- 1College of Public Health, Chongqing Medical University, Chongqing, China
- 2Nanan District Center for Disease Control and Prevention, Chongqing, China
- 3College of Exercise Medicine, Chongqing Medical University, Chongqing, China
Background: This study aims to explore the relationship between sleep duration and Activity of Daily Living (ADL) disability among older adults in China. ADL disability severely impacts the quality of life of older adults and is associated with various physical and mental health issues. With the aging population in China, the burden of ADL disability is increasing.
Methods: Data were sourced from the 2018 national follow-up of the Chinese Longitudinal Healthy Longevity Survey (CLHLS), including 9,572 participants aged 65 and above. Sleep duration was assessed via self-reported questionnaire and categorized into short (<7 h), medium (7–8 h), and long (≥9 h). ADL disability was evaluated through Basic Activities of Daily Living (BADL) and Instrumental Activities of Daily Living (IADL). Logistic regression models were used to analyze the relationship between sleep duration and ADL disability, with subgroup analyses conducted to explore differences by gender and physical activity.
Results: The study found a significant non-linear relationship between sleep duration and ADL disability. Compared to older adults with a sleep duration of 7–8 h, those with over 9 h of sleep had a significantly higher risk of BADL and IADL disability (OR = 1.36, OR = 1.35). Subgroup analyses indicated that this relationship existed among older adults of different genders, age, and physical activity levels.
Conclusion: For older adults in China, maintaining a sleep duration of 7–8 h may be an effective strategy for preventing ADL disability. Both excessively long and short sleep duration are associated with an increased risk of ADL disability in this population.
1 Introduction
Activities of Daily Living (ADL) refer to the basic competencies required for individuals to independently care for themselves, including dressing, eating, and bathing (1). ADL disability is a significant health issue that can lead to decreased quality of life and heightened vulnerability to the surrounding environment (2). Presently, ADL disability is primarily evaluated through Basic Activities of Daily Living (BADL) and Instrumental Activities of Daily Living (IADL) (3, 4). Existing research has demonstrated that ADL disability is strongly associated with physical and mental health issues, including depression, cognitive impairment, frailty, and sarcopenia (5–7). Beyond this, demographic factors, lifestyle behaviors, and health conditions are also significantly linked with ADL disability (8–10). ADL disability not only severely affects the individual patient and family but also poses significant challenges to socio-economic development and the public health system (11). Currently, with the aging population, China is facing an increasing burden of ADL disability, which has become a significant public health issue. A study indicates that the prevalence of ADL disability among individuals aged 60 years and older in China is 23.8% (12). By 2026, the number of individuals aged 65 years and older with ADL disabilities is projected to reach 96.2 million (13). Therefore, to mitigate the burden of ADL disability on individuals, families, and society, it is crucial to identify its risk factors and implement corresponding preventive and intervention measures.
Sleep duration is a critical factor influencing the physical and mental health of older adults and is associated with increased risks of cognitive impairment, cardiovascular disease, type 2 diabetes, and sarcopenia, among others (14–17). Numerous studies have demonstrated a statistically significant ‘U-shaped’ or ‘J-shaped’ association between sleep duration and conditions such as cognitive impairment, depression, and various chronic diseases (18–24). This suggests that patients may face an elevated risk of cognitive impairment, depressive symptoms, and various chronic diseases when sleep duration is either too long or too short. Additionally, other studies have reported that patients experience accelerated cognitive decline when sleep duration is either too long or too short (21). Concurrently, it should be noted that differences in sleep duration requirements exist between age groups and genders, which means they are differently affected by sleep duration (25, 26).
Several previous studies have examined the relationship between sleep duration and ADL disability, but findings have been inconsistent. In 2015, the National Sleep Foundation suggested that the recommended amount of sleep for older adults is 7 to 8 h (27). A study based on the Guangxi Longevity Population Database reported that excessive sleep duration (greater than 12 h) is associated with an increased risk of ADL disability in the oldest population (older than 90 years), and that the optimal sleep duration for this population is 8 to 10 h (28). Luo et al. (29) and Zou et al. (30) demonstrated an association between sleep durations of less than 7 h or more than 7 h and an increased risk of ADL disability in individuals aged over 65 years. Meanwhile, Lee et al. (31) found that older adults with greater limitations in basic activities of daily living (BADL) and instrumental activities of daily living (IADL) experienced more difficulty achieving the recommended sleep duration. These inconsistent results may be attributed to differences in study populations, methods, and designs (17). Moreover, socio-economic, cultural, and ethnic factors may contribute to the heterogeneity observed among different countries or regions in this context (32). However, it is worth noting that current research on sleep duration and ADL disability in older adults remains limited, with insufficient exploration of BADL and IADL classifications. In addition, prior studies on the association between sleep duration and ADL disability in older adults have focused primarily on the overall older adult population, without adequately exploring differences in this association by factors such as gender and physical activity. Therefore, further exploration of the relationship between sleep duration and ADL disability in older adults is necessary to enrich the research in this area and provide a basis for future studies.
In summary, this study aimed to further explore the relationship between sleep duration and ADL disability in older adults, based on existing findings and using data from the Chinese Longitudinal Healthy Longevity Survey (CLHLS), to provide a scientific basis for future research and the development of prevention and intervention strategies for ADL disability in older adults.
2 Materials and methods
2.1 Participants
Data for this study were sourced from the Chinese Longitudinal Healthy Longevity Survey (CLHLS). The CLHLS is a national prospective longitudinal study organized by the Peking University Centre for Healthy Aging and Development (CHADS) to investigate issues related to aging. Since 1998, the CLHLS has conducted eight national surveys. More information can be found in other related topics (33).
National follow-up data from CLHLS 2018 were used in this study. To begin with, this study excluded participants with missing data on ADL disability (n = 892) and sleep duration (n = 1,610); in addition, participants with missing data on covariates were excluded (n = 3,729). Finally, participants aged under 65 years were excluded (n = 71). Ultimately, 9,572 participants were enrolled in this study. The detailed flowchart of participant inclusion and exclusion for this study is presented in Figure 1.
2.2 Assessment of sleep duration
Self-reported sleep duration data were obtained using the question, “How many hours of sleep do you currently get per day?” To better understand the relationship between sleep duration and ADL disability in older adults, this study categorized sleep duration into three groups: short (less than 7 h), medium (7 to 8 h), and long (9 h or more), based on the National Sleep Foundation criteria (27).
2.3 Assessment of ADL disability
Participants’ ADL disability status can be assessed through the BADL or IADL. BADL in the CLHLS comprises six items: (1) bathing; (2) eating; (3) dressing; (4) indoor transfers; (5) toileting; (6) incontinence control. IADL comprises eight items: (1) Can you go to your neighbor’s house alone? (2) Can you go out shopping alone? (3) Can you cook alone if needed? (4) Can you do laundry alone if needed? (5) Can you walk 2 miles continuously? (6) Can you lift about 10 pounds (5 kg)? (7) Can you squat down and stand up three times in a row? (8) Can you travel alone on public transport? Participants were considered to have ADL disability if they were unable to perform one or more of the 14 items independently.
2.4 Covariates
In order to obtain more reliable results, we included the following covariates that may affect activities of daily living disability based on available references: age (65 to 74, 75 to 89, 90 years or older), gender (male, female), residence (city, town, rural), currently smoking (yes, no), currently drinking (yes, no), marital status (married, unmarried/separated/widowed), physical exercise (yes, no), BMI (obese, overweight, normal, underweight), depression (yes, no), and cognitive impairment (yes, no) (34, 35). Assessment criteria for depression and cognitive impairment are detailed in Supplementary Tables S1, S2.
2.5 Ethical considerations
Data for this study were sourced from the CLHLS and used in accordance with the Declaration of Helsinki. Ethical approval was obtained from the Biomedical Ethics Committee of Peking University (IRB00001052-13074) (36). Participants and their families have signed an informed consent form.
2.6 Statistical analysis
Statistical analyses of the study were performed using Stata version 18.0 and R version 4.4.1. GraphPad Prism version 9.0 was used to visualize the results of the subgroup analyses. Descriptive statistics were used to summarize the baseline characteristics of the study population. Logistic models were used to estimate the risk ratio (OR) and its corresponding 95% confidence interval (CI) for the association between sleep duration and disability in activities of daily living in older adults. Restricted cubic spline bars were plotted to explore potential non-linear relationships between sleep duration and ADL disability. The Akaike Information Criterion (AIC) was applied to determine the optimal number of knots for the spline. Wald’s test assessed the linearity of the observed relationship. Model 1 was a crude model. Model 2 is adjusted for age, gender, residence, smoking, drinking, marital status, physical exercise, and BMI. Model 3 further adjusted for depression and cognitive impairment based on Model 2. Subgroup analyses based on Model 3 were conducted to examine potential differences in the correlation between sleep duration and ADL disability across gender, age, and physical exercise groups. Statistical significance was set at p < 0.05 for two-sided tests.
3 Results
3.1 Baseline characteristics
This study included 9,572 participants, with 4,575 males (47.8%) and 4,997 females (52.2%). The majority of older adult participants resided in rural areas (43.7%). Among the participants, the largest group (38.3%) reported sleeping 7 to 8 h per day, followed by those who slept less than 7 h (37.8%). In contrast, the smallest proportion (23.9%) reported sleeping more than 9 h. The survey results showed that 1,482 participants (15.5%) experienced BADL disability, and 5,552 participants (58.0%) had IADL disability. The 2018 CLHLS data showed that ADL had good internal consistency, with a Cronbach’s alpha of 0.82.
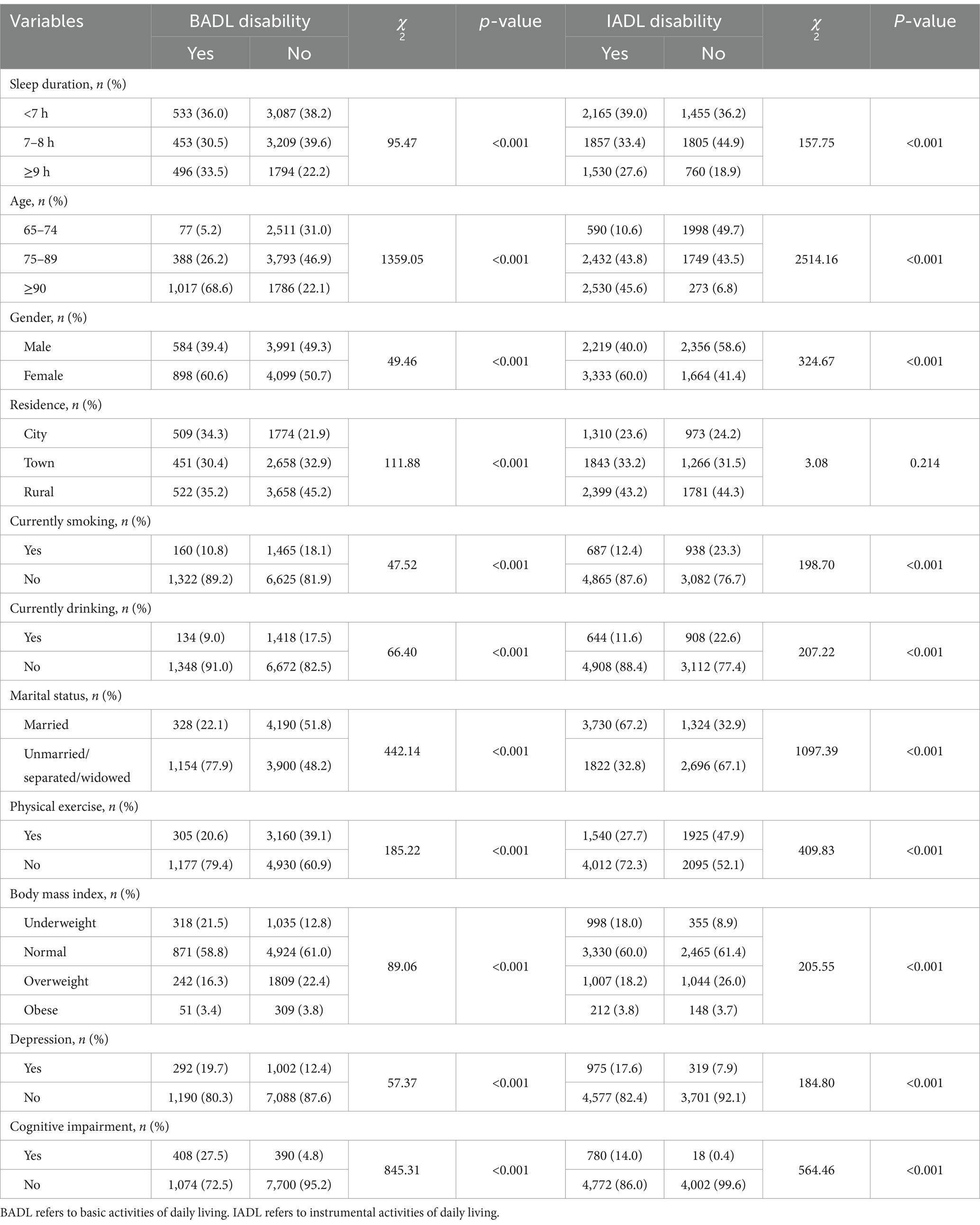
In this study, significant differences in BADL and IADL were found between groups of older adult participants with different sleep durations, ages, genders, smoking, drinking, marital status, physical exercise, BMI, depression, and cognitive impairment (p < 0.05). All these associations were statistically significant at the p < 0.05 level, as detailed in Table 1.
3.2 Association of sleep duration with disability in activities of daily living
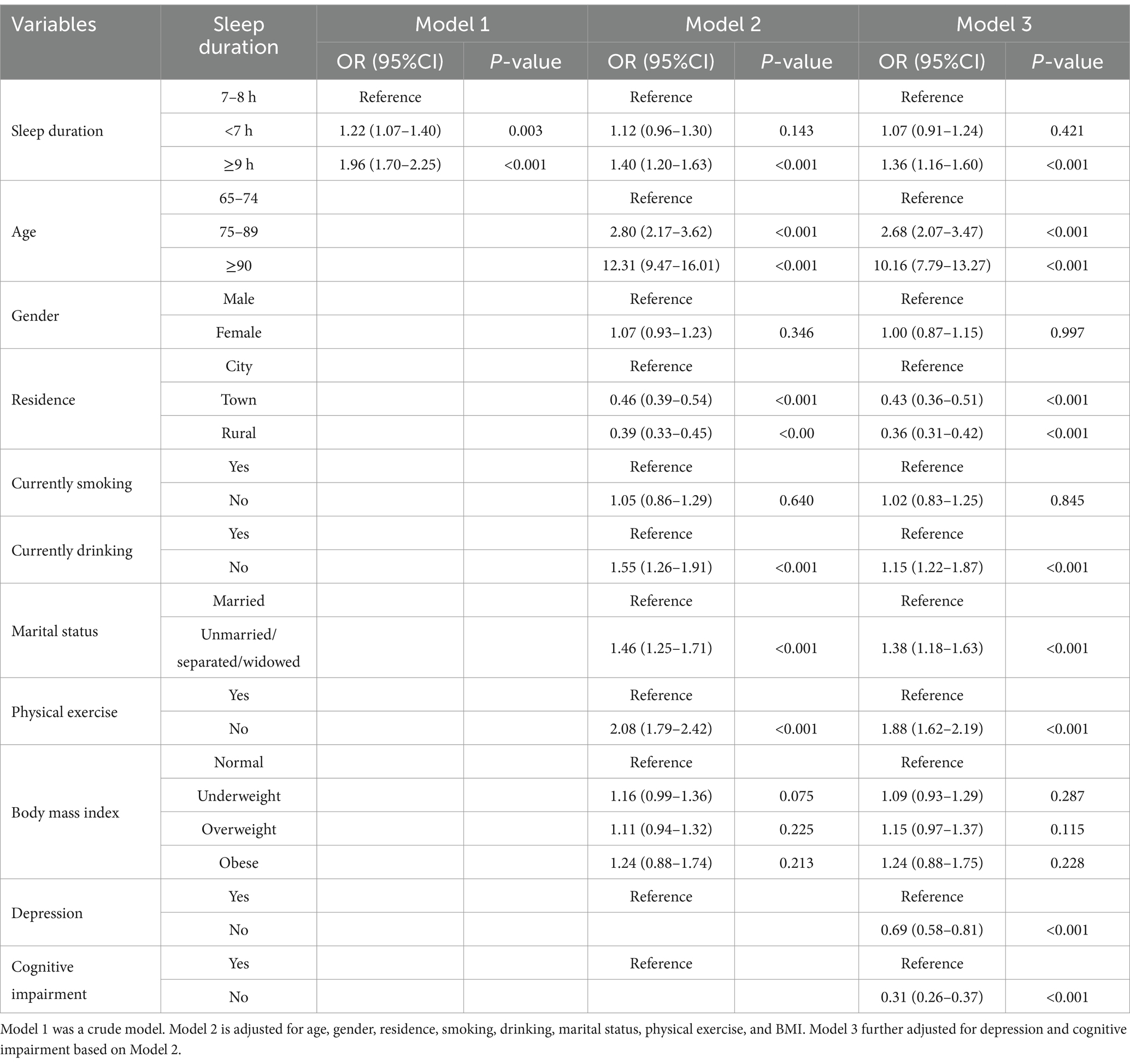
Figure 2 demonstrates a significant statistical association between sleep duration and both Basic Activities of Daily Living (BADL) and Instrumental Activities of Daily Living (IADL) (p < 0.001). A non-linear relationship is observed between sleep duration and BADL or IADL (p < 0.001). In Model 1 (shown in Table 2), compared to individuals with 7–8 h of sleep, those with less than 7 h and more than 9 h of sleep have a significantly higher risk of BADL disability (OR = 1.22, p = 0.003; OR = 1.96, p < 0.001). In Model 3, after adjusting for all covariates, compared to those with 7–8 h of sleep, the risk of BADL disability in individuals with less than 7 h of sleep is no longer statistically significant (p = 0.421), while those with more than 9 h of sleep still exhibit a higher risk of BADL disability (OR = 1.36, p < 0.001). Similarly, in Model 1 (Supplementary Table S4), individuals with less than 7 h and more than 9 h of sleep have a significantly higher risk of IADL disability (OR = 1.45, p < 0.001; OR = 1.96, p < 0.001). In Model 3, the risk of IADL disability remains significantly higher in those with less than 7 h and more than 9 h of sleep (OR = 1.17, p = 0.007; OR = 1.35, p < 0.001).
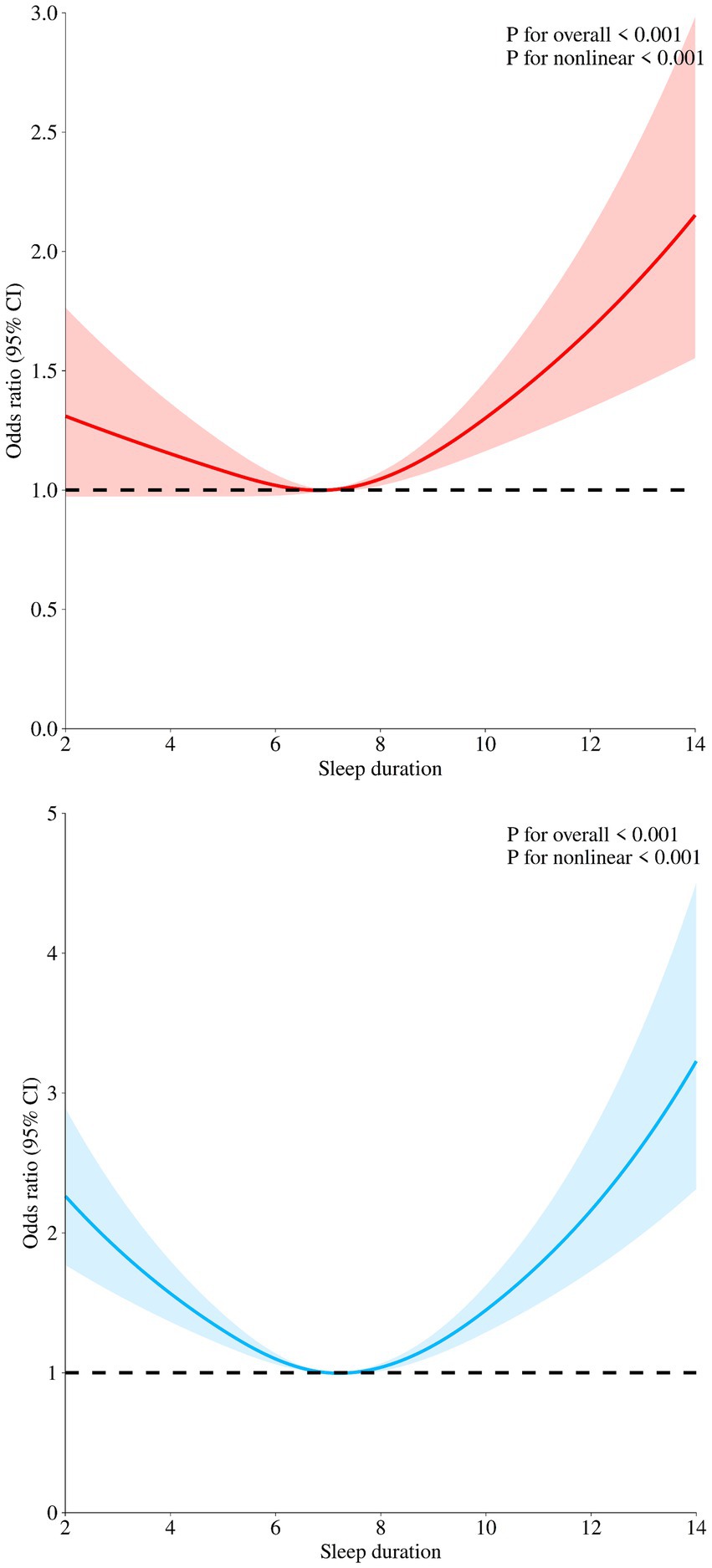
Figure 2. Restricted cubic spline regression analysis for sleep duration and BADL and IADL. The red curve indicates the association between sleep duration and BADL in older adults. The blue curve indicates the association between sleep duration and IADL in older adults.
3.3 Subgroup analysis of sleep duration and disability in activities of daily living
To further explore the association between sleep duration and ADL disability in older adult individuals with different gender, physical exercise, and age levels, we conducted subgroup analyses based on gender, physical exercise, and age (as shown in Figures 3, 4 and Supplementary Figure S1). The results indicated that, compared to older adult individuals with 7–8 h of sleep, those with sleep durations of 9 h or more had a higher risk of IADL and BADL disability, regardless of whether they were male or female participants. Among older adult individuals who engage in physical exercise, no significant difference in the risk of BADL and IADL disability was observed between those who slept less than 7 h and those who slept 7–8 h (p = 0.202, p = 0.748).
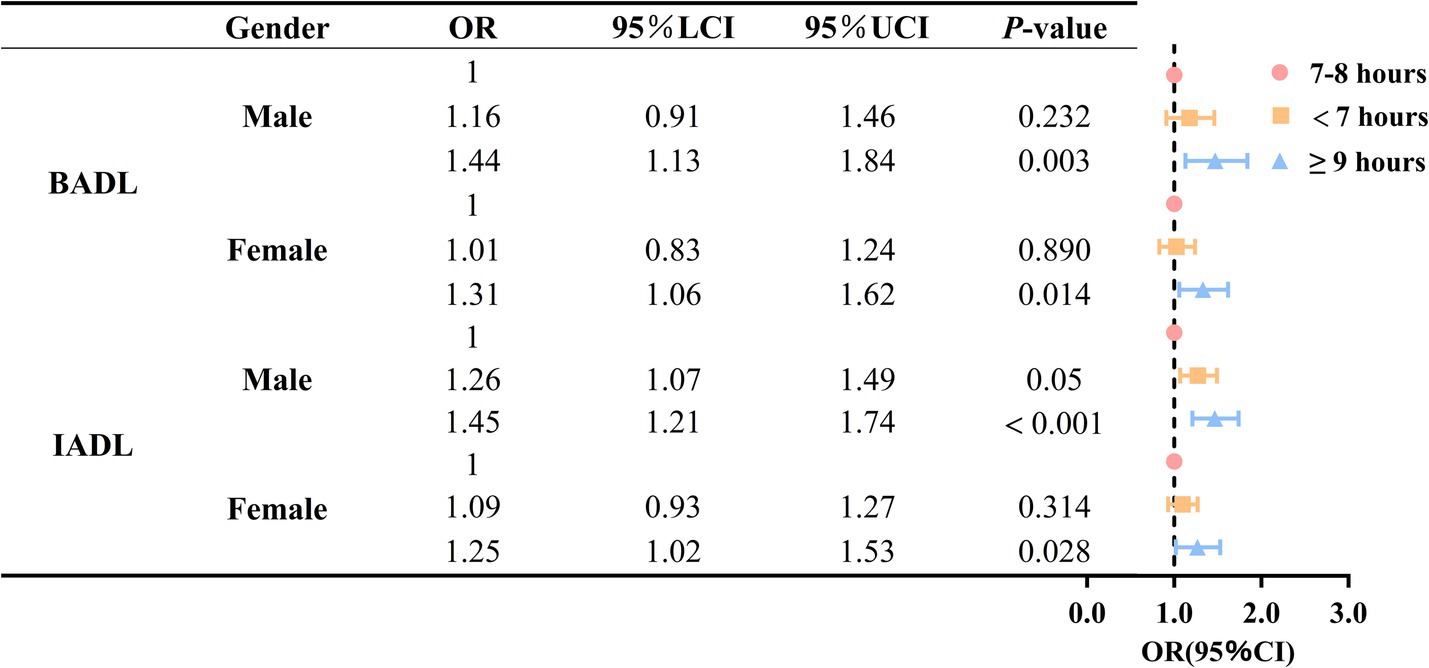
Figure 3. Association between sleep duration and disability in activities of daily living based on gender stratification.
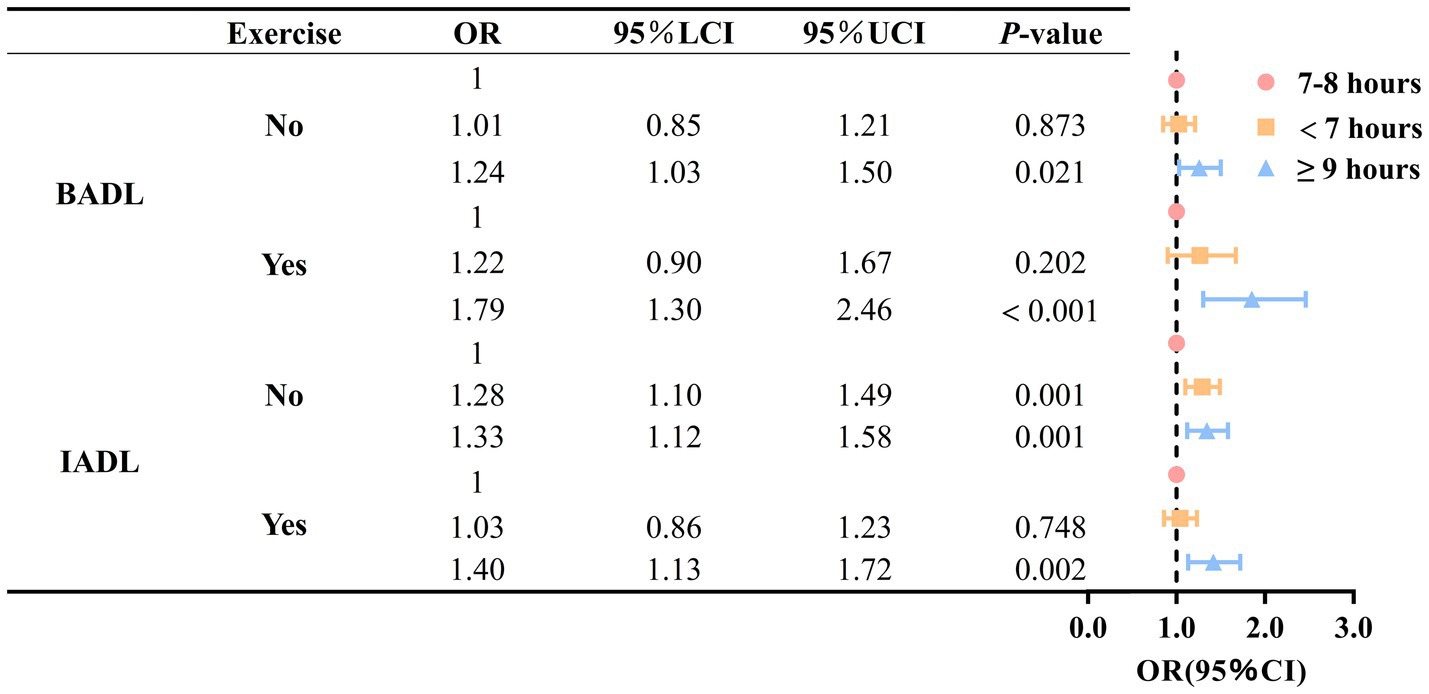
Figure 4. Association between sleep duration and disability in activities of daily living based on physical activity stratification.
4 Discussion
This study examined the association between sleep duration and ADL disability in older adults. The results of the study demonstrated a non-linear relationship between sleep duration and BADL and IADL disability in older adults. For older adults, 7–8 h of sleep is optimal, and either too long or too short a sleep duration is associated with an increased risk of ADL disability. Previous studies have demonstrated that BADL and IADL disabilities are significant risk factors for older adults who struggle to meet the recommended sleep duration (31). Thus, a bidirectional relationship may exist between sleep duration and ADL disability in older adults. Additionally, the association between sleep duration and ADL disability varied by gender and physical exercise. Specifically, when sleep duration is 9 h or more, older men exhibited a greater proportion of the increased risk of BADL disability compared to older women. When sleep duration was either too long or too short, the proportion of ADL disability risk increased more among older adults who engaged in physical exercise than among those who did not.
Our study demonstrated a U-shaped relationship between sleep duration and ADL disability in older adults, with both shorter and longer sleep durations than optimal being associated with an increased risk of ADL disability. Multiple physical and psychological risk factors may mediate this association, including depressive symptoms, cognitive impairment, and chronic diseases like cardiovascular disease and diabetes. Depressive symptoms are more common in older adults (37, 38). Yan et al. reported that ADL disability is strongly associated with depressive symptoms in older adults (39, 40). Older adults with depressive symptoms are more likely to experience physical dysfunction and ADL disability, which may in turn contribute to the development of depressive symptoms (40). Concurrently, sleep duration also demonstrates a bidirectional relationship with depressive symptoms (41). In this context, an optimal sleep duration of 8 h reduces the risk of depression, whereas both prolonged and shortened sleep durations increase this risk (42).
Cognitive impairment also plays an important role in this association. Several previous studies have demonstrated that cognitive decline directly impacts ADL ability in older adults, with this effect being particularly pronounced in those with dementia and cognitive loss (43, 44). Additionally, through a comprehensive analysis of two nationally representative aging cohorts, Ma et al. indicated a U-shaped relationship between sleep duration and cognitive functioning (45). Both shorter (6 h or less) and longer (8 h or more) sleep durations negatively affect cognitive performance in older adults, increasing the risk of cognitive impairment and dementia, particularly with extreme sleep durations of 4 h or less or 10 h or more per night (45, 46).
Furthermore, the role of various chronic diseases in the relationship between sleep duration and ADL disability in older adults is noteworthy. Existing studies indicate that chronic degenerative diseases (CDDs), including obesity, cardiovascular disease, diabetes, and inflammation, are among the primary causes of ADL disability in older adults (8, 47–49). A Polish study identified the comorbidity of chronic diseases as the primary risk factor for BADL disability in older adults, with the risk of BADL disability increasing as the number of coexisting chronic diseases rises (50). The pain caused by these chronic diseases may also limit physical activity, thus inducing IADL disability in older adults (50). Simultaneously, an association between sleep duration and chronic disease has been demonstrated. Dashti et al. (51) investigated the relationship between short sleep duration and chronic diseases, concluding that short sleep duration is associated with increased total calorie, fat, and protein intake, thereby contributing to chronic diseases such as obesity, type 2 diabetes, and cardiovascular disease. Simultaneously, the risk of certain chronic diseases also demonstrates a U-shaped relationship with sleep duration, where only an appropriate sleep duration can maintain a low risk, as seen in chronic kidney disease and various cardiovascular diseases (52–54). This appropriate sleep duration tends to be closer to the recommended time, between 6 and 9 h.
Subgroup analyses demonstrate the robustness of the study findings. Research shows that both long and short sleep times are associated with increased ADL disability risk in the older adult, regardless of gender, physical status, or age subgroup. Moreover, subgroup analyses revealed gender and physical exercise differences in the association between sleep duration and ADL disability in older adults. Firstly, when sleep duration is 9 h or more, older men exhibited a greater proportion of the increased risk of ADL disability compared to older women. This may be attributed to the physiological differences between men and women. Research indicates that women require more sleep than men (55, 56). Furthermore, as women are required to perform a significant portion of unpaid work (e.g., care for family members) in addition to paid work, they are more likely to experience sleep disorders and have lower sleep quality compared to men (55, 57). Therefore, appropriately extending sleep duration may improve their physical health while mitigating the adverse effects of prolonged sleep.
Secondly, when sleep duration was too long or too short, the increase in risk of ADL disability was more pronounced in older adults who were physically exercising compared to those who were not. This finding differs from previous studies that typically concluded older adults participating in physical exercise have a relatively low risk of ADL disability (58–61). This may be attributed to the fact that the CLHLS questionnaire, when assessing participants’ physical exercise, only indicates whether they are currently exercising, without evaluating the frequency or intensity of their physical exercise. Therefore, this subgroup analysis can only reflect the magnitude of the change in the risk of ADL disability in older adults caused by excessive or insufficient sleep duration, but not the intensity of the original risk or the intensity of the increase. The conclusion should thus be interpreted with caution. It may also be that older adults who participate in physical activity are in better physical condition, sleep better, and require less sleep than those who do not participate in physical activity. Therefore, sleeping too much may have a more pronounced effect on their increased risk of disability in daily mobility.
It is also worth noting that the distribution of sleep duration among Chinese older adults is distinct from other global regions. Our study found that the proportion of Chinese seniors with optimal sleep duration is lower than that in other global regions, while the proportion of those with short sleep duration is higher (62–65). This may be attributed to a range of factors including culture, lifestyle, social support systems, health behaviors, and psychological factors (66, 67). Simultaneously, this may also indicate that sleep duration has a greater influence on the risk of ADL disability in Chinese older adults than in those from other countries and regions. Based on these findings, future studies should focus more on Chinese older adults with short sleep duration.
Finally, current evidence indicates that patients’ sleep duration can be improved through pharmacotherapy, including benzodiazepines, antihistamines, etc. (68). Nevertheless, certain medications may heighten the risk of adverse effects in older adults, potentially compromising their ADL capacity (69). For instance, benzodiazepines may impair cognitive performance and neuromotor function in older adults (69, 70). Therefore, pharmacological interventions targeting adverse sleep duration in older adults must be exercised with caution. In addition, studies have shown that certain lifestyle habits related to health are associated with sleep duration, such as frequent alcohol use, heavy coffee intake, and bedtime mobile phone use (71). Thus, clinicians should prioritize non-pharmacological interventions in clinical practice and aim to improve patients’ sleep duration through behavioral or psychological interventions wherever feasible. Concurrently, policymakers should strive to promote healthy lifestyle habits and enhance public awareness of sleep hygiene through community-based health education.
5 Innovations and limitations
This study has several notable strengths. To begin with, the data used in this study are nationally representative; In addition, the study is clinically significant for maintaining the physical and mental health and self-care capacity of Chinese older adults. However, this study also has several limitations. First, the data used in this study were derived from a self-assessment questionnaire, which may introduce recall bias. Second, the cross-sectional design limits the exploration of causal relationships. Finally, the CLHLS database records only whether participants currently engage in physical exercise, without assessing the frequency or intensity of physical exercise, which may potentially confound the study results.
6 Conclusion
In conclusion, a sleep duration of 7–8 h seems to be optimal for Chinese older adults, and too long or too short a sleep duration is associated with an increased risk of ADL disability in this population. Maintaining a sleep duration of 7–8 h may be an effective strategy for preventing ADL disability in Chinese older adults.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number (s) can be found: https://opendata.pku.edu.cn/dataverse/CHADS.
Ethics statement
This study was based on publicly available datasets. Ethical review and approval was not required for the study, in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants in accordance with the national legislation and the institutional requirements.
Author contributions
DC: Conceptualization, Methodology, Software, Writing – original draft, Writing – review & editing. YZe: Conceptualization, Writing – original draft, Writing – review & editing. MC: Resources, Supervision, Writing – review & editing. YZh: Investigation, Methodology, Writing – review & editing. YQ: Supervision, Writing – review & editing. MY: Resources, Supervision, Writing – review & editing. XH: Funding acquisition, Resources, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Humanities and Social Sciences Research Program of Chongqing Municipal Education Commission [Grant no. 23SKGH042] and Chongqing Municipal Education Science Planning Project (2024 Teaching Reform Research Specialized Key Project, Research on Students’ Health Literacy Enhancement Path in the New Era with the Collaboration of Family, School, and Society [Grant no. K24ZG2040059]).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1580101/full#supplementary-material
References
1. Li, J, Lin, S, Yan, X, Pei, L, and Wang, Z. Adverse childhood experiences and trajectories of ADL disability among middle-aged and older adults in China: findings from the CHARLS cohort study. J Nutr Health Aging. (2022) 26:1034–41. doi: 10.1007/s12603-022-1863-z
2. Dai, S, Wang, S, Jiang, S, Wang, D, and Dai, C. Bidirectional association between handgrip strength and ADLs disability: a prospective cohort study. Front Public Health. (2023) 11:1200821. doi: 10.3389/fpubh.2023.1200821
3. Liu, H, Ma, Y, Lin, L, Sun, Z, Li, Z, and Jiang, X. Association between activities of daily living and depressive symptoms among older adults in China: evidence from the CHARLS. Front Public Health. (2023) 11:1249208. doi: 10.3389/fpubh.2023.1249208
4. Zeng, Q, Ding, J, Tu, R, He, H, Wang, S, Huang, Y, et al. The mediating effect of depressive symptoms on the association between childhood friendship and physical function in middle-aged and older adults: evidence from the China health and retirement longitudinal study (CHARLS). J Affect Disord. (2024) 359:196–205. doi: 10.1016/j.jad.2024.05.087
5. Wang, S, Yu, M, Huang, W, Wang, T, Liu, K, and Xiang, B. Longitudinal association between ADL disability and depression in middle-aged and elderly: national cohort study. J Nutr Health Aging. (2025) 29:100450. doi: 10.1016/j.jnha.2024.100450
6. Li, Q, Cen, W, Yang, T, and Tao, S. Association between depressive symptoms and sarcopenia among middle-aged and elderly individuals in China: the mediation effect of activities of daily living (ADL) disability. BMC Psychiatry. (2024) 24:432. doi: 10.1186/s12888-024-05885-y
7. Ji, D, Guo, H, Qiu, S, Dong, L, Shen, Y, Shen, Z, et al. Screening for frailty and its association with activities of daily living, cognitive impairment, and falls among community-dwelling older adults in China. BMC Geriatr. (2024) 24:576. doi: 10.1186/s12877-024-05173-0
8. Zhang, Y, Xiong, Y, Yu, Q, Shen, S, Chen, L, and Lei, X. The activity of daily living (ADL) subgroups and health impairment among Chinese elderly: a latent profile analysis. BMC Geriatr. (2021) 21:30. doi: 10.1186/s12877-020-01986-x
9. Qi, SG, Wang, ZH, Wang, LM, Wang, H, Zhang, H, and Li, ZX. Incidence of activities of daily living disability and related factors in community-dwelling older adults in China. Zhonghua Liu Xing Bing Xue Za Zhi. (2019) 40:272–6. doi: 10.3760/cma.j.issn.0254-6450.2019.03.004
10. Chauhan, S, Kumar, S, Bharti, R, and Patel, R. Prevalence and determinants of activity of daily living and instrumental activity of daily living among elderly in India. BMC Geriatr. (2022) 22:64. doi: 10.1186/s12877-021-02659-z
11. Man, W, Wang, S, and Yang, H. Exploring the spatial-temporal distribution and evolution of population aging and social-economic indicators in China. BMC Public Health. (2021) 21:966. doi: 10.1186/s12889-021-11032-z
12. Qian, JH, Wu, K, Luo, HQ, Cao, PY, and Ren, XH. Prevalence of loss of activities of daily living and influencing factors in elderly population in China. Zhonghua Liu Xing Bing Xue Za Zhi. (2016) 37:1272–6. doi: 10.3760/cma.j.issn.0254-6450.2016.09.018
13. Ansah, JP, Chiu, CT, Wei-Yan, AC, Min, TLS, and Matchar, DB. Trends in functional disability and cognitive impairment among the older adult in China up to 2060: estimates from a dynamic multi-state population model. BMC Geriatr. (2021) 21:380. doi: 10.1186/s12877-021-02309-4
14. Fang, Y, Yang, MJ, Ning, D, Huang, H, He, Y, Huang, Y, et al. Associations between sleep duration trajectories and risk of cardio-metabolic disease among middle-aged and older Chinese adults. J Affect Disord. (2024) 362:126–33. doi: 10.1016/j.jad.2024.06.114
15. Liu, W, Wu, Q, Wang, M, Wang, P, and Shen, N. Prospective association between sleep duration and cognitive impairment: findings from the China health and retirement longitudinal study (CHARLS). Front Med. (2022) 9:971510. doi: 10.3389/fmed.2022.971510
16. Zhou, Z, and Tian, X. Prevalence and association of sleep duration and different volumes of physical activity with type 2 diabetes: the first evidence from CHARLS. BMC Public Health. (2024) 24:3331. doi: 10.1186/s12889-024-20743-y
17. Lv, X, Peng, W, Jia, B, Lin, P, and Yang, Z. Longitudinal association of sleep duration with possible sarcopenia: evidence from CHARLS. BMJ Open. (2024) 14:e079237. doi: 10.1136/bmjopen-2023-079237
18. Ding, R, Ding, P, Tian, L, Kuang, X, Huang, B, and Lin, C. Associations between sleep duration, depression status, and cognitive function among Chinese elderly: a community-based study. J Affect Disord. (2024) 366:273–82. doi: 10.1016/j.jad.2024.08.200
19. Fjell, AM, Sørensen, Ø, Wang, Y, Amlien, IK, Baaré, WFC, Bartrés-Faz, D, et al. Is short sleep bad for the brain? Brain structure and cognitive function in short sleepers. J Neurosci Off J Soc Neurosci. (2023) 43:5241–50. doi: 10.1523/JNEUROSCI.2330-22.2023
20. Antza, C, Kostopoulos, G, Mostafa, S, Nirantharakumar, K, and Tahrani, A. The links between sleep duration, obesity and type 2 diabetes mellitus. J Endocrinol. (2021) 252:125–41. doi: 10.1530/JOE-21-0155
21. Chen, WC, and Wang, XY. Longitudinal associations between sleep duration and cognitive impairment in Chinese elderly. Front Aging Neurosci. (2022) 14:1037650. doi: 10.3389/fnagi.2022.1037650
22. Henry, A, Katsoulis, M, Masi, S, Fatemifar, G, Denaxas, S, Acosta, D, et al. The relationship between sleep duration, cognition and dementia: a Mendelian randomization study. Int J Epidemiol. (2019) 48:849–60. doi: 10.1093/ije/dyz071
23. Chen, R, Chen, Q, Lu, G, Zhang, M, Zhang, M, Yang, H, et al. Sleep duration and depressive symptoms in Chinese middle-aged and older adults: the moderating effects of grip strength. J Affect Disord. (2023) 339:348–54. doi: 10.1016/j.jad.2023.07.059
24. Covassin, N, and Singh, P. Sleep duration and cardiovascular disease risk: epidemiologic and experimental evidence. Sleep Med Clin. (2016) 11:81–9. doi: 10.1016/j.jsmc.2015.10.007
25. Sabia, S, Dugravot, A, Léger, D, Ben Hassen, C, Kivimaki, M, and Singh-Manoux, A. Association of sleep duration at age 50, 60, and 70 years with risk of multimorbidity in the UK: 25-year follow-up of the Whitehall II cohort study. PLoS Med. (2022) 19:e1004109. doi: 10.1371/journal.pmed.1004109
26. Jonasdottir, SS, Minor, K, and Lehmann, S. Gender differences in nighttime sleep patterns and variability across the adult lifespan: a global-scale wearables study. Sleep. (2021) 44:zsaa 169. doi: 10.1093/sleep/zsaa169
27. Hirshkowitz, M, Whiton, K, Albert, SM, Alessi, C, Bruni, O, Don Carlos, L, et al. National Sleep Foundation's updated sleep duration recommendations: final report. Sleep Health. (2015) 1:233–43. doi: 10.1016/j.sleh.2015.10.004
28. Wang, Z, Ni, X, Gao, D, Fang, S, Huang, X, Jiang, M, et al. The relationship between sleep duration and activities of daily living (ADL) disability in the Chinese oldest-old: a cross-sectional study. Peer J. (2023) 11:e14856. doi: 10.7717/peerj.14856
29. Luo, M, Dong, Y, Fan, B, Zhang, X, Liu, H, Liang, C, et al. Sleep duration and functional disability among Chinese older adults: cross-sectional study. JMIR Aging. (2024) 7:e53548. doi: 10.2196/53548
30. Zou, H, Jiang, L, Hou, Y, Zhang, L, and Liu, J. Long and short sleep durations can affect cognitive function in older adults through the chain mediation effect of ADL and depression: evidence from CHARLS 2018. Aging Clin Exp Res. (2024) 36:224. doi: 10.1007/s40520-024-02881-w
31. Lee, Y-H, Kong, D, Lee, Y-TH, Lin, C-H, Liu, C-T, and Chang, Y-C. Functional disabilities and changes in sleep quality and duration among older adults: results from a longitudinal study in China, 2005–2014. Eur Geriatric Med. (2022) 13:967–75. doi: 10.1007/s41999-022-00619-3
32. Chen, T, Wu, Z, Shen, Z, Zhang, J, Shen, X, and Li, S. Sleep duration in Chinese adolescents: biological, environmental, and behavioral predictors. Sleep Med. (2014) 15:1345–53. doi: 10.1016/j.sleep.2014.05.018
33. Chinese Longitudinal Healthy Longevity Survey (CLHLS-HF): Peking University Open Research Data; (1998). Available online at: https://opendata.pku.edu.cn/dataverse/CHADS (Accessed February 10, 2025).
34. Brumback-Peltz, C, Balasubramanian, AB, Corrada, MM, and Kawas, CH. Diagnosing dementia in the oldest-old. Maturitas. (2011) 70:164–8. doi: 10.1016/j.maturitas.2011.07.008
35. Min, SH, Topaz, M, Lee, C, and Schnall, R. Understanding changes in mental health symptoms from young-old to old-old adults by sex using multiple-group latent transition analysis. Gero Sci. (2023) 45:1791–801. doi: 10.1007/s11357-023-00729-1
36. Goodyear, MD, Krleza-Jeric, K, and Lemmens, T. The declaration of Helsinki. BMJ. (2007) 335:624–5. doi: 10.1136/bmj.39339.610000.BE
37. Moreno, X, Gajardo, J, and Monsalves, MJ. Gender differences in positive screen for depression and diagnosis among older adults in Chile. BMC Geriatr. (2022) 22:54. doi: 10.1186/s12877-022-02751-y
38. Tengku Mohd, TAM, Yunus, RM, Hairi, F, Hairi, NN, and Choo, WY. Social support and depression among community dwelling older adults in Asia: a systematic review. BMJ Open. (2019) 9:e026667. doi: 10.1136/bmjopen-2018-026667
39. He, M, Ma, J, Ren, Z, Zhou, G, Gong, P, Liu, M, et al. Association between activities of daily living disability and depression symptoms of middle-aged and older Chinese adults and their spouses: a community based study. J Affect Disord. (2019) 242:135–42. doi: 10.1016/j.jad.2018.08.060
40. Yan, Y, Du, Y, Li, X, Ping, W, and Chang, Y. Physical function, ADL, and depressive symptoms in Chinese elderly: evidence from the CHARLS. Front Public Health. (2023) 11:1017689. doi: 10.3389/fpubh.2023.1017689
41. Fang, H, Tu, S, Sheng, J, and Shao, A. Depression in sleep disturbance: a review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med. (2019) 23:2324–32. doi: 10.1111/jcmm.14170
42. Dong, L, Xie, Y, and Zou, X. Association between sleep duration and depression in US adults: a cross-sectional study. J Affect Disord. (2022) 296:183–8. doi: 10.1016/j.jad.2021.09.075
43. Mograbi, DC, Faria Cde, A, Fichman, HC, Paradela, EM, and Lourenço, RA. Relationship between activities of daily living and cognitive ability in a sample of older adults with heterogeneous educational level. Ann Indian Acad Neurol. (2014) 17:71–6. doi: 10.4103/0972-2327.128558
44. Zhou, C, Yang, G, Theeboom, M, Yang, H, Zhu, R, Zhou, Z, et al. Role of visual function and performance of activities of daily living in cognitive function in patients with mild cognitive impairment: a cross-sectional study. Frontiers in aging. Neuroscience. (2025) 17:17. doi: 10.3389/fnagi.2025.1505815
45. Ma, Y, Liang, L, Zheng, F, Shi, L, Zhong, B, and Xie, W. Association between sleep duration and cognitive decline. JAMA Netw Open. (2020) 3:e2013573. doi: 10.1001/jamanetworkopen.2020.13573
46. Chen, JC, Espeland, MA, Brunner, RL, Lovato, LC, Wallace, RB, Leng, X, et al. Sleep duration, cognitive decline, and dementia risk in older women. Alzheimers Dement. (2016) 12:21–33. doi: 10.1016/j.jalz.2015.03.004
47. Di Renzo, L, Gualtieri, P, and De Lorenzo, A. Diet, nutrition and chronic degenerative diseases. Nutrients. (2021) 13:1372. doi: 10.3390/nu13041372
48. Di Renzo, L, Gualtieri, P, Romano, L, Marrone, G, Noce, A, Pujia, A, et al. Role of personalized nutrition in chronic-degenerative diseases. Nutrients. (2019) 11:1707. doi: 10.3390/nu11081707
49. Fong, JH. Disability incidence and functional decline among older adults with major chronic diseases. BMC Geriatr. (2019) 19:323. doi: 10.1186/s12877-019-1348-z
50. Ćwirlej-Sozańska, A, Wiśniowska-Szurlej, A, Wilmowska-Pietruszyńska, A, and Sozański, B. Determinants of ADL and IADL disability in older adults in southeastern Poland. BMC Geriatr. (2019) 19:297. doi: 10.1186/s12877-019-1319-4
51. Dashti, HS, Scheer, FA, Jacques, PF, Lamon-Fava, S, and Ordovás, JM. Short sleep duration and dietary intake: epidemiologic evidence, mechanisms, and health implications. Adv Nutr. (2015) 6:648–59. doi: 10.3945/an.115.008623
52. Ai, S, Zhang, J, Zhao, G, Wang, N, Li, G, So, HC, et al. Causal associations of short and long sleep durations with 12 cardiovascular diseases: linear and nonlinear Mendelian randomization analyses in UK biobank. Eur Heart J. (2021) 42:3349–57. doi: 10.1093/eurheartj/ehab170
53. Jiang, B, Tang, D, Dai, N, Huang, C, Liu, Y, Wang, C, et al. Association of Self-Reported Nighttime Sleep Duration with chronic kidney disease: China health and retirement longitudinal study. Am J Nephrol. (2023) 54:249–57. doi: 10.1159/000531261
54. Park, S, Lee, S, Kim, Y, Lee, Y, Kang, MW, Kim, K, et al. Short or long sleep duration and CKD: a Mendelian randomization study. J Am Soc Nephrol. (2020) 31:2937–47. doi: 10.1681/ASN.2020050666
55. Burgard, SA, and Ailshire, JA. Gender and time for sleep among U.S. adults. Am Sociol Rev. (2013) 78:51–69. doi: 10.1177/0003122412472048
56. Zuo, L, Chen, X, Liu, M, Dong, S, Chen, L, Li, G, et al. Gender differences in the prevalence of and trends in sleep patterns and prescription medications for insomnia among US adults, 2005 to 2018. Sleep Health. (2022) 8:691–700. doi: 10.1016/j.sleh.2022.07.004
57. Scovelle, AJ, Hewitt, B, Lallukka, T, O'Neil, A, and King, TL. Time use, time pressure and sleep: is gender an effect modifier? Eur J Pub Health. (2023) 33:411–7. doi: 10.1093/eurpub/ckad038
58. Bai, F, Leng, M, Zhang, Y, Guo, J, and Wang, Z. Effectiveness of intensive versus regular or no exercise in older adults after hip fracture surgery: a systematic review and meta-analysis. Braz J Phys Ther. (2023) 27:100482. doi: 10.1016/j.bjpt.2023.100482
59. Ellegaard, K, von Bülow, C, Røpke, A, Bartholdy, C, Hansen, IS, Rifbjerg-Madsen, S, et al. Hand exercise for women with rheumatoid arthritis and decreased hand function: an exploratory randomized controlled trial. Arthritis Res Ther. (2019) 21:158. doi: 10.1186/s13075-019-1924-9
60. Hishikawa, N, Takahashi, Y, Fukui, Y, Tokuchi, R, Furusawa, J, Takemoto, M, et al. Yoga-plus exercise mix promotes cognitive, affective, and physical functions in elderly people. Neurol Res. (2019) 41:1001–7. doi: 10.1080/01616412.2019.1672380
61. Kim, D. The effects of a combined physical activity, recreation, and art and craft program on ADL, cognition, and depression in the elderly. J Phys Ther Sci. (2017) 29:744–7. doi: 10.1589/jpts.29.744
62. Åkerstedt, T, Ghilotti, F, Grotta, A, Bellavia, A, Lagerros, YT, and Bellocco, R. Sleep duration, mortality and the influence of age. Eur J Epidemiol. (2017) 32:881–91. doi: 10.1007/s10654-017-0297-0
63. Liu, J, Zhang, T, Luo, J, Chen, S, and Zhang, D. Association between sleep duration and grip strength in U.S. older adults: an NHANES analysis (2011-2014). Int J Environ Res Public Health. (2023) 20:3416. doi: 10.3390/ijerph20043416
64. Nazar, G, Leiva, AM, Troncoso, C, Martínez, A, Petermann-Rocha, F, Villagrán, M, et al. Association between sleep duration and cognitive impairment in older people. Rev Med Chile. (2019) 147:1398–406. doi: 10.4067/S0034-98872019001101398
65. Nutakor, JA, Dai, B, Gavu, AK, and Antwi, OA. Relationship between chronic diseases and sleep duration among older adults in Ghana. Qual Life Res Int J Qual Life Asp Treat Care Rehab. (2020) 29:2101–10. doi: 10.1007/s11136-020-02450-4
66. Chaput, JP, Dutil, C, Featherstone, R, Ross, R, Giangregorio, L, Saunders, TJ, et al. Sleep duration and health in adults: an overview of systematic reviews. Appl Physiol Nutr Metabol. (2020) 45:S218–31. doi: 10.1139/apnm-2020-0034
67. Hakimi, S, Kaur, S, Ross-White, A, Martin, LJ, and Rosenberg, MW. A systematic review examining associations between physical activity, sedentary behaviour, and sleep duration with quality of life in older adults aged 65 years and above. Appl Physiol Nutr Metabol. (2023) 48:97–162. doi: 10.1139/apnm-2022-0298
68. Zee, PC, Bertisch, SM, Morin, CM, Pelayo, R, Watson, NF, Winkelman, JW, et al. Long-term use of insomnia medications: an appraisal of the current clinical and scientific evidence. J Clin Med. (2023) 12:1629. doi: 10.3390/jcm12041629
69. Tseng, LY, Huang, ST, Peng, LN, Chen, LK, and Hsiao, FY. Benzodiazepines, z-hypnotics, and risk of dementia: special considerations of half-lives and concomitant use. Neurotherapeutics. (2020) 17:156–64. doi: 10.1007/s13311-019-00801-9
70. Masse, M, Henry, H, Cuvelier, E, Pinçon, C, Pavy, M, Beeuwsaert, A, et al. Sleep medication in older adults: Identifying the need for support by a community pharmacist. Basel, Switzerland: Healthcare (2022). 10 p.
Keywords: sleep duration, activity of daily living, physical activity, older adults, observational study, disability, CLHLS
Citation: Cai D, Zeng Y, Chen M, Zhong Y, Quan Y, Ye M and Huang X (2025) Association between sleep duration and disability in activities of daily living among Chinese older adults: a nationwide observational study. Front. Public Health. 13:1580101. doi: 10.3389/fpubh.2025.1580101
Edited by:
Muralikrishnan Dhanasekaran, Auburn University, United StatesReviewed by:
Mack Shelley, Iowa State University, United StatesTakuya Ataka, Oita University, Japan
Copyright © 2025 Cai, Zeng, Chen, Zhong, Quan, Ye and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoxiao Huang, MTAwNjc0QGNxbXUuZWR1LmNu
†These authors have contributed equally to this work
 Dahuan Cai1†
Dahuan Cai1† Mengliang Ye
Mengliang Ye Xiaoxiao Huang
Xiaoxiao Huang