- Department of Otorhinolaryngology Head and Neck Surgery, Zhongshan Hospital of Traditional Chinese Medicine, Affiliated to Guangzhou University of Chinese Medicine, Zhongshan, Guangdong, China
Background: Complete hearing loss, especially the age-related type, poses a significant public health challenge globally. This study aims to assess the global burden on the prevalence of complete hearing loss from 1992 to 2021 and forecast trends up to 2036.
Methods: Using data from the Global Burden of Disease (GBD) Study 2021, we assessed the global burden of complete hearing loss across 204 countries and territories. We analyzed temporal trends in ASPR using Joinpoint regression, evaluated the contributions of age, period, and cohort effects through Age-Period-Cohort modeling, and performed decomposition analysis to determine the impact of demographic and epidemiological changes on prevalence trends. Predictions of future ASPR trends were made using Bayesian Age-Period-Cohort (BAPC) and Autoregressive Integrated Moving Average (ARIMA) models.
Results: By 2021, the global prevalence of complete hearing loss had reached 9.9 million cases, with the ASPR declining from 134.35 to 117.79 per 100,000. The overall Estimated Annual Percentage Change (EAPC) was−0.45. The most significant reductions were observed in low-SDI regions, particularly Sub-Saharan Africa (EAPC: −0.74). In contrast, high-SDI regions, including North America and Western Europe, showed more modest declines (EAPC: −0.18). Notably, East Asia exhibited a 62.3% increase in prevalence, with high-income Asia Pacific showing the highest relative rise at 83.97%. Age-related hearing loss remained the dominant cause, especially among individuals aged 60 and above. Males were more affected than females. Population aging and growth were the major drivers of the increased prevalence in high-SDI regions, while population growth was the primary factor in low-SDI areas.
Conclusion: The burden of complete hearing loss remains high in prevalence, particularly in aging populations within high-SDI regions, despite overall reductions in ASPR. Significant regional disparities remain, highlighting the need for targeted interventions to improve access to hearing care and affordable technologies in low-SDI regions.
Introduction
Complete hearing loss is the most severe hearing impairment, which significantly impacts communication abilities, quality of life, and overall well-being. Hearing loss is a global public health issue that affects millions of people worldwide, with profound implications for individuals and societies (1–3). The etiology of complete hearing loss is multifactorial, involving genetic, environmental, and lifestyle factors (3). Age-related hearing loss, also known as presbycusis, is the most common cause and typically affects individuals over the age of 60 (4). Recent advancements in cochlear implants and hearing aids have provided some relief to those affected. However, challenges remain, particularly in low-and middle-income countries where access to healthcare and assistive technologies is limited (2, 5, 6). Moreover, the stigma associated with hearing loss often leads to social isolation and mental health issues, exacerbating the burden on individuals and healthcare systems (7, 8).
Globally, the distribution of hearing loss is uneven, with significant disparities between regions and socio-demographic groups. High-income countries generally report lower prevalence rates due to better access to healthcare and early intervention programs (9). In contrast, low-and middle-income countries bear a disproportionate burden of hearing loss, driven by factors such as poor healthcare infrastructure, lack of awareness, and higher exposure to risk factors (10). The Global Burden of Disease (GBD) study highlights these disparities, revealing that regions like Sub-Saharan Africa and South Asia have some of the highest rates of hearing loss, while North America and Europe have comparatively lower rates (11). These findings underscore the need for targeted public health interventions to address the growing burden of hearing loss globally.
Using data from the GBD study, this study aims to assess the global burden of complete hearing loss from 1992 to 2021, focusing on age-related causes, and forecast trends up to 2036.
Materials and methods
Data source
This study utilized data from the GBD Study 20211, which offers comprehensive epidemiological estimates for a wide array of diseases and injuries across 204 countries and territories. The GBD database, maintained by the Institute for Health Metrics and Evaluation (IHME), provides detailed information on disease prevalence, incidence, and mortality, stratified by age, sex, and location from 1990 to 2021 (11, 12). For this analysis, we focused on the prevalence of complete hearing loss, examining data from 1992 to 2021 to understand temporal trends and geographic variations in disease burden. The study also utilized the Socio-Demographic Index (SDI) to stratify countries and regions, facilitating an analysis of the relationship between socio-economic development and prevalence of complete hearing loss. The SDI data are available for download on IHME Websites2.
Statistical analysis
The prevalence of complete hearing loss was assessed in terms of the age-standardized prevalence rate (ASPR) per 100,000 population. We calculated ASPR for the years 1992 and 2021 to examine changes over this period. The temporal trends in ASPR were analyzed using the Estimated Annual Percentage Change (EAPC). EAPC was calculated for the global population, as well as stratified by gender, SDI quintiles, and geographical regions (13). Joinpoint regression analysis was utilized to identify significant shifts in the trends of ASPR over time. This method pinpointed specific points where the trend notably changed, allowing for the calculation of the annual percentage change (APC) within each identified segment (14). To explore the effects of age, period, and birth cohort on the prevalence of complete hearing loss, we employed an Age-Period-Cohort model. This approach was used to distinguish the independent effects of aging, temporal trends, and generational differences on hearing loss prevalence (15). To predict the future trends in ASPR from 2022 to 2036, we applied the Bayesian Age-Period-Cohort (BAPC) model and the Autoregressive Integrated Moving Average (ARIMA) model (16–18).
To quantify the contributions of population growth, aging, and epidemiological changes to the observed trends on prevalence of complete hearing loss, we conducted a decomposition analysis. This analysis disaggregates the overall change in prevalence into components attributable to demographic and epidemiological factors (19). The decomposition was performed across different SDI quintiles to assess how socio-economic development influenced these factors. Health inequality in prevalence of complete hearing loss was assessed using the slope index of inequality (SII) and concentration curves (3, 20). SII measures the absolute difference in prevalence between the highest and lowest socio-economic groups, while concentration curves depict the cumulative distribution of prevalence relative to SDI rank. These methods were used to evaluate changes in the distribution of hearing loss burden from 1992 to 2021, particularly in relation to socio-economic disparities.
We employed geospatial mapping techniques to visualize the global distribution of ASPR and EAPC, highlighting regions with high and low burdens of hearing loss. In addition, we analyzed the prevalence of hearing loss across different age groups and genders, with a focus on identifying demographic patterns and trends. Bar charts and line graphs were generated to depict these relationships, providing a comprehensive view of the factors influencing hearing loss prevalence.
Joinpoint regression analysis was conducted using Joinpoint software (version 5.2.0)3. Except the Joinpoint regression analysis, other statistical analyses were conducted using R software (version 4.4.1)4, with specific packages (such as “Joinpoint,” “Epi,” “BAPC,” “INLA,” etc.) utilized for the respective analyses. p < 0.05 suggests statistically significant.
Results
ASPR in 1992 and 2021 and its temporal trends from 1992 to 2021
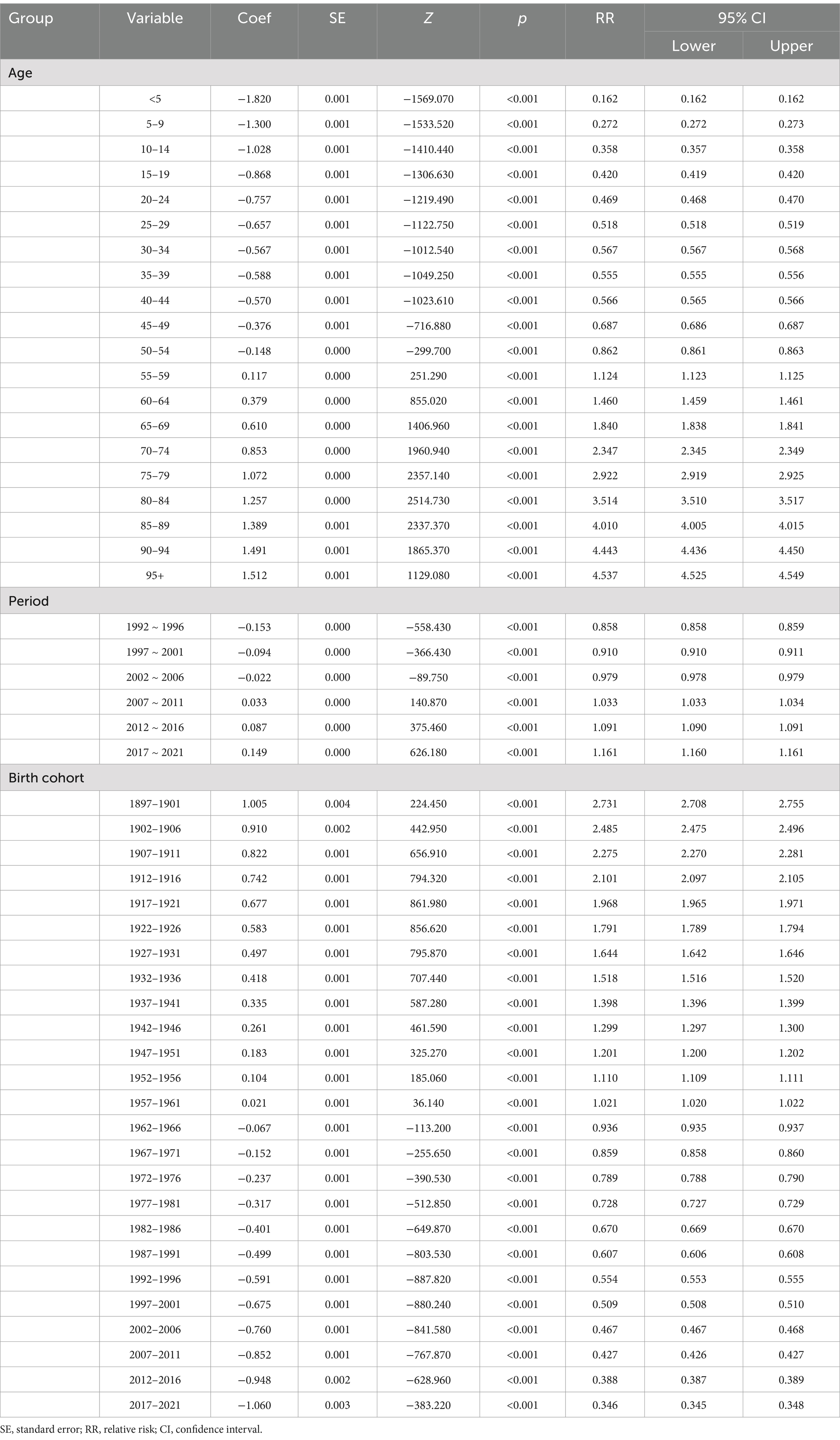
By 2021, the global prevalence of complete hearing loss had increased to nearly 9.9 million cases, with an ASPR of 117.79 per 100,000 population, which represents a slight decrease from the 134.35 per 100,000 recorded in 1992. The overall EAPC was −0.45. Notably, the trend differed between males and females, with males experiencing a more pronounced reduction in ASPR (from 131.36 to 114.03 per 100,000) compared to females (from 136.51 to 120.78 per 100,000) (Table 1). The EAPC for males was −0.48, slightly higher than the −0.42 observed for females. When examining SDI levels, significant disparities emerged (Table 1). Low SDI regions showed a marked decline in ASPR, from 203.52 to 167.32 per 100,000, with an EAPC of −0.74. Low-middle SDI regions experienced a more pronounced decline with an EAPC of −0.93. In contrast, high SDI regions saw a more modest decrease in ASPR (from 112.41 to 105.35 per 100,000) with an EAPC of −0.18, indicating that while improvements have been made, they have been less substantial compared to lower SDI regions. Geographically, the burden of complete hearing loss also varied significantly across 21 regions (Table 1). For instance, North Africa and the Middle East witnessed a substantial decrease in ASPR from 277.9 to 192.41 per 100,000, with a striking EAPC of −1.31. Moreover, in high-income areas such as North America and the Asia Pacific, the decrease in ASPR was modest, with EAPCs of −0.33 and −0.33, respectively, (Table 1).
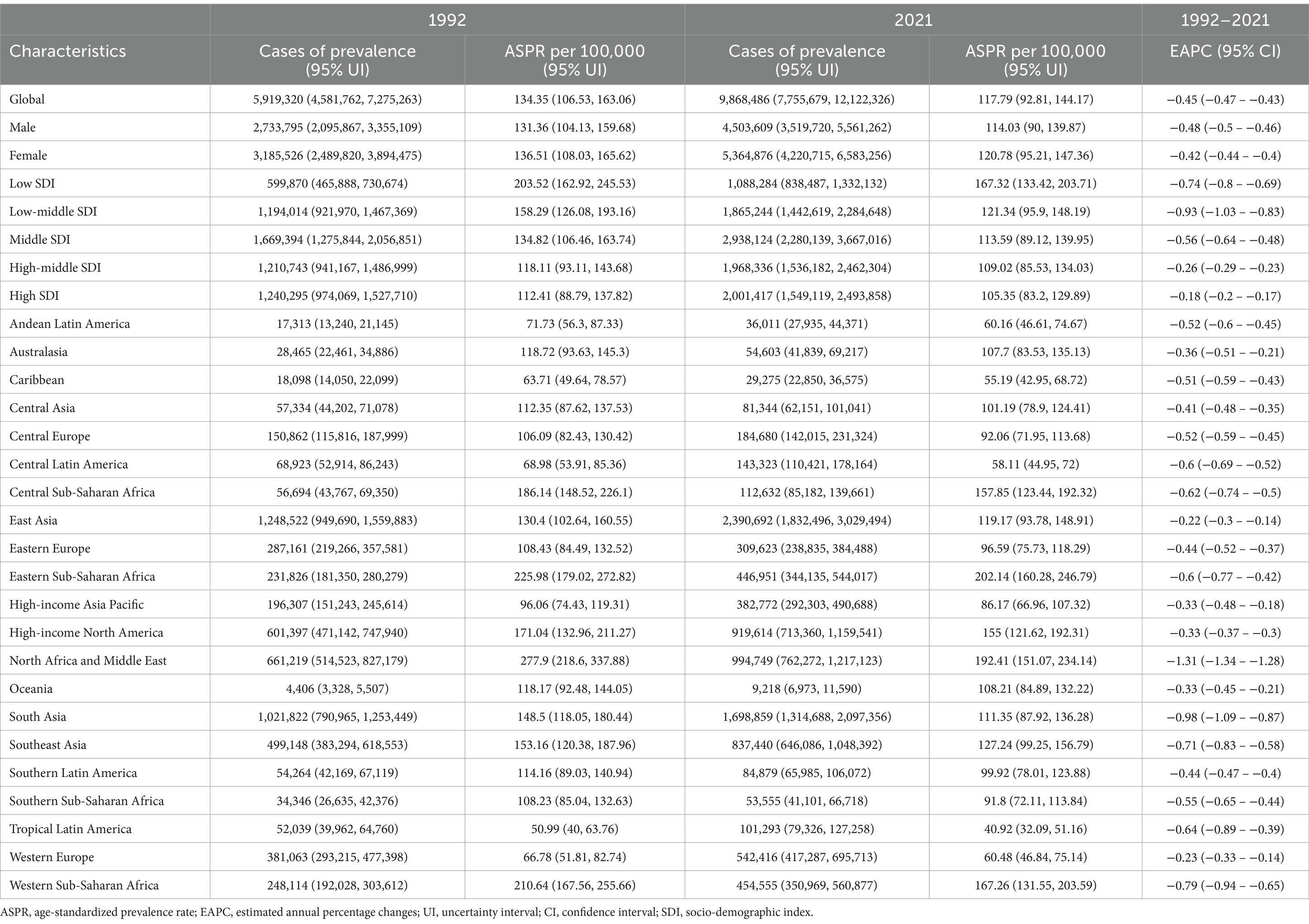
Table 1. The cases of prevalence and ASPR of complete hearing loss in 1992 and 2021, and its temporal trends from 1992 to 2021.
Supplementary Table S1 depicts the cases of prevalence and ASPR of complete hearing loss in 1992 and 2021, and its temporal trends from 1992–2021 among 204 countries and territories. In the world map of ASPR in 2021 (Figure 1A), the Horn of Africa, parts of the Middle East, and specific regions in North Africa demonstrate notably higher ASPR values, while South America (particularly Brazil) and parts of Central America exhibit lower ASPR values. In the world map of EAPC from 1992 to 2021 (Figure 1B), areas with slower reduction in EAPC include North America, China, Australia, and parts of Northern Europe, while areas with greater decreases in EAPC include portions of the Middle East, Persian Gulf, and select African territories.
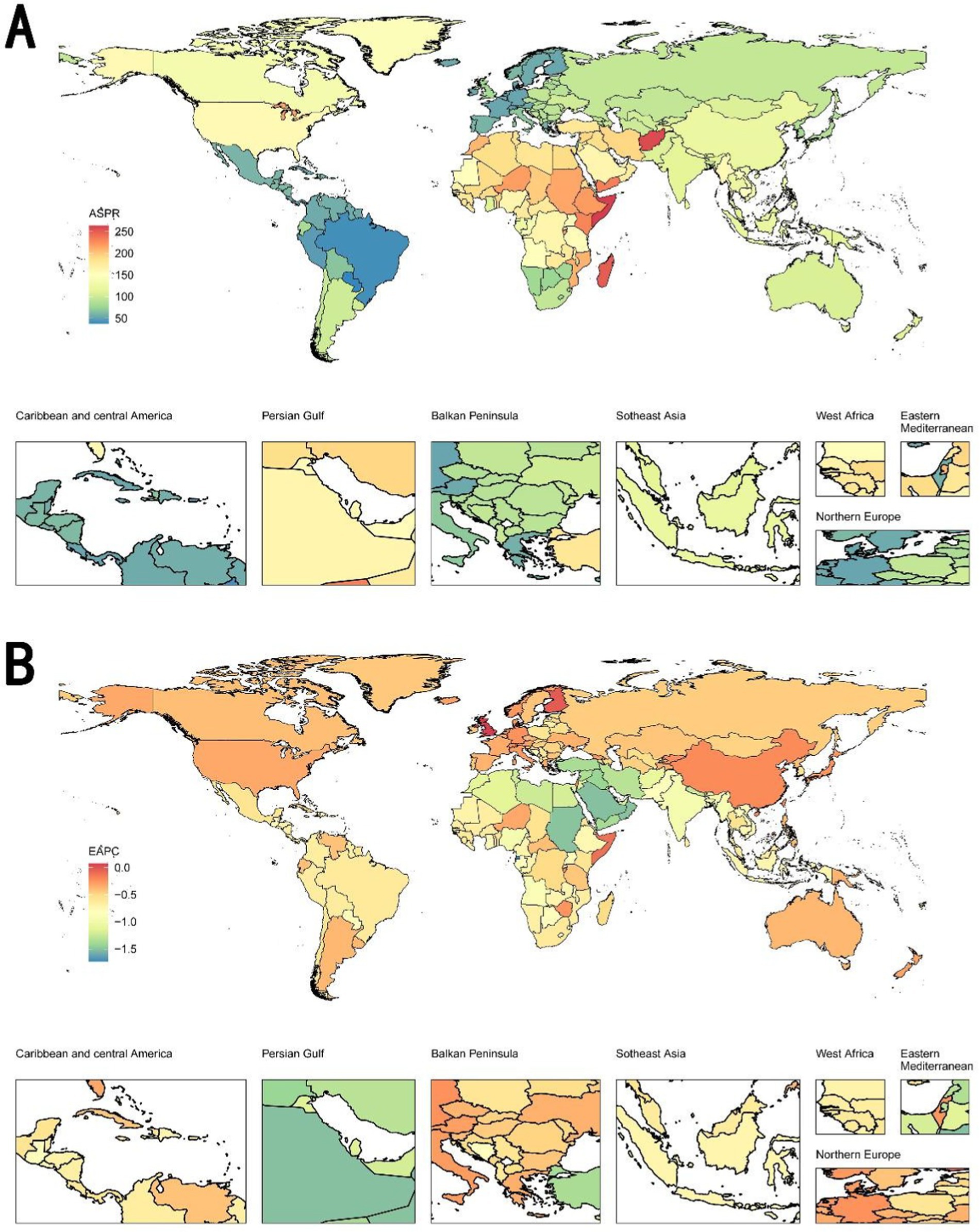
Figure 1. World maps of ASPR in 2021 and EAPC from 1992 to 2021 on complete hearing loss. (A) World map of ASPR in 2021. The Horn of Africa, parts of the Middle East, and specific regions in North Africa demonstrate notably higher ASPR values, while South America (particularly Brazil) and parts of Central America exhibit lower ASPR regions in South America, parts of Africa, and some countries in Eastern Europe show relatively higher ASPR. Conversely, many regions in North America, Northern Europe, and Southeast Asia exhibit lower ASPR values. (B) World map of EAPC from 1992 to 2021. Areas with slower reduction or slight increases in EAPC include North America, China, Australia, and parts of Northern Europe, while areas with higher reduction in EAPC include portions of the Middle East, Persian Gulf, and select African territories. ASPR, age-standardized prevalence rate; EAPC, estimated annual percentage change.
Prevalence rate in 1992 and 2021, and its relative change between 1992 and 2021
The prevalence rate increased by 16.13%, from 107.68 per 100,000 in 1992 to 125.05 per 100,000 in 2021 (Table 2). When examining gender differences, both males and females experienced an increase in prevalence rates, with females showing a slightly higher relative change of 16.81% compared to 15.25% in males (Table 2). High-SDI regions exhibited the most substantial increase in prevalence rate, rising by 31.80% from 138.8 per 100,000 in 1992 to 182.94 per 100,000 in 2021 (Table 2). Similarly, high-middle SDI regions saw a 35.46% increase in prevalence. In contrast, low SDI regions experienced a decrease in prevalence by 14.54%. Geographically, East Asia witnessed a dramatic increase of 62.30% in the prevalence rate of complete hearing loss, the highest among all regions (Table 2). High-income Asia Pacific also saw a notable increase of 83.97%. Conversely, regions like Central Sub-Saharan Africa and Eastern Sub-Saharan Africa experienced declines in prevalence rates by 15.50 and 8.72%, respectively. In Western Sub-Saharan Africa, the prevalence rate decreased significantly by 23.67%. However, these trends contrast with the increases seen in regions such as Central Europe, where the prevalence rate rose by 32.94%, and Central Latin America, which saw a significant increase of 41.10%.
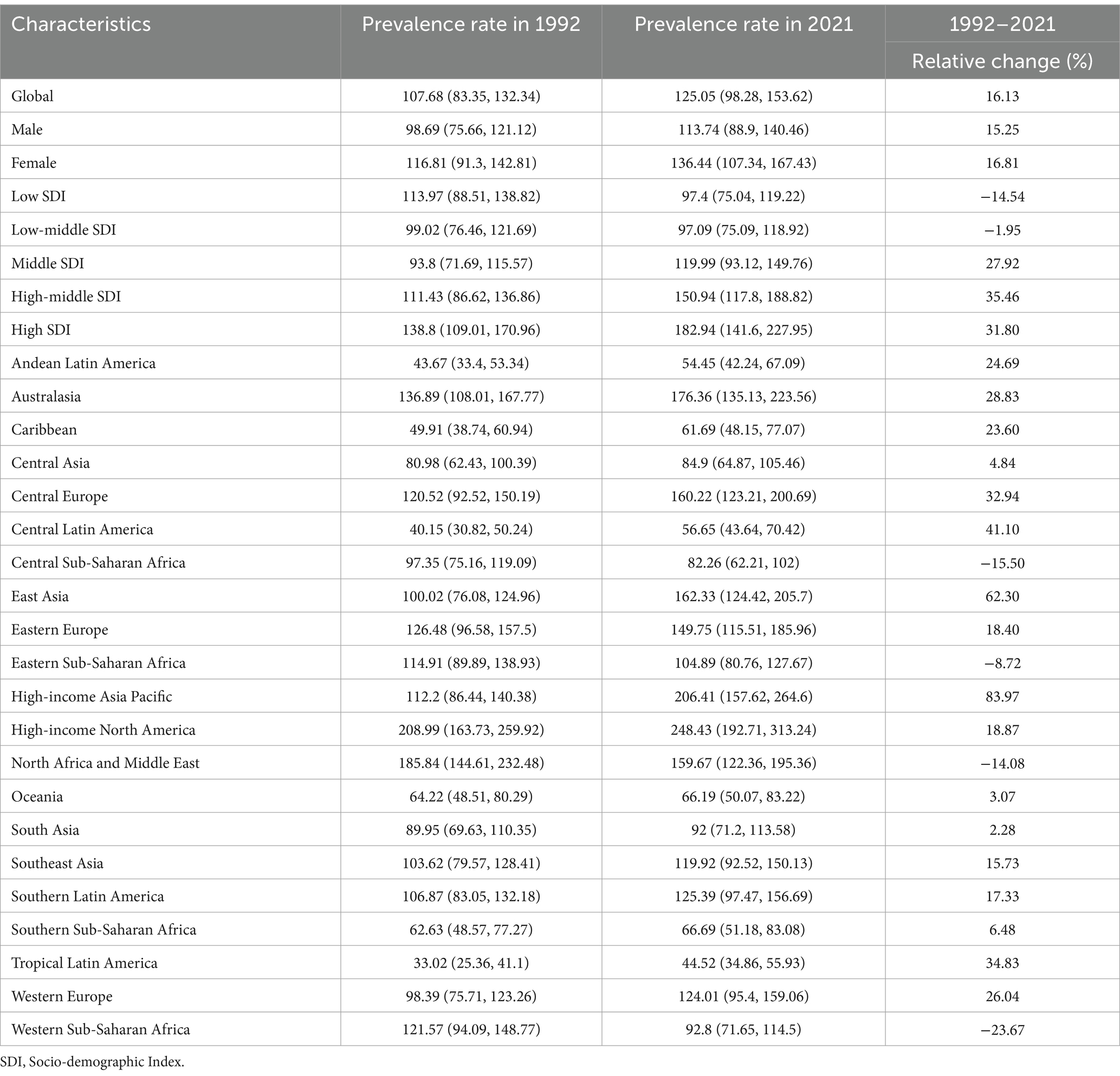
Table 2. The prevalence rate of complete hearing loss in 1992 and 2021, and its relative change between 1992 and 2021.
Supplementary Table S2 depicts the prevalence rate of complete hearing loss in 1992 and 2021, and its relative change from 1992–2021 among 204 countries and territories. In the world map of prevalence in 2021 (Figure 2A), the United States and Canada exhibited the highest prevalence rates globally, while Brazil, Colombia, and Peru demonstrate substantially lower rates. In the world map of relative change from 1992 to 2021 (Figure 2B), Sudan and Mauritania exhibit high increases of relative change, while Nigeria, Angola, and Algeria show notable decreases.
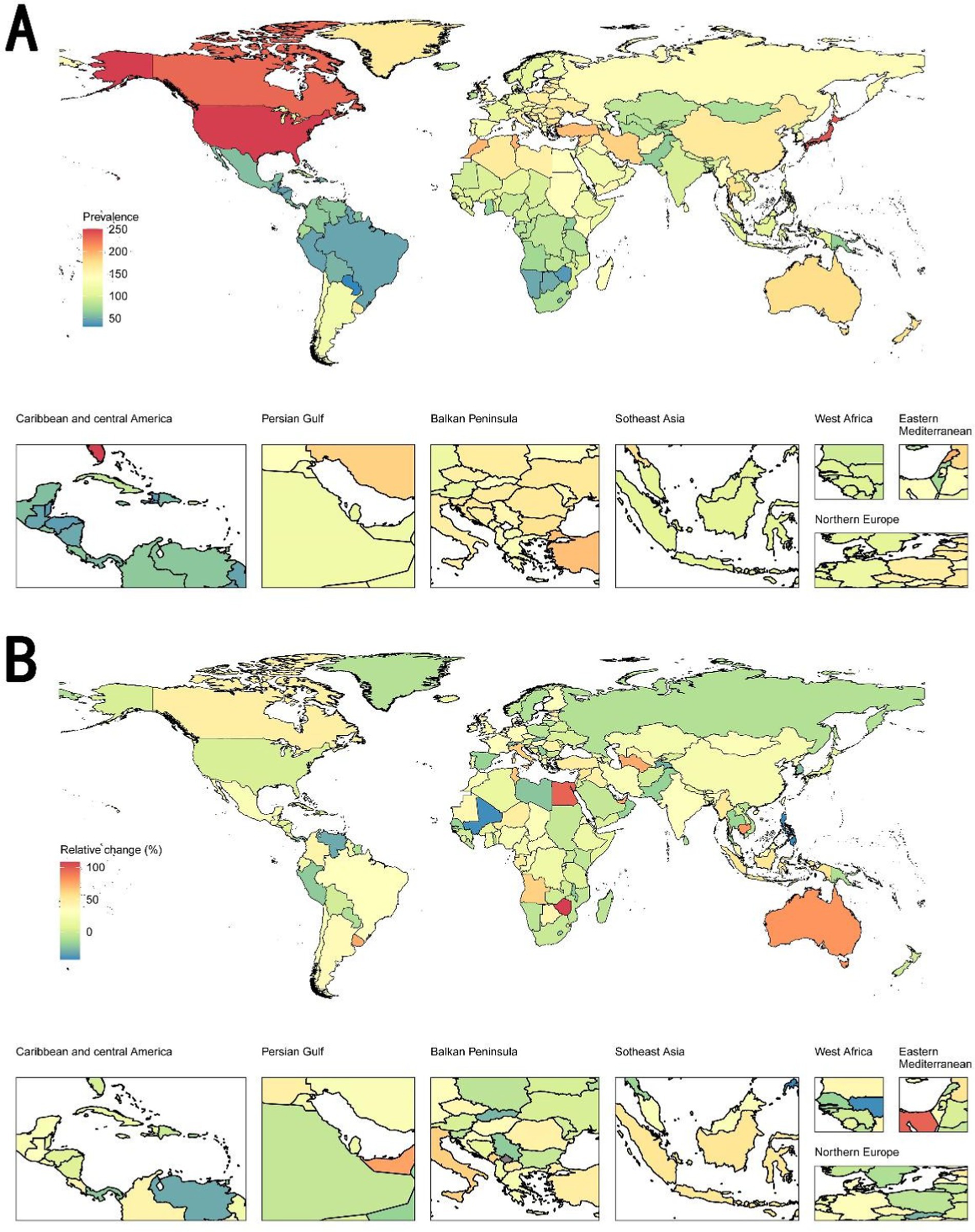
Figure 2. World maps of prevalence rate in 2021 and relative change from 1992 to 2021 on complete hearing loss. (A) World maps of prevalence rate in 2021. The United States and Canada exhibited the highest prevalence rates globally, while Brazil, Colombia, and Peru demonstrate substantially lower rates. (B) World map of relative change from 1992 to 2021. Regions marked in red indicate an increase in prevalence, while regions in green show a decrease. Sudan and Mauritania exhibit high increases of relative change, while Nigeria, Angola, and Algeria show notable decreases.
Age and temporal trends on prevalence
Figure 3A illustrates that the prevalence of complete hearing loss increases sharply with age in 2021, particularly after age of 60. The rate is slightly higher in females compared to males, especially in the older age groups. Figure 3B displays that the number of prevalent cases has steadily increased over the years for both males and females, while ASPR has slightly decreased during the same period.
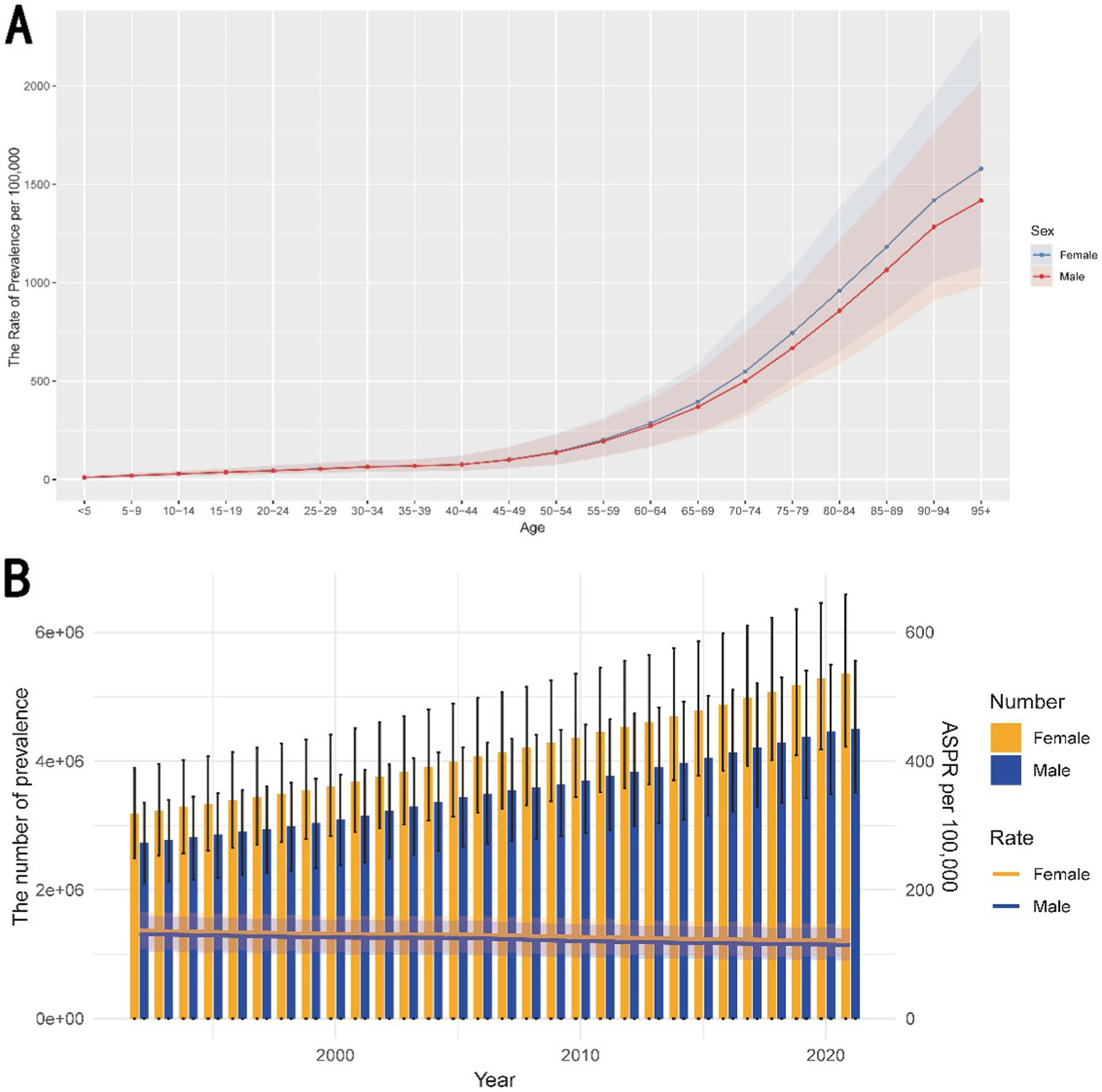
Figure 3. Age and temporal trends on prevalence of complete hearing loss. (A) The trend of prevalence with the increasing age. The graph illustrates the rate of prevalence per 100,000 population across different age groups in 2021, separately for males and females. The prevalence of hearing loss increases sharply with age, particularly after age of 60. This trend suggests that aging is a significant risk factor for hearing loss, with a higher burden observed in older females compared to males. (B) The temporal trend on prevalence from 1992 to 2021. It displays the temporal trends in the number of prevalent cases and ASPR per 100,000 population from 1992 to 2021, again disaggregated by sex. The number of prevalent cases has steadily increased over the years for both males and females, while ASPR has slightly decreased during the same period. ASPR, age-standardized prevalence rate.
The number of prevalence in different ages and SDI in 2021
Supplementary Figure S1A shows that the prevalence increases significantly with age, with a noticeable gender disparity. Females exhibit higher prevalence rates than males in most age groups, particularly from ages 45–90, where the difference is most pronounced. Supplementary Figure S1B illustrates that the prevalence is highest in middle SDI regions, with females showing a higher prevalence compared to males.
Joinpoint regression analysis of ASPR
Table 3 and Supplementary Figure S2A shows that for males, the ASPR steadily decreased from 1992 to 2021, with three distinct phases identified by the joinpoint analysis. The 1992–2000 period showed significant decline (APC = −0.54%, p < 0.001), followed by a plateau phase during 2000–2005 (APC = −0.05%, p = 0.28). The most pronounced reduction occurred during 2005–2011 (APC = -0.82%, p < 0.001), followed by a moderate but significant continuing decline through 2011–2021 (APC = −0.44%, p < 0.001). Supplementary Figure S2B demonstrates that for females, the ASPR also experienced a continuous decline over the study period. The rate of decrease was slightly more gradual in females compared to males. The first segment from 1992 to 2000 showed a significant decline (APC = −0.47, p < 0.001), followed by a slower decline from 2000 to 2005 (APC = −0.14, p < 0.001). The decline became more pronounced from 2005 to 2015 (APC = −0.55, p < 0.001), and this trend persisted from 2015 to 2021 (APC = −0.35, p < 0.001).
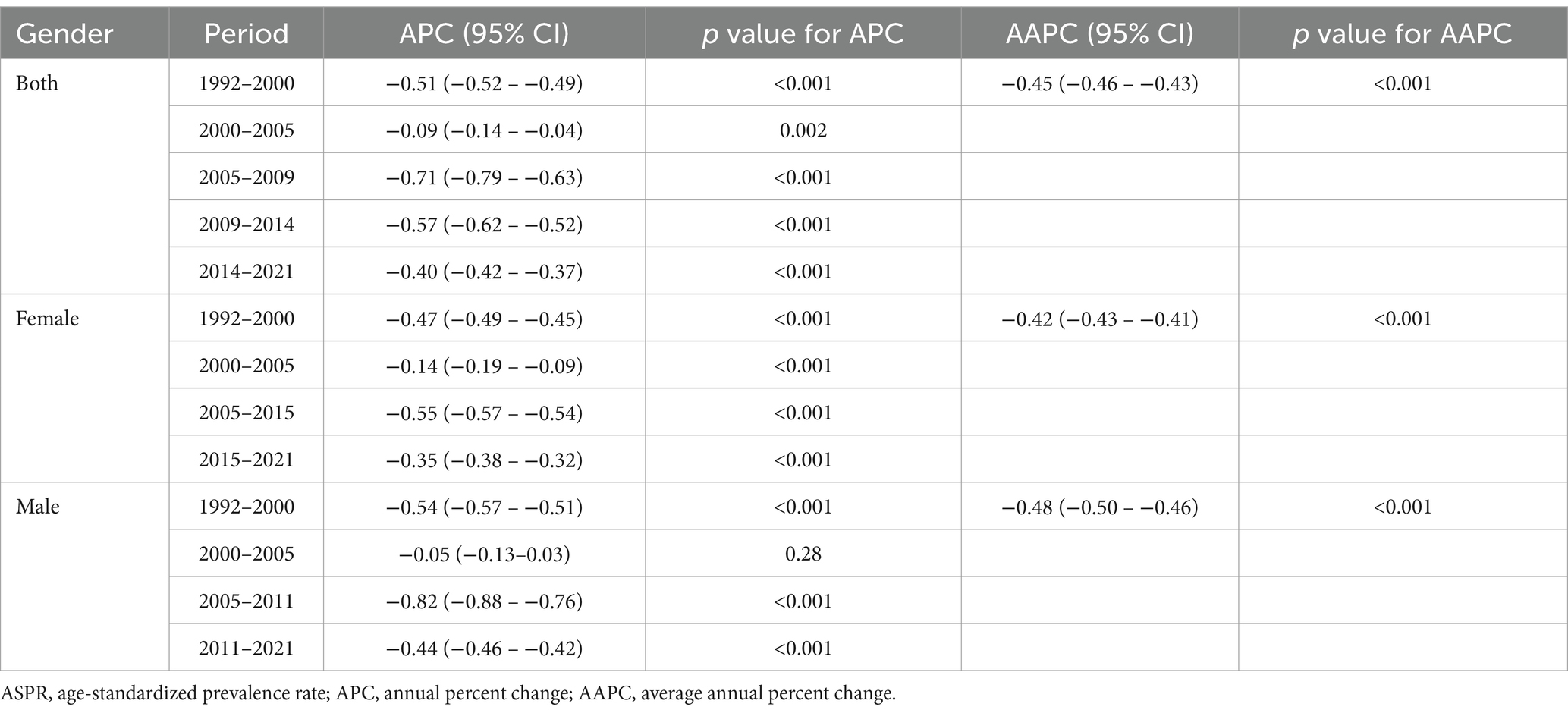
Table 3. Joinpoint regression analysis: trends in ASPR among both sexes, males, and females, 1992–2021.
Age, period, and cohort effects on prevalence
For age, Supplementary Figure S3 shows a sharp increase in risk with advancing age. The relative risks (RRs) escalate significantly starting from the age group of 45–49 years, peaking in the oldest age group (90–94 years and 95+). For period, Supplementary Figure S3 shows a slight increase in relative risk across the periods from 1992–1996 to 2017–2021. For birth cohort, Supplementary Figure S3 shows a decreasing trend in relative risk across successive birth cohorts from 1897–1901 to 2017–2021. The detailed data is shown in Table 4.
Supplementary Figure S4 presents the Age-Period-Cohort analysis, showing the interaction between age, periods, and cohorts in determining the prevalence rates.
Decomposition analysis of prevalence
Supplementary Figure S5A shows that population growth is the most significant contributor to the increase in complete hearing loss cases across all sexes, with the largest impact observed in females. In higher SDI regions, aging is the dominant factor driving the increase in prevalence of complete hearing loss (Supplementary Figure S5B). However, in lower SDI regions (low-middle and low SDI areas), population growth is the predominant factor.
Frontier analysis of ASPR
Supplementary Figure S6A demonstrates a positive correlation between SDI and the prevalence of complete hearing loss from 1992 to 2021. Higher SDI levels are associated with a decreased prevalence of hearing loss, with a noticeable upward trend over the two decades. Supplementary Figure S6B focuses on the trend analysis of specific countries.
Health inequality analysis of prevalence
In 1992, the SII was negative (−17.16) (Supplementary Figure S7A). However, by 2021, this trend had reversed, with an SII of 39.19, reflecting a higher prevalence of hearing loss in countries with higher SDI. Supplementary Figure S7B presents a concentration curve that compares the cumulative distribution of the population ranked by SDI with the cumulative fraction of hearing loss prevalence. The concentration index was 0.03 in 1992 and − 0.05 in 2021, indicating a shift toward a more equitable distribution.
The correlation between SDI and ASPR of complete hearing loss
Supplementary Figure S8A suggests that regions with lower SDI, such as Sub-Saharan Africa and South Asia, have higher ASPR. These regions show a gradual decline in ASPR over time but remain higher compared to high SDI regions like Western Europe and North America. Supplementary Figure S8B indicates that countries having lower SDI, such as Somalia and Afghanistan, showing higher ASPR, while high SDI countries like Luxembourg and Singapore exhibit lower ASPR.
Prevalence of complete hearing loss in different causes
Figure 4A displays the distribution of prevalence across various age groups in 2021. The prevalence of age-related and other hearing loss markedly increases with age, peaking in the 70–74 age group. This is followed by a slight decline in the older age groups. Congenital birth defects and hearing loss due to meningitis are significantly less prevalent and are relatively consistent across all age groups, with a noticeable concentration in younger populations for congenital birth defects. Figure 4B shows the temporal trends in the prevalence of these hearing loss types from 1992 to 2021. Age-related and other hearing loss has steadily increased over the years, reflecting the aging global population. Congenital birth defects and hearing loss due to meningitis, however, have shown only minor fluctuations over time, with congenital birth defects maintaining a slightly increasing trend, while the prevalence of hearing loss due to meningitis has a substantial decrease.
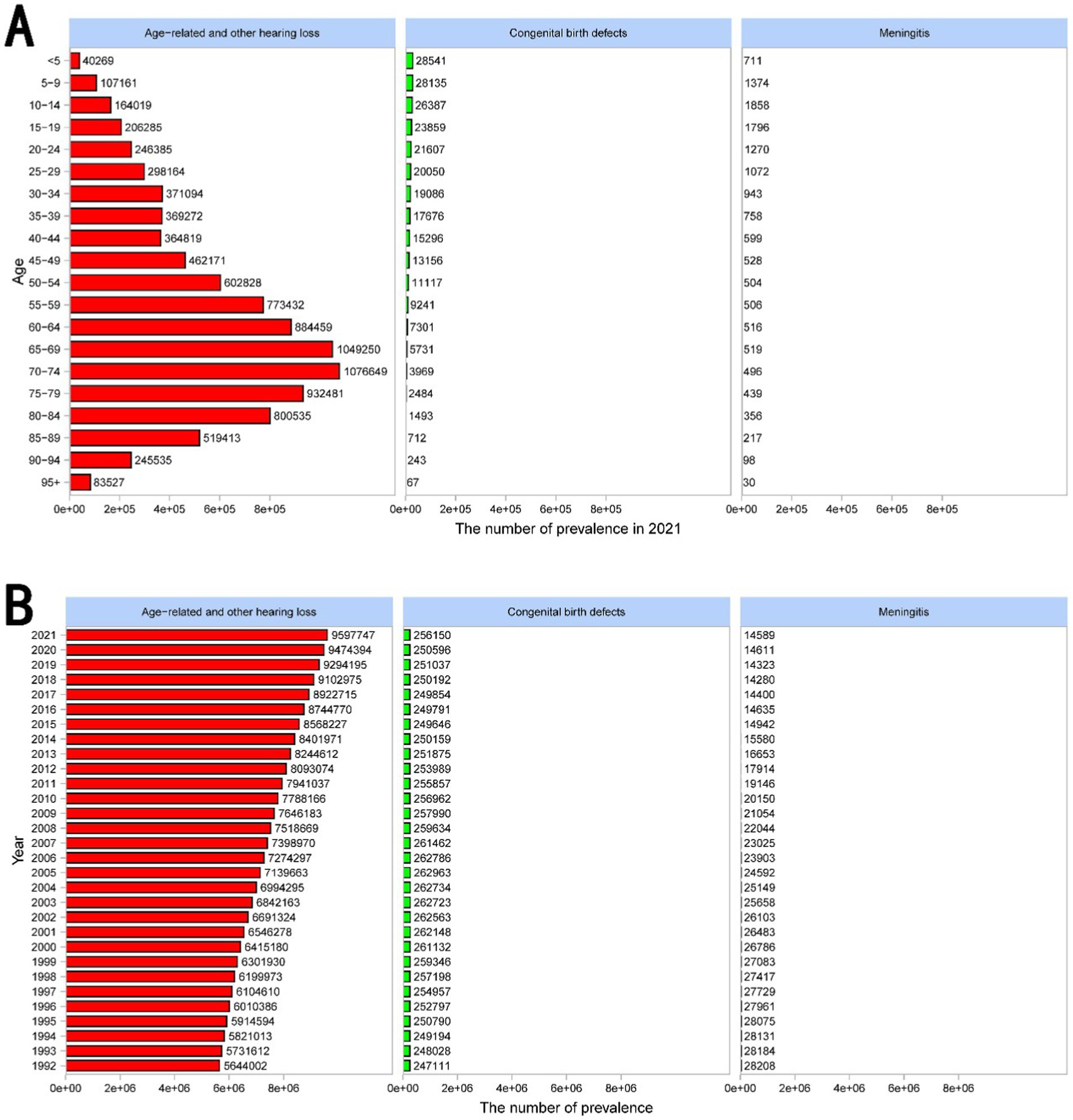
Figure 4. Prevalence of complete hearing loss across all age groups and years in different causes. (A) The bar chart displays the distribution of prevalence across various age groups in 2021. The prevalence of age-related and other hearing loss markedly increases with age, peaking in the 70–74 age group. This is followed by a slight decline in the older age groups. Congenital birth defects and hearing loss due to meningitis are significantly less prevalent and are relatively consistent across all age groups, with a noticeable concentration in younger populations for congenital birth defects. (B) The bar chart shows the temporal trends in the prevalence of these hearing loss types from 1992 to 2021. Age-related and other hearing loss has steadily increased over the years, reflecting the aging global population. Congenital birth defects and hearing loss due to meningitis, however, have shown only minor fluctuations over time, with congenital birth defects maintaining a slightly increasing trend, while the prevalence of hearing loss due to meningitis has a substantial decrease.
Supplementary Figures S9–S11 illustrates the prevalence of age-related and other hearing loss, congenital birth defects, and meningitis across gender, SDI, and 21 regions in 2021.
These figures all indicate that age-related and other hearing loss is the dominant cause of complete hearing loss. According to the introduction of the GBD database, age-related and other hearing loss includes causes not identified as meningitis, chronic otitis media, or congenital, which is dominantly caused by presbycusis.
Prediction of ASPR from 2022 to 2036
Figures 5A,B illustrates the BAPC model predictions for ASPR for both males and females from 2022 to 2036. The forecasted trend shows a potential stabilization in the decline, suggesting that the rate may plateau or slightly decrease further.
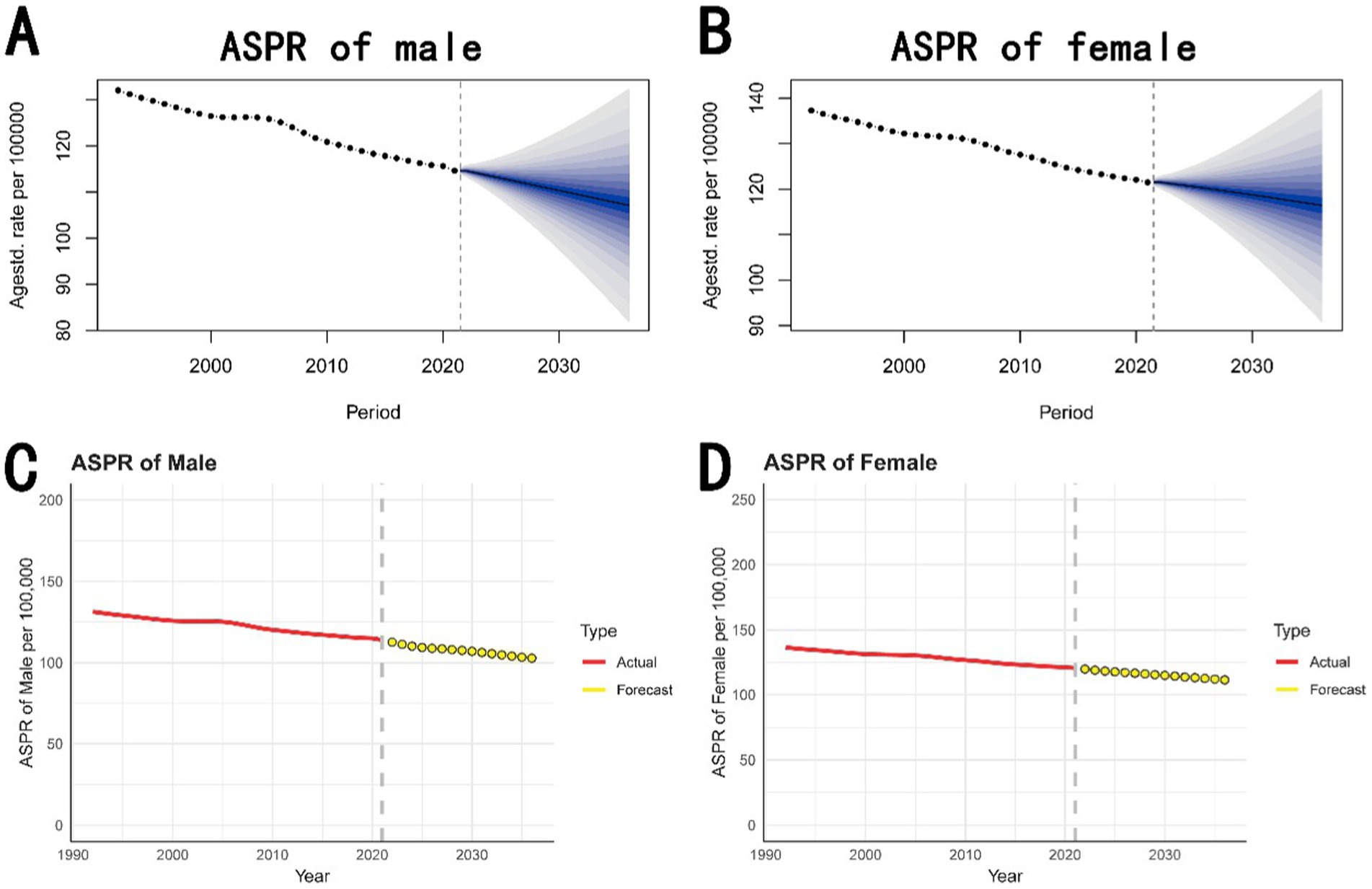
Figure 5. Prediction of ASPR from 2022 to 2036. (A,B) The prediction for males and females based on the BAPC model. It forecasts a decline in ASPR for both males and females from 2022 to 2036, with credible intervals indicating the uncertainty of these projections. (C,D) The prediction for males and females based on the ARIMA model. It similarly predicts a continuing decrease in ASPR, with forecasts extending to 2036. ASPR, age-standardized prevalence rate; BAPC, Bayesian age-period-cohort; ARIMA, autoregressive integrated moving average.
Figures 5C,D presents the ARIMA model forecasts for ASPR for both males and females from 2022 to 2036. It shows that while the prevalence of complete hearing loss may decrease over time, the reduction rate may slow down in the future.
Discussion
This study provides a comprehensive analysis of the global trends in the prevalence and ASPR of complete hearing loss from 1992 to 2021, with a particular focus on age-related hearing loss. The findings indicate a global decline in ASPR, particularly among males, and significant regional and socio-demographic disparities. Regions with lower SDI levels, such as Sub-Saharan Africa and South Asia, experienced the most substantial reductions in ASPR, while high SDI regions, including East Asia, Western Europe, and North America, saw only modest declines. Despite the global decrease in ASPR, the overall prevalence of complete hearing loss has increased, particularly in high and high-middle SDI regions, driven largely by the aging population. The study underscores the growing public health challenge posed by age-related hearing loss, especially in regions with rapidly aging populations. The implications of both models (BAPC and ARIMA) showing a potential stabilization in the decline of ASPR for 2021–2036.
The impact of complete hearing loss on the quality of life in older adults is profound, affecting communication, social, emotional, and cognitive well-being (21, 22). Individuals with age-related hearing loss often struggle to maintain social connections and engage in everyday activities, leading to social isolation, depression, and anxiety (8, 23, 24). This isolation can exacerbate feelings of loneliness and contribute to mental health decline (25, 26). Age-related/untreated hearing loss increases the risk of developing dementia and other cognitive impairments (27–29).
Public health interventions aimed at reducing the burden of age-related hearing loss have shown varying degrees of effectiveness, depending on the socio-demographic context (3, 7, 30, 31). Age-related hearing loss (presbycusis) is the leading cause of hearing impairment in older adults, presenting a growing public health concern globally (21, 30). This condition, marked by a gradual decline in high-frequency hearing, worsens with age. As life expectancy increases, particularly in high-income regions, the prevalence of age-related hearing loss has risen significantly. Advanced healthcare systems in these areas have extended life spans, contributing to a higher prevalence of hearing loss as more people live longer with conditions that predispose them to auditory decline (31). High and high-middle SDI regions, including North America, Western Europe, and East Asia, have seen an increase in prevalence, driven largely by aging populations. These regions face a growing burden of age-related hearing loss, with East Asia experiencing a particularly dramatic rise. The advanced healthcare systems in these regions, while extending life spans, have also resulted in a higher prevalence of hearing loss among the older adult (32). High-SDI regions have more widespread in access to healthcare and hearing aids, with a modest decline in ASPR, suggesting positive impacts from these interventions (33). However, these improvements are not consistent across all low-SDI regions. Many still face substantial challenges, including limited resources, inadequate healthcare infrastructure, and barriers to healthcare access. Thus, the burden of hearing loss remains high, exacerbated by the lack of widespread public health interventions and limited availability of hearing aids and other assistive devices. It underscores the importance of early intervention and access to health interventions and hearing aids to mitigate cognitive decline and improve overall quality of life (34–36). To address these challenges, innovative approaches are needed, such as telemedicine, community-based education, and the development of affordable, low-cost hearing aids tailored for low-resource settings (37, 38). Public-private partnerships and international collaborations are crucial to making these technologies more accessible and affordable.
The trends of prevalence in complete hearing loss underscore the need for targeted public health strategies that address the specific challenges posed by complete hearing loss in aging populations. For example, in Western Europe and North America, where demographic shifts have led to an increase in the number of older adults at risk for hearing loss, studies suggest that up to 70% of individuals aged 70 and older may be impacted by this condition (18). Despite a modest global decline in ASPR, high-SDI regions have experienced less pronounced reductions, likely due to the overwhelming impact of aging populations. This highlights the need for public health strategies that specifically target the hearing health of older adults, including the development and implementation of age-specific hearing loss prevention programs and improved access to hearing aids and cochlear implants (39–41). People with presbycusis may benefit from novel therapies and treatments that would prevent or reverse hearing loss. In low to low-middle SDI regions, such as parts of Sub-Saharan Africa and South Asia, there has been a notable decline in the ASPR. This suggests that public health interventions, improved healthcare access, and educational programs aimed at hearing loss prevention are beginning to show positive effects. For example, Western Sub-Saharan Africa has made significant progress in reducing hearing loss over the past three decades, likely due to targeted initiatives and better access to basic healthcare services (42).
The stable decline of ASPR in for 2021–2036 may be contributed by expected improvements in hearing care accessibility and technological advancements in hearing aids and interventions (33, 38–40). However, the sustained number of prevalence may suffered from continued aging populations globally and limitations of current prevention strategies for age-related hearing loss in many countries (39–42).
This study offers several key strengths that enhance its contribution to the understanding of global hearing loss trends. Firstly, it utilizes comprehensive data from the GBD Study, covering an extensive timeframe from 1992 to 2021, allowing for a robust analysis of long-term trends and regional variations in complete hearing loss. The use of advanced statistical methods, including Joinpoint regression, Age-Period-Cohort modeling, and decomposition analysis, provides a nuanced understanding of the factors influencing hearing loss prevalence. Moreover, the study highlights age-related hearing loss (the most common form of hearing impairment among older adults), addressing a critical public health issue with growing global relevance. By highlighting the disparities between high and low-SDI regions, the research underscores the importance of targeted public health interventions and the need for equitable access to hearing care. Additionally, the projection of future trends up to 2036 offers valuable insights for policymakers and healthcare providers, aiding in the planning and implementation of effective hearing loss prevention and management strategies.
Several limitations need to be acknowledged. One limitation is the potential for reporting biases and inconsistencies in data collection across different regions, which could affect the accuracy of the findings. Additionally, the study did not account for potential confounding factors, such as variations in diagnostic criteria, access to healthcare services, and cultural differences, which could influence the observed trends in ASPR and prevalence. Another limitation is lack of the detailed cause of age-related and other hearing loss. Though age-related hearing loss is by far the largest cause of hearing loss, it is rarely recorded as a category in the GBD database.
Conclusion
The prevalence of complete hearing loss remains high, particularly in aging populations within high-SDI regions, despite overall reductions in ASPR. Significant regional disparities remain, highlighting the need for targeted interventions to improve access to hearing care and affordable technologies in low-SDI regions. Despite progress in healthcare, significant disparities remain, underscoring the need for more equitable access to hearing care. Future research should prioritize understanding the diverse causes of hearing loss and developing affordable interventions for low-resource settings.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: http://ghdx.healthdata.org/gbd-results-tool.
Author contributions
G-JH: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Visualization, Writing – original draft. Z-JF: Supervision, Validation, Writing – review & editing. B-QL: Conceptualization, Methodology, Project administration, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by National Demonstration Pilot Project for the Inheritance and Innovative Development of Traditional Chinese Medicine (No. GZYZS2024D07 and No. YN2024B012), Medical Science and Technology Research Fund of Guangdong Province (No. A2024627), Social Welfare Science and Technology Research Project of Zhongshan City (No. 2023B1068), Special Research Project for the Inheritance and Innovative Development of Traditional Chinese Medicine of Zhongshan City (No. 2024B3011), and Medical Research Project of Zhongshan City (No. 2023J162).
Acknowledgments
We are grateful to the GBD study 2021 data, which were available online from the Global Health Data Exchange (GHDx) query tool (http://ghdx.healthdata.org/gbd-results-tool).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1526719/full#supplementary-material
\Footnotes
1. ^https://vizhub.healthdata.org/gbd-results/
2. ^https://ghdx.healthdata.org/data-type/estimate
References
1. GBD 2019 Hearing Loss Collaborators. Hearing loss prevalence and years lived with disability, 1990-2019: findings from the global burden of disease study 2019. Lancet. (2021) 397:996–1009. doi: 10.1016/S0140-6736(21)00516-X
2. Haile, LM, Orji, AU, Reavis, KM, Briant, PS, Lucas, KM, Alahdab, F, et al. Hearing loss prevalence, years lived with disability, and hearing aid use in the United States from 1990 to 2019: findings from the global burden of disease study. Ear Hear. (2024) 45:257–67. doi: 10.1097/AUD.0000000000001420
3. Jiang, C, Han, K, Yang, F, Yin, S, Zhang, L, Liang, B, et al. Global, regional, and national prevalence of hearing loss from 1990 to 2019: a trend and health inequality analyses based on the global burden of disease study 2019. Ageing Res Rev. (2023) 92:102124. doi: 10.1016/j.arr.2023.102124
5. Chadha, S, Kamenov, K, and Cieza, A. The world report on hearing, 2021. Bull World Health Organ. (2021) 99:242–242A. doi: 10.2471/BLT.21.285643
6. Ye, X, Zhu, D, Chen, S, Shi, X, Gong, R, Wang, J, et al. Effects of providing free hearing aids on multiple health outcomes among middle-aged and older adults with hearing loss in rural China: a randomized controlled trial. BMC Med. (2022) 20:124. doi: 10.1186/s12916-022-02323-2
7. Goman, AM, and Lin, FR. Prevalence of hearing loss by severity in the United States. Am J Public Health. (2016) 106:1820–2. doi: 10.2105/AJPH.2016.303299
8. Motala, A, Johnsrude, IS, and Herrmann, B. A longitudinal framework to describe the relation between age-related hearing loss and social isolation. Trends Hear. (2024) 28:1881549385. doi: 10.1177/23312165241236041
9. Stevens, G, Flaxman, S, Brunskill, E, Mascarenhas, M, Mathers, CD, and Finucane, M. Global and regional hearing impairment prevalence: an analysis of 42 studies in 29 countries. Eur J Pub Health. (2013) 23:146–52. doi: 10.1093/eurpub/ckr176
10. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1223–49. doi: 10.1016/S0140-6736(20)30752-2
11. GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the global burden of disease study 2021. Lancet. (2024) 403:2133–61. doi: 10.1016/S0140-6736(24)00757-8
12. Yu, H, Yin, X, Mao, Y, Chen, M, Tang, Q, and Yan, S. The global burden of nasopharyngeal carcinoma from 2009 to 2019: an observational study based on the global burden of disease study 2019. Eur Arch Otorhinolaryngol. (2022) 279:1519–33. doi: 10.1007/s00405-021-06922-2
13. Lei, S, Chen, L, Ji, P, Li, K, Li, Q, Huang, C, et al. Global burdens of nasopharyngeal carcinoma in children and young adults and predictions to 2040. Oral Oncol. (2024) 155:106891. doi: 10.1016/j.oraloncology.2024.106891
14. Zhang, Y, Liu, J, Han, X, Jiang, H, Zhang, L, Hu, J, et al. Long-term trends in the burden of inflammatory bowel disease in China over three decades: a joinpoint regression and age-period-cohort analysis based on GBD 2019. Front Public Health. (2022) 10:994619. doi: 10.3389/fpubh.2022.994619
15. Li, Y, Ning, Y, Shen, B, Shi, Y, Song, N, Fang, Y, et al. Temporal trends in prevalence and mortality for chronic kidney disease in China from 1990 to 2019: an analysis of the global burden of disease study 2019. Clin Kidney J. (2023) 16:312–21. doi: 10.1093/ckj/sfac218
16. Gong, Y, Jiang, Q, Zhai, M, Tang, T, and Liu, S. Thyroid cancer trends in China and its comparative analysis with G20 countries: projections for 2020–2040. J Glob Health. (2024) 14:4131. doi: 10.7189/jogh.14.04131
17. Wu, B, Li, Y, Shi, B, Zhang, X, Lai, Y, Cui, F, et al. Temporal trends of breast cancer burden in the Western Pacific region from 1990 to 2044: implications from the global burden of disease study 2019. J Adv Res. (2024) 59:189–99. doi: 10.1016/j.jare.2023.07.003
18. Lin, FR, Thorpe, R, Gordon-Salant, S, and Ferrucci, L. Hearing loss prevalence and risk factors among older adults in the United States. J Gerontol A Biol Sci Med Sci. (2011) 66:582–90. doi: 10.1093/gerona/glr002
19. Qi, J, Li, M, Wang, L, Hu, Y, Liu, W, Long, Z, et al. National and subnational trends in cancer burden in China, 2005-20: an analysis of national mortality surveillance data. Lancet Public Health. (2023) 8:e943–55. doi: 10.1016/S2468-2667(23)00211-6
20. Chen, J, Cui, Y, Deng, Y, Xiang, Y, Chen, J, Wang, Y, et al. Global, regional, and national burden of cancers attributable to particulate matter pollution from 1990 to 2019 and projection to 2050: worsening or improving? J Hazard Mater. (2024) 477:135319. doi: 10.1016/j.jhazmat.2024.135319
21. Jafari, Z, Kolb, BE, and Mohajerani, MH. Age-related hearing loss and tinnitus, dementia risk, and auditory amplification outcomes. Ageing Res Rev. (2019) 56:100963. doi: 10.1016/j.arr.2019.100963
22. Slade, K, Plack, CJ, and Nuttall, HE. The effects of age-related hearing loss on the brain and cognitive function. Trends Neurosci. (2020) 43:810–21. doi: 10.1016/j.tins.2020.07.005
23. Chern, A, Irace, AL, and Golub, JS. The laterality of age-related hearing loss and depression. Otol Neurotol. (2022) 43:625–31. doi: 10.1097/MAO.0000000000003531
24. Andries, E, Nelen, J, de Smit, S, Sluyts, M, Gilles, A, Van Rompaey, V, et al. The effect of anxiety and depression on cognition in older adults with severe-to-profound hearing loss. Eur Arch Otorhinolaryngol. (2024) 281:75–81. doi: 10.1007/s00405-023-08080-z
25. Mick, P, Kawachi, I, and Lin, FR. The association between hearing loss and social isolation in older adults. Otolaryngol Head Neck Surg. (2014) 150:378–84. doi: 10.1177/0194599813518021
26. Arjmandi, MK, Neils-Strunjas, J, Nemati, S, Fridriksson, J, Newman-Norlund, S, Newman-Norlund, R, et al. Age-related hearing loss, cognitive decline, and social interaction: testing a framework. J Speech Lang Hear Res. (2024) 67:2743–60. doi: 10.1044/2024_JSLHR-23-00810
27. Katanga, JA, Hamilton, CA, Walker, L, Attems, J, and Thomas, AJ. Age-related hearing loss and dementia-related neuropathology: an analysis of the United Kingdom brains for dementia research cohort. Brain Pathol. (2023) 33:e13188. doi: 10.1111/bpa.13188
28. Ying, G, Zhao, G, Xu, X, Su, S, and Xie, X. Association of age-related hearing loss with cognitive impairment and dementia: an umbrella review. Front Aging Neurosci. (2023) 15:1241224. doi: 10.3389/fnagi.2023.1241224
29. Griffiths, TD, Lad, M, Kumar, S, Holmes, E, McMurray, B, Maguire, EA, et al. How can hearing loss cause dementia? Neuron. (2020) 108:401–12. doi: 10.1016/j.neuron.2020.08.003
30. Tsai, DB, Bush, ML, Weinreich, HM, Schwartz, SR, and Anne, SAdunka OF, et al. Clinical practice guideline: age-related hearing loss. Otolaryngol Head Neck Surg. (2024) 170:S1–S54. doi: 10.1002/ohn.750
31. Goman, AM, Reed, NS, and Lin, FR. Addressing estimated hearing loss in adults in 2060. JAMA Otolaryngol Head Neck Surg. (2017) 143:733–4. doi: 10.1001/jamaoto.2016.4642
32. Clark, D, Zhou, Z, Hussain, SM, Tran, C, Britt, C, Storey, E, et al. Low-dose aspirin and progression of age-related hearing loss: a secondary analysis of the ASPREE randomized clinical trial. JAMA Netw Open. (2024) 7:e2424373. doi: 10.1001/jamanetworkopen.2024.24373
33. Olusanya, BO, Neumann, KJ, and Saunders, JE. The global burden of disabling hearing impairment: a call to action. Bull World Health Organ. (2014) 92:367–73. doi: 10.2471/BLT.13.128728
34. Cederroth, CR, Dyhrfjeld-Johnsen, J, and Canlon, B. Pharmacological approaches to hearing loss. Pharmacol Rev. (2024) 76:1063–88. doi: 10.1124/pharmrev.124.001195
35. Livingston, G, Huntley, J, Sommerlad, A, Ames, D, Ballard, C, Banerjee, S, et al. Dementia prevention, intervention, and care: 2020 report of the lancet commission. Lancet. (2020) 396:413–46. doi: 10.1016/S0140-6736(20)30367-6
36. Livingston, G, Sommerlad, A, Orgeta, V, Costafreda, SG, Huntley, J, Ames, D, et al. Dementia prevention, intervention, and care. Lancet. (2017) 390:2673–734. doi: 10.1016/S0140-6736(17)31363-6
37. Denham, MW, Arnold, ML, Sanchez, VA, Lin, FR, Tucker, LH, Gomez, MC, et al. Design and methods of the early age-related hearing loss investigation randomized controlled trial. Otol Neurotol. (2024) 45:594–601. doi: 10.1097/MAO.0000000000004093
38. Zhao, R, Yue, T, Xu, Z, Zhang, Y, Wu, Y, Bai, Y, et al. Electroencephalogram-based objective assessment of cognitive function level associated with age-related hearing loss. Geroscience. (2024) 46:431–46. doi: 10.1007/s11357-023-00847-w
39. Arnold, ML, Heslin, BJ, Dowdy, M, Kershner, SP, Phillips, S, Lipton, B, et al. Longitudinal policy surveillance of private insurance hearing aid mandates in the United States: 1997-2022. Am J Public Health. (2024) 114:407–14. doi: 10.2105/AJPH.2023.307551
40. Chien, W, and Lin, FR. Prevalence of hearing aid use among older adults in the United States. Arch Intern Med. (2012) 172:292–3. doi: 10.1001/archinternmed.2011.1408
41. Swords, C, Ghedia, R, Blanchford, H, Arwyn-Jones, J, Heward, E, Milinis, K, et al. Socioeconomic and ethnic disparities associated with access to cochlear implantation for severe-to-profound hearing loss: a multicentre observational study of UK adults. PLoS Med. (2024) 21:e1004296. doi: 10.1371/journal.pmed.1004296
Keywords: hearing loss, aging, global burden of disease, trend, prediction
Citation: Huang G-J, Fan Z-J and Lu B-Q (2025) The global prevalence of complete hearing loss in 204 countries and territories from 1992 to 2021: a systematic analysis for the global burden of disease study 2021. Front. Public Health. 13:1526719. doi: 10.3389/fpubh.2025.1526719
Edited by:
João Manuel R. S. Tavares, University of Porto, PortugalReviewed by:
Andrea Migliorelli, University Hospital of Ferrara, ItalyRichard Lutze, University of North Carolina at Chapel Hill, United States
Copyright © 2025 Huang, Fan and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Biao-Qing Lu, Ymlhb3FpbmdsdXp5eUBvdXRsb29rLmNvbQ==
 Guan-Jiang Huang
Guan-Jiang Huang Zhi-Jun Fan
Zhi-Jun Fan Biao-Qing Lu
Biao-Qing Lu