- 1Moderna, Melbourne, VIC, Australia
- 2Moderna, Singapore, Singapore
- 3Moderna, Hong Kong, Hong Kong SAR, China
- 4Moderna, Seoul, Republic of Korea
- 5Moderna, Tokyo, Japan
- 6Moderna, Taipei, Taiwan
This comprehensive synthesis of severe COVID-19 risk factors specific to the Asia-Pacific (APAC) region addresses gaps in previous global studies, which often overlook regional demographic, epidemiological, and healthcare system variations. Three databases (PubMed, Ovid MedLine, Scopus) and two preprint platforms (BioRxiv, MedRxiv) were searched between December 1, 2019, and March 31, 2023. English-language publications from 11 APAC countries/regions (Australia, Hong Kong, Japan, Macau, New Zealand, Philippines, Singapore, South Korea, Taiwan, Thailand and Vietnam) reporting conditions associated with severe COVID-19 outcomes in adults (aged ≥16 years) were included. Of 295 publications screened, 123 met inclusion criteria, mostly from South Korea (n = 68) and Japan (n = 23). Common risk factors included older age, male sex, obesity, diabetes, heart failure, renal disease, and dementia. Less commonly hypertension, chronic obstructive pulmonary disease, cardio-and cerebrovascular disease, immunocompromise, autoimmune disorders, and mental illness were reported. To date, no prior region-specific synthesis of risk factors for severe COVID-19 outcomes across the APAC region has been identified. The findings support the development of tailored vaccination strategies and public health interventions at both national and regional levels, helping ensure high-risk populations are prioritized in ongoing COVID-19 prevention and management efforts.
Summary
• This review highlights risk factors for severe COVID-19 outcomes in APAC populations including age, immunocompromise, obesity, diabetes, heart failure, renal disease, dementia and mental illness.
• Understanding APAC-specific risk factors can support vaccination strategies and improve the targeting of high-risk groups.
Introduction
SARS-CoV-2, the virus responsible for COVID-19, causes a spectrum of disease ranging from mild to severe, with a proportion of patients developing critical illness, particularly early in the pandemic (1, 2). Extensive research has been undertaken globally to identify demographics, lifestyle factors, and medical conditions that may increase the risk of severe COVID-19 outcomes (i.e., hospitalization, intensive care unit [ICU] admission, and death) (2, 3). The presence of preexisting medical conditions including hypertension, diabetes, cardiovascular disease (CVD), dementia, chronic respiratory disease, chronic kidney disease (CKD), cancer, and chronic liver disease are associated with an increased risk of COVID-19-related severe outcomes and mortality (4–6). Although numerous studies have investigated risk factors for severe COVID-19 outcomes globally, few have focused specifically on the Asia-Pacific (APAC) region. These studies often overlook ethnic and geographic differences, as well as social and healthcare variations, unique to the APAC region (7). For instance, elevated smoking rates among low-and-middle-income men in APAC countries contribute to region-specific incidence rates of CVD, stroke, and cancers (8, 9). Similarly, multimorbidity, defined as the presence of ≥2 conditions (10), is increasingly prevalent in Asia. A unique ‘lean diabetic’ phenotype (characterized by diabetes and low body mass index [BMI]), and evidence that Asian patients can experience heart failure (HF) up to a decade earlier than European and Northern American patients, may influence COVID-19 disease burden in the region (11).
Globally, COVID-19 vaccination has substantially improved clinical outcomes, as demonstrated by reductions in COVID-19–related hospitalizations, ICU admissions, and mortality (6, 12, 13). However, to optimize vaccination strategies in the APAC region, it is essential to understand the key medical risk factors that contribute to severe COVID-19 disease. Despite extensive global research, a critical gap remains in identifying and quantifying risk factors specific to APAC populations, where variations in demographics, disease burden and healthcare systems may influence outcomes. This review addresses this gap and contributes the following:
• Presents, to the best of current knowledge, the first synthesis of medical risk factors for severe COVID-19 outcomes focused specifically on the APAC region
• Synthesizes evidence in the context of region-specific health characteristics, such as earlier onset of chronic diseases and unique phenotypes like lean diabetes
• Highlights medical conditions that may be under-recognized in regional vaccination guidelines
• Identifies substantial heterogeneity across APAC studies in the definitions of risk conditions and outcomes, as well as methodological variability, underscoring the need for standardized approaches
• Informs more tailored, risk-based public health and vaccination strategies suited to the APAC context
Methods
Search strategy and eligibility criteria
A literature search was conducted across three electronic databases (PubMed, Ovid MedLine, and Scopus) and two preprint platforms (BioRxiv and MedRxiv) between December 1, 2019, and March 31, 2023. English-language publications from 11 APAC countries/regions (Australia, Hong Kong, Japan, Macau, New Zealand, Philippines, Singapore, South Korea, Taiwan, Thailand, and Vietnam) were included if they reported adjusted hazard ratios (aHRs) or odds ratios (aORs) for age, sex, and underlying medical conditions associated with severe COVID-19 outcomes. Studies were limited to research articles (cohort, cross-sectional, and case-controlled studies) of adults aged ≥16 years. Publications were also excluded if they contained pooled data where country- or region-level data could not be isolated and individually evaluated. Two independent reviewers (MT and CC) evaluated each study based on selection criteria, comparability, and outcome assessment. Discrepancies were resolved through discussion with a third reviewer (AKB).
Data extraction and synthesis
Data were extracted from eligible studies on study design, setting, population characteristics, risk factors examined, comparator groups, and reported outcomes. Both positively and negatively associated findings were included, and results were grouped by risk factor and outcome (e.g., hospitalization, ICU admission, or mortality). A narrative synthesis was performed to summarize patterns across studies. Additional methodological detail is available in the Supplementary methods.
Quality assessment of individual studies
Although not designed as a systematic review or meta-analysis, this review employed a robust and comprehensive approach to identify, screen, and extract data from the literature (Supplementary Table 17). Priority was given to larger cohort studies (n > 1,000) for common conditions. For less prevalent conditions (e.g., neurological or autoimmune diseases), studies with at least 50 participants were included if quantitative risk estimates were reported.
To mitigate potential publication bias, a known limitation of narrative reviews, the search strategy also included two preprint server databases. In addition, backward citation searches were conducted to enhance comprehensiveness.
Results
Literature search
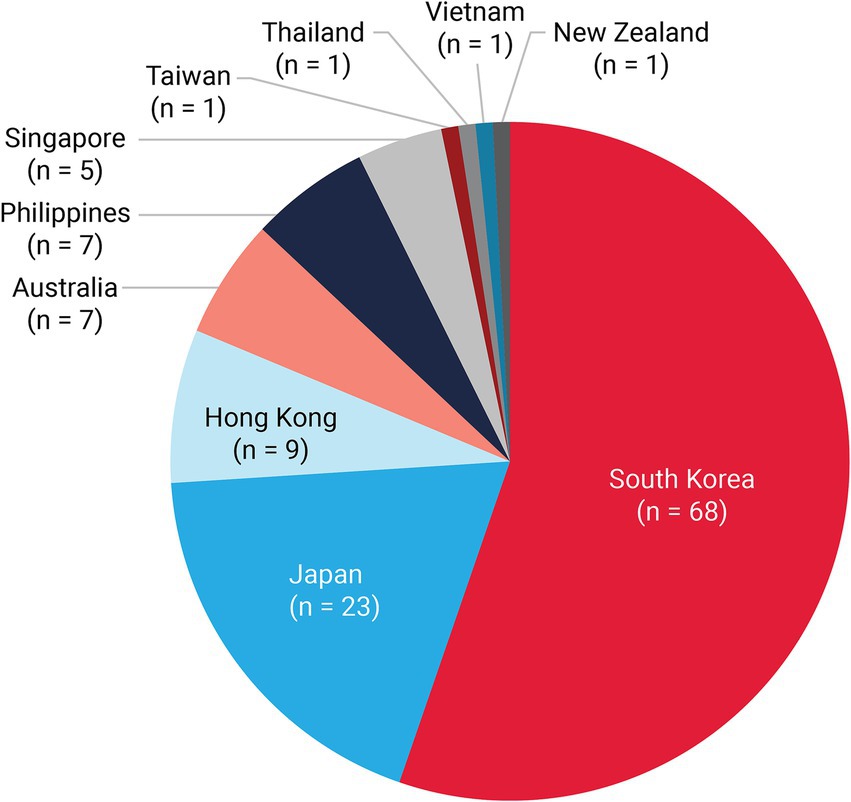
The literature search identified 409 studies; 295 full-text articles were screened, and 123 met the inclusion criteria for data extraction (Figure 1). Most publications originated from South Korea (n = 68) and Japan (n = 23; Figure 2) and were conducted during early pandemic phases, with 83 studies published in 2020 and 2021. Only 23 studies examined outcomes during periods when the Delta and Omicron SARS-CoV-2 variants were predominant (from mid-2021).
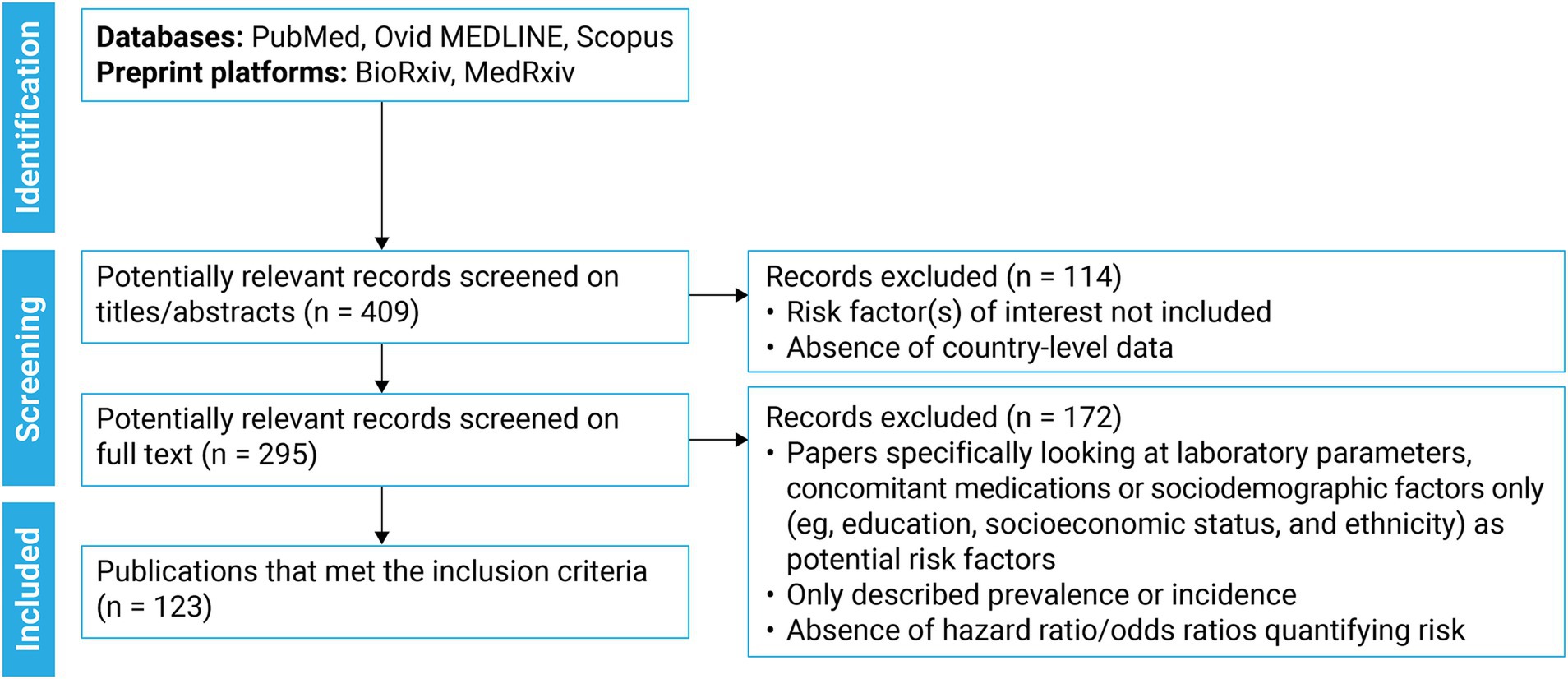
Figure 2. Country/region of origin for included studiesa (N = 123). N, number of studies. aMacau had 0 studies included.
Key risk factors for severe COVID-19 outcomes and mortality
The number of risk factors included per individual study varied widely (range: 1–24 factors), as did the total study sample sizes (range: 84–937,758 individuals). Studies varied in the definitions and number of severe outcomes tested for statistical association. The risk factors most commonly associated with severe COVID-19 outcomes included older age, male sex, obesity (BMI ≥25 or ≥30 kg/m2), diabetes, HF, renal disease (including CKD), and dementia (Table 1). Other associated conditions included hypertension, chronic obstructive pulmonary disease (COPD), CVD, cerebrovascular disease, immunocompromise, autoimmune diseases, and mental illness (Table 1).
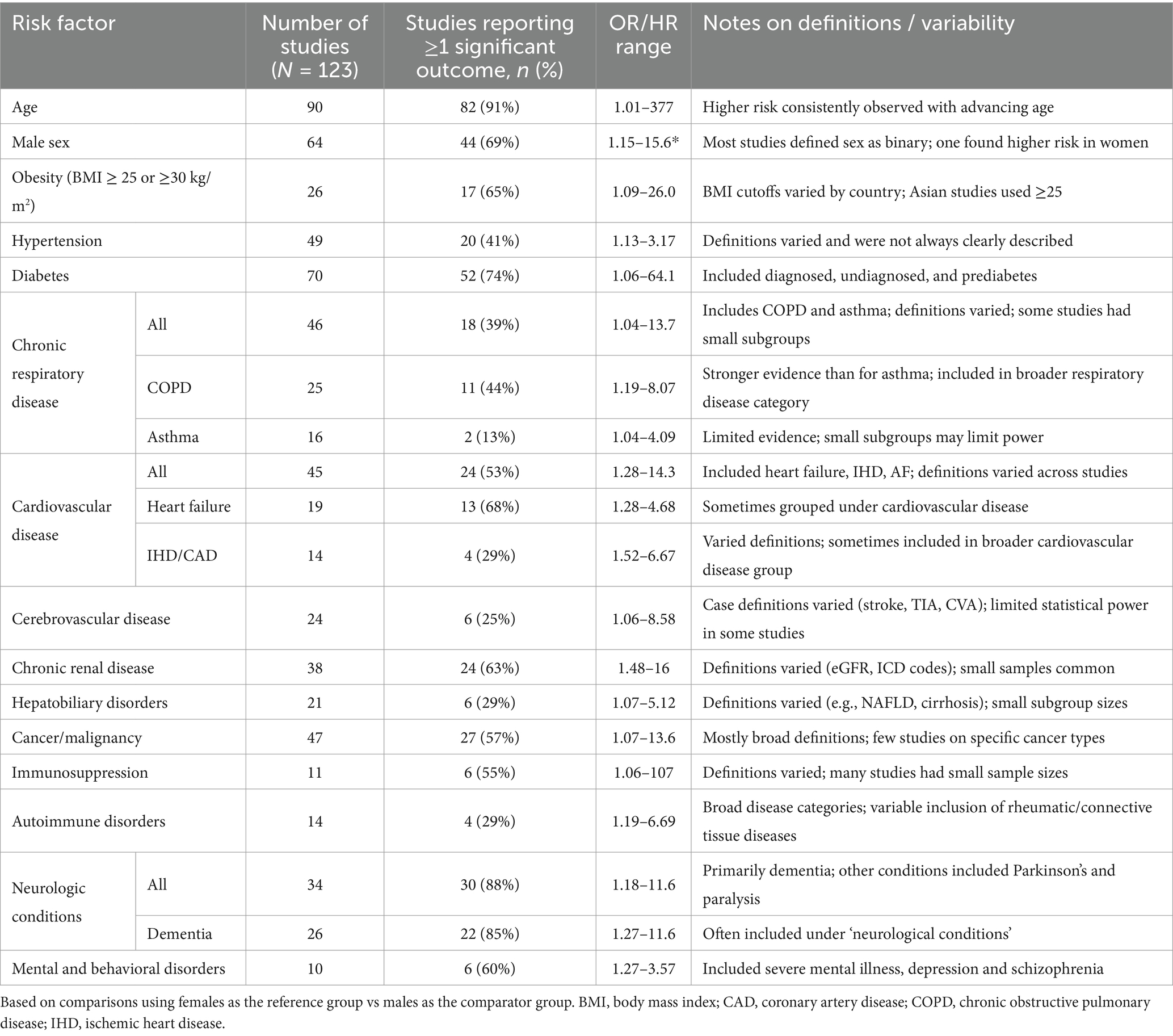
Table 1. Risk factors for severe COVID-19 and corresponding number, frequency and observed OR/HR ranges for included studies.
Age
Ninety studies assessed age as a potential risk factor for severe outcomes from COVID-19 infection. Of these, 82 studies (91%) reported a significant association between older age and increased risk of at least one severe COVID-19 outcome (Table 1; Supplementary Table 1). Studies that assessed risk across different age strata consistently reported an incremental increase in risk with advancing age, most notably in adults aged ≥50 years. A nationwide study of 937,758 adults in Japan found that compared with younger adults (aged 20–49 years), the aOR for COVID-19 mortality was 8.8 for those aged 50–64 years (14).
Sex
Sixty-four studies compared the risk of severe outcomes from COVID-19 infection between women and men (Table 1). Overall, 44 (69%) found a significantly increased risk for men (Supplementary Table 2); 1 study found an increased risk for women in a South Korean study of 5,571 patients hospitalized with COVID-19 (15), and the remainder did not find any significant differences between sex. Overall, these studies were conducted in a variety of populations (e.g., hospitalized adults) and the potential for underlying sex biases because of sex-associated risk factors for certain medical conditions and differences in health service utilization needs to be considered when interpreting these findings.
Obesity (BMI ≥25 or ≥30 kg/m2)
Twenty-six studies assessed obesity on the risk of severe COVID-19 outcomes (Table 1). Clinical definitions of obesity varied between studies, with a BMI of ≥25 kg/m2 often used for Asian populations compared with the typical threshold of ≥30 kg/m2 in non-Asian populations. This variation reflects ethnic differences in body composition and metabolic profiles, highlighting the importance of population-appropriate clinical thresholds when interpreting and comparing COVID-19 risk. Almost two-thirds of the studies (17/26; 65%) showed an increased risk of at least 1 reported outcome in individuals with obesity and/or BMI ≥25 or ≥30 kg/m2. No studies showed a decrease in associated risk of severe outcomes among those with obesity. Across studies with large sample sizes (n > 1,000) of individuals classified as overweight or obese, the reported OR (95% CI) for severe COVID-19 outcomes ranged from 1.19 (1.02–1.38) to 6.85 (3.18–14.78; Supplementary Table 3). Several studies evaluated risk levels across different BMI categories. Although some studies indicated a higher risk of severe outcomes among individuals with a BMI ≥30 kg/m2 vs. those with a BMI ranging from 25 to 29 kg/m2, this observation was not uniform across all studies.
Hypertension
Forty-nine studies explored hypertension as a potential risk factor (Table 1). The clinical definition of hypertension varied and was not always clearly described. Twenty studies (41%) found a substantially increased risk of severe COVID-19 outcomes among patients with hypertension, including 10 studies with large cohorts (n > 1,000). Among these studies, the aORs and aHRs ranged from aHR 1.13 (1.01–1.26) to aOR 3.17 (1.05–10.40; Supplementary Table 4).
Diabetes
The impact of diabetes on the risk of severe COVID-19 outcomes was assessed in 70 studies (Table 1). Fifty-two studies (74%) found diabetes was associated with an increased risk of severe outcomes for at least 1 of the outcomes assessed. Of the remainder, 18 studies found no significant association between people with and without diabetes; a single study found a lower risk of COVID-19 hospitalization, albeit in a very small group with diabetes (n < 100) in a cross-sectional internet study (16). Among 12 large (n > 1,000) studies, the aOR (95% CI) for severe COVID-19 outcomes across the different outcomes reported ranged from 1.06 (1.02–1.10) to 2.02 (1.44–2.84; Supplementary Table 5). Two studies also assessed the risk of severe COVID-19 outcomes among patients with prediabetes and/or undiagnosed diabetes, with contrasting results (17, 18).
Chronic respiratory diseases
A total of 46 studies investigated chronic respiratory diseases, including COPD (25 studies) and asthma (16 studies; Table 1). Eighteen studies (39%) reported an increased risk of severe outcomes among patients with a chronic respiratory disease for at least 1 reported outcome. Among the different case definitions for chronic respiratory disease, more evidence was found for COPD (11/25 studies) than asthma (2/16 studies). Many studies included small subpopulations, potentially limiting their ability to accurately detect risk. For larger studies (risk factor cohort n > 50), the reported OR (95% CI) ranged from aOR, 1.04 (1.01–1.08) to OR, 4.19 (1.60–10.98; Supplementary Table 6).
Cardiovascular diseases
Forty-five studies assessed CVD, including HF (19 studies) and ischemic heart disease/coronary artery disease (14 studies), using varying case definitions. Overall, 24 (53%) studies found a substantially increased risk of severe COVID-19 outcomes from at least 1 of the outcomes assessed (Table 1). Among those exploring HF, 13/19 studies (68%) found a significant association with severe COVID-19 outcomes with the aOR (95% CI) ranging from 1.28 (1.24–1.33) to 3.17 (1.88–5.34; Supplementary Table 7). Two of the 5 studies investigating atrial fibrillation (AF) and 1 of the 7 studies investigating peripheral vascular disease (PVD) reported a significant risk of severe COVID-19 outcomes (19, 20).
Cerebrovascular diseases
Twenty-four studies assessed the risk of severe COVID-19 outcomes in patients with cerebrovascular diseases (Table 1), including 15 studies examining cerebrovascular disease broadly and 7 studies specifically addressing conditions defined as stroke, transient ischemic attack (TIA), or cerebrovascular accident (CVA), with varying case definitions. Five of the 15 studies of cerebrovascular disease and 1 of the 7 studies of patients with a history of stroke/TIA/CVA showed an increased risk of severe COVID-19 outcomes (Supplementary Table 8).
Renal disease
Thirty-eight studies assessed renal disease as a risk factor for severe COVID-19 outcomes, including CKD (24 studies), renal/kidney disease (10 studies), and renal failure (2 studies). Case definitions and criteria used to define CKD varied and cohort sizes were generally small (n < 300). Of these, 24/38 studies (63%) showed a significantly increased risk of severe COVID-19 outcomes in patients with preexisting kidney/renal disease (Table 1). For studies with a risk factor cohort >50 patients, the aOR (95% CI) for severe outcomes ranged from 1.48 (1.42–1.55) to 5.59 (2.48–12.63; Supplementary Table 9). In a large study from Japan that included 20,638 adults with renal disease using broad International Classification of Diseases, Tenth Revision (ICD-10) codes, the aORs (95% CI) were 1.48 (1.42–1.55) for severe COVID-19 disease and 1.67 (1.59–1.75) for mortality (14).
Hepatobiliary disorders (including chronic liver disease)
Twenty-one studies assessed whether hepatobiliary disorders were associated with severe outcomes after COVID-19 infection. Case definitions varied, ranging from broad categories like chronic liver disease and liver disease (9 studies) to specific conditions like chronic hepatitis or cirrhosis, hepatitis B/C, and non-alcoholic fatty liver disease (NAFLD). Overall, 6 studies (29%) showed that hepatobiliary disorders were associated with an increased risk of severe outcomes (Table 1). Of these, 5 studies assessed liver disease/cirrhosis and the sixth study of a large, nationwide study in South Korea found that NAFLD was associated with an increased risk of severe COVID-19 outcomes, although results for mortality were less certain and showed wide confidence intervals (Supplementary Table 10) (21).
Cancer/malignancy
Forty-seven studies explored cancer as a potential risk factor with almost all studies using broad case definitions such as ‘cancer’, ‘malignancy’ or ‘malignant tumor’. Five studies focused on specific cancer types. Cohort sizes also varied widely, ranging from 6 to 42,854 participants. Overall, 27/47 studies (57%) found a significantly increased risk of severe COVID-19 outcomes (Table 1). In a large Korean study, malignancy was associated with an increased risk of severe COVID-19 outcomes including invasive mechanical ventilation (IMV) and other markers of disease severity (high-flow nasal cannula use, acute HF and renal replacement therapy; Supplementary Table 11) (22). However, malignancy was not found to be an independent risk factor for in-hospital mortality among patients with COVID-19 (aOR, 1.24 [95% CI, 0.92–1.66]) (22). Variations between countries in the associations between cancer and COVID-19 related hospitalization and mortality should be interpreted in the context of regional palliative care service provision and cultural variations in place of death.
Immunosuppression
Eleven studies evaluated the risk of severe COVID-19 outcomes in populations with immune-suppressive illnesses or those receiving immunosuppressive medications (Table 1). Five studies focused on HIV/AIDS and 6 studies examined individuals described as immunocompromised, immunosuppressed, or having immunodeficiency, although definitions between studies varied (e.g., use of corticosteroids, biologics, and immunosuppressive drugs; lymphocytopenia; bone marrow dysfunction; hospitalization with organ transplant, hematopoietic cancer, rheumatoid arthritis, Crohn’s disease, or ulcerative colitis). Ten studies included very small cohorts of patients with immunosuppression, ranging from 4 to 129 participants, along with 1 larger study from Korea with 5,186 participants (22). Therefore, quantitative approaches to assess associations and the ability to adjust for confounding factors were limited. Overall, 6/11 studies (55%) found a significantly increased risk of severe COVID-19 outcomes in patients who were immunosuppressed/ immunocompromised. The aOR (95% CI) in these studies varied from 1.06 (1.05–1.07) for IMV to 107 (6.38 to >999) for mortality (Supplementary Table 12).
Autoimmune disorders (rheumatic and connective tissue diseases)
Fourteen studies investigated whether autoimmune disorders increased the risk of severe outcomes from COVID-19 infection. Most studies used broad case definitions such as ‘rheumatic disease’, ‘autoimmune disease’, and ‘connective tissue disease.’ Overall, 4 of the 14 studies (29%) showed a significant increased risk in patients with autoimmune or connective tissue disorders for at least 1 outcome (Table 1). Among the 3 studies including >1,000 participants with autoimmune diseases, the aOR (95% CI) for severe COVID-19 outcomes and/or mortality ranged from 1.19 (1.12–1.26) to 1.81 (1.02–3.18; Supplementary Table 13). In a Korean nationwide cohort study of >8,000 patients with autoimmune inflammatory rheumatic diseases (inflammatory arthritis or connective tissue disease), high-dose corticosteroids use (≥10 mg/day), but not disease-modifying antirheumatic drugs, was associated with increased risk of severe COVID-19 infection and COVID-19–related death (23).
Neurological conditions
Thirty-four studies explored neurological conditions as potential risk factors, with most focusing on dementia (26 studies), hemiplegia/paraplegia/paralysis (4 studies), chronic neurological disorders (3 studies), and Parkinson disease (2 studies). Overall, 30/34 studies (88%) found a significantly increased risk of severe COVID-19 outcomes in patients with neurological conditions (Table 1). A large Japanese study that included >20,000 patients with COVID-19 with diagnosed dementia (using ICD-10 codes) found it was an independent risk factor for severe COVID-19 outcomes (aOR, 1.27 [95% CI, 1.23–1.32]) and death (1.58 [1.52–1.65]; Supplementary Table 14) (14). Another Japanese study observed a greater than 3-fold increased risk of mortality among adults aged >50 years with Parkinson’s disease (OR: 3.57 [95% CI: 1.08, 10.2]) (24).
Mental health and behavioral disorders
Ten studies investigated mental and behavioral disorders and the risk of severe outcomes from COVID-19 infection. Definitions varied across studies and included ‘mental disorder’ and ‘mental illnesses,’ for which studies were larger, and more specific conditions, including schizophrenia and depression/anxiety, wherein cohort sizes were smaller. Overall, 6/10 studies (60%) found a significantly increased risk of severe COVID-19 outcomes for patients with mental and behavioral disorders (Table 1). The aOR (95% CI) for severe COVID-19 outcomes ranged from 1.27 (1.01–1.66) to 3.57 (1.36–9.38; Supplementary Table 15). In a Korean nationwide cohort study of >1,000 patients with a previous diagnosis of a mental illness, severe mental illness (nonaffective or affective disorders with psychotic features) was associated with an increased risk of severe COVID-19 outcomes (OR: 1.27 [95% CI: 1.01, 1.66]) (25).
Other medical conditions
There were 18 studies that were categorized as other medical conditions, of which 9 showed significant associations (Supplementary Table 16).
Discussion
This review identified several risk factors associated with severe COVID-19 outcomes, including older age, male sex, obesity (BMI ≥25 or ≥30 kg/m2), HF, chronic renal disease (including CKD), cancer, immunosuppression and dementia, consistent with global reviews and meta-analyses (2, 26–28). Some risk factors, such as older age and immunocompromise align with current COVID-19 recommendations in the APAC region. However, a large volume of evidence was associated with other conditions, including CVD, hypertension, diabetes (and prediabetes), kidney disease and liver disease, less consistently reflected in regional vaccine guidance. Regional authorities and medical society guidance varies, and often broad disease categories for COVID-19 vaccination are advised, with limited examples of specific conditions. This may result in vulnerable populations being overlooked for targeted prevention.
Associations with severe COVID-19 outcomes were identified under the categories of hypertension, diabetes (including prediabetes), and CVD. This finding is consistent with a recent meta-analysis of cardiometabolic risk factors in the APAC region that demonstrated a 2.85-fold increase in COVID-19–associated mortality for diabetes, a 2.5-fold increase for hypertension, and a 2.75-fold increase for CVD (29). A large volume of evidence was identified to indicate an association between HF and severe COVID-19 outcomes. Given the rapidly rising prevalence of HF in the region, and the earlier onset observed in Asian populations compared to other regions (11), the findings highlight the need for increased awareness of preventative strategies among younger individuals with HF. By 2050, ischemic heart disease and stroke are projected to be the most prevalent subtypes of CVD in the region, with high systolic blood pressure the leading risk factor (8). Regional variations in CVD burden indicate high ischemic heart disease mortality in Central Asia, while stroke is a key driver in Southeast Asia (30). This is largely attributed to regional differences in the burden of AF and flutter, leading to a rise in thromboembolic strokes. Ongoing focus on effective strategies to reduce the burden of CVD-associated severe COVID-19 outcomes among Asian populations is warranted from this review.
This review identified an association between severe COVID-19 disease and neurological conditions, particularly dementia. This finding is consistent with global studies reporting a > 7-fold increased risk of COVID-19 hospitalization and death among older patients with preexisting dementia (31), a phenomenon that has biological (neuronal injury) and environmental explanations (32, 33). Importantly, with Asia now at the forefront of population aging, and Hong Kong, South Korea and Japan expected to have approximately 40% of their populations aged ≥65 years by 2050 (34), regional dementia case estimates are rising in the APAC region (35). Mental and behavioral disorders were found to be associated with an increased risk of severe COVID-19 outcomes. These conditions, along with dementia, are notably under-represented in regional guidelines. This review supports global evidence, for example, a UK Biobank study showing individuals with serious mental illness (SMI) were hospitalized with COVID-19 twice as often as those without SMI (36). SMI was also associated with higher rates of illness and death than heart disease, COPD, and diabetes.
This review suggests that the risk of severe COVID-19 outcomes in patients with liver and kidney disease may be influenced by the stage or severity of these conditions. Global studies have shown that patients with advanced liver disease, such as cirrhosis, and those with CKD stages 4–5 are at substantially higher risk of severe COVID-19 complications which is reflected in current vaccine recommendations across the region (37, 38). While current vaccine recommendations typically focus on the presence of individual medical conditions, it is crucial to consider the cumulative burden of conditions when assessing the risk of severe COVID-19 disease. Given the high prevalence and clustering of cardiometabolic conditions in APAC populations, such as hypertension, diabetes, and increasingly, obesity, risk assessment tools and vaccine prioritization strategies may be enhanced by incorporating measures of multimorbidity (11). Specific recommendations for COVID-19 vaccination for those with multimorbidity and elevated metabolic risks may be warranted. Other regionally relevant exposures, such as elevated smoking prevalence in certain APAC subgroups, may also contribute to underlying cardiovascular and respiratory vulnerability, and warrant further exploration.
A key strength of this analysis is its broad and inclusive review of the available literature across selected APAC countries; however, several limitations must be acknowledged. As a narrative review focused on conceptual themes in the literature, no formal risk-of-bias assessment was conducted, nor was publication bias quantified, as would typically be done in a systematic review. This synthesis is based on published studies and may inadvertently over-represent positive findings due to publication bias. A high degree of heterogeneity was observed across studies, including variations in the definitions of risk conditions and severe outcomes (influenced by definitions and data availability in national health and insurance databases), reported parameters, statistical analyses, modeling approaches, and adjustment for confounding factors. Some studies had small samples sizes, limiting the precision of estimates and the ability to adjust for covariates. Most studies did not account for smoking or medication use for comorbidities, and residual confounding and statistical robustness were limitations of some included studies. Most included studies collected data early in the pandemic, before the introduction of vaccines and/or specific antiviral medications, potentially limiting the applicability of findings to the current context in which these interventions are widely available. Future research should aim to standardize definitions of risk factors and outcomes, adopt more robust confounding adjustments, and include studies that evaluate post-vaccination era cohorts. Regional multicenter collaborations could help reduce heterogeneity and support targeted systematic reviews focusing on specific risk factors identified in this review. Where appropriate, meta-analyses of these data could more accurately quantify risk among Asian populations and improve generalizability.
In summary, this review synthesizes region-specific evidence, identifying several under-recognized risk factors for severe COVID-19 outcomes. These findings complement global evidence but also highlight important regional nuances. Improved identification of high-risk groups, particularly those with dementia, mental illness, and cardiometabolic multimorbidity, can strengthen targeted prevention efforts in APAC settings.
Conclusion
This review appears to be the first synthesis of risk factors for severe COVID-19 outcomes specific to the Asia-Pacific region, based on currently available evidence. Beyond the well-established risks of older age and immunocompromise, several high-priority conditions, such as AF, PVD, dementia, and mental health disorders, were identified as often overlooked in current guidance. To improve protection for vulnerable groups, public health agencies in APAC should update vaccination frameworks to explicitly include these conditions, expand access to boosters and antivirals for individuals with multimorbidity, and integrate region-specific evidence into national risk assessment and public health messaging. Continued surveillance and evidence synthesis will be critical to adapting COVID-19 policy for emerging variants and population needs.
Author contributions
MT: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AB: Conceptualization, Data curation, Formal analysis, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing. SO: Conceptualization, Methodology, Validation, Writing – review & editing. MC: Conceptualization, Methodology, Validation, Writing – review & editing. BL: Conceptualization, Methodology, Validation, Writing – review & editing. TI: Conceptualization, Methodology, Validation, Writing – review & editing. Y-CW: Conceptualization, Methodology, Validation, Writing – review & editing. CC: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Moderna, Inc.
Acknowledgments
The authors(s) acknowledge assistance with literature searching and data extraction from Bastion Brands provided by Stephanie Yee and Nick Tsimplis and Medical writing and editorial assistance were provided by Louansha Nandlal of MEDiSTRAVA in accordance with Good Publication Practice (GPP 2022) guidelines.
Conflict of interest
MT, AB, SO, MC, BL, TI, Y-CW, and CC are employees of Moderna, Inc., and hold stock/stock options in the company.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Correction note
This article has been corrected with minor changes. These changes do not impact the scientific content of the article.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1562179/full#supplementary-material
References
1. WHO. Coronavirus disease (COVID-19). Available online at: https://www.who.int/health-topics/coronavirus#tab=tab_1. Accessed 25 November 2024.
2. Booth, A, Reed, AB, Ponzo, S, Yassaee, A, Aral, M, Plans, D, et al. Population risk factors for severe disease and mortality in COVID-19: a global systematic review and meta-analysis. PLoS One. (2021) 16:e0247461. doi: 10.1371/journal.pone.0247461
3. Fang, X, Li, S, Yu, H, Wang, P, Zhang, Y, Chen, Z, et al. Epidemiological, comorbidity factors with severity and prognosis of COVID-19: a systematic review and meta-analysis. Aging (Albany NY). (2020) 12:12493–503. doi: 10.18632/aging.103579
4. Wiersinga, WJ, Rhodes, A, Cheng, AC, Peacock, SJ, and Prescott, HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. (2020) 324:782–93. doi: 10.1001/jama.2020.12839
5. Petrilli, CM, Jones, SA, Yang, J, Rajagopalan, H, O’Donnell, L, Chernyak, Y, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in new York City: prospective cohort study. BMJ. (2020) 369:m1966. doi: 10.1136/bmj.m1966
6. Mediavilla, JR, Lozy, T, Lee, A, Kim, J, Kan, VW, Titova, E, et al. Molecular and clinical epidemiology of SARS-CoV-2 infection among vaccinated and unvaccinated individuals in a large healthcare organization from New Jersey. Viruses. (2023) 15:1699. doi: 10.3390/v15081699
7. Centers for Disease Control and Prevention. Underlying medical conditions associated with higher risk for severe COVID-19: Information for healthcare professionals. (2023). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html. Accessed 15 May 2023 2023.
8. Goh, RSJ, Chong, B, Jayabaskaran, J, Jauhari, SM, Chan, SP, Kueh, MTW, et al. The burden of cardiovascular disease in Asia from 2025 to 2050: a forecast analysis for East Asia, South Asia, South-East Asia, Central Asia, and high-income Asia Pacific regions. Lancet Reg Health West Pac. (2024) 49:101138. doi: 10.1016/j.lanwpc.2024.101138
9. OECD/WHO. Health at a glance: Asia/Pacific 2022: Measuring Progress towards universal health coverage. Paris: OECD Publishing (2022).
10. World Health Organization. Multimorbidity: Technical series on safer primary care. (2016). Available online at: https://iris.who.int/bitstream/handle/10665/252275/9789241511650-eng.pdf Accessed 15 May 2024.
11. Ang, N, Chandramouli, C, Yiu, K, Lawson, C, and Tromp, J. Heart failure and multimorbidity in Asia. Curr Heart Fail Rep. (2023) 20:24–32. doi: 10.1007/s11897-023-00585-2
12. Watson, OJ, Barnsley, G, Toor, J, Hogan, AB, Winskill, P, and Ghani, AC. Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect Dis. (2022) 22:1293–302. doi: 10.1016/S1473-3099(22)00320-6
13. Bruxvoort, KJ, Sy, LS, Qian, L, Ackerson, BK, Luo, Y, Lee, GS, et al. Real-world effectiveness of the mRNA-1273 vaccine against COVID-19: interim results from a prospective observational cohort study. Lancet Reg Health Am. (2022) 6:100134. doi: 10.1016/j.lana.2021.100134
14. Miyashita, K, Hozumi, H, Furuhashi, K, Nakatani, E, Inoue, Y, Yasui, H, et al. Changes in the characteristics and outcomes of COVID-19 patients from the early pandemic to the delta variant epidemic: a nationwide population-based study. Emerg Microbes Infect. (2023) 12:2155250. doi: 10.1080/22221751.2022.2155250
15. Shin, EK, Choi, HY, and Hayes, N. The anatomy of COVID-19 comorbidity networks among hospitalized Korean patients. Epidemiol Health. (2021) 43:e2021035. doi: 10.4178/epih.e2021035
16. Nishimura, M, Asai, K, Tabuchi, T, Toyokura, E, Kawai, T, Miyamoto, A, et al. Association of combustible cigarettes and heated tobacco products use with SARS-CoV-2 infection and severe COVID-19 in Japan: a JASTIS 2022 cross-sectional study. Sci Rep. (2023) 13:1120. doi: 10.1038/s41598-023-28006-3
17. Fukushima, T, Chubachi, S, Namkoong, H, Asakura, T, Tanaka, H, Lee, H, et al. Clinical significance of prediabetes, undiagnosed diabetes and diagnosed diabetes on critical outcomes in COVID-19: integrative analysis from the Japan COVID-19 task force. Diabetes Obes Metab. (2023) 25:144–55. doi: 10.1111/dom.14857
18. Koh, H, Moh, AMC, Yeoh, E, Lin, Y, Low, SKM, Ooi, ST, et al. Diabetes predicts severity of COVID-19 infection in a retrospective cohort: a mediatory role of the inflammatory biomarker C-reactive protein. J Med Virol. (2021) 93:3023–32. doi: 10.1002/jmv.26837
19. Zhou, J, Lakhani, I, Chou, O, Leung, KSK, Lee, TTL, Wong, MV, et al. Clinical characteristics, risk factors and outcomes of cancer patients with COVID-19: a population-based study. Cancer Med. (2023) 12:287–96. doi: 10.1002/cam4.4888
20. Chang, Y, Jeon, J, Song, TJ, and Kim, J. Association between the fatty liver index and the risk of severe complications in COVID-19 patients: a nationwide retrospective cohort study. BMC Infect Dis. (2022) 22:384. doi: 10.1186/s12879-022-07370-x
21. Yoo, HW, Jin, HY, Yon, DK, Effenberger, M, Shin, YH, Kim, SY, et al. Non-alcoholic fatty liver disease and COVID-19 susceptibility and outcomes: a Korean Nationwide cohort. J Korean Med Sci. (2021) 36:e291. doi: 10.3346/jkms.2021.36.e291
22. Baek, MS, Lee, MT, Kim, WY, Choi, JC, and Jung, SY. COVID-19-related outcomes in immunocompromised patients: a nationwide study in Korea. PLoS One. (2021) 16:e0257641. doi: 10.1371/journal.pone.0257641
23. Shin, YH, Shin, JI, Moon, SY, Jin, HY, Kim, SY, Yang, JM, et al. Autoimmune inflammatory rheumatic diseases and COVID-19 outcomes in South Korea: a nationwide cohort study. Lancet Rheumatol. (2021) 3:e698–706. doi: 10.1016/S2665-9913(21)00151-X
24. Nojiri, S, Irie, Y, Kanamori, R, Naito, T, and Nishizaki, Y. Mortality prediction of COVID-19 in hospitalized patients using the 2020 diagnosis procedure combination administrative database of Japan. Intern Med. (2023) 62:201–13. doi: 10.2169/internalmedicine.0086-22
25. Lee, SW, Yang, JM, Moon, SY, Yoo, IK, Ha, EK, Kim, SY, et al. Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study. Lancet Psychiatry. (2020) 7:1025–31. doi: 10.1016/S2215-0366(20)30421-1
26. Bedston, S, Almaghrabi, F, Patterson, L, Agrawal, U, Woolford, L, Anand, SN, et al. Risk of severe COVID-19 outcomes after autumn 2022 COVID-19 booster vaccinations: a pooled analysis of national prospective cohort studies involving 7.4 million adults in England, Northern Ireland, Scotland and Wales. Lancet Reg Health Eur. (2024) 37:100816. doi: 10.1016/j.lanepe.2023.100816
27. Dessie, ZG, and Zewotir, T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect Dis. (2021) 21:855. doi: 10.1186/s12879-021-06536-3
28. Saragih, ID, Saragih, IS, Batubara, SO, and Lin, CJ. Dementia as a mortality predictor among older adults with COVID-19: a systematic review and meta-analysis of observational study. Geriatr Nurs. (2021) 42:1230–9. doi: 10.1016/j.gerinurse.2021.03.007
29. Ru Ying Fong, AL, Gao, F, Yap, JJL, and Yeo, KK. Cardiometabolic risk factors and COVID-19 outcomes in the Asia-Pacific region: a systematic review, Meta-analysis and Meta-regression of 84,011 patients. J Asian Pacific Society Cardiol. (2023). 2:e22
30. Turana, Y, Tengkawan, J, Chia, YC, Nathaniel, M, Wang, JG, Sukonthasarn, A, et al. Hypertension and stroke in Asia: a comprehensive review from HOPE Asia. J Clin Hypertens (Greenwich). (2021) 23:513–21. doi: 10.1111/jch.14099
31. Atkins, JL, Masoli, JAH, Delgado, J, Pilling, LC, Kuo, CL, Kuchel, GA, et al. Preexisting comorbidities predicting COVID-19 and mortality in the UK biobank community cohort. J Gerontol A Biol Sci Med Sci. (2020) 75:2224–30. doi: 10.1093/gerona/glaa183
32. Kanberg, N, Ashton, NJ, Andersson, LM, Yilmaz, A, Lindh, M, Nilsson, S, et al. Neurochemical evidence of astrocytic and neuronal injury commonly found in COVID-19. Neurology. (2020) 95:e1754–9. doi: 10.1212/WNL.0000000000010111
33. Wei, G, Diehl-Schmid, J, Matias-Guiu, JA, Pijnenburg, Y, Landin-Romero, R, Bogaardt, H, et al. The effects of the COVID-19 pandemic on neuropsychiatric symptoms in dementia and carer mental health: an international multicentre study. Sci Rep. (2022) 12:2418. doi: 10.1038/s41598-022-05687-w
34. United Nations. World Social Report 2023: Leaving no one behind in an ageing world. (2023). Available online at: https://www.un.org/development/desa/dspd/wp-content/uploads/sites/22/2023/01/2023wsr-fullreport.pdf.
35. GBD 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the global burden of disease study 2019. Lancet Public Health. (2022) 7:e105–25. doi: 10.1016/S2468-2667(21)00249-8
36. Hassan, L, Peek, N, Lovell, K, Carvalho, AF, Solmi, M, Stubbs, B, et al. Disparities in COVID-19 infection, hospitalisation and death in people with schizophrenia, bipolar disorder, and major depressive disorder: a cohort study of the UK biobank. Mol Psychiatry. (2022) 27:1248–55. doi: 10.1038/s41380-021-01344-2
37. Jdiaa, SS, Mansour, R, El Alayli, A, Gautam, A, Thomas, P, and Mustafa, RA. COVID-19 and chronic kidney disease: an updated overview of reviews. J Nephrol. (2022) 35:69–85. doi: 10.1007/s40620-021-01206-8
Keywords: COVID-19, severe outcomes, mortality, Asia-Pacific, risk factors, SARS-CoV-2, comorbidity, epidemiology
Citation: Thompson M, Buttery AK, Oh SX, Chan M, Lee BH, Iino T, Wang Y-CA and Clarke C (2025) Risk factors for severe COVID-19 outcomes in the Asia-Pacific region: a literature review. Front. Public Health. 13:1562179. doi: 10.3389/fpubh.2025.1562179
Edited by:
Carmine Siniscalchi, University of Parma, ItalyReviewed by:
Miodrag Zivkovic, Singidunum University, SerbiaFrancisco Rodrigues, Polytechnic Institute of Castelo Branco, Portugal
Copyright © 2025 Thompson, Buttery, Oh, Chan, Lee, Iino, Wang and Clarke. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Madeline Thompson, bWFkZWxpbmUudGhvbXBzb25AbW9kZXJuYXR4LmNvbQ==
†These authors share first authorship
 Madeline Thompson
Madeline Thompson Amanda K. Buttery
Amanda K. Buttery Shu Xin Oh2
Shu Xin Oh2