- 1Centre for Positive Health Sciences, RCSI University of Medicine and Health Sciences, Dublin, Ireland
- 2Department of Political Science, Faculty of Law, Economics, Political and Administrative Sciences, “Petre Andrei” University of Iași, Iași, Romania
- 3National Institute for Research & Development in Informatics – ICI, Bucharest, Romania
- 4ADV, Alături de Voi Foundation, Iași, Romania
- 5Research Institute for Quality of Life – Romanian Academy, Bucharest, Romania
Introduction: There is growing interest and demand for leveraging digital technology to enhance the reach and scalability of health and wellbeing interventions, as a solution to the global burden of noncommunicable diseases. For positive health sciences, digital technology has been identified as a feasible solution to increasing the accessibility, scalability and reach of positive health interventions. While digital health solutions have the potential to improve the health and wellbeing of communities and reduce the burden on health systems, these solutions often take a one-size-fits-all approach in their design and implementation. This study aimed to conduct a Community-Based Participatory Research (CBPR) informed needs assessment in Athy (Ireland) and Iași (Romania) to identify lifestyle-related health challenges, barriers, and digital engagement preferences in preparation for implementing the Connect5 digital health coaching intervention.
Methods: A mixed-methods cross-sectional design was employed, involving quantitative surveys (n = 219 in Ireland; n = 205 in Romania) and qualitative interviews/focus groups. Surveys assessed sociodemographic characteristics, lifestyle habits, barriers, support needs, and digital health perspectives.
Results: Both communities reported challenges with sleep, physical activity, sedentary behavior, and stress, with common barriers including lack of time (due to work/study/childcare) and the high cost of healthy food. Notable variations in lifestyle needs, barriers, and support preferences were observed across sociodemographic groups within each community, including gender, age, education, and residency. Lower socioeconomic groups faced more systemic barriers like high food costs or lack of safe outdoor spaces. Despite different levels of prior engagement with digital solutions, both communities showed strong interest in digital health coaching solutions.
Discussion: The findings from this needs assessment will inform the design and implementation of the upcoming Connect5 project and provide broader insights for future digital health initiatives. They highlight the importance of integrating community voices and sociodemographic insights to ensure that digital health solutions are relevant, inclusive, and equitable, ultimately promoting sustained engagement, reducing health disparities, and improving population wellbeing.
1 Introduction
Leveraging digital technologies is vital for achieving universal health coverage, enhancing health promotion, and serving disadvantaged populations (1). Moreover, digital technology offers a promising solution to combat the global burden of noncommunicable disease (NCDs) (2–4), which are responsible for 41 million deaths annually, accounting for 70% of all global deaths, and 40% of premature deaths among individuals under 70 years (5, 6). NCDs such as cardiovascular disease, type-2 diabetes mellitus, chronic respiratory diseases and certain cancers are largely preventable through the elimination of lifestyle risk factors like tobacco use, poor nutrition, low physical inactivity, and alcohol use (5, 7, 8), making health promotion interventions particularly effective for tackling the global NCD burden. Despite significant investments and advancements in health promotion interventions, progress has been slow, with only a 2% global reduction in premature deaths recorded between 2010 and 2019 (9). This limited progress may be partly due to the scalability and accessibility constraints of traditional health promotion efforts, especially when targeting hard-to-reach and vulnerable populations (10–12).
Digital technologies can help overcome these limitations by providing scalable, accessible, cost-effective, and equitable health promotion and disease prevention interventions (1, 13). The integration of digital technologies across various sectors of health and wellbeing is catalyzing transformative change toward more accessible and equitable services that address the NCD burden at a lower cost (14–16). Recognized by the World Health Organization (WHO) as a key enabler of the Sustainable Development Goals (1, 3), this transformative shift toward digital health has sparked a digital revolution within healthcare systems (17). Digital health technologies, like smartphone applications and wearable devices, are gaining popularity and show strong potential for supporting lifestyle changes and chronic disease management (4, 18–20). Key advantages include personalized real-time support, convenience, accessibility, broad reach, scalability, security, efficiency, effortless access to evidence-based educational materials, and proven efficacy (18). Together, these innovations present a powerful opportunity to transform how health promotion, prevention, and chronic disease management are delivered. Notably, one emerging field that stands to benefit significantly from these digital advancements is positive health sciences; a holistic and multidimensional field of research which takes the care continuum past the point of absence of disease and focuses on the knowledge, skills, and empowerment required for individuals and communities to thrive (21).
Positive Health Sciences (PHS) is deeply rooted in the theoretical foundations of positive psychology (22), lifestyle medicine (23), and health psychology (21, 24, 25). PHS is also grounded in the emerging concept of meliotropism that describes the dynamic orientation and tendency of human beings toward meaningful, prosocial, health-promoting actions that benefit individuals and communities alike (26). PHS provides a range of positive health interventions that aim to build a person’s meliotropic orientation toward positive health; most notably, positive health coaching (PHC). PHC has been developed to effectively translate positive health science and research into a feasible intervention that can support individuals to make changes for better health (27, 28). However, like many health promotion and disease prevention approaches, PHC faces challenges related to scalability and accessibility. In response, researchers are increasingly exploring digital technologies as a means to broaden the reach and impact of positive health interventions.
We have previously tested the integration of digital technologies and PHS through a coach-led digital positive health intervention for Irish-based hospital workers during the COVID-19 pandemic, called RCSI Coach Connect (25, 29, 30). This digital health solution yielded positive engagement, improved health (related to the pillars of lifestyle medicine), and mitigated burnout among 23 hospital workers (29). Building on the feasibility of this positive health intervention, we are now in the process of developing a digital initiative for community implementation that we call Connect5.
The Connect5 project is a community-based study that aims to effectively support positive health changes in communities by implementing a human coach-led digital health solution. We hope to implement PHC in a way that is both scalable, accessible and meaningful to the community. This solution will be designed using the theoretical foundations of PHS and delivered through PHC via a digital health smartphone application. However, researchers have highlighted the limitations and risks of adopting a one-size-fits-all approach to digital interventions (31–33). They emphasize the importance of accounting for the distinct socioeconomic and environmental factors that shape health and wellbeing in each community, and the need to embed these considerations into the design of community-based interventions (32–34).
Digital health provision can both revolutionize the delivery of health interventions, empower individuals and promote agency, but also risks isolating and excluding certain populations and groups (32, 33, 35, 36). The WHO (2021) has highlighted that while digital technologies are rapidly advancing to improve access to care, this is not sustainable or equitable across all populations and groups. Digitally excluded groups include older adults, socioeconomically disadvantaged populations, rural communities, ethnic and racial minority groups, and individuals with low digital literacy (32, 35–37). There is a clear digital divide that is crucial to bridge to ensure equitable and meaningful access to digital health (1). Research has highlighted the importance of contextually sensitive digital health technology as a solution for bridging this divide (33, 38). This approach advocates for the move away from a techno-deterministic design focus to one that is more contextually informed. Contextually sensitive technology essentially considers sociocultural factors in the design of digital health interventions to ensure technology is appropriate for communities and is meeting their specific health needs (33).
To address these challenges in digital health, a Community-Based Participatory Research (CBPR) informed approach to project design and implementation will be adopted for the design and implementation of Connect5. CBPR is a method of research that places vital community stakeholders at the center of research, using their experiential knowledge to co-create the research framework and health interventions alongside researchers and other health experts, where all stakeholders carry equal weighting (39–41). CBPR also emphasizes viewing the community as a dynamic social entity, rather than just a research cohort (40, 41). This approach provides a framework for understanding how these dynamic social entities, influenced by its specific socioeconomic and environmental determinants, defines health priorities and needs. As such, allowing researchers to co-design health promotion and prevention interventions according to the context and preferences of the targeted communities.
To deliver a digital health intervention tailored to the needs of the Connect5 target communities, this study conducted a parallel CBPR-informed needs assessment in Athy, Co. Kildare (Ireland) and Iași (Romania). The objectives were to explore community members’ health and wellbeing habits, needs, and barriers, and to gather perspectives on digital technology and positive health coaching to inform the implementation of the Connect5 intervention at each site. Based on the literature, the following research questions guided the assessment:
1. What are the primary health and wellbeing challenges and unmet needs in each target community?
2. What are community members’ current levels of engagement with, and attitudes toward, digital health technologies?
3. How do community members perceive positive health coaching, and what preferences do they have for coaching delivery methods?
2 Materials and methods
2.1 Setting
Two communities were selected for this study; Athy in Ireland, and Iasi in Romania. Athy is a rural community with a population of 10,837 people according to the 2022 National census (Central Statistics Office, 2022). Iași on the other hand, is the fourth largest city in Romania, the metropolitan area including Iași city plus 19 surrounding communes has a population of 423,154 according to the 2021 Romanian national census (National Statistics Institute, 2021). The Irish needs assessment was conducted by the Centre of Positive Health Science at the Royal College of Surgeons in Ireland (RCSI) University of Medicine and Health Sciences, in conjunction with Kildare County Council and local Sláintecare Healthy Communities supports. The Romanian needs assessment was conducted by researchers working for Fundația Alături de Voi (ADV Romania), a charity organization that promotes social entrepreneurship among Romanian communities.
2.2 Ethics
Ethical approval for this study was obtained from the RCSI Research Ethics Committee, Dublin (Reference number: REC202210030). Written informed consent was obtained from all respondents prior taking part in the survey. Romanian respondents consented to the use of their anonymous data for research purposes as outlined by ADV Romania. In order to maintain anonymity, no identifiable information was collected during the survey data collection. Participants in interviews and focus groups were pseudonymized rather than anonymized to allow for data linkage and analysis while protecting their identities.
2.3 Study design
A quantitative cross-sectional study was used to assess the needs of residents in Athy in Ireland and Iași in Romania.
2.3.1 Quantitative needs assessment survey
A cross-sectional needs assessment survey was conducted to explore the health and lifestyle needs of individuals living, working, or engaging in activities in Athy, Ireland, and the metropolitan area of Iași, Romania. The survey was developed by the research team at the RCSI Centre for Positive Health Sciences in English and translated to Romanian by ADV Romania (Supplementary Table S9). The survey was developed as an exploratory tool to gather informal insights into lifestyle habits, barriers, and support needs, and was not intended or designed as a validated psychometric instrument. The Romanian version was translated by a bilingual subject expert and reviewed for clarity and cultural appropriateness, but no formal validation was performed, as the study did not aim to conduct country-to-country comparisons. The survey in both communities aimed to assess respondents’ socio-demographic characteristics, lifestyle habits, needs, and behaviors, structured around the pillars of lifestyle medicine: sleep, nutrition, physical activity, stress management, substance use, and social relationships, with the addition of meaning and purpose in life. In 2019, researchers reported the results of a cohort study of 6,985 American adults, which described how purpose in life was significantly associated with longer life- and health-span (42). This survey also used existing literature on standards of health according to these pillars to provide context participants completing the assessment. For example, the recommended target for sleep was 7–8 h per night (43), and the target for physical activity was 150 min of moderate-intensity activity (44). We also sought to gather insights into respondents’ engagement with technology, their perspectives on digital health solutions, and their interest in PHC. The questionnaire included both closed-ended questions, covering demographic background, lifestyle behaviors and needs, barriers to lifestyle changes and preferences for a smartphone-based health intervention. Open-ended questions were used to gather other barriers and solutions to lifestyle changes participants may have that were not in the predefined list.
2.4 Sample and recruitment
Residents of Athy and Iași who were over the age of 18 were invited to take part in the quantitative survey and qualitative interviews or focus groups. The Irish survey was disseminated by researchers at the Centre of Positive Health Science at RCSI, both online using secure Microsoft (MS) Forms and in hard copy at the local library and other local resource offices in Athy associated with Sláintecare Healthy Communities and Kildare County Council. The dissemination process was conducted in collaboration with officers and healthcare workers based at these two agencies in Ireland. To further broaden the reach, local online advertisement through Facebook was also used in Athy to target community members and to capture residents who may not be engaged with existing community support systems. The paid Facebook campaign was restricted to adults over 18 years residing and/or working in Athy and the surrounding hinterland (up to 5 Km).
The anonymous needs assessment survey was simultaneously distributed in Iași, Romania by the research group embedded within AVD Romania. The needs assessment was distributed online only through email or WhatsApp groups to the network of collaborators at AVD Romania and the Coalition of Organizations of Patients with Chronic Diseases in Romania (COPAC). Respondents were among the beneficiaries or clients of these collaborating institutions and non-governmental organizations (NGOs), as well as among their family members or friends.
2.5 Data collection and analysis
Anonymous survey data were collected in 2023 from completed online (MS Forms) or paper surveys distributed in both communities. Survey data were compiled in MS Excel, cleaned and analyzed using Stata 18.0 (45) and SPSS (46). All 59 categorical variables (5 sociodemographic variables, 12 lifestyle habits variables, 17 lifestyle barriers variables, 10 support with lifestyle variables and 15 digital health and coaching variables) were converted from string to numerical format, and descriptive statistics (frequencies and percentages) were calculated. For analysis, questions with more than three response options were grouped into two categories. For example, responses to the question with options “never, rarely, sometimes, often, and always” were consolidated into “never or rarely” and “sometimes, often, and always.” Additionally, for “yes,” “no,” and “I do not know” questions, if “I do not know” responses accounted for less than 5% of the total, they were recorded as empty cells. A global chi-square test of association was conducted to assess potential differences across sociodemographic groups in relation to lifestyle habits, lifestyle barriers, support needs, and perspectives on digital health coaching within each community.
It is important to note that given the differences in sampling, demographics, and cultural context, direct statistical comparisons between the Romanian and Irish communities were not feasible. Importantly, the primary aim of the study was to assess community-specific needs to inform targeted intervention design, rather than to conduct cross-community comparisons. Cross-country findings are not intended for direct comparison, but rather to highlight context-specific insights.
3 Results
3.1 Demographics
The Romanian and Irish surveys had 205 and 219 respondents, respectively. The socio-demographic characteristics of both communities are described in Table 1.
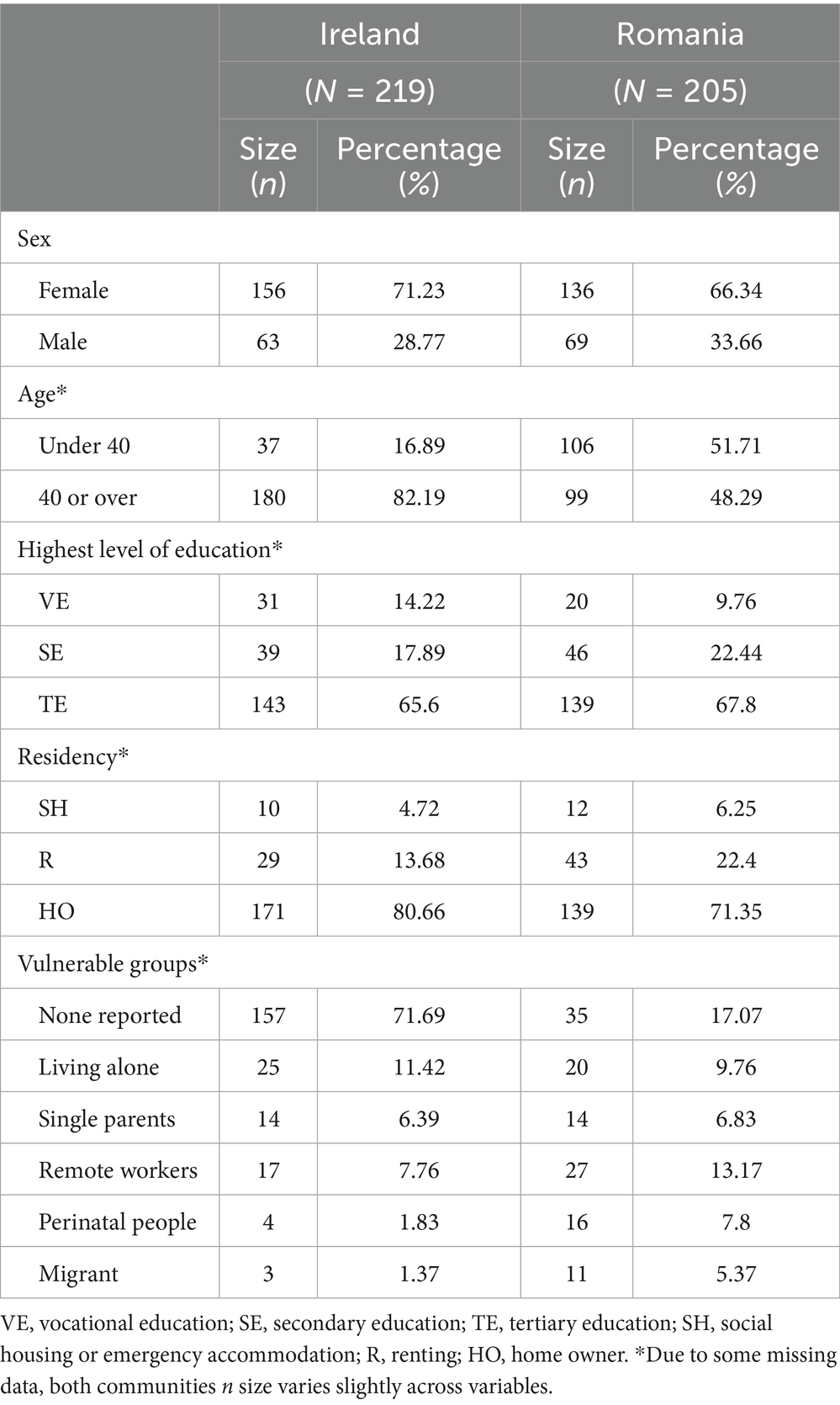
Table 1. Socio-demographic profile of participants in the study from Ireland (Athy) and Romania (Iasi).
3.1.1 Irish respondents
A total of 219 respondents completed the Irish questionnaire (Table 1). The majority of respondents were female (71%), aged 40 years or older (82%). A large proportion of respondents had attended third-level education (66%), while 18% had attended secondary school and 14% vocational school as the highest level of educational attainment. Eighty percent of respondents were homeowners, with a small proportion renting (14%) or living in social housing or emergency accommodation (5%). Finally, 28% of respondents reported belonging to one or more vulnerable groups (i.e., living alone, single parent, remote workers, perinatal people, or migrants).
3.1.2 Romanian respondents
Two hundred and five Iasi residents completed the Romanian questionnaire (Table 1). The majority of respondents were female (66%). The representation of respondents over and under 40 years old was marginally different (48 and 52%, respectively). In terms of highest level of education attained, 68% of respondents had attended third-level education, 22% attended secondary school, and 10% attended vocational school. Seventy-one percent of respondents were homeowners, 21% of the sample rented, and 6% were living in social housing or emergency accommodation. Finally, 83% of respondents reported belonging to one or more vulnerable groups.
3.2 Lifestyle-related findings
The needs assessment survey delivered in Athy, Ireland, and Iași, Romania, collected data to better understand the specific health and wellbeing needs of the two communities. Lifestyle-related findings provided insights into the percentage of respondents who meet the recommended guidelines of sleep, physical activity, healthy eating, social relationships, meaning and purpose in life, stress management, and substance use (Table 2). These findings also highlighted the barriers to engaging with lifestyle behaviors of the above areas, and what support is needed within the two communities (Tables 3, 4 respectively).
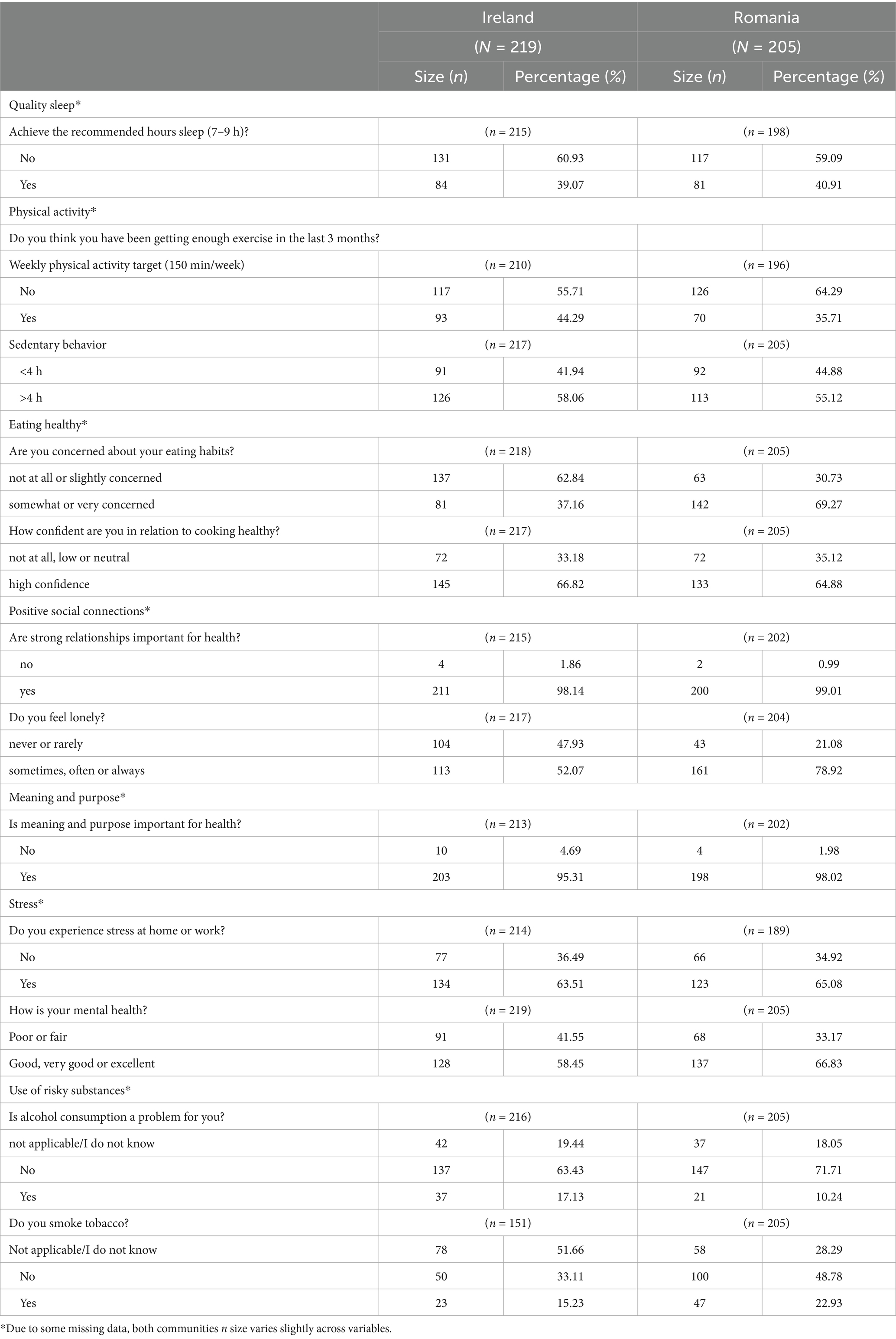
Table 2. Lifestyle habits and concerns related to the pillars of lifestyle medicine of participants in both communities, Ireland (Athy) and Romania (Iasi).
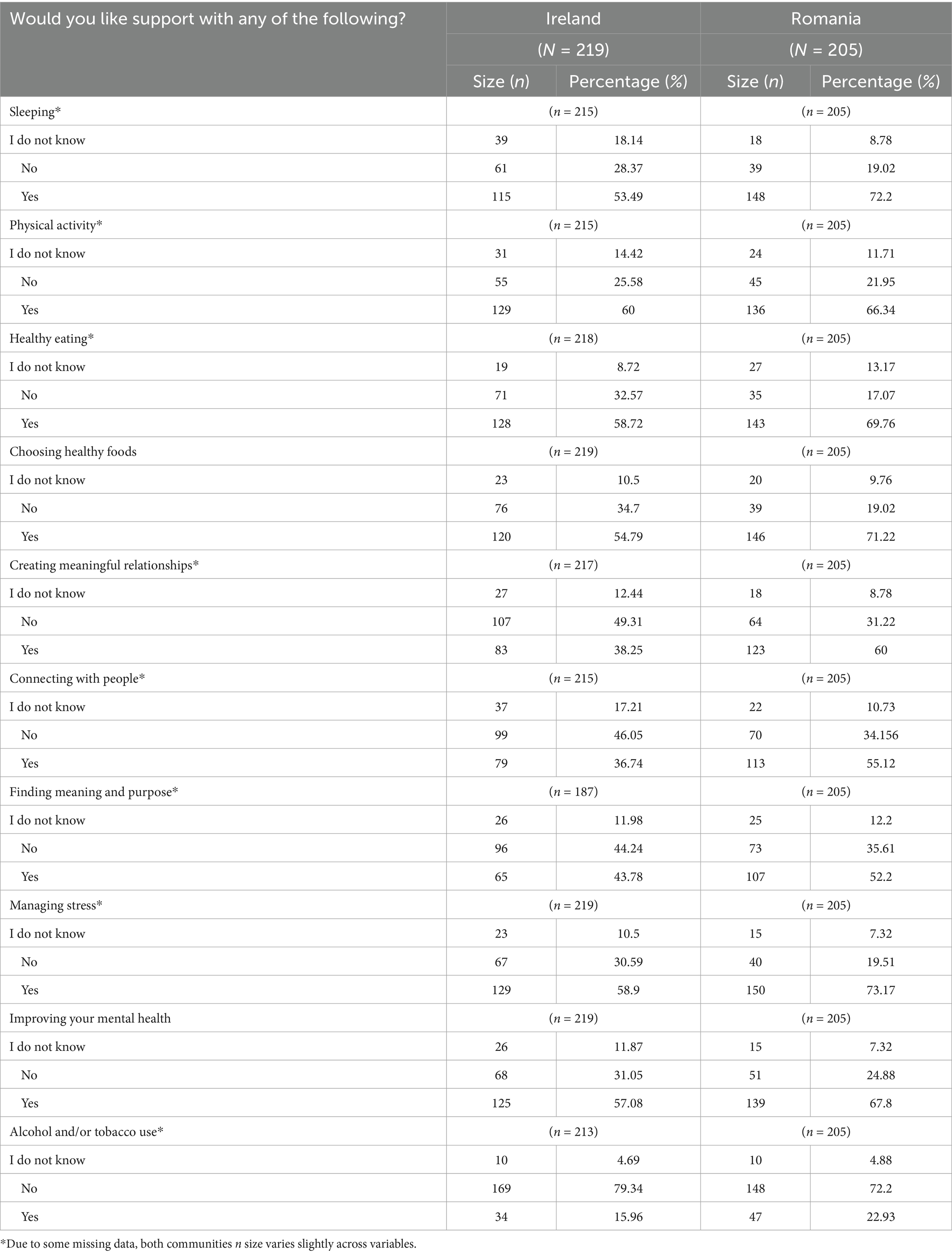
Table 3. Supports required by both communities, Athy in Ireland and Iasi in Romania, related to the pillars of lifestyle medicine.
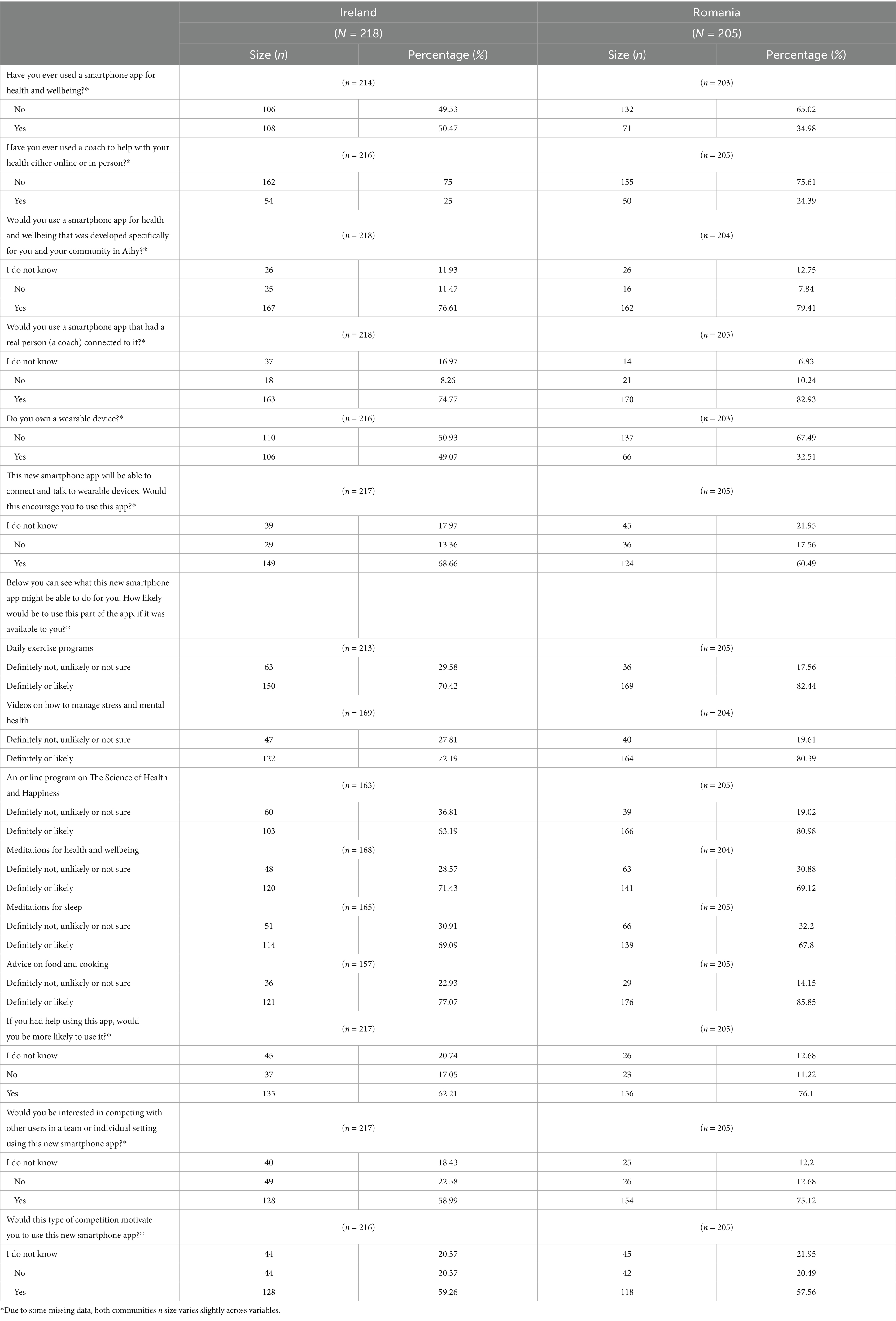
Table 4. Perspectives on digital health technology and Positive Health Coaching among participants from both communities, Ireland (Athy) and Romania (Iasi).
3.2.1 Athy, Ireland
Less than 40% of respondents from Athy achieved the recommended 7–9 h of sleep per night (Table 2). Over half (54%) did not meet physical activity targets, and 58% reported sedentary behavior of ≥4 h/day. In relation to nutrition and food habits, 63% were not concerned about their eating habits, though two-thirds (67%) expressed confidence in preparing healthy meals. Nearly all respondents valued relationships (98%) and having meaning and purpose (95%). However, 52% reported loneliness, 63% experienced stress at work or home, and only 58% rated their mental health as good to excellent. Seventeen percent consumed alcohol and 15% smoked tobacco.
Barriers to sleep, physical activity, and healthy eating were also assessed (Table S10). Key barriers to physical activity included low motivation (53%), lack of time due to work/study (41%) or caring responsibilities (18%), as well as fatigue, trauma, and safety concerns raised in open responses. Suggested solutions included affordable facilities, safer roads, child-friendly and flexible exercise options, and improved community initiatives. For healthy eating, high food costs (40%) and lack of time (40%) were the main barriers, with additional challenges including household food preferences (23%) and limited knowledge (11%). Sleep was most often affected by stress and worry (67%), followed by work (38%) and screen use (30%).
Barriers to sleep, physical activity, and healthy eating were also assessed (Supplementary Table S10). Key barriers to physical activity included low motivation (53%), lack of time due to work/study (41%) or caring responsibilities (18%), in addition to open responses (n = 12) citing fatigue (33%) and chronic pain or chronic disease (33%). Suggested solutions (n = 101) included safer roads and public spaces (20%), and improved community initiatives and access to exercise groups (10%). For healthy eating, high food costs (40%) and lack of time (40%) were the main barriers, with additional challenges including household food preferences (23%) and limited knowledge (11%). Sleep was most often affected by stress and worry (67%), followed by work (38%) and screen use (30%).
When asked about supports (Table 3), respondents expressed the greatest need for help with physical activity (60%), healthy eating (59%), stress (59%), mental health (57%), and sleep (53%). Fewer respondents sought support with social connection (36–44%) or substance use (16%).
3.2.2 Iași, Romania
In Iași, 41% of respondents achieved the recommended 7–9 h of sleep per night (Table 2). Most did not meet physical activity targets (61%) and over half (55%) reported ≥4 h/day of sedentary behavior. While 69% were concerned about their eating habits, 65% felt confident cooking healthy meals. Nearly all respondents valued relationships (99%) and purpose in life (98%). However, loneliness was common, with only 21% rarely or never experiencing it. Two-thirds reported stress at work/home (65%) and good to excellent mental health (67%). Finally, 10 and 23% of Romanian respondents consumed alcohol and smoked tobacco, respectively.
Like Athy, barriers to sleep, physical activity, and healthy eating were assessed (Table 3). Key barriers to physical activity included lack of time due to work/study (42%) or caring responsibilities (28%), and limited access to facilities (23%). Other challenges cited were lack of time (18%), and lack of adapted environments to exercise (16.5%). Suggested solutions included affordable gyms, community-based group activities, accessible facilities for those with health conditions.
For healthy eating, the main barrier was cost (66%), followed by lack of time to cook (32%), taste preferences (14%), and limited knowledge (12%). Respondents also mentioned difficulties accessing healthy produce and managing portion sizes. Stress and worry (58%) were the most common barriers to sleep, followed by work (43%), childcare (27%), and screen use (16%), alongside health problems and environmental factors.
Support needs were high across domains, with respondents seeking help for stress (73%), sleep (72%), healthy eating (70–71%), physical activity (66%), and mental health (68%). More than half also desired support with relationships (60%) and purpose in life (52%). Demand for lifestyle support was greater overall in the Romanian sample compared to the Irish sample (Table 3).
3.3 Lifestyle habits, barriers and support needs according to sociodemographic groups
3.3.1 Athy, Ireland
Gender and age differences were most pronounced in the Irish sample (Supplementary Tables S1–S3 for habits, barriers and required support respectively). Women were less likely to meet physical activity targets (61% vs. 37% of men, p = 0.004) and more often cited childcare as a barrier (23 and 7% respectively; p = 0.008). They also reported higher levels of loneliness (58% vs. 37%, p = 0.003) and stress (67% vs. 46%, p = 0.007).
Respondents under 40 were more likely to experience loneliness (76% vs. 47%, p = 0.002), while those over 40 had higher tobacco use (45% vs. 30%, p = 0.003). Younger participants reported lack of time due to work or study as a barrier to exercise, while older adults more often cited injury and disability.
By education and housing, mental health status and exercise barriers differed. Those in social housing reported poorer mental health (80% poor/fair vs. 39–48% in other groups, p = 0.031), and greater difficulty accessing safe outdoor spaces for exercise. In contrast, respondents with third-level education more often reported work or study as a barrier to exercise (Supplementary Table S2).
3.3.2 Iași, Romania
Significant differences in lifestyle habits and barriers were observed across gender, education and residency groups among Romanian respondents (Supplementary Tables S4–S6 for habits, barriers and required support respectively).
Alcohol and tobacco consumption rates were higher among men compared to women (alcohol: M = 23%, F = 4%, p = 0.000; tobacco use: M = 36%, F = 16%, p = 0.004). Additionally, a higher proportion of men reported TV and phones as a barrier to getting adequate sleep, and food not being enjoyed by family as a barrier to healthy eating, compared to women (M = 18%, F = 7%, p = 0.002; M = 25%, F = 10%, p = 0.025). Whereas 33% of women reported higher rates of childcare and caring responsibilities as barriers to exercise, compared to 17% of men (p = 0.022).
Those with third-level education had higher levels of sedentary behavior (61%, p = 0.041) and higher rates of loneliness (84%, p = 0.031) but reported better mental health (72%, p = 0.036). They were also more likely to cite work/study as barriers to exercise and cooking, while those with vocational or secondary education more often reported food cost and taste as barriers to healthy eating. Similarly, those with secondary education also identified living arrangements as a barrier to sleep.
Housing strongly shaped lifestyle barriers. Social housing residents were least likely to meet physical activity targets (p = 0.028) and more often cited lack of safe outdoor spaces and embarrassment when exercising as the main barriers to exercise (58%, p = 0.003 and 41%, p = 0.002 respectively). More respondents in social housing also reported perceived food unpalatability as a barrier to healthy eating (49%, p = 0.009), and sleep disruptions due to living arrangements as a barrier to sleep (30%, p = 0.039). Alternatively, homeowners reported work as a barrier to sleep (50%, p = 0.026).
In terms of support needs, significant differences were observed among the gender and residency sociodemographic groups (Supplementary Table S6). Men expressed greater interest in substance use support (32%, p = 0.002). Residents of social or emergency housing and renters reported greater interest for support with sleep hygiene (p = 0.046) and mental health (p = 0.027); additionally, social housing and emergency housing residents expressed a need for support with social connections (p = 0.009), and substance use (p = 0.042).
3.4 Perspective on digital health technology and positive health coaching
Overall, both communities, Athy and Iași, responded positively to the role of digital technology and PHC in helping them achieve their health goals (Table 4).
3.4.1 Athy, Ireland
In the Irish sample, half of respondents (50%) had never used a health or wellbeing smartphone app, and three-quarters (75%) had never engaged with a health coach. Despite this, most expressed interest in digital tools: 77% reported willingness to use a community-specific health and wellbeing app, and 75% welcomed integrated health coaching. Nearly half (49%) owned a wearable device, and 69% indicated that device connectivity would encourage app use. Interest in specific app features was high, with 70% likely to use daily exercise programs, 72% stress management videos, 71% meditation for health, 69% meditation for sleep, and 77% food and cooking advice. Support in using the app was seen as important, with 62% more likely to engage if guidance were provided. Gamification was also appealing, with 59% expressing interest and the same proportion reporting it would motivate regular use.
3.4.2 Iași, Romania
In the Romanian sample, 65% of respondents had never used a smartphone health app and 76% had not engaged with a health coach. Nonetheless, most expressed interest in digital support: 79% were willing to use a community-specific health and wellbeing app, and 83% supported the integration of health coaching. Wearable ownership was lower than in Ireland, with 32% owning a device, but 60% reported that connectivity would encourage app use. Interest in app features was strong, with 82% likely to use daily exercise programs, 80% stress management videos, 69% meditation for health, 68% meditation for sleep, and 86% food and cooking advice. Engagement was also linked to support, with 76% more likely to use the app if guidance were provided. Gamification features were appealing to 75% of respondents, and 58% indicated that gamification would motivate use.
3.5 Perspective on digital health technology and positive health coaching according to sociodemographic groups
3.5.1 Athy, Ireland
In Athy, Ireland, significant differences were observed in the education group (Supplementary Table S7). Respondents with a third-level education degree (TE) were significantly more likely to have used a health and wellbeing app (60%) and a health coach (32%) compared to those with vocational education (VE) (42 and 6%) and secondary education (SE) (26 and 13%) (p = 0.001 and p = 0.002 respectively). Additionally, respondents with third-level education were more likely to engage in meditations for health and well-being (80%) compared to respondents with vocational (50%) and secondary-level education (55%) (p = 0.002). No other significant differences were observed across gender, age, or residency groups.
3.5.2 Iași, Romania
In Romania, significant differences in perspectives on digital health and coaching were observed across gender, age and education groups (Supplementary Table S8).
Women reported greater interest in specific digital health features compared with men. Seventy-five percent of women indicated willingness to use meditation for health and wellbeing and meditation for sleep, compared with 57 and 54% of men (p = 0.01 and p = 0.002). Cooking advice features were also more popular among women, with 90% expressing interest (p = 0.026).
Younger respondents (<40 years) reported higher prior engagement with digital health tools. Forty-five percent had used a smartphone health app compared to 24% of those over 40 (p = 0.002), and 31% had worked with a health coach compared to 17% of older respondents (p = 0.02). Wearable device ownership was also more common among younger adults (45% vs. 18%, p < 0.001).
Education level was associated with differences in wearable use and app preferences. Respondents with third-level education were more likely to own a wearable device (44%) compared with vocational (5%) and secondary-educated participants (9%) (p < 0.001), and more often indicated that device connectivity would encourage app use (72% vs. 30% vocational, 39% secondary; p < 0.001). In terms of app features, third-level and secondary-level respondents expressed greater interest in daily exercise programs (86 and 80%) compared with vocational (60%, p = 0.014). Similarly, interest in meditation for health and wellbeing was higher among third-level and secondary-educated respondents (75% each) compared with vocational (40%, p = 0.012). Meditation for sleep was also more popular among those with third-level education (74%) compared with vocational (45%) and secondary education (41%, p = 0.011).
4 Discussion
Digital health interventions (DHI) are often criticized for a lack of user involvement and cultural and contextual considerations in design and adoption, understanding technical support needs and considering the individual characteristics of end-users (33, 38). Understanding context and the specific needs of specific populations is critical for ensuring that DHIs are inclusive and accessible, particularly for vulnerable groups or digitally hesitant populations (38, 47, 48). This needs assessment was a critical step in informing the contextually sensitive design of a subsequent community-based DHI called Connect5.
The results of this study revealed interesting findings across, between, and within the two communities of Ireland and Romania. At a broader comparative level, the sociodemographic characteristics of the two communities exhibited some commonalities and differences. Respondents in Ireland and Romania were predominantly women and individuals with third-level education. However, differences emerged in age distribution and representation of vulnerable or disadvantaged groups. Ireland had an older sample, with the majority of respondents being over 40 years old, whereas Romania had a much higher representation of vulnerable or disadvantaged groups. These demographic commonalities and differences are important to consider when examining variations in health behaviors, perceived barriers, and support needs discussed later in this section.
Similarly, although lifestyle habits and barriers to healthy lifestyle behaviors appeared similar across the two communities, some differences emerged relating to barriers of healthier lifestyles and preferences for support. Both communities reported challenges with sleep, exercise, sedentary behavior, and stress. Common barriers to healthy lifestyle behaviors in both Ireland and Romania included: (1) physical activity - lack of time for exercise due to work, study, and childcare or caregiving responsibilities, with low motivation being a particularly significant barrier for Irish respondents; (2) consuming healthy food – high cost of food (especially in Romania), lack of time for cooking or preparing meals, and individual or family preferences for unhealthy foods; and (3) sleep - difficulty getting adequate sleep due to stress and worry in both communities, as well as work, children, and screen time. While work and children were more significant barriers to sleep in the Romanian community, the Irish community reported screen time as a more problematic factor. These barriers highlight the complexities individuals face in maintaining healthy habits across various aspects of their lives. Regarding support demand and preference, participants in Ireland most commonly expressed interest in support for physical activity, followed by healthy eating and food choices, then stress and mental health. In contrast, Romanian participants prioritized support for stress, followed by sleep, then healthy eating patterns and food choices.
Although both communities generally reported similar lifestyle behavior challenges and barriers, there was a notable contrast in their support needs and preferences. These findings no highlight the pressing need to address gaps in community support systems and the requirement to empower individuals to build a strong foundation for a healthy lifestyle. These results also reflect the reality that communities are dynamic social entities, influenced by socioeconomic and environmental determinants which defines health priorities and the contextualized needs from community to community (40, 49). The dynamic social factors shaping health determinants and community priorities extended beyond the documented differences between communities. Interestingly, this study highlighted that health and wellbeing needs were not generalizable to the community as a whole. Instead, distinct patterns in health and wellbeing behaviors, barriers, and needs were observed across sociodemographic groups within the two communities.
4.1 Sociodemographic factors shaping health behavior, barriers and lifestyle support preferences
Notable differences in health behaviors, barriers, and support needs emerged across sociodemographic groups in Ireland and Romania. Both communities reported meaningful sociodemographic differences across gender and age groups, though these differences were associated with distinctly different outcomes. Additional sociodemographic differences in educational attainment were reported in Romania and residency status in Ireland.
4.1.1 Gender
In both Ireland and Romania, gender differences significantly shaped health behaviors, barriers, and support needs. Women in Athy reported significantly more feelings of loneliness, higher stress levels, and lower physical activity than men. When asked about barriers to a healthy lifestyle, women in both communities faced significantly more barriers to exercise due to childcare and caring responsibilities, with the addition of stress as a barrier for women in Athy. Gender-specific lifestyle challenges were highlighted for men as well, specifically within the Romanian cohort. Men in Iași reported significantly higher alcohol and tobacco use compared to women, as well as a greater need for support with substance use.
These patterns reflect extensive evidence showing how gender disparities shape key determinants of health, including individuals’ motivation, opportunities, and barriers to healthy living. A wide body of research supports these findings, consistently showing that women are more likely to experience stress and social isolation, as well as childcare and caring responsibilities as barriers to engaging with healthier lifestyles (50–56). Contextually, our results also aligned with previous Irish studies showing that women in Ireland tend to be less active than men (57–61). In contrast, the higher levels of tobacco and alcohol use among men in Romania, echo consistent international findings indicating that men experience more smoke- and alcohol-related health problems and challenges (62, 63). Patterns of gender-based differences in lifestyle habits, barriers and support needs identified in this study and confirmed by the wider body of literature underscore the influence of deeply embedded social roles and responsibilities. These findings highlight the importance of gender-sensitive health promotion strategies that address the specific challenges and barriers women and men face within their communities.
4.1.2 Age
Our needs assessment also found age-specific health needs across both communities, which were generally consistent with the existing scientific literature. In Ireland, respondents under 40 years reported significantly poorer mental health and greater loneliness. This finding aligns with evidence that younger adults often experience heightened psychological distress due to work, social and financial pressures, which usually decreases with age (64). Patterns of tobacco use also showed age-related differences in Ireland. Adults over 40 years reported significantly higher tobacco consumption than their younger counterparts, despite research suggesting that smoking rates are typically higher in adults under 40 (65, 66). This discrepancy may reflect lower cessation rates among older smokers, as highlighted by Fidler and colleagues (67), as well intensive governmental health promotion campaigns in Ireland, since 2005. While some progress in cessation is evident among older Irish adults, continued targeted interventions remain essential (68). However, the absence of similar or significant patterns of lifestyle habits in Romanian respondents suggests that cultural or contextual factors may influence age-related differences.
Despite this, age-specific barriers to health were reported in both settings. Time constraints due to work and study emerged as a prominent barrier to physical activity, particularly among Irish respondents under 40 years. This is consistent with research showing time as one of the most commonly cited obstacles to physical activity (69). Similarly, the younger Romanian cohort (under 40 years) exhibited significantly more barriers to healthy eating due to a lack of knowledge about healthy foods compared to the older cohort. Existing research has reported similar patterns of heightened sense of awareness and increased knowledge of healthy eating among older adults, suggesting knowledge grows with age (70, 71). Finally, among older adults in Athy, injury and disability were commonly reported as barriers to exercise, which reflects existing research linking physical limitations and fear of injury to reduced exercise participation in older populations (72).
Together, these patterns offer valuable insight into the distinct needs and challenges of younger and older cohorts in Ireland and Romania. The findings suggest that interventions promoting work–life balance and time management for physical activity, along with targeted nutrition education, would benefit younger adults in both communities. Meanwhile, older adults may require additional support and resources for managing injury-related barriers to exercise, as well as enhanced smoking cessation services tailored to their specific needs.
4.1.3 Education levels
Respondents from lower socioeconomic groups were more affected by environmental and systemic health determinants, whereas higher socioeconomic groups experienced more individual-level barriers. This was particularly evident in Romania, where respondents with third-level education reported lack of time due to work and study commitments as a major barrier to exercise, and lack of time to cook as a barrier to healthy eating, significantly more than those with vocational or secondary level education. Similar patterns were observed in Ireland, where third-level educated respondents also reported time constraints as a key barrier. However, the Romanian data revealed additional nuances between education groups. Respondents with vocational or secondary education in Romania more frequently reported the high cost of healthy food as a barrier to healthy eating and living arrangements, and work (secondary level only) as a barrier to sleep. However, work also significantly impacted the sleep of respondents with third-level education.
Other barriers which disproportionately affected respondents with a maximum secondary or vocational educational attainment, included injury and disability as a barrier to exercise, and the perceived unpalatability of healthy food. Lifestyle habits also varied across education levels in Romania. Those with third-level education reported more sedentary behavior and greater experiences of loneliness, while those with vocational or secondary education reported higher stress levels and poorer mental health. These findings suggest lifestyle habits and barriers vary between education groups and may reflect deeper socioeconomic and structural inequalities. Our findings support existing research that demonstrates that social inequality and structural barriers exist in the ability of lower socioeconomic groups to stay healthy, even with cost-free and equal access to health care (73, 74). These barriers ultimately lead to lower socioeconomic groups facing greater challenges in adopting healthier lifestyles (74). However, it should be noted that while individual-level barrier was cited as more common among high socioeconomic groups, it’s important to recognize that even these barriers can be shaped broadly by societal pressures and expectations.
4.1.4 Residency
Lifestyle habits, support needs, and barriers that correlated with the residency of respondents continue to underscore the critical role of systemic and environmental barriers uniquely experienced by individuals based on their socioeconomic status (73, 74). Residency correlated with similar trends to those observed by education level. Similar to respondents with third-level education, renters and homeowners also reported a lack of time as a barrier to exercise. Similarly, the perceived unpalatability of respondents or their family was a barrier to healthy eating for those living in social housing, Furthermore, their living arrangements negatively impacted sleep, much like respondents with secondary or vocational education as the highest level of educational attainment. One notable deviation was that work commitments impacted renters and homeowners, similar to how they affected those with vocational and secondary education. Additional findings relating to residency and lifestyle habits showed that those living in social housing in Ireland were disproportionately affected by poor mental health compared with the other groups.
Additional insights emerged when examining the support needs and barriers experienced by individuals in lower socioeconomic groups, such as social housing residents. While the subsample of Romanian respondents in social housing who did not meet recommended physical activity targets was small, these findings align with previous research reporting that lower socioeconomic groups tend to have significantly lower levels of physical activity (75). Furthermore, the present study found that social housing residents faced heightened barriers due to limited access to safe outdoor spaces and embarrassment about exercising, consistent with evidence linking environmental disadvantage and social stigma to lower physical activity engagement (76, 77). These barriers create significant obstacles to engaging in health-promoting behaviors. Patterns in support needs further reflect the social disadvantages associated with living in social housing. Significant correlations between support needs and residency status pointed to greater reported demand for support related to risky substance use, mental health, and sleep among Romanian social housing residents, while Irish respondents in social housing more frequently reported a need for support in connecting with other people. Significant correlations between support needs and residency indicated greater reported demand for support related to risky substance use, mental health, and sleep for Romanian respondents in social housing, whereas Irish residents more often identified a need for social connection support. These support trends echo existing studies on the long-term impact of housing insecurity on mental health and wellbeing (78, 79).
While the behaviors, preferences, and needs across and within communities of this needs assessment align with existing literature, it is evident from the results that generalizability is still not possible, nor should it be promoted. Different socioeconomic groups expressed different challenges and preferences reflecting complex intersections between individual, environmental, and social factors within and across Ireland and Romania. These findings reinforce that the one-size-fits-all approach is insufficient for digital health and community interventions (31). Instead, CBPR approaches like the one applied in this study are essential for identifying both community-wide and subgroup-specific needs. This ensures that health promotion and prevention interventions are designed according to the context and preferences of the targeted communities and the groups within it.
4.2 Digital health and PHC
Both communities showed strong interest in digital health solutions and PHC. Despite a large proportion of respondents having never engaged with a health app or health coaching, the majority of respondents across communities and sociodemographic groups were willing and interested in using a community-specific health and wellbeing app with a health coach. Likewise, the ownership of wearable devices like smartwatches (i.e., Garmin, Fitbit, and Apple Watch) was relatively low. However, a majority of respondents still reported an interest in the ability to connect wearable devices to the digital solution and its ability to motivate and encourage use of the DHI. These findings highlight the acceptability and potential for a coach-led digital positive health intervention to bridge gaps in health support, particularly for vulnerable groups. These levels of acceptability align with previous findings indicating a growing interest in health and well-being digital technology across various population groups (80).
However, it is important to note that younger individuals and those with higher education were more likely to have used health apps, engaged with a health coach, and owned wearable devices than older respondents and those with secondary or vocational education. This suggests that these services may typically be more accessible or catered to higher socioeconomic groups and younger digital generations, despite needs and preferences reported as higher in lower socioeconomic or marginalized groups. Although the purpose of digital health is to improve the availability and accessibility of services like health coaching to typically hard-to-reach populations, research has shown that this is often not the case; lower socioeconomic populations, people with migrant backgrounds, older adults, women, and negatively racialized groups are usually at risk of being marginalized or excluded from digital health interventions (81–83). Technology and DHI are not socially neutral. They are shaped by the context in which they are established (81). Results from the scientific literature has indicated that inequity in societies and healthcare systems is usually reflected or exacerbated in digital health applications and use (81–83). In addition, not everyone has equal access or opportunity to benefit from the digitalization of health services (83).
Additionally, barriers to access include inadequate skills (i.e., digital skills), lack of time, capacity, resources or confidence in the digital intervention, as well as broader political, social, and economic systemic factors that hinder engagement with DHIs (81, 83). To overcome this inequity, an intersectional approach to digital health is recommended, which considers barriers to engagement and social determinants of health in its design and delivery (82, 83). This has also been advised by WHO (2021) in their global strategy on digital health 2020–2025, where relevant factors of inequalities should be assessed to ensure that access for specific populations is guaranteed, and no one is left behind (84).
Regarding the specific DHI proposed for the subsequent Connect5 project, respondents showed a preference for gamification features, suggesting that incorporating gamification elements could enhance engagement. Respondents were also asked about different application features like exercise programs, stress management videos, food and cooking advice, and guided meditation. While all features were positively received by respondents, there were some differences in preferences according to sociodemographic groups. For example, in both countries, women and respondents with third-level and secondary-level education showed greater interest in meditation features compared to men and respondents with vocational education. Likewise, respondents with third level and secondary level education showed greater interest in daily exercise programs. While there were only slight differences in features preferred among different sociodemographic groups, these findings continue to support the overall hypothesis that digital health interventions should be tailored to the targeted community and sociodemographic groups that exist within the community for sustainable engagement and experience. This is supported by a systematic review by Lattie and colleagues (2019) that identified that improving user experience and tailoring user engagement appeared vital for the sustainable implementation of digital mental health interventions. These barriers are in line with previous studies that identified key factors that would increase uptake and engagement of digital health solutions, including digital literacy and technical support, personalization, social networking, and gamification, endorsing the importance of tailored smartphone app features and engagement strategies (80).
Our needs assessment found that each of these factors was identified as important for sustaining engagement with the DHI. However, one other factor was identified in this needs assessment, the presence of a human health coach and human technological support on the digital platform. Respondents across both communities responded positively to the added feature of a human health coach on the digital application. Likewise, the addition of support in using the digital health technology and navigating the application seemed to correlate with respondents being more likely to engage with the intervention. A recent systematic review supports these findings (85). While AI and human coaches produced similar health and wellbeing outcomes, human coaches could build better relationships and rapport with participants, which in turn supported increased and sustainable engagement with the digital health interventions. Due to the strong sense of connection, warmth and authenticity of human coaching, participants generally reported a preference for the addition of human coaching in digital health interventions (85).
5 Strengths and limitations
The study’s strength lies in the use of a CBPR approach, prioritizing the voices of community members in co-designing digital health interventions. The research captures a broad range of health behaviors, barriers, and support preferences across two diverse communities. Additionally, it highlights the strong acceptability of digital health coaching among participants. By giving participants a central role in shaping the intervention, the study fosters greater community buy-in and supports the development of solutions that are culturally appropriate. This approach ensures that the digital health coaching intervention is not only relevant but also well-received, increasing its potential for adoption and sustained engagement within the communities.
We identified three main limitations in our study. First, despite efforts to recruit a diverse sample from the general population, the Irish cohort primarily consisted of middle-aged women (40 years or older), with low male participation (29%). A similar gender distribution was observed in the Romanian group; however, the age distribution was younger, with 52% of respondents under 40 years old. Nevertheless, the study provided valuable insights into health behaviors and digital health needs across different demographic groups. Sampling bias may have occurred in the Romanian cohort due to recruitment strategies through AVD Romania and the Coalition of Organizations of Patients with Chronic Diseases in Romania (COPAC). This recruitment method may have contributed to the Romanian group having a greater proportion (82%) of respondents belonging to disadvantaged groups and expressing a greater need for support. While this sample composition may have influenced the findings, it also highlights the needs of vulnerable groups, particularly those living with chronic illness, who require the most attention in health interventions. Second, the sample sizes within specific sociodemographic groups were limited, which reduced the statistical power of our descriptive and exploratory analyses. While the study provides valuable insights into lifestyle habits and support needs within these communities, we acknowledge that the findings should be interpreted with caution given the uneven representation of certain groups. Further research with larger, more balanced samples across sociodemographic groups is needed to strengthen the generalizability of these findings and provide a more comprehensive understanding of health needs in both communities. Finally, the reliance on self-reported data may have introduced response bias, as respondents might overestimate or underestimate their health behaviors, lifestyle habits, or support needs due to recall issues or social desirability.
6 Conclusion
Digitalizing positive health interventions has the potential to increase accessibility and scalability of health and wellbeing support across different communities. Such interventions can play a meaningful role in reducing the burden and prevalence of NCDs, aligning with the global UN goal of reducing NCD-related premature mortality rates. However, to ensure the effectiveness and relevance of DHIs for communities, it is vital to understand the socioeconomic and environmental determinants of health within targeted communities. This inclusive approach allows for the development of context-sensitive studies. This study employed a CBPR approach to assess the specific health and wellbeing needs of citizens in Athy, Ireland and Iași, Romania, ahead of the contextual adaptation and implementation of a subsequent project. Connect5, is a digital positive health coaching intervention, designed to promote greater health and wellbeing among community residents in both Athy and Iași.
The CBPR-informed needs assessments identified shared requirements for support in lifestyle areas such as sleep, physical activity, sedentary behavior, and stress management across both communities. Study respondents expressed strong interest in digital health coaching, particularly preferring interventions that combine human coaching with digital technology. The assessment revealed important variations in lifestyle needs and preferences not only between Romania and Ireland but also within sociodemographic subgroups based on gender, age, and socioeconomic status. These findings emphasize that effective DHIs require community engagement in a co-design process, integration of human support, and targeted approaches that address the specific needs of different community subgroups to promote health equity and improve population wellbeing.
6.1 Implications for future research
We encourage researchers and community support workers to move away from one-size-fits-all approaches when it comes to designing and delivering health interventions. Along with other researchers, we advocate the use of bottom-up CBPR approach to tailor digital health solutions and reduce health inequities, especially at a community level. While this study included vulnerable populations, the sample was skewed toward higher socioeconomic backgrounds. Future research must prioritize reaching marginalized and digitally excluded groups to ensure their needs are fully reflected in equitable digital health solutions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by RCSI Research Ethics Committee, Dublin (Reference number: REC202210030). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MI-C: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing, Resources, Supervision. CL: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. RO’D: Data curation, Conceptualization, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing – review & editing. CI: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing. DV: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing. MI: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing. IE: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing. AA: Resources, Supervision, Validation, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration. PD: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was kindly funded by Sláintecare Healthy Communities and Kildare County Council (Grant code RCSI 23230A01).
Acknowledgments
We would like to acknowledge the support of Sláintecare Healthy Communities Ireland and Kildare County Council. We also extend our sincere thanks to Aoife Breslin, Labour Councillor for Athy; Maria Healy, Local Development Officer for Sláintecare Healthy Communities, Kildare County Council; Majella Fennelly, Athy and Monasterevin Sports Hub Coordinator; the staff of Athy Library; Athy Family Resource Centre; the Coalition of Organizations of Patients with Chronic Diseases in Romania; and the communities of Athy and Iași for their generous support in facilitating this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1673205/full#supplementary-material
References
2. Leal Neto, O, and Von Wyl, V. Digital transformation of public health for noncommunicable diseases: narrative viewpoint of challenges and opportunities. JMIR Public Health Surveill. (2024) 10:e49575. doi: 10.2196/49575
3. World Health Organization. International telecommunication union. Going digital for noncommunicable diseases: The case for action. Geneva: World Health Organization (2024).
4. Widmer, RJ, Collins, NM, Collins, CS, West, CP, Lerman, LO, and Lerman, A. Digital health interventions for the prevention of cardiovascular disease: a systematic review and meta-analysis. Mayo Clin Proc. (2015) 90:469–80. doi: 10.1016/j.mayocp.2014.12.026
5. NCD Countdown Collaborators. NCD countdown 2030: worldwide trends in non-communicable disease mortality and progress towards sustainable development goal target 3.4. Lancet. (2018) 392:1072–88. doi: 10.1016/S0140-6736(18)31992-5
6. GBD Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1223–49. doi: 10.1016/S0140-6736(20)30752-2
7. Beaglehole, R, Bonita, R, Horton, R, Adams, C, Alleyne, G, Asaria, P, et al. Priority actions for the non-communicable disease crisis. Lancet. (2011) 377:1438–47. doi: 10.1016/S0140-6736(11)60393-0
8. Zhang, Y, Pan, X, Chen, J, Cao, A, Zhang, Y, Xia, L, et al. Combined lifestyle factors, incident cancer, and cancer mortality: a systematic review and meta-analysis of prospective cohort studies. Br J Cancer. (2020) 122:1085–93. doi: 10.1038/s41416-020-0741-x
9. United Nations. The sustainable development goals report. Department of Economic and Social Affairs (2021). Availalbe onilne at: https://unstats.un.org/sdgs/report/2021/ (Accessed June 3, 2025).
10. Birkholz, L, Weber, P, Helsper, N, Kohler, S, Dippon, L, Rutten, A, et al. Multi-level stakeholders’ perspectives on implementation and scaling up community-based health promotion in Germany. Health Promot Int. (2023) 38. doi: 10.1093/heapro/daad045
11. Nickel, S, and von dem Knesebeck, O. Effectiveness of community-based health promotion interventions in urban areas: a systematic review. J Community Health. (2020) 45:419–34. doi: 10.1007/s10900-019-00733-7
12. Silva, KL, Sena, RR, Belga, SMMF, Silva, PM, and Rodrigues, AT. Health promotion: challenges revealed in successful practices. Rev Saude Publica. (2014) 48:76–85. doi: 10.1590/S0034-8910.2014048004596
13. Vu, H, François, KK, Hung, NX, Trung, NV, and Hieu, NL. Potential of digital health solutions in facing shifting disease burden and double burden in low-and middle-income countries. mDigitalization of medicine in low-and middle-income countries: Paradigm changes in healthcare and biomedical research : Springer International Publishing: Cham; (2024). p. 51–68
14. Denizard-Thompson, NM, Miller, DP, Snavely, AC, Spangler, JG, Case, LD, and Weaver, KE. Effect of a digital health intervention on decreasing barriers and increasing facilitators for colorectal cancer screening in vulnerable patients. Cancer Epidemiol Biomarkers Prev. (2020) 29:1564–9. doi: 10.1158/1055-9965.EPI-19-1199
15. Haregu, T, Delobelle, P, Issaka, A, Shrestha, A, Panniyammakal, J, Thankappan, KR, et al. Digital health solutions for community-based control of diabetes during COVID-19 pandemic: a scoping review of implementation outcomes. J Diabetes Sci Technol. (2024) 18:1480–8. doi: 10.1177/19322968231167
16. Koh, A, Swanepoel, DW, Ling, A, Ho, BL, Tan, SY, and Lim, J. Digital health promotion: promise and peril. Health Promot Int. (2021) 36:i70–80. doi: 10.1093/heapro/daab134
17. Singh, V, and Singh, A. Digital health revolution: Enhancing wellbeing through technology. Implementing sustainable development goals in the service sector. Hershey: IGI Global Scientific Publishing; (2024). p. 213–219
18. Chatterjee, A, Prinz, A, Gerdes, M, and Martinez, S. Digital interventions on healthy lifestyle management: systematic review. J Med Internet Res. (2021) 23:e26931. doi: 10.2196/26931
19. Philippe, TJ, Sikder, N, Jackson, A, Koblanski, ME, Liow, E, Pilarinos, A, et al. Digital health interventions for delivery of mental health care: systematic and comprehensive meta-review. JMIR Mental Health. (2022) 9:e35159. doi: 10.2196/35159
20. Shan, R, Sarkar, S, and Martin, SS. Digital health technology and mobile devices for the management of diabetes mellitus: state of the art. Diabetologia. (2019) 62:877–87. doi: 10.1007/s00125-019-4864-7
21. O’Boyle, CA, Lianov, L, Burke, J, Frates, B, and Boniwell, I. Positive health: An emerging new construct In: Routledge international handbook of positive health sciences. London: Routledge (2023). 2–23.
22. Seligman, ME, and Csikszentmihalyi, M. Positive psychology: An introduction (2000) 55:5–14. doi: 10.1037/0003-066X.55.1.5
23. Egger, GJ, Binns, AF, and Rossner, SR. The emergence of “lifestyle medicine” as a structured approach for management of chronic disease. Med J Aust. (2009) 190:143–5. doi: 10.5694/j.1326-5377.2009.tb02317.x
24. Krantz, DS, Grunberg, NE, and Baum, A. Health psychology. Annu Rev Psychol. (1985) 36:349–83. doi: 10.1146/annurev.ps.36.020185.002025
25. Loughnane, C, O’Donovan, R, Duggan, A, and Dunne, P. Learning through reflection: a team’s reflection on a digital, text-based positive health coaching intervention for healthcare professionals. Int J Evidence Based Coaching Mentor. (2025) 23:371–83. doi: 10.24384/h3kz-7s59
26. Dunne, PJ, Byrne, E, Burke, J, and Duggan, A. Meliotropism: a new concept in positive health sciences and human flourishing. Health Promot Int. (2025) 11:11–8. doi: 10.31234/osf.io/agphy_v1
27. van Nieuwerburgh, C, and Knight, J. Positive health coaching: Adopting a dialogical approach to health and wellbeing In: Routledge International Handbook of Positive Health Sciences. London: Routledge (2023). 220–36.
28. Loughnane, C, Burke, J, Byrne, E, Iglesias-Cans, M, Scott, C, Collins, M, et al. Positive health coaching: a conceptual analysis. Front Psychol. (2025) 16:1597867. doi: 10.3389/fpsyg.2025.1597867
29. O’Donovan, R, Loughnane, C, Donnelly, J, Kelly, R, Kemp, D, McCarthy, L, et al. Healthcare workers’ experience of a coach-led digital platform for better well-being. Coaching. (2024) 17:207–25. doi: 10.1080/17521882.2024.2304793
30. O’Donovan, R, Loughnane, C, van Nieuwerburgh, C, Duggan, A, and Dunne, P. The potential of human positive health coaching through a digital health platform to prompt reflection and engagement in behaviour change. Int J Evidence Based Coach Mentor. (2024) 22:136–76. doi: 10.24384/TJWP-JR55
31. Al-Dhahir, I, Reijnders, T, Faber, JS, van den Berg-Emons, RJ, Janssen, VR, Kraaijenhagen, RA, et al. The barriers and facilitators of eHealth-based lifestyle intervention programs for people with a low socioeconomic status: scoping review. J Med Internet Res. (2022) 24:e34229. doi: 10.2196/34229
32. Badr, J, Motulsky, A, and Denis, JL. Digital health technologies and inequalities: a scoping review of potential impacts and policy recommendations. Health Policy. (2024) 146:105122. doi: 10.1016/j.healthpol.2024.105122
33. Tariq, A, and Durrani, S. One size does not fit all: the importance of contextually sensitive mHealth strategies for frontline female health workers In: E Baulch, J Watkins, and A Tariq, editors. mHealth innovation in Asia: Grassroots challenges and practical interventions. Dordrecht (NL) : Springer. (2018). 7–29.
34. Kumar, S, and Preetha, G. Health promotion: an effective tool for global health. Indian J Community Med. (2012) 37:5–12. doi: 10.4103/0970-0218.94009
35. Guo, C, Ashrafian, H, Ghafur, S, Fontana, G, Gardner, C, and Prime, M. Challenges for the evaluation of digital health solutions - a call for innovative evidence generation approaches. NPJ Digital Med. (2020) 3:110. doi: 10.1038/s41746-020-00314-2
36. Mumtaz, H, Riaz, MH, Wajid, H, Saqib, M, Zeeshan, MH, Khan, SE, et al. Current challenges and potential solutions to the use of digital health technologies in evidence generation: a narrative review. Front Digital Health. (2023) 5:1203945. doi: 10.3389/fdgth.2023.1203945
37. Fiordelli, M, Diviani, N, and Schulz, PJ. Mapping mHealth research: a decade of evolution. J Med Internet Res. (2013) 15:e95. doi: 10.2196/jmir.2430
38. Kowatsch, T, Otto, L, Harperink, S, Cotti, A, and Schlieter, H. A design and evaluation framework for digital health interventions. Inform Technol. (2019) 61:253–63. doi: 10.1515/itit-2019-0019
39. Collins, SE, Clifasefi, SL, Stanton, J, Straits, KJ, Gil-Kashiwabara, E, Rodriguez Espinosa, P, et al. Community-based participatory research (CBPR): towards equitable involvement of community in psychology research. Am Psychol. (2018) 73:884. doi: 10.1037/amp0000167
40. Leung, MW, Yen, IH, and Minkler, M. Community based participatory research: a promising approach for increasing epidemiology’s relevance in the 21st century. Int J Epidemiol. (2004) 33:499–506. doi: 10.1093/ije/dyh010
41. Oetzel, JG, Wallerstein, N, Duran, B, Sanchez-Youngman, S, Nguyen, T, Woo, K, et al. Impact of participatory health research: a test of the community-based participatory research conceptual model. Biomed Res Int. (2018) 2018:7281405. doi: 10.1155/2018/7281405
42. Alimujiang, A, Wiensch, A, Boss, J, Fleischer, NL, Mondul, AM, McLean, K, et al. Association between life purpose and mortality among US adults older than 50 years. JAMA Netw Open. (2019) 2:e194270. doi: 10.1001/jamanetworkopen.2019.4270
43. Hirshkowitz, M, Whiton, K, Albert, SM, Alessi, C, Bruni, O, DonCarlos, L, et al. National sleep foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. (2015) 1:40–3. doi: 10.1016/j.sleh.2014.12.010
44. World Health Organization. WHO guidelines on physical activity and sedentary behaviour. Geneva: World Health Organization (2020).
45. StataCorp. Stata Statistical Software. 18 R. (2023). Avaialble online at: https://www.stata.com/ (Accessed June 5, 2025).
46. IBM Corp. IBM SPSS statistics for windows. 29.0 V. (2022). Avaiallbe online at: https://hadoop.apache.org (Accessed June 5, 2025).
47. Malloy, J, Partridge, SR, Kemper, JA, Braakhuis, A, and Roy, R. Co-design of digital health interventions with young people: a scoping review. Digit Health. (2023) 9:1–31. doi: 10.1177/205520762312191
48. Wang, G, Chang, F, Gu, Z, Kasraian, D, and van Wesemael, PJ. Co-designing community-level integral interventions for active ageing: a systematic review from the lens of community-based participatory research. BMC Public Health. (2024) 24:649. doi: 10.1186/s12889-024-18195-5
49. Oetzel, JG, Boursaw, B, Magarati, M, Dickson, E, Sanchez-Youngman, S, Morales, L, et al. Exploring theoretical mechanisms of community-engaged research: a multilevel cross-sectional national study of structural and relational practices in community-academic partnerships. Int J Equity Health. (2022) 21:59. doi: 10.1186/s12939-022-01663-y
50. Cody, R, and Lee, C. Physical activity barriers for mothers of preschool children. ACHPER Healthy Lifestyles J. (1999) 46:18–22. doi: 10.5555/19991810242
51. Gyllensten, K, and Palmer, S. The role of gender in workplace stress: a critical literature review. Health Educ J. (2005) 64:271–88. doi: 10.1177/001789690506400
52. Haering, S, Meyer, C, Schulze, L, Conrad, E, Blecker, MK, El-Haj-Mohamad, R, et al. Sex and gender differences in risk factors for posttraumatic stress disorder: a systematic review and meta-analysis of prospective studies. J Psychopathol Clin Sci. (2024) 133:429–44. doi: 10.1037/abn0000918
53. Kim, YB, and Lee, SH. Gender differences in correlates of loneliness among community-dwelling older Koreans. Int J Environ Res Public Health. (2022) 19:7334. doi: 10.3390/ijerph19127334
54. King, AC, Castro, C, Wilcox, S, Eyler, AA, Sallis, JF, and Brownson, RC. Personal and environmental factors associated with physical inactivity among different racial-ethnic groups of U.S. middle-aged and older-aged women. Health Psychol. (2000) 19:354–64. doi: 10.1037//0278-6133.19.4.354
55. McKeon, G, Mastrogiovanni, C, Teychenne, M, and Rosenbaum, S. Barriers and facilitators to participating in an exercise referral scheme among women living in a low socioeconomic area in Australia: a qualitative investigation using the COM-B and theoretical domains framework. Int J Environ Res Public Health. (2022) 19:12312. doi: 10.3390/ijerph191912312
56. Lovell, GP, El Ansari, W, and Parker, JK. Perceived exercise benefits and barriers of non-exercising female university students in the United Kingdom. Int J Environ Res Public Health. (2010) 7:784–98. doi: 10.3390/ijerph7030784
57. Collier, C, MacPhail, A, and O’Sullivan, M. Student discourse on physical activity and sport among Irish young people. Irish Educ Stud. (2007) 26:195–210. doi: 10.1080/03323310701296193
58. Cowley, ES, Watson, PM, Foweather, L, Belton, S, Thompson, A, Thijssen, D, et al. “Girls aren’t meant to exercise”: perceived influences on physical activity among adolescent girls—the HERizon project. Children. (2021) 8:31. doi: 10.3390/children8010031
59. Lawler, M, Heary, C, and Nixon, E. Variations in adolescents’ motivational characteristics across gender and physical activity patterns: a latent class analysis approach. BMC Public Health. (2017) 17:661–13. doi: 10.1186/s12889-017-4677-x
60. Livingstone, M, Robson, P, McCarthy, S, Kiely, M, Harrington, K, Browne, P, et al. Physical activity patterns in a nationally representative sample of adults in Ireland. Public Health Nutr. (2001) 4:1107–16. doi: 10.1079/PHN2001192
61. Lunn, PD. The sports and exercise life-course: a survival analysis of recall data from Ireland. Soc Sci Med. (2010) 70:711–9. doi: 10.1016/j.socscimed.2009.11.006
62. Higgins, ST, Kurti, AN, Redner, R, White, TJ, Gaalema, DE, Roberts, ME, et al. A literature review on prevalence of gender differences and intersections with other vulnerabilities to tobacco use in the United States, 2004–2014. Prev Med. (2015) 80:89–100. doi: 10.1016/j.ypmed.2015.06.009
63. Probst, C, Roerecke, M, Behrendt, S, and Rehm, J. Gender differences in socioeconomic inequality of alcohol-attributable mortality: a systematic review and meta-analysis. Drug Alcohol Rev. (2015) 34:267–77. doi: 10.1111/dar.12184
64. Kessler, RC, Berglund, P, Demler, O, Jin, R, Merikangas, KR, and Walters, EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. (2005) 62:593–602. doi: 10.1001/archpsyc.62.6.593
65. Library HND. Factsheet: smoking and vaping - the Irish situation. Health Research Board. (2025). Available online at: https://www.drugsandalcohol.ie/30909/
66. Rahilly, CR, and Farwell, WR. Prevalence of smoking in the United States: a focus on age, sex, ethnicity, and geographic patterns. Curr Cardiovasc Risk Rep. (2007) 1:379–83. doi: 10.1007/s12170-007-0062-0
67. Fidler, J, Ferguson, S, Brown, J, Stapleton, J, and West, R. How does rate of smoking cessation vary by age, gender and social grade? Findings from a population survey in England. Addiction. (2013) 108:1680–5. doi: 10.1111/add.12241
68. Pesce, G, Marcon, A, Calciano, L, Perret, JL, Abramson, MJ, Bono, R, et al. Time and age trends in smoking cessation in Europe. PLoS One. (2019) 14:e0211976. doi: 10.1371/journal.pone.0211976
69. Silliman, K, Rodas-Fortier, K, and Neyman, M. Survey of dietary and exercise habits and perceived barriers to following a healthy lifestyle in a college population. Calif J Health Promot. (2004) 2:10–9. doi: 10.32398/cjhp.v2i2.1729
70. Paquette, MC. Perceptions of healthy eating: state of knowledge and research gaps. Can J Public Health. (2005) 96:S15-9, S6-21. doi: 10.1007/BF03405196
71. Sethi, S, and Rastogi, M. Perception of healthy eating: role of knowledge, attitude, and practices. SALT J Scientific Res Healthcare. (2023) 3:16–23. doi: 10.56735/ms2303021623
72. Kowalczyk, A, Nowicka, M, and Sas-Nowosielski, K. Age-related differences in motives for and barriers to exercise among women exercising in fitness centers. New Educ Rev. (2017) 49:30–9. doi: 10.15804/tner.2017.49.3.02
73. Borodulin, K, Sipila, N, Rahkonen, O, Leino-Arjas, P, Kestila, L, Jousilahti, P, et al. Socio-demographic and behavioral variation in barriers to leisure-time physical activity. Scand J Public Health. (2016) 44:62–9. doi: 10.1177/1403494815604080
74. Nielsen, JB, Leppin, A, Gyrd-Hansen, D, Jarbøl, DE, Søndergaard, J, and Larsen, PV. Barriers to lifestyle changes for prevention of cardiovascular disease–a survey among 40–60-year old Danes. BMC Cardiovasc Disord. (2017) 17:1–8. doi: 10.1186/s12872-017-0677-0
75. Gidlow, C, Johnston, LH, Crone, D, Ellis, N, and James, D. A systematic review of the relationship between socio-economic position and physical activity. Health Educ J. (2006) 65:338–67. doi: 10.1177/00178969060693
76. Snuggs, S, Clot, S, Lamport, D, Sah, A, Forrest, J, Helme Guizon, A, et al. A mixed-methods approach to understanding barriers and facilitators to healthy eating and exercise from five European countries: highlighting the roles of enjoyment, emotion and social engagement. Psychol Health. (2025) 40:852–79. doi: 10.1080/08870446.2023.2274045
77. van Stappen, V, Latomme, J, Cardon, G, De Bourdeaudhuij, I, Lateva, M, Chakarova, N, et al. Barriers from multiple perspectives towards physical activity, sedentary behaviour, physical activity and dietary habits when living in low socio-economic areas in Europe. The Feel4Diabetes study. Int J Environ Res Public Health. (2018) 15:2840. doi: 10.3390/ijerph15122840
78. Carnemolla, P, and Skinner, V. Outcomes associated with providing secure, stable, and permanent housing for people who have been homeless: an international scoping review. J Plann Lit. (2021) 36:508–25. doi: 10.1177/08854122211012911
79. Singh, A, Daniel, L, Baker, E, and Bentley, R. Housing disadvantage and poor mental health: a systematic review. Am J Prev Med. (2019) 57:262–72. doi: 10.1016/j.amepre.2019.03.018
80. Szinay, D, Jones, A, Chadborn, T, Brown, J, and Naughton, F. Influences on the uptake of and engagement with health and well-being smartphone apps: systematic review. J Med Internet Res. (2020) 22:e17572. doi: 10.2196/17572
81. Coetzer, JA, Loukili, I, Goedhart, NS, Ket, JCF, Schuitmaker-Warnaar, TJ, Zuiderent-Jerak, T, et al. The potential and paradoxes of eHealth research for digitally marginalised groups: a qualitative meta-review. Soc Sci Med. (2024) 350:116895. doi: 10.1016/j.socscimed.2024.116895
82. Hendl, T, and Shukla, A. Can digital health democratize health care? Bioethics. (2024) 38:491–502. doi: 10.1111/bioe.13266
83. Kaihlanen, A-M, Virtanen, L, Buchert, U, Safarov, N, Valkonen, P, Hietapakka, L, et al. Towards digital health equity-a qualitative study of the challenges experienced by vulnerable groups in using digital health services in the COVID-19 era. BMC Health Serv Res. (2022) 22:188. doi: 10.1186/s12913-022-07584-4
84. World Health Organization. Global strategy on digital health 2020–2025. Geneva: World Health Organization (2021).
Keywords: positive health sciences, positive health coaching, digital health interventions, health promotion, disease prevention, needs assessment, community-based participatory research, lifestyle medicine
Citation: Iglesias-Cans M, Loughnane C, O’Donovan R, Iftimoaei C, Vasiliu D, Iftimoaei M, Enache I, Achitei A and Dunne PJ (2025) A lifestyle-based needs assessment of two European communities prior to the development and deployment of a digital health coaching smartphone application. Front. Public Health. 13:1673205. doi: 10.3389/fpubh.2025.1673205
Edited by:
Han Feng, Tulane University, United StatesReviewed by:
Chenguang Zhang, University of Texas Health Science Center at Houston, United StatesMayana Bsoul, Tulane University, United States
Copyright © 2025 Iglesias-Cans, Loughnane, O’Donovan, Iftimoaei, Vasiliu, Iftimoaei, Enache, Achitei and Dunne. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marina Iglesias-Cans, bWFyaW5haWNhbnNAcmNzaS5pZQ==
 Marina Iglesias-Cans
Marina Iglesias-Cans Croia Loughnane
Croia Loughnane Roisin O’Donovan
Roisin O’Donovan Ciprian Iftimoaei
Ciprian Iftimoaei Diana Vasiliu4
Diana Vasiliu4 Manuela Iftimoaei
Manuela Iftimoaei Ingrid Enache
Ingrid Enache Angela Achitei
Angela Achitei Padraic J. Dunne
Padraic J. Dunne