysis included examining factors associated with peer support during the secondary distribution of HIVST among index participants. Additionally, we explored the occurrence of high-risk behaviors between index participants and alters during the HIVST distribution process. Utilizing logistic regression, we analyzed sexual behaviors associated with peer support among alters during the distribution of HIVST. Subsequently, all index participants were subjected to an online 3-month follow-up survey after ordering the kits. We conducted follow-ups with the index participants to assess testing uptake rates and changes in high-risk behaviors among them after ordering the HIVST kits.
Statistical analysis
All data analyses were conducted in R 4.1.2 for Windows 10. Chi-squared tests were used to compare baseline socio-demographic characteristics of index participants and alters, as well as baseline and follow-up characteristics of index participants’ sexual behaviors. In this study, Cramer’s V was employed to quantify the level of association between the Internet-based HIVST and condomless anal sexual behaviors among index participants. Univariate logistic regression analysis was used to evaluate factors associated with providing peer support among index participants and factors associated with peer support among alter participants. Multivariable logistic regression analysis was conducted to evaluate factors associated with peer support among alter participants. Two-sided p-values < 0.05 were considered statistically significant, and odds ratios (OR) with (95% CI) were estimated. Covariates, which had a larger number or a wide distribution within the sample, were selected as the reference to ensure the stability and reliability of the model. Factors with a p-value of < 0.1 in the univariate analyses for peer support were included in the multivariate logistic regression model.
Ethical considerations
This study was approved by the Zhuhai Center for Disease Control and Prevention. A signed digital informed consent form was obtained from all the participants before collecting any study information or specimens. Participants joined the study voluntarily and were free to withdraw from the study at any time. The project staff had signed confidentiality agreements with the Zhuhai Center for Disease Control and Prevention.
Results
Participants characteristics
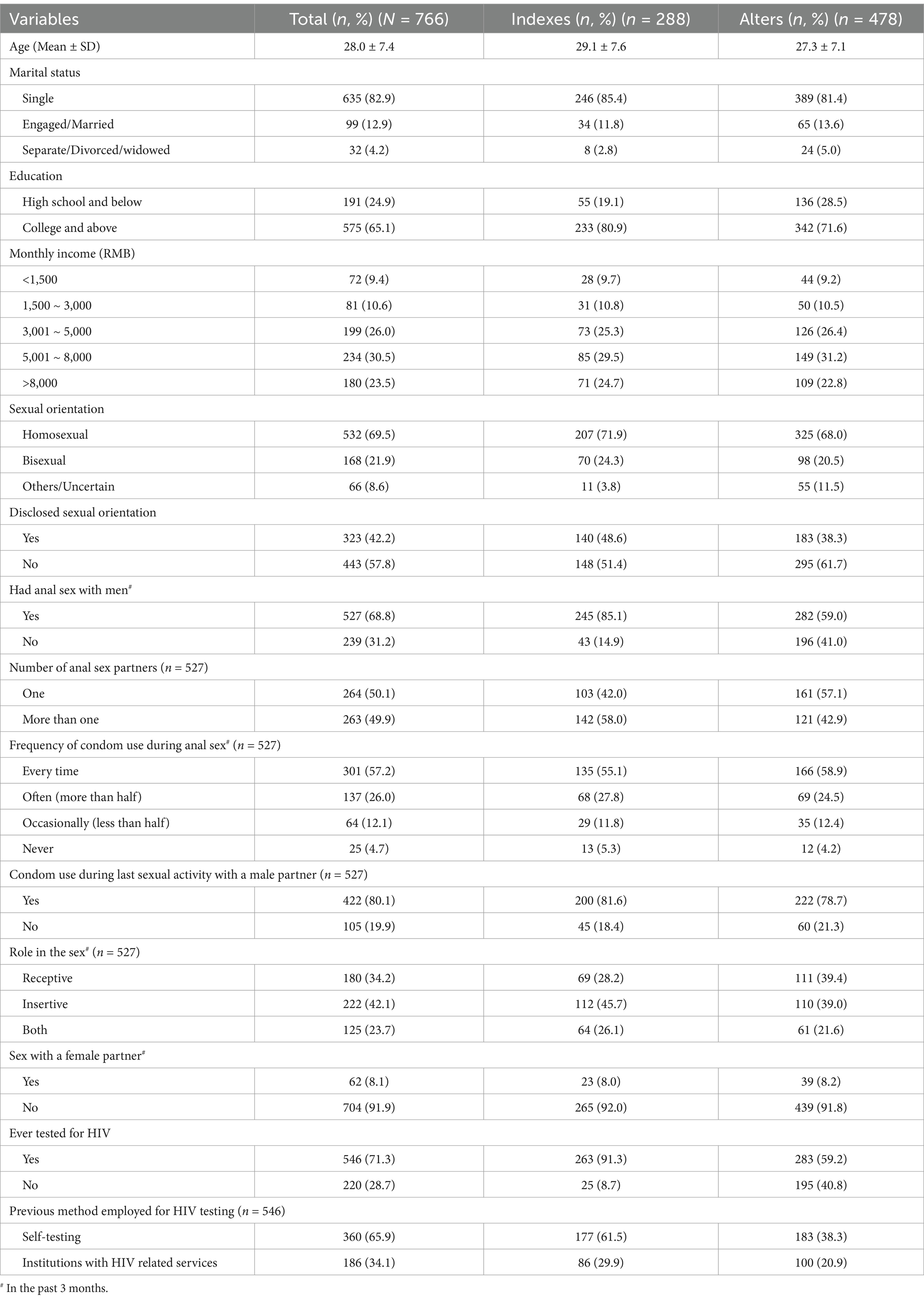
Our study recruited a total of 288 participants, and they distributed HIVST kits to 478 alters, who were from 94 cities in China, and most of them were located in Zhuhai. Table 1 shows the characteristics of the study participants. The mean age for index participants and alters was 29.1 (standard deviation [SD], 7.6) years and 27.3 (SD, 7.1) years, respectively. Index participants had higher proportions of obtaining university or higher education than alters (80.9% vs. 71.6%, p = 0.004). More index participants had disclosed their same-sex behaviors to individuals than their sexual partners (48.6% vs. 38.3%, p = 0.006).
Index participants were more likely to have anal sex (85.1% vs. 59.0%, p < 0.001) and have more than one anal sex partner in the past 3 months (58.0% vs. 42.9%, p < 0.001). The frequency of condom use in the past 3 months and condom use during the last sexual activity were similar between the two groups. Compared with alters, the role during anal sex was more likely to be insertive among index participants in the past 3 months (45.7% vs. 39.0%, p = 0.03). Moreover, index participants were more likely to have tested for HIV (91.3% vs. 59.2%, p < 0.001).
Peer-supported HIVST
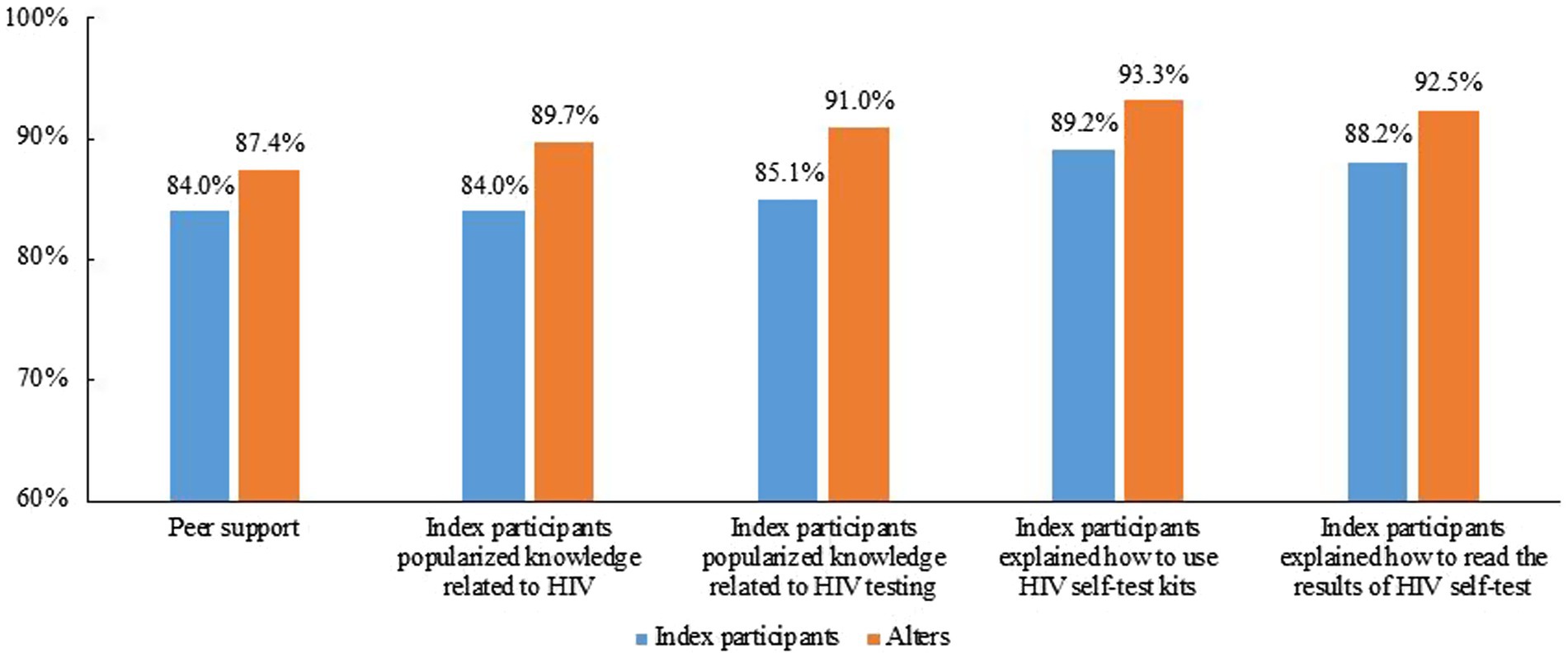
Figure 2 shows the peer support during the distribution of HIVST kits. Overall, 84.0% (242/288) of the index participants reported that they provided peer support to the alters and 87.4% (418/478) of the alter participants reported that they received peer support from the index participants.
Overall, 84.0, 85.1, 89.2, and 88.2% index participants reported that they provided HIV-related knowledge, HIV testing relevant knowledge, how to conduct HIVST, and how to read the results of HIVST, respectively, with 89.7, 91.0, 93.3, 92.5% reported by alters.
Characteristics between index participants who reported providing peer support and not providing peer support
Table 2 shows the characteristics between index participants who reported providing peer support and those not providing peer support among index participants. Index participants ever being asked for advice about HIV and other sexually transmitted infections (STIs) were more likely to provide peer support to alters (odd ratio (20): 1.85 95%CI: 1.01–3.37). There were no significant differences in talking to others about HIV and STIs and providing others with information about HIV and STIs between index participants who reported peer support and non-peer support.
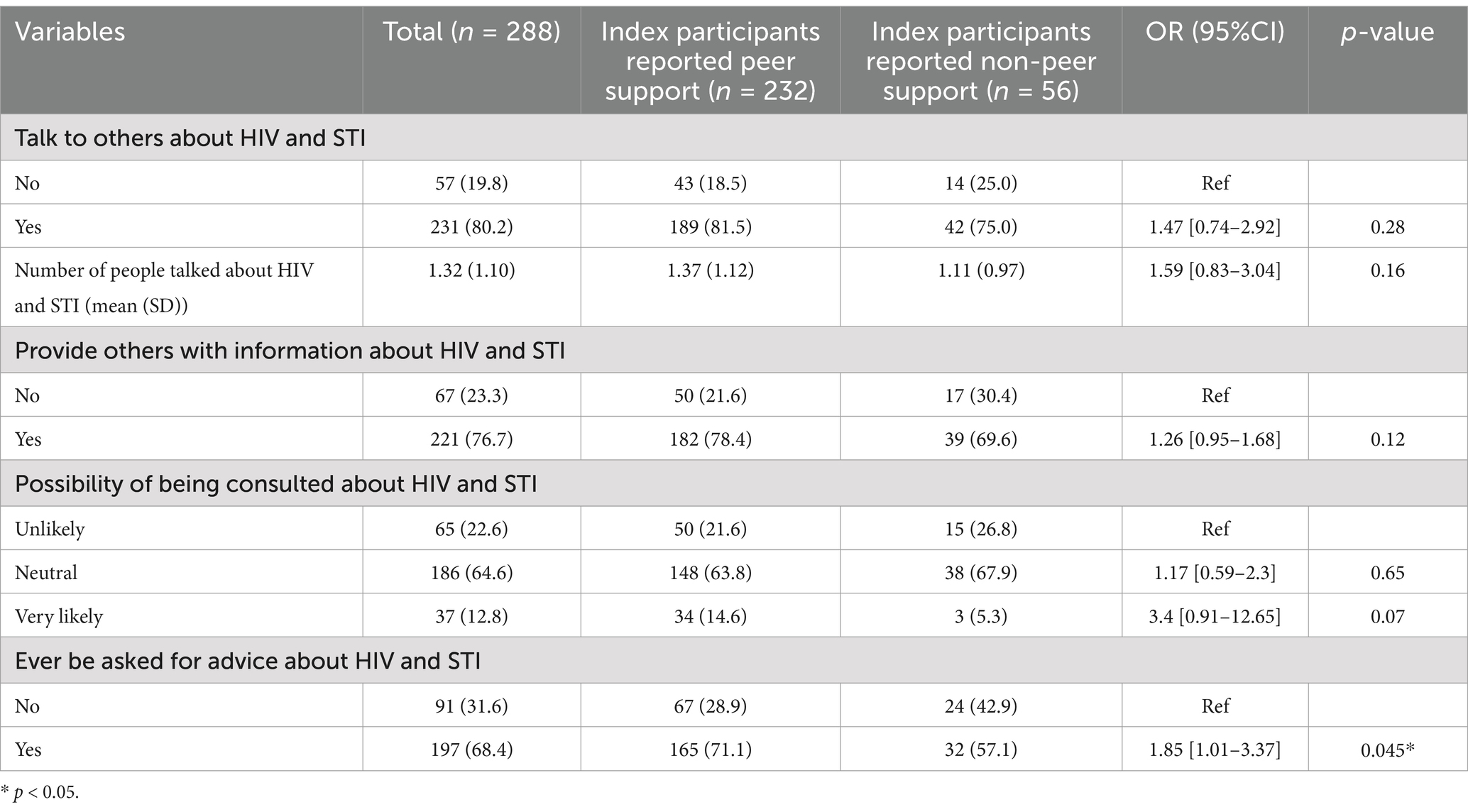
Table 2. Factors associated with peer support during the Internet-based HIVST kits secondary distribution among index participants.
Sexual behaviors associated with peer support among alters during the distribution of HIVST
Table 3 shows that there were no significant differences in the relationship with index participants, concurrent use of HIVST with index participants, engaging in sexual activity with index participants on the day of testing, having had sex with index participants before or after the test, and condom use during sexual encounters with index participants between alter participants reported peer support and those who did not report peer support.
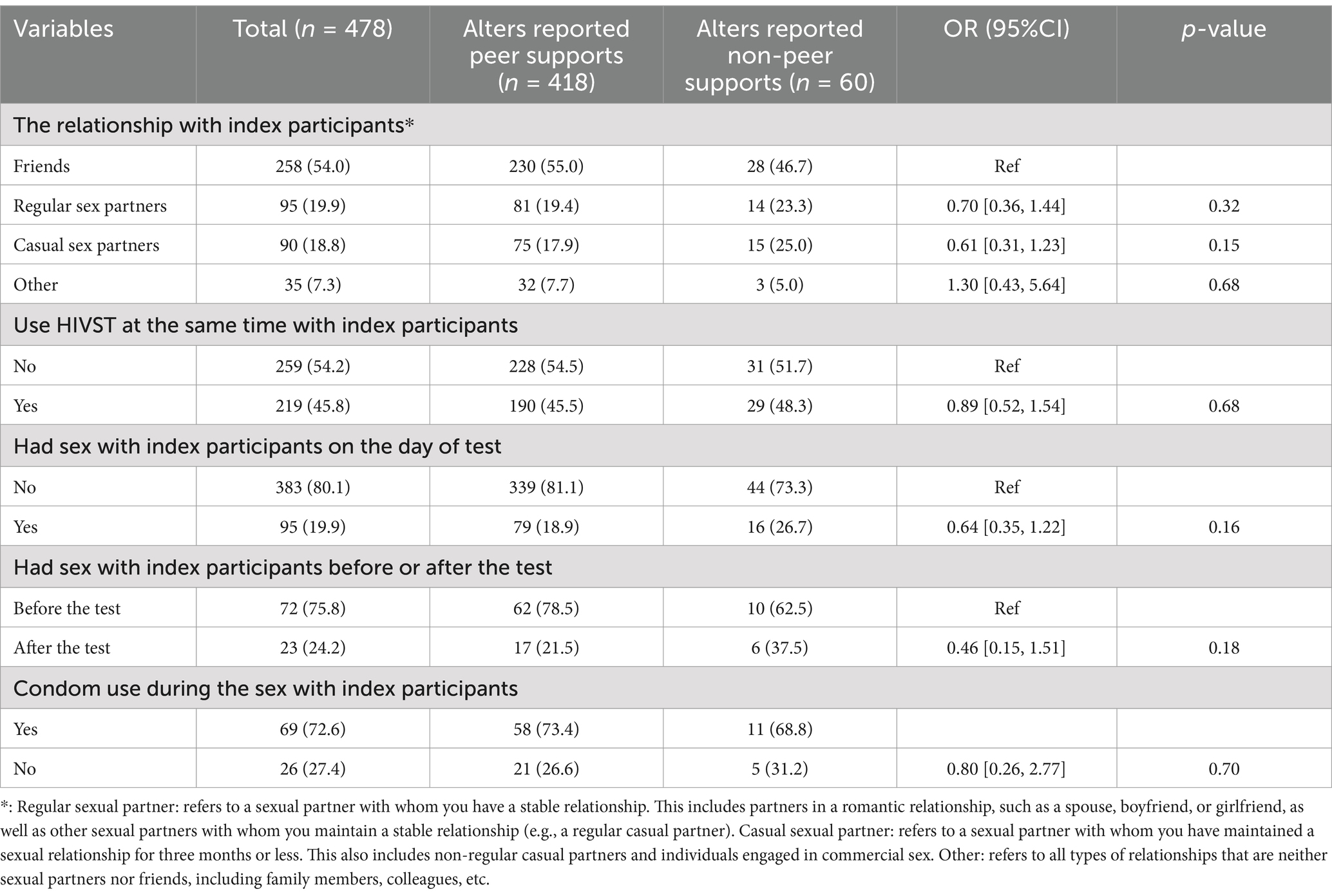
Table 3. Sexual behaviors associated with peer support among alters during the distribution of HIVST kits.
Table 4 shows that alters who did not test for HIV were more likely to report peer support, compared with those who had ever taken in HIVST [aOR: 2.23, 95%CI: 1.18–4.37].
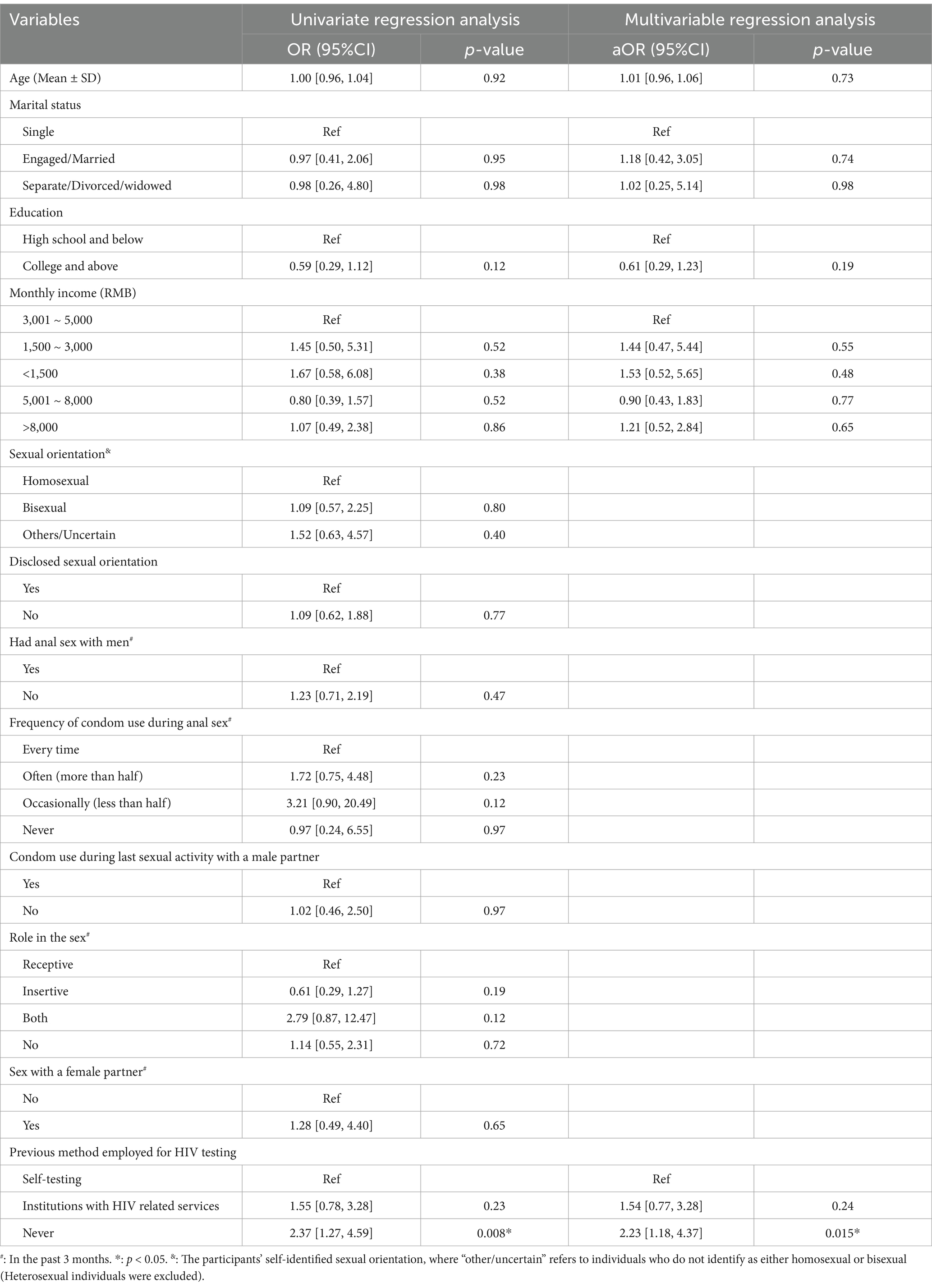
Table 4. Logistic regression analysis of sexual behaviors associated with peer support among alters during the distribution of HIVST kits.
Changes in sexual behaviors in index participants
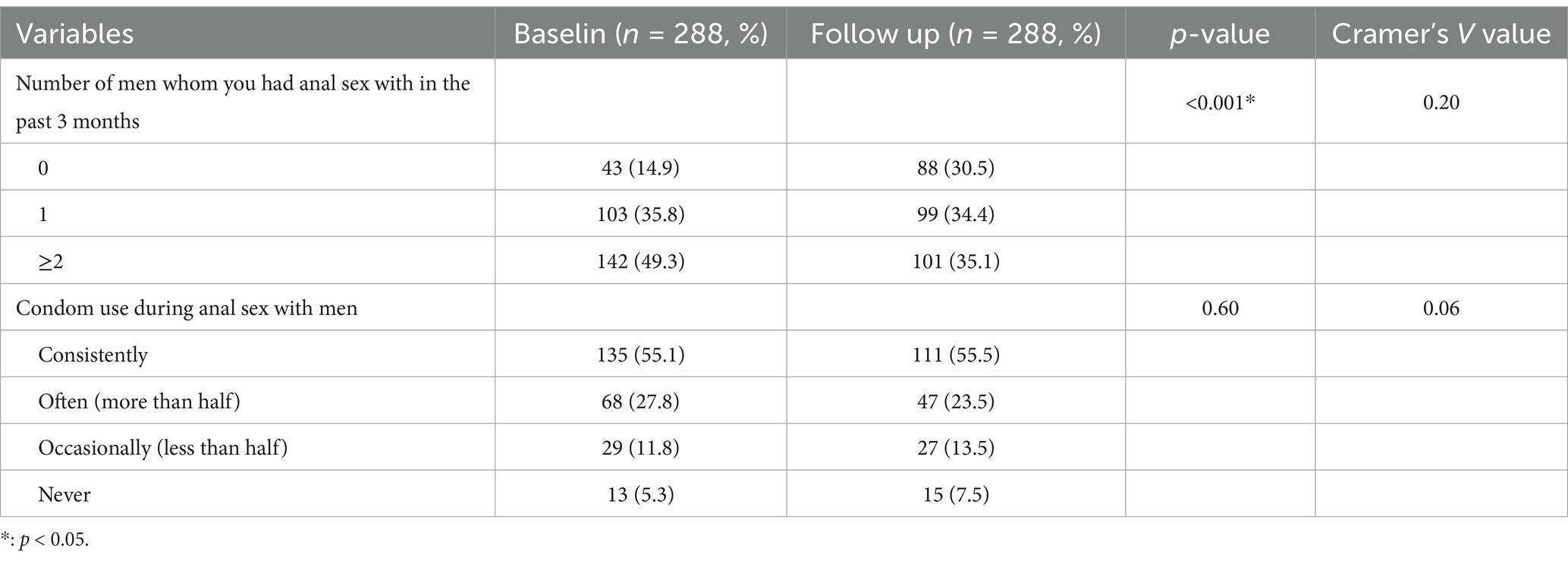
Table 5 shows the changes in sexual behaviors in index participants after 3 months of follow-up. After 3 months of follow-up, there was a moderate level of association between Internet-based HIVST and a decrease in the occurrence of anal sex with men, as indicated by a Cramer’s V coefficient of 0.20. However, there was no significant difference between the Internet-based HIVST and condomless anal sexual behaviors among index participants.
Discussion
Internet/digital-based HIVST among MSM has demonstrated a very high rate of usage in China (21). Understanding whether the index MSM will provide support to the alters is essential in planning network distribution of HIVST kits to improve HIV testing and intervention coverage. Our study contributes to the literature by assessing the occurrence of peer support and HIV-related high-risk behaviors during the process of HIVST kits distribution among MSM in China. We found that the proportion of index participants conducting peer support during the distribution of self-testing kits was over 84%, a very high level, which is an important intervention measure for alter participants. Meanwhile, after 3 months of follow-up, there was a moderate level of association between Internet-based HIVST and a decrease in the occurrence of anal sex with men, indicating that self-testing can influence the occurrence of high-risk behaviors. This study has significant public health implications for the promotion of peer support among MSM through self-testing kits distribution, as well as the simultaneous reduction of high-risk behaviors through both testing and peer support.
Our study demonstrated three important benefits over previously studied online secondary distribution of HIVST (14, 22). First, our study showed that peer support occurred during the process of Internet-based HIVST kits distribution and maintained a high frequency. Not only did the index participants take the initiative to provide peer support to the alters but also the alters self-reported receiving peer support from the index participants. This is a crucial finding, as it suggests that the digital-based peer support within the MSM community potentially enhances the effectiveness of HIV prevention initiatives. Peer support could advance the awareness of HIV testing and provide information about the location and availability of HIV services, and offer social support and referrals for services, which increase access to facility-based HIV testing services and improve HIV testing uptake (23, 24). As the main part of peer support, HIV-related knowledge delivery to the key population will promote HIV prevention (3). Our previous study demonstrated that alters have a significantly higher HIV infection rate than index participants (14); this implies that, as a group of MSM, alters should be the focus of targeted interventions, and Internet-based HIVST kits distribution is an important approach to provide peer support to a group of MSM who lack HIV-related prevention measures and may hold a strong promise to improve peer support coverage. While a meta-analysis revealed that HIVST was linked to a 47% lower rate of linkage to care compared to facility-based HIV testing, this disparity was attributed to insufficient counseling support in self-testing contexts (25).
Second, we observed that the index participants who delivered HIVST kits were significantly reduced for having anal sex and number of sex partners; meanwhile, the results of having condom sex during the 3 months follow-up were significantly increased. Reducing risk behaviors such as these would result in new HIV infections declination. In the United States, HIV incidence has declined overall in recent years, but rates of new infections remain high, particularly among MSM (26). Nearly all of these new infections occur as a direct result of sexual risk behavior, which among MSM involves having insertive or receptive anal sex without using an effective method of prevention (27, 28). A meta-analysis of 15 studies also found that peer-led HIV interventions might reduce unprotected anal intercourse among HIV-negative MSM (7). Meanwhile, a great deal of evidence shows that the Internet has emerged as the most popular platform for facilitating sex networking among MSM (29–33). Another study in Hong Kong found that Internet-based interventions have used several different aspects, including disseminating prevention messages (34). These findings suggested that internet-based HIVST appears to be a promising approach of behavior interventions among MSM.
Third, we found that risk behaviors occurred in the process of HIVST kits distribution between the index and the alters, such as the index participants engaging in condomless sex with alters and engaging in sex behaviors before HIV testing. These risk behaviors can result in HIV transmission. Joint United Nations Program on HIV/AIDS (UNAIDS) proposed the “95-95-95” target, which increases the capacity for identification of new cases for early diagnosis and immediate treatment, helping to control the spread of the virus (35–37). Increasing awareness of HIV status can decrease risk behaviors in key populations. Engaging in sexual activity before HIV testing may hinder the immediate detection of potential HIV infections and impede efforts to halt HIV transmission. Even though the self-testing results are negative, we still suggest practicing safe sex with condoms due to the existence of window periods. Therefore, providing additional warning information on high-risk behaviors and the window period may be helpful in reducing such behaviors.
Our study has limitations. First, our study was an integration of our previous two studies from which we figured out the data of peer support and risk behaviors (14, 38). Therefore, we are not sure the sample size is satisfied for our purpose. However, it could be an important reference for further study in this area. Second, we have selection bias in our study, and we measured index participants based on those who delivered HIVST kits and analyzed their demographic characteristics. However, in reality, the absence of index participants to deliver HIVST does not necessarily indicate a lack of capability to deliver HIVST kits to alters. Therefore, information about this subset of individuals is missing from the sample. Third, we did not make follow-ups for the alters, so we do not know whether the risk behaviors were reduced for alters. In our previous studies, we demonstrated that alters are the primary users of HIVST kits, but we believe that if they apply the HIVST kits themselves or make a secondary distribution, then the alters will become the index, and their risk behaviors will be changed similar to the index participants in this study (14, 38). Fourth, this study did not ask the participants about the site where the peer support occurred, whether it happened online by chatting APP such as WeChat or in person, and which was the main situation. Finally, our study relies on self-reported data, introducing potential recall and social desirability biases.
Conclusion
This study has enhanced our understanding of the occurrence of peer support and HIV-related high-risk behaviors during the process of HIVST kits secondary distribution. These findings have important implications for improving HIV prevention coverage and have the potential to reduce risk behaviors among key populations. This study provides evidence that Internet-based HIVST appears to be a promising approach for behavior interventions among MSM.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: the data sets generated and analyzed during this study are not publicly available due confidentiality principle. Requests to access these datasets should be directed to OTMwMjI0bGhAMTYzLmNvbQ==.
Ethics statement
The studies involving humans were approved by ethical approval prior to launching the study. Ethical approval was obtained from the institutional review board of the Zhuhai Municipal Center for Diseases Prevention and Control in China (ZHCDC201801).
Author contributions
HL: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. YN: Conceptualization, Data curation, Writing – review & editing. XH: Data curation, Formal analysis, Investigation, Project administration, Resources, Writing – review & editing. DW: Formal analysis, Software, Writing – review & editing. XY: Data curation, Methodology, Software, Writing – review & editing. WT: Funding acquisition, Validation, Writing – original draft, Writing – review & editing. YZ: Funding acquisition, Methodology, Project administration, Resources, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by funding from the Medical Science and Technology Research Foundation of Guangdong (A2023161).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1522425/full#supplementary-material
References
1. He, N. Research Progress in the epidemiology of HIV/AIDS in China. China CDC Wkly. (2021) 3:1022–30. doi: 10.46234/ccdcw2021.249
2. National Center for AIDS & STD Control and Prevention, The Chinese Center for Disease Control and Prevention (CDC). Annals of information on comprehensive prevention and treatment for AIDS, STD and hepatitis C. (2020) Available online at: https://ncaids.chinacdc.cn/
3. Cabral, HJ, Davis-Plourde, K, Sarango, M, Fox, J, Palmisano, J, and Rajabiun, S. Peer support and the HIV continuum of care: results from a multi-site randomized clinical trial in three urban clinics in the United States. AIDS Behav. (2018) 22:2627–39. doi: 10.1007/s10461-017-1999-8
4. He, J, Wang, Y, Du, Z, Liao, J, He, N, and Hao, Y. Peer education for HIV prevention among high-risk groups: a systematic review and meta-analysis. BMC Infect Dis. (2020) 20:338. doi: 10.1186/s12879-020-05003-9
5. Ngo, AD, Ha, TH, Rule, J, and Dang, CV. Peer-based education and the integration of HIV and sexual and reproductive health services for young people in Vietnam: evidence from a project evaluation. PLoS One. (2013) 8:e80951. doi: 10.1371/journal.pone.0080951
6. Yan, H, Zhang, R, Wei, C, Li, J, Xu, J, Yang, H, et al. A peer-led, community-based rapid HIV testing intervention among untested men who have sex with men in China: an operational model for expansion of HIV testing and linkage to care. Sex Transm Infect. (2014) 90:388–93. doi: 10.1136/sextrans-2013-051397
7. Ye, S, Yin, L, Amico, R, Simoni, J, Vermund, S, Ruan, Y, et al. Efficacy of peer-led interventions to reduce unprotected anal intercourse among men who have sex with men: a meta-analysis. PLoS One. (2014) 9:e90788. doi: 10.1371/journal.pone.0090788
8. Veronese, V, Ryan, KE, Hughes, C, Lim, MS, Pedrana, A, and Stoové, M. Using digital communication technology to increase HIV testing among men who have sex with men and transgender women: systematic review and Meta-analysis. J Med Internet Res. (2020) 22:e14230. doi: 10.2196/14230
9. De Boni, RB, Veloso, VG, Fernandes, NM, Lessa, F, Corrêa, RG, Lima, RS, et al. An internet-based HIV self-testing program to increase HIV testing uptake among men who have sex with men in Brazil: descriptive cross-sectional analysis. J Med Internet Res. (2019) 21:e14145. doi: 10.2196/14145
10. Simoni, JM, Nelson, KM, Franks, JC, Yard, SS, and Lehavot, K. Are peer interventions for HIV efficacious? A systematic review. AIDS Behav. (2011) 15:1589–95. doi: 10.1007/s10461-011-9963-5
11. Johnson, CC, Kennedy, C, Fonner, V, Siegfried, N, Figueroa, C, Dalal, S, et al. Examining the effects of HIV self-testing compared to standard HIV testing services: a systematic review and meta-analysis. J Int AIDS Soc. (2017) 20:21594. doi: 10.7448/IAS.20.1.21594
12. Xiu, X, Qin, Y, Bao, Y, Chen, Y, Wu, H, Huang, X, et al. The practice and potential role of HIV self-testing in China: systematic review and Meta-analysis. JMIR Public Health Surveill. (2022) 8:e41125. doi: 10.2196/41125
13. Li, S, Zhang, J, Mao, X, Lu, T, Gao, Y, Zhang, W, et al. Feasibility of indirect secondary distribution of HIV self-test kits via WeChat among men who have sex with men: National Cross-sectional Study in China. J Med Internet Res. (2021) 23:e28508. doi: 10.2196/28508
14. Wu, D, Zhou, Y, Yang, N, Huang, S, He, X, Tucker, J, et al. Social media-based secondary distribution of human immunodeficiency virus/syphilis self-testing among Chinese men who have sex with men. Clin Infect Dis. (2021) 73:e2251–7. doi: 10.1093/cid/ciaa825
15. Masters, SH, Agot, K, Obonyo, B, Napierala Mavedzenge, S, Maman, S, and Thirumurthy, H. Promoting partner testing and couples testing through secondary distribution of HIV self-tests: a randomized clinical trial. PLoS Med. (2016) 13:e1002166. doi: 10.1371/journal.pmed.1002166
16. Olawore, O, Astatke, H, Lillie, T, Persaud, N, Lyons, C, Kamali, D, et al. Peer recruitment strategies for female sex workers not engaged in HIV prevention and treatment Services in Côte d'Ivoire: program data analysis. JMIR Public Health Surveill. (2020) 6:e18000. doi: 10.2196/18000
17. Tiwari, R, Wang, J, Han, H, Kalu, N, Sims, LB, Katz, DA, et al. Sexual behaviour change following HIV testing services: a systematic review and meta-analysis. J Int AIDS Soc. (2020) 23:e25635. doi: 10.1002/jia2.25635
18. Ramachandran, S, Mishra, S, Condie, N, and Pickles, M. How do HIV-negative individuals in sub-Saharan Africa change their sexual risk behaviour upon learning their serostatus? A systematic review. Sex Transm Infect. (2016) 92:571–8. doi: 10.1136/sextrans-2015-052354
19. Fonner, VA, Denison, J, Kennedy, CE, O'Reilly, K, and Sweat, M. Voluntary counseling and testing (VCT) for changing HIV-related risk behavior in developing countries. Cochrane Database Syst Rev. (2012) 9:Cd001224. doi: 10.1002/14651858.CD001224.pub4
20. McMahon, SA, Musoke, DK, Wachinger, J, Nakitende, A, Amongin, J, Nanyiri, E, et al. Unintended uses, meanings, and consequences: HIV self-testing among female sex workers in urban Uganda. AIDS Care. (2021) 33:1278–85. doi: 10.1080/09540121.2020.1837722
21. Zhang, J, Tucker, J, Tang, W, Wang, H, Chu, Z, Hu, Q, et al. Internet-based HIV self-testing among men who have sex with men through pre-exposure prophylaxis: 3-month prospective cohort analysis from China. J Med Internet Res. (2021) 23:e23978. doi: 10.2196/23978
22. Okoboi, S, Castelnuovo, B, Van Geertruyden, JP, Lazarus, O, Vu, L, Kalibala, S, et al. Cost-effectiveness of peer-delivered HIV self-tests for MSM in Uganda. Front Public Health. (2021) 9:651325. doi: 10.3389/fpubh.2021.651325
23. Nnko, S, Kuringe, E, Nyato, D, Drake, M, Casalini, C, Shao, A, et al. Determinants of access to HIV testing and counselling services among female sex workers in sub-Saharan Africa: a systematic review. BMC Public Health. (2019) 19:15. doi: 10.1186/s12889-018-6362-0
24. Dutcher, MV, Phicil, SN, Goldenkranz, SB, Rajabiun, S, Franks, J, Loscher, BS, et al. "positive examples": a bottom-up approach to identifying best practices in HIV care and treatment based on the experiences of peer educators. AIDS Patient Care STDs. (2011) 25:403–11. doi: 10.1089/apc.2010.0388
25. Witzel, TC, Eshun-Wilson, I, Jamil, MS, Tilouche, N, Figueroa, C, Johnson, CC, et al. Comparing the effects of HIV self-testing to standard HIV testing for key populations: a systematic review and meta-analysis. BMC Med. (2020) 18:381. doi: 10.1186/s12916-020-01835-z
26. Centers for Disease Control and Prevention. HIV basic statistics. Available online at: https://www.cdc.gov/hiv/basics/statistics.html (Accessed September 26, 2022)
27. Beyrer, C, Baral, SD, van Griensven, F, Goodreau, SM, Chariyalertsak, S, Wirtz, AL, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. (2012) 380:367–77. doi: 10.1016/S0140-6736(12)60821-6
28. Centers for Disease Control and Prevention. HIV and Gay and Bisexual Men: HIV Risk Behaviors (2022) Available online at: https://www.cdc.gov/hiv/group/msm/msm-content/risk-behaviors.html.
29. Abara, W, Annang, L, Spencer, SM, Fairchild, AJ, and Billings, D. Understanding internet sex-seeking behaviour and sexual risk among young men who have sex with men: evidences from a cross-sectional study. Sex Transm Infect. (2014) 90:596–601. doi: 10.1136/sextrans-2014-051545
30. Liau, A, Millett, G, and Marks, G. Meta-analytic examination of online sex-seeking and sexual risk behavior among men who have sex with men. Sex Transm Dis. (2006) 33:576–84. doi: 10.1097/01.olq.0000204710.35332.c5
31. Li, XF, Zhang, BC, Chu, QS, Wang, N, Wang, YF, and Yu, ZZ. Associations between partner-seeking activities through internet and sexual risk behaviours related to HIV/AIDS among men who have sex with men in China. Zhonghua Liu Xing Bing Xue Za Zhi. (2008) 29:685–8.
32. Zhong, F, Lin, P, Xu, H, Wang, Y, Wang, M, He, Q, et al. Possible increase in HIV and syphilis prevalence among men who have sex with men in Guangzhou, China: results from a respondent-driven sampling survey. AIDS Behav. (2011) 15:1058–66. doi: 10.1007/s10461-009-9619-x
33. Bull, SS, and McFarlane, M. Soliciting sex on the internet: what are the risks for sexually transmitted diseases and HIV? Sex Transm Dis. (2000) 27:545–50. doi: 10.1097/00007435-200010000-00008
34. Lau, JT, Lau, M, Cheung, A, and Tsui, HY. A randomized controlled study to evaluate the efficacy of an internet-based intervention in reducing HIV risk behaviors among men who have sex with men in Hong Kong. AIDS Care. (2008) 20:820–8. doi: 10.1080/09540120701694048
35. 2021 Ud. Joint United Nations Programme on HIV/AIDS (UNAIDS). Geneva (2021); Available online at: https://www.unaids.org/en/resources/documents/2021/2021_unaids_data (Accessed August 27, 2015).
36. Lundgren, JD, Babiker, AG, Gordin, F, Emery, S, Grund, B, Sharma, S, et al. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. (2015) 373:795–807. doi: 10.1056/NEJMoa1506816
37. Grinsztejn, B, Hosseinipour, MC, Ribaudo, HJ, Swindells, S, Eron, J, Chen, YQ, et al. Effects of early versus delayed initiation of antiretroviral treatment on clinical outcomes of HIV-1 infection: results from the phase 3 HPTN 052 randomised controlled trial. Lancet Infect Dis. (2014) 14:281–90. doi: 10.1016/S1473-3099(13)70692-3
Keywords: men who have sex with men, HIV, HIV self-testing, peer support, behavior
Citation: Lyu H, Ni Y, He X, Wang D, Yu X, Tang W and Zhou Y (2025) Peer support to improve the secondary distribution of Internet-based HIV self-testing kits among men who have sex with men in Zhuhai, China. Front. Public Health. 13:1522425. doi: 10.3389/fpubh.2025.1522425
Edited by:
Zisis Kozlakidis, International Agency for Research on Cancer (IARC), FranceReviewed by:
Tolulope Olumide Afolaranmi, University of Jos, NigeriaOlivia Sison, University of the Philippines Manila, Philippines
Copyright © 2025 Lyu, Ni, He, Wang, Yu, Tang and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weiming Tang, d2VpbWluZ190YW5nQG1lZC51bmMuZWR1; Yi Zhou, emhvdXlpXzg4OEAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
 Hang Lyu
Hang Lyu Yuxin Ni
Yuxin Ni Xi He4
Xi He4 Weiming Tang
Weiming Tang Yi Zhou
Yi Zhou