- 1Department of Public Health, University of Naples Federico II, Naples, Italy
- 2PhD National Program in One Health Approaches to Infectious Diseases and Life Science Research, Department of Public Health, Experimental and Forensic Medicine, University of Pavia, Pavia, Italy
- 3Interdepartmental Research Center in Healthcare Management and Innovation in Healthcare (CIRMIS), Naples, Italy
- 4Department of Primary Care and Public Health, School of Public Health, Imperial College, London, United Kingdom
Introduction: Since the COVID-19 pandemic onset, preventive measures (e.g., social distancing, hand hygiene, mask usage) and vaccines have been pivotal in mitigating transmission and reducing public health burdens. Although adherence to these measures, influenced by factors such as ventilation and exposure duration, has been extensively validated, their long-term sustainability faces socio-economic challenges.
Objectives: To investigate the association between risk perception and adherence to preventive behaviors and conduct a meta-analysis comparing these behaviors in vaccinated versus unvaccinated subgroups.
Methods: A systematic review following PRISMA guidelines identified studies (2021–2024) analyzing risk perception and preventive behaviors. Potential biases were assessed using the MMAT tool. A meta-analysis calculated pooled effect sizes across subgroups.
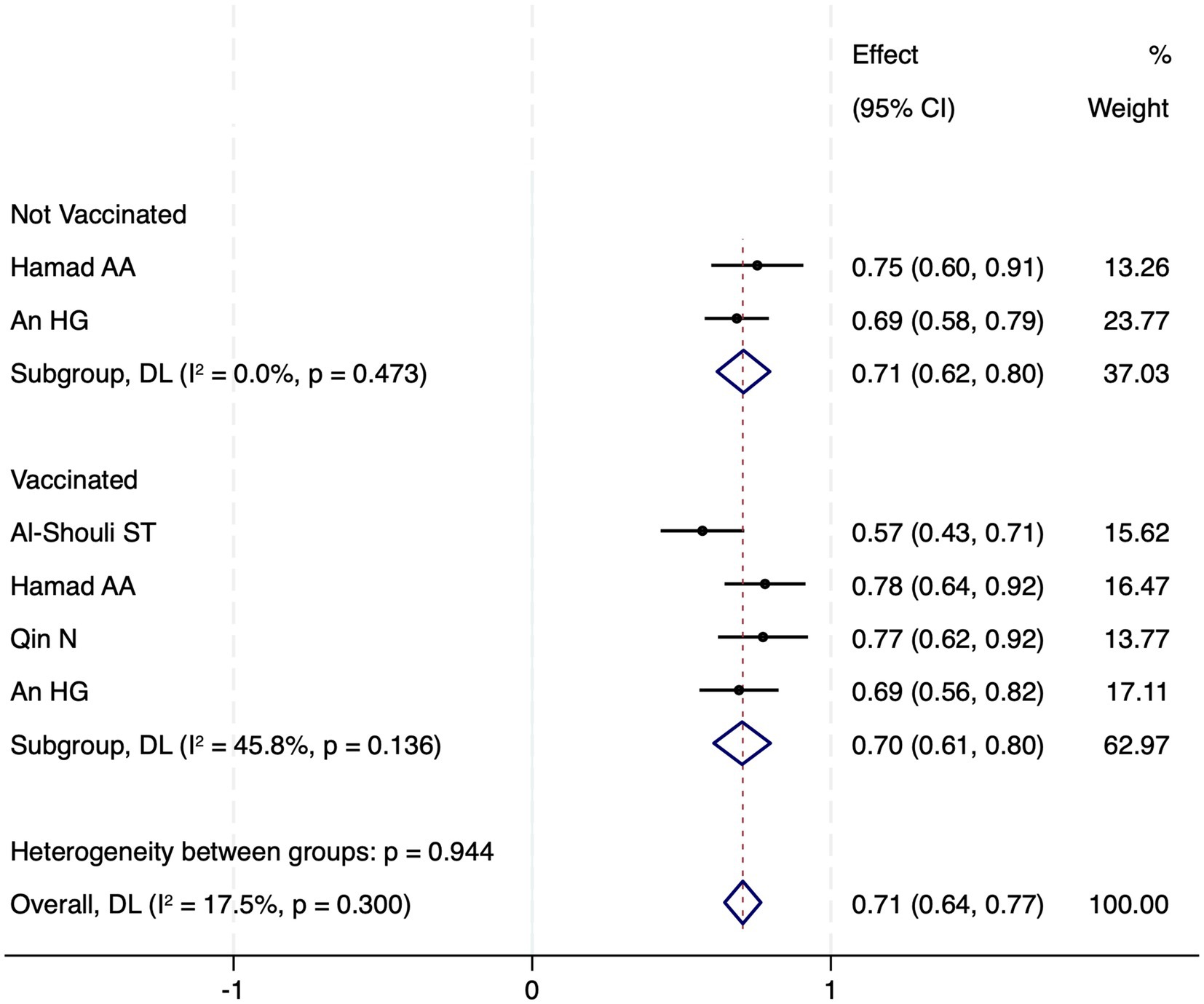
Results: Of 1,594 screened studies, 10 met inclusion criteria (six for meta-analysis, n = 9,115). Populations included adults, students, and healthcare professionals across 24 countries. Most vaccinated individuals maintained preventive behaviors despite stable or declining risk perception, though social distancing and hand hygiene adherence decreased over time. Booster-vaccinated individuals exhibited higher compliance than partially vaccinated or unvaccinated counterparts. Unvaccinated individuals intending to vaccinate reported higher risk perception than those refusing vaccination. Meta-analysis revealed no significant difference in risk perception between vaccinated (70.3, 95% CI 60.8–79.8) and unvaccinated subgroups (70.8, 95% CI 61.9–79.6; I2 = 17.5%), suggesting limited influence on behavior maintenance.
Conclusion: While vaccination and preventive measures curbed COVID-19 transmission, risk perception alone does not robustly predict sustained adherence, potentially due to risk compensation. Future research should prioritize determinants of long-term behavioral retention in public health strategies.
1 Introduction
Since the World Health Organization (WHO) declared COVID-19 a global pandemic in March 2020 (1), coordinated efforts to limit viral transmission and mitigate strain on public health systems have been implemented worldwide (2). Preventive measures, including lockdowns, social distancing, hand hygiene, and mask usage, were widely recognized as effective strategies to reduce transmission (3). Concurrently, the rapid development and deployment of COVID-19 vaccines played a critical role in pandemic control (4).
Airborne transmission risk is modulated by factors such as ventilation quality (5), exposure duration (6), and adherence to preventive measures (7–9). These interventions not only curtailed COVID-19 spread but also reduced the incidence of other airborne diseases, such as seasonal influenza (10, 11). However, long-term adherence to measures like physical distancing has proven challenging due to socio-economic and behavioral barriers (12, 13). Lockdowns and travel restrictions further strained global economies and supply chains (14), underscoring the need for sustainable strategies.
Successful immunization campaigns enabled a gradual return to normalcy (15–17), yet maintaining preventive behaviors remains critical to minimize pathogen transmission and bolster pandemic preparedness (18).
Risk perception—defined as the intuitive assessment of potential hazards—shapes health-related decision-making (19, 20). This cognitive process involves two components: (1) estimating the probability of harm and (2) subjectively evaluating its severity (21). Differently, risk preferences reflect stable tendencies toward risk avoidance or acceptance (22). Both constructs influence health behaviors, including vaccination uptake and adherence to preventive measures (23).
The introduction of COVID-19 vaccines raised questions about their impact on risk perception and behavioral adherence. Vaccinated individuals may exhibit risk compensation; wherein reduced threat perception diminishes protective behaviors (24). While evidence suggests vaccination lowers self-perceived risk and compliance (24), individuals with heightened public health awareness often sustain preventive practices, particularly in high-risk settings (25, 26). Motivation, mediated by risk perception, remains a key predictor of adherence (27), though messaging and individual awareness also play roles (28).
As the success of current and future public health campaigns on reducing the impact of COVID-19 and other infectious diseases dwell on the possibility to improve both vaccination uptake and adherence to non-pharmaceutical intervention. While the implementation of these measures, during the pandemic, was common and widely accepted, the post-pandemic transition has seen a significant drop in both vaccination and adherence to preventive measures (29). However, understanding the dynamic of retaining preventive measures, not only for the purpose of containing the impact of pandemic, but also for the effect on other air-borne transmitted infection is pivotal to prevent their diffusion. Therefore, this systematic review and meta-analysis aim to assess the impact of COVID-19 vaccination on risk perception change as a predictor of sustained preventive behaviors during the COVID-19 pandemic.
2 Methods
This systematic review and meta-analysis examined the association between COVID-19 vaccination and risk perception change as a predictor of sustained preventive behaviors during the COVID-19 pandemic. The study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (30).
2.1 Eligibility criteria
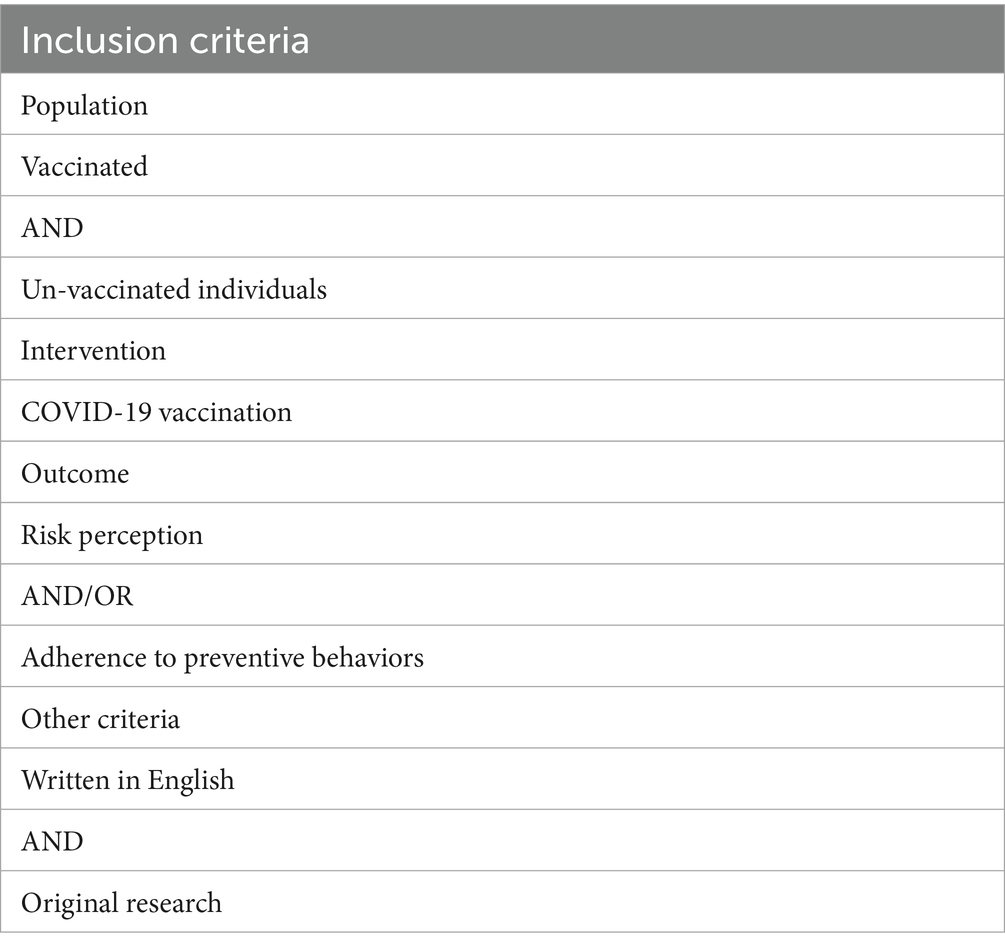
Eligible studies included original research (e.g., cohort, cross-sectional, case-control, or qualitative studies) addressing risk perception, preventive behaviors, and vaccination status across all ages, genders, races, and socioeconomic groups. Exclusion criteria included non-English publications, reviews, commentaries, and studies lacking primary data. A summary of eligibility criteria is provided in Table 1.
2.2 Search strategy
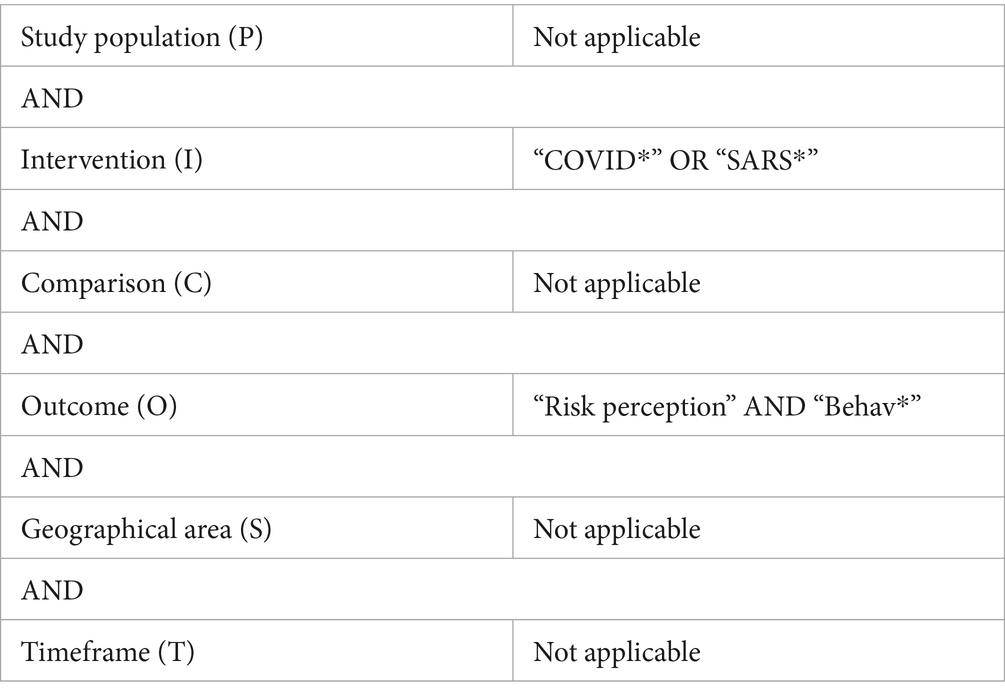
This systematic review used the PICO framework to define the inclusion criteria as follows: Population (P): individuals of any age, gender, race, or socioeconomic group; Intervention/Exposure (I): COVID-19 vaccination; Comparator (C): not applicable; Outcomes (O): changes in risk perception and sustained preventive behaviors.
A systematic search was conducted in PubMed/MEDLINE, Embase, PsycINFO (EBSCOhost), Health Technology Assessment Database, and Web of Science (Clarivate) from January 2020 to 22 March 2025 using the following Boolean string: (“risk perception”) AND (“COVID*” OR “SARS*”) AND (“Behav*”). Additional studies were identified through manual searches of reference lists from relevant reviews. The correspondence between PICO elements and search terms is reported in Table 2.
2.3 Data extraction and quality assessment
Two reviewers (MS and CF) independently screened titles/abstracts using Rayyan Artificial Intelligence (31), resolving discrepancies through discussion with a senior reviewer (RP). Full texts were reviewed for ambiguous abstracts. Data on study design, population, outcomes, and risk perception metrics were extracted into a standardized Excel template. Study quality was assessed using the Mixed Methods Appraisal Tool (MMAT), revised version (32), which evaluates methodological rigor across five domains (quantitative, qualitative, mixed methods). Scores range from 0% (no criteria met) to 100% (all criteria met). Studies were retained regardless of quality but flagged for sensitivity analysis if scoring below 50%. For mixed-methods studies, the overall score reflected the weakest component.
2.4 Statistical analysis
Studies from the systematic review were included in a meta-analysis comparing risk perception between vaccinated and unvaccinated subgroups. Risk perception scores were standardized as percentages [mean/ (scale maximum) × 100]. Subgroups included: Vaccinated: fully vaccinated (four doses), boosted (three doses), or partially vaccinated (1–2 doses); and Unvaccinated: no doses received.
Pooled effect sizes were calculated using random-effects models (DerSimonian-Laird estimator) with inverse-variance weighting. Heterogeneity was assessed via I2 statistics, and meta-regression explored variance across subgroups. Analyses were performed in Stata (MP 18.0) with the meta and metan packages.
3 Results
3.1 Study selection
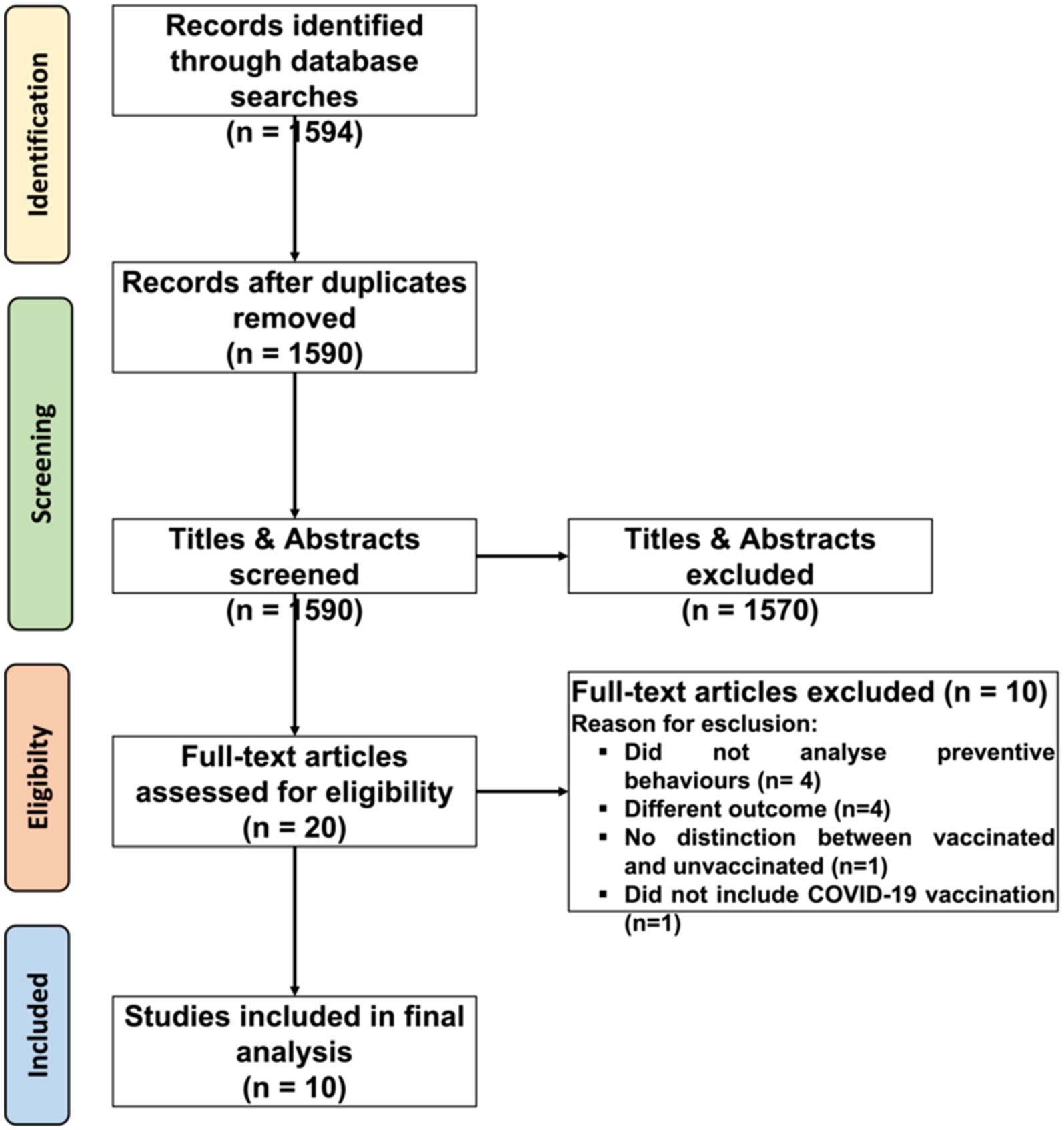
The main research identified 1,594 studies. Following deduplication in Rayyan, 1,590 unique records were retained. Title and abstract screening excluded 1,570 studies, leaving 20 for full-text assessment. Of these, 10 met inclusion criteria, as illustrated in the PRISMA flow diagram (Figure 1). Excluded studies (n = 10) were omitted due to: absence of preventive behavior assessments (n = 4), irrelevant outcomes (n = 4), lack of vaccination status distinction (n = 1), or no COVID-19 vaccination focus (n = 1). Grey literature, conference papers, dissertations, and editorials were excluded a priori.
3.2 Study characteristics
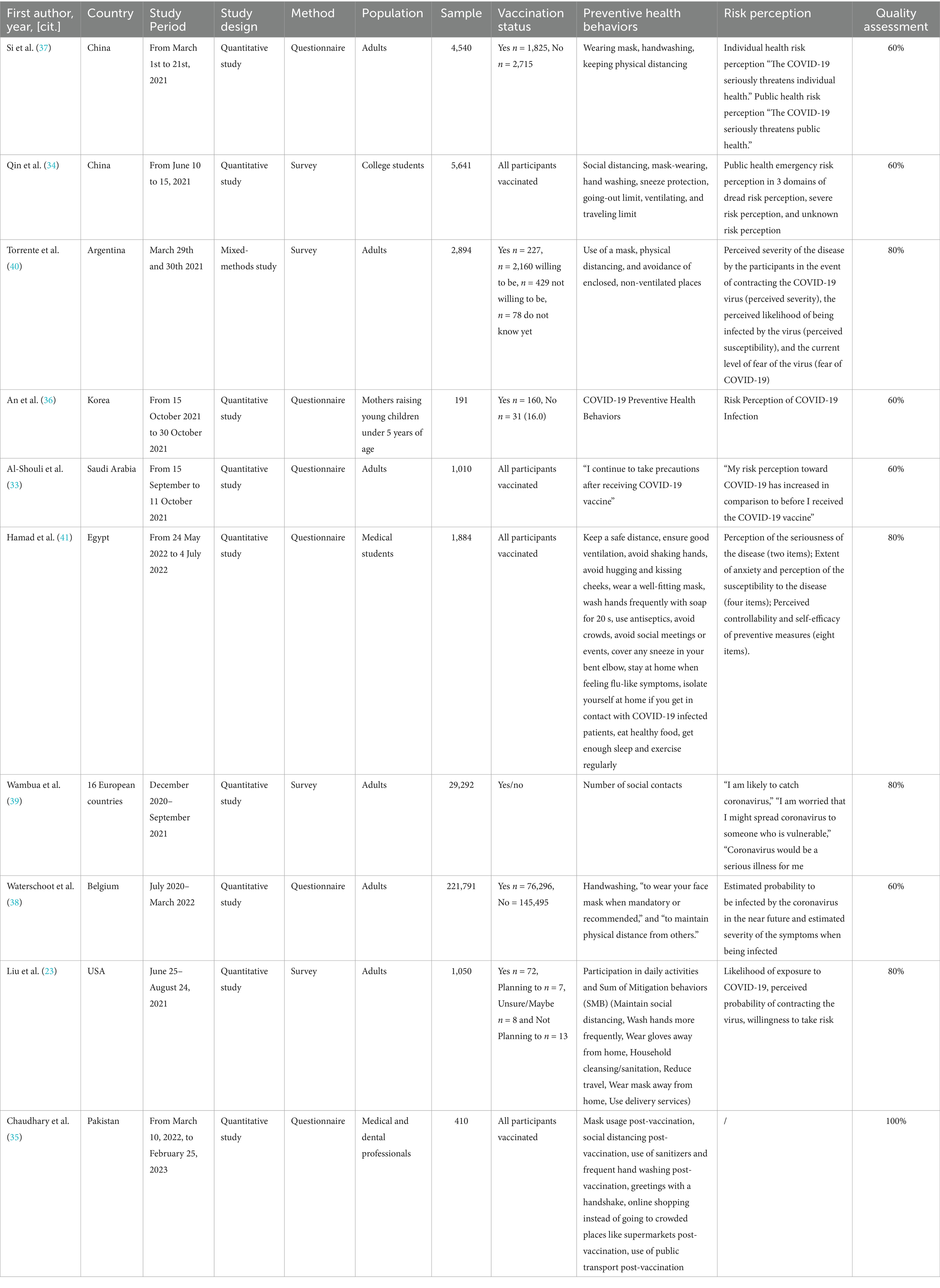
The 10 included studies (2021–2024) comprised nine quantitative investigations (six questionnaire-based, three survey-based) and one mixed-methods study (Table 3). Geographically, studies took place in Argentina (n = 1), Belgium (n = 1), China (n = 2), Egypt (n = 1), South Korea (n = 1), Pakistan (n = 1), Saudi Arabia (n = 2), the USA (n = 1), and 16 European nations (n = 1). Study populations focused on general adults (n = 6), college/medical students (n = 2), healthcare professionals (n = 1), and mothers of young children (n = 1), with sample sizes ranging from 191 to 221,791 participants.
Vaccination status categorizations varied: three studies included vaccinated-only cohorts (33–35), four compared vaccinated and unvaccinated individuals (36–39), two stratified by vaccination intent (23, 40), and one differentiated between boosted, partially vaccinated, and unvaccinated subgroups (41). Protective behaviors assessed encompassed mask-wearing, hand hygiene, distancing, and crowd avoidance. Risk perception metrics included personal risk (e.g., perceived severity, infection likelihood) and general risk (e.g., public health impact).
3.3 Vaccination status and its impact on risk perception and protective behaviors
Vaccinated individuals predominantly sustained protective behaviors despite static or diminished risk perception. For instance, 62%–78% of vaccinated participants maintained consistent mask use post-vaccination (33, 38, 39), though declines in handwashing (−15%) and distancing (−22%) coincided with increased public transport use (+18%) (35). Notably, boosted individuals demonstrated higher adherence (OR = 1.4, 95% CI 1.1–1.8) than partially or unvaccinated counterparts (41). Unvaccinated individuals intending to vaccinate reported elevated infection risk perception relative to vaccine-refusers (Δ = 12.3%, p < 0.01) (23). Conversely, no significant behavioral or perceptual differences emerged among mothers of young children regardless of vaccination status (36).
3.4 Meta-analysis
Six studies (n = 9,115) were included in the meta-analysis after standardizing risk perception scores as percentages (mean/scale maximum × 100). Excluded studies (n = 4) lacked comparable risk perception metrics. Pooled estimates revealed minimal differences between vaccinated (70.3, 95% CI 60.8–79.8) and unvaccinated subgroups (70.8, 95% CI 61.9–79.6) (Figure 2). Meta-regression confirmed no significant between-group disparity (β = −0.5%, p = 0.87), with low heterogeneity (I2 = 17.5%). A random-effects model corroborated negligible overall variance (τ2 = 0.02, Q = 6.1, p = 0.41).
4 Discussion
Risk perception and adherence to protective behaviors are pivotal to pandemic management, modulating viral transmission and the efficacy of containment strategies. While COVID-19 vaccination reduced disease severity and transmission, its impact on risk perception and behavioral adherence exhibited marked heterogeneity. Overall, adherence levels remained similar between vaccinated and unvaccinated individuals, with meta-analyses confirming negligible differences and low variance across groups. While some vaccinated individuals sustained protective measures despite static risk perception, others engaged in risk compensation, perceiving vaccination as sufficient protection. These dynamics underscore the need for nuanced public health messaging to promote sustained behavioral adherence.
The 10 studies analyzed—spanning diverse regions, including the USA, China, Belgium, and 16 European nations—reflect varied cultural, social, and political contexts shaping health behaviors. This geographical diversity strengthens generalizability, though it introduces variability in risk perception metrics and behavioral norms.
A significant proportion of vaccinated individuals, maintained precautions post-vaccination, likely driven by persistent awareness of residual risks or social responsibility (33, 34). However, declines in handwashing (−15%) and distancing (−22%) alongside increased public transport use (+18%) (35) suggest risk compensation behaviors (42), wherein perceived vaccine-derived security reduced vigilance. This aligns with evidence that COVID-19 vaccination lowers self-perceived risk and adherence (42–44) underscoring the need to address behavioral complacency in public health campaigns.
Notably, boosted individuals exhibited higher adherence and risk perception than partially/unvaccinated counterparts (41), potentially reflecting heightened awareness of waning immunity. Conversely, unvaccinated individuals intending to vaccinate reported elevated risk perception compared to vaccine refusers (23), suggesting fear of infection and vaccine confidence synergistically drive uptake (45–47).
The meta-analysis revealed no significant difference in risk perception between vaccinated (70.3, 95% CI 60.8–79.8) and unvaccinated subgroups (70.8, 95% CI 61.9–79.6; β = −0.5%, p = 0.87). This null finding may reflect risk compensation: vaccinated individuals, despite inherently higher baseline risk perception (38, 39), may offset perceived protection via reduced behavioral adherence, attenuating measurable differences between groups. Such compensation is well-documented in health psychology, wherein interventions reducing perceived risk inadvertently disincentivize precautionary behaviors (42–44).
5 Policy
Understanding the interplay between COVID-19 vaccination status, risk perception, and protective behaviors is critical for designing adaptive public health strategies. While vaccination campaigns have been pivotal in curtailing disease severity and transmission, their influence on behavioral adherence—marked by risk compensation in some subgroups—demands nuanced policy approaches.
To sustain precautionary measures, initiatives should leverage messaging that: (1) underscores communal responsibility through narratives emphasizing protection of vulnerable populations, as shown in studies linking higher perceived collective risk with greater adherence (48); (2) highlights the persistence of viral evolution, including risks of breakthrough infections and asymptomatic transmission consistent with evidence indicating that awareness of residual risk predicts sustained protective behaviors (49); and (3) addresses risk compensation by reframing vaccination as complementary to—not substitutive for—preventive behaviors. Tailored, culturally resonant communication, disseminated via trusted community leaders and digital platforms, can mitigate complacency while fostering equitable adherence (50).
Integrating these evidence-based insights into policy frameworks will optimize population-level vaccine efficacy and resilience against future pandemics, ensuring public health strategies evolve in tandem with behavioral and epidemiological realities.
6 Strengths and limitations
This study offers several strengths. First, it systematically examines the interplay between COVID-19 vaccination status, risk perception, and adherence to preventive behaviors across diverse populations and geographic contexts, enhancing ecological validity. By including both vaccinated and unvaccinated subgroups, it enables nuanced comparisons of behavioral patterns. Adherence to PRISMA guidelines and the integration of meta-analytic methods further bolster methodological rigor, providing a robust quantitative synthesis of global evidence.
However, limitations must be acknowledged. First, the relatively small number of included studies (n = 10, of which six were included in the meta-analysis) constrains the external validity of our findings. This limited evidence base may reduce the generalizability of results across different populations, settings, and time periods. To mitigate this, we performed a comprehensive search across multiple databases and applied a rigorous screening process, ensuring that all eligible studies were captured. Further high-quality studies are therefore needed to validate and extend these findings in broader and more diverse cohorts. Second, while the low heterogeneity (I2 = 17.5%) supports internal consistency, the exclusion of studies with divergent methodologies—though necessary to ensure analytical coherence—may have omitted contextually relevant insights. Nonetheless, sensitivity analyses confirmed that the overall conclusions remained stable despite these exclusions. Third, variations in study design and data collection methods (e.g., self-reported behaviors, cross-sectional frameworks) may have introduced bias, limiting causal inference. To reduce this impact, we carefully assessed study quality and applied consistent inclusion criteria, thereby increasing comparability across studies. Fourth, the predominance of cross-sectional designs precludes longitudinal assessment of risk perception dynamics. Although this limits the ability to infer causality or long-term trends, the convergence of findings across independent studies strengthens confidence in the overall conclusions. Future research should adopt time-series or cohort approaches to expand on these results. Fifth, this review was not prospectively registered in PROSPERO, which may reduce transparency and increase the risk of selective reporting. However, we strictly followed PRISMA guidelines to ensure methodological rigor and transparency, and a complete description of the methodology is provided in the Supplementary material. Finally, restricting the search to English-language studies may have introduced selection bias. This choice, however, is common practice in systematic reviews, as the majority of international scientific literature is conventionally published in English. Moreover, accurate interpretation of findings in multiple foreign languages would have required expertise beyond the scope of the review team. By focusing on English-language studies, we minimized the risk of misinterpretation or inconsistent data extraction, ultimately strengthening the reliability of the synthesis.
7 Conclusion
The relationship between COVID-19 vaccination, risk perception, and protective behaviors is shaped by cognitive evaluations, affective responses, and socio-contextual factors. While COVID-19 incidence has markedly declined and preventive measures are no longer widely practiced in many contexts, our findings remain relevant by illustrating how vaccination can interact with risk perception and behavioral adherence. The meta-analytic null finding—no significant difference in risk perception between vaccinated and unvaccinated subgroups—suggests that baseline perceptual differences may be offset by behavioral adjustments post-vaccination.
These insights underscore the necessity of public health strategies that go beyond one-size-fits-all messaging. In future pandemic scenarios or vaccination campaigns for respiratory infections such as influenza or RSV, emphasizing communal responsibility, residual transmission risks, and the complementary role of vaccination and preventive behaviors may mitigate complacency. Moreover, integrating psychological, behavioral, and epidemiological evidence can inform preparedness frameworks and support the design of behaviorally informed interventions. By applying these lessons across infectious threats, policymakers can strengthen resilience, ensure adaptive health strategies, and sustain population-level protection even as epidemiological conditions evolve.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
MS: Writing – review & editing, Writing – original draft. CF: Writing – review & editing, Writing – original draft. FR: Writing – review & editing. PM: Writing – review & editing. RP: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1661015/full#supplementary-material
References
1. Cucinotta, D, and Vanelli, M. Who declares COVID-19 a pandemic. Acta Biomed. (2020) 91:157–60. doi: 10.23750/abm.v91i1.9397
2. Ayouni, I, Maatoug, J, Dhouib, W, Zammit, N, Fredj, SB, Ghammam, R, et al. Effective public health measures to mitigate the spread of COVID-19: a systematic review. BMC Public Health. (2021) 21:1015. doi: 10.1186/s12889-021-11111-1
3. World Health Organization (WHO). Advice for the public: coronavirus disease (COVID-19) (2023). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed April, 4, 2024).
4. U.S. Food and Drug Administration. FDA approves first COVID-19 vaccine (2021). Available online at: https://www.fda.gov/news-events/press-announcements/fda-approves-first-covid-19-vaccine (accessed April, 4, 2024).
5. Riediker, M, and Tsai, DH. Estimation of viral aerosol emissions from simulated individuals with asymptomatic to moderate coronavirus disease 2019. JAMA Netw Open. (2020) 3:e2013807. doi: 10.1001/jamanetworkopen.2020.13807
6. Vuorinen, V, Aarnio, M, Alava, M, Alopaeus, V, Atanasova, N, Auvinen, M, et al. Modelling aerosol transport and virus exposure with numerical simulations in relation to SARS-CoV-2 transmission by inhalation indoors. Saf Sci. (2020) 130:104866. doi: 10.1016/j.ssci.2020.104866
7. Esposito, S, Principi, N, Leung, CC, and Migliori, GB. Universal use of face masks for success against COVID-19: evidence and implications for prevention policies. Eur Respir J. (2020) 55:2001260. doi: 10.1183/13993003.01260-2020
8. Peeples, L. Face masks: what the data say. Nature. (2020) 586:186–9. doi: 10.1038/d41586-020-02801-8
9. Ramanathan, K, Antognini, D, Combes, A, Paden, M, Zakhary, B, Ogino, M, et al. Planning and provision of ECMO services for severe ARDS during the COVID-19 pandemic and other outbreaks of emerging infectious diseases. Lancet Respir Med. (2020) 8:518–26. doi: 10.1016/S2213-2600(20)30121-1
10. Lu, L, Peng, J, Wu, J, and Lu, Y. Perceived impact of the COVID-19 crisis on SMEs in different industry sectors: evidence from Sichuan, China. Int J Disaster Risk Reduct. (2021) 55:102085. doi: 10.1016/j.ijdrr.2021.102085
11. Chu, DK, Duda, S, Solo, K, Yaacoub, S, and Schunemann, H. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. J Vasc Surg. (2020) 72:1500. doi: 10.1016/j.jvs.2020.07.040
12. Subbaraman, N. Return to the lab: scientists face shiftwork, masks and distancing as coronavirus lockdowns ease. Nature. (2020) 582:15–6. doi: 10.1038/d41586-020-01587-z
13. Steinbrook, R. Filtration efficiency of face masks used by the public during the COVID-19 pandemic. JAMA Intern Med. (2021) 181:470. doi: 10.1001/jamainternmed.2020.8234
14. Naseer, S, Khalid, S, Parveen, S, Abbass, K, Song, H, and Achim, MV. COVID-19 outbreak: impact on global economy. Front Public Health. (2023) 10:1009393. doi: 10.3389/fpubh.2022.1009393
15. Hezam, IM, Nayeem, MK, Foul, A, and Alrasheedi, AF. COVID-19 vaccine: a neutrosophic MCDM approach for determining the priority groups. Results Phys. (2021) 20:103654. doi: 10.1016/j.rinp.2020.103654
16. Zhang, L, Tao, Y, Shen, M, Fairley, CK, and Guo, Y. Can self-imposed prevention measures mitigate the COVID-19 epidemic? PLoS Med. (2020) 17:e1003240. doi: 10.1371/journal.pmed.1003240
17. Forman, R, Shah, S, Jeurissen, P, Jit, M, and Mossialos, E. COVID-19 vaccine challenges: what have we learned so far and what remains to be done? Health Policy. (2021) 125:553–67. doi: 10.1016/j.healthpol.2021.03.013
18. Lee, JK, Bullen, C, Ben Amor, Y, Bush, SR, Colombo, F, Gaviria, A, et al. Institutional and behaviour-change interventions to support COVID-19 public health measures: a review by the lancet commission task force on public health measures to suppress the pandemic. Int Health. (2021) 13:399–409. doi: 10.1093/inthealth/ihab022
19. Pratt, JW. Risk aversion in the small and in the large. Econometrica. (1976) 44:420. doi: 10.2307/1912743
20. Sitkin, SB, and Pablo, AL. Reconceptualizing the determinants of risk behavior. Acad Manag Rev. (1992) 17:9. doi: 10.2307/258646
22. Kassas, B, Morgan, SN, Lai, JH, Kropp, JD, and Gao, Z. Perception versus preference: the role of self-assessed risk measures on individual mitigation behaviors during the COVID-19 pandemic. PLoS One. (2021) 16:e0254756. doi: 10.1371/journal.pone.0254756
23. Liu, J, Kassas, B, Lai, J, Kropp, J, and Gao, Z. Understanding the role of risk preferences and perceptions in vaccination decisions and post-vaccination behaviors among U.S. households. Sci Rep. (2024) 14:3190. doi: 10.1038/s41598-024-52408-6
24. De Nicolò, V, Villari, P, and De Vito, C. Impact of COVID-19 vaccination on risk perception: a cross-sectional study on vaccinated people. Eur J Pub Health. (2022) 32:ckac129.664. doi: 10.1093/eurpub/ckac129.664
25. Wise, T, Zbozinek, TD, Michelini, G, Hagan, CC, and Mobbs, D. Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States. R Soc Open Sci. (2020) 7:200742. doi: 10.1098/rsos.200742
26. Chen, YL, Lin, YJ, Chang, YP, Chou, WJ, and Yen, CF. Differences in sources of information, risk perception, and cognitive appraisals between people with various latent classes of motivation to get vaccinated against COVID-19 and previous seasonal influenza vaccination: facebook survey study with latent profile analysis in Taiwan. Vaccines. (2021) 9:1203. doi: 10.3390/vaccines9101203
27. Ferrer, RA, Klein, WMP, Avishai, A, Jones, K, Villegas, M, and Sheeran, P. When does risk perception predict protection motivation for health threats? A person-by-situation analysis. PLoS One. (2018) 13:e0191994. doi: 10.1371/journal.pone.0191994
28. Hitchman, SC, Geber, S, Tribelhorn, L, and Friemel, TN. COVID-19 vaccination and changes in preventive behaviours: findings from the 2021 vaccine roll-out in Switzerland. Eur J Pub Health. (2023) 33:482–9. doi: 10.1093/eurpub/ckad050
29. Hamson, E, Forbes, C, Wittkopf, P, Pandey, A, Mendes, D, Kowalik, J, et al. Impact of pandemics and disruptions to vaccination on infectious diseases epidemiology past and present. Hum Vaccin Immunother. (2023) 19:2219577. doi: 10.1080/21645515.2023.2219577
30. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
31. Ouzzani, M, Hammady, H, Fedorowicz, Z, and Elmagarmid, A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. (2016) 5:210. doi: 10.1186/s13643-016-0384-4
32. Hong, QN, Fàbregues, S, Bartlett, G, Boardman, F, Cargo, M, Dagenais, P, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. (2018) 34:285–91. doi: 10.3233/EFI-180221
33. Al-Shouli, ST, AlAfaleq, NO, Almansour, M, Alsadhan, M, Alsalem, N, Alqahtani, M, et al. Assessment of risk perception of COVID-19 post vaccination amongst the general population of Riyadh region. Vaccines. (2023) 11:1276. doi: 10.3390/vaccines11071276
34. Qin, N, Shi, S, Ma, G, Li, X, Duan, Y, Shen, Z, et al. Associations of COVID-19 risk perception, eHealth literacy, and protective behaviors among Chinese college students following vaccination: a cross-sectional study. Front Public Health. (2022) 9:776829. doi: 10.3389/fpubh.2021.776829
35. Chaudhary, FA, Khattak, O, Khalid, MD, Khattak, MU, Khan, FH, Khatoon, F, et al. Changes in complacency to adherence to COVID-19 preventive behavioral measures and mental health after COVID-19 vaccination among medical and dental healthcare professionals. Hum Vaccin Immunother. (2024) 20:2369358. doi: 10.1080/21645515.2024.2369358
36. An, HG, and Yoon, CM. A study on determinants of COVID-19 preventive health behaviors of mothers with young children in South Korea. Healthcare. (2022) 10:2111. doi: 10.3390/healthcare10102111
37. Si, R, Yao, Y, Zhang, X, Lu, Q, and Aziz, N. Investigating the links between vaccination against COVID-19 and public attitudes toward protective countermeasures: implications for public health. Front Public Health. (2021) 9:702699. doi: 10.3389/fpubh.2021.702699
38. Waterschoot, J, Vansteenkiste, M, Yzerbyt, V, Morbée, S, Klein, O, Luminet, O, et al. Risk perception as a motivational resource during the COVID-19 pandemic: the role of vaccination status and emerging variants. BMC Public Health. (2024) 24:731. doi: 10.1186/s12889-024-18020-z
39. Wambua, J, Loedy, N, Jarvis, CI, Wong, KLM, Faes, C, Grah, R, et al. The influence of COVID-19 risk perception and vaccination status on the number of social contacts across Europe: insights from the CoMix study. BMC Public Health. (2023) 23:1350. doi: 10.1186/s12889-023-16252-z
40. Torrente, F, Low, D, and Yoris, A. Risk perception, but also political orientation, modulate behavioral response to COVID-19: a randomized survey experiment. Front Psychol. (2022) 13:13. doi: 10.3389/fpsyg.2022.900684
41. Hamad, AA, Selim, R, Amer, BE, Diab, RA, Elazb, M, Elbanna, EH, et al. COVID-19 risk perception and adherence to preventive measures among medical students after receiving COVID-19 vaccination: a multicenter cross-sectional study in Egypt. Vaccine. (2022) 11:7. doi: 10.3390/vaccines11010007
42. Yan, Y, Bayham, J, Richter, A, and Fenichel, EP. Risk compensation and face mask mandates during the COVID-19 pandemic. Sci Rep. (2021) 11:3174. doi: 10.1038/s41598-021-82574-w
43. Wadud, Z, Rahman, SM, and Enam, A. Face mask mandates and risk compensation: an analysis of mobility data during the COVID-19 pandemic in Bangladesh. BMJ Glob Health. (2022) 7:e006803. doi: 10.1136/bmjgh-2021-006803
44. Meleady, R, and Hodson, G. Reductions in perceived COVID-19 threat amid UK’S mass public vaccination programme coincide with reductions in outgroup avoidance (but not prejudice). Br J Soc Psychol. (2022) 61:1286–304. doi: 10.1111/bjso.12537
45. Wu, J, Li, Q, Silver Tarimo, C, Wang, M, Gu, J, Wei, W, et al. COVID-19 vaccine hesitancy among Chinese population: a large-scale national study. Front Immunol. (2021) 12:781161. doi: 10.3389/fimmu.2021.781161
46. Wang, J, Lu, X, Lai, X, Lyu, Y, Zhang, H, Fenghuang, Y, et al. The changing acceptance of COVID-19 vaccination in different epidemic phases in China: a longitudinal study. Vaccines. (2021) 9:191. doi: 10.3390/vaccines9030191
47. Li, L, Jing, R, Guo, J, Song, Y, Geng, S, Wang, J, et al. The associations of geographic location and perceived risk of infection with the intentions to get vaccinated against COVID-19 in China. Expert Rev Vaccines. (2021) 20:1351–60. doi: 10.1080/14760584.2021.1969917
48. Atkinson, M, Neville, F, Ntontis, E, and Reicher, S. Social identification and risk dynamics: how perceptions of (inter) personal and collective risk impact the adoption of COVID-19 preventative behaviors. Risk Anal. (2024) 44:322–32. doi: 10.1111/risa.14155
49. Lam, CN, Kumar, N, Herzig, SE, Unger, JB, and Sood, N. Associations between COVID-19 infection, symptom severity, perceived susceptibility, and long-term adherence to protective behaviors: the Los Angeles pandemic surveillance cohort study. PLoS One. (2025) 20:e0326097. doi: 10.1371/journal.pone.0326097
Keywords: COVID-19, risk perception, adherence, preventive behaviors, systematic review, meta-analysis
Citation: Sorrentino M, Fiorilla C, Rubba F, Montuori P and Palladino R (2025) Does COVID-19 vaccination affect risk perception and adherence to preventive behaviors? A systematic review and meta-analysis. Front. Public Health. 13:1661015. doi: 10.3389/fpubh.2025.1661015
Edited by:
Sunjoo Kang, Yonsei University, Republic of KoreaReviewed by:
Vasuki Rajaguru, Yonsei University Health System, Republic of KoreaPutri Winda Lestari, Universitas Binawan, Indonesia
Mei Yang, The Third People’s Hospital of Chengdu, China
Copyright © 2025 Sorrentino, Fiorilla, Rubba, Montuori and Palladino. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michele Sorrentino, bWljaGVsZS5zb3JyZW50aW5vQHVuaW5hLml0
 Michele Sorrentino
Michele Sorrentino Claudio Fiorilla
Claudio Fiorilla Fabiana Rubba
Fabiana Rubba Paolo Montuori
Paolo Montuori Raffaele Palladino
Raffaele Palladino