- 1Department of Respiratory and Critical Care Medicine, Affiliated Hospital of North Sichuan Medical College, Nanchong, Sichuan, China
- 2Department of Critical Care Medicine, Affiliated Hospital of North Sichuan Medical College, Nanchong, Sichuan, China
- 3Department of Pulmonary and Critical Care Medicine, Center of Respiratory Medicine, National Center for Respiratory Medicine, China-Japan Friendship Hospital, Beijing, China
Background: Occupational risks contribute substantially to the global burden of pneumoconiosis, chronic obstructive pulmonary disease (COPD), tracheal-bronchus-and-lung (TBL) cancer, and asthma; however, comprehensive, up-to-date global, regional, and national estimates remain limited.
Methods: Data from the Global Burden of Disease Study (GBD) 2021 were analyzed to quantify the burden of these diseases attributable to occupational exposure across 204 countries between 1990 and 2021, stratified by sex, age, socio-demographic index (SDI), and geographic region.
Results: In 2021, occupational risks led to 30,546 deaths due to pneumoconiosis, 285,628 deaths due to COPD, 585,451 deaths due to TBL (the highest among the four diseases), and 18,315 deaths due to asthma, with disability-adjusted life years (DALYs) of 1.8, 6.1, 12.6, and 0.4 million, respectively. Male patients exhibited higher burdens of all diseases, reflecting greater exposure to male-dominated industries. Geographically, middle SDI regions had the highest absolute cases for pneumoconiosis and COPD, high-SDI regions for TBL cancer, and low-middle SDI regions for asthma. While age-standardized rates declined for most outcomes over time, the absolute burdens increased owing to population growth and aging, with demographic factors driving up to 80% of the increase in total cases. Health inequities persisted, with lower SDI regions bearing a disproportionate burden, despite modest improvements in absolute inequalities.
Conclusion: These findings highlight the need for strengthened occupational health regulations, targeted interventions in high-risk regions, and policies addressing population dynamics to mitigate the impact of workplace exposure on respiratory health.
1 Introduction
Occupational respiratory diseases pose a significant global public health challenge, with workplace exposures to harmful agents substantially contributing to the burden of pneumoconiosis, chronic obstructive pulmonary disease (COPD), tracheal-bronchus-and-lung (TBL) cancer, and asthma (1–3). Among these, pneumoconiosis, a group of interstitial lung diseases caused by the inhalation of mineral dust, such as silica, coal, and asbestos, has long been recognized as a major occupational hazard (4). In 2024, the National Health Commission of China highlighted the high prevalence of pneumoconiosis that accounted for approximately 90% of all reported occupational disease cases nationwide (5). Mining, construction, and manufacturing workers are particularly vulnerable, and the disease often leads to irreversible lung damage, diminished quality of life, and premature death (6). COPD, a progressive disease characterized by persistent airflow limitation, is also strongly linked to occupational exposures. Inhalation of dust, fumes, and chemical vapors in the workplace can exacerbate symptoms and accelerate disease progression (7). A landmark study published in The Lancet in 2007 highlighted the significant role of occupational factors in the onset and advancement of COPD (3, 8). Similarly, TBL cancer, which is the leading cause of cancer-related deaths worldwide, has a well-established occupational dimension. Workplace exposure to carcinogens, such as asbestos, arsenic, and polycyclic aromatic hydrocarbons, markedly increases the risk of lung cancer (9). The International Agency for Research on Cancer has classified multiple occupational exposures as carcinogenic to humans, reaffirming the critical link between the occupational environment and cancer risk (10). Asthma, a chronic inflammatory disease of the airway, can be caused or aggravated by occupational exposure. Substances such as isocyanates, flour dust, and animal proteins trigger occupational asthma (11) that constitutes a substantial proportion of adult-onset cases and often results in reduced work productivity and impaired quality of life (12).
Despite well-documented associations between occupational exposure and respiratory diseases, comprehensive and up-to-date assessments of the global, regional, and national burdens attributable to these risks remain scarce. Existing research has often focused on specific regions or occupational groups (13). For example, some studies have highlighted the high prevalence of pneumoconiosis among miners in certain countries, whereas others have examined the impact of industrial chemicals on COPD in localized manufacturing settings (14). Therefore, there is a pressing need for systematic and longitudinal analyses of evidence-based prevention and intervention strategies (15).
The Global Burden of Disease (GBD) study provides a robust framework for quantifying health losses owing to diseases, injuries, and risk factors across different geographic levels (16). By analyzing data between 1990 and 2021, this study aimed to estimate the burdens of pneumoconiosis, COPD, TBL cancer, and asthma attributable to occupational exposure. These findings aimed to identify high-risk populations and regions, support policy development, and guide the implementation of targeted interventions to mitigate the impact of occupational respiratory diseases (17).
2 Methods
2.1 Data sources
This study draws on GBD 2021, which compiles mortality, morbidity, and risk-factor data across 204 countries and territories from diverse sources (vital registration, surveys, clinical records, registries, and literature) (15). We extracted occupational exposure and attributable burden estimates for pneumoconiosis, COPD, TBL cancer, and asthma. GBD ensures cross-location comparability using standardized models—CODEm for cause-specific mortality and DisMod-MR 2.1 for nonfatal outcomes—that adjust for underreporting and misclassification and provide 95% uncertainty intervals. Population size and age structure are incorporated via UN Population Division estimates, and results are reported as counts and age-standardized rates per 100,000 using the GBD standard population.
In this study, “occupational risks” were defined according to the GBD 2021 classification. In brief, exposures were categorized as mineral dusts for pneumoconiosis; dust, fumes, and chemical vapors for COPD; occupational carcinogens for TBL cancer; and sensitizing agents for asthma. Specifically, pneumoconiosis was attributed to prolonged exposure to mineral dusts (e.g., silica, coal, asbestos); COPD was linked primarily to workplace exposure to dust, fumes, and chemical vapors; TBL cancer was associated with carcinogens such as asbestos, arsenic, and polycyclic aromatic hydrocarbons; and asthma was related to sensitizers including isocyanates, flour dust, and animal proteins.
The data included deaths, disability-adjusted life years (DALYs), years lived with disability (YLDs), and years of life lost (YLLs) between 1990 and 2021.
Country-level socio-demographic index (SDI) values, a composite measure of income per capita, education, and fertility rates, were obtained from the GBD 2021 database to stratify the analyses by development status. The geographic classifications followed the GBD regions (54 regions) and SDI quintiles (low, low-middle, middle, high-middle, and high) (18).
2.2 Statistical analysis
2.2.1 Burden disaggregation
The disease burden of pneumoconiosis, COPD, TBL cancer, and asthma attributable to occupational risks was stratified by sex, age groups (5-year intervals from 0–4 to ≥95 years), SDI regions, GBD regions, and individual countries in 2021. Age-standardized rates (ASRs) were calculated using the GBD global reference population to enable cross-regional comparisons.
2.2.2 Temporal trend analysis
Linear regression analysis was applied to assess the temporal trends in age-standardized death, DALYs, YLDs, and YLLs rates between 1990 and 2021. The estimated annual percentage changes (EAPCs) with 95% confidence intervals (CIs) were calculated for each trend segment. EAPCs were derived from the regression coefficient (β) of the natural log-transformed rates against calendar year: EAPC = 100 × (e^β − 1). Trends were categorized as increasing (EAPC > 0), decreasing (EAPC < 0), or stable (EAPC = 0).
2.2.3 Forecasting to 2050
The Bayesian age-period-cohort (BAPC) model was employed to project the burden of occupational risk-related pneumoconiosis, COPD, TBL cancer, and asthma up to 2050. Autoregressive Integrated Moving Average (ARIMA) models and Exponential Smoothing (ES) models were used for the sensitivity analysis.
2.2.4 Decomposition analysis
A demographic decomposition approach partitioned the changes in total deaths, DALYs, YLDs, and YLLs from 1990 to 2021 into three components: (1) population growth, (2) aging (population age structure shifts), and (3) epidemiological changes (age-specific rate variations). The analysis followed the formula:
ΔBurden = ΔPopulation + ΔAging + ΔEpidemiology.
The contribution percentages were calculated for each component.
2.2.5 Health inequality assessment
Health inequities across the SDI quintiles and countries were evaluated using the Slope Index of Inequality (SII) and CI. The SII quantified the absolute differences in ASRs between the highest and lowest SDI groups, whereas the CI measured the relative inequality across the full SDI spectrum.
2.3 Software and validation
All analyses were conducted using the R statistical software (version 4.2.2; R Foundation for Statistical Computing). Key packages included forecast for time-series modeling, and decomp for decomposition analysis. Ethical approval was waived because this study utilized fully anonymized aggregated GBD data.
3 Results
3.1 Disease burden in 2021
In 2021, occupational risks contributed substantially to the global burden of pneumoconiosis, COPD, TBL cancer, and asthma. For pneumoconiosis, there were 30,546 deaths (95% uncertainty interval [UI]: 24,722–43,991), corresponding to an age-standardized death rate (ASDR) of 0.35 (95% UI: 0.28–0.50) per 100,000 population. The disease also caused 1,761,566 DALYs (95% UI: 1,420,293–2,248,898), with an age-standardized DALY rate (ASDAR) of 20.75 (95% UI: 16.7–26.5). Of these, 725,527 were YLDs (ASYLDR 8.71; 95% UI: 5.59–12.66) and 1,036,039 were YLLs (ASYLLR 4.66; 95% UI: −0.45–12.42) (Supplementary Tables S1–S4).
For COPD, occupational exposures were responsible for 285,628 deaths (95% UI: 217,606–354,452), yielding an ASDR of 3.36 (95% UI: 2.56–4.15). The total DALYs reached 6,120,478 (95% UI: 4,668,066–7,778,938), with an ASDAR of 70.41 (95% UI: 53.84–89.37). These were mainly driven by YLLs (6,042,447 cases), while YLDs contributed a smaller share (78,031 cases, ASYLDR 0.91; 95% UI: 0.60–1.26) (Supplementary Tables S5–S8).
For TBL cancer, occupational risks accounted for 585,451 deaths (95% UI: 470,475–715,711), corresponding to an ASDR of 7.03 (95% UI: 5.64–8.67). This represented the highest burden among the four diseases, with 12,601,863 DALYs (95% UI: 10,575,240–14,969,388) and an ASDAR of 147.29 (95% UI: 123–174.54). The burden was primarily from YLLs (10,550,544 cases, ASYLLR 123.5; 95% UI: 101.14–147.67), although YLDs also contributed over two million cases (ASYLDR 23.79; 95% UI: 18.87–28.51) (Supplementary Tables S9–S12).
For asthma, occupational exposures were linked to 18,315 deaths (95% UI: 16,054–20,938), with an ASDR of 0.22 (95% UI: 0.19–0.25). The total DALYs were 446,894 (95% UI: 392,414–512,871), with an ASDAR of 5.22 (95% UI: 4.58–5.97). These were composed of 59,941 YLDs (ASYLDR 0.70; 95% UI: 0.47–0.98) and 386,953 YLLs (ASYLLR 4.52; 95% UI: 3.93–5.25) (Supplementary Tables S13–S16).
When stratified by sex, men consistently carried a higher burden of pneumoconiosis, COPD, TBL cancer, and asthma attributable to occupational risks than women, reflecting greater occupational exposure (Supplementary Tables S1–S16 and Supplementary Figures S1–S4). Age-specific analyses revealed a typical pattern of increasing burden with age, peaking in older adults, followed by a decline (Supplementary Figures S5–S8).
Geographical comparisons showed that middle-SDI regions reported the highest absolute numbers of pneumoconiosis and COPD; high-SDI regions bore the greatest burden of TBL cancer; and low-middle-SDI regions carried the largest burden of asthma. However, patterns of ASRs differed, highlighting the influence of demographic structure and exposure intensity (Supplementary Figures S9–S12).
Finally, significant heterogeneity was observed among the 54 GBD regions and 204 countries, emphasizing substantial differences in occupational exposures and disease outcomes worldwide. Detailed estimates for each region and country are provided in Supplementary Figures S13–S20.
3.2 Temporal trend between 1990 and 2021
Between 1990 and 2021, ASRs of pneumoconiosis, COPD, TBL cancer, and asthma attributable to occupational risks generally showed a declining trend, with the exception of ASYLDRs for TBL cancer and asthma, which remained stable or slightly increased. For pneumoconiosis, decreases were observed in DALYs, YLDs, and YLLs, whereas other indicators showed upward trends across the four diseases (Supplementary Figures S21–S24 and Supplementary Tables S1–S16).
When stratified by sex and age, the temporal patterns were broadly consistent with the global trend, with both men and women, as well as most age groups, showing gradual declines in ASRs across all four diseases (Supplementary Figures S25–S32). Similarly, across SDI regions, the overall patterns remained comparable, though the magnitude of the decline varied (Supplementary Figures S33–S36).
Marked regional heterogeneity was observed. For example, ASRs of pneumoconiosis declined substantially in East Asia, South Asia, and most African regions, but showed increases in Oceania and Australasia. COPD-related burdens decreased across much of Europe and high-income Asia Pacific, while rising trends were observed in East Asia and parts of the Western Pacific. TBL cancer demonstrated sustained increases in several Asian and Middle Eastern regions, contrasting with declining burdens in North America and parts of Europe. Asthma showed decreasing ASRs in many low- and middle-income regions but increasing burdens in Oceania and high-income North America (Supplementary Figures S37–S40).
At the national level, additional variations were evident, with some countries experiencing accelerated declines, while others continued to show rising trends. Detailed country-specific trajectories are provided in Supplementary Figures S41–S44 and Supplementary Tables S1–S16.
3.3 Predicted results between 2022 and 2050
Regarding the projections of the BAPC, ARIMA, and ES models from 2022 to 2050, a consistent upward trend is observed in the number of cases for both sexes. However, for the corresponding ASRs, the trends are either relatively stable or decreasing (Supplementary Figures S45–S56). Globally, COPD-related deaths attributable to occupational risks are projected to rise from about 285,000 in 2021 to more than 400,000 by 2050 (95% UI: 350,000–460,000). Over the same period, deaths from TBL cancer linked to occupational exposures are expected to increase from roughly 585,000 to over 800,000 (95% UI: 720,000–910,000). Similarly, asthma-related DALYs attributable to occupational exposures are anticipated to grow from 0.45 million in 2021 to approximately 0.60 million by 2050 (95% UI: 0.52–0.70 million).
It is important to note that the predicted increases in absolute numbers of COPD- and TBL cancer–related deaths, as well as asthma-related DALYs, may not solely reflect current occupational environments but also the long latency periods characteristic of many occupational diseases. For example, tracheal, bronchus, and lung cancer can take up to three decades to develop after carcinogenic exposure. As such, part of the projected future burden likely represents the cumulative effects of historic exposures, particularly in regions with a legacy of mining, asbestos use, or other high-risk industries. This latency implies that even if occupational exposure controls are strengthened today, measurable reductions in disease burden may only become evident after several decades. Conversely, regions that industrialized more recently may still experience rising burdens despite improvements in regulation, as prior exposures continue to manifest as disease outcomes over the projection horizon.
3.4 Decomposition analysis
Over the past 31 years, a significant global increase in the burden of pneumoconiosis, COPD, TBL cancer, and asthma attributable to occupational risk has been observed. This increase was predominantly fueled by positive population growth and was partially mitigated by negative shifts in epidemiological transitions and aging (Figures 1–4).
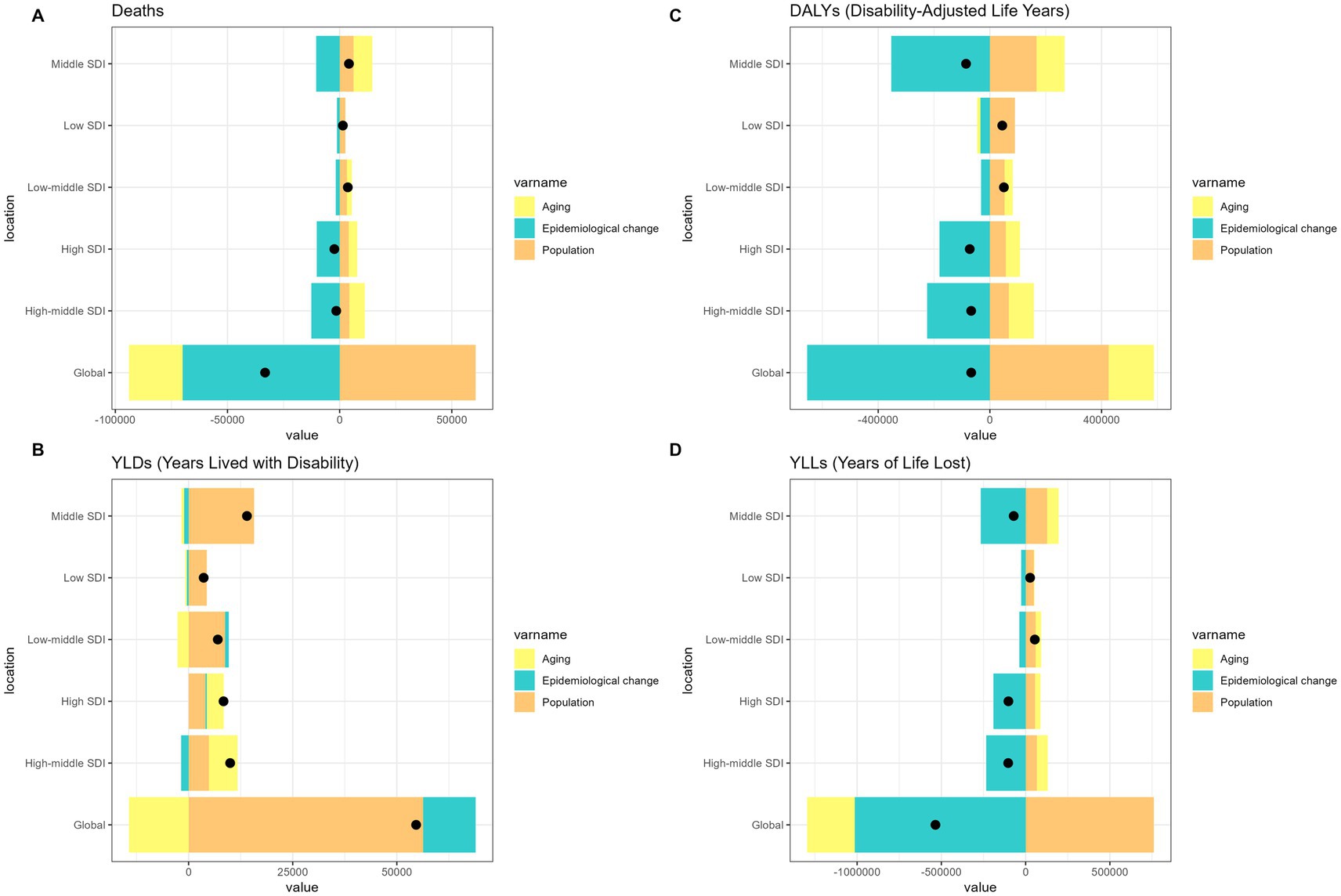
Figure 1. Alterations in the number of cases of pneumoconiosis attributable to occupational risks based on the population-level determinants of population growth, aging, and epidemiological alteration between 1990 and 2021 at the global level and by SDI quintile. SDI, socio-demographic index.
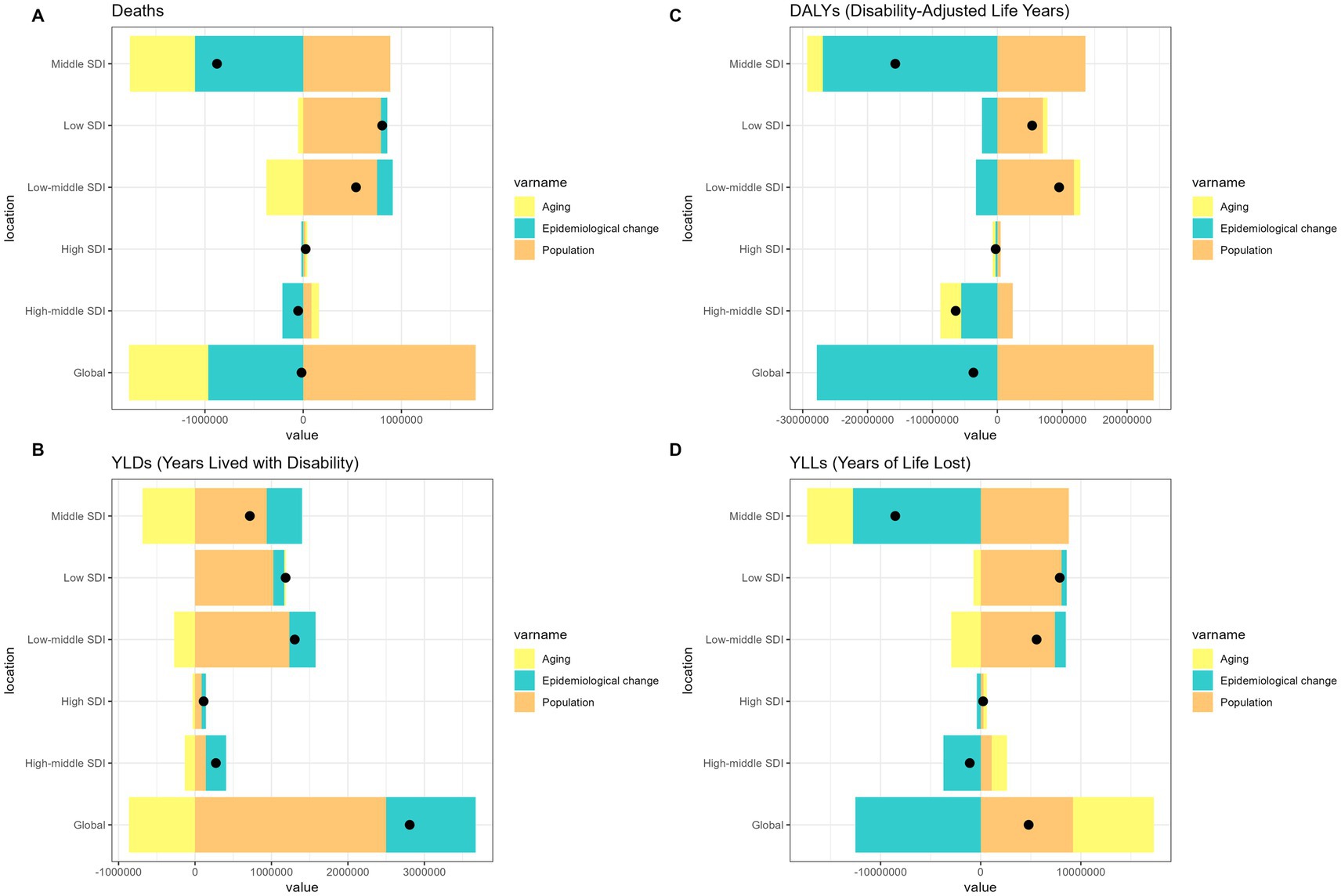
Figure 2. Alterations in the number of cases of chronic obstructive pulmonary disease attributable to occupational risks based on the population-level determinants of population growth, aging, and epidemiological alteration between 1990 and 2021 at the global level and by SDI quintile. SDI, socio-demographic index.
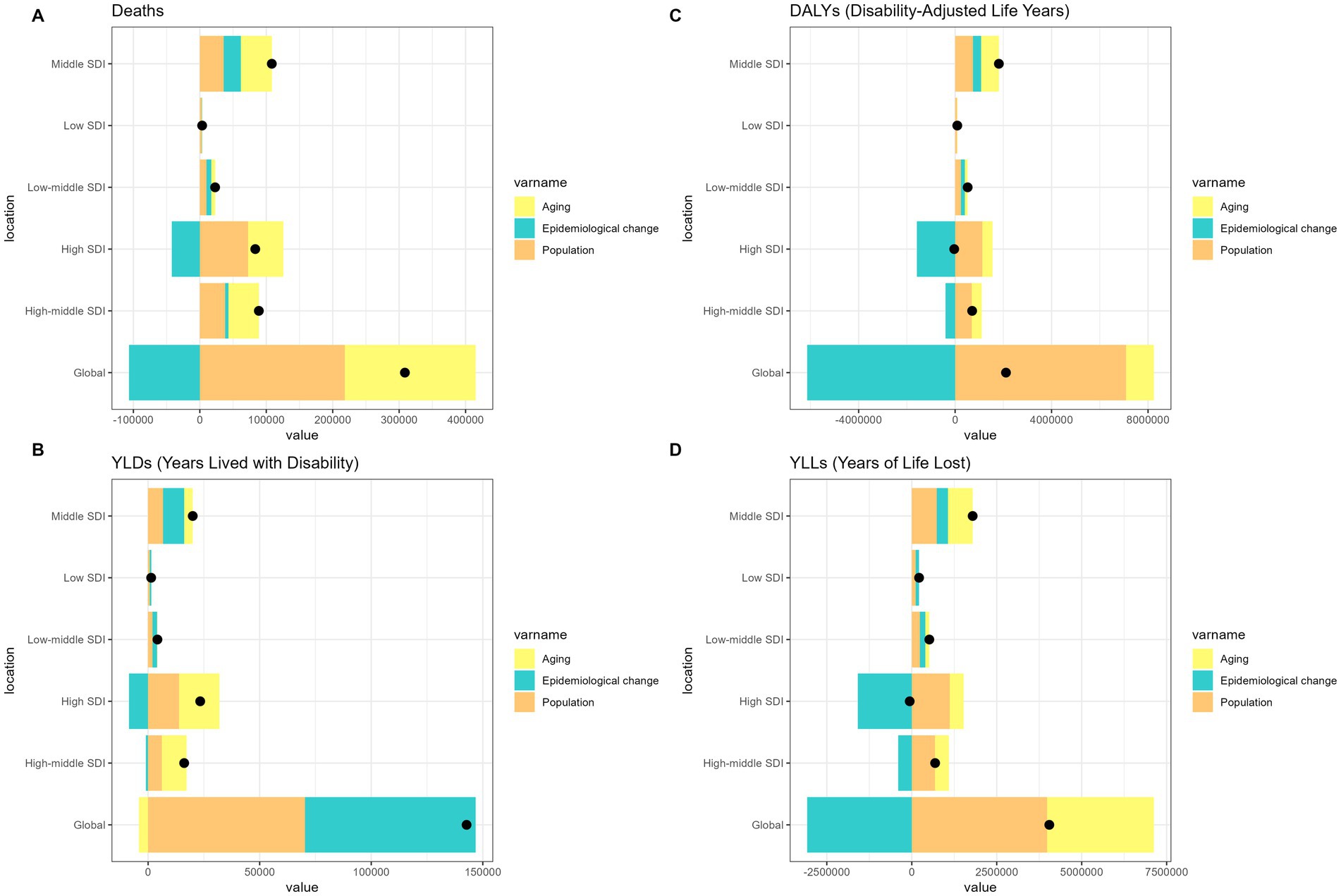
Figure 3. Alterations in the number of cases of tracheal-bronchus-and-lung cancer attributable to occupational risks based on the population-level determinants of population growth, aging, and epidemiological alteration between 1990 and 2021 at the global level and by SDI quintile. SDI, socio-demographic index.
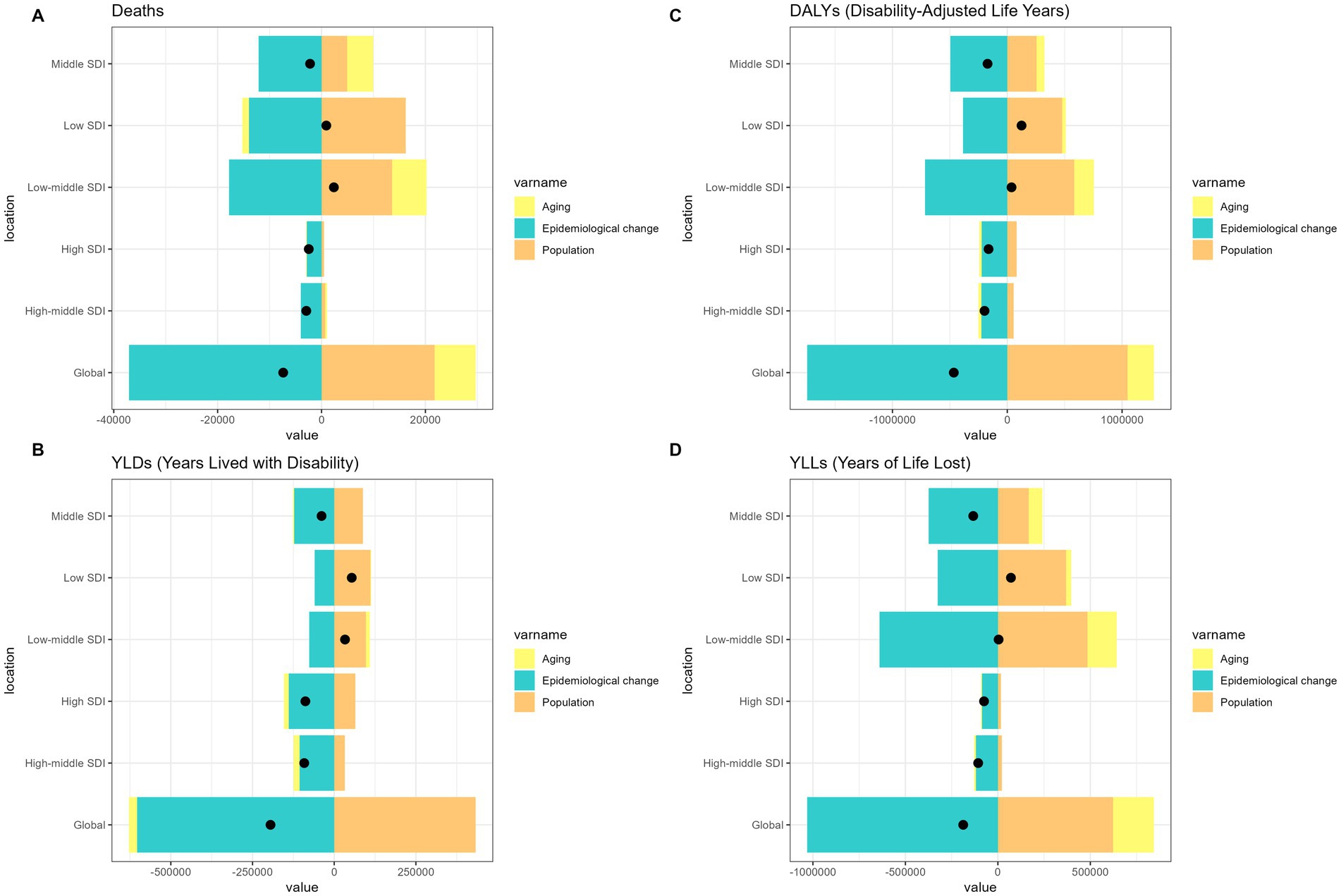
Figure 4. Alterations in the number of cases of asthma attributable to occupational risks based on the population-level determinants of population growth, aging, and epidemiological alteration between 1990 and 2021 at the global level and by SDI quintile. SDI, Socio-demographic index.
3.5 Health inequality analysis
Globally, the ASRs burden of pneumoconiosis, COPD, TBL cancer, and asthma attributable to occupational risks is primarily concentrated in areas with lower SDI. Between 1990 and 2021, the SII demonstrated an improvement in inequality among lower SDI countries. In contrast, the concentration index of ASRs showed a relatively stable trend, reflecting a consistent burden concentration in countries with lower SDI (Supplementary Figures S57–S60).
4 Discussion
This study provides a comprehensive analysis of the global, regional, and national burdens of pneumoconiosis, COPD, TBL cancer, and asthma attributable to occupational risks between 1990 and 2021. In 2021, occupational risks contributed to a substantial disease burden, with TBL cancer accounting for the highest number of deaths (585,451; DALYs, 12,601,863), followed by COPD (285,628 deaths; 6,120,478 DALYs). Pneumoconiosis, which causes fewer deaths (30,546), had a high burden of YLDs (725,527), reflecting its irreversible nature. Asthma attributable to occupational risks had the lowest mortality rate (18,315 deaths), but remained a significant cause of morbidity. Male patients consistently bore a higher burden across all diseases because of the historically higher exposure in male-dominated industries (19). Geographically, the middle SDI regions had the highest absolute burden of pneumoconiosis and COPD, the high-SDI regions reported the highest TBL cancer burden, and the low-middle SDI regions had the highest asthma burden. Temporal trends showed declining ASRs for most outcomes; however, absolute numbers increased owing to population growth and aging, highlighting the need for sustained interventions (20).
Our findings are broadly consistent with prior epidemiological evidence. We observed a substantial occupational burden of COPD, echoing earlier systematic reviews that identify workplace exposures as key contributors to COPD onset and progression (21, 22). The high prevalence of pneumoconiosis in China and India likewise accords with recent national reports, which note that pneumoconiosis constitutes over 90% of all occupational diseases in China (23, 24). Notable discrepancies also emerged. Although our projections indicate continued growth in TBL cancer cases through 2050, other studies have documented declining trends in asbestos-related outcomes, which may reflect differences in modeling strategies and time horizons (25, 26). In addition, while we estimate a decreasing burden of occupational asthma in select low-income regions, previous work reports rising asthma prevalence in Africa (27). Such divergences likely stem from heterogeneity in data sources, surveillance capacity, and whether demographic dynamics are explicitly incorporated into the modeling framework. Overall, by leveraging the GBD 2021 framework, our study provides the most up-to-date global estimates and, in several respects, complements and extends the existing literature.
The dominance of TBL cancer in high-SDI regions aligns with the historical exposure to well-characterized carcinogens, such as asbestos and arsenic, in industrialized settings (28, 29). For example, a 2019 study in Environmental Health Perspectives linked long-term occupational carcinogen exposure in North America and Western Europe to an elevated lung cancer risk, consistent with our findings of stable to increasing ASRs in these regions despite stricter regulations (29). In contrast, the high burden of pneumoconiosis in middle SDI regions, such as China and India, indicates inadequate dust control in mining and construction industries (30, 31). China’s National Health Commission noted that pneumoconiosis accounts for 90% of the occupational diseases in the country, a finding reflected in our data showing a peak ASRs in East Asia (30).
The COPD attributable to occupational risks demonstrated a complex pattern, while high-SDI regions, such as Australasia saw declining ASRs, upper-middle SDI regions (Eastern Europe) experienced increases, possibly because of persistent exposure to coal dust and chemical fumes in transitioning economies (32, 33). The Lancet highlighted occupational factors as key drivers of COPD progression, which our decomposition analysis confirmed, showing that epidemiological changes (improved workplace safety) only partially offset the population growth effects (33).
Occupational asthma, although less lethal, poses a significant burden in low-middle SDI regions, likely due to exposure to organic dust (flour and wood dust) and isocyanates in manufacturing without adequate respiratory protection (34, 35). A recent study associated rising asthma incidence in South Asia with informal sector employment, which is consistent with our findings of high burdens in low-middle SDI clusters (35).
The decline in age-standardized death and DALY rates for most diseases reflects progress in mitigating occupational hazards, primarily through the reduction of workplace exposures to hazardous substances. Key drivers include the global phase-out of asbestos (linked to pneumoconiosis and TBL cancer), implementation of dust-control strategies, stricter occupational health regulations, and structural changes in industry that have shifted workers away from high-exposure sectors (25, 36). Although workplace ventilation improvements may contribute, the critical factor is reduced intensity and duration of exposure to harmful agents. In addition, changes in non-occupational determinants likely influenced disease trends. For example, declining smoking prevalence in some high-SDI countries has reduced COPD incidence, while persistently high smoking rates in low- and middle-SDI regions may have attenuated progress. For TBL cancer, the rising number of YLDs despite relatively stable ASRs suggests improved survival associated with early detection and treatment in high-SDI regions; however, this contrasts with the poorer prognosis in low-SDI settings lacking adequate screening programs (37).
The regional disparities in trend directions are striking. These regional differences likely reflect variation in industrial structure, regulatory enforcement, and the availability of occupational health resources across countries. The decline observed in East Asia, particularly in China, is plausibly related to the recent adoption of stricter exposure control measures and strengthened occupational health legislation. By contrast, the increases in Oceania and Australasia are likely tied to legacy exposures in mining-oriented economies, where workers continue to experience long-term consequences despite improved contemporary standards. In high-SDI regions such as North America and Western Europe, the comparatively high burden of TBL is consistent with historical exposure to asbestos and other carcinogens, although tighter regulations have tempered further growth. Conversely, in low-SDI regions, the persistent burden of occupational asthma may stem from inadequate regulation, limited access to personal protective equipment, and weak health surveillance systems, which together lead to underrecognition and delayed intervention. Oceania and Australasia saw increasing pneumoconiosis ASRs, possibly due to legacy exposures in mining sectors with aging workforces (38), whereas sharp declines in East Asia reflect China’s recent occupational health reforms (30). For asthma, unexpected increases in high-SDI regions such as North America may be related to underdiagnosis in subtle exposure scenarios (laboratory chemicals), whereas declines in sub-Saharan Africa could stem from reduced industrialization or data limitations (27).
The concentration of the disease burden in regions with lower SDI highlights systemic inequities in occupational health protection. SII improvements suggest a narrowing of absolute gaps, but stable CIs indicate persistent relative disparities. This mirrors global trends in occupational health, where low-income countries lack regulatory frameworks and surveillance systems, leading to higher exposure to unregulated hazards (39, 40). Interventions must prioritize resource-constrained regions by combining engineering controls (dust extraction), personal protective equipment, and health monitoring (41). The International Labor Organization emphasizes that improving workplace safety could prevent 86% of occupational lung disease deaths, underscoring the cost-effectiveness of policy action (42).
This study has few limitations that warrant consideration. First, the reliance on GBD data assumes accurate quantification of occupational exposure, which may be underreported in regions with limited surveillance, particularly for niche hazards, such as rare industrial chemicals (43). Second, our analysis aggregated diverse occupational risks (dust, fumes, and carcinogens), potentially obscuring hazard-specific contributions (44). Third, projections for 2050 assume stable socioeconomic and policy environments, which may not account for future technological advancements or regulatory shifts (global asbestos bans) (45). Finally, sex disparity analysis, while showing male predominance, did not explore sex-specific exposure pathways (maternal occupational risks affecting offspring asthma) highlighting a gap for future research (46).
5 Conclusion
This study highlights the enduring global burden of occupational respiratory diseases with distinct regional and demographic patterns. While ASRs have declined in many areas, population growth and aging threaten to exacerbate absolute burdens, particularly in the middle and low-middle SDI regions. Addressing these disparities requires coordinated action, including strengthening occupational health regulations in developing economies, investing in exposure monitoring, and promoting sex-sensitive interventions. The GBD framework provides a critical tool for prioritization, but sustained political will and international collaboration are essential to translate evidence into actionable policies and reduce preventable workplace risks.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
SL: Conceptualization, Data curation, Formal analysis, Funding acquisition, Writing – original draft, Writing – review & editing. XDi: Data curation, Formal analysis, Funding acquisition, Writing – original draft, Writing – review & editing. XDa: Formal analysis, Project administration, Writing – original draft, Writing – review & editing. QZ: Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Key Project of the Affiliated Hospital of North Sichuan Medical College (2023ZD008), the Project of the Doctoral Initiation Fund (2023GC002), Scientific Research and Development Program Project (2024PTZK008), and Sichuan Province Clinical Key Specialty Construction Project (2023GZZKP002).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1652216/full#supplementary-material
References
1. Reid, PA, and Reid, PT. Occupational lung disease. J R Coll Physicians Edinb. (2013) 43:44–8. doi: 10.4997/JRCPE.2013.111
2. American Thoracic Society. Idiopathic pulmonary fibrosis: diagnosis and treatment. International consensus statement. American Thoracic Society (ATS), and the European Respiratory Society (ERS). Am J Respir Crit Care Med. (2000) 161:646–64. doi: 10.1164/ajrccm.161.2.ats3-00
3. Mannino, DM, and Buist, AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. (2007) 370:765–73. doi: 10.1016/S0140-6736(07)61380-4
4. Grosse, Y, Lajoie, P, Billard, M, Krewski, D, Rice, J, Baan, RA, et al. Development of a database on tumors and tumor sites in humans and in experimental animals for 'group 1 agents identified through volume 109 of the IARC monographs. J Toxicol Environ Health B Crit Rev. (2019) 22:237–43. doi: 10.1080/10937404.2019.1642601
5. Chen, HL, Li, CH, Zhai, PY, Zhuang, X, Lian, YL, Qiao, X, et al. Survival and disease burden analyses of occupational pneumoconiosis during 1958-2021 in Huangshi city, China: a retrospective cohort study. BMC Public Health. (2024) 24:1437. doi: 10.1186/s12889-024-18847-6
6. Viegi, G, Simoni, M, Scognamiglio, A, Baldacci, S, Pistelli, F, Carrozzi, L, et al. Indoor air pollution and airway disease. Int J Tuberc Lung Dis. (2004) 8:1401–15.
7. Chan-Yeung, M, and Malo, JL. Occupational asthma. N Engl J Med. (1995) 333:107–12. doi: 10.1056/NEJM199507133330207
8. Halbert, RJ, Natoli, JL, Gano, A, Badamgarav, E, Buist, AS, and Mannino, DM. Global burden of COPD: systematic review and meta-analysis. Eur Respir J. (2006) 28:523–32. doi: 10.1183/09031936.06.00124605
9. Boffetta, P, Jourenkova, N, and Gustavsson, P. Cancer risk from occupational and environmental exposure to polycyclic aromatic hydrocarbons. Cancer Causes Control. (1997) 8:444–72. doi: 10.1023/a:1018465507029
10. Middleton, DRS, Wedekind, R, Hall, AL, Suonio, E, DeBono, N, Vermeulen, R, et al. Critical reviews of exposure assessment in carcinogenic hazard identification: the IARC monographs experience. Occup Environ Med. (2024) 81:366–72. doi: 10.1136/oemed-2023-109277
11. Tarlo, SM, Balmes, J, Balkissoon, R, Beach, J, Beckett, W, Bernstein, D, et al. Diagnosis and management of work-related asthma: American College of Chest Physicians consensus statement. Chest. (2008) 134:1S–41S. doi: 10.1378/chest.08-0201
12. Balmes, J, Becklake, M, Blanc, P, Henneberger, P, Kreiss, K, Mapp, C, et al. American thoracic society statement: occupational contribution to the burden of airway disease. Am J Respir Crit Care Med. (2003) 167:787–97. doi: 10.1164/rccm.167.5.787
13. Steenland, K, Burnett, C, Lalich, N, Ward, E, and Hurrell, J. Dying for work: the magnitude of US mortality from selected causes of death associated with occupation. Am J Ind Med. (2003) 43:461–82. doi: 10.1002/ajim.10216
14. Seixas, NS, Robins, TG, Attfield, MD, and Moulton, LH. Exposure-response relationships for coal mine dust and obstructive lung disease following enactment of the Federal Coal Mine Health and safety act of 1969. Am J Ind Med. (1992) 21:715–34. doi: 10.1002/ajim.4700210511
15. GBD 2021 Risk Factors Collaborators. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990-2021: a systematic analysis for the global burden of disease study 2021. Lancet. (2024) 403:2162–203. doi: 10.1016/S0140-6736(24)00933-4
16. Murray, CJ, Vos, T, Lozano, R, Naghavi, M, Flaxman, AD, Michaud, C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380:2197–223. doi: 10.1016/S0140-6736(12)61689-4
17. Lim, SS, Vos, T, Flaxman, AD, Danaei, G, Shibuya, K, Adair-Rohani, H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380:2224–60. doi: 10.1016/S0140-6736(12)61766-8, Erratum in: Lancet. 2013 Apr 13; 381(9874):1276. Erratum in: Lancet. 2013 Feb 23; 381(9867):628. AlMazroa, Mohammad A [added]; Memish, Ziad A [added].
18. Lu, Y, Shang, Z, Zhang, W, Hu, X, Shen, R, Zhang, K, et al. Global, regional, and national burden of spinal cord injury from 1990 to 2021 and projections for 2050: a systematic analysis for the global burden of disease 2021 study. Ageing Res Rev. (2025) 103:102598. doi: 10.1016/j.arr.2024.102598
19. Cohen, RA, Go, LHT, and Rose, CS. Global trends in occupational lung disease. Semin Respir Crit Care Med. (2023) 44:317–26. doi: 10.1055/s-0043-1766117
20. Murray, CJL. GBD 2021 collaborators. Findings from the global burden of disease study 2021. Lancet. (2024) 403:2259–62. doi: 10.1016/S0140-6736(24)00769-4
21. Alif, SM, Dharmage, SC, Bowatte, G, Karahalios, A, Benke, G, Dennekamp, M, et al. Occupational exposure and risk of chronic obstructive pulmonary disease: a systematic review and meta-analysis. Expert Rev Respir Med. (2016) 10:861–72. doi: 10.1080/17476348.2016.1190274
22. Christenson, SA, Smith, BM, Bafadhel, M, and Putcha, N. Chronic obstructive pulmonary disease. Lancet. (2022) 399:2227–42. doi: 10.1016/S0140-6736(22)00470-6
23. Li, J, Yin, P, Wang, H, Wang, L, You, J, Liu, J, et al. The burden of pneumoconiosis in China: an analysis from the global burden of disease study 2019. BMC Public Health. (2022) 22:1114. doi: 10.1186/s12889-022-13541-x
24. Zhou, D, Zhu, D, Li, N, and Han, B. Exploration of three incidence trend prediction models based on the number of diagnosed pneumoconiosis cases in China from 2000 to 2019. J Occup Environ Med. (2021) 63:e440–4. doi: 10.1097/JOM.0000000000002258
25. Ou, Z, Li, X, Cui, J, Zhu, S, Feng, K, Ma, J, et al. Global, regional, and national burden of asbestosis from 1990 to 2019 and the implications for prevention and control. Sci Total Environ. (2023) 904:166346. doi: 10.1016/j.scitotenv.2023.166346
26. Jani, CK, Kareff, SA, Morgenstern-Kaplan, D, et al. Evolving trends in lung cancer risk factors in the ten most populous countries: an analysis of data from the 2019 Global Burden of Disease Study. EClinicalMedicine. (2025). 79:103033. doi: 10.1016/j.eclinm.2024.103033
27. Adeloye, D, Chan, KY, Rudan, I, and Campbell, H. An estimate of asthma prevalence in Africa: a systematic analysis. Croat Med J. (2013) 54:519–31. doi: 10.3325/cmj.2013.54.519
28. Loomis, D, Guha, N, Hall, AL, and Straif, K. Identifying occupational carcinogens: an update from the IARC monographs. Occup Environ Med. (2018) 75:593–603. doi: 10.1136/oemed-2017-104944
29. Olsson, A, Guha, N, Bouaoun, L, Kromhout, H, Peters, S, Siemiatycki, J, et al. Occupational exposure to polycyclic aromatic hydrocarbons and lung cancer risk: results from a pooled analysis of case-control studies (SYNERGY). Cancer Epidemiol Biomarkers Prev. (2022) 31:1433–41. doi: 10.1158/1055-9965.EPI-21-1428
30. Ding, Q, Schenk, L, and Hansson, SO. Occupational diseases in the People's Republic of China between 2000 and 2010. Am J Ind Med. (2013) 56:1423–32. doi: 10.1002/ajim.22245
31. Lu, C, Dasgupta, P, Cameron, J, Fritschi, L, and Baade, P. A systematic review and meta-analysis on international studies of prevalence, mortality and survival due to coal mine dust lung disease. PLoS One. (2021) 16:e0255617. doi: 10.1371/journal.pone.0255617
32. Boschetto, P, Quintavalle, S, Miotto, D, Lo Cascio, N, Zeni, E, and Mapp, CE. Chronic obstructive pulmonary disease (COPD) and occupational exposures. J Occup Med Toxicol. (2006) 1:11. doi: 10.1186/1745-6673-1-11
33. Balmes, JR. Occupational contribution to the burden of chronic obstructive pulmonary disease. J Occup Environ Med. (2005) 47:154–60. doi: 10.1097/01.jom.0000152923.07801.e1
34. Tarlo, SM, and Lemiere, C. Occupational asthma. N Engl J Med. (2014) 370:640–9. doi: 10.1056/NEJMra1301758
35. Wang, JQ, Liang, YY, Zhao, ZX, et al. The study for asthma in older adults: a combined analysis of the effects of occupational asthmagens, high body-mass index and smoking. Front Public Health. (2025) 13:1625623. doi: 10.3389/fpubh.2025.1625623
36. Lin, RT, Chien, LC, Jimba, M, Furuya, S, and Takahashi, K. Implementation of national policies for a total asbestos ban: a global comparison. Lancet Planet Health. (2019) 3:e341–8. doi: 10.1016/S2542-5196(19)30109-3
37. Sung, H, Ferlay, J, Siegel, RL, Laversanne, M, Soerjomataram, I, Jemal, A, et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
38. Shi, P, Xing, X, Xi, S, Jing, H, Yuan, J, Fu, Z, et al. Trends in global, regional and national incidence of pneumoconiosis caused by different aetiologies: an analysis from the global burden of disease study 2017. Occup Environ Med. (2020) 77:407–14. doi: 10.1136/oemed-2019-106321
39. Rushton, L. The global burden of occupational disease. Curr Environ Health Rep. (2017) 4:340–8. doi: 10.1007/s40572-017-0151-2
40. Schlünssen, V, Mandrioli, D, Pega, F, Momen, NC, Ádám, B, Chen, W, et al. The prevalences and levels of occupational exposure to dusts and/or fibres (silica, asbestos and coal): a systematic review and meta-analysis from the WHO/ILO joint estimates of the work-related burden of disease and injury. Environ Int. (2023) 178:107980. doi: 10.1016/j.envint.2023.107980
41. Klionsky, DJ, Abdel-Aziz, AK, Abdelfatah, S, Abdellatif, M, Abdoli, A, Abel, S, et al. Guidelines for the use and interpretation of assays for monitoring autophagy (4th edition)1. Autophagy. (2021) 17:1–382. doi: 10.1080/15548627.2020.1797280
42. Takala, J, Hämäläinen, P, Saarela, KL, Yun, LY, Manickam, K, Jin, TW, et al. Global estimates of the burden of injury and illness at work in 2012. J Occup Environ Hyg. (2014) 11:326–37. doi: 10.1080/15459624.2013.863131
43. Kauppinen, TP. Assessment of exposure in occupational epidemiology. Scand J Work Environ Health. (1994) 20:19–29.
44. Brigham, E, Allbright, K, and Harris, D. Health disparities in environmental and occupational lung disease. Clin Chest Med. (2020) 41:623–39. doi: 10.1016/j.ccm.2020.08.009
45. Murray, CJ, and Lopez, AD. Measuring the global burden of disease. N Engl J Med. (2013) 369:448–57. doi: 10.1056/NEJMra1201534
Keywords: pneumoconiosis, chronic obstructive pulmonary disease, tracheal-bronchus-and-lung cancer, asthma, occupational risks
Citation: Lin S, Ding X, Dang X and Zhan Q (2025) Global, regional, and national disease burden of pneumoconiosis, chronic obstructive pulmonary disease, tracheal-bronchus-and-lung cancer, and asthma attributable to occupational risks, 1990–2021: a systematic analysis for the global burden of disease study 2021. Front. Public Health. 13:1652216. doi: 10.3389/fpubh.2025.1652216
Edited by:
Alberto Modenese, University of Modena and Reggio Emilia, ItalyReviewed by:
Peter E. J. Baldwin, Health and Safety Executive, United KingdomChao Wang, Jilin University, China
Antonio Ramón Gómez-García, Espiritu Santo University, Ecuador
Copyright © 2025 Lin, Ding, Dang and Zhan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qingyuan Zhan, ZHJ6aGFucXlAMTYzLmNvbQ==; Shan Lin, ZHIuc2hhbmxpbkBmb3htYWlsLmNvbQ==
†These authors have contributed equally to this work
 Shan Lin
Shan Lin Xuefeng Ding2†
Xuefeng Ding2† Qingyuan Zhan
Qingyuan Zhan