- 1Department of Epidemiology and Health Statistics, School of Public Health, Wenzhou Medical University, Wenzhou, China
- 2School of Mental Health, Wenzhou Medical University, Wenzhou, China
- 3Development and Planning Office of Wenzhou Medical University (University-Local Cooperation Office), Wenzhou, China
Objectives: We aimed to explore the association between body mass index (BMI) trajectories and subsequent healthy aging in Chinese older adults.
Methods: A prospective, population-based cohort study. Older adults (≥60 years) from the Chinese Longitudinal Health and Longevity Survey with three measurements of BMI (2008, 2011, 2014) were eligible for follow-up. Healthy aging was evaluated in 2018 and was defined as being free of major chronic diseases, no physical limitations, no cognitive impairment, and good mental health. We identified BMI trajectories by latent class growth modeling and explored their association with healthy aging by logistic regression model.
Results: Of 2,698 older Chinese (median [IQR] age: 78.00 [71.00, 86.00] years; female: 51.82%), 518 (19.20%) participants had reached healthy aging after follow-up. Three BMI trajectories were identified: low-normal stable (49.30%), normal slight increase (43.07%), and overweight to obesity (7.64%). Compared with the normal slight increase trajectory, the overweight to obesity trajectory had significantly lower odds of healthy aging (OR = 0.57, 95%CI: 0.36, 0.93). Interestingly, among the four dimensions of healthy aging, the low-normal stable trajectory was associated with lower odds of no cognitive impairment, and the overweight to obesity trajectory was associated with lower odds of no major chronic diseases. Additionally, higher BMI variability was associated with lower odds of healthy aging independent of baseline BMI.
Conclusions: Maintaining weight to stave off the transition from overweight to obesity is crucial for healthy aging among older Chinese. The findings underscore the critical importance of monitoring dynamic changes in BMI in older Chinese adults.
Introduction
The global population is aging at an accelerating rate, with the proportion of people over the age of 60 will increase from 1 billion (12%) in 2015 to 2.1 billion (22%) in 2050 (1). In China, by the end of 2023, the proportion of the population aged 60 and above has reached 21.1%, and diversified health problems of older adults led to increase economic burden, aging intensifies has become a public health problem (2, 3). The United Nations's 2020 World Report proclaimed 2021–2030 as the “Decade of Healthy Aging” (4). The concept of “healthy aging” (or “successful aging”) is high cognitive and physiological functioning, low risk of disease and disability, and active engagement in life according to Rowe and Kahn's framework model in 1987 (5). The average rate of healthy aging was 35.8% (6), China only has a rate of 15.7%, whereas East Asian countries such as South Korea and Japan have rates of 25.5% and 29.2%, respectively (7). To effectively promote the sound development of an aging society, attention has been directed toward key variables influencing healthy aging including moderate exercise, a nutritious diet, maintenance of a healthy weight, and other lifestyle habits (8).
Body mass index [BMI, calculated as weight (kg) divided by height squared (m2)] is a common indicator of body fat and fitness in adults and is associated with mortality, specific diseases and health conditions, but in older adults, relying on a single-point BMI measurement is not sufficient to capture the long-term effects of body size on health outcomes as BMI can fluctuate over time (9). In recent years, many studies on the BMI trajectories of older adults have shown that chronically overweight or obesity, continue to increase after becoming overweight, are at increased risk of developing health problems such as hypertension, diabetes, cardiovascular disease, cognitive impairment, and frailty compared with those in the normal weight stable group (10–12). However, the association between BMI trajectories in older adults (≥60 years) and overall health assessed using multidimensional structures is unclear.
In this cohort study, we aimed to identify the trajectories of BMI among Chinese older adults and to explore their association with subsequent healthy aging. Since fluctuations in BMI within the normal range are a normal physiological phenomenon, we hypothesized that participants from overweight to obesity would have a lower rate of healthy aging compared to those with the normal stable BMI.
Methods
Study design and participants
We used data from the Chinese Longitudinal Health and Longevity Survey (CLHLS), an on-going national representative prospective cohort study of Chinese individuals aged ≥60 years, covering approximately 85% of the population in China (13, 14). Since 1988, CLHLS has been gathering demographic, lifestyle, and health information every 2–3 years through face-to-face interviews conducted by trained health workers from local Centers for Disease Control and Prevention and community hospitals (14). Details about CLHLS have been described elsewhere (13). CLHLS is considered to be of high quality because of its few missing data, high response rate, low dropout rate (average per wave was 4.85%), and compatibility with other countries' data (15). The CLHLS was approved by the Research Ethics Committee of Peking University (IRB00001052-13074), and the written informed consent of all participants were obtained.
BMI variables were collected from 2008, so a total of 5,245 participants (≥60 years) surveyed in 2008, 2011, and 2014 were eligible for this study. We excluded 1,158 participants with five major chronic diseases at baseline (8, 16, 17), 353 participants with missing weight data in any one of these three surveys, 809 participants without follow-up data after 2014, and 227 participants with missing healthy aging data (2018), leaving 2,698 eligible participants for this study (eFigure 1). To assess the possibility of potential selection bias, we compared the included participants (n = 2,698) with those excluded due to the lack of follow-up or healthy aging data (n = 1,036) and found that the basic characteristics were largely comparable between these included and excluded participants, except that excluded participants were more likely to be from urban areas (eTable 1). This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.
Exposure assessment
Weight and height of all participants were measured three times in 2008, 2011, and 2014. It was measured by trained medical staff using standardized programs. BMI is calculated by dividing the weight (kg) by the square of the height (m). According to the recommended standards of adults in China (18), body type was divided into underweight (<18.5 kg/m2), normal (18.5–23.9 kg/m2), overweight (24.0–27.9 kg/m2), and obesity (≥28.0 kg/m2). Based on the BMI in 2008, 2011, and 2014, we identified BMI trajectories using Latent Class Growth Modeling (LCGM) (19). In the secondary analysis, we used the standard deviation of BMI from three wave surveys to evaluate the variability of BMI.
Assessment of healthy aging
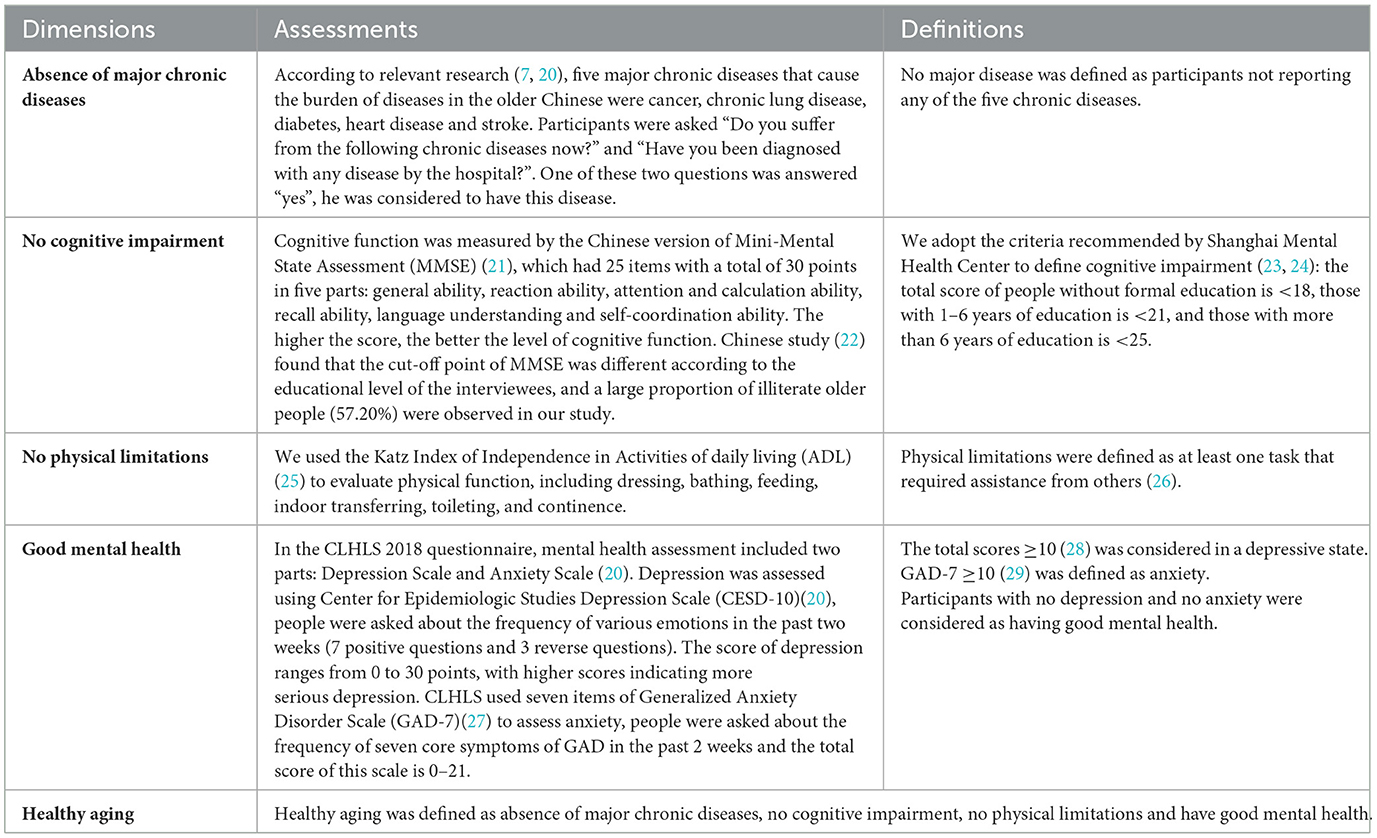
Based on previous research and the framework of Rowe and Kahn's concepts (5, 16), healthy aging was evaluated in 2018 and was defined as having no five major chronic diseases (cancer, chronic lung disease, diabetes, heart disease and stroke), no cognitive impairment (assessed by the Chinese version of Mini-Mental State Assessment (MMSE) and education-stratified cutoffs), no physical limitations [evaluated by the Katz Index of Independence in Activities of daily living (ADL)] and good mental health [no depression (Center for Epidemiologic Studies Depression Scale, CESD-10) or anxiety (Generalized Anxiety Disorder Scale, GAD-7)]. If any one of the criteria was not met, it was defined as usual aging. Detailed descriptions of each of the 4 domains of healthy aging are listed in Table 1 (7, 20–29).
Assessment of potential covariates
The covariate information was collected in 2008 based on previous studies (15). Demographic characteristics included age, gender (male, female), ethnicity (Han Chinese, others) (30), residence district (city, town, rural), education (illiteracy, primary school and below, junior high school and above), marital status (15) (married and living with spouse, others), living expenses (adequate, inadequate), and occupation (farmer, others). Lifestyle information included sleep quality (good, fair, poor), sleep duration (31) (<7, 7–8, >8 h/day), smoking status (never, former, current), drinking status (never, former, current), exercise status (never, former, current) and dietary diversity (Dietary Diversity Score, DDS), and BMI at baseline (underweight, normal, overweight, and obesity). If the participant was unable to answer, then the questions (except those that had to be filled out by the participant) could be answered by an adult family member who was most familiar with the participant's living situation.
When the covariates in 2008 were missing (variables are missing in <5% of the participants), we used the data collected in 2011 or 2014 to impute them. Finally, the proportion of missing values in covariates was 0.07% (missing values for occupation and education were 2 and 2, respectively).
Statistical analyses
We used Latent Class Growth Modeling (LCGM) (19) (R [lcmm package]) to identify subgroups with similar latent BMI trajectories in three waves. Generally, we fitted the longitudinal BMI data into the model with a mixture of multiple latent trajectories by the maximum likelihood method (17). We implemented linear, quadratic and cubic models and used the Bayesian Information Criterion (BIC) and entropy to identify the optimal number and shapes of trajectory groups (eTable 2), and the proportion of participants in each trajectory should meet the condition of at least 5% of the population (32). Then, the posterior probabilities computed via Bayes' theorem were used to test the identification ability, with detailed methods found in the LCGM tutorial (19, 33).
The Chi-square test was used to compare differences in categorical variables and Kruskal–Wallis test in ordinal data and non-normal continuous data. We used logistic regression models to estimate the odds ratios (ORs) and 95% confidence intervals (CIs). Model I was adjusted for baseline age, gender. Model II was additionally adjusted for residence district, ethnic group, educational level, marital status, living expenses and occupation. Model III was additionally adjusted for lifestyle factors, including smoking history, drinking status, exercise, dietary diversity, sleep quality, and sleep duration. Model IV was additionally adjusted for body mass index at baseline. To explore the stability and heterogeneity of the associations between different BMI trajectories with healthy aging in different lifestyle situations, we further performed stratified analyses by sex, age and lifestyle (smoking, drinking, exercise, diet, sleep quality and sleep duration). We used the likelihood ratio test to evaluate the statistical significance of the multiplicative interaction between lifestyles and BMI trajectories.
To compare with previous studies, we conducted a secondary analysis utilizing 2014 BMI data to investigate its correlation with healthy aging and its various dimensions through the application of restricted cubic spline curves and threshold effect analysis. For verifying the robustness of the results, we conducted a series of sensitivity analyses, the specific methods are presented in Supplementary data (Appendix 1).
All statistical analyses were performed using Empower (R) (https://www.empowerstats.net/cn/, X & Y solutions, Inc. Boston MA) and R (https://www.r-project.org/). All P-values were 2-sided and P < 0.05 was considered statistically significant.
Results
The median (IQR) age of the 2,698 older adults was 78.00 (71.00–86.00) years, and 51.82% of them were female. After the four-year follow-up period from 2014 to 2018, 928 (34.40%) had no five major chronic diseases, 1,249 (46.29%) had no physical limitations, 994 (36.84%) had good mental health, and 1,296 (48.04%) had no cognitive dysfunction. A total of 518 participants (19.20%) had reached healthy aging, while the rest were normal aging, and 1,051 of them died during this period.
Trajectories of BMI in older adults from 2008 to 2014
Three different BMI trajectories in older adults from 2008 to 2014 were identified (eTable 2): the average BMI of 1,330 (49.30%) participants maintained around 19 kg/m2 (low-normal stable trajectory), 1,162 (43.07%) participants had a moderate increase in BMI from 21.77 kg/m2 to 23.17 kg/m2 (normal slight increase trajectory), and 206 (7.64%) participants had an increase in BMI from overweight to obesity (overweight to obesity trajectory) (Figure 1). We calculated the posterior probability of each individual being assigned to each trajectory group and assigned it to the trajectory group with the highest posterior probability. The average posterior probabilities for each trajectory groups were >0.70 (0.853, 0.888, and 0.903, respectively), suggesting that each trajectory we fitted had high internal reliability and was sufficiently distinguishable among participants with different BMIs.
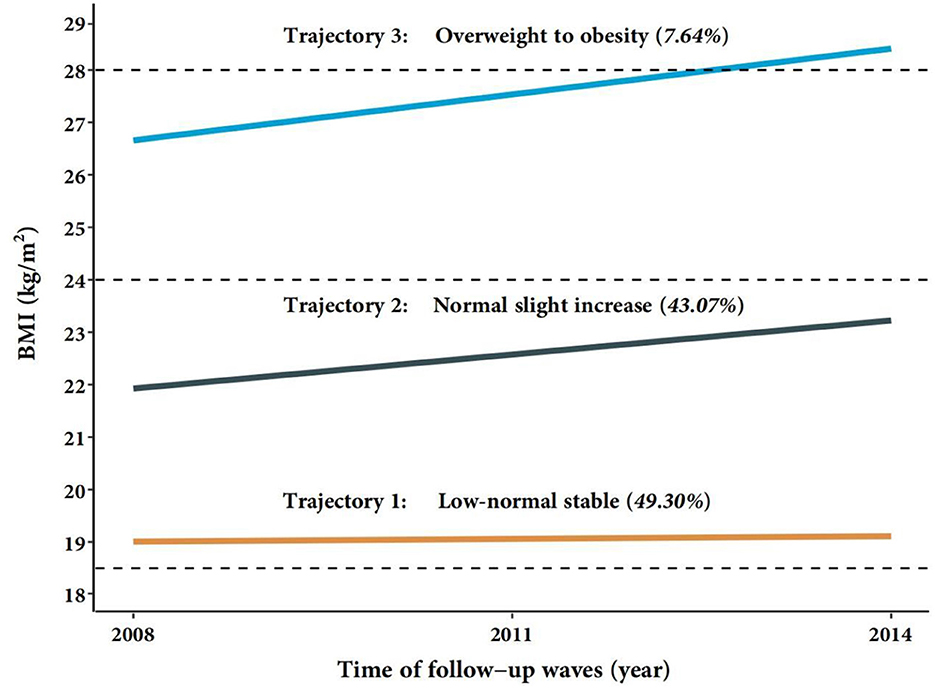
Figure 1. Trajectories of BMI in the Chinese order adults from 2008 to 2014. BMI, body mass index. Low-normal stable (n = 1,330); Normal slight increase (n = 1,162); Overweight to obesity (n = 206); Total (n = 2,698).
Baseline characteristics of participants
Table 2 showed the age-adjusted baseline characteristics of participants with different BMI trajectories. Compared with the normal slight increase trajectory, participants with the overweight to obesity trajectory were slightly younger, tended to be female, non-farmers, had exercise, and had better dietary diversity. Conversely, participants with the low-normal stable trajectory were slightly older, more likely to be female, illiterate, farmer, living alone, non-smokers, non-drinkers, non-exercisers, had worse sleep quality, and had worse dietary diversity. All P < 0.05.
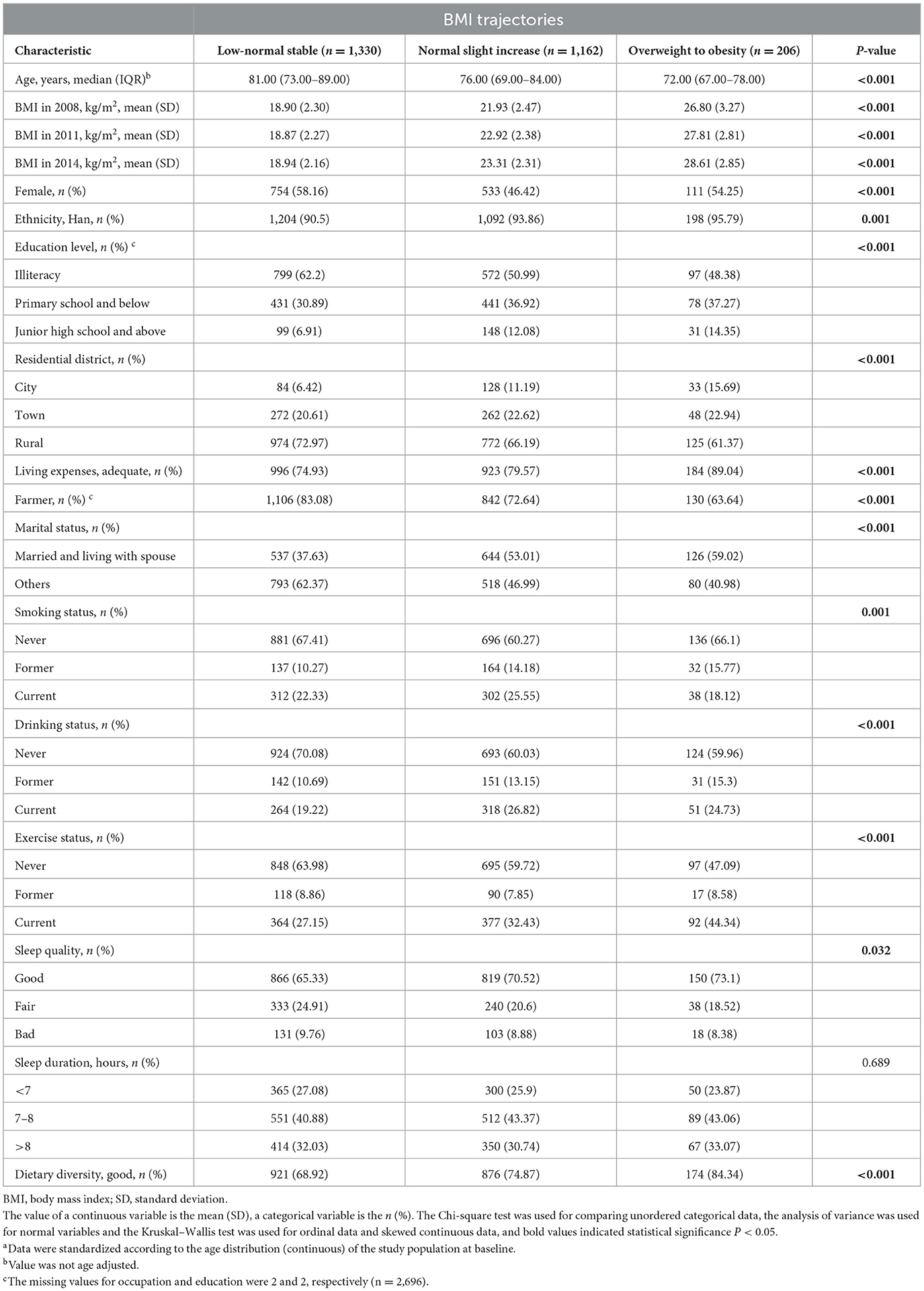
Table 2. Age-adjusted baseline characteristics of participants by BMI trajectories in the CLHLS studya (n = 2,698).
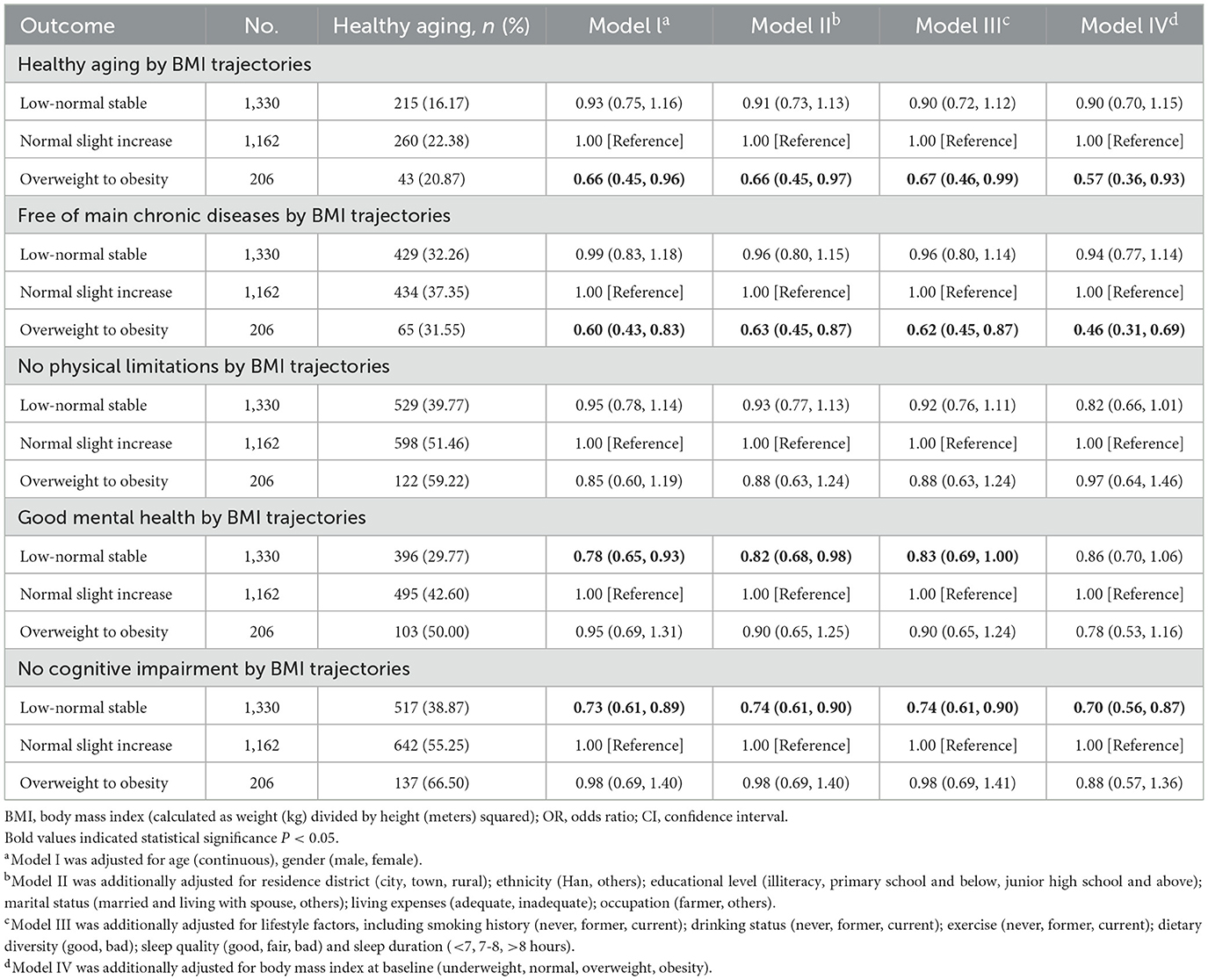
Association between different BMI trajectories and healthy aging in older adults
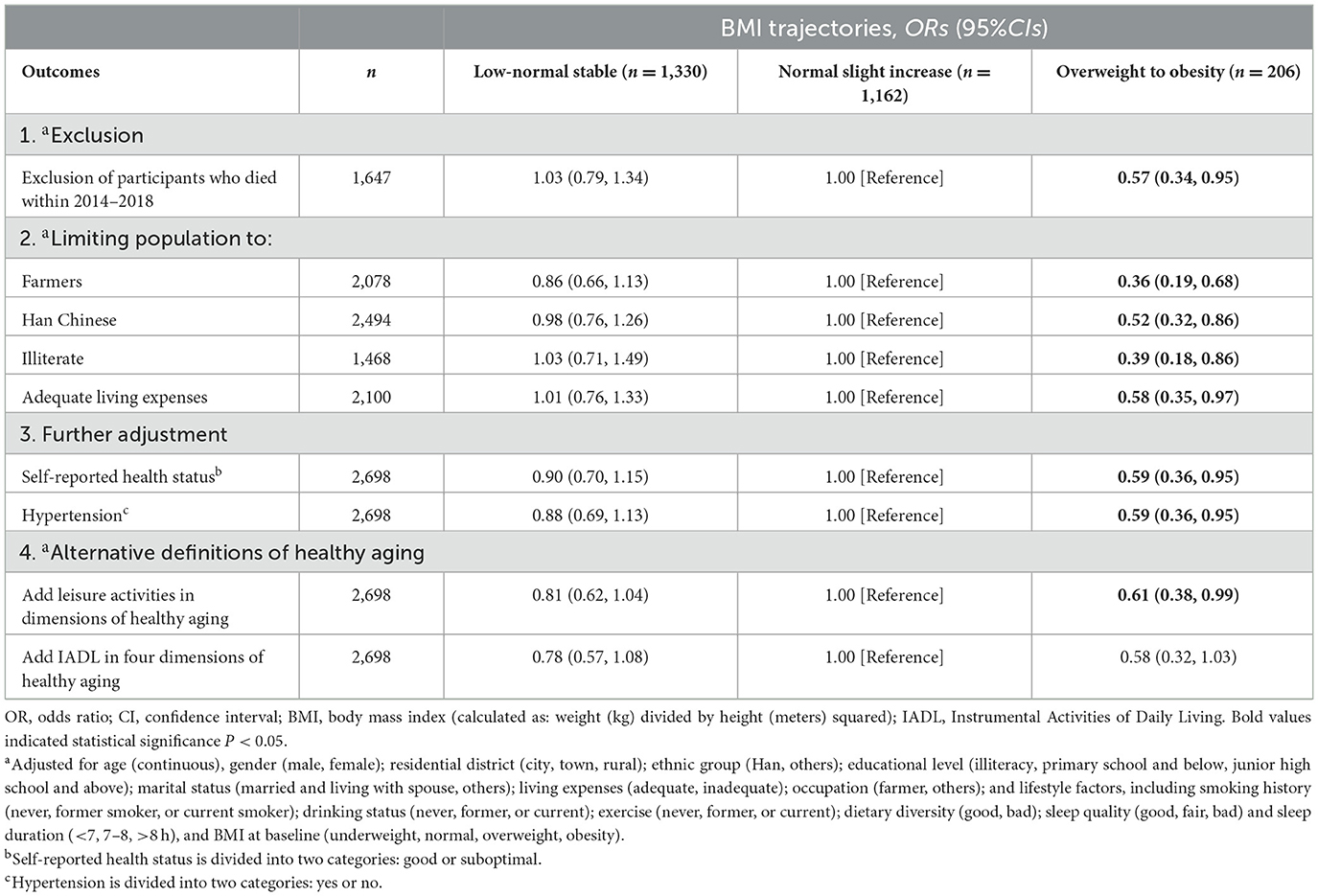
Table 3 summarized the ORs of healthy aging and its four dimensions associated with BMI trajectories. Compared with the normal slight increase trajectory, the overweight to obesity trajectory was significantly associated with lower odds of healthy aging after adjustment for potential confounders. The multivariable-adjusted ORs for Model 4 were 0.90 (95%CI: 0.70, 1.15) for the low-normal stable trajectory and 0.57 (95%CI: 0.36, 0.93) for the overweight to obesity trajectory. The association between BMI trajectories and the four dimensions of healthy aging differed. Compared with the normal slight increase trajectory, older adults in the overweight to obesity trajectory had a multivariable-adjusted OR of 0.46 (95%CI: 0.31, 0.69) for being free of chronic disease. In contrast, those in the low-normal stable trajectory had a multivariable-adjusted OR of 0.70 (95%CI: 0.56, 0.87) for no cognitive impairment.
In the stratified analyses, the associations between BMI trajectories and healthy aging were consistent among subgroups of different gender, age, BMI, lifestyles including smoking, drinking, exercise, diet, sleep quality and sleep duration, all P for interaction >0.05 (Figure 2). Specifically, in almost every subgroup, the overweight to obesity trajectory was consistently associated with lower odds of healthy aging.
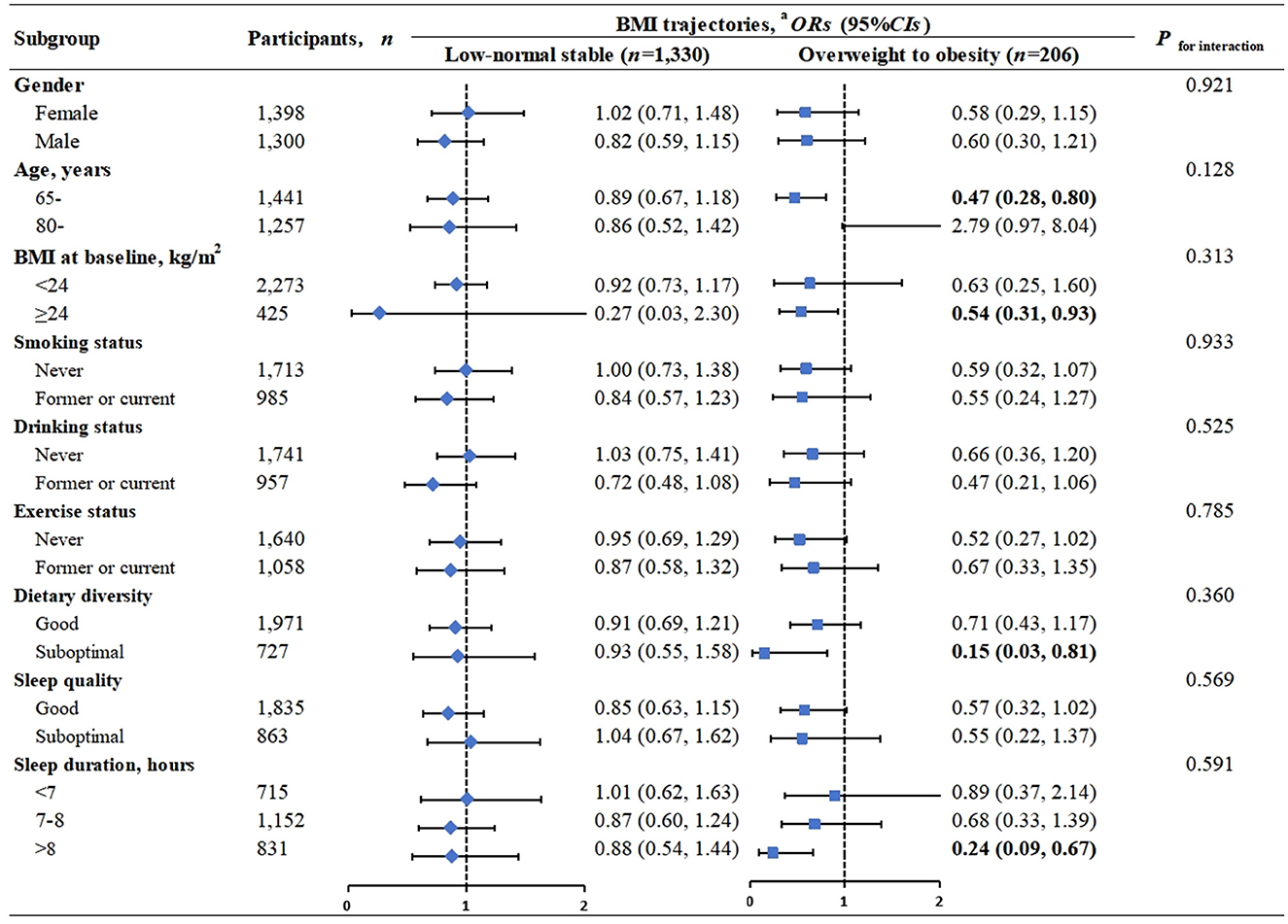
Figure 2. Association of healthy aging with BMI trajectories, stratification analyses. BMI, body mass index (calculated as weight (kg) divided by height (meters) squared); OR, odds ratio; CI, confidence interval. The Normal slight increase trajectory (n = 1,162) is included as the reference group. Bold values indicated statistical significance P < 0.05. aAdjusted for age (continuous), gender (male, female); residential district (city, town, rural); ethnic group (Han, others); educational level (illiteracy, primary school and below, junior high school and above); marital status (married and living with spouse, others); living expenses (adequate, inadequate); occupation(farmer, others); and lifestyle factors, including smoking history (never, former, current); drinking status (never, former, current); exercise(never, former, current); dietary diversity (good, bad); sleep quality (good, fair, bad) and sleep duration (<7, 7–8, >8 h), and BMI at baseline (underweight, normal, overweight, obesity), except for the stratification factor itself.
Based on the results of Appendix 2, Table 4, and eTable 3, we discovered our findings remained robust in several sensitivity analyses.
Joint associations of BMI trajectories and variability of BMI with healthy aging
Appendix 2 and Figure 3 indicated that compared to individuals with a normal slight increase trajectory and the least BMI variability, the odds of healthy aging were lowest among those with an overweight to obesity trajectory and a BMI standard deviation in the fourth quartile (OR = 0.39, 95%CI: 0.18, 0.86). Higher BMI variability is an important marker of healthy aging independent of baseline BMI.
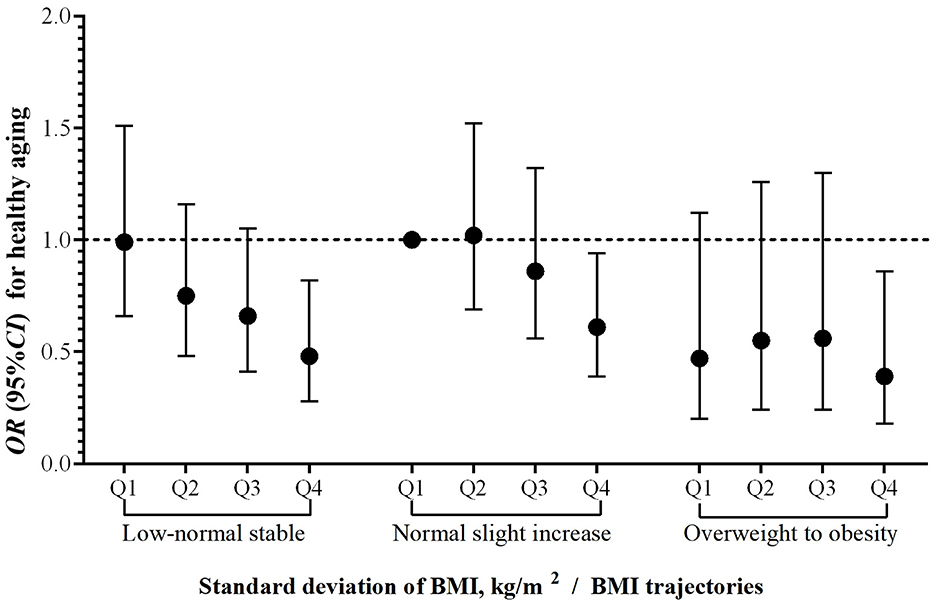
Figure 3. Joint effects of BMl trajectories and variability of BMl on healthy aging. Abbreviations BMI, body mass index (calculated as weight (kg) divided by height (meters) squared); OR, odds ratio; CI, confidence interval. Standard deviation of BMI was divided into four groups using quartiles (Q1–Q4). The horizontal dashed line indicates an OR of 1.00; the vertical error bars represent 95% CIs. Adjusted for age (continuous), gender (male, female); residential district (city, town, rural); ethnic group (Han, others); educational level (illiteracy, primary school and below, junior high school and above); marital status (married and living with spouse, others); living expenses (adequate, inadequate); occupation (farmer, others); and lifestyle factors, including smoking history (never, former smoker, or current smoker); drinking status (never, former, or current); exercise (never, former, or current); dietary diversity (good, bad); sleep quality (good, fair, bad) and sleep duration (<7, 7–8, >8 h), and BMI at baseline (underweight, normal, overweight, obesity).
Association between BMI in 2014 and healthy aging and its four dimensions
In comparison to older adults with a normal weight range (BMI = 18.5–23.9 kg/m2), being underweight (BMI <18.5 kg/m2) poses a risk to mental health and cognitive function, while obesity (BMI ≥ 28 kg/m2) is associated with risk for chronic disease but is considered a protective factor for cognitive function. Restrictive cubic spline plots demonstrated an inverted U-shaped correlation between BMI and all three dimensions of healthy aging except for cognitive function (eTable 5; eFigure 2).
Discussion
Main findings
We identified three BMI trajectories from 2008 to 2014 in this cohort study and found that the BMI trajectory of most Chinese older people was stable at a normal or low-normal level. Compared with participants with a normal slight increase trajectory, those with overweight to obesity trajectory had significantly lower odds of healthy aging, and this association was more pronounced on the chronic disease dimension. We also observed a linear negative association between the variation (standard deviation) in BMI and healthy aging. Moreover, compared to participants with normal slight increase trajectory and the least BMI variability, the subsequent healthy aging rate is significantly reduced for those with the overweight to obesity trajectory and with a large variation in BMI.
Comparison with other studies and explanations
This study used three repeated measurements to model BMI trajectories during older adulthood among Chinese older adults, an approach validated in previous studies (19, 34, 35). Existing studies in older adults (36–38), further confirms that this measurement frequency are sufficient to model BMI trajectories in this population. The trajectory analysis revealed that the BMI trajectories of most Chinese older adults tend to stay within the normal weight range (BMI: 18.5–23.9 kg/m2), which was consistent with the survey results in Taiwan (11). However, the distribution of BMI trajectories in older adults differed by region. An early study of the BMI trajectory in the United States found that 70%-80% of middle-aged and older people were overweight and obesity (39). The first survey conducted in Asia on the BMI trajectory (38) found that BMI for older Japanese was mainly within the normal weight range (BMI: 18.5–25.0 kg/m2), which is also similar to our results. Such differences may be attributed to racial differences, lifestyle and dietary habits. A study involving the analysis of BMI trajectories in older adults showed significant racial differences among Black, White, and Hispanic individuals (39). Therefore, it is recommended to focus on BMI trajectories between different populations and further study the BMI trajectories and their changing mechanisms in Asian and non-Asian older adults.
To the best of our knowledge, this is the first prospective study to investigate the association between BMI trajectories and healthy aging in older adults. Many current studies had focused on BMI and individual health outcomes among adults, and found that having a high BMI was related to chronic diseases (8), psychological problems (40), cognitive impairment (41) and disability (9, 26). A Canadian study (10) showed that individuals in the Overweight-Stable, Obesity I-Stable, and Obesity II -Stable groups experienced more chronic diseases, cognitive impairment, and declines in self-rated overall health than those in the Normal-Stable group. Therefore, our study combines the four aspects of chronic diseases, cognitive health, mental and physical function to evaluate healthy aging, which provides more concrete evidence for the association between BMI trajectories and the overall health of older adults. Previous studies commonly used frailty as the primary outcome, for example, studies conducted in the USA (42), Finland (43), Taiwan (China) (11) have shown that low and very high BMI are associated with a higher risk of frailty development in middle-aged and older people. Although frailty and healthy aging were defined differently, they are both an overall indicator that can measure the health and quality of life of older people. Thus, the findings of our study are similar to these findings, in which we observed that individuals in the overweight to obesity trajectory were significantly associated with reduced rates of healthy aging compared with those in the normal slight increase trajectory.
According to a literature review, some cross-sectional studies have shown a significant association between lower body weight or BMI and successful aging (44, 45). In our study, this result is not significant but a similar trend exists. Similar to our findings, several studies showed that overweight was significantly associated with a shorter healthy life expectancy (20). For example, a higher BMI in midlife was associated with significantly lower odds of healthy aging in French (8), and relevant research in China (46) showed that preventing central obesity and avoiding BMI increases were beneficial to the successful aging of older adults, which is consistent with our research results. Therefore, our study supplements evidence on BMI trajectories and healthy aging in older adults.
The impact mechanisms of BMI on healthy aging are complex. Firstly, the increase in body fat (which comes with a high BMI) is what brings about metabolic consequences due to its inflammatory effects (such as cytokine release, adipocyte death, and macrophage infiltration) in adipose tissue (47), along with high leptin (due to the increase in fat mass itself) (48). This inflammatory process generates insulin resistance, elevated blood glucose, and, in turn, increased sorbitol levels, which reduce anti-inflammatory molecules (like glutathione), producing fewer vasodilators (49). This exposure leads to greater susceptibility to atherosclerotic processes (17). Secondly, an increase in pro-inflammatory adipocytokines secreted by adipose tissue may lead to low-grade systemic inflammation, inducing various chronic diseases (8, 11). Higher body weight, especially obesity may cause multiple comorbidities and pose greater risks to human health. In addition, in present society, being overweight may lead to a person's low self-esteem and subsequent depressive symptoms, which in turn can have a negative impact on healthy aging (44). These mechanisms suggest that the overweight to obesity trajectory in older adults is an important marker of unhealthy aging and should be alerted.
Strengths and limitations
This study has several advantages and limitations. Our results are based on a large national cohort of older adults in a developing country with high response rates and high follow-up compliance; a prospective cohort design was used in this study; the results of the overall health status of the older adult population were assessed using a comprehensive assessment of healthy aging; the LCGM was used to identify the change trajectory of BMI over time; and detailed consideration of various potential confounders.
In interpreting our findings, we should be aware of these limitations. First, there may be measurement errors in measures such as height and weight, and measures of health outcomes are largely self-reported, with potential recall bias issues as with other studies using self-rated results (10, 17), but repeated measurements have attempted to address this limitation. Second, the duration of follow-up was too short, so reverse causation may still be unavoidable. In addition, due to limitations in data availability, this study was unable to obtain additional follow-up measurements of BMI, potentially leading to the oversight of more intriguing trends in BMI changes. Finally, this is an observational study, therefore, we cannot rule out unmeasurable residual confounding factors. Moreover, our participants are focused on the Chinese older adults, which may affect the generalizability of our findings to other ethnic populations. While our study minimizes the confounding of sociocultural-economic status, changes of BMI can vary by age, race, and other settings. Therefore, further studies in different populations are needed to confirm our findings.
Conclusion
Our cohort study found that most Chinese older adults aged 60 and above had stable normal or low BMI. Compared to individuals with the normal slight increase trajectory, individuals with the overweight to obesity trajectory had a significantly lower odds of healthy aging, and a stronger association existed for the chronic disease dimension. Interestingly, we found that individuals in the low-normal stable trajectory were associated with lower odds of cognitive impairment. Therefore, this study suggests that maintaining a stable normal weight and avoiding excessive weight variation are key factors for healthy aging. These findings add new evidence to previous research on healthy aging and provide further scientific support for weight management suggestions, that is, maintaining a stable and normal weight can obtain long-term health benefits.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
This study was based on publicly available data (CLHLS). Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients'/participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements. For the CLHLS data: the studies involving humans were approved by the research ethics committee of Peking University (IRB00001052-13074); the studies were conducted in accordance with the local legislation and institutional requirements; the participants provided their written informed consent to participate in this study; and informed consent was obtained from literate participants and legal guardian(s)/next of kin of illiterate participants; written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data.
Author contributions
XK: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. PD: Conceptualization, Validation, Writing – review & editing. LT: Supervision, Writing – review & editing. HS: Conceptualization, Software, Validation, Writing – review & editing. SW: Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by grants from the National Social Science Foundation of China (Grant Number: 21BRK021) and the Major Humanities and Social Sciences Research Projects in Zhejiang higher education institutions (Grant Number: 2024QN063). The funding source had no role in the design and conduct of the study, the collection, management, analysis, and interpretation of the data, the preparation, review, and approval of the manuscript, or the decision to submit the manuscript for publication.
Acknowledgments
Thanks to the participants and researchers from the Chinese Longitudinal Healthy Longevity Survey and the participants of Wenzhou Medical University for their valuable contributions.
Conflict of interest
The authors declare that the study did not involve any commercial or financial relationships that can be interpreted as potential conflicts of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1538261/full#supplementary-material
References
1. World Health Organization. Ageing and Health. (2018) Geneva: World Health Organization. Available online at: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health
2. Ministry of Civil Aviation. 2023 Statistical Bulletin of Civil Affairs Development. (2024) Beijing: Ministry of Civil Aviation
3. The Lancet Healthy Longevity. The lancet healthy longevity: health for all, for longer. Lancet Healthy Longev. (2020) 1:e1. doi: 10.1016/S2666-7568(20)30022-2
4. World Health Organization. Decade of Healthy Ageing 2020-2030. (2020) Geneva: World Health Organization. Available online at: https://www.who.int/docs/default-source/decade-of-healthy-ageing/final-decade-proposal/decade-proposal-final-apr2020-en.pdfvrsn=b4b75ebc_5
5. Rowe JW, Kahn RL. Human aging: usual and successful. Science. (1987) 237:143–9. doi: 10.1126/science.3299702
6. Depp CA, Jeste DV. Definitions and predictors of successful aging: a comprehensive review of larger quantitative studies. Am J Geriat Psychiat. (2006) 14:6–20. doi: 10.1097/01.JGP.0000192501.03069.bc
7. Nakagawa T, Cho J, Yeung DY, Ailshire J. Successful aging in East Asia: comparison among China, Korea, and Japan. J Gerontol B Psychol Sci Soc Sci. (2021) 76:S17–S26. doi: 10.1093/geronb/gbaa042
8. Ruhunuhewa I, Adjibade M, Andreeva VA, Galan P, Hercberg S, Assmann KE, et al. Prospective association between body mass index at midlife and healthy aging among French adults. Obesity. (2017) 25:1254–62. doi: 10.1002/oby.21853
9. Gray LA, Breeze PR, Williams EA, BMI. trajectories, morbidity, and mortality in England: a two-step approach to estimating consequences of changes in BMI. Obesity. (2022) 30:1898–907. doi: 10.1002/oby.23510
10. Wang M, Yi Y, Roebothan B, Colbourne J, Maddalena V, Wang PP, et al. Body Mass Index Trajectories among Middle-Aged and Elderly Canadians and Associated Health Outcomes. J Environ Public Health. (2016) 2016:7014857. doi: 10.1155/2016/7014857
11. Ho HE, Yeh CJ, Chu WM, Lee MC. Midlife body mass index trajectory and risk of frailty 8 years later in Taiwan. J Nutr Health Aging. (2019) 23:849–55. doi: 10.1007/s12603-019-1226-6
12. Singh-Manoux A, Dugravot A, Shipley M, Brunner EJ, Elbaz A, Sabia S, et al. Obesity trajectories and risk of dementia: 28 years of follow-up in the Whitehall II study. Alzheimers Dement. (2018) 14:178–86. doi: 10.1016/j.jalz.2017.06.2637
13. Zeng Y. Towards deeper research and better policy for healthy aging—using the unique data of chinese longitudinal healthy longevity survey. China Economic J. (2012) 5:131–49. doi: 10.1080/17538963.2013.764677
14. Zeng Y, Feng Q, Gu D, Vaupel JW. Demographics, phenotypic health characteristics and genetic analysis of centenarians in China. Mech Ageing Dev. (2017) 165:86–97. doi: 10.1016/j.mad.2016.12.010
15. Zhang Y, Xiong Y, Yu Q, Shen S, Chen L, Lei X. The activity of daily living (ADL) subgroups and health impairment among Chinese elderly: a latent profile analysis. BMC Geriatr. (2021) 21:30. doi: 10.1186/s12877-020-01986-x
16. Shi H, Huang T, Schernhammer ES, Sun Q, Wang M. Rotating night shift work and healthy aging after 24 years of follow-up in the nurses' health study. JAMA Netw Open. (2022) 5:e2210450. doi: 10.1001/jamanetworkopen.2022.10450
17. Song M, Hu FB, Wu K, Must A, Chan AT, Willett WC, et al. Trajectory of body shape in early and middle life and all cause and cause specific mortality: results from two prospective US cohort studies. BMJ. (2016) 353:i2195. doi: 10.1136/bmj.i2195
18. Choo V, WHO reassesses appropriate body-mass index for Asian populations. Lancet. (2002) 360:235. doi: 10.1016/S0140-6736(02)09512-0
19. Andruff H, Carraro N, Thompson A, Gaudreau P, Louvet B. Latent class growth modelling: a tutorial. TQMP. (2009) 5:11–24. doi: 10.20982/tqmp.05.1.p011
20. Luo H, Ren X, Li J, Wu K, Wang Y, Chen Q, et al. Association between obesity status and successful aging among older people in China: evidence from CHARLS. BMC Public Health. (2020) 20:767. doi: 10.1186/s12889-020-08899-9
21. Katzman R, Zhang MY, Ouang Ya Q, Wang ZY, Liu WT, Yu E, et al. A Chinese version of the Mini-Mental State Examination; impact of illiteracy in a Shanghai dementia survey. J Clin Epidemiol. (1988) 41:971–8. doi: 10.1016/0895-4356(88)90034-0
22. Zhang MY, Katzman R, Salmon D, Jin H, Cai GJ, Wang ZY, et al. The prevalence of dementia and Alzheimer's disease in Shanghai, China: impact of age, gender, and education. Ann Neurol. (1990) 27:428–37. doi: 10.1002/ana.410270412
23. Lin Y, Zhang Q, Wang T, Zeng Z. Effect of living arrangements on cognitive function in Chinese elders: a longitudinal observational study. BMJ Open. (2022) 12:e050410. doi: 10.1136/bmjopen-2021-050410
24. Cui GH, Yao YH, Xu RF, Tang HD, Jiang GX, Wang Y, et al. Cognitive impairment using education-based cutoff points for CMMSE scores in elderly Chinese people of agricultural and rural Shanghai China. Acta Neurol Scand. (2011) 124:361–7. doi: 10.1111/j.1600-0404.2010.01484.x
25. Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of Adl: a standardized measure of biological and psychosocial function. JAMA. (1963) 185:914–9. doi: 10.1001/jama.1963.03060120024016
26. Lv YB, Yuan JQ, Mao C, Gao X, Yin ZX, Kraus VB, et al. Association of body mass index with disability in activities of daily living among Chinese adults 80 years of age or older. JAMA Netw Open. (2018) 1:e181915. doi: 10.1001/jamanetworkopen.2018.1915
27. Liu Y, Xu Y, Yang X, Miao G, Wu Y, Yang S. The prevalence of anxiety and its key influencing factors among the elderly in China. Front Psychiatry. (2023) 14:1038049. doi: 10.3389/fpsyt.2023.1038049
28. Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. (1994) 10:77–84. doi: 10.1016/S0749-3797(18)30622-6
29. Toussaint A, Husing P, Gumz A, Wingenfeld K, Harter M, Schramm E, et al. Sensitivity to change and minimal clinically important difference of the 7-item Generalized Anxiety Disorder Questionnaire (GAD-7). J Affect Disord. (2020) 265:395–401. doi: 10.1016/j.jad.2020.01.032
30. Zeng Y, Feng Q, Hesketh T, Christensen K, Vaupel JW. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: a cohort study. Lancet. (2017) 389:1619–29. doi: 10.1016/S0140-6736(17)30548-2
31. Zhang M, Lv X, Chen Y, Tu L, Fan Z, Yao Y, et al. Excessive sleep increased the risk of incidence of cognitive impairment among older Chinese adults: a cohort study based on the Chinese Longitudinal Healthy Longevity Survey (CLHLS). Int Psychogeriatr. (2022) 34:725–34. doi: 10.1017/S1041610221000168
32. Gilmour H, Stranges S, Kaplan M, Feeny D, McFarland B, Huguet N, et al. Longitudinal trajectories of sleep duration in the general population. Health Rep. (2013) 24:14–20. doi: 10.1016/j.healthplace.2013.09.001
33. Jones B, Nagin DS. Advances in group-based trajectory modeling and an sas procedure for estimating them. Sociol Method Res. (2007) 35:542–71. doi: 10.1177/0049124106292364
34. Jones Bl Nagin Ds, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res. (2001) 29:374–93. doi: 10.1177/0049124101029003005
35. Kan Y, Liu L, Li X, Pang J, Bi Y, Zhang L, et al. Association between distinct body mass index trajectories according to the group-based trajectory modeling and the risk of incident diabetes: a systematic review. Obes Rev. (2022) 23:e13508. doi: 10.1111/obr.13508
36. Zheng H, Tumin D, Qian Z. Obesity and mortality risk: new findings from body mass index trajectories. Am J Epidemiol. (2013) 178:1591–9. doi: 10.1093/aje/kwt179
37. Zheng R, Du M, Zhang B, Xin J, Chu H, Ni M, et al. Body mass index (BMI) trajectories and risk of colorectal cancer in the PLCO cohort. Br J Cancer. (2018) 119:130–2. doi: 10.1038/s41416-018-0121-y
38. Murayama H, Liang J, Bennett JM, Shaw BA, Botoseneanu A, Kobayashi E, et al. Trajectories of body mass index and their associations with mortality among older japanese: do they differ from those of western populations? Am J Epidemiol. (2015) 182:597–605. doi: 10.1093/aje/kwv107
39. Botoseneanu A, Liang J. Latent heterogeneity in long-term trajectories of body mass index in older adults. J Aging Health. (2013) 25:342–63. doi: 10.1177/0898264312468593
40. Mezuk B, Chen Y, Yu C, Guo Y, Bian Z, Collins R, et al. Depression, anxiety, and prevalent diabetes in the Chinese population: findings from the China Kadoorie Biobank of 05 million people. J Psychosom Res. (2013) 75:511–7. doi: 10.1016/j.jpsychores.2013.09.008
41. Ren Z, Li Y, Li X, Shi H, Zhao H, He M, et al. Associations of body mass index, waist circumference and waist-to-height ratio with cognitive impairment among Chinese older adults: based on the CLHLS. J Affect Disord. (2021) 295:463–70. doi: 10.1016/j.jad.2021.08.093
42. Mezuk B, Lohman MC, Rock AK, Payne ME. Trajectories of body mass indices and development of frailty: Evidence from the health and retirement study. Obesity. (2016) 24:1643–7. doi: 10.1002/oby.21572
43. Stenholm S, Strandberg TE, Pitkala K, Sainio P, Heliovaara M, Koskinen S. Midlife obesity and risk of frailty in old age during a 22-year follow-up in men and women: the Mini-Finland Follow-up Survey. J Gerontol A Biol Sci Med Sci. (2014) 69:73–8. doi: 10.1093/gerona/glt052
44. Dahany MM, Drame M, Mahmoudi R, Novella JL, Ciocan D, Kanagaratnam L, et al. Factors associated with successful aging in persons aged 65 to 75 years. Eur Geriatr Med. (2014) 5:365–70. doi: 10.1016/j.eurger.2014.09.005
45. Schietzel S, Chocano-Bedoya PO, Sadlon A, Gagesch M, Willett WC, Orav EJ, et al. Prevalence of healthy aging among community dwelling adults age 70 and older from five European countries. BMC Geriatr. (2022) 22:174. doi: 10.1186/s12877-022-02755-8
46. Lv YB, Liu S, Yin ZX, Gao X, Kraus VB, Mao C, et al. Associations of body mass index and waist circumference with 3-year all-cause mortality among the oldest old: evidence from a Chinese community-based prospective cohort study. J Am Med Dir Assoc. (2018) 19:672–8 e674. doi: 10.1016/j.jamda.2018.03.015
47. Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science. (1993) 259:87–91. doi: 10.1126/science.7678183
48. Sánchez-Ortega H, Jiménez-Cortegana C, Novalbos-Ruiz JP, Gómez-Bastero A, Soto-Campos JG, Sánchez-Margalet V. Role of leptin as a link between asthma and obesity: a systematic review and meta-analysis. Int J Mol Sci. (2022) 24:546. doi: 10.3390/ijms24010546
Keywords: trajectory, body mass index, healthy aging, LCGM, variability
Citation: Kuang X, Ding P, Tian L, Shi H and Wang S (2025) Association of BMI trajectories and healthy aging among Chinese older adults: a national cohort study. Front. Public Health 13:1538261. doi: 10.3389/fpubh.2025.1538261
Received: 02 December 2024; Accepted: 08 May 2025;
Published: 09 June 2025.
Edited by:
Edwin van Teijlingen, Bournemouth University, United KingdomReviewed by:
Lídia Vaqué-Alcázar, University of Barcelona, SpainPedro Paulo Scariot, Sao Francisco University, Brazil
Copyright © 2025 Kuang, Ding, Tian, Shi and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shize Wang, d3N6OTM5OEAxMjYuY29t; Hongying Shi, c2h5aW5nOTE4QDE2My5jb20=
 Xiaodan Kuang
Xiaodan Kuang Pan Ding
Pan Ding Liuhong Tian
Liuhong Tian Hongying Shi
Hongying Shi Shize Wang3*
Shize Wang3*