- Department of Nutrition, Dietetics, and Food Sciences, Utah State University, Logan, UT, United States
Background: Dietary acculturation—the process by which migrants adopt the dietary patterns of their host country—has become increasingly relevant given the unprecedented scale of international migration. This phenomenon is often associated with a shift from traditional diets toward host-country patterns that are higher in ultra processed foods, added sugars, and fats, with potential implications for chronic disease risk.
Objective: This mini-review aims to synthesize global evidence on the dietary transformations experienced by migrant populations and to assess the health implications and modulating factors influencing these changes.
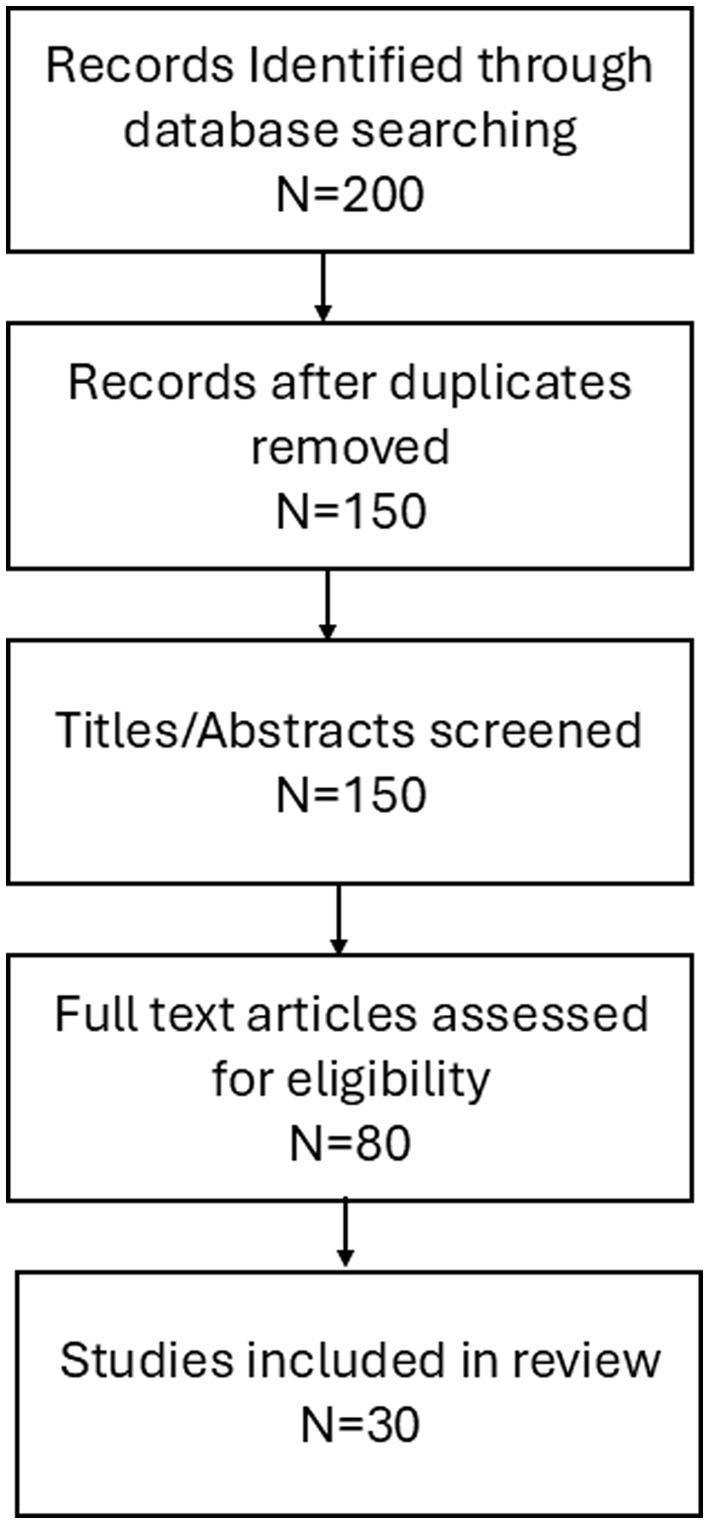
Methods: A targeted literature search was conducted in PubMed, Scopus, and Web of Science for articles published between January 2000 and April 2024, using keywords related to dietary acculturation, migration, and health outcomes. After applying inclusion and exclusion criteria, 30 studies directly addressing dietary change and health outcomes post-migration were included. Key themes were identified through iterative synthesis.
Results: Evidence indicates a consistent trend of dietary acculturation across diverse migrant groups, typically involving increased consumption of energy-dense, processed foods (a 15–20% increase) and decreased intake of traditional staples such as whole grains (down by 10–15%), pulses, and fresh vegetables. These dietary shifts are associated with a heightened risk of obesity (increasing by 5–10%), type 2 diabetes (7–12% rise), and cardiovascular diseases. Factors such as length of residence (1–5 years), age at migration (20–30 years), socioeconomic status (bottom 20%), food environment (availability dropping by 30%), and health literacy significantly modulate these changes. Emerging evidence also points to changes in gut microbiota as a consequence of dietary transformation.
Conclusion: Dietary acculturation among migrant populations is a multifaceted process that increases the risk of nutrition-related chronic diseases. There is a critical need for culturally sensitive public health interventions and policies that support the preservation of healthy traditional diets while facilitating healthy adaptation to new food environments. Addressing research gaps—such as longitudinal data and the experiences of underrepresented migrant groups—will strengthen strategies to mitigate adverse health outcomes.
Introduction
International migration is a complex process affecting individuals’ daily lives, social structures, and health behaviors, including dietary patterns. As of 2020, over 281 million people lived outside their country of birth, underscoring the global relevance of understanding how migration influences health and nutrition (1, 2). A consistent finding across epidemiological and public health research is that dietary habits often undergo substantial transformation following migration. Migrants frequently shift from traditional diets—rich in whole grains, legumes, fruits, and vegetables—to eating patterns characterized by higher intakes of processed foods, added sugars, and saturated fats (2, 3, 4). For example, some migrant groups experience a 20–40% reduction in the consumption of traditional staples and a 30% increase in processed food intake within a decade of resettlement (2, 4, 5). These changes are frequently linked to increased rates of obesity, type 2 diabetes, and cardiovascular disease; prevalence rates for these conditions are 1.5 to 2 times higher among migrants after acculturation compared to their pre-migration status or host-country natives (6, 7). The drivers of these dietary shifts are multifactorial and include socioeconomic constraints, the food environment, acculturation pressures, and changes in time allocation and occupational demands (2). Figure 1 presents a conceptual framework illustrating how demographic factors, health outcomes, the food environment, and socioeconomic factors interact to shape dietary transitions and health risks among migrant populations.
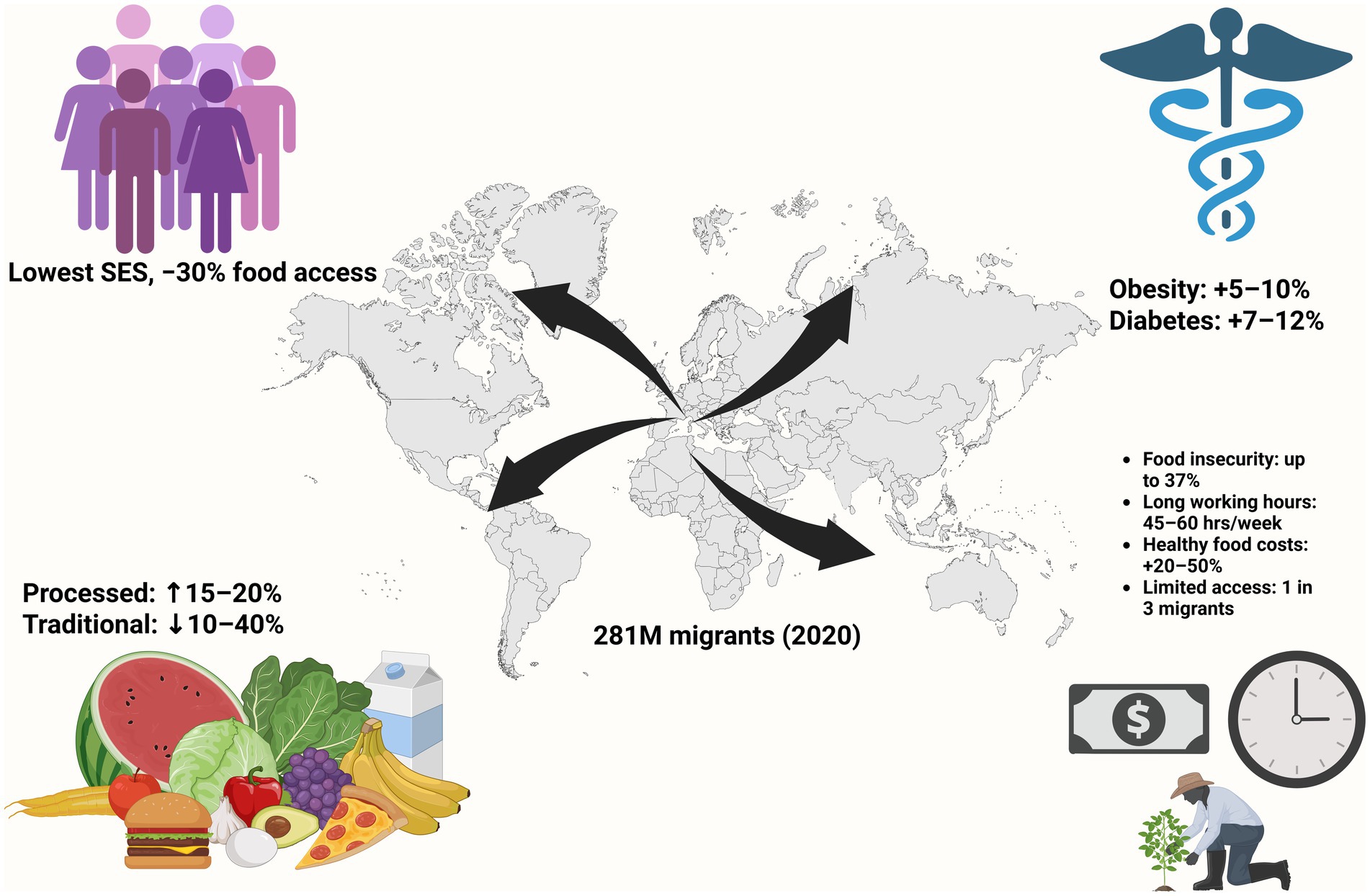
Figure 1. Conceptual framework illustrating the drivers and consequences of dietary acculturation in migrant populations. SES, socioeconomic status. Created in BioRender. Van Vliet, S. (2025) https://BioRender.com/ghtni6q.
Despite the growing body of literature, significant research gaps remain, including a lack of longitudinal data, limited representation of refugees and undocumented migrants, and insufficient focus on structural determinants such as food security and health literacy (8–11). Most existing reviews focus on high-income host countries, leaving a knowledge gap regarding dietary acculturation in low- and middle-income settings and among diverse migration contexts (6, 9, 12, 13). To address these limitations, future research should adopt interdisciplinary approaches, integrate qualitative and quantitative data, and employ community-based participatory research methods to develop culturally tailored interventions that promote healthy eating behaviors among migrant populations. Dietary acculturation has significant impacts on migrant health, with ultra processed food adoption driving increased chronic disease risk (14). The objective of this mini-review is to synthesize current global evidence on the patterns and determinants of dietary acculturation among migrant populations. By integrating data across continents, migrant groups, and study designs, this review highlights the health consequences of dietary transitions, identifies key modulating factors, and discusses emerging areas such as gut microbiota and mental health. The review also provides a conceptual framework to guide future research and inform culturally sensitive public health interventions aimed at preserving healthy dietary practices in migrant communities.
Methods
A focused review of existing literature was undertaken to consolidate evidence pertaining to dietary acculturation and its effects on the health of migrant populations. Searches were conducted in PubMed, Scopus, and Web of Science for relevant articles published between January 2000 and April 2024. The search strategy incorporated combinations of terms such as “dietary acculturation,” “migration,” “nutrition transition,” “migrant diet,” “traditional foods,” “health outcomes,” “chronic disease,” “refugees,” and “immigrants.” Approximately 200 article titles and abstracts were initially assessed for relevance. Studies were included if they investigated dietary changes occurring among migrants or refugees post-migration and reported associations with health outcomes, including obesity, diabetes, cardiovascular disease, or food insecurity. Studies were excluded if they exclusively examined pre-migration dietary habits, involved non-human subjects, or lacked original data or review content pertinent to acculturation and health. Following a thorough full-text review and the application of these criteria, 30 articles were selected for in-depth synthesis. To establish a conceptual framework, additional resources were consulted, including models describing dietary acculturation processes and dietary patterns prevalent in host countries. The reference lists of selected articles were also reviewed to identify additional relevant studies. Key themes—such as dietary transformations, modulating factors, health implications, and structural determinants—were identified through an iterative process based on recurring concepts within the selected literature. The synthesis emphasized quantitative data and comparative results across different migrant groups whenever feasible.
Study selection flow
A total of 200 records were identified through database searching. After removal of duplicates, 150 unique records remained for screening. Titles and abstracts were screened, resulting in 80 full-text articles assessed for eligibility. After applying inclusion and exclusion criteria, 30 studies were included in the final synthesis (Figure 2).
Dietary transformations and modulating factors
Global patterns of dietary acculturation
Dietary acculturation among migrant populations typically involves a shift from traditional diets—rich in whole grains, legumes, fruits, and vegetables—to host-country patterns characterized by higher intakes of processed foods, refined sugars, and saturated fats (15). Across diverse cultural and geographic contexts, consistent patterns of dietary transformation have been documented among migrant groups; these shifts commonly involve the displacement of traditional dietary staples with energy-dense, micronutrient-poor alternatives readily available in the host country (2, 4). For instance, South Asian migrants in Europe tend to increase their consumption of Ultraprocessed meat and dairy products while decreasing their carbohydrate intake and switching from whole grains to refined sources, leading to lower fiber intake (4, 16). Similar trends have been observed among Latin American migrants in the United States, where traditional diets high in fruits, vegetables, and legumes are replaced by diets high in processed foods, sugary beverages, and ultra processed animal products (17, 18). Furthermore, the transition often includes increased consumption of fast foods and sweetened beverages, coupled with reduced intake of traditional dishes prepared at home. The impact of dietary acculturation extends beyond individual food choices, influencing overall meal patterns and eating behaviors (19).
Dietary acculturation encompasses various dimensions, including changes in food choices, preparation methods, meal timing, and eating behaviors, as well as a decline in the consumption of traditional foods (20). This multifaceted process is shaped by factors such as the availability and accessibility of traditional foods in the host country, socioeconomic status, cultural identity, and social networks. Despite the widespread acknowledgement of dietary acculturation, growing evidence suggests that the relationship between dietary habits, immigration, and acculturation is intricate and multifaceted (20, 21). Migrants are exposed to new food environments, marketing strategies, and social norms surrounding eating, which can significantly influence their dietary choices; the degree of dietary change varies considerably among individuals and groups, depending on their level of integration into the host society, cultural preservation efforts, and access to resources that support healthy eating.
Age and gender
Age and gender play significant roles in shaping dietary acculturation patterns among migrant populations, with younger migrants often exhibiting greater dietary shifts due to increased exposure to host-country food environments and social influences. Additionally, dietary acculturation can exhibit gender-specific patterns, with men and women potentially responding differently to migration-related factors. For example, among South Asian migrants in New Zealand, 63% of women reported a reduction in green leafy vegetable consumption post-migration, while 44% of men reported an increase in alcohol intake (22). In the United Kingdom, South Asian women’s fiber intake was reported to decrease by up to 40%, and alcohol intake among South Asian men increased from negligible levels to 15–25% after migration. Qualitative evidence from Syrian migrants in Germany supports these trends, with younger men adopting more Western food habits such as frequent fast food consumption, while women—especially those with children—are more likely to retain traditional cooking practices. Older migrants generally retain stronger ties to their traditional dietary practices, while younger individuals are more likely to adopt host-country dietary habits (13).
Length of residence
Length of residence in the host country is a critical determinant of dietary acculturation, with longer durations typically associated with more pronounced dietary changes. Migrants who have resided in the host country for extended periods often exhibit greater assimilation into the prevailing food culture, leading to increased consumption of local foods and decreased reliance on traditional dietary staples. However, the relationship between length of residence and dietary habits is not always linear, as some studies have found that dietary changes may plateau or even reverse after a certain period. This could be due to a renewed emphasis on cultural identity and traditional practices, or to health concerns arising from prolonged exposure to less healthy host-country diets (18, 23–25).
Socioeconomic status and education
Socioeconomic status (SES) and education are powerful determinants of dietary choices among migrant populations, influencing both access to healthy foods and the knowledge and resources necessary to make informed dietary decisions (2, 26). Migrant households with limited financial resources may face barriers to accessing fresh produce and nutritious foods, particularly in urban areas where healthy options may be more expensive and less readily available. Conversely, higher levels of education are generally associated with greater awareness of the health implications of dietary choices, as well as a greater capacity to navigate the complexities of the host-country food environment (27–29). Lower SES exacerbates unhealthy behaviors, especially when combined with loneliness and a lack of integration in the host country (25). Moreover, higher levels of education may empower migrants to critically evaluate dietary information and resist the influence of marketing tactics promoting unhealthy foods (2).
Social environment and type of migration
The social environment and migration context exert a profound influence on dietary acculturation, shaping food choices and eating behaviors through social norms, cultural values, and access to social support networks (20, 21, 30). Migrants often encounter new social norms and expectations related to food, which can either promote or hinder the adoption of healthier dietary practices (2). For instance, migrants who settle in communities with strong ethnic enclaves may be more likely to maintain traditional dietary practices, while those who are more isolated may be more susceptible to the influences of the host-country food environment. Furthermore, the type of migration (e.g., economic migration, family reunification, refugee resettlement) can also impact dietary acculturation, as different migration contexts may be associated with varying levels of social support, economic opportunities, and exposure to cultural influences (23, 31). Migrants often grapple with adjusting to novel culinary landscapes and dietary norms in their adopted nations, which can lead to shifts in food preferences and consumption patterns (2).
Food environment and access
The food environment plays a central role in shaping dietary acculturation, with the availability, affordability, and accessibility of various food options influencing dietary choices and eating behaviors among migrant populations. Migrants moving from low- and middle-income countries to high-income countries undergo a rapid shift from conventional eating habits to industrialized food options, causing negative health outcomes (3). Migrants who settle in areas with limited access to fresh produce and healthy food options may face significant barriers to maintaining a nutritious diet, while those who reside in food deserts may be more reliant on processed foods and fast food outlets. The food environment of the host country plays a significant role in modifying dietary patterns of immigrants (5). Supermarkets, farmers’ markets, and ethnic grocery stores can all influence dietary choices by providing access to a diverse range of food options, while food advertising and marketing can shape food preferences and consumption patterns (32). Food insecurity, busier lifestyles, and children’s preferences can also influence the dietary patterns of migrants (2). Changes in dietary behavior due to migration are likely to impact health (1, 2, 19, 20, 33). It is crucial to acknowledge that newcomers can acculturate into the host culture while retaining or not retaining their cultural roots (2). Food serves as a crucial strategy for integrating into a new environment, particularly for immigrants (34). The food environment and its intersection with cultural and socioeconomic variables are key determinants of dietary behavior among migrant populations.
Impact on gut microbiota
Recent studies indicate that dietary acculturation leads to measurable changes in the gut microbiota of migrants (35). These changes may have significant implications for digestive health, immune function, and even mental well-being (4). The gut microbiota, a complex ecosystem of microorganisms residing in the digestive tract, plays a crucial role in human health, influencing everything from nutrient absorption and immune function to mental health and disease risk (36). Dietary shifts associated with migration, such as increased consumption of processed foods, saturated fats, and sugars, can disrupt the balance of the gut microbiota, leading to decreased diversity and an overgrowth of opportunistic pathogens (37). A diet high in fiber, fermented foods, and plant-based proteins promotes a diverse and resilient gut microbiota. As a defense mechanism, gut epithelial cells produce a mucosal barrier to segregate microbiota from host immune cells and reduce intestinal permeability. An impaired interaction between gut microbiota and the mucosal immune system can lead to an increased abundance of potentially pathogenic gram-negative bacteria and their associated metabolic changes, disrupting the epithelial barrier and increasing susceptibility to infections (37). The composition of the gut microbiota is intricately linked to dietary patterns, with specific dietary components promoting the growth of certain microbial species while suppressing others.
Discussion
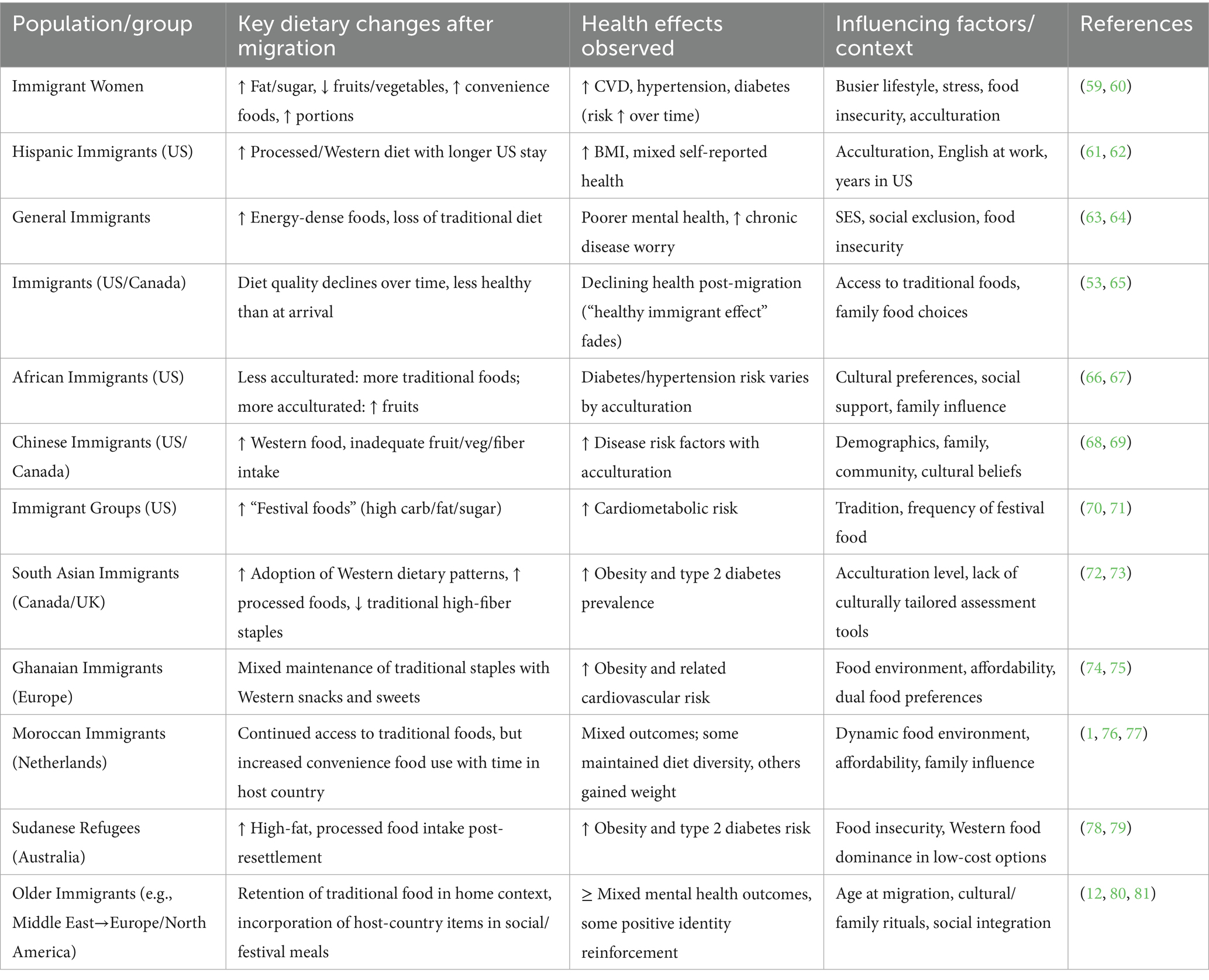
Our review of dietary transformations in migrant populations reveals several key findings. Across diverse groups, migration is frequently accompanied by a shift away from traditional, high-fiber dietary staples toward greater consumption of energy-dense, ultra processed foods (4). This transition is strongly influenced by acculturation level, socioeconomic status, and the surrounding food environment. The resulting dietary changes are consistently associated with higher prevalence of obesity, type 2 diabetes, cardiovascular diseases, and, in some groups, poorer mental health outcomes. These patterns and their associated health outcomes are summarized in Table 1, which provides an overview of the dietary changes, health risks, and modulating factors observed among the major migrant groups included in this review. Notably, the pace and extent of dietary acculturation—and the associated health risks—vary by age, gender, migration context, and the degree of social and cultural integration (20). These findings underscore the need for culturally tailored interventions that respect dietary preferences and traditions while addressing the broader determinants of health. This heterogeneity is detailed in Table 1, which illustrates how dietary changes and health outcomes differ according to population subgroup, geographic context, and influencing factors such as length of residence, socioeconomic status, and social support.
Addressing the complex and multifactorial nature of dietary transformation in migrant populations requires a collaborative, multisectoral approach (6). Policymakers, healthcare providers, researchers, and community organizations must work together to reduce barriers related to unemployment, low income, inadequate housing, and limited access to healthy foods (38). Effective interventions should be culturally sensitive, available in multiple languages, and designed with input from the communities they aim to serve. Community-based participatory research is particularly valuable for engaging migrants in the development, implementation, and evaluation of nutrition interventions (39). Nutrition education programs should focus on building practical skills and knowledge, and can be delivered through community centers, schools, workplaces, and healthcare settings. Public health initiatives must address both individual behavior and social context, recognizing the powerful influence of family, social networks, and community norms on food choices (40).
Technology-enabled approaches, such as mobile apps, telehealth, and SMS-based interventions, offer new opportunities to deliver accessible, personalized nutrition support (41). Community-based programs—including cooking classes, gardening, and food assessments—can foster social connection and empower migrants to make healthier choices (42). Policy-level actions, such as subsidies for healthy foods, taxes on unhealthy products, regulations on food marketing, and improved food labeling, are critical to create supportive food environments and address systemic barriers (43). It is also essential to enhance clinician knowledge about culturally relevant nutrition and the importance of food in disease prevention. Ongoing monitoring and evaluation, supported by robust research and adequate funding, will ensure that interventions remain effective and responsive to evolving needs (44).
Improving dietary habits and health outcomes for migrants also means understanding and addressing the broader psychosocial challenges many face, including acculturative stress, discrimination, and social isolation (20). Mental health support, culturally sensitive counseling, and peer-led programs can complement nutrition interventions and address interconnected health needs. Interventions targeting migrant mothers or other family influencers may be particularly effective in shaping household dietary practices. Structural measures such as food labeling, restricting marketing of unhealthy foods to children, and ensuring access to healthy retailers are necessary complements to individual-focused strategies. Initiatives like community gardens and farmers’ markets can increase access to fresh produce, foster engagement, and build resilience at the local level (45–47).
Healthcare access and patient-provider communication are additional priorities. Migrants often have limited health literacy, face language barriers, or lack familiarity with host-country healthcare systems. Training clinicians in cultural competence and employing interpreters or bilingual staff can help bridge these gaps, as can providing health information in multiple languages and tailored to cultural context. Policy frameworks should ensure that healthcare for migrants is affordable, equitable, and responsive to diverse needs. Active involvement of community health workers and family members further supports effective care and outreach (48).
Despite these advances, many migrant health policies still overlook lifestyle-related risk factors and preventive care. A comprehensive approach, integrating culturally appropriate health promotion, routine migration history assessment, and awareness of cultural health practices, is needed to address inequities in access and outcomes. Effective interventions should be linguistically and culturally appropriate, address administrative and legal barriers, and ensure ongoing coordination and funding. Given the continued rise in global migration, addressing the health needs of migrants is an urgent public health priority. Policies should recognize the diversity of migrant experiences, ethical imperatives for equity, and the benefits of investing in the health and well-being of all communities (38, 49, 50).
Limitations and future directions
Research on dietary transformations and health implications in migrant populations faces several limitations that need to be addressed in future studies. One major challenge is the heterogeneity of migrant populations, as migrants come from diverse cultural, socioeconomic, and geographical backgrounds. This heterogeneity makes it difficult to generalize findings from one migrant group to another. Studies often lack longitudinal data, making it challenging to track dietary changes and health outcomes over time and to establish causal relationships. Future research should focus on using longitudinal designs to understand the long-term effects of dietary transformations on the health of migrant populations. Many studies rely on self-reported dietary data, which are subject to recall bias and social desirability bias, thus, future studies should incorporate more objective measures of dietary intake, such as biomarkers and dietary records, to improve the accuracy of data collection. There is a need for more culturally sensitive research methods that account for the unique experiences and perspectives of migrant populations (11).
Community-based participatory research approaches, which involve collaboration with community members in all stages of the research process, can be particularly valuable for ensuring that research is culturally relevant and responsive to community needs (39). Qualitative research methods, such as focus groups and in-depth interviews, can provide valuable insights into the lived experiences of migrant populations and the factors that influence their dietary choices. Future research should explore the complex interplay of factors that contribute to dietary transformations in migrant populations, including socioeconomic status, cultural norms, access to healthcare, and the food environment (20). Additionally, there is a need for more intervention studies that evaluate the effectiveness of different strategies for promoting healthy eating among migrant populations.
Furthermore, future research should address the gaps in our understanding of the dietary transformations and health implications in specific migrant groups, such as refugees and undocumented immigrants. Given the increasing number of refugees worldwide, there is a pressing need for research that examines the unique nutritional challenges faced by this population (51). The intersection of these factors can create unique challenges for refugees in accessing healthy foods and maintaining traditional dietary practices. Acculturation processes can lead to the abandonment of traditional diets and the adoption of less healthy eating patterns. In addition, future research should explore the role of the food environment in shaping dietary choices among migrant populations.
More research is needed to understand how these factors influence dietary choices and health outcomes in migrant populations. Understanding how migration and acculturation affect dietary habits, especially among Latino immigrants, is crucial (21). Studies on Mexican immigrant women suggest that dietary acculturation is complex, highlighting the importance of considering cultural aspects in designing strategies to improve their diet and health (52). Longitudinal studies are needed to monitor dietary habits over time and understand how they change in response to acculturation and other factors (53). There is a need to develop and validate culturally appropriate tools for assessing dietary intake and acculturation in migrant populations (6). Given that dietary acculturation is specific to the culture and country of origin, it is important to define the population group when examining measures of dietary acculturation (6).
Sub-Saharan African immigrants in Western countries have not been studied extensively regarding changes in their eating habits. It is important to conduct further research on migration trends, dietary habits, and dietary acculturation of Sub-Saharan African immigrants living in the United States, the United Kingdom, and France (54). More studies are needed to understand the factors that promote healthy dietary choices and prevent chronic diseases in migrant populations (6, 13, 54, 55). Comprehensive dietary and health screenings, culturally appropriate nutrition education resources, and interventions are needed to improve refugees’ dietary intake and nutritional status (51). Dietary habits are critical for preventing and treating chronic diseases, but the role of diet in immigrant transitions is not well understood (19). Migrants often experience significant changes in their dietary habits as they adapt to new environments (56). The availability of familiar foods, affordability, and cultural influences all play a role in shaping their food choices. More research is needed to understand how these factors interact to affect the health of migrant populations. Effective strategies are needed to promote healthy eating and prevent chronic diseases in migrant populations.
Conclusion
Migration is a multifaceted phenomenon that profoundly influences dietary habits and health outcomes, and dietary acculturation, the process by which migrants adopt the dietary practices of their host country, plays a pivotal role in these transformations (26). Migrants often experience a shift in their dietary patterns as they navigate new food environments, socioeconomic conditions, and cultural norms (1). These dietary changes can have both positive and negative consequences for their health, increasing the risk of chronic diseases such as obesity, type 2 diabetes, and cardiovascular disease. The effect of demographic and socio-cultural variables on changes in food habits after migration should also be considered (57). For instance, obesity levels were observed to be elevated among African migrants residing in England compared to those in other European countries (58). The extent of dietary change varies depending on individual circumstances and the degree of integration into the host society.
Addressing the nutritional challenges faced by migrant populations requires a multi-pronged approach that considers the complex interplay of factors that influence their dietary choices. Promoting culturally sensitive nutrition education programs, improving access to healthy and affordable foods, and creating supportive social environments are essential steps in fostering healthy eating habits among migrants. Future research should focus on developing and evaluating interventions that are tailored to the specific needs and cultural backgrounds of different migrant groups. By understanding the dietary transformations and health implications in migrant populations, we can develop effective strategies to promote their health and well-being, ensuring that they have the opportunity to thrive in their new environments.
Author contributions
JV: Writing – original draft, Writing – review & editing. MD: Writing – review & editing, Writing – original draft. SV: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Gen AI was used in the creation of this manuscript. Generative AI (ChatGPT by OpenAI) was used to assist in refining the language, improving clarity, and generating summaries and title suggestions. All content was reviewed, edited, and verified by the author(s) to ensure accuracy and intellectual integrity.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. O’Mara, J, Waterlander, W, and Nicolaou, M. Exploring the role of the food environment in dietary acculturation: a study amongst Moroccan immigrants in the Netherlands. Int J Environ Res Public Health. (2021) 18:3328. doi: 10.3390/ijerph18073328
2. Sauter, A, Kikhia, S, von, SJ, and Loss, J. Factors influencing the nutritional behavior of Syrian migrants in Germany — results of a qualitative study. BMC Public Health. (2021) 21:1334. doi: 10.1186/s12889-021-11268-9
3. Berggreen-Clausen, A, Pha, SH, Alvesson, HM, Andersson, A, and Daivadanam, M. Food environment interactions after migration: a scoping review on low- and middle-income country immigrants in high-income countries. Public Health Nutr. (2021) 25:136–58. doi: 10.1017/s1368980021003943
4. Holmboe-Ottesen, G, and Wandel, M. Changes in dietary habits after migration and consequences for health: a focus on south Asians in Europe. Food Nutr Res. (2012) 56:18891. doi: 10.3402/fnr.v56i0.18891
5. Paxton, A, Pillai, A, Phelan, K, Cevette, N, and Bah, F. Dietary acculturation of recent immigrants from West Africa to new York City. Face à face Regards sur la santé (2016) Available online at: https://journals.openedition.org/faceaface/1023 (Accessed June 2025).
6. Lee, S, Kellow, NJ, Choi, T, and Huggins, CE. Assessment of dietary acculturation in east Asian populations: a scoping review. Adv Nutr. (2020) 12:865–86. doi: 10.1093/advances/nmaa127
7. D’Alonzo, KT, Johnson, S, and Fanfan, D. A biobehavioral approach to understanding obesity and the development of obesogenic illnesses among Latino immigrants in the United States. Biol Res Nurs. (2012) 14:364–74. doi: 10.1177/1099800412457017
8. Orjuela-Grimm, M, Deschak, CI, Aragón-Gama, AC, Carreño, SB, Hoyos, L, Mundo, V, et al. Migrants on the move and food (in)security: a call for research. J Immigr Minor Health. (2021) 24:1318–27. doi: 10.1007/s10903-021-01276-7
9. Dondi, A, Piccinno, V, Morigi, F, Sureshkumar, S, Gori, D, and Lanari, M. Food insecurity and major diet-related morbidities in migrating children: a systematic review. Nutrients. (2020) 12:379. doi: 10.3390/nu12020379
10. Fouché, C, Richter, S, Vallianatos, H, Mason, A, Fernández-Sánchez, H, Mazzucato, V, et al. African immigrant child health: a scoping review. J Migration Health. (2021) 4:100054. doi: 10.1016/j.jmh.2021.100054
11. Tiedje, K, Wieland, ML, Meiers, SJ, Mohamed, AA, Formea, CM, Ridgeway, JL, et al. A focus group study of healthy eating knowledge, practices, and barriers among adult and adolescent immigrants and refugees in the United States. Int J Behav Nutr Phys Act. (2014) 11:63. doi: 10.1186/1479-5868-11-63
12. Lillekroken, D, Bye, A, Halvorsrud, L, Terragni, L, and Debesay, J. Food for soul—older immigrants’ food habits and meal preferences after immigration: a systematic literature review. J Immigr Minor Health. (2024) 26:775–805. doi: 10.1007/s10903-023-01571-5
13. Babashahi, M, and Shokri, S. Social, cultural and economic factors affecting food behaviors in immigrants; a review study. J Health. (2021) 12:285–300. doi: 10.52547/j.health.12.2.285
14. Allen, JD, Caspi, CE, Yang, M, Leyva, B, Stoddard, AM, Tamers, SL, et al. Pathways between acculturation and health behaviors among residents of low-income housing: the mediating role of social and contextual factors. Soc Sci Med. (2014) 123:26–36. doi: 10.1016/j.socscimed.2014.10.034
15. Marchioni, DML, Claro, RM, Levy, RB, and Monteiro, CA. Patterns of food acquisition in Brazilian households and associated factors: a population-based survey. Public Health Nutr. (2011) 14:1586–92. doi: 10.1017/s1368980011000486
16. Raza, Q, Nicolaou, M, Snijder, MB, Stronks, K, and Seidell, JC. Dietary acculturation among the south-Asian Surinamese population in the Netherlands: the HELIUS study. Public Health Nutr. (2016) 20:1983–92. doi: 10.1017/s1368980016000914
17. Ayala, GX, Baquero, B, and Klinger, S. A systematic review of the relationship between acculturation and diet among Latinos in the United States: implications for future research. J Am Diet Assoc. (2008) 108:1330–44. doi: 10.1016/j.jada.2008.05.009
18. Marín-Guerrero, AC, Rodríguez-Artalejo, F, Guallar-Castillón, P, López-García, E, and Gutiérrez-Fisac, JL. Association of the duration of residence with obesity-related eating habits and dietary patterns among Latin-American immigrants in Spain. Br J Nutr. (2014) 113:343–9. doi: 10.1017/s0007114514003614
19. Azar, KMJ, Chen, EW-C, Holland, AT, and Palaniappan, L. Festival foods in the immigrant diet. J Immigr Minor Health. (2012) 15:953–60. doi: 10.1007/s10903-012-9705-4
20. Mude, W, and Nyanhanda, T. Food behaviours and eating habits among sub-Saharan African migrant mothers of school-aged children in South Australia. J Migration Health. (2022) 7:100149. doi: 10.1016/j.jmh.2022.100149
21. Formagini, T, Rodriguez, D, Dias, J, and Brooks, JV. Reassessing established assumptions of dietary habits in the USA in the context of migration and acculturation: a qualitative study of Latino immigrants. J Racial Ethn Health Disparities. (2024) 12:1333–43. doi: 10.1007/s40615-024-01967-5
22. Parackal, S. Post-migration food habits of New Zealand south Asian migrants: implications for health promotion practice. J Migration Health. (2023) 7:100182. doi: 10.1016/j.jmh.2023.100182
23. Almohanna, A, Conforti, F, Eigel, WN, and Barbeau, WE. Impact of dietary acculturation on the food habits, weight, blood pressure, and fasting blood glucose levels of international college students. J Am Coll Heal. (2015) 63:307–14. doi: 10.1080/07448481.2015.1025075
24. Satia, JA. Dietary acculturation and the nutrition transition: an overviewThis is one of a selection of papers published in the CSCN–CSNS 2009 conference, entitled can we identify culture-specific healthful dietary patterns among diverse populations undergoing nutrition transition?This paper is being published without benefit of author’s corrections. Appl Physiol Nutr Metab. (2010) 35:219–23. doi: 10.1139/h10-007
25. Spadea, T, Rusciani, R, Mondo, L, and Costa, G. Health-related lifestyles among migrants in Europe. In: Springer Briefs in Public Health. Cham, Switzerland: Springer International Publishing (2018). 57.
26. Hakim, OA. Impact of migration on the eating habit and physical activity patterns among Saudi students living in South Korea. Global J Health Sci. (2020) 13:48. doi: 10.5539/gjhs.v13n2p48
27. Basnyat, S, and Chamberlain, K. Dietary acculturation of Nepalese women in Aotearoa, New Zealand. In: Proceedings. MDPI. (2019) 37:9. doi: 10.3390/proceedings2019037009
28. Arman, G, Tuncil, E, and Fisunoğlu, M. Does educational status affect the food choice? Clin Nutr. (2018) 37:S131. doi: 10.1016/j.clnu.2018.06.1491
29. Bookari, K. What is the level of nutrition literacy of Saudi adolescents? A national wide exploratory cross-sectional study. Frontiers. Nutrition. (2023) 9:1113910. doi: 10.3389/fnut.2022.1113910
30. Ramírez, AS, Wilson, M, and Miller, LMS. Segmented assimilation as a mechanism to explain the dietary acculturation paradox. Appetite. (2021) 169:105820. doi: 10.1016/j.appet.2021.105820
31. Mahmoodi, M, George, RM, and Gokhale, D. Dietary acculturation of international students in Pune, India: a cross-sectional study. Nutr Health. (2021) 28:271–6. doi: 10.1177/02601060211019678
32. Yi, SS, Russo, R, Liu, B, Kum, SS, Rummo, PE, and Li, Y. Characterising urban immigrants’ interactions with the food retail environment. Public Health Nutr. (2020) 24:3009–17. doi: 10.1017/s1368980020002682
33. Downs, S, Fox, E, Mutuku, V, Muindi, Z, Fatima, T, Pavlovic, I, et al. Food environments and their influence on food choices: a Case study in informal settlements in Nairobi, Kenya. Nutrients. (2022) 14:2571. doi: 10.3390/nu14132571
34. Gustavsen, GW, Dong, D, Nayga, RM, and Rickertsen, K. Ethnic variation in immigrants’ diets and food acculturation – United States 1999–2012. Agricul Resource Econ Rev. (2020) 50:43. doi: 10.1017/age.2020.17
35. Damas, OM, Estes, D, Avalos, DJ, Quintero, MA, Morillo, D, Caraballo, F, et al. Hispanics coming to the US adopt US cultural behaviors and eat less healthy: implications for development of inflammatory bowel disease. Dig Dis Sci. (2018) 63:3058–66. doi: 10.1007/s10620-018-5185-2
36. Gai, Z, Dong, Y, Xu, F, Zhang, J, Yang, Y, and Wang, Y. Changes in the gut microbiota composition of healthy young volunteers after administration of Lacticaseibacillus rhamnosus LRa05: a placebo-controlled study. Front Nutr. (2023) 10:1359484. doi: 10.3389/fnut.2023.1105694
37. Yoo, JY, Gröer, M, Dutra, SVO, Sarkar, A, and McSkimming, D. Gut microbiota and immune system interactions. Microorganisms. (2020) 8:1587. doi: 10.3390/microorganisms8101587
38. Kristiansen, M, and Sheikh, A. The health of low-income migrant Workers in Gulf Cooperation Council Countries. Health Hum Rights. (2014) 22. doi: 10.13140/2.1.5130.8163
39. Ranisavljev, M, Kurniawan, AL, Ferrero, E, Shinde, S, Zhao, S, Partap, U, et al. Community-based interventions addressing multiple forms of malnutrition among adolescents in low- and middle-income countries: a scoping review. Nutr J. (2025) 24:69. doi: 10.1186/s12937-025-01136-2
40. Story, M, Kaphingst, KM, Robinson-O’Brien, R, and Glanz, K. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health. (2007) 29:253–72. doi: 10.1146/annurev.publhealth.29.020907.090926
41. Porri, D, Morabito, LA, Cavallaro, P, Rosa, EL, Pomi, AL, Pepe, G, et al. Time to act on childhood obesity: the use of technology. Front Pediatr. (2024) 12:1359484. doi: 10.3389/fped.2024.1359484
42. Downer, S, Berkowitz, SA, Harlan, TS, Olstad, DL, and Mozaffarian, D. Food is medicine: actions to integrate food and nutrition into healthcare. BMJ. (2020) 369:m2482. doi: 10.1136/bmj.m2482
43. Laar, A, Addo, P, Aryeetey, R, Agyemang, C, Zotor, F, Asiki, G, et al. Perspective: food environment research priorities for Africa—lessons from the Africa food environment research network. Adv Nutr. (2022) 13:739–47. doi: 10.1093/advances/nmac019
44. Rodgers, GP, and Collins, FS. Precision nutrition—the answer to “what to eat to stay healthy”. JAMA. (2020) 324:735. doi: 10.1001/jama.2020.13601
45. Collie-Akers, V, Fawcett, SB, Schultz, JA, Fleming, K, RES, R, Ritchie, LD, et al. Association of Multisetting Community Programs and Policies with Child Body Mass Index: the healthy communities study. Prev Chronic Dis. (2020) 17:190196. doi: 10.5888/pcd17.190196
46. Jaskiewicz, L, Dombrowski, RD, Drummond, HM, Barnett, GM, Mason, M, and Welter, CR. Partnering with community institutions to increase access to healthful foods across municipalities. Prev Chronic Dis. (2013) 10:E167. doi: 10.5888/pcd10.130011
47. Parker, L, Burns, AC, and Sánchez, EJ. Actions for healthy eating. (2009). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK219682/ [Accessed January 2025]
48. Vissandjée, B, Short, WE, and Bates, K. Health and legal literacy for migrants: twinned strands woven in the cloth of social justice and the human right to health care. BMC Int Health Hum Rights. (2017) 17:e1–e4. doi: 10.1186/s12914-017-0117-3
49. Tahzib, F, Davidovitch, N, and Labonté, R. Migration, justice and health: reimagining the earth as one country and humankind its citizens. Public Health. (2019) 172:105–7. doi: 10.1016/j.puhe.2019.03.016
50. Squires, A, Thompson, R, Sadarangani, T, Amburg, P, Sliwinski, K, Curtis, CA, et al. International migration and its influence on health. Res Nurs Health. (2022) 45:503–11. doi: 10.1002/nur.22262
51. Khuri, J, Wang, Y, Holden, K, Fly, AD, Mbogori, T, Müeller, S, et al. Dietary intake and nutritional status among refugees in host countries: a systematic review. Adv Nutr. (2022) 13:1846–65. doi: 10.1093/advances/nmac051
52. Nogales, BO, Torres, JM, Alvarado, AV, and Vega-López, S. Perceptions of dietary acculturation among Mexican immigrant women residing in a southwestern US metropolitan area. Current Develop Nutrition. (2020) 4:nzaa043_107. doi: 10.1093/cdn/nzaa043_107
53. Sanou, D, O’Reilly, EK, Ngnie-Teta, I, Batal, M, Mondain, N, Andrew, C, et al. Acculturation and nutritional health of immigrants in Canada: a scoping review. J Immigr Minor Health. (2013) 16:24–34. doi: 10.1007/s10903-013-9823-7
54. Ngoubene-Atioky, AJ, Case, J, Tokplo, L, and Baur, C. Migration trends and dietary patterns in sub-Saharan African adult immigrants: a comparative analysis of populations in France, the UK, and the USA. Migration Stud. (2019) 9:1116–43. doi: 10.1093/migration/mnz038
55. Horlyck-Romanovsky, M, Huang, TT-K, Ahmed, R, Echeverría, SE, Wyka, K, Leung, MM, et al. Intergenerational differences in dietary acculturation among Ghanaian immigrants living in new York City: a qualitative study. J Nutritional Sci. (2021) 10:e69. doi: 10.1017/jns.2021.69
56. Satia-Abouta, J, Patterson, RE, Neuhouser, ML, and Elder, JP. Dietary acculturation. J Am Diet Assoc. (2002) 102:1105–18. doi: 10.1016/s0002-8223(02)90247-6
57. Wandel, M, Råberg, M, Kumar, BN, and Holmboe-Ottesen, G. Changes in food habits after migration among south Asians settled in Oslo: the effect of demographic, socio-economic and integration factors. Appetite. (2007) 50:376–85. doi: 10.1016/j.appet.2007.09.003
58. Osei-Kwasi, HA, Boateng, D, Asamane, EA, Akparibo, R, and Holdsworth, M. Transitioning food environments and diets of African migrants: implications for non-communicable diseases. Proc Nutr Soc. (2022) 82:69–79. doi: 10.1017/s0029665122002828
59. Hyman, I, Guruge, S, Makarchuk, M, Cameron, JI, and Micevski, V. Promotion of healthy eating: among new immigrant women in Ontario. Can J Diet Pract Res. (2002) 63:125–9. doi: 10.3148/63.3.2002.125
60. Tseng, M, Wright, DJ, and Fang, CY. Acculturation and dietary change among Chinese immigrant women in the United States. J Immigr Minor Health. (2014) 17:400–7. doi: 10.1007/s10903-014-0118-4
61. Cho, Y, Frisbie, WP, Hummer, RA, and Rogers, RG. Nativity, duration of residence, and the health of Hispanic adults in the United States. Int Migr Rev. (2004) 38:184–211. doi: 10.1111/j.1747-7379.2004.tb00193.x
62. Akresh, IR. Dietary assimilation and health among Hispanic immigrants to the United States. J Health Soc Behav. (2007) 48:404–17. doi: 10.1177/002214650704800405
63. M, Alegrı́a, Álvarez, K, and K, DM. Immigration and mental health. Curr Epidemiol Rep. (2017) 4:145–55. doi: 10.1007/s40471-017-0111-2
64. LeCroy, MN, Suss, R, Russo, R, Sifuentes, S, Beasley, JM, Barajas-Gonzalez, RG, et al. Looking across and within: immigration as a unifying structural factor impacting cardiometabolic health and diet. Ethn Dis. (2023) 33:130–9. doi: 10.18865/ed.33.2-3.130
65. Vang, ZM, Sigouin, J, Flénon, A, and Gagnon, A. Are immigrants healthier than native-born Canadians? A systematic review of the healthy immigrant effect in Canada. Ethn Health. (2016) 22:209–41. doi: 10.1080/13557858.2016.1246518
66. Osokpo, O, Lewis, LM, Bracy, DP, Adeniji, D, Bankole, AO, and Riegel, B. Dietary behaviors of African immigrants living with diabetes and/or hypertension: a qualitative study. Innov Aging. (2024) 8:933. doi: 10.1093/geroni/igae098.3009
67. Sofolahan-Oladeinde, Y, Iwelunmor, J, Tshiswaka, DI, and Conserve, D. Acculturation and its influence on the health perceptions, health behaviors, and health outcomes of African immigrants in the United States: a review of the literature. (2024) Available online at: https://elicit.com/notebook/9c9f7596-94e1-4f5f-a7dd-6f6c4066bdec#1850c76d90ed61ad95e605baeb74f9c7 (Accessed May 6, 2025).
68. Rosenmöller, DL, Gašević, D, Seidell, JC, and Lear, SA. Determinants of changes in dietary patterns among Chinese immigrants: a cross-sectional analysis. Int J Behav Nutr Phys Act. (2011) 8:42. doi: 10.1186/1479-5868-8-42
69. Zou, P, Ba, D, Luo, Y, Yang, Y, Zhang, C, Zhang, H, et al. Dietary characteristics and influencing factors on Chinese immigrants in Canada and the United States: a scoping review. Nutrients. (2022) 14:2166. doi: 10.3390/nu14102166
70. Guadamuz, JS, Kapoor, K, Lazo, M, Eleazar, A, Yahya, T, Kanaya, AM, et al. Understanding immigration as a social determinant of health: cardiovascular disease in Hispanics/Latinos and south Asians in the United States. Curr Atheroscler Rep. (2021) 23:25. doi: 10.1007/s11883-021-00920-9
71. MN, LeCroy, Suss, R, Russo, RG, Sifuentes, S, Beasley, JM, Barajas-Gonzalez, RG, et al. Back looking across and within: immigration as a unifying structural factor impacting cardiometabolic health and diet. (2023) Available online at: https://elicit.com/notebook/06aa839e-6044-4525-b818-fff766629775#1850f0375726008bf46af5629edcf436 (Accessed May 6, 2025).
72. LeCroy, MN, and Stevens, J. Dietary intake and habits of south Asian immigrants living in Western countries. Nutr Rev. (2017) 75:391–404. doi: 10.1093/nutrit/nux023
73. Lesser, IA, Gašević, D, and Lear, SA. The association between acculturation and dietary patterns of south Asian immigrants. PLoS One. (2014) 9:e88495. doi: 10.1371/journal.pone.0088495
74. Galbete, C, Nicolaou, M, Meeks, K, Aikins, A, De-Graft, AJ, Amoah, S, et al. Food consumption, nutrient intake, and dietary patterns in Ghanaian migrants in Europe and their compatriots in Ghana. Food Nutr Res. (2017) 61:1341809. doi: 10.1080/16546628.2017.1341809
75. Boateng, D, Agyemang, C, Beune, E, KAC, Meeks, Smeeth, L, Schulze, M, et al. Back migration and cardiovascular disease risk among Ghanaian populations in Europe: the RODAM study (research on obesity and diabetes among African migrants). (2017) Available online at: https://elicit.com/notebook/a512ac92-f50b-4a08-8ea1-814fd33ca98d#1850f10d274be9df9bea160ba80810ed (Accessed May 6, 2025).
76. Nicolaou, M, Benjelloun, S, Stronks, K, RMV, Dam, Seidell, JC, and Doak, CM. Back influences on body weight of female Moroccan migrants in the Netherlands: A qualitative study. (2012) Available online at: https://elicit.com/notebook/fbb4a59a-2c16-4877-8aa9-402a4c44ae2e#1850f14aa40811190a2aa7c368318970 (Accessed May 6, 2025).
77. Nicolaou, M, Doak, CM, van, DRM, Brug, J, Stronks, K, and Seidell, JC. Cultural and social influences on food consumption in Dutch residents of Turkish and Moroccan origin: a qualitative study. J Nutr Educ Behav. (2009) 41:232–41. doi: 10.1016/j.jneb.2008.05.011
78. Mude, W, Burgess, T, and Mwanri, L. “We should eat it wisely, in a good way”: Knowledge, perceptions and understanding of childhood obesity and overweight among Sudanese refugee parents in South Australia. (2013) Available online at: https://elicit.com/notebook/c7c9bdf5-4f87-455b-90b6-b9013a7fb3c6#185100bb5c9cf732b0345abda2b57ac8 [Accessed June 2025]
79. Renzaho, AMN, and Burns, C. Post-migration food habits of sub-Saharan African migrants in Victoria: a cross-sectional study. Nutr Diet. (2006) 63:91–102. doi: 10.1111/j.1747-0080.2006.00055.x
80. Hassan, D, and Hekmat, S. Dietary acculturation of Arab immigrants: in the greater Toronto area. Can J Diet Pract Res. (2012) 73:143–6. doi: 10.3148/73.3.2012.143
81. Elshahat, S. Dietary patterns and behaviours among Arab newcomers in Western countries: A call for equitable and accessible food systems. (2020) Available online at: https://elicit.com/notebook/b11c8189-0260-4e76-98d7-18759f1c3527#1851012230de30066531134349324342 (Accessed May 6, 2025).
Keywords: dietary acculturation, migration, nutrition transition, migrant health, chronic disease risk, food environment, socioeconomic determinants, gut microbiota
Citation: Varre JV, Dustin M and Van Vliet S (2025) Dietary transformations and health implications in migrant populations: a global perspective. Front. Nutr. 12:1623556. doi: 10.3389/fnut.2025.1623556
Edited by:
Megan Carney, University of Arizona, United StatesReviewed by:
Assia Bouhoudan, Abdelmalek Essaadi University, MoroccoTafadzwa Nyanhanda, Victoria University, Australia
Copyright © 2025 Varre, Dustin and Van Vliet. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Stephan Van Vliet, c3RlcGhhbi52YW52bGlldEB1c3UuZWR1
 Joseph Vinod Varre
Joseph Vinod Varre Mia Dustin
Mia Dustin Stephan Van Vliet
Stephan Van Vliet