- 1State Key Laboratory for Diagnosis and Treatment of Severe Zoonotic Infectious Diseases, Key Laboratory for Zoonoses Research of the Ministry of Education, Department of Epidemiology and Biostatistics, School of Public Health, Jilin University, Changchun, Jilin, China
- 2The People's Hospital of Lincang, Lincang, Yunnan, China
- 3Yunnan Center for Disease Control and Prevention, Kunming, Yunnan, China
- 4School of Disaster and Emergency Medicine, Tianjin University, Tianjin, China
Objectives: To establish the first large-scale epidemiological profile of scoliosis among children and adolescents in Yunnan, China, and identify key demographic, anthropometric, and geographic determinants in this multi-ethnic, high-altitude region.
Study design: A population-based cross-sectional screening survey using multistage stratified cluster sampling.
Methods: A population-based cross-sectional survey of 69,811 students aged 6–18 was conducted in 2021 using multistage stratified cluster sampling across Yunnan, which included demographic information (gender, ethnicity, grade), anthropometric measurements (height, weight), and scoliosis outcomes (presence and severity assessed via scoliometer-based Angle of Trunk Rotation). Regional covariates (altitude, economic status) were also incorporated. Multi-factor regression analysis identified risk factors.
Results: Initial screening identified 1,379 scoliosis cases, yielding an overall detection rate of 1.98%. The rate was significantly higher in females than in males (2.4% vs. 1.6%, p < 0.001), with males showing higher rates at ages 14 and 16, and females exhibiting consistently higher detection during early and mid-adolescence and a peak at age 17 (3.7%). The detection rate also increased progressively with education level (primary school: 1.0%; middle school: 2.7%; high school: 3.3%). Multivariable regression analysis indicated that scoliosis risk was positively associated with female sex (AOR = 1.738, 95% CI: 1.546–1.954), higher education levels (middle school: AOR = 1.703, 95% CI: 1.408–2.059; high school: AOR = 1.891, 95% CI: 1.534–2.331), and greater height (per cm AOR = 1.060, 95% CI: 1.052–1.069). Protective factors included rural residence (AOR = 0.717, 95% CI: 0.638–0.805), minority ethnicity (AOR = 0.856, 95% CI: 0.760–0.964), moderate (AOR = 0.515, 95% CI: 0.452–0.586) or low GDP (AOR = 0.067, 95% CI: 0.044–0.104), medium (AOR = 0.075, 95% CI: 0.049–0.116) or high altitude (AOR = 0.098, 95% CI: 0.068–0.140), and greater weight (AOR = 0.955, 95% CI: 0.947–0.962).
Conclusion: The elevated detection rate in Yunnan highlights the influence of regional sociodemographic and environmental factors. Findings support tailored screening strategies, particularly for urban female adolescents and minority populations in high-altitude areas.
Introduction
Spinal curvature abnormalities mainly include scoliosis and kyphosis, with scoliosis being the most common form (1). Scoliosis is a three-dimensional deformity characterized by lateral curvature and vertebral rotation in one or more spinal segments (2). According to the criteria of the Scoliosis Research Society (SRS), scoliosis is diagnosed when the Cobb angle measured from a standing anteroposterior X-ray exceeds 10° (3).
Idiopathic scoliosis (IS) accounts for 80% of all cases, with adolescent idiopathic scoliosis (AIS) comprising the vast majority (80%) of these cases. The term “idiopathic” indicates that its etiology remains unclear (4). AIS shows significant regional variations in prevalence, with rates reported as follows: 1–3% in the United States (3), 5.2% in Germany (5), and 0.4–2.5% in Asia (6). Scoliosis remains highly prevalent in China, with notable regional differences (7, 8). A 2021 meta-analysis of data from 2 million primary and secondary school students revealed a primary screening positivity rate of 4.40% and a diagnostic rate of 1.23% for scoliosis in mainland China (9). In recent years, the incidence has continued to rise (10). Notably, adolescents, particularly those aged 11 and older, represent a high-risk group for scoliosis (11). Scoliosis has become the third most significant health issue affecting children and adolescents, following myopia and obesity (12). If left untreated, early symptoms may remain hidden, and untreated scoliosis can progressively develop into bodily deformity, leading to potential damage to pulmonary and neurological functions, and even psychological disorders (3, 13). Some patients also experience comorbidities that exacerbate the disease burden. Therefore, early screening and targeted interventions for children and adolescents are critical in delaying disease progression, reducing surgical risks, and easing the economic burden (14).
Scoliosis screening programs originated in the 1960s in the United States (15), while China began its scoliosis screening initiatives in 1995 in Hong Kong (16). Since then, mainland cities such as Beijing and Guangzhou have followed suit in implementing adolescent scoliosis screening programs (17). Both domestic and international scholars generally agree that adolescents are the primary focus for scoliosis screening and intervention (15). Yunnan Province, located in the southwestern frontier of China, is characterized by complex geography, diverse ethnicities, dispersed populations, and unequal medical resources, which have led to a late start and substantial challenges in scoliosis screening efforts (18). Existing research has mainly focused on major cities, with a lack of large-scale epidemiological data from southwestern regions and areas inhabited by ethnic minorities (9). Conducting scoliosis screening research in this region will help assess the spinal health status of children and adolescents in non-central urban areas and provide scientific evidence for regional prevention and control strategies. This study, based on common disease monitoring data from 32 counties in Yunnan Province in 2021, aims to evaluate the initial screening detection rate of scoliosis among primary and secondary school students, analyze the distribution characteristics of scoliosis patients, and explore influencing factors in children and adolescents.
Methods
Study design
This large-scale scoliosis screening study analyzed 2021 surveillance data from Yunnan Province, a mountainous frontier region in southwestern China with an average elevation of 1,980 meters and diverse subtropical to tropical climates. As a key hub within the China-Myanmar-Laos Economic Corridor and the Greater Mekong Subregion, Yunnan’s distinct geographical and socioeconomic profile offers valuable insights for other middle-income mountainous areas.
Data were obtained from the Yunnan Province for 2021 were obtained from the Yunnan Provincial Center for Disease Control and Prevention, covering 16 prefecture-level cities. Using a stratified sampling approach based on the 2021 National Technical Manual for Surveillance and Intervention on Common Diseases and Health Determinants in Students, we selected at least one urban and one suburban/rural site per city. Urban regions contributed seven randomly selected schools (two primary, two junior high, and three senior high schools), while suburban/rural regions contributed five (two primary, two junior high, and one senior high school). Within each school, cluster sampling was performed with grade as the stratification variable and class as the sampling unit, ensuring at least 80 participants per grade. The final analytic sample comprised 69,811 students across 32 counties or districts. The study protocol was approved by the Medical Ethics Committee of the Yunnan Provincial Center for Disease Control and Prevention (Approval No. 2025-8).
Data collection and physical examination
Data were collected in accordance with the above manual using the Student Key Common Diseases Detection Form (Primary and Secondary School Edition), which included general demographic characteristics (screening site, grade, gender, ethnicity, date of birth, date of physical examination, height, weight, etc.), as well as outcome indicators for scoliosis detection (presence, type, and severity).
Altitude data were obtained from a high-precision digital elevation model (DEM) provided by the Institute of Geographic Sciences and Natural Resources Research, Chinese Academy of Sciences. The median altitude for each monitoring site was extracted using ArcGIS software (version 18.0). Gross domestic product (GDP) data were retrieved from the Yunnan Statistical Yearbook 2021, with county-level per capita GDP serving as the economic indicator. Countries were divided into high, medium, and low groups (tertiles) based on ranked values.
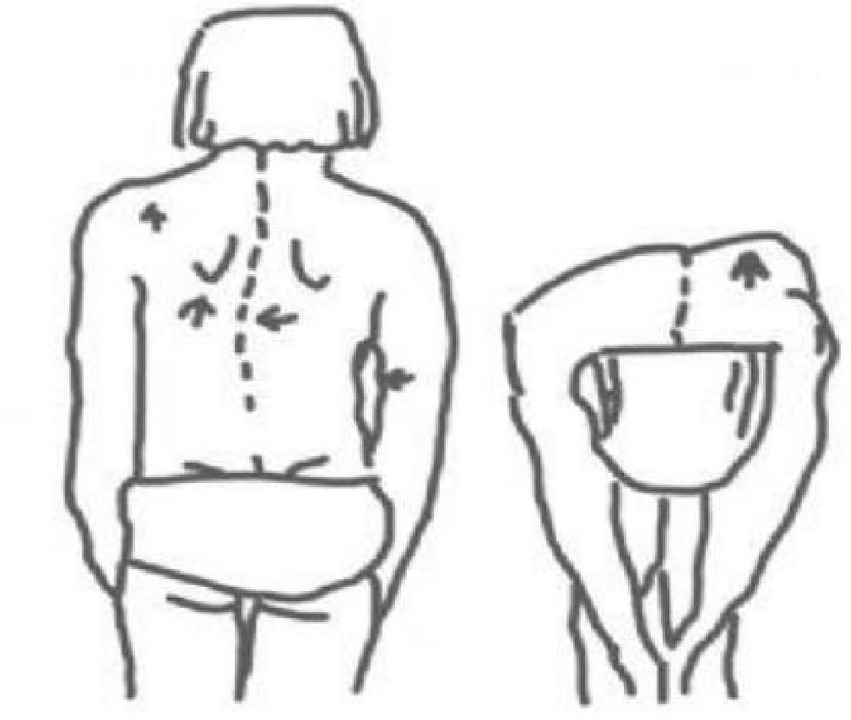
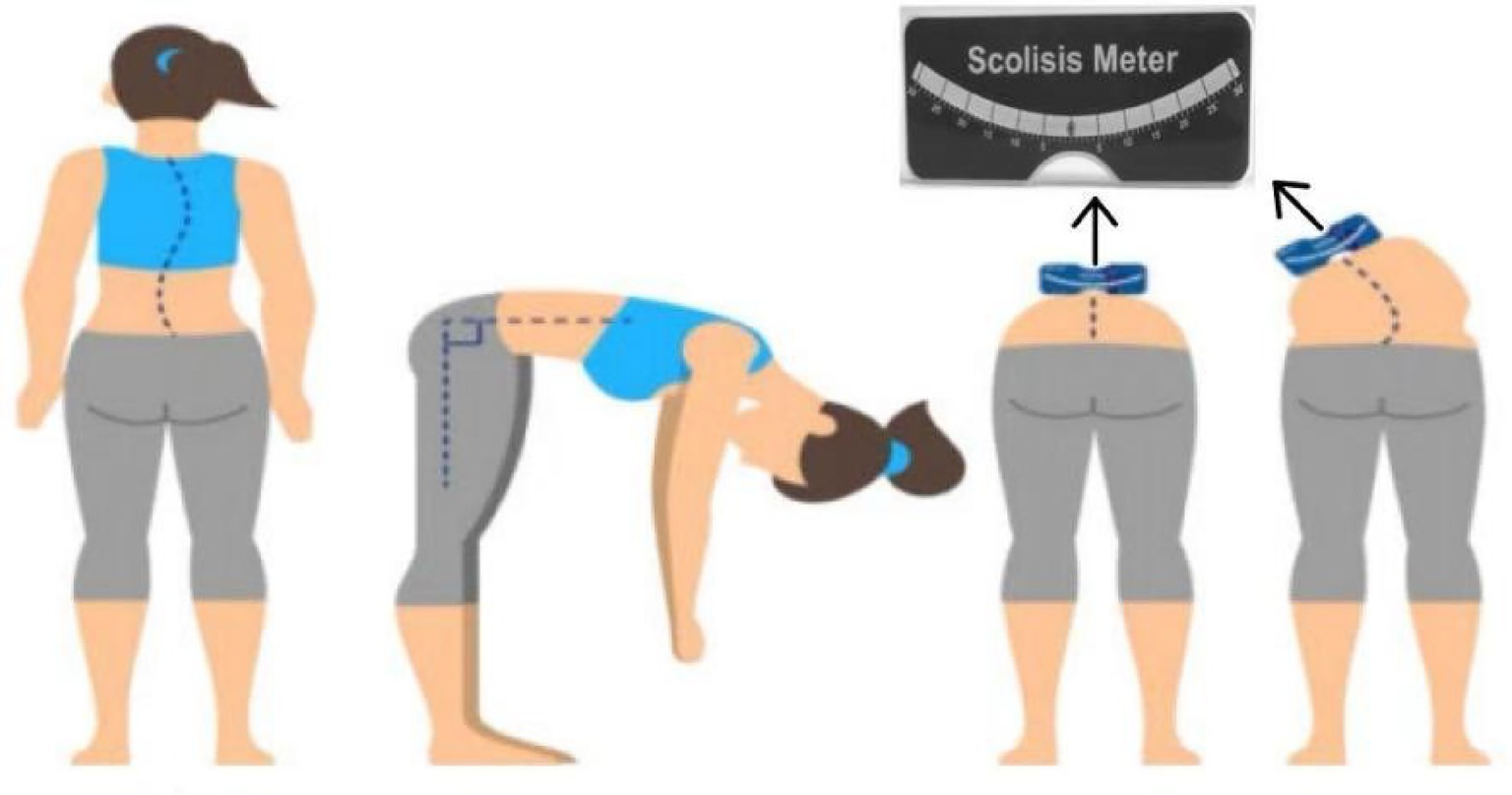
The scoliosis screening was conducted by professionally trained technicians who passed a rigorous examination. Prior to the screening, the teachers, students, and their parents were informed about the screening content, and informed consent was obtained. The screening method followed the Technical Guidelines for the Prevention and Control of Spinal Curvature Abnormalities in Children and Adolescents (GB/T 16133-2014, China’s recommended national standard for medical practice) (19), and the procedures were as follows: ① General inspection: The subject was asked to remove their shoes and stand naturally. For males, the upper body was left exposed; for females, only undergarments were worn. The examiner observed from behind whether both shoulders were level, scapulae were symmetrical, the lumbar curve was even, iliac crests were at the same level, and there was no deviation in the line of the spinous processes (Figure 1). ② The examinee stood with their back to the examiner, knees straight and ankles together. With arms extended and palms together, the trunk was slowly bent forward to approximately 90°. The hands were placed between the knees to avoid compensatory shifts. The examiner viewed the back horizontally from thoracic to lumbar regions, checking for symmetry along both sides of the spine. The test was considered positive if a unilateral rib hump, paraspinal asymmetry, or muscular prominence was observed, indicating a high suspicion of scoliosis. ③ Angle of trunk rotation (ATR) measurement: While maintaining the forward-bending position, a scoliometer was used to measure the ATR sequentially in the thoracic, thoracolumbar, and lumbar regions. The maximum ATR value and its location were recorded. An ATR ≥ 5°at the most prominent asymmetric site suggested a high likelihood of scoliosis. This threshold effectively identifies most cases of scoliosis with a Cobb angle ≥ 10°during screening. ④ Spinal movement test: Individuals with suspected abnormalities in the general inspection but a negative forward bending test performed spinal flexion, extension, left and right lateral bending, and left and right axial rotation twice each. The examiner then rechecked the spine for any residual curvature (Figure 2).
Scoliosis screening outcomes were classified as follows: No Scoliosis (No abnormalities on general inspection and forward bending test, and a static ATR < 5°); Postural Inbalance (Abnormal general inspection, positive forward bending test, or static ATR ≥ 5°, but with ATR < 5° after the movement test); Positive Screening (Any one of the following: abnormal general inspection, positive forward bending test, or static ATR ≥ 5°, with ATR remaining ≥5° after the movement test). For analytical purposes, the “No Scoliosis” and “Postural Inbalance” groups were collectively classified as screening-negative, while the “Positive Screening” group was classified as screening-positive. Students with positive screening results were strongly referred to medical institutions for radiographic examination (Cobb angle measurement) to confirm diagnosis (Figure 3).
Results
Basic characteristics
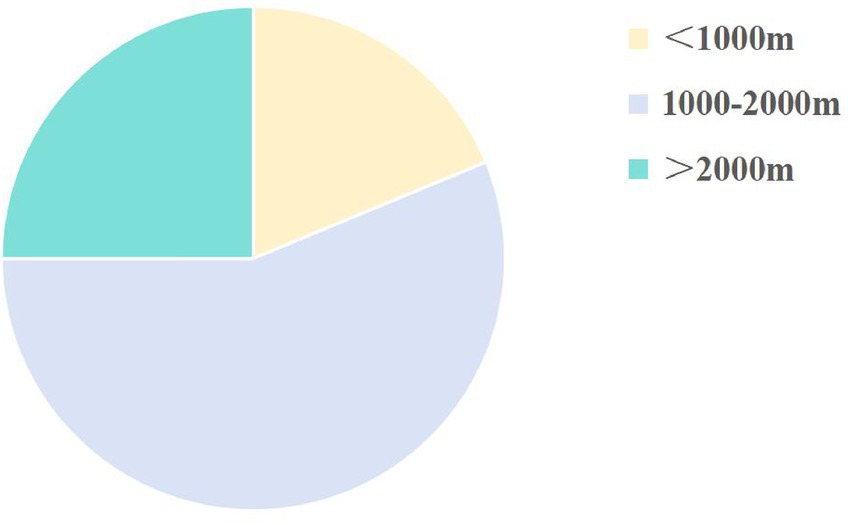
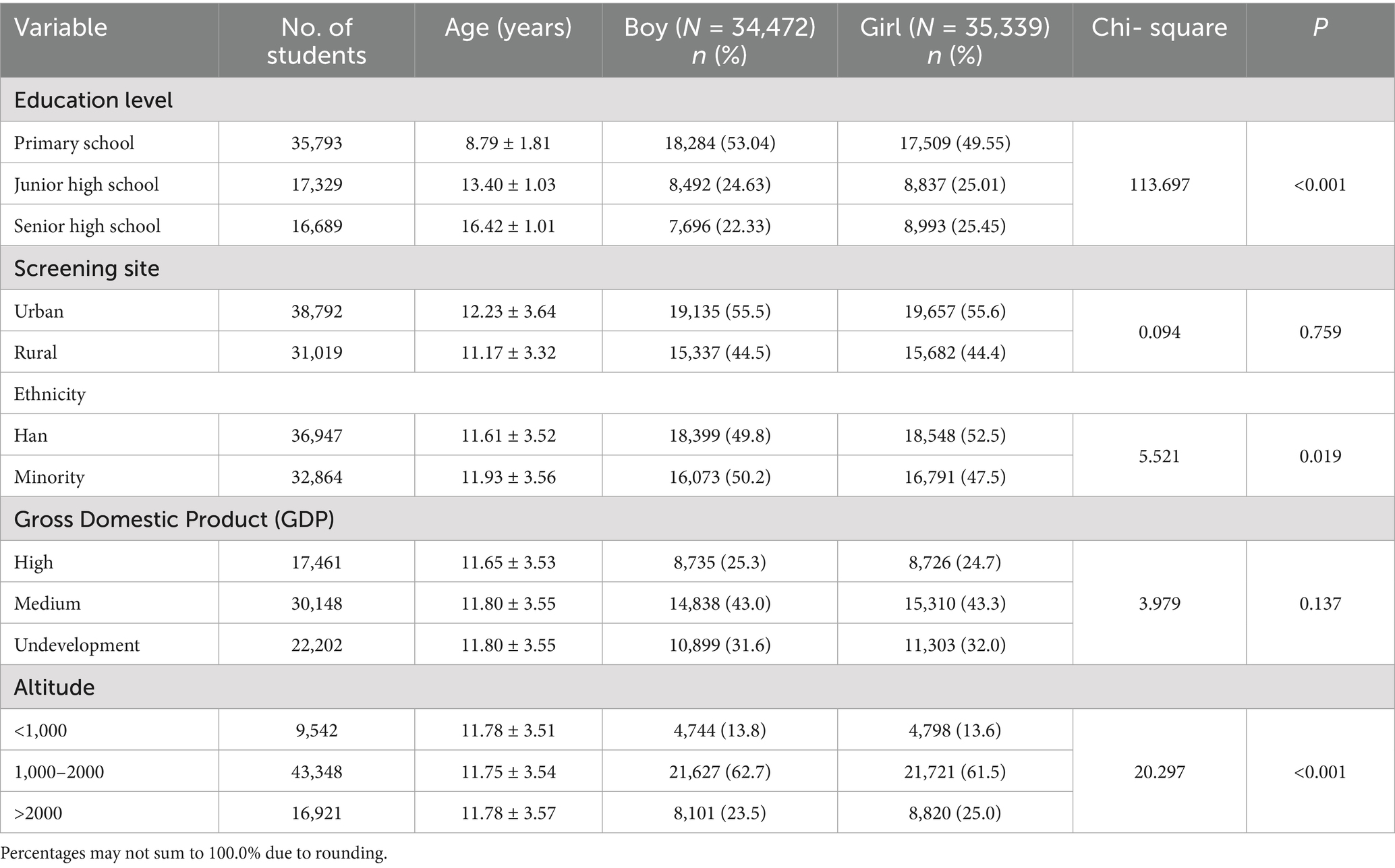
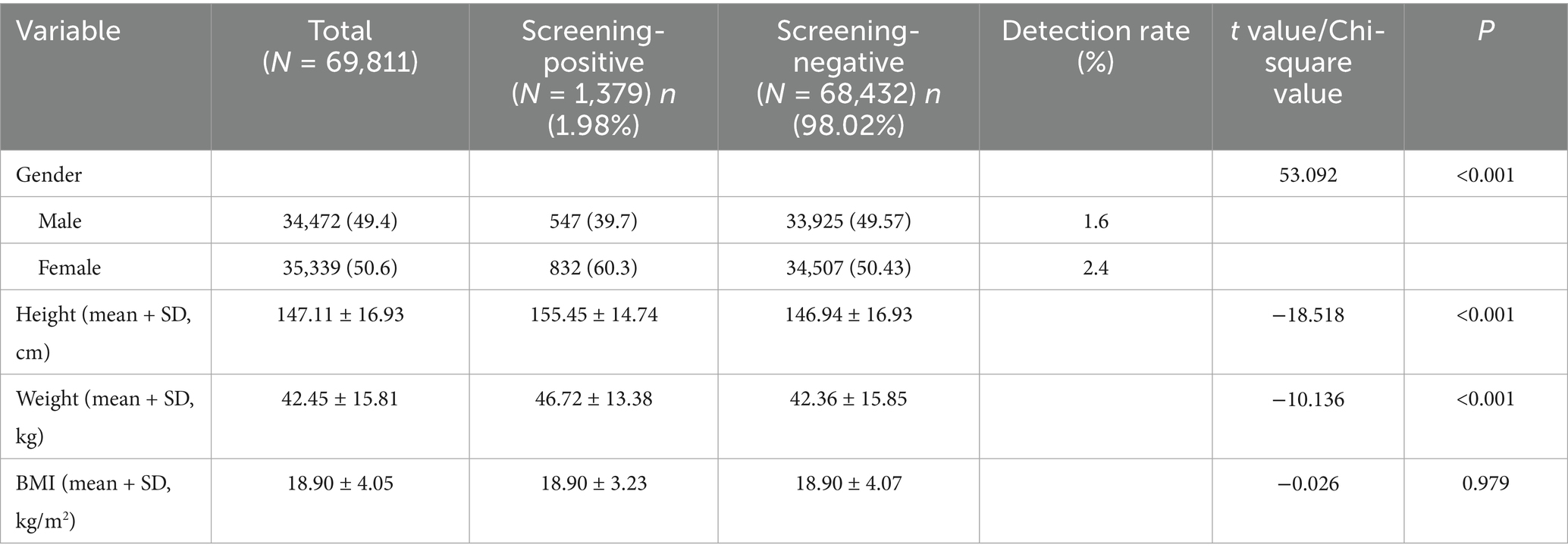
A total of 69,811 students aged 6–18 years were screened in this study, including 34,472 males (49.38%) and 35,339 females (50.62%). Regarding regional distribution, more than half of the students were from urban areas (55.57%, 38,792 students), while 44.43% (31,019 students) were from rural areas. Primary school students comprised the majority of the study population (51.27%, 35,793 students), followed by middle school students (24.82%, 17,329 students) and high school students (23.91%, 16,689 students). Ethnic distribution was diverse, with Han students representing 52.92% (36,947 students) and minority ethnic students accounting for 47.08% (32,864 students). Additionally, the study population was widely distributed across various geographic altitudes and levels of economic development. Most students lived in regions with altitudes ranging from 1,000 to 2000 meters (62.09%, 43,348 students, Figure 4), and were primarily concentrated in areas with moderate economic development (43.19%, 30,148 students). Detailed data can be found in Table 1.
Detection rate
A total of 1,379 positive cases were identified in this scoliosis screening, resulting in an overall detection rate of 1.98%. A significant sex disparity was observed, with a markedly higher detection rate among female students compared to their male counterparts (2.4% vs. 1.6%; p < 0.001; Table 2).
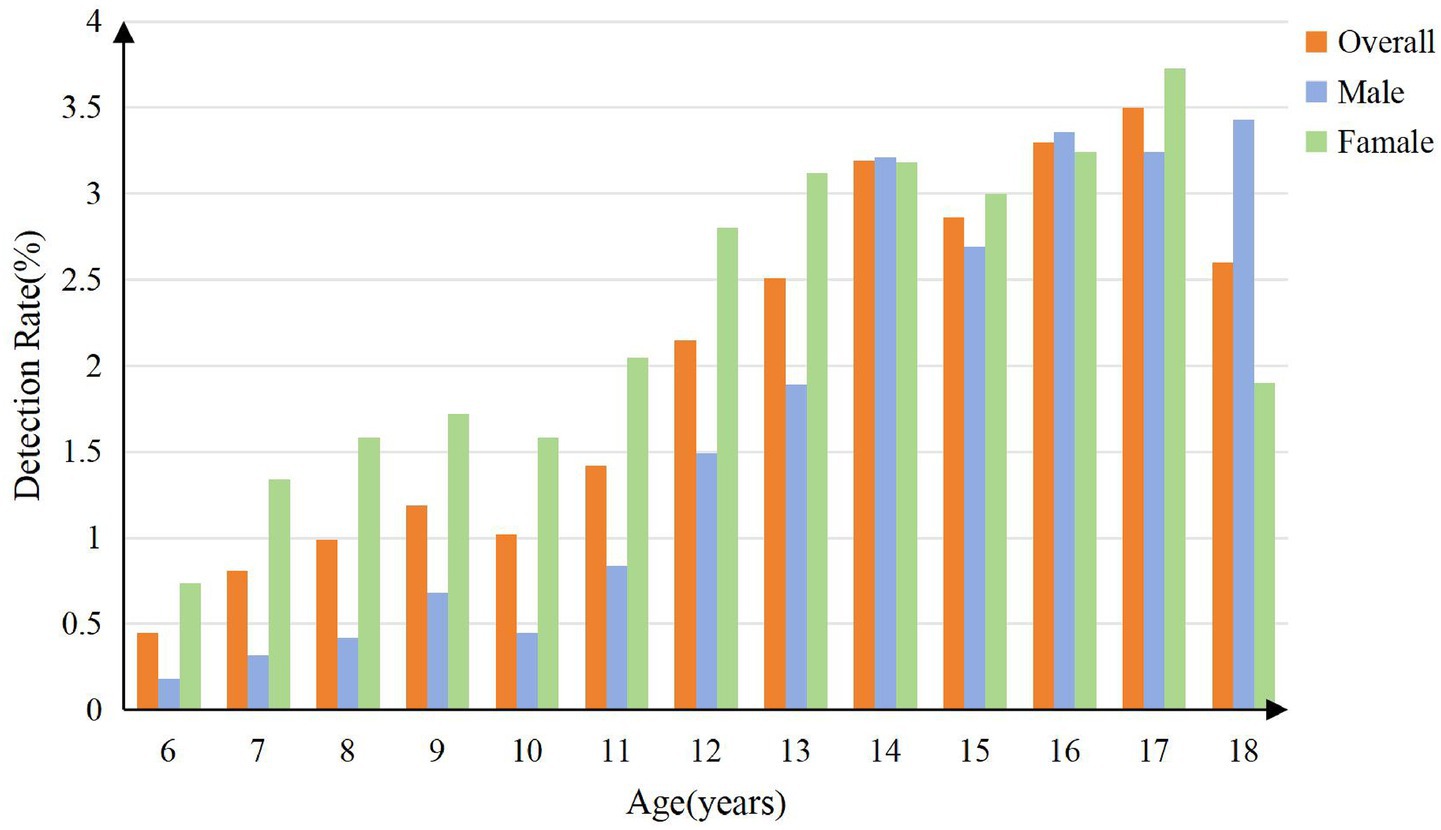
The disparity exhibited a dynamic pattern across age groups. As shown in Figure 5, the detection rate was consistently higher in females, particularly during early and mid-adolescence (ages 6–14, 16, and 17), while males showed a higher detection rate at ages 14, 16, and 18 years. The detection rate peaked at 17 years for females (3.7%), which was significantly higher than the peak for males (3.4%) at 18 years. A secondary peak was also observed for males at 16 years (3.4%).
Regarding anthropometric measures, screening-positive cases were significantly taller and heavier than negative cases (p < 0.001 for both; Table 2). However, no significant intergroup difference was found in Body Mass Index (BMI).
Detection rates stratified by screening site, ethnicity, education level, GDP, and altitude
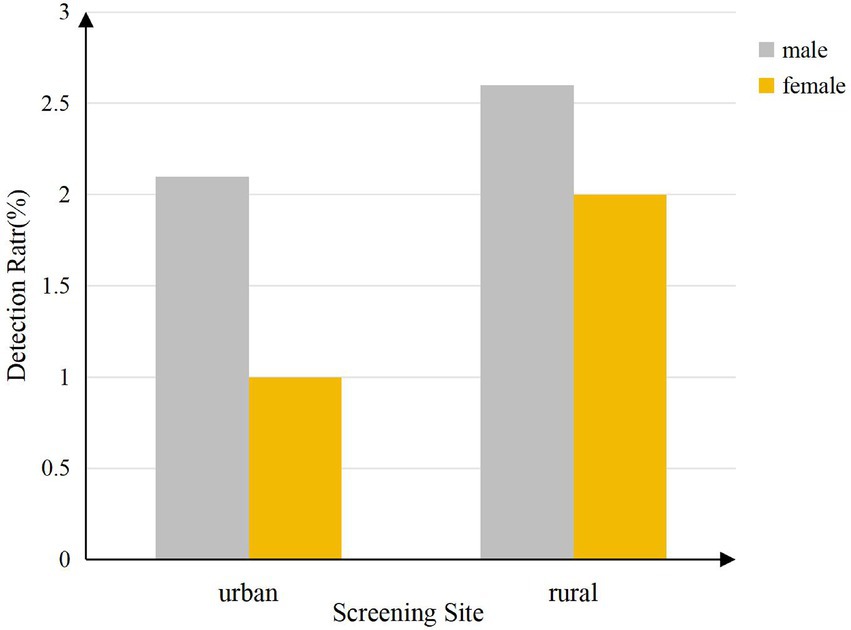
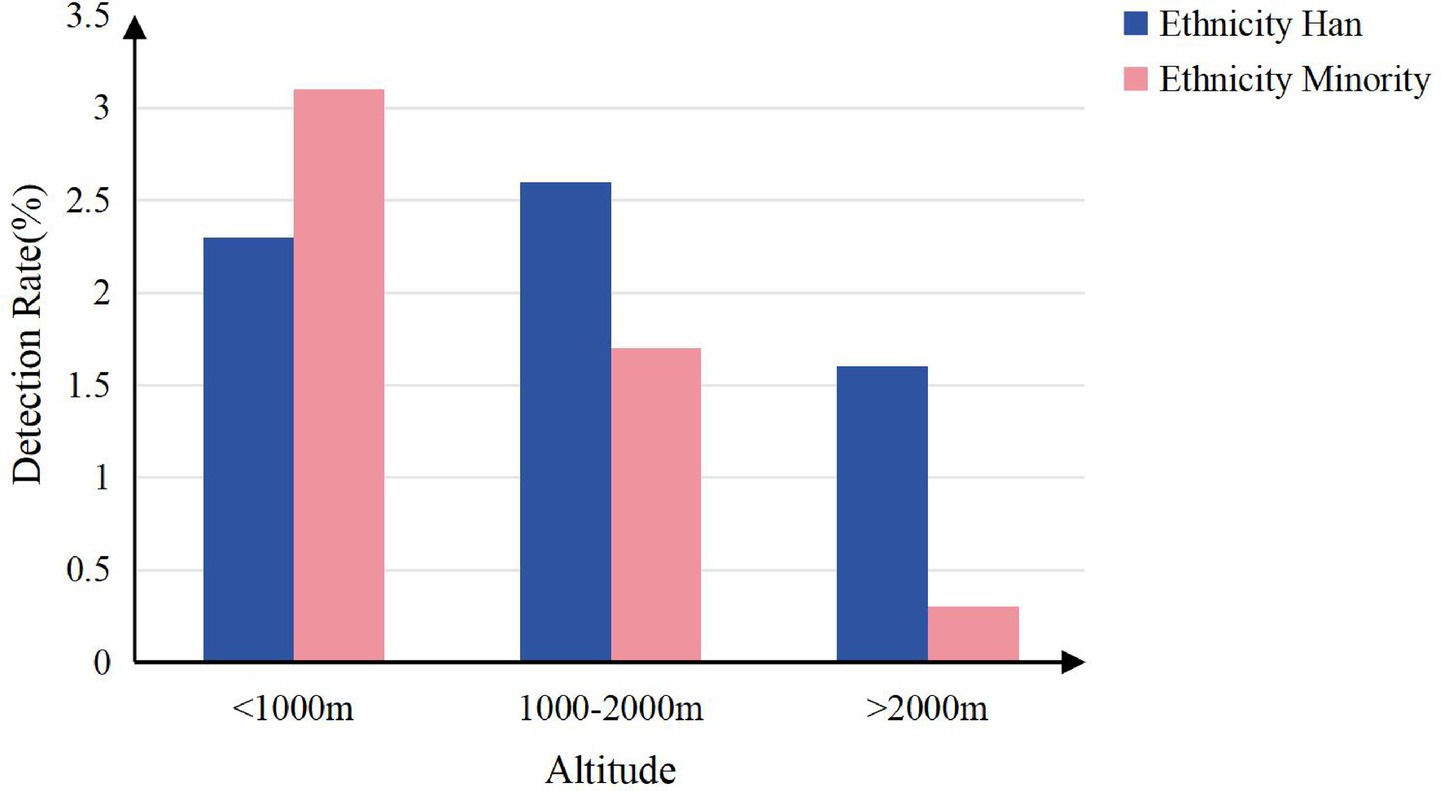
Scoliosis detection rates varied significantly across key demographic and geographic variables (all p < 0.001; Table 3). Higher detection rates were observed in urban areas (2.4%), the Han ethnic group (2.4%), senior high school students (3.3%), high-GDP regions (3.2%), and areas with altitude below 2000 meters (2.3–2.7%). The lowest rate was observed in regions above 2000 meters (0.7%).

Table 3. Scoliosis detection rates among students stratified by ethnicity, education level, and GDP.
Detection rates stratified by screening sites, altitude, and counties
Scoliosis detection rates differed significantly by screening site, altitude group (p < 0.001; Figures 6, 7), with higher rates observed in urban areas (2.4% vs. 1.5% rural) and lower altitudes (2.7% at <1,000 m vs. 0.7% at >2000 m), and varied widely across counties (range: 0.1–7.4%; Table 4).
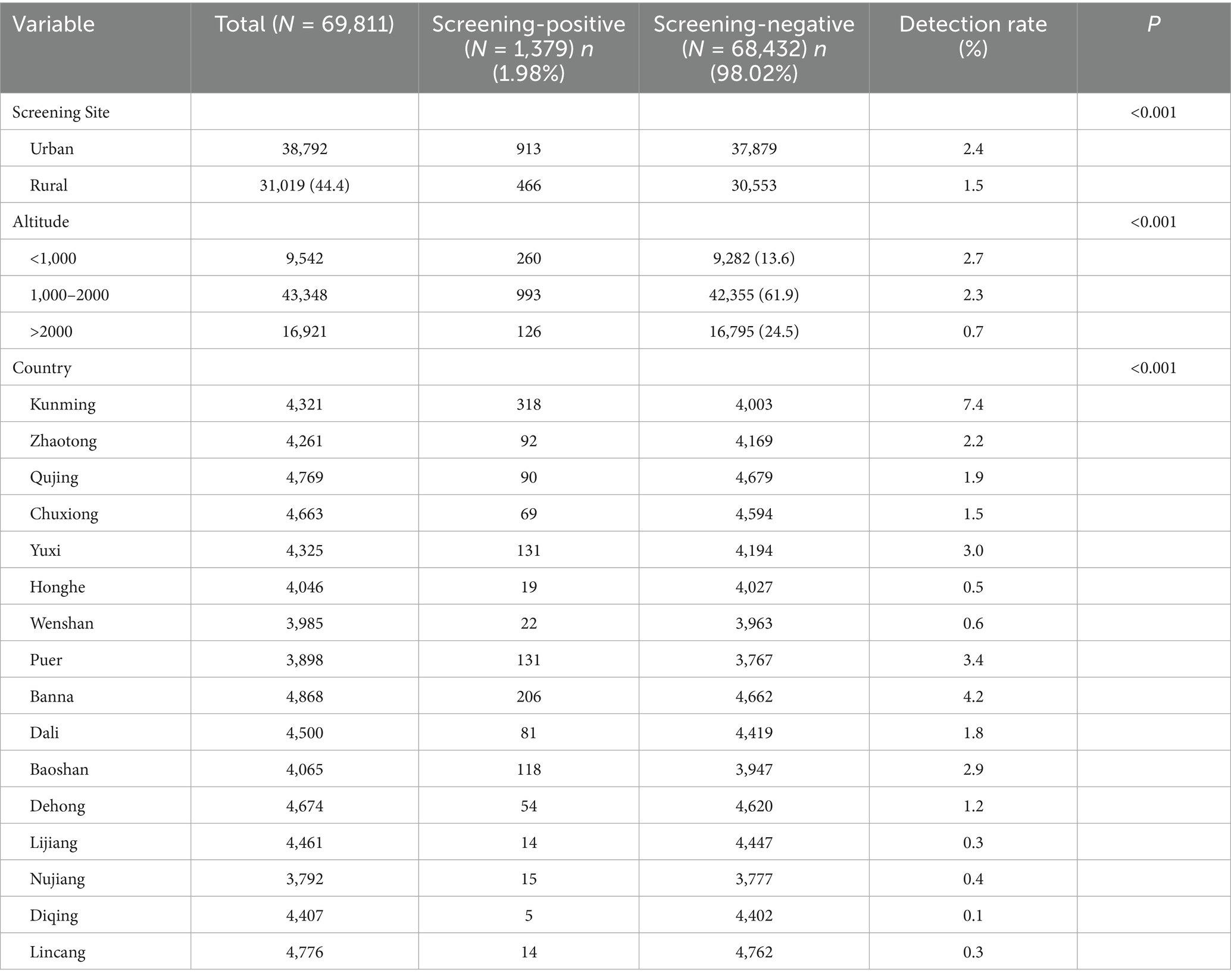
Table 4. Scoliosis detection rates among students stratified by screening site, altitude and country.
Correlation analysis and variance inflation factor assessment
A two-step approach was used to assess and address potential multicollinearity among the independent variables before constructing the multi-factor regression model. The variables of interest included Gender, Height, Weight, BMI, Ethnicity, Education Level, Screening Site, GDP and Altitude.
First, Spearman correlation analysis was conducted (Figure 8). A strong correlation was identified between BMI and both height (ρ = 0.89) and weight (ρ = 0.88). Due to its strong collinearity with these anthropometric measures and to avoid model instability, BMI was excluded from subsequent analyses based on a pre-defined correlation coefficient threshold of |ρ| > 0.8. Next, variance inflation factors (VIFs) were calculated for the remaining variables to further assess multicollinearity. After excluding BMI, all variables had VIF values well below the conservative threshold of 5, indicating that severe multicollinearity was not a concern for the final multivariate model.
Multi-factor regression analysis and factors associated with scoliosis
Multi-factor regression analyses identified multiple factors associated with scoliosis (Table 5). Female participants had significantly higher odds of scoliosis than males (OR = 1.50, 95% CI: 1.34–1.67). Height (OR = 1.03 per cm, 95% CI: 1.03–1.04) and weight (OR = 1.02 per kg, 95%CI: 1.01–1.02) were both positively associated with scoliosis. Participants from minority ethnic groups had lower odds compared to the Han majority (OR = 0.61, 95% CI: 0.54–0.68). Educational level exhibited a strong gradient: using primary school as the reference, the odds were significantly higher for middle school (OR = 2.76, 95% CI: 2.40–3.17) and high school students (OR = 3.40, 95% CI: 2.97–3.89) compared to those with primary school education. Screenings conducted in rural areas (OR = 0.63, 95%CI: 0.57–0.71), and in regions with medium (OR = 0.54, 95%CI: 0.48–0.61) or low GDP (OR = 0.41, 95% CI: 0.35–0.47), were associated with reduced odds. Living at higher altitudes (1000–2000 m: OR = 0.84, 95% CI: 0.73–0.96; >2000 m: OR = 0.27, 95% CI: 0.22–0.33) appeared to offer a protective effect.
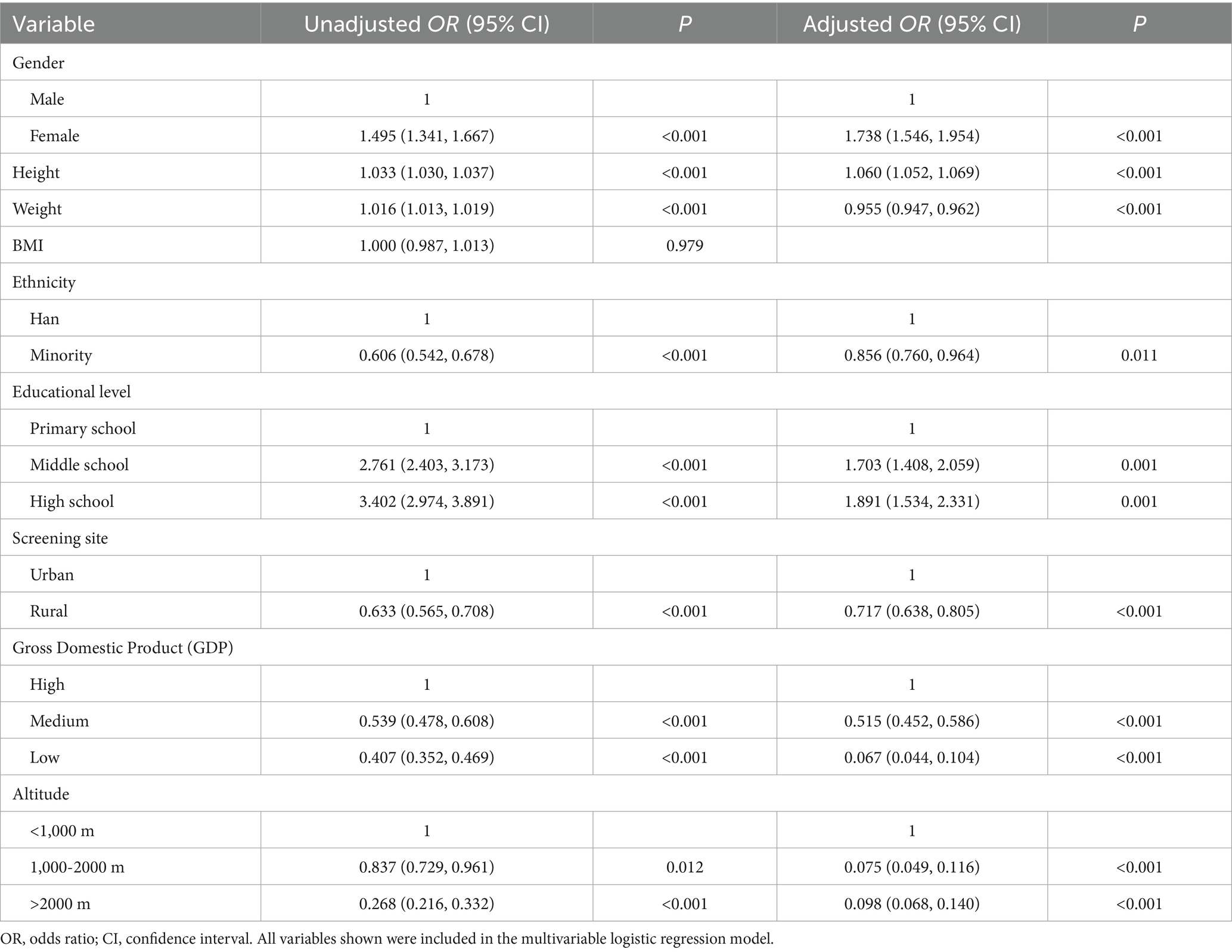
Table 5. Multi-factor regression analysis of factors associated with scoliosis in the unadjusted model and the adjusted model (N = 69,811).
To address multicollinearity (VIF > 10), BMI was excluded from the final adjusted model. The model revealed several notable findings: the risk for female gender increased (AOR = 1.74, 95% CI: 1.55–1.95), while the effect of height became more pronounced (AOR = 1.06 per cm, 95% CI: 1.05–1.07). Conversely, weight exhibited a significant protective effect (AOR = 0.96 per kg, 95% CI: 0.95–0.96). The protective association for minority ethnicity remained significant (AOR = 0.86, 95% CI: 0.76–0.96). Particularly robust were the protective effects of low GDP (AOR = 0.07, 95% CI: 0.04–0.10) and high altitudes.
Discussion
Prevalence of scoliosis in Yunnan Province
The global prevalence of adolescent idiopathic scoliosis (AIS) is approximately 1.34% (20), with significant regional variations. In the United States, the prevalence of AIS among individuals aged 10–16 years ranges from 1 to 3% (3), while in Germany, it is as high as 5.2% (5). In Asia, the prevalence varies between 0.4 and 2.5% (6), and in mainland China, the overall prevalence among primary and secondary school students was reported to be 1.23% in 2021 (9). In this study, the detection rate in Yunnan Province was 1.98%, which is higher than the global average (1.34%) and the national average in China (1.23%), but lower than the rates reported in central and coastal metropolitan areas such as Taiyuan (3.1%) and Guangzhou (8.2%) (21). These differences may be attributed to variations in screening criteria, ethnic disparities, economic development levels, and lifestyle factors.
Gender, age, and scoliosis
The results of this study revealed that the detection rate of scoliosis was significantly higher in females aged 6–14, 16, and 17 years compared to males, with the highest rate observed at 17 years before it declining at 18 years. In contrast, males exhibited slightly higher detection rates than females at 14 and 16, with a significant peak at 18 years. From age 11 onward, the detection rate in females consistently surpassed that in males, but it tended to stabilize or gradually decline with age, consistent with findings from previous studies (9, 22, 23). Adolescents, particularly those aged 11–18 years, represent a high-risk group for scoliosis (24). Scoliosis typically develops during the pre-pubertal stage and progresses rapidly throughout adolescence, resulting in markedly higher detection rates in adolescents compared to children under 11 years of age (25). The incidence of adolescent idiopathic scoliosis (AIS) is higher in females than in males (26), with an earlier peak onset age (13 years) in females, potentially due to factors such as pubertal development, estrogen fluctuations, and changes in bilateral spinal muscle tension (9). A study on Turkish AIS patients further revealed abnormal growth patterns with significant sexual dimorphism during puberty: female patients exhibited higher BMI pre- and during the growth spurt, whereas males showed lower BMI at pubertal stage 5. This suggests that distinct pathophysiological processes may underlie AIS in males and females, which could partially explain the gender-specific and age-stage-specific (e.g., mid-to-late puberty) risk elevations observed in the present study (27). Estrogen plays a critical role in the development and progression of AIS by abnormally modulating bone metabolism, affecting spinal biomechanical stability, and influencing the paraspinal muscle system through receptor-mediated mechanisms (28). Additionally, abnormal leptin bioavailability may contribute to reduced BMI and increased AIS risk in adolescent females (29).
Body development and scoliosis
Epidemiological surveys show that the prevalence of spinal curvature abnormalities increases significantly with educational level. High school students have approximately 1.9 times the risk of suspected scoliosis compared to primary school students (OR = 1.891, 95% CI: 1.534–2.331). The incidence of suspected scoliosis peaks at age 17 (overall: 3.50%; females: 3.73%), which is about 2 years later than the previously reported peak at age 15 (30). This difference may be attributed to variations in study design, such as using skeletal maturity instead of chronological age for staging, as well as modifiable risk factors, including academic pressure, sedentary behavior, and insufficient physical activity, all of which may affect the age distribution of scoliosis (31, 32). These three factors, particularly in high school, often occur together: increased academic burden leads to prolonged periods of fixed postures (such as sitting and studying), while physical activity significantly decreases. The stability and physiological curvature of the spine depend on the support from surrounding muscles and ligaments (33). A lack of exercise and poor lifestyle habits, such as insufficient care for the back, can result in reduced bone density, poor skeletal development, and weakened muscles and ligaments, making it difficult to maintain normal spinal curvature (34). This is supported by clinical research that further confirms adolescents with moderate scoliosis (Cobb angle >20°) exhibit significantly lower bone mineral density and vitamin D deficiency compared to their peers with mild or no scoliosis (35). Moreover, Chow et al.’s (36) comparative study on the effects of different backpack loads (0, 7.5, 10, 12.5, and 15% BW) on scoliosis indicated that improper backpack carriage methods (37, 38) and excessive load increase asymmetric spinal loading, impair postural balance, and thereby elevate the risk of muscle fatigue and scoliosis progression. A longitudinal study in the UK involving 4,640 participants suggested that, after adjusting for confounding factors such as gender and age, children who engaged in moderate-to-high-intensity physical activity had a 30% lower risk of developing scoliosis (31, 39). Therefore, early posture education and promoting regular physical activity during the primary school years, when behavioral habits are more malleable, are crucial.
This study found that primary and secondary school students with lower body weight and taller height had a higher detection rate of scoliosis, consistent with the findings of Qui et al. (40). Spinal abnormalities in students with lower body weight are more easily identified, whereas in obese individuals, the accumulation of back fat may interfere with the accuracy of the Adams Forward Bend Test (FBT) and the Angle of Trunk Rotation (ATR) measurements. Fluctuations in body weight may also affect spinal stability, potentially influencing ATR readings. Nutritional levels indirectly impact ATR values by affecting height, weight, and BMI (41). Regions with higher economic development typically offer better nutritional resources and healthcare, which may accelerate height growth in adolescents. However, students in these areas are more likely to adopt sedentary lifestyles (42), characterized by reduced physical activity and increased screen time (43). The observed urban–rural disparity in detection rates (AOR = 0.717) may reflect multiple factors, including differences in healthcare access and lifestyle between regions. However, the specific mechanisms and impacts of these associations require further research for validation.
Ethnic and scoliosis
This study revealed ethnic disparities in scoliosis detection rates, with a higher detection rate among the Han population relative to non-Han groups, aligning with earlier findings by Sun et al. (21). Several genetic loci, including SLC39A8 and ABO, have been established as significantly associated with adolescent idiopathic scoliosis risk in the Han Chinese population (44, 45). However, ethnic disparities in scoliosis prevalence likely arise from a combination of influences. Variations in genetic susceptibility, socioeconomic status, cultural background, lifestyle, and living environment across ethnic groups may collectively contribute to scoliosis risk (46, 47). Differences in nutritional intake and physical activity may further modulate spinal development. These hypotheses require further validation through large-scale multicenter studies and long-term follow-up to clarify the mechanistic role of ethnicity in the pathogenesis and progression of scoliosis.
Altitude and scoliosis
Previous studies have suggested that high-altitude environments may be a risk factor for scoliosis, potentially mediated by mechanisms such as chronic hypoxia, low atmospheric pressure, and vitamin deficiencies (48, 49). In contrast, this study observed a significantly lower incidence of scoliosis among children and adolescents residing in medium- and high-altitude regions (≥1,000 meters) compared to those in low-altitude areas, suggesting a potential protective role of altitude. The following factors may help explain this discrepancy:
First, the unique geographical environment of Yunnan Province, which includes its low-latitude plateau setting, prolonged sunlight exposure, and distinctive patterns of temperature and humidity, may contribute to specific influences on spinal development. Additionally, long-term residence at high altitude may promote physiological adaptations or select for genetic traits that confer greater tolerance to hypoxic conditions, potentially reducing susceptibility to scoliosis. Second, children and adolescents in high-altitude areas tend to engage in higher levels of physical activity, which may enhance paraspinal muscle strength and spinal stability. Sufficient ultraviolet radiation also facilitates vitamin D synthesis, which supports skeletal health (35, 50). Furthermore, hypoxic conditions may stimulate the expression of angiogenic factors or modulate energy metabolism pathways, possibly offering protective effects on spinal development (51).
Study limitations
Owing to the constraints of large-scale screening, our analysis represents only a preliminary exploration of risk factors, and some potential influences may not have been fully accounted for. Moreover, the cross-sectional design precludes causal inference and may not completely control for all confounding variables. Additionally, limited by the procedures of the screening study, we relied solely on the Adam’s Forward Bend Test (ATR) as a screening tool. This means that, since the protocol did not include subsequent confirmatory X-ray diagnosis, it could not be determine the prevalence of scoliosis or its changes over time. Future research should aim to refine screening strategies, establish standardized referral and follow-up protocols, and incorporate more robust methodologies—such as longitudinal cohorts or experimental studies—to further clarify the mechanisms of scoliosis and advance the standardization and systematization of screening programs.
Conclusion
This study conducted scoliosis screening among 69,811 primary and junior high school students across 32 counties or districts within 16 prefecture-level cities in Yunnan Province, China. The screening aimed to assess the detection rate and identify influencing factors for scoliosis among children and adolescents in the region. Results showed an overall detection rate of 1.98%. Higher risk was associated with female gender, senior high school students, and greater height. Lower risk was observed among students in rural areas, ethnic minorities, regions with moderate or low economic development, medium and high-altitude regions, and those with higher body weight. These findings highlight the importance of enhancing scoliosis screening programs in Yunnan by focusing on high-risk groups including female adolescents, senior high school students, and urban students. Additionally, tailored interventions should be implemented to address health disparities in rural and ethnic minority communities.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Scientific Research Ethics Committee of Yunnan Provincial Center for Disease Control and Prevention (Yunnan Provincial Center for Disease Control and Prevention). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
SS: Conceptualization, Data curation, Formal analysis, Writing – original draft. YH: Conceptualization, Data curation, Formal analysis, Writing – original draft. QZ: Conceptualization, Data curation, Writing – review & editing. TS: Data curation, Investigation, Project administration, Writing – review & editing. WA: Data curation, Investigation, Project administration, Writing – review & editing. LD: Data curation, Investigation, Project administration, Writing – review & editing. MT: Data curation, Investigation, Project administration, Writing – review & editing. JH: Data curation, Formal analysis, Visualization, Writing – review & editing. RS: Data curation, Formal analysis, Visualization, Writing – review & editing. YS: Project administration, Supervision, Writing – review & editing. XY: Project administration, Supervision, Writing – review & editing. LC: Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Yunnan Xingdian Talent Support Program – Famous Doctor Project (Grant No.: XDYC-MY-2022-0075). This study was also supported by the Innovation Foundation of Tianjin University (Grant No.: 2025XJ-0020).
Acknowledgments
We gratefully thank the staff members of the Center for Disease Control and Prevention of Yunnan for their assistance in the data collection, and validation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1659046/full#supplementary-material
Abbreviations
AOR, adjusted odds ratios; CI, Confidence Interval; AIS, Adolescent Idiopathic Scoliosis; IS, Idiopathic Scoliosis; DEM, digital elevation model; GDP, Gross Domestic Product.
References
1. Lonstein, JE. Congenital spine deformities: scoliosis, kyphosis, and lordosis. Orthop Clin North Am. (1999) 30:387–405. doi: 10.1016/S0030-5898(05)70094-8
2. Spinal Surgery Group, Society of Osteology, Chinese Medical Association. Adolescent scoliosis screening in China: clinical practice guideline and pathway. Chin J Orthop. (2020) 40:1574–82. doi: 10.3760/cma.j.cn121113-20201108-00643
3. Kuznia, AL, Hernandez, AK, and Lee, LU. Adolescent idiopathic scoliosis: common questions and answers. Am Fam Physician. (2020) 101:19–23. Available online at: https://pubmed.ncbi.nlm.nih.gov/31894928/
4. Negrini, S, Donzelli, S, Aulisa, AG, Czaprowski, D, Schreiber, S, de Mauroy, JC, et al. 2016 Sosort guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. (2018) 13:3. doi: 10.1186/s13013-017-0145-8
5. Kamtsiuris, P, Atzpodien, K, Ellert, U, Schlack, R, and Schlaud, M. Prevalence of somatic diseases in German children and adolescents. Results of the German health interview and examination survey for children and adolescents (Kiggs). Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. (2007) 50:686–700. doi: 10.1007/s00103-007-0230-x
6. Fong, DY, Lee, CF, Cheung, KM, Cheng, JC, Ng, BK, Lam, TP, et al. A meta-analysis of the clinical effectiveness of school scoliosis screening. Spine (Phila Pa 1976). (2010) 35:1061–71. doi: 10.1097/BRS.0b013e3181bcc835
7. Huang, J, Zhou, X, Li, X, Guo, H, Yang, Y, Cheong, IOH, et al. Regional disparity in epidemiological characteristics of adolescent scoliosis in China: data from a screening program. Front Public Health. (2022) 10:935040. doi: 10.3389/fpubh.2022.935040
8. Zhang, H, Guo, C, Tang, M, Liu, S, Li, J, Guo, Q, et al. Prevalence of scoliosis among primary and middle school students in mainland China: a systematic review and meta-analysis. Spine. (2015) 40:41–9. doi: 10.1097/BRS.0000000000000664
9. Xu, S, Su, YJ, and Wang, Z. The prevalence and characteristics of primary and middle-school students in China: a Meta-analysis based on 72 epidemiological research. Chin J Spine Spinal Cord. (2021) 31:901–10. doi: 10.3969/j.issn.1004-406X.2021.10.05
10. Fu, X, Meng, S, Huang, X, Li, W, Ye, B, and Chen, S. The prevalence of scoliosis among adolescents in China: a systematic review and meta-analysis. J Orthop Surg Res. (2024) 19:585. doi: 10.1186/s13018-024-05077-0
11. Grossman, DC, Curry, SJ, Owens, DK, Barry, MJ, Davidson, KW, Doubeni, CA, et al. Screening for adolescent idiopathic scoliosis: US preventive services task force recommendation statement. JAMA. (2018) 319:165–72. doi: 10.1001/jama.2017.19342
12. Yan, B, Lu, X, Nie, G, and Huang, Y. China urgently needs a nationwide scoliosis screening system. Acta Paediatr. (2020) 109:2416–7. doi: 10.1111/apa.15326
13. Charles, YP, Diméglio, A, Marcoul, M, Bourgin, J-F, Marcoul, A, and Bozonnat, M-C. Influence of idiopathic scoliosis on three-dimensional thoracic growth. Spine. (2008) 33:1209–18. doi: 10.1097/BRS.0b013e3181715272
14. Li, M, Nie, Q, Liu, J, and Jiang, Z. Prevalence of scoliosis in children and adolescents: a systematic review and meta-analysis. Front Pediatr. (2024) 12:1399049. doi: 10.3389/fped.2024.1399049
15. Linker, B. A dangerous curve: the role of history in America's scoliosis screening programs. Am J Public Health. (2012) 102:606–16. doi: 10.2105/AJPH.2011.300531
16. Luk, KD, Lee, CF, Cheung, KM, Cheng, JC, Ng, BK, Lam, TP, et al. Clinical effectiveness of school screening for adolescent idiopathic scoliosis: a large population-based retrospective cohort study. Spine (Phila Pa 1976). (2010) 35:1607–14. doi: 10.1097/BRS.0b013e3181c7cb8c
18. Liu, XM, Zhou, Y, Liu, M, and Wang, Q. Status and analysis of scoliosis screening among adolescents in Southwest China. Med J West China. (2023) 35:1203–7. doi: 10.3969/j.issn.1672-3511.2023.08.021
19. General Administration of Quality Supervision I A, Quarantine of the People's Republic of China S, Gb/T16133-2014 A O T P S R O C. Screening of spinal curvature abnormality of children and adolescents. Beijing: Standards Press of China (2015).
20. Dunn, J, Henrikson, NB, Morrison, CC, Blasi, PR, Nguyen, M, and Lin, JS. Screening for adolescent idiopathic scoliosis: evidence report and systematic review for the US preventive services task force. JAMA. (2018) 319:173–87. doi: 10.1001/jama.2017.11669
21. Sun, Y, Liu, WJ, Xiong, LH, Li, M, Chen, SY, He, WY, et al. Scoliosis and associated factors among middle school students in Guangzhou City. Chin J School Health. (2021) 42:1865. doi: 10.16835/j.cnki.1000-9817.2021.12.026
22. Zou, Y, Lin, Y, Meng, J, Li, J, Gu, F, and Zhang, R. The prevalence of scoliosis screening positive and its influencing factors: a school-based cross-sectional study in Zhejiang Province, China. Front Public Health. (2022) 10:773594. doi: 10.3389/fpubh.2022.773594
23. Suh, S-W, Modi, HN, Yang, J-H, and Hong, JY. Idiopathic scoliosis in Korean schoolchildren: a prospective screening study of over 1 million children. Eur Spine J. (2011) 20:1087–94. doi: 10.1007/s00586-011-1695-8
24. Kastrinis, A, Koumantakis, G, Tsekoura, M, Nomikou, E, Katsoulaki, M, Theodosopoulos, E, et al. The effect of Schroth method on postural control and balance in patients with adolescent idiopathic scoliosis: a literature review. Adv Exp Med Biol. (2023) 1425:469–76. doi: 10.1007/978-3-031-31986-0_45
25. Konieczny, MR, Senyurt, H, and Krauspe, R. Epidemiology of adolescent idiopathic scoliosis. J Child Orthop. (2013) 7:3–9. doi: 10.1007/s11832-012-0457-4
26. Morais, T, Bernier, M, and Turcotte, F. Age- and sex-specific prevalence of scoliosis and the value of school screening programs. Am J Public Health. (1985) 75:1377–80. doi: 10.2105/ajph.75.12.1377
27. Bala, KA, and Bala, MM. Pubertal stage-dependent anthropometric variations in Turkish children with adolescent idiopathic scoliosis: an in-depth analysis. Med Sci Monit. (2023) 29:e940864. doi: 10.12659/MSM.940864
28. Xu, SH, Jiang, CY, Wang, XQ, and Yang, HJ. Research advances of correlation between estrogen and idiopathic scoliosis. J Clin Pediatr Surg. (2024) 23:493–5. doi: 10.3760/cma.j.cn101785-202208053-019
29. Tam, EMS, Liu, Z, Lam, T-P, Ting, T, Cheung, G, Ng, BKW, et al. Lower muscle mass and body fat in adolescent idiopathic scoliosis are associated with abnormal leptin bioavailability. Spine. (2016) 41:940–6. doi: 10.1097/BRS.0000000000001376
30. Danielsson, AJ. Natural history of adolescent idiopathic scoliosis: a tool for guidance in decision of surgery of curves above 50°. J Child Orthop. (2013) 7:37–41. doi: 10.1007/s11832-012-0462-7
31. Peng, Y, Wang, S-R, Qiu, G-X, Zhang, JG, and Zhuang, QY. Research progress on the etiology and pathogenesis of adolescent idiopathic scoliosis. Chin Med J. (2020) 133:483–93. doi: 10.1097/CM9.0000000000000652
32. Wanya, H, Yan, Z, Xin, T, Huiling, Q, Jinghui, C, and Ying, N. Cross-sectional, surveillance and longitudinal study of poor visual acuity in gui'an new distinct of Guizhou Province. Chin J School Health. (2023) 44:291:–294+8. doi: 10.16835/j.cnki.1000-9817.2023.02.030
33. Izzo, R, Guarnieri, G, Guglielmi, G, and Muto, M. Biomechanics of the spine. Part I: spinal stability. Eur J Radiol. (2013) 82:118–26. doi: 10.1016/j.ejrad.2012.07.024
34. Briggs, AM, Greig, AM, Wark, JD, Fazzalari, NL, and Bennell, KL. A review of anatomical and mechanical factors affecting vertebral body integrity. Int J Med Sci. (2004) 1:170–80. doi: 10.7150/ijms.1.170
35. Bala, MM, and Bala, KA. Association among complete blood count parameters, bone mineral density, and cobb angle in cases of adolescent idiopathic scoliosis. Med Sci Monit. (2023) 29:e940355. doi: 10.12659/MSM.940355
36. Chow, DH, Kwok, ML, Cheng, JC, Lao, ML, Holmes, AD, Au-Yang, A, et al. The effect of backpack weight on the standing posture and balance of schoolgirls with adolescent idiopathic scoliosis and normal controls. Gait Posture. (2006) 24:173–81. doi: 10.1016/j.gaitpost.2005.08.007
37. Haselgrove, C, Straker, L, Smith, A, O'Sullivan, P, Perry, M, and Sloan, N. Perceived school bag load, duration of carriage, and method of transport to school are associated with spinal pain in adolescents: an observational study. Aust J Physiother. (2008) 54:193–200. doi: 10.1016/S0004-9514(08)70026-6
38. Huang, L, Yang, Z, Wang, R, and Xie, L. Physiological and biomechanical effects on the human musculoskeletal system while carrying a suspended-load backpack. J Biomech. (2020) 108:109894. doi: 10.1016/j.jbiomech.2020.109894
39. Tobias, JH, Fairbank, J, Harding, I, Taylor, HJ, and Clark, EM. Association between physical activity and scoliosis: a prospective cohort study. Int J Epidemiol. (2019) 48:1152–60. doi: 10.1093/ije/dyy268
40. Qui, Y, Qiu, XS, Sun, X, Wang, B, Yu, Y, Zhu, ZZ, et al. Body mass index in girls with adolescent idiopathic scoliosis. Chin J Surg. (2008) 46:588–91. Available online at: https://pubmed.ncbi.nlm.nih.gov/18844053/
41. Adamczewska, K, Wiernicka, M, Kamińska, E, Małecka, J, Dąbrowska, A, and Malchrowicz-Mośko, E. Annual observation of changes in the angle of trunk rotation. Trunk asymmetry predictors. A study from a scoliosis screening in school adolescents. Int J Environ Res Public Health. (2020) 17:1899. doi: 10.3390/ijerph17061899
42. Guthold, R, Stevens, GA, Riley, LM, and Bull, FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc Health. (2020) 4:23–35. doi: 10.1016/S2352-4642(19)30323-2
43. Parry, SP, Coenen, P, O'sullivan, PB, O'Sullivan, PB, Maher, CG, Straker, LM, et al. Workplace interventions for increasing standing or walking for decreasing musculoskeletal symptoms in sedentary workers. Cochrane Database Syst Rev. (2017) 2017:CD012486. doi: 10.1002/14651858.CD012487.pub2
44. Wu, Z, Wang, Y, Dai, Z, Qiu, Y, Xu, L, Zhu, Z, et al. Genetic variants of abo and Sox 6 are associated with adolescent idiopathic scoliosis in Chinese Han population. Spine. (2019) 44:E1063–7. doi: 10.1097/BRS.0000000000003062
45. Qianyu, Z. Overview of the current knowledge on the etiology of adolescent idiopathic scoliosis. Chin J Bone Joint Surg. (2021) 14:337–43. doi: 10.3969/j.issn.2095-9958.2021.05.05
46. Zavatsky, JM, Peters, AJ, Nahvi, FA, Bharucha, NJ, Trobisch, PD, Kean, KE, et al. Disease severity and treatment in adolescent idiopathic scoliosis: the impact of race and economic status. Spine J. (2015) 15:939–43. doi: 10.1016/j.spinee.2013.06.043
47. Ratahi, ED, Crawford, HA, Thompson, JM, and Barnes, MJ. Ethnic variance in the epidemiology of scoliosis in New Zealand. J Pediatr Orthop. (2002) 22:784–7. doi: 10.1097/01241398-200211000-00018
48. Guanghong, P. Epidemiological study on the risk of scoliosis amongprimary and secondary school students at differentelevations in Dali, Yunnan Province. (2023).
49. Guanghong, P, Xiaowen, W, Zhi, Z, Jiang, LU, Caihong, LI, Zixiang, YAN, et al. Detection rate and influencing factors of suspected scoliosis among primary and middle school students in Dali bai autonomous prefecture. Chin J Orthop. (2022) 21:1433–40. doi: 10.3760/cma.j.cn121113-20220611-00333
50. Laird, E, Ward, M, Mcsorley, E, Strain, JJ, and Wallace, J. Vitamin D and bone health: potential mechanisms. Nutrients. (2010) 2:693–724. doi: 10.3390/nu2070693
Keywords: scoliosis, adolescents, epidemiology, high-altitude, ethnic minorities
Citation: Song S, He Y, Zhen Q, Shui T, An W, Dai L, Tan M, Hao J, Song R, Shen Y, Yan X and Chang L (2025) Large-scale school scoliosis screening in a multi-ethnic, high-altitude region of southwestern China: an epidemiological study of 69,811 children and adolescents. Front. Public Health. 13:1659046. doi: 10.3389/fpubh.2025.1659046
Edited by:
Yakun Liu, Soochow University, ChinaReviewed by:
Yunzhong Cheng, Capital Medical University, ChinaAlinda Nur Ramadhani, University of Aisyiyah Surakarta, Indonesia
Mehmet Murat Bala, Hacettepe University, Türkiye
Ruixin Liang, Hong Kong Polytechnic University, Hong Kong SAR, China
Copyright © 2025 Song, He, Zhen, Shui, An, Dai, Tan, Hao, Song, Shen, Yan and Chang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Litao Chang, NzgzMjcxMzVAcXEuY29t; Xiangyu Yan, eWFueGlhbmd5dUB0anUuZWR1LmNu; Yong Shen, c2hlbnlvbmdAamx1LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
 Shanshan Song1†
Shanshan Song1† Qing Zhen
Qing Zhen Tiejun Shui
Tiejun Shui Xiangyu Yan
Xiangyu Yan