- School of Health Administration, Texas State University, San Marcos, TX, United States
Introduction: Food insecurity (FI) and social isolation (SI) are interconnected social determinants of health that disproportionately affect older adults. While FI and SI have been studied independently, their combined effects on malnutrition and quality of life (QoL) have not been adequately synthesized. This systematic review aimed to evaluate the efficacy of combined FI and SI interventions over the past decade, identify reported facilitators and barriers, and explore technology-based approaches to inform future research.
Methods: This study follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines and the Kruse Protocol. Peer-reviewed empirical studies were identified through systematic searches of PubMed, Web of Science, CINAHL, and ScienceDirect. Inclusion criteria targeted non-randomized controlled trials and community-based interventions focused on adults ≥ 65 years in the past 10 years. Six studies were examined using a narrative approach, supported by data matrices.
Results: The studies suggested a relationship between FI and SI, among individuals with physical impairment, low income, and reduced access to community resources. Women were most affected. Although the studies were observational and varied in quality, findings indicated that FI and SI are associated with adverse health outcomes, such as depression, diabetes, cognitive decline, and reduced QoL. Promising interventions included commensality programs, food service apps, and technology supported community engagement, though barriers such as limited digital literacy, high costs, and infrastructure gaps persist.
Conclusion: The review underscores the need for integrated interventions as the global older adult population grows. Due to limited methodological rigor, definitive conclusions cannot be drawn. Future research should use robust designs-randomized controlled trials, mixed methods, and longitudinal studies, and address structural barriers, including digital exclusion, to improve health outcomes.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD420250418740.
1 Introduction
While the consequences of both Food Insecurity (FI) and Social Isolation (SI) are known to have negative impacts on the physiological and psychological health of older adults age ≥ 65 years, the intersection of FI and SI is largely an unresearched area. FI is a problematic term to define. It can be described as a condition characterized by limited access to nutritious food, uncertain availability of food, and lack of socially acceptable means to obtain food (1). It also contributes to malnutrition, a condition that arises when a person’s diet lacks sufficient nutrients or contains too much of certain nutrients, leading to health problems (2, 3). SI is an objectively observable condition that exacerbates the psychosocial difficulties individuals experience due to a lack of social proximity and engagement, even if they do not subjectively feel lonely (4). The rising rate of FI combined with a higher risk of SI associated with increasing age disproportionately affects the quality of life of older adults (1) and can be addressed through nutrition support programs. For older adults, age-related physical comorbidities, the death or loss of friends and family, and impairments in cognition and sensory systems limit the frequency of social interaction. This in turn, reduces access to resources (5) information about quality food (6) and awareness of food services available within the community (7).
SI and FI are interrelated social determinants of health that frequently co-occur and influence one another, particularly in older adult populations. This relationship can be understood through an ecological or social determinants framework (8), which emphasizes that health outcomes are shaped by a dynamic interaction across multiple levels: individual, interpersonal, community, and societal. At the individual level, factors such as age, gender, race/ethnicity, income, education, health status (including depression, BMI, and limitations in daily activities), and length of time in the U.S. can directly influence an older adult’s vulnerability to both SI and FI. Moving to the interpersonal level, the presence or absence of emotional and financial support networks, such as family, friends, or caregivers can either buffer against or exacerbate the risks of isolation and limited food access. At the institutional level, access-related challenges—such as lack of private insurance, limited routine healthcare, and long travel distances to grocery stores—can further restrict food availability and deepen social disconnection. Community-level influences also play a significant role. Factors like rural versus urban residence, regional geographic differences, and the availability of community-based resources (e.g., meal delivery programs or senior centers) can support or hinder both social engagement and nutritional well-being. Finally, at the policy and societal level, broader structural elements, especially access to food assistance programs like the Supplemental Nutrition Assistance Program (SNAP), are crucial in shaping outcomes and reducing disparities related to SI and FI.
When considering FI, approximately 6.9 to 8.3% of the United States’ older adult population are at risk due to economic decline (9, 10). In fact, FI and malnutrition have associations with many diseases which affect older adults. More precisely, older adults experiencing FI not only have low nutrient intake, but also suffer from poor health, depression, diabetes, obesity, and functional limitations (11–13). Studies also posit that cognitive function can be negatively affected by FI and malnutrition (14–18). Furthermore, there is evidence that cardiometabolic risk may be present in those exposed to FI (19).
A population-level intervention addressing FI and SI for older adults would involve a policy or program designed to improve access to food, through community-based initiatives that simultaneously foster social connection and reduce feelings of isolation. These include community gardens, community kitchens, congregate meal programs, or social support networks linked to food distribution programs (20). Key elements of such intervention involve connecting people to resources such as screening for FI, providing referrals to food assistance programs, like Supplemental Nutrition Assistance Program (SNAP) proving free or low-cost meals, and building skills and confidence through nutrition education. These programs aim to enhance community food security and social support by implementing “check-in” systems within food distribution programs to ensure regular contact with vulnerable individuals. For older adults, partnering with local community centers or senior centers for food accessibility alongside social activities are effective as individuals connect while assisting with food distribution and consumption based upon culturally appropriate and local needs.
Some key interventions that attempt to address FI and SI in older adults include eating together or commensality, a health-promoting activity that contributes to improved health outcomes (21) with enhanced social support supplemented by dietary intake in multiple ways (22). Community-organized activities, such as Food Classes for Older Adults (FCOA), can provide sustainable commensality for homebound older adults who are often unable to cook for themselves (22.7%), those who are unable to shop for themselves (31.4%), and those who (14.6%) report money as a concern (23). When such programs are supported by apps or technology, they are more effective, as technology-based interventions such as mHealth provide the opportunity to stay socially connected (24) thus mitigating SI, and reducing the adverse impacts of FI (25).
Internet Food Delivery Applications (IFDA) are one way to mitigate the psychological issues of loneliness or depression and redress SI in older adults. Connecting to older adults, the service providers of IFDA optimize and enhance the nutrition status and deepen their understanding of how the issues of SI can factor into the pathophysiology of older adults as well. While services of this kind are common in some places of the United States, some regions are still in dire need. For example, in central Texas, there is a significant population of underserved, poor, insecure, malnourished, and socially isolated older adults (26, 27). Given that these measures are important social determinants (28) of health, programs that address these issues are necessary. Texas is ranked 44th in the United States for those aged 65 and older in poverty with an overall state poverty rate of 10% (26). With 33% Hispanic population, nearly 19% of the population aged 60 and older report food insecurity (29). The average malnutrition crude death rate in Texas is 65.6 per 100,000 before the COVID-19 pandemic based on 2014–2018 American Community Survey data (30), which worsened during the pandemic as malnutrition is a risk factor for COVID-19 mortality (29, 31).
The purpose of this systematic review was to identify and analyze the efficacy of combined SI and FI interventions for older adults over the past 10 years and analyze the facilitators and barriers in the published literature. We also attempted to review studies that implemented technology-based interventions and collected insights about FI and SI that might lead future researchers to additional interventions.
2 Materials and methods
2.1 Protocol and registration
This review was conducted in accordance with the Kruse Protocol (32) and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA, 2020) (33). The review is registered with PROSPERO (ID: CRD420250418740).
2.2 Inclusion and exclusion criteria
The criteria used to choose the articles for this systematic review consist of peer-reviewed empirical studies (non-clinical trials) and community programs/interventions that address FI, SI, or malnutrition with respect to the older adults ≥ 65 years old, over the last 10 years, regardless of geographic boundaries.
This study excluded randomized controlled trials (RTC), studies on interventions that targeted individuals < 65 years old, and systematic reviews published before 2012 (to prevent confounding results). This was done because systematic literature reviews already reported results from studies that may have been included in our analysis.
2.3 Information sources
Authors queried four databases: PubMed (MEDLINE), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Science, and ScienceDirect. These four databases were chosen because of their focus on health and nutrition research. Also, they are readily available to most researchers, and they are exhaustive in their content. MEDLINE was excluded from all but PubMed to help eliminate duplicates.
2.4 Search strategy
Starting with the key terms from the articles used in the introduction, a Boolean search string was created. We vetted these terms in the Medical Subject Headings (MeSH) of the U.S. Library of Medicine. Our final search string was: (“food insecurity” OR “nutrient insufficient” OR “food supply”) AND (“older adult” OR “elderly” OR “senior adult” OR “mature adult”) AND “social isolation.” We used the same search strategy in all databases and used similar filter strategies because not all databases utilize identical tools.
We included the term “intervention” in the Boolean search string: (“food insecurity” OR “nutrient insufficient” OR “food supply”) AND (“older adult” OR “elderly” OR “senior adult” OR “mature adult”) AND “intervention” AND “social isolation,” in our search for published articles within the last 10 years, and we could not find any articles (zero articles). It was only after we removed the term “intervention” that we were able get the 392 articles which the study was based upon. This shows the need for research regarding interventions in this area.
2.5 Selection process
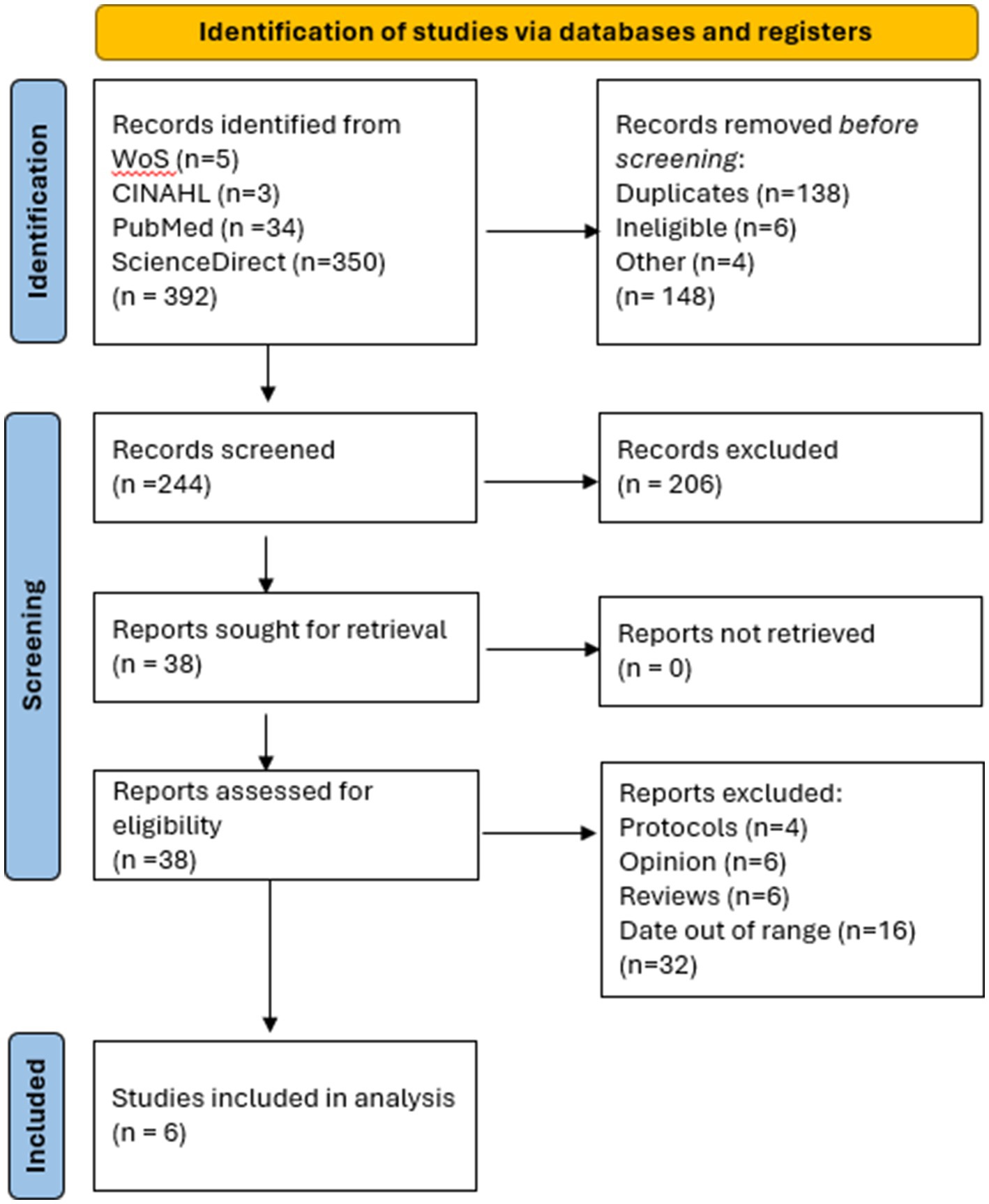
This study followed the Kruse Protocol for systematic literature that consists of a series of three consensus meetings among the authors. The first consensus meeting consists of finding the articles that met the inclusion criteria and assessed their relevance to the topic and calculating the Kappa statistic of agreement. The second consensus meeting involved summarizing articles using a literature matrix manager in Excel, which required searching for identical key terms across all databases. After conducting the searches and filtering the results (34), we screened the abstracts for relevance and calculated a kappa statistic to assess agreement. To ensure that each abstract was screened by at least two observers, the project leader assigned an agreed-upon workload. Thus, we created the flow diagram of study selection procedure (Figure 1) (33).
2.6 Data collection process
Data was extracted using an Excel spreadsheet standardized by the Kruse Protocol. We analyzed each article and grouped the observations. Weekly consensus meetings were used over a period of 7 months to ensure a continuity of process which included both the data extraction and full analysis steps.
2.7 Data items
Standard fields were collected, as identified by the Kruse Protocol: From the Google Scholar step, we collected date of publication, authors, study title, journal, impact factor from Journal Citation Reports, study design, key terms, experimental intervention, results, and comments from each reviewer; from the article filtering step, we collected the number of results before and after each filter applied in all four databases, the filters used, and the articles excluded by each filter. In the abstract screening step we collected database source (MEDLINE, CINAHL, Web of Science, and ScienceDirect), date of publication, authors, study title, journal, screening decision for each reviewer, notes about rejections, consensus meeting one, determination of screening decision, and a set of rejection criteria; Finally, in the analysis step we collected database source, date of publication, authors, study title, participants, experimental intervention, results compared with a control group, medical outcomes, study design, sample size, bias effect size, country of origin, statistics used, the strength and quality of evidence, effectiveness of intervention, general observations about FI and SI, facilitators to adoption, and barriers to adoption (32). Most of these fields are standardized on the Excel spreadsheet, but the last four items were specific to the research objective.
2.8 Effect measures
The preferred measure of effect was the Cohen d, however, the only measure of effect reported in the articles kept was the Odds Ratio. Because we accepted mixed methods and qualitative studies, we were unable to standardize summary measures, as would be performed in a meta-analysis. Measures of effect are summarized in tables for those studies in which it was reported. The kappa statistic was calculated and reported (35, 36).
2.9 Synthesis methods
The Kruse Protocol for conducting a systematic literature review typically includes a thematic analysis, commensurate with techniques used in the American Psychological Association (37). Observations were grouped into themes, and themes were organized into affinity matrices for further analysis.
2.10 Additional analyses and certainty assessment
During the data-extraction step, effect sizes were calculated and tabulated. We combined the observations and effect sizes for the certainty assessment. Themes and observations were sorted based on frequency in affinity matrices. This does not imply importance: this action only provides the probability of encountering a theme or observations in the group of articles selected for analysis.
3 Results
The flow diagram of study selection procedure (Figure 1) shows that a total of 392 results were provided by the four research databases from our search string, of which 138 were duplicates. A total of 244 articles were screened. Screening removed 206 results, leaving 38 full-text studies to be analyzed. A Cohen kappa was calculated from this process (k = 0.95, high agreement) (35, 36). During the analysis phase, an additional 32 studies were removed (not caught in the abstract screening process). This left 6 articles for full analysis.
3.1 Study characteristics
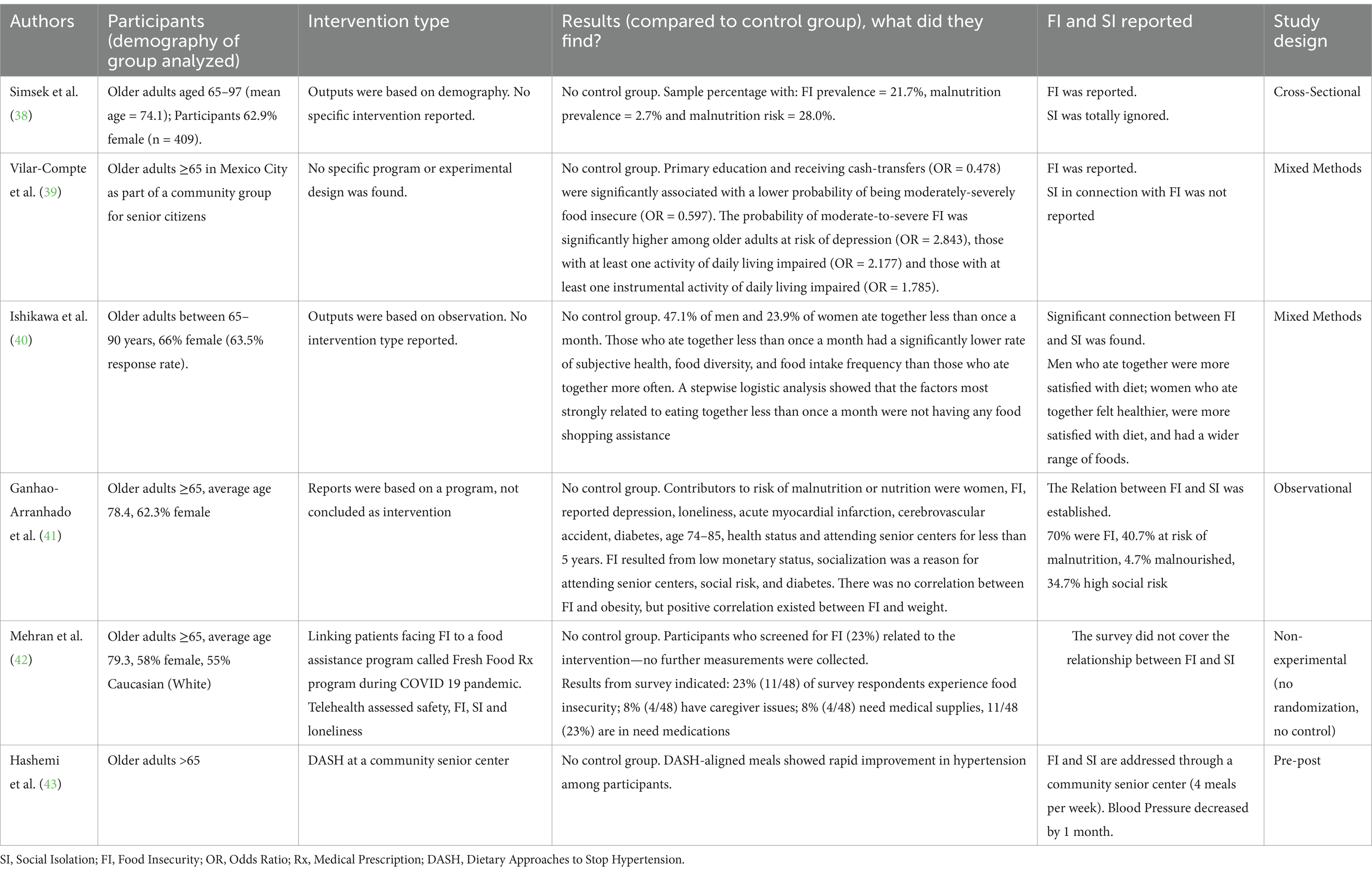
Following the PRISMA 2020 checklist, we extracted data fields for each study: participants, intervention, comparison (control or other group), outcomes, and study design or statistics (Table 1). We found six studies published in the following years: 2013 (38), 2016 (39), 2017 (40), 2018 (41), 2021 (42), and 2022 (43). All studies involved older adults (over 60 years), and all reported elements of FI, SI, or malnutrition. Table 1 summarizes the study characteristics in a manner established in the literature (44).
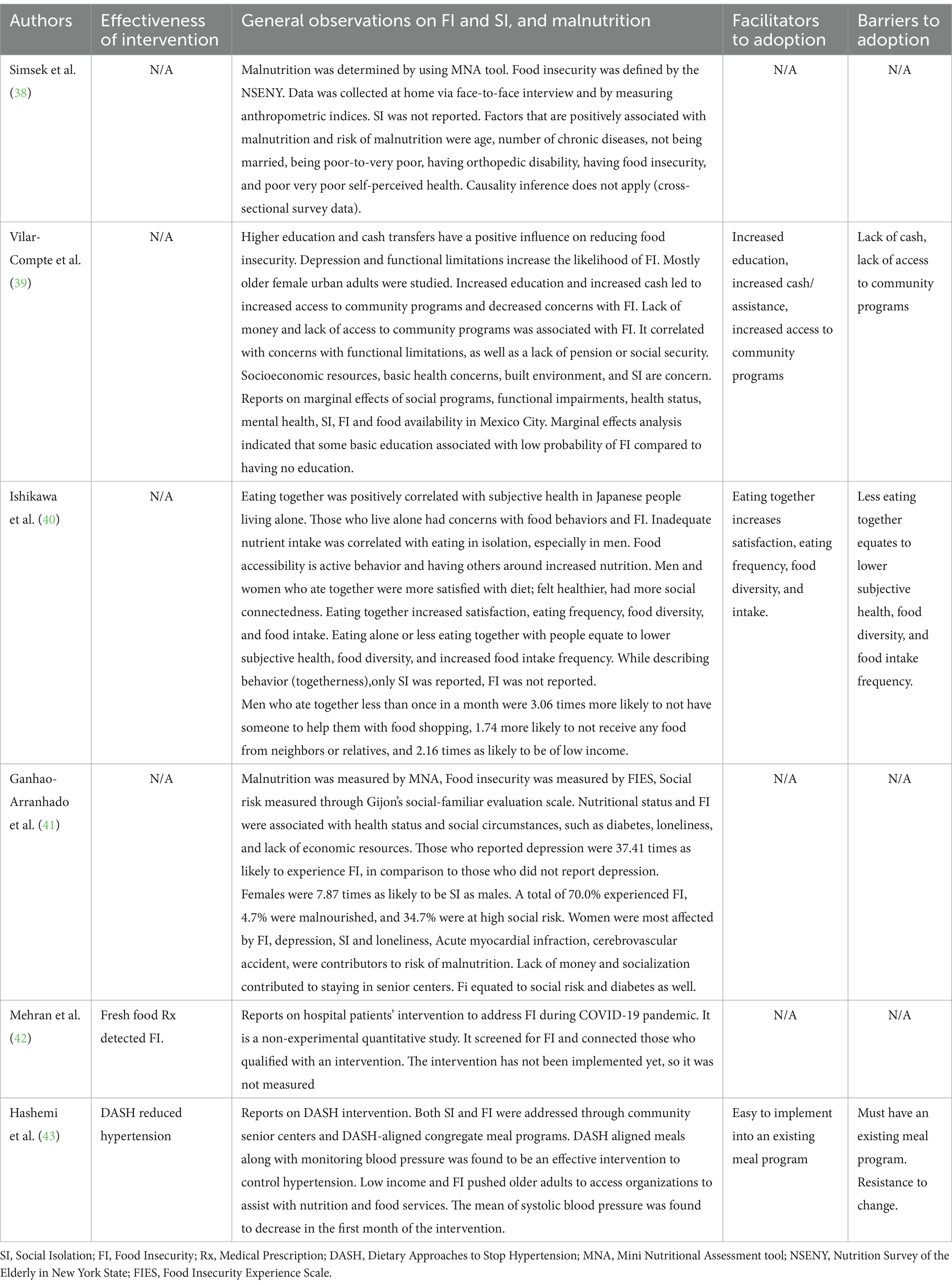
3.2 Results of individual studies
Reviewers recorded the observations in Table 2 from each article in accordance with the objective statement. Several studies in this review suggest an association between FI and SI, particularly noting that lack of access to community programs contributes to both limited food availability and reduced social support for older adults living alone with functional limitations and limited resources. People who ate together, which means people with social or community support, had less SI and more food security. A thematic analysis was conducted to make further sense of the information collected from the articles (37). Articles listed in this study used various themes to summarize the results and observations, but these themes did not always match the authors’ observations exactly. These themes can be seen in the affinity matrix in Table 3. The thematic analysis helps make sense of the data extracted. When an observation re-occurred, it became a theme. However, due to the small number of articles surrounding the topic, observations (themes without recurrence) were also included in the affinity matrix.
3.3 Risk of bias in studies and reporting of biases
The Johns Hopkins Nursing Evidence-Based Practice (JHNEBP) quality assessment tool (45) was used to evaluate bias and the overall quality of each study. The JHNEBP tool classifies strength of evidence in the following categories: Level I include randomized controlled trials; Level II include quasi-experimental studies without randomization; and Level III include observational and qualitative studies. Levels IV and V, include expert opinions, which were excluded from this review. To minimize the influence of bias on our findings, instances of bias were grouped and briefly analyzed, as bias can affect interpretation and generally limit external validity (46). The most common biases identified were sample bias (38, 39, 41–43), selection bias (38–43), and an affective health bias (42). Four of the six studies (38, 41–43) lacked intervention, and none included a control group, which weakens internal validity. Selection and affective health biases further threaten internal validity, while sample bias impacts external validity. Overall, the methodological limitations of these studies reduce the generalizability of their findings to broader populations.
The quality assessments showed that five out of six (83%) articles were level III non-experimental or qualitative studies, or meta-analyses. The quality of evidence showed that all six studies were level A (High), because the results were consistent, and the sample sizes were adequate.
3.4 Additional analysis and certainty of evidence
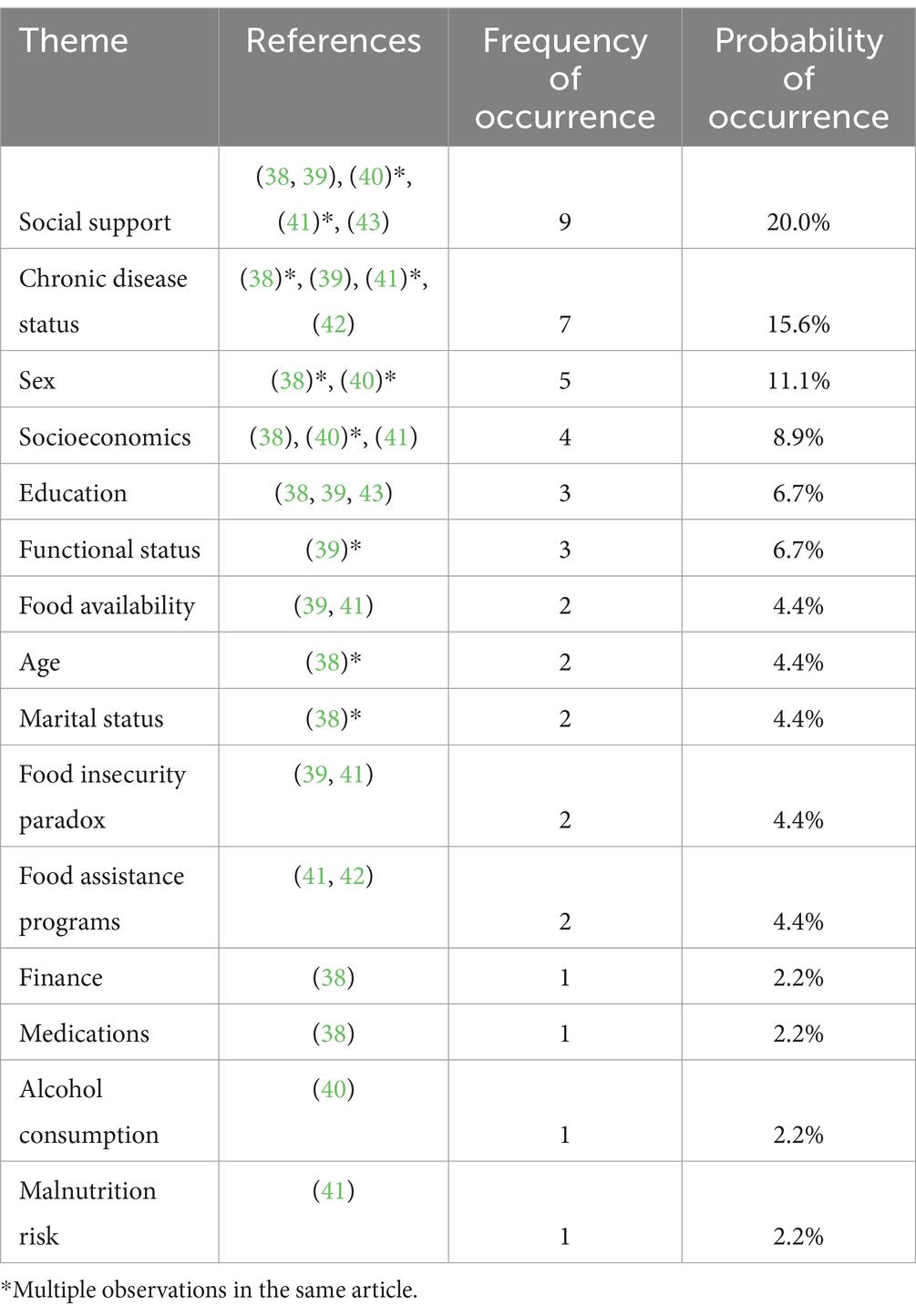
Table 3 summarizes the results of the observed thematic analysis: 11 themes and four individual observations were identified by the reviewers for a total of 45 occurrences in the literature.
In Table 3, the authors presented the descriptive statistics of the themes used in the reviewed studies. Of the 45 occurrences, nine (20%) identified social support as a factor (38–41, 43). Seven occurrences (15.6%) identified chronic disease status as a factor (38, 39, 41, 42). Five occurrences (11.1%) identified sex as a factor (40). Four occurrences (8.9%) identified socioeconomics as a factor (38, 40, 41). Three occurrences (6.7%) identified education as a factor (38, 39, 43). Three occurrences (6.7%) identified functional status as a factor. Physical limitations overall can lead to FI (39). Two occurrences (4.4%) identified food availability as a factor (38, 39). Two occurrences (4.4%) identified age as a factor (38). FI was identified to be highest in 60 + years individuals (38). Two occurrences (4.4%) identified the FI paradox as a factor (39, 41). Two occurrences (4.4%) identified food assistance programs as a factor (39, 42).
3.5 Interventions to address food insecurity and social isolation
Out of the six articles reviewed, only two interventions were identified (33%). The intervention of Fresh Food Rx linked patients facing FI to a food assistance program during the height of the COVID-19 pandemic through telehealth (42). The intervention of Dietary Approaches to Stop Hypertension (DASH) was used in community centers that served older adults (43). The DASH aligned meals found positive control of hypertension within one month (43).
4 Discussion
This systematic literature review examined six articles published over the past 10 years from five different countries, focusing on interventions addressing SI, FI, and malnutrition. The review reveals a significant gap in literature, as only six studies met the inclusion criteria. Notably, none of these studies employed a specific intervention model or utilized randomized controlled trials (RCTs), highlighting the limited evidence base in this area. The studies primarily relied on descriptive statistics and inferential analyses, including logistic regression and pre-test/post-test designs. The pre-post-test study consisted of a nutritional intervention to address blood pressure, FI, SI, and malnutrition using Dietary-Approach to-Stop-Hypertension (DASH) -based diet congregate meal program in community senior centers in New York City. The major objective of this intervention was to assess the effectiveness of DASH diet in lowering systolic blood pressure. The intervention was effective in lowering systolic blood pressure among DASH participants. Moreover, compared with individuals who did not experience FI, those who experienced FI reported higher systolic blood pressure (43).
Some validated instruments such as the Mini Nutritional Assessment survey was used to measure malnutrition levels, the Food Insecurity Experience Scale were used to assess FI, and Gijon’s social-familiar evaluation scale was used to measure social risk. These studies were conducted in different countries including Turkey (1 study) (38), Mexico (1 study) (39), Japan (1 study) (40), Portugal (1 study) (41), and the United States (2 studies) (42, 43). One of the articles from the U.S. was limited as it was a letter to the editor regarding an intervention to address FI among hospitalized patients during COVID-19 pandemic (42). The major findings from our review show that social factors and health status are the factors mostly associated with FI and malnutrition among older adults.
The social factors associated with FI consisted of being female, lack of money including pension and/or social security, lack of socialization, living alone loneliness, high level of social risk, low education level, and lack of access to community food programs (39, 41). The health-related factors associated with FI consisted of the presence of diabetes, depression, and physical impairment (41).
The social factors associated with malnutrition or the risk of malnutrition consisted of older age (≥ 70), being single, being a woman, being lonely and eating alone (not eating together with peers), poverty, and dealing with FI (38, 40, 41). The health status associated with malnutrition and/or risk of malnutrition consisted of poor health status and presence of chronic and acute diseases (depression, presence of orthopedic disability, acute myocardial infarction, and cerebrovascular accident) (38, 41).
None of the reviewed studies specifically targeted SI; however, by addressing FI and malnutrition, they implicitly engaged with aspects of SI. Although we anticipated identifying app-based food service interventions designed to address both FI and SI, none of the six studies employed mobile applications as a tool for meal delivery or social support. Most existing studies are cross-sectional and more appropriate for scoping reviews. Research on technology-based solutions for FI or SI is also limited, likely due to the complex challenges in public health, markets, and supply chains. An interdisciplinary approach combining public health, economics, and technology could help develop more effective, integrated interventions.
This systematic review has several limitations. First, although we queried four databases to reduce sampling bias, this approach yielded 138 duplicate articles, potentially reflecting overlapping coverage rather than expanding the diversity of sources. Second, the generalizability of the findings is limited. None of the studies were conducted across multiple countries, introducing selection bias and limiting global applicability. Furthermore, within-country generalizability is also constrained, as the study samples were not representative of the broader older adult populations in their respective nations. Third, five of the six studies exhibited sampling bias, with a predominance of female participants. Finally, methodological limitations, particularly the absence of randomized controlled trials (RCTs), mixed methods approach, and longitudinal data pose significant concerns regarding internal and external validity. These limitations restrict the extent to which the reviewed interventions can be confidently applied to the older adult populations.
Although our systematic review is based on six articles, it is a valuable review because it underscores the need for gold standards in research, randomized controlled trials (RCTs) using robust experiments to assess the effectiveness of interventions to address SI, FI, or malnutrition affecting the QoL of older adults. While RCTs focus on specific outcomes they may not capture the overall impact of an intervention, particularly where existing confounding variables like human behavior require holistic examination. Observational studies or non-randomized controlled trials in the form of cohort studies, case studies, or longitudinal research provide such insights into real-world applicability and scalability.
A notable gap in literature remains, as many technology-based interventions report only short-term impacts and are often tested on homogenous groups, limiting their relevance to diverse populations (47). Future research should employ longitudinal designs to evaluate the sustained effects of these interventions on FI and SI over time. Moreover, existing studies frequently neglect key behavioral and psychosocial indicators—such as social connectedness, mental health, and self-efficacy—that are closely tied to both challenges (48). Using validated scales for depression, loneliness, and perceived social support alongside food security measures would allow for a more comprehensive understanding of outcomes (49). Additionally, assessing technological barriers such as device availability, internet access, and user interface challenges is essential. Current evaluations often rely heavily on quantitative metrics like app usage or survey data, missing the nuanced, long-term behavioral shifts that digital interventions may produce (50). Comparative analysis of various approaches such as mobile apps, online forums, and telemedicine can further inform best practices and guide the integration of technology into public health strategies to more effectively and equitably address the intertwined issues of FI and SI.
Digital literacy also plays a vital role in addressing the overlapping challenges of SI and FI, in older adults, but significant barriers remain in the form of limited digital proficiency in older adults. Many lack the knowledge to navigate essential online platforms for food assistance programs like SNAP or WIC and cannot easily participate in telehealth services or virtual social activities (51). Cost is another major obstacle, as fixed incomes for older adults often make internet service, devices, and up-to-date technology unaffordable (52). Moreover, physical limitations, such as impaired vision or reduced mobility, and the absence of reliable broadband in rural or underserved areas further restrict digital access (53). To address these challenges, community-based initiatives have begun integrating food engagement with digital support. Programs such as virtual communal meals, online cooking classes, and recipe sharing platforms promote commensality, the shared experience of eating together, which enhances emotional and social well-being. Some holistic approaches that foster digital inclusion while meeting both nutritional and social needs include Commons Table, senior center tech workshops, library digital training, and device donation programs. However, large-scale technological solutions often fall short in addressing the specific needs of marginalized or underserved populations.
As the market for food production and distribution is often fragmented, with many players in the food supply chain with myriad interest; cost, accessibility, or infrastructure, particularly in low-resource settings, makes it difficult for developing advanced technology or food distribution innovations. Traditionally, public health research has focused on understanding the social, behavioral, and epidemiological aspects of FI and malnutrition, often relying on policy interventions or community-based solutions (54). Technologies that aim to address these issues may need to manage sensitive personal data, such as health and nutrition information. This raises concerns about privacy, consent, and ethical considerations, which could deter both research and technological development in this area.
5 Conclusion
FI, SI, and malnutrition are frequently associated with poorer outcomes in older adults and highlight the need for further research to clarify causal pathways and the extent of impact. Based on this systematic review, there has been a lack of interventions addressing these three issues simultaneously. Moreover, there is a need for conducting a scoping review that synthesizes information about the barriers and facilitators to improving food security and decreasing SI in older adults. A scoping review might suggest factors for consideration in developing potential interventions and by using a broader search criterion to capture all relevant information. Additionally, while technology could be leveraged to facilitate food delivery, to our knowledge, no app-based interventions have been published. We urge more technology-driven solutions to address these key challenges faced by older adults.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
KS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. CK: Formal analysis, Methodology, Software, Writing – review & editing. MM: Writing – review & editing. ZR: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Xiao, Y, Yin, S, Bai, Y, Wang, J, Cui, J, Yang, Y, et al. A positive association between food insecurity and the prevalence of overactive bladder in US adults. Front Nutr. (2024) 10:1329687. doi: 10.3389/fnut.2023.1329687
2. Zheng, P, Wang, B, Luo, Y, Duan, R, and Feng, T. Research progress on predictive models for malnutrition in cancer patients. Front Nutr. (2024) 11:1438941. doi: 10.3389/fnut.2024.1438941
3. Ryan, CH, Morgan, C, Malacarne, JG, and Belarmino, EH. An asset-based examination of contextual factors influencing nutrition security: The case of rural northern New England. Nutrients. (2025) 17:295. doi: 10.3390/nu17020295
4. Sen, K, Prybutok, G, and Prybutok, V. The use of digital technology for social wellbeing reduces social isolation in older adults: a systematic review. SSM-Popul Health. (2021) 17:101020. doi: 10.1016/j.ssmph.2021.101020
5. Yodmai, K, Somrongthong, R, Nanthamongkolchai, S, and Suksatan, W. Effects of the older family network program on improving quality of life among older adults in Thailand. J Multidiscip Healthc. (2021) 14:1373–83. doi: 10.2147/JMDH.S315775
6. Ryan, AM, Prado, CM, Sullivan, ES, Power, DG, and Daly, LE. Effects of weight loss and sarcopenia on response to chemotherapy, quality of life, and survival. Nutrition. (2019) 67-68:110539. doi: 10.1016/j.nut.2019.06.020
7. Saredakis, D, Keage, HA, Corlis, M, Ghezzi, ES, Loffler, H, and Loetscher, T. The effect of reminiscence therapy using virtual reality on apathy in residential aged care: multisite nonrandomized controlled trial. J Med Internet Res. (2021) 23:e29210. doi: 10.2196/29210
8. Goldberg, SL, and Mawn, BE. Predictors of food insecurity among older adults in the United States. Public Health Nurs. (2015) 32:397–407. doi: 10.1111/phn.12173
9. Coleman-Jensen, A, Rabbitt, MP, Gregory, CA, and Singh, A. Statistical supplement to household food security in the United States in 2020 (2021).
10. Vaudin, AM, Moshfegh, AJ, and Sahyoun, NR. Measuring food insecurity in older adults using both physical and economic food access, NHANES 2013–18. J Nutr. (2022) 152:1953–62. doi: 10.1093/jn/nxac058
11. Pengpid, S, Peltzer, K, and Anantanasuwong, D. Bidirectional association between probable depression and multimorbidity among middle-aged and older adults in Thailand. J Multidiscip Healthc. (2023) 16:11–9. doi: 10.2147/JMDH.S394078
12. Gundersen, C, and Ziliak, JP. Food insecurity and health outcomes. Health Aff. (2015) 34:1830–9. doi: 10.1377/hlthaff.2015.0645
13. Saenz, JL, Kessler, J, and Nelson, E. Food insecurity across the life-course and cognitive function among older Mexican adults. Nutrients. (2022) 14:1462. doi: 10.3390/nu14071462
14. Frith, E, and Loprinzi, PD. Food insecurity and cognitive function in older adults: brief report. Clin Nutr. (2018) 37:1765–8. doi: 10.1016/j.clnu.2017.07.001
15. Gao, X, Scott, T, Falcon, LM, Wilde, PE, and Tucker, KL. Food insecurity and cognitive function in Puerto Rican adults. Am J Clin Nutr. (2009) 89:1197–203. doi: 10.3945/ajcn.2008.26941
16. Na, M, Dou, N, Ji, N, Xie, D, Huang, J, Tucker, KL, et al. Food insecurity and cognitive function in middle to older adulthood: a systematic review. Adv Nutr (Bethesda, MD). (2020) 11:667–76. doi: 10.1093/advances/nmz122
17. Portela-Parra, ET, and Leung, CW. Food insecurity is associated with lower cognitive functioning in a national sample of older adults. J Nutr. (2019) 149:1812–7. doi: 10.1093/jn/nxz120
18. Wong, JC, Scott, T, Wilde, P, Li, Y-G, Tucker, KL, and Gao, X. Food insecurity is associated with subsequent cognitive decline in the Boston Puerto Rican health study. J Nutr. (2016) 146:1740–5. doi: 10.3945/jn.115.228700
19. Miguel, ES, Lopes, SO, Araújo, SP, Priore, SE, Alfenas, RCG, and Hermsdorff, HHM. Association between food insecurity and cardiometabolic risk in adults and the elderly: a systematic review. J Glob Health. (2020) 10:020402. doi: 10.7189/jogh.10.020402
20. Ahn, H, Kim, DW, Ko, Y, Ha, J, Shin, YB, Lee, J, et al. Updated systematic review and meta-analysis on diagnostic issues and the prognostic impact of myosteatosis: a new paradigm beyond sarcopenia. Ageing Res Rev. (2021) 70:101398. doi: 10.1016/j.arr.2021.101398
21. do Nascimento, LA, MJR, A, Golin, N, Suíter, E, Morinaga, CV, Avelino Silva, TJ, et al. Nutritional status predicts functional recovery and adverse outcomes in older adults: a prospective cohort study. J Cachexia Sarcopenia Muscle. (2025) 16:e13819. doi: 10.1002/jcsm.13819
22. Allen-Perkins, D, Rivero Jiménez, B, López-Lago Ortiz, L, Conde Caballero, D, and Mariano, JL. The impact of loneliness and social isolation on dietary choices and practices among older adults: a systematic review of qualitative and mixed-methods research. J Popul Ageing. (2024):1–35. doi: 10.1007/s12062-024-09475-4
23. Zarei, M, Qorbani, M, Djalalinia, S, Sulaiman, N, Subashini, T, Appanah, G, et al. Food insecurity and dietary intake among elderly population: a systematic review. Int J Prev Med. (2021) 12:8. doi: 10.4103/ijpvm.IJPVM_61_19
24. Sen, K, Laheji, N, Ramamonjiarivelo, Z, Renick, C, Osborne, R, and Beauvais, B. Examining the Effect of Contactless Intergenerational Befriending Intervention on Social Isolation Among Older Adults and Students’ Attitude Toward Companionship: Content Analysis. JMIR Aging. (2023) 7:e47908. doi: 10.2196/47908
25. Gomes, LA, Gregório, MJ, Iakovleva, TA, Sousa, RD, Bessant, J, Oliveira, P, et al. A home-based eHealth intervention for an older adult population with food insecurity: feasibility and acceptability study. J Med Internet Res. (2021) 23:e26871. doi: 10.2196/26871
26. Bergeron, C, John, J, Sribhashyam, M, Odonkor, G, Oloruntoba, O, Merianos, A, et al. County-level characteristics driving malnutrition death rates among older adults in Texas. J Nutr Health Aging. (2021) 25:862–8. doi: 10.1007/s12603-021-1626-2
27. Lengfelder, L, Mahlke, S, Moore, L, Zhang, X, Williams, G III, and Lee, J. Prevalence and impact of malnutrition on length of stay, readmission, and discharge destination. J Parenter Enter Nutr. (2022) 46:1335–42. doi: 10.1002/jpen.2322
28. Turner, A, LaVeist, ATA, Richard, P, and Gaskin, DJ. Economic impacts of health disparities in Texas 2020. Available at: https://www.episcopalhealth.org/wp-content/uploads/2021/01/Econ-Impacts-of-Health-Disparities-Texas-2020-FINAL-002.pdf (2021).
29. Nhim, V, Bencomo-Alvarez, AE, Dwivedi, AK, Gadad, SS, and Eiring, AM. Abstract PO-200: border differences on breast cancer incidence and survival between non-Hispanic white and Hispanic patients: a Texas population-based study. Cancer Epidemiol Biomarkers Prev. (2022) 31:PO-200. doi: 10.1158/1538-7755.DISP21-PO-200
30. Bauer, C, Zhang, K, Lee, M, Fisher-Hoch, S, Guajardo, E, McCormick, J, et al. Census tract patterns and contextual social determinants of health associated with COVID-19 in a Hispanic population from South Texas: a spatiotemporal perspective. JMIR Public Health Surveill. (2021) 7:e29205. doi: 10.2196/29205
31. Snider, JT, Linthicum, MT, Wu, Y, LaVallee, C, Lakdawalla, DN, Hegazi, R, et al. Economic burden of community-based disease-associated malnutrition in the United States. J Parenter Enter Nutr. (2014) 38:77S–85S. doi: 10.1177/0148607114550000
32. Kruse, CS. Writing a systematic review for publication in a health-related degree program. JMIR Res Protoc. (2019) 8:e15490. doi: 10.2196/15490
33. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 Statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
34. Kruse, C, Fohn, J, Wilson, N, Patlan, EN, Zipp, S, and Mileski, M. Utilization barriers and medical outcomes commensurate with the use of telehealth among older adults: systematic review. JMIR Med Inform. (2020) 8:e20359. doi: 10.2196/20359
35. Light, RJ. Measures of response agreement for qualitative data: some generalizations and alternatives. Psychol Bull. (1971) 76:365–77. doi: 10.1037/h0031643
36. McHugh, ML. Interrater reliability: the kappa statistic. Biochem Med. (2012) 22:276–82. doi: 10.11613/BM.2012.031
37. Braun, V, and Clarke, V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
38. Simsek, H, Meseri, R, Sahin, S, and Ucku, R. Prevalence of food insecurity and malnutrition, factors related to malnutrition in the elderly: a community-based, cross-sectional study from Turkey. Eur Geriatric Med. (2013) 4:226–30. doi: 10.1016/j.eurger.2013.06.001
39. Vilar-Compte, M, Martínez-Martínez, O, Orta-Alemán, D, and Perez-Escamilla, R. Functional limitations, depression, and cash assistance are associated with food insecurity among older urban adults in Mexico City. J Health Care Poor Underserved. (2016) 27:1537–54. doi: 10.1353/hpu.2016.0130
40. Ishikawa, M, Takemi, Y, Yokoyama, T, Kusama, K, Fukuda, Y, Nakaya, T, et al. "Eating together" is associated with food behaviors and demographic factors of older Japanese people who live alone. J Nutr Health Aging. (2017) 21:662–72. doi: 10.1007/s12603-016-0805-z
41. Ganhão-Arranhado, S, Paúl, C, Ramalho, R, and Pereira, P. Food insecurity, weight and nutritional status among older adults attending senior centres in Lisbon. Arch Gerontol Geriatr. (2018) 78:81–8. doi: 10.1016/j.archger.2018.06.004
42. Mehran, NA, Ferris, C, Yang, M, and Zimmer, RP. Calling all house call patients: an intervention for older adults during the COVID-19 pandemic. J Am Geriatr Soc. (2021) 69:600–1. doi: 10.1111/jgs.16998
43. Hashemi, A, Vasquez, K, Guishard, D, Naji, M, Ronning, A, George-Alexander, G, et al. Implementing DASH-aligned congregate meals and self-measured blood pressure in two senior centers: an open label study. Nutr Metab Cardiovasc Dis. (2022) 32:1998–2009. doi: 10.1016/j.numecd.2022.05.018
44. Kruse, C, and Heinemann, K. Facilitators and barriers to the adoption of telemedicine during the first year of COVID-19: systematic review. J Med Internet Res. (2022) 24:e31752. doi: 10.2196/31752
45. Newhouse, R, Dearholt, S, Poe, S, Pugh, LC, and White, KM. Evidence-based practice: a practical approach to implementation. J Nurs Adm. (2005) 35:35–40. doi: 10.1097/00005110-200501000-00013
46. Pannucci, CJ, and Wilkins, EG. Identifying and avoiding bias in research. Plast Reconstr Surg. (2010) 126:619–25. doi: 10.1097/PRS.0b013e3181de24bc
47. Yap, JM, Tantono, N, Wu, VX, and Klainin-Yobas, P. Effectiveness of technology-based psychosocial interventions on diabetes distress and health-relevant outcomes among type 2 diabetes mellitus: a systematic review and meta-analysis. J Telemed Telecare. (2024) 30:262–84. doi: 10.1177/1357633X211058329
48. Preston, AJ, and Rew, L. Connectedness, self-esteem, and prosocial behaviors protect adolescent mental health following social isolation: a systematic review. Issues Ment Health Nurs. (2022) 43:32–41. doi: 10.1080/01612840.2021.1948642
49. Gallegos, D, Eivers, A, Sondergeld, P, and Pattinson, C. Food insecurity and child development: a state-of-the-art review. Int J Environ Res Public Health. (2021) 18:8990. doi: 10.3390/ijerph18178990
50. Thomas Craig, KJ, Morgan, LC, Chen, C-H, Michie, S, Fusco, N, Snowdon, JL, et al. Systematic review of context-aware digital behavior change interventions to improve health. Transl Behav Med. (2021) 11:1037–48. doi: 10.1093/tbm/ibaa099
51. Vasan, A, Kenyon, CC, Roberto, CA, Fiks, AG, and Venkataramani, AS. Association of remote vs in-person benefit delivery with WIC participation during the COVID-19 pandemic. JAMA. (2021) 326:1531–3. doi: 10.1001/jama.2021.14356
52. Chan, DYL, Lee, SWH, and Teh, P-L. Factors influencing technology use among low-income older adults: a systematic review. Heliyon. (2023) 9:e20111. doi: 10.1016/j.heliyon.2023.e20111
53. Hambly, H, and Rajabiun, R. Rural broadband: gaps, maps and challenges. Telematics Inform. (2021) 60:101565. doi: 10.1016/j.tele.2021.101565
Keywords: food insecurity, social isolation, malnutrition, technology, intervention
Citation: Sen K, Kruse CS, Mileski M and Ramamonjiarivelo Z (2025) Interventions to reduce social isolation and food insecurity in older adults: a systematic review. Front. Nutr. 12:1607057. doi: 10.3389/fnut.2025.1607057
Edited by:
Florencia Ceriani, Universidad de la República, UruguayReviewed by:
Shashi Kant Bhatia, Konkuk University, Republic of KoreaDaniel Simancas, Universidad UTE, Ecuador
Copyright © 2025 Sen, Kruse, Mileski and Ramamonjiarivelo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Keya Sen, a2V5YXNlbkB0eHN0YXRlLmVkdQ==
†ORCID: Keya Sen, orcid.org/0000-0002-4013-8835
Clemens Scott Kruse, orcid.org/0000-0002-7636-1086
Michael Mileski, orcid.org/0000-0003-1503-6869
Zo Ramamonjiarivelo, orcid.org/0000-0001-5756-3582
 Keya Sen
Keya Sen Clemens Scott Kruse†
Clemens Scott Kruse† Zo Ramamonjiarivelo
Zo Ramamonjiarivelo