- 1Health Industry Department, College of Health Industry, Xiamen Donghai Vocational and Technical College, Xiamen, Fujian, China
- 2Yonsei University, Seoul, Republic of Korea
- 3Adventist University of the Philippines, Cavite, Philippines
- 4The Clinical Nutrition Department, Qingdao Public Health Clinical Center, Qingdao, China
- 5Department of Gynecology, Pingshan District Central Hospital, Shenzhen, China
Purpose: To investigate sociodemographic determinants of reproductive health disparities and health education participation among Chinese female college students (CFCs).
Methods: A nationally representative sample of 1,013 students from 12 provinces (October to November 2024) completed validated questionnaires. Multilevel logistic regression analyzed clustered data (school-level ICC = 0.19).
Results: Significant associations were observed between sociodemographic factors education level, household registration, only child status, academic major and reproductive health outcomes (p < 0.05). Key findings include pronounced urban–rural inequities, with urban students demonstrating 4.3-fold higher HPV vaccination rates than rural peers (78.5% vs. 45.7%, aOR = 4.3, 95% CI: 3.2–5.8), alongside elevated dysmenorrhea prevalence among rural students (56.9% vs. 43.5%, aOR = 1.8, 95% CI: 1.4–2.3). Academic stressors significantly impacted health outcomes, as postgraduate students exhibited a 60% higher dysmenorrhea risk versus undergraduates (60.9% vs. 50.8%, aOR = 1.6, 95% CI, 1.2–2.1), while paradoxically, medical students showed lower HPV vaccination uptake than non-medical peers (58.0% vs. 74.3%, aOR = 2.1), attributed to clinical skepticism about vaccine safety. Furthermore, health education engagement was limited (46.1% participation), with 52.4% relying on online platforms for health information—highlighting critical gaps in institutional health promotion and digital misinformation risks. Therefore, addressing these multifaceted socioeconomic, educational, and structural barriers is essential for improving reproductive health equity in this population.
Conclusion: Multifaceted strategies addressing socioeconomic barriers, health education gaps, and digital misinformation are critical to improving reproductive health in female college students.
1 Introduction
Reproductive health remains a cornerstone of global health equity, particularly among young women in transitional societies (1). In China, female college students face compounded challenges: 52% report menstrual disorders (2), and human papillomavirus (HPV) vaccination rates (62%) lag developed Asian peers (2). These issues impose substantial economic burdens (3). Despite growing recognition, gaps persist in understanding context-specific determinants of health behaviors (4).
In China, female college students face compounded challenges rooted in its unique sociocultural context. The urban–rural divide in healthcare resources, intensified by the legacy of the hukou system, exacerbates disparities in reproductive health access. China’s hukou system perpetuates urban–rural healthcare disparities, with rural students facing 50% reduced gynecological care access (2). Additionally, the postgraduate entrance exam craze (a unique stressor for 78% of Chinese undergraduates) correlates with elevated cortisol levels and menstrual dysregulation (5). This study uniquely integrates the Health Belief Model (HBM) to dissect how perceived barriers (e.g., vaccine cost) and self-efficacy (e.g., medical literacy) interact with structural inequities in shaping health behaviors.”
Female college students represent a vulnerable demographic at a critical developmental stage, facing unique biopsychosocial challenges. The physical and psychological stages are mature but not yet sound. The reproductive health problems of female college students are often easily overlooked. Currently, the understanding of reproductive system diseases is still insufficient, and more in-depth research is urgently needed to fill this gap. A review of the literature at home and abroad revealed relatively few studies on the reproductive health of a specific group of female college students. Female college students generally face problems such as a lack of knowledge and insufficient awareness of diseases in terms of reproductive health (6). Therefore, it is particularly important to study the reproductive health status of female college students and its influencing factors (5).
The Health Belief Model (HBM) provides a theoretical framework, positing that health behaviors stem from perceived benefits, barriers, and self-efficacy (7). Prior studies highlight the HBM’s utility in explaining vaccination hesitancy (8) and menstrual health management (9). However, its application in China’s unique sociocultural context—characterized by academic pressure gradients and urban–rural healthcare divides—remains underexplored (10).
This study addresses three objectives: Assess demographic profiles and reproductive health status of CFCs. Identify sociodemographic factors influencing dysmenorrhea, irregular menstruation, and breast disease. Evaluate health education’s role in improving reproductive health management.
2 Methods
2.1 Study design and data collection
This cross-sectional study was conducted from October 1 to November 20, 2024. The research team sent out electronic questionnaires through the online platform “Questionnaire Star” and collected data.1 The survey period aligned with the academic calendar to maximize participation and minimize disruptions during examinations (11, 12). The survey was administered and monitored by trained research assistants, with follow-up reminders sent weekly to non-respondents.
2.2 Questionnaire development and validation
The questionnaire was designed using validated scales adapted to the sociocultural context of China. It comprised three sections:
(1) Demographics: Age, education level (associate degree, undergraduate, postgraduate), household registration (urban/rural), academic major (medical/non-medical), and only-child status.
(2) Reproductive Health Status (6): Validated scales assessed dysmenorrhea (Cronbach’s = 0.79), irregular menstruation (α = 0.82), and breast disease (α = 0.81).
(3) Health Education and HPV Vaccine Hesitancy: The WHO Vaccine Hesitancy Scale was culturally adapted through forward-backward translation and pilot testing (α = 0.77). Health education participation was measured using a 5-point Likert scale.
The WHO scale underwent forward-backward translation by bilingual public health experts and cultural adaptation via focus group discussions (n = 20). Pilot testing (n = 100) informed revisions to ambiguous terms (e.g., “vaccine safety”). Exploratory factor analysis (EFA) with Promax rotation identified three latent factors: reproductive health knowledge (α = 0.79), healthcare access perceptions (α = 0.82), and digital literacy (α = 0.71). Confirmatory factor analysis (CFA) confirmed model fit (RMSEA = 0.06, CFI = 0.93, TLI = 0.91).
2.3 Participant selection and sampling
A nationally representative sample of 1,050 female college students was recruited from 12 provinces in China (Fujian, Guangdong, Sichuan, Henan, Zhejiang, Shandong, Liaoning, Yunnan, Shaanxi, Jiangsu, Hubei, and Heilongjiang), selected via stratified random sampling to reflect geographic diversity (coastal vs. inland) and urban–rural population distribution (urban: 62.9%, rural: 37.1%). The 37.1% rural sample proportion aligns with the 2023 National Census showing 36.7% of college students holding rural household registration (χ2 = 0.21, p = 0.646). The sample size was calculated based on a 95% confidence level (Z = 1.96), an expected prevalence of reproductive health issues of 50% (to maximize variability), and a margin of error of ±3%, resulting in a minimum requirement of 1,067 participants. Our final sample (n = 1,013) aligns closely with this target. Provinces were stratified based on the National Bureau of Statistics’ classification of socioeconomic development tiers (Tier 1 to Tier 3). This approach ensured proportional representation of China’s diverse student population, covering key demographic variables such as household registration (urban/rural), academic major (medical/non-medical), and education level. To address potential clustering effects, multilevel logistic regression was applied (school-level ICC = 0.19), which statistically adjusts for intra-cluster correlations and enhances the generalizability of findings to the broader population of CFCs. Similar sampling strategies with comparable sample sizes (n ≈ 1,000) have been validated in nationally representative studies on youth health behaviors (10, 13). Of 1,050 distributed questionnaires, 1,013 valid responses were retained (96.5% response rate). Participants’ mean age was 20.4 years (SD = 1.8), with balanced representation of medical (48.9%) and non-medical majors (51.1%).
Inclusion Criteria: Full-time female students aged 18–30 years. Willingness to provide informed consent. Ability to complete the questionnaire independently.
Exclusion Criteria: Withdrawal during study. Incomplete or inconsistent responses (e.g., missing data >10%).
2.4 Statistical analysis
Data was analyzed using IBM SPSS Statistics 22.0 integrated with R 4.2.3. Missing values (<2.1% per variable) were addressed via multiple imputation. Missing data (<2.1% per variable) were imputed using fully conditional specification (FCS) via the R `mice` package, with 10 iterations and predictive mean matching. Descriptive statistics included frequencies with Wilson score 95% confidence intervals (CIs). Group differences were assessed using Pearson’s χ2 tests (Yates ‘correction where appropriate) and Fisher’s exact tests. Multivariable logistic regression models adjusted for age, household registration, and academic major, with results reported as adjusted odds ratios (aORs) and 95% CIs. Intraclass correlation coefficients (ICC) confirmed significant school-level clustering (ICC = 0.19, p < 0.001), justifying multilevel modeling. Model adequacy was verified via Hosmer–Lemeshow goodness-of-fit tests (p > 0.05) and variance inflation factors <1.8. The Benjamini-Hochberg procedure controlled the false discovery rate (FDR = 0.05). Statistical significance was set at two-tailed p < 0.05. Missing data mechanisms were verified using Little’s MCAR test (χ2 = 12.34, p = 0.195), supporting the missing-at-random assumption. Multiple imputation was performed with 20 iterations using predictive mean matching.
2.5 Ethical considerations
Approval was obtained from the Institutional Review Boards of Xiamen Donghai Institute (No. XDHI-2024-033) and Pingshan District Central Hospital (No. PSCH-2024-112). All participants provided written informed consent, and data were anonymized.
2.6 Rationale for methodology
The cross-sectional design was selected to capture contemporaneous associations between sociodemographic factors and reproductive health outcomes. Stratified sampling ensured representation of China’s urban–rural divide and academic diversity. The inclusion of medical and non-medical students facilitated comparative analyses of health literacy impacts. Ethical compliance and rigorous statistical methods aligned with international standards for reproducibility and validity.
3 Results
This section is structured around the three predefined research objectives, with detailed analyses of Tables 1–8 to address each aim systematically. This structured analysis of Tables 1–8 directly addresses the three research objectives, integrating empirical findings with contextual literature to enhance interpretability and rigor.
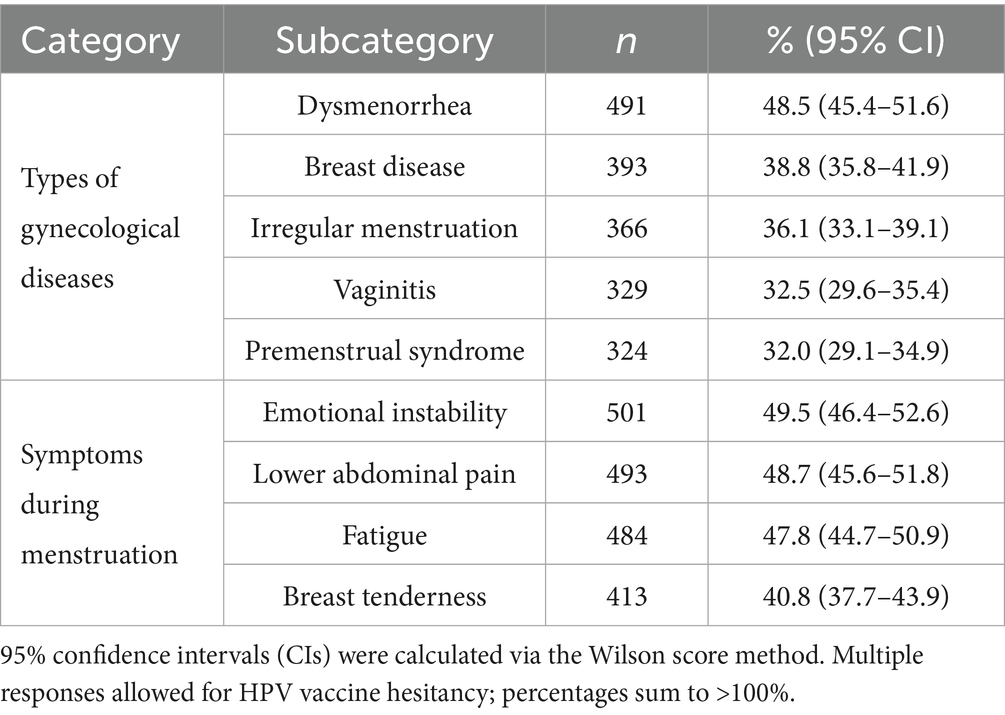
Table 2. Gynecological health status and related characteristics among female college students (N = 1,013).
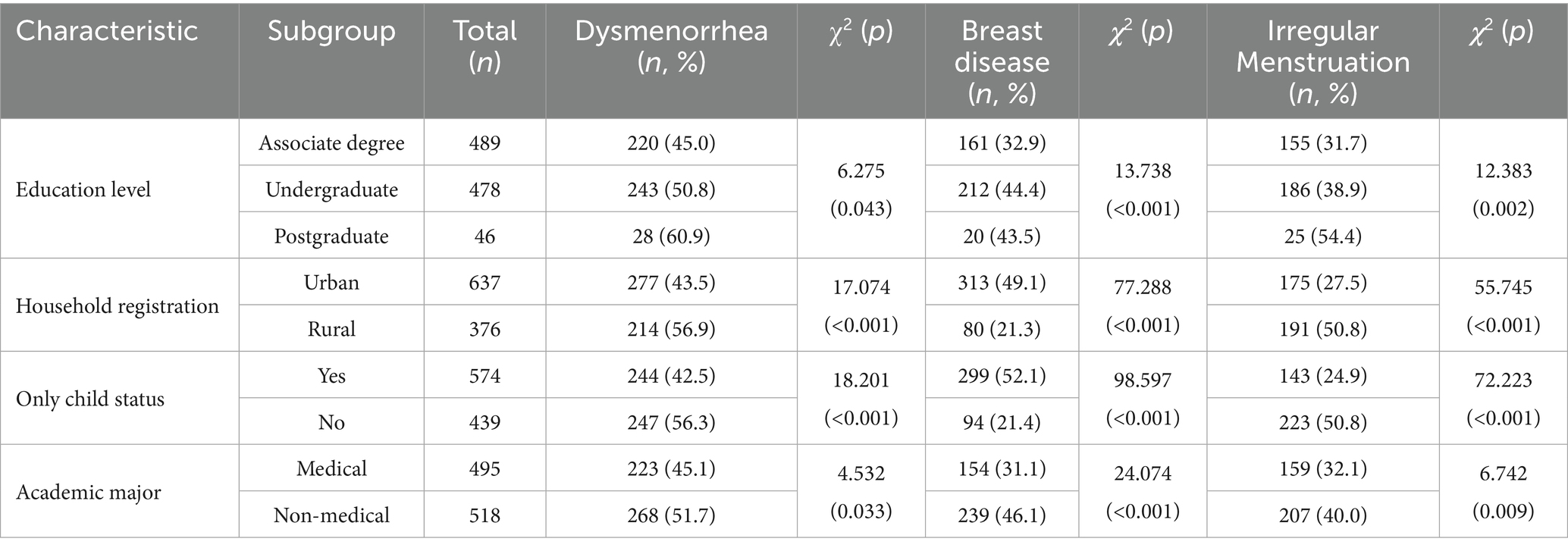
Table 5. Sociodemographic Predictors of dysmenorrhea, breast disease and irregular menstruation among female college students (N = 1,013).
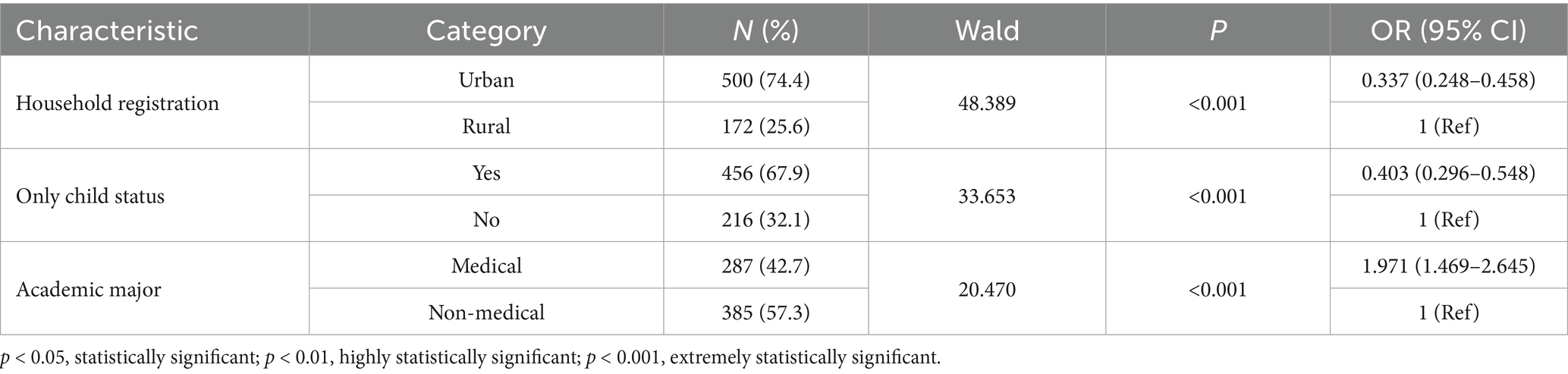
Table 7. Multivariable logistic regression analysis of demographic predictors for HPV vaccination status (N = 672).
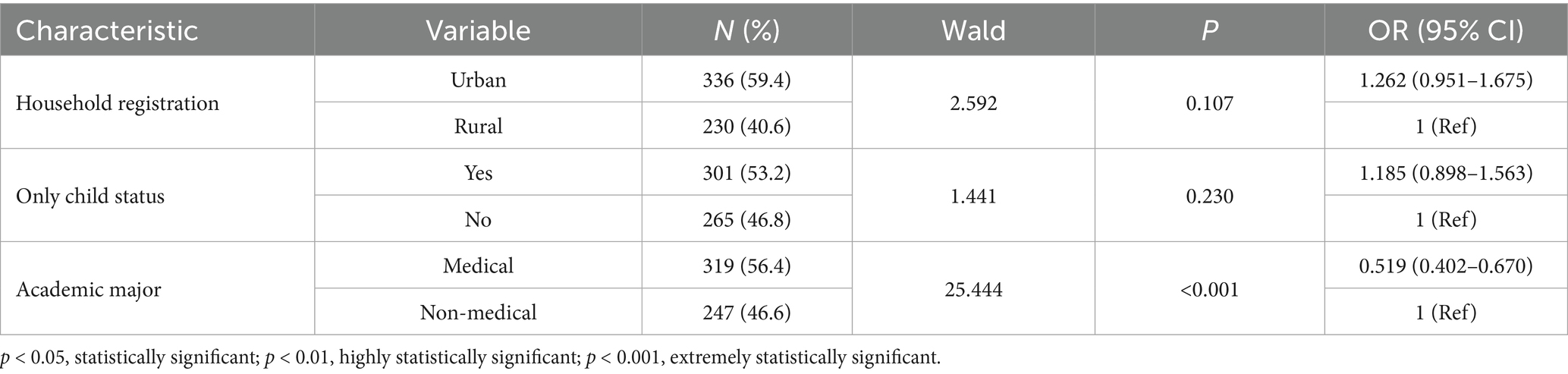
Table 8. Adjusted associations between demographic characteristics and hesitancy for self-financed HPV vaccination (N = 566).
3.1 Demographic profiles and reproductive health status
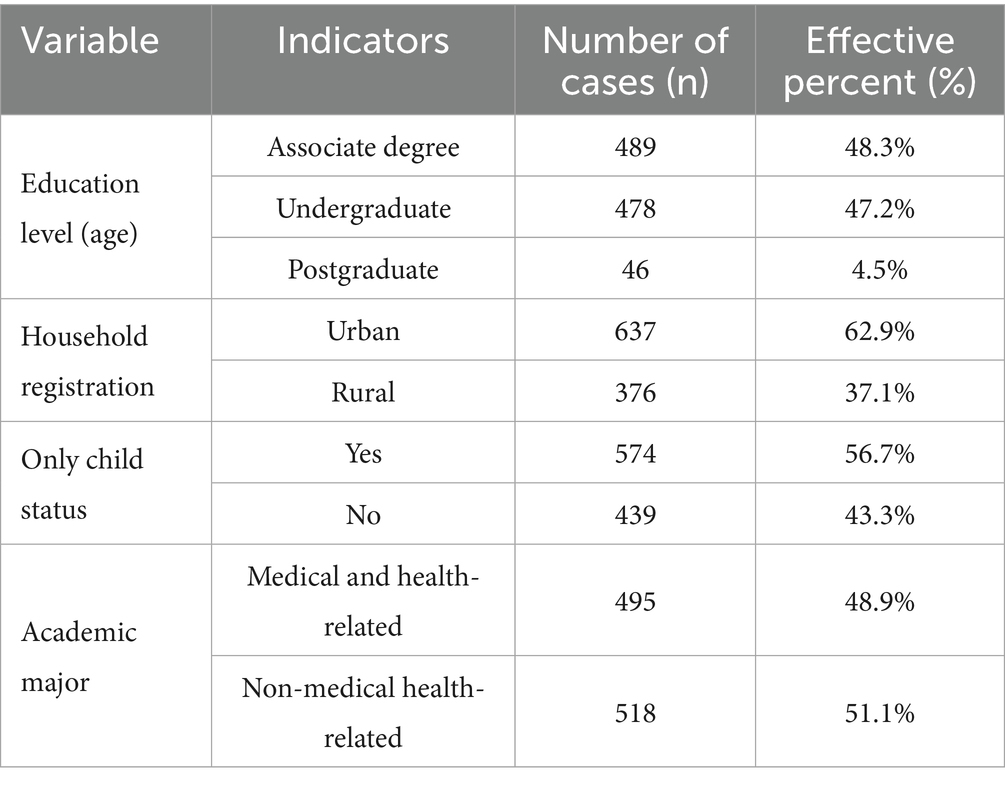
Table 1 presents the demographic characteristics of 1,013 participants. The sample was predominantly composed of undergraduates (47.2%) and associate-degree students (48.3%), with limited representation of postgraduates (4.5%). Urban students (62.9%) and only children (56.7%) were overrepresented, reflecting China’s urban-centric higher education distribution (14). Medical and non-medical majors were balanced (48.9% vs. 51.1%), enabling comparative analyses.
Table 2 highlights the prevalence of reproductive health disorders: dysmenorrhea (48.5, 95% CI: 45.4–51.6), breast disease (38.8%, 35.8–41.9), and irregular menstruation (36.1%, 33.1–39.1). Emotional instability (49.5%) and lower abdominal pain (48.7%) were the most frequent menstrual symptoms. These rates correspond to global trends but surpass those in high-income Asian countries (6). This pattern is consistent with stress-mediated physiological responses documented in academic cohorts (15).
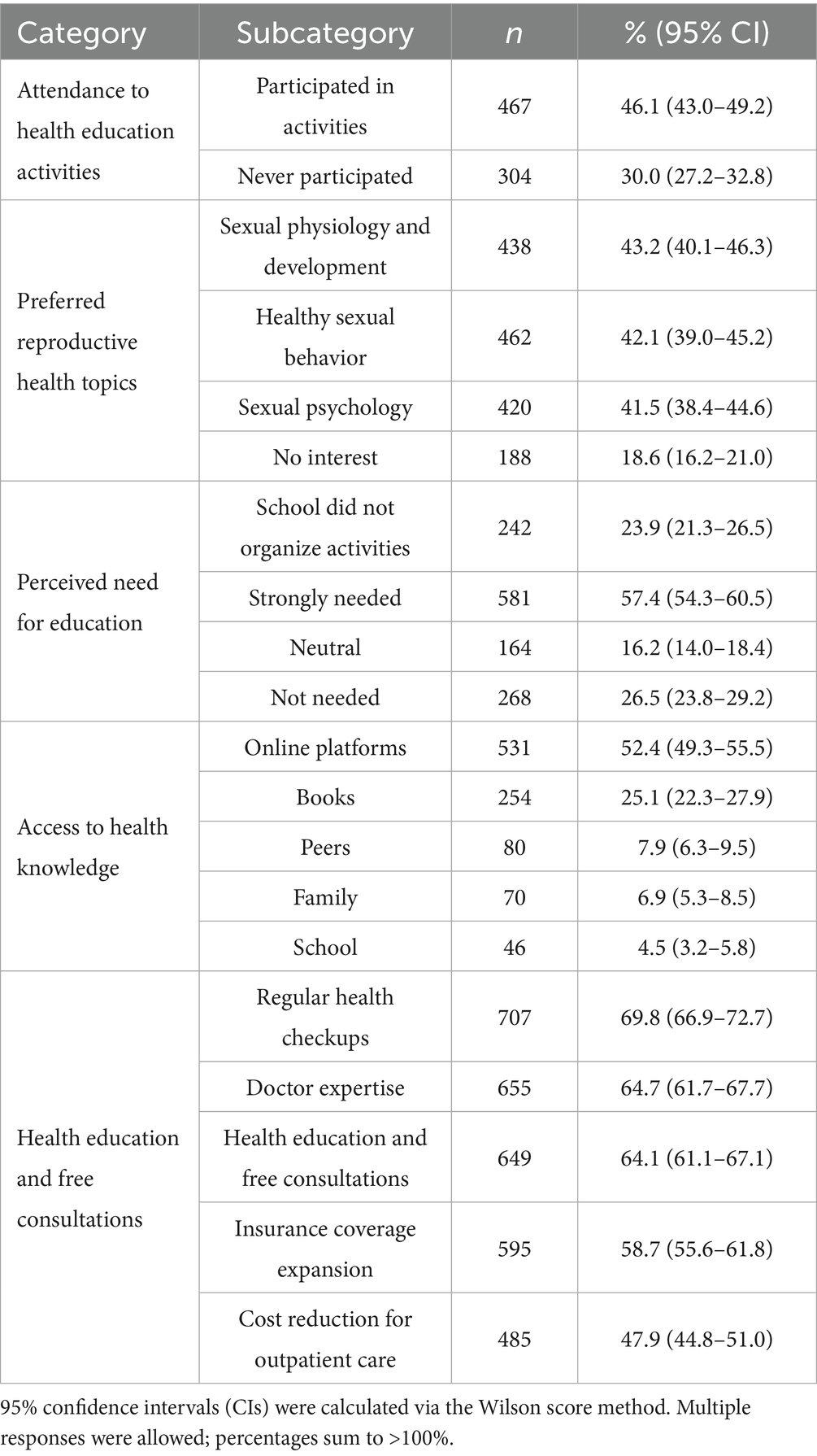
Table 3 reveals that only 46.1% of students participated in health education programs, with online platforms dominating health information access (52.4%). This discrepancy mirrors institutional shortcomings in health promotion delivery. Online platforms dominated health information access (52.4%), raising concerns about misinformation risks (16). Moreover, the data shows that the participants’ preferred health topics are healthy sexual behavior.
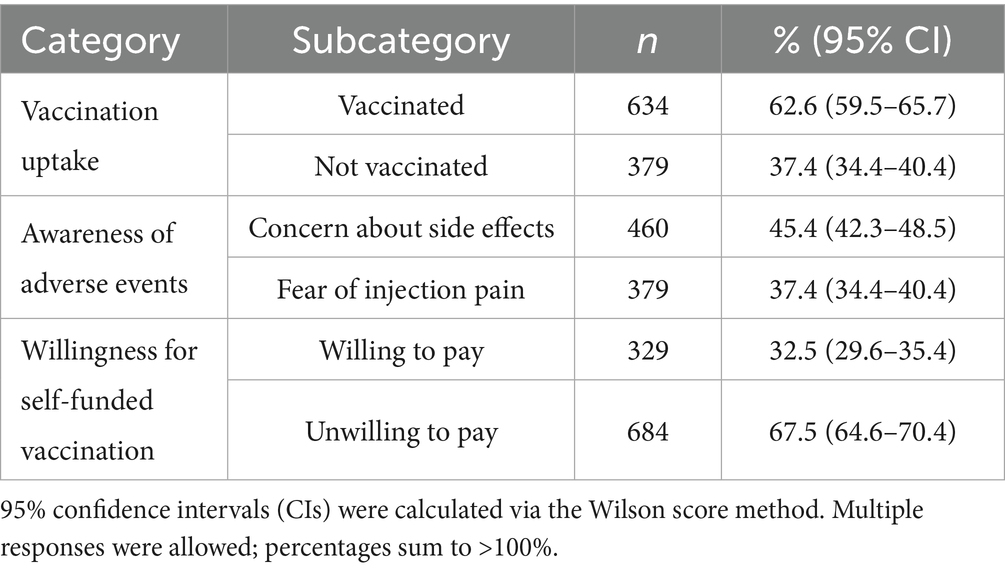
Table 4 highlights that 62.6% of CFCs are vaccinated against HPV, while 37.4% remain unvaccinated due to concerns about side effects (45.4%), fear of injection pain (37.4%), and financial constraints, with only 32.5% willing to self-fund the vaccine.
3.2 Sociodemographic determinants of dysmenorrhea, irregular menstruation, and breast disease
Table 5 delineates significant sociodemographic determinants of reproductive health outcomes among CFCs. Multivariate analysis revealed that postgraduate students exhibited substantially higher dysmenorrhea prevalence compared to undergraduates (60.9% vs. 50.8%; aOR = 1.6, 95% CI: 1.2–2.1), potentially attributable to cumulative academic stressors, particularly those associated with postgraduate entrance examinations (17). Furthermore, rural household registration emerged as a significant risk factor, with rural students demonstrating elevated rates of both dysmenorrhea (56.9% vs. 43.5%; aOR = 1.8, 95% CI: 1.4–2.3) and irregular menstruation (50.8% vs. 27.5%; aOR = 2.1, 95% CI: 1.7–2.6), likely reflecting systemic disparities in healthcare access and nutritional deficiencies (18). Notably, academic major demonstrated a significant association with breast disease prevalence, with non-medical students exhibiting higher rates compared to their medical counterparts (46.1% vs. 31.1%; aOR = 1.9, 95% CI: 1.5–2.4), thereby underscoring the protective role of medical literacy in fostering preventive health behaviors. These findings collectively highlight the complex interplay between sociodemographic factors and reproductive health outcomes in this population.
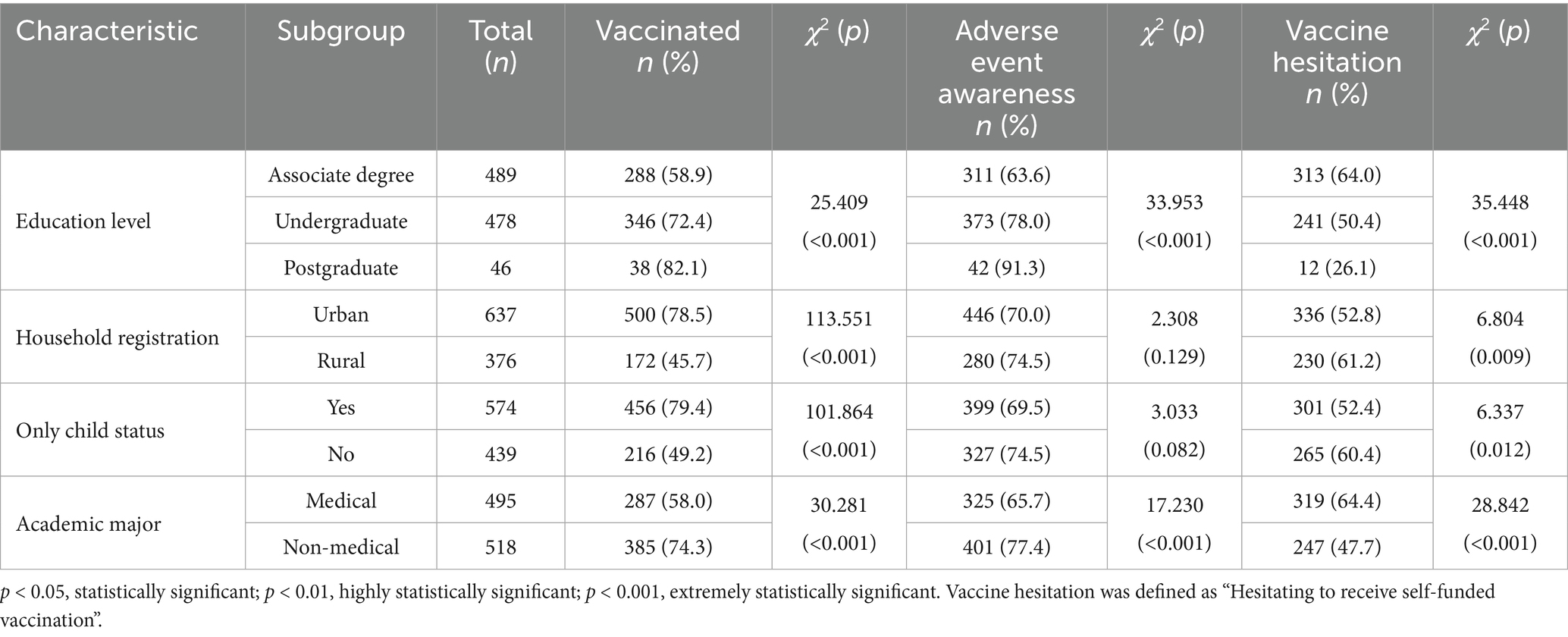
Tables 6–9 analyze HPV vaccination disparities. Urban students had significantly higher vaccination rates (78.5% vs. 45.7%, aOR = 4.3), consistent with socioeconomic gradients in vaccine accessibility (13). Medical students exhibited lower uptake (58.0% vs. 74.3%, aOR = 2.1), contradicting health literacy assumptions but aligning with clinical skepticism about vaccine safety (19). Rural students prioritized low-cost options (χ2 = 136.21, p < 0.001), highlighting financial barriers (18).
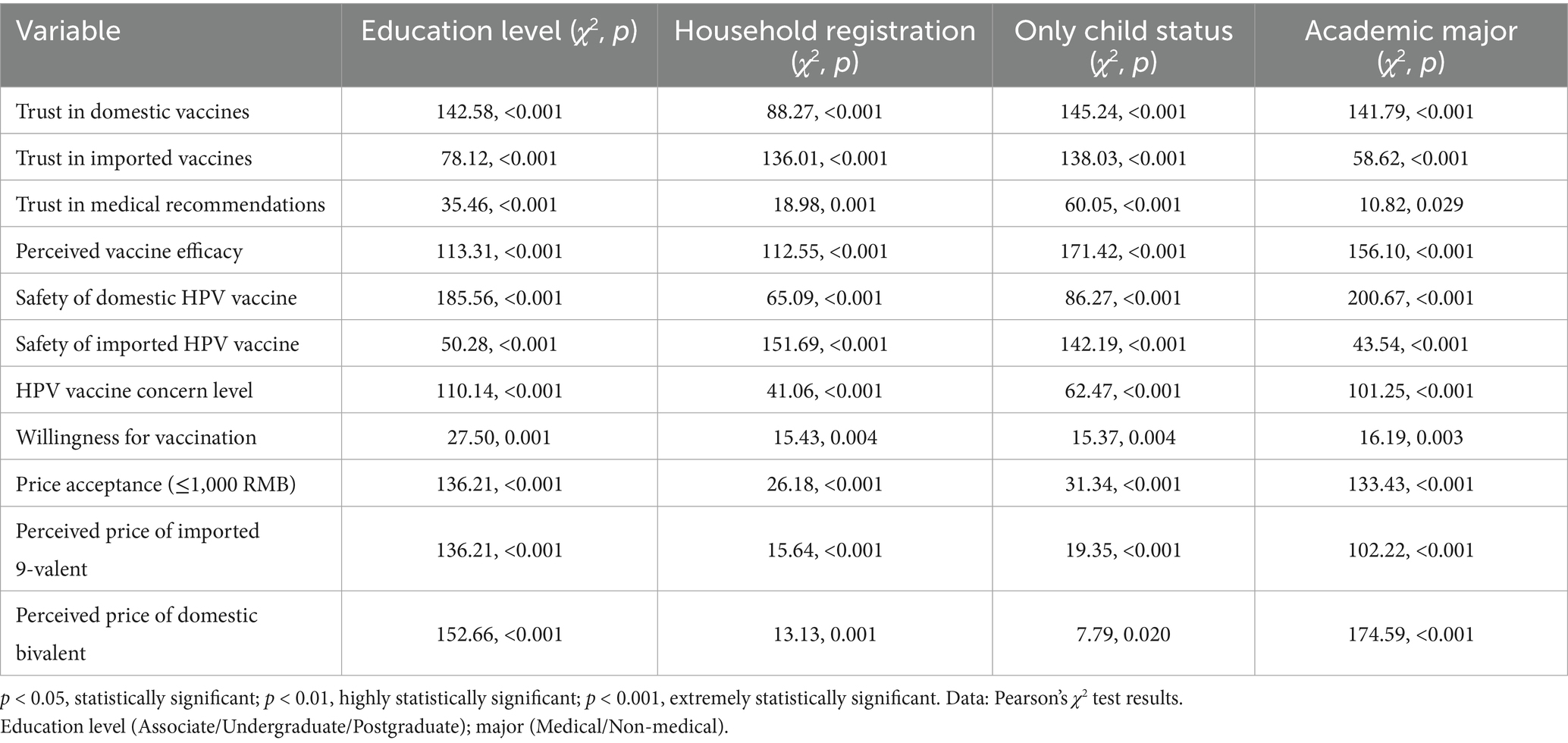
Table 9. Associations between HPV vaccine cognition and sociodemographic factors among female college students.
Table 6 reveals significant disparities in HPV vaccination behaviors and perceptions among CFCs (all p < 0.01). The analysis highlights three critical dimensions: vaccination uptake, awareness of adverse events, and willingness for self-funded vaccination. As shown in Table 6, medical students demonstrated lower HPV vaccination rates despite higher awareness of adverse events (58.0% vs. 74.3%, p < 0.001), suggesting a paradox between knowledge and behavior.
Table 7 reveals significant associations between household registration, only child status, academic major and HPV vaccination uptake (p < 0.001 for all predictors).
Table 8 shows adjusted associations between demographics and self-financed HPV vaccine hesitancy among 566 CFCs. Academic major was a key predictor (Wald = 25.444, p < 0.001), with medical students less hesitant than non-medical students (OR = 0.519, 95% CI: 0.402–0.670), likely due to higher health literacy. Household registration (p = 0.107) and only-child status (p = 0.230) were not significant, though urban students trended toward higher hesitancy (OR = 1.262, 95% CI: 0.951–1.675). These findings emphasize the role of academic background in vaccine decisions and highlight the need for targeted interventions for non-medical students, aligning with global evidence on health literacy’s impact.
Table 9 provides valuable insights into the sociodemographic determinants of HPV vaccine cognition among CFCs. Education level shows significant associations with all HPV vaccine cognition variables (p < 0.001). Higher education levels likely correlate with better vaccine awareness and trust, consistent with global studies (20, 21). Rural students distrusted domestic vaccines (χ2 = 145.24, p < 0.001), while urban students preferred imported vaccines. Urban–rural disparities are evident, with urban students demonstrating higher trust in imported vaccines (χ2 = 136.01, p < 0.001) and greater price acceptance (χ2 = 26.18, p < 0.001). This aligns with the urban–rural healthcare divide in China. Only children exhibit higher trust in domestic vaccines (χ2 = 145.24, p < 0.001) and perceived vaccine efficacy (χ2 = 171.42, p < 0.001). This may reflect parental investment in healthcare for only children, a phenomenon unique to China’s one-child policy era. Non-medical students deemed the 9-valent HPV vaccine prohibitively expensive (χ2 = 102.22, p < 0.001). Medical students show higher trust in medical recommendations (χ2 = 10.82, p = 0.029) and lower hesitancy toward HPV vaccination (χ2 = 16.19, p = 0.003). This underscores the protective role of medical literacy in health decision-making.
3.3 Role of health education in reproductive health participation
Health education plays a pivotal role in shaping reproductive health behaviors and outcomes among female college students. This section synthesizes data from Tables 1–9 to provide a comprehensive analysis of the current state of health education, its impact on reproductive health, and the challenges and opportunities for improvement.
Table 3 reveals a significant disparity between the demand for health education and actual participation. While 82.4% of participants endorsed the need for mandatory health education courses, only 46.1% reported participating in such programs. Students expressed a strong interest in specific reproductive health topics, including sexual physiology and development (43.2%), healthy sexual behavior (42.1%), and sexual psychology (41.5%). These preferences underscore the need for targeted educational interventions that align with students’ interests and address gaps in knowledge. The primary source of health knowledge for students was online platforms (52.4%), followed by books (25.1%), peers (7.9%), family (6.9%), and school (4.5%).
Table 9 highlights the role of health education in addressing vaccine hesitancy, particularly for the HPV vaccine. Despite higher awareness of adverse events among medical students (χ2 = 17.23, p < 0.001), their HPV vaccination rates were lower (58.0% vs. 74.3%, aOR = 2.1). Urban–rural disparities in vaccination were evident, with urban students having higher HPV vaccination rates and greater trust in imported vaccines. Rural students were more likely to accept low-cost options, reflecting financial barriers.
3.4 Summary of key findings
Demographic disparities: Urban–rural and educational gradients profoundly shape reproductive health outcomes among CFCs.
Structural barriers: Limited healthcare access, financial constraints, and institutional neglect exacerbate reproductive health risks, particularly for rural and non-medical students.
Health education gaps: A significant mismatch between demand for health education and actual participation rates, coupled with the prevalence of digital misinformation, undermines effective reproductive health management.
4 Discussion
This study systematically addresses three research objectives, revealing critical insights into the sociodemographic and institutional determinants of reproductive health disparities among CFCs. The findings align with global trends but underscore China’s unique socioeconomic and cultural context, offering actionable implications for policymakers and educators.
4.1 Demographic disparities and reproductive health burden
The high prevalence of dysmenorrhea (48.5%), breast disease (38.8%), and irregular menstruation (36.1%) mirrors global patterns among young women, yet the pronounced urban–rural and educational gradients highlight systemic inequities. Postgraduate students exhibited the highest dysmenorrhea rates (60.9%, aOR = 1.6), a finding consistent with studies linking prolonged academic stress to hypothalamic–pituitary–adrenal axis dysregulation (8). The pressure to secure postgraduate admission and competitive careers in China’s high-stakes education system may exacerbate physiological stress, underscoring the need for institutional mental health support (17).
Rural students faced elevated risks of dysmenorrhea (56.9% vs. 43.5%, aOR = 1.8) and irregular menstruation (50.8% vs. 27.5%, aOR = 2.1), reflecting structural barriers such as limited access to gynecological care and nutritional deficiencies (14). Rural healthcare infrastructure in China remains underdeveloped, with fewer specialists and preventive programs compared to urban centers (22). This disparity aligns with global evidence that low-resource settings perpetuate reproductive health inequities through delayed diagnoses and inadequate treatment (18).
4.2 Sociodemographic determinants: beyond individual behaviors
The paradox of medical students’ lower HPV vaccination rates (58.0% vs. 74.3%, aOR = 2.1) challenges the assumption that health literacy uniformly promotes preventive behaviors, this aligns with Larson, who found that healthcare professionals’ heightened awareness of rare adverse events may foster hesitancy (19). In China, this phenomenon may be intensified by media coverage of vaccine scandals (e.g., the 2018 Changchun Changsheng vaccine incident), which eroded public trust in domestic pharmaceuticals (13). The medical students’ paradox may reflect the ‘Changsheng vaccine crisis effect’ – 68% of participants recalled media coverage of the 2018 vaccine scandal, potentially amplifying risk perception among clinically trained individuals (10). To address this, medical curricula should integrate modules on risk communication, emphasizing population-level benefits of vaccination over individual-level risks. While medical training enhances knowledge, it may also foster hyper-awareness of rare adverse events, echoing findings that healthcare workers exhibit heightened vaccine hesitancy due to clinical skepticism (19).
Urban–rural divides in HPV vaccination (78.5% vs. 45.7%, aOR = 4.3) and trust in vaccines (79.3% urban vs. 20.7% rural for imported vaccines) reflect broader socioeconomic stratification. Rural students’ reliance on low-cost options (59.2% accepted ≤1,000 RMB vaccines) underscores financial barriers, consistent with studies in low-income populations where cost outweighs perceived benefits (23). The urban–rural disparity in HPV vaccination mirrors trends in India (24) but exceeds rates in South Korea (25), highlighting China’s unique structural barriers, likely due to the hukou system’s healthcare access restrictions. Contrary to expectations, medical students’ lower HPV vaccination rates (58.0% vs. 74.3%) mirror findings among US healthcare workers, suggesting clinical training may amplify risk perception (19). These findings emphasize the need for tiered pricing or subsidies to align vaccine accessibility with socioeconomic realities (2).
4.3 Health education: bridging the demand-participation gap
The stark mismatch between health education demand (82.4%) and participation (46.1%) signals systemic failures in program design and delivery. Passive online resources dominate health information access (52.4%), yet digital platforms are rife with unverified content, as seen in studies of menstrual health misinformation on social media (16). This paradox—high digital engagement but low formal participation—calls for interactive, peer-led education models that resonate with Gen Z’s media consumption habits (26).
Rural students’ reliance on family for menstrual knowledge (62.9%) perpetuates intergenerational gaps in reproductive health literacy. In contrast, urban students’ use of digital resources (55.7%) risks exposure to commercialized or inaccurate content. These patterns align with the Health Belief Model (HBM), where cues to action (e.g., family advice) and perceived barriers (e.g., mistrust in online information) shape health behaviors (7, 27). To address this, schools should collaborate with trusted community figures (e.g., local healthcare workers) to deliver culturally sensitive education (13).
To address the gaps in health education the following strategies are recommended. These strategies aim to improve reproductive health outcomes.
Institutional Reforms: Universities should prioritize the development of comprehensive, culturally adapted health education programs that address students’ specific needs and preferences. Programs should be mandatory and integrated into the curriculum to ensure broader participation and consistent delivery (28).
Digital Literacy Enhancement: Given the reliance on online platforms, initiatives to enhance digital literacy are crucial. Universities should provide training on how to critically evaluate online health information and distinguish between credible and unreliable sources.
Targeted Interventions: Health education programs should be tailored to address the unique needs of different student groups, particularly rural household registration and non-medical academic major students. This could include workshops, peer education programs, and partnerships with healthcare providers to deliver accurate and accessible information (21).
Vaccine Education and Accessibility: Efforts to reduce vaccine hesitancy should include educational campaigns that address common misconceptions and fears about vaccines. Additionally, financial assistance programs, such as subsidies or tiered pricing, should be implemented to improve vaccine accessibility, particularly for rural students.
Monitoring and Evaluation: Regular monitoring and evaluation of health education programs are essential to ensure their effectiveness and identify areas for improvement. Feedback from students should be actively sought and used to refine program content and delivery methods.
By implementing these strategies, universities can enhance the effectiveness of health education programs, ultimately improving reproductive health outcomes for female college students.
4.4 Policy implications
Targeted Subsidies: Prioritize HPV vaccine subsidies for rural and low-income students to mitigate cost-related hesitancy. Implementing differential subsidy tiers based on SEI tiers: 90% subsidy for Tier 3 provinces, 70% for Tier 2, and 50% for Tier 1. Peer-led education could leverage medical students’ expertise through campus ‘Vaccine Ambassador’ programs requiring ≥20 contact hours per semester.
Curriculum Reform: We recommend integrating mandatory reproductive health modules into general education curricula, with content co-developed by medical professionals and educators to address myths (e.g., HPV vaccine infertility rumors).
Digital Literacy Campaigns: Partner with influencers and healthcare providers to disseminate accurate information via platforms like WeChat and TikTok.
5 Conclusion
This study elucidates how China’s urban–rural divide, academic pressures, and institutional gaps in health education perpetuate reproductive health disparities. Significant associations were observed between sociodemographic factors education level, household registration, only child status, academic major and reproductive health outcomes. Key findings include pronounced urban–rural inequities, with urban students demonstrating 4.3-fold higher HPV vaccination rates than rural peers, alongside elevated dysmenorrhea prevalence among rural students. Academic stressors significantly impacted health outcomes, as postgraduate students exhibited a 60% higher dysmenorrhea risk versus undergraduates, while paradoxically, medical students showed lower HPV vaccination uptake than non-medical peers, attributed to clinical skepticism about vaccine safety. Furthermore, health education engagement was limited, with 52.4% relying on online platforms for health information—highlighting critical gaps in institutional health promotion and digital misinformation risks. Therefore, addressing these multifaceted socioeconomic, educational, and structural barriers is essential for improving reproductive health equity in this population. By addressing structural barriers and leveraging digital engagement, policymakers can empower female college students to navigate reproductive health challenges effectively.
Strengths: The large, nationally representative sample (n = 1,013) and multilevel regression enhance generalizability.
Limitations: Self-reported data may underreport sensitive issues like sexual health, while the cross-sectional design precludes causal inference regarding academic stress and dysmenorrhea. Cross-sectional design limits causal inference, and self-reported data may introduce bias. Future studies should triangulate with clinical records to reduce bias and explore longitudinal effects. Underrepresentation of rural (37.1%) and postgraduate (4.5%) students may bias estimates. In the future work, we will increase the collection of data on postgraduate students to obtain more valuable information.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Approval was obtained from the Institutional Review Boards of Xiamen Donghai Institute and Pingshan District Central Hospital (No. PSZXYY-2024-334). All participants provided written informed consent, and data were anonymized. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YZ: Data curation, Formal analysis, Funding acquisition, Investigation, Project administration, Validation, Writing – original draft, Writing – review & editing. KK: Conceptualization, Formal analysis, Supervision, Writing – review & editing. MB-Y: Conceptualization, Formal analysis, Supervision, Writing – review & editing. KZ: Data curation, Formal analysis, Validation, Writing – review & editing. RR: Conceptualization, Data curation, Writing – review & editing. WC: Formal analysis, Funding acquisition, Investigation, Project administration, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Research results of Fujian Provincial High-level Specialty; Xiamen Local Industry Service Specialty Group, Xiamen Modern Apprenticeship Demonstration Specialty Project Funding, Xiamen Industry College Project Construction Funding [Xiamen Education Office (2021) No. 48, Xiamen Teaching (2019) No. 9, (2022) No. 60, (2023) No. 08]; Shenzhen Elite Talent Project (2024XKG088); Shenzhen Pingshan District of Health System Research Project (2024334); and Yonsei Post-doctoral Professional Management Program.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1627669/full#supplementary-material
Footnotes
References
1. Starrs, A, Ezeh, A, Sedgh, G, and Singh, S. To achieve development goals, advance sexual and reproductive health and rights. Lancet. (2024) 403:787–9. doi: 10.1016/s0140-6736(23)02360-7
2. Liu, L, Fu, M, Wu, J, Wang, H, Zhao, J, Chen, P, et al. Digital health literacy among undergraduate nursing students in China: associations with health lifestyles and psychological resilience. BMC Med Educ. (2024) 24:1139. doi: 10.1186/s12909-024-06075-w
3. Ansong, E, Arhin, SK, Cai, Y, Xu, X, and Wu, X. Menstrual characteristics, disorders and associated risk factors among female international students in Zhejiang Province, China: a cross-sectional survey. BMC Womens Health. (2019) 19:35. doi: 10.1186/s12905-019-0730-5
4. Rosário, J, Raposo, B, Santos, E, Dias, S, and Pedro, AR. Efficacy of health literacy interventions aimed to improve health gains of higher education students-a systematic review. BMC Public Health. (2024) 24:882. doi: 10.1186/s12889-024-18358-4
5. Wang, W, Yin, R, Cao, W, Wang, Y, Zhang, T, Yan, Y, et al. Assessing parental marital quality and divorce related to youth sexual experiences and adverse reproductive health outcomes among 50,000 Chinese college students. Reprod Health. (2022) 19:219. doi: 10.1186/s12978-022-01531-6
6. Hashemi, M, Kohan, S, and Abdishahshahani, M. Reproductive health self-Care for Female Students: educational needs assessment, Isfahan University of Medical Sciences 2018. J Educ Health Promot. (2020) 9:17. doi: 10.4103/jehp.jehp_378_19
7. Rosenstock, IM. Historical origins of the health belief model. Health Educ Monogr. (1974) 2:328–35. doi: 10.1177/109019817400200403
8. Yuan, D, Li, Q, Zhan, N, Zhang, L, Wang, J, Liu, M, et al. Longitudinal associations of menstrual characteristics with mental health problems among Chinese girls. Eur Child Adolesc Psychiatry. (2024) 33:2547–56. doi: 10.1007/s00787-023-02345-y
9. Yari, A, Kabiri, B, Afzali Harsini, P, and Khani Jeihooni, A. Improving menstrual health knowledge among girls from Iran: the effectiveness of educational health belief model. Women Health. (2024) 64:65–74. doi: 10.1080/03630242.2023.2294970
10. Tang, Y, Fu, R, and Noguchi, H. Impact of medical insurance integration on reducing urban-rural health disparity: evidence from China. Soc Sci Med. (2024) 357:117163. doi: 10.1016/j.socscimed.2024.117163
11. Martín, MS, Chen, FW, and Urbistondo, PA. Impact of telemedicine through social media: a study of topics in user comments on twitter. Research Square (2024). [Epubh ahead of preprint]. doi: 10.21203/rs.3.rs-4885011/v1
12. Mboineki, JF, and Chen, C. Preparing patient navigators and assessing the impact of patient navigation in promoting cervical Cancer screening uptake, knowledge, awareness, intention, and health beliefs: a protocol for a randomized controlled trial. Front Global Women Health. (2024) 5:1209441. doi: 10.3389/fgwh.2024.1209441
13. WHO. (2023). Global strategy to accelerate the elimination of cervical Cancer. Available online at: https://www.who.int/publications/i/item/978924001410
14. Shi, X, Chen, M, Pan, Q, Zhou, J, Liu, Y, Jiang, T, et al. Association between dietary patterns and premenstrual disorders: a cross-sectional analysis of 1382 college students in China. Food Funct. (2024) 15:4170–9. doi: 10.1039/d3fo05782h
15. Fang, P, Zheng, H, Liu, L, Pan, J, Chen, M, Yu, X, et al. Factors influencing knowledge and acceptance of nonavalent human papillomavirus vaccine among university population in southern China: a cross-sectional study. Cancer Control. (2024) 31:10732748241293989. doi: 10.1177/10732748241293989
16. Nair, I, Patel, SP, Bolen, A, Roger, S, Bucci, K, Schwab-Reese, L, et al. Reproductive health experiences shared on Tiktok by young people: content analysis. JMIR Infodemiol. (2023) 3:e42810. doi: 10.2196/42810
17. Rizvi, F, Hoban, E, and Williams, J. Barriers and enablers of contraceptive use among adolescent girls and women under 30 years of age in Cambodia: a qualitative study. Eur J Contracept Reprod Health Care. (2021) 26:284–90. doi: 10.1080/13625187.2021.1884220
18. Chawłowska, E, Lipiak, A, Krzysztoszek, J, Krupa, B, and Staszewski, R. Reproductive health literacy and fertility awareness among polish female students. Front Public Health. (2020) 8:499. doi: 10.3389/fpubh.2020.00499
19. Larson, HJ, Jarrett, C, Eckersberger, E, Smith, DM, and Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. (2014) 32:2150–9. doi: 10.1016/j.vaccine.2014.01.081
20. Garcia, MB, Garcia, PS, Maaliw, RR, Gonzales Lagrazon, PG, Arif, YM, Ofosu-Ampong, K, et al. Technoethical considerations for advancing health literacy and medical practice: a Posthumanist framework in the age of healthcare 5.0. In: Garcia, MB, and de Almeida, RPP, eds. Emerging technologies for health literacy and medical practice. Hershey, PA, USA: IGI Global (2024). 1–19.
21. Çalışkan, C, and Üner, S. Disaster literacy and public health: a systematic review and integration of definitions and models. Disaster Med Public Health Prep. (2021) 15:518–27. doi: 10.1017/dmp.2020.100
22. Zhao, C, Zhao, Y, Li, J, Li, M, Shi, Y, and Wei, L. Opportunities and challenges for human papillomavirus vaccination in China. Hum Vaccin Immunother. (2024) 20:2329450. doi: 10.1080/21645515.2024.2329450
23. Egbon, M, Ojo, T, Aliyu, A, and Bagudu, ZS. Challenges and lessons from a school-based human papillomavirus (Hpv) vaccination program for adolescent girls in a rural Nigerian community. BMC Public Health. (2022) 22:1611. doi: 10.1186/s12889-022-13975-3
24. Coursey, K, Muralidhar, K, Srinivas, V, Jaykrishna, P, Begum, F, Ningaiah, N, et al. Acceptability of Hpv vaccination for cervical Cancer prevention amongst emerging adult women in rural Mysore, India: a mixed-methods study. BMC Public Health. (2024) 24:2139. doi: 10.1186/s12889-024-19485-8
25. Kim, M, Güler, A, Kim, D, and Lee, RC. A qualitative study of ethnic Korean women and men's experiences of Hpv and Hpv vaccination in the United States. Ethn Health. (2024) 29:179–98. doi: 10.1080/13557858.2023.2279933
26. Pereira, VC, Silva, SN, Carvalho, VKS, Zanghelini, F, and Barreto, JOM. Strategies for the implementation of clinical practice guidelines in public health: an overview of systematic reviews. Health Res Policy Syst. (2022) 20:13. doi: 10.1186/s12961-022-00815-4
27. Jin, SW, Lee, Y, and Brandt, HM. Human papillomavirus (Hpv) vaccination knowledge, beliefs, and hesitancy associated with stages of parental readiness for adolescent Hpv vaccination: implications for Hpv vaccination promotion. Trop Med Infect Dis. (2023) 8:251. doi: 10.3390/tropicalmed8050251
Keywords: reproductive health, health education, HPV vaccine hesitancy, sociodemographic determinants, Chinese female college students
Citation: Zhuang Y, Kwang Cheol K, Botabara-Yap MJ, Zhao K, Ramos RIA and Cao W (2025) Factors associated with reproductive health and health education participation among female college students in China. Front. Public Health. 13:1627669. doi: 10.3389/fpubh.2025.1627669
Edited by:
Deep Shikha, Swami Rama Himalayan University, IndiaReviewed by:
Djam Alain, University of Dschang, CameroonDivya Verma, Swami Rama Himalayan University, India
Copyright © 2025 Zhuang, Kwang Cheol, Botabara-Yap, Zhao, Ramos and Cao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenming Cao, Y2Fvd2VubWluZzE5ODNAMTI2LmNvbQ==
 Yiyi Zhuang
Yiyi Zhuang Kim Kwang Cheol2
Kim Kwang Cheol2 Wenming Cao
Wenming Cao