- 1Department of Cardiological, Thoracic and Vascular Sciences and Public Health, University of Padova, Padova, Italy
- 2Department of Statistical Sciences, University of Padova, Padova, Italy
Background: Life satisfaction and quality of life are essential indicators of wellbeing in older adults. Social capital has been increasingly recognized as a key factor influencing these outcomes. This study systematically reviewed and synthesized existing evidence on the association between social capital and quality of life and life satisfaction among older adults through a systematic review and meta-analysis.
Methods: A comprehensive literature search was performed in MEDLINE (via PubMed), PsycINFO, and CINAHL (via EBSCO) from inception to January 15, 2025. Observational studies reporting quantitative associations between social capital and quality of life and life satisfaction in adults aged ≥60 years were included. Unadjusted effect sizes (r) were pooled using random-effects models for meta-analysis to account for variability across studies. Subgroup meta-analyses were conducted to examine differences based on publication period, geographic location, and quality of life measures. Between-study heterogeneity was tested using the I2 index, and publication bias was investigated using funnel plots, Egger's test, and Begg's test.
Results: We identified 13 studies that included 5,880 older participants from seven countries. Meta-analyses revealed life satisfaction (r = 0.25, 95% CI: 0.20–0.31) and quality of life (r = 0.35, 95% CI: 0.19–0.49) all demonstrated significant associations with social capital. The overall pooled effect size (r = 0.27, 95% CI: 0.22–0.32) demonstrated a consistent positive relationship. Subgroup analyses showed that cognitive social capital (r = 0.35, 95% CI: 0.18–0.49) had a stronger association than structural social capital (r = 0.24, 95% CI: 0.19–0.29). Regional differences were not statistically significant (p = 0.182), although the effect sizes varied across continents: America (r = 0.24, 95% CI: 0.16–0.32), and Asia (r = 0.30, 95% CI: 0.23–0.37). Statistical heterogeneity was observed across meta-analyses (I2 = 68.9–95.5%). Publication bias was not significant based on Egger's and Begg's tests.
Conclusions: The findings of this meta-analysis suggest that social capital, particularly its cognitive dimension, plays an important role in enhancing quality of life and life satisfaction outcomes, with differences across time and geographic regions.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD42025638236, identifier: CRD42025638236.
Introduction
Population aging is rapidly reshaping global demographics, emerging as one of the major trends of the 21st century. Individuals worldwide are experiencing longer lifespans with most expecting to live into their mid-sixties and beyond (1). Countries across all income levels are reporting growth in both the number and percentage of older adults in their populations (2). The population of individuals aged 60 or older is projected to rise from 1 billion in 2020 to 1.4 billion by 2030, representing approximately one in every six adults. By 2050, the number of older adults is projected to double to 2.1 billion, while those aged 80 and above are forecasted to triple, reaching 426 million (2). Population aging first emerged in high-income countries, like Japan, where around 28% of the population is above 65. According to WHO report (2), over 66% of people aged 60 and older will be living in these regions by 2050. However, the most significant changes are now occurring in low- and middle-income countries (3). These demographic shifts are creating complex challenges for communities globally, involving healthcare and caregiving, regardless of a nation's cultural, economic, or political structure (4). Rising life expectancy poses challenges for healthy aging, increasing vulnerability among older adults. A strong community social environment enhances healthy aging by reinforcing social capital.
Social capital, defined by the networks, relationships, social norms, and social trust that facilitate collective action and collaboration, is of considerable significance for an aging population (5). People with strong social connections have improved physical and mental health, including lower risk of depression, loneliness, and cognitive decline, and better quality of life (5–7). Social connections motivate older people to actively participate in their communities and lead healthy lifestyles because they provide a sense of purpose and belonging (8). Individuals who feel supported by their relationships, such as family, friends, and community members are more likely to maintain good mental health, cope effectively with challenges, and experience overall life satisfaction (9). Generally, social capital can be classified as structural social capital, that is, the observable features of social networks that is, belonging to organizations and community groups, or cognitive social capital, the composite of trust, reciprocity, and shared values (10). Structural social capital provides pathways to essential resources, medical care, and community involvement, while cognitive social capital strengthens emotional resilience and interpersonal trust (10). More broadly, social capital is thought to provide a better quality of life and resilience in older adults; therefore, the need for building social networks in communities dealing with an aging population is imperative (11). However, existing studies show inconsistent results due to variations in context, measurement of social capital, and study design. Recent research indicates that there are typically higher levels of quality of life among older adults who are socially engaged, trust people, and have network support, but results are mixed across different socioeconomic, cultural, or health contexts (12–14). While there is an increasing interest in these community forces, the existing literature still has not fully presented overview on the current state of quality of life of aged population nor incorporated a range of academic perspectives. This meta-analysis addresses these gaps by providing a comprehensive and quantitative synthesis of the association between social capital and quality of life in older adults. This review aims to synthesize global evidence on the association between social capital (structural and cognitive) and quality of life and life satisfaction among older adults.
Methods
The review protocol was preregistered in the International Prospective Register of Systematic Reviews (PROSPERO; CRD42025638236) to ensure transparency and minimize reporting bias. The review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (15) for evidence identification, screening, and synthesis (see in Supplementary Table S2).
Search strategy
A thorough search was carried out across three major databases: Medline (PubMed), CINAHL, and PsycINFO, from their inception up to January 15, 2025. Search terms combined concepts related to older adults, social capital, and outcomes of interest. Boolean operators were applied to refine the strategy. The specific search strings utilized are provided in Supplementary Table S1. Upon retrieval, the records were imported into Zotero software (version 7) for management, where duplicates were systematically detected and eliminated. Additionally, the reference lists of the selected studies were scrutinized to detect any potentially relevant articles that might have been missed in the primary database screening.
Inclusion criteria
Articles were included if they met all of the following criterias:
1. Participants were aged 60 years or older.
2. The study employed an observational design (cross-sectional, cohort, or case-control).
3. The article was written in English.
4. The study investigated quantitatively the association between social capital and quality of life or life satisfaction among older populations.
Exclusion criteria
Articles were excluded if they met any of the following criteria:
1. Publications such as literature reviews, meta-analyses, case reports, editorials, commentaries, theses, or book chapters.
2. Studies that involved only patients with specific medical conditions.
Data extraction
Data extraction was performed utilizing a customized Microsoft Excel spreadsheet developed in line with the aims of our review. Two authors independently extracted key study characteristics, including the first author's surname, year of publication, survey year and country of origin, participant demographics, such as age range, mean age, gender distribution, sample size, and effect sizes, specifically indicators of social capital and quality of life metrics. Discrepancies were addressed through discussion between two authors (S.A and A.B.).
Risk of bias assessment
The risk of bias in the included studies was evaluated using the modified Newcastle-Ottawa Scale (NOS) for observational studies (16). Two authors (S.A. and A.B.) independently performed the risk of bias assessment. Examining three important domains—participant selection, comparability, and outcome evaluation, the scale offers a methodical structure. Studies were graded as low (≥8 points), moderate (5–7 points), or high (< 5 points) risk of bias (16). Discrepancies between the authors were resolved through consensus to settle differences in ratings.
Data synthesis
All statistical analyses were performed using R, version 4.4.2 (RStudio) with the support of the “meta” package (version 8.1-0) and “metafor” package (version 4.8-0). A random-effects meta-analysis was utilized to pool the effect sizes across studies, thus assuring the results are generalizable to a wider population. For the meta-analysis, we selected the Pearson r correlation coefficient as the effect size to represent the association between social capital and quality of life and life satisfaction. All outcomes were transformed into Fisher z values and subsequently converted back to their original scale for reporting the pooled results (17). The outcome measurement was the correlation coefficient (r), with 95% confidence intervals displayed in a forest plot. Pooled effect sizes were characterized according to the McGrath and Meyer (18) framework as high (r ≥ 0.37), moderate (0.10 < r < 0.37), or weak (r ≤ 0.10). Study heterogeneity was quantified using I2 values and tested for statistical significance with Cochran's Q test (19). A funnel plot offered a preliminary qualitative evaluation, whereas quantitative analyses, such as the Begg's and Egger's tests (20, 21) were employed to measure potential bias. Subgroup meta-analyses were performed to investigate variations in effect sizes based on key categorical variables. The parameters included components of social capital (structural and cognitive), publication timeframes (before 2015 and from 2015 onward), and geographic locations (America and Asia). Univariable meta-regression analyses were performed to investigate the impact of possible continuous mediators on the observed heterogeneity across studies. The mediators comprised mean age, methodological quality, survey year, publication year, male proportion, and sample size. R2 values were computed to measure the extent of heterogeneity explained by the incorporated modifiers. The robustness of our findings was tested through sensitivity analyses, where each study was systematically excluded, and the pooled effect size was recomputed (22). The findings were deemed statistically significant at p < 0.05. All significance tests were two-sided.
Results
A total of 2,341 records (Figure 1) were identified (PubMed: 1,685; CINAHL: 294; PsycINFO: 359; manual literature search: three). After removing 389 duplicates and one retracted article, 1,951 records remained for screening. Of these, 1,834 were excluded based on titles and abstracts, leaving 117 full-text reports for review. Six could not be retrieved, and 98 were excluded for various reasons (irrelevance, age < 60, missing data, or duplication). Ultimately, 13 studies met the inclusion criteria and were included in the review and meta-analysis.
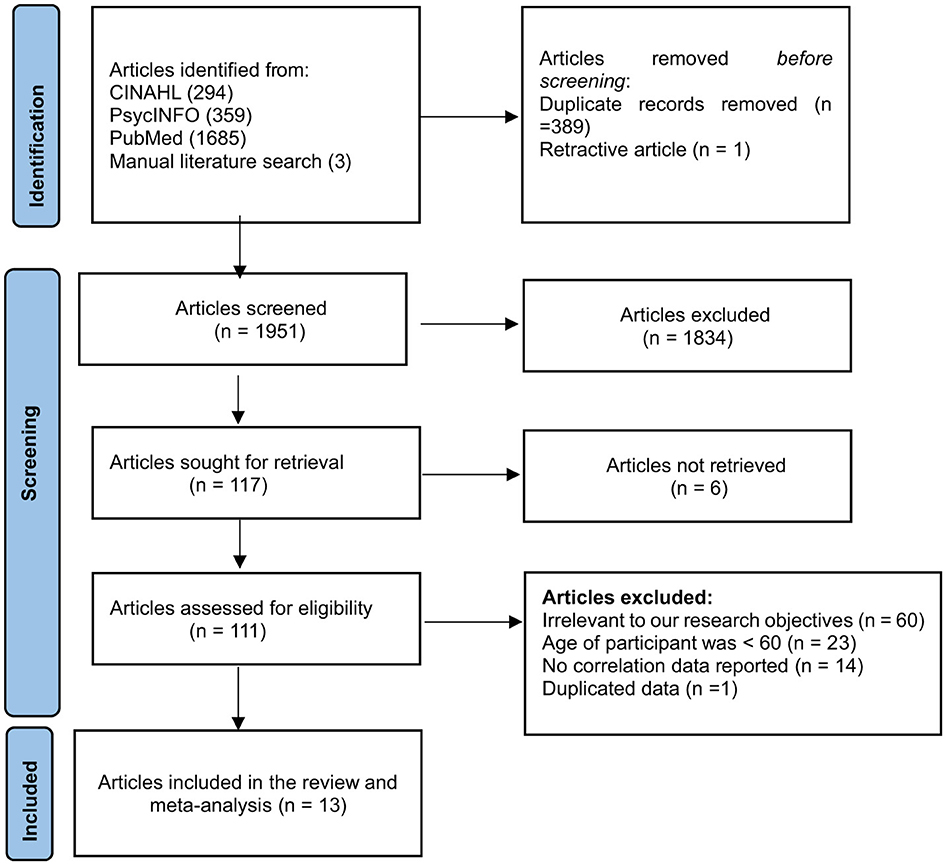
Figure 1. Study selection (PRISMA) flowchart of the association between social capital and quality of life.
Study characteristics
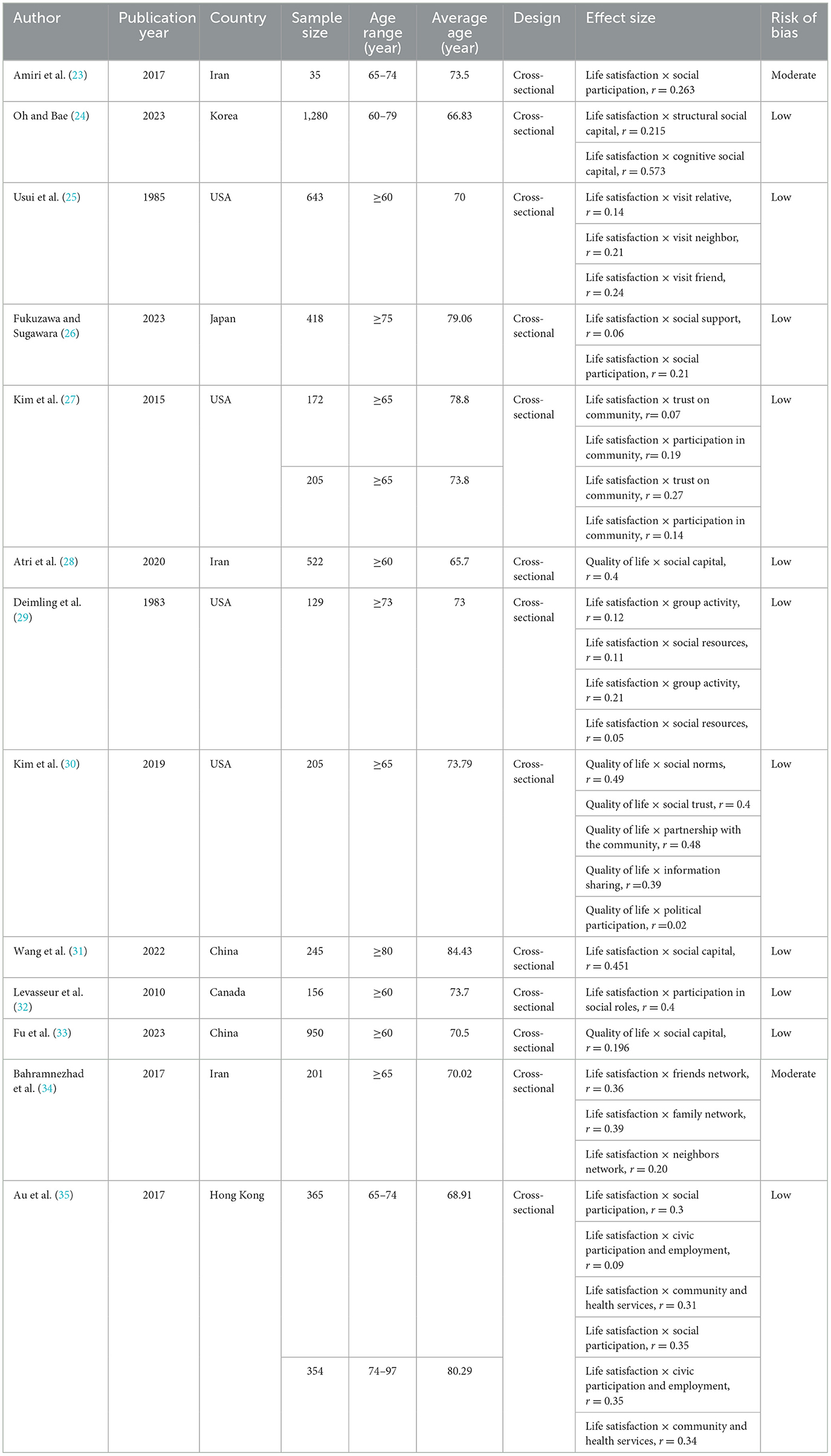
A detailed overview of key study characteristics is provided in Table 1. The sample comprised 13 studies (23–35), all published between 1983 (29) and 2023 (24), with a significant portion published recently (77% of the research studies were published after 2010). Sample sizes ranged from 35 (23) to 1,280 (24) participants. The average weighted age of the samples in the review was 73.4 years. Seven effect sizes focused on the association of social capital with quality of life, while 27 focused on life satisfaction. In the included studies, a variety of indicators were used to measure social capital. These indicators encompassed both interpersonal and community-level constructs such as social support, trust in the community, social norms, participation in community activities, and civic engagement. To enable comparability across studies, we classified these diverse measures into two overarching domains: cognitive social capital (24%) and structural social capital (71%). Cognitive social capital consists of several elements, including perceived trust, social support, and shared norms. Structural social capital incorporates observable behaviors and interactions, such as social participation, network ties, group activities, and participation in civic or political activities. Four (31%) studies were conducted in the USA, 3 (23%) in Iran, 2 (15%) in China while one (7%) each in Canada, Hong Kong, South Korea, and Japan. The risk of bias analysis based on NOS indicated that 12 (92%) studies were classified as having a low risk of bias, while 1 (8%) study exhibited a moderate risk of bias. The comprehensive evaluation findings are displayed in Supplementary Table S2.
Meta-analysis
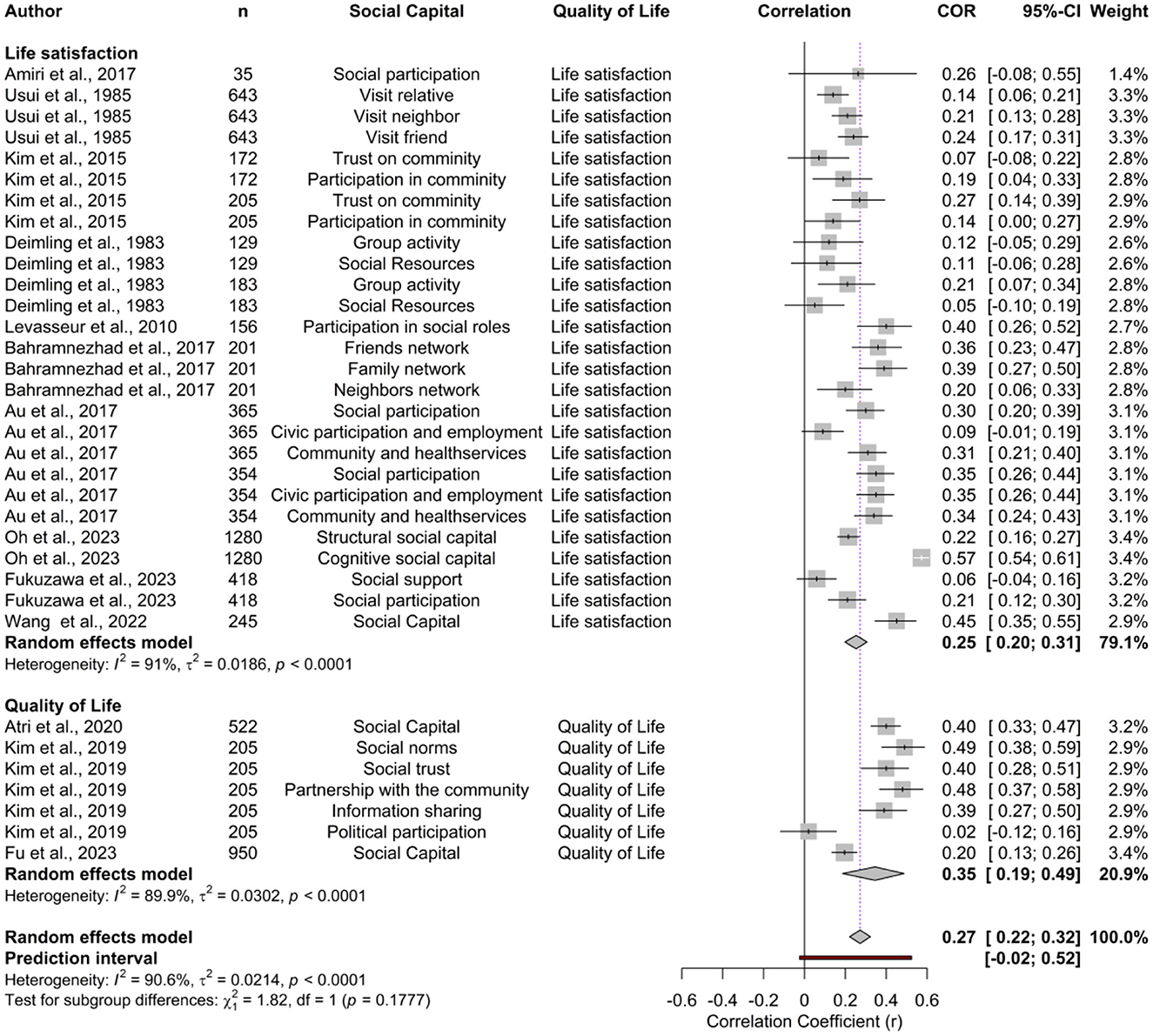
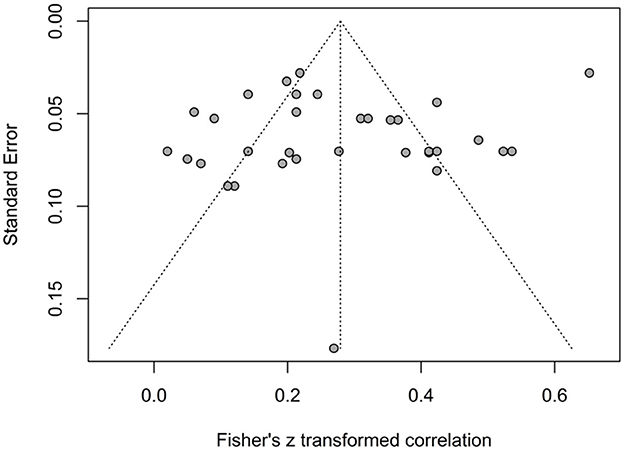
The correlation coefficient estimates reported by the individual studies ranged from 0.02 (95% CI: −0.12 to 0.16) to 0.57 (95% CI: 0.54–0.61). The forest plot illustrating the effect sizes for social capital and quality of life and life satisfaction is presented in Figure 2. Using a random-effects model, the overall pooled correlation across all studies was r = 0.27 (95% CI: 0.22–0.32 p < 0.001), reflecting a consistent positive association between social capital and quality of life in older adults. The prediction interval ranged from −0.02 to 0.52, suggesting that while most future studies are expected to find a positive association. Substantial heterogeneity was observed (Q = 350.61, τ2 = 0.0214, I2 = 90.6%, p < 0.001), indicating considerable variability across studies. The symmetrical distribution of points in the funnel plot (Figure 3), Egger test (t = −0.98, p-value = 0.3325) and Begg and Mazumdar test (z = 0.43, p-value = 0.6650) revealed no evidence of publication bias.
Subgroup analyses
The subgroup meta-analyses are presented in Table 2. When stratified by the dimensions of social capital, cognitive social capital demonstrated a stronger association with quality of life, with a pooled effect size of 0.35 (95% CI: 0.18–0.49; I2 = 95.3) compared to structural social capital, which had a pooled effect size of 0.24 (95% CI: 0.19–0.29; I2 = 79.2), though the difference was not statistically significant (p = 0.1513). This suggests that factors such as trust, reciprocity, and perceived support may play a more important role in enhancing quality of life than structural elements like participation in organizations.
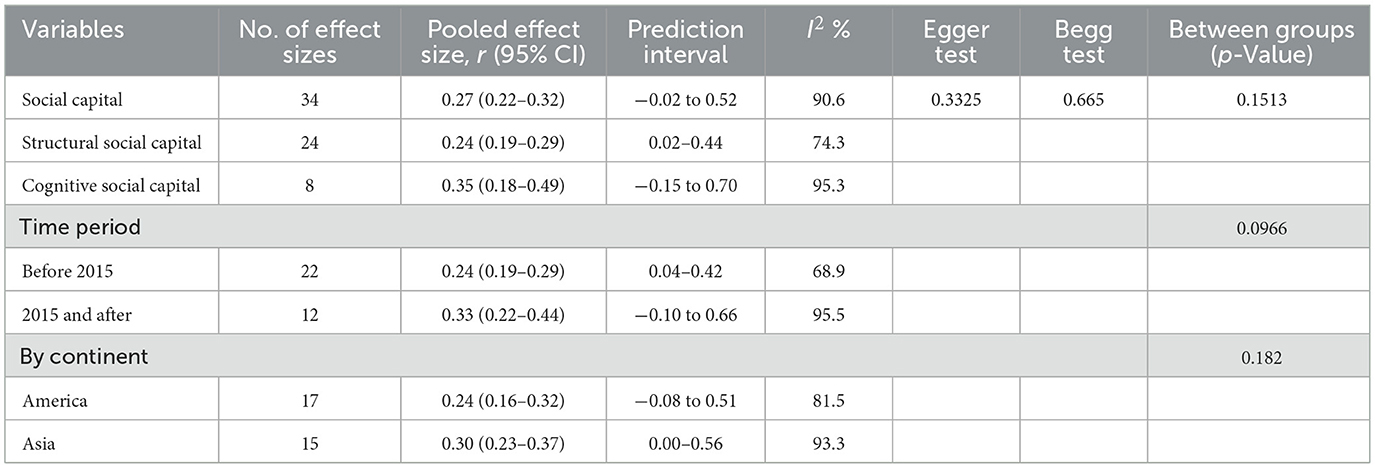
Table 2. Summary of subgroup analysis pooled effect sizes of the association between social capital and quality of life.
In terms of quality-of-life measures, the pooled effect sizes were relatively consistent across life satisfaction and overall quality of life, with values of 0.25 (95% CI: 0.20–0.31; I2 = 91.0), and 0.35 (95% CI: 0.19–0.49; I2 = 89.9), respectively. Despite high heterogeneity, no significant differences were observed between these subgroups (p = 0.1777). This pooled correlation measure indicates that the beneficial impact of social capital is not limited to one specific outcome but applies broadly to older adults' perceived quality of life. When analyzed by time periods, studies published before 2015 reported a pooled effect size of 0.24 (95% CI: 0.19–0.29; I2 = 68.9), whereas those published in 2015 and after showed a stronger pooled effect size of 0.33 (95% CI: 0.22–0.44; I2 = 95.5). Furthermore, regional analysis revealed that studies from Asia exhibited a marginally greater pooled effect size (0.33, 95% CI: 0.23–0.37; I2 = 93.3) than studies from America (0.24, 95% CI: 0.16–0.32; I2 = 93.3), though the difference was again not statistically significant (p = 0.182). Although heterogeneity was high in the magnitude of the association across most subgroups (I2 > 70%), the overall direction of results was consistent: higher social capital is reliably associated with better quality of life among older adults, even if the strength of the association varies across contexts.
Sensitivity analysis
The leave-one-out sensitivity analysis illustrated evaluated the robustness of the random-effects meta-analysis. The results demonstrated that eliminating any individual study did not significantly impact the overall pooled correlation coefficient. All pooled effect size values from omitting studies remained consistent within the range of 0.26 (95% CI: 0.21–0.31) to 0.28 (95% CI: 0.23–0.33). This analysis confirmed that the overall findings are stable and not unduly influenced by any single study, thereby reinforcing the robustness of the results.
Meta-regression
The effect of study characteristics on the association between social capital and quality of life among older adults was investigated in a meta-regression analysis. The results showed that the year of publication (β = 0.0044, p = 0.0203) was a significant predictor suggesting that more recent research reported a somewhat larger impact of social capital on quality of life. This trend explained 13.79% of the between-study variability, indicating that time contributes to differences in effect sizes. However, factors including sample size, male ratio, and risk of bias evaluation exhibited no significant effect on the pooled effect size.
Discussion
Our meta-analysis suggests that social capital is positively associated with quality of life and life satisfaction. Despite high variability, the consistent findings across different measures could suggest that promoting social capital could be an effective strategy for enhancing seniors' quality of life and life satisfaction. The findings will significantly influence public health programs and policies intended to improve the quality of life for aging adults across the globe. This aligns with previous studies highlighting the importance of relationships and community ties for wellbeing and quality of life (36, 37), as well as studies evaluating the effects of social prescribing interventions.
However, subgroup analysis showed cognitive social capital had a greater association than structural social capital, emphasizing the stronger influence of cognitive social dimensions (i.e., trust, reciprocity, shared values) than structural elements (i.e., network size). Our results are similar to a study conducted in Germany (38). Ferlander (36) similarly studied a sample in Sweden and found that cognitive social capital has a greater and consistent association than structural ties, to quality of life and happiness. Cognitive social capital reflects trust, belonging, and mutual support that directly enhances quality of life, while structural social capital refers to external networks that may not always bring real benefits (37). These findings suggest that prioritizing emotional and trust-based approaches to improve life satisfaction can be beneficial for old adults. These results imply that interventions should address the more emotional and psychological aspects of relationships that produce larger meaningful improvements in quality of life for older adults (e.g., programs addressing community trust). From a practical perspective, this means that interventions should not only encourage participation in groups but also strengthen feelings of trust, reciprocity, and belonging. Programs that focus on building safe and supportive community environments may therefore be more impactful than those that only expand social networks.
When considering specific outcomes, the association of social capital with quality of life appeared somewhat stronger (r = 0.35) than with life satisfaction (r = 0.25). Although this difference was not statistically significant, the trend suggests that social capital may influence broader assessments of wellbeing more strongly than evaluations of life satisfaction alone. One possible explanation is that quality of life measures typically captures multiple domains such as physical, psychological, and social functioning, where social capital can exert cumulative effects (39, 40). In contrast, life satisfaction reflects a more global judgment, which may be influenced by additional factors beyond health, psychology, or functioning status (41–43). These findings indicate that while social capital benefits both subjective and multidimensional wellbeing in older adults, its impact may be particularly pronounced in domains encompassed by quality of life assessments (37, 44).
Interestingly, studies published after 2015 had a stronger association between social capital and quality of life than studies published before 2015. This may reflect a growing awareness of social capital's relevance to aging populations, as well as improvements in measurement techniques over time (45–48). However, also changes in family relationships across cohorts now entering older ages may result in changes in risks of needing to provide care for others, widening gaps in the necessity of social support (49).
Limitations
This meta-analysis has some limitations. Therefore, the findings of this study need to be interpreted with caution. A main limitation of the current meta-analysis is the high degree of heterogeneity across the published literature. Significant heterogeneity could be attributed to variations in study participants, study methodology, outcome assessment, or cultural context and can adversely affect the pooled effect size, thereby impacting the validity of the results. To overcome the heterogeneity problem, we used random effect meta-analyses models. Nonetheless, statistical analyses (20, 21), along with funnel plot assessments, indicated that there was no significant publication bias, which should strengthen the reliability of the current results. Second, the current meta-analysis only included peer-reviewed literature in English, which raises the possibility of selection bias due to the exclusion of valuable information from sources not in English or the gray literature. Third, we only used unadjusted measures of association (simple correlations) to limit causal inference, as these measures do not account for possible confounding variables that might mediate or confound the association. However, we performed a sensitivity analysis and detected no substantial fluctuation in the results, which supports the robustness of the findings.
Conclusions
This meta-analysis demonstrates that higher levels of social capital are consistently associated with improved life satisfaction and quality of life in older adults. Cognitive social capital, encompassing trust, reciprocity, and shared values, emerged as a stronger predictor of wellbeing than structural social capital, such as network size or organizational participation. These findings suggest that interventions and policies should prioritize the quality of social relationships and trust-building efforts, rather than focusing solely on increasing the number of social ties.
At the same time, the substantial heterogeneity observed across studies reduces the certainty of the pooled estimates, highlighting the need for cautious interpretation. Future research should therefore aim to develop standardized tools for assessing social capital, conduct longitudinal studies to clarify causal mechanisms, and extend investigations to low- and middle-income countries, where evidence is scarce. Such steps would enhance comparability across studies and provide a stronger evidence base to guide effective interventions and policies for promoting healthy aging.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
AB: Data curation, Validation, Supervision, Writing – review & editing, Methodology, Conceptualization, Funding acquisition, Writing – original draft, Resources. SA: Data curation, Formal analysis, Methodology, Conceptualization, Software, Investigation, Writing – original draft, Writing – review & editing, Visualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Open Access funding provided by Università degli Studi di Padova | University of Padua, Open Science Committee.
Acknowledgments
This paper was developed within the project funded by Next Generation EU—the “Age-It—Ageing well in an ageing society” project (PE0000015), National Recovery and Resilience Plan (NRRP)—PE8—Mission 4, C2, Intervention 1.3. The views and opinions expressed are only those of the authors and do not necessarily reflect those of the European Union or the European Commission. Neither the European Union nor the European Commission can be held responsible for them.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1668696/full#supplementary-material
References
1. Department of Economic and Social Affairs. World Population Ageing 2023: Challenges and Opportunities of Population Ageing in the Least Developed Countries. New York: United Nations (2024). Available online at: https://discovery.csiro.au/discovery/fulldisplay?docid=cdi_proquest_ebookcentral_EBC31209917.
2. World Health Organization. Decade of Healthy Ageing: Baseline Report. Geneva: WHO (2021). Available online at: https://www.who.int/publications/i/item/9789240017900.
3. Statistics Bureau of Japan. Population Estimates, 2023. Tokyo: SBJ (2023). Available online at: https://www.prb.org/resources/countries-with-the-oldest-populations-in-the-world/.
4. Rony MKK, Parvin MR, Wahiduzzaman M, Akter K, Ullah M. Challenges and advancements in the health-related quality of life of older people. Adv Public Health. (2024) 2024:1–18. doi: 10.1155/2024/8839631
5. Bai Z, Wang Z, Shao T, Qin X, Hu Z. Association between social capital and loneliness among older adults: a cross-sectional study in Anhui Province, China. BMC Geriatr. (2021) 21:595. doi: 10.1186/s12877-020-01973-2
6. Saeri AK, Cruwys T, Barlow FK, Stronge S, Sibley CG. Social connectedness improves public mental health: investigating bidirectional relationships in the New Zealand attitudes and values survey. Aust N Z J Psychiatry. (2018) 52:365–74. doi: 10.1177/0004867417723990
7. Holt-Lunstad J. Social connection as a critical factor for mental and physical health: evidence, trends, challenges, and future implications. World Psychiatry. (2024) 23:312–32. doi: 10.1002/wps.21224
8. AshaRani P, Lai D, Koh J, Subramaniam M. Purpose in life in older adults: a systematic review on conceptualization, measures, and determinants. Int J Environ Res Public Health. (2022) 19:5860. doi: 10.3390/ijerph19105860
9. Thoits PA. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav. (2011) 52:145–61. doi: 10.1177/0022146510395592
10. Bhandari H, Yasunobu K. What is social capital? A comprehensive review of the concept. Asian J Soc Sci. (2009) 37:480–510. doi: 10.1163/156853109X436847
11. Cannuscio C, Block J, Kawachi I. Social capital and successful aging: the role of senior housing. Ann Intern Med. (2003) 139:395–9. doi: 10.7326/0003-4819-139-5_Part_2-200309021-00003
12. Ehsan AM, Klaas HS, Bastianen A, Spini D. Social support and social participation as determinants of quality of life in older Europeans: a longitudinal study. SSM Pop Health. (2021) 13:100746. doi: 10.1016/j.ssmph.2021.100747
13. Giezendanner S, Krones T, Schmid M, Camenzind B, Rubli Truchard E, Jäger C, et al. Factors associated with health-related quality of life among home-dwelling older adults aged 75 or older in Switzerland. Health Qual Life Outcomes. (2022) 20:56. doi: 10.1186/s12955-022-02080-z
14. Zhang C, Liu M, Li Y, Wang Y. Enjoying the golden years: social participation and life satisfaction among Chinese older adults. Front Public Health. (2024) 12:1381707. doi: 10.3389/fpubh.2024.1377869
15. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
16. Vivekanantham A, Edwin C, Pincus T, Matharu M, Parsons H, Underwood M. The association between headache and low back pain: a systematic review. J Headache Pain. (2019) 20:82. doi: 10.1186/s10194-019-1031-y
17. Higgins JPT. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
18. McGrath RE, Meyer GJ. When effect sizes disagree: the case of r and d. Psychol Methods. (2006) 11:386–401. doi: 10.1037/1082-989X.11.4.386
19. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis. Chichester: Wiley (2009). doi: 10.1002/9780470743386
20. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 50:1088–101. doi: 10.2307/2533446
21. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
22. Wallace BC, Schmid CH, Lau J, Trikalinos TA. Meta-analyst: software for meta-analysis of binary, continuous and diagnostic data. BMC Med Res Methodol. (2009) 9:80. doi: 10.1186/1471-2288-9-80
23. Amiri E, Khiavi FF, Dargahi H, Dastjerd E. Retirement homes: social participation and quality of life. Electron Physician. (2017) 9:4108–13. doi: 10.19082/4108
24. Oh E, Bae S. The relationship between personality, social capital, and life satisfaction of elderly Koreans. Psychogeriatrics. (2023) 23:494–502. doi: 10.1111/psyg.12960
25. Usui WM, Keil TJ, Durig KR. Socioeconomic comparisons and life satisfaction of elderly adults. J Gerontol. (1985) 40:110–4. doi: 10.1093/geronj/40.1.110
26. Fukuzawa A, Sugawara I. Social support and participation as factors relating to Ikigai and life satisfaction in lonely older Japanese. Ageing Int. (2023) 48:465–81. doi: 10.1007/s12126-022-09486-6
27. Kim BJ, Linton KF, Lum W. Social capital and life satisfaction among Chinese and Korean elderly immigrants. J Soc Work. (2015) 15:87–100. doi: 10.1177/1468017313504699
28. Atri SB, Pakpour V, Khalili AF, Jafarabadi MA, Kharajo ZN. Social capital and its predictive role in quality of life among the elderly referring to health centers in Tabriz, Iran: a community-based study. J Caring Sci. (2020) 9:212–7. doi: 10.34172/jcs.2020.032
29. Deimling G, Harel Z, Noelker L. Racial differences in social integration and life satisfaction among aged public housing residents. Int J Aging Hum Dev. (1983) 17:203–12. doi: 10.2190/4QHN-EKBF-N7L0-9UD3
30. Kim BJ, Chen L, Lee Y, Xu L. Quality of life of elderly Chinese immigrants: focusing on living arrangements and social capital. Educ Gerontol. (2019) 45:377–89. doi: 10.1080/03601277.2019.1640973
31. Wang X, Wang P, Wang P, Cao M, Xu X. Relationships among mental health, social capital and life satisfaction in rural senior older adults: a structural equation model. BMC Geriatr. (2022) 22:782. doi: 10.1186/s12877-022-02761-w
32. Levasseur M, Desrosiers J, Whiteneck G. Accomplishment level and satisfaction with social participation of older adults: association with quality of life and best correlates. Qual Life Res. (2010) 19:665–75. doi: 10.1007/s11136-010-9633-5
33. Fu Y, Zhang S, Guo X, Lu Z, Sun X. Socioeconomic status and quality of life among older adults with hypertension in rural Shandong, China: a mediating effect of social capital. Front Public Health. (2023) 11:1248291. doi: 10.3389/fpubh.2023.1248291
34. Bahramnezhad F, Chalik R, Bastani F, Taherpour M, Navab E. The social network among the elderly and its relationship with quality of life. Electron Physician. (2017) 9:4306–11. doi: 10.19082/4306
35. Au AML, Chan SCY, Yip HM, Kwok JYC, Lai KY, Leung KM, et al. Age-friendliness and life satisfaction of young-old and old-old in Hong Kong. Curr Gerontol Geriatr Res. (2017) 2017:6215917. doi: 10.1155/2017/6215917
36. Ferlander S. The importance of different forms of social capital for health. Acta Sociol. (2007) 50:115–28. doi: 10.1177/0001699307077654
37. Xu Z, Zhang W, Zhang X, Wang Y, Chen Q, Gao B, et al. Multi-level social capital and subjective wellbeing among the elderly: understanding the effect of family, workplace, community, and society social capital. Front Public Health. (2022) 10:772601. doi: 10.3389/fpubh.2022.772601
38. Adedeji A, Silva N, Bullinger M. Cognitive and structural social capital as predictors of quality of life for sub-Saharan African migrants in Germany. Appl Res Qual Life. (2021) 16:1003–17. doi: 10.1007/s11482-019-09784-3
39. Pinquart M, Sörensen S. Influences of socioeconomic status, social network, and competence on subjective well-being in later life: a meta-analysis. Psychol Aging. (2000) 15:187–224. doi: 10.1037//0882-7974.15.2.187
40. Webber MP, Huxley PJ, Harris T. Social capital and the course of depression: six-month prospective cohort study. J Affect Disord. (2011) 129:149–57. doi: 10.1016/j.jad.2010.08.005
41. Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess. (1985) 49:71–5. doi: 10.1207/s15327752jpa4901_13
42. George LK. Still happy after all these years: research frontiers on subjective well-being in later life. J Gerontol B Psychol Sci Soc Sci. (2010) 65B:331–9. doi: 10.1093/geronb/gbq006
43. Nyqvist F, Forsman AK, Giuntoli G, Cattan M. Social capital as a resource for mental well-being in older people: a systematic review. Aging Ment Health. (2013) 17:394–410. doi: 10.1080/13607863.2012.742490
44. Coll-Planas L, Nyqvist F, Puig T, Urrútia G, Solà I, Monteserín R. Social capital interventions targeting older people and their impact on health: a systematic review. J Epidemiol Community Health. (2017) 71:663–72. doi: 10.1136/jech-2016-208131
45. Ehsan A, Klaas HS, Bastianen A, Spini D. Social capital and health: a systematic review of systematic reviews. SSM Pop Health. (2019) 8:100425. doi: 10.1016/j.ssmph.2019.100425
46. Nascimento P, Roberto MS, Santos AS. (2021). Validation of the personal social capital scale-16 in Portugal: preliminary data on Portuguese and immigrants. Health Promot. Int. 36:1705–15. doi: 10.1093/heapro/daab022
47. Zhang W, Jiang Y, Wang L, Wang S, Wang F. Relationship between social capital and quality of life among adult stroke patients: a cross-sectional study in Anhui, China. Health Qual Life Outcomes. (2022) 20:90. doi: 10.1186/s12955-022-01925-x
48. World Health Organization. Child, Early and Forced Marriage Legislation in 37 Asia-Pacific Countries. Geneva WHO (2016). Available online at: https://iris.who.int/items/14e71ada-611c-4442-b8e0-c195e421143e.
Keywords: social capital, quality of life, older adults, systematic review, meta-analysis
Citation: Buja A and Akhtar S (2025) The association between social capital and quality of life in old adults: a systematic review and meta-analysis. Front. Public Health 13:1668696. doi: 10.3389/fpubh.2025.1668696
Received: 18 July 2025; Accepted: 09 October 2025;
Published: 06 November 2025.
Edited by:
Marcia G. Ory, Texas A&M University, United StatesReviewed by:
Ramkrishna Mondal, All India Institute of Medical Sciences (Patna), IndiaXue Zhou, Mudanjiang Medical University, China
Copyright © 2025 Buja and Akhtar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sohail Akhtar, U29oYWlsLmFraHRhckB1bmlwZC5pdA==
 Alessandra Buja
Alessandra Buja Sohail Akhtar
Sohail Akhtar