- 1Graduate School of Public Health, Hanyang University, Seoul, Republic of Korea
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, National Medical Center, Seoul, Republic of Korea
- 3Division of Tuberculosis Prevention and Control, Korea Disease Control and Prevention Agency, Cheongju, Republic of Korea
- 4Center for Global Health Practice, Institute of Health and Society, Hanyang University College of Medicine, Seoul, Republic of Korea
Introduction: Tuberculosis (TB) remains a significant global health concern, with foreign migrants in the Republic of Korea (ROK) representing a particularly vulnerable group; despite comprising only 3.5% of the population, they account for over 5% of annual TB cases and exhibit disproportionately high rates of lost to follow up (LTFU) from treatment compared to native Koreans. This mixed-methods study aimed to identify key factors influencing non-adherence to treatment and LTFU among migrants.
Methods: Utilizing national TB surveillance data from 2016 to 2018 for 4,011 migrant and 64,620 native patients, quantitative analysis were employed to identify factors associated with LTFU for migrants. Complementary in-depth qualitative interviews with Public-Private Mix (PPM) nurses provided deeper insights into barriers to adherence.
Results: The study revealed a significantly higher LTFU rate (21.5%) among migrant patients compared to domestic patients (2.3%). Key contributing factors included nationality (highest crude odds for migrants from Thailand, Central, and North Asia), living arrangements (increased risk for those not with family or living alone), and male gender. Drug-resistant TB made patients over four times more likely to discontinue treatment and systemic issues such as frequent care transfers and the presence of comorbidities. Qualitative findings highlighted inadequate patient education and misconceptions about TB severity (often seen as a “mild cold”), leading to premature discontinuation. Poor medical interpretation services and low awareness among migrants of free TB treatment under the PPM program were also critical barriers.
Discussion: These findings imply that high LTFU among migrant patients is multifactorial, stemming from personal, clinical, and systemic issues. Addressing this disparity requires targeted interventions, including culturally tailored multilingual educational campaigns, improved medical interpretation, and increased awareness of PPM program eligibility and free treatment. Streamlining interfacility care transfer processes (such as the “Tuberculosis Relief Belt” initiative), expanding PPM coverage, and ensuring access to specialized care for comorbid conditions are also essential. Addressing these multifaceted challenges is critical to reducing LTFU rates and enhancing treatment continuity and outcomes, thereby advancing TB control efforts in ROK’s shifting migration context.
1 Introduction
Tuberculosis (TB) remains a significant global health challenge (1). While the Republic of Korea (ROK) has drastically reduced the incidence from 5,168 cases per 100,000 in 1965 to 38 cases per 100,000 in 2023 (2, 3) and TB-related mortality has also shown marked improvement, critical public health challenges remain (3–5). TB is designated as a nationally notifiable disease under the Infectious Diseases Control and Prevention Act, mandating that all new diagnoses be reported to community health centers within 24 h (6). Established in 2000, the Korean National Tuberculosis Surveillance System (KNTSS) continuously monitors patient demographics, diagnostic outcomes, treatment modalities, and overall patient prognoses. Furthermore, the introduction of the Public-Private Mix (PPM) program in 2011, which emphasizes nurse-led patient monitoring, contributed to a substantial 43.2% reduction in TB-related deaths from 2013 to 2023 (5, 7).
Migrant communities represent particularly vulnerable groups in the ROK’s TB landscape. Although foreign-born individuals account for only 3.5% of the total population (8), they now contribute to more than 5% of annual TB cases, a significant increase from 0.3% in 2001 to 5.7% in 2023 (9, 10). Notably, Chinese nationals, especially Korean Chinese from northeastern China, account for nearly half of all TB cases among migrants (11, 12). Although the general population in the ROK experienced a decline in LTFU—from 5.3% in 2011 to 2.4% in 2018 (13, 14)—migrant populations continue to face disproportionately high risks (12). Interestingly, although migrants had lower overall odds of treatment success (odds ratio [OR] 0.71, 95% confidence interval [CI] 0.46–1.12), this difference was not statistically significant. However, migrants demonstrate lower rates of treatment completion, as verified through microbiological confirmation, suggesting that despite effective initial therapy, disengagement often occurs during the continuation phase (12).
Migrant patients with TB face multifaceted barriers to continuing treatment (15). Socioeconomic challenges—including financial constraints, unstable employment, and housing insecurity—often intersect with healthcare system obstacles such as limited access to specialized PPM nurses (16–18). In addition, clinical factors such as drug-resistant TB and comorbid conditions such as diabetes and cancer further increase the risk of LTFU (12, 19–22). Despite the growing recognition of these challenges, the specific determinants of LTFU among migrant populations in the ROK remain underexplored. This study addresses this gap by analyzing TB cases among migrants reported to the KNTSS between 2016 and 2018 and comparing them with native TB cases to identify key risk factors for treatment discontinuation. Complementary in-depth interviews with PPM nurses working in regions with large migrant populations provided additional insights into the unique barriers faced by these patients.
2 Materials and methods
This mixed method study was designed to investigate the factors affecting non-adherence and LTFU from TB treatment among foreign migrants in ROK, comparing them to native Korean TB patients. The study combined a retrospective cohort analysis of national health system data with complementary qualitative interviews.
2.1 Study design and setting
The quantitative element involved a retrospective cohort study utilizing national TB surveillance data from ROK, for the period between January 2016 and December 2018. The qualitative component involved in-depth interviews with Public-Private Mix (PPM) nurses.
2.2 Participants and data source
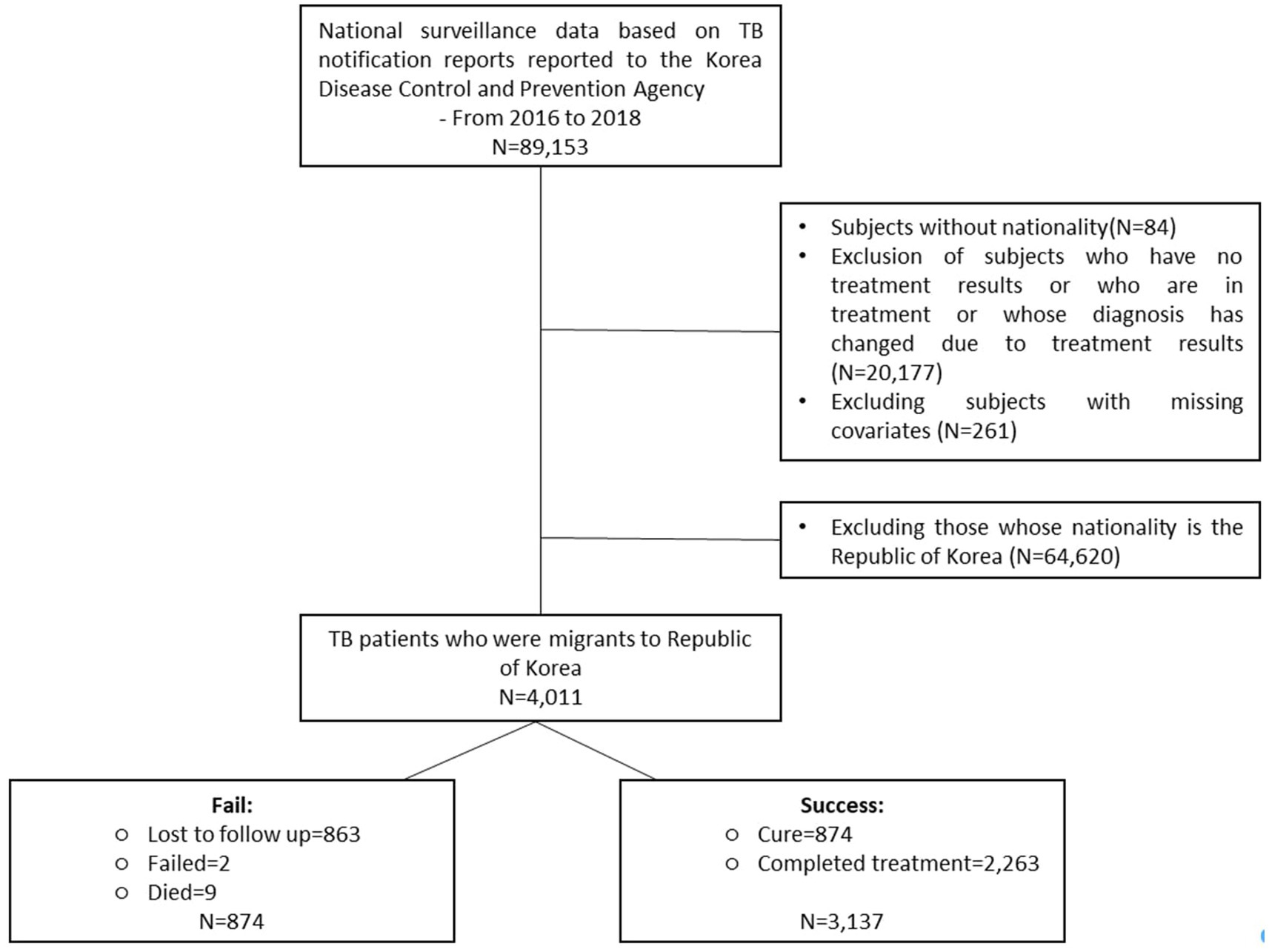
The initial dataset comprised of 89,153 notified TB cases. After exclusions for diagnostic changes, ongoing treatment, missing covariates or unrecorded nationality, the final study cohort comprised 64,620 Korean and 4,011 foreign nationals (Figure 1). Participants for qualitative interviews included specialist doctors and PPM nurses from various hospital settings (Supplementary file S1), selected through a purposive sampling approach.
2.3 Operational definition and variables
Thirteen variables were examined and organized into three domains:
• Sociodemographic profiles: This included sex, age, nationality, living arrangement, smoking status, and geographical region of residence.
• Disease profiles and health system: This included TB treatment history, disease site, drug resistance status, PPM program enrollment, care transfer, and type of treatment facility.
• Comorbidities: This domain assessed the presence of diabetes, cancer, or other chronic conditions.
TB case definitions, recommended treatment regimens and monitoring framework, and reporting procedures are summarized in the Supplementary file S2, as outlined in the National TB Management Guideline (23). Treatment outcomes were defined according to the 2020 World Health Organization (WHO) guidelines (23), classifying cases as either “successful” (cure or treatment completion), or “unsuccessful” (treatment failure, LFTU, or death). The primary outcome of interest was LTFU, which was defined as a treatment interruption lasting 2 months or more.
2.4 Data collection
Quantitative data were systematically collected from the Korean National Tuberculosis Surveillance System (KNTSS), which maintains comprehensive records on patient demographics, diagnostic outcomes, treatment modalities, and prognoses. For the qualitative phase, in-person, individual interviews were conducted with PPM nurses at their respective institutions, lasting up to an hour and audio-recorded with consent. All personal identifiers were removed during verbatim transcription to ensure confidentiality. No incentives were provided for participation.
2.5 Data analysis
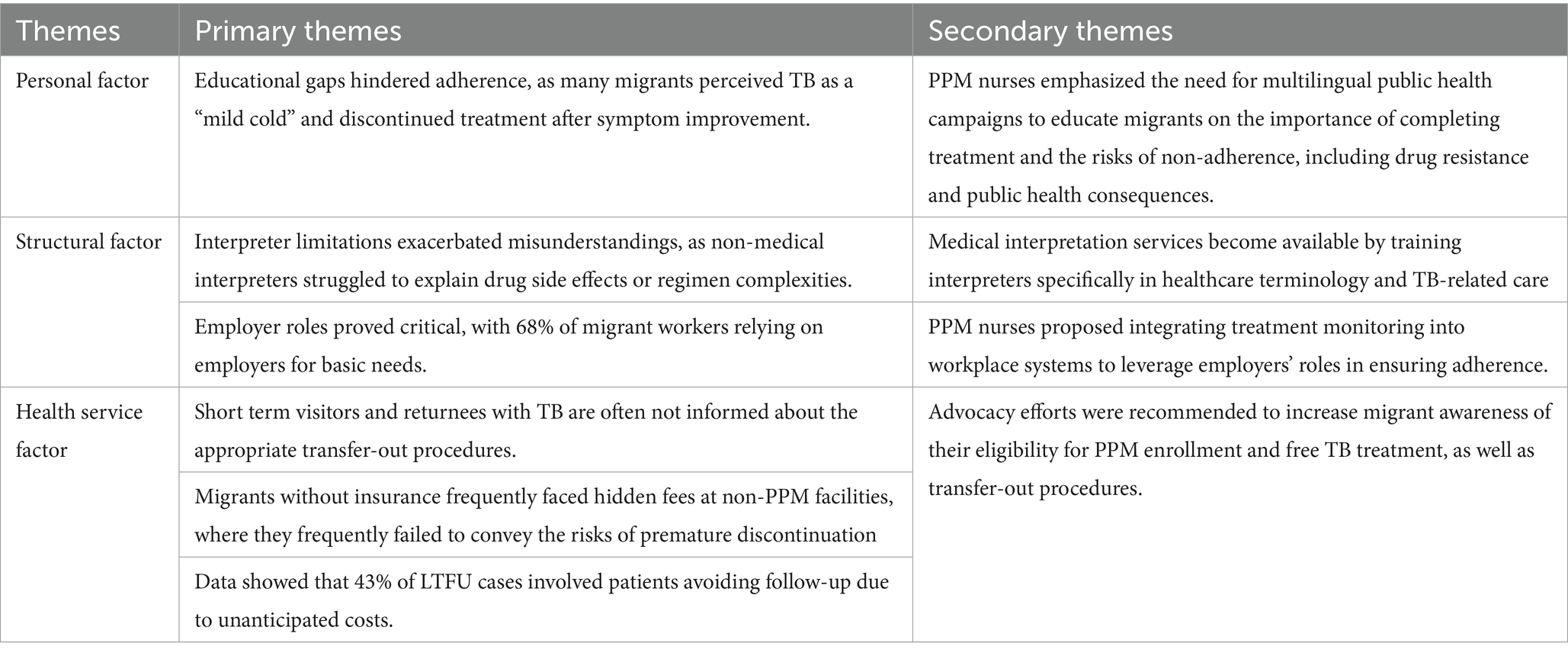
For quantitative analysis, chi-square tests and multivariate logistic regression analyses were employed to identify risk factors associated with LTFU. Data were analyzed using STATA 17. Qualitative data were analyzed using a thematic approach, with themes emerging inductively from the transcripts. Researchers identified recurring patterns and salient issues, which were then synthesized into three principal themes: Personal Factors (patient attitudes, behaviors, and circumstances), Structural Factors (living arrangements, socioeconomic and environmental barriers), and Health Service-Related Factors (resource limitations, coordination gaps, and systemic challenges). This inductive method provided critical context for the quantitative findings and illuminated specific barriers contributing to treatment discontinuation among migrant TB patients. The consistency of these themes was regularly reviewed throughout the interview process.
3 Results
3.1 Characteristics of patients with TB: migrants versus residents
This retrospective cohort study analyzed TB cases in ROK between 2016 and 2018, including 4,011 migrant patients, 2,415 males and 1,596 females and 64,620 nationals. Participants’ demographic characteristics are presented in Supplementary file S3. Registered foreigners increased from 1,161,677 in 2016 to 246,626 in 2018, with TB incidence among migrants declining over time (221.1 to 144.5 per 100,000), averaging 178.2, approximately 2.5 times the national incidence (71.0 per 100,000) (8, 10, 24, 25). Nationality-specific disparities were evident: Mongolian nationals had the highest TB incidence (216.7), while Uzbek nationals had the lowest (48.5).
Migrant patients were predominantly aged 30–49 and more likely to live alone (54.4% versus. 45.0%). They had a higher prevalence of drug-resistant TB (3.8% vs. 1.5%, p < 0.001) and lower access to PPM nurses (52.9% vs. 73.9%). Although comorbidities, such as diabetes (4.2% vs. 14.1%) and cancer (2.0% vs. 6.4%), were less common, their presence had a more pronounced impact on treatment discontinuation. Migrants experienced significantly higher LTFU rates (21.5% vs. 2.3%, p < 0.001) and lower treatment completion (56.4% vs. 75.3%), despite similar cure rates (21.8% vs. 20.1%).
3.2 Sex-based differences among migrants
Female migrants were concentrated in the ≤30 and ≥70 age groups, while males were predominantly aged 30–69. Men were more likely to live alone (59.5%) and women were more likely to live with family (47.8%). Smoking patterns differed notably—95.3% of women were non-smokers versus 55.2% of men who were current or former smokers.
3.3 Determinants of lost to follow-up among migrants
Unadjusted analysis identified several key risk factors for LTFU, including Thai origin (OR 5.28), Central and North Asian nationality (OR 2.96), living alone (OR 2.39), drug-resistant TB (OR, 3.78), care transfers (OR, 7.10) diabetes (OR 1.77) and cancer (OR 1.74), and receiving care in clinics or hospitals as opposed to general hospitals (OR range: 1.51–1.90) (Table 1). Female sex was associated with lower odds of LTFU (OR, 0.73).
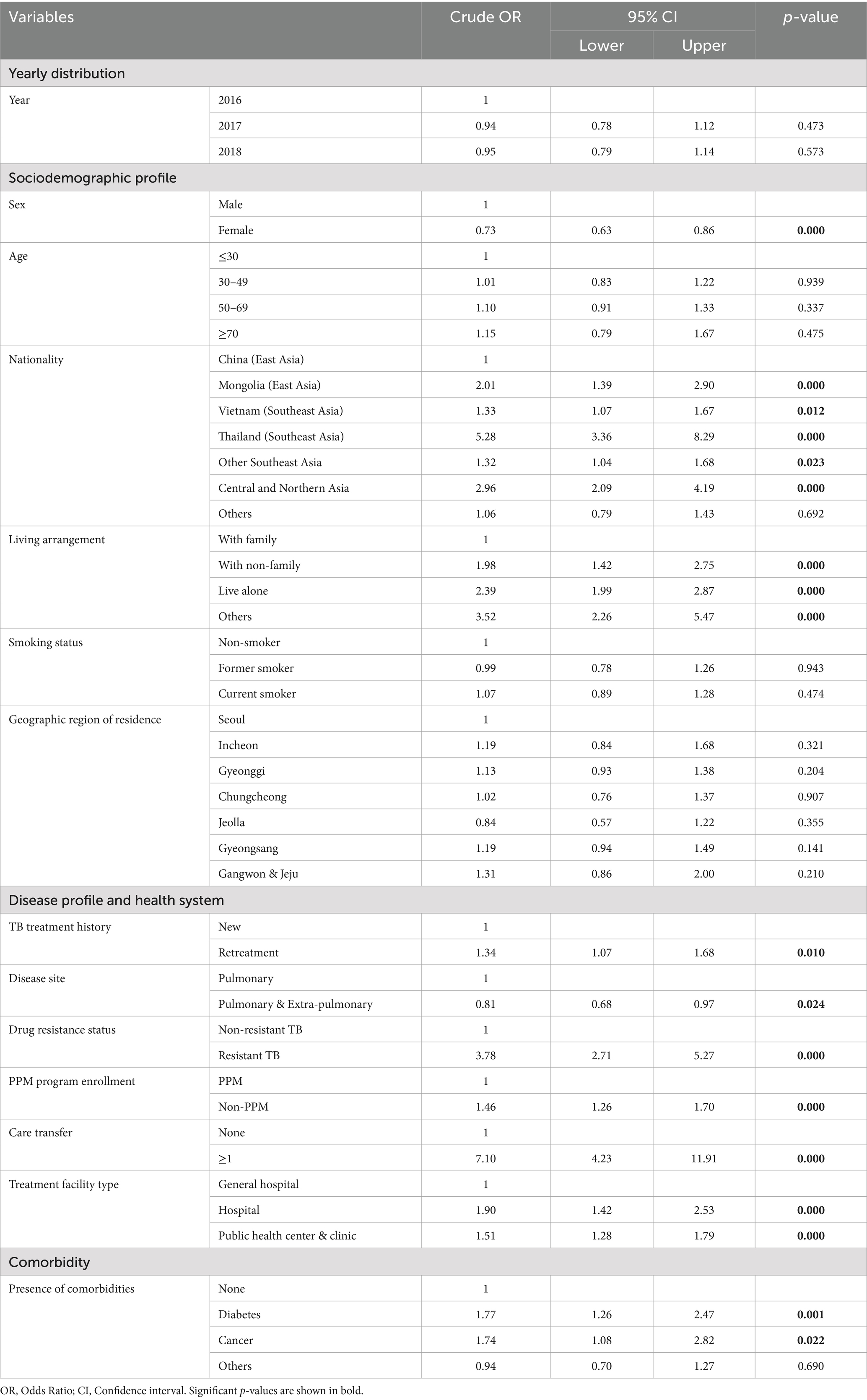
Table 1. Univariable analysis of lost to follow-up among TB patients who were migrants, registered and treated from 2016 to 2018.
Multivariate analysis confirmed similar patterns, with adjusted odds highest among Thai (aOR 5.73), Mongolian (aOR 2.31), and Vietnamese (aOR 1.79) migrants (Table 2). Living alone (aOR 2.31), having drug-resistant TB (aOR 4.43), diabetes (aOR 2.29), cancer (aOR 2.50), undergoing care transfers (aOR 7.91), and receiving clinic-based treatment (aOR 1.49) were all independently associated with increased risk.
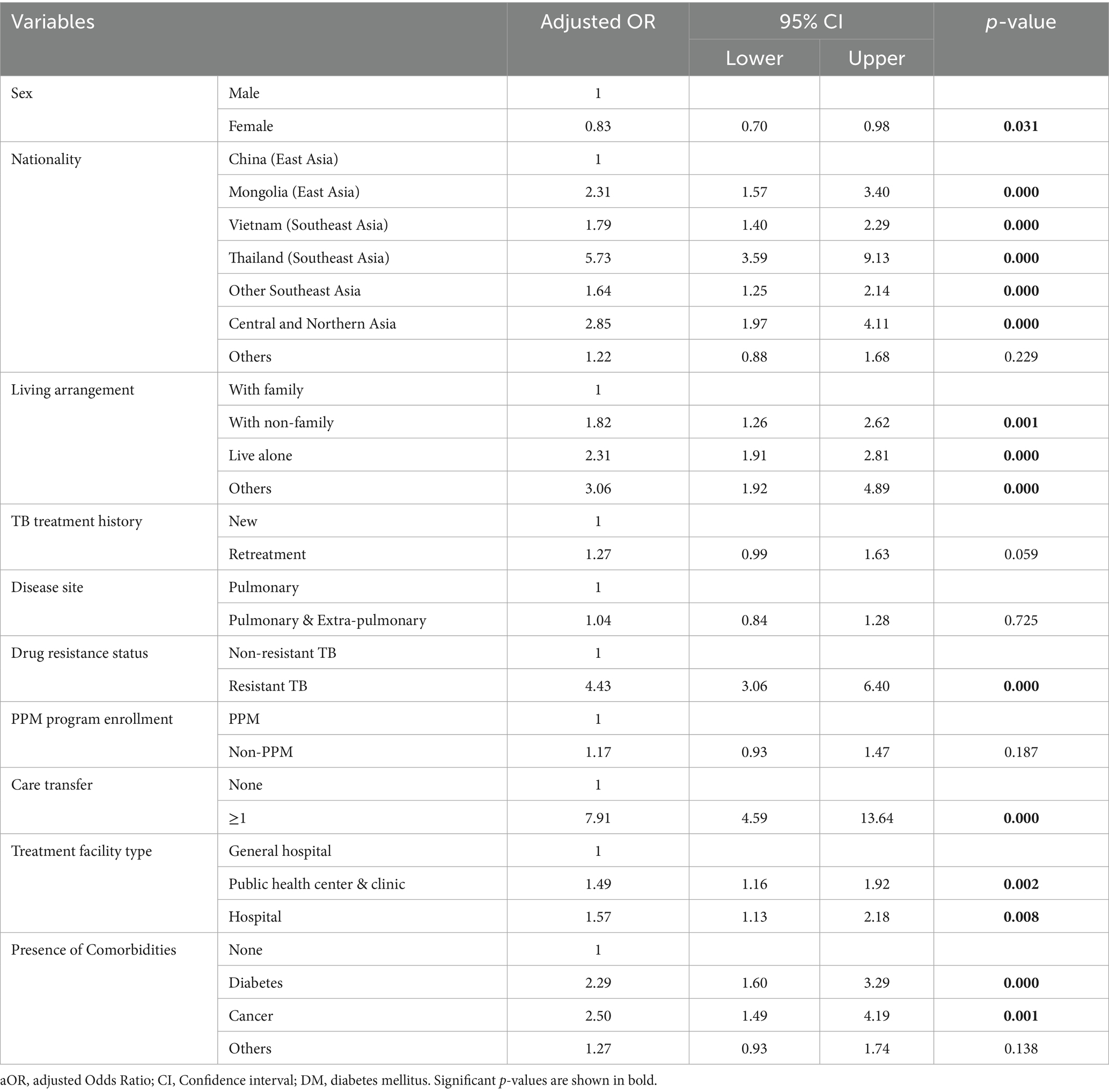
Table 2. Determinants of lost to follow-up among patients with TB patients who were migrants, registered, and treated from 2016 to 2018.
3.4 Qualitative insights into treatment discontinuation
By engaging nurses directly involved in TB management under the PPM framework, three major themes emerged from the in-depth interviews regarding the barriers that contribute to LTFU among migrant patients with TB (Table 3).
4 Discussion
This study offers crucial insights into the significant challenge of TB treatment adherence among foreign migrants in ROK, revealing a substantially higher rate of LTFU compared to native Korean patients. Despite comprising only 3.5% of the total population, foreign migrants accounted for over 5% of annual TB cases between 2016 and 2018, with an average incidence rate of 178.2 per 100,000, approximately 2.5 times higher than the national average. This disproportionate burden highlights an urgent need for targeted interventions.
The follow-up discontinuation rate among migrant patients with TB was significantly higher (21.5%) than that among domestic patients (2.3%). This significant disparity poses a critical barrier to global TB elimination efforts (26, 27). Previous research indicates that migration itself increases the likelihood of treatment discontinuation, with foreign nationals showing a higher tendency to disengage from care (19, 28). The mixed-methods approach utilized in this study provided a comprehensive understanding of the various determinants contributing to this issue. Several sociodemographic factors were found to profoundly influence LTFU among migrants.
Nationality emerged as a critical determinant of LTFU, with higher discontinuation rates seen among those from Thailand, Mongolia, and Vietnam compared to Chinese nationals. These elevated rates may partially due to systemic misclassification; Many migrants leave ROK for further care without formal transfer procedures, resulting in delayed immigration verification and erroneous classification as LTFU. Previous studies have similarly found that patients who depart without notifying health staff are flagged as LTFU once their exit is confirmed (19). Migrants with repeated treatment interruptions are often prioritized for deportation once non-infectious, contributing to higher discontinuation rates compared to residents.
Living arrangement also strongly influenced follow-up adherence. Migrants in single-person or non-family households were more likely to discontinue care than those living with their families, reflecting a lack of social and emotional support, less favorable living conditions, and limited access to healthcare (29, 30). Family presence is widely recognized as a protective factor, promoting adherence through motivation and oversight for medication adherence (31). Additional barriers—such as stigma, psychological distress, and insufficient treatment support—further hinder continuity of care for individuals living alone or in non-family environments (32, 33). Integration of housing support programs with local social welfare services has demonstrated effectiveness in mitigating risks such as drug-resistant TB, relapse, and mortality, ultimately improving overall treatment outcomes (28, 34).
The analysis identified a consistent gender disparity in TB treatment adherence, with female sex associated with lower odds of LTFU in both univariable (OR 0.73) and multivariate (aOR 0.83) models. This suggests that sex-specific factors may shape adherence patterns. Migrant females were more likely to live with family (47.8%) than males (29.3%), while males predominantly lived alone (59.5%). Since family support plays a key role in promoting medication adherence through emotional and practical support, this difference in living arrangements likely contributes to the disparity. Additionally, females reported lower smoking rates (95.3% non-smokers) versus males (37.5% current, 17.7% former smokers), indicating healthier behaviors that may support treatment completion. Females were also more often enrolled in the PPM program (58.5% vs. 49.2%), enhancing their access to structured nurse-led monitoring. These overlapping factors—social support, lifestyle, and program engagement—underscore the multifaceted gendered influences on treatment outcomes.
Clinical factors also contributed to the high LTFU rates. Drug-resistant TB significantly increased the risk of treatment discontinuation, with affected patients being 4.43 times more likely to be LTFU than those with drug-susceptible TB. The extended treatment duration, often triple that of standard regimens, and the severe side effects of second-line drugs contributes to voluntary interruption (35). These challenges underscore the need for enhanced adherence strategies, including continuous monitoring, comprehensive patient education, as well as targeted support for those with drug-resistant TB (12, 36, 37). While less common among migrants than natives, the presence of comorbidities such as diabetes and cancer significantly increased the odds of LTFU for migrants. This highlights the need for integrated care that addresses co-existing health conditions, a point also recognized in the National TB Management Guidelines which list diabetes and cancer as high-risk factors for TB progression (38).
Crucial systemic and health system factors were also identified. Migrants who experienced one or more care transfers were significantly more likely to be LTFU. This indicates that frequent transfers disrupt treatment continuity due to delays in record sharing, inconsistent protocols, and insufficient communication (39). Also, migrants had less access to PPM nurses (52.9%) compared to native Koreans (73.9%). PPM nurses are crucial for patient management, including initial investigations for reported patients and conducting vulnerability assessments for customized care (19, 40). The qualitative findings revealed that this disparity was compounded by low awareness among migrants of the availability of free TB treatment under the PPM program, leading to perceived costs at non-PPM facilities and avoidance of follow-up.
PPM nurses reported that many migrants perceived TB as a “mild cold” and prematurely discontinued treatment once symptoms improved, and are unaware of the significant risks associated with incomplete care, such as the development of drug-resistant TB and the possibility of relapse (31, 41). This underscores the urgent need for culturally and linguistically tailored educational campaigns that clearly explain TB’s severity, the importance of completing the full treatment course, and the risks of drug resistance and relapse (41–43). The qualitative data also highlighted significant language barriers and limitations of non-medical interpreters in effectively explaining complex medical information, such as drug side effects and regimen complexities. Improving medical interpretation services with trained professionals possessing specialized healthcare and TB-related knowledge is crucial to bridge these communication gaps.
These findings resonate with existing literature emphasizing that patient education, robust social support, and accessible, consistent care are fundamental to improving TB treatment adherence (19, 31). The study’s insights reinforce that overcoming high LTFU rates among migrant TB patients in the ROK necessitates a multi-faceted approach that extends beyond clinical management to address underlying social, cultural, and systemic barriers. This implies the need for proactive outreach, culturally sensitive health education, strengthened interpreter services, and policy reforms to ensure seamless, affordable, and comprehensive care for this vulnerable population. The “Tuberculosis Relief Belt” initiative represents a positive step in strengthening patient referral systems and providing financial subsidies to vulnerable groups, including support for treatment costs, outsourced medical expenses, caregiving, nutrition, and patient transport (28, 38).
While this study offers valuable insights, it is important to acknowledge its limitations. The authors themselves noted the lack of detailed clinical data, such as lung X-rays or smear/culture data, which could have made the study more robust. Similarly, the absence of detailed socioeconomic indicators (e.g., visa type, specific occupation, income, education level) limited a more nuanced understanding of disease progression and socioeconomic vulnerabilities. Additionally, the small sample size of multidrug-resistant cases restricted a thorough examination of its specific association with LTFU. Future research should aim to incorporate these variables for a more complete understanding.
4.1 Recommendations
To counter the perception of TB as a “mild cold” and prevent premature treatment discontinuation, the 2025 National TB Management Guidelines already highlight patient counseling and education as vital for successful treatment completion, covering transmission, adherence, and side effect monitoring (31). This existing framework can be leveraged to launch targeted, multilingual public health campaigns that explicitly detail the TB treatment process, emphasize the necessity of completing the full course, and explain the significant risks of non-adherence, such as drug resistance and relapse. These campaigns should utilize accessible materials, potentially drawing from resources on the “TB ZERO website” (44). Public-Private Mix (PPM) nurses and public health center TB management personnel are ideally positioned to deliver this critical education, as their roles include patient counseling and education.
Eligible migrant patients should be actively connected to ROK’s expanded “Tuberculosis Relief Belt” initiative, which is already recognized as a “pivotal measure to close gaps in TB care.” This initiative strengthens patient referral systems and provides targeted financial subsidies for socioeconomically vulnerable populations—including support for treatment costs, outsourced medical expenses, caregiving, nutrition, and patient transport (28, 38). Migrants are identified as a socioeconomically vulnerable group. The National Medical Center is specifically tasked with operating this support program.
Access to PPM programs should be also expanded by increasing the presence of dedicated PPM nurses in primary healthcare facilities, where many migrants receive initial care but which currently “lack dedicated PPM nurses.” Simultaneously, establish clear pathways for integrated care that ensures migrants with comorbidities, such as diabetes and cancer, receive specialized management. These conditions are recognized as high-risk factors in the National TB Management Guidelines, and primary care facilities often lack the necessary specialists. PPM is one of the most prioritized flagship programs under the Korean Diseases Control Agency, where its coverage has been gradually increased up to 81.5% (45).
In conclusion, this study demonstrated that migrant patients with TB in the ROK experience significantly higher rates of LTFU than native patients. The key factors contributing to this disparity include nationality, living arrangement, gender, drug-resistant TB, the presence of comorbidities, frequent care transfers, and type of treatment facility. Migrants from certain countries are disproportionately affected and often discontinue care due to transnational movements and limited support systems. Social isolation, particularly among those living alone or in non-family households, further increases the risk of treatment discontinuation, whereas the prolonged treatment required for drug-resistant TB creates additional adherence challenges. Qualitative insights further revealed barriers, such as educational gaps, misconceptions, poor medical interpretation, and low awareness of free treatment and PPM eligibility. Addressing these issues requires culturally tailored education, employer support, improved interpretation services, and a streamlined care system.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: the dataset is not in public domain as it is part of the national TB surveillance data. Requests to access these datasets should be directed to Sumin Jeon, amVvbnN1bWluMzhAZ21haWwuY29t.
Ethics statement
The studies involving humans were approved by Hanyang University Ethic Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
SJ: Formal analysis, Data curation, Methodology, Writing – original draft, Investigation, Writing – review & editing. JL: Writing – review & editing, Methodology, Investigation. IJ: Methodology, Conceptualization, Writing – review & editing. SSi: Conceptualization, Methodology, Writing – review & editing. IL: Investigation, Writing – review & editing, Methodology. YKi: Investigation, Writing – review & editing. AH: Data curation, Writing – review & editing, Investigation. S-EL: Data curation, Writing – review & editing, Investigation. SSe: Data curation, Investigation, Writing – review & editing. HK: Writing – review & editing, Data curation, Investigation. YKw: Data curation, Investigation, Writing – review & editing. CS: Investigation, Writing – review & editing, Data curation. J-SJ: Supervision, Conceptualization, Writing – review & editing, Funding acquisition. SK: Conceptualization, Supervision, Writing – original draft, Writing – review & editing, Validation.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by funding from the Division of Tuberculosis Prevention and Control, Korea Disease Control Foundation, funding number: 20210415C54-00. The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1641182/full#supplementary-material
References
2. Lee, YK, Lee, SH, Son, HJ, and Go, UY. Overview of tuberculosis control and prevention policies in Korea. Public Health Wkly Rep. (2015) 8:651–6. Available at: https://www.phwr.org/journal/archives_view.html?eid=Y29udGVudF9udW09MTg5NA==
3. Lee, HW, Kim, JS, Kim, JE, Park, YJ, Shin, JH, Cho, GW, et al. Characteristics of notified tuberculosis cases in the Republic of Korea (2023). Public Health Wkly Rep. (2024) 17:1591–608. Available at: https://www.phwr.org/journal/view.html?doi=10.56786/PHWR.2024.17.37.2
4. Lee, HJK, In, HK, and Kim, Y. Characteristics and trends in deaths from tuberculosis in the Republic of Korea (2001–2020). Public Health Wkly Rep. (2021) 14:3400–12. Available at: https://www.phwr.org/journal/view.html?pn=vol&uid=620&vmd=Full
5. Lee, HW, Kim, JS, Kim, JE, and Park, YJ. Characteristics and trends of tuberculosis deaths in 2023: an analysis of cause-of-death statistics from Statistics Korea. Public Health Wkly Rep. (2025) 18:137–54. Available at: https://www.phwr.org/journal/view.html?doi=10.56786/PHWR.2025.18.3.3
6. Infectious Disease Control and Prevention. ACT (2016-12-02). The Infectious Diseases Control and Prevention Act No 17475, Aug 12, 2020.
7. Lee, HW, Kim, JS, Park, GJ, and Choi, HY. Characteristics and trends in deaths from tuberculosis in the Republic of Korea (2022). Public Health Wkly Rep. (2022) 17:421–37. Available at: https://www.phwr.org/journal/view.html?doi=10.56786/PHWR.2024.17.11.1
9. KCDC (2016) Annual Report on the Notified TB in the Republic of Korea. Korea Center for Diseases Control (2015).
10. KDCA (2025) Annual report on the notified TB in the Republic of Korea. Korea Diseases Control and Prevention Agency (2024).
11. Sun, LJ. Epidemiology of tuberculosis in foreign immigrants and the associated factors on treatment outcome. South Korea: Korea University Graduate School (2020).
12. Min, GH, Kim, Y, Lee, JS, Oh, JY, Hur, GY, Lee, YS, et al. Social and clinical characteristics of immigrants with tuberculosis in South Korea. Yonsei Med J. (2017) 58:592–7. doi: 10.3349/ymj.2017.58.3.592
13. Min, J, and Sang, KJ. Results of the Korean National Private-Public mix Tuberculosis Control Project: analysis of the indicators for tuberculosis management in 2017–2019. Public Health Wkly Rep. (2021) 14:1926–33. Available at: https://www.phwr.org/journal/view.html?pn=vol&uid=521&vmd=Full
14. Jeong, D, Kang, HY, Kim, J, Lee, H, Yoo, BN, Kim, HS, et al. Cohort profile: Korean tuberculosis and post-tuberculosis cohort constructed by linking the Korean national tuberculosis surveillance system and National Health Information database. J Prev Med Public Health. (2022) 55:253–62. doi: 10.3961/jpmph.21.635
15. Seyedmehdi, SM, Jamaati, H, Varahram, M, Tabarsi, P, Marjani, M, Moniri, A, et al. Barriers and facilitators of tuberculosis treatment among immigrants: an integrative review. BMC Public Health. (2024) 24:3514. doi: 10.1186/s12889-024-21020-8
16. Cho, KS. Tuberculosis control in the Republic of Korea. Epidemiol Health. (2018) 40:e2018036. doi: 10.4178/epih.e2018036
17. Sharani, ZZ, Ismail, N, Yasin, SM, Zakaria, Y, Razali, A, Demong, NAR, et al. Characteristics and determinants of loss to follow-up among tuberculosis (TB) patients who smoke in an industrial state of Malaysia: a registry-based study of the years 2013–2017. BMC Public Health. (2022) 22:638. doi: 10.1186/s12889-022-13020-3
18. Park, S, Kim, HY, and Lee, YM. Unmet healthcare needs and related factors among immigrants: a cross-sectional secondary analysis of 2019 Korea community health survey data. Inquiry. (2023) 60:469580221146828. doi: 10.1177/00469580221146828
19. Kim, HW, Min, J, Ko, Y, Oh, JY, Jeong, YJ, Lee, EH, et al. Risk of loss to follow-up among tuberculosis patients in South Korea: whom should we focus on? Front Public Health. (2023) 11:1247772. doi: 10.3389/fpubh.2023.1247772
20. NECA. Establishing evidence for tuberculosis control through data linkage. National Evidence-based Healthcare Collaborating Agency (2022).
21. Baker, MA, Harries, AD, Jeon, CY, Hart, JE, Kapur, A, Lönnroth, K, et al. The impact of diabetes on tuberculosis treatment outcomes: a systematic review. BMC Med. (2011) 9:81. doi: 10.1186/1741-7015-9-81
22. Jeong, D, Mok, J, Jeon, D, Kang, HY, Kim, HJ, Kim, HS, et al. Prevalence and associated factors of diabetes mellitus among patients with tuberculosis in South Korea from 2011 to 2018: a nationwide cohort study. BMJ Open. (2023) 13:e069642. doi: 10.1136/bmjopen-2022-069642
23. WHO. Definitions and reporting framework for tuberculosis – 2013 revision. World Health Organization (2013).
26. de Vries, SG, Cremers, AL, Heuvelings, CC, Greve, PF, Visser, BJ, Bélard, S, et al. Barriers and facilitators to the uptake of tuberculosis diagnostic and treatment services by hard-to-reach populations in countries of low and medium tuberculosis incidence: a systematic review of qualitative literature. Lancet Infect Dis. (2017) 17:e128–43. doi: 10.1016/S1473-3099(16)30531-X
27. Lönnroth, K, Mor, Z, Erkens, C, Bruchfeld, J, Nathavitharana, RR, van der Werf, MJ, et al. Tuberculosis in migrants in low-incidence countries: epidemiology and intervention entry points. Int J Tuberc Lung Dis. (2017) 21:624–36. doi: 10.5588/ijtld.16.0845
28. Kim, Y, Lee, JY, Jeong, I, Kim, J, Kim, J, Han, J, et al. Factors related to successful tuberculosis treatment in vulnerable groups. Korean J Med. (2022) 97:50–9. doi: 10.3904/kjm.2022.97.1.50
29. Park, JH, Min, S, Eoh, Y, and Park, SH. The elderly living in single-person households in South Korea: a latent profile analysis of self-esteem, life satisfaction, and depression. Qual Life Res. (2021) 30:1083–92. doi: 10.1007/s11136-020-02693-1
30. Choi, H, Chung, H, Muntaner, C, Lee, M, Kim, Y, Barry, CE, et al. The impact of social conditions on patient adherence to pulmonary tuberculosis treatment. Int J Tuberc Lung Dis. (2016) 20:948–54. doi: 10.5588/ijtld.15.0759
31. Abarca Tomás, B, Pell, C, Bueno Cavanillas, A, Guillén Solvas, J, Pool, R, and Roura, M. Tuberculosis in migrant populations. A systematic review of the qualitative literature. PLoS One. (2013) 8:e82440. doi: 10.1371/journal.pone.0082440
32. Chen, X, Xu, J, Chen, Y, Wu, R, Ji, H, Pan, Y, et al. The relationship among social support, experienced stigma, psychological distress, and quality of life among tuberculosis patients in China. Sci Rep. (2021) 11:24236. doi: 10.1038/s41598-021-03811-w
33. Park, E-H, and Choi, S-E. Support system, stigma and self-care behaviors in patients with pulmonary tuberculosis. J Korean Biol Nurs Sci. (2020) 22:288–96. Available at: https://jkbns.org/journal/view.php?doi=10.7586/jkbns.2020.22.4.288
34. Kim, H, Choi, H, Yu, S, Lee, AY, Kim, HO, Joh, JS, et al. Impact of housing provision package on treatment outcome among homeless tuberculosis patients in South Korea. Asia Pac J Public Health. (2019) 31:603–11. doi: 10.1177/1010539519871779
35. Liebenberg, D, Gordhan, BG, and Kana, BD. Drug resistant tuberculosis: implications for transmission, diagnosis, and disease management. Front Cell Infect Microbiol. (2022) 12:943545. doi: 10.3389/fcimb.2022.943545
36. Yu, S, Sohn, H, Kim, HY, Kim, H, Oh, KH, Kim, HJ, et al. Evaluating the impact of the nationwide public-private mix (PPM) program for tuberculosis under National Health Insurance in South Korea: a difference in differences analysis. PLoS Med. (2021) 18:e1003717. doi: 10.1371/journal.pmed.1003717
37. Massud, A, Khan, AH, Syed Sulaiman, SA, Ahmad, N, Shafqat, M, and Ming, LC. Unsuccessful treatment outcome and associated risk factors. A prospective study of DR-TB patients from a high burden country, Pakistan. PLoS One. (2023) 18:e0287966. doi: 10.1371/journal.pone.0287966
38. KDCA. National tuberculosis control guidelines 2025. Korea Diseases Control and Prevention Agency (2025).
39. Lee, JY, Myong, JP, Kim, Y, Jeong, I, Kim, J, Sin, S, et al. Identifying predictors of unfavorable treatment outcomes in tuberculosis patients. Int J Environ Res Public Health. (2024) 21:1454. doi: 10.3390/ijerph21111454
40. Go, U, Park, M, Kim, UN, Lee, S, Han, S, Lee, J, et al. Tuberculosis prevention and care in Korea: evolution of policy and practice. J Clin Tuberc Other Mycobact Dis. (2018) 11:28–36. doi: 10.1016/j.jctube.2018.04.006
41. Park, CK, Shin, HJ, Kim, YI, Lim, SC, Yoon, JS, Kim, YS, et al. Predictors of default from treatment for tuberculosis: a single center case-control study in Korea. J Korean Med Sci. (2016) 31:254–60. doi: 10.3346/jkms.2016.31.2.254
42. Creswell, J, Raviglione, M, Ottmani, S, Migliori, GB, Uplekar, M, Blanc, L, et al. Tuberculosis and noncommunicable diseases: neglected links and missed opportunities. Eur Respir J. (2011) 37:1269–82. doi: 10.1183/09031936.00084310
43. Cho, KS. Tuberculosis control in the Republic of Korea. South Korea: Korea Institute for Health and Social Affairs (2017).
44. KDCA. (2025). TB ZERO. Available online at: https://tbzero.kdca.go.kr/tbzero/index.jsp.
Keywords: tuberculosis, lost to follow-up, migrants, Republic of Korea, private-public mix
Citation: Jeon S, Lee JY, Jeong I, Sin S, Lee I, Kim Y, Han AY, Lee S-E, Seo S, Kim H, Kwon Y, Song C, Joh J-S and Kim SH (2025) Determinants of the lost to follow-up status among patients with tuberculosis who emigrated to the Republic of Korea: a mixed-method study. Front. Public Health. 13:1641182. doi: 10.3389/fpubh.2025.1641182
Edited by:
Adwoa Asante-Poku, University of Ghana, GhanaReviewed by:
Margaret Haworth-Brockman, University of Manitoba, CanadaSigifredo Pedraza-Sanchez, National Institute of Medical Sciences and Nutrition Salvador Zubirán, Mexico
Copyright © 2025 Jeon, Lee, Jeong, Sin, Lee, Kim, Han, Lee, Seo, Kim, Kwon, Song, Joh and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joon-Sung Joh, c3NhYmFuYTc3N0BnbWFpbC5jb20=; Sung Hye Kim, c3VuZ2h5ZWtpbUBoYW55YW5nLmFjLmty
 Sumin Jeon
Sumin Jeon Ji Yeon Lee2
Ji Yeon Lee2 Sung Hye Kim
Sung Hye Kim