- 1School of Nursing, The University of Hong Kong, Pokfulam, Hong Kong SAR, China
- 2Alice Lee Centre for Nursing Studies, National University of Singapore, Singapore, Singapore
- 3School of Nursing, Shanghai Jiao Tong University, Shanghai, China
- 4Hong Kong Council on Smoking and Health, Wan Chai District, Hong Kong SAR, China
Objective: Parental smokers account for approximately one-third of smokers worldwide and often exhibit distinct smoking and quitting behaviors compared to non-parental smokers. Understanding these differences is crucial for developing targeted cessation interventions; however, current evidence remains limited.
Methods: This secondary analysis pooled individual participant data from 10 community-based smoking cessation trials conducted in Hong Kong between 2010 and 2020 (N = 10,871 adult daily smokers). We compared parental smokers (those with at least one child) and non-parental smokers in terms of sociodemographic characteristics, smoking behaviors, nicotine dependence (Heaviness of Smoking Index), quitting motivation, and cessation outcomes at 6 months post-intervention. Outcomes included biochemically validated abstinence (exhaled carbon monoxide <4 ppm and salivary cotinine <10 ng/mL) and self-reported 7-day point-prevalence abstinence (PPA). Multivariable regression models were adjusted for age, sex, education, income, and trial year.
Results: Of the participants, 42.2% were parental smokers, who were older and had lower education and income (all p < 0.001). They had higher daily cigarette consumption (mean: 14.8 vs. 12.9, adjusted β = 1.59, p = 0.004) and higher nicotine dependence (9.2% vs. 5.9%, AOR = 1.36, p < 0.001). A large number of parental smokers had past quit attempts (61.8% vs. 54.0%, AOR = 1.25, p < 0.001) and intentions to quit within 30 days (61.2% vs. 46.4%, AOR = 1.31, p < 0.001). At 6 months, parental smokers showed higher validated abstinence (7.7% vs. 5.9%, AOR = 1.37, p < 0.001) and self-reported 7-day PPA (15.6% vs. 13.9%, AOR = 1.21, p = 0.002). Among parental smokers, those co-living with children had greater abstinence than those not necessarily co-living, for both self-reported 7-day PPA (AOR = 1.43, 95% CI 1.03–1.98, p = 0.032) and validated abstinence (AOR = 1.62, 95% CI 1.04–2.52, p = 0.032).
Conclusion: Parental smokers showed higher nicotine dependence but greater motivation and higher abstinence rates following brief community-based interventions. Tailored programs should address their elevated addiction while leveraging their motivation to enhance cessation success.
1 Introduction
Approximately 33% of smokers worldwide are parental smokers (1). Becoming a parent often serves as a pivotal moment to reconsider smoking behaviors. Research has reported that parental smokers often display greater motivation to quit smoking, driven by a heightened sense of responsibility for their children’s health (2). Consequently, smokers, especially those co-living with children, demonstrate a higher intention to quit and have made more quitting attempts than those without children (3). In the United States, 40% of parental smokers have made at least one quit attempt after childbirth (4). Additionally, parents are more likely to set positive examples of healthy lifestyles for their children, which leads to the perceived higher importance of cessation and prompts sustained efforts to quit (5).
Although parental smokers may display greater motivation to quit smoking, the extent of their success in achieving cessation remains inconclusive. Studies found that greater readiness to quit may predict higher success rates in smoking cessation (6, 7), but parental smokers face challenges in both quitting and maintaining abstinence, resulting in higher relapse rates (8). Moreover, half of the maternal smokers who quit smoking during pregnancy relapsed at 6 months postpartum (9–11). This discrepancy between high motivation to quit and low sustained abstinence rates among parental smokers suggests distinct smoking behaviors and challenges in quitting compared to the general smoking population.
Social cognitive theory (SCT) (12) posits that individuals become increasingly aware of the health risks associated with tobacco use (e.g., secondhand smoke exposure and behavioral modeling) upon becoming parents. This heightened awareness may generate a stronger intention to quit smoking. Parental smokers may demonstrate their commitment to protecting their children’s wellbeing by achieving abstinence, underscoring the concept of parenthood as a “teachable moment” for smoking cessation. The effectiveness of such behavioral changes is further enhanced when parents receive tailored interventions designed to support cessation efforts.
Previous smoking cessation interventions for parents have largely centered on pregnant women (13–16) and expectant fathers (17, 18), which may be due to the vulnerability of fetal and infant health to secondhand smoke exposure (19, 20). Behavioral interventions [such as brief counseling (21, 22), toll-free helplines (5, 23), and mobile programs via short message service (SMS) (24)], as well as pharmacological methods such as nicotine replacement therapy (25) and bupropion (26), have shown effectiveness in aiding cessation. However, the comparative effectiveness of these approaches between parental and non-parental smokers remains uncertain. Identifying the relative effectiveness of different cessation interventions becomes imperative to formulate tailored interventions aimed at supporting parental smokers in their cessation journey.
This study examined differences in smoking characteristics and cessation outcomes between smokers with and without children in Hong Kong. We further examined how residential status (whether parents co-live with their children), number of children, sex of parental smokers, and whether they received financial incentive might affect smoking behavior, considering differences in the perceived risk of tobacco smoke exposure. Additionally, cessation outcomes were explored according to the type of behavioral interventions received.
2 Methods
2.1 Participant and procedure
This is a prospective secondary analysis of data from 10 randomized controlled trials (RCTs) nested within Hong Kong’s annual “Quit-to-Win” (QTW) community campaign (2010–2021; no trials in 2011, and parental data not collected in 2014). Each trial was registered with ClinicalTrials.gov and followed the guidelines for strengthening the reporting of observational studies in epidemiology (STROBE).
At each annual Quit-to-Win Contest (see Supplementary Table S1; Supplementary Figure S1), participants were recruited at community hotspots (e.g., transport hubs, streets of urban business areas, and shopping malls) across all 18 districts of Hong Kong. Trained smoking cessation (SC) advisors approached potential participants, enrolling Chinese-speaking residents aged 18 years or above who smoked at least one cigarette daily in the past 3 months (verified by exhaled carbon monoxide ≥4 ppm). Eligible individuals were then randomly allocated to intervention or control arms. Smokers using SC medication or other SC services, or who were physically or mentally unable to communicate, were excluded. Deidentified baseline data from all 10,871 RCT participants from 2010 to 2021 were included in the analyses, regardless of treatment allocation. Data were collected after obtaining written consent for participation.
2.2 Measures
2.2.1 Sociodemographic characteristics
Sociodemographic characteristics were collected as categorical variables, including sex, age group, educational attainment, marital status, having children (aged<18) or not, number of children, and monthly household income. For data collection from 2010 to 2016, parental smokers were defined as individuals who reported having children, as information on co-residence with children was not collected during this period. From 2017 to 2021, smokers with children were asked whether they lived with their children in the same household, allowing for a more specific classification of parental smokers as those residing with their children. Subgroup analyses were conducted to assess differences in the associations between smoking and quitting characteristics among parental smokers, stratified by residential status, number of children, sex, and receipt of financial incentive.
2.3 Smoking and quitting characteristics
2.3.1 Nicotine dependence
Daily cigarette consumption was assessed as the average number of cigarettes smoked per day (CPD) over the past 7 days and subsequently categorized into four groups: “10 or fewer,” “11–20,” “21–30,” and “31 or more,” based on the Heaviness of Smoking Index (HSI) categorization. Time to first cigarette after waking was categorized into “>60 min,” “31–60 min,” “6–30 min,” and “<5 min.” Categorized CPD and time to first cigarette were then combined to calculate the HSI score (range: 0–6), with a score of 5–6 indicating a high level of nicotine dependence.
2.3.2 Motivation to quit
Past quit attempts were assessed using the question “When was the last time you abstained from smoking for 24 h or longer when trying to quit?” Responses were dichotomized into “ever attempted” and “never attempted.”
Intention to quit was assessed by asking, “When will you intend to quit smoking?,” with responses “within 7 days,” “within 30 days,” “within 60 days,” and “undecided.” Perceptions of quitting were assessed using perceived importance, confidence, and difficulty to quit on a scale of 0 (not at all) to 10 (very).
2.3.3 Smoking abstinence outcomes
Smoking abstinence outcomes measured at 6-month follow-up included biochemically validated abstinence, self-reported 7-day point-prevalent abstinence (PPA), smoking reduction by at least 50%, and the accumulated number of quitting attempts. Biochemical validation of abstinence was performed using exhaled carbon monoxide testing with the piCO Smokerlyzer (< 4 ppm considered indicative of abstinence). Outcomes were classified as a binary variable, “quit” or “not quit.”
Salivary cotinine was assessed using the NicAlert test strip (<10 ng/mL defined as abstinence) and similarly categorized as “quit” or “not quit.” Smoking reduction by at least 50% was defined as a reduction in cigarette consumption by 50% or more compared with baseline and was categorized as “yes” or “no.” The accumulated number of quitting attempts was determined by whether a participant had made a quit attempt in the past 7 days and was categorized as “yes” or “no.”
2.3.4 Community-based interventions
A total of 26 intervention groups from 10 RCTs were included to evaluate the effectiveness of various behavioral smoking cessation interventions versus brief advice as a control on abstinence outcomes (see Supplementary Table S1; Supplementary Figure S1). The results of each trial were published elsewhere.
Interventions were categorized into six types based on their main components: (1) self-help materials (a 12-page cessation booklet); (2) very brief advice (30-s general cessation advice); (3) brief advice (5-min cessation counseling using the Ask, Warn, Advise, Refer, and Do-it-again [AWARD] model); (4) active referral to cessation services (proactively introducing existing cessation services with a referral card and providing participants’ contact details to service providers to arrange clinic visits); (5) short message services (SMS) delivering regular text messages; and (6) personalized cessation support via instant messaging (IM).
Participants in higher-intensity intervention groups (active referral, SMS, and IM) also received self-help materials and brief advice at baseline. All participants, regardless of group assignment, received self-help materials as the basic intervention. Since 2013, a financial incentive of HK$500 (≈US$64) was provided to participants who passed the biochemical validation at both 3- and 6-month follow-ups (total HK$1000 ≈ US $128).
2.4 Statistical analyses
Given that the proportion of missing data was < 10%, available case analyses were used for all baseline measures. We used an intention-to-treat approach for smoking cessation outcomes by treating participants with missing data as having no changes in smoking behavior from baseline.
Descriptive statistics were used to compare sociodemographic and smoking characteristics between participants with and without children. Differences in nicotine dependence and abstinence outcomes by co-living status with children were assessed using binary logistic regression models, with all outcome measures dichotomized. Associations between parental status (having children or not) and smoking characteristics (e.g., CPD, time to first cigarette, and nicotine dependence) were analyzed using multinomial logistic regression models, allowing for category-specific odds ratios without assuming proportional odds. An ordinal logistic regression analysis was applied to test for linear trends across ordered categories of smoking characteristics. The associations between self-efficacy of quitting (continuous variables) and parental status were estimated using a linear regression analysis, with beta-coefficients (βs) reported. All regression analyses were adjusted for sex, age, educational attainment, year of inclusion, and type of interventions.
Subgroup analyses were conducted to examine the effectiveness of the different smoking cessation interventions on biochemically validated abstinence at the 6-month follow-up, stratified by parental status. These analyses used independent binary logistic regression models adjusted for sex, age, educational attainment, and the predictors of successful quit attempts (i.e., nicotine dependence level, past quit attempt(s) within 1 year, and intention to quit within 60 days at baseline). Within the parental smoker group, additional subgroup analysis explored whether quit outcomes varied by co-living status with children, number of children, sex of the parental smoker, and whether they received a financial incentive. All analyses were conducted in Stata/MP version 16.1 (StataCorp, United States) with statistical significance set at a p-value of < 0.05.
3 Results
3.1 Baseline characteristics
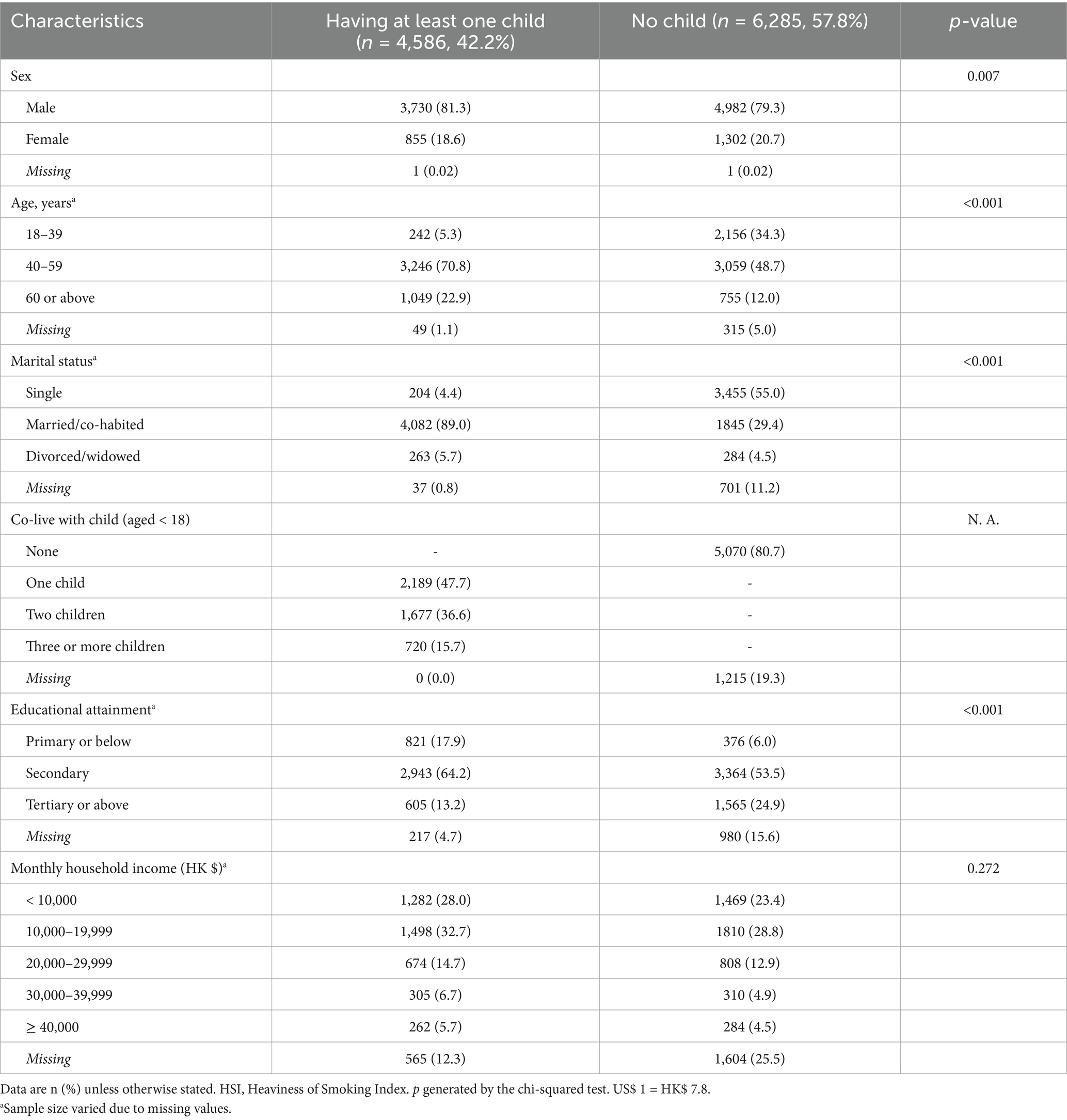
Among 10,871 participants, 8,500 (78.2%) completed the 6-month follow-up, with similar retention rates between parental (78.5%) and non-parental smokers (77.9%). Table 1 shows that 42.2% were parental smokers. Compared with non-parental smokers, parental smokers were older, had lower educational attainment, and had lower income (all p < 0.001).
3.2 Smoking and quitting characteristics among smokers with and without children
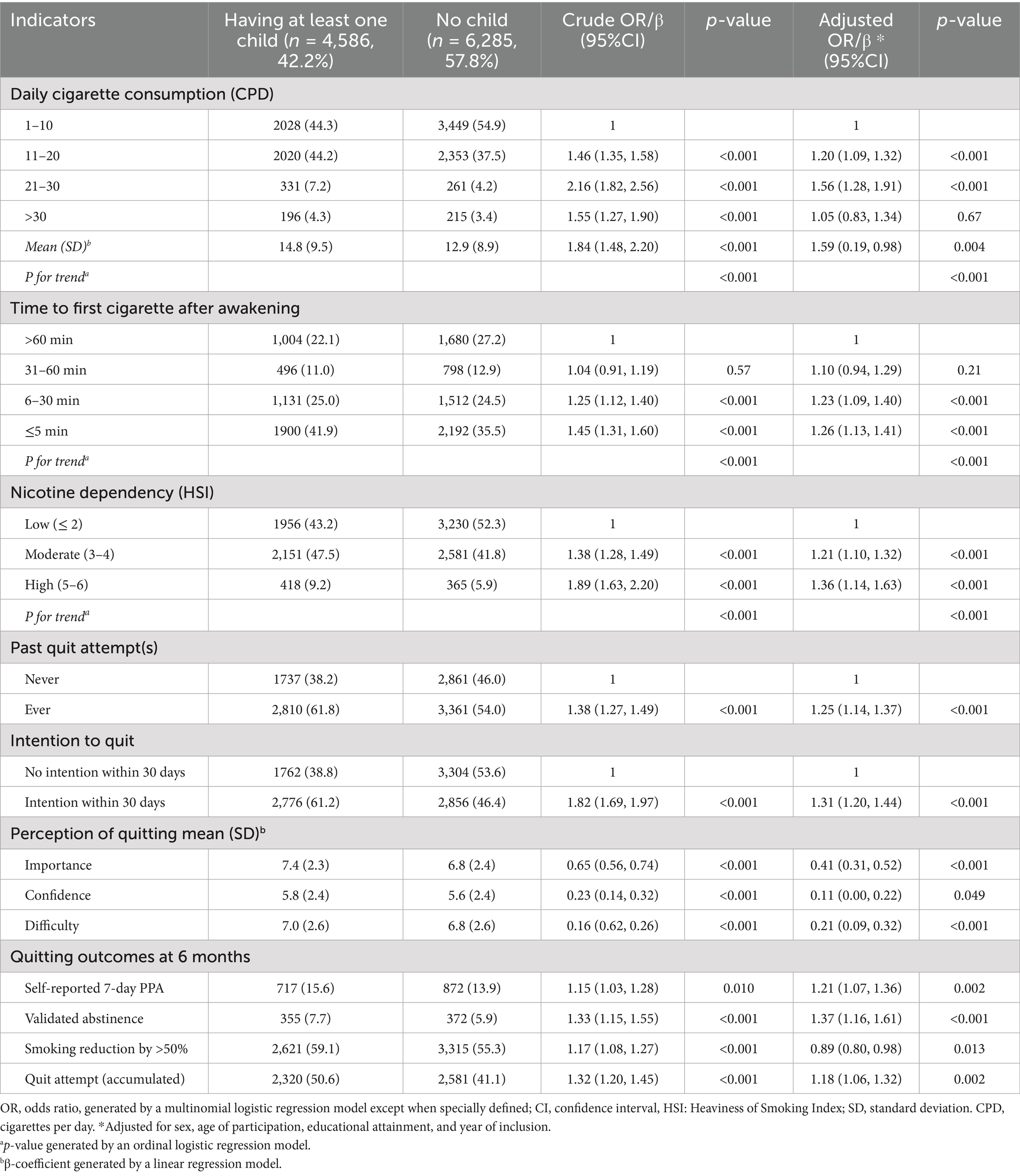
Table 2 shows that parental smokers had higher cigarette consumption (mean 14.8 (9.5) vs. 12.9(8.9), adjusted β = 1.59, p = 0.004), were more likely to smoke immediately after awakening (≤5 min: 41.9% vs. 35.5%, adjusted odds ratio, AOR = 1.26, 95% CI 1.13–1.41, p < 0.001), and had higher nicotine dependence (high: 9.2% vs. 5.9%, AOR = 1.36, 95% CI 1.14–1.63, p < 0.001).
For quitting intention, parental smokers reported more past quit attempts (61.8% vs. 54.0%, AOR = 1.25, 95% CI 1.14–1.37) and had stronger intention to quit within 30 days (61.2% vs. 46.4%, AOR = 1.31, 95% CI 1.20–1.44). Additionally, parental smokers perceived higher importance (7.4% vs. 6.8%, AOR = 0.41, 95% CI 0.31–0.52) but also higher difficulty (7.0% vs. 6.8%, AOR = 0.21, 95%CI 0.09–0.32) of quitting, as compared to non-parental smokers (all Ps < 0.001).
At 6-month follow-up, parental smokers showed significantly higher validated abstinence (7.7% vs. 5.9%, AOR = 1.37, 95% CI 1.16–1.61, p < 0.001), self-reported 7-day PPA (15.6% vs. 13.9%, AOR = 1.21, 95% CI 1.07–1.36, p = 0.002), and more accumulated quit attempts (50.6% vs. 41.1%; AOR = 1.18, 95% CI 1.06–1.32, p = 0.002).
3.3 Subgroup analyses
Table 3 shows that parental smokers who co-live with their children have significantly higher smoking abstinence at 6 months for both self-reported 7-day PPA (18.8% vs. 13.9%, AOR = 1.43, 95% CI 1.03–1.98, p = 0.032) and validated abstinence (9.9% vs. 6.5%, AOR = 1.62, 95% CI 1.04–2.52, p = 0.032) than those who have children but do not necessarily co-live with children. No significant differences were observed in quitting outcomes between smokers with fewer children vs. with more children, between smoking fathers vs. mothers, and between those that received a financial incentive vs. those that did not (all p > 0.05).
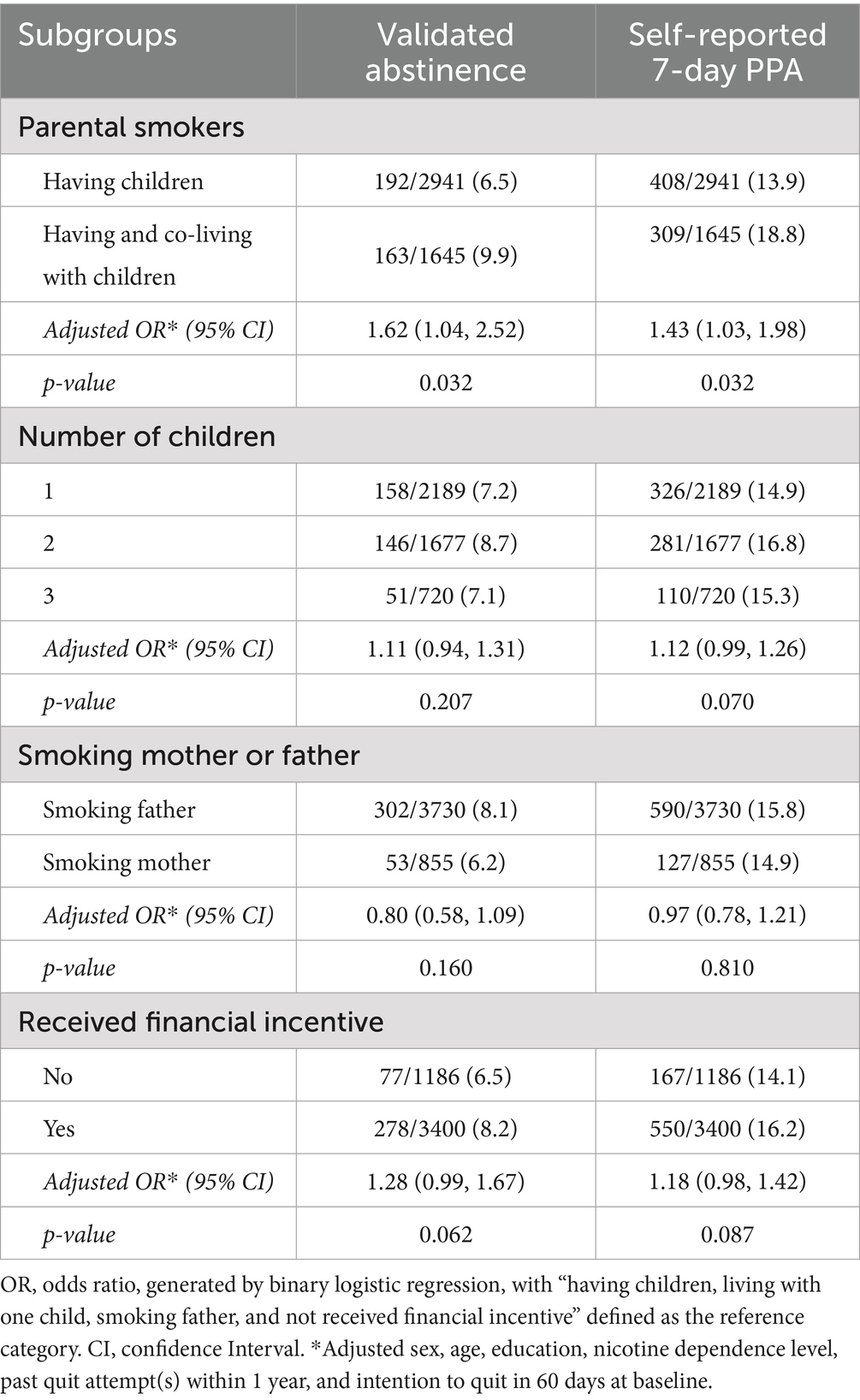
Table 3. Quitting outcomes for parental smokers by residential status, number of children, sex of parental smokers, and receipt of financial incentive (N = 4,586).
Table 4 assesses the effectiveness of different interventions on smoking cessation among smokers with and without children. Parental smokers had both higher biochemically validated abstinence (total: 7.7% vs. 5.9%, AOR = 1.37, 95% CI 1.16–1.61, p < 0.001) and self-reported abstinence (total: 15.6% vs. 13.9%, AOR = 1.21, 95% CI 1.07–1.36, p = 0.002) at 6 months after receiving all types of community-based brief intervention.
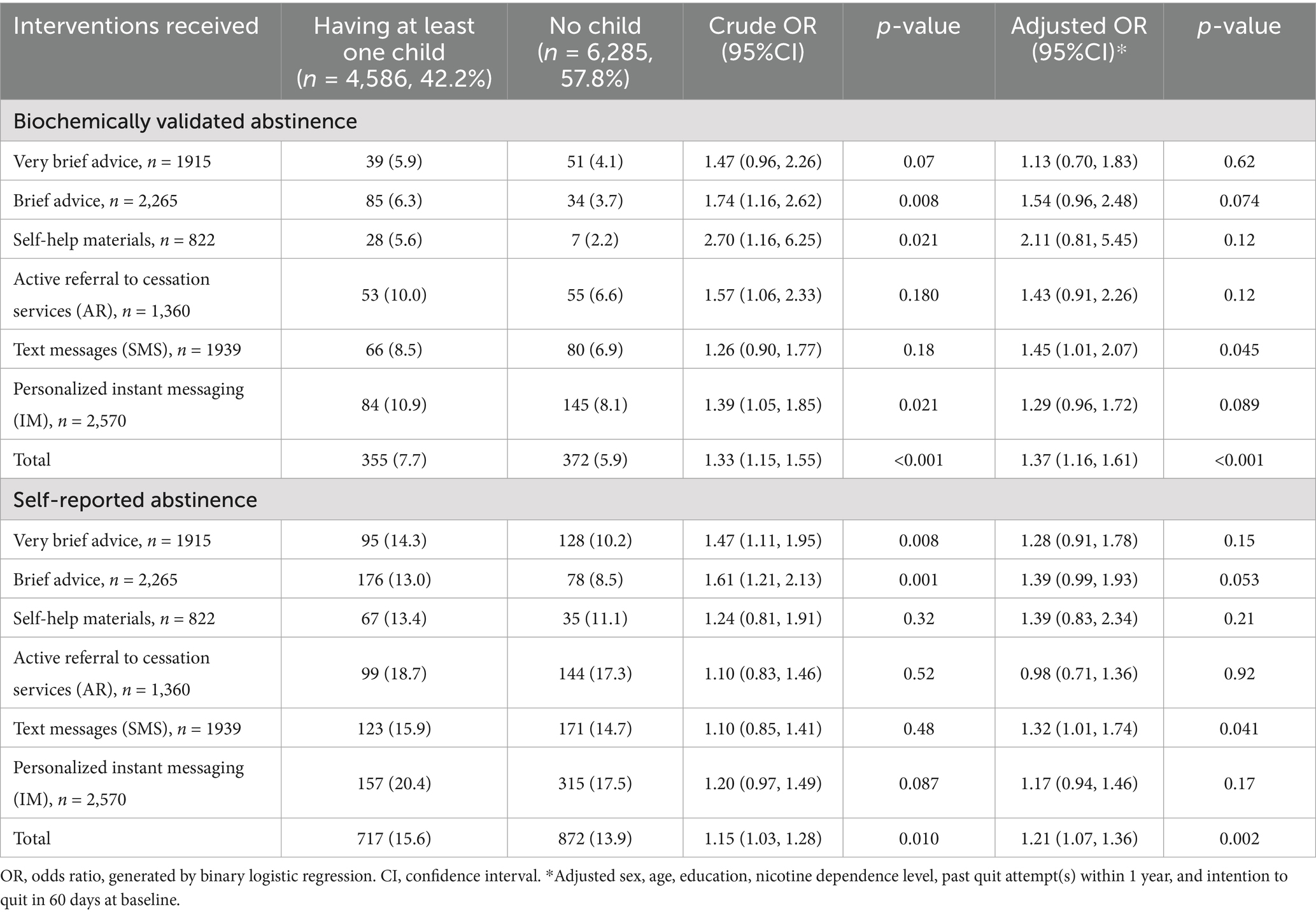
Table 4. Effect of community-based brief interventions on quitting outcomes at 6 months by whether having a child (N = 10,871).
4 Discussion
The present study investigated the impact of parenthood on smoking behavior and cessation outcomes among smokers in Hong Kong. Baseline characteristic analysis revealed that parental smokers are associated with lower income and educational attainment. Several studies have found a similar strong association between parents’ socioeconomic status and indoor smoking prevalence (27, 28). Parental smokers with lower educational attainment often reside in communities with higher smoking acceptance, where people are more inclined to perceive smoking in the presence of children as normal (29, 30). Socially disadvantaged individuals often experience greater daily stress and consequently smoke more cigarettes as a coping mechanism (31), with stress possibly mediating the relationship between socioeconomic status and smoking prevalence (32).
For this study, parenthood was associated with more intensive smoking patterns and higher addiction levels, as evidenced by a greater proportion of parental smokers who smoked over 15 cigarettes per day and smoked within 5 min of awakening. Time to first cigarette is recognized as a stronger predictor of physiological nicotine dependence, whereas the number of cigarettes per day better reflects psychological dependence on nicotine’s negatively reinforcing effects (33). This may suggest that parental smokers have both stronger physiological and psychological nicotine dependence, making them more persistent smokers compared to non-parental smokers. The demands of parenting may increase parental smokers’ reliance on smoking as a coping mechanism for stress, anxiety, or fatigue (34). These factors together make parental smokers more resistant to quitting and more persistent in their smoking behavior than non-parental smokers.
On the other hand, parental smokers demonstrated greater motivation to quit, perceived quitting as more important, and had more successful quitting at 6 months post-intervention. Parenthood is a known motivating factor for smoking cessation as well as a protective factor to deter smoking initiation (5, 35). Parental smokers are more likely to consider their children’s potential adverse health outcomes when making decisions regarding smoking and quitting (2). However, their high nicotine dependence increases the likelihood of relapse, which may explain their more frequent past quit attempts. This finding aligns with prior evidence reporting that smoking fathers with more quit attempts have a higher risk of nicotine dependence (36).
Subgroup analyses showed that parental smokers living with children had more favorable quitting outcomes at 6 months post-intervention compared to parental smokers who do not live with children. The presence of children in the household may enhance the success of smoking cessation efforts among parents, potentially driven by increased concern about secondhand smoke exposure on children’s health. The lack of significant differences in quitting outcomes between smokers with fewer vs. more children could potentially be due to the overarching motivation that parenthood provides for smoking cessation. Parents may be equally motivated to quit to protect their children’s health, regardless of family size. The lack of significant differences in quitting outcomes for smoking mothers and fathers may be explained by the progressive convergence of gender roles, leading to less pronounced differences in smoking patterns between mothers and fathers. The absence of differential effects by financial incentive suggests that intrinsic motivations, such as the desire to protect children from tobacco-related disease, may be equal to or more important than extrinsic rewards in supporting cessation among parental smokers.
Community-based behavioral interventions were found to be effective in supporting smoking cessation among parents. Such brief intervention models provided more convenient ways for parental smokers to access smoking cessation information, counseling, and services. Proactively approaching parental smokers and providing brief advice, a self-help booklet, and active referral for smoking cessation services showed higher cessation outcomes in parental smokers, echoing prior research showing that proactively enrolling parents in smoking quitlines during pediatric visits is associated with greater quitline use compared to mere provider recommendations (37). Cessation programs that effectively deliver assistance to parents who might not otherwise receive it are likely to achieve more favorable outcomes (38). However, to select the most appropriate type of intervention, more information is necessary. This aligns with the CEASE program’s recommendation to consider multiple perspectives when developing and implementing a tailored practice change program (39).
This study has several limitations. First, although the data were derived from 10 RCTs, several design limitations preclude causal inference. The intervention components were not entirely identical across trials, participants were not randomized according to parental status, and the original trials were not designed to evaluate the causal impact of parental status on cessation outcomes. As the study design used a secondary analysis approach, a definitive cause-and-effect relationship could not be established. Second, the generalizability of findings, especially the differences in cessation outcomes by the sex of parental smokers, may be constrained as the study primarily included Chinese-speaking Hong Kong residents. Parenting and smoking norms differ markedly between East Asian societies and the West. In East Asia, smoking is accepted among men, symbolizing masculinity and authority, whereas it is less accepted among women (40). This contrasts with Western societies, with less gender disparity in smoking rates (41, 42). Third, the exclusion of individuals using smoking cessation medication or other services might have introduced bias. Finally, other factors that potentially influence parents’ smoking and cessation behavior, including children’s age and health status or the presence of other smokers in the household (e.g., spouse or cohabitants), were not measured in this study. Future studies examining a comprehensive range of child- and family-related health and smoking behavior are warranted.
5 Conclusion
Parental smokers exhibited not only greater nicotine dependence but also stronger motivation to quit than non-parental smokers, and they achieved higher abstinence rates following brief community-based interventions. Tailored cessation strategies that address nicotine dependence and harness parental motivation are warranted to increase cessation rates and inform future tobacco control policy.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by The University of Hong Kong/ Hospital Authority Hong Kong West Cluster Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YG: Investigation, Writing – original draft. ML: Investigation, Writing – original draft. TL: Formal analysis, Writing – review & editing. DC: Writing – review & editing, Formal analysis. NG: Methodology, Writing – review & editing. HT: Writing – review & editing, Resources. VL: Resources, Writing – review & editing. SC: Writing – review & editing, Supervision. MW: Supervision, Writing – review & editing. SZ: Writing – review & editing, Supervision, Project administration.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1687893/full#supplementary-material
References
1. Census and Statistics Department (2023) Thematic household survey report - report no. 79- pattern of smoking. Available online at: https://www.censtatd.gov.hk/en/wbr.html?ecode=B11302012024XX01 (Accessed: 21 May 2025).
2. Nabi-Burza, E, Wasserman, R, Drehmer, JE, Walters, BH, Luo, M, Ossip, D, et al. Spontaneous smoking cessation in parents. J Smok Cessat. (2021) 2021:5526715. doi: 10.1155/2021/5526715
3. Kanis, J, Byczkowski, T, and Mahabee-Gittens, EM. Motivation to quit smoking in parental smokers in the pediatric emergency department. Pediatr Emerg Care. (2014) 30:546–51. doi: 10.1097/PEC.0000000000000179
4. Friebely, J, Rigotti, NA, Chang, Y, Hall, N, Weiley, V, Dempsey, J, et al. Parent smoker role conflict and planning to quit smoking: a cross-sectional study. BMC Public Health. (2013) 13:164. doi: 10.1186/1471-2458-13-164
5. Caldwell, AL, Tingen, MS, Nguyen, JT, Andrews, JO, Heath, J, Waller, JL, et al. Parental smoking cessation: impacting children’s tobacco smoke exposure in the home. Pediatrics. (2018) 141:S96–S106. doi: 10.1542/peds.2017-1026M
6. Burns, RJ, Rothman, AJ, Fu, SS, Lindgren, B, Vock, DM, and Joseph, AM. Longitudinal care improves cessation in smokers who do not initially respond to treatment by increasing cessation self-efficacy, satisfaction, and readiness to quit: a mediated moderation analysis. Annals Behav Med: Pub Society Behav Med. (2016) 50:58–69. doi: 10.1007/s12160-015-9732-1
7. Layoun, N, Hallit, S, Waked, M, Aoun Bacha, Z, Godin, I, Leveque, A, et al. Predictors of past quit attempts and duration of abstinence among cigarette smokers. J Epidemiol Global Health. (2017) 7:199–206. doi: 10.1016/j.jegh.2017.06.003
8. Bottorff, JL, Radsma, J, Kelly, M, and Oliffe, JL. Fathers’ narratives of reducing and quitting smoking. Sociol Health Illn. (2009) 31:185–200. doi: 10.1111/j.1467-9566.2008.01126.x
9. Klesges, LM, Johnson, KC, Ward, KD, and Barnard, M. Smoking cessation in pregnant women. Obstet Gynecol Clin N Am. (2001) 28:269–82. doi: 10.1016/s0889-8545(05)70200-x
10. Mullen, PD, Richardson, MA, Quinn, VP, and Ershoff, DH. Postpartum return to smoking: who is at risk and when. American J Health Promotion: AJHP. (1997) 11:323–30.
11. Seeker-Walker, RH, Solomon, LJ, Flynn, BS, Skelly, JM, Lepage, SS, Goodwin, GD, et al. Smoking relapse prevention counseling during prenatal and early postnatal care. Am J Prev Med. (1995) 11:86–93.
12. Attarabeen, O, Alkhateeb, F, Sambamoorthi, U, Larkin, K, Newton, M, and Kelly, K. Impact of cognitive and social factors on smoking cessation attempts among US adult Muslim smokers. Innovations in Pharmacy. (2020) 11:18. doi: 10.24926/iip.v11i3.3382
13. Diamanti, A, Papadakis, S, Schoretsaniti, S, Rovina, N, Vivilaki, V, Gratziou, C, et al. Smoking cessation in pregnancy: an update for maternity care practitioners. Tob Induc Dis. (2019) 17:57. doi: 10.18332/tid/109906
14. Jones, SE, Hamilton, S, Bell, R, Araújo-Soares, V, and White, M. Acceptability of a cessation intervention for pregnant smokers: a qualitative study guided by normalization process theory. BMC Public Health. (2020) 20:1512. doi: 10.1186/s12889-020-09608-2
15. Lumley, J, Oliver, S, and Waters, E. Interventions for promoting smoking cessation during pregnancy. Cochrane Database of Systematic Reviews. (2000) CD001055. doi: 10.1002/14651858.CD001055
16. Oncken, CA. Prenatal tobacco prevention and cessation interventions for women in low- and middle-income countries. Acta Obstet Gynecol Scand. (2010) 89:442–53. doi: 10.3109/00016341003678450
17. Luk, TT, Lam, TH, Leung, WC, Leung, KY, Cheung, KW, Kwa, C, et al. Brief advice, nicotine replacement therapy sampling, and active referral for expectant fathers who smoke cigarettes: a randomized clinical trial. JAMA Intern Med. (2021) 181:1081–9. doi: 10.1001/jamainternmed.2021.2757
18. Xia, W, Li, HCW, Cai, W, Song, P, Zhou, X, Lam, KWK, et al. Effectiveness of a video-based smoking cessation intervention focusing on maternal and child health in promoting quitting among expectant fathers in China: a randomized controlled trial. PLoS Med. (2020) 17:e1003355. doi: 10.1371/journal.pmed.1003355
19. Crawford, JT, Tolosa, JE, and Goldenberg, RL. Smoking cessation in pregnancy: why, how, and what next. Clin Obstet Gynecol. (2008) 51:419–35. doi: 10.1097/GRF.0b013e31816fe9e9
20. Hammoud, AO, Bujold, E, Sorokin, Y, Schild, C, Krapp, M, and Baumann, P. Smoking in pregnancy revisited: findings from a large population-based study. Am J Obstet Gynecol. (2005) 192:1856–62. doi: 10.1016/j.ajog.2004.12.057
21. Hovell, MF, Zakarian, JM, Matt, GE, Liles, S, Jones, JA, Hofstetter, CR, et al. Counseling to reduce children’s secondhand smoke exposure and help parents quit smoking: a controlled trial. Nicotine & Tobacco Res: Official J Society for Res Nicotine Tobacco. (2009) 11:1383–94. doi: 10.1093/ntr/ntp148
22. Winickoff, JP, Buckley, VJ, Palfrey, JS, Perrin, JM, and Rigotti, NA. Intervention with parental smokers in an outpatient pediatric clinic using counseling and nicotine replacement. Pediatrics. (2003) 112:1127–33. doi: 10.1542/peds.112.5.1127
23. Matkin, W, Ordóñez-Mena, JM, and Hartmann-Boyce, J. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. (2019) 5:CD002850. doi: 10.1002/14651858.CD002850.pub4
24. Whittaker, R. Mobile phone text messaging and app-based interventions for smoking cessation. Cochrane Database Syst Rev. (2019) 10:CD006611. doi: 10.1002/14651858.CD006611.pub5
25. Dai, S, Chan, MHM, Kam, RKT, Li, AM, Au, CT, and Chan, KCC. Monthly motivational interview counseling and nicotine replacement therapy for smoking parents of pediatric patients: a randomized controlled trial. Front Pediatr. (2022) 10:798351. doi: 10.3389/fped.2022.798351
26. Kranzler, HR, Washio, Y, Zindel, LR, Wileyto, EP, Srinivas, S, Hand, DJ, et al. Placebo-controlled trial of bupropion for smoking cessation in pregnant women. American J Obstetrics Gynecol MFM. (2021) 3:100315. doi: 10.1016/j.ajogmf.2021.100315
27. Luu, NM, Tran, TTH, Luong, NK, Phan, TH, Phan, VC, Khuong, QL, et al. Smoking cessation, quit attempts and predictive factors among Vietnamese adults in 2020. Asian Pac J Cancer Prev. (2023) 24:1701–10. doi: 10.31557/APJCP.2023.24.5.1701
28. Saito, J, Shibanuma, A, Yasuoka, J, Kondo, N, Takagi, D, and Jimba, M. Education and indoor smoking among parents who smoke: the mediating role of perceived social norms of smoking. BMC Public Health. (2018) 18:211. doi: 10.1186/s12889-018-5082-9
29. Chuang, Y-C, Cubbin, C, Ahn, D, and Winkleby, MA. Effects of neighbourhood socioeconomic status and convenience store concentration on individual level smoking. J Epidemiol Community Health. (2005) 59:568–73. doi: 10.1136/jech.2004.029041
30. Dai, S. ‘Parental knowledge, attitude, and practice on tobacco use, smoking cessation, and children’s environmental tobacco smoke exposure. Front Public Health. (2021) 9:733667. doi: 10.3389/fpubh.2021.733667
31. Meyer, IH, Schwartz, S, and Frost, DM. Social patterning of stress and coping: does disadvantaged social statuses confer more stress and fewer coping resources? Soc Sci Med. (2008) 67:368–79. doi: 10.1016/j.socscimed.2008.03.012
32. Jahnel, T, Ferguson, SG, Shiffman, S, and Schüz, B. Daily stress as link between disadvantage and smoking: an ecological momentary assessment study. BMC Public Health. (2019) 19:1284. doi: 10.1186/s12889-019-7631-2
33. Hobkirk, AL, Krebs, NM, and Muscat, JE. Income as a moderator of psychological stress and nicotine dependence among adult smokers. Addict Behav. (2018) 84:215–23. doi: 10.1016/j.addbeh.2018.04.021
34. Barroso-Hurtado, M, Suárez-Castro, D, Martínez-Vispo, C, Becoña, E, and López-Durán, A. Perceived stress and smoking cessation: the role of smoking urges. Int J Environ Res Public Health. (2023) 20:1257. doi: 10.3390/ijerph20021257
35. Görlitz, K, and Tamm, M. Parenthood and smoking. Econ Hum Biol. (2020) 38:100874. doi: 10.1016/j.ehb.2020.100874
36. Guo, Y, Liu, DY, Wang, YJ, Huang, MJ, Jiang, N, Hou, Q, et al. Family functioning and nicotine dependence among smoking fathers: a cross-sectional study. BMC Public Health. (2023) 23:658. doi: 10.1186/s12889-023-15475-4
37. Drehmer, JE, Hipple, B, Nabi-Burza, E, Ossip, DJ, Chang, Y, Rigotti, NA, et al. Proactive enrollment of parents to tobacco quitlines in pediatric practices is associated with greater quitline use: a cross-sectional study. BMC Public Health. (2016) 16:520. doi: 10.1186/s12889-016-3147-1
38. Nabi-Burza, E, Drehmer, JE, Hipple Walters, B, Rigotti, NA, Ossip, DJ, Levy, DE, et al. Treating parents for tobacco use in the pediatric setting: the clinical effort against secondhand smoke exposure cluster randomized clinical trial. JAMA Pediatr. (2019) 173:931–9. doi: 10.1001/jamapediatrics.2019.2639
39. Winickoff, JP. The clinical effort against secondhand smoke exposure (CEASE) intervention: a decade of lessons learned. J Clin Outcomes Manag: JCOM. (2012) 19:414–9.
40. Kodriati, N, Pursell, L, and Hayati, EN. A scoping review of men, masculinities, and smoking behavior: the importance of settings. Glob Health Action. (2018) 11:1589763. doi: 10.1080/16549716.2019.1589763
41. Lushniak, B.D. (2014) The health consequences of smoking—50 years of progress: a report of the surgeon general. Available online at: https://stacks.cdc.gov/view/cdc/21569 (Accessed: 21 May 2025).
Keywords: parental smokers, smoking cessation, smoking behaviors, nicotine dependence, community-based intervention, behavioral interventions
Citation: Ge Y, Li M, Luk TT, Cheung DYT, Guo N, Tong HSC, Lai VWY, Chan SSC, Wang MP and Zhao S (2025) Higher nicotine dependence and greater smoking abstinence in parental than non-parental smokers: a secondary analysis of smoking cessation trials. Front. Public Health. 13:1687893. doi: 10.3389/fpubh.2025.1687893
Edited by:
James Clifford, East Carolina University, United StatesReviewed by:
Anqi Cheng, China-Japan Friendship Hospital, ChinaM. A. Rifat, BRAC University, Bangladesh
Copyright © 2025 Ge, Li, Luk, Cheung, Guo, Tong, Lai, Chan, Wang and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shengzhi Zhao, bHViYWJlenpAY29ubmVjdC5oa3UuaGs=
†These authors have contributed equally to this work and share first authorship
 Yiran Ge1†
Yiran Ge1† Tzu Tsun Luk
Tzu Tsun Luk Derek Yee Tak Cheung
Derek Yee Tak Cheung Ningyuan Guo
Ningyuan Guo Man Ping Wang
Man Ping Wang Shengzhi Zhao
Shengzhi Zhao