- 1Global Medical Affairs and Research, Abbott Nutrition, Columbus, OH, United States
- 2Nutrition Science, Abbott Nutrition, Granada, Spain
- 3Global Medical Affairs and Research, Abbott Nutrition, Bogotá, Colombia
- 4Ateneo de Manila University School of Medicine and Public Health, Pasig, Philippines
- 5Universidad del Rosario-Escuela de Medicina, Bogotá, Colombia
Worldwide, 1 in 5 children under 5 years experiences undernutrition; most commonly in in low- and middle-income countries. Inadequate nutrient and energy intake places children at risk of stunted growth, which is associated with delayed development, increased mortality, and reduced productivity in adulthood. We investigated global approaches for managing stunting in young children (ages 1–5 years) by reviewing research on nutrition-focused interventions and public health frameworks. Our aim was to identify components of effective nutritional care and monitoring. We screened 1,636 studies, reviewed 207 abstracts and full-texts, and included 9 studies for final analysis. These studies, conducted in China, Colombia, Guatemala, Haiti, India, Mexico (n = 2), Peru, and Vietnam evaluated clinical outcomes such as anthropometrics and dietary intake. Most interventions included caregiver nutrition education (n = 7), but none used routine and frequent nutrition screening; only 4 included frequent follow-ups, 3 assessed breastfeeding frequency, and 4 used macronutrient and micronutrient supplementation when indicated. Economic outcomes were reported in 4 studies, while process and clinical outcomes were commonly reported (n = 7). Based on our review, effecting stunting interventions should include: (i) routine screening of every child for nutritional risk based on WHO and UNICEF guidance, (ii) caregiver-targeted nutrition education (iii) supplementation with macro- and micronutrients as needed, and (iv) regular follow-up to monitor growth and nutritional status. Although the evidence base was small, stringent inclusion criteria focused on community-based, multi-component interventions. This highlights the need for expanded implementation research, particularly in under resourced regions. Comprehensive, multi-level strategies are essential to address the long-term health risks of pediatric undernutrition.
1 Introduction
Pediatric undernutrition remains a significant challenge today, particularly in low- and middle-income countries. More than one in five children under the age of five are affected by undernutrition, primarily due to inadequate intake of energy, protein and key micronutrients essential for healthy growth (1, 2). Beyond nutrient intake, early growth is also influenced by infections, subclinical pathogen exposure, and alterations in gut microbial communities during the first 1,000 days of life. Additionally, infections, subclinical pathogen carriage, and the metabolic impact of ‘dysbiotic’ commensal gut microbial communities can also influence undernutrition during the first 1,000 days (3). Infant gut microbiota affects the somatotropic axis through regulation of Insulin-like Growth Factor-1 (IGF-1) and growth hormone production, thereby affecting growth (3). These biological and environmental contributors disrupt hormonal pathways such as the somatotropic axis, further exacerbating growth faltering.
Stunting, defined as impaired linear growth or failure to achieve expected height for age, affected 22.3% (148.1 million) children under five globally in 2022 (4). Although some global regions have seen progress, stunting remains highly prevalent in low- and middle-income countries, with an estimated 95% of affected children residing in Asia or Africa. Latin America and the Caribbean also continue to face high rates, with Central America reporting prevalence as high as 16.9% (4). This persistence reflects not only nutritional deficits but also broader socio-economic inequalities and gaps in public health infrastructure (5, 6).
Despite widespread recognition of the 1,000 day window as the most critical period for stunting prevention (5, 7–9), growth faltering can also occur in later childhood (10, 11). Evidence suggests that nutritional interventions beyond infancy may still improve both linear growth and cognitive development (11–15), though catch-up growth after age two must be approached cautiously due to its association with increased risk for overweight, obesity, and cardiometabolic disease in adulthood (16, 17). Therefore, stunting prevention strategies must ensure nutrient adequacy without promoting excessive energy intake. Rapid catch-up growth after age two has been particularly linked with these long-term risks, underscoring the need for nutrient and energy adequacy (16, 17).
Undernutrition in early life has both immediate and long-term consequences, including impaired immune function, increased infection-related mortality (13), and delayed physical and cognitive development which may impact adulthood performance, resulting in shorter adult stature, reduced educational attainment, increased risk of chronic diseases, and lower economic productivity (2, 5, 16). This low individual productivity is a major barrier to individual and national development (16, 18, 19).
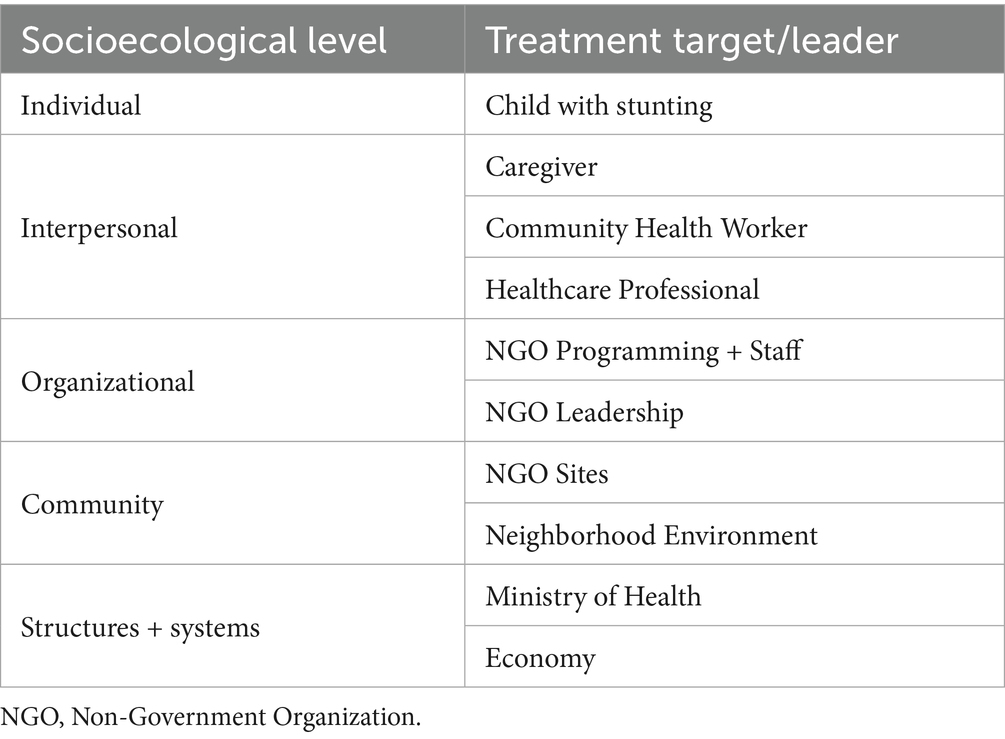
Global health frameworks such as the WHO and UNICEF conceptual models highlight the need for multi-level, multi-component strategies to prevent and treat undernutrition and stunting (19–21). These frameworks emphasize the importance of maternal nutrition, early initiation of breastfeeding, timely complementary feeding, and community-level improvements in hygiene and healthcare access (Table 1). Globally, only 44% of infants aged 0–6 months are exclusively breastfed, and fewer than one in four children aged 6–23 months meet the minimum criteria for dietary diversity and feeding frequency appropriate for their age (8). UNICEF guidance emphasizes the importance and efficacy of caregiver education, vitamin and mineral supplementation in nutrient-poor settings, and access to fortified foods aligned with national standards (9). They also call for implementation of targeted, context-specific programs that integrate caregiver education, access to fortified foods or supplements, and regular growth monitoring.
Despite significant policy momentum, including the 2012 World Health Assembly resolution to reduce stunting by 40% by 2025 and the UN Sustainable Development Goal to end all forms of malnutrition by 2030, progress has been insufficient (4, 18, 20). A 2021 Lancet series reinforced the need for scalable, locally adapted programs that address nutritional needs at multiple socio-ecological levels, from household feeding practices to national health policies (18, 22, 23).
Community-based nutrition interventions offer a promising delivery model, particularly for reaching under-resourced populations. These programs can incorporate low-cost supplements, caregiver counseling, child health monitoring, and behavior change strategies that engage families and local networks (24–27). When designed with cultural and contextual sensitivity, such interventions may also yield economic benefits, with some estimates suggesting returns on investment as high as 17% and benefit–cost ratios of 5:1 (28).
Despite these promising models, large-scale implementation remains challenging. The Lancet maternal and child undernutrition series (2021) highlighted uneven progress toward stunting reduction across low- and middle-income countries and emphasized the need for multi-sectoral efforts aligned with the UN Sustainable Development Goals (18). Earlier work from the 2013 Lancet series had already underscored the potential for greater private sector involvement in shaping affordable, scalable nutrition interventions (18). However, limited research exists on how to operationalize such partnerships effectively. The 2021 series further emphasized the need for robust implementation science and adaptive strategies that respond to what works in specific local contexts, underscoring persistent gaps in translating global frameworks into sustainable programs (29).
1.1 Aim for literature review
Although several studies have evaluated stunting prevention and intervention strategies, there remains limited research on the effectiveness and implementation of comprehensive, community-based nutritional care programs for young children. This review aims to address this gap by synthesizing evidence from studies that implemented multi-component community nutrition interventions. We specifically sought to understand which strategies have demonstrated clinical, health, or economic benefit, and how these strategies were integrated and sustained in community settings. The review was guided by the WHO and UNICEF frameworks and focused on practical implementation of nutritional care at multiple levels, from caregivers to health systems, to support improved growth outcomes among children at risk for or with stunting.
2 Methods for literature review
For our literature review, we searched publications from January 1990 to September 2023 from databases Allied & Complementary Medicine™, Embase®, EMCare®, FSTA®, and MEDLINE®. MeSH terms included “nutritional interventions,” “nutritional supplement,” “pediatric,” “malnutrition,” and “stunting.” Criteria for study inclusion were children aged 0–10; community-based; use of a nutrition supplement; nutrition education; clinical, health, or economic outcomes. Additional studies authors were aware of that were not already identified by the search were added manually (manual search) if they met study criteria. Although stunting most commonly originates in the first 1,000 days of life, this review included studies with participants aged 0–10 years to capture long-term outcomes of early-life interventions and evaluate follow-up impacts in later childhood. Notably, most included studies enrolled children younger than 5 years, aligning with the early-life focus of stunting prevention. Despite targeted manual searching, no studies from Sub-Saharan Africa met our predefined inclusion criteria, which required both nutrition education and supplementation components with stunting-specific outcomes. As such, all included studies were from Latin America and Asia. Studies were compared by their intervention components among 5 categories:
• Nutrient Intake Intervention: nutrition provided as part of the intervention.
• Education: topics included as part of the intervention.
• Education Mode: active (synchronous) or passive (asynchronous education such as flyers or posters).
• Other Resources Provided: other resources such as deworming program, farm animals, farming equipment, community gardens, etc.
• Follow-Up: non-frequent (greater than monthly/more than 4 weeks); frequent (at least once per month).
Trends were identified if the majority within an intervention component category had similar findings. While several included studies reported additional outcomes such as wasting and underweight which are expected, common concurrent conditions when evaluating nutritional recovery conditions, our review was limited to evaluating effects on stunting (height-for-age z-scores). This paper presents a narrative review based on a systematic search to identify representative interventions focused on stunting outcomes, rather than an exhaustive synthesis. The use of strict inclusion criteria, specifically requiring studies to combine nutrition education with supplementation and report stunting-related outcomes, was intentional to ensure focus, but may have limited the number of studies eligible for inclusion.
3 Results of our focused literature review
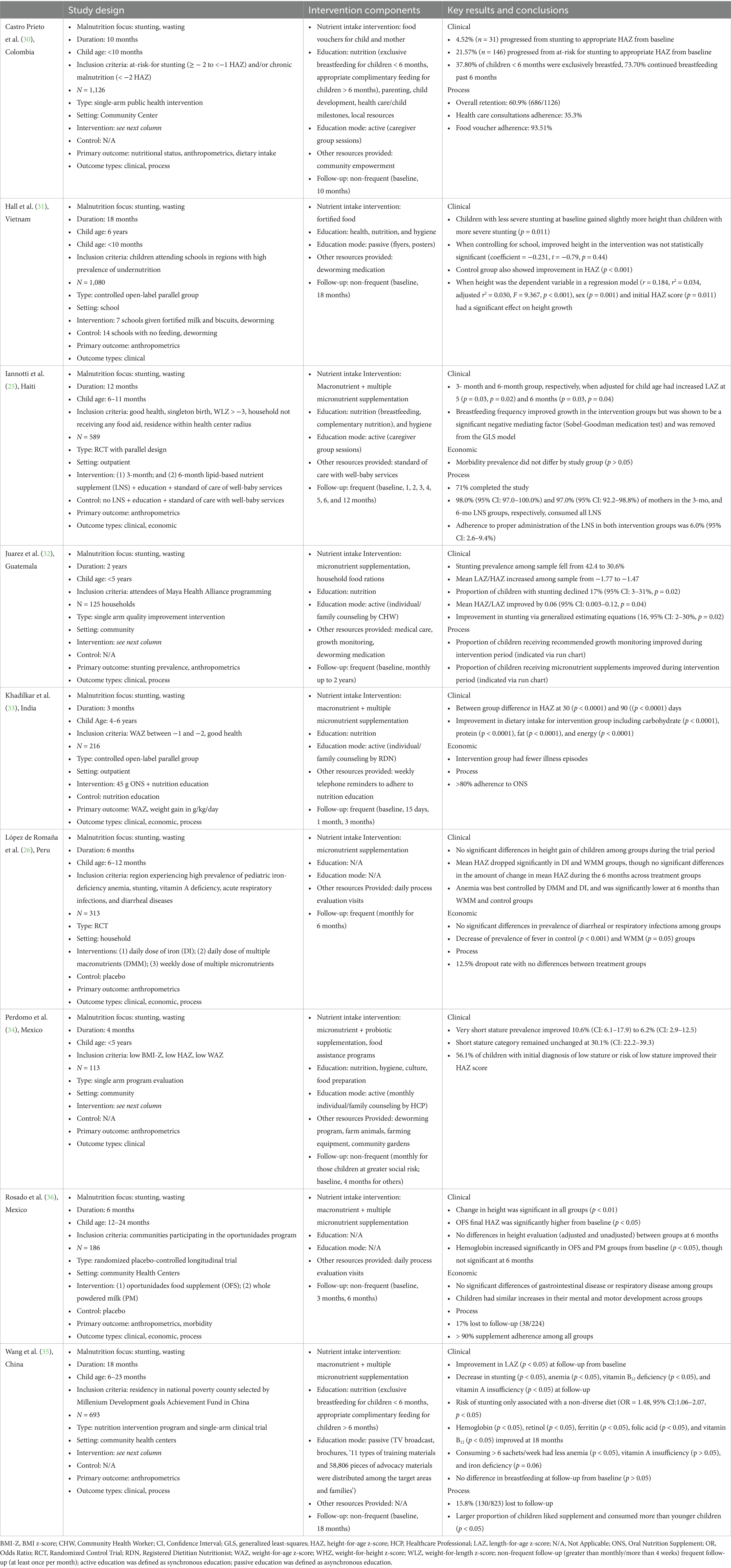
We initially identified 1,636 studies, narrowed the field to 207 abstracts/texts for review, and ultimately found 9 relevant research studies for a final analysis. In these 9 studies, researchers in China, Colombia, Guatemala, Haiti, India, Mexico, Peru, and Vietnam used various intervention components, then followed clinical (such as anthropometrics and dietary intake), economic (such as morbidity and illness incidence), and process (such as retention and adherence) (Table 2). We examined strengths and weaknesses of each research program. While most studies included nutrition education components for caregivers (n = 7) (25, 30–35), no study included routine and frequent screening for nutrition risk in pediatric populations, only 4 included frequent follow-ups (25, 26, 32, 33), only 3 studies measured breast feeding frequency (25, 30, 35), and only 4 used supplemental nutrition with macronutrients + multiple micronutrients when indicated (25, 33, 35, 36). Only 4 studies reported economic outcomes (25, 26, 33, 36), though most (n = 7) reported process outcomes along with clinical outcomes (25, 26, 30, 32, 33, 35, 36).
3.1 Studies involving multiple components (nutrition, education, other resources) had a synergistic and greater impact on outcomes (n = 7)
We found that studies using health education of caregivers or those using supplements fortified with multiple macronutrients and multiple micronutrients resulted in significant increases in height-for-age scores (37). Studies that included a nutritional, educational, and other resource components and/or frequent follow-ups showed greater improvements in stunting and other outcomes (25, 30–35). Studies that included only a nutritional and educational component with non-frequent follow-up had mixed results regarding improvement in stunting and/or wasting (31, 35, 36). The exact synergistic recipe of intervention components leading to greater results was unclear.
3.2 Studies with frequent follow-up had better outcomes (n = 4)
Most studies with frequent follow-up showed a trend of improvement in stunting outcomes (n = 3/4) (25, 32, 33), though it is important to note that the one study without good stunting outcomes included a supplement with micronutrients only but not additional resources (26). When reported, studies with frequent follow-up (at least once a month) also had good nutrition supplementation adherence (>80%) and low attrition rates. Those studies with less frequent follow-up (greater than 1 month between follow-ups) (30, 31, 34–36), had mixed results in whether stunting improvement was observed, and were mixed in their approach on length of frequency in between follow-ups, type of supplement, education, and other resources.
3.3 Comprehensive studies with macronutrient + multiple micronutrient supplements yielded better clinical outcomes (n = 4)
Children consuming macronutrient + multiple micronutrient supplements as part of a comprehensive nutrition intervention programs showed significant improvements in stunting (25, 33, 35), whereas when consuming a macronutrient + multiple micronutrient supplement without frequent follow-up and no education, improvements in stunting were not observed (36). This trend was similar among interventions that utilized micronutrient supplements or receiving food vouchers as part of comprehensive nutrition intervention programs (30, 32, 34). When studies did not utilize macronutrient + multiple micronutrient supplements or active education, there were no improvements in stunting (26, 31).
4 Discussion
The results of this review revealed that there is no single feeding strategy for addressing growth stunting in young children nor is there a universal best-practice package of interventions. However, our synthesis showed that multi-component interventions, those combining nutrition education, macronutrient and micronutrient supplementation, and regular follow-up, consistently led to better improvements in stunting-related outcomes.
Our review included studies from middle- and low-income countries around the world; however, the final selection was limited to studies from Latin America and South Asia due to the inclusion criteria. This geographic distribution reflects a limitation of available evidence, not of global need, and suggests a need for expanded research in other high-burden regions, particularly Sub-Saharan Africa and Southeast Asia (Table 2).
Although the interventions studied varied in scope and intensity, some consistent trends were observed. Studies that included multiple components, particularly those combining nutrition education with fortified supplements and frequent follow-up, reported more favorable changes in height-for-age scores, adherence, and retention. Conversely, studies that lacked any one of these components often had mixed or less pronounced results. However, the precise configuration of components yielding the greatest benefit remains unclear. Importantly, none of the included studies employed routine nutritional risk screening, and only four assessed economic outcomes, highlighting significant implementation gaps that future research should address.
Although many interventions had broader nutrition goals, our synthesis focused specifically on stunting, in line with the global emphasis on addressing chronic malnutrition. Although well-known regional programs such as the DREAM initiative in Malawi (38) and the Rainbow Project in Zambia (39) address important aspects of undernutrition, they were excluded from our analysis as they did not meet the full inclusion criteria, specifically, the combination of nutrition education, supplementation, and stunting outcomes. These efforts are nonetheless critical and offer complementary insights into ongoing nutrition and early childhood development interventions in Sub-Saharan Africa.
Although the UNICEF action framework (24) for complementary feeding encourages action by private institutions, the lack of knowledge about how to implement a multi-faceted intervention may impede those actions. Another recent review echoes this: creating and sustaining multi-sector partnerships to combat pediatric malnutrition has its challenges, and mirrors our review’s findings for the need for comprehensive, multi-faceted nutritional care programs (40).
With the development and evolution of sophisticated frameworks by WHO and UNICEF (Figure 1) (19, 21), as well as clearly enunciated principles, (21, 23) there is a clear call for multi-component approaches to impact the public health challenge of growth impairment due to nutritional insufficiency, as highlighted by our review. This call is echoed by a recent literature review highlighting how sustained, government-led, multi-sectoral strategies in Nepal, Bangladesh, and Vietnam have led to significant reductions in stunting prevalence over the past two decades (41). Our review supports this call for action, however, the exact recipe for synergistic intervention components with the most impact is unclear and future research should explore these components. Understanding these meaningful contributions by partners across different sectors are imperative to reduce stunting while improving the development of improved food environments, including their environmental sustainability, “to [create] sustainable, profitable models that explicitly include benefits to society and the environment” (23).
Guided by the frameworks of the United Nations, the World Health Organization, and the World Bank, we encourage stakeholders across multiple sectors to work together and implement nutrition-focused solutions at global, regional, and local levels. Such multi-component strategies and multi-level approaches are expected to lead to lasting and meaningful changes for care of children who are at risk of undernutrition and growth impairment (42, 43).
4.1 Multi-component and multi-level strategies for addressing growth stunting
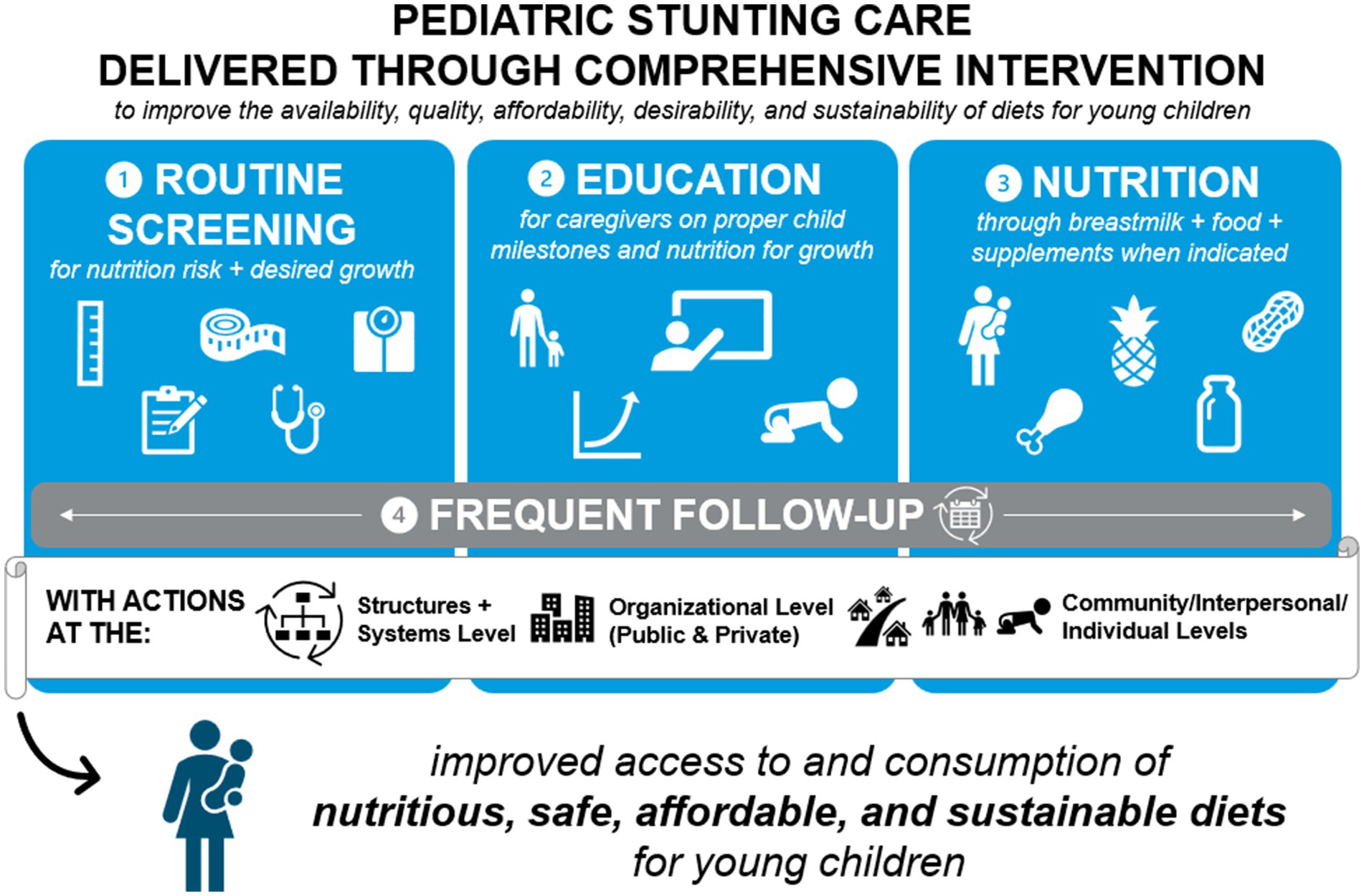
Based on our review of strategies used by researchers across different care sites and world locations, we identified four key approaches to address growth stunting in young children, complemented by recommendations of the WHO and UNICEF. However, real-world implementation of these strategies faces substantial operational, cultural, and policy-level barriers, which must be addressed to optimize program impact.
4.1.1 Regular nutritional screening
We underscore the importance of incorporating nutritional screening into regular community and clinical practices, especially in under-resourced communities where pediatric malnutrition/stunting is prevalent. Various screening tools are available to identify children at nutritional risk, defined as those due to their dietary characteristics, increased demands in their energy expenditure, or changes in anthropometric dynamics, have a greater probability of malnutrition, so selection can be tailored to meet needs by site and world region. Despite this, routine screening is rarely implemented though guidance from the WHO and UNICEF highlights the importance of screening for early identification. Logistical challenges, such as inadequate access to healthcare facilities and lack of calibrated measurement tools undermine screening efficacy (44). Additionally, workforce-related constraints, including limited personnel and insufficient training, further hinder consistent assessment and referral (45). These systemic limitations were also evident in our review, where none of the included studies integrated routine nutritional screening into the intervention protocol, highlighting a key gap that must be addressed to enable early identification and timely action.
4.1.2 Community-engaged research
Engagement of local communities, particularly through partnerships with champions and leaders, plays a crucial role in improving intervention design, delivery and sustainability. We continue to emphasize the benefits of culturally competent care strategies that are developed in collaboration with the communities they aim to serve (43). Community involvement enhances program relevance and acceptability, ensures cultural alignment, and facilitates dissemination of findings in both local and scientific domains (46). However, gaining community buy-in remains a challenge, particularly when interventions are not perceived as culturally relevant. Qualitative research from rural Ethiopia revealed that low parental education, lack of nutrition knowledge, cultural norms, and gender inequalities were among the major barriers to appropriate child feeding, underscoring how such sociocultural factors can limit program participation and effectiveness (47). Additionally, in siloed operational environments, limited cross-sector collaboration and lack of community-based coordination can diminish the potential impact of such programs (48). To overcome these issues, it is critical to embed trust-building, cultural tailoring, and intersectoral alignment into community nutrition programs from the outset.
4.1.3 Nutritional care with nutrition education + nutritional supplements
A key finding of our review was that interventions combining caregiver education with macro- and micronutrient supplementation were more effective in improving height-for-age z-scores than interventions using either strategy alone (5, 49). This combination was associated with improvements in both clinical outcomes and program retention.
However, real-world implementation of such combined approaches is frequently limited by resource constraints. Financial and supply-chain bottlenecks, including inconsistent delivery of supplements, inadequate infrastructure, and lack of regulatory incentives, undermine access and adherence (50, 51). Shortages of skilled personnel and limited parental knowledge also affect uptake (52, 53). Addressing these limitations through investments in workforce capacity, localized supply chain management, and culturally sensitive caregiver education can improve the reach and effectiveness of nutritional interventions.
4.1.4 Follow-up with ongoing monitoring
Sustained follow-up is essential to assess intervention impact, reinforce caregiver behavior, and maintain adherence. Our review noted that programs with frequent follow-up and monitoring reported stronger gains in growth and retention (54). Follow-up activities should include anthropometric tracking, health and nutrition status checks, and evaluation of cost-effectiveness to ensure long-term feasibility (54).
Nonetheless, adherence to follow-up schedules remains a major challenge in many low-income settings. Program structure, such as inflexible scheduling, long travel distances, and limited home outreach contributes to poor attendance, with fewer than 14% of caregiver-child pairs in some settings completing the recommended number of visits (55). Socio-cultural factors, including stigma, body image concerns, and lack of health equity in care access, have been shown to contribute to non-compliance and early dropout in pediatric nutrition interventions (56). Additionally, systemic barriers, like weak policy frameworks, limited insurance coverage, and inadequate infrastructure, impede the establishment of robust follow-up mechanisms (57).
Addressing these challenges requires stronger institutional support, stakeholder engagement, and application of implementation science frameworks to scale follow-up protocols without compromising quality (58, 59). Tailoring monitoring systems to community needs and leveraging digital innovations, such as tools piloted in the INFANT and Nutrition Now programs, may further improve reach and sustainability (60, 61).
4.2 Limitations
One major limitation of this review is the small number of studies (n = 9) that met the inclusion criteria, which limits the generalizability of our findings. This restricted evidence base stems from the stringent inclusion criteria that required studies to include community-based, multi-component interventions specifically targeting stunting outcomes. While this approach enhanced relevance, it narrowed the pool of eligible studies. Future reviews with broader inclusion criteria or alternative designs may capture a wider spectrum of interventions and settings. This study is a narrative review informed by a systematic search, not a full systematic review. It did not employ a formal quality appraisal of included studies, and selection was purposive to capture illustrative examples of multi-component nutrition interventions addressing stunting.
5 Conclusion
Our review on nutritional care for children with undernutrition presenting as stunting identified studies involving a range of interventions at multiple socio-ecological levels. Based on these study findings, we propose that comprehensive approaches to care include routine screening for nutritional risk, nutrition education for caregivers, use of nutritional supplements with macro- and micro-nutrients when indicated, and frequent follow-up on growth and nutritional status.
Given the significant burdens that undernutrition and growth stunting impose on children and societies worldwide, future studies of such comprehensive nutritional care are needed to confirm the feasibility and effectiveness for improvement of clinical, health, and economic outcomes.
Author contributions
AS: Writing – original draft, Writing – review & editing. EO: Writing – review & editing. SL: Writing – review & editing. CS: Writing – review & editing. MV: Writing – review & editing. CR: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Abbott Laboratories (Abbott Park, IL, USA) provided funding to support publication of this Review article. The funder was not involved in the study design, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Acknowledgments
We thank Ken Scholz (affiliated with Innovative BioPharma, LLC, Boulder, CO, USA) for medical writing support, Cecilia Hofmann, PhD (C Hofmann & Associates, Western Springs, IL, USA) for their editorial assistance and Bhavadharini Balaji, PhD (Wunderbar Medical & Scientific Writing, Ontario, Canada) for medical writing and literature synthesis support. Portions of this Review were presented at the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition on May 15-18, 2024, in Milan, Italy.
Conflict of interest
AS, EO, SL, and CS were employees of Abbott Laboratories while the work was completed. MG declares speaker honoraria from Abbott.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. UNICEF. Child malnutrition UNICEF2023 Available online at: https://data.unicef.org/topic/nutrition/malnutrition/#:~:text=In%202022%2C%2022.3%20per%20cent,204.2%20million%20to%20148.1%20million (Accessed August 19, 2025).
2. Reinhardt, K, and Fanzo, J. Addressing chronic malnutrition through multi-sectoral, sustainable approaches: a review of the causes and consequences. Front Nutr. (2014) 1:13. doi: 10.3389/fnut.2014.00013
3. Robertson, RC, Manges, AR, Finlay, BB, and Prendergast, AJ. The human microbiome and child growth-first 1000 days and beyond. Trends Microbiol. (2019) 27:131–47. doi: 10.1016/j.tim.2018.09.008
4. World Health Organization (WHO). Levels and trends in child malnutrition: UNICEF/WHO/World Bank Group joint child malnutrition estimates: key findings of the 2023 edition. New York: UNICEF and WHO (2023).
5. de Onis, M, and Branca, F. Childhood stunting: a global perspective. Matern Child Nutr. (2016) 12:12–26. doi: 10.1111/mcn.12231
6. Mwangome, M, and Prentice, AM. Tackling the triple threats of childhood malnutrition. BMC Med. (2019) 17:210. doi: 10.1186/s12916-019-1464-9
7. Shrimpton, R, Victora, CG, de Onis, M, Lima, RC, Blössner, M, and Clugston, G. Worldwide timing of growth faltering: implications for nutritional interventions. Pediatrics. (2001) 107:E75. doi: 10.1542/peds.107.5.e75
8. Victora, CG, de Onis, M, Hallal, PC, Blossner, M, and Shrimpton, R. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics. (2010) 125:e473–80. doi: 10.1542/peds.2009-1519
9. Adair, LS, Fall, CH, Osmond, C, Stein, AD, Martorell, R, Ramirez-Zea, M, et al. Associations of linear growth and relative weight gain during early life with adult health and human capital in countries of low and middle income: findings from five birth cohort studies. Lancet. (2013) 382:525–34. doi: 10.1016/S0140-6736(13)60103-8
10. Leroy, JL, Ruel, M, Habicht, JP, and Frongillo, EA. Linear growth deficit continues to accumulate beyond the first 1000 days in low- and middle-income countries: global evidence from 51 national surveys. J Nutr. (2014) 144:1460–6. doi: 10.3945/jn.114.191981
11. Prentice, AM, Ward, KA, Goldberg, GR, Jarjou, LM, Moore, SE, Fulford, AJ, et al. Critical windows for nutritional interventions against stunting. Am J Clin Nutr. (2013) 97:911–8. doi: 10.3945/ajcn.112.052332
12. Crookston, BT, Schott, W, Cueto, S, Dearden, KA, Engle, P, Georgiadis, A, et al. Postinfancy growth, schooling, and cognitive achievement: young lives. Am J Clin Nutr. (2013) 98:1555–63. doi: 10.3945/ajcn.113.067561
13. Lundeen, EA, Behrman, JR, Crookston, BT, Dearden, KA, Engle, P, Georgiadis, A, et al. Growth faltering and recovery in children aged 1-8 years in four low- and middle-income countries: young lives. Public Health Nutr. (2014) 17:2131–7. doi: 10.1017/S1368980013003017
14. Mani, S. Is there complete, partial, or no recovery from childhood malnutrition?—Empirical evidence from Indonesia. Oxf Bull Econ Stat. (2012) 74:691–715. doi: 10.1111/j.1468-0084.2011.00670.x
15. Schott, WB, Crookston, BT, Lundeen, EA, Stein, AD, and Behrman, JR. Periods of child growth up to age 8 years in Ethiopia, India, Peru and Vietnam: key distal household and community factors. Soc Sci Med. (2013) 97:278–87. doi: 10.1016/j.socscimed.2013.05.016
16. Black, RE, Alderman, H, Bhutta, ZA, Gillespie, S, Haddad, L, Horton, S, et al. Maternal and child nutrition: building momentum for impact. Lancet. (2013) 382:372–5. doi: 10.1016/S0140-6736(13)60988-5
17. Soliman, A, De Sanctis, V, and Elalaily, R. Nutrition and pubertal development. Indian J Endocrinol Metab. (2014) 18:S39–47. doi: 10.4103/2230-8210.145073
18. Victora, CG, Christian, P, Vidaletti, LP, Gatica-Domínguez, G, Menon, P, and Black, RE. Revisiting maternal and child undernutrition in low-income and middle-income countries: variable progress towards an unfinished agenda. Lancet. (2021) 397:1388–99. doi: 10.1016/S0140-6736(21)00394-9
19. World Health Organization (2014) Global nutrition targets 2025: stunting policy brief. World Health Organization. Available at: https://www.who.int/publications/i/item/WHO-NMH-NHD-14.3 (Accessed August 19, 2025).
20. United Nations. Sustainable development: the 17 goals Department of Economic and Social Affairs (2023). Available at: https://sdgs.un.org/goals (Accessed August 19, 2025).
21. UNICEF. UNICEF conceptual framework on maternal and child nutrition. New York, NY: UNICEF (2021).
22. Victora, CG, Adair, L, Fall, C, Hallal, PC, Martorell, R, Richter, L, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet. (2008) 371:340–57. doi: 10.1016/S0140-6736(07)61692-4
23. Swinburn, BA, Kraak, VI, Allender, S, Atkins, VJ, Baker, PI, Bogard, JR, et al. The global syndemic of obesity, undernutrition, and climate change: the lancet commission report. Lancet. (2019) 393:791–846. doi: 10.1016/S0140-6736(18)32822-8
24. United Nations Children’s Fund (UNICEF). Improving young children’s diets during the complementary feeding period. New York, NY: UNICEF Programming Guidance (2020).
25. Iannotti, LL, Dulience, SJ, Green, J, Joseph, S, Francois, J, Antenor, ML, et al. Linear growth increased in young children in an urban slum of Haiti: a randomized controlled trial of a lipid-based nutrient supplement. Am J Clin Nutr. (2014) 99:198–208. doi: 10.3945/ajcn.113.063883
26. Lopez de Romana, G, Cusirramos, S, Lopez de Romana, D, and Gross, R. Efficacy of multiple micronutrient supplementation for improving anemia, micronutrient status, growth, and morbidity of Peruvian infants. J Nutr. (2005) 135:646S–52S. doi: 10.1093/jn/135.3.646S
27. Rosado, JL, Lopez, P, Munoz, E, Martinez, H, and Allen, LH. Zinc supplementation reduced morbidity, but neither zinc nor iron supplementation affected growth or body composition of Mexican preschoolers. Am J Clin Nutr. (1997) 65:13–9. doi: 10.1093/ajcn/65.1.13
28. Galasso, E, and Wagstaff, A. The aggregate income losses from childhood stunting and the returns to a nutrition intervention aimed at reducing stunting. Econ Hum Biol. (2019) 34:225–38. doi: 10.1016/j.ehb.2019.01.010
29. Shekar, M, Condo, J, Pate, MA, and Nishtar, S. Maternal and child undernutrition: progress hinges on supporting women and more implementation research. Lancet. (2021) 397:1329–31. doi: 10.1016/S0140-6736(21)00577-8
30. Castro Prieto, PA, Trujillo Ramirez, KM, Moreno, S, Holguin, JS, Pineda, DM, Tomasi, S, et al. Reduction of chronic malnutrition for infants in Bogota, Colombia. BMC Public Health. (2021) 21:690. doi: 10.1186/s12889-021-10620-3
31. Hall, A, Hanh, TT, Farley, K, Quynh, TP, and Valdivia, F. An evaluation of the impact of a school nutrition programme in Vietnam. Public Health Nutr. (2007) 10:819–26. doi: 10.1017/S1368980007382530
32. Juarez, M, Dionicio, C, Sacuj, N, Lopez, W, Miller, AC, and Rohloff, P. Community-based interventions to reduce child stunting in rural Guatemala: a quality improvement model. Int J Environ Res Public Health. (2021) 18:773. doi: 10.3390/ijerph18020773
33. Khadilkar, A, Dhongade, A, and Agrawal, N. Growth, nutrient intake and frequency of illness in children aged 4-6 years: a randomised controlled study. J Clin Diagn Res. (2021) 15:OC11–6. doi: 10.7860/JCDR/2021/49599.15605
34. Perdomo, CD, Rodriguez, ER, Carrasco Magallanes, H, Flores Navarro, HE, Matul Perez, SE, and Moyano, D. Impact of a community program for child malnutrition. Rev Chil Pediatr. (2019) 90:411–21. doi: 10.32641/rchped.v90i4.901
35. Wang, J, Chang, S, Zhao, L, Yu, W, Zhang, J, Man, Q, et al. Effectiveness of community-based complementary food supplement (Yingyangbao) distribution in children aged 6-23 months in poor areas in China. PLoS One. (2017) 12:e0174302. doi: 10.1371/journal.pone.0174302
36. Rosado, JL, Lopez, P, Garcia, OP, Alatorre, J, and Alvarado, C. Effectiveness of the nutritional supplement used in the Mexican Oportunidades programme on growth, anaemia, morbidity and cognitive development in children aged 12-24 months. Public Health Nutr. (2011) 14:931–7. doi: 10.1017/S1368980010003344
37. Putri, R, Nuzuliana, R, and Kurniawati, HF, editors. Management of stunting to improved children nutritional status and cognitive is needed to reduce the negative impact of stunting on children 1st International Respati Health Conference (IRHC) [July 2019]; (2019); Yogyakarta, Indonesia.
38. Buonomo, E, de Luca, S, Tembo, D, Scarcella, P, Germano, P, Doro Altan, AM, et al. Nutritional rehabilitation of HIV-exposed infants in Malawi: results from the drug resources enhancement against AIDS and malnutrition program. Int J Environ Res Public Health. (2012) 9:421–34. doi: 10.3390/ijerph9020421
39. Moramarco, S, Amerio, G, Kasengele Chipoma, J, Nielsen-Saines, K, Palombi, L, and Buonomo, E. Filling the gaps for enhancing the effectiveness of community-based programs combining treatment and prevention of child malnutrition: results from the rainbow project 2015(−)17 in Zambia. Int J Environ Res Public Health. (2018) 15:1807. doi: 10.3390/ijerph15091807
40. Beggs, B, Bustos, M, Brubacher, LJ, Little, M, Lau, L, and Dodd, W. Facilitators and barriers to implementing complex community-based interventions for addressing acute malnutrition in low- and lower-middle income countries: a scoping review. Nutr Health. (2024) 30:447–62. doi: 10.1177/02601060241253327
41. Jalaludin, MY, Fauzi, MD, Sidiartha, IGL, John, C, Aviella, S, Novery, E, et al. Addressing stunting in children under five: insights and opportunities from Nepal, Bangladesh, and Vietnam-a review of literature. Children (Basel). (2025) 12:641. doi: 10.3390/children12050641
42. Keats, EC, Das, JK, Salam, RA, Lassi, ZS, Imdad, A, Black, RE, et al. Effective interventions to address maternal and child malnutrition: an update of the evidence. Lancet Child Adolesc Health. (2021) 5:367–84. doi: 10.1016/S2352-4642(20)30274-1
43. Key, KD, Furr-Holden, D, Lewis, EY, Cunningham, R, Zimmerman, MA, Johnson-Lawrence, V, et al. The continuum of community engagement in research: a roadmap for understanding and assessing Progress. Prog Community Health Partnersh. (2019) 13:427–34. doi: 10.1353/cpr.2019.0064
44. Meshkovska, B, Gebremariam, MK, Atukunda, P, Iversen, PO, Wandel, M, and Lien, N. Barriers and facilitators to implementation of nutrition-related actions in school settings in low- and middle-income countries (LMICs): a qualitative systematic review using the consolidated framework for implementation research (CFIR). Implement Sci Commun. (2023) 4:73. doi: 10.1186/s43058-023-00454-y
45. Kuppala, VS, Tabangin, M, Haberman, B, Steichen, J, and Yolton, K. Current state of high-risk infant follow-up care in the United States: results of a national survey of academic follow-up programs. J Perinatol. (2012) 32:293–8. doi: 10.1038/jp.2011.97
46. Balls-Berry, JE, and Acosta-Perez, E. The use of community engaged research principles to improve health: community academic partnerships for research. P R Health Sci J. (2017) 36:84–5.
47. Fikadu, K, Yihune, M, Boynito, WG, and Hailemariam, Z. Exploring multiple barriers to proper child feeding practices in rural districts of Ethiopia. Food Sci Nutr. (2025) 13:e4757. doi: 10.1002/fsn3.4757
48. Ouedraogo, O, Doudou, MH, Drabo, KM, Kiburente, M, Cisse, D, Mesenge, C, et al. Facilitating factors and challenges of the implementation of multisectoral nutrition programmes at the community level to improve optimal infant and young child feeding practices: a qualitative study in Burkina Faso. Public Health Nutr. (2021) 24:3756–67. doi: 10.1017/S136898002000347X
49. Murray, RD. Assessing nutritional risk among infants and tddlers in primary care practice. Pediatr Ann. (2018) 47:e465–9. doi: 10.3928/19382359-20181016-01
50. Sun, Y, Ma, J, Wei, X, Dong, J, Wu, S, and Huang, Y. Barriers to and facilitators of the implementation of a micronutrient powder program for children: a systematic review based on the consolidated framework for implementation research. Nutrients. (2023) 15:5073. doi: 10.3390/nu15245073
51. Santoso, SI, and Rodiyah, I. Achievements and barriers in evaluating stunting prevention programs in Keboguyang Village, Indonesia. Ind J Cult Comm Dev. (2024) 15. doi: 10.21070/ijccd.v15i3.1104
52. Chen, L, Huang, H, Jiang, S, Yao, H, Xu, L, Huang, Q, et al. Facilitators and barriers to the implementation of dietary nutrition interventions for community-dwelling older adults with physical frailty and sarcopenia: a qualitative meta-synthesis. Int J Nurs Sci. (2024) 11:18–30. doi: 10.1016/j.ijnss.2023.12.007
53. Kelleher, E, Davoren, MP, Harrington, JM, Shiely, F, Perry, IJ, and McHugh, SM. Barriers and facilitators to initial and continued attendance at community-based lifestyle programmes among families of overweight and obese children: a systematic review. Obes Rev. (2017) 18:183–94. doi: 10.1111/obr.12478
54. Murray, R, Kerr, K, Brunton, C, Williams, J, DeWitt, T, and Wulf, K. A first step towards eliminating malnutrition: a proposal for universal nutrition screening in pediatric practice. Nutr Diet Suppl. (2021) 13:17–24. doi: 10.2147/NDS.S287981
55. Agbozo, F, Colecraft, E, Jahn, A, and Guetterman, T. Understanding why child welfare clinic attendance and growth of children in the nutrition surveillance programme is below target: lessons learnt from a mixed methods study in Ghana. BMC Nurs. (2018) 17:25. doi: 10.1186/s12912-018-0294-y
56. Bodepudi, S, Hinds, M, Northam, K, Reilly-Harrington, NA, and Stanford, FC. Barriers to care for pediatric patients with obesity. Life (Basel). (2024) 14:884. doi: 10.3390/life14070884
57. Newsome, FA, Dilip, A, Armstrong, SC, Salloum, RG, and Cardel, MI. Scaling-up stage 4 pediatric obesity clinics: identifying barriers and future directions using implementation science. Obesity (Silver Spring). (2021) 29:941–3. doi: 10.1002/oby.23162
58. Gelman, R, Whelan, J, Spiteri, S, Duric, D, Oakhill, W, Cassar, S, et al. Adoption, implementation, and sustainability of early childhood feeding, nutrition and active play interventions in real-world settings: a systematic review. Int J Behav Nutr Phys Act. (2023) 20:32. doi: 10.1186/s12966-023-01433-1
59. Marshall, S, Johnson, BJ, Hesketh, KD, Campbell, KJ, Fraser, K, Love, P, et al. Mapping intervention components from a randomized controlled trial to scale-up of an early life nutrition and movement intervention: the INFANT program. Front Public Health. (2022) 10:1026856. doi: 10.3389/fpubh.2022.1026856
60. Overby, NC, Hillesund, ER, Helland, SH, Helle, C, Wills, AK, Lamu, AN, et al. Evaluating the effectiveness and implementation of evidence-based early-life nutrition interventions in a community setting a hybrid type 1 non-randomized trial - the nutrition now project protocol. Front Endocrinol (Lausanne). (2022) 13:1071489. doi: 10.3389/fendo.2022.1071489
61. Medin, AC, Vik, FN, Helle, C, Helland, SH, Wills, AK, Osorio, NG, et al. Scaling up evidence-based digital early life nutrition interventions in a county setting: an implementation trial - protocol for phase 2 of the nutrition now project. Front Public Health. (2023) 11:1326787. doi: 10.3389/fpubh.2023.1326787
Keywords: stunting, pediatric malnutrition, program evaluation, child health, nutrition programs
Citation: Sharn AR, Oliveros E, Lai S, Sanchez CP, Villa-Real Guno MJ and Rojas Montenegro C (2025) Multi-faceted nutritional interventions are imperative to reduction of stunting among children in low- and middle-income countries. Front. Nutr. 12:1479850. doi: 10.3389/fnut.2025.1479850
Edited by:
Mousumi Bhattacharjee, Tata Institute of Social Sciences, IndiaReviewed by:
Robert Morrison Dempster, The Research Institute at Nationwide Children’s Hospital, United StatesLeonardo Palombi, University of Rome Tor Vergata, Italy
Aydan Kansu Tanca, Ankara University, Türkiye
Copyright © 2025 Sharn, Oliveros, Lai, Sanchez, Villa-Real Guno and Rojas Montenegro. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amy R. Sharn, YW15LnNoYXJuQGFiYm90dC5jb20=
 Amy R. Sharn
Amy R. Sharn Elena Oliveros
Elena Oliveros Stephanie Lai1
Stephanie Lai1 Claudia P. Sanchez
Claudia P. Sanchez