- 1School of Traditional Chinese Medicine, Beijing University of Chinese Medicine, Beijing, China
- 2School of Nursing, Beijing University of Chinese Medicine, Beijing, China
- 3Nursing Department, China-Japan Friendship Hospital, Beijing, China
Background: Dietary behaviour among kidney transplant recipients (KTRs) is a critical factor influencing long-term postoperative outcomes. However, research focusing on the dietary behaviour of KTRs remains limited. The aim of this study was to examine the dietary behaviour and explore the influencing factors of dietary behaviour in KTRs based on a health promotion model.
Methods: This was a cross-sectional study. A total of 289 KTRs from four hospitals were recruited from October 2022 to March 2023 by convenience sampling method. Participants completed a survey consisting of a general information questionnaire, the Dietary Self-management Ability Scale, the Perceived Dietary Behaviour Benefit and Barrier Questionnaire, the Self-Rating Depression Scale, and the Adapted Health Eating Cognitive Beliefs Questionnaire. The survey was administered both online and on-site. Data were analysed with Spearman’s correlation analysis and path analysis.
Results: Dietary behaviour was at moderate level, with an index score of 78%. Depression (β = −0.207, p < 0.001), perceived behaviour benefits (β = 0.220, p < 0.001), perceived behaviour barriers (β = −0.234, p < 0.001), attitude (β = 0.135, p = 0.026), and social support (β = 0.166, p = 0.001) directly predicted dietary behaviour, while depression, attitude, and social support exhibited indirect effect on dietary behaviour.
Conclusion: Medical staff could help KTRs change their poor dietary attitude and negative mode, guide them to receive more social support and perceived benefits, reduce their perceived barriers. These positive shifts could ultimately facilitate the emergence of healthy dietary behaviour and enhancement of quality of life.
1 Introduction
Kidney transplantation, the earliest solid organ transplantation to be clinically developed, is characterised by the largest number of transplantation cases and a highly advanced technology (1). According to the World Health Organization (2), the global count of kidney transplants in 2021 reached a total of 92,532.
Dietary behaviour among kidney transplant recipients (KTRs) is a critical factor that significantly influences their health outcomes. The Kidney Disease Outcome Quality Initiative (KDOQI) Clinical Practice Guideline for Nutrition in Chronic Kidney Disease recommends that KTRs maintain a protein intake of 1.0–1.2 g/kg body weight per day and an energy intake of 25–35 kcal/kg body weight per day, while also considering multivitamin and vitamin D supplementation, and managing electrolyte levels based on individual needs (3). Additionally, increasing fruits and vegetables and following a Mediterranean diet are suggested to improve overall health outcomes (3). A healthy dietary behaviour among KTRs has been proven to lower the risk of metabolic and cardiovascular diseases (4), contribute to the restoration of renal function, and reduce overall mortality (5).
KDOQI of the National Kidney Foundation has released evidence-based recommendations suggesting that disease diagnosis, level of physical activity, age, gender, weight status, nutritional knowledge, beliefs, and depression should be taken into account when assessing a recipient’s dietary intake and energy requirements (3). Additionally, previous international clinical studies have verified the influence of coping resources, such as social support, on the dietary habits of patients with chronic illness (6). However, there is a scarcity of theoretically-based research exploring the interplay between these variables and their effects on the dietary behaviour of KTRs.
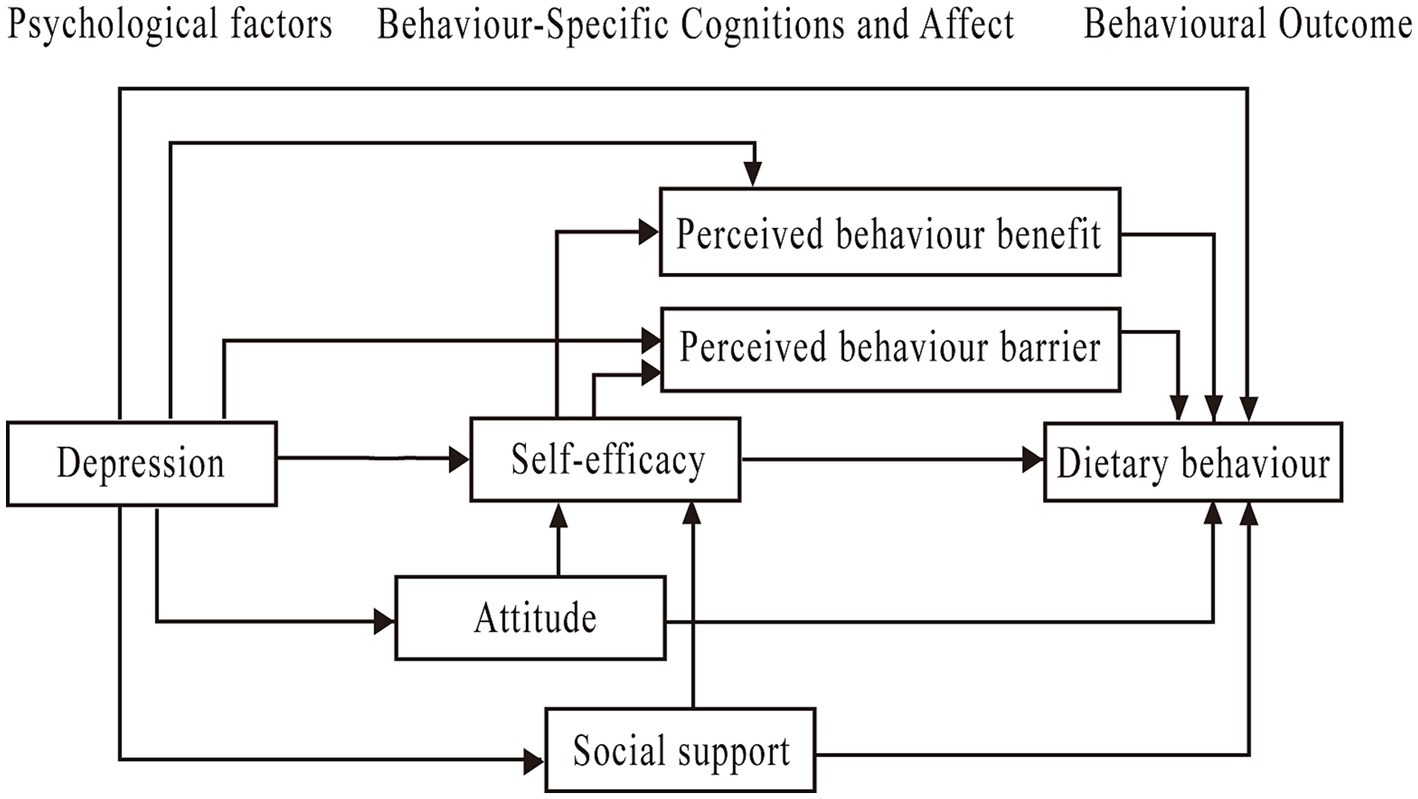
Health Promotion Model (HPM), initially formulated in 1987 by American nurse practitioner Pender and her colleagues, is thought to be a paradigm for explaining health-promoting behaviour (7). The HPM classifies the factors influencing health-promoting behaviour into three primary categories. (i) Individual characteristics and experiences. Personal traits (physical, psychological, and sociocultural) and previously related behaviour are included. (ii) Behaviour-specific cognitions and affect, such as perceived benefit and barrier, perceived self-efficacy, activity-related affect, interpersonal influences from families and caregivers and situational influences. (iii) Behavioural outcome, such as healthy dietary behaviour. Grounded in HPM model, there are interactions between different behaviour-specific perceptions and emotion, for example, activity-related affect (dietary attitude) influencing perceived self-efficacy, perceived self-efficacy influencing perceived barriers, and self-efficacy being considered as a significant predictor of changes in health behaviour (8).
Over 50% of studies have found significant associations between health behaviour and factors such as perceived benefit and barrier, self-efficacy, and social support (9). Previous studies have demonstrated the significance of cultivating health beliefs and fostering attitudinal shifts to facilitate behavioural modifications (10), and individuals with positive attitudes exhibiting a greater propensity to adhere to health behaviour (11). And dietary attitude of female college students were negatively associated with their levels of depression (12).
In addition, researchers have pointed out that there is a significant correlation between perceived self-efficacy and perceived benefit (13). Additionally, empirical evidence has demonstrated a positive correlation between social support and self-efficacy among patients with chronic diseases (14). Enhancing patients’ self-efficacy by means of providing social support has been found to have a positive impact on modifying health behaviours (15). Therefore, the purpose of our study was to employ the HPM for investigating the influencing factors of dietary behaviour in KTRs. The hypothetical theoretical model was formulated based on existing literature and theories (see Figure 1). Perceived benefit, perceived barrier, self-efficacy, depression, and attitude were considered to have a direct influence on dietary behaviour of KTRs. Depression could indirectly impact the dietary behaviour through perceived benefit, perceived barrier, self-efficacy, attitude, and social support. Self-efficacy was considered a common mediating variable between dietary attitude and perceived behaviour benefit, social support and perceived behaviour benefit, dietary attitude and perceived behaviour barrier, and social support and perceived behaviour barrier.
2 Materials and methods
2.1 Study design and participants
This was a cross-sectional study involving KTRs from four tertiary hospitals located in four provinces of mainland China. Participants were recruited between October 2022 and March 2023. Convenience sampling was used. Study design followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement (see Supplementary material).
Sample size calculation was determined based on five to ten times of the number of free parameters in the SEM (16). In this study, the number of free parameters in the initial model was 32. Considering a potential sample loss of 20%, a final sample size of 200–400 was necessary. Ultimately, a total of 343 questionnaires were distributed and 289 valid questionnaires were returned, with an effective recovery rate of 84.26%.
The inclusion criteria were as follows: (1) aged ≥18 years; (2) with a functional transplanted kidney; (3) with necessary reading and writing ability; and (4) voluntary participation. The exclusion criteria were as follows: (1) second or multiple kidney transplantation; (2) multiple organ transplant recipients; (3) with other severe diseases; and (4) pregnant women. KTRs who met the inclusion and exclusion criteria were invited to participate in the questionnaire survey.
2.2 Procedure
The study was approved by the Ethics Committee in Beijing University of Chinese Medicine (2023BZYLL0107). This study was conducted across multiple hospitals, and questionnaires were distributed and collected either on-site or online, depending on the circumstances at each hospital. KTRs were recruited from hospital transplant follow-up clinics. All participants received either verbal or written information about the study. Professionally trained researchers provided a detailed explanation of the study’s purpose and procedures, ensuring participants understood that withdrawing would not impact their future care. Following the completion of the informed consent forms, participants proceeded to fill out the questionnaires. All questionnaires used in this study were in Chinese. Additionally, all personal data concerning the individuals were anonymized.
2.3 Measures
A self-designed general information questionnaire, including demographic characteristics and disease-related information, was used to assess KTR’s general condition. Demographic characteristics included age, sex, BMI, ethnicity, habitual residence, employment status, education level, marital status, insurance status, and economic burden. Disease-related information included the time after transplantation, donor type, rejection, infection, and number of hospitalizations.
Dietary Self-Management Ability Scale was used to assess KTR’s dietary attitude and behaviours. The dietary attitude dimension contains 9 items with a score range of 9–45, investigating recipients’ willingness and levels of support for reasonable diet. For example, “I believe that reasonable diet after transplantation has a significant impact on physical and functional recovery.” The dietary behaviour dimension contains 10 items with a score range of 10–50, investigating dietary choice, intake and control, and physical activity. For example, “I adjust my daily water intake based on urine volume and body weight.” Each item was measured with a 5-point Likert scale from 1 (totally disagree) to 5 (totally agree). The scores for each dimension were calculated as the sum of the item scores within that dimension. Higher scores indicated better dietary attitude and behaviours. The scale has been validated in KTRs and has shown good psychometric properties (17). In this study, Cronbach’s α coefficient for the entire scale was 0.888.
Perceived Dietary Behaviour Benefit and Barrier Questionnaire was used to assess KTR’s perceived dietary behaviour benefits and barriers. The questionnaire was self-designed by the research team according to the research purpose, combined with a literature review and expert consultation. Each of the two dimensions contains 6 items. Each item was rated on a 5-point Likert scale from 1 (totally disagree) to 5 (totally agree). Higher scores indicated more perceived dietary behaviour benefits or greater perceived dietary behaviour barriers. For example, “it can help me maintain ideal body weight,” or “it is hard to follow the post-transplant diet when eating out frequently.” Seven experts were invited to assess item-level content validity (ICVI) and scale-level content validity (SCVI). Being equal or greater than 0.79 was considered relevant (18). In this study, expert SCVI was 0.929, and ICVI ranged from 0.857 to 1.000. Cronbach’s α coefficients of Perceived Dietary Behaviour Benefit and Barrier Questionnaire were 0.927 and 0.738, respectively.
Self-rating Depression Scale was used to measure KTR’s depression (19). It comprised 20 items and each item was rated on a 4-point Likert scale ranging from 1 (no) to 4 (always). Depression scores range from 20 to 80, with higher scores indicating more severe depression symptoms. The depression symptoms were evaluated based on standard scores. The total score was calculated by summing the scores of each item, and the result was then multiplied by 1.25. The standard score was obtained by rounding up to the nearest whole number. According to the Chinese norm results, the final standard scores were categorised as follows: normal (<50), mild (50–59), moderate (60–69), and severe (>70) (19). This scale has been validated in KTRs and has shown good psychometric properties (20). In this study, the Cronbach’s α coefficient of this scale was 0.860.
Adapted Health-Eating Cognitive Beliefs Questionnaire was used to assess KTR’s self-efficacy and social support. This questionnaire was adapted by the researchers based on Health Eating Cognitive Beliefs Questionnaire (21), according to literature reviews and expert consultations. The content evaluation of the questionnaire was assessed by experts. Modifications included changing the original scale from “healthy eating” to “healthy eating after transplantation,” and changing the 4-point Likert scale for the social support dimension to a 5-point Likert scale (1 = completely non-conforming, 5 = completely conforming). Self-efficacy scores range from 7 to 35, and social support scores range from 5 to 25, with higher scores indicating higher corresponding indicators. SCVI and ICVI values obtained from expert evaluations in this study were all 1.000, indicating good content validity. The Cronbach’s α coefficients of self-efficacy and social support were 0.811 and 0.812, respectively.
Scoring indicators of dietary behaviour and related factors in HPM were calculated using the following formula: the median score of each variable or dimension divided by the maximum possible score for that variable or dimension, multiplied by 100%. Based on these calculations, different variables were categorised into three levels: high (>80%), medium (60–80%), and low (<60%) (22).
2.4 Statistical analyses
Data were conducted employing SPSS 26.0 (IBM Corp.) and Mplus 8.3 (23). Two-sided tests were used with a significance level of p < 0.05. Descriptive data were presented as frequencies, percentages, means, standard deviations, medians and quartiles. Non-parametric test was adopted to ascertain demographic information and disease-related data pertaining to dietary behaviour. All statistically significant indicators were adjusted for multiple comparisons using the Bonferroni post-hoc test. The significance level after applying the Bonferroni correction for multiple comparisons was set to α′ = 0.05/n, where n represents the number of tests conducted. Spearman’s correlation was adopted to explore the association between dietary behaviour and various associated variables in HPM. The variance inflation factor (VIF) was employed to evaluate multicollinearity among the associated variables. VIF values of <5 indicate the absence of significant multicollinearity. VIF values between 5 and 10 suggest moderate multicollinearity, warranting cautious interpretation of the coefficients or consideration of merging/removing variables. VIF values of ≥10 indicate severe multicollinearity, necessitating remedial action.
To validate the hypothesized conceptual model, path analysis was used. Those variables that were significantly correlated with dietary behaviour entered into the path analysis to explore the influencing factors of dietary behaviour in KTRs. The collected data were incorporated into the path analysis for parameters estimation. The rationality of the parameters, the significance of the path, the goodness of fit, and other indices were integrated to assess the appropriateness of the sample data for the hypothetical model and the robustness of the model’s explanation power. If the hypothetical model exhibited a poor fit, it was necessary to correct the model. Through continuous evaluation, the most reasonable model with the best model fit and the strongest explanatory power was obtained. The fit of the sample data to the hypothetical theoretical model was assessed by various model indexes, including Chi-square degrees of freedom (χ2/df), Comparative Fit Index (CFI), Tacker-Lewis Index (TLI), Root Mean Square Error of Approximation (RMSEA) and Standardized Root Mean Square Residual (SRMR). Generally, χ2/df < 3, CFI and TLI > 0.90, RMSEA < 0.05, and SRMR < 0.08 indicate a good fit for the model, while RMSEA<0.08 are considered an acceptable fit (16, 24).
3 Results
3.1 Participant profile
Among the 289 KTRs, 58.82% were male. The mean age of the recipients was 44.37 ± 10.37 years. The mean Body Mass Index (BMI) was 22.20 ± 3.13 kg/m2, with the majority of recipients falling within the normal weight range. The majority of the recipients identified as Han ethnicity (93.43%). Most of the recipients resided in cities and towns (75.78%). A total of 51.56% of KTRs had attained college education or higher. The majority of recipients were married (79.24%), employed (52.94%), and relied on medicaid insurance payments (97.92%). Approximately 83.04% of KTRs experienced an economic burden. The time after transplantation ranged from 3 to 300 months. The percentage of deceased donors was 90.31%. In total, 20.42% of recipients had experienced rejection, and 28.03% experienced infection. Among the recipients, 67.13% were readmitted to the hospital.
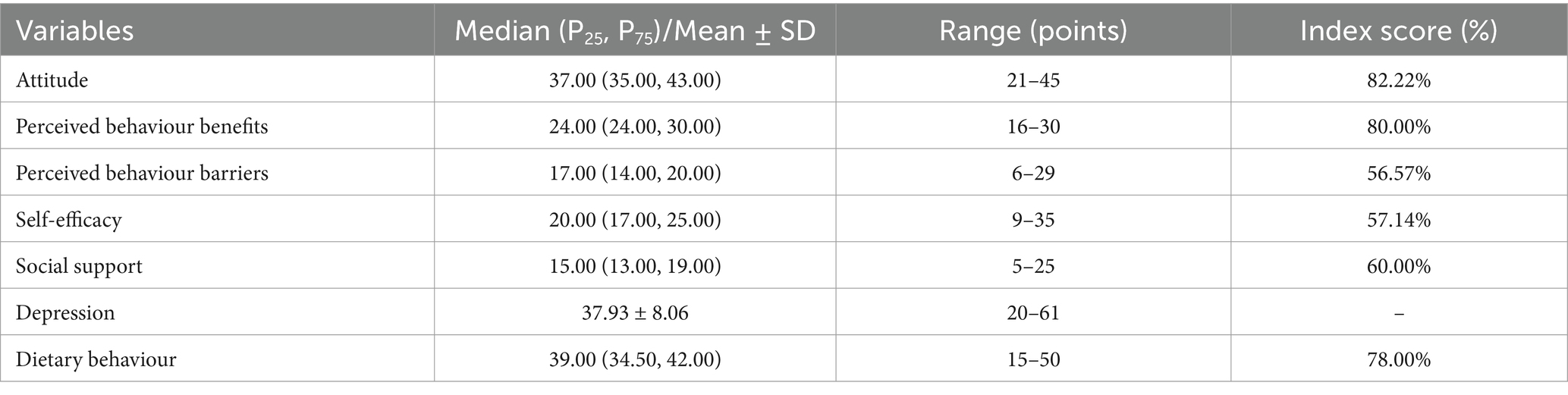
The participants reported high levels of attitude and perceived behaviour benefits, as well as moderate levels of social support, self-efficacy, and perceived behaviour barriers. About 41.86% of participants were classified as depressed. Score of dietary behaviour was at a moderate level (Table 1).
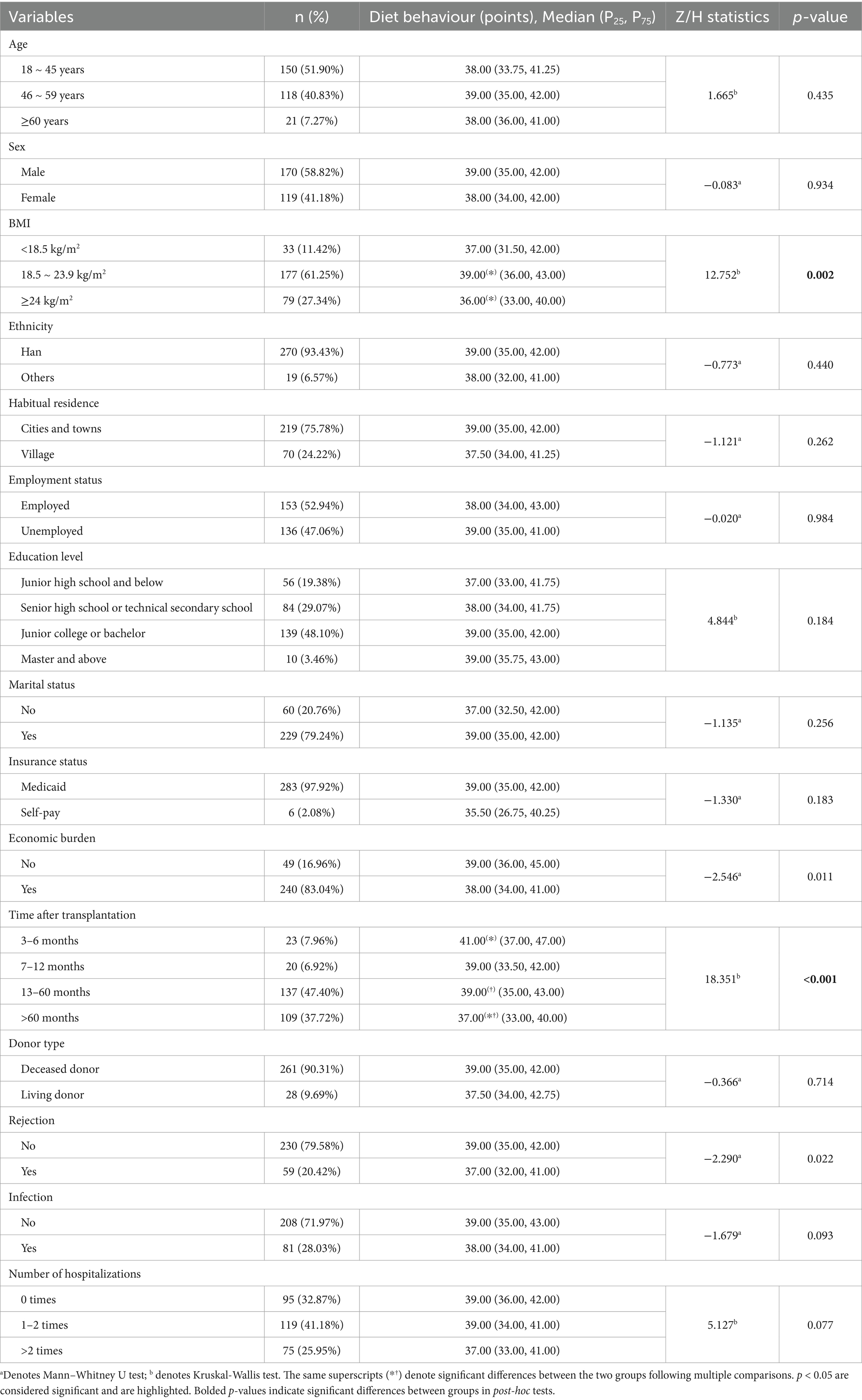
3.2 Univariate analyses of demographic and clinical characteristics
The results of the non-parametric test indicate a significant association between BMI and dietary behaviour among KTRs. Further analysis using the Bonferroni post-hoc test revealed a significant difference between the normal BMI group and the high BMI group (adjusted p = 0.001 < 0.017). Recipients without financial burdens exhibited better dietary behaviour (p = 0.011). With an increased post-transplantation duration, score of dietary behaviour decreased (p < 0.001). The Bonferroni post-hoc test indicated significant differences in score between recipients at 3–6 months and those at over 60 months post-transplant (adjusted p = 0.003 < 0.008), as well as between those at 13–60 months and those at over 60 months (adjusted p = 0.004 < 0.008). Recipients without a history of rejection demonstrated better dietary behaviour (p = 0.022). Detailed results are presented in Table 2.
3.3 Correlation analyses between variables in the HPM
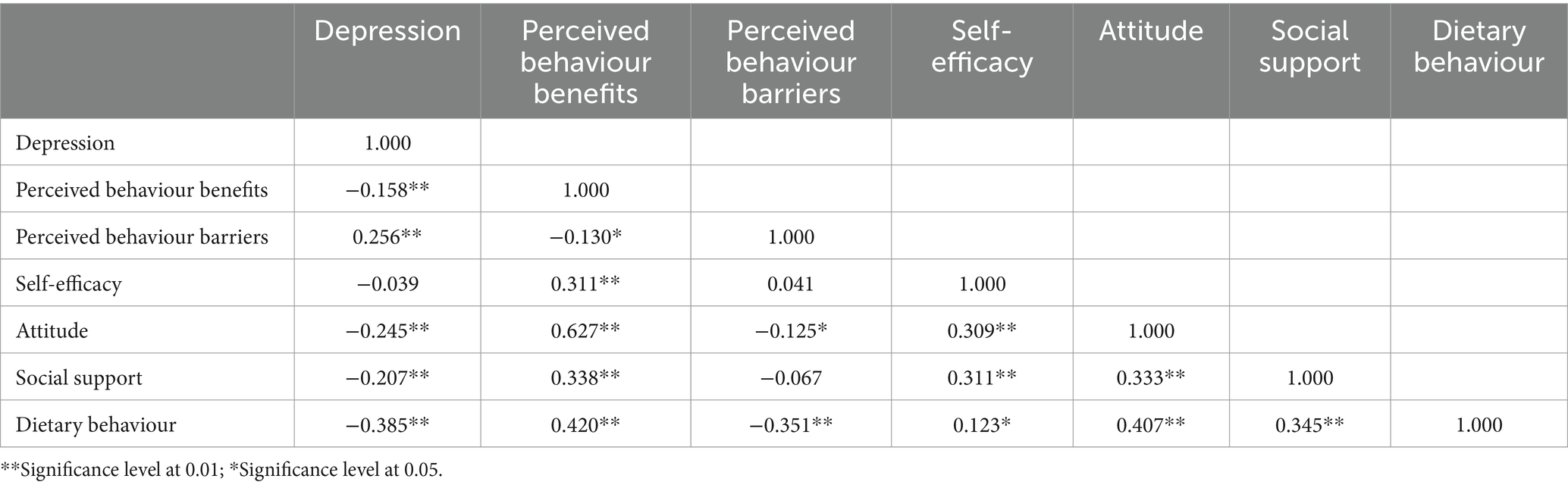
Table 3 illustrates that the dietary behaviour of KTRs was positively associated with perceived behaviour benefits, self-efficacy, attitude, and social support (r = 0.420, 0.123, 0.407, and 0.345, respectively; p < 0.05) and negatively associated with depression and perceived barriers (r = −0.385 and −0.351, respectively; p < 0.01).
3.4 Path analysis exploring the influencing factors of dietary behaviour in KTRs
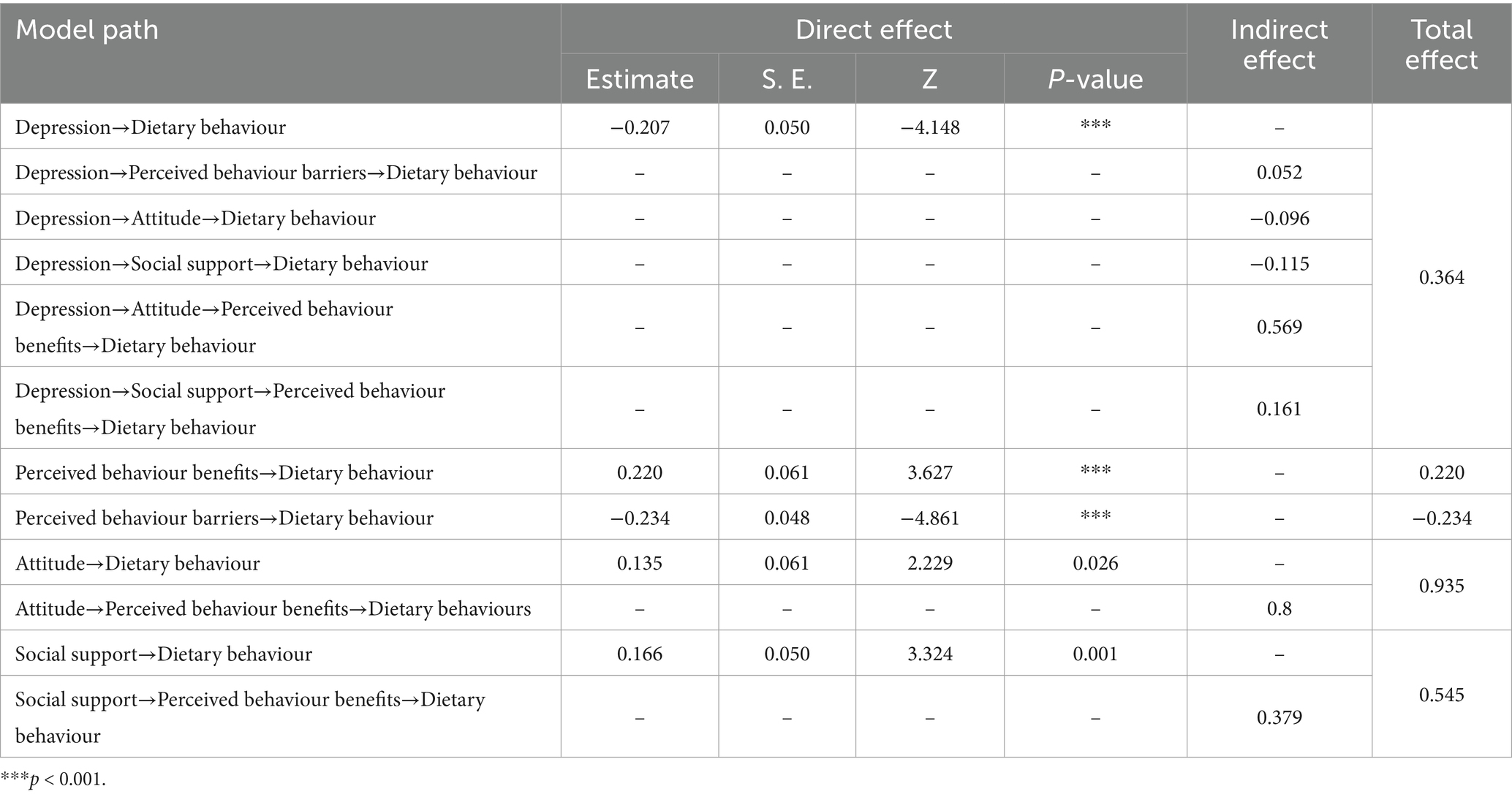
Non-parametric tests yielded statistically significant differences among different BMI levels, different financial burdens, post-transplantation time, and rejection situation, suggesting that these variables may be predictors of dietary behaviour. We used the above factors as control variables for dietary behaviour. Depression, attitude, perceived benefits, perceived barriers, social support, and self-efficacy, which were significantly correlated with dietary behaviour, entered into the path analysis model. But the initial hypothesized model exhibited inadequate fit, so direct paths from self-efficacy to dietary behaviour were removed, as well as the paths from depression to self-efficacy, the path from self-efficacy to perceived barriers, and the path from depression and self-efficacy to perceived benefits. Paths from attitude and social support to perceived benefits in KTRs and the connection between attitude and social support were incorporated (16, 25). The final path analysis results, illustrated in Figure 2, exhibited suitable fit indices: χ2/df = 2.079, RMSEA = 0.061, CFI = 0.945, TLI = 0.912, SRMR = 0.067. All correlations were statistically significant (p < 0.05).
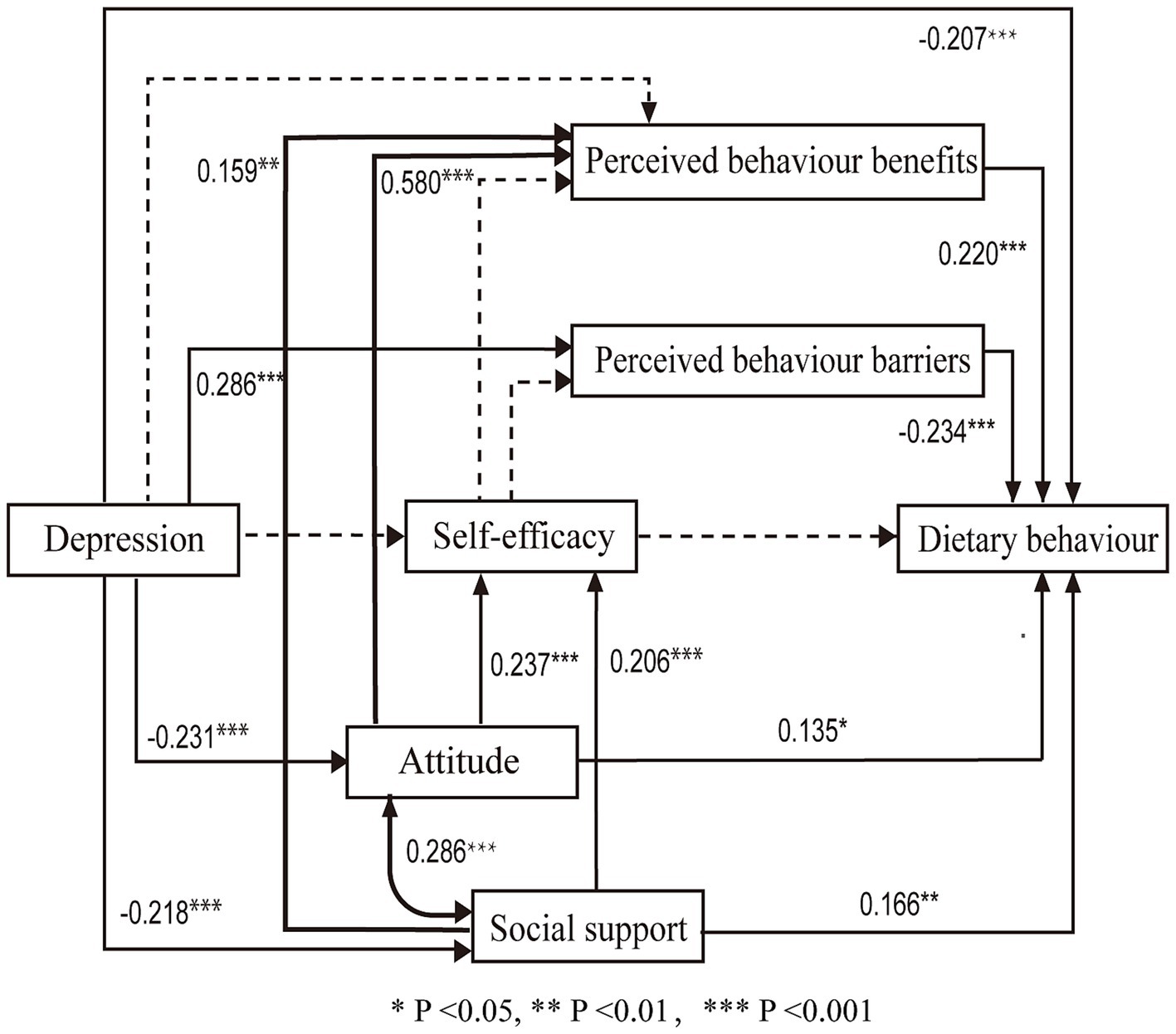
Figure 2. Standardized estimates in the path analysis. The associations among the variables are depicted with solid lines. The new lines are bold. The non-significant paths are depicted with dotted lines for comparison with the initial model. *P < 0.05, **P < 0.01, ***P < 0.001.
Figure 2 summarises the crucial path associations. Table 4 displays the direct, indirect, and total effects on dietary behaviour. Depression (β = −0.207, p < 0.001), perceived behaviour benefits (β = 0.220, p < 0.001), perceived behaviour barriers (β = −0.234, p < 0.001), attitude (β = 0.135, p = 0.026) and social support (β = 0.166, p = 0.001) directly predicted dietary behaviour. Among these, depression, attitude, and social support exhibited indirect effects on dietary behaviour. The total effects of these five factors were 0.364, 0.220, −0.234, 0.935, and 0.545, respectively.
In addition, depression predicted perceived barriers (β = 0.286, p < 0.001), attitude (β = −0.231, p < 0.001), and social support (β = −0.218, p < 0.001). Attitude (β = 0.580, p < 0.001; β = 0.237, p < 0.001) and social support (β = 0.159, p = 0.001; β = 0.206, p < 0.001) both directly predicted perceived benefits and self-efficacy. Notably, attitude and social support exhibited a positive correlation (p < 0.001). However, the VIF values for these two factors were both 1.115, indicating the absence of multicollinearity between them. Generally, all factors collectively accounted for 38.06% of the variance. Attitude, social support, depression, perceived barriers, and perceived benefits were important factors influencing dietary behaviour.
4 Discussion
This study, grounded in the HPM, investigated the current dietary behaviour and associated factors among KTRs. Several key findings were identified: (1) The dietary behaviour of KTRs was found to be at a moderate level. (2) Recipients with an absence of financial burdens, no history of rejection, normal BMI, and a shorter post-transplant duration exhibited better dietary behaviour. (3) Depression, perceived behaviour benefits, perceived behaviour barriers, attitude, and social support directly predicted dietary behaviour, while depression, attitude, and social support exhibited an indirect effect on dietary behaviour.
4.1 Dietary behaviour in kidney transplant recipients: a moderate level
In this study, KTRs had a dietary behaviour index score of 78.00%, indicating a moderate level. This finding is inconsistent with the finding of Lin’s study (26), which evaluated the adherence of KTRs to recommended dietary guidelines by measuring their daily nutrient intake compliance, revealing a notably low adherence rate. Such discrepancies may stem from recent advancements in information technology and the emergence of new health education methods. With the development of information technology, many newly developed applications such as MyFitnessPal can help KTRs calculate the amount of various nutrients in their diet, which makes their dietary compliance more convenient and feasible (27). Meanwhile, in recent years, kidney transplant physicians and follow-up professionals have paid more attention to health education and dietary risk monitoring in daily interventions, which may make the dietary behaviour scores of the participants in this study at a moderate level.
4.2 Influence of demographic and clinical characteristics on dietary behaviour
This study’s findings suggested that recipients with absence of financial burdens and no history of rejection exhibited better dietary behaviour. This observation can be attributed to the fact that recipients with a lower economic burden may find it easier to purchase low-fat and low-carbohydrate foods (28), which may contribute to improved dietary behaviour. Moreover, recipients without a history of rejection tend to achieve higher dietary behaviour scores, possibly because those with better dietary practices avoid foods that could affect drug concentrations, thereby reducing the risk of rejection (29). Additionally, our non-parametric analysis found that normal BMI and shorter post-transplant duration were associated with higher dietary behaviour scores. Subsequent multiple comparison analyses revealed that recipients with a normal BMI exhibited better dietary behaviour compared to those with higher BMI. This finding is consistent with previous research suggesting that recipients with a normal BMI are more inclined to consume a Mediterranean diet and exhibit better dietary behaviour (30). Furthermore, compared with the recipients whose postoperative period exceeded 60 months, those whose postoperative period was between 3 and 6 months or between 13 and 60 months performed better in terms of dietary behaviour scores. This trend suggests that as KTRs gradually return to normal life, increased social engagement and participation in daily activities may result in a reduced emphasis on dietary habits. Moreover, the effectiveness of dietary education for KTRs may decline as the follow-up period extends (31). These findings underscore the influence of demographic and clinical characteristics on the dietary behaviour of KTRs. Consequently, interventions aimed at improving dietary behaviour should be tailored to the specific circumstances of the recipients.
4.3 Direct and indirect effects of depression, and behaviour-specific cognitions and affect factors on dietary behaviour
This study identified both direct and indirect factors influencing dietary behaviour through path analysis. In terms of direct factors, the current study found that depression, perceived behaviour benefits, perceived behaviour barriers, attitude, and social support could directly predict dietary behaviour. A corpus of research on depression and dietary behaviour has illuminated a close association between patients’ psychological status and dietary behaviour (32). For instance, the adoption of the Mediterranean diet has been associated with a diminished incidence of depression (33), while a heightened risk of depression has been linked to escalated red meat consumption (34). This finding further demonstrated that an enhancement in perceived benefits could promote healthy dietary behaviour, consistent with previous findings (35). This may be attributed to the tendency of recipients who recognise the advantages of healthy behaviour to amend detrimental dietary habits. Conversely, research has shown that the greater individuals perceived dietary barriers, the more difficult it was for them to change their dietary behaviour and adhere to post-transplant dietary directives, ultimately resulting in lower dietary behaviour scores (36). Furthermore, it was found that recipients with positive attitudes are likely to exhibit better dietary habits. Research has indicated that patients with diabetics with a positive attitude exhibited a 3.2-fold likelihood (95% CI: 1.5–6.7) to follow dietary recommendations compared to their counterparts with negative attitudes (37). Additionally, we observed that social support positively influenced dietary behaviour in KTRs, corroborating the results of several previous studies (38, 39). This effect may be attributable to the proactive problem-solving strategies employed by recipients with high levels of social support, who are also more attentive to their post-operative health status, thereby enhancing their dietary behaviour (39). Future research should prioritise exploring interventions that target both direct pathways to enhance dietary behaviour.
This study also found that depression, attitude, and social support exhibited indirect effects on dietary behaviour. These results were different from those of previous studies, which primarily focused on direct associations (37) and did not consistently identify the same indirect pathways influencing behaviour (15, 40). In this study, depression exhibited an indirect association with dietary behaviour, which is broadly consistent with the theoretical underpinnings of the HPM (7). Depressed recipients may have a bad attitude and social support and thus perceive fewer benefits, which may lead to poor dietary behaviour. They may also have more perceived barriers, followed by poor dietary behaviour. Additionally, the current study indicated that attitude indirectly influenced dietary behaviour through perceived benefits, thus extending the pathways of attitude’s indirect effect on dietary behaviour. This finding is inconsistent with previous research, which has indicated that attitude, particularly instrumental attitude, may indirectly affect behaviour through factors such as behavioural intention (41, 42). Similarly, mirroring the indirect effect of attitude, social support also indirectly influenced dietary behaviour through perceived benefits, a finding that differs from prior studies (15). Previous research has suggested that social support may indirectly affect behaviour, such as fruit and vegetable intake, by influencing self-efficacy (15). These findings highlight the indirect effects of improving depression, fostering positive attitude, and bolstering social support to improve dietary behaviour. In this study, attitude and social support exhibited a positive correlation. A positive attitude enhances levels of food literacy (43). Furthermore, food literacy is most closely associated with social support among recipients post-transplant (44). Consequently, a favourable attitude may encourage recipients to actively seek social support. Additionally, beneficial social support factors, including social roles and communication patterns, significantly affect patients’ beliefs and attitudes (45). This further contributes to our understanding of how social support influences attitude.
4.4 Theoretical implications
This study extends the application of the HPM theory within the context of dietary behaviour among KTRs. In contrast to the initial hypothesised model, this study incorporated novel pathways from attitude and social support to perceived benefits in KTRs, as well as a connection between attitude and social support. However, some pathways from the initial model were also removed. In this study, there was no significant association between self-efficacy and depression, perceived benefits, or perceived barriers. Similarly, no significant correlation was observed between depression and perceived benefits. Overall, path analysis explained only 38.06% of the variance in dietary behaviour of KTRs, slightly lesser than the previous study (46). The slight reduction of explanatory power may result from the exclusion of commitment to action planning and immediate competing demands and preferences in our study. Therefore, in future research, the relationship between the variables in behaviour-specific cognition and affect warrants further examination.
4.5 Limitations
This study has several limitations. Firstly, the utilisation of self-reported questionnaires introduces the potential for reporting bias. Secondly, being a cross-sectional study, causal inferences are not supported. Thirdly, although our data were collected from four hospitals across different regions, the sample size is relatively small, which may result in selection bias and limit the generalisability of the findings to participants from diverse cultural backgrounds and regions. Future research should consider increasing the sample size and employing stratified or random sampling methods to reduce bias and better account for inter-hospital variability.
5 Conclusion
This study revealed that the scores of dietary behaviour among KTRs were at a moderate level and were notably influenced by psychological factors and behaviour-specific cognitive factors. Depression, perceived benefits, perceived barriers, attitude, and social support directly predicted dietary behaviour, and that depression, attitude, and social support exhibited indirect effects on dietary behaviour. These findings suggest that intervention about changing poor dietary attitude and negative mode, guiding them to receive more social support and perceived benefits, reducing their perceived barriers about dietary behaviour should be given. Healthcare professionals can also explore additional strategies, such as utilising digital behaviour change interventions, to enhance long-term dietary adherence in KTRs.
Data availability statement
The datasets presented in this article are not readily available because the dataset may be protected by copyright, and its use may require permission or licensing from the corresponding author. Requests to access the datasets should be directed to Hongxia Liu, aG9uZ3hpYV90QDE2My5jb20=.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Beijing University of Chinese Medicine (2023BZYLL0107). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JF: Conceptualization, Data curation, Software, Writing – original draft, Writing – review & editing. XLin: Conceptualization, Writing – original draft, Writing – review & editing. CW: Software, Data curation, Writing – original draft. QW: Writing – original draft, Writing – review & editing. KL: Software, Writing – review & editing. SZ: Writing – review & editing. PZ: Resources, Writing – review & editing. XLi: Software, Writing – original draft. HL: Conceptualization, Methodology, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the National Natural Science Foundation of China (Grant no. 82072553).
Acknowledgments
Sincere gratitude is extended to the study participants. Additionally, appreciation goes to the medical professionals, including doctors and nurses, who contributed to the data collection process.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2025.1467667/full#supplementary-material
References
1. Chinese Scientific Registration System for Kidney Transplantation. (2023). Available online at: http://www.csrkt.org/main/index.do (Accessed March 23, 2023)
2. Global Observatory on Donation and Transplantation. (2023). Available online at: http://www.transplant-observatory.org/summary/ (Accessed March 23, 2023)
3. Ikizler, TA, Burrowes, JD, Byham-Gray, LD, Campbell, KL, Carrero, JJ, Chan, W, et al. KDOQI clinical practice guideline for nutrition in CKD: 2020 Update. Am J Kidney Dis. (2020) 76:S1–S107. doi: 10.1053/j.ajkd.2020.05.006
4. Goldfarb Cyrino, L, Galpern, J, Moore, L, Borgi, L, and Riella, LV. A narrative review of dietary approaches for kidney transplant patients. Kidney Int Rep. (2021) 6:1764–74. doi: 10.1016/j.ekir.2021.04.009
5. Oste, MCJ, Gomes-Neto, AW, Corpeleijn, E, Gans, ROB, de Borst, MH, van den Berg, E, et al. Dietary approach to stop hypertension (DASH) diet and risk of renal function decline and all-cause mortality in renal transplant recipients. Am J Transplant. (2018) 18:2523–33. doi: 10.1111/ajt.14707
6. Teleki, S, Zsido, AN, Komocsi, A, Lenard, L, Kiss, EC, and Tiringer, I. The role of social support in the dietary behavior of coronary heart patients: an application of the health action process approach. Psychol Health Med. (2019) 24:714–24. doi: 10.1080/13548506.2018.1550259
7. Walker, SN, Sechrist, KR, and Pender, NJ. The health-promoting lifestyle profile: development and psychometric characteristics. Nurs Res. (1987) 36:76–81.
8. Schwarzer, R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol. (2008) 57:1–29. doi: 10.1111/j.1464-0597.2007.00325.x
9. Shin, Y, Yun, S, Pender, NJ, and Jang, H. Test of the health promotion model as a causal model of commitment to a plan for exercise among Korean adults with chronic disease. Res Nurs Health. (2005) 28:117–25. doi: 10.1002/nur.20060
10. Rav-Marathe, K, Wan, TT, and Marathe, S. A systematic review on the KAP-O framework for diabetes education and research. Med Res Arch. (2016) 4:1–21.
11. Jia, W. Health education: people’s medical publishing house. Beijing: People’s Medical Publishing House (1998).
12. Park, SH, Oh, EY, Kim, SH, and Chang, KJ. Relationship among dietary taurine intake, dietary attitudes, dietary behaviors, and life stress by depression in Korean female college students. Adv Exp Med Biol. (2019) 1155:293–300. doi: 10.1007/978-981-13-8023-5_28
13. Fang, JL, Chen, WT, Wang, YJ, Zhao, J, Wang, JW, and Shao, CH. Factors associated with medication adherence in community patients with coronary artery disease based on health belief model (HBM): a cross-sectional study. J Fudan Univ Med Sci. (2019) 47:378–84. doi: 10.3969/j.issn.1672-8467.2020.03.011
14. Al-Dwaikat, TN, Rababah, JA, Al-Hammouri, MM, and Chlebowy, DO. Social support, self-efficacy, and psychological wellbeing of adults with type 2 diabetes. West J Nurs Res. (2021) 43:288–97. doi: 10.1177/0193945920921101
15. Chang, MW, Schaffir, J, Brown, R, and Wegener, DT. Mediation by self-efficacy in the relation between social support and dietary intake in low-income postpartum women who were overweight or obese. Appetite. (2019) 140:248–54. doi: 10.1016/j.appet.2019.05.031
16. Wu, ML. Structural equation modeling-AMOS advanced practice. Chongqing University Press. (2013). Available at: https://www.cqup.com.cn/index.php?m=content&c=index&a=show&catid=16&id=11809
17. Zhang, W, Zeng, L, Li, J, Deng, X, Jin, M, Chen, Z, et al. Construction and reliability and validity tests of the dietary self-management ability scale for kidney transplant recipients. Ann Palliat Med. (2020) 9:352–8. doi: 10.21037/apm.2020.03.07
18. DeVon, HA, Block, ME, Moyle-Wright, P, Ernst, DM, Hayden, SJ, Lazzara, DJ, et al. A psychometric toolbox for testing validity and reliability. J Nurs Scholarsh. (2007) 39:155–64. doi: 10.1111/j.1547-5069.2007.00161.x
19. Zung, WW. A self-rating depression scale. Arch Gen Psychiatry. (1965) 12:63–70. doi: 10.1001/archpsyc.1965.01720310065008
20. Lin, X, Lin, J, Liu, H, Teng, S, and Zhang, W. Depressive symptoms and associated factors among renal-transplant recipients in China. Int J Nurs Sci. (2016) 3:347–53. doi: 10.1016/j.ijnss.2016.11.003
21. Wen, X. The development and application of healthy eating cognitive beliefs questionnaire in chronic kidney disease based on health action process approach theory. Jilin Province, China: Jilin Universsity (2020).
22. Xing, L, Chen, QY, Li, JN, Hu, ZQ, Zhang, Y, and Tao, R. Self-management and self-efficacy status in liver recipients. Hepatobiliary Pancreat Dis Int. (2015) 14:253–62. doi: 10.1016/s1499-3872(15)60333-2
24. MacCallum, RC, Browne, MW, and Sugawara, HM. Power analysis and determination of sample size for covariance structure modeling. Psychol Methods. (1996) 1:130–49. doi: 10.1037/1082-989X.1.2.130
25. Jichuan, W, Xiaoqian, W, and Baofa, J. Structural equation model: method and application. Beijing: Higher Education Press (2011).
26. Lin, IH, Wong, TC, Nien, SW, Chou, YT, Chiang, YJ, Wang, HH, et al. Dietary compliance among renal transplant recipients: a single-center study in Taiwan. Transplant Proc. (2019) 51:1325–30. doi: 10.1016/j.transproceed.2019.02.026
27. Evenepoel, C, Clevers, E, Deroover, L, Van Loo, W, Matthys, C, and Verbeke, K. Accuracy of nutrient calculations using the consumer-focused online app MyFitnessPal: validation study. J Med Internet Res. (2020) 22:e18237. doi: 10.2196/18237
28. Kenawy, AS, Gheith, O, Al-Otaibi, T, Othman, N, Abo Atya, H, Al-Otaibi, M, et al. Medication compliance and lifestyle adherence in renal transplant recipients in Kuwait. Patient Prefer Adherence. (2019) 13:1477–86. doi: 10.2147/ppa.S209212
29. Moore, LW. Food, food components, and botanicals affecting drug metabolism in transplantation. J Ren Nutr. (2013) 23:e71–3. doi: 10.1053/j.jrn.2013.02.002
30. Tarsitano, MG, Porchetti, G, Caldara, R, Secchi, A, and Conte, C. Obesity and lifestyle habits among kidney transplant recipients. Nutrients. (2022) 14:2892. doi: 10.3390/nu14142892
31. Topbaş, E, Kavalalı, T, Öztürk, F, Can, S, Dedekoç, Ş, and Sapcı, Y. The impact of controlled fluid and salt intake training in patients undergoing haemodialysis. J Ren Care. (2015) 41:247–52. doi: 10.1111/jorc.12133
32. Bremner, JD, Moazzami, K, Wittbrodt, MT, Nye, JA, Lima, BB, Gillespie, CF, et al. Diet, stress and mental health. Nutrients. (2022) 12:2428. doi: 10.3390/nu12082428
33. Sánchez-Villegas, A, Ruíz-Canela, M, Gea, A, Lahortiga, F, and Martínez-González, MA. The association between the mediterranean lifestyle and depression. Clin Psychol Sci. (2016) 4:1085–93. doi: 10.1177/2167702616638651
34. Kazemi, S, Keshteli, AH, Saneei, P, Afshar, H, Esmaillzadeh, A, and Adibi, P. Red and white meat intake in relation to mental disorders in Iranian adults. Front Nutr. (2021) 8:710555. doi: 10.3389/fnut.2021.710555
35. Khodaveisi, MP, Omidi, AM, Farokhi, SM, and Soltanian, ARP. The effect of pender’s health promotion model in improving the nutritional behavior of overweight and obese women. Int J Community Based Nurs Midwifery. (2017) 5:165–74.
36. Vaughan, CA, Ghosh-Dastidar, M, and Dubowitz, T. Attitudes and barriers to healthy diet and physical activity: a latent profile analysis. Health Educ Behav. (2018) 45:381–93. doi: 10.1177/1090198117722818
37. Adam, HMI, Elmosaad, YM, Ahmed, AEE, Khan, A, and Mahmud, I. Dietary knowledge, attitude and practice among type 2 diabetes mellitus patients in Sudan: a hospital-based cross-sectional study. Afr Health Sci. (2021) 21:32–40. doi: 10.4314/ahs.v21i1.6
38. Zang, G, Shi, QY, Li, B, Zhang, QQ, Zhang, L, Jin, WW, et al. Qualitative research on the psychological experience of renal transplantation patients with renal dysfunction undergoing hemodialysis. J Nurs Train. (2022) 37:1894–7. doi: 10.16821/j.cnki.hsjx.2022.20.017
39. Zhao, SM, Dong, FF, Qiu, HZ, and Li, D. Quality of life, adherence behavior, and social support among renal transplant recipients in China: a descriptive correlational study. Transplant Proc. (2018) 50:3329–37. doi: 10.1016/j.transproceed.2018.05.026
40. Zrinyi, M, Juhasz, M, Balla, J, Katona, E, Ben, T, Kakuk, G, et al. Dietary self-efficacy: determinant of compliance behaviours and biochemical outcomes in haemodialysis patients. Nephrol Dial Transplant. (2003) 18:1869–73. doi: 10.1093/ndt/gfg307
41. Song, J, Shin, SY, Kim, K, Son, YJ, Kim, J, and Jang, I. Self-care behavior based on integrated behavioral model in patients with atrial fibrillation: a structural equation modeling approach. West J Nurs Res. (2024) 46:114–24. doi: 10.1177/01939459231218949
42. Pedrinelli, V, Rossi, A, and Brunetto, MA. Theory of planned behavior applied to the choice of food with preservatives by owners and for their dogs. PLoS One. (2024) 19:e0294044. doi: 10.1371/journal.pone.0294044
43. Moshtagh, M, Daneshvar, M, and Ghaedamini Harouni, G. Social determinants of food literacy in Iranian adult population: a cross-sectional study. Food Sci Nutr. (2025) 13:e70044. doi: 10.1002/fsn3.70044
44. Boslooper-Meulenbelt, K, Patijn, O, Battjes-Fries, MCE, Haisma, H, Pot, GK, and Navis, GJ. Barriers and facilitators of fruit and vegetable consumption in renal transplant recipients, family members and healthcare professionals-a focus group study. Nutrients. (2019) 11:2427. doi: 10.3390/nu11102427
45. Maddison-Roberts, H, Jones, C, and Satherley, RM. Gluten-free diet management and well-being in children with celiac disease: a qualitative study. Pediatr Allergy Immunol. (2025) 36:e70061. doi: 10.1111/pai.70061
46. Shahroodi, MV, Sany, SBT, Khaboshan, ZH, Orooji, A, Esmaeily, H, Ferns, G, et al. Psychosocial determinants of changes in dietary behaviors among Iranian women: an application of the pender’s health promotion model. Community Health Equity Res Policy. (2022) 42:209–18. doi: 10.1177/0272684X20976825
Keywords: kidney transplant recipients, dietary behaviour, depression, health promotion model, path analysis
Citation: Fang J, Lin X, Wei C, Wang Q, Lin K, Zhang S, Zhao P, Li X and Liu H (2025) Factors associated with dietary behaviour in kidney transplant recipients: a cross-sectional study. Front. Nutr. 12:1467667. doi: 10.3389/fnut.2025.1467667
Edited by:
Joanna Rog, European University in Radom, PolandReviewed by:
Jeanette Mary Andrade, University of Florida, United StatesDi Shen, People’s Hospital of Xinjiang Uygur Autonomous Region, China
Copyright © 2025 Fang, Lin, Wei, Wang, Lin, Zhang, Zhao, Li and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongxia Liu, aG9uZ3hpYV90QDE2My5jb20=
†These authors have contributed equally to this work
 Jiaxin Fang
Jiaxin Fang Xiaohong Lin1†
Xiaohong Lin1† Keke Lin
Keke Lin Hongxia Liu
Hongxia Liu