- 1School of Health, University of the Sunshine Coast, Murrumba Downs, QLD, Australia
- 2School of Educational Psychology and Counselling, Monash University, Melbourne, VIC, Australia
Background: Despite public health campaigns promoting infant sleep safety, SUDI (including SIDS and fatal sleep accidents) remains one of the most significant contributors to post-neonatal infant death in many high-income countries. Bedsharing remains common despite predominant risk elimination guidelines, with many families struggling to follow rigid rules of avoidance. Risk minimisation considers the complexities of family life and recognises most infant deaths in shared sleep environments are associated with additional risk factors.
Purpose and methods: Integrative review methodology was used to investigate the information parents need to minimise risk for infants under 12 months who share a sleep surface. Database searches included Scopus, CINAHL, PubMed, PsycNET and Emcare to identify peer-reviewed publications published January 2013–March 2025. Quality appraisal was undertaken using the QuADs tool.
Results: A total of 60 articles met eligibility criteria. Twelve themes were generated from the data and grouped under four key domains: 1. Challenges in creating safer shared sleep environments, 2. Solutions/strategies used by parents to address challenges, 3. Family experiences when risk factors are present, and 4. Information needs of parents and caregivers. Families reported sharing sleep with infants, intentionally and accidentally, including those at a higher risk of SUDI. Bedsharing often occurs outside of a conscious parental ‘choice’, while families frequently refrain from disclosing bedsharing practices to health professionals. In the absence of formal guidance on safer shared sleep strategies, families generated their own solutions potentially increasing risk.
Conclusion: Parents need universal access to non-judgmental, neutrally-worded support that allows them to ‘prepare to share’ and employ strategies to enhance infant sleep safety wherever, and whenever it occurs.
1 Introduction
New parents make frequent, dynamic decisions regarding their baby’s care and safety in the context of their family’s circumstances; including infant sleep location (1, 2). Preparation and decision-making are influenced by cultural and societal norms and values within communities (1, 3, 4), as well as a family’s economic situation including access to stable accommodation and material basics (5, 6). In most non-Western societies, intentionally sharing sleep on the same sleep surface with a baby is the cultural norm (6–15). In Western, Educated, Industrialised, Rich, Democratic (WEIRD) and predominantly white societies (16), cots and cribs dominate perceptions of ‘ideal’ infant sleep practices, with separate sleep location becoming a valued societal norm during the last 200 years (1, 2, 17, 18).
Despite successes of public health campaigns promoting infant sleep safety in the 1990s, reductions in rates of deaths attributed to Sudden Unexpected Death in Infancy [SUDI; including Sudden Infant Death Syndrome (SIDS) and fatal sleep accidents] have slowed, in some nations plateaued (19–21), while even increased in some countries (22, 23). SUDI remains one of the leading contributors to post-neonatal mortality (24). SUDI which occur in shared sleep environments contribute significantly to total infant mortality each year (25–29). Factors known to increase an infant’s vulnerability (smoke-exposure in pregnancy and postnatally; being born premature or of low birth weight; sharing sleep on a sofa, or with an adult under the influence of drugs or alcohol), increase the risk of SIDS and fatal sleep accident (27, 28, 30–41). Scholarly debate (8, 42–44) continues on how to address shared sleep in infant sleep guidance (27, 28, 30–41).
Public health approaches generally fall into three broad categories: 1. Risk elimination as strict instruction (e.g., ‘do not bedshare’) (45, 46), 2. Risk elimination as preferred practice while framing infant sleep practices as parental choice (e.g., ‘it is not safe, but if you choose to, follow these precautions’) (47, 48), and 3. Risk minimisation guidance (e.g., ‘shared sleep is common and happens intentionally and unintentionally’; strategies to reduce risk are provided using neutral language without presenting one option as ‘preferred’ or ‘safest’) (49–53). A rapid review of international documents shows varied language in Western societies to convey these approaches (see Supplementary Table A), supported by a recent evaluation of the consistency of infant safer sleep messaging in Australia by Kruse et al. (54).
Risk elimination, advocated by the American Academy of Pediatrics (AAP), advises against bedsharing under any circumstances (45). This strategy assumes that cribs/cots offer a universal, simple solution for safer infant sleep for all families, with policies focused on ensuring parental compliance with this advice. While the AAP guidelines have influenced safe sleep public health campaigns in many countries, this approach has not significantly reduced SUDI rates which have risen in the US since 2020 (22). Shared sleeping remains a common practice in Western societies for many reasons (8, 21, 42, 55–59).
Shared sleep or bedsharing aligns with human evolutionary design, supporting mothers and infants and prolonging breastfeeding (4, 60–64); strongly suggesting the focus of infant sleep safety should include risk mitigation for shared sleep rather than solely advocating for avoidance. Historically, safe sleep messages have been unidirectional, information giving based on the assumption that a parent’s actions are influenced with information alone (65). Recently, UK and Australian researchers have codesigned safer sleep messages and policy guidelines to improve acceptability and uptake (49, 66, 67).
Building on Salm Ward and Doering’s (68, 69) earlier reviews of mother-infant bedsharing this integrative review examines literature published during the last decade, which centres on shared sleeping using a parent-focused lens. Understanding parent and caregiver experiences with safer sleep advice and information needs is crucial for safer sleep campaigns. By considering diverse family circumstances, this review aims to inform more effective public health messaging and resources. A systematic approach was employed to explore the primary research question: ‘What information do parents want and need to minimise risk if they have an infant under 12 months of age who shares the same sleep surface, intentionally or not?’
2 Methods
An integrative review methodology was chosen to explore the multifaceted phenomenon of shared sleeping because this process supports holistic exploration of complex, health related topics including the flexibility to integrate diverse methodologies (70). Whittemore and Knafl’s five-step integrative review framework (71) was used to guide this review (71): problem identification, literature search, data evaluation, data analysis and presentation.
2.1 Search strategy
Four objectives guided research question development using the PICo model (72) (Population, Phenomenon of Interest, Context), to identify these key concepts: 1. Sleep safety challenges, 2. Strategies used, 3. Family experiences with risk factors, and 4. Parental information needs. Literature databases including Scopus, CINAHL, PubMed, PsycNET, and Emcare were searched using relevant keywords for peer reviewed studies published between January 2013 and 13 March 2025. The search strategy was guided by a university librarian. Eligible studies focused on bed-sharing with infants under 12 months of age and reported primary caregiver perceptions or experiences related to reasons for caregiver-infant bed-sharing, associated challenges, and/or solutions and strategies to address these challenges. Studies were included if they were empirical, peer reviewed publications, including systematically conducted literature reviews and publicly available theses published in English between 1 January 2013 and 13 March 2025. Detailed review objectives, inclusion and exclusion criteria, and search strings are contained in Supplementary Table B.
2.2 Study selection
A systematic search identified 762 studies with 17 additional articles found through a hand search of included reference lists. After duplicate removal (n = 239), two researchers (CG, JY) screened titles and abstracts. A third researcher (TD) joined for full text screening and all discrepancies were resolved through discussion and consensus. Ultimately, 60 articles met eligibility criteria. See Figure 1 for PRISMA (RRID: SCR_018721) flowchart.
2.3 Quality appraisal
The Quality Assessment for Diverse Studies (QuADS) tool (73) was chosen to undertake methodological and reporting quality of eligible studies to capture the complexity and depth of the topic. No studies were excluded based on this quality assessment. Notably, some studies (n = 5, 8%) provide minimal or no detail relating to recruitment data, over a quarter of studies lacked caregiver sampling details appropriate to study aims (n = 17, 28%), and many lacked stakeholder involvement in design (n = 40, 69%; Supplementary Table C).
2.4 Data analysis
Key data points were extracted and tabulated, including authors, study details, shared sleep approaches and grouped across the four key domains related to the review objectives. See Figure 2. Extracted data covered bedsharing rationale, SUDI risk profiles, challenges, solutions, with information needs differentiated as parent perspectives and/or author conclusions. Data analysis followed Whittemore and Knafl’s framework ( 71 ), emphasising data reduction and display. Table 1 contains a summary of data with full extraction details contained in Supplementary Table D.
3 Results
3.1 Eligible study characteristics
Of the 60 eligible studies, the majority were empirical (59/60, 98%) with one narrative literature review. Among empirical studies, 49% (29/59) were qualitative, 33% (n = 20/59) mixed methods, and 15% (n = 9/59) quantitative studies. Publications were spread across the inclusion period ranging from 1 to 9 publications per year.
3.2 Study sample participants
Most studies included women/mothers (54/60, 90%), with 36 (60%) focusing exclusively on women/mothers as participants. Families with increased SUDI risk, frequently considered priority populations for safe sleep messaging, were represented in 55% (n = 33) of studies, including: African-American/American-Indian families (11/33, 33%) (65, 74–83), low socio-economic status (n = 5/33, 15%) (76, 79, 84–86), adolescent mothers (n = 4/33, 12%) (85, 87–89), Māori/ Pasifika families (n = 4/33, 12%) (10, 90–92), premature/low-birthweight infants (n = 4/33, 12%) (93–96), families experiencing social deprivation (n = 4/33, 12%) (80, 96–98), parents with opioid use history (n = 2/33, 6%) (96, 99), and refugee and/or transient families (n = 1/33, 3%) (100). Smoking exposure was noted in 15 studies (15/60, 25%) (75, 79, 85, 91, 92, 96, 97, 100–107). Breastfeeding, a known protective factor, was a focus in eight (13%) studies (60, 74, 80, 108–112).
3.3 Country of origin
Just over half of the studies were from the USA (n = 31, 51.6%), with others from Australasia (20%), Europe (18%), Sub-Saharan Africa (3.5%), Asia (3.5%), and single studies from Jordan, Ecuador, and Canada.
3.4 Approaches used for shared sleep safety
Shared sleep philosophies underpinning the approach to safer sleep messaging and assumptions in published studies were grouped into five categories: (a) risk elimination, viewing all shared sleep as hazardous (n = 20) (74, 75, 78, 80, 82, 83, 86–89, 93, 98–100, 113–118); (b) risk minimisation, acknowledging its occurrence and focusing on reducing risks (n = 17) (60, 76, 84, 92, 95, 97, 101, 103–105, 107–110, 119–121); (c) exploratory, describing the phenomenon without a specific aim of risk reduction or elimination (n = 16) (10, 81, 85, 91, 102, 106, 111, 112, 122–129); (d) exploratory with a risk minimisation aim (n = 5) (65, 90, 94, 96, 130); and (e) exploratory with a risk elimination aim (n = 2) (77, 79). See Table 1.
3.5 Analysis of results
This analysis systematically addresses the four study objectives. Twelve themes generated from the data were grouped under four domains. Themes will be identified, compared and discussed to address the related objectives. Figure 2 summarises key domains and themes.
3.5.1 Domain 1: challenges in creating safer shared sleep environments
Four themes were generated regarding the challenges parents faced in creating safer shared sleep environments: Shared sleep with babies is intentional and unintentional; Intention versus practical reality; Censorship to avoid criticism and judgement; and Mother-centric guidance creates cultural and caregiver gaps in safer sleep education. Despite being advised against co-sleeping (10, 65, 75–79, 83, 88, 90, 93, 95, 96, 98, 106, 113, 116–118), many parents engaged in both intentional and unintentional shared sleep due to the practical challenges and emotional demands of infant care, often without guidance or support. In more than half of the included studies (n = 32, 53%), parent reports consistently suggested that they were unprepared for the reality of infant sleep and related care both day and night (frequent waking, feeding, comfort and settling through co-regulation), and this often led to reactive and/or unintentional (spontaneous) shared sleep (10, 65, 74, 77, 78, 81, 83–85, 87–89, 91, 93–95, 97–99, 103, 106, 111, 113, 115–120, 123, 124, 127, 130). The factors associated with unintentionally falling asleep with a baby included infant-related factors such as night-time feeding requirements (65, 74, 81, 85, 87, 95, 97, 103, 106, 116, 117, 119), infant temperament/preferences (10, 65, 77, 78, 84, 88, 93, 96, 116, 123, 127), infant wakefulness (113, 123, 127), and the need for extra comfort and soothing when babies were unsettled, sick or experiencing discomfort (81, 83, 89, 91, 95, 96, 98, 99, 106, 113, 115, 120, 124). Adult-related factors included the experience of overwhelming exhaustion and fatigue because of the intensity of infant care around sleep (65, 74, 77, 78, 84, 85, 91, 94, 96–99, 103, 111, 113, 116, 117, 120, 130). and maternal anxiety (65, 83, 96).
Unintentional and some forms of reactive sleep (in response to infant need or circumstance) (10, 77, 78, 81, 83–85, 87–89, 91, 93–99, 103, 106, 111, 113, 115–120, 123, 124, 127, 130) often occurred in locations or environments that increase the risk of sleep accidents and SUDI (including SIDS), particularly if no pre-planning was involved (65, 74, 76, 85, 91, 97, 102, 107, 113, 117, 119, 120, 130). The reality of infant care created dynamic challenges for parents as they negotiated meeting their infant’s needs in ways that also met their own physiological need for rest and sleep in the context of their family’s life. The perceived comfort of their infant (or alleviating the experience of discomfort) provided by sharing sleep was a clear priority for parents (10, 60, 65, 77–79, 81–85, 87–89, 91, 95, 98, 99, 103, 108, 112, 113, 116, 123, 124, 127, 130) alongside providing for infant safety. Most parents in the reported studies (n = 34/60) initially planned, and had prepared, a surface (e.g., bassinet/cot) to sleep their baby separately, predominantly due to information provided by health professionals, but reported they now shared sleep some of the time and in some instances, for all sleep due to a variety of reasons (10, 65, 77, 78, 81, 83–85, 87–89, 91, 93–99, 103, 105, 106, 111, 113, 115–120, 123, 124, 127, 130).
Not all parents felt they could openly discuss or even disclose shared sleep with health professionals as they knew it went against recommendations (65, 83–85, 89, 90, 96, 99, 108). Interestingly, 52% of breastfeeding physicians who reported bedsharing in a study by Louis-Jacques et al. (112) did not disclose this practice to their child’s physician (despite being medical peers). A limited number of studies (n = 6) described shared sleeping occurring due to lack of access to a cot/crib/bassinet, including the ability to procure one (75, 79, 92, 95, 117, 121). Parents reported that many health professionals did not appear to be forthcoming with risk minimisation strategies (65, 76, 110). In the absence of formal guidance, parents self-generated strategies and solutions to address their safety fears/concerns and minimise risk for their infant (See Table 2). The most common parental fears were of potential smothering or suffocation (65, 83, 91, 95–97, 113, 115, 121, 122), baby rolling off the bed or other sleep surface (couch/sofa) (65, 76, 78, 88, 89, 94, 99, 103, 108, 113, 116, 121, 130), co-sleeping itself (i.e., bedsharing) so sleeping on a sofa to avoid bedsharing (65, 74, 76, 116, 119, 120, 130), the fear of choking or aspiration (77, 79, 96, 121) and fragility of their baby which drove a parental compulsion--often described as a need--to share sleep in order to monitor baby closely. This was further evident in reports by parents of premature or medically complex babies (93, 94, 96, 122), and babies experiencing withdrawals from opioids (96, 99). Table 2 provides a summary of the solutions which parents employed to address challenges stemming from parent fears.
While mothers were participants in 90% (n = 54) of eligible studies and were exclusive participants in 60% (n = 36), it was clear that for many of the families, other caregivers (usually fathers and grandmothers) provided direct care for the infant (10, 77–79, 84, 85, 88, 91, 97, 107, 127). Fathers and other caregivers sharing sleep with infants were reported in 17 studies (10, 77–80, 84, 87, 90, 98, 116, 119–121, 123, 128–130). Limited guidance for the broader caregiving circle created challenges for mothers, who had to share and ‘enforce’ safe sleep advice while managing differing opinions (83, 87). This led to conflicts in some families (83, 87, 94), especially as other caregivers, often responsible for daytime infant care, had varying practices (78, 94). Studies indicated that sleep safety was often less prioritised during daytime and times of changed routine (78, 84, 97, 99, 103, 113, 120).
Nine studies utilised the term ‘parent’, ‘parenting’ and/or ‘parental’ in framing discussion of research methods, results and findings but the data were unclear if caregivers other than the mother were present in the infant’s sleep environment (75, 88, 93, 95, 110, 113, 115, 122, 125). Analysis of infant deaths was fraught with similar concerns. For example, the term ‘adults’ was used by Pease et al. (107) in a comparative analysis of infant deaths (n = 540) occurring between 1993 and 2020. Results from a retrospective cohort study (n = 477 infant deaths) by Bamber et al. (102) indicated that some of these deaths occurred in the presence of more than one adult, without any description of the adult’s relationship with the infant. In contrast, Weil’s (89) bivariate analysis of sleep related infant deaths in a Illinois dataset, identified the presence of fathers and ‘other’ persons at the times of death.
Breastfeeding was encouraged in cohorts with and without an increased risk of SUDI due to the many benefits breastfeeding offers for both mothers and their babies (75, 76, 79–81, 90–92, 94, 110, 112). Breastfeeding and co-sleeping practices are closely related and mutually supportive. Parents found the advice to avoid co-sleeping challenging as it seemingly contradicted the practical implications of successful breastfeeding (90, 108).
3.5.2 Domain 2: solutions and strategies to address challenges
Two themes were identified related to solutions and strategies: Proactive bedsharing decisions contribute to sleep safety insights; and Unplanned sleep sharing increases risks for infants. Results indicated that parents who proactively planned to bedshare with their infant actively attempted to minimise risk in their shared sleep environment and sometimes sought access to resources and information to guide their attempts (65, 76–79, 84, 88–92, 94–97, 99, 101, 103, 108, 113, 115, 116, 121, 129, 130). Some solutions generated by parents were in alignment with contemporary risk minimisation approaches (49) for example keeping loose bedding/pillows away from baby (65, 76, 84, 113, 116), use of a firm, flat mattress (108, 120, 122) and not smoking if bed-sharing or during pregnancy (76, 84, 91, 113, 122). Other actions may have inadvertently increased risk (49) such as sleeping on chairs/sofas to avoid bed-sharing (65, 74, 76, 116, 119, 120, 130) or placing blankets/pillows around baby or on floor for protection in an attempt to prevent or cushion a potential fall (65, 76, 88, 99, 103, 113, 116) (please see Table 3 for a summary of the alignment of parent-generated solutions to address safer shared sleeping challenges with current risk minimisation strategies).
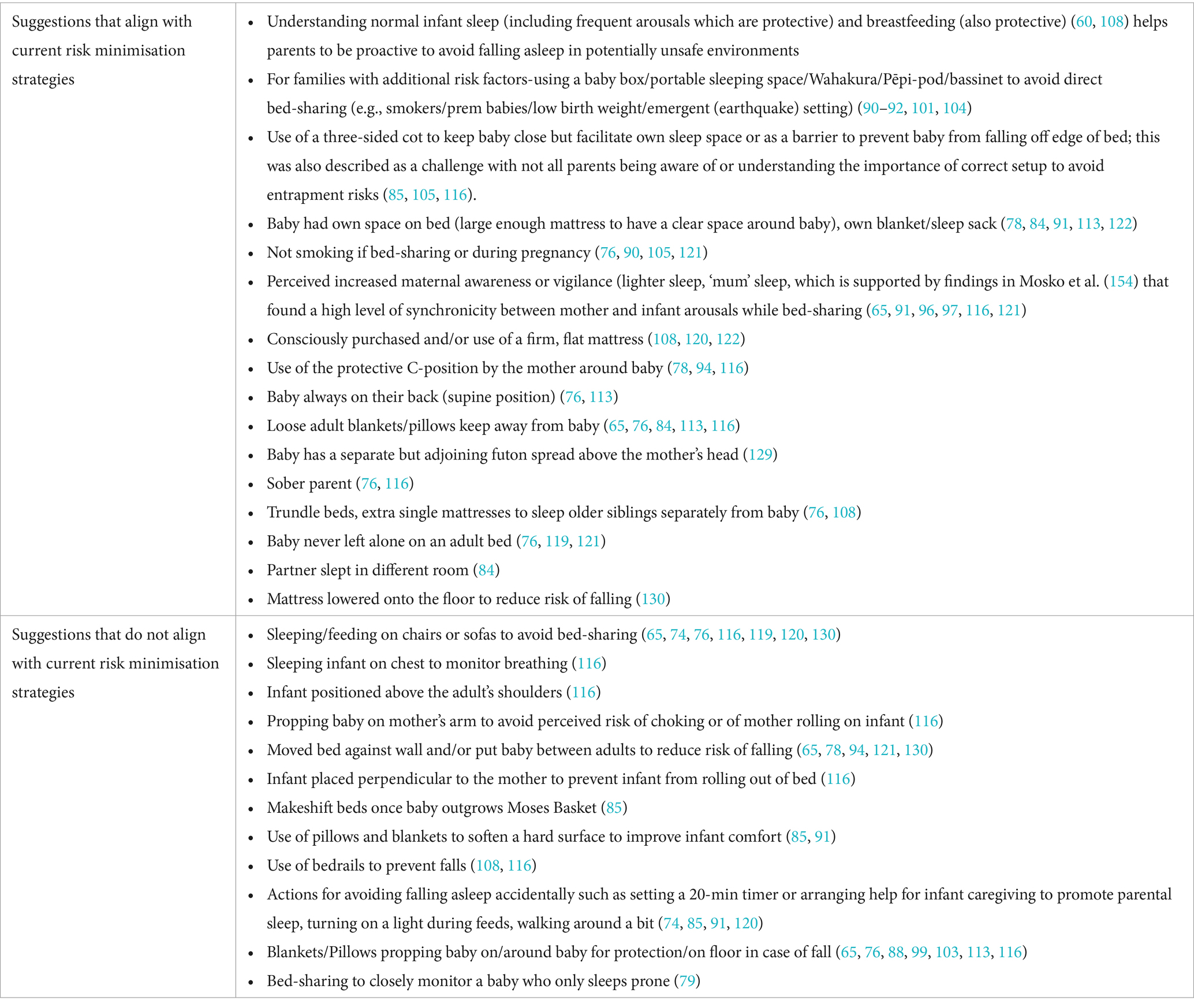
Table 3. Alignment of parent-generated solutions to address safer shared sleeping challenges with current risk minimisation strategies.
Safety concerns prompted these parental solutions related to suffocation, baby rolling or falling, co-sleeping itself, choking/aspiration, the infant’s perceived fragility and infant’s comfort (alleviating perceived discomfort; see Table 2). Some parents, particularly those participating in studies based in North America, accessed alternative guidance (to the AAP) such as La Leche League International’s Safe Sleep 7 guidance to inform their risk minimisation actions (94, 113).
The presence of siblings and older children in the household was reported in 39% (n = 22) of the eligible literature; and in some instances, were described as sharing the bed with the mother and infant (117, 128, 129). Some studies described actions parents took to facilitate a separate sleep space for their older child/ren, to separate from the new baby (e.g., trundle beds) (76, 108).
3.5.3 Domain 3: family experience when risk factors are present
Four themes were generated regarding the experience of families when risk factors were present: Families share sleep for similar reasons regardless of risk profile; Exclusive focus on risk elimination for families with risk factors; Risk elimination overlooks spontaneous shared sleep occurrences; Portable sleep spaces enable safer co-sleeping for vulnerable babies. There was broad agreement (83%, n = 50/60) across the literature that certain factors are associated with a higher risk of SUDI, particularly in the shared sleep environment. These circumstances include an infant who is smoke-exposed, premature, low birthweight, non-sober caregiver (alcohol or drug-effected), young maternal age, low socioeconomic status, infant not breastfed or a member of a priority population (population groups who have been identified as having higher rates of SUDI than the general population). In these circumstances, it appeared to be the norm for any form of shared sleep to be advised against regardless of whether the research study was utilising a risk elimination, exploratory, or risk minimisation approach to guide recommendations for practice (10, 60, 75–80, 82–95, 97–111, 113–120, 122, 124, 128, 130). A distinct exception was Barrett et al. (96) who recommended practitioners discuss safer ways of co-sleeping as part of the safer sleep planning for these particular families. Parents and families who met criteria for one or more of these associated risk factors frequently expressed awareness of the advice not to co-sleep with their infant (10, 75, 76, 79, 80, 84, 87, 90–94, 96–99). However, results of this review strongly indicated that these families are sharing sleep for similar reasons as their lower-risk peers (Table 4). Most parents (majority mothers) from these priority populations planned to sleep their baby separately but reported they now shared sleep intermittently or regularly (10, 77, 78, 83, 87–89, 91, 93–99, 120). Parents felt unable to discuss their practices with health professionals due to fear of judgment, stigma, or punitive action, including child safety referrals, consistent with their ‘low risk’ counterparts (84, 89, 96, 99). Parents reported that few health professionals were forthcoming with risk minimisation strategies (76, 110).
In contrast, evaluations of several, novel in-bed portable sleep space (PSS) programs (NZ Pēpi-Pod® Program (91, 92, 104) and wahakura programs (91)) described valuable culturally-appropriate tools that supported parents to make shared sleep safer in the first few months of life (41, 131, 132). McIntosh et al. (91) conducted a randomised controlled trial in New Zealand with 211 women who met eligibility criteria including maternal smoking, second-hand smoke exposure, low birthweight, airway issues, or a family history of SUDI. The Pēpi-Pod® (in-bed infant sleep space designed for 0–4 months) was widely accepted and used by nearly half of participants at 2 months. However, bedsharing remained high (61% at 2 months, 81% at 4 months, when most infants had outgrown the pod). The intervention also appeared to support breastfeeding, likely due to close maternal–infant contact. Similarly, in an evaluation by Cowan et al. (104), 13% of parents were direct bedsharing after discontinuing use of the Pēpi-Pod® when their baby had outgrown the device. Importantly, the primary purpose of Pēpi-Pod Program® (sleep space dimensions: 72cmL x 40cmW x 15.5 cm) and wahakura programs is not to eliminate bedsharing, but rather to support close, proximate care while protecting vulnerable, smoke-exposed infants during a developmentally vulnerable period (0–14 weeks) from suffocation (133). Infant airway protection strategies are key features of Pēpi-Pod Program® educational materials (133, 134). Notably, results indicate a continued occurrence of direct bedsharing before, during and after implementation. Similarly, Hauck et al. (75) reported that 16% of participants in the U. S. National Crib Distribution Program continued bedsharing, with no report of risk reduction strategies provided. Ball et al. (101) evaluated two infant sleep spaces: a shallow, transparent propylene box (72.5cmL x 33.5cmW x 18cmH) with safe sleep information (written and video), and a higher-sided (65cmL x 40cmW x 28cmH), opaque cardboard box with access to on-line education. Parents preferred the lower-sided propylene option, describing easier visual and physical access to their baby in addition to hygiene and portability benefits (101). Salm Ward et al. (117) also reported that 28.8% of 66 respondents sometimes fell asleep with their infants on sofas, chairs, or in bed while feeding during follow-up of a safe sleep and crib distribution program.
3.5.4 Domain 4: information needs of parents and caregivers
Two themes related to the information needs of parents and caregivers were identified: Risk elimination is incompatible with practical reality; ‘Prepare to share’: universal, neutral risk minimisation advice is needed for all, regardless of intent. Few studies (n = 4/60) collected and described parents’ information needs on shared sleep (4/60) (77, 89, 94, 113) or safe sleep more broadly (n = 6/60) (65, 78, 93, 96, 97, 115). Only 11% (7/60) explored preferred delivery of existing messages (65, 78, 82, 83, 89, 91, 97) while 56% (34/60) offered author-led recommendations for future safe sleep information provision to parents (See Supplementary Table D for individual study detail). Notably, 35% (21/60) called for more guidance to improve shared sleep safety (60, 65, 74, 76, 84, 85, 92, 95–97, 101, 103–105, 107–110, 119–121).
Of the 10 studies addressing parental perspectives on their information needs for shared or safer sleep (65, 77, 78, 89, 93, 94, 96, 97, 113, 115), findings showed a clear desire for practical risk minimisation strategies to support sleep, shared sleep and infant sleep positioning. Herman et al. (77), noted that current safe infant sleep recommendations often fail to meet real-world needs; a view echoed in 46% (28/60) of studies in which parents found that the advice not to co-sleep was not always achievable in practice (10, 65, 75–81, 83, 84, 91, 93, 95–99, 103, 105, 106, 115–117, 120, 123, 124, 130). Parents in other studies described safe sleep advice as ‘unrealistic’ (65, 113), ‘not feasible’ (115), ‘condescending’ (97), ‘ridiculous’ (87), and ‘rigid’ (89) and ‘not incorporating the needs of the child’ (89). Some reported that advice not to co-sleep went against their instinct (88, 90, 97) or was not applicable to them (85, 108, 111, 119, 127, 130). Pakistani mothers in a study by Crane and Ball (119) repeatedly expressed that the safe sleep guidance was not written for them, but for their white counterparts. These findings highlight the need for culturally sensitive, relevant and inclusive safer sleep advice (119, 127).
Parents requested targeted safer sleep education to include the broader infant caregiving circle to help combat the conflicting advice and care practices parents face, when information provision is mother-centric (10, 77–79, 84, 85, 88, 91, 94, 97, 107, 127). Social supports (in-community and online) were identified as important, timely sources of information to mothers as they navigate the complexity of infant sleep, their child’s dynamic development, and their family’s life (89, 96, 115). Results indicate there is a wide variation in the quality of the safer sleep advice provided within these, often unmoderated, spaces (115).
Results suggest that mothers are motivated and feel confident in minimising suffocation risks (89), however parents often believe ‘SIDS’ is largely an unavoidable phenomenon, and feel they can do little to ‘prevent’ it (78, 79, 83). Understanding the rationale underpinning safer sleep recommendations was a priority for mothers in two UK-based studies (96, 97). These mothers expressed the desire for health professionals to take the time to explain why they advised certain practices and to allow parents time to absorb the information and ask questions. Participants expressed the need for individualised and collaborative conversations with trusted others (96, 97). Fathers too, wanted to be treated as competent, responsible infant caregivers and for messaging to acknowledge their active involvement (78).
4 Discussion
This review explored the research question: ‘What information do parents want and need to minimise risk if they have an infant under 12 months of age who shares the same sleep surface, intentionally or not?’. The challenges parents and caregivers face in navigating safer sleep messaging, the strategies parents employed in making shared sleep safer for their baby, parental experiences with higher risk infants, and the information they seek, were identified. This discussion provides a synthesis of these findings, comparing and contrasting themes generated from this review with those originally identified by Salm Ward (69) over a decade ago. Education, practice and policy implications for contemporary health professionals and families will also be presented.
The literature highlights several challenges parents face in creating safer shared sleep environments. Many parents share sleep, intentionally and unintentionally, due to factors such as infant needs (e.g., nighttime feeding, comfort) and exhaustion, despite being aware of associated risks in some circumstances. Acknowledging parental fatigue as a separate driver for shared sleep is an important addition to Salm Ward’s (69) earlier findings. This finding highlights the common and consistent occurrence of unintentional shared sleep due to parent exhaustion (65, 74, 77, 78, 84, 85, 91, 94, 96–99, 103, 111, 113, 116, 117, 120, 130), a phenomenon not adequately addressed by safe sleep approaches that assume shared sleep is always a conscious choice (68, 69).
Human sleep physiology dictates that we will sleep (135) and in the postpartum context, breastfeeding-induced hormones also promote sleep (13, 74, 136, 137). Given our human biology, it seems appropriate that sleep safety policies should educate parents on the likelihood of falling asleep with their baby, regardless of intention, and provide strategies for how to prepare the environment to make it safer if it occurs (60, 65, 74–76, 85, 93, 98, 106, 117, 119, 120, 122). Simply having a separate sleep space, and an intention not to share, is likely to be insufficient (65, 74). Providing universal, neutral guidance on how to minimise risks when sharing sleep can help prevent sleep-related accidents, including among ‘accidental bedsharers’. Preparing families with this information is not a promotion of bedsharing, nor an endorsement. Rather, this prepare to share approach recognises that many parents do- and will-bedshare, and ensures they have access to evidence-based safety information regardless of intent or circumstance.
This review highlighted a gap in the current literature, demonstrating that most education on sleep safety focusses on mothers, often overlooking the roles of other caregivers. This reflects an outdated assumption of a nuclear family model, excluding the important role of fathers and multigenerational caregiving, which could be leveraged in future infant sleep safety approaches. Earlier recommendations by Pease et al. support the need for safer sleep messaging to include all caregivers (138).
Although it is well documented that parents and caregivers often share sleep with their infants, research frequently lacks clarity about who exactly is involved (75, 82, 87, 89, 90, 92, 98, 101, 103, 119, 122, 125). Ambiguous and inconsistent language, especially in studies reporting infant deaths (102, 107), makes it difficult to determine the identity, relationship, and caregiving role (active or passive) of those sharing the sleep environment. These details are vital for accurately assessing risk and tailoring education and support to specific family circumstances. While previous research has highlighted the need to consider partners in bedsharing (13), and this review underscores the involvement of a broader range of caregivers beyond parents.
This review supports earlier findings (40, 139) that infant sleep safety is often deprioritised during daytime naps, routine disruptions (e.g., illness, travel) and emergencies (78, 97, 99, 103, 113). Future risk minimisation guidelines should address these contexts specifically (49), such as the Australian Breastfeeding Association’s Supporting Safer Sleep for Babies in Evacuation Centres (140). Parents and carers desire guidance in safely adapting to novel environments while continuing to act responsively to their baby’s needs.
Extensive accounts in the contemporary literature highlighted an earlier finding from Rowe (141): parental intentions to balance family sleep needs while maximising infant safety (10, 60, 65, 77–79, 81–85, 87–89, 91, 95, 96, 98, 99, 103, 108, 113, 116, 123, 124, 127, 130). When following standard safe sleep advice (i.e., risk elimination or risk elimination as preferred practice) was not feasible, parents created their own solutions especially to prevent infant rolling or falls (from the bed/sleep space), often without formal guidance.
A concerning finding was that many parents fear judgement and feel unsafe disclosing bedsharing with healthcare providers, leading to underreporting (65, 83–85, 89, 90, 96, 99, 109). Salm Ward and Doering’s (68) review also highlighted stigma as a key factor contributing to underreporting. These results demonstrate that parents and carers have a clearly expressed desire, and need, for health professionals to engage in open, non-judgemental conversations regarding bedsharing and to provide anticipatory guidance without negative rhetoric (65, 96, 142). Proactive guidance from health professionals is the safest and most appropriate option, as merely providing risk minimisation guidance after shared sleep disclosure is insufficient. This approach overlooks parents who either do not disclose or unintentionally share sleep for many and diverse reasons, as highlighted in this review (65, 96). Parents who reported bedsharing offered valuable insights into safer sleep strategies. Their contributions highlighted practical gaps and the utility of risk minimisation approaches. Incorporating parental expertise and experiences could improve safer sleep messaging, as supported by Pease et al. (138).
Intention to bedshare appeared to be associated with better preparation and uptake of practices which protect an infant’s airway. In line with findings from the Salm Ward review (69), parents who plan to bedshare were more likely to take steps to minimise risks, while unplanned shared sleep (60, 75, 76, 85, 93, 98, 106, 117, 119, 120, 122), and in particular, sofa sharing (29, 74, 76, 85, 91, 97, 102, 107, 113, 117, 119, 120, 130), may increase the likelihood of fatal sleeping accidents and SUDI. These findings, again, highlight the imperative for accessible risk minimisation resources as part of universal safer sleep guidance, regardless of a parent’s sleep location plan (65). An important finding from this review is that families with factors increasing SUDI risk, share sleep with their infants for similar reasons as lower-risk counterparts. This was also evident in Salm Ward’s earlier review (69). This raises concern about the blanket advice to avoid co-sleeping, which fails to consider the dynamic and complex interplay of infant and adult sleep needs. Factors such as feeding (breast, bottle, mixed), settling, soothing and adult sleep environment all contribute to shared sleep plans and actions, which are not always intentional. Unintentional, spontaneous shared sleep exists beyond active, parental choice, regardless of risk profile. Ignoring non-volitional aspects of sleep may worsen outcomes for marginalised families, deepen disparities in infant sleep safety, and fail to address the universal challenge of managing sleep needs of both infant and their families (4).
Results from this review indicate the need to address socio-economic conditions (e.g., poverty, housing, food and job insecurity) (103, 143) that drive factors increasing the risk of SUDI. Smoking, substance use and lower breastfeeding rates (4, 37, 136, 144, 145) are all associated with social deprivation. For families and their babies to thrive, efforts to address these factors require sustained, meaningful effort to reduce systemic factors which fuel disparities in communities (5, 6, 143, 144, 146).
The use of portable, in-bed sleeping devices (e.g., Pēpi-Pod® Program or wahakura) for vulnerable infants (e.g., smoke-exposed, LBW, premature) within culturally appropriate education programs offers a safer sleep intervention that aligns with families’ preferences to keep their baby close in bed. This approach is supported by New Zealand and Australian findings, and emphasise the importance of trust, culturally competent delivery, and parent involvement in successful health promotion, which has been associated with infant mortality reductions in both countries (28, 134). However a recent study evaluation has also highlighted how monitoring for program fidelity is essential to ensure such programs are delivered as intended and reach the target population (147). While these in-bed sleep devices provide safer sleep options for vulnerable babies, they do not eliminate the need for ongoing risk minimisation guidance, especially once babies grow out of the spaces (usually by 4–5 months) as bed-sharing remains common in the early years of childhood. Recent Australian clinical guidelines, codesigned and based on risk minimisation (49) have emphasised this importance of considering the interaction of sleep environments and the dynamic growth and development of infants, particularly during their first year.
Parents in this review clearly expressed that the current safe sleep messaging approaches, based on risk elimination, are insufficient to meet their needs, particularly for non-white, non-Western cultures, where bed-sharing is a common practice. Many parents suggested or clearly stated that the current advice and messages were not applicable or practicable to them (10, 65, 75–81, 83, 84, 91, 93, 95–99, 103, 105, 106, 115–117, 119, 120, 123, 124, 130). These findings are supported by Volpe and Ball (148) who identified ‘trade-offs’ between aligning with or against safe sleep guidance was a reality for most mothers. Interestingly, despite parents reporting that risk elimination advice and actual infant care were incompatible, many studies continued to reinforce, in their conclusions, the importance of risk elimination messaging, sometimes contradicting or failing to respond to the evidence they presented (75, 77–80, 93, 98, 99, 113, 115, 117).
Parents were open to, and desired opportunities, to learn ways to improve safety while bed-sharing with their infants. This supports findings identified in the Salm Ward review that messaging on safer bed-sharing was needed (69). There was a distinct and expressed need for advice to encompass all infant caregivers, not only mothers. Online social support was valued for providing timely answers, support and solidarity as they navigated their infant’s needs and evolving family circumstances (89, 115).
Caregivers (mostly mothers) expressed a need for non-judgemental support from health professionals to improve shared sleep safety through conversations, and specifically time to process and ask questions about the rationale underpinning safer sleep guidance (96, 97). Understanding the ‘why’ or the rationale underpinning messages emerged as a key finding to inform future research and public health campaigns. Developing improved messaging including safer sleep conversations that incorporate the reasons for advice may help parents better apply these understandings when responding in novel sleep situations (96, 97).
4.1 Research opportunities
This review identified several research opportunities, particularly the need for studies that investigate best practice approaches to incorporate identified parent information needs, including risk minimisation strategies, into parent-facing resources with parents and caregivers involved as key stakeholders. Parents have articulated several fears and safety concerns relevant to current infant sleep messaging highlighting the importance of participatory research approaches supporting the co-development and co-design of safer infant sleep messages, campaigns and specific interventions with parents as active contributors (149).
Building on findings by Shiells et al. (150), there is potential to improve the impact of safer sleep information by using evidence-based behaviour change models, such as COM-B, to focusing on factors influencing human actions, including capabilities, opportunities and motivations. The Baby Sleep Planner (66), developed through co-design with parents and practitioners in the UK, offers an interesting and potentially promising framework for developing and evaluating context specific resources in different locations (151).
Parent fatigue was a distinct and relatively unexplored driver of unintentional shared sleep. Future research should investigate the contextual factors and environments that contribute to unintentional shared sleep among fatigued parents, evaluate how safer sleep interventions can be adapted to acknowledge and address caregiver exhaustion without resulting in increased caregiver-infant separation, early breastfeeding cessation or reduction in parental responsiveness (18, 152, 153), and explore the influence of support systems in reducing fatigue-related sleep risks, including the role of other family members.
Shared sleep safety for broader caregiving circles including other family members, and the influence of shared sleeping with older infants, toddlers and children is also a priority for further exploration. Review findings also highlighted a paucity of studies examining shared sleep safety from the perspectives of parents and caregivers with multiple infants, disabilities (physical, cognitive, psychosocial), and from Australian Aboriginal and Torres Strait Islander families, culturally and linguistically diverse families, LGBTIQA+ families, and foster carers.
4.2 Strengths and limitations
Infant sleep safety is a public health priority, and the integrative review method provided a robust framework to critically analyse both qualitative and quantitative findings for ‘evidence-based patient-oriented healthcare’ (70). Building on Salm Ward’s study (69), this review expanded the scope to include parents, caregivers, challenges, solutions, priority group needs, and implications for health professional support, offering a contemporary perspective on infant mortality prevention. An expert librarian guided the search strategy to ensure inclusion of relevant evidence since 2013, and the QuADS tool assessed the methodological quality of diverse studies (71).
Notable limitations are the focus on English-language publications, which may bias the review towards WEIRD populations, and an absence of broader cultural wisdom and perspectives. Some study samples were un-representative of their target parent cohorts (e.g., 97% of participants were mothers rather than broader ‘parent’ or ‘caregiver’ cohorts described in study aims and conclusions), with a considerable proportion of studies lacking detailed description of recruitment outcomes (n = 21, 35% scored ≤2, QuADS tool-Question 9, Supplementary Table C) potentially contributing to sampling bias. Although approaches to shared sleep messaging vary in the literature, many study authors did not state their assumptions, instead implicitly adopting a risk elimination lens that shaped interpretations of caregiver ‘noncompliance’ and information needs. Although the QuADS tool assessed study quality, no cut-off level was established for exclusion, resulting in varying levels of methodological rigor and transparency in reporting across studies.
5 Conclusion
Current safer sleep guidelines often assume that shared sleep is a deliberate decision, yet the insights from this review highlight the critical mismatch between policy assumptions and real-world behaviour. Shared sleep is common for many families and embracing this reality with proactive education and guidelines is vital to ensure the safety of infants, day and night. Families deserve support that reflects their lived experiences. This review has highlighted that parents are willing and able to co-create evidence-based resources, public health campaigns and strategies that empower parents with the knowledge they need to make shared sleep safer. Evidence from this review challenges researchers, policy makers and health professionals to shift their focus from risk elimination approaches by acknowledging the prevalence of shared sleep, fostering collaboration with consumers, and prioritising co-designed risk minimisation education that meets the needs of contemporary parents. In doing so, we can make safer shared sleep a shared priority wherever, and whenever, it occurs.
Author contributions
CG: Validation, Methodology, Conceptualization, Investigation, Writing – review & editing, Visualization, Data curation, Writing – original draft, Formal analysis. JY: Writing – review & editing, Formal analysis, Methodology, Writing – original draft, Data curation, Conceptualization, Validation, Investigation, Visualization, Supervision. TD: Data curation, Supervision, Investigation, Writing – review & editing. LD'S: Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. CG was the recipient of the University of the Sunshine Coast 2022 Roberta M. C. Taylor Rural and Remote Nursing and Midwifery Scholarship.
Acknowledgments
The authors would like to acknowledge the contribution of Anna Pease in providing a critical review of this manuscript prior to submission.
Conflict of interest
JY has been seconded from UniSC to support the Queensland Government’s scaled implementation of the Pēpi-Pod® Program. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1629678/full#supplementary-material
References
1. Ramos, PV , Hoogerwerf, PJ , Smith, PK , Finley, C , Okoro, UE , and Jennissen, CA . Pre- and postnatal safe sleep knowledge and planned as compared to actual infant sleep practices. Inj Epidemiol. (2023) 10:55. doi: 10.1186/s40621-023-00467-0
2. Lau, A , and Hall, W . Safe sleep, day and night: mothers' experiences regarding infant sleep safety. J Clin Nurs. (2016) 25:2816–26. doi: 10.1111/jocn.13322
3. Salm Ward, TC , Robb, SW , and Kanu, FA . Prevalence and characteristics of bed-sharing among black and white infants in Georgia. Matern Child Health J. (2016) 20:347–62. doi: 10.1007/s10995-015-1834-7
4. Reimer, A , Specker, BL , Hockett, CW , Strasser, K , Ahrendt, L , and McCormack, LA . Factors associated with breastfeeding initiation and continuation at two months postpartum in American Indian women: an exploratory analysis. Am Indian Alsk Native Ment Health Res. (2024) 31:71–92. doi: 10.5820/aian.3101.2024.71
5. Alston, M , Thomas, D , Jambulingam, M , Hunt, A , Grover, R , Bronner, L, et al. Examining the relationship between sleep-related infant deaths and social determinants of health in urban communities. J Racial Ethn Health Disparities. (2022) 9:779–85. doi: 10.1007/s40615-021-01016-5
6. Bartick, M , and Tomori, C . Sudden infant death and social justice: a syndemics approach. Matern Child Nutr. (2019) 15:e12652. doi: 10.1111/mcn.12652
7. Ahn, YM , Yang, KM , Ha, HI , and Cho, JA . Cultural variation in factors associated with sudden infant death during sleep. BMC Pediatr. (2021) 21:443. doi: 10.1186/s12887-021-02894-8
8. Ball, HL , and Volpe, LE . Sudden infant death syndrome (SIDS) risk reduction and infant sleep location - moving the discussion forward. Soc Sci Med. (2013) 79:84–91. doi: 10.1016/j.socscimed.2012.03.025
9. Subcomision de Lactancia, M , Trabajo de Muerte Subita, Grupo , del Inesperada, L , Jenik, A , and Conti, R . Bedsharing at home, breastfeeding and sudden infant death.Recommendations for health professionals. Arch Argent Pediatr (2017); 115:s105–s110. doi: 10.5546/aap.2017.s105
10. Fangupo, LJ , Lucas, AW , Taylor, RW , Camp, J , and Richards, R . Sleep and parenting in ethnically diverse Pacific families in southern New Zealand: a qualitative exploration. Sleep Health. (2022) 8:89–95. doi: 10.1016/j.sleh.2021.11.002
11. Hernández Rivero, C . Colecho, sueño y lactancia humana. Gac Med Caracas. (2021) 129:S652–8. doi: 10.47307/GMC.2021.129.s3.19
12. Owens, JA . Sleep in children: cross-cultural perspectives. Sleep Biol Rhythms. (2004) 2:165–73. doi: 10.1111/j.1479-8425.2004.00147.x
13. Mileva-Seitz, VR , Bakermans-Kranenburg, MJ , Battaini, C , and Luijk, MP . Parent-child bed-sharing: the good, the bad, and the burden of evidence. Sleep Med Rev. (2017) 32:4–27. doi: 10.1016/j.smrv.2016.03.003
14. Netsi, E , Santos, IS , Stein, A , Barros, FC , Barros, AJD , and Matijasevich, A . A different rhythm of life: sleep patterns in the first 4 years of life and associated sociodemographic characteristics in a large Brazilian birth cohort. Sleep Med. (2017) 37:77–87. doi: 10.1016/j.sleep.2017.06.001
15. Sharts-Hopko, NC . Co-sleeping. MCN Am J Matern Child Nurs. (2005) 30:142. doi: 10.1097/00005721-200503000-00020
16. Fuentes, A . WEIRD indeed, but there is more to the story: anthropological reflections on Henrich’s “the weirdest people in the world”. Relig, Brain Behav. (2022) 12:284–90. doi: 10.1080/2153599X.2021.1991458
17. Byars, KC , and Simon, SL . Behavioral treatment of pediatric sleep disturbance: ethical considerations for pediatric psychology practice. Clin Pract Pediatr Psychol. (2016) 4:241–8. doi: 10.1037/cpp0000149
18. D'Souza, L , and Cassels, T . Contextual considerations in infant sleep: offering alternative interventions to families. Sleep Health. (2023) 9:618–25. doi: 10.1016/j.sleh.2022.05.006
19. Vincent, A , Chu, NT , Shah, A , Avanthika, C , Jhaveri, S , Singh, K, et al. Sudden infant death syndrome: risk factors and newer risk reduction strategies. Cureus. (2023) 15:e40572. doi: 10.7759/cureus.40572
20. Hauck, FR , and Tanabe, KO . Beyond "Back to sleep": ways to further reduce the risk of sudden infant death syndrome. Pediatr Ann. (2017) 46:e284–90. doi: 10.3928/19382359-20170721-01
21. Cole, R , Young, J , Kearney, L , and Thompson, JMD . Infant care practices, caregiver awareness of safe sleep advice and barriers to implementation: a scoping review. Int J Environ Res Public Health. (2022) 19:7712. doi: 10.3390/ijerph19137712
22. Centers for Disease Control and Prevention . (2024). Trends in SUID rates by cause of death, 1990—2022: Centers for Disease Control and Prevention. Available online at: https://www.cdc.gov/sudden-infant-death/data-research/data/sids-deaths-by-cause.htmlhttps://www.cdc.gov/sudden-infant-death/data-research/data/sids-deaths-by-cause.html (Accessed February 13, 2025).
23. de Visme, S , Chalumeau, M , Levieux, K , Patural, H , Harrewijn, I , Briand-Huchet, E, et al. National variations in recent trends of sudden unexpected infant death rate in Western Europe. J Pediatr. (2020) 226:179–185.e4. doi: 10.1016/j.jpeds.2020.06.052
24. Rhoda, NR , Turawa, E , Engel, M , Ayouni, I , Zuhlke, L , Coetzee, D, et al. Prevalence of sudden unexpected death of infants and its subcategories in low- or middle-income countries: a systematic review protocol. BMJ Open. (2025) 15:e091246. doi: 10.1136/bmjopen-2024-091246
25. Carpenter, R , McGarvey, C , Mitchell, EA , Tappin, DM , Vennemann, MM , Smuk, M, et al. Bed sharing when parents do not smoke: is there a risk of SIDS? An individual level analysis of five major case-control studies. BMJ Open. (2013) 3:e002299. doi: 10.1136/bmjopen-2012-002299
26. Heathfield, LJ , Martin, LJ , and Ramesar, R . A 5-year retrospective analysis of infant death at Salt River mortuary, Cape Town. SAJCH S Afr J Child Health. (2020) 14:148–54. doi: 10.7196/SAJCH.2020.v14i3.1720
27. MacFarlane, ME , Thompson, JMD , Wilson, J , Lawton, B , Taylor, B , Elder, DE, et al. Infant sleep hazards and the risk of sudden unexpected death in infancy. J Pediatr. (2022) 245:56–64. doi: 10.1016/j.jpeds.2022.01.044
28. Mitchell, EA , Thompson, JM , Zuccollo, J , MacFarlane, M , Taylor, B , Elder, D, et al. The combination of bedsharing and maternal smoking leads to a greatly increased risk of sudden unexpected death in infancy: the new Zealand Nationwide SUDI case control study. N Z Med J. (2017) 130:52–64.
29. Queensland Family and Child Commission (2023). Deaths of children and young people Queensland 2022–23
30. Bartick, M , Tomori, C , and Ball, HL . Babies in boxes and the missing links on safe sleep: human evolution and cultural revolution. Matern Child Nutr. (2018) 14:e12544. doi: 10.1111/mcn.12544
31. Blair, PS , Sidebotham, P , Pease, A , and Fleming, PJ . Bed-sharing in the absence of hazardous circumstances: is there a risk of sudden infant death syndrome? An analysis from two case-control studies conducted in the UK. PLoS One. (2014) 9:e107799. doi: 10.1371/journal.pone.0107799
32. Carlin, RF , and Moon, RY . Risk factors, protective factors, and current recommendations to reduce sudden infant death syndrome: a review. JAMA Pediatr. (2017) 171:175–80. doi: 10.1001/jamapediatrics.2016.3345
33. Colvin, JD , Collie-Akers, V , Schunn, C , and Moon, RY . Sleep environment risks for younger and older infants. Pediatrics. (2014) 134:e406–12. doi: 10.1542/peds.2014-0401
34. Fitzgerald, DA , Jeffery, H , Arbuckle, S , du Toit-Prinsloo, L , O'Sullivan, T , and Waters, K . Sudden unexpected death in infancy [SUDI]: what the clinician, pathologist, coroner and researchers want to know. Paediatr Respir Rev. (2022) 41:14–20. doi: 10.1016/j.prrv.2021.08.002
35. Fleming, P , Pease, A , and Blair, P . Bed-sharing and unexpected infant deaths: what is the relationship? Paediatr Respir Rev. (2015) 16:62–7. doi: 10.1016/j.prrv.2014.10.008
36. Garstang, JJ , and Sidebotham, P . Qualitative analysis of serious case reviews into unexpected infant deaths. Arch Dis Child. (2019) 104:30–6. doi: 10.1136/archdischild-2018-315156
37. Godoy, M , and Maher, M . A ten-year retrospective case review of risk factors associated with sleep-related infant deaths. Acta Paediatr. (2022) 111:1176–85. doi: 10.1111/apa.16281
38. Jullien, S . Sudden infant death syndrome prevention. BMC Pediatr. (2021) 21:320. doi: 10.1186/s12887-021-02536-z
39. Kanits, F , L'Hoir, MP , Boere-Boonekamp, MM , Engelberts, AC , and Feskens, EJM . Risk and preventive factors for SUDI: need we adjust the current prevention advice in a low-incidence country. Front Pediatr. (2021) 9:758048. doi: 10.3389/fped.2021.758048
40. Rechtman, LR , Colvin, JD , Blair, PS , and Moon, RY . Sofas and infant mortality. Pediatrics. (2014) 134:e1293–300. doi: 10.1542/peds.2014-1543
41. Watson, K . An evaluation of a safe sleep health promotion strategy amongst aboriginal and Torres Strait islander families and health care providers. Queensland: University of the Sunshine Coast (2018).
42. Cole, R , Young, J , Kearney, L , and Thompson, JMD . Infant care practices and parent uptake of safe sleep messages: a cross-sectional survey in Queensland, Australia. BMC Pediatr. (2020) 20:27. doi: 10.1186/s12887-020-1917-5
43. Gordon, RA , Rowe, HL , and Garcia, K . Promoting family resilience through evidence-based policy making: reconsidering the link between adult–infant bedsharing and infant mortality. Fam Relat. (2015) 64:134–52. doi: 10.1111/fare.12099
44. Hauck, FR , Darnall, RA , and Moon, RY . Parent-infant bedsharing is not recommended. JAMA Pediatr. (2014) 168:387–8. doi: 10.1001/jamapediatrics.2013.5169
45. Moon, RY. (2023). How to keep your sleeping baby safe: AAP policy explained healthychildren.org: American Academy of Pediatrics; Available online at: https://www.healthychildren.org/English/ages-stages/baby/sleep/Pages/A-Parents-Guide-to-Safe-Sleep.aspx (Accessed February 21, 2024).
46. HealthEd . (2023). Keep your baby safe during sleep - HE1228: Ministry of Health. Available online at: https://healthed.govt.nz/products/keep-your-baby-safe-during-sleep#:~:text=The%20full%20resource:%20Every%20year,%20too (Accessed October 1, 2024).
47. Red Nose Australia . (2024). Co-sleeping with your baby: Red Nose Australia. Available online at: https://rednose.org.au/article/Co-sleeping_with_your_baby (Accessed February 21, 2024).
48. The Lullaby Trust . (2025). Co-sleeping with your baby: The Lullaby Trust. Available online at: https://www.lullabytrust.org.uk/safer-sleep-advice/co-sleeping/ (Accessed July 26, 2025).
49. Queensland Clinical Guidelines . (2022). Safer Infant sleeping. In: Queensland health, editor. Guideline No. MN22.71V1-R27 ed. Australia: State of Queensland.
50. Blair, PS , Ball, HL , McKenna, JJ , Feldman-Winter, L , Marinelli, KA , Bartick, MC, et al. Bedsharing and breastfeeding: the academy of breastfeeding medicine protocol #6, revision 2019. Breastfeed Med. (2020) 15:5–16. doi: 10.1089/bfm.2019.29144.psb
51. UNICEF UK . (2022). Caring for your baby at night: United Kingdom committee for UNICEF. Available online at: https://www.unicef.org.uk/babyfriendly/wp-content/uploads/sites/2/2018/08/Caring-for-your-baby-at-night-web.pdf (Accessed February 21, 2024).
52. Australian College of Midwives . (2014). Position statement for bed sharing and co-sleeping. Australian College of Midwives. Available online at: https://midwives.org.au/Web/Web/About-ACM/Guiding-Documents.aspx#:~:text=Midwives%20should%20be%20aware%20of,%20and (Accessed September 19, 2024).
53. National Institute for Health and Care Excellence (2021). Postnatal Care: NICE guideline [NG194] UK: NICE National Institute for Health and Care Excellence. Available online at: https://www.nice.org.uk/guidance/ng194/chapter/recommendations#bed-sharing (Accessed February 22, 2022).
54. Kruse, SP , D’Souza, L , Young, J , and Tuncer, HGG . A systematic evaluation and comparison of the consistency of infant safer sleep messaging in Australia. Front Commun. (2025):10. doi: 10.3389/fcomm.2025.1527164
55. Bombard, JM , Kortsmit, K , Warner, L , Shapiro-Mendoza, CK , Cox, S , Kroelinger, CD, et al. Vital signs: trends and disparities in infant safe sleep practices - United States, 2009-2015. MMWR Morb Mortal Wkly Rep. (2018) 67:39–46. doi: 10.15585/mmwr.mm6701e1
56. Kanits, F , L'Hoir, MP , Boere-Boonekamp, MM , Engelberts, AC , and Feskens, EJM . Renewed attention needed for prevention of sudden unexpected death in infancy in the Netherlands. Front Pediatr. (2021) 9:757530. doi: 10.3389/fped.2021.757530
57. McKenna, JJ , and Gettler, LT . Supporting a 'bottom-up,' new, no-holds-barred, psycho-anthro-pediatrics: making room (scientifically) for bedsharing families. Sleep Med Rev. (2017) 32:1–3. doi: 10.1016/j.smrv.2016.06.003
58. Rudzik, AEF , and Ball, HL . Biologically normal sleep in the mother-infant dyad. Am J Hum Biol. (2021) 33:e23589. doi: 10.1002/ajhb.23589
59. Gates, K , Chahin, S , Damashek, A , Dickson, C , Lubwama, G , Lenz, D, et al. The relation of maternal psychosocial risk factors to infant safe sleep practices. Matern Child Health J. (2024) 28:1061–71. doi: 10.1007/s10995-023-03880-5
60. Barry, ES , and McKenna, JJ . Reasons mothers bedshare: a review of its effects on infant behavior and development. Infant Behav Dev. (2022) 66:101684. doi: 10.1016/j.infbeh.2021.101684
61. Karaburun, IEG , and Yalcin, SS . Breast refusal: an analysis of frequency, onset timing, recovery status, and their interplay with breastfeeding self-efficacy and maternal depression. BMC Public Health. (2024) 24:3568. doi: 10.1186/s12889-024-21023-5
62. Wood, NK , and Helfrich-Miller, KR . Changes in breastfeeding relationships when frontline essential working mothers return to work during the COVID-19 pandemic: a longitudinal qualitative online study. J Adv Nurs. (2025) 81:409–22. doi: 10.1111/jan.16219
63. Wolf, RL , Skobic, I , Pope, BT , Zhu, A , Chamas, H , Sharma, N, et al. Mother-infant bed-sharing is associated with increased breastfeeding: a systematic review. Breastfeed Med. (2025) 20:205–18. doi: 10.1089/bfm.2024.0060
64. McKenna, JJ , and Gettler, LT . There is no such thing as infant sleep, there is no such thing as breastfeeding, there is only breastsleeping. Acta Paediatr. (2016) 105:17–21. doi: 10.1111/apa.13161
65. Sahud, H , Berger, RP , Hamm, M , Heineman, E , Cameron, F , Wasilewski, J, et al. Understanding parental choices related to infant sleep practices in the United States using a mixed methods approach. BMC Pediatr. (2025) 25:9. doi: 10.1186/s12887-024-05332-7
66. Pease, A , Ingram, J , Lambert, B , Patrick, K , Pitts, K , Fleming, PJ, et al. A risk assessment and planning tool to prevent sudden unexpected death in infancy: development and evaluation of the baby sleep planner. JMIR Pediatr Parent. (2024) 7:e49952. doi: 10.2196/49952
67. Metro North Health . (2023). Co-design in metro north health, creating better healthcare together: Queensland Government (metro north health). Available online at: https://metronorth.health.qld.gov.au/get-involved/co-design#:~:text=Co-design%20in%20Metro%20North%20Health.%20Creating (Accessed August 5, 2024).
68. Salm Ward, TC , and Doering, JJ . Application of a socio-ecological model to mother-infant bed-sharing. Health Educ Behav. (2014) 41:577–89. doi: 10.1177/1090198114543010
69. Salm Ward, TC . Reasons for mother–infant bed-sharing: a systematic narrative synthesis of the literature and implications for future research. Matern Child Health J. (2015) 19:675–90. doi: 10.1007/s10995-014-1557-1
70. Dhollande, S , Taylor, A , Meyer, S , and Scott, M . Conducting integrative reviews: a guide for novice nursing researchers. J Res Nurs. (2021) 26:427–38. doi: 10.1177/1744987121997907
71. Whittemore, R , and Knafl, K . The integrative review: updated methodology. J Adv Nurs. (2005) 52:546–53. doi: 10.1111/j.1365-2648.2005.03621.x
72. Denzin, NK , and Lincoln, YS . The sage handbook of qualitative research. 3rd ed. Thousand Oaks, CA: Sage Publications Ltd. (2005). xix p.
73. Harrison, R , Jones, B , Gardner, P , and Lawton, R . Quality assessment with diverse studies (QuADS): an appraisal tool for methodological and reporting quality in systematic reviews of mixed- or multi-method studies. BMC Health Serv Res. (2021) 21:144. doi: 10.1186/s12913-021-06122-y
74. Hauck, FR , Moon, RY , Kerr, SM , Corwin, MJ , Heeren, T , Colson, E, et al. Mothers falling asleep during infant feeding. Pediatrics. (2024) 154:72. doi: 10.1542/peds.2024-066072
75. Hauck, FR , Tanabe, KO , McMurry, T , and Moon, RY . Evaluation of bedtime basics for babies: a national crib distribution program to reduce the risk of sleep-related sudden infant deaths. J Community Health. (2015) 40:457–63. doi: 10.1007/s10900-014-9957-0
76. Gaydos, LM , Blake, SC , Gazmararian, JA , Woodruff, W , Thompson, WW , and Dalmida, SG . Revisiting safe sleep recommendations for African-American infants: why current counseling is insufficient. Matern Child Health J. (2015) 19:496–503. doi: 10.1007/s10995-014-1530-z
77. Herman, S , Adkins, M , and Moon, RY . Knowledge and beliefs of African-American and American Indian parents and supporters about infant safe sleep. J Community Health. (2015) 40:12–9. doi: 10.1007/s10900-014-9886-y
78. Hirsch, HM , Mullins, SH , Miller, BK , and Aitken, ME . Paternal perception of infant sleep risks and safety. Inj Epidemiol. (2018) 5:9. doi: 10.1186/s40621-018-0140-4
79. Mathews, AA , Joyner, BL , Oden, RP , Alamo, I , and Moon, RY . Comparison of infant sleep practices in African-American and US Hispanic families: implications for sleep-related infant death. J Immigr Minor Health. (2015) 17:834–42. doi: 10.1007/s10903-014-0016-9
80. Kadakia, A , Joyner, B , Tender, J , Oden, R , and Moon, RY . Breastfeeding in African Americans may not depend on sleep arrangement: a mixed-methods study. Clin Pediatr (Phila). (2015) 54:47–53. doi: 10.1177/0009922814547565
81. Lerner, RE , Camerota, M , Tully, KP , and Propper, C . Associations between mother-infant bed-sharing practices and infant affect and behavior during the still-face paradigm. Infant Behav Dev. (2020) 60:101464. doi: 10.1016/j.infbeh.2020.101464
82. Zoucha, R , Walters, CA , Colbert, AM , Carlins, E , and Smith, E . Exploring safe sleep and SIDS risk perception in an African-American community: focused ethnography. Public Health Nurs. (2016) 33:206–13. doi: 10.1111/phn.12235
83. Stiffler, D , Matemachani, SM , and Crane, L . Considerations in safe to sleep® messaging: learning from African–American mothers. J Spec Pediatr Nurs. (2020) 25:e12277. doi: 10.1111/jspn.12277
84. Clarke, J . Velcro babies: A qualitative study exploring maternal motivations in the night-time care of infants. Christchurch, New Zealand: University of Otago (2016).
85. Ellis, C . Safely sleeping?: An exploration of mothers' understanding of safe sleep practices and factors that influence reducing risks in their infant's sleep environment [Ph.D.]. England: University of Warwick (United Kingdom) (2019).
86. Feld, H , Ceballos Osorio, J , Bahamonde, M , Young, T , Boada, P , and Rayens, MK . Poverty and paternal education associated with infant safe sleep intentions in a peri-urban community in Ecuador. Glob Pediatr Health. (2021) 8:2333794X211044112. doi: 10.1177/2333794X211044112
87. Yuma-Guerrero, PJ , Duzinski, SV , Brown, JM , Wheeler, TC , Barczyk, AN , and Lawson, KA . Perceptions of injury and prevention practices among pregnant and parenting teenagers. J Trauma Nurs. (2013) 20:3–9. doi: 10.1097/JTN.0b013e3182866157
88. Caraballo, M , Shimasaki, S , Johnston, K , Tung, G , Albright, K , and Halbower, AC . Knowledge, attitudes, and risk for sudden unexpected infant death in children of adolescent mothers: a qualitative study. J Pediatr. (2016) 174:78–83.e2. doi: 10.1016/j.jpeds.2016.03.031
89. Weil, LE . Prevention of unintentional, sleep-related infant deaths: Current sleep practices, caregiver beliefs, and promotion of safe sleep practices through effective preventive interventions. US: ProQuest Information & Learning (2020).
90. George, M , Theodore, R , Richards, R , Galland, B , Taylor, R , Matahaere, M, et al. Moe Kitenga: a qualitative study of perceptions of infant and child sleep practices among Māori whānau. AlterNative Int J Indig Peoples. (2020) 16:153–60. doi: 10.1177/1177180120929694
91. MacFarlane, M , Thompson, JMD , Mitchell, EA , Lawton, B , McLardy, EM , Jonas, SD, et al. Pēpē‐infant sleep practices and sudden unexpected death in infancy in Aotearoa New Zealand. Int J Gynaecol Obstet. (2021) 155:305–17. doi: 10.1002/ijgo.13910
92. McIntosh, C , Trenholme, A , Stewart, J , and Vogel, A . Evaluation of a sudden unexpected death in infancy intervention programme aimed at improving parental awareness of risk factors and protective infant care practices. J Paediatr Child Health. (2018) 54:377–82. doi: 10.1111/jpc.13772
93. Capper, B , Damato, EG , Gutin-Barsman, S , and Dowling, D . Mothers' decision making concerning safe sleep for preterm infants: what are the influencing factors? Adv Neonatal Care. (2022) 22:444–55. doi: 10.1097/ANC.0000000000000952
94. Hwang, SS , Parker, MG , Colvin, BN , Forbes, ES , Brown, K , and Colson, ER . Understanding the barriers and facilitators to safe infant sleep for mothers of preterm infants. J Perinatol. (2021) 41:1992–9. doi: 10.1038/s41372-020-00896-5
95. Tully, KP , Holditch-Davis, D , and Brandon, D . The relationship between planned and reported home infant sleep locations among mothers of late preterm and term infants. Matern Child Health J. (2015) 19:1616–23. doi: 10.1007/s10995-015-1672-7
96. Barrett, S , Barlow, J , Cann, H , Pease, A , Shiells, K , Woodman, J, et al. Parental decision making about safer sleep practices: a qualitative study of the perspectives of families with additional health and social care needs. PLoS One. (2024) 19:e0298383. doi: 10.1371/journal.pone.0298383
97. Pease, A , Ingram, J , Blair, PS , and Fleming, PJ . Factors influencing maternal decision-making for the infant sleep environment in families at higher risk of SIDS: a qualitative study. BMJ Paediatr Open. (2017) 1:e000133. doi: 10.1136/bmjpo-2017-000133
98. Beth Howard, M , Parrish, BT , Singletary, J , and Jarvis, L . Infant safe sleep in the District of Columbia: better for both. Health Promot Pract. (2024) 25:196–203. doi: 10.1177/15248399221131834
99. Morrison, TM , Standish, KR , Wanar, A , Crowell, L , Safon, CB , Colvin, BN, et al. Drivers of decision-making regarding infant sleep practices among mothers with opioid use disorder. J Perinatol. (2023) 43:923–9. doi: 10.1038/s41372-023-01701-9
100. Hamadneh, S , Kassab, M , Hamadneh, J , and Amarin, Z . Sudden unexpected infant death in Jordan and the home environment. Pediatr Int. (2016) 58:1333–6. doi: 10.1111/ped.13016
101. Ball, HL , Taylor, CE , and Yuill, CM . A box to put the baby in: UK parent perceptions of two baby box programmes promoted for infant sleep. Int J Environ Res Public Health. (2021) 18:1473. doi: 10.3390/ijerph182111473
102. Bamber, AR , Kiho, L , Upton, S , Orchard, M , and Sebire, NJ . Social and behavioural factors in non-suspicious unexpected death in infancy; experience from metropolitan police project indigo investigation. BMC Pediatr. (2016) 16:6. doi: 10.1186/s12887-016-0541-x
103. Cole, R , Young, J , Kearney, L , and Thompson, JMD . Challenges parents encounter when implementing infant safe sleep advice. Acta Paediatr. (2021) 110:3083–93. doi: 10.1111/apa.16040
104. Cowan, S , Bennett, S , Clarke, J , and Pease, A . An evaluation of portable sleeping spaces for babies following the Christchurch earthquake of February 2011. J Paediatr Child Health. (2013) 49:364–8. doi: 10.1111/jpc.12196
105. Gaertner, VD , Malfertheiner, SF , Postpischil, J , Brandstetter, S , Seelbach-Gobel, B , Apfelbacher, C, et al. Implementation of safe infant sleep recommendations during night-time sleep in the first year of life in a German birth cohort. Sci Rep. (2023) 13:875. doi: 10.1038/s41598-023-28008-1
106. Hutchison, BL , Thompson, JM , and Mitchell, EA . Infant care practices related to sudden unexpected death in infancy: a 2013 survey. N Z Med J. (2015) 128:15–22.
107. Pease, A , Turner, N , Ingram, J , Fleming, P , Patrick, K , Williams, T, et al. Changes in background characteristics and risk factors among SIDS infants in England: cohort comparisons from 1993 to 2020. BMJ Open. (2023) 13:e076751. doi: 10.1136/bmjopen-2023-076751
108. Bailey, C . Breastfeeding mothers' experiences of bedsharing: a qualitative study. Breastfeed Rev. (2016) 24:33–40.
109. Bailey, C , Tawia, S , and McGuire, E . Breastfeeding duration and infant sleep location in a cohort of volunteer breastfeeding counselors. J Hum Lact. (2020) 36:354–64. doi: 10.1177/0890334419851801
110. Huber, R , Menon, M , Russell, RB , Smith, S , Scott, S , and Berns, SD . Community infant safe sleep and breastfeeding promotion and population level-outcomes: a mixed methods study. Midwifery. (2024) 132:103953. doi: 10.1016/j.midw.2024.103953
111. Rudzik, AEF , and Ball, HL . Exploring maternal perceptions of infant sleep and feeding method among mothers in the United Kingdom: a qualitative focus group study. Matern Child Health J. (2016) 20:33–40. doi: 10.1007/s10995-015-1798-7
112. Louis-Jacques, AF , Bartick, M , Awomolo, A , Zhang, J , Feldman-Winter, L , Leonard, SA, et al. Bedsharing among breastfeeding physicians: results of a nationwide survey. PLoS One. (2024) 19:e0305625. doi: 10.1371/journal.pone.0305625
113. Moon, RY , Mindell, JA , Honaker, S , Keim, S , Roberts, KJ , McAdams, RJ, et al. The tension between AAP safe sleep guidelines and infant sleep. Pediatrics. (2024) 153:1. doi: 10.1542/peds.2023-064675
114. Osei-Poku, GK , Mwananyanda, L , Elliot, PA , MacLeod, WB , Somwe, SW , Pieciak, RC, et al. Assessing infant sleep practices and other risk factors of SIDS in Zambia: a cross-sectional survey of mothers in Lusaka, Zambia. BMC Pediatr. (2022) 22:660. doi: 10.1186/s12887-022-03712-5
115. Pretorius, K , Choi, E , Kang, S , and Mackert, M . Sudden infant death syndrome on Facebook: qualitative descriptive content analysis to guide prevention efforts. J Med Internet Res. (2020) 22:e18474. doi: 10.2196/18474
116. Salm Ward, TC . "things changed very quickly": maternal intentions and decision-making about infant sleep surface, location, and position. Birth. (2024) 51:373–83. doi: 10.1111/birt.12793
117. Salm Ward, TC , Miller, TJ , and Naim, I . Evaluation of a multisite safe infant sleep education and crib distribution program. Int J Environ Res Public Health. (2021) 18:6956. doi: 10.3390/ijerph18136956
118. Shin, SH , Choi, C , Shih, SF , Tomlinson, CA , and Kimbrough, T . A hospital-based infant safe sleep intervention and safe sleep practices among Young women: a prospective longitudinal study. Matern Child Health J. (2023) 27:2113–20. doi: 10.1007/s10995-023-03716-2
119. Crane, D , and Ball, HL . A qualitative study in parental perceptions and understanding of SIDS-reduction guidance in a UK bi-cultural urban community. BMC Pediatr. (2016) 16:23. doi: 10.1186/s12887-016-0560-7
120. Doering, JJ , Lim, PS , Salm Ward, TC , and Davies, WH . Prevalence of unintentional infant bedsharing. Appl Nurs Res. (2019) 46:28–30. doi: 10.1016/j.apnr.2019.02.003
121. Osei-Poku, GK , Mwananyanda, L , Elliott, PA , MacLeod, WB , Somwe, SW , Pieciak, RC, et al. Qualitative assessment of infant sleep practices and other risk factors of sudden infant death syndrome (SIDS) among mothers in Lusaka, Zambia. BMC Pediatr. (2023) 23:245. doi: 10.1186/s12887-023-04051-9
122. Doering, JJ , Marvin, A , and Strook, S . Parent decision factors, safety strategies, and fears about infant sleep locations. Appl Nurs Res. (2017) 34:29–33. doi: 10.1016/j.apnr.2017.01.002
123. Gettler, LT , Kuo, PX , Sarma, MS , Lefever, JEB , Cummings, EM , McKenna, JJ, et al. Us fathers' reports of bonding, infant temperament and psychosocial stress based on family sleep arrangements. Evol Med Public Health. (2021) 9:460–9. doi: 10.1093/emph/eoab038
124. Gilmour, H , Ramage-Morin, PL , and Wong, SL . Infant bed sharing in Canada. Health Rep. (2019) 30:13–9. doi: 10.25318/82-003-x201900700002-eng
125. Gustafsson, S , Jacobzon, A , Lindberg, B , and Engstrom, A . Parents' strategies and advice for creating a positive sleep situation in the family. Scand J Caring Sci. (2022) 36:830–8. doi: 10.1111/scs.13020
126. Hwang, SS , Rybin, DV , Heeren, TC , Colson, ER , and Corwin, MJ . Trust in Sources of advice about infant care practices: the SAFE study. Matern Child Health J. (2016) 20:1956–64. doi: 10.1007/s10995-016-2011-3
127. Luijk, MP , Mileva-Seitz, VR , Jansen, PW , van IJzendoorn, MH , Jaddoe, VW , Raat, H, et al. Ethnic differences in prevalence and determinants of mother-child bed-sharing in early childhood. Sleep Med. (2013) 14:1092–9. doi: 10.1016/j.sleep.2013.04.019
128. Murray, L , Tran, T , Thang, VV , Cass, L , and Fisher, J . How do caregivers understand and respond to unsettled infant behaviour in Vietnam? A qualitative study. Child Care Health Dev. (2018) 44:62–70. doi: 10.1111/cch.12474
129. Shimizu, M , Park, H , and Greenfield, PM . Infant sleeping arrangements and cultural values among contemporary Japanese mothers. Front Psychol. (2014) 5:718. doi: 10.3389/fpsyg.2014.00718
130. Cunningham, HM , Vally, H , and Bugeja, L . Bed-sharing in the first 8 weeks of life: an Australian study. Matern Child Health J. (2018) 22:556–64. doi: 10.1007/s10995-017-2424-7
131. Tipene-Leach, D , and Abel, S . Innovation to prevent sudden infant death: the wahakura as an indigenous vision for a safe sleep environment. Aust J Prim Health. (2019) 25:406–9. doi: 10.1071/PY19033
132. Young, J , and Shipstone, R . Shared sleeping surfaces and dangerous sleeping environments In: JR Duncan and RW Byard , editors. SIDS sudden infant and early childhood death: The past, the present and the future. Adelaide (AU): University of Adelaide Press (2018)
133. Young, J , Watson, K , Craigie, L , Neville, J , and Hunt, J . Best practice principles for research with aboriginal and Torres Strait islander communities in action: case study of a safe infant sleep strategy. Women Birth. (2019) 32:460–5. doi: 10.1016/j.wombi.2019.06.022
134. McEniery, J.A. YJ , Cruice, D.C. , Archer, J. , and Thompson, J.M.D. (2022). Measuring the effectiveness of the Pēpi-pod® program in reducing infant mortality in Queensland. State of Queensland. Available online at: https://www.childrens.health.qld.gov.au/__data/assets/pdf_file/0017/176120/d8ea8e6a94ab355470c435a2363fbc6cfc129023.pdf (Accessed August 10, 2025).
135. Grandner, MA , and Fernandez, FX . The translational neuroscience of sleep: a contextual framework. Science. (2021) 374:568–73. doi: 10.1126/science.abj8188
136. Gutierrez-de-Teran-Moreno, G , Ruiz-Litago, F , Ariz, U , Fernandez-Atutxa, A , Mulas-Martin, MJ , Benito-Fernandez, E, et al. Successful breastfeeding among women with intention to breastfeed: from physiology to socio-cultural factors. Early Hum Dev. (2022) 164:105518. doi: 10.1016/j.earlhumdev.2021.105518
137. Marinelli, KA , Ball, HL , McKenna, JJ , and Blair, PS . An integrated analysis of maternal-infant sleep, breastfeeding, and sudden infant death syndrome research supporting a balanced discourse. J Hum Lact. (2019) 35:510–20. doi: 10.1177/0890334419851797
138. Pease, A , Garstang, JJ , Ellis, C , Watson, D , Ingram, J , Cabral, C, et al. Decision-making for the infant sleep environment among families with children considered to be at risk of sudden unexpected death in infancy: a systematic review and qualitative metasynthesis. BMJ Paediatr Open. (2021) 5:e000983. doi: 10.1136/bmjpo-2020-000983
139. Hayman, RM , McDonald, G , Baker, NJ , Mitchell, EA , and Dalziel, SR . Infant suffocation in place of sleep: New Zealand national data 2002-2009. Arch Dis Child. (2015) 100:610–4. doi: 10.1136/archdischild-2014-306961
140. Australian Breastfeeding Association KidSafe Queensland Inc.and University of the Sunshine Coast . (2024). Supporting safer sleep for babies in evacuation centres [fact sheet]. Australian Breastfeeding Association. Available online at: https://www.breastfeeding.asn.au/emergency-resources-babies-and-toddlers (Accessed July 31, 2025).
141. Rowe, J . A room of their own: the social landscape of infant sleep. Nurs Inq. (2003) 10:184–92. doi: 10.1046/j.1440-1800.2003.00167.x
142. Nelson, CS , Wissow, LS , and Cheng, TL . Effectiveness of anticipatory guidance: recent developments. Curr Opin Pediatr. (2003) 15:630–5. doi: 10.1097/00008480-200312000-00015
143. Shipstone, RA , Young, J , Kearney, L , and Thompson, JMD . Applying a social exclusion framework to explore the relationship between sudden unexpected deaths in infancy (SUDI) and social vulnerability. Front Public Health. (2020) 8:563573. doi: 10.3389/fpubh.2020.563573
144. Hauck, FR , and Blackstone, SR . Maternal smoking, alcohol and recreational drug use and the risk of SIDS among a US urban black population. Front Pediatr. (2022) 10:809966. doi: 10.3389/fped.2022.809966
145. Jawed, A , and Jassal, M . When there is no air, the cradle will fall: a narrative review of tobacco-related content across infant safe sleep interventions. Front Pediatr. (2022) 10:994702. doi: 10.3389/fped.2022.994702
146. McManus, V , Abel, S , McCreanor, T , and Tipene-Leach, D . Narratives of deprivation: women's life stories around Maori sudden infant death syndrome. Soc Sci Med. (2010) 71:643–9. doi: 10.1016/j.socscimed.2010.04.028
147. Mitchell, EA , Cowan, S , Wilson, J , and Thompson, J . Who is supplied with in-bed sleepers (Pēpi-pod and Wahakura) for reducing SUDI in New Zealand? J Paediatr Child Health. (2025) 1–8. doi: 10.1111/jpc.70136
148. Volpe, LE , Ball, HL , and McKenna, JJ . Nighttime parenting strategies and sleep-related risks to infants. Soc Sci Med. (2013) 79:92–100. doi: 10.1016/j.socscimed.2012.05.043
149. Mery, JN , Vladescu, JC , Sidener, TM , Reeve, KF , and Day-Watkins, J . Safe to sleep: a systematic review of the safe infant sleep training literature across relevant personnel. J Neonatal Nurs. (2021) 27:381–95. doi: 10.1016/j.jnn.2021.06.001
150. Shiells, K , Cann, H , Pease, A , McGovern, R , Woodman, J , Barrett, S, et al. A behaviour change analysis of safer sleep interventions for infants at risk of sudden and unexpected death. Child Abuse Rev. (2024) 33:2860. doi: 10.1002/car.2860
151. Pease, A , Lambert, B , Ingram, J , Bradley, N , Fleming, P , Blair, PS, et al. Baby sleep project protocol: a realist evaluation of an intervention to reduce preventable infant mortality. BMJ Open. (2025) 15:e091414. doi: 10.1136/bmjopen-2024-091414
152. Tomori, C , Palmquist, AE , and Dowling, S . Contested moral landscapes: negotiating breastfeeding stigma in breastmilk sharing, nighttime breastfeeding, and long-term breastfeeding in the U.S. and the U.K. Soc Sci Med. (2016) 168:178–85. doi: 10.1016/j.socscimed.2016.09.014
153. Whittingham, K , and Douglas, P . Optimizing parent–infant sleep from birth to 6 months: a new paradigm. Infant Ment Health J. (2014) 35:614–23. doi: 10.1002/imhj.21455
Keywords: newborn health, public health interventions, maternal health, health disparities, sleep health, infant sleep safety, social determinants of health, sudden unexpected death in infancy
Citation: Grubb C, Young J, Downer T and D’Souza L (2025) Beyond the rules: an integrative review of parental perspectives on safer infant sleep in shared environments. Front. Public Health. 13:1629678. doi: 10.3389/fpubh.2025.1629678
Edited by:
Camille Aupiais, Université Sorbonne Paris Nord, FranceReviewed by:
Anna Pease, University of Bristol, United KingdomSophie De Visme, INSERM, Délégation régionale Grand-Ouest, France
Peter Blair, University of Bristol, United Kingdom
Copyright © 2025 Grubb, Young, Downer and D’Souza. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Carly Grubb, Y21nMDM1QHN0dWRlbnQudXNjLmVkdS5hdQ==
 Carly Grubb
Carly Grubb Jeanine Young
Jeanine Young Terri Downer
Terri Downer Levita D’Souza
Levita D’Souza