- 1Department of Nursing Science, Faculty of Medicine, Universiti Malaya, Kuala Lumpur, Malaysia
- 2Department of Physiology, North Henan Medical University, Xinxiang, China
- 3Department of Geriatric Medicine, Shengli Clinical Medical College of Fujian Medical University, Fuzhou, China
- 4Fujian Provincial Center for Geriatrics, Fuzhou University Affiliated Provincial Hospital, Fuzhou, China
- 5School of Nursing, Henan University of Science and Technology, Luoyang, Henan, China
- 6Rheumatology Unit, The First Affiliated Hospital, College of Clinical Medicine of Henan University of Science and Technology, Luoyang, China
Background: This study aimed to investigate the prevalence of depression, anxiety, and perceived stress among nursing home caregivers in China and to examine the associated factors.
Methods: A multicenter cross-sectional study was conducted among 1,341 caregivers in nursing homes across Henan Province, China. Standardized instruments were applied, including the Self-Rating Depression Scale (SDS), Self-Rating Anxiety Scale (SAS), and the 10-item Perceived Stress Scale (PSS-10). Descriptive statistics, univariate analysis, and multivariable logistic regression were performed to identify independent predictors of psychological distress.
Results: The prevalence of depression and anxiety was 34.8 and 10.8%, respectively, while 49.6% of caregivers reported moderate-to-high levels of stress. Significant predictors included city region, type of nursing home, educational level, monthly income, working hours, night shifts, presence of chronic diseases, attention to mental health, and participation in psychological training. Higher education and moderate income were protective factors, whereas employment in rural private nursing homes, low engagement in mental health practices, and the presence of chronic diseases increased risks. Longer working hours and more frequent night shifts were unexpectedly associated with lower stress levels.
Conclusion: Depression and stress represent the major psychological concerns among nursing home caregivers in China. Targeted interventions should prioritize routine mental health screening, workplace-based psychological support, and policy measures aimed at improving working conditions and access to training, thereby safeguarding caregiver well-being and supporting the sustainability of long-term care services.
1 Introduction
The rapid acceleration of global population aging has become one of the most pressing public health and social challenges of the 21st century (1). China, which accounts for one-fifth of the world’s older population (2), had 220 million people aged 65 years or above by the end of 2024, representing 15.6% of the total population (3). This number is projected to reach 366 million by 2050 (4). Such unprecedented demographic shifts have greatly intensified the demand for long-term care services and imposed considerable pressure on professional caregivers (5). Caregiving, whether provided formally or informally, involves substantial physical, emotional, and social demands, often leading to fatigue, stress, and burnout among care providers (6). These challenges are particularly pronounced in institutional settings where care needs are continuous and complex.
Nursing home caregivers play a crucial role in providing physical, emotional, and social support for older adults, particularly those who are frail, disabled, or living with chronic illnesses (7). However, caregiving in nursing homes is characterized by heavy physical workload and high emotional demands, while a global shortage of long-term care workers has become increasingly severe (8). In China, the long-term care sector faces substantial challenges. Nursing home caregivers often endure intense workloads, time pressure, and limited resources (9), alongside insufficient training, low wages, and limited social recognition (10, 11). These unfavorable conditions may lead to significant psychological distress (12).
Evidence suggests that nursing home caregivers represent a high-risk yet often overlooked group in terms of mental health (13). A systematic review by Gray, Birtles (14) reported that more than 20% of nursing home caregivers experienced anxiety and depressive symptoms, which was markedly higher than the prevalence among hospital nurses (15). A cross-sectional survey in northeastern China found that 44% of caregivers reported anxiety and 19.4% reported depressive symptoms (12). Studies from Germany, France, Spain, and Japan also indicated high prevalence rates of anxiety and depression among caregivers in long-term care facilities (16–20). In addition, perceived stress, defined as the individual’s subjective appraisal of external stressors, has been recognized as a key construct for understanding caregivers’ mental health (21). Elevated levels of perceived stress have been strongly linked to negative outcomes such as sleep disturbances, emotional exhaustion, somatic complaints, and health-damaging behaviors (20, 22).
Anxiety, depression, and perceived stress among nursing home caregivers are influenced by multiple demographic, occupational, and psychosocial factors. Individual characteristics, such as older age, lack of marital support, and poor health, have been shown to be associated with higher psychological distress (23–25). Occupational stressors, including heavy workload, low salary, shift work, and limited organizational support, also contribute substantially to emotional strain in long-term care (26–28). Night shifts and irregular work schedules may disrupt circadian rhythms, thereby increasing risks of depression, sleep problems, and somatic symptoms (12, 29).
Although awareness of caregivers’ mental health burden is growing, research in China remains limited, particularly large-scale, multicenter investigations that not only document the prevalence of psychological symptoms but also identify associated sociodemographic and occupational factors. To our knowledge, no prior study has systematically examined the comorbidity of anxiety, depression, and stress among Chinese nursing home caregivers. Identifying modifiable risk and protective factors is essential for developing targeted interventions, policy responses, and support mechanisms for caregivers. Therefore, the present study aimed to: (1) assess the prevalence of anxiety, depression, and perceived stress among nursing home caregivers in China; and (2) identify the risk and protective factors associated with these mental health outcomes.
2 Methods
2.1 Samples and data collection
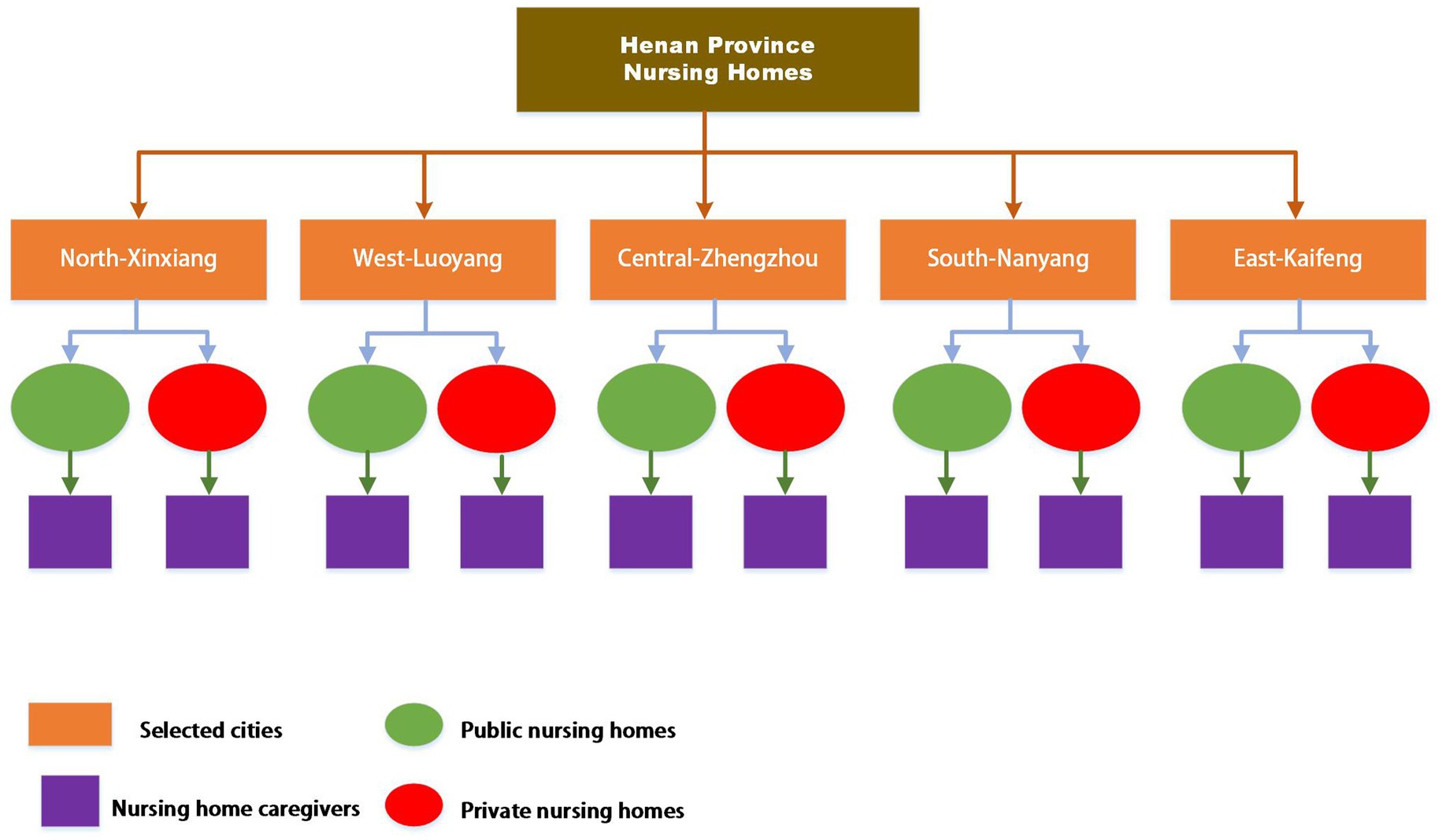
This multicenter cross-sectional study was conducted among nursing home caregivers in Henan Province, China, between November 2024 and February 2025. To ensure representativeness, a multi-stage cluster sampling strategy was applied. In the first stage, stratified random sampling was performed at the city level. The 18 prefecture-level cities in Henan Province were categorized into five geographic regions (north, south, east, west, and central). One city was randomly selected from each region: Zhengzhou, Xinxiang, Luoyang, Nanyang, and Kaifeng. In the second stage, public and private nursing homes were identified in each selected city, and disproportionate stratified sampling was used to select a total of 46 facilities (18 public and 28 private). In the third stage, eligible caregivers were recruited from the selected facilities using convenience sampling. The multi-stage sampling procedure is illustrated in Figure 1.
The required sample size was estimated according to the formula by Chow, Shao (30), with a significance level of α = 0.05 (95% confidence). When the allowable error (δ) was set at 0.05 and the estimated standard deviation (σ) was 0.83, the sample size was calculated as:
To account for a 20% potential non-response or sampling bias (31), the final target sample was 1,324 (1,059 ÷ 0.8 ≈ 1,324). The final valid sample of 1,341 caregivers exceeded this target, ensuring adequate statistical power and representativeness.
Inclusion criteria were: (1) currently employed as a caregiver in a nursing home, and (2) having worked at the institution for at least 6 months. Caregivers who were on leave or declined participation were excluded. With the support of institutional administrators, the research team first obtained formal permission from nursing home directors to conduct the survey (see Supplementary material), obtained the complete list of caregivers, and coordinated survey schedules. The study purpose, procedures, and confidentiality assurances were explained to all potential participants, and informed consent was obtained. Caregivers then voluntarily completed a structured questionnaire via the secure online platform Wenjuanxing, ensuring both convenience and data integrity.
The research team consisted of one doctoral student, one psychologist, and four trained data collectors. All team members received systematic training on study procedures, ethical principles, and participant support. Written permission was obtained from all participating institutions prior to data collection. Survey administration was scheduled in coordination with caregivers’ working hours to minimize disruption to daily care tasks.
2.2 Instruments
2.2.1 Sociodemographic questionnaire
A structured questionnaire was used to collect sociodemographic characteristics, including gender, age, and years of work experience, among others.
2.2.2 Self-rating anxiety scale (SAS)
Anxiety symptoms were assessed using the Self-Rating Anxiety Scale (SAS) developed by Zung (32) and translated and validated into Chinese by Wang, Zhengyu (33). The scale contains 20 items rated on a 4-point scale (“none or a little of the time” = 1 to “most or all of the time” = 4). Fifteen items are positively worded, and five (items 5, 9, 13, 17, and 19) are reverse scored. The raw total score is multiplied by 1.25 to yield a standardized score ranging from 25 to 100. Scores <50 indicate no anxiety, 50–59 mild anxiety, 60–69 moderate anxiety, and ≥70 severe anxiety. In this study, Cronbach’s α was 0.807.
2.2.3 Self-rating depression scale (SDS)
Depressive symptoms were measured using the Self-Rating Depression Scale (SDS) developed by Zung and translated into Chinese by Wang, zhengyu (34). The SDS consists of 20 items rated on a 4-point scale (1 = rarely to 4 = most of the time). Ten items are positively worded, while items 2, 5, 6, 11, 12, 14, 16, 17, 18, and 20 are reverse scored. The raw score is multiplied by 1.25 to yield a standardized score (range: 25–100), with higher scores indicating greater severity of depression. Scores <50 indicate no depression, 50–59 mild, 60–69 moderate, and ≥70 severe depression (35). In this study, Cronbach’s α was 0.850.
2.2.4 Perceived stress Scale-10 (PSS-10)
Perceived stress was measured using the 10-item Perceived Stress Scale (PSS-10) developed by Cohen, Kamarck (36) and translated into Chinese by Ng (37). The scale assesses the degree to which life situations are perceived as unpredictable, uncontrollable, and overwhelming over the past month. Items are rated on a 5-point Likert scale ranging from 0 (never) to 4 (very often), yielding a total score of 0–40. Scores of 0–13 indicate very low stress, 14–18 low to moderate stress, 19–25 moderate to high stress, and 26–40 high stress. Items 4, 5, 7, and 8 are reverse scored. In this study, Cronbach’s α was 0.775.
2.3 Statistical analyses
All statistical analyses were performed using SPSS version 26.0. Descriptive statistics were used to summarize the characteristics of the sample. Continuous variables were expressed as means and standard deviations (SD), while categorical variables were presented as frequencies and percentages. To examine differences in anxiety, depression, and perceived stress across sociodemographic groups, univariate analysis was conducted, with independent-samples t tests and one-way analysis of variance (ANOVA) used for continuous variables.
Multivariable logistic regression models were employed to identify independent factors associated with anxiety, depression, and perceived stress. Variables that were significant in the bivariate analyses were entered into the regression models. Odds ratios (ORs) with 95% confidence intervals (CIs) were reported. All tests were two-tailed, and a p-value < 0.05 was considered statistically significant.
Prior to multivariable logistic regression analyses of SAS, SDS, and PSS-10, collinearity diagnostics confirmed no multicollinearity (VIFs < 2), and Hosmer–Lemeshow tests indicated good model fit for all outcomes (SAS: χ2 = 9.226, p = 0.324; SDS: χ2 = 9.334, p = 0.315; PSS: χ2 = 6.987, p = 0.538), supporting robust assessment of sociodemographic and work-related influences on psychological distress, see Supplementary Tables S1–S6.
3 Result
3.1 Descriptive information
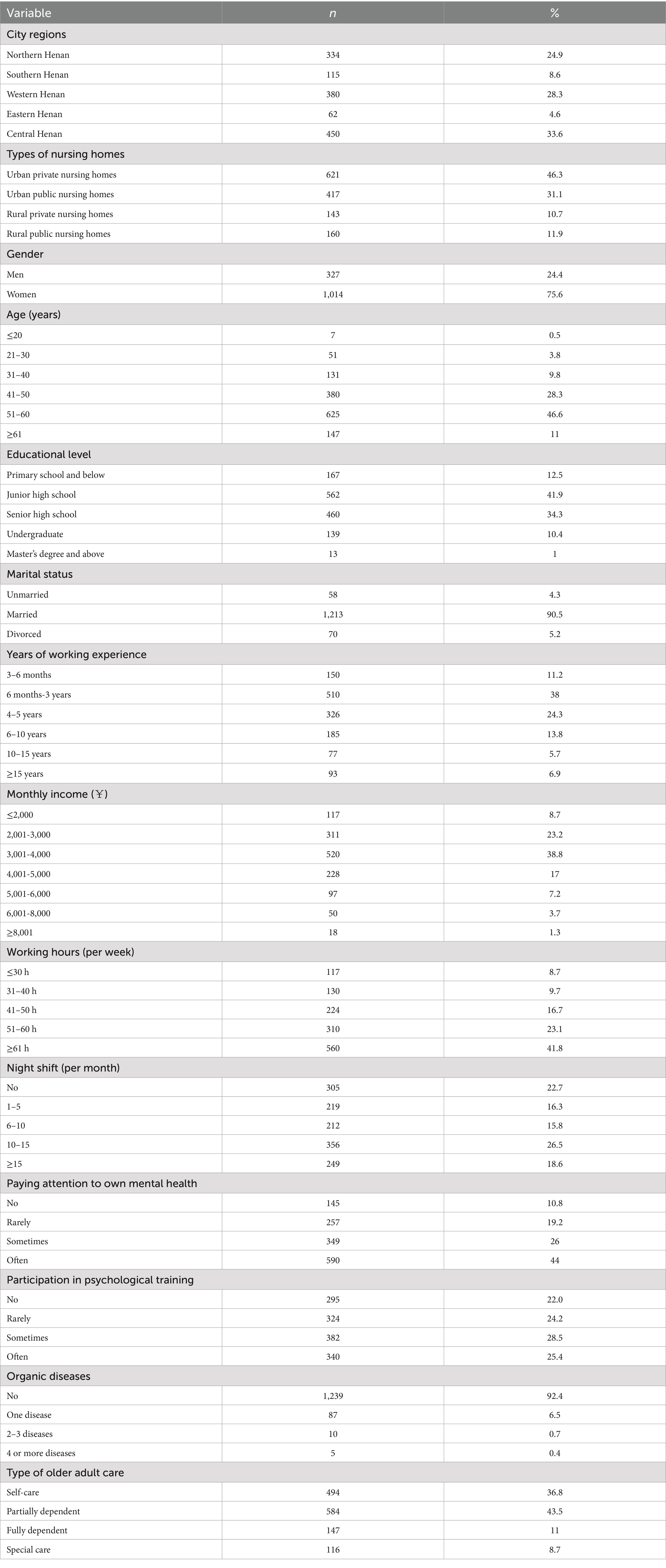
The online survey was validated on the Wenjuanxing platform prior to data download. Of the 1,500 distributed questionnaires, 147 were excluded due to incomplete responses, resulting in a final sample of 1,341 nursing home caregivers (response rate: 89.4%). The majority were women (75.6%), aged 51–60 years (46.6%), and married (90.5%). Most caregivers had a junior high school (41.9%) or senior high school education (34.3%). Over one-third (38.0%) had worked for 6 months to 3 years, and 24.3% had 4–5 years of work experience. Regarding income, 38.8% earned between RMB 3,001 and 4,000 monthly, and 41.8% reported working more than 61 h per week. Approximately 44.0% often paid attention to their own mental health, and 25.4% frequently participated in psychological training. Most participants reported no organic disease (92.4%), and the largest group cared for partially dependent older adults (43.5%), see Table 1.
3.2 Prevalence of depression, anxiety and stress
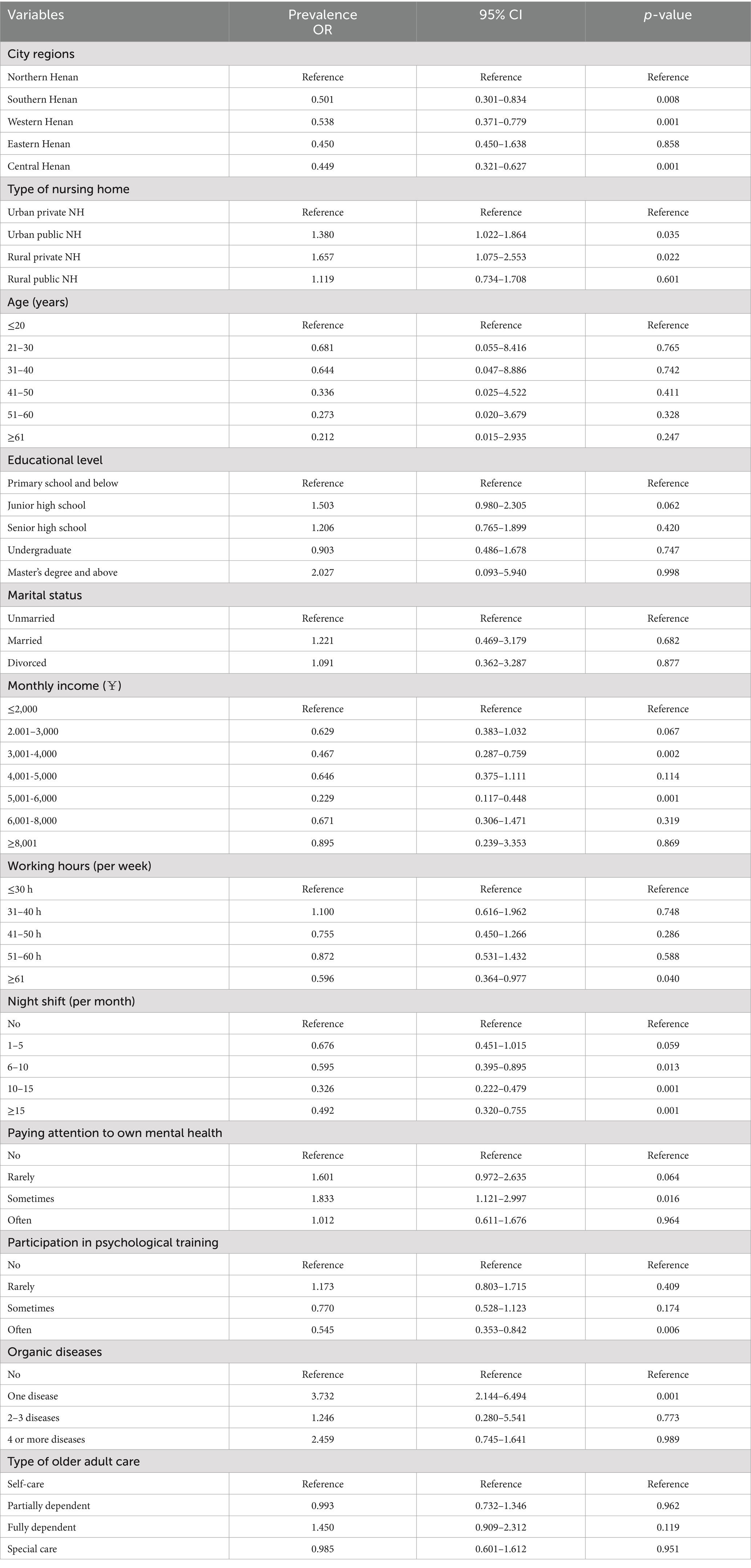
The mean SAS score was 39.31 ± 8.39, with 89.2% of caregivers showing no anxiety, while 9.0% had mild anxiety, and only 1.8% experienced moderate-to-severe anxiety. The mean SDS score was 44.93 ± 11.22, with 65.2% having no depression, 34.8% had depression, 21.3% mild depression, and 13.5% moderate-to-severe depression. The mean PSS-10 score was 12.92 ± 6.01; half of the caregivers (50.4%) reported very low stress, 32.4% low to moderate stress, and 17.2% moderate-to-high or high stress (Table 2).
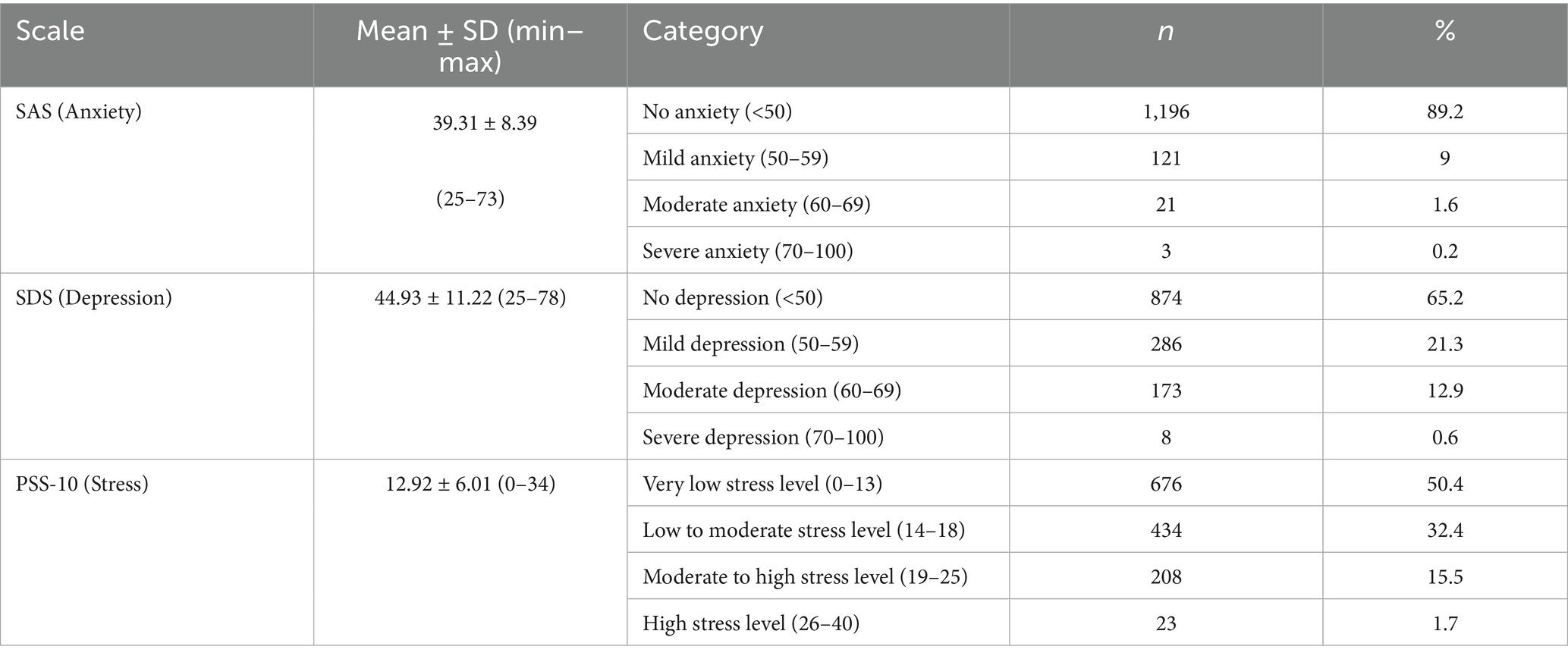
Table 2. Distribution of anxiety, depression, and stress levels among nursing home caregivers (N = 1,341).
3.3 Bivariate factors associated with anxiety, depression, and stress
Bivariate analyses showed that city region, type of nursing home, age, educational level, marital status, monthly income, working hours, night shifts, attention to mental health, participation in psychological training, and presence of organic diseases were significantly associated with anxiety, depression, and stress (all p < 0.05). Type of older adult care was significantly related to depression and stress but not anxiety. In contrast, gender and years of working experience showed no significant associations with any of the three outcomes (all p > 0.05), see Table 3.
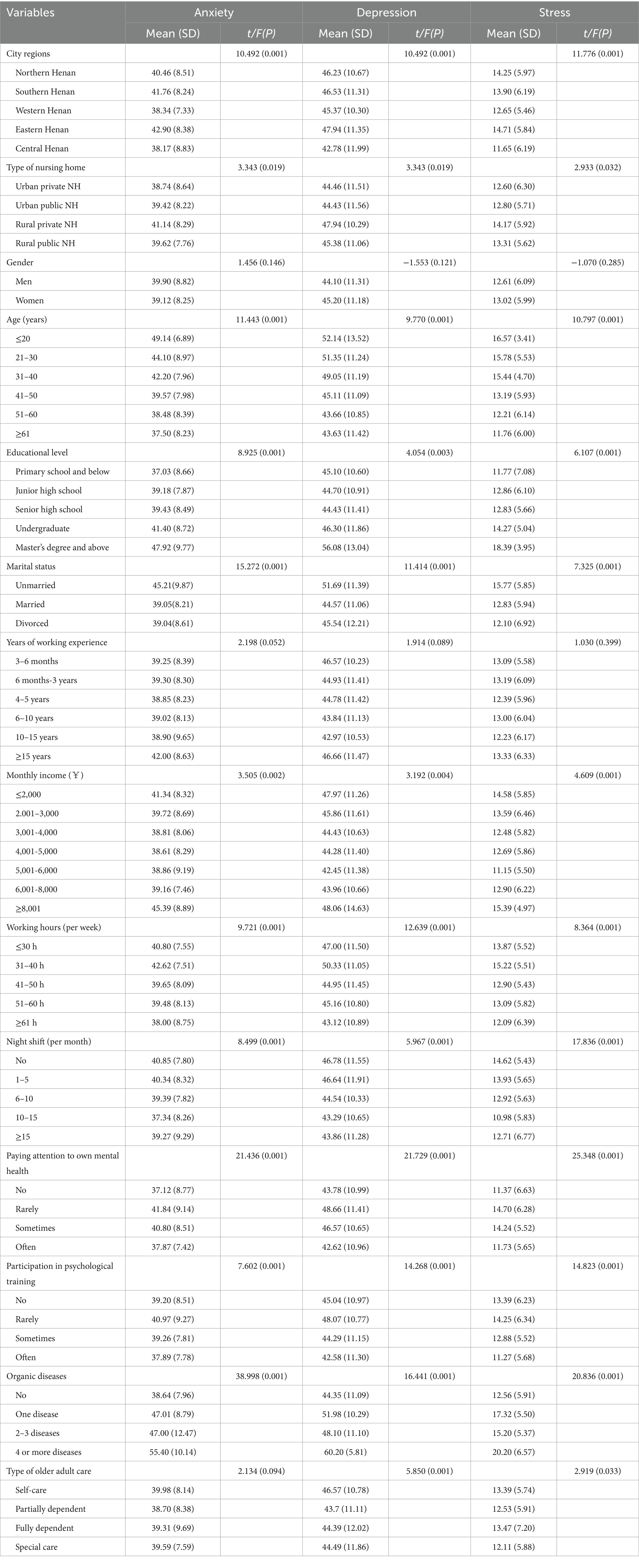
Table 3. Univariate analysis of sociodemographic characteristics associated with anxiety, depression, and stress (N = 1,341).
3.4 Multivariable factors associated with anxiety, depression, and stress
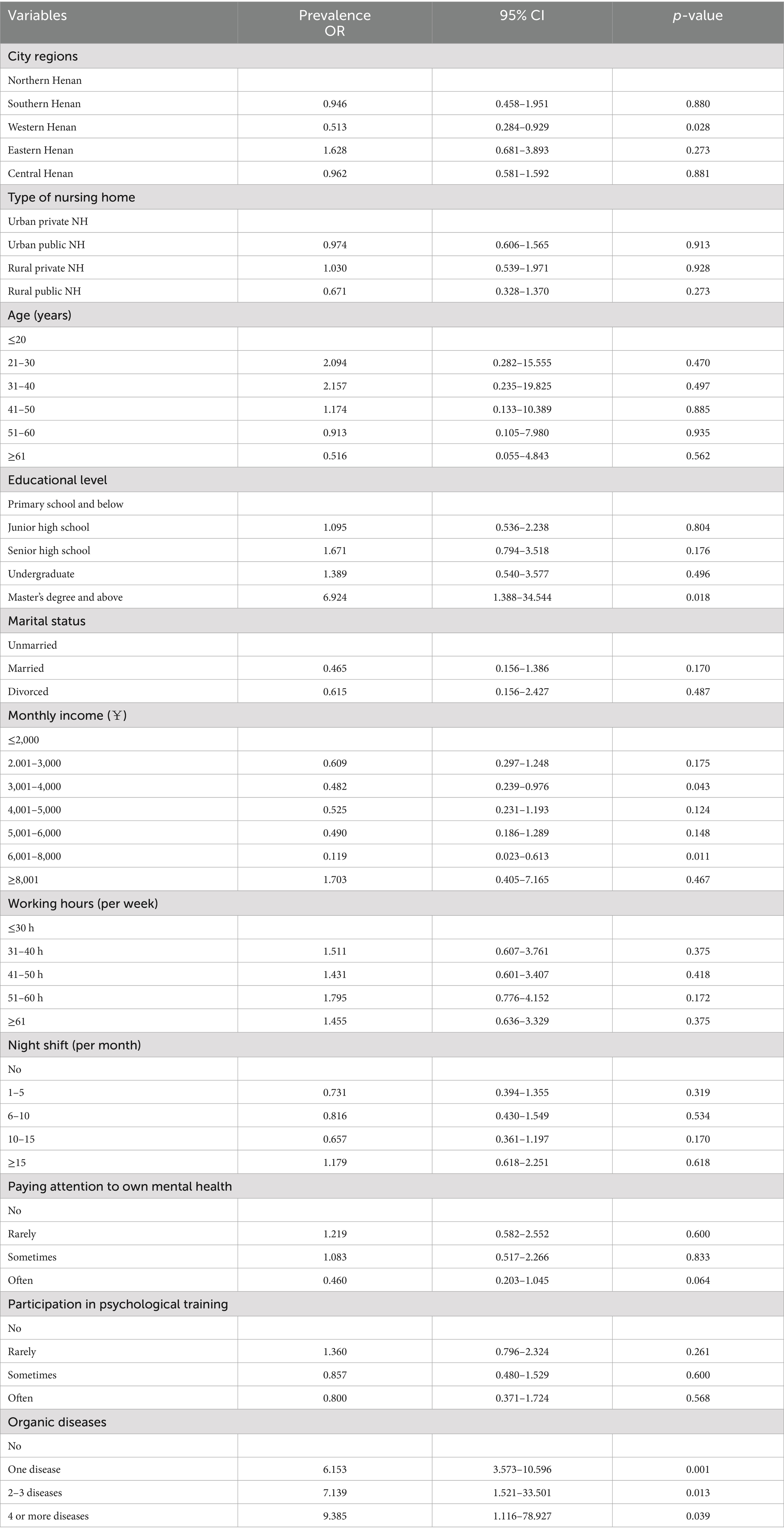
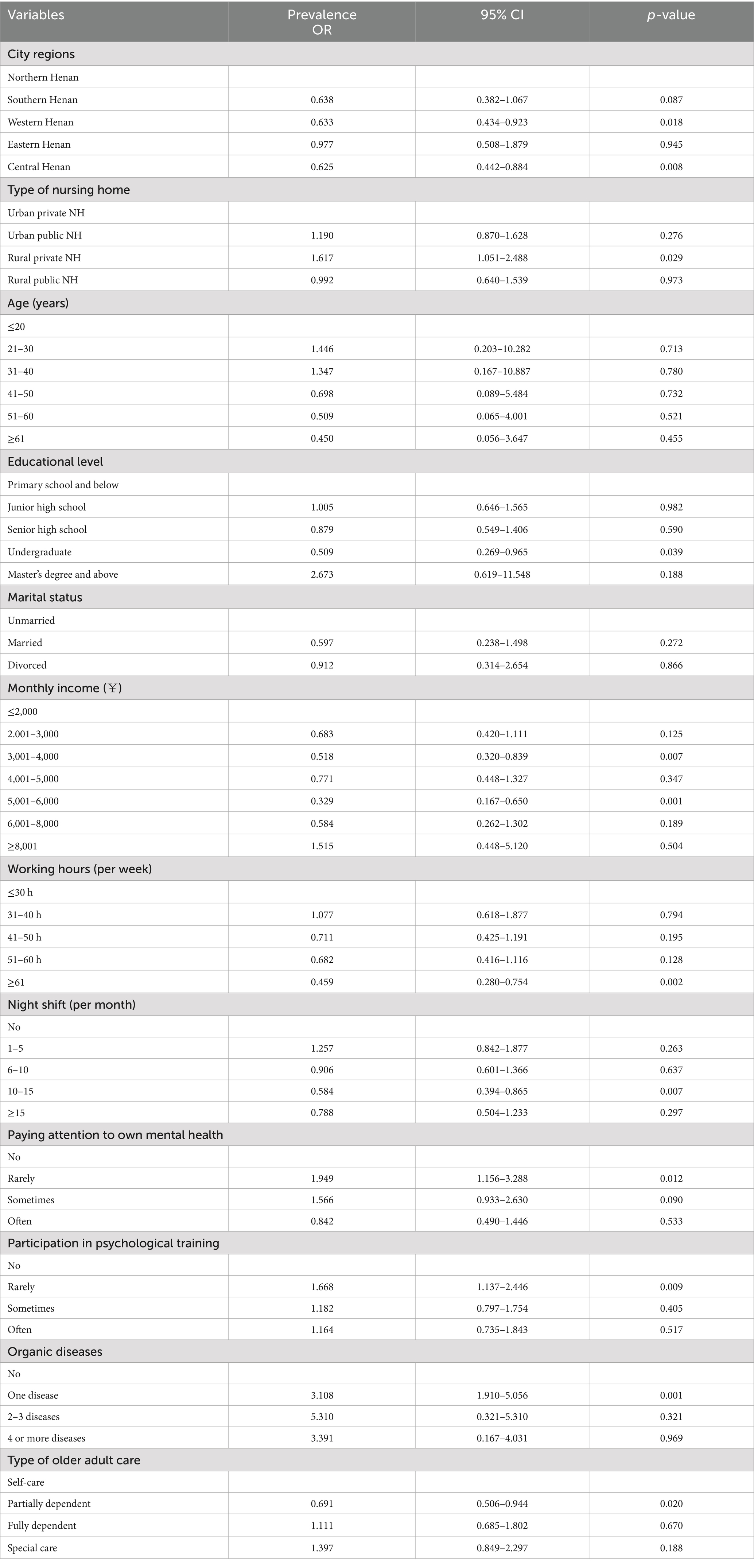
Multivariable logistic regression analyses identified several independent factors associated with anxiety, depression, and perceived stress among nursing home caregivers (Tables 4–6).
For anxiety, significant predictors included city region, educational level, monthly income, and presence of chronic diseases. Caregivers with a master’s degree or above had significantly higher odds of anxiety (OR = 6.924, 95% CI = 1.388–34.544), whereas those with moderate income levels of 3,001–4,000 RMB (OR = 0.482, 95% CI = 0.239–0.976) and 6,001–8,000 RMB (OR = 0.119, 95% CI = 0.023–0.613) showed lower odds. The presence of chronic diseases increased the likelihood of anxiety in a dose–response manner, with one disease (OR = 6.153, 95% CI = 3.573–10.596), 2–3 diseases (OR = 7.139, 95% CI = 1.521–33.501), and 4 or more diseases (OR = 9.385, 95% CI = 1.116–78.927) all associated with higher odds.
For depression, significant factors included city region, type of nursing home, educational level, working hours, night shifts, attention to mental health, participation in psychological training, and presence of chronic diseases. Higher education (undergraduate: OR = 0.509, 95% CI = 0.269–0.965) and income (3,001–4,000 RMB: OR = 0.518, 95% CI = 0.320–0.839; 5,001–6,000 RMB: OR = 0.329, 95% CI = 0.167–0.650) were protective factors, whereas employment in rural private nursing homes (OR = 1.617, 95% CI = 1.051–2.488), limited attention to mental health (rarely: OR = 1.949, 95% CI = 1.156–3.288), infrequent participation in psychological training (rarely: OR = 1.668, 95% CI = 1.137–2.446), and presence of chronic diseases (one disease: OR = 3.108, 95% CI = 1.910–5.056) were associated with increased odds of depression.
Perceived stress was independently associated with city region, type of nursing home, monthly income, working hours, night shifts, attention to mental health, participation in psychological training, and presence of chronic diseases. Higher monthly income (3,001–4,000 RMB: OR = 0.467, 95% CI = 0.287–0.759; 5,001–6,000 RMB: OR = 0.229, 95% CI = 0.117–0.448), longer working hours (≥61 h/week: OR = 0.596, 95% CI = 0.364–0.977), and more frequent night shifts (6–10/month: OR = 0.595, 95% CI = 0.395–0.895; 10–15/month: OR = 0.326, 95% CI = 0.222–0.479; ≥15/month: OR = 0.492, 95% CI = 0.320–0.755) were associated with lower levels of stress, while employment in urban public (OR = 1.380, 95% CI = 1.022–1.864) or rural private nursing homes (OR = 1.657, 95% CI = 1.075–2.553), limited attention to mental health (sometimes: OR = 1.833, 95% CI = 1.121–2.997), infrequent participation in psychological training (rarely: OR = 1.668, 95% CI = 1.137–2.446), and presence of chronic diseases (one disease: OR = 3.732, 95% CI = 2.144–6.494) were linked to an increased risk of stress.
Overall, regional disparities, income, education level, chronic disease burden, and engagement in mental health practices emerged as independent predictors across all three psychological outcomes.
4 Discussion
This multicenter study examined the prevalence of depression, anxiety, and perceived stress, as well as associated factors, among nursing home caregivers in Henan Province, China. The findings revealed that depression was the most prevalent psychological problem, followed by stress, whereas anxiety was relatively uncommon. Multiple sociodemographic, occupational, health-related, and behavioral factors showed independent associations with these outcomes. These results add new empirical evidence to the body of research on caregivers’ mental health and highlight priority areas for intervention and policy development.
In this sample, 34.8% of caregivers experienced depression, 49.8% reported varying levels of stress, and only 10.8% presented with anxiety. Depression and stress emerged as the dominant psychological concerns, while anxiety prevalence was notably lower than in studies conducted among Japanese and Spanish caregivers (18, 19). One plausible explanation lies in the age distribution of this sample, as 56.6% of participants were aged 51 years or older. According to psychosocial development theory, individuals in middle and late adulthood generally demonstrate stronger emotional regulation and psychological stability under stress (38). Consistent with prior research, age was negatively correlated with anxiety, indicating that older caregivers tend to report lower anxiety levels (39, 40).
The prevalence of depression in this study is consistent with findings from several domestic (12, 29) and international studies (18, 19, 41). For example, Chen, Cao (29) reported a prevalence of 36.3% in Shandong Province, while Santos-Orlandi, Brigola (42) found a rate of 29.6% among Brazilian caregivers. Stress prevalence was also comparable to international reports (19, 20). Collectively, these findings underscore the global significance of depression and stress as occupational health challenges in long-term care facilities.
Marked regional disparities were identified, with caregivers in the southern, western, and central regions reporting better mental health than those in the northern and eastern regions. This finding aligns with evidence that inequalities in socioeconomic conditions and healthcare resources influence mental health outcomes (43, 44). Education showed complex effects. Postgraduate education was linked to higher anxiety, which may reflect role mismatch and career frustration, whereas a bachelor’s degree appeared protective against depression, consistent with research connecting health literacy to psychological resilience (45, 46). Income demonstrated a U-shaped relationship, where moderate income was most protective, while both low- and high-income groups experienced greater psychological distress. This trend is consistent with broader socioeconomic health research (47, 48). Although not significant in multivariate models, bivariate analyses suggested that unmarried caregivers were more vulnerable, underscoring the protective influence of social support (25, 49).
Institutional characteristics also significantly influenced mental health. Caregivers in rural private nursing homes reported higher levels of depression and stress, aligning with prior findings that underfunded institutions impose heavier burdens on staff (44). Interestingly, longer working hours and more frequent night shifts were associated with lower levels of depression and stress, contrary to most previous studies (23, 29). This paradoxical pattern may reflect the “healthy worker effect,” income-related stress buffering, or cultural adaptation to shift work (50). Longitudinal studies are needed to verify these explanations.
Physical illness emerged as a strong predictor of psychological distress, with risk increasing alongside the number of chronic conditions. This finding is consistent with prior research showing that physical morbidity contributes to depression, anxiety, and stress through both biological and psychosocial pathways (23, 51). Caregivers with chronic diseases face compounded burdens, suggesting the need for integrated physical and psychological support.
Several modifiable factors were found to be protective. Caregivers who regularly attended to their mental health and participated in psychological training reported lower risks of depression and stress. This finding aligns with evidence supporting the effectiveness of psychoeducation, mindfulness, and stress management interventions (52–54). However, only one-quarter of caregivers in this study reported regular participation in psychological training, highlighting substantial gaps in institutional support.
4.1 Theoretical framing and inferential model
From a theoretical perspective, the current findings can be interpreted through an inferential model based on the ABC Theory of Emotion (55) and the stress and coping theory (56). Anchored in these frameworks, our results can be organized into a concise inferential pathway. Contextual and individual exposures, such as region, facility type, education, income, and chronic disease, constitute the “activating events” (A) that shape caregivers’ cognitive appraisal (B), which is operationalized here as perceived stress. These appraisals then give rise to “emotional consequences” (C), observed as depression and anxiety. This structure helps explain why predictors that elevate moderate-to-high perceived stress, such as lower income, rural private facilities, and chronic disease, also increase risks of depression and anxiety, whereas resource variables including attention to mental health and psychological training are broadly protective. In other words, training and proactive mental health attention likely enhance adaptive appraisal and coping, thereby attenuating the A → B → C cascade. While causal inference is limited by the cross-sectional design, this theory-grounded model provides a foundation for future longitudinal and structural equation modeling studies to quantify indirect effects (exposure → perceived stress → symptoms) and to examine whether workplace training strengthens resilience pathways within the aging care workforce.
4.2 Implications
These findings have important implications. Clinically, routine screening for depression and stress should be prioritized, particularly among caregivers with chronic illnesses and those working in resource-limited institutions. At the policy level, efforts are needed to improve working conditions, ensure fair compensation, and expand access to psychological training. From a research perspective, longitudinal and interventional studies are essential to clarify causal pathways and evaluate the effectiveness of workplace-based interventions.
4.3 Strengths and limitations
This study benefits from a large, multi-center sample and the use of validated scales, providing robust evidence on an under-researched population. Nonetheless, several limitations must be acknowledged. The cross-sectional design precludes causal inference, self-reported measures may introduce bias, and findings from Henan Province may not generalize to other regions or countries. Future research should adopt longitudinal and mixed-method approaches across diverse settings.
5 Conclusion
Depression and stress are significant psychological concerns among nursing home caregivers in China, influenced by regional, educational, economic, institutional, health-related, and behavioral factors. Addressing these challenges requires coordinated clinical, organizational, and policy-level interventions to promote caregivers’ mental well-being and ensure the sustainability of older adult care services in an aging society.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Sanquan College of Xinxiang Medical College. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
Z-RF: Methodology, Data curation, Writing – original draft, Formal analysis. MC: Methodology, Supervision, Funding acquisition, Writing – review & editing. ZX: Writing – original draft, Formal analysis, Investigation, Data curation. MJ: Investigation, Data curation, Methodology, Writing – original draft. YY: Investigation, Data curation, Writing – review & editing, Formal analysis. LM: Writing – original draft, Software, Methodology. CC: Writing – review & editing, Validation, Supervision.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We sincerely thank all nursing home caregivers who participated in this study for their valuable time and contributions. We also appreciate the support from the participating institutions that facilitated data collection across multiple sites in Henan Province, China.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1690840/full#supplementary-material
References
1. Luan, JY, Tian, YH, Jim, CY, Liu, X, Yan, MX, and Wu, LZ. Assessing spatial accessibility of community hospitals for the elderly in Beijing, China. Int J Environ Res Public Health. (2023) 20:890. doi: 10.3390/ijerph20010890
2. Chen, X, Giles, J, Yao, Y, Yip, W, Meng, Q, Berkman, L, et al. The path to healthy ageing in China: a Peking University–lancet commission. Lancet. (2022) 400:1967–2006. doi: 10.1016/S0140-6736(22)01546-X
3. China MoCAotPsRo. (2024) Annual report on China’s aging affairs 2025. Available online at: https://www.gov.cn/lianbo/bumen/202507/content_7033724.htm (Accessed May 10, 2025).
4. Choi, M. Factors associated with eHealth use among community dwelling older adults. Int J Nurs Pract. (2022) 28:e13092. doi: 10.1111/ijn.13092
5. Martinez L, R, Pardo-Garcia, I, and Escribano-Sotos, F. Aging, dependence, and long-term care: a systematic review of employment creation. J Health Care Organ Provision Financ. (2021) 58:00469580211062426.
6. Omolara, J, and Ochieng, J. Occupational health and safety challenges faced by caregivers and the respective interventions to improve their wellbeing. Int J Innov Sci Res Technol. (2024) 9:3225–51. doi: 10.38124/ijisrt/IJISRT24JUN1000
7. Zhang, H, and Sun, H. Knowledge, attitude and self-efficacy of elderly caregivers in Chinese nursing homes: a cross-sectional study in Liaoning Province. BMJ Open. (2019) 9:e029869. doi: 10.1136/bmjopen-2019-029869
8. World Health Organization The state of the health workforce in the WHO African region, 2021. Geneva: World Health Organization, (2021)
9. Han, Y, He, Y, Lyu, J, Yu, C, Bian, M, and Lee, L. Aging in China: perspectives on public health. Elsevier; (2020). p. 11–17.
10. Feng, Z, Glinskaya, E, Chen, H, Gong, S, Qiu, Y, Xu, J, et al. Long-term care system for older adults in China: policy landscape, challenges, and future prospects. Lancet. (2020) 396:1362–72. doi: 10.1016/S0140-6736(20)32136-X
11. Subject Group of the Social Welfare Center MoCAoC. Research on the current situation, problems, and countermeasures of employees in Chinese nursing institutions: data analysis based on the national nursing institution data reporting system of 239,312 employees. Chinese Civil Affairs. (2015) 14:29–31.
12. Yang, JH, Lu, Y, Liu, S, Dai, M, and Zhang, H. Prevalence and related factors of depression and anxiety in a cohort of Chinese elderly caregivers in the nursing home. J Affect Disord. (2021) 295:1456–61. doi: 10.1016/j.jad.2021.09.026
13. Reynolds, CF, Jeste, DV, Sachdev, PS, and Blazer, DG. Mental health care for older adults: recent advances and new directions in clinical practice and research. World Psychiatry. (2022) 21:336–63. doi: 10.1002/wps.20996
14. Gray, KL, Birtles, H, Reichelt, K, and James, IA. The experiences of care home staff during the COVID-19 pandemic: a systematic review. Aging Ment Health. (2022) 26:2080–9. doi: 10.1080/13607863.2021.2013433
15. Maharaj, S, Lees, T, and Lal, S. Prevalence and risk factors of depression, anxiety, and stress in a cohort of Australian nurses. Int J Environ Res Public Health. (2019) 16:61.
16. Hering, C, Gangnus, A, Budnick, A, Kohl, R, Steinhagen-Thiessen, E, Kuhlmey, A, et al. Psychosocial burden and associated factors among nurses in care homes during the COVID-19 pandemic: findings from a retrospective survey in Germany. BMC Nurs. (2022) 21:41. doi: 10.1186/s12912-022-00807-3
17. Franza, F, Basta, R, Solomita, B, Conte, G, Vacca, A, Chung, S, et al. Anxiety and burnout in Alzheimer’s caregivers in COVID-19 pandemic. J Neurol Sci. (2021) 429:119961. doi: 10.1016/j.jns.2021.119961
18. Takahashi, E, Ekoyama,, Tachikawa, HM, Shiratori, Y, Ota, M, and Takahashi, S. Mental health of caregivers working in nursing homes during the COVID-19 pandemic. Dementia Geriatr Cogn Disord. (2022) 51:233–40. doi: 10.1159/000524953
19. Martín, PA, Villanueva, A, and Quintana, JM. Evaluation of the mental health of care home staff in the Covid-19 era. What price did care home workers pay for standing by their patients? Int J Geriatr Psychiatry. (2021) 36:1810–9. doi: 10.1002/gps.5602
20. Wollesen, B, Hagemann, D, Pabst, K, Schlüter, R, Bischoff, LL, Otto, AK, et al. Identifying individual stressors in geriatric nursing staff-a cross-sectional study. Int J Environ Res Public Health. (2019) 16:3587. doi: 10.3390/ijerph16193587
21. Sołtys, A, and Wnuk, M. Psychological mechanisms of caregiver involvement in caregiving for individuals with Alzheimer’s disease: analysis of the moderated mediation model. J Clin Med. (2025) 14:5134. doi: 10.3390/jcm14145134
22. Loo, YX, Yan, S, and Low, LL. Caregiver burden and its prevalence, measurement scales, predictive factors and impact: a review with an Asian perspective. Singapore Med J. (2022) 63:593–603. doi: 10.11622/smedj.2021033
23. Torquati, L, Mielke, GI, Brown, WJ, Burton, NW, and Kolbe-Alexander, TL. Shift work and poor mental health: a Meta-analysis of longitudinal studies. Am J Public Health. (2019) 109:e13–20. doi: 10.2105/AJPH.2019.305278
24. Adarkwah, CC, Labenz, J, and Hirsch, O. Burnout and work satisfaction are differentially associated in gastroenterologists in Germany. F1000Res. (2022) 11:368. doi: 10.12688/f1000research.110296.3
25. Pieh, C, T, OR, Budimir, S, and Probst, T. Relationship quality and mental health during COVID-19 lockdown. PLoS One. (2020) 15:e0238906. doi: 10.1371/journal.pone.0238906
26. Adams, GC, Wrath, AJ, Le, T, and Alaverdashvili, M. A longitudinal exploration of the impact of social anxiety and individual attachment on depression severity. J Affect Disord. (2019) 257:250–6. doi: 10.1016/j.jad.2019.07.051
27. Li, Q, Zhang, H, Zhang, M, Li, T, Ma, W, An, C, et al. Prevalence and risk factors of anxiety, depression, and sleep problems among caregivers of people living with neurocognitive disorders during the COVID-19 pandemic. Front Psych. (2021) 11:590343. doi: 10.3389/fpsyt.2020.590343
28. Zhang, XR, Huang, QM, Wang, XM, Cheng, X, Li, ZH, Wang, ZH, et al. Prevalence of anxiety and depression symptoms, and association with epidemic-related factors during the epidemic period of COVID-19 among 123,768 workers in China: a large cross-sectional study. J Affect Disord. (2020) 277:495–502. doi: 10.1016/j.jad.2020.08.041
29. Chen, CY, Lu, Y, Zheng, X, Kong, B, Dong, H, et al. Factors associated with mental health outcomes among caregivers of older adults in long-term care facilities during COVID-19 post-epidemic era in Shandong, China. Front Psych. (2022) 13:1011775. doi: 10.3389/fpsyt.2022.1011775
30. Chow, S-C, Shao, J, Wang, H, and Lokhnygina, Y. Sample size calculations in clinical research. Boca Raton: Chapman and Hall/CRC (2017).
31. Zhang, S, Cao, J, and Ahn, C. A GEE approach to determine sample size for pre-and post-intervention experiments with dropout. Comput Stat Data Anal. (2014) 69:114–21. doi: 10.1016/j.csda.2013.07.037
32. Zung,. A rating instrument for anxiety disorders. Psychosomatics. (1971) 12:371–9. doi: 10.1016/S0033-3182(71)71479-0
34. Wang, z, and Chi, y. The self-rating depression scale (SDS). Shanghai Psychiatry. (1984) 2:71–2.
35. Zung, GJA. Personality dimension and self-rating depression scale. J Clin Psychol. (1971) 27:247-+. doi: 10.1002/1097-4679(197104)27:2<247::AID-JCLP2270270230>3.0.CO;2-6
36. Cohen, KT, and Mermelstein, R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96.
37. Ng, S-m. Validation of the 10-item Chinese perceived stress scale in elderly service workers: one-factor versus two-factor structure. BMC Psychol. (2013) 1:1–8. doi: 10.1186/2050-7283-1-9
38. Sheldon, KM, and Kasser, T. Getting older, getting better? Personal strivings and psychological maturity across the life span. Dev Psychol. (2001) 37:491–501. doi: 10.1037/0012-1649.37.4.491
39. Villaume, SC, Chen, S, and Adam, EK. Age disparities in prevalence of anxiety and depression among US adults during the COVID-19 pandemic. JAMA Netw Open. (2023) 6:e2345073. doi: 10.1001/jamanetworkopen.2023.45073
40. Brenes, GA. Age differences in the presentation of anxiety. Aging Ment Health. (2006) 10:298–302. doi: 10.1080/13607860500409898
41. Husky, VR, Teguo, MT, Alonso, J, Bruffaerts, R, Swendsen, J, et al. Nursing home workers’ mental health during the COVID-19 pandemic in France. J Am Med Dir Assoc. (2022) 23:1095–100. doi: 10.1016/j.jamda.2022.04.001
42. Santos-Orlandi, AA, Brigola, AG, Ottaviani, AC, Luchesi, BM, Souza, ÉN, Moura, FG, et al. Elderly caregivers of the elderly: frailty, loneliness and depressive symptoms. Rev Bras Enferm. (2019) 72:88–96. doi: 10.1590/0034-7167-2018-0137
43. Chao, F. The evaluation of rural territorial functions: a case study of Henan, China. J Resour Ecol. (2017) 8:242–50.
44. Du, P, Dong, T, and Ji, J. Current status of the long-term care security system for older adults in China. Res Aging. (2021) 43:136–46. doi: 10.1177/0164027520949117
45. Liu, L, Fu, M, Wu, J, Wang, H, Zhao, J, Chen, P, et al. Digital health literacy among undergraduate nursing students in China: associations with health lifestyles and psychological resilience. BMC Med Educ. (2024) 24:1139. doi: 10.1186/s12909-024-06075-w
46. Tsaras, K, Papathanasiou, IV, Vus, V, Panagiotopoulou, A, Katsou, MA, Kelesi, M, et al. Predicting factors of depression and anxiety in mental health nurses: a quantitative cross-sectional study. Med Arch. (2018) 72:62–7. doi: 10.5455/medarh.2017.72.62-67
47. Steptoe, A, Deaton, A, and Stone, AA. Subjective wellbeing, health, and ageing. Lancet. (2015) 385:640–8. doi: 10.1016/S0140-6736(13)61489-0
48. Li, C, Ning, G, Wang, L, and Chen, F. More income, less depression? Revisiting the nonlinear and heterogeneous relationship between income and mental health. Front Psychol. (2022) 13:1016286. doi: 10.3389/fpsyg.2022.1016286
49. Uecker, JE. Marriage and mental health among young adults. J Health Soc Behav. (2012) 53:67–83. doi: 10.1177/0022146511419206
50. Sousa-Ribeiro, M, Lindfors, P, and Knudsen, K. Sustainable working life in intensive care: a qualitative study of older nurses. Int J Environ Res Public Health. (2022) 19:6130. doi: 10.3390/ijerph19106130
51. Eatough, EM, Way, JD, and Chang, C-H. Understanding the link between psychosocial work stressors and work-related musculoskeletal complaints. Appl Ergon. (2012) 43:554–63. doi: 10.1016/j.apergo.2011.08.009
52. Han, A. Effects of mindfulness-based interventions on depressive symptoms, anxiety, stress, and quality of life in family caregivers of persons living with dementia: a systematic review and meta-analysis. Res Aging. (2022) 44:494–509. doi: 10.1177/01640275211043486
53. Günaydin, N. Effects of group psychoeducation on depression, anxiety, stress and coping with stress of nursing students. A randomized controlled study. Perspect Psychiatr Care. (2021) 58:640–50. doi: 10.1111/ppc.12828
54. Dolan, N, Simmonds-Buckley, M, Kellett, S, Siddell, E, and Delgadillo, J. Effectiveness of stress control large group psychoeducation for anxiety and depression: systematic review and meta-analysis. Br J Clin Psychol. (2021) 60:375–99. doi: 10.1111/bjc.12288
55. Ellis, A. The revised ABC’S of rational-emotive therapy (RET). J Ration Emot Cogn Behav Ther. (1991) 9:139–72. doi: 10.1007/BF01061227
Keywords: nursing home caregivers, depression, anxiety, perceived stress, long-term care
Citation: Fan Z-R, Chong MC, Xiaona Z, Jing M, You YL, Ma L and Che CC (2025) Prevalence and factors associated with depression, anxiety and stress among nursing home caregivers in China: a multi-center cross-sectional study. Front. Public Health. 13:1690840. doi: 10.3389/fpubh.2025.1690840
Edited by:
Shane Andrew Thomas, Federation University Australia, AustraliaReviewed by:
Lucio Inguscio, Sapienza University of Rome, ItalyRajesh Kumar, All India Institute of Medical Sciences, Rishikesh, India
Copyright © 2025 Fan, Chong, Xiaona, Jing, You, Ma and Che. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chong Chin Che, Y2hlY2hvbmdjaGluQHVtLmVkdS5teQ==
 Zhi-Ru Fan
Zhi-Ru Fan Mei Chan Chong
Mei Chan Chong Zheng Xiaona
Zheng Xiaona Ma Jing5
Ma Jing5 Lili Ma
Lili Ma Chong Chin Che
Chong Chin Che