- Department of Health Administration, Kongju National University, Gongju, Republic of Korea
Various mental disorders are becoming increasingly prevalent worldwide. Young adults are particularly vulnerable to mental health issues amid rapid lifestyle changes and socioeconomic pressures. This study adopted hybrid machine learning methods, combining existing statistical analysis and machine learning, to determine which factors affect young adults’ mental health, considering recent changes. We used 4-year data (2019–2022) derived from the Community Health Survey, and the final study sample included 141,322 young people aged 19–34. We selected variables based on a literature review and feature selection and performed complex sample logistic regression analysis. New variables that had not previously been discussed (unmet medical needs, chewing difficulty, and accident/addiction experiences) were derived and found to significantly impact depression and subjective stress. These factors’ impact on mental health was generally greater than that of the theoretical background variables. In conclusion, this study emphasizes the need to consistently monitor various factors in today’s rapidly changing environment when devising policies aimed at managing young adults’ mental health.
1 Introduction
Various mental disorders are continuously becoming increasingly prevalent worldwide (1), with young adults among society’s most vulnerable to mental health disturbances, and the general health loss associated with these issues peaks among people aged 25–35 (2, 3). Young adults transitioning from adolescence to adulthood are also considered particularly vulnerable to depression and stress (4). Mental health exhibits different patterns according age (5), and the incidence of chronic problems, including anxiety disorders and depression, increases during young adulthood (6). Mental health problems developed in adolescence often persist in young adults (7), and these problems may be exacerbated by comorbid mental disorders, such as functional impairment as a consequence of depression (8).
It is crucial to appreciate the factors that can cause mental health to deteriorate differentially for each age group. Young adults are widely exposed to psycho-emotional difficulties associated with life changes and pressures from academic study, employment, marriage, childbirth, and financial independence (9). Compared to other age groups, young adults who experience poor mental health are more likely to suffer from long-term mental disorders (10). While children and adolescents are typically supported and guided by parents and school systems (11) and relatively stable social safety nets are in place for those in middle and old age (12, 13), young adults are highly susceptible to mental health difficulties owing to the pressures of newfound independence and social instability.
The factors that affect young adults’ mental health may be personal, socioeconomic, environmental, or cultural. Previous studies have examined the influences of lifestyle (14), physical activity (15), employment (16), academic study (17), family environment (18), housing type (19), and stigma (20). These factors are major risk factors in young adults’ adverse mental health (21, 22). However, socioeconomic and cultural environments have recently changed at an unprecedentedly rapid pace, including changes in educational environments and occupational structure (23) and improved access to digital environments (24), significantly influencing the lifestyles and structures of young adults (25). To reflect these rapid environmental changes, it is important to continuously monitor the risk factors for mental health disturbances within wider theoretical considerations.
Recently, there have been attempts to use artificial intelligence (AI), such as machine learning (ML) and deep learning, to study this topic (26–28). To reflect the changing environment, it is necessary to accumulate quantitative and qualitative results for each life stage using the latest data. ML techniques are practical for handling vast amounts of unstructured data (29), which makes it useful for identifying risk factors that are difficult to detect with traditional statistical methods. However, ML has limitations with respect to interpreting relationships between variables (30). One effective means of addressing these limitations is to combine ML techniques with traditional statistical analysis methods.
This study explored the factors affecting the mental health of young adults using a hybrid machine learning/traditional statistics technique. Specifically, we confirmed theoretical variables based on a literature review, selected variables via ML, compared and evaluated models, and confirmed the associations between the new variables selected by ML. Our method can flexibly explore the factors that influence young adults’ mental health in response to environmental changes.
2 Methods
2.1 Data resources and participants
We used data from the Community Health Survey (CHS) organized by the Korea Disease Control and Prevention Agency. The CHS is a nationwide and representative survey that has been conducted among adults aged 19 or older every year since 2008. The survey includes various health-related questions, covering health behaviors, mental health, unmet medical needs, and social and physical environments. The sampling process involves stratification by housing type (Dong/Eup/Myeon), followed by a two-stage sampling method. First, the sample regions are selected via probability proportional systematic extraction; then final households are selected through systematic extraction. The CHS operates a 4-year survey cycle, and we used data from the period 2019–2022. From among the survey’s 919,395 participants, 141,322 young people aged 19–34 were ultimately selected after excluding missing data and incomplete responses. This study was granted exemption by the Institutional Review Board of Kongju National University in view of using raw data from the Community Health Survey in Korea (IRB number: 2023-102).
2.2 Study design
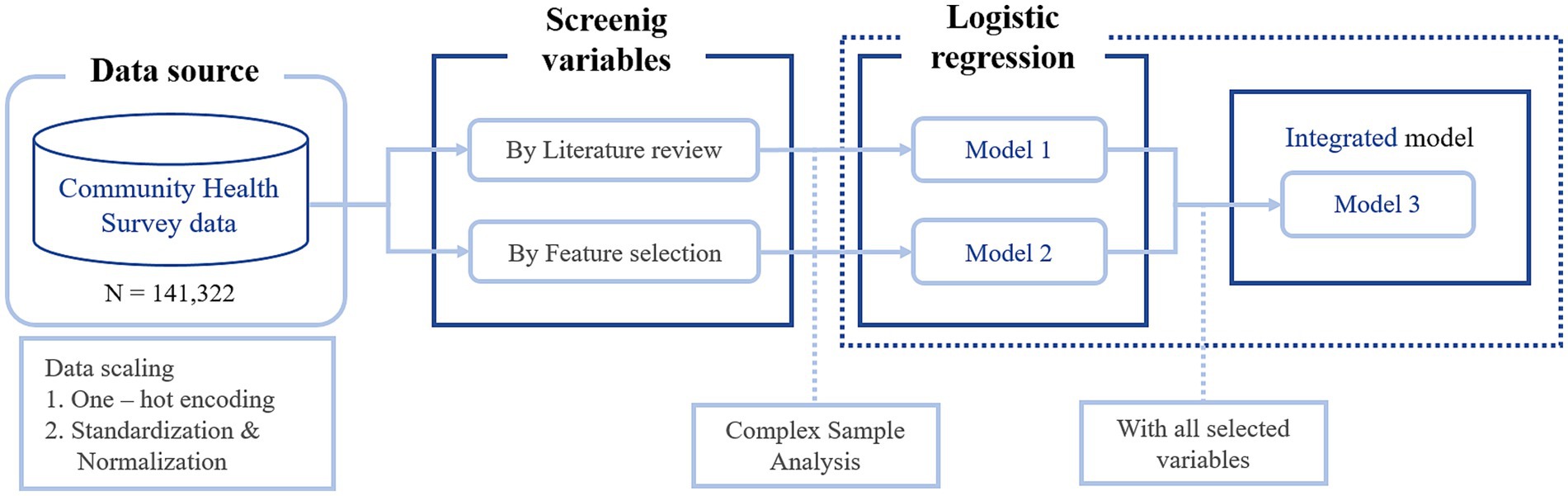
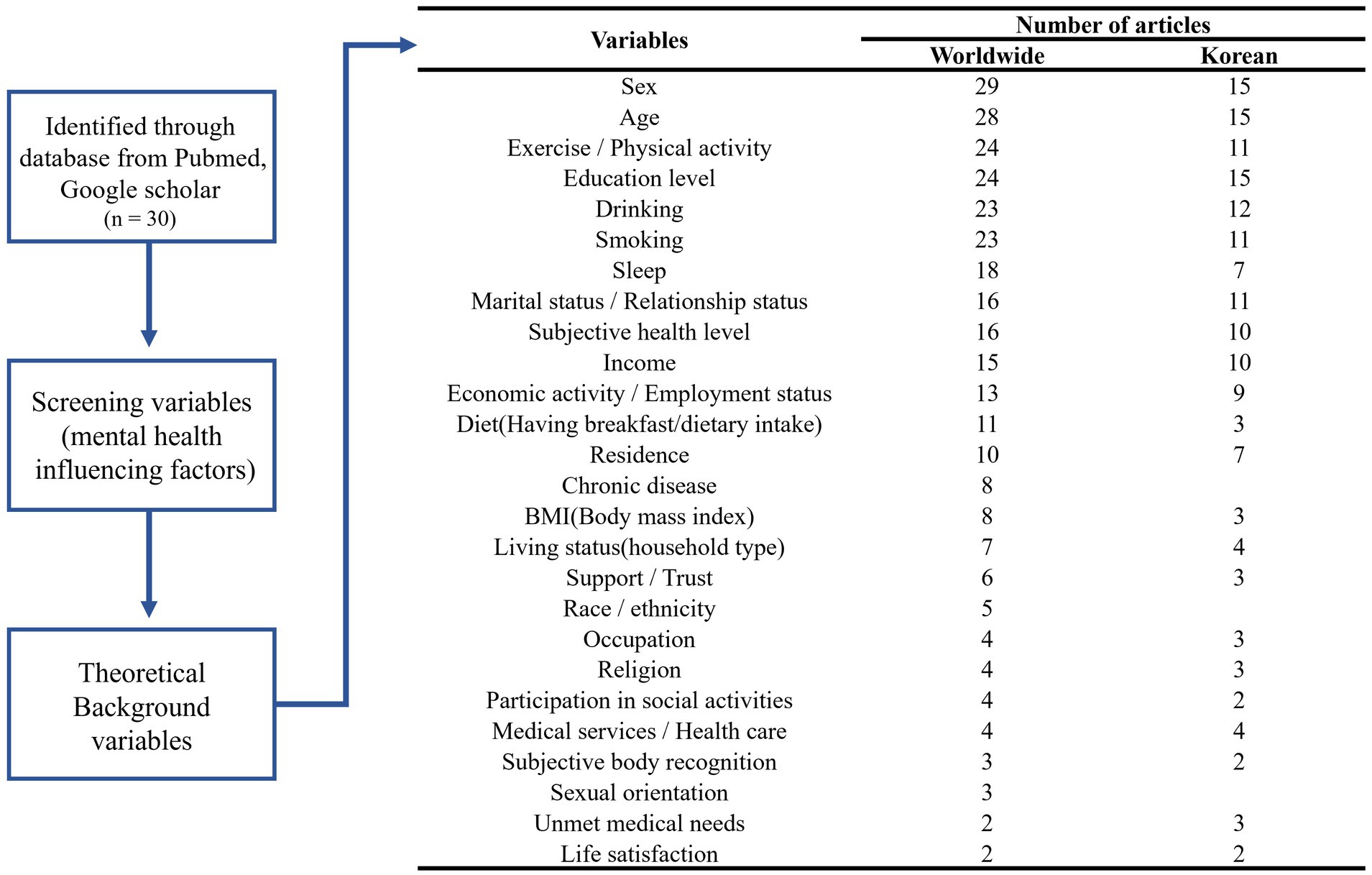
We used a hybrid machine learning approach that combines traditional statistical analysis with ML. Two main processes were used to select the factors influencing young adults’ mental health. First, we searched the literature, selecting 15 papers from PubMed published within the last 10 years. The following search string was used: (mental health OR depression OR depressive OR stress) AND (young adult OR young people). We also selected 15 Korean papers from Google Scholar because we used survey data from the Korean context. Next, variables were selected by feature selection on all variables in the data. Feature selection can reduce model complexity and improve performance by removing irrelevant variables to identify the optimal subset from a wide range of data (31). Following each process, we constructed Models 1 and 2 and performed logistic regression analysis to evaluate the impact of the selected variables on the mental health of young adults. Finally, we compared the impact of variables in an integrated model (Model 3) based on all selected variables. The overall flow of the study design is presented in Figure 1.
2.3 Variables
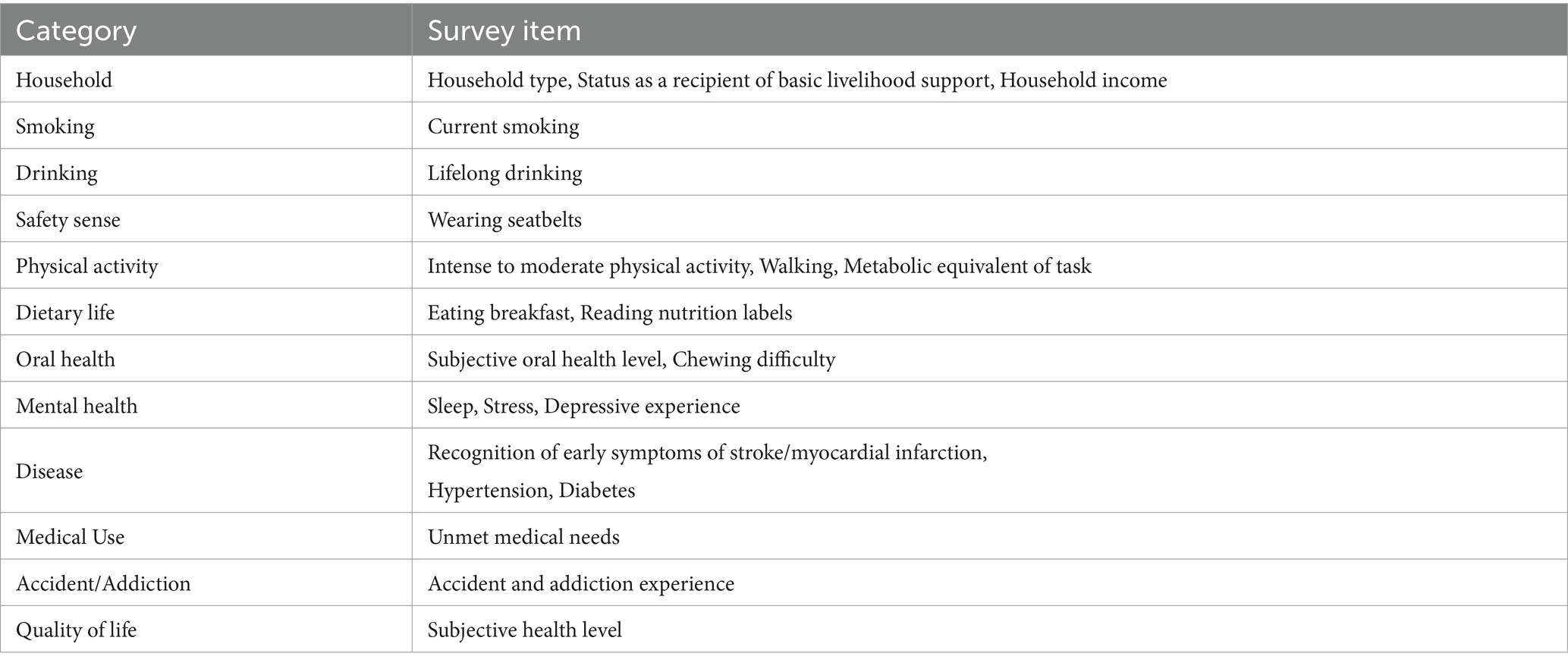
Mental health-related variables were defined as the experience of depression and subjective stress level. Depression experience was assessed using the CHS item, ‘During the past year, have you ever felt so sad or hopeless for two consecutive weeks or more that it disrupted your daily life?’ Respondents who answered ‘yes’ were classified as having experienced depression. Subjective stress level was measured by asking, ‘How much stress do you usually feel in your daily life?’ Those who answered ‘very much’ or ‘a lot’ were classified as experiencing a high level of subjective stress. For logistic regression analysis, demographic variables such as sex, age, education level, marital status, economic activity, and residential area were designated as basic adjustment variables. Detailed variables from the CHS used in the study, including demographic, behavioral, and health-related categories such as smoking, drinking, physical activity, and mental health items, are presented in Table 1.
2.4 Data analysis
We analyzed the data using R version 4.3.1 and IBM SPSS Statistics 25.0, with a significance level set at α = 0.05. Feature selection was conducted using lasso regression to identify factors influencing mental health. Lasso is an extension of generalized linear regression, which continuously performs shrinkage operations to reduce the possibility of model overfitting (32). It reduces the variance of regression coefficients and selects more relevant and interpretable variables from large sets of multicollinear variables (33). Considering that the CHS has a complex sample design, we performed complex sample logistic regression considering weights.
3 Results
3.1 Screening factors affecting mental health
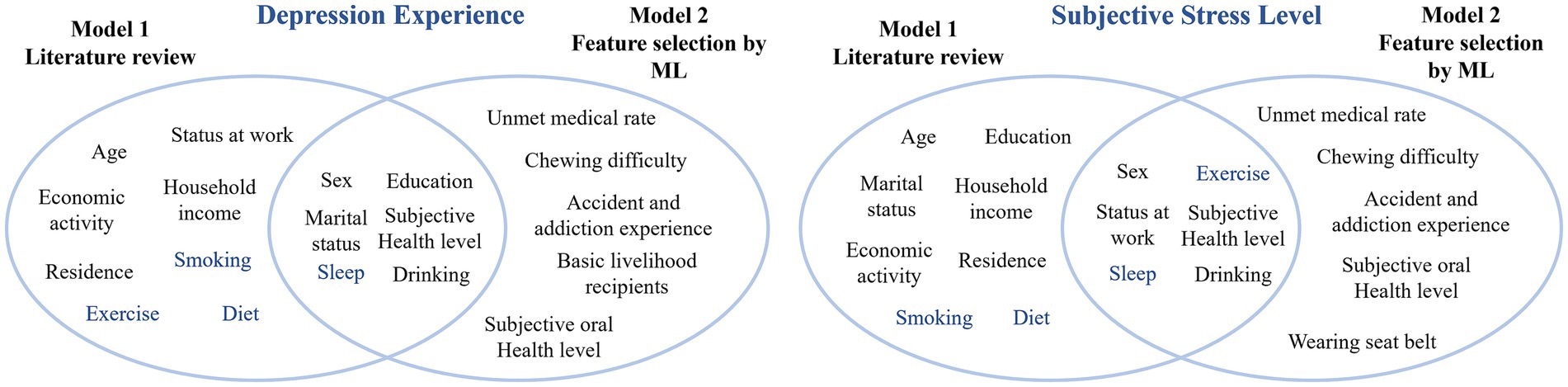
Figure 2 presents the outcome of the literature review, including the screening steps and the distribution of mental health-related variables identified from both global and Korean studies. Subjective health level, smoking, drinking, breakfast consumption, sleep duration, and exercise were selected as theoretical background variables, excluding sociodemographic variables. As a result of feature selection for mental health variables, subjective health level, sex, sleep, and drinking were commonly selected among the theoretical background variables. Excluding variables overlapping with the theoretical background, unmet medical needs, chewing difficulty, the number of accidents and addiction experiences, and subjective oral health were selected. Figure 3 presents the variables selected based on the literature review and feature selection. In this study, variables that selected only through feature selection were designated key factors, using the top 3–5% as a cutoff.
3.2 Complex sample logistic regression analysis
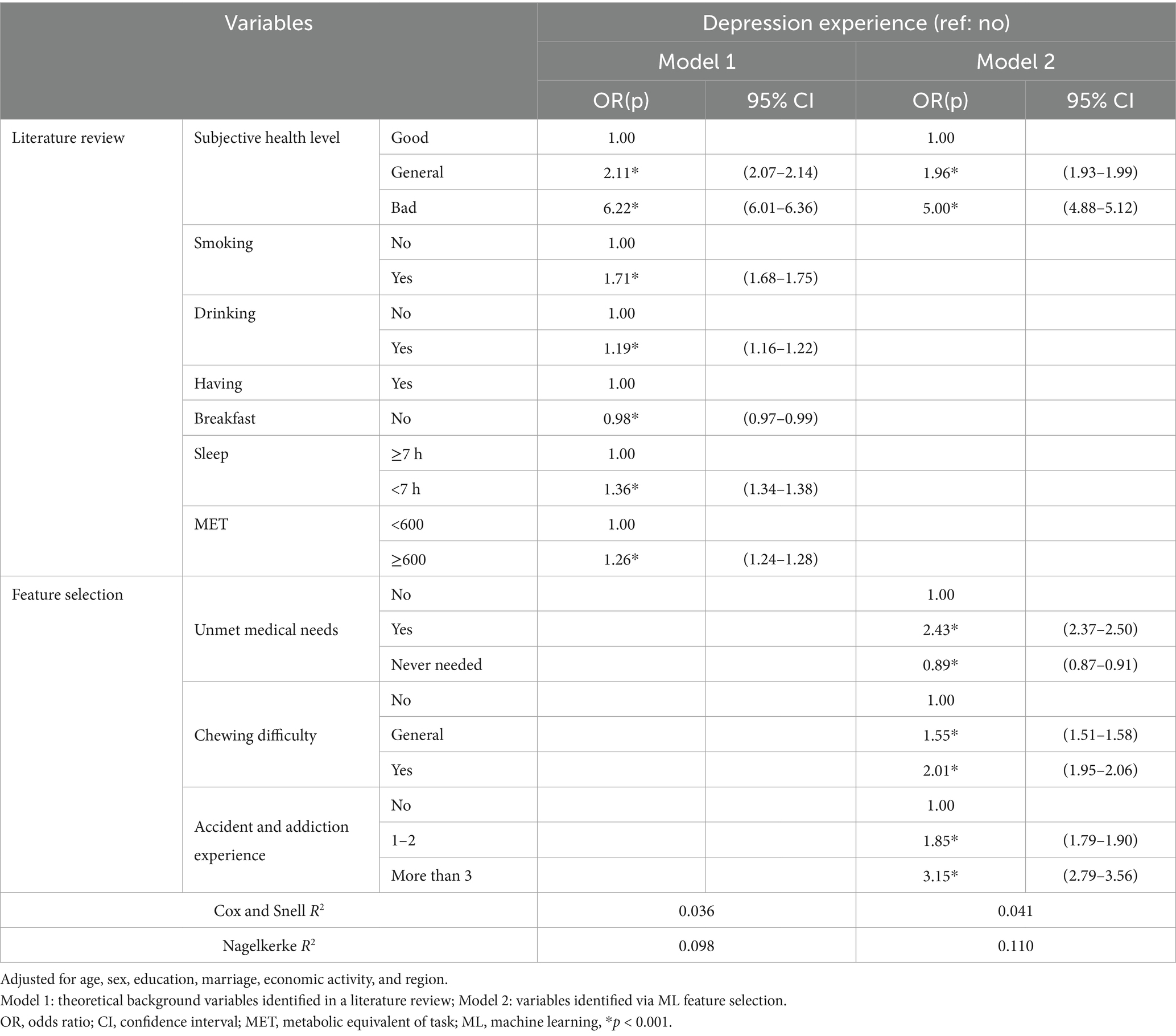
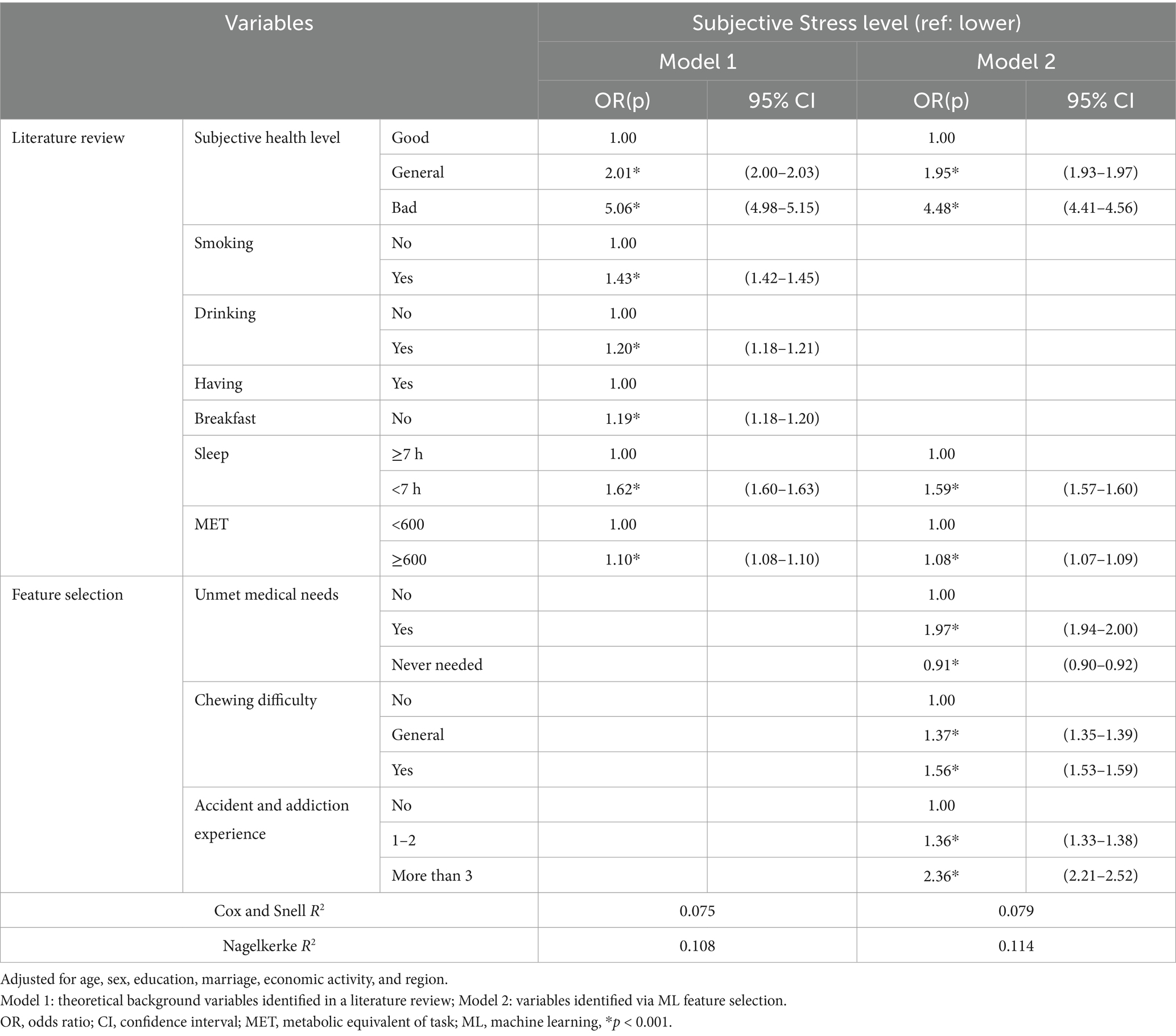
Tables 2, 3 present the results of a complex sample logistic regression analysis that adjusted for age, sex, education, marriage, economic activity, and region to investigate the impact of selected independent variables on mental health. All variables in Models 1 and 2 had a statistically significant impact on depression (p < 0.001). In the theoretical background variables, subjective health showed the strongest association, indicating that worse subjective health increased the likelihood of experiencing depression. For key factors, people experiencing unmet medical needs or discomfort when chewing showed a greater tendency to experience depression. A higher number of accident/addiction experiences also increased the likelihood of experiencing depression.
Regarding subjective stress levels, all variables had a significant impact (p < 0.001). Subjective health had the highest impact, whereby people with worse subjective health were more vulnerable to subjective stress. In the theoretical background variables, people who smoke or who sleep for less than 7 h at night were more likely to experience higher levels of subjective stress. Regarding the key factors, people experiencing unmet medical needs and chewing difficulty or more accident/addiction experiences tended to be more susceptible to subjective stress. Comparison of Models 1 and 2 for both dependent variables revealed that the odds ratio (OR) values of key factors were generally higher than those of theoretical background variables. Results of the complex sample logistic regression for all models are presented in Supplementary Tables 1, 2.
3.3 Key factors in the integrated model
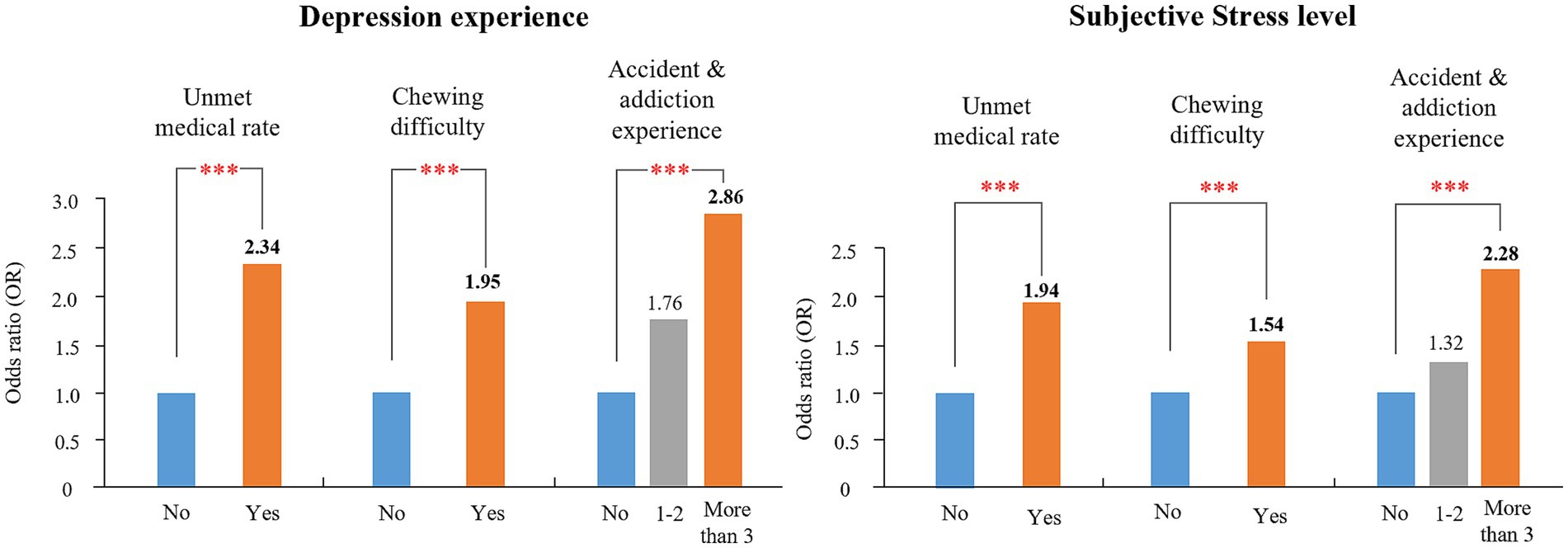
We compared the impact of theoretical background variables and key factors on mental health by constructing an integrated model, Model 3. Figure 4 shows the OR values of the key factors associated with depression experience and subjective stress level. Both mental health variables showed a similar pattern, with the highest OR value for accidents/addiction, followed by unmet medical needs and chewing difficulty.
4 Discussion
We explored the factors influencing the mental health of young adults, considering changes in socioeconomic and cultural environments. We integrated a review of the literature with statistical analysis and ML based on the most up-to-date data available to reflect recent changes. We identified previously undiscussed variables affecting young adults’ mental health, such as unmet medical needs, chewing difficulty, and accident/addiction experiences; these significantly impacted depression and subjective stress.
Sex, subjective health level, sleep, and alcohol consumption are commonly related to depression and stress in young adults (34–37). Young adulthood is generally perceived as a healthy stage in the life cycle, with low use of medical services. However, in Korea (38) and elsewhere (39, 40) young adults are in fact more likely than older adult to experience unmet medical needs, whereby the availability of certain services is compromised by lengthy waiting times in hospitals or the lack of medical resources in certain residential areas (41). Recently, the emergence and development of various digital health technologies, such as mobile-health and AI-based health platforms, have increased expectations regarding healthcare services among young people, who engage extensively with social media (42). Arguably, therefore, young adults are more likely today to complain about their unmet medical needs arising from temporal constraints (43) or lack of satisfaction with medical services (44). Unmet medical needs are significantly correlated with high levels of stress and depression (38) and strongly associated with depression in young adults (45).
Young adulthood is associated with a high frequency of trauma and accidents (46), with a rate that is higher than those of other age groups (47, 48). Young adults’ use of digital devices has rapidly increased in recent years, and as the digital environment continues to change, the possibility of new threats, such as cyberbullying or cyberstalking, is also increasing (49). These can lead to symptoms of post-traumatic stress disorder (PTSD) and contribute to other mental health problems, such as depression, anxiety, and suicidal thoughts (50–52). Previous studies have also demonstrated that young adults who experience trauma are more likely to develop extensive mental health problems, including PTSD (53). PTSD is not a temporary condition but can degrade an individual’s daily life and social function in the long term. Therefore, early intervention to mediate traumatic experiences during young adulthood is crucial.
Furthermore, young adults often engage in substance use (54). Substance addiction has become a serious problem (55) as a result of recent trends such as the increasing use of e-cigarettes and synthetic drugs (56), and increased exposure to these substances via social media and online (57). Addiction to substances is associated with mental disorders in young adults and may even be a contributing factor (58). Use of multiple substances, in particular, may be an important predictor of increased depression. Recent studies have demonstrated that the concurrent use of both alcohol and cannabis may be associated with depressive symptoms in young adults (59). Stress in young adults is associated with addiction (60), and stressful life events can lead to substance abuse (61). Therefore, future research that considers the interaction between substance use, addiction, and mental health in young adults is warranted.
Young adults often have cavities and periodontal diseases stemming from childhood and may need to have several teeth extracted (62). According to the 2017 National Health Statistics, the prevalence of periodontal disease in young adults aged 19–29 years has shown a continuous annual increase (63). Research into Korean adults’ oral health also indicates a higher proportion of teeth requiring treatment or extraction with a decrease in age (64). Moreover, young adults are increasingly seeking orthodontic treatment to address malocclusion or aesthetic concerns (65). Cavities, periodontal disease, tooth loss, and malocclusion can all affect oral health and cause chewing difficulties. Chewing difficulties are also associated with emotions and can diminish individuals’ willingness to participate in various activities (66), leading to depression and stress (67, 68). Notably, individuals experiencing chewing problems have been shown to exhibit a progressively higher risk of depressive symptoms, indicating that such difficulties may have a stronger association with moderate to severe depression than with mild symptoms (69). Given that most oral health projects are focused on the older adult or children, policies aimed specifically at improving young adults’ oral health are required.
In this study, we proposed a hybrid ML approach to address the limitations of other statistical analysis methods. Traditional methods identify important variables for analyzing risk factors of specific diseases based on medical knowledge, theoretical background, and literature reviews. However, the process of variable selection based on theoretical grounds cannot wholly exclude subjectivity (70). As an alternative, ML-based feature selection methods have been suggested (71) and used in several recent studies (72, 73). ML-based methods efficiently extract the most relevant features when analyzing various variables from a large dataset (74) but tend to be more complex and less interpretable than more traditional approaches (75). While they are useful for evaluating variables that are not predicted by traditional modeling, their ability to show the direction of association is limited (76). Using a combination of both methods can facilitate the exploration of influencing factors and effectively analyze their impact. Russel et al. (77) found that feature selection complemented logistic regression and identified new variables, demonstrating its value when used with traditional statistical methods. In this study, we compared models based on a literature review and ML feature selection to identify factors not previously considered in the literature.
4.1 Limitations
This study is significant in that it applied exploratory analysis to a nationwide representative sample to identify the factors affecting young adults’ mental health across a wide range of categories. Nevertheless, there are limitations to mention. First, as a cross-sectional study that used data from the CHS, it is difficult to identify the causal relationship between the selected variables and mental health. Second, self-reported mental health status and other variables (health behaviors, etc.) are susceptible to recall and social biases and thus may not provide accurate information. Finally, the findings should be interpreted with caution, as the data are derived from a specific sociocultural setting, limiting their generalizability to other populations with different cultural backgrounds.
5 Conclusion
We applied a hybrid ML/traditional statistics methodology to identify and explore the factors influencing young adults’ mental health in light of recent environmental and lifestyle changes. Unmet medical needs, chewing difficulties, and the number of accidents and addiction experiences were newly derived key factors. We confirmed the effects of these factors that have previously largely been overlooked. This work emphasizes the need to establish policies aimed at managing young adults’ mental health by continuously monitoring the influencing factors in a rapidly changing environment.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found at: Korea Disease Control and Prevention Agency.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the [patients/participants OR patients/participants legal guardian/next of kin] was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
NP: Writing – original draft, Writing – review & editing. HW: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by a 2024 research grant from Kongju National University (KNU) and the National Research Foundation (NRF) of Korea grant funded by the Korea government (MSIT) (RS-2024-00350688).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1562280/full#supplementary-material
References
1. World Health Organization. Depression and other common mental disorders: Global health estimates. Geneva: World Health Organization (2017).
2. Santomauro, DF, Herrera, AMM, Shadid, J, Zheng, P, Ashbaugh, C, Pigott, DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12. doi: 10.1016/S0140-6736(21)02143-7
3. Yoch, M, and Sirull, R In: Institute for Health Metrics and Evaluation, editor. New global burden of disease analyses show depression and anxiety among the top causes of health loss worldwide, and a significant increase due to the COVID-19 pandemic. Seattle: Institute for Health Metrics and Evaluation. (2021)
4. Schwartz, SJ, and Petrova, M. Prevention science in emerging adulthood: a field coming of age. Prev Sci. (2019) 20:305–9. doi: 10.1007/s11121-019-0975-0
5. Dijk, H, and Mierau, J. Mental health over the life course: evidence for a U-shape? Health Econ. (2023) 32:155–74. doi: 10.1002/hec.4614
6. Massetti, GM, Thomas, CC, King, J, Ragan, K, and Lunsford, NB. Mental health problems and cancer risk factors among young adults. Am J Prev Med. (2017) 53:S30–9. doi: 10.1016/j.amepre.2017.04.023
7. Reinherz, HZ, Paradis, AD, Giaconia, RM, Stashwick, CK, and Fitzmaurice, G. Childhood and adolescent predictors of major depression in the transition to adulthood. Am J Psychiatry. (2003) 160:2141–7. doi: 10.1176/appi.ajp.160.12.2141
8. Kessler, RC, Berglund, P, Demler, O, Jin, R, Merikangas, KR, and Walters, EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. (2005) 62:593–602. doi: 10.1001/archpsyc.62.6.593
9. Oliver, JM, Reed, CKS, Katz, BM, and Haugh, JA. Students' self-reports of help-seeking: the impact of psychological problems, stress, and demographic variables on utilization of formal and informal support. Soc Behav Pers. (1999) 27:109–28. doi: 10.2224/sbp.1999.27.2.109
10. Newman, DL, Moffitt, TE, Caspi, A, Magdol, L, Silva, PA, and Stanton, WR. Psychiatric disorder in a birth cohort of young adults: prevalence, comorbidity, clinical significance, and new case incidence from ages 11 to 21. J Consult Clin Psychol. (1996) 64:552–62. doi: 10.1037/0022-006X.64.3.552
11. Schulte-Körne, G. Mental health problems in a school setting in children and adolescents. Dtsch Arztebl Int. (2016) 113:183. doi: 10.3238/arztebl.2016.0183
12. Lachman, ME. Development in midlife. Annu Rev Psychol. (2004) 55:305–31. doi: 10.1146/annurev.psych.55.090902.141521
13. Antonucci, TC, Ajrouch, KJ, and Birditt, KS. The convoy model: explaining social relations from a multidisciplinary perspective. The Gerontologist. (2014) 54:82–92. doi: 10.1093/geront/gnt118
14. Walther, J, Aldrian, U, Stüger, HP, Kiefer, I, and Ekmekcioglu, C. Nutrition, lifestyle factors, and mental health in adolescents and young adults living in Austria. Int J Adolesc Med Health. (2014) 26:377–86. doi: 10.1515/ijamh-2013-0310
15. Lubans, D, Richards, J, Hillman, C, Faulkner, G, Beauchamp, M, Nilsson, M, et al. Physical activity for cognitive and mental health in youth: a systematic review of mechanisms. Pediatrics. (2016) 138:1642. doi: 10.1542/peds.2016-1642
16. Canivet, C, Bodin, T, Emmelin, M, Toivanen, S, Moghaddassi, M, and Östergren, P-O. Precarious employment is a risk factor for poor mental health in young individuals in Sweden: a cohort study with multiple follow-ups. BMC Public Health. (2016) 16:1–10. doi: 10.1186/s12889-016-3358-5
17. Pedrelli, P, Nyer, M, Yeung, A, Zulauf, C, and Wilens, T. College students: mental health problems and treatment considerations. Acad Psychiatry. (2015) 39:503–11. doi: 10.1007/s40596-014-0205-9
18. Patel, V, Flisher, AJ, Hetrick, S, and McGorry, P. Mental health of young people: a global public-health challenge. Lancet. (2007) 369:1302–13. doi: 10.1016/S0140-6736(07)60368-7
19. Caputo, J. Parental coresidence, young adult role, economic, and health changes, and psychological well-being. Soc Ment Health. (2020) 10:199–217. doi: 10.1177/2156869318812008
20. Pedersen, ER, and Paves, AP. Comparing perceived public stigma and personal stigma of mental health treatment seeking in a young adult sample. Psychiatry Res. (2014) 219:143–50. doi: 10.1016/j.psychres.2014.05.017
21. Johnstad, PG. Unhealthy behaviors associated with mental health disorders: a systematic comparative review of diet quality, sedentary behavior, and cannabis and tobacco use. Front Public Health. (2023) 11:1268339. doi: 10.3389/fpubh.2023.1268339
22. Gariépy, G, Danna, SM, Hawke, L, Henderson, J, and Iyer, SN. The mental health of young people who are not in education, employment, or training: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. (2022) 57:1–15. doi: 10.1007/s00127-021-02212-8
23. Mindell, DA, and Reynolds, E. The work of the future: Building better jobs in an age of intelligent machines. Cambridge (MA): MIT Press. (2022) doi: 10.7551/mitpress/14109.001.0001
24. Berryman, C, Ferguson, CJ, and Negy, C. Social media use and mental health among young adults. Psychiatry Q. (2018) 89:307–14. doi: 10.1007/s11126-017-9535-6
25. Kulkova, I. Socio-cultural consequences of population adaptation towards dynamic development caused by digitalization. Digital Transformation and New Challenges. Cham: Springer; (2021). 157–166.
26. Graham, S, Depp, C, Lee, EE, Nebeker, C, Tu, X, Kim, HC, et al. Artificial intelligence for mental health and mental illnesses: an overview. Curr Psychiatry Rep. (2019) 21:116. doi: 10.1007/s11920-019-1094-0
27. Su, C, Xu, Z, Pathak, J, and Wang, F. Deep learning in mental health outcome research: a scoping review. Transl Psychiatry. (2020) 10:116. doi: 10.1038/s41398-020-0780-3
28. Baba, A, and Bunji, K. Prediction of mental health problem using annual student health survey: machine learning approach. JMIR Ment Health. (2023) 10:e42420. doi: 10.2196/42420
29. Al-Shamiri, AYR, ed. (2021) Employing machine learning algorithms to discover risk factors of glaucoma. 4th International Conference on Pattern Recognition and Artificial Intelligence (PRAI); IEEE.
30. Kolyshkina, I, and Simoff, S. Interpretability of machine learning solutions in public healthcare: the CRISP-ML approach. Front Big Data. (2021) 4:660206. doi: 10.3389/fdata.2021.660206
31. Ahmad, HF, Mukhtar, H, Alaqail, H, Seliaman, M, and Alhumam, A. Investigating health-related features and their impact on the prediction of diabetes using machine learning. Appl Sci. (2021) 11:1173. doi: 10.3390/app11031173
32. McEligot, AJ, Poynor, V, Sharma, R, and Panangadan, A. Logistic LASSO regression for dietary intakes and breast cancer. Nutrients. (2020) 12:2652. doi: 10.3390/nu12092652
33. Tibshirani, R. Regression shrinkage and selection via the lasso. J R Stat Soc Series B Stat Methodol. (1996) 58:267–88. doi: 10.1111/j.2517-6161.1996.tb02080.x
34. Pedrelli, P, Shapero, B, Archibald, A, and Dale, C. Alcohol use and depression during adolescence and young adulthood: a summary and interpretation of mixed findings. Curr Addict Rep. (2016) 3:91–7. doi: 10.1007/s40429-016-0084-0
35. Aschbrenner, KA, Naslund, JA, Salwen-Deremer, JK, Browne, J, Bartels, SJ, Wolfe, RS, et al. Sleep quality and its relationship to mental health, physical health and health behaviours among young adults with serious mental illness enrolled in a lifestyle intervention trial. Early Interv Psychiatry. (2022) 16:106–10. doi: 10.1111/eip.13129
36. Mokrue, K, and Acri, MC. Subjective health and health behaviors as predictors of symptoms of depression and anxiety among ethnic minority college students. Soc Work Ment Health. (2015) 13:186–200. doi: 10.1080/15332985.2014.911238
37. Wickham, SR, Amarasekara, NA, Bartonicek, A, and Conner, TS. The big three health behaviors and mental health and well-being among Young adults: a cross-sectional investigation of sleep, exercise, and diet. Front Psychol. (2020) 11:579205. doi: 10.3389/fpsyg.2020.579205
38. Jung, B, and Ha, I-H. Determining the reasons for unmet healthcare needs in South Korea: a secondary data analysis. Health Qual Life Outcomes. (2021) 19:1–17. doi: 10.1186/s12955-021-01737-5
39. Nelson, CH, and Park, J. The nature and correlates of unmet health care needs in Ontario, Canada. Soc Sci Med. (2006) 62:2291–300. doi: 10.1016/j.socscimed.2005.10.014
40. Marshall, EG. Do young adults have unmet healthcare needs? J Adolesc Health. (2011) 49:490–7. doi: 10.1016/j.jadohealth.2011.03.005
42. Lupton, D. Young people’s use of digital health technologies in the global north: narrative review. J Med Internet Res. (2021) 23:e18286. doi: 10.2196/18286
43. Huh, S, and Kim, S. Unmet needs for health care among Korean adults: differences across age groups. Korean J Health Econ Policy. (2007) 13:1–16.
44. Moret, L, Nguyen, JM, Volteau, C, Falissard, B, Lombrail, P, and Gasquet, I. Evidence of a non-linear influence of patient age on satisfaction with hospital care. Int J Qual Health Care. (2007) 19:382–9. doi: 10.1093/intqhc/mzm041
45. Bo Kyung, K, Jeong Ho, S, and Dong Wook, L. Factors associated with depression in Korean young adults: analysis based on the 2018 Korea national health and nutrition examination survey. Korean J Fam Pract. (2021) 11:296–303. doi: 10.21215/kjfp.2021.11.4.296
46. Breslau, N, Kessler, RC, Chilcoat, HD, Schultz, LR, Davis, GC, and Andreski, P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit area survey of trauma. Arch Gen Psychiatry. (1998) 55:626–32. doi: 10.1001/archpsyc.55.7.626
47. Difino, M, Bini, R, Reitano, E, Faccincani, R, Sammartano, F, Briani, L, et al. Epidemiology of trauma admissions in a level 1 trauma center in northern Italy: a nine-year study. Updat Surg. (2021) 73:1963–73. doi: 10.1007/s13304-021-00991-y
48. Harna, B, Arya, S, and Bahl, A. Epidemiology of trauma patients admitted to a trauma center in New Delhi, India. Ind J Crit Care Med. (2020) 24:1193–7. doi: 10.5005/jp-journals-10071-23605
49. Paat, Y-F, and Markham, C. Digital crime, trauma, and abuse: internet safety and cyber risks for adolescents and emerging adults in the 21st century. Soc Work Ment Health. (2021) 19:18–40. doi: 10.1080/15332985.2020.1845281
50. Flory, JD, and Yehuda, R. Comorbidity between post-traumatic stress disorder and major depressive disorder: alternative explanations and treatment considerations. Dialogues Clin Neurosci. (2015) 17:141–50. doi: 10.31887/DCNS.2015.17.2/jflory
51. Olatunji, BO, Cisler, JM, and Tolin, DF. Quality of life in the anxiety disorders: a meta-analytic review. Clin Psychol Rev. (2007) 27:572–81. doi: 10.1016/j.cpr.2007.01.015
52. Krysinska, K, and Lester, D. Post-traumatic stress disorder and suicide risk: a systematic review. Arch Suicide Res. (2010) 14:1–23. doi: 10.1080/13811110903478997
53. Lewis, SJ, Arseneault, L, Caspi, A, Fisher, HL, Matthews, T, Moffitt, TE, et al. The epidemiology of trauma and post-traumatic stress disorder in a representative cohort of young people in England and Wales. Lancet Psychiatry. (2019) 6:247–56. doi: 10.1016/S2215-0366(19)30031-8
54. Esmaeelzadeh, S, Moraros, J, Thorpe, L, and Bird, Y. Examining the association and directionality between mental health disorders and substance use among adolescents and Young adults in the U.S. and Canada-a systematic review and Meta-analysis. J Clin Med. (2018) 7:543. doi: 10.3390/jcm7120543
55. Kim, S, Weekes, J, Young, MM, Adams, N, and Kolla, NJ. Trends of repeated emergency department visits among adolescents and young adults for substance use: a repeated cross-sectional study. PLoS One. (2023) 18:e0282056. doi: 10.1371/journal.pone.0282056
56. Fleming, CB, Ramirez, JJ, Rhew, IC, Hultgren, BA, Hanson, KG, Larimer, ME, et al. Trends in alcohol, cigarette, e-cigarette, and non-prescribed pain reliever use among young adults in Washington state after legalization of nonmedical cannabis. J Adolesc Health. (2022) 71:47–54. doi: 10.1016/j.jadohealth.2022.03.006
57. Oksanen, A, Miller, BL, Savolainen, I, Sirola, A, Demant, J, Kaakinen, M, et al. Social media and access to drugs online: a nationwide study in the United States and Spain among adolescents and young adults. Eur. J. Psychol. Appl. Legal Context. (2021) 13:29–36. doi: 10.5093/ejpalc2021a5
58. Degenhardt, L, and Hall, W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet. (2012) 379:55–70. doi: 10.1016/S0140-6736(11)61138-0
59. Fleming, CB, Duckworth, JC, Rhew, IC, Abdallah, DA, Guttmannova, K, Patrick, ME, et al. Young adult simultaneous alcohol and marijuana use: between- and within-person associations with negative alcohol-related consequences, mental health, and general health across two-years. Addict Behav. (2021) 123:107079. doi: 10.1016/j.addbeh.2021.107079
60. Tavolacci, MP, Ladner, J, Grigioni, S, Richard, L, Villet, H, and Dechelotte, P. Prevalence and association of perceived stress, substance use and behavioral addictions: a cross-sectional study among university students in France, 2009–2011. BMC Public Health. (2013) 13:1–8. doi: 10.1186/1471-2458-13-724
61. Low, NC, Dugas, E, O’Loughlin, E, Rodriguez, D, Contreras, G, Chaiton, M, et al. Common stressful life events and difficulties are associated with mental health symptoms and substance use in young adolescents. BMC Psychiatry. (2012) 12:1–10. doi: 10.1186/1471-244X-12-116
62. Ji, m g. A study on the activity limitation realities caused by oral disease in some university students. J Korea Inst Electron Commun Sci. (2013) 8:371–8. doi: 10.13067/JKIECS.2013.8.2.371
63. Ministry of Health and Welfare. Korea health statistics 2018: Korea national health and nutrition examination survey (KNHANES VII-3). Sejong: Ministry of Health and Welfare (2019).
64. Jin-Ah, J, Jin, K, and Mi-Gyung, S. The effect of oral health status and oral health behaviors on depression and stress awareness in Korean adults: the 8th Korea national health and nutrition examination survey (2019). Health Welfare. (2021) 23:137–58. doi: 10.23948/kshw.2021.9.23.3.137
65. Bagga, DK. Adult orthodontics versus adolescent orthodontics: an overview. J Oral Health Community Dent. (2010) 4:42–7. doi: 10.5005/johcd-4-2-42
66. Back, J-U, and Park, M-H. Ability for chewing a social activity and connection with the life function of a senior citizen. J Technologic Dent. (2007) 29:87–103.
67. Kim, YS, Kim, HN, Lee, JH, Kim, SY, Jun, EJ, and Kim, JB. Association of stress, depression, and suicidal ideation with subjective oral health status and oral functions in Korean adults aged 35 years or more. BMC Oral Health. (2017) 17:101. doi: 10.1186/s12903-017-0391-4
68. Hwang, SH, Park, SG, and Min, JY. Relationship between chewing ability and depressive symptoms. Community Dent Health. (2013) 30:254–6.
69. Lee, E-S, and Do, K-Y. Association between chewing problems and depression in Korean adults. J Korean Soc Dent Hyg. (2019) 19:753–63. doi: 10.13065/jksdh.20190064
70. Greenland, S, Daniel, R, and Pearce, N. Outcome modelling strategies in epidemiology: traditional methods and basic alternatives. Int J Epidemiol. (2016) 45:565–75. doi: 10.1093/ije/dyw040
71. Breiman, L. Heuristics of instability and stabilization in model selection. Ann Stat. (1996) 24:2350–83. doi: 10.1214/aos/1032181158
72. De La Garza, ÁG, Blanco, C, Olfson, M, and Wall, MM. Identification of suicide attempt risk factors in a national US survey using machine learning. JAMA Psychiatr. (2021) 78:398–406. doi: 10.1001/jamapsychiatry.2020.4165
73. Huang, AA, and Huang, SY. Use of machine learning to identify risk factors for insomnia. PLoS One. (2023) 18:e0282622. doi: 10.1371/journal.pone.0282622
74. Ghosh, P, Azam, S, Jonkman, M, Karim, A, Shamrat, FJM, Ignatious, E, et al. Efficient prediction of cardiovascular disease using machine learning algorithms with relief and LASSO feature selection techniques. IEEE Access. (2021) 9:19304–26. doi: 10.1109/ACCESS.2021.3053759
75. Beam, AL, and Kohane, IS. Big data and machine learning in health care. JAMA. (2018) 319:1317–8. doi: 10.1001/jama.2017.18391
76. Tran, V, Saad, T, Tesfaye, M, Walelign, S, Wordofa, M, Abera, D, et al. Helicobacter pylori (H. pylori) risk factor analysis and prevalence prediction: a machine learning-based approach. BMC Infect Dis. (2022) 22:655. doi: 10.1186/s12879-022-07625-7
Keywords: young adult, mental health, depression, subjective stress, machine learning
Citation: Park N and Woo H (2025) Change in lifestyle and mental health in young adults: an exploratory study with hybrid machine learning. Front. Public Health. 13:1562280. doi: 10.3389/fpubh.2025.1562280
Edited by:
Xiao Yang, Sichuan University, ChinaReviewed by:
Isidora S. Vujcic, University of Belgrade, SerbiaCarlos Aníbal Martínez Martínez, National Autonomous University of Honduras, Honduras
Copyright © 2025 Park and Woo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hyekyung Woo, aGt3b29Aa29uZ2p1LmFjLmty
 Nayoung Park
Nayoung Park Hyekyung Woo
Hyekyung Woo