- 1Department of Psychology, Virginia Tech, Blacksburg, VA, United States
- 2Department of Human Nutrition, Food, and Exercise, Virginia Tech, Blacksburg, VA, United States
In the United States, almost 10% of Americans will experience an eating disorder in their lifetime. Despite evidence that eating disorders occur across socio-economic backgrounds, the stereotypes of eating disorders being a disease of affluence persist. The experience of food insecurity, defined as limited or inconsistent physical and economic access to a sufficient amount and variety of nutritious food needed for a healthy life, is significantly associated with greater eating disorder symptoms. There are several reasons eating disorder symptoms may develop in people experiencing food insecurity, including food/benefit distribution cycles, shame, and weight bias. This Perspective highlights the relationship between food insecurity and eating disorders and provides informed recommendations specific to dietetic practice. Guidance is provided for Registered Dietitian Nutritionists (RDNs) in settings that serve individuals at risk of, or experiencing, food insecurity. RDNs should be informed on best practices for screening for eating disorders and providing appropriate referrals to eating disorder specific care, as well as encouraging realistic, achievable health behaviors, and using non-stigmatizing language.
Introduction
In the United States, an estimated 9%, or 28.8 million, of Americans will experience an eating disorder in their lifetime (1). Eating disorders are mental health conditions characterized by disturbances in eating patterns and body image that arise from a combination of biological, psychological, and social factors. Despite evidence that eating disorders occur across socio-economic backgrounds, stereotypes of eating disorders being a disease of affluence persist (2, 3).
The experience of food insecurity, defined as limited or inconsistent physical and economic access to a sufficient amount and variety of nutritious food needed for a healthy life, is significantly associated with greater eating disorder symptoms, including dietary restriction not due to food scarcity, extreme weight control behaviors, and binge eating, and eating disorder diagnoses, such as bulimia nervosa and binge eating disorder (4–11). Compared to individuals with adequate food access, individuals experiencing food insecurity are 3–5 times more likely to also experience an eating disorder (7). Strikingly, this association remains present even when controlling for relevant socio-demographic factors such as age, gender, race, income, and education, highlighting the strong relationship between food insecurity and eating disorders (7, 12, 13). A summary of a sample of studies of eating disorders among individuals experiencing food insecurity is presented in the top panel of Table 1.
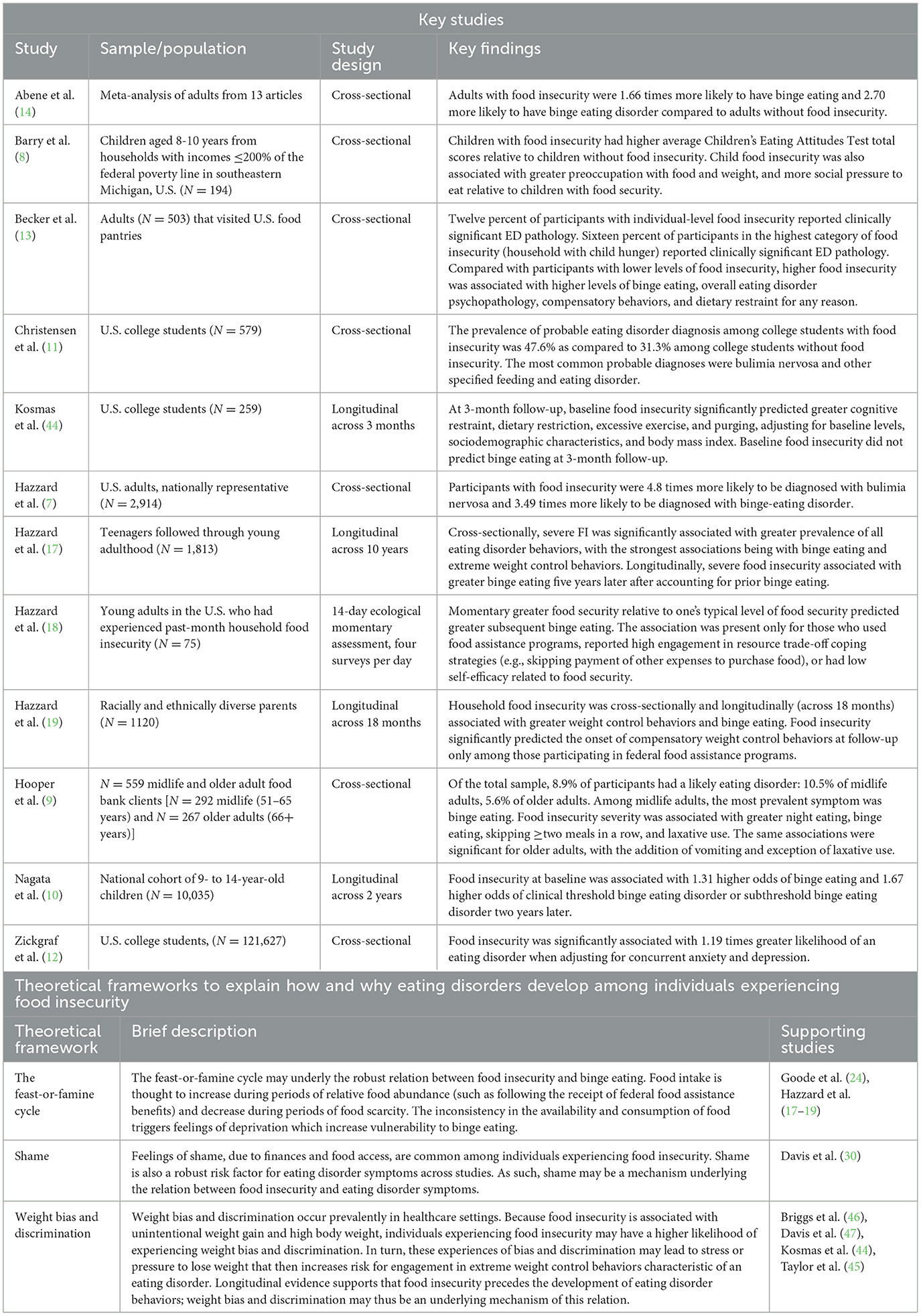
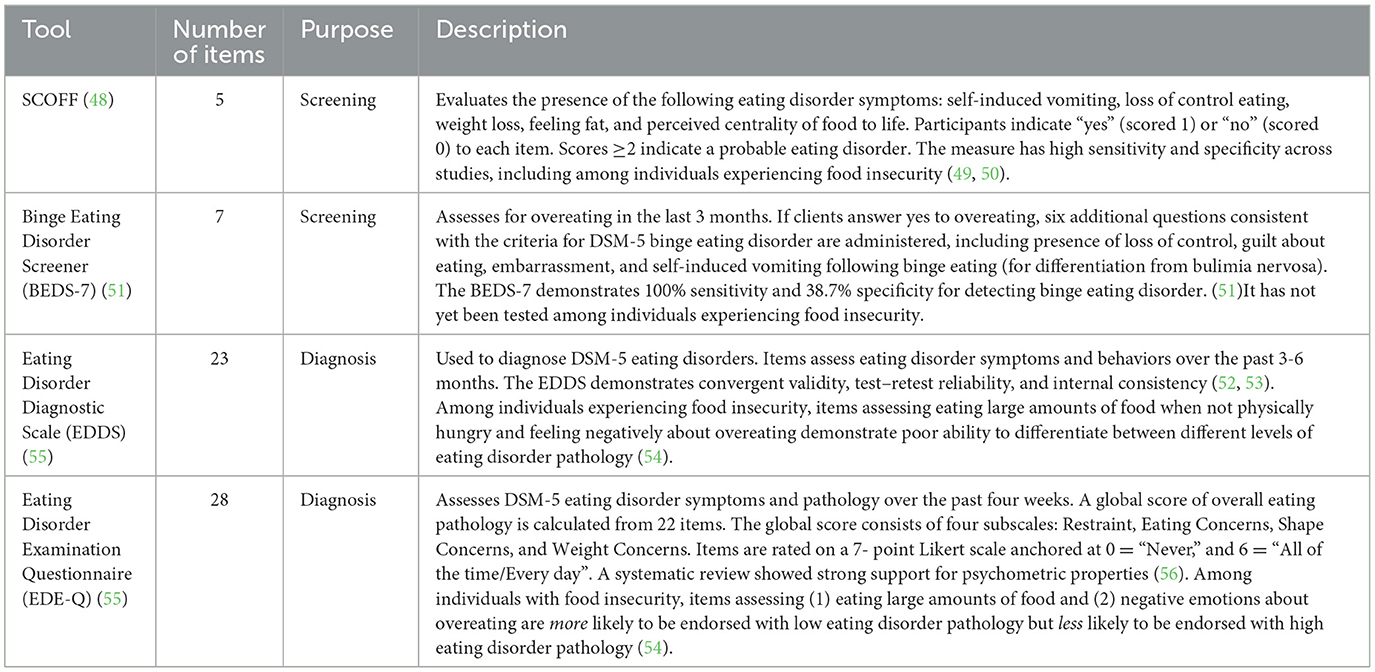
Table 1. Summary of key studies (top panel) and theoretical frameworks (bottom panel) describing the relation between eating disorders and food insecurity.
When working with clients with food insecurity, Registered Dietitian Nutritionists (RDNs) are uniquely positioned to assess eating disorder symptoms and develop individualized eating and nutrition recommendations. Considering the intersection between eating disorder symptoms and food insecurity, special attention is warranted to mutually address both concerns with each unique individual, while not exacerbating eating disorder symptoms.
The aim of this Perspective is to provide guidance to dietetic practitioners in settings that serve individuals at risk of, or experiencing, food insecurity. We first summarize the literature on the overlap between food insecurity and eating disorders. We then describe foundational theories underlying the development of eating disorder symptoms in the context of experiencing or having previously experienced food insecurity. We then offer theory- and evidence-informed recommendations for dietitians. Finally, we provide recommendations to help ensure that nutrition interventions do not inadvertently contribute to the development or exacerbation of eating disorders among individuals experiencing or who have previously experienced food insecurity.
How and why do eating disorder symptoms develop among individuals experiencing food insecurity?
Several hypotheses exist for how and why eating disorder symptoms develop in the context of food insecurity, including food distribution cycles, shame, and weight bias. These factors can present independently or in conjunction with one another.
The feast-or-famine cycle
Of the many eating disorder symptoms, there is a particularly robust relationship between food insecurity and binge eating, defined as consuming a large amount of food while experiencing a loss of control (14). One prevailing theory for the development of binge eating within food insecurity is the “feast or famine cycle”, whereby food intake increases during periods of relative food abundance and decreases when food again becomes scarce (15, 16). Inconsistency in the availability and consumption of food, regardless of the reason for food restriction (e.g., due to a desire for weight loss/maintenance or due to food scarcity), is thought to trigger feelings of deprivation, predict preoccupation with food, and increase vulnerability to subsequent binge eating (17–20). Having autonomy and agency to choose foods to purchase and consume is associated with greater food satisfaction and eating behavior regulation (21). However, experiencing food insecurity makes it difficult to have autonomy in food choices, given limited access to sufficient quantity and variety of foods, and the limitations on types of foods that can be purchased with some federal nutrition assistance benefits (22). This lack of autonomy may be a contributor to feelings of deprivation that lead to binge eating among individuals experiencing food insecurity—research should evaluate this possibility.
Food distribution frequency may also contribute to the “feast or famine” phenomena and serve as a factor, notably monthly benefit distribution schedules of nutrition assistance, such as Supplemental Nutrition Assistance Program (SNAP) benefits. This consistent yet infrequent disbursement may unintentionally facilitate the feast or famine cycle for some recipients, compared to staggered distributions (23). A 2023 study demonstrated that relative food abundance at one time point predicted later engagement in binge eating (18). This relationship was strongest among individuals reporting use of food assistance programs. An additional study showed that experiences of loss of control and emotional eating occurred frequently upon disbursement of benefits when food supply was high, and also occasionally when resources were diminishing, with some participants noting that worrying about food access resulted in overeating (24). The cyclical nature of food availability may play a role in the onset and maintenance of binge eating. Importantly, although prior work has included both longitudinal and cross-sectional designs, more work using longitudinal designs (across short and extended time periods) and experimental methods to demonstrate temporal and causal effects is needed.
Shame
Many individuals experiencing food insecurity reported feeling ashamed of their financial limitations (25, 26). Shame is a negative emotion that occurs as a result of feeling morally inferior to others (27). Shame about finances and food access may translate to attitudes toward eating. For example, individuals receiving SNAP benefits have described a sense of morality around needing to make “good food choices” (24). Additionally, they reported feeling pressure to engage in extreme behaviors to lose weight (24). Importantly, shame is a robust predictor of eating disorder symptoms, including binge eating, purging, and excessive exercise (28, 29). Women experiencing food insecurity and an eating disorder or other mental health disorder have reported higher levels of shame than women experiencing food insecurity without a mental health disorder (30). As such, shame may be a mechanism underlying the relationship between food insecurity and eating disorder symptoms. Of note, prior work on shame, eating disorders, and food insecurity has been cross-sectional; longitudinal and experimental designs are needed to support the potential temporal and causal effects of food insecurity on shame and subsequent eating disorder symptoms.
Weight bias and discrimination
Weight bias and discrimination may also be contributors to eating disorders among individuals experiencing food insecurity. Weight bias is defined as generalized negative beliefs about people of high body weight (31). Weight discrimination is defined as poor treatment of an individual due to their body size (32). Unfortunately, weight bias and discrimination are often viewed as socially acceptable forms of discrimination in our society (33, 34). Weight bias in particular is prevalent in healthcare settings—including among dietitians (35, 36)—and is associated with less healthcare utilization and worse health outcomes among people of higher body weight (31). Although most practitioners aim to avoid discrimination, implicit biases—unconscious attitudes or stereotypes—can sometimes lead to unintentional stigmatization. Because stigmatization for any reason can result in stress that leads to or exacerbates maladaptive coping behaviors, such as eating disorder symptoms, it is crucial that practitioners take steps to recognize their own implicit biases to avoid unintentional stigmatization and to support clients whose eating behavior might be influenced by external sources of bias and discrimination.
The presence of food insecurity is associated with unintentional weight gain and high body weight (6, 37), resulting in a higher likelihood of experiencing weight bias and weight discrimination. Research has identified low diet quality, including lower consumption of nutrient-dense foods and higher consumption of energy-dense and highly processed foods, as a strong contributor (38). This discrepancy can be partially attributed to greater availability and affordability of ultraprocessed and energy-dense foods in low-income vs. high-income areas (39, 40). Concerningly, weight discrimination is a powerful social determinant of health (33). Across studies, the experience of weight discrimination and internalization of weight bias among individuals with food insecurity is associated with a higher number of eating disorder symptoms, lower quality of life, and psychosocial impairment (41–43).
The experience of weight bias and discrimination, in conjunction with higher weight, among individuals experiencing food insecurity may lead to engagement in inappropriate weight control behaviors. For example, the experience of food insecurity predicts later engagement in self-induced vomiting, excessive exercise, and dietary restriction not due to food scarcity (19, 44). Individuals experiencing food insecurity and weight-based discrimination report finding the experience stressful and using dietary restriction to mitigate weight gain (45, 46). Finally, weight bias predicts eating disorder diagnosis among women experiencing current food insecurity, even after adjusting for current weight (47), suggesting that weight bias is robustly associated with eating disorder pathology regardless of weight status. Notably, research in this area has been largely cross-sectional and self-report survey-based; future research should use longitudinal or experimental designs to verify the potential causal effects of this model.
A summary of these frameworks and supporting studies is presented in the bottom panel of Table 1.
Recommendations for dietetic practice
Eating disorder screening
Because individuals with food insecurity are more likely to experience an eating disorder than individuals without food insecurity, RDNs should ideally screen individuals who are currently experiencing or have experienced food insecurity for eating disorders or eating disorder symptoms. Based on research on the feast or famine cycle (18, 24), this recommendation is particularly pertinent for individuals currently receiving nutrition assistance benefits. A recommended screening measure is the SCOFF (48), which is widely used, brief, and demonstrates good sensitivity and specificity in detecting eating disorders, including among individuals experiencing food insecurity (49, 50). The SCOFF includes five items that assess whether an individual (1) engages in self-induced vomiting, (2) has concern about losing control while eating, (3) has experienced recent weight loss, (4) perceives themselves as “too fat”, and (5) experiences food as “dominating” their life. The SCOFF and other common eating disorder screening and diagnostic tools are summarized in Table 2 (51–56). In addition to screening and diagnostic measures, RDNs can ask their clients open-ended questions regarding how food insecurity may influence the individual's eating behavior, weight, and exercise routine. Because eating disorder assessments were not developed with food insecurity considerations in mind (39), it is possible that clients could have trouble answering some questions. For example, they may eat small meals for reasons that vary, perhaps due to lack of access to food and other times due to eating disorder-related thought patterns. Correspondingly, recommendations to increase meal size should be tailored to reflect the reason(s) for limiting size. To allow for comprehensive assessment, open-ended and semi-structured questions are needed in addition to screening instruments such as the SCOFF. See Table 3 for examples of preliminary questions RDNs may ask clients following the administration of screening instruments. We note that the preliminary example questions presented in the Table 3 were generated by our research team (i.e., a clinical psychologist, RDN, Assistant Director and Director of the Virginia Cooperative Extension Family Nutrition Program). Importantly, the preliminary questions have not yet been systematically investigated or piloted in any practitioner or client populations. We recommend that future research investigate these and other culturally sensitive questions to assess eating patterns and eating disorder symptoms among individuals experiencing food insecurity to ensure that they yield the information intended.
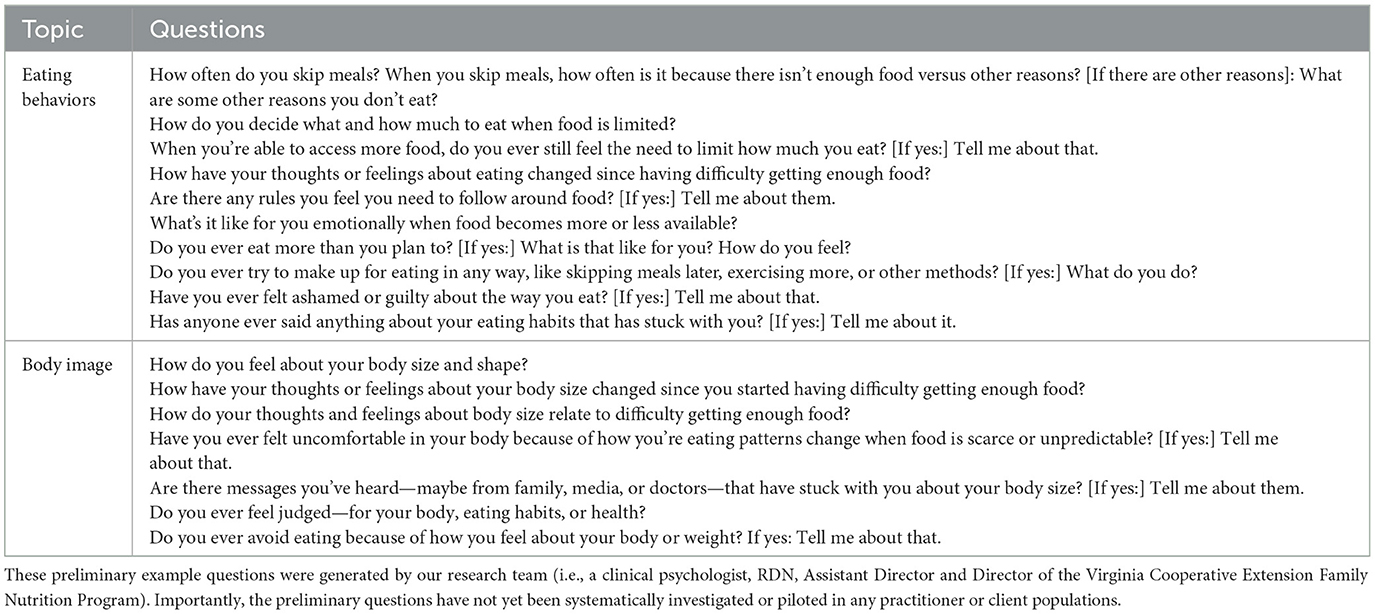
Table 3. Preliminary questions that may be used to further assess eating disorder behaviors and cognitions in individuals experiencing food insecurity.
Referrals to eating disorder-specific care
When eating disorder symptoms are detected, individuals should be referred to eating disorder-specific mental health care that can be provided simultaneously with medical nutrition therapy. A comprehensive treatment team for addressing eating disorders includes a therapist, dietitian, and physician, as well as possible adjunctive care. Referrals may be sourced from the National Eating Disorders Association Provider Finder, a database of therapists who specialize in eating disorders (57). Fortunately, access to eating disorder specialists via telehealth has expanded access to treatment in more rural settings and for those with more limited access to healthcare (58). Unfortunately, in some countries, eating disorder and mental health care is not universally covered by health insurance, and individuals experiencing food insecurity may be un- or under-insured (59). In these cases, it may be difficult to find affordable eating disorder and mental health care (59). Digital, self-guided interventions are low-cost, low-burden, and can be accessible via Smartphone or computer (60). As such, digital interventions offered alongside medical nutrition counseling or within programs that target individuals who are at risk of food insecurity, such as the Supplemental Nutrition Assistance Program—Education (SNAP-Ed) and the Expanded Food and Nutrition Education Program (EFNEP) offer promising alternatives to traditional eating disorder and mental healthcare. Future research should investigate the implementation and outcomes of such interventions.
Encouraging realistic and achievable health behaviors
Practitioners should be cautious about prescribing health behaviors and recommending weight loss in the context of food insecurity. If individuals feel pressure to lose weight, particularly from health professionals, but have limited access and autonomy around food, they may resort to extreme measures, such as extreme dietary restriction, to manage weight (45, 46). Because dietary restriction increases risk for binge eating, it is unlikely to yield weight loss (61). Practitioners should discuss with their clients the harms of using extreme weight control methods and emphasize health behavior engagement rather than weight outcomes. A weight-neutral approach focused on actionable health behaviors and outcomes rather than a weight-centric approach focused on weight outcomes can encourage clients to prioritize their health while maintaining a positive relationship with food and their bodies. A 2019 review suggests that weight-neutral approaches for health may be as effective as traditional weight-loss methods for improving physical, psychological, and behavioral outcomes (62). For example, practitioners should educate clients on eating as consistently as possible to reduce binge eating vulnerability, while also recognizing that this may be challenging for individuals experiencing food insecurity. Practitioners may also educate individuals on the health benefits of engaging in regular movement that does not require a great deal of resources or time (e.g., walking, yoga at home) to increase mobility and heart health, avoiding cigarette smoking, limiting alcohol use, and prioritizing healthy sleep practices (e.g., sleeping 6–8 h/night). Each of these recommendations lessens pressure on diet quality and weight-related outcomes and increases emphasis on caring for oneself, which may prevent or reduce pathological eating and weight control behaviors as well as risk for other chronic health problems (63, 64).
Practicing compassion and using non-stigmatizing language
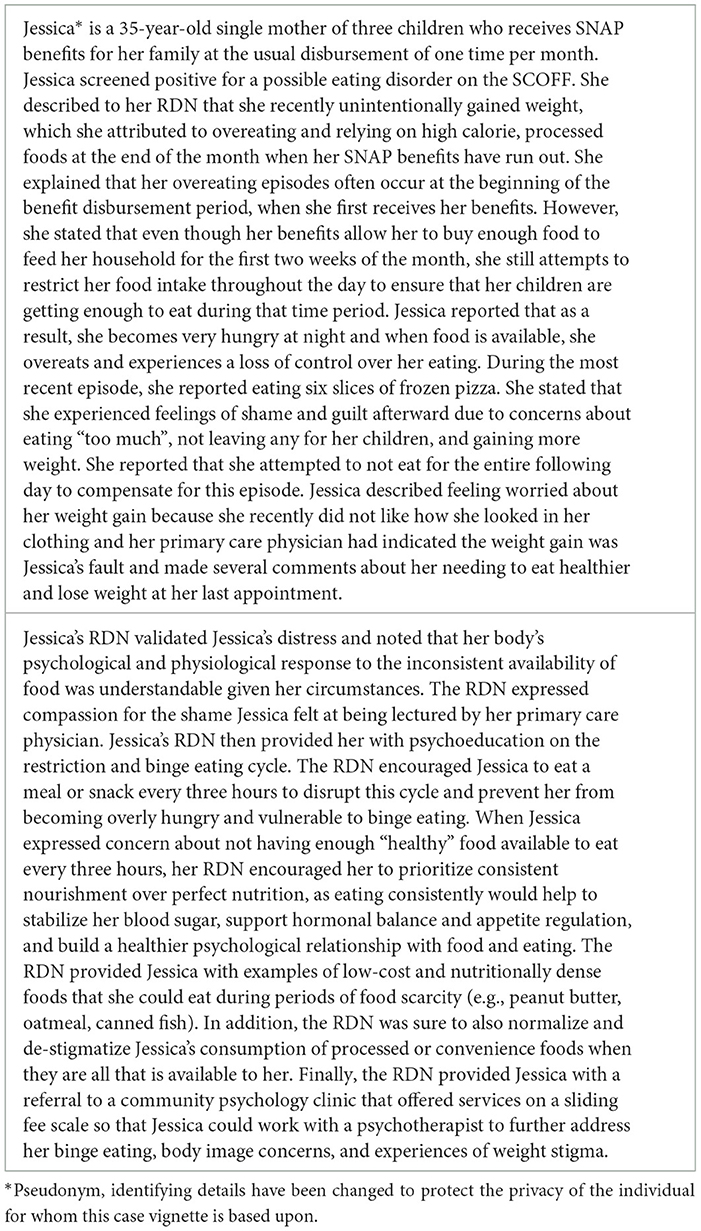
Unbiased and compassionate care is especially important for clients experiencing food insecurity, given potential high levels of shame, which increases vulnerability to eating disorders (25, 26, 30). Frequent compassionate responses that express care, non-judgment, and validation of the individual's specific challenges are recommended. Relatedly, it is also crucial to recognize that individuals experiencing food insecurity are often subject to a myriad of stereotypes related to finances, health, and weight, all of which can interfere with their access to resources and perceived ability to change their behaviors (45). Recommendations related to reducing or maintaining weight may be intended to help enhance a patient's health, but such a recommendation could inflict harm rather than improve health. Practitioners should avoid encouraging changes in a client's weight unless it is markedly impacting their health. Even so, prescribing weight loss to manage health conditions, such as heart disease, non-alcohol fatty liver disease, or joint pain, may be counterproductive, given that achieving and sustaining weight loss overtime is statistically unlikely (65–67). A BMI of 25–30 is associated with the lowest mortality rates of all weight categories, suggesting that addressing weight with clients in this BMI range may not be necessary (68, 69). A focus on weight may even be counterproductive as weight cycling—losing and gaining weight frequently—itself is associated with negative health outcomes (70–72). Further, multiple large-scale randomized clinical trials indicate that decreases in disease incidence can occur with improved diet quality (e.g., greater consumption of fruits, vegetables, whole grains, etc.) and physical activity among individuals of all sizes, whether or not weight change occurs in the process (73–76). This suggests that compassionate encouragement of health behaviors without an emphasis on weight is likely to enhance health. Employing a weight-neutral approach with all clients, but particularly those experiencing food insecurity, can encourage clients to practice health behaviors without triggering disordered eating patterns. An example of a case vignette is presented in Table 4.
International parallels and considerations
Although this Perspective focuses primarily on United States-based nutrition assistance programs (e.g., SNAP, EFNEP), the parallels described exist internationally. For example, Canada's Prenatal Nutrition Program (77), the United Kingdom's Healthy Start vouchers (78), and Brazil's Bolsa Família Program (79) each include some form and combination of food, financial support and nutrition education, and RDNs are often involved, at some level, in these efforts. Such programs exist because food insecurity is an urgent international concern: nearly 2.4 billion people, equivalent to 29.6 percent of the global population, experience food insecurity (80). Importantly, meta-analyses, systematic reviews, and recent empirical studies indicate that the association between food insecurity and eating disorders is present across countries and cultures (14, 81, 82).
Notably, access to treatment for eating disorders varies significantly depending on the structure of a country's healthcare system (83, 84). Universal healthcare, as provided in the United Kingdom and Australia, for example, provides more consistent access to not only general and primary medical care but also mental health services, which may contribute to more timely detection and treatment of eating disorders regardless of food security status (85). However, despite greater coverage of services, barriers still exist, particularly for populations with low-income and/or food insecurity, including long waitlists, limited coverage for specialized care, and geographical constraints for in-person care (86–88).
In countries with private insurance coverage, as in the United States, structural barriers to eating disorder treatment are substantial (89, 90). Being un- or under-insured, incurring high out-of-pocket expenses, and having limited financial and/or geographical access to specialty eating disorder care is unfortunately common among individuals with low income and/or food insecurity (91). Although publicly funded insurance such as Medicaid and Medicare may cover some ED care in some settings, access is still limited compared to individuals with private insurance (91–93).
Future research is critically needed to develop accessible, culturally-sensitive adaptations of existing assessment tools and frameworks for treating individuals experiencing food insecurity and eating disorders across cultures and contexts.
Discussion
Individuals experiencing food insecurity are highly vulnerable to eating disorders. Eating disorder symptoms are detectable using brief screening measures, but additional open-ended questions may be needed to understand circumstances surrounding behaviors to help tailor interventions. Integrating mental health care alongside dietetic counseling for individuals experiencing food insecurity could help address both food insecurity and disordered eating simultaneously. Digital, self-guided interventions incorporated within existing service use may be one promising pathway forward. Finally, dietitians should be mindful of weight bias and discrimination as common experiences in this group, and provide weight-neutral care that emphasizes health behavior engagement rather than weight management.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
HD: Conceptualization, Writing – original draft, Writing – review & editing. EM: Conceptualization, Writing – original draft, Writing – review & editing. ES: Conceptualization, Writing – original draft, Writing – review & editing. SM: Conceptualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Economics DA. The Social and Economic Cost of Eating Disorders in the United States of America: A Report for the Strategic Training Initiative for the Prevention of Eating Disorders and the Academy for Eating Disorders. Available online at: https://www.hsph.harvard.edu/striped/report-economic-costs-of-eating-disorders/ (Accessed July 16, 2025).
2. Mitchison D, Basten C, Griffiths S, Murray SB. Beneath the tip of the iceberg: Why so many people with eating disorders are not referred for treatment. Aust Fam Physician. (2017) 46:539–40. doi: 10.3316/informit.919926867748528
3. Huryk KM, Drury CR, Loeb KL. Diseases of affluence? A systematic review of the literature on socioeconomic diversity in eating disorders. Eat Behav. (2021) 43:101548. doi: 10.1016/j.eatbeh.2021.101548
4. Hazzard VM, Loth KA, Hooper L, Becker CB. Food insecurity and eating disorders: a review of emerging evidence. Curr Psychiat Reports. (2020) 22:74. doi: 10.1007/s11920-020-01200-0
5. Lydecker JA, Grilo CM. Food insecurity and bulimia nervosa in the United States. Int J Eat Disord Jun. (2019) 52:735–9. doi: 10.1002/eat.23074
6. Rasmusson G, Lydecker JA, Coffino JA, White MA, Grilo CM. Household food insecurity is associated with binge-eating disorder and obesity. Int J Eat Disord. (2019) 52:28–35. doi: 10.1002/eat.22990
7. Hazzard VM, Barry MR, Leung CW, Sonneville KR, Wonderlich SA, Crosby RD. Food insecurity and its associations with bulimic-spectrum eating disorders, mood disorders, and anxiety disorders in a nationally representative sample of U.S. adults. Soc Psychiatry Psychiatr Epidemiol. (2022) 57:1483–90. doi: 10.1007/s00127-021-02126-5
8. Barry MR, Sonneville KR, McGowan AR, Needham BL, Kobayashi LC, Leung CW. Caregiver-reported household food insecurity and child-reported food insecurity in relation to eating disorder risk factors and symptoms among preadolescent children. Int J Eat Disord. (2022) 55:1331–41. doi: 10.1002/eat.23784
9. Hooper SC, Kilpela LS, Gomez F, Middlemass KM, Becker CB. Eating disorder pathology in a sample of midlife and older adults experiencing food insecurity. Eat Behav. (2023) 49:101742. doi: 10.1016/j.eatbeh.2023.101742
10. Nagata JM, Chu J, Cervantez L, Ganson KT, Testa A, Jackson DB, et al. Food insecurity and binge-eating disorder in early adolescence. Int J Eat Disord. (2023) 56:1233–9. doi: 10.1002/eat.23944
11. Christensen KA, Forbush KT, Richson BN, Thomeczek ML, Perko VL, Bjorlie K, et al. Food insecurity associated with elevated eating disorder symptoms, impairment, and eating disorder diagnoses in an American University student sample before and during the beginning of the COVID-19 pandemic. Int J Eat Disord. (2021) 54:1213–23. doi: 10.1002/eat.23517
12. Zickgraf HF, Hazzard VM, O'Connor SM. Food insecurity is associated with eating disorders independent of depression and anxiety: Findings from the 2020–2021 healthy minds study. Int J Eat Disord. (2022) 55:354–61. doi: 10.1002/eat.23668
13. Becker CB, Middlemass K, Taylor B, Johnson C, Gomez F. Food insecurity and eating disorder pathology. Int J Eat Disord. (2017) 50:1031–40. doi: 10.1002/eat.22735
14. Abene JA, Tong J, Minuk J, Lindenfeldar G, Chen Y, Chao AM. Food insecurity and binge eating: A systematic review and meta-analysis. Int J Eat Disord. (2023) 56:1301–22. doi: 10.1002/eat.23956
15. Dinour LM, Bergen D, Yeh MC. The food insecurity-obesity paradox: a review of the literature and the role food stamps may play. J Am Diet Assoc Nov. (2007) 107:1952–61. doi: 10.1016/j.jada.2007.08.006
16. Frayn M, Trainor C, Lin M, Pitts A, Drexler SA, Patarinski AGG, et al. Patient perceptions of the relationship between food insecurity and eating disorder treatment: A qualitative exploration. Int J Eat Disord. (2022) 55:332–42. doi: 10.1002/eat.23661
17. Hazzard VM, Hooper L, Larson N, Loth KA, Wall MM, Neumark-Sztainer D. Associations between severe food insecurity and disordered eating behaviors from adolescence to young adulthood: findings from a 10-year longitudinal study. Prevent Med. (2022) 154:106895. doi: 10.1016/j.ypmed.2021.106895
18. Hazzard VM, Loth KA, Crosby RD, Wonderlich SA, Engel SG, Larson N, et al. Relative food abundance predicts greater binge-eating symptoms in subsequent hours among young adults experiencing food insecurity: Support for the “feast-or-famine” cycle hypothesis from an ecological momentary assessment study. Appetite. (2023) 180:106316. doi: 10.1016/j.appet.2022.106316
19. Hazzard VM, Loth KA, Fertig AR, Trofholz AC, de Brito JN, Doering AC, et al. Household food insecurity is associated with greater prevalence and 18-month incidence of a range of disordered eating behaviors in a racially and ethnically diverse sample of parents. Eat Behav. (2023) 49:101728. doi: 10.1016/j.eatbeh.2023.101728
20. Keys A, Brožek J, Henschel A, Mickelsen O, Taylor HL. The Biology of Human Starvation. (1950). University of Minnesota Press.
21. Teixeira PJ, Patrick H, Mata J. Why we eat what we eat: the role of autonomous motivation in eating behaviour regulation. Nutr Bullet. (2011) 36:102–7. doi: 10.1111/j.1467-3010.2010.01876.x
22. Andriessen T, van der Horst H, Morrow O. Forms of autonomy and dependence in food aid: unravelling how they are related and perceived by recipients. Agricult Human Values. (2025). doi: 10.1007/s10460-025-10715-2
23. Hamrick KS, Andrews M, SNAP. Participants' eating patterns over the benefit month: a time use perspective. PLoS ONE. (2016) 11:e0158422. doi: 10.1371/journal.pone.0158422
24. Goode RW, Godoy SM, Olson K, et al. “If I start panicking over having enough, then I start eating too much”: Understanding the eating behaviors of SNAP recipients in larger bodies during COVID-19. Eat Behav. (2023) 49:101741. doi: 10.1016/j.eatbeh.2023.101741
25. Swales S, May C, Nuxoll M, Tucker C. Neoliberalism, guilt, shame and stigma: a Lacanian discourse analysis of food insecurity. J Community Appl Soc Psychol. (2020) 30:673–87. doi: 10.1002/casp.2475
26. Pineau C, Williams PL, Brady J, Waddington M, Frank L. Exploring experiences of food insecurity, stigma, social exclusion, and shame among women in high-income countries: a narrative review. Canadian Food Stud. (2021) 8:473. doi: 10.15353/cfs-rcea.v8i3.473
28. O'Loghlen E, Grant S, Galligan R. Shame and binge eating pathology: a systematic review. Clin Psychol Psychother. (2022) 29:147–63. doi: 10.1002/cpp.2615
29. Blythin SPM, Nicholson HL, Macintyre VG, Dickson JM, Fox JRE, Taylor PJ. Experiences of shame and guilt in anorexia and bulimia nervosa: a systematic review. Psychol Psychother. (2020) 93:134–59. doi: 10.1111/papt.12198
30. Davis HA, Kells M, Todorov S, Kosmas J, Wildes JE. Comorbid eating, depressive, and anxiety psychopathology is associated with elevated shame in women with food insecurity. Int J Eat Disord. (2023) 56:1087–97. doi: 10.1002/eat.23913
31. Pearl RL, Sheynblyum M. How weight bias and stigma undermine healthcare access and utilization. Curr Obesity Reports. (2025) 14:11. doi: 10.1007/s13679-025-00605-3
32. Pearl RL, Puhl RM. Weight bias internalization and health: a systematic review. Obesity Rev. (2018) 19:1141–63. doi: 10.1111/obr.12701
33. Pearl RL, Donze LF, Rosas LG, Agurs-Collins T, Baskin ML, Breland JY, et al. Ending weight stigma to advance health equity. Am J Prev Med. (2024) 67:785–91. doi: 10.1016/j.amepre.2024.06.021
34. Pearl RL. Weight bias and stigma: public health implications and structural solutions. Soc Issues Policy Rev. (2018) 12:146–82. doi: 10.1111/sipr.12043
35. Lawrence BJ, Kerr D, Pollard CM, Theophilus M, Alexander E, Haywood D, et al. Weight bias among health care professionals: a systematic review and meta-analysis. Obesity. (2021) 29:1802–12. doi: 10.1002/oby.23266
36. Jung FU, Luck-Sikorski C, Wiemers N, Riedel-Heller SG. Dietitians and nutritionists: stigma in the context of obesity. A systematic review. PLoS ONE. (2015) 10:e0140276. doi: 10.1371/journal.pone.0140276
37. Franklin B, Jones A, Love D, Puckett S, Macklin J, White-Means S. Exploring mediators of food insecurity and obesity: a review of recent literature. J Community Health. (2012) 37:253–64. doi: 10.1007/s10900-011-9420-4
38. O'Brien KS, Latner JD, Puhl RM, Vartanian LR, Giles C, Griva K, et al. The relationship between weight stigma and eating behavior is explained by weight bias internalization and psychological distress. Appetite. (2016) 102:70–6. doi: 10.1016/j.appet.2016.02.032
39. Gupta S, Rose CM, Buszkiewicz J, Ko LK, Mou J, Cook A, et al. Characterising percentage energy from ultra-processed foods by participant demographics, diet quality and diet cost: findings from the Seattle Obesity Study (SOS) III. Br J Nutr. (2021) 126:773–81. doi: 10.1017/S0007114520004705
40. Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clini Nutr. (2004) 79:6–16. doi: 10.1093/ajcn/79.1.6
41. Cuauro SE, Santos N, Andrade E, Dani AW, Sanchious SN, Hooper SC, et al. Internalized weight stigma and weight discrimination: associations with quality of life and psychosocial impairment in a sample living with food insecurity. Int J Environ Res Public Health. (2023) 20:7147. doi: 10.3390/ijerph20247147
42. Gastón-Panthaki A, Serrano A, Virani N, Sylvestre J, Crisafulli BF, Becker CB. Food insecurity, weight-based discrimination, weight self-stigma, and mental health in post-bariatric surgery patients. Body Image. (2023) 45:46–53. doi: 10.1016/j.bodyim.2023.01.009
43. Becker CB, Middlemas K, Gomez F, Kilpela LS. An exploratory examination of internalized weight stigma in a sample living with food insecurity. Body Image. (2021) 37:238–45. doi: 10.1016/j.bodyim.2021.03.006
44. Kosmas JA, Garza M, Kells M, Hahn SL, Davis HA. Food insecurity predicts excessive exercise, dietary restriction, cognitive restraint, and purging, but not binge eating, in College Students Across 3 Months. Int J Eat Disord. 58:952–63. doi: 10.1002/eat.24401
45. Taylor EA, Foster JS, Mobley AR. A qualitative investigation of body weight and weight loss-related attitudes of mothers and fathers in the context of food insecurity. Eat Weight Disord. (2020) 25(6):1663–9. doi: 10.1007/s40519-019-00804-7
46. Briggs R, Rowden H, Lagojda L, Robbins T, Randeva HS. The lived experience of food insecurity among adults with obesity: a quantitative and qualitative systematic review. J Public Health. (2024) 46:230–49. doi: 10.1093/pubmed/fdae016
47. Davis HA, Meredith K, G. PAG, and Wildes JE. Preliminary associations of body weight, weight bias, and dietary restriction with eating disorder diagnosis in women experiencing food insecurity. Eat Disord. (2024) 32:473–92. doi: 10.1080/10640266.2024.2322322
48. Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ. (1999) 319:1467. doi: 10.1136/bmj.319.7223.1467
49. Richson BN, Hazzard VM, Christensen KA, Hagan KE. Do the SCOFF items function differently by food-security status in U.S. college students?: statistically, but not practically, significant differences. Eat Behav. (2023) 49:101743. doi: 10.1016/j.eatbeh.2023.101743
50. Kutz AM, Marsh AG, Gunderson CG, Maguen S, Masheb RM. Eating disorder screening: a systematic review and meta-analysis of diagnostic test characteristics of the SCOFF. J Gen Intern Med. (2020) 35:885–93. doi: 10.1007/s11606-019-05478-6
51. Herman BK, Deal LS, DiBenedetti DB, Nelson L, Fehnel SE, Brown TM. Development of the 7-item binge-eating disorder screener (BEDS-7). Prim Care Companion CNS Disord. (2016) 18:25291. doi: 10.4088/PCC.15m01896
52. Stice E, Telch CF, Rizvi SL. Development and validation of the Eating Disorder Diagnostic Scale: a brief self-report measure of anorexia, bulimia, and binge-eating disorder. Psychol Assess. (2000) 12:123. doi: 10.1037//1040-3590.12.2.123
53. Masheb RM, Ramsey CM, Marsh AG, Decker SE, Maguen S, Brandt CA, et al. DSM-5 eating disorder prevalence, gender differences, and mental health associations in United States military veterans. Int J Eat Disord. (2021) 54:1171–80. doi: 10.1002/eat.23501
54. O'Connor SM, Hazzard VM, Zickgraf HF. Exploring differential item functioning on eating disorder measures by food security status. Eat Weight Disord. (2022) 27:1449–55. doi: 10.1007/s40519-021-01289-z
55. Fairburn CG. Appendix B: Eating disorder examination questionnaire (EDE-Q6.0). In: Cognitive Behavior Therapy And Eating Disorders. New York, NY: Guilford Press (2008).
56. Berg KC, Peterson CB, Frazier P, Crow SJ. Psychometric evaluation of the eating disorder examination and eating disorder examination-questionnaire: a systematic review of the literature. Int J Eat Disord. (2012) 45:428–38. doi: 10.1002/eat.20931
57. National Eating Disorders Association. National Eating Disorders Association Provider Finder. Available online at: https://www.nationaleatingdisorders.org/get-help/
58. Cook-Cottone C, Harriger JA, Tylka TL, Wood-Barcalow NL. Virtually possible: strategies for using telehealth in eating disorder treatment learned from the COVID-19 pandemic. Eat Disord. (2024) 32:99–119. doi: 10.1080/10640266.2023.2261762
59. Moitra M, Owens S, Hailemariam M, Wilson KS, Mensa-Kwao A, Gonese G, et al. Global mental health: where we are and where we are going. Curr Psychiatry Rep. (2023) 25:301–11. doi: 10.1007/s11920-023-01426-8
60. Ramos G, Hernandez-Ramos R, Taylor M, Schueller SM. State of the science: using digital mental health interventions to extend the impact of psychological services. Behav Therapy. (2024) 55:1364–79. doi: 10.1016/j.beth.2024.04.004
61. de Oliveira J, Ferro J, Guimarães VHD, da Luz FQ. Try not to think about food: An association between fasting, binge eating and food cravings. Journal of the National Medical Association. 2024/10/01/2024;116(5):588-599. doi: 10.1016/j.jnma.2024.09.005
62. Dugmore JA, Winten CG, Niven HE, Bauer J. Effects of weight-neutral approaches compared with traditional weight-loss approaches on behavioral, physical, and psychological health outcomes: a systematic review and meta-analysis. Nutr Rev. (2019) 78:39–55. doi: 10.1093/nutrit/nuz020
63. Schwartz J, Rhodes R, Bredin SSD, Oh P, Warburton DER. Effectiveness of approaches to increase physical activity behavior to prevent chronic disease in adults: a brief commentary. J Clin Med. (2019) 8:295. doi: 10.3390/jcm8030295
64. Hernández B, Scarlett S, Moriarty F, Romero-Ortuno R, Kenny RA, Reilly R. Investigation of the role of sleep and physical activity for chronic disease prevalence and incidence in older Irish adults. BMC Public Health. (2022) 22:1711. doi: 10.1186/s12889-022-14108-6
65. Hall KD, Kahan S. Maintenance of lost weight and long-term management of obesity. Med Clin North Am Jan. (2018) 102:183–97. doi: 10.1016/j.mcna.2017.08.012
66. Fischer M, Oberänder N, Weimann A. Four main barriers to weight loss maintenance? A quantitative analysis of difficulties experienced by obese patients after successful weight reduction. Eur J Clin Nutr. (2020) 74:1192–200. doi: 10.1038/s41430-020-0559-x
67. Fothergill E, Guo J, Howard L, Kerns JC, Knuth ND, Brychta R, et al. Persistent metabolic adaptation 6 years after “The Biggest Loser” competition. Obesity. (2016) 24:1612–9. doi: 10.1002/oby.21538
68. Xu H, Cupples LA, Stokes A, Liu C-T. Association of obesity with mortality over 24 years of weight history: findings from the framingham heart study. JAMA Network Open. (2018) 1:e184587–e184587. doi: 10.1001/jamanetworkopen.2018.4587
69. Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. (2013) 309:71–82. doi: 10.1001/jama.2012.113905
70. Zou H, Yin P, Liu L, Duan W, Li P, Yang Y, et al. Association between weight cycling and risk of developing diabetes in adults: a systematic review and meta-analysis. J Diabetes Investig Apr. (2021) 12:625–32. doi: 10.1111/jdi.13380
71. Quinn DM, Puhl RM, Reinka MA. Trying again (and again): weight cycling and depressive symptoms in U. S. adults. PLoS ONE. (2020) 15:e0239004. doi: 10.1371/journal.pone.0239004
72. Byun SS, Bello NA, Liao M, Makarem N, Aggarwal B. Associations of weight cycling with cardiovascular health using American Heart Association's Life's Simple 7 in a diverse sample of women. Prev Med Rep Dec. (2019) 16:100991. doi: 10.1016/j.pmedr.2019.100991
73. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. (2002) 346:393–403. doi: 10.1056/NEJMoa012512
74. Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. (2001) 344:1343–50. doi: 10.1056/NEJM200105033441801
75. Li G, Zhang P, Wang J, Gregg EW, Yang W, Gong Q, et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet. (2008) 371:1783–9. doi: 10.1016/S0140-6736(08)60766-7
76. Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and diabetes study. Diabetes Care Apr. (1997) 20:537–44. doi: 10.2337/diacare.20.4.537
77. Mildon A, Francis J, Stewart S, Underhill B, Ng YM, Richards E, et al. Effect on breastfeeding practices of providing in-home lactation support to vulnerable women through the Canada Prenatal Nutrition Program: protocol for a pre/post intervention study. Int Breastfeed J. (2021) 16:49. doi: 10.1186/s13006-021-00404-1
78. Thomas M, Moore JB, Onuselogu DA, Dalton A, Rains T, Lowry E, et al. Supermarket top-up of Healthy Start vouchers increases fruit and vegetable purchases in low-income households. Nutr Bullet. (2023) 48:353–64. doi: 10.1111/nbu.12627
79. Rezende LF, Wahrhaftig J. Bridging observational and experimental evidence to eradicate poverty: lessons from the Bolsa Familia Program. Lancet Global Health. (2025) 13:e385–6. doi: 10.1016/S2214-109X(25)00008-7
80. UNICEF. The State of Food Security and Nutrition in the World 2023. (2023). Available online at: https://data.unicef.org/resources/sofi-2023/
81. Hallward L, Nagata JM, Testa A, Jackson DB, Ganson KT. Associations between gender identity, eating disorder psychopathology, and food insecurity among Canadian adolescents and young adults during the COVID-19 pandemic. Eat Behav. (2023) 49:101723. doi: 10.1016/j.eatbeh.2023.101723
82. Bidopia T, Carbo AV, Ross RA, Burke NL. Food insecurity and disordered eating behaviors in children and adolescents: a systematic review. Eat Behav. (2023) 2023:101731. doi: 10.1016/j.eatbeh.2023.101731
83. Berkowitz SA, Drake C, Byhoff E. Food insecurity and social policy: a comparative analysis of welfare state regimes in 19 countries. Int J Soc Det Health Health Serv. (2024) 54:76–86. doi: 10.1177/27551938231219200
84. Acle A, Cook BJ, Siegfried N, Beasley T. Cultural considerations in the treatment of eating disorders among racial/ethnic minorities: a systematic review. J Cross Cult Psychol. (2021) 52:468–88. doi: 10.1177/00220221211017664
85. Maguire S, Bryant E, Ivancic L, Nassar N, Collective MR. Universal healthcare reform for community treatment of eating disorders in Australia: report of the first 2 years of operation. Public Health Res Pract. (2023) 33:2211 doi: 10.17061/phrp32232211
86. Ahmed M, Maguire S, Dann KM, Scheneuer F, Kim M, Miskovic-Wheatley J, et al. Socioeconomic inequity in the utilization of healthcare among people with eating disorders in Australia. Psychol Med. (2024) 54:3863–75. doi: 10.1017/S0033291724002290
87. Asaria A. Improving eating disorder care for underserved groups: a lived experience and quality improvement perspective. J Eat Disord. (2025) 13:11. doi: 10.1186/s40337-024-01145-2
88. Brown R, Murphy-Morgan C, Downs J, Branley-Bell D. A call for strategy on eating disorders: the need for a comprehensive eating disorder strategy in England and specific guidance for the remote delivery of eating disorder services. J Eat Disord. (2025) 13:54. doi: 10.1186/s40337-025-01224-y
89. Penwell TE, Bedard SP, Eyre R, Levinson CA. Eating disorder treatment access in the united states: perceived inequities among treatment seekers. Psychiatric Services. (2024) 75:944–52. doi: 10.1176/appi.ps.20230193
90. Mikhail ME, Cordell KD, Downey AE, Snowden LR, Accurso EC. Predictors of Outpatient and Inpatient Service Utilization Among Publicly–Insured Youth With Eat Disord. Int J Eat Disord. (2025) 58:181–92. doi: 10.1002/eat.24301
91. Moreno R, Buckelew SM, Accurso EC, Raymond-Flesch M. Disparities in access to eating disorders treatment for publicly-insured youth and youth of color: a retrospective cohort study. Journal of Eat Disord. (2023) 11:10. doi: 10.1186/s40337-022-00730-7
92. Presskreischer R, Steinglass JE, Anderson KE. Eating disorders in the U. S. Medicare population. Int J Eat Disord. (2022) 55:362–71. doi: 10.1002/eat.23676
Keywords: eating disorders, food insecurity, stigma, RDN, weight neutral
Citation: Davis HA, Myers E, Serrano E and Misyak S (2025) Detecting and addressing eating disorders among individuals experiencing food insecurity: considerations for dietetic practice. Front. Nutr. 12:1668349. doi: 10.3389/fnut.2025.1668349
Received: 17 July 2025; Accepted: 11 August 2025;
Published: 12 September 2025.
Edited by:
Abdullahi Aborode, Mississippi State University, United StatesReviewed by:
Zainab Tiamiyu, Augusta University, United StatesJerry Adesola Adeyemo, Klinikum Hochsauerland, Germany
Abiodun Adewolu, Crescent University, Nigeria
Copyright © 2025 Davis, Myers, Serrano and Misyak. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Heather A. Davis, aGVhdGhlcmRhdmlzQHZ0LmVkdQ==
 Heather A. Davis
Heather A. Davis Emily Myers
Emily Myers Elena Serrano1
Elena Serrano1