- 1Department of Community Health and Epidemiology, College of Medicine, University of Saskatchewan, Saskatoon, SK, Canada
- 2Department of Global Public Health, Karolinska Institutet (KI), Solna, Sweden
Background: Self-rated health (SRH) is a globally recognized measure of health status. Previous studies have established that inadequate sleep duration and trouble falling asleep combinedly has a greater negative impact on health than either factor alone. This study aims to investigate the excess relative risk due to the interaction between short sleep duration and trouble sleeping on SRH.
Method: We used the 2017–18 Canadian Community Health Survey (CCHS) publicly used microdata file. SRH was measured on a 5-point Likert scale from poor to excellent and dichotomized into “Good or Better” and “Fair or Poor.” Sleep duration was categorized into “Less than 7 h” and “More than 7 h,” while trouble sleeping was categorized as “Yes” or “No.” A joint variable derived from these created four groups: “no sleep issues,” “fewer sleeping hours (<7 h) only,” “trouble sleeping only,” and “fewer hours & trouble sleeping.” A weighted univariable and multivariable logistic regression with robust variance estimation was conducted to estimate relative risk due to interaction.
Results: Among Canadian adults, 40.96% reported less than 7 h of sleep, and 48.38% reported trouble sleeping. Approximately 11% had Fair or Poor SRH. The odds ratio for Fair or Poor SRH was 1.34 (95% CI: 1.23–1.46) for short sleep duration, 2.38 (95% CI: 2.18–2.61) for troubled sleep, and 2.97 (95% CI, 2.66–3.33) for both conditions. The adjusted RERI was 0.80 (95% CI, 0.40–1.21).
Implication: These results imply that shorter duration of sleep and troubled sleeping may increase the negative influence on self-rated health.
1 Background
Sleep is essential for maintaining health and enhancing overall well-being (1). Previous studies have highlighted the importance of adequate sleep- both duration and quality- for physical and mental health among diverse groups of population around the world (2–4). Multiple studies revealed that insufficient sleep duration significantly increases the risk of obesity, hypertension, coronary heart disease, and stroke among generally healthy populations (5–8). On the other hand, research indicates that sufficient sleep can enhance memory (9) and is linked with self-reported happiness and improved academic achievement (10, 11). A systematic review further revealed that improved sleep quality correlates with numerous positive health outcomes, including better cardiovascular, metabolic, and mental health (12). Kwok et al. (13) conducted a systematic review and reported a divergent result, which revealed that poor quality of sleep and longer duration of sleep had an impact on coronary heart disease and increased moderate risk of mortality, respectively. Nevertheless, many studies highlighted the importance of combined short sleep duration and poor sleep quality, which may increase the likelihood of adverse health outcomes.
Impaired sleep is also associated with poor self-rated health (SRH) (2, 14–18), also known as self-assessed or self-perceived health. SRH is a single-item measure where individuals can evaluate their current health status on a four or five-point scale ranging from excellent to poor. This method is widely used for its reliability and simplicity. Numerous studies across the world have consistently demonstrated that SRH is an effective predictor of mortality from various diseases (19–21). In certain professions such as sports, athletes reported that poor sleep affects not only how they perform, but also how they feel, recover, and even how they define themselves (22). People of all age groups who slept less than 7 h per day reported poor SRH (23, 24). However, adults were more likely to report insufficient sleep. In contrast, Anderson et al. found that among young people, reduced sleep duration exhibited an inverted quadratic relationship with poor SRH, which they attributed to variations in sleep quality (2). Furthermore, Ding et al. (16) conducted a cross-sectional study that revealed that the joint effect of shorter sleep duration and trouble sleeping was much higher than the independent effects of these two sleep variables among medical students.
Similarly, Wang et al. (25) identified that shorter duration of sleep and trouble sleeping had an additive interaction effect on depressive symptoms, indicating that there might be a possibility of the additive effect of trouble sleeping on shorter duration of sleep on SRH. Previously, we conducted a cross-sectional study on the Canadian adult population, where we identified that people with shorter durations and trouble sleeping reported higher poor SRH than those with no sleep issues (14). Although the Odds of poor SRH were reported to be higher among the people with both sleep issues than the individualized odds of shorter sleep and sleep trouble, the additive effect remains unexplored. While previous studies, such as Ding et al. (16) and Wang et al. (25), have examined the joint effects of sleep duration and quality, they differ in outcome focus, study population, and analytical approach. For example, Wang et al. assessed the combined impact of impaired sleep on depressive symptoms among Americans using Relative Excess Risk due to Interaction (RERI), whereas Ding et al. used multivariable-adjusted odds ratios to examine the joint effects of sleep impairment on general health outcomes among Chinese medical students. In contrast, our study uniquely applies an additive interaction framework, specifically RERI, to assess the combined effects of short sleep duration and poor sleep quality on SRH among Canadian adults. This approach enables a more nuanced understanding of potential synergistic effects, which are particularly relevant for informing public health interventions. To the best of our knowledge, this is the first population-based study to investigate the additive interaction between these two sleep-related factors in relation to SRH among Canadian adults using RERI.
2 Methods
2.1 Study design
This study utilized the publicly available microdata file from the 2017–2018 Canadian Community Health Survey (CCHS) (26). The CCHS is a cross-sectional survey employing a complex multistage design to randomly collect data on sociodemographic and health factors from a nationally representative sample of Canadians aged 12 and older. Data was gathered from all provinces and territories.
2.2 Sample size and ethical consideration
The initial survey sample size was 113,290. However, for this study, we focused on a subset of participants with available sleep-related data, totaling 56,675 respondents from Prince Edward Island, Quebec, Alberta, British Columbia, Yukon, and Nunavut. Further restricting the analysis to participants aged 18 and older resulted in a final sample size of 52,378. Given the public availability of the data, this study did not require ethical review.
2.3 Study variables
2.3.1 Dependent variable
Self-rated health (SRH) was measured on a five-point Likert scale question, asking participants, “In general, would you say your health is… (Poor, Fair, Good, Very Good, Excellent).” For analysis, we dichotomized SRH into two categories: Good or Better (combining Good, Very Good, and Excellent) and Fair or Poor (combining Fair and Poor).
2.3.2 Independent variables
Two sleep-related variables were selected from the CCHS survey: sleep duration and trouble sleeping. Sleep duration was measured by asking participants to report their average number of hours of sleep per night, which we later categorized as “<7 h” and “≥7 h.” Trouble sleeping was assessed based on the question “How often do you have trouble going to sleep or staying asleep?” and was recoded as a binary variable with “Yes” and “No” responses. Additional sociodemographic variables (age group, sex, ethnicity, marital status, highest education, income, employment status, and immigration status) were also extracted from the CCHS dataset and recoded similarly to the previously published article from the same population (14).
2.4 Statistical analysis
Data analysis was conducted by using STATA version 15 (27). We have considered the survey weight during all analyses. To account for the complex sampling design of the dataset, including stratification, clustering, and sample weights, we used the Taylor Series Linearization method to estimate variances and 95% confidence intervals. This was implemented through the ‘svy’ command suite in STATA. A chi-square test with survey weighting was conducted to identify the sociodemographic group difference based on sleeping hours and trouble sleeping. Sample distribution was reported as a weighted percentage, and a significant value was reported if p < 0.05. In continuation of the previous study, we followed the procedure to report both unadjusted and adjusted RERI (14) by following the steps below.
2.5 Calculating RERI on the additive scale by using stratification
We created a combined variable to analyze RERI based on stratified data. We created a combined variable named “impaired sleep” and categorized it into four groups: No sleep issues (E−M−), Fewer sleeping hours (<7 h) only (E+M−), trouble sleeping only (E−M+), and both fewer sleeping hours & trouble sleeping (E+M+). We used stratification to estimate the RERI, as this approach allows for a direct and interpretable comparison of joint effects across specific combinations of sleep duration and quality categories. This method aligns with the assumptions of additive interaction models and facilitates transparent calculation of stratum-specific risks relative to the reference group. We calculated the RERI based on the following formula to evaluate the value on the additive scale (28).
Later, we used the “non-linear combination coefficient” (nlcom) command in STATA to calculate the 95% confidence interval (CI) and p-value for the reported RERI (29). A calculated RERI greater than “0” indicates supra-additivity with positive interaction on the additive scale (29).
In the final model, we included all significant variables from the univariable logistic regression in a multivariable logistic regression framework, incorporating potential interaction terms to calculate the adjusted RERI on the additive scale by the steps as mentioned above.
3 Result
3.1 Sociodemographic characteristics of the participants based on sleeping duration and quality
Table 1 shows the weighted percentages of Canadian adults based on sleeping duration and quality. Notably, 40.96 and 48.38% of Canadian adults reported having less than 7 h of sleep and trouble going to sleep or staying asleep, respectively. A higher percentage of individuals reporting less than 7 h of sleep rate their health as “Fair or Poor” (52.69%) compared to those sleeping more than 7 h (47.31%). One-third (32.82%) of the respondents reporting health as “Fair or Poor” experience trouble sleeping compared to those with “Good or Better” health (53.78%), with a significant p-value (<0.001). Age, sex, ethnicity, and employment status showed significant differences across the groups regarding sleep duration and trouble sleeping. Older adults (65 and above) have a higher proportion of sleeping more than 7 h (64.68%) compared to younger age groups; conversely, younger adults (less than 40 years) reported the highest proportion (53.33%) of trouble sleeping. Females (60.34%) are more likely to sleep over 7 h than males (57.71%), whereas men have the highest percentage of trouble sleeping (Male vs. Female: 59.05% vs. 44.37%). While a significantly higher percentage (61.07%) of white Canadian adults reported having slept less than 7 h, the prevalence of having trouble going to sleep among white (51.00%) was slightly lower than among non-white (54.90%) Canadians. Marital status and income show some variation in sleep duration, though not statistically significant. Conversely, respondents who were married (53.07%) and had an income of more than 40 thousand (52.20%) reported a significantly higher percentage of trouble sleeping. There was no significant difference across the education groups in terms of sleep duration and quality. Non-immigrants (60.29%) are also more likely to report less sleep duration compared to immigrants; oppositely, immigrants reported a significantly higher prevalence of trouble sleeping than non-immigrants (55.17 vs. 50.45).
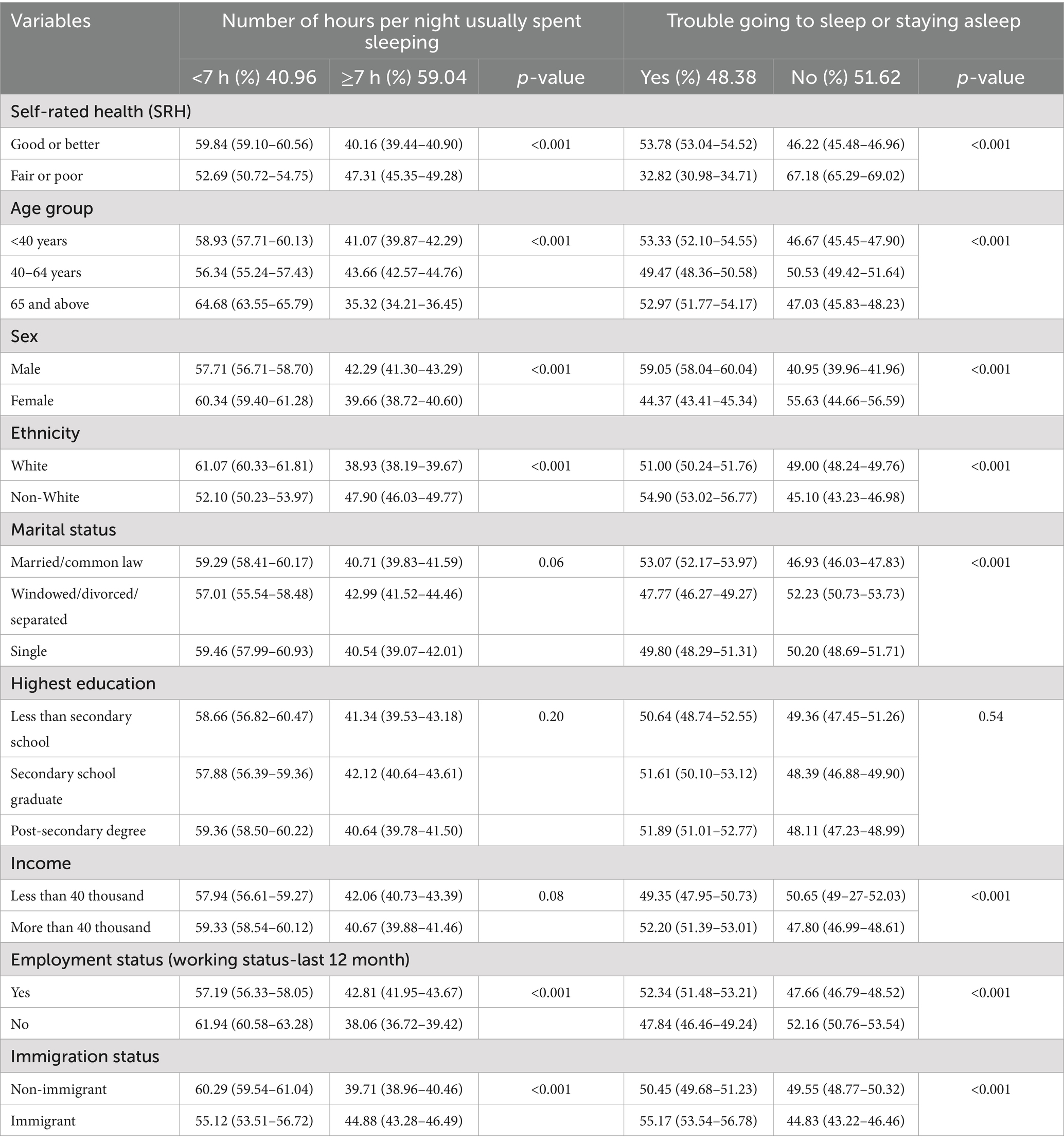
Table 1. Distribution of participants’ characteristics (in terms of weighted percentages) across the sleeping issue.
3.2 Sleep variables and socio-demographic factors related with poor SRH
Table 2 illustrates the association between sleep duration and trouble sleeping with SRH. Respondents who slept less than 7 h had reported 1.34 times (95% CI: 1.23–1.46, p < 0.001) times higher odds for “Fair or Poor” SRH in comparison to the respondents who slept more than 7 h. Similarly, respondents who reported trouble sleeping reported 2.38 times (95% CI: 2.18–2.61, p < 0.001) higher odds for “Fair or Poor” SRH in comparison to the respondents who had no trouble issue with their sleep. Table 2 also illustrates that the older age group (65yeras and above OR = 3.76, 95% CI: 3.34–4.23, p < 0.01), female (OR = 1.10, 95% CI: 0.82–1.19, p < 0.05), unemployment status (OR = 4.11, 95% CI: 3.73–4.52, p < 0.001) are significantly related with Fair or Poor SRH. And higher income (OR = 0.40, 95% CI: 0.37–0.44, p < 0.001) and with post-secondary education (OR = 0.27, 95% CI: 0.24–0.30, p < 0.001) respondents reported 60 and 73% Good or Better SRH, respectively.
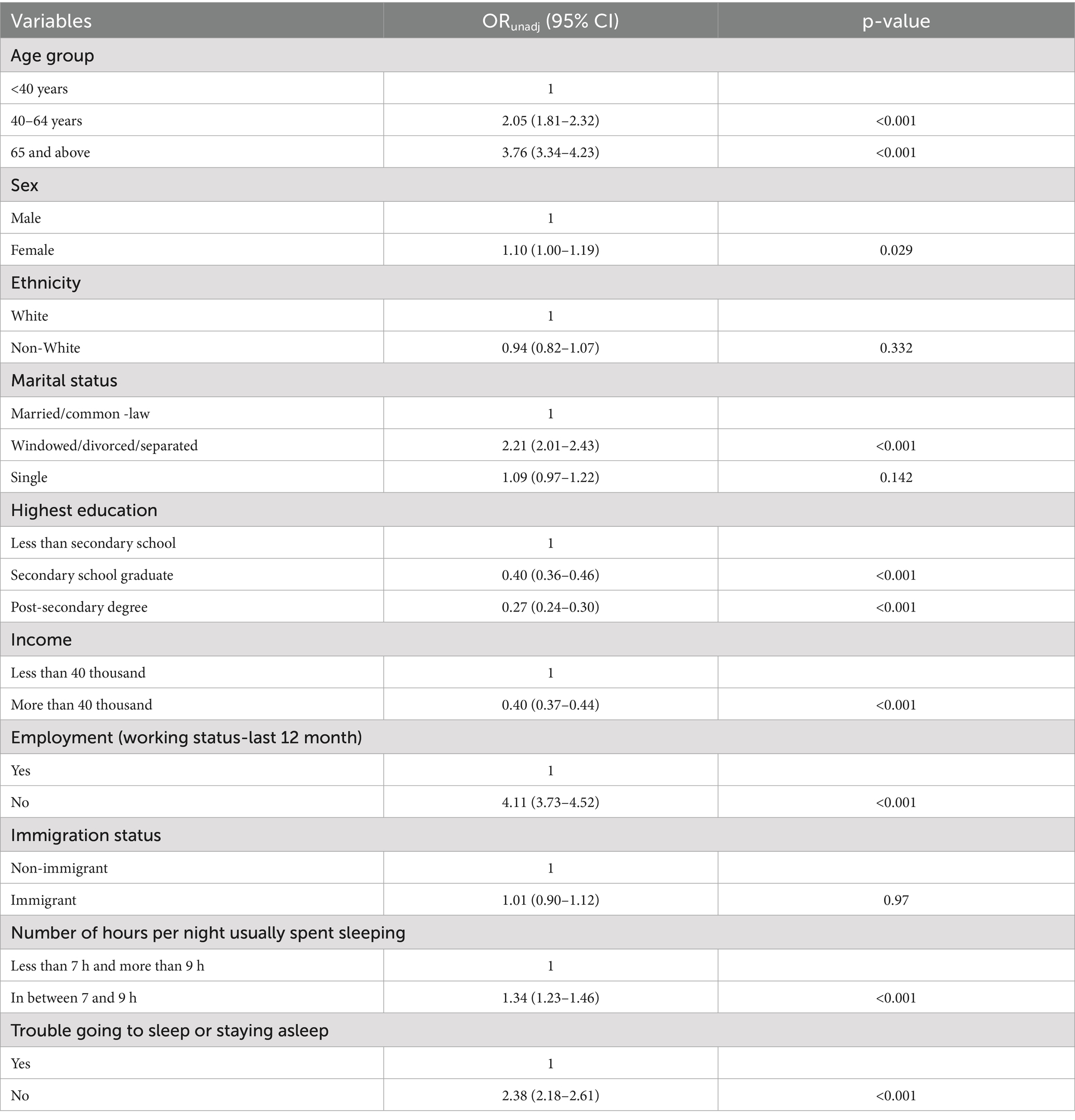
Table 2. Unadjusted odds ratios with 95% Taylor linearization confidence intervals (ORunadj (95% CI)) for the association of sociodemographic and sleep related factors with SRH, CCSH, 2017–2018, Canada.
3.3 The combined effect of fewer sleeping hours and trouble sleeping on SRH
When respondents had fewer sleeping hours (<7 h), the OR for Fair or Poor SRH was 1.14 (95% CI: 0.98–1.33, p = 0.09), OR for only trouble sleeping was 1.98 (95% CI: 1.76–2.24, p < 0.001). Moreover, the respondents who had faced both fewer sleep and trouble sleeping had reported a 2.97 (95% CI: 2.66–3.33, p < 0.001) times higher likelihood of developing Fair or Poor health in comparison to the respondents who had no issue with sleep (Table 3). To assess the access risk of the combined effect of the sleep issue on health, we have conducted the RERI on the additive scale by using the stratified OR’s value from the combined variable, by using nlcom command in STATA and the following formula:
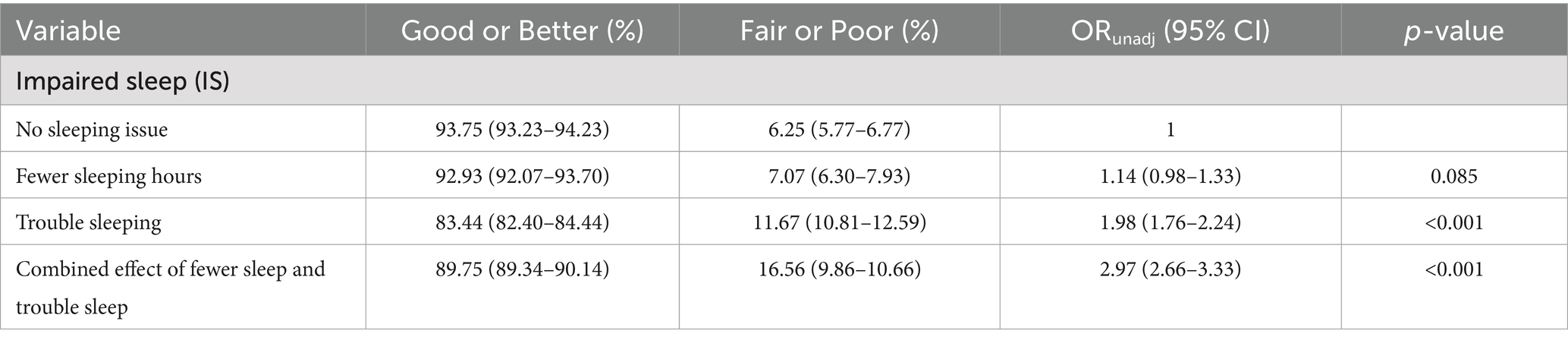
Table 3. Unadjusted odds ratios (ORunadj) with 95% Taylor linearization confidence intervals (95% CI) for the association between SRH and combined effect (stratified) of fewer sleep and trouble sleep, CCSH, 2017–2018, Canada.
RERI (from additive scale) 0.85 (95% CI: 0.54–1.17) indicates joint effect of sleep variables shows a positive supra-additive interaction on Fair or Poor SRH.
Based on the results from univariable logistic regression and the associations observed in Table 1, we identified potential confounders for inclusion in the final model examining the relationship between impaired sleep and SRH. After adjusting for potential confounders (age, sex, marital status, education, income, and working status), in final analysis, we found that individuals who reported fewer than 7 h of sleep had 1.31 times higher odds of reporting Fair or Poor SRH (95% CI: 1.09–1.57, p = 0.003) (Table 4). Those who experienced only trouble sleeping had 2.24 times higher odds (95% CI: 1.94–2.58, p < 0.001). Notably, respondents reporting both short sleep duration and trouble sleeping had a 3.35-fold higher likelihood (95% CI: 2.94–3.83, p < 0.001) of fair or poor SRH compared to those without any sleep issues (Table 4, Supplementary Table 1). From this final model (by using nlcom command in STATA and formula below):
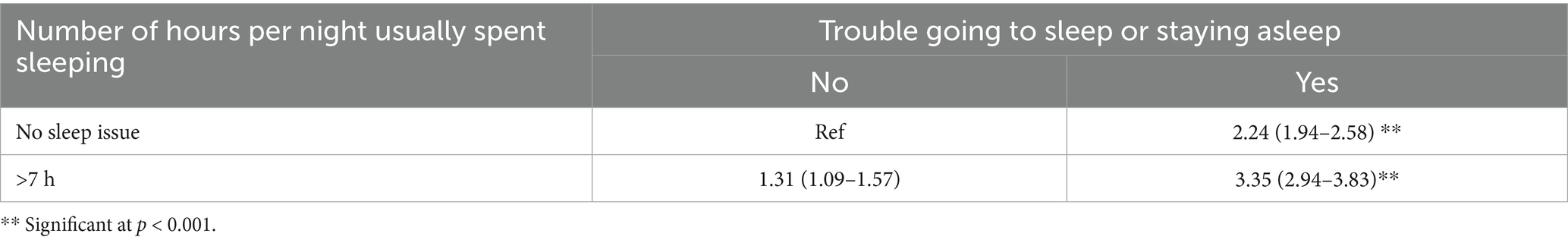
Table 4. Adjusted odds ratios (ORadj) with 95% Taylor linearization confidence intervals (95% CI) for the association between SRH and combined effect (stratified) of fewer sleep and trouble sleep, CCSH, 2017–2018, Canada.
The RERI value of 0.80 (95% CI: 0.40–1.21), calculated on the additive scale after adjusting for confounders, also indicates a positive supra-additive interaction between sleep duration and sleep trouble on fair or poor self-rated health (SRH). From this final model, the adjusted RERI value further confirmed a synergistic effect of the combined sleep issues on SRH.
4 Discussion
This study explored the combined effects of short sleep duration (<7 h) and trouble sleeping on SRH among Canadian adults, utilizing data from the 2017–2018 Canadian Community Health Survey. The results revealed significant additive interactions between these sleep disturbances, emphasizing their compounded negative impact on SRH.
We first assessed if socio-demographic factors (age, sex, and socio-economic status) altered the link between impaired sleep and self-rated health (SRH). No significant modification was found, so the final model only adjusted for these variables as potential confounders. After removing non-significant interaction terms, the adjusted RERI remained positive (RERIadj = 0.80; 95% CI: 0.40–1.21), indicating a possible supra-additive effect, meaning the combined impact of short sleep and sleep difficulty might be greater than the sum of their individual effects. However, because the lower confidence interval bound is close to zero, there is some uncertainty, and the joint effect could partly be due to unmeasured or residual confounding.
The relationship between sleep disturbances and SRH has been extensively studied, consistently demonstrating that both short sleep duration (24) and poor sleep quality (30, 31) are independently associated with adverse health outcomes. Additionally, Seow et al. (32) reported independent and combined associations of sleep duration and sleep quality with common physical and mental disorders.
Our findings reinforce previous observations, indicating that Canadian adults who both experience short sleep duration (<7 h) and encounter difficulties sleeping are nearly three times more likely to report Fair or Poor SRH than those without sleep problems. This is consistent with the research conducted by Ding and colleagues (16) which found that medical students with short sleep duration and poor sleep quality also had higher odds of reporting suboptimal SRH, which is further evidenced by a recent systematic review (33). However, another systematic review (2) reported that poor sleep quality was associated with worse SRH in long sleep duration but not short sleep duration.
The combined effects of reduced sleep duration and difficulties with sleep can be scientifically elucidated through their impact on mental health, particularly in relation to depression. Research has demonstrated that sleep deprivation leads to neurobiological changes, including a reduction in dopamine receptor availability in the striatum, which negatively affects mood regulation and heightens the risk of depression (34). Additionally, chronic sleep deprivation disrupts the hypothalamic–pituitary–adrenal (HPA) axis, resulting in increased cortisol levels and heightened stress responses (35). This physiological stress can exacerbate emotional dysregulation, further elevating the likelihood of developing depressive symptoms (25).
Sleep disruption is associated with increased activity of the sympathetic nervous system and the hypothalamic–pituitary–adrenal axis, metabolic effects, changes in circadian rhythms, and proinflammatory responses. In otherwise healthy adults, short-term consequences of sleep disruption include increased stress responsivity, somatic pain, reduced quality of life, emotional distress, mood disorders, and cognitive, memory, and performance deficits. Long-term consequences of sleep disruption in otherwise healthy individuals include hypertension, dyslipidaemia, cardiovascular disease, weight-related issues, metabolic syndrome, type-2 diabetes mellitus, and colorectal cancer (36). Additionally, all-cause mortality is increased in men with sleep disturbances (36, 37). The combined effect may accelerate health deterioration, as indicated by the supra-additive risk identified in the study.
From a public health perspective, the high prevalence of short sleep duration (40.96%) and trouble sleeping (48.38%) among Canadian adults suggests that a substantial portion of the population is at elevated risk for Fair or Poor SRH due to these combined sleep disturbances. Targeted interventions, such as sleep hygiene education and cognitive-behavioral therapy for insomnia (CBT-I), are essential to mitigate these risks and enhance overall health outcomes (38).
This study has several strengths, including its utilization of large, comprehensive, and representative population-based data. However, certain regions such as Nunavut and Yukon are overrepresented, while others are excluded, which may limit the generalizability of our findings to all Canadian adults across provinces and territories. Nonetheless, this study provides substantial evidence on additive effect of sleep duration and sleep quality on SRH among Canadian adults. These findings can inform policymakers and healthcare professionals in planning and developing different intervention approaches to reduce sleep disturbance and improve SRH among diverse population groups in Canada. Clinically, our results highlight the importance of routinely assessing both sleep duration and quality during patient evaluations, as their combined impact may significantly affect overall health perceptions and wellbeing. Healthcare providers should be aware that patients presenting with poor sleep quality and short sleep duration are at increased risk for poor health outcomes, which could warrant early intervention or referral to sleep specialists.
It is important to note that, the cross-sectional nature of the survey data, the causal relationship could not be established. Moreover, our study focused exclusively on short sleep duration (<7 h) in combination with poor sleep quality and did not account for long sleep duration (>9 h), which has also been shown in previous research to adversely affect self-rated health. Besides, this study relies on secondary administrative data, which does not include information related with potential confounders, such as medication use. As a result, we were unable to account for the potential effects of medications on sleep quality and overall quality of life, which may confound the observed relationships between impaired sleep and SRH. This study also did not account for certain confounders such as comorbidities, obesity, medication use, and alcohol intake, which may influence sleep and health outcomes. Future studies should explore the full spectrum of sleep duration to better understand its joint effects with sleep quality on health outcomes.
Our study provides valuable insights on joint effect of sleep duration and quality on SRH of Canadian adults. The nearly threefold increase in Fair or Poor SRH among those experiencing both short sleep duration and sleep difficulties aligns with some previous research, though conflicting evidence exists. These findings underscore the complex interplay between sleep and health, suggesting that both sleep duration and quality should be considered in health assessments and interventions. Future longitudinal research with qualitative component is needed to fully understand these relationships across different populations and contexts.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www150.statcan.gc.ca/n1/daily-quotidien/191022/dq191022d-eng.htm.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
SK: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Writing – original draft, Writing – review & editing. NS: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. JM: Methodology, Project administration, Writing – original draft, Writing – review & editing. NN: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1632239/full#supplementary-material
References
1. Grandner, MA, and Fernandez, FX. The translational neuroscience of sleep: a contextual framework. Science. (2021) 374:568–73. doi: 10.1126/science.abj8188
2. Andreasson, A, Axelsson, J, Bosch, JA, and Balter, LJ. Poor sleep quality is associated with worse self-rated health in long sleep duration but not short sleep duration. Sleep Med. (2021) 88:262–6. doi: 10.1016/j.sleep.2021.10.028
3. Kader, SB, Abonyi, S, Dosman, JA, Karunanayake, CP, King, M, Seesequasis, W, et al. Association between insomnia and four domains of health based on an indigenous medicine wheel: findings from two Saskatchewan first nation communities. Can J Public Health. (2024) 115:880–91. doi: 10.17269/s41997-024-00935-0
4. Scott, AJ, Webb, TL, Martyn-St James, M, Rowse, G, and Weich, S. Improving sleep quality leads to better mental health: a meta-analysis of randomised controlled trials. Sleep Med Rev. (2021) 60:101556. doi: 10.1016/j.smrv.2021.101556
5. Itani, O, Jike, M, Watanabe, N, and Kaneita, Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med. (2017) 32:246–56. doi: 10.1016/j.sleep.2016.08.006
6. Jike, M, Itani, O, Watanabe, N, Buysse, DJ, and Kaneita, Y. Long sleep duration and health outcomes: a systematic review, meta-analysis and meta-regression. Sleep Med Rev. (2018) 39:25–36. doi: 10.1016/j.smrv.2017.06.011
7. Li, J, Cao, D, Huang, Y, Chen, Z, Wang, R, Dong, Q, et al. Sleep duration and health outcomes: an umbrella review. Sleep Breath. (2022) 26:1479–501. doi: 10.1007/s11325-021-02458-1
8. St-Onge, MP, Grandner, MA, Brown, D, Conroy, MB, Jean-Louis, G, Coons, M, et al. Sleep duration and quality: impact on lifestyle behaviors and cardiometabolic health: a scientific statement from the American Heart Association. Circulation. (2016) 134:444. doi: 10.1161/CIR.0000000000000444
9. Ficca, G, and Salzarulo, P. What in sleep is for memory. Sleep Med. (2004) 5:225–30. doi: 10.1016/j.sleep.2004.01.018
10. Diekelmann, S, Wilhelm, I, and Born, J. The whats and whens of sleep-dependent memory consolidation. Sleep Med Rev. (2009) 13:309–21. doi: 10.1016/j.smrv.2008.08.002
11. Kyprianidou, M, Panagiotakos, D, Kambanaros, M, Makris, KC, and Christophi, CA. Quality of sleep in the Cypriot population and its association with multimorbidity: a cross-sectional study. Front Public Health. (2021) 9:693332. doi: 10.3389/fpubh.2021.693332
12. Lian, Y, Yuan, Q, Wang, G, and Tang, F. Association between sleep quality and metabolic syndrome: a systematic review and meta-analysis. Psychiatry Res. (2019) 274:66–74. doi: 10.1016/j.psychres.2019.01.096
13. Kwok, CS, Kontopantelis, E, Kuligowski, G, Gray, M, Muhyaldeen, A, Gale, CP, et al. Self-reported sleep duration and quality and cardiovascular disease and mortality: a dose-response Meta-analysis. J Am Heart Assoc. (2018) 7:e008552. doi: 10.1161/JAHA.118.008552
14. Kader, SB, Shakurun, N, Janzen, B, and Pahwa, P. Impaired sleep, multimorbidity, and self-rated health among Canadians: findings from a nationally representative survey. J Multimorbidity Comorbidity. (2024) 14:26335565241228549. doi: 10.1177/26335565241228549
15. Conklin, AI, Yao, CA, and Richardson, CG. Chronic sleep disturbance, not chronic sleep deprivation, is associated with self-rated health in adolescents. Prev Med. (2019) 124:11–6. doi: 10.1016/j.ypmed.2019.04.014
16. Ding, P, Li, J, Chen, H, Zhong, C, Ye, X, and Shi, H. Independent and joint effects of sleep duration and sleep quality on suboptimal self-rated health in medical students: a cross-sectional study. Front Public Health. (2022) 10:957409. doi: 10.3389/fpubh.2022.957409
17. Geiger, SD, Sabanayagam, C, and Shankar, A. The relationship between insufficient sleep and self-rated health in a nationally representative sample. J Environ Public Health. (2012):2012:518263. doi: 10.1155/2012/518263
18. Magee, CA, Caputi, P, and Iverson, DC. Relationships between self-rated health, quality of life and sleep duration in middle aged and elderly Australians. Sleep Med. (2011) 12:346–50. doi: 10.1016/j.sleep.2010.09.013
19. Wu, S, Wang, R, Zhao, Y, Ma, X, Wu, M, Yan, X, et al. The relationship between self-rated health and objective health status: a population-based study. BMC Public Health. (2013) 13:320. doi: 10.1186/1471-2458-13-320
20. Benjamins, MR, Hummer, RA, Eberstein, IW, and Nam, CB. Self-reported health and adult mortality risk: an analysis of cause-specific mortality. Soc Sci Med. (2004) 59:1297–306. doi: 10.1016/j.socscimed.2003.01.001
21. Boardman, JD. Self-rated health among U.S. adolescents. J Adolesc Health. (2006) 38:401–8. doi: 10.1016/j.jadohealth.2005.01.006
22. Longo, V, Gottschlich, D, Turner, S, and Qiu, H. A qualitative analysis of the role of sleep disorders in sports injuries among competitive athletes in Canada. Int J Sport Stud Health. (2025) 8:19–26. doi: 10.61838/kman.intjssh.8.2.3
23. Jean-Louis, G, Shochat, T, Youngstedt, SD, Briggs, AQ, Williams, ET, Jin, P, et al. Age-associated differences in sleep duration in the US population: potential effects of disease burden. Sleep Med. (2021) 87:168–73. doi: 10.1016/j.sleep.2021.09.004
24. Štefan, L, Juranko, D, Prosoli, R, Barić, R, and Sporiš, G. Self-reported sleep duration and self-rated health in young adults. J Clinic Sleep Med. (2017) 13:899. doi: 10.5664/jcsm.6662
25. Wang, S, Rossheim, ME, Nandy, RR, and Nguyen, US. Interaction between sleep duration and trouble sleeping on depressive symptoms among U.S. adults, NHANES 2015-2018. J Affect Disord. (2024) 351:285–92. doi: 10.1016/j.jad.2024.01.260
26. Government of Canada SC. Canadian community health survey - annual component (CCHS) [internet]. (2024) Available online at: https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3226 (Accessed January 13, 2025).
28. VanderWeele, TJ, and Knol, MJ. A tutorial on interaction. Epidemiologic. Methods. (2014) 3:33–72. doi: 10.1515/em-2013-0005
29. Cho, SS, Ju, YS, Paek, D, Kim, H, and Jung-Choi, K. The combined effect of long working hours and low job control on self-rated health: an interaction analysis. J Occup Environ Med. (2017) 60:475. doi: 10.1097/JOM.0000000000001241
30. Canever, JB, Cândido, LM, Wagner, KJP, Danielewicz, AL, Cimarosti, HI, and de Avelar, NCP. Association between sleep problems and self-perception of health among community-dwelling older adults: data from the 2019 national health survey. Aging Health Res. (2024) 4:100192. doi: 10.1016/j.ahr.2024.100192
31. Silva-Costa, A, Griep, RH, and Rotenberg, L. Associations of a short sleep duration, insufficient sleep, and insomnia with self-rated health among nurses. PLoS One. (2015) 10:e0126844. doi: 10.1371/journal.pone.0126844
32. Seow, LSE, Tan, XW, Chong, SA, Vaingankar, JA, Abdin, E, Shafie, S, et al. Independent and combined associations of sleep duration and sleep quality with common physical and mental disorders: results from a multi-ethnic population-based study. PLoS One. (2020) 15:e0235816. doi: 10.1371/journal.pone.0235816
33. Amiri, S. Sleep duration, sleep quality, and insomnia in association with self-rated health: a systematic review and meta-analysis. Sleep Med Res. (2023) 14:66–79. doi: 10.1016/j.smrv.2021.101429
34. Luo, ZC, and Gao, TM. Dopamine switches affective states under acute sleep deprivation. Neurosci Bull. (2024) 40:1205–8. doi: 10.1007/s12264-024-01216-z
35. Minkel, J, Moreta, M, Muto, J, Htaik, O, Jones, C, Basner, M, et al. Sleep deprivation potentiates HPA axis stress reactivity in healthy adults. Health Psychol. (2014) 33:1430–4. doi: 10.1037/a0034219
36. Medic, G, Wille, M, and Hemels, ME. Short- and long-term health consequences of sleep disruption. Nat Sci Sleep. (2017) 9:151–61. doi: 10.2147/NSS.S134864
37. Merlino, G, Lorenzut, S, Gigli, GL, Del Negro, I, Tereshko, Y, Smeralda, C, et al. Insomnia and daytime sleepiness predict 20-year mortality in older male adults: data from a population-based study. Sleep Med. (2020) 73:202–7. doi: 10.1016/j.sleep.2020.06.025
38. Qaseem, A, Kansagara, D, Forciea, MA, Cooke, M, and Denberg, TD. For the clinical guidelines Committee of the American College of physicians. Management of Chronic Insomnia Disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. (2016) 165:125–33. doi: 10.7326/M15-2175
Keywords: self rated health, sleep quality, trouble sleeping, CCHS, sleep health, RERI
Citation: Kader SB, Shakurun N, Mumin J and Noor N (2025) Joint effect of sleep duration and sleep quality on self-rated health among Canadian adults: estimating relative excess risk due to interaction from a nationwide survey. Front. Public Health. 13:1632239. doi: 10.3389/fpubh.2025.1632239
Edited by:
Christos Theleritis, University General Hospital Attikon, GreeceReviewed by:
Morteza Taheri, University of Tehran, IranDimitrios Papadopoulos, 401 General Military Hospital of Athens, Greece
Copyright © 2025 Kader, Shakurun, Mumin and Noor. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jubayer Mumin, anViYXllci5tdW1pbkBraS5zZQ==
 Shirmin Bintay Kader
Shirmin Bintay Kader Nahin Shakurun
Nahin Shakurun Jubayer Mumin
Jubayer Mumin Naomi Noor
Naomi Noor