- Department of Cardiology, Shengjing Hospital of China Medical University, Shenyang, Liaoning, China
Background: Controlling Nutritional Status (CONUT) score, a novel marker reflecting the malnutrition, has been demonstrated to predict all-cause mortality and major adverse cardiovascular events (MACE) in a wide range of diseases. The research intends to assess the clinical effects of malnutrition on patients who have percutaneous coronary intervention (PCI) after acute myocardial infarction (AMI).
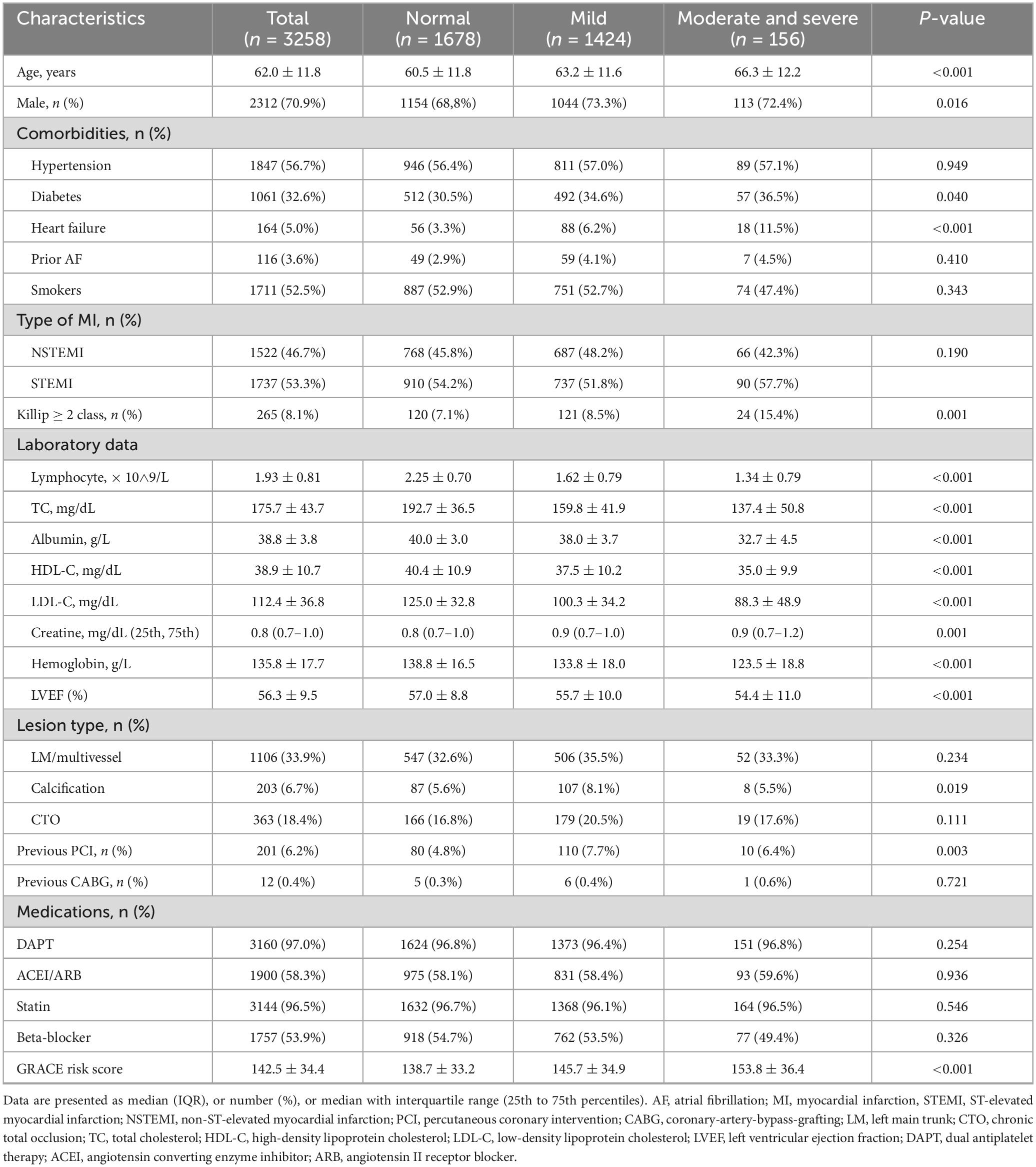
Methods: In this retrospective observational study, we consecutively enrolled 3258 patients diagnosed with AMI from 2010 to 2016. Patients were categorized into three groups based on the CONUT score: normal, mild malnutrition, and moderate and severe malnutrition. The primary outcome was all-cause mortality. We develop cox proportional hazards models to investigate the relationship between the CONUT score and all-cause mortality among patients who underwent PCI after AMI.
Results: According to the assessment via the CONUT score, a total of 43.7% patients experienced mild malnutrition, and 4.8% patients experienced moderate and severe malnutrition. During a median follow-up period of 8.6 years, there were 610 patients (18.7%) suffered from all-cause mortality. As malnutrition severity intensified, the occurrence of the primary endpoint saw a steady rise. After adjusting for multiple variables, the group classified with moderate and severe malnutrition exhibited an odds ratio of 1.56 (95% CI 1.13 to 2.15, p = 0.007) for the primary endpoint. Incorporating the CONUT score augments the prognostic accuracy of the GRACE risk score in predicting all-cause mortality (Absolute Integrated Discrimination Improvement = 0.008, p < 0.001; Category-free Net Reclassification Improvement = 0.144, p = 0.001).
Conclusion: Malnutrition is prevalent among patients with AMI and is significantly associated with an increased incidence of all-cause mortality. As a nutritional assessment tool, the CONUT score effectively aids in risk stratification and predicts poor prognosis in patients. Additional prospective clinical trials are required to evaluate the influence of nutritional interventions on outcomes in patients undergoing PCI after AMI.
1 Introduction
Acute myocardial infarction (AMI) is a major contributor to death globally and imposes significant costs related to medical treatment and work-related disabilities (1). Even though percutaneous coronary intervention (PCI) represents a sophisticated advanced therapy for AMI, this disease remains a prevalent and deadly form of cardiovascular illness, continuing to pose significant challenges to public health (2, 3). To enhance outcomes for AMI patients following PCI, it is crucial to further recognize those at heightened risk and strive to minimize the occurrence of negative events.
Malnutrition has been consistently identified by various studies as an independent risk factor for cardiovascular diseases, involving coronary artery disease (CAD), heart failure, cardiomyopathy, non-valvular atrial fibrillation (AF) and peripheral vascular disease (4–9). It is significantly associated with elevated all-cause mortality and increased incidence of major adverse cardiovascular events (MACE). Previous studies have suggested that the elevated mortality risk of AMI associated with malnutrition may be attributable to inflammatory mechanisms (10, 11). Inflammation can impair endothelial cell function, increase lipoprotein permeability, and facilitate the progression of atherosclerosis. Besides, inflammation may further exacerbate malnutrition (12, 13). Stenvinkel et al. reported that inflammation and malnutrition are closely linked to arteriosclerosis, and they have referenced Malnutrition-Inflammation-Atherosclerosis (MIA) syndrome (14). Currently, the American Heart Association (AHA) has demonstrated through the implementation of nutritional intervention measures that such approaches can reduce high-sensitivity C-reactive protein (CRP) level, thereby effectively improving patient prognosis (15). Consequently, timely and accurate assessment of patients’ nutritional status holds critical importance in clinical practice. With the aid of multiple nutritional assessment tools, the malnutrition status of patients can not only be quantified but also serve as an auxiliary factor for risk stratification. It provides clinicians with a more efficient approach to address patients’ malnutrition status. The Controlling Nutritional Status (CONUT) score is a nutritional assessment tool which comprises serum albumin, total cholesterol and lymphocyte counts, and its simplicity and effectiveness have been acknowledged (16–18). Nonetheless, the research surrounding the CONUT score, which serves to forecast the outcomes for patients experiencing AMI and undergoing PCI, remains sparse.
Accordingly, we intend to illustrate the incidence and long-term outcomes related to malnutrition in AMI patients following PCI while utilizing the CONUT score. Furthermore, the study aims to explore if the CONUT score can enhance the prognostic capabilities of the GRACE risk score concerning all-cause mortality.
2 Materials and methods
2.1 Study population
This retrospective observational study involved the inclusion of 3398 patients who were admitted to the cardiovascular department of ShengJing Hospital, part of China Medical University, and were ultimately underwent PCI after diagnosing with AMI during the period from January 2010 to December 2016. Patients who lost to follow-up (n = 29), lacked crucial baseline laboratory data (n = 75) were excluded. We also excluded 8 patients with a diagnosis of malignancy, 6 patients with a diagnosis of infection (19), and 22 patients with a diagnosis of severe liver dysfunction. Ultimately, 3258 patients were screened for analysis (Supplementary Figure 1). AMI was defined as acute myocardial injury with clinical evidence of acute myocardial ischemia according to Fourth Universal Definition of Myocardial Infarction by European Society of Cardiology (20). The study has been approved by Research Ethics Committee of ShengJing Hospital of China Medical University and conducted according to the principles of the Declaration of Helsinki.
2.2 Nutritional screening tools and clinical measurements
After enrollments, this study utilizes the CONUT points-scoring system to categorize the population into three groups. The CONUT scoring system is designed to evaluate nutritional health, incorporating three critical indicators: serum albumin, total cholesterol and lymphocyte cells (17, 18). Three laboratory variables were converted to the corresponding scores and add the scores together can obtain the CONUT scores. A score ranging from 0 to 1 was defined as normal nutritional status, while scores ranging from 2 to 4, 5 to 8, and 9 to 12 respectively indicate mild, moderate, and severe malnutrition (Supplementary Table 1).
The Laboratory data were measured by laboratory clinic in ShengJing Hospital of China Medical University. Fasting venous blood samples were gathered from all patients within 24 h of admission. Lymphocytes and hemoglobin were conducted using an automated blood counter (Unicell DxH800 Coulter, Beckman Coulter Corp., United States) with optical light scatter counting. The total cholesterol, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), serum albumin and creatine were calculated from an enhanced immunonephelometric assay on an automated analyzer (AU5800, Beckman Coulter Corp., United States). The left ventricular ejection fraction was measured using standardized echocardiography performed by the Department of Ultrasound at ShengJing Hospital, China Medical University within the first 48 h of admission (21).
2.3 Outcomes and follow-up
The primary outcome was all-cause mortality. We conducted follow-up via telephone interviews and review of medical records. The terminal survival status within the cohort was determined in October 2023. The follow-up phase concluded on 31 October 2023, or upon the occurrence of death.
2.4 Statistical analysis
Continuous variables which is normally distributed were expressed as mean ± SD, while those without normally distributed variables were expressed as a median with interquartile range (IQR). Categorical variables were expressed as n (%). Continuous variables compared between groups using the ANOVA and the Kruskal-Wallis test. Categorical variables were compared using the χ2 test. Time-to-event outcomes were illustrated using Kaplan-Meier survival curves, and the log-rank test was employed to evaluate differences in survival between groups. Univariable and two multivariate cox regression models were performed to assess the independent associations of CONUT with all-cause mortality. Model 1 of multivariate cox regression was adjusted for age and sex, while Model 2 was adjusted for age, sex, hypertension, diabetes, heart failure, prior AF, type of AMI (ST and non-ST segment elevation myocardial infarction), previous history of PCI, previous history of coronary-artery-bypass-grafting (CABG), left main trunk (LM)/multivessel coronary artery disease, calcification, chronic total occlusion (CTO), LDL-C, HDL-C, creatine, left ventricular ejection fraction (LVEF), dual antiplatelet therapy (DAPT), statin, angiotensin converting enzyme inhibitor (ACEI) and beta-blocker. Results were represented as hazard ratios (HRs) with associated 95% confidence intervals (CIs). In addition, we stratified the study population by age, gender, type of MI, and the presence or absence of comorbidities such as hypertension, diabetes, heart failure, and AF, and conducted multivariate COX regression analysis for each subgroup. In order to compare whether CONUT scores have the capacity to enhance the prognostic value in all-cause mortality in contrast to the traditional GRACE risk score, we utilized Harrell C-statistics, category-free net reclassification improvement (NRI) and absolute integrated discrimination improvement (IDI) to access the predictable value. All p-values were two-sided, and p-values < 0.05 were regarded as statistically significant. Above statistical analysis was conducted using IBM SPSS Statistics 26.
3 Results
3.1 Baseline characteristics
Table 1 outlines the baseline characteristics of the study cohort. From the total of 3258 patients included, 1737 had STEMI (53.3%), and 1522 had NSTEMI (46.7%). Most of them were male (70.9%), and the median age was 62.0 ± 11.8 years. Nearly 50% of the patients reported being smokers, and over one-third exhibited left main trunk or multivessel coronary artery disease. Among these patients, 48.5% (n = 1580) of patients were identified as malnourished using the CONUT scoring system. In addition, 43.7% (n = 1,424) had mild malnutrition and 4.8% (n = 156) had moderate and severe malnutrition, respectively. Patients with a lower nutritional status tended to be older, and had diabetes mellitus, heart failure, a diagnosis of STEMI and worse Killip class. In laboratory data, the moderate and severe malnutrition group exhibited lower levels of lymphocytes, total cholesterol (TC), albumin, and hemoglobin. The moderate and severe malnutrition group also exhibited a higher GRACE risk score, suggesting a heightened likelihood of all-cause mortality. The usage of medications following the onset of AMI showed no significant variation among the three different groups.
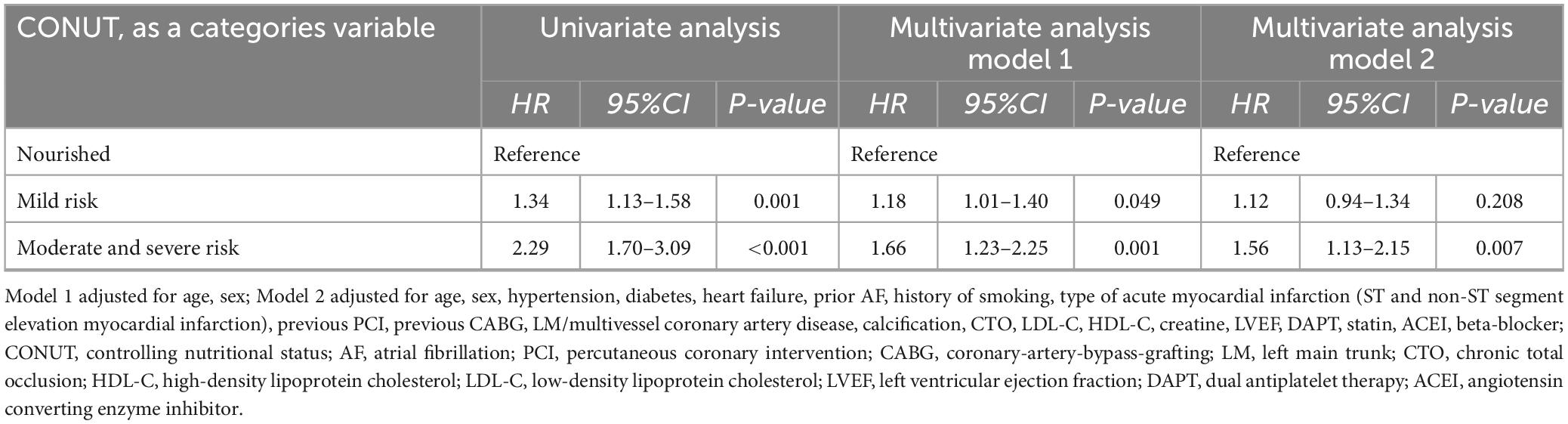
3.2 Prognostic factors for patients with different risks of malnutrition and outcomes
Following the adjustment for variables such as age and sex, model 1 indicated that patients within the moderate and severe malnutrition category faced a heightened risk relative to those classified as adequately nourished (HR 1.66, 95% CI 1.23 to 2.25, p = 0.001). Furthermore, after adjusting for all variables outlined in Supplementary Table 2, model 2 indicated that patients classified within the moderate and severe malnutrition category exhibited an elevated risk in comparison to those in the normal nutrition category (HR 1.56, 95% CI 1.13 to 2.15, p = 0.007) (Table 2).
Moreover, during a median follow-up of 8.6 years, 610 patients died after discharge. On Kaplan-Meier curve analysis, an increased all-cause mortality was observed among malnourished patients compared to nourished patients in the long-term prognosis. The moderate and severe malnutrition group exhibited the highest mortality (Figure 1). In subgroup analysis, the results showed that malnutrition had no significant difference in the prognosis impact on different characteristic populations (Figures 2A, B).

Figure 1. Analysis of the Kaplan-Meier curves for all-cause mortality categorized by the CONUT score among patients who underwent PCI after AMI.
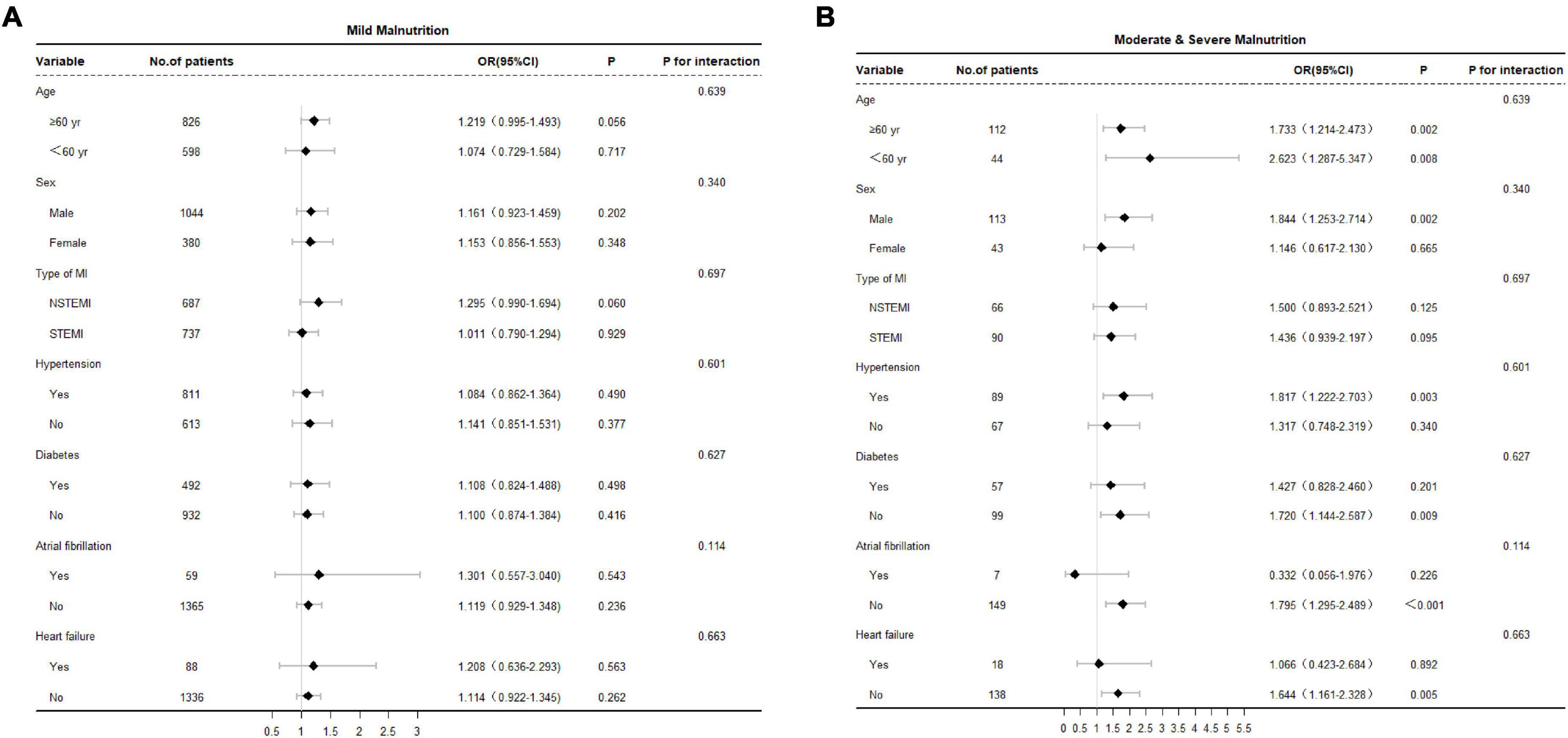
Figure 2. (A) Stratified analysis of the mild malnutrition group and all-cause mortality among patients who underwent PCI after AMI. Adjusted for research center, age, sex, hypertension, diabetes, atrial fibrillation and heart failure. (B) Stratified analysis of the moderate and severe malnutrition group and all-cause mortality among patients who underwent PCI after AMI. Adjusted for research center, age, sex, hypertension, diabetes, atrial fibrillation and heart failure.
Furthermore, we calculated the corresponding areas under the curve (AUC) and constructed the receiver operating characteristic (ROC) curve for both the GRACE risk score and the combined CONUT + GRACE risk score using C-statistics. The AUCs were 0.640 (p < 0.001, 95% CI: 0.615 to 0.664) and 0.651 (p < 0.001,95% CI: 0.627 to 0.676) respectively. The new model formed by GRACE risk score combined with CONUT can improve the prediction efficiency of GRACE risk score (NRI = 0.144, p = 0.001; IDI = 0.008, p < 0.001) (Figure 3 and Table 3).
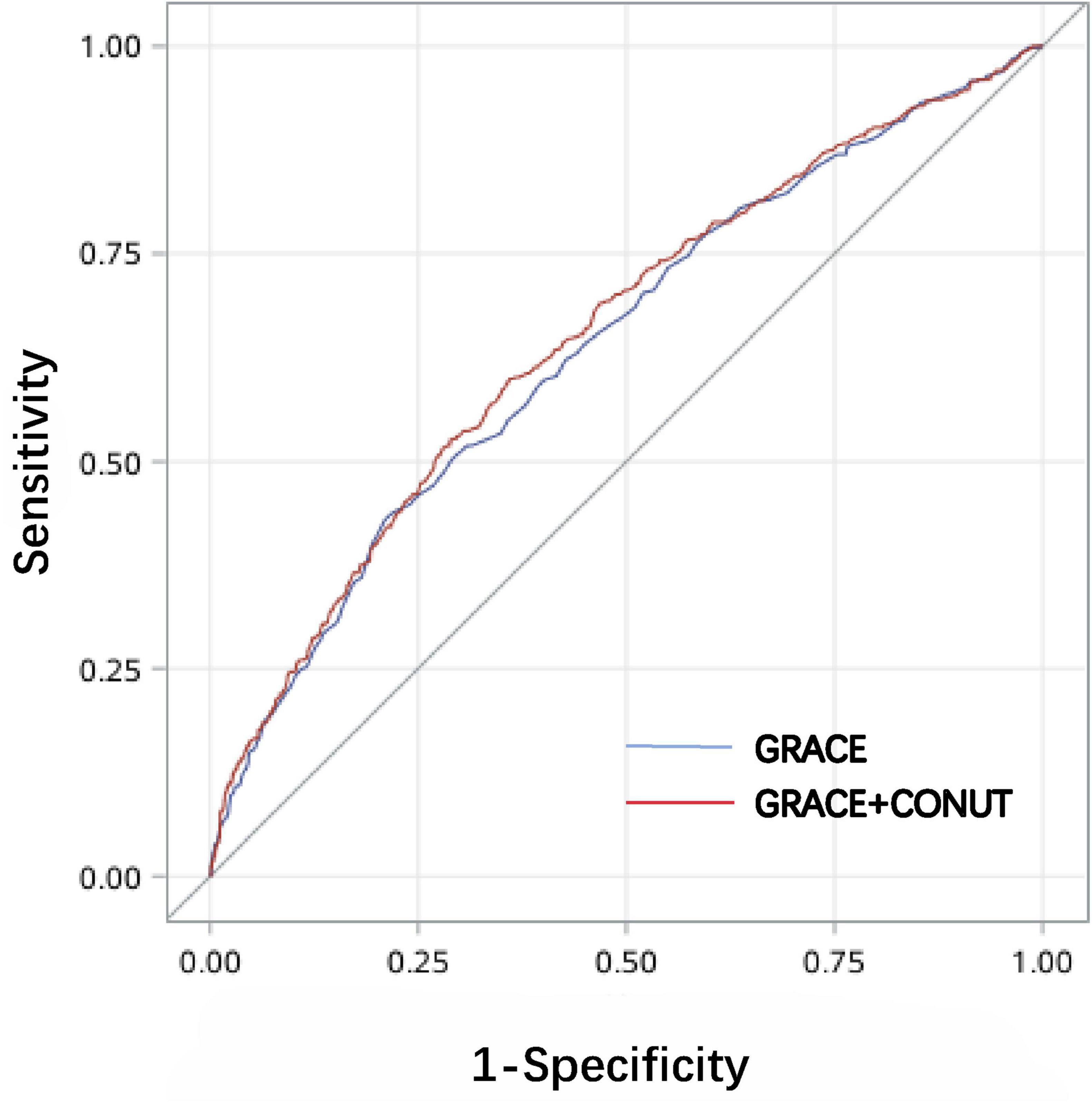
Figure 3. ROC curve analysis for both the GRACE risk score and the combined CONUT + GRACE risk score.

Table 3. Evaluating the effectiveness of the integrated the CONUT score alongside the GRACE risk Score for forecasting all-cause mortality.
4 Discussion
In the analysis conducted retrospectively, we observed that (1) patients suffering from AMI frequently experience malnutritional conditions, with our study revealing that nearly 48.5% of the patients experienced malnutrition, with 4.8% experienced moderate and severe malnutrition. (2) Malnutrition is an independent predictor of all-cause mortality in patients who underwent PCI after AMI, and the CONUT score, as a nutritional assessment tool, can assist in risk stratification. (3) The CONUT score can increase the prognostic value of the GRACE risk score for predicting all-cause mortality in AMI patients who underwent PCI. These aspects underscore the critical need for mitigating malnutrition risks and stress the importance of prompt intervention.
The incidence of malnutrition is very common among patients with AMI. Huang Y et al. found that malnutrition accounted for 53.8% in a cohort of 1180 AMI patients based on the PNI score (22). Basta G et al. showed that 55% of patients were malnourished in their evaluation of the nutritional status within a STEMI cohort (23). In our study, the prevalence of malnutrition was comparable to that reported in prior research. However, Wada et al. found that a significant proportion, approximately 20% of patients with coronary artery disease who underwent PCI were identified as being at high risk for malnutrition (24). Another study examined malnutrition prevalence in a group of 207 patients diagnosed with NSTEMI, uncovering a rate of 24.4% (25). The incidence of malnutrition in both studies was lower compared to our study. The potential reasons for this distinction may include different study population and different scoring system compared to our study.
Within our study cohort, it was observed that malnutrition independently contributed to all-cause mortality among patients who underwent PCI after AMI. Various previous investigations have also shown that malnutrition acts as an independent predictor of AMI when evaluated using different assessment methods. Li M et al. indicated that Prognostic Nutritional Index (PNI) was an independent predictor of long-term prognosis in elderly STEMI patients (26). Additionally, another study employed the Geriatric Nutrition Risk Index (GNRI) to gauge nutritional status, highlighting a notable connection between GNRI and unfavorable outcomes in AMI patients following PCI (27). Few studies have utilized the CONUT score to assess the relationship between malnutrition and the prognosis of patients who underwent PCI after AMI. PNI, GNRI, and CONUT score are widely recognized and commonly utilized nutritional assessment tools (28). We selected CONUT as the nutritional assessment tool for our study based on the findings of Raposeiras Roubín S et al., who evaluated the predictive value of PNI, GNRI, and CONUT for all-cause mortality and MACE in ACS patients. Their results suggested that the predictive capability of the CONUT score ranked the highest (29).
The GRACE risk score exhibits superior predictive performance for both in-hospital mortality and one-year mortality in patients with AMI (30). As AMI management and catheter devices have changed considerably since the establishment of the GRACE score, it is therefore important to develop a new scoring model for prospective risk stratification that is suitable for the current era of AMI management (31). Our research found that CONUT can improve the predictive efficiency of GRACE risk score. This may can be more effectively aid in the risk stratification of patients following PCI after AMI.
The pathophysiology of the relationship between high CONUT scores and poor clinical outcomes in AMI patients is not clearly known. The CONUT score is calculated based on the serum albumin, total cholesterol level and the lymphocyte count in the peripheral blood. The serum albumin has been confirmed by multiple studies as an indicator related to inflammation (32, 33). The activity of proinflammatory cytokines is contributed to the decrease in serum albumin levels (10, 34). On the other hand, atherosclerosis is increasingly recognized as a chronic inflammatory disease with an autoimmune component. A decrease in lymphocytes may cause immunosuppression in the patient, which can influence cardiac remodeling process after AMI and lead to poor prognosis (35–38). Meanwhile, the immune system primarily mediates its immune response by recognizing LDL antibodies, thereby generating oxidized LDL and triggering inflammation in the arterial wall (39). The above-mentioned evidence supports that the rationality of the CONUT score in assessing the prognosis of AMI patients, and indicates that there is an interaction and mutual promotion relationship between malnutrition, inflammation and immune response. All these findings strongly underscore the importance for physicians to incorporate malnutrition identification into their daily practice. Especially, patients with AMI are generally elderly, fragile patients with comorbidities. The CONUT score will provide important guidance for subsequent nutritional intervention measures. Shah B et al. indicates that dietary interventions can reduce high-sensitivity CRP level, which may have a beneficial effect on the prognosis of coronary heart disease (15). In the future, more well-designed experiments should be conducted to evaluate the specific effects of nutritional interventions on the prognosis of patients who underwent PCI after AMI.
Our study is subject to several limitations. Firstly, it was a single-center, retrospective study. All of our patients were of Chinese ethnicity, which may not reflect the prognosis observed in other ethnic groups, thereby limiting the general applicability of our findings. Secondly, we only utilized simple screening tools to assess nutritional status, without conducting direct comparisons with other well-established nutritional assessment tools, such as the Subjective Global Assessment and the Mini Nutritional Assessment. Furthermore, since the assessment of nutrition was carried out at just one point in time, it limited our ability to track the evolving nutritional conditions of the patients over the study period. Assessing long-term clinical outcomes using information collected at just one moment carries fundamental limitations. Besides, regarding medical therapy, we only conducted statistical analysis on the medication treatment of patients after discharge, without covering the medication situation before admission (such as the application of statins). This limitation may have a certain impact on the accuracy of cholesterol levels in the baseline data. Ultimately, while numerous clinically significant factors were incorporated in the multivariate evaluation, it is likely that unaccounted confounding variables still exist.
5 Conclusion
Malnutrition is prevalent among patients with AMI and is significantly associated with an increased incidence of all-cause mortality. The CONUT score, serving as a nutritional assessment tool, plays a key role in assisting with risk categorization and forecasting patients’ poor prognosis. The predictive capability of the GRACE risk score regarding all-cause mortality can be improved by incorporating the CONUT score. Early screening of malnutrition using the CONUT score can provide a foundation for guiding subsequent clinical nutritional interventions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
YS: Writing – original draft, Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Software. SH: Writing – review and editing, Data curation, Methodology, Project administration, Software, Supervision, SZ: Software, Methodology, Project administration, Writing – review and editing. YY: Methodology, Project administration, Software, Writing – review and editing. MW: Data curation, Project administration, Visualization, Writing – review and editing. ZS: Conceptualization, Writing – review and editing, Funding acquisition, Methodology, Project administration.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2025.1604470/full#supplementary-material
References
1. Grøsland M, Telle K, Øien H. Effect of hospital assignment on mortality for AMI patients. BMC Health Serv Res. (2023) 23:413. doi: 10.1186/s12913-023-09441-4
2. Lim S, Choo E, Choi I, Hwang Y, Lee K, Lee S, et al. Impact of the risk of malnutrition on bleeding, mortality, and ischemic events in patients with acute myocardial infarction. Nutr Metab Cardiovasc Dis. (2023) 33:65–74. doi: 10.1016/j.numecd.2022.10.009
3. Bueno H, Rossello X, Pocock S, Van de Werf F, Chin C, Danchin N, et al. In-hospital coronary revascularization rates and post-discharge mortality risk in Non-ST-Segment elevation acute coronary syndrome. J Am Coll Cardiol. (2019) 74:1454–61. doi: 10.1016/j.jacc.2019.06.068
4. Arero G, Arero A, Mohammed S, Vasheghani-Farahani A. Prognostic Potential of the Controlling Nutritional Status (CONUT) score in predicting all-cause mortality and major adverse cardiovascular events in patients with coronary artery disease: A meta-analysis. Front Nutr. (2022) 9:850641. doi: 10.3389/fnut.2022.850641
5. Xu D, Shen R, Hu M, Fan Q, Wu J. Prognostic impact of CONUT score in older patients with chronic heart failure. BMC Geriatr. (2024) 24:738. doi: 10.1186/s12877-024-05330-5
6. Clark A, Sze S. Impact of malnutrition using geriatric nutritional risk index in heart failure with preserved ejection fraction. JACC Heart Fail. (2019) 7:676–7. doi: 10.1016/j.jchf.2019.06.002
7. Li P, Li C, Mishra A, Cai P, Lu X, Sherif A, et al. Impact of malnutrition on in-hospital outcomes in takotsubo cardiomyopathy. Nutrition. (2022) 93:111495. doi: 10.1016/j.nut.2021.111495
8. Matsuo Y, Kumakura H, Kanai H, Iwasaki T, Ichikawa S. The geriatric nutritional risk index predicts long-term survival and cardiovascular or limb events in peripheral arterial disease. J Atheroscler Thromb. (2020) 27:134–43. doi: 10.5551/jat.49767
9. Söner S, Güzel T, Aktan A, Kılıç R, Arslan B, Demir M, et al. Predictive value of nutritional scores in non-valvular atrial fibrillation patients: Insights from the AFTER-2 study. Nutr Metab Cardiovasc Dis. (2025) 35:103794. doi: 10.1016/j.numecd.2024.103794
10. Henein M, Vancheri S, Longo G, Vancheri F. The role of inflammation in cardiovascular disease. Int J Mol Sci. (2022) 23:12906. doi: 10.3390/ijms232112906
11. Fonseca F, Izar M. Role of inflammation in cardiac remodeling after acute myocardial infarction. Front Physiol. (2022) 13:927163. doi: 10.3389/fphys.2022.927163
12. Libby P, Ridker P, Maseri A. Inflammation and atherosclerosis. Circulation. (2002) 105:1135–43. doi: 10.1161/hc0902.104353
13. Patel S, Celermajer D, Bao S. Atherosclerosis-underlying inflammatory mechanisms and clinical implications. Int J Biochem Cell Biol. (2008) 40:576–80. doi: 10.1016/j.biocel.2007.11.017
14. Stenvinkel P, Heimbürger O, Lindholm B, Kaysen G, Bergström J. Are there two types of malnutrition in chronic renal failure? Evidence for relationships between malnutrition, inflammation and atherosclerosis (MIA syndrome). Nephrol Dial Transplant. (2000) 15:953–60. doi: 10.1093/ndt/15.7.953
15. Shah B, Newman J, Woolf K, Ganguzza L, Guo Y, Allen N, et al. Anti-inflammatory effects of a vegan diet versus the American Heart Association-recommended diet in coronary artery disease trial. J Am Heart Assoc. (2018) 7:e011367. doi: 10.1161/JAHA.118.011367
16. Serón-Arbeloa C, Labarta-Monzón L, Puzo-Foncillas J, Mallor-Bonet T, Lafita-López A, Bueno-Vidales N, et al. Malnutrition screening and assessment. Nutrients. (2022) 14:2392. doi: 10.3390/nu14122392
17. Salinas M, Flores E, Blasco A, López-Garrigós M, Puche C, Asencio A, et al. CONUT: A tool to assess nutritional status. First application in a primary care population. Diagnosis. (2020) 8:373–6. doi: 10.1515/dx-2020-0073
18. Ignacio de Ulíbarri J, González-Madroño A, de Villar N, González P, González B, Mancha A, et al. CONUT: A tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. (2005) 20:38–45.
19. Levy M, Fink M, Marshall J, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med. (2003) 29:530–8. doi: 10.1007/s00134-003-1662-x
20. Thygesen K, Alpert J, Jaffe A, Chaitman B, Bax J, Morrow D, et al. Fourth Universal definition of myocardial infarction (2018). J Am Coll Cardiol. (2018) 72:2231–64. doi: 10.1016/j.jacc.2018.08.1038
21. Mitchell C, Rahko P, Blauwet L, Canaday B, Finstuen J, Foster M, et al. Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: Recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. (2019) 32:1–64. doi: 10.1016/j.echo.2018.06.004
22. Huang Y, Zhang Q, Li P, Chen M, Wang R, Hu J, et al. The prognostic nutritional index predicts all-cause mortality in critically ill patients with acute myocardial infarction. BMC Cardiovasc Disord. (2023) 23:339. doi: 10.1186/s12872-023-03350-4
23. Basta G, Chatzianagnostou K, Paradossi U, Botto N, Del Turco S, Taddei A, et al. The prognostic impact of objective nutritional indices in elderly patients with ST-elevation myocardial infarction undergoing primary coronary intervention. Int J Cardiol. (2016) 221:987–92. doi: 10.1016/j.ijcard.2016.07.039
24. Kanda D, Ikeda Y, Takumi T, Tokushige A, Sonoda T, Arikawa R, et al. Impact of nutritional status on prognosis in acute myocardial infarction patients undergoing percutaneous coronary intervention. BMC Cardiovasc Disord. (2022) 22:3. doi: 10.1186/s12872-021-02448-x
25. Lu J, Huang Z, Wang J, Zhao X, Yang Y, Wu B, et al. Prevalence and prognostic impact of malnutrition in critical patients with acute myocardial infarction: Results from Chinese CIN cohort and American MIMIC-III Database. Front Nutr. (2022) 9:890199. doi: 10.3389/fnut.2022.890199
26. Li M, Cai J, Jiang K, Li Y, Li S, Wang Q, et al. Prognostic nutritional index during hospitalization correlates with adverse outcomes in elderly patients with acute myocardial infarction: A single-center retrospective cohort study. Aging Clin Exp Res. (2024) 36:56. doi: 10.1007/s40520-024-02702-0
27. Abe H, Miyazaki T, Tomaru M, Nobushima Y, Ajima T, Hirabayashi K, et al. Poor nutritional status during recovery from acute myocardial infarction in patients without an early nutritional intervention predicts a poor prognosis: A single-center retrospective study. Nutrients. (2023) 15:4748. doi: 10.3390/nu15224748
28. Dent E, Hoogendijk E, Visvanathan R, Wright O. Malnutrition screening and assessment in hospitalised older people: A review. J Nutr Health Aging. (2019) 23:431–41. doi: 10.1007/s12603-019-1176-z
29. Raposeiras Roubín S, Abu Assi E, Cespón Fernandez M, Barreiro Pardal C, Lizancos Castro A, Parada J, et al. Prevalence and prognostic significance of malnutrition in patients with acute coronary syndrome. J Am Coll Cardiol. (2020) 76:828–40. doi: 10.1016/j.jacc.2020.06.058
30. Kawamura Y, Yoshimachi F, Murotani N, Karasawa Y, Nagamatsu H, Kasai S, et al. Comparison of mortality prediction by the GRACE score, multiple biomarkers, and their combination in all-comer patients with acute myocardial infarction undergoing primary percutaneous coronary intervention. Intern Med. (2023) 62:503–10. doi: 10.2169/internalmedicine.9486-22
31. Granger C, Goldberg R, Dabbous O, Pieper K, Eagle K, Cannon C, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. (2003) 163:2345–53. doi: 10.1001/archinte.163.19.2345
32. Eckart A, Struja T, Kutz A, Baumgartner A, Baumgartner T, Zurfluh S, et al. Relationship of nutritional status, inflammation, and serum albumin levels during acute illness: A prospective study. Am J Med. (2020) 133:713–22.e7. doi: 10.1016/j.amjmed.2019.10.031.
33. Doweiko J, Nompleggi D. The role of albumin in human physiology and pathophysiology, Part III: Albumin and disease states. JPEN J Parenter Enteral Nutr. (1991) 15:476–83. doi: 10.1177/0148607191015004476
34. Ross R. Atherosclerosis–an inflammatory disease. N Engl J Med. (1999) 340:115–26. doi: 10.1056/NEJM199901143400207
35. Kobiyama K, Ley K. Atherosclerosis. Circ Res. (2018) 123:1118–20. doi: 10.1161/CIRCRESAHA.118.313816
36. Pearson T, Mensah G, Alexander R, Anderson J, Cannon R, Criqui M, et al. Markers of inflammation and cardiovascular disease: Application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. (2003) 107:499–511. doi: 10.1161/01.cir.0000052939.59093.45
37. Girardot T, Rimmelé T, Venet F, Monneret G. Apoptosis-induced lymphopenia in sepsis and other severe injuries. Apoptosis. (2017) 22:295–305. doi: 10.1007/s10495-016-1325-3
38. Kologrivova I, Shtatolkina M, Suslova T, Ryabov V. Cells of the immune system in cardiac remodeling: Main players in resolution of inflammation and repair after myocardial infarction. Front Immunol. (2021) 12:664457. doi: 10.3389/fimmu.2021.664457
Keywords: malnutrition, CONUT, acute myocardial infarction, percutaneous coronary intervention, prognosis
Citation: Song Y, Han S, Zhang S, Yuan Y, Wang M and Sun Z (2025) Controlling Nutritional Status (CONUT) score for predicting all-cause mortality in patients who underwent percutaneous coronary intervention after acute myocardial infarction: a cohort study. Front. Nutr. 12:1604470. doi: 10.3389/fnut.2025.1604470
Received: 01 April 2025; Accepted: 13 June 2025;
Published: 08 July 2025.
Edited by:
Youhua Wang, Shanghai University of Traditional Chinese Medicine, ChinaReviewed by:
Yang Zou, Jiangxi Provincial People’s Hospital, ChinaSerdar Soner, Diyarbakır Gazi Yaşargil Training and Research Hospital, Türkiye
Copyright © 2025 Song, Han, Zhang, Yuan, Wang and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhaoqing Sun, c3Vuemhhb3FpbmdAdmlwLjE2My5jb20=
†These authors have contributed equally to this work
 Yang Song
Yang Song Su Han†
Su Han† Shiru Zhang
Shiru Zhang Zhaoqing Sun
Zhaoqing Sun