- 1School of Physical Education, China University of Mining and Technology, Xuzhou, Jiangsu, China
- 2School of Physical Education and Coaching Science, Capital University of Physical Education and Sports, Beijing, China
- 3Department of Physical Education, Tianjin Medical University, Tianjin, China
Background: As a behavioral addiction, internet addiction disorder has become a global problem that seriously affects people’s mental health. Although physical and mental exercise is believed to help alleviate related symptoms, there is currently a lack of systematic research evaluating the intervention effects of different physical and mental exercises on internet addiction disorder.
Objective: To systematically evaluate the effects of different physical and mental exercise modes and amounts on the alleviation of symptoms of internet addiction.
Method: Randomized controlled trials (RCTs) on the effects of different physical and mental exercise modes on internet addiction published between October 2000 and February 2025 were retrieved through PubMed, Web of Science, EBSCO, Cochrane Library, and CNKI systems. After independently screening literature, extracting data, and evaluating the risk of bias in the included studies by two independent researchers, a random effects model was used for meta-analysis using RevMan 5.4 and Stata 19.0 software. Perform dose-response analysis using R software.
Results: Twenty-four randomized controlled trials involving 1,711 participants were included. Compared with the control group, all physical and mental exercise methods significantly improved symptoms of internet addiction disorder (SMD = −1.63, 95% CI: −2.04, −1.22). Mindfulness meditation showed the strongest effect (SMD = −2.04, 95% CI: −3.23, −0.85). The study determined a non-linear U-shaped dose-response relationship, with the best effect occurring at 730 MET min/week.
Conclusion: This study provides theoretical support for non pharmacological interventions to improve symptoms of internet addiction disorder. For those who hope to improve their internet addiction through physical and mental exercise, mindfulness meditation is the first choice. In addition, controlling the exercise dose within the optimal range (e.g., 730 MET min/week) can significantly enhance the intervention effect.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD42025631096, CRD42025631096
Background
Internet Addiction Disorder (IAD) is a kind of behavioral addiction, which refers to a mental and behavioral disorder caused by uncontrolled Internet use. It usually shows clinical characteristics such as overuse, withdrawal symptoms, tolerance and negative effects (1). In 2013, internet gaming disorder, a subtype of IAD, was officially included for the first time by the American Psychiatric Association (APA) in the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders, Part 3, “List of Subjects for Further Research” (2). IAD affects approximately 14.22% of the global population, with significant regional variations (0.8–26.7%) (3). College students face particularly high risk due to two key factors: (1) developmental vulnerability—newfound internet freedom without fully matured self-regulation abilities, and (2) environmental pressures related to academics and social identity formation (4, 5). Research demonstrates that IAD severity positively correlates with the magnitude of adverse physical and mental health outcomes (6). As an emerging mental health issue, IAD has not yet formed a mature and complete treatment system. Most current treatments are adapted from approaches used for substance addictions, such as alcohol and drug dependencies (7).
Mind–body exercise represents a promising intervention approach for IAD, as these practices enhance self-regulation, stress management, and impulse control—all key factors in addiction recovery. Király et al. emphasized in the consensus guidelines on internet use during the COVID-19 pandemic that structured physical activity and psychosomatic interventions can help prevent and alleviate IAD symptoms (8). For prevention, Zhu et al. found that regular physical activity significantly reduces problematic gaming behavior, particularly among young adults (9). Similarly, Throuvala et al.’s systematic review indicates that school programs incorporating mindfulness and physical activity effectively prevent IAD in young adults, with high compliance and sustainability (10). For treatment applications, mind–body exercise shows promise for IAD intervention. However, two key limitations exist in current research: first, the lack of systematic comparison between different mind–body exercise methods prevents determination of optimal clinical interventions (11); second, insufficient quantitative research on dose-response relationships makes it difficult to establish optimal exercise prescriptions (including frequency, intensity, and duration) (12). These gaps limit evidence-based application and personalized prescription development of mind–body exercise as a non-pharmacological intervention for IAD.
In summary, to our knowledge, this study is among the first to systematically evaluate the differences in the effectiveness of seven mind–body exercise methods: Tai Chi, Baduanjin, DanceSports, Mindfulness, Aerobicdance, Yoga, and Qigong, in improving IAD symptoms. Through dose-response analysis, we quantify the optimal intervention parameters for IAD symptom improvement. This provides empirical basis for large-scale promotion of IAD intervention strategies and advances personalized, precise IAD treatment approaches.
Materials and methods
Registration
This investigation adhered to the Systematic Review and Meta-Analysis PRISMA reporting framework and received advance registration in the PROSPERO database under identification code CRD42025631096. This pre registration step ensures transparency of the method and compliance with standardized review practices.
Search strategy
Search protocols for identifying IAD and physical-mental exercise interventions were formulated utilizing Medical Subject Headings (MeSH) terminology combined with Boolean logic operators. The comprehensive retrieval methodology incorporated both standardized MeSH classifications and relevant keywords. Box 1 presents the detailed query structure implemented within the PubMed database platform.
BOX 1. PubMed search strategy.
#1 (“Mind”[Title/Abstract] OR “body exercise”[Title/Abstract] OR “Mind–body exercise”[Title/Abstract] OR “Taichi”[Title/Abstract] OR “Baduanjin”[Title/Abstract] OR “Mindfulness”[Title/Abstract] OR “Dance Sport”[Title/Abstract]) OR “Qigong”[Title/Abstract] OR “Yoga”[Title/Abstract] OR “Aerobicdance”[Title/Abstract] AND “Internet Addiction Disorder”[MeSH Terms]
#2 “Sports”[Title/Abstract] OR “Sport”[Title/Abstract] OR “Athletics”[Title/Abstract] OR “Athletic”[Title/Abstract]
#3 #1 OR #2
#4 “Internet Addiction Disorder”[Title/Abstract] OR “Addiction Disorder, Internet”[Title/Abstract] OR “Addiction Disorders, Internet”[Title/Abstract] OR “Disorder, Internet Addiction”[Title/Abstract] OR “Disorders, Internet Addiction”[Title/Abstract] OR “Internet Addiction Disorders”[Title/Abstract] OR “Internet Addiction”[Title/Abstract] OR “Addiction, Internet”[Title/Abstract] OR “Addictions, Internet”[Title/Abstract] OR “Internet Addictions”[Title/Abstract] OR “Internet Gaming Disorder”[Title/Abstract] OR “Disorder, Internet Gaming”[Title/Abstract] OR “Disorders, Internet Gaming”[Title/Abstract] OR “Gaming Disorder, Internet”[Title/Abstract] OR “Gaming Disorders, Internet”[Title/Abstract] OR “Internet Gaming Disorders[Title/Abstract] OR Smartphone Addiction[Title/Abstract] OR Addiction, Smartphone[Title/Abstract] OR Addictions, Smartphone[Title/Abstract] OR Smartphone Addictions[Title/Abstract] OR Social Media Addiction[Title/Abstract] OR Addiction, Social Media[Title/Abstract] OR Addictions, Social Media[Title/Abstract] OR Media Addiction, Social[Title/Abstract] OR Media Addictions, Social[Title/Abstract] OR Social Media Addictions[Title/Abstract]
#5 “randomized controlled trial”[Publication Type] OR “controlled clinical trial”[Publication Type]
#6 #3 AND #4 AND #5
Inclusion and exclusion criteria
Literature inclusion criteria
This investigation adhered rigorously to the PRISMA guidelines (13), establishing comprehensive search protocols and selection criteria based on PICOS methodology in evidence-based practice. Only randomized controlled trials examining how structured exercise interventions impact Internet Addiction Disorder among young adults (18–29 years) were selected for analysis. Experimental cohorts participated in various movement-based or contemplative practices—including Tai Chi, Baduanjin, Mindfulness, Dancesports, Aerobic dance, Yoga, or Qigong—while control conditions included no treatment, treatment as usual, or waitlist controls without structured mind–body interventions. Assessment utilized identical IAD measurement instruments across both groups, administered pre- and post-intervention. Intervention efficacy was determined when the differential calculation between baseline and concluding measurements yielded negative values, Indicating an improvement in symptoms of internet addiction.
Exclusion criteria
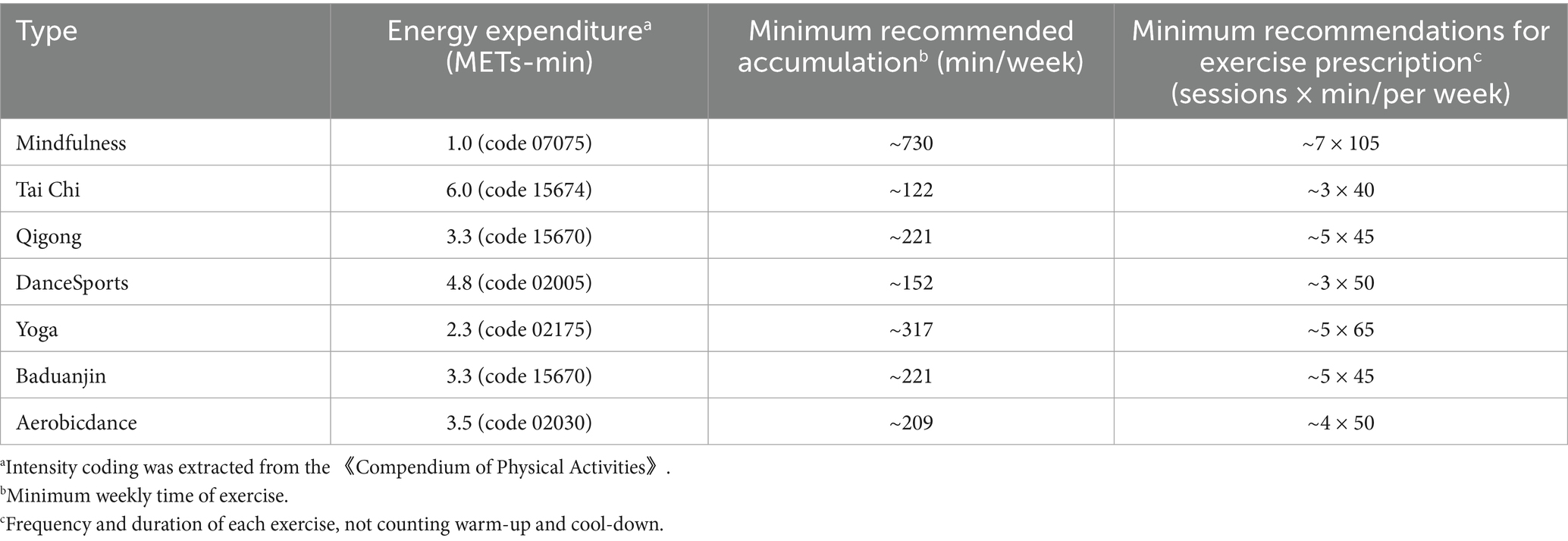
Non RCT experiments; animal studies; descriptive research, reviews, secondary analyses, conference abstracts, and duplicated publications; studies lacking standard statistical presentation (x ± s) or with unextractable metrics; research with confounding interventions making isolation of treatment effects impossible; and studies with incomplete data reporting or unconvertible measurements (Table 1).
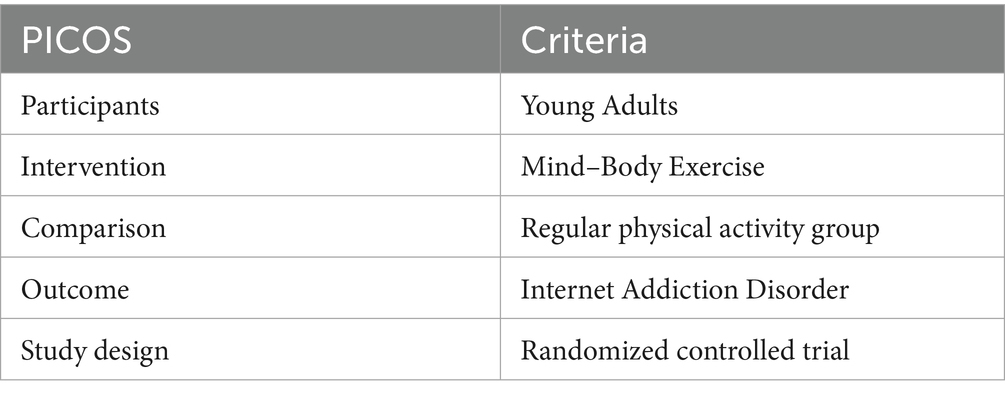
Table 1. PICOS-based eligibility criteria (participation, intervention comparison, outcomes, and study design).
Literature screening and data extraction
After excluding duplicate literature using NoetExpress V4. X software, two researchers independently screened based on inclusion and exclusion criteria and cross checked the results. Disagreements were resolved through discussion until consensus was reached, with a third researcher serving as arbitrator when necessary. Cohen’s kappa coefficient was calculated to assess inter-rater reliability during the screening process, achieving K = 0.94. The data extraction content mainly includes: (1) publication details (title, first author); (2) Participant characteristics (sample size, age, gender, etc.); (3) Intervention standards (type, duration, frequency, pre- and post test scores of the intervention group and control group on the IAD Scale, etc.); (4) The inter rater reliability of the measurement tools and results, as well as the data encoding, is 94%. Any differences are resolved through re examination and consensus meetings. Use the Cochrane Bias Risk Tool for randomized controlled trials to assess the risk of bias.
After extracting the mean (M) and standard deviation (SD) of the scale measurement results before and after intervention experiments from various literature, two researchers calculated the difference in mean values between pre- and post-intervention measurements. For studies not reporting the pre-post correlation coefficient, we assumed R = 0.5 following recommendations from the Cochrane Handbook (14). This assumption was tested in sensitivity analyses using alternative values (R = 0.4, 0.6) to assess the robustness of our findings. When studies reported standard error (SE) rather than standard deviation, we converted values using standard formulae. we converted it to R = 0.5, as shown below:
This study referred to meta-analyses by other scholars, and the results were similar, with R-values of 0.5 (15) and. After sensitivity analysis, the study ultimately chose R = 0.5. In addition, if the original research data is provided as SE, SD is obtained by multiplying the SE of the mean by the square root of the sample size, where N is the sample size:
Data encoding and management
According to pre-defined categories, the included exercise intervention programs are coded as TC (Tai Chi), BDJ (Baduanjin), MF (Mindfulness), DS (DanceSports), QG (Qigong), AD (Aerobicdance), YG (Yoga). We quantified intervention intensity using metabolic equivalent of task (MET) values, where 1 MET represents energy expenditure at rest. MET values were assigned to each intervention based on the 2024 Adult Physical Activity Guidelines (16), the American College of Sports Medicine Exercise Testing and Prescription Guidelines (17), and clinical exercise dosage literature (18). Specifically, we assigned: TC = 3.0 METs, BDJ = 2.5 METs, MF = 1.5 METs, DS = 4.5 METs, QG = 2.5 METs, AD = 5.0 METs, and YG = 3.0 METs. For mindfulness, which is not traditionally measured in METs, we used values from similar seated, focused attention activities. Daily dose was calculated as MET × daily intervention time, and weekly dose as weekly frequency × daily dose. To ensure network connectivity for analysis, we classified interventions into standardized weekly dosage categories: 0 (CG), 100, 200, 300, 400, 500, 600, 700, 1,000, 1,200 METs·min/week.
Data analysis
Meta-analysis
Meta analysis was conducted on the data extracted from the literature using Stata19.0 software. Due to the different measurement tools used for the same indicator in the included literature and the fact that the experimental data were continuous variables, standardized mean difference (SMD) and 95% confidence interval (95% CD) were used as effect measures to merge the effect sizes (19). When p < 0.05, there is a significant difference between the experimental group and the control group, indicating that the results of the meta-analysis are statistically significant (20). When testing heterogeneity, if the heterogeneity I2 is less than 50%, the fixed effects model is used for analysis. If I2 is greater than 50%, the random effects model is used for analysis (21). Use subgroup analysis, sensitivity analysis, and meta regression analysis to determine whether the included studies are biased or require heterogeneity source testing (22).
Dose-response analysis
A Bayesian random-effects framework was employed to evaluate dose-response associations between mind–body exercise interventions and IAD utilizing the “brms” package (version 4.3.1) in R (23, 24). This methodological approach facilitates modeling of nested effect size structures within studies, thereby accounting for statistical dependencies when multiple effect sizes derive from identical participant cohorts. Standardized mean difference (SMD) changes in IAD were modeled through both linear and non-linear specifications (natural spline with 3 or 4 knots) to appropriately adjust for weekly physical activity dosage gradients. Weakly informative prior distributions were specified for the key parameters (overall effect size μ [0, 1] and between-study heterogeneity Tau [0, 1]) (25), with sensitivity analyses incorporating alternative prior specifications (μ [0, 0.5] and Tau [0, 0.5]) conducted to examine the robustness of posterior probability distributions. Optimal model selection proceeded via quantitative comparison of expected log pointwise predictive density, effective parameter count, and cross-validation information criteria. In addition, we adopted a refinement strategy of saving results every 40 iterations to optimize the data monitoring process and reduce storage requirements (26). Model convergence assessment utilized the potential scale reduction factor criterion (PSRF < 1.05) complemented by visual examination of Markov Chain Monte Carlo (MCMC) trace plots and posterior density distributions (27). Comprehensive technical specifications regarding MCMC implementation parameters (iteration quantity, burn-in period duration, thinning intervals) are delineated in Supplementary material S1.
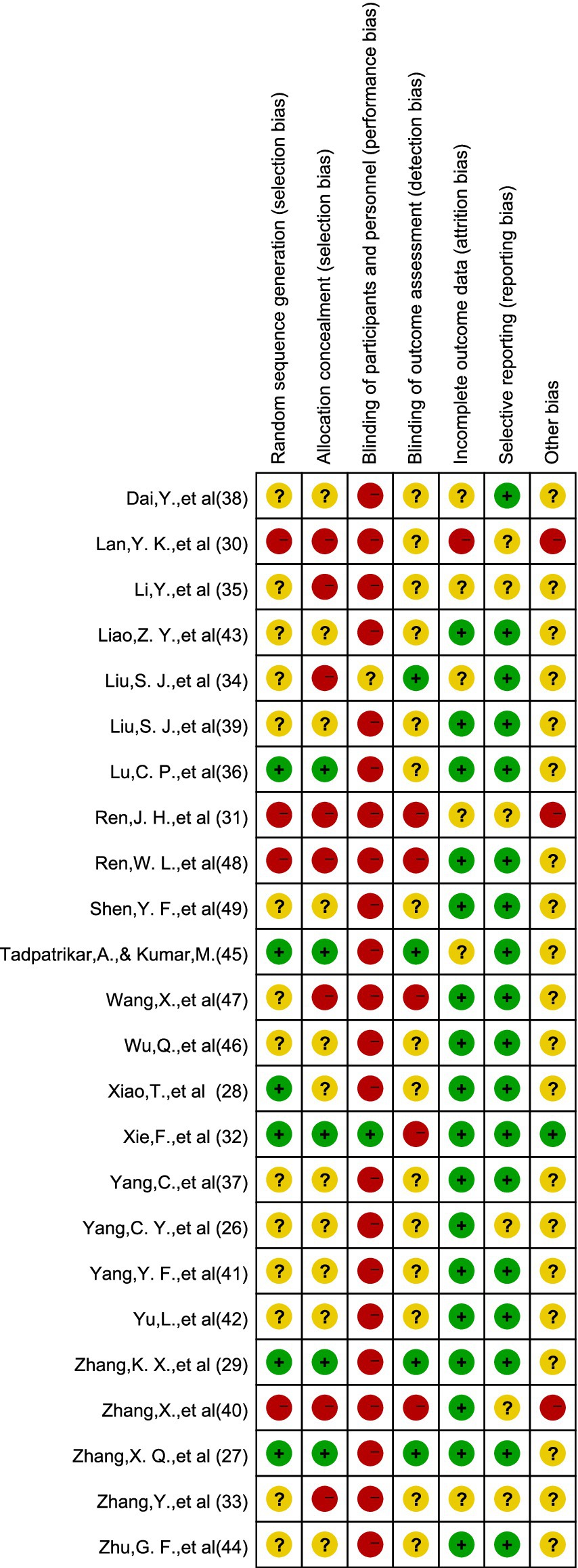
Inclusion in literature bias risk assessment
For quality assessment of included randomized controlled trials, we applied the Second Edition of Cochrane Risk Bias Tool (RoB 2) through RevMan 5.4 software platform. The assessment procedure involved dual independent evaluations conducted by separate investigators. Their comprehensive analysis examined multiple bias domains: generation of randomization sequences, concealment methods for allocation, blinding protocols for both participants and researchers, measures ensuring outcome assessor blinding, approaches to handling missing outcome information, selective outcome reporting issues, plus additional potential bias sources.
The research quality rating adopts a three-level standard: those who fully meet the standard are marked as “+,” indicating low-risk bias; Those who completely do not meet the criteria are marked as “-,” indicating high-risk bias; Those who do not explicitly describe relevant information in the literature are marked with “?,” indicating unknown risk bias. If the results of two researchers are inconsistent during the evaluation process, the third researcher will participate in the discussion.
Results
Data selection
The PRISMA flowchart illustrates the research selection process, as shown in Figure 1. Systematically retrieve databases using pre-defined retrieval strategies. A preliminary search has identified 170 potential studies. After using EndNote software for database management and deleting 32 duplicate studies, there are still 82 studies. After independent screening of titles, abstracts, and complete manuscripts by three researchers, a total of 24 studies were included in the final analysis, including both English and Chinese literature.
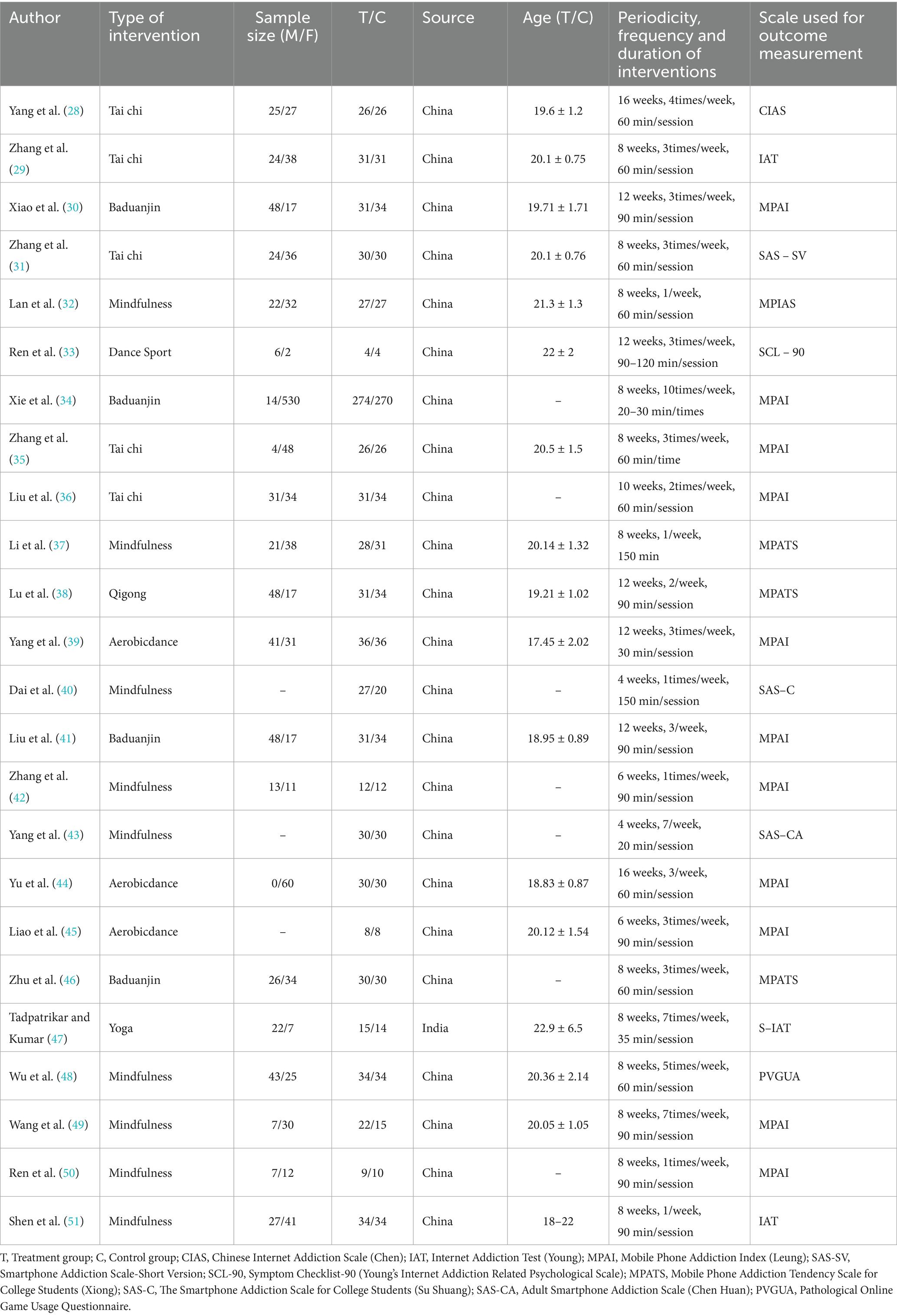
Characteristics included in the study
The study included 24 studies conducted between 2000 and 2025, involving 1,711 young Adults aged 18–24 with a median age of 24. Sports interventions include intervention forms such as Tai Chi, Baduanjin, Mindfulness, Aerobicdance, sports dance, and yoga. Specifically, 143 participants from 5 research groups received Tai Chi, 367 participants from 4 research groups received Baduanjin, 223 participants from 9 research groups received mindfulness meditation, 74 participants from 3 research groups received aerobic fitness exercises, 4 participants from 1 research group received sports dance, 15 participants from 1 research group received yoga, and 31 participants from 1 research group received qigong. The intervention duration ranges from 4 weeks to 16 weeks, with a median duration of 10 weeks. The intervention frequency is 1–10 times per week, with a median frequency of 5.5 times. The duration of each session is 30–150 min, with a median duration of 90 min. The detailed features included in the study are shown in Table 2.
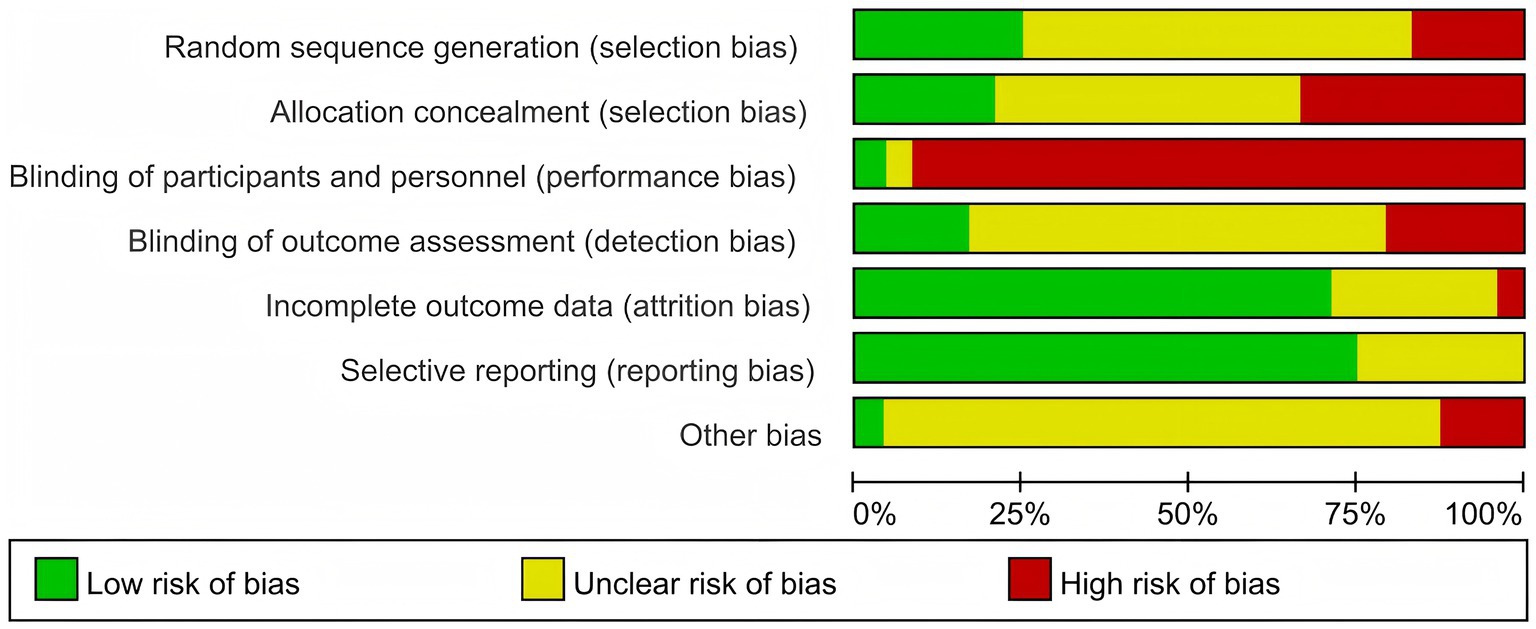
Risk of bias and evidence assessment
Risk of bias
Figures 2, 3 show detailed information on bias risk assessment. Among the 24 studies included, 3 (12.5%) were assessed as low-risk, 11 (45.8%) had certain issues, and 10 (41.7%) showed high-risk bias. From the perspective of bias types, implementation bias is the most prominent, with about 95% of studies showing a high risk of participant and researcher blinding. This is due to the inherent characteristics of mental health intervention research, as participants and implementers often cannot completely blind intervention types. It is worth noting that the risk of incomplete outcome data (loss bias) and selective reporting (report bias) is relatively low, with approximately 70–80% of studies rated as low-risk, indicating good methodological quality in terms of data integrity and reporting transparency. There is a certain proportion of unclear risk (about 50%) in the blind methods of random sequence generation, allocation concealment, and result evaluation, mainly due to insufficient details in the original research report rather than substantial flaws in the research design.
Overall, although there is heterogeneity in the methodological quality of the included studies, it does not affect the overall reliability and clinical significance of the results of this study.
Evidence evaluation
According to the CINeMA system, the overall quality of evidence is assessed as low due to the risk of bias and inconsistency.
Meta analysis of the effect of physical and mental exercise on improving symptoms of young Adults IAD.
A meta-analysis of 24 controlled studies was also conducted (N = 1,711). The overall results of the meta-analysis are presented in Figure 4. Compared with the control group, we found that the experimental intervention had a significant effect on reducing the primary outcome measure (SMD = −1.63, 95% CI: −2.04, −1.22). The I2 statistic showed substantial heterogeneity (I2 = 92%, df = 23, p < 0.00001). Analysis of the forest plot shows that all included studies demonstrated negative effect values, indicating a consistent direction of effect for the intervention. The most significant effect was observed in Yang, Y. F., et al., 2021 (SMD = −7.29, 95% CI: −8.73, −5.85), while the smallest effect was found in Lan, Y. K., et al., 2018 (SMD = −0.05, 95% CI: −0.58, 0.49). Given the high heterogeneity, we employed a random-effects model for analysis, with an overall effect test of Z = 7.77 (p < 0.00001), indicating that the intervention effect was statistically significant.
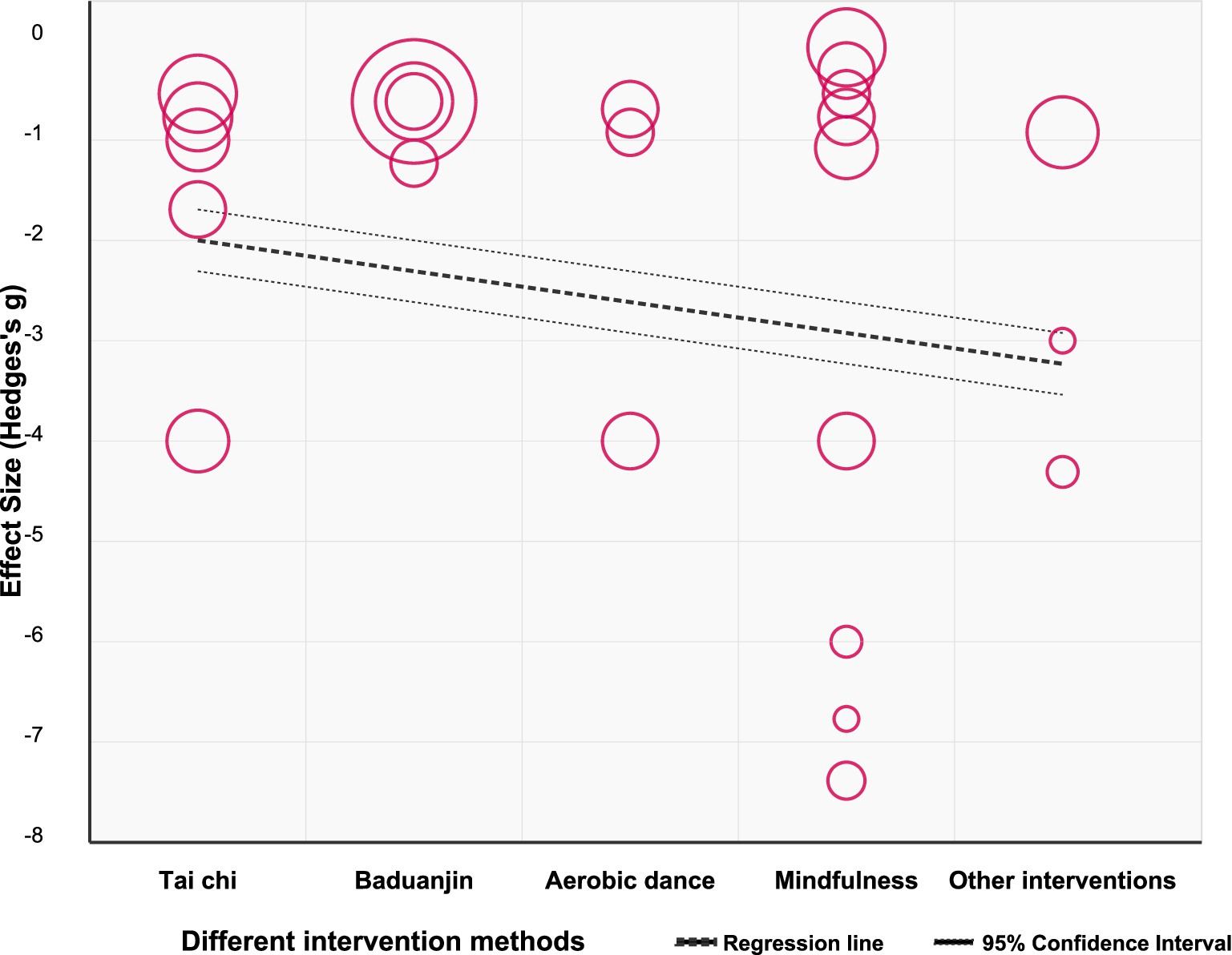
Meta analysis on the improvement effect of different physical and mental exercises on Young Adults IAD
Figure 5 shows the impact of different physical and mental exercises on young Adults IAD test scores. We screened all included studies and conducted screening based on the original implementation status. In the study, we divided the data into Tai Chi (n = 5), Baduanjin (n = 4), aerobic fitness exercises (n = 3), mindfulness meditation (n = 9), and other intervention methods (n = 3). Compared with the control group, the intervention group had a significant positive effect on the scores of young Adults IAD tests [SMD = −10.35, 95% CI (−13.39, −7.30), p < 0.0001], indicating that the degree of IAD in the intervention group was significantly reduced. The physical and mental exercise intervention method involved in the experiment had a strong positive effect on IAD and the effect was significantly better than that of the control group. However, there is a high degree of heterogeneity among the studies (I2 = 92%). Subgroup analysis showed that although the differences between subgroups did not reach statistical significance (p = 0.23), there were apparent differences in the effect size values: mindfulness meditation [SMD = −12.90, 95% CI (−23.52, −2.29)] and Tai Chi [SMD = −10.59, 95% CI (−16.01, −5.17)] showed higher effect sizes, which is consistent with the results shown in Figure 6. However, the notably wide confidence intervals for these subgroups suggest substantial statistical instability in these estimates, warranting caution in interpretation. These wide intervals likely reflect the limited number of studies in each subgroup and considerable methodological variation.
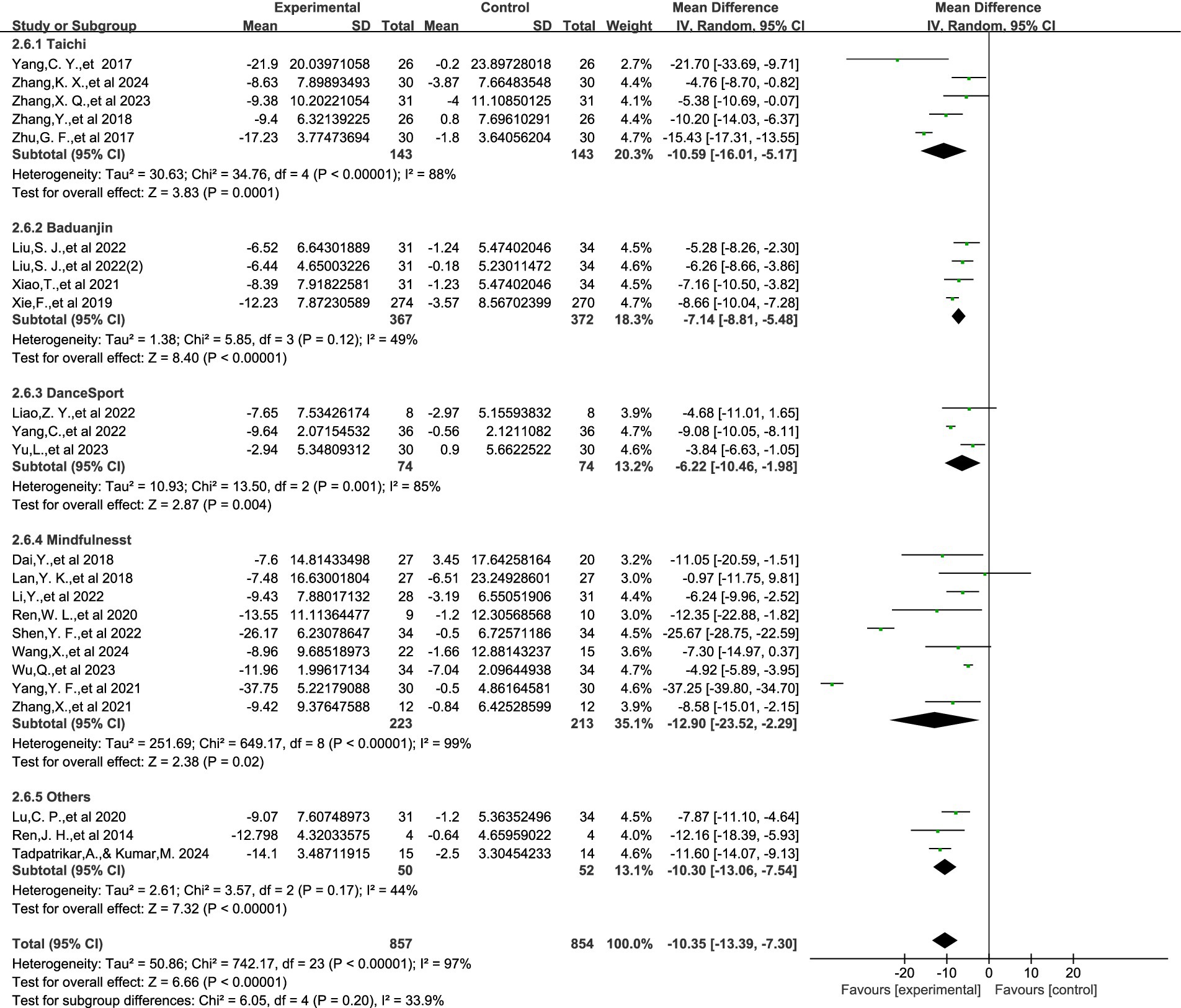
Figure 5. The impact of different physical and mental exercises on the improvement of symptoms of IAD.
Although the effect of Ba Duan Jin [SMD = −7.14, 95% CI (−8.81, −5.48)] is relatively small, it has a narrow confidence interval and low heterogeneity (I2 = 49%), providing the most accurate and reliable estimate. Given the instability of some subgroup findings, these comparative effectiveness results should be considered preliminary rather than definitive, and future research with larger samples is needed to confirm potential differential effects between mind–body exercise modalities.
Subgroup analysis
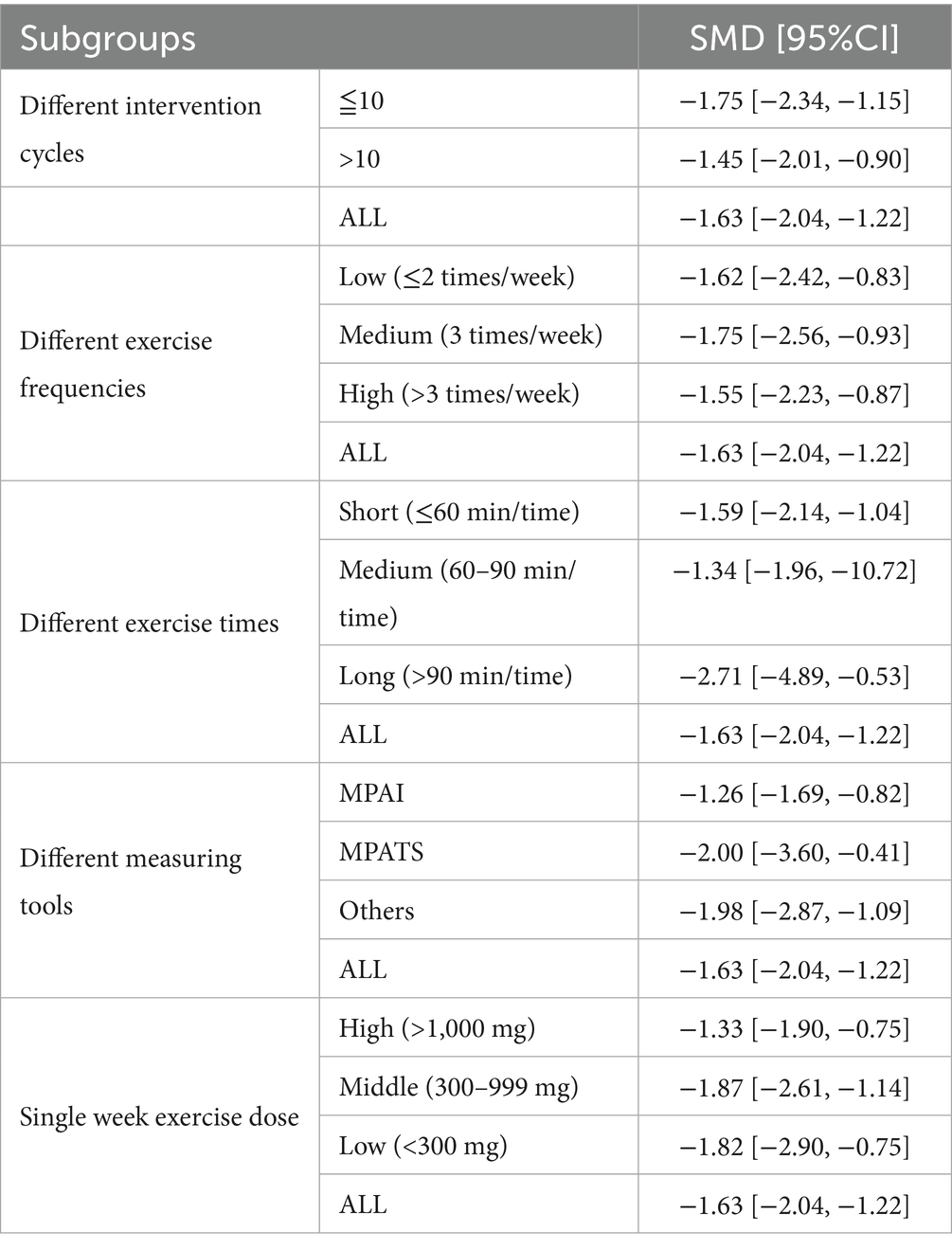
The study conducted subgroup analysis based on “exercise frequency, exercise time, intervention cycle, measurement tools, and intervention intensity.” The analysis results are shown in Table 2.
According to Tables 3, 4, there is significant statistical heterogeneity among the 24 studies included [I2 = 92%, Q = 273.91, p < 0.0001]. Notwithstanding this substantial heterogeneity, the aggregate effect size [SMD = −1.63, 95% CI (−2.04, −1.22)] demonstrates a statistically significant therapeutic effect of mind–body exercise interventions on young adults’ Internet Addiction Disorder symptomatology.
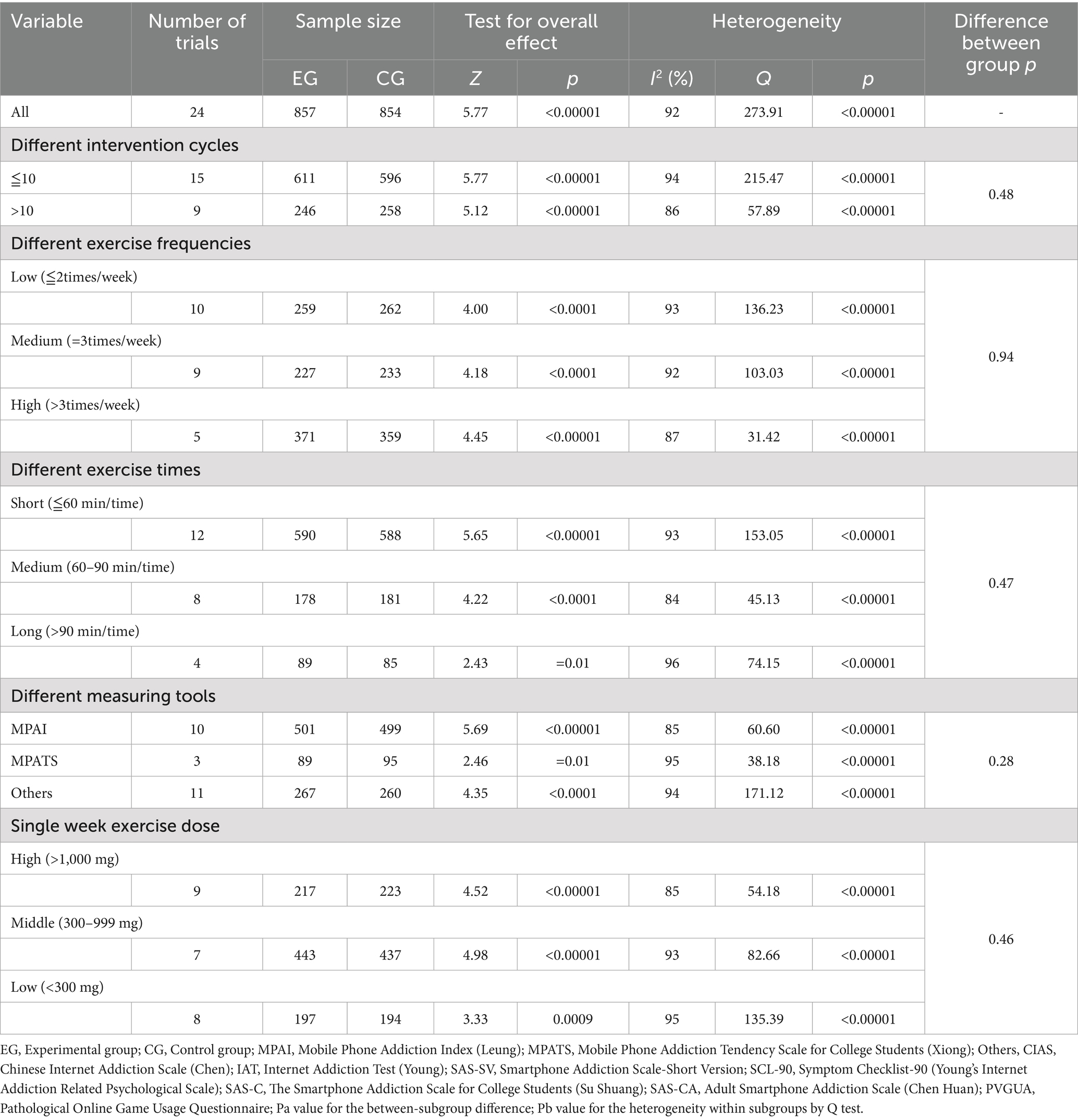
Table 3. Subgroup analysis to assess the effect of interventions on young Adults’ intervention addiction.
Analysis of different intervention cycles shows that both short intervention cycles (<10 times) and long intervention cycles (≥10 times) have significant intervention effects on young Adults IAD through physical and mental exercise (both p < 0.0001). Both subgroups showed high heterogeneity, with higher heterogeneity observed in the short intervention period (I2 = 94%, Q = 215.47) compared to the short intervention period (I2 = 86%, Q = 57.89). Analysis of different exercise frequencies showed that low frequency (≤2 times/week), medium frequency (=3 times/week), and high frequency (>3 times/week) all produced statistically significant effects (all p < 0.00001). Analysis of different exercise durations revealed that extended session interventions (>90 min/session) demonstrated the most pronounced effect magnitude (SMD = −2.71), albeit with concomitant elevation in inter-study variability as evidenced by heterogeneity indices (I2 = 96%, Q = 74.15). Analysis of different measurement tools shows that studies using MPATS measurement exhibit high strain efficiency (SMD = −2.00) and moderate heterogeneity (I2 = 95%, Q = 38.18). Single week exercise dose analysis showed that different dose levels produced significant intervention effects (all p < 0.00001), but the low-dose group had higher heterogeneity (I2 = 95%, Q = 135.39).
Despite comprehensive stratified analyses, the substantial heterogeneity between studies (I2 = 92%) remained predominantly unexplained, a phenomenon frequently encountered in meta-analytic evaluations of complex behavioral interventions (52). This heterogeneity may be attributable to unmeasured moderating variables, methodological variations in intervention implementation protocols, and research design discrepancies (53). As articulated by Guyatt et al., when intervention effects demonstrate consistent directionality and statistical significance across studies, therapeutic efficacy may be reasonably inferred despite the presence of heterogeneity (53). It warrants emphasis that all subgroup analyses revealed statistically significant therapeutic effects of mind–body exercise on IAD symptomatology (all p < 0.00001), suggesting that despite methodological and clinical heterogeneity, the intervention efficacy remains robust across diverse experimental conditions.
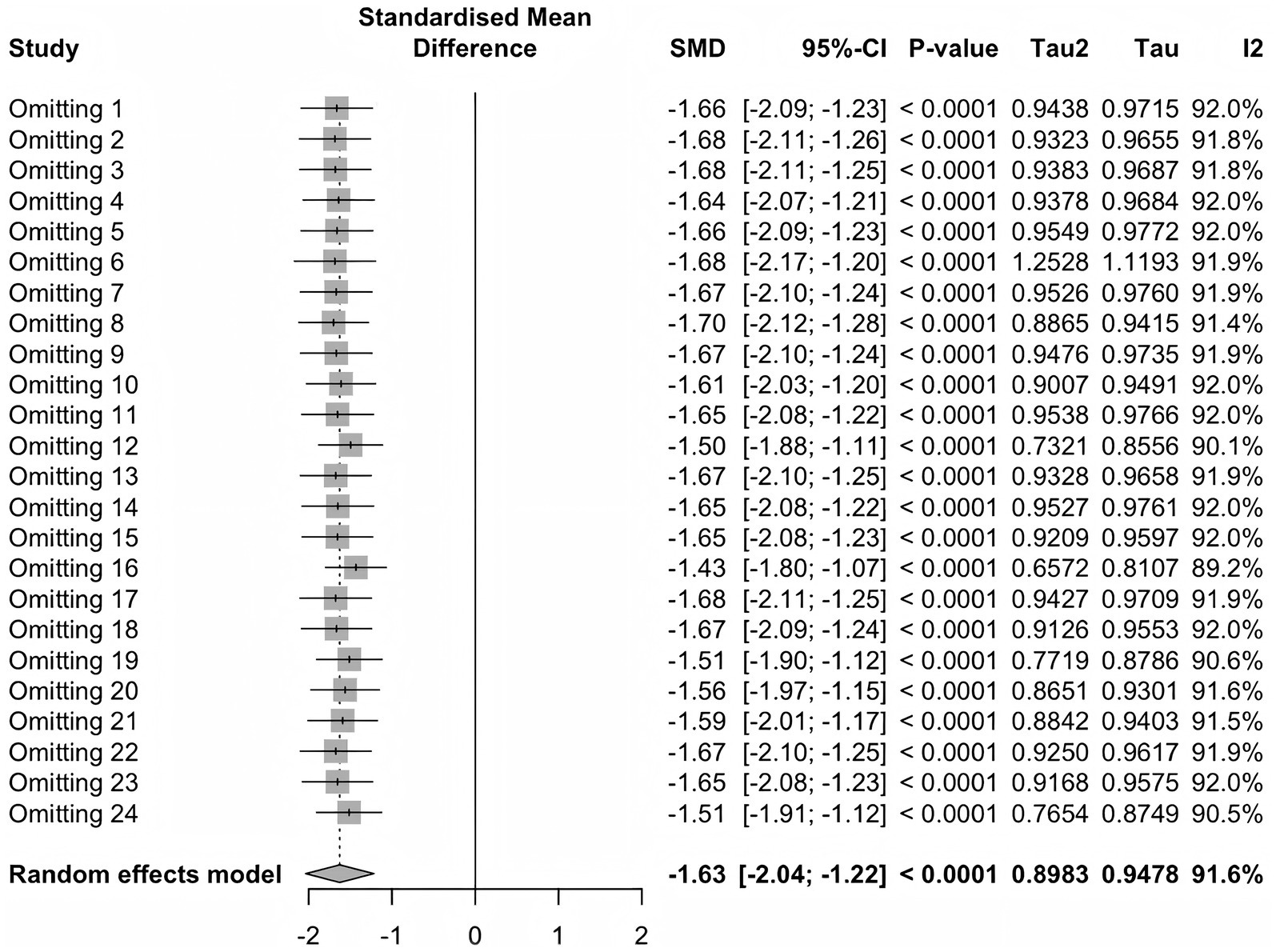
Sensitivity analysis
Sensitivity analysis showed that regardless of which study was excluded (Figure 7), the standardized mean deviation (SMD) remained between −1.43 and −1.70, with p values < 0.0001, indicating consistent statistical significance.
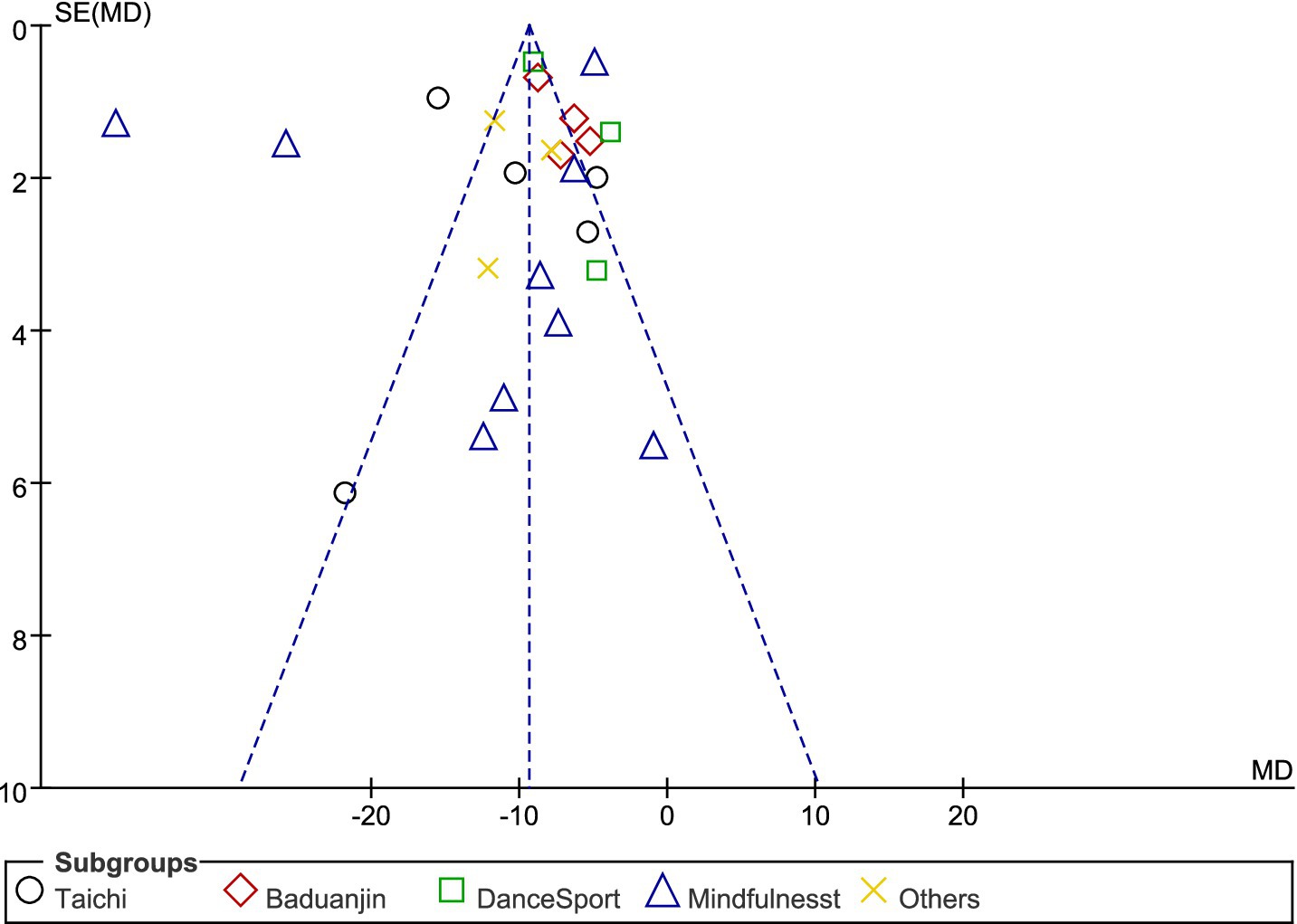
Publication bias
Examination of the funnel plot (Figure 8) suggests potential publication bias in our meta-analysis. The distribution of studies shows some asymmetry, with several small studies (having larger standard errors) displaying more negative effect sizes than would be expected in an unbiased sample. Studies are clustered predominantly on the left side of the mean effect size (represented by the vertical dotted line), particularly those with larger standard errors. This pattern indicates that smaller studies with less significant or positive results might be underrepresented in the literature. However, most studies fall within the expected triangular region defined by the funnel boundaries, suggesting that the observed asymmetry may not severely compromise the validity of our findings. The overall effect size (SMD = −1.63, 95% CI: −2.04, −1.22) appears robust, as demonstrated in our forest plot analysis (Figure 3), with consistent negative effect directions across the 24 included studies. While some publication bias cannot be ruled out, the magnitude and consistency of effects across multiple studies, particularly those with larger sample sizes, support the reliability of our main conclusion that the intervention significantly reduces the primary outcome measure compared to control conditions.
Bayesian dose-response meta-analysis results
The overall dose-response relationship of exercise
The overall dose-response relationship between exercise dosage and internet addiction exhibits a non-linear dose-dependent U-shaped curve (Figure 9). When exercise dosage is below the threshold of 150 MET min/week (blue dashed line on the left), therapeutic efficacy for IAD symptomatology demonstrates limited magnitude with substantial response variability; as dosage parameters increase, therapeutic efficacy exhibits progressive enhancement, reaching optimal efficacy at 730 MET min/week; upon exceeding the threshold of 1,100 MET min/week (blue dashed line on the right), marginal therapeutic benefit demonstrates significant attenuation, with concomitant expansion of the 95% confidence interval (dashed boundary), indicating increased outcome uncertainty in high-dosage regimens. At a weekly level of 600MET [the recommended lower limit of physical activity for energy expenditure by the World Health Organization (54)], the predictive effect was high (SMD = −1.92, 95% Crl −3.22, −0.58, SD = 0.67). Similarly, at 1200 METmin/week (the recommended upper limit for energy expenditure and physical activity by the World Health Organization), the predictive effect is moderate (SMD = −1.20, 95% Crl −2.86, 0.49, SD = 0.86), but the SD value is larger. The optimal intervention effect was achieved at 730MET per week (SMD = −1.99, 95% CrI −3.28, −0.71, SD = 0.65).
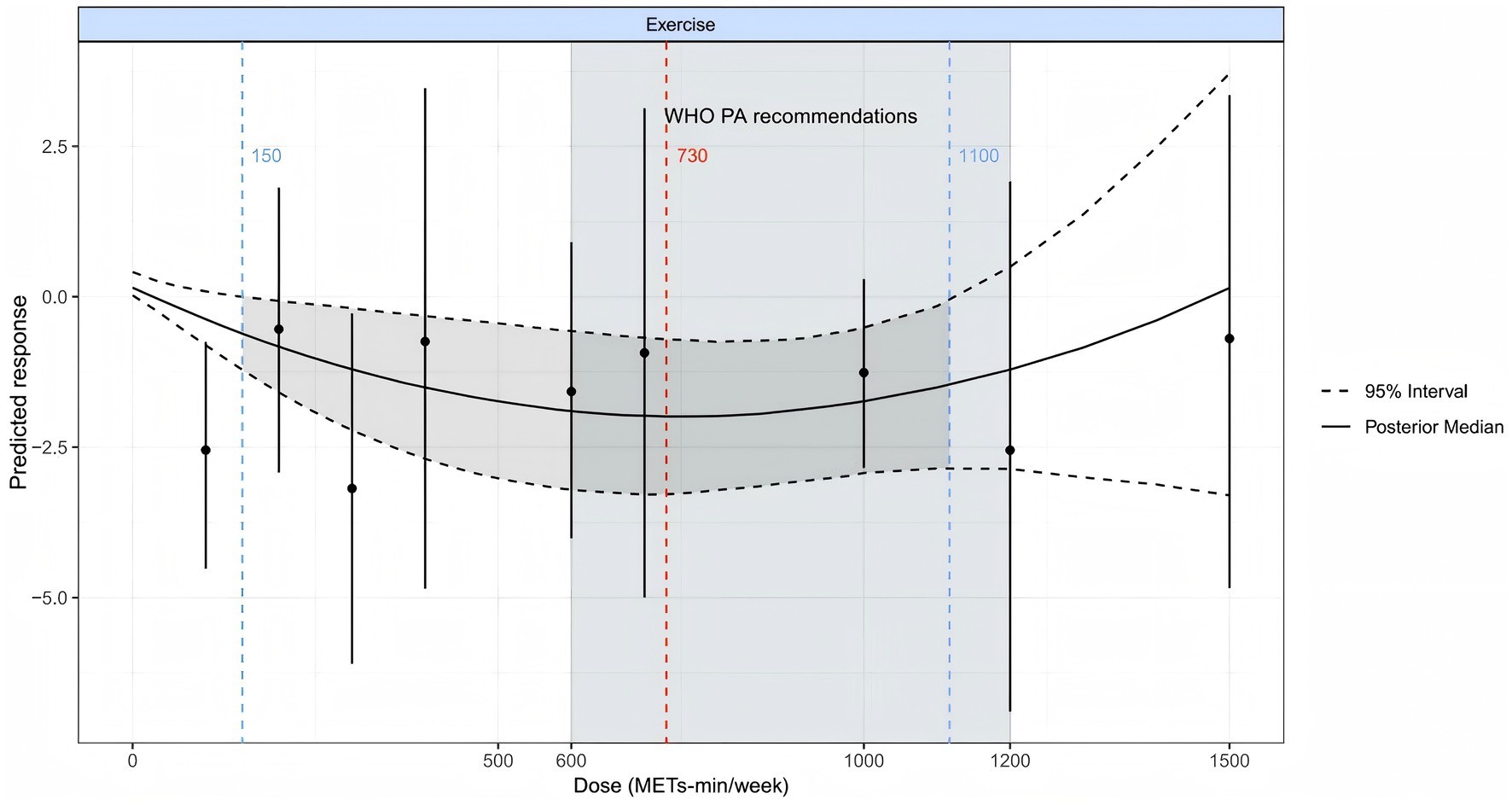
Figure 9. The dose-response relationship of improving IAD through physical and mental exercise. The gray area represents statistically significant regions (p < 0.05), where the confidence interval does not cross zero effects, indicating reliable improvement in internet addiction. The red dashed line represents the optimal dosage for achieving the best results, while the black short solid line represents the original dataset. MET, task metabolic equivalent; PA, Physical activity; SMD, Standardized mean deviation; WHO, World Health Organization.
Discussion
Main findings
This study analyzed the impact of physical and mental exercise on young Adults IAD and its dose-response relationship. The seven mind–body exercise interventions examined demonstrated statistically significant therapeutic efficacy for IAD symptomatology. Intervention-specific subgroup analyses revealed differential therapeutic potency across modalities, with Mindfulness [SMD = −12.90, 95% CI (−23.52, −2.29)] demonstrating the most pronounced aggregate effect magnitude, followed by Tai Chi [SMD = −10.59, 95% CI (−16.01, −5.17)], other intervention methodologies [SMD = −10.30, 95% CI (−13.06, −7.54)], Baduanjin [SMD = −7.14, 95% CI (−8.81, −5.48)], and Aerobicdance [SMD = −6.22, 95% CI (−10.46, −1.98)]. It warrants acknowledgment that the expansive confidence intervals observed for certain intervention modalities suggest substantial statistical imprecision in these effect estimations.
The study also found a non-linear dose-response relationship between physical and mental exercise and IAD, exhibiting a typical U-shaped relationship. The estimated optimal effective dose is 730 MET min/week, which is equivalent to 221 min of Qigong (3.3 MET), 152 min of DanceSports (4.8 MET), 317 min of Yoga (2.3 MET), 730 min of Mindfulness (1.0 MET), 122 min of Tai chi (6.0 MET), 221 min of Baduanjin (3.3 MET), or 209 min of Aerobicdance (3.5 MET). When the physical and mental exercise dose reaches 1,100 MET minutes per week, the improvement of IAD symptoms reaches a stable state. It is worth noting that the optimal dose of 730 MET min/week observed by us falls within the recommended range of physical activity by the World Health Organization (WHO) (600–1,100 MET min/week, light blue area in the figure), indicating that following WHO’s general activity recommendations is also applicable for improving symptoms of IAD and does not require special adjustments. Finally, sensitivity analysis showed that factors such as high risk of bias, short intervention time, and different measurement tools did not significantly affect the effectiveness of physical and mental exercise interventions.
Characteristics and limitations of included RCTs
Study characteristics and methodological heterogeneity
The 24 included randomized controlled trials, spanning from 2000 to 2025, exhibited substantial methodological heterogeneity that requires careful consideration. The studies involved 1,711 young adults aged 18–24 years with a median age of 24, representing a relatively homogeneous population in terms of age demographics. However, several methodological variations were observed across studies that may influence the interpretation of our findings.
Intervention characteristics and variability: The intervention protocols varied considerably across studies. Intervention duration ranged from 4 weeks to 16 weeks (median: 10 weeks), with frequency varying from 1 to 10 times per week (median: 5.5 times), and session duration spanning 30–150 min (median: 90 min). This wide variation in dosage parameters created challenges for standardization and may contribute to the observed heterogeneity (I2 = 92%). The diverse implementation approaches across different cultural contexts (predominantly Chinese studies with one Indian study) may also introduce cultural and methodological variations that affect intervention effectiveness.
Measurement tool inconsistencies: A significant methodological challenge emerged from the use of multiple IAD assessment instruments across studies. The included studies employed various scales including MPAI, MPATS, CIAS, IAT, SAS-SV, SCL-90, SAS-C, SAS-CA, and PVGUA. While all these instruments measure aspects of internet-related addiction behaviors, they differ in their focus areas (general internet addiction vs. smartphone addiction vs. gaming addiction), scoring systems, and psychometric properties. This heterogeneity in outcome measurement tools may have contributed to the observed statistical heterogeneity and complicates direct comparison across studies.
Risk of bias assessment and quality concerns
The risk of bias assessment revealed significant methodological limitations across the included studies. Only 3 studies (12.5%) were assessed as low-risk, while 11 studies (45.8%) had certain methodological concerns, and 10 studies (41.7%) showed high-risk bias. The most prominent issue was implementation bias, with approximately 95% of studies showing high risk regarding participant and researcher blinding. This limitation is inherent to physical and mental exercise intervention research, as complete blinding of intervention types is often practically impossible.
Randomization and allocation concerns: Approximately 50% of studies showed unclear risk in random sequence generation and allocation concealment, primarily due to insufficient methodological details in the original research reports rather than fundamental design flaws. This lack of transparency in reporting randomization procedures raises concerns about selection bias and the overall validity of treatment effect estimates.
Data integrity and reporting quality: Encouragingly, the risk of incomplete outcome data (attrition bias) and selective reporting (reporting bias) was relatively low, with approximately 70–80% of studies rated as low-risk. This suggests reasonable methodological quality in terms of data integrity and reporting transparency, which supports the reliability of the primary outcome data used in our meta-analysis.
Methodological challenges identified through systematic review
Sample size limitations: Several studies included in our analysis had relatively small sample sizes, with some interventions represented by very few participants (e.g., 4 participants for sports dance, 15 for yoga). These small sample sizes limit the precision of effect estimates and may contribute to the wide confidence intervals observed in some subgroup analyses.
Control group heterogeneity: The control conditions varied across studies, ranging from waitlist controls to regular physical activity groups. This variation in control group characteristics may influence the magnitude of observed treatment effects and contribute to between-study heterogeneity.
Cultural and contextual factors: The predominance of studies conducted in Chinese populations may limit the generalizability of findings to other cultural contexts. Cultural factors may influence both the acceptability and effectiveness of different mind–body interventions, suggesting that our findings may require validation in more diverse populations.
Comparison of the effects and mechanism explanation of different physical and mental exercise intervention methods.
The research results indicate that mindfulness meditation has a significantly higher effect on improving IAD compared to other physical and mental exercise interventions [SMD = −12.90, 95%CI (−23.52, −2.29), p < 0.0001]. While this substantial effect magnitude warrants judicious interpretation given the expansive confidence interval, mindfulness meditation’s potential therapeutic superiority may be attributable to multifaceted neurobiological mechanisms. From a neuroplasticity perspective, Tang et al. demonstrated that mindfulness training significantly potentiates functional connectivity between default mode and executive control networks, thereby optimizing attentional regulation and self-referential processing capacities (55); Hölzel et al. further elucidated that 8-week mindfulness training protocols induce significant volumetric enhancement in prefrontal cortical and anterior cingulate cortical regions (56), structural modifications that directly augment cognitive control capacities and may contribute to executive function enhancement in IAD patients. At the neurotransmitter level, Khoury et al.’s systematic review delineated several neurochemical regulatory pathways associated with mindfulness practice: enhancement of affective state through serotonergic stabilization, anxiolytic effects via GABAergic potentiation, and attenuation of chronic stress responsivity through inhibition of hypothalamic–pituitary–adrenal axis activation and subsequent cortisol secretion (57). Regarding social cognition, Vago and Silbersweig’s investigation demonstrated that mindfulness practice significantly enhances participants’ self-awareness and interpersonal functioning through insular activation and potentiation of functional connectivity between anterior cingulate cortical and prefrontal regions (58).
In contrast, traditional Chinese sports such as Tai Chi and Baduanjin have also played a positive role in improving IAD. Tai Chi combines the characteristics of physical activity, breath control, and mindfulness, and research has shown that it can effectively regulate the function of the autonomic nervous system. The review by Song et al. suggests that practicing Tai Chi can increase vagus nerve activity, reduce sympathetic nervous system excitability, and thus lower levels of stress hormones such as cortisol. This has positive implications for alleviating the stress response hyperactivity commonly found in internet addicts (59). Wang et al. confirmed through a randomized controlled trial that 24 weeks of Tai Chi practice can significantly reduce anxiety levels in college students (p < 0.01) and improve heart rate variability indicators, indicating positive regulation of autonomic nervous system function. In terms of brain function (60), Wei et al. used functional magnetic resonance imaging technology to find that after 12 weeks of Tai Chi training, participants showed increased activity in the prefrontal cortex, especially the dorsolateral prefrontal cortex, which is closely related to executive control and impulse suppression, and executive dysfunction is a typical feature of internet addicts (61). As a traditional Chinese fitness qigong, although the movements of Baduanjin are relatively simple, its impact on the neuroendocrine system is also worth paying attention to. The systematic review by Zou et al. showed that practicing Baduanjin can effectively reduce serum cortisol and norepinephrine levels, while improving mental health (62).
The subgroups composed of Qigong, DanceSports, and Yoga also showed higher efficacy, although their mechanisms of action were different, they have been widely proven to improve IAD. This type of physical and mental activity can effectively regulate the hypothalamic pituitary adrenal (HPA) axis function and improve the common neuroendocrine imbalance in internet addicts. The systematic review by Pascoe et al. confirms that yoga practice can significantly reduce cortisol levels, which is directly related to stress response dysregulation in internet addicts (63). Secondly, these activities optimize the balance of neurotransmitters. Streeter et al. found through magnetic resonance spectroscopy that yoga practice can significantly increase GABA levels, and low GABA levels are closely related to difficulty in impulse control (64). Field et al. found that regular yoga practice can reduce sympathetic nervous system activity while increasing levels of anti stress neurotransmitters (65). In addition, these activities promote the optimization of functional connectivity in key brain regions. The meta-analysis by Fox et al. found that yoga and meditation practices can affect the structure of brain regions related to attention control and emotion regulation, which is crucial for improving self-control related to IAD (66). The study by Li et al. on individuals addicted to online games showed that physical and mental intervention activities can significantly improve their attention control ability and impulse suppression function (67). Chen et al. found that psychological intervention combined with physical activity can effectively reduce internet usage time and improve self-regulation ability (68). The study by Du et al. confirmed that physical activity intervention can significantly improve the internet usage behavior and mental health status of college students (69).
Aerobicdance affect IAD symptoms by regulating various neurotransmitters. Research has shown that aerobic exercise promotes dopamine secretion, which is transmitted through the basal ganglia to the prefrontal cortex and motor cortex, helping to restore the neurological function of addicts (70). This exercise can increase dopamine levels in the striatum, hypothalamus, and brainstem of different genders. Research has found that young Adults with IAD who engage in regular aerobic exercise have significantly higher levels of serum brain-derived neurotrophic factor (BDNF) compared to the non exercise group (p < 0.05), and their IAD scores are significantly reduced, with a negative correlation between the two (r = −0.58) (71). High intensity exercise stimulates BDNF gene expression through β-hydroxybutyrate ketone bodies, promotes neural plasticity, and improves cognitive function (72). Although Tai Chi, Baduanjin, and Aerobicdance perform well in regulating the autonomic nervous system, improving heart rate variability, and enhancing prefrontal cortex activity, their targeted effects on core attention deficit and emotional control ability in internet addicts are usually not as significant as mindfulness meditation (73), resulting in slightly lower overall intervention effects on IAD symptoms.
These findings not only reveal the underlying mechanisms by which different forms of exercise improve internet addiction, but also have significant implications for public health and clinical practice. Internet addiction is closely related to attention deficit, impulse control disorder, difficulty regulating emotions, and social dysfunction (74). Mindfulness provides a comprehensive intervention strategy for these issues by simultaneously enhancing neural activity in the anterior cingulate gyrus and insula regions and regulating key neurotransmitter systems. For high-risk IAD populations such as teenagers, college students, and professionals facing high stress, Mindfulness—a low threshold, high compliance intervention with dual cognitive and emotional regulation benefits—has considerable potential for application (75, 76) Incorporating mindfulness into campus mental health programs, community health promotion programs, and IAD prevention strategies may provide an economical and feasible approach to improving IAD symptoms, enhancing self-regulation abilities, and reducing related mental health risks.
In summary, Mindfulness as a single intervention method has more high-quality research support (77), and its mechanism in improving attention control, emotion regulation, and impulse control is more clear (56, 78). Mindfulness has shown significant therapeutic effects on IAD by enhancing self-awareness, reducing automated response patterns, and improving executive function. These findings are consistent with the views of Kuss and Lopez Fernandez that interventions based on cognitive and behavioral dual regulation are more effective in alleviating IAD behavior, providing profound guidance for public health policies and clinical practice.
Dose-response relationship analysis
Research has found a U-shaped relationship between physical and mental exercise and symptoms of IAD, with the optimal physical and mental exercise dose being 730 MET min/week. Li et al. found that among American adults, after 8 weeks of mindfulness guided recovery enhancement (MORE) intervention, participants’ symptoms of online gaming disorder were significantly reduced, especially those who maintained near 750 MET min/week showed the best symptom improvement and maintenance effects (67). Yao et al. reported that a moderate intensity intervention (approximately 750 MET min/week) combining reality therapy and mindfulness can significantly reduce cross temporal decision-making impulsivity in young people with online gaming disorders (79), while interventions below 600 or above 1,000 MET min/week have relatively weaker effects. Low exercise doses cannot fully activate the autonomic mechanism, while high exercise doses may lead to decreased compliance and excessive fatigue. Based on these findings, it is recommended that physical and mental exercise interventions for young people with IAD, including Qigong, DanceSports, Yoga, Mindfulness, Tai chi, and Aerobicdance, should be maintained at the optimal dose of 730 MET min/week to achieve the most ideal intervention effect.
Practical implications of the U-shaped dose-response relationship for exercise recommendations
Our dose-effect analysis revealed a distinct U-shaped curve relationship between physical-mental exercise and Internet Addiction Disorder (IAD) improvement. Research data identified an optimal exercise intensity point (approximately 730 MET minutes weekly total), where intervention effectiveness reached its peak. This finding holds significant practical value, demonstrating that insufficient or excessive exercise levels both diminish the efficacy of IAD interventions. These results provide scientific basis for developing precise treatment protocols while highlighting the crucial role of moderate exercise in the therapeutic process. On the one hand, insufficient exercise cannot provide sufficient neurobiological stimulation, leading to impaired regulation mechanisms of neurotransmitters such as dopamine and serotonin, which cannot effectively improve symptoms of IAD (80). On the contrary, excessive exercise can cause physical fatigue and increased stress, leading to a decrease in self-regulation ability and exacerbating symptoms of IAD (81). Therefore, only moderate physical and mental exercise can effectively regulate the brain’s reward pathway (82), repair dopamine pathway blockages caused by IAD, and become a key factor in improving IAD.
This U-shaped correlation additionally establishes a foundation for tailored exercise regimens. The quantification of physical activity through standardized metrics like MET minutes enables healthcare practitioners and public health specialists to precisely determine optimal exercise parameters—including intensity levels and time commitments—for maximizing therapeutic outcomes in IAD patients. Such evidence-based recommendations allow for individualized treatment approaches that can effectively target IAD symptomatology through carefully calibrated physical activity protocols. For example, for young people who have already shown a tendency toward IAD, adhering to this optimal exercise dosage can effectively activate the normal regulatory mechanisms of neurotransmitters such as dopamine and serotonin, help restore prefrontal cortex function, enhance executive control ability, and avoid negative effects associated with excessive exercise.
In addition, this finding is consistent with the guidelines for moderate intensity physical and mental exercise intervention recommended by the World Health Organization (54) and the IAD Research Association (83), which further emphasizes the importance of maintaining an appropriate level of physical activity when dealing with IAD. Incorporating this optimal exercise dosage into campus health education, psychological counseling services, and young Adults health promotion programs can not only effectively alleviate symptoms of IAD, but also improve mental health problems such as depression, anxiety, and social disorders caused by excessive internet use (67), thereby promoting the physical and mental health development of young Adults on a broader scale.
In summary, the U-shaped dose-response relationship revealed in this study suggests that precise regulation of exercise dosage is crucial in developing physical and mental exercise interventions aimed at alleviating symptoms of IAD. By adjusting the intensity and duration of exercise appropriately to achieve the optimal dosage, symptoms of IAD can be minimized to the greatest extent possible, and executive function and self-regulation abilities can be improved. This discovery provides clear clinical guidance for exercise prescriptions targeting young people with IAD, and has substantial application value for educational institutions, mental health services, and public health policy-making. Table 5 lists exercise recommendations to improve symptoms of IAD.
Comparison with existing studies
The results of this study are highly consistent with existing literature. Previous investigations have demonstrated that low to moderate intensity mind–body interventions produce statistically significant therapeutic effects in ameliorating IAD symptomatology (84). Gong and Lin’s empirical research corroborates that moderate to low-intensity mindfulness meditation protocols effectively enhance psychological wellbeing among collegiate populations, including reduction of anxiety and depressive symptomatology frequently comorbid with IAD. These findings provide additional theoretical substantiation for the efficacy of mindfulness in attenuating IAD-related psychopathology.
In contradistinction to conventional meta-analytic methodologies, this investigation employed comparative effect measure quantification to systematically evaluate and hierarchically categorize the relative efficacy of diverse intervention modalities. Furthermore, this study represents the first implementation of Bayesian dose-response analytical techniques to empirically quantify optimal dosage parameters for mind–body exercise interventions in IAD, thereby establishing an evidence-based foundation for the development of personalized intervention protocols.
Practical and applied significance
The empirical findings herein demonstrate substantial therapeutic efficacy for non-pharmacological intervention modalities in ameliorating Internet Addiction Disorder symptomatology among young adult populations. Mindfulness-based practices emerge as potentially superior therapeutic modalities for exercise-mediated IAD symptom reduction, though with acknowledgment of statistical limitations. Of particular clinical relevance, adherence to empirically derived optimal exercise dosage parameters (730 MET minutes/week) appears to yield significant enhancement of intervention efficacy. This investigation contributes substantive empirical evidence supporting the implementation of structured physical and contemplative exercise protocols within educational institutions and public health frameworks addressing IAD prevention and treatment among young adult demographic cohorts.
Methodological strengths and limitations
This investigation’s principal methodological strength resides in its integration of network meta-analytic techniques with Bayesian statistical frameworks, facilitating systematic comparative evaluation of diverse mind–body exercise interventions for young adult IAD symptomatology while simultaneously quantifying optimal dosage parameters. This methodological approach enables synthesis of both direct and indirect comparative evidence, thereby providing more comprehensive efficacy evaluations—a particularly valuable contribution given that previous empirical investigations rarely conducted comparative analyses of multiple intervention modalities within single experimental designs.
Notwithstanding the substantive empirical findings, methodological limitations merit critical examination. Substantial methodological heterogeneity characterizes the corpus of incorporated randomized controlled trials, manifesting in divergent randomization protocols, variable allocation concealment procedures, inconsistent blinding methodologies, and heterogeneous outcome reporting mechanisms. Studies exhibiting elevated or indeterminate bias coefficients potentially attenuate effect size estimation precision and circumscribe the generalizability of observed therapeutic efficacy parameters.
Furthermore, analyses predominantly relied on self-reported IAD measurements (MPAI, MPATS, SAS-SV, etc.). These instruments are susceptible to recall bias and social desirability effects, potentially compromising outcome accuracy. Inconsistent questionnaire item interpretation across studies may introduce additional variability in IAD assessment metrics.
Conclusion
Bayesian network meta-analysis in this investigation confirmed significant IAD improvement effects from various physical and mental exercise modalities among young adults, with mindfulness demonstrating particularly robust efficacy. Analysis revealed a distinct U-shaped dose-response correlation between exercise interventions and IAD symptom amelioration. The identified optimal intervention dosage approximates 730 MET minutes weekly. Exercise regimens below 150 MET minutes weekly yield limited benefits with substantial variability, while dosages exceeding 1,100 MET minutes weekly exhibit diminishing marginal returns. Results underscore the critical importance of moderate activity levels for IAD improvement, as excessive exercise potentially diminishes intervention effectiveness through induced fatigue and physiological stress responses. These findings provide valuable guidance for developing evidence-based exercise intervention protocols, optimizing methodological approaches and dosage parameters, and elucidating underlying mechanisms through which physical-mental exercise mitigates IAD symptomatology in subsequent research initiatives.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
SJ: Conceptualization, Investigation, Software, Visualization, Writing – original draft, Writing – review & editing. HaoW: Software, Visualization, Writing – original draft. DC: Investigation, Methodology, Writing – original draft. JY: Methodology, Visualization, Writing – original draft. HaozW: Investigation, Software, Writing – original draft. WC: Methodology, Validation, Writing – original draft, Writing – review & editing. DZ: Investigation, Project administration, Writing – original draft. WZ: Formal analysis, Software, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1670168/full#supplementary-material
References
1. Shaw, M, and Black, DW. Internet addiction: definition, assessment, epidemiology and clinical management. CNS Drugs. (2008) 22:353–65. doi: 10.2165/00023210-200822050-00001
2. Manus, J-M. DSM-5-TR diagnostic and statistical manual of mental disorders. Revue Francophone Des Laboratoires. (2024) 2024:14. doi: 10.1016/s1773-035x(24)00069-8
3. Meng, SQ, Cheng, JL, Li, YY, Yang, XQ, Zheng, JW, Chang, XW, et al. Global prevalence of digital addiction in general population: a systematic review and meta-analysis. Clin Psychol Rev. (2022) 92:102128. doi: 10.1016/j.cpr.2022.102128
4. Stockdale, L, and Coyne, SM. Video game addiction in emerging adulthood: cross-sectional evidence of pathology in video game addicts as compared to matched healthy controls. J Affect Disord. (2018) 225:265–72. doi: 10.1016/j.jad.2017.08.045
5. Takeuchi, H, Taki, Y, Hashizume, H, Asano, K, Asano, M, Sassa, Y, et al. Impact of videogame play on the brain's microstructural properties: cross-sectional and longitudinal analyses. Mol Psychiatry. (2016) 21:1781–9. doi: 10.1038/mp.2015.193
6. Hossin, MZ, Islam, A, Billah, M, Haque, M, and Uddin, J. Is there a gradient in the association between internet addiction and health? PLoS One. (2022) 17:e0264716. doi: 10.1371/journal.pone.0264716
7. Chang, CH, Chang, YC, Yang, L, and Tzang, R-F. The comparative efficacy of treatments for children and young adults with internet addiction/internet gaming disorder: an updated meta-analysis. Int J Environ Res Public Health. (2022) 19:2612. doi: 10.3390/ijerph19052612
8. Király, O, Potenza, MN, Stein, DJ, King, DL, Hodgins, DC, Saunders, JB, et al. Preventing problematic internet use during the COVID-19 pandemic: consensus guidance. Compr Psychiatry. (2020) 100:152180. doi: 10.1016/j.comppsych.2020.152180
9. Zhu, S, Zhuang, Y, Lee, P, Li, JC-M, and Wong, PWC. Leisure and problem gaming behaviors among children and adolescents during school closures caused by COVID-19 in Hong Kong: quantitative cross-sectional survey study. JMIR Serious Games. (2021) 9:e26808. doi: 10.2196/26808
10. Throuvala, MA, Griffiths, MD, Rennoldson, M, and Kuss, DJ. School-based prevention for adolescent internet addiction: prevention is the key. A systematic literature review. Curr Neuropharmacol. (2019) 17:507–25. doi: 10.2174/1570159X16666180813153806
11. Kuss, DJ, and Lopez-Fernandez, O. Internet addiction and problematic internet use: a systematic review of clinical research. World J Psychiatry. (2016) 6:143–76. doi: 10.5498/wjp.v6.i1.143
12. King, DL, Delfabbro, P, Wu, AMS, Doh, YY, Kuss, DJ, Pallesen, S, et al. Treatment of internet gaming disorder: an international systematic review and CONSORT evaluation. Clin Psychol Rev. (2017) 54:123–33. doi: 10.1016/j.cpr.2017.04.002
13. Arya, S, Kaji, AH, and Boermeester, MA. PRISMA reporting guidelines for meta-analyses and systematic reviews. JAMA Surg. (2021) 156:789–90. doi: 10.1001/jamasurg.2021.0546
14. Higgins, J, Thomas, J, Chandler, J, Cumpston, M, Li, T, and Page, MJ. Cochrane handbook for systematic reviews of interventions. 2nd ed. Chichester (UK): John Wiley & Sons, Ltd (2019).
15. López-Valenciano, A, Mayo, X, Liguori, G, Copeland, R, Lamb, M, and Jiménez, A. Changes in sedentary behaviour in European Union adults between 2002 and 2017. BMC Public Health. (2020) 20:1–10. doi: 10.1186/s12889-020-09293-1
16. Herrmann, SD, Willis, EA, Ainsworth, BE, Barreira, TV, Hastert, M, Kracht, CL, et al. 2024 adult compendium of physical activities: a third update of the energy costs of human activities. J Sport Health Sci. (2024) 13:6–12. doi: 10.1016/j.jshs.2023.10.010
17. American College of Sports Medicine. ACSM's guidelines for exercise testing and prescription Lippincott Williams & Wilkins (2013).
18. Wasfy, MM, and Baggish, AL. Exercise dose in clinical practice. Circulation. (2016) 133:2297–313. doi: 10.1161/CIRCULATIONAHA.116.018093
19. Wang, D, and Zhang, P. Meta analysis of the effect of different forms of exercise on the prevention and treatment of carotid atherosclerosis. Sports Sci. (2019) 39:75–87.
20. Zhang, T, Dong, S, and Zhou, Z. Advanced meta analysis method. Shanghai: Fudan University Press.
21. Liu, Y, Li, L, Ma, Y, Liang, Z, Sun, Z, Cui, J, et al. Meta analysis of the incidence of internet addiction among Chinese college students. Chin J Evid Based Med. (2021) 21:61–8.
22. Wu, Y, Chen, L, Yu, Z, and Liu, Y. Meta analysis of the effect of exercise on the prevention and treatment of non-alcoholic fatty liver disease. Fujian Sports Sci Technol. (2020) 39:1–8.
23. Bürkner, PC. Advanced Bayesian multilevel modeling with the R package brms. R J. 10:395. doi: 10.32614/RJ-2018-017
24. Etzioni, RD, and Kadane, JB. Bayesian statistical methods in public health and medicine. Annu Rev Public Health. (1995) 16:23–41. doi: 10.1146/annurev.pu.16.050195.000323
25. Williams, D. R., Rast, P., and Bürkner, P. C. Bayesian meta-analysis with weakly informative prior distributions. (2018).
26. Betancourt, M, and Girolami, M. Hamiltonian Monte Carlo for hierarchical models In: Current trends in Bayesian methodology with applications, vol. 79 (2015). 2–4.
27. Brooks, SP, and Gelman, A. General methods for monitoring convergence of iterative simulations. J Comput Graph Stat. (1998) 7:434–55. doi: 10.1080/10618600.1998.10474787
28. Yang, CY, and Zeng, GF. Effects of Tai Chi exercise on internet addiction among college students. Chin J Sch Health. (2017) 38:292–4.
29. Zhang, X, Yang, H, Zhang, K, Zhang, J, Xiaoyan, L, Guo, H, et al. Effects of exercise or tai chi on Internet addiction in college students and the potential role of gut microbiota: A randomized controlled trial. J Affect Disord. (2023) 327:404–15. doi: 10.1016/j.jad.2023.02.002
30. Xiao, T, Jiao, C, Yao, J, Yang, Z, Liu, S, et al. Effects of basketball and Baduan exercise interventions on problematic smartphone use and mental health among college students: a randomized controlled trial. Evid Based Complement Alternat Med. (2021) 2021:8880716. doi: 10.1155/2021/8880716
31. Zhang, K, Guo, H, Zhang, X, Yang, H, Yuan, G, Zhu, Z, et al. Effects of aerobic exercise or Tai Chi Chuan interventions on problematic mobile phone use and the potential role of intestinal flora: a multi-arm randomized controlled trial. J Psychiatr Res. (2024) 170:394–407. doi: 10.1016/j.jpsychires.2023.12.032
32. Lan, Y, Ding, JE, Li, W, Li, J, Zhang, Y, Liu, M, et al. A pilot study of a group mindfulness-based cognitive-behavioral intervention for smartphone addiction among university students. J Behav Addict. (2018) 7:1171–6. doi: 10.1556/2006.7.2018.103
33. Ren, JH, Ao, ZH, He, CL, Bo, L, and Jiawei, W. Experimental Study on Sports Intervention for Internet Addiction in College Students [J]. Heilongjiang Med Sci. (2014) 37:93–4.
34. Xie, F. Status of mobile phone addiction among nursing students and intervention research using Baduanjin health education Shanxi Medical University (2019).
35. Zhang, Y. Research on the relationship between college students’ mobile phone dependence and physical health and exercise intervention Gannan Normal University (2018).
36. Liu, SJ, Liu, YN, and Wang, L. An empirical study on exercise intervention and group cognitive therapy for college students’ mobile phone dependence. Chin J Sch Health. (2022) 43:825–9.
37. Li, Y. Effects of mindfulness training on response inhibition in college students with mobile phone addiction Guizhou Medical University (2022).
38. Lu, C, Zou, L, Becker, B, Mark, DG, Yu, Q, Chen, S-T, et al. Comparative effectiveness of mind-body exercise versus cognitive behavioral therapy for college students with problematic smartphone use: a randomized controlled trial[J]. Int J Ment Health Promot. (2020) 22:271–82. doi: 10.32604/IJMHP.2020.014419
39. Yang, C. Experimental Study on the Effect of Aerobic Fitness and Badminton on Moderate Cell Phone Addiction in Vocational School Students[D] Yangzhou University (2022) doi: 10.27441/d.cnki.gyzdu.2022.000378
40. Dai, Y. A Randomized Controlled Study of Mindfulness Training to Reduce Mobile Phone Dependence Level in Mobile Phone Dependents[D] Zhejiang Normal University (2018).
41. Liu, SJ. Research on the Intervention Effect of Different Motor Skills and Group Cognition on College Students’ Mobile Phone Dependence[D] Wuhan University of Technology (2019) doi: 10.27381/d.cnki.gwlgu.2019.001621
42. Zhang, X. Study on the Influence and Intervention of Junior Middle School Students’ Perceived Social Support and Loneliness on Mobile Phone Dependence[D] Hebei University (2021) doi: 10.27103/d.cnki.ghebu.2021.001962
43. Yang, YF. Research on the Influence of College Students’ Mobile Phone Psychological Craving on Mobile Phone Addiction and Addiction Intervention[D] Jiangnan University (2021) doi: 10.27169/d.cnki.gwqgu.2021.001830
44. Yu, L, Xia, JM, and Lei, Y. Research on the comprehensive intervention of aerobic exercise on female college students’ mobile phone addiction[J]. Sichuan Sports Sci. (2023) 42:70–3. doi: 10.13932/j.cnki.sctykx.2023.06.15
45. Liao, ZY, Mai, ZZF, and Chen, ZJ. Effects of basketball and aerobic exercise intervention on improving smartphone addiction symptoms and mental health of college students[J]. Sports Sci Technol Lit Bull. (2022) 30:160–162,171. doi: 10.19379/j.cnki.issn.1005-0256.2022.06.043
46. Zhu, GF. Research on physical exercise intervention for college students’ mobile phone addiction tendency[J]. Zhejiang Sports Sci. (2017) 39:90–7.
47. Tadpatrikar, A, Sharma, MK, Bhargav, H, et al. Yoga as an adjuvant with multimodal psychological interventions for excessive use of technology: a randomized controlled trial from India[J]. Int J Yoga. (2024) 17:37–45. doi: 10.4103/ijoy.ijoy_187_23
48. Wu, Q, Shen, Y, Yuan, QQ, Qiu, J, and Li, Y. The impact of mindfulness intervention on adolescent patients with internet game addiction [J]. Huaxia Medical. (2023) 36:169–72. doi: 10.19296/j.cnki.1008-2409.2023-032-32
49. Wang, X, Cheng, ZH, Peng, Y, and Niu, C. A Study on the Intervention of Mindfulness Cognitive Therapy in Improving Anxiety and Depression in College Students with Mobile Phone Addiction [J]. Psychology Monthly. (2024) 19:69–73. doi: 10.19738/j.cnki.psy.2024.19.019
50. Ren, WL. The Intervention Effect of Mindfulness Training on High School Students’ Mobile Game Addiction [D] Hebei North University (2020) doi: 10.27767/d.cnki.ghbbf.2020.000192
51. Shen, YF. The Effect of Mindfulness Training on Attentional Bias in College Students with Mobile Phone Dependence[D] North China University of Science and Technology (2022) doi: 10.27108/d.cnki.ghelu.2022.000031
52. Higgins, JPT. Commentary: Heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol. (2008) 37:1158–60. doi: 10.1093/ije/dyn204
53. Guyatt, G, Oxman, AD, Kunz, R, Woodcock, J, Brozek, J, Helfand, M, et al. GRADE guidelines: 7. Rating the quality of evidence—inconsistency. J Clin Epidemiol. (2011) 64:1294–302. doi: 10.1016/j.jclinepi.2011.03.017
54. Bull, F, Al-Ansari, SS, Biddle, SJH, Bull, FC, Biddle, S, Borodulin, K, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. (2020) 54:1451–62. doi: 10.1136/bjsports-2020-102955
55. Tang, YY, Hölzel, BK, and Posner, MI. The neuroscience of mindfulness meditation[J]. Nat Rev Neurosci. (2015) 16:213–25. doi: 10.1038/nrn3916
56. Hölzel, BK, Carmody, J, Vangel, M, Congleton, C, Yerramsetti, SM, Gard, T, et al. Mindfulness practice leads to increases in regional brain gray matter density[J]. Psychiatry Res Neuroimaging. (2011) 191:36–43. doi: 10.1016/j.pscychresns.2010.08.006
57. Khoury, B, Sharma, M, Rush, SE, and Fournier, C. Mindfulness-based stress reduction for healthy individuals: A meta-analysis[J]. J Psychosom Res. (2015) 78:519–28. doi: 10.1016/j.jpsychores.2015.03.009
58. Vago, DR, and Silbersweig, DA. Self-awareness, self-regulation, and self-transcendence (S-ART): a framework for understanding the neurobiological mechanisms of mindfulness[J]. Front Hum Neurosci. (2012) 6:296. doi: 10.3389/fnhum.2012.00296
59. Song, QH, Shen, GQ, Xu, RM, et al. Effect of Tai Chi exercise on the physical and mental health of the elder patients suffered from anxiety disorder[J]. Int J Physiol Pathophysiol Pharmacol. (2014) 6:55.
60. Wang, C, Bannuru, RR, Ramel, J, Kupelnick, B, Scott, T, and Schmid, CH. Tai Chi on psychological well-being: systematic review and meta-analysis[J]. BMC Complement Altern Med. (2010) 10:1–16. doi: 10.1186/1472-6882-10-23
61. Wei, G-X, Xu, T, Fan, F, Dong, H-M, Jiang, L, Li, H-J, et al. Can Taichi reshape the brain? A brain morphometry study[J]. PloS one. (2013) 8:e61038. doi: 10.1371/journal.pone.0061038
62. Zou, L, Pan, Z, Yeung, A, et al. A review study on the beneficial effects of Baduan**[J]. J Altern Complement Med. (2018) 24:324–35. doi: 10.1089/acm.2017.0241
63. Pascoe, MC, Thompson, DR, and Ski, CF. Yoga, mindfulness-based stress reduction and stress-related physiological measures: A meta-analysis[J]. Psychoneuroendocrinology. (2017) 86:152–68. doi: 10.1016/j.psyneuen.2017.08.008
64. Streeter, CC, Whitfield, TH, Owen, L, Rein, T, Karri, SK, Yakhkind, A, et al. Effects of yoga versus walking on mood, anxiety, and brain GABA levels: a randomized controlled MRS study[J]. J Altern Complement Med. (2010) 16:1145–52. doi: 10.1089/acm.2010.0007
65. Field, T, Diego, M, Delgado, J, and Medina, L. Yoga and social support reduce prenatal depression, anxiety and cortisol[J]. J Bodyw Mov Ther. (2013) 17:397–403. doi: 10.1016/j.jbmt.2013.03.010
66. Fox, KCR, Nijeboer, S, Dixon, ML, Fox, KC, Floman, JL, Ellamil, M, et al. Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners[J]. Neurosci Biobehav Rev. (2014) 43:48–73. doi: 10.1016/j.neubiorev.2014.03.016
67. Li, W, Garland, EL, McGovern, P, O’Brien, JE, Tronnier, C, and Howard, MO. Mindfulness-oriented recovery enhancement for internet gaming disorder in US adults: A stage I randomized controlled trial[J]. Psychol Addict Behav. (2017) 31:393–402. doi: 10.1037/adb0000269
68. Chen, P, Wang, D, Shen, H, Yu, L, Gao, Q, Mao, L, et al. Physical activity and health in Chinese children and adolescents: expert consensus statement (2020). Br J Sports Med. (2020) 54:1321–31. doi: 10.1136/bjsports-2020-102261
69. Du, Z, and Zhang, X. Analysis of the mediating effects of self-efficacy and self-control between physical activity and internet addiction among Chinese college students[J]. Front Psychol. (2022) 13:1002830. doi: 10.3389/fpsyg.2022.1002830
70. Hu, J. Neuropsychological Mechanisms and Evidence of Mindfulness-Based Interventions for Addiction. J Educ Human Soc Sci. (2023) 8:904–908. doi: 10.54097/ehss.v8i.4379
71. Matei, D, Trofin, D, Iordan, DA, Onu, I, Condurache, I, Ionite, C, et al. The Endocannabinoid System and Physical Exercise. Int J Mol Sci. (2023) 24:1989. doi: 10.3390/ijms24031989
72. Sleiman, SF, Henry, J, Al-Haddad, R, et al. Exercise promotes the expression of brain derived neurotrophic factor (BDNF) through the action of the ketone body β-hydroxybutyrate. eLife. (2016) 5:e15092. doi: 10.7554/elife.15092
73. Khoury, B, Knäuper, B, Schlosser, M, Carrière, K, and Chiesa, A. Effectiveness of traditional meditation retreats: A systematic review and meta-analysis[J]. J Psychosom Res. (2016) 92:16–25. doi: 10.1016/j.jpsychores.2016.11.006
74. Wong, HY, Mo, HY, Potenza, MN, Chan, MNM, Lau, WM, Chui, TK, et al. Relationships between severity of internet gaming disorder, severity of problematic social media use, sleep quality and psychological distress[J]. Int J Environ Res Public Health. (2020) 17:1879. doi: 10.3390/ijerph17061879
75. Tang, YY, Tang, R, and Posner, MI. Mindfulness meditation improves emotion regulation and reduces drug abuse[J]. Drug Alcohol Depend. (2016) 163:S13–8.
76. Zhang, JY, Ji, XZ, Meng, LN, and Cai, YJ. Effects of modified mindfulness-based stress reduction (MBSR) on the psychological health of adolescents with subthreshold depression: a randomized controlled trial[J]. Neuropsychiatr Dis Treat. (2019):2695–704. doi: 10.2147/NDT.S216401
77. Stevens, MWR, King, DL, Dorstyn, D, Dorstyn, N, and Delfabbro, PH. Cognitive–behavioral therapy for Internet gaming disorder: A systematic review and meta-analysis[J]. Clin Psychol Psychother. (2019) 26:191–203. doi: 10.1002/cpp.2341
78. Garland, EL, and Howard, MO. Mindfulness-based treatment of addiction: current state of the field and envisioning the next wave of research[J]. Addict Sci Clin Pract. (2018) 13:1–14.
79. Yao, YW, Chen, PR, Chiang-shan, RL, et al. Combined reality therapy and mindfulness meditation decrease intertemporal decisional impulsivity in young adults with Internet gaming disorder[J]. Comput Human Behav. (2017) 68:210–6. doi: 10.1016/j.chb.2016.11.038
80. Liu, J, Nie, J, and Wang, Y. Effects of Group Counseling Programs, Cognitive Behavioral Therapy, and Sports Intervention on Internet Addiction in East Asia: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. (2017) 14:1470–19. doi: 10.3390/ijerph14121470
81. Li, S, Qianjin, W, Tang, C, et al. Exercise-Based Interventions for Internet Addiction: Neurobiological and Neuropsychological Evidence. Front Psychol. (2020) 11:1296. doi: 10.3389/fpsyg.2020.01296
82. Chen, H, Dong, G, and Li, K. Overview on brain function enhancement of Internet addicts through exercise intervention: Based on reward-execution-decision cycle. Front Psych. (2023) 14:1094583. doi: 10.3389/fpsyt.2023.1094583
83. Brand, M, Young, K, Laier, C, Wölfling, K, and Potenza, MN. Integrating psychological and neurobiological considerations regarding the development and maintenance of specific Internet-use disorders: An Interaction of Person-Affect-Cognition-Execution (I-PACE) model. Neurosci Biobehav Rev. (2016) 71:252–266. doi: 10.1016/j.neubiorev.2016.08.033
Keywords: internet addiction disorder, physical and mental exercise, dose-response relationship, young adults, exercise intervention
Citation: Jia S, Wang H, Chu D, Yao J, Wang H, Chen W, Zhang D and Zhang W (2025) The intervention effect of physical and mental exercise on young adults internet addiction disorder: a systematic review and Bayesian model analysis. Front. Public Health. 13:1670168. doi: 10.3389/fpubh.2025.1670168
Edited by:
Chaoxin Jiang, East China Normal University, ChinaReviewed by:
Teruhisa Uwatoko, Kyoto University of Education, JapanEmad Amkhatirah, Central South University, China
Copyright © 2025 Jia, Wang, Chu, Yao, Wang, Chen, Zhang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenjia Chen, Mjc3NDYzODI4QHFxLmNvbQ==; Dazhong Zhang, NTc4Nzg3NjI5QHFxLmNvbQ==; Wenzhong Zhang, NTY0MDM3NTI0QHFxLmNvbQ==
 Shiguan Jia
Shiguan Jia Hao Wang2
Hao Wang2 Wenjia Chen
Wenjia Chen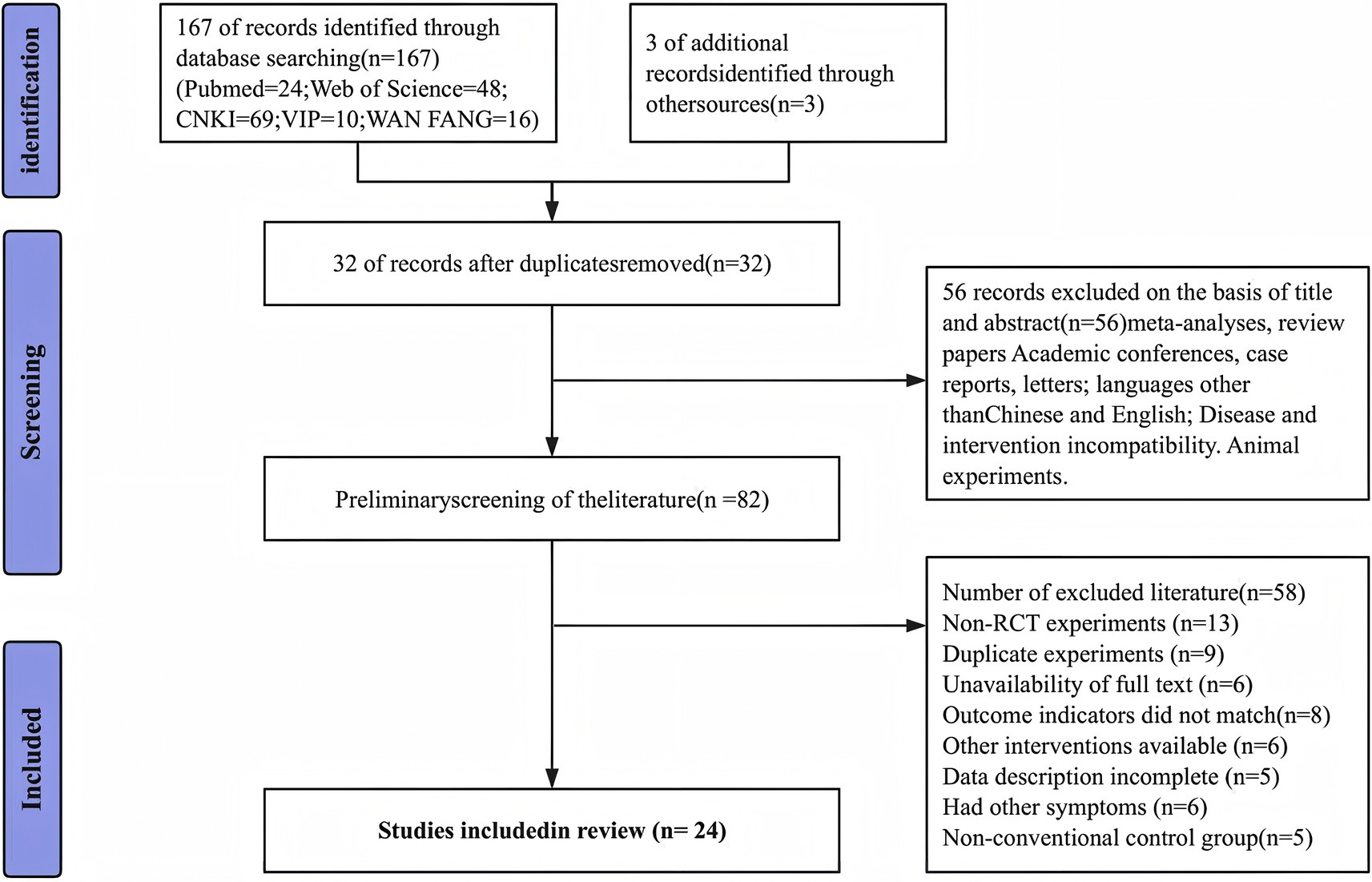
![Forest plot displaying a meta-analysis of 24 studies comparing experimental and control groups. The plot shows individual study results, standard mean differences, and confidence intervals. A diamond at the bottom indicates the overall effect size, favoring the experimental group with a standardized mean difference of -1.63, 95% CI [-2.04, -1.22]. Heterogeneity is reported with Tau² = 0.90, Chi² = 273.91, df = 23, I² = 92%. The test for overall effect shows Z = 7.77 (P < 0.00001), suggesting significant findings.](https://www.frontiersin.org/files/Articles/1670168/fpubh-13-1670168-HTML/image_m/fpubh-13-1670168-g004.jpg)