- 1Council for Responsible Nutrition, UK (CRN UK), Coventry, United Kingdom
- 2Nestlé Health Science, Vevey, Switzerland
- 3Amway Corporation, Ada, MI, United States
- 4Department of Regulatory, Medical, Safety, Quality and Compliance (RMSQC), Bayer Consumer Care AG, Basel, Switzerland
Micronutrient inadequacy is a significant issue in Europe, partly driven by an evolving food landscape. Food supplements play a critical role in offsetting these gaps, particularly in vulnerable groups, and contribute to the overall health resilience, wellbeing, and productivity across the life-course and population. However, both the extent and impact of micronutrient insufficiency and the essential role of food supplements remain underrecognized in public health, clinical training, and practice. We examine the reasons behind this widespread under-acknowledgment, along with selected evidence demonstrating the tangible benefits of food supplements in bridging micronutrient gaps and fostering health resilience. We discuss the health policy implications of incorporating food supplements into public health strategies to enhance nutritional status, help reduce the risk of chronic diseases, improve workforce productivity, and reduce healthcare costs across Europe. Ultimately, we call for an integrated approach to nutrition policy that fully recognizes and utilizes the value of food supplements in supporting a healthier and more resilient European population.
1 Introduction
Food supplements are concentrated sources of micronutrients, or other substances with nutritional or physiological effects, marketed in the form of tablets, capsules, powders or liquids in measured doses (1). These were developed in response to an evolving understanding of the importance of micronutrients to maintain physiological homeostasis and good health (2), as well as the growing awareness that supplementation would be needed to address gaps in dietary intake that could lead to micronutrient deficiency, with later recognition that food supplements could support resilience and optimal health (3–5). Food supplements are regulated as foods in Europe, to ensure that they can effectively bridge dietary gaps without posing health risks (1).
Despite the direct and multifaceted relationship between micronutrient status and health (6), the prevalence of low micronutrient intake in Europe (7), and the relatively long historical use of food supplements (3), acknowledgment of their importance among policy makers is still lacking—both in public health and clinical practice. Our present review focuses on the changing food landscape that has contributed to micronutrient inadequacies across Europe, and the evidence for the role of food supplements in helping bridge nutritional gaps and promoting health resilience in the general population and specific subgroups. Integrated nutrition policies must be developed and implemented to acknowledge the public health crisis caused by micronutrient inadequacy in Europe and the tangible positive impact of food supplements. Vitamin D will be used as a case in point, considering its critical roles in health (8), the insufficiency of European dietary supplies compared to Reference Intakes (RI) (9–12), the prevalence of suboptimal serum 25-hydroxyvitamin D (25(OH)D) levels throughout Europe (13), and the consequences of vitamin D dietary insufficiency and deficiency (14).
2 Balanced nutrition is essential for public health
Nutrition has long been recognized to be a cornerstone of human health—a critical foundation for growth and vitality. Balanced nutrition, which includes an adequate supply of micronutrients, underpins immune resilience and supports cardiometabolic function, reproductive health, cognitive and brain development, and overall physical and mental health (15). The need for a sufficient intake of micronutrients extends throughout life—from preconception, fetal development, and infancy (16), to early childhood and adolescence (17), and continues into adulthood and old age (18, 19). Dietary reference values were designed to safely prevent micronutrient deficiencies in different groups of healthy individuals (20); however, these levels may not be sufficient to promote optimal health (19, 21).
Poor nutrition has a substantial impact on society by increasing strain on healthcare systems, reducing resilience to health crises, and leading to higher rates of chronic diseases and shorter life expectancies—even in the developed world, where micronutrient-poor food is abundant (22–25). It has been suggested that the presence of one or more micronutrient deficiencies should be considered in all chronic diseases, particularly in vulnerable groups (6, 26). The World Health Organization has highlighted the economic burden of poor nutrition, estimating that addressing nutrient insufficiencies could save billions in healthcare costs globally (27, 28).
3 Current nutritional needs and gaps within Europe
To maintain yield and ensure food security, modern agricultural practices have needed to adapt to increasing demand, environmental pollutants, and climate change (24, 29). The subsequent depletion of micronutrients in staple crops, along with the ready availability of low-micronutrient convenience foods, has contributed to an insufficient availability of micronutrients in the food supply (30, 31).
Despite the abundance of food in high-income countries, nutrient inadequacy is a significant issue, with many individuals not meeting the recommended intakes for essential micronutrients, especially among certain demographics (7, 32–34). For example, vitamin D deficiency is well established in Europe and has been described as reaching “pandemic” levels, affecting up to 40% of the population (13). A low vitamin D status can lead to an increased risk of fatigue, muscle aches, pains and weakness, infections, osteomalacia, rickets, osteoporosis, falls and fractures, and may contribute to autoimmune disorders such as type 1 diabetes (14, 35). In addition, widespread insufficiencies have been reported across Europe for vitamins A and B12, folate, iron, calcium, iodine, magnesium, and zinc, particularly in vulnerable populations (Table 1). The decreased availability of micronutrients in the European food supply has led to an increasing reliance on food supplements to maintain micronutrient sufficiency—in 2022, over 90% of over 13,000 people questioned in 14 countries reported using a food supplement within the last 12 months (36). The true prevalence of micronutrient deficiencies in Europe, especially in high-risk populations, is one of the key initial aims of the ongoing Zero Hidden Hunger EU initiative (37, 38).
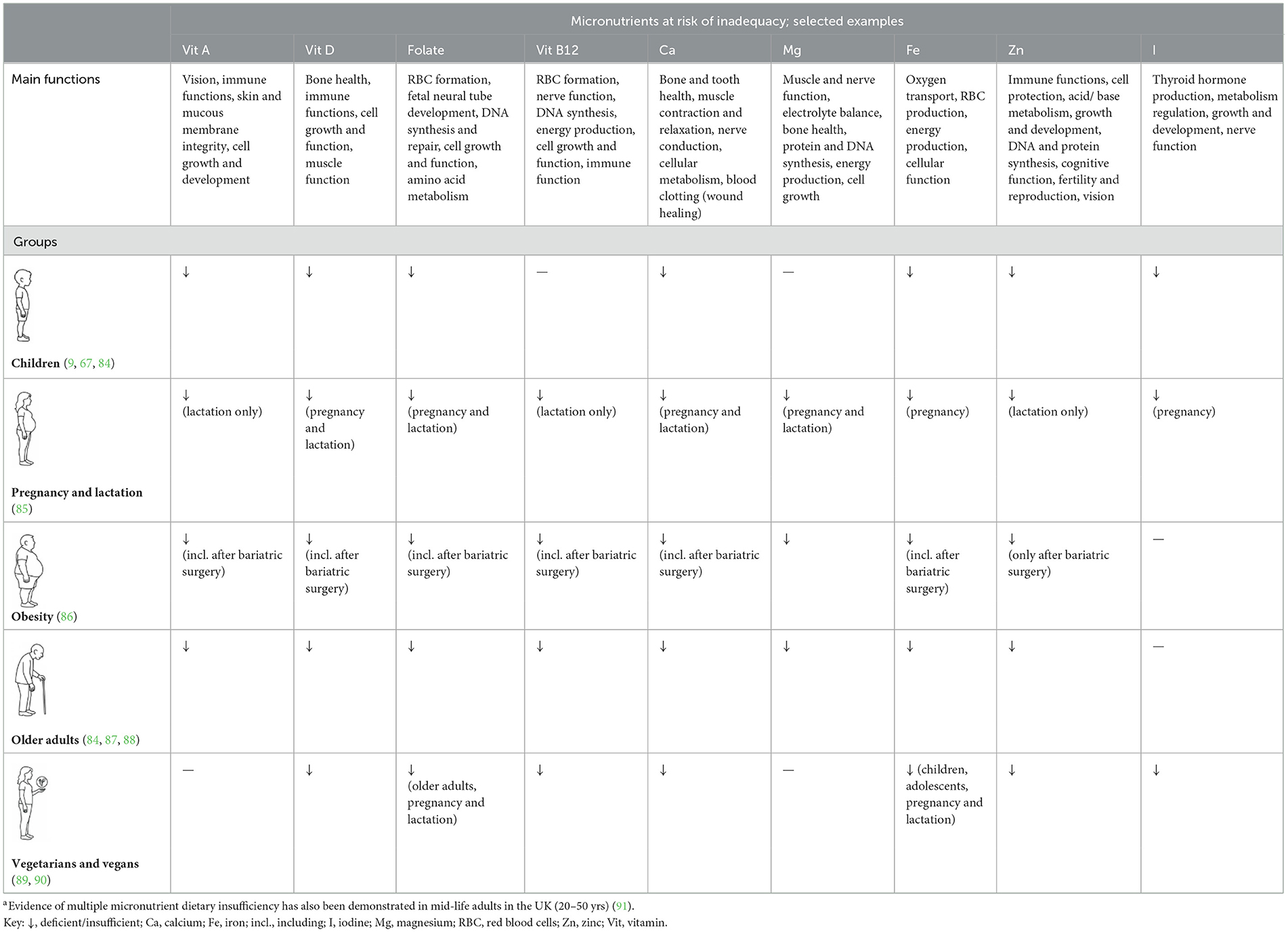
Table 1. Overview of various vulnerable groups at risk of selected micronutrient insufficiency and deficiency in Europe.a
4 Lack of recognition of micronutrient insufficiencies
The prevalence of dietary insufficiency and suboptimal micronutrient status across Europe, as well as the health problems caused by micronutrient insufficiencies, are under-recognized issues. Clinical training for primary healthcare providers is generally limited with respect to micronutrients and the needs of distinct cohorts, with only basic information on their role and a focus on treatment of key deficiencies such as iron and vitamin D—i.e., frank deficiency diseases (e.g., nutritional rickets, anemia, osteoporosis, osteomalacia). The long-term impact of micronutrient inadequacy on overall health resilience is an educational gap that needs to be addressed. This lack of knowledge means that healthcare providers may not see a need to routinely assess micronutrient deficiencies or consider them to be a factor in poor health. A greater emphasis on nutrition training for health professionals, including information on how to integrate micronutrient knowledge into preventive or therapeutic care, is essential to help improve population health and wellbeing (39–41).
Furthermore, nutrition research and policies for food strategies in public health often focus on macronutrient-level issues such as calorie intake and risk of obesity (42). The role of micronutrients is often overlooked, apart from those with clear, large-scale evidence, such as vitamin D for rickets or folic acid fortification to reduce the risk of neural tube defects during pregnancy (43). This lack of acknowledgment of the significant impact of multiple micronutrient insufficiencies on public health has led to insufficient funding and research in this area. It is only recently, for example, that awareness has begun to change with respect to the target RI; these were primarily designed to prevent deficiency—but may be too low for optimal health across different populations (19, 21). For example, in the case of vitamin D, it has been suggested that the RI is insufficient to fully support immune function, muscle function, fracture risk, cardiometabolic health, and those with underlying health conditions that predispose them to vitamin D deficiency, including obesity (44, 45).
5 Food supplements are vital to bridge nutritional gaps
Eating a healthy, varied diet is the foundation to good nutrition and a fundamental self-care measure for good health (46). Yet in practice, it is not always possible to consume an adequate quantity of the right foods every day to satisfy micronutrient needs (32). Furthermore, simply preventing micronutrient deficiency is not always sufficient to provide health resilience and optimal health or reduce the risk of chronic disease for all (19, 21). Additionally, it may not be feasible to achieve sufficiently high micronutrient intakes required via diet alone, particularly in those at risk of micronutrient insufficiency such as children, teenagers, pregnant and breastfeeding women, the elderly, and those with restrictive diets (Table 1) (32). Therefore, the use of a food supplement alongside the daily diet can help to address nutritional gaps and mitigate the problems caused by suboptimal nutrition.
5.1 Impact on individuals
As the global life expectancy continues to increase (47), it is vital that individuals take steps throughout life to remain healthy into older age to minimize the risk of age-related chronic non-communicable diseases such as obesity, type 2 diabetes, and hypertension (48). Nutrition has an impact on every aspect of health, and micronutrients are essential for homeostasis and physical health, cognitive function, wellbeing, and stress resilience (15). Food supplements can play a key role in self-care to support and maintain overall health, with the potential to help reduce the risk of chronic diseases.
For example, vitamin D supplementation (especially in autumn, winter, and early spring, i.e., before the beginning of April) is recommended to avoid the occurrence of rickets and osteomalacia in northern and western Europe (49). Daily use of vitamin D supplements (50 μg; 2,000 IU) throughout the year is recommended by some for the general adult population to achieve and maintain adequate vitamin D status and prevent deficiency (50). It has been estimated that supplementation with vitamin D plus calcium in adults with osteoporosis would prevent more than half a million fractures each year in the European Union (EU) alone (51). In addition, research is showing that enhanced vitamin D status might help to reduce the risk of upper respiratory tract infections (52), and optimizing vitamin D status may reduce the risk of type 2 diabetes and improve outcomes for those with chronic health conditions (53, 54). As such, food supplements can play a critical role in promoting health across different populations. Depending on the desired outcome, different levels of supplementation may be required—highlighting the need for flexibility in supplementation regimens and the importance of supplements as a tool for achieving and maintaining resilience and optimal health.
5.2 Impact on healthcare systems and economies
In addition to the individual health benefits that could be achieved by bridging micronutrient gaps with food supplements, there could be a considerable socioeconomic impact in the form of reduced healthcare costs, greater productivity, and associated long-term savings.
For example, vitamin D facilitates the intestinal absorption of calcium and phosphorus (both required to form the bone component, hydroxyapatite) and interacts with parathyroid hormone to stimulate the renal reabsorption of calcium and to activate osteoclasts (responsible for bone resorption); vitamin D deficiency leads to impaired bone mineralization (55). Using vitamin D plus calcium supplements to help to address fractures in adults with osteoporosis in the EU could save approximately €5.7 billion every year; i.e., €5.58 saved for every €1 spent on calcium and vitamin D (51). Vitamin D supplementation may also be cost-effective in avoiding rickets in children and osteomalacia in adults (56), as well as type 2 diabetes in adults (57). In fact, it has been estimated that raising the mean concentration of 25(OH)D at the population level could reduce the incidence and mortality rates for eight of the top ten leading causes of death in the US, as well as improve adverse pregnancy and birth outcomes (44). Furthermore, better nutrition leads to a healthier population that is more productive and less prone to absenteeism (58, 59), with a consequent boost in economic growth (60). Supplementation with vitamin D, for example, could enhance productivity in the workforce (61). Over the long term, cost-effective national and regional preventive strategies such as food supplements could help to reduce the risk of chronic disease, improve health-related quality of life of individuals, relieve the nutrition-related financial burden on healthcare systems, and subsequently contribute to European economic growth.
6 Future perspectives
Research into the scale of the true prevalence of micronutrient insufficiencies across Europe will be a first step to address the lack of widespread awareness of the problem. The Zero Hidden Hunger EU initiative aims to provide better data on the prevalence, causes, and costs of micronutrient deficiencies across different regions and populations—including strategies to communicate this information to policymakers (62). This will help to inform public policy to eradicate micronutrient deficiency within Europe (37). It is also important to increase recognition that the evolving nature of the food landscape has a big impact on the prevalence of micronutrient deficiencies (24, 30). The adverse effects of climate change on nutrient levels in crops (63), for example, as well as changes in dietary consumption patterns from an omnivore diet to one that contains more plant-based food (64) and the reliance on convenience foods (65), may increase reliance on food supplements to maintain micronutrient sufficiency.
There is a need to implement proactive nutritional strategies that will promote optimal health rather than simply prevent micronutrient deficiencies (19, 21, 66). To achieve this, it will be necessary to devise appropriate dietary recommendations that better support overall health and wellbeing. The EU's “Food 2030” strategy (29) emphasizes personalized nutrition and the role of supplements in achieving optimal health. Future research should acknowledge that people require different levels and combinations of nutrients to adequately support their own optimal health—a complex issue that could be dependent on factors such as genetics, lifestyle, nutrient interactions, and other interdependent factors (67–69).
In the meantime, nutritional policies should include fortifying foods with essential micronutrients [such as folic acid (70), vitamin D (71, 72) or iodine (73–76)] and encouraging the safe use of food supplements (1, 77) to enhance nutritional status and thereby help to reduce the risk of chronic disease and minimize healthcare costs. These actions are necessary complements to dietary improvement efforts and will help to ensure a healthier, more resilient population across Europe.
Identifying those specific individuals who would benefit most from a food supplement is also essential. In the case of vitamin D, guidelines specifically target infants and young children, pregnant and breastfeeding women, people over 65, people who have low or no exposure to the sun, and people with dark skin (78). However, it is likely that most individuals would benefit from daily supplementation, particularly during the autumn, winter, and spring months—including those with conditions that predispose them to vitamin D inadequacy (50). Thus, an integrated approach for food supplements in nutrition policy is required, to ensure that the right individuals benefit from micronutrient supplementation.
To increase awareness that food supplements can help to bridge micronutrient gaps, it is vital to include more comprehensive information about the prevalence, impact, and management of micronutrient insufficiencies in the training of healthcare professionals, including how to implement this knowledge and the importance of nutritional self-care for the general public (4, 39).
6.1 Challenges in achieving optimal health and nutrition
Defining optimal health is challenging. It is often described as being a state of complete physical, mental, and social wellbeing, not merely the absence of disease—a broad definition that lacks specificity. Factors such as demographics, genetic predisposition, environmental and lifestyle factors, and pre-existing conditions vary between individuals, making it difficult to establish concrete guidelines for achieving optimal health. These factors also influence specific micronutrient requirements, further complicating the establishment of universal dietary recommendations for optimal health. Ideally, adaptive frameworks would need to be developed to enable personalized nutrition that can accommodate individual differences without oversimplifying health outcomes—a task that requires much more extensive research.
Current models for determining micronutrient needs often rely on population averages, which may not accurately reflect the needs of specific individuals. These models can overlook the nuanced interactions between micronutrients and individual health conditions. Widespread micronutrient assessment in the general population would confirm specific micronutrient needs, but any measures used would need to be accurate, standardized, quick to perform, cost-effective, and provide rapid feedback to facilitate their acceptance and adoption in clinical and public health settings (19).
Another challenge is the methodological aspects employed in some lower-quality clinical micronutrient intervention studies. For example, inadequate trial design can mean that results are less than useful for advancing our understanding of the relationship between micronutrients and health outcomes (44). It is well-established that vitamin D is crucial for bone health (79), and some intervention studies have indicated that it has beneficial effects on bone (44). Yet negative results from other studies can lead to a lack of confidence when the totality of the evidence is assessed (80). A common methodological oversight may explain the conflicting results. In this instance, it is now understood that the nature of intervention—i.e., high-dose bolus vitamin D (e.g., 100,000 IU in one dose), as opposed to a more physiologically-favorable daily lower dose of vitamin D—can lead to false negative outcomes or nil treatment effects. The current consensus is that pharmacological-strength bolus doses of vitamin D may be limited in their applications in these type of research settings (81, 82).
In addition, researchers conducting meta-analyses require access to the appropriate datasets to scientifically determine the effects of micronutrient supplementation. Analyses that use individual participant data are a more favorable form of data to capture the extent of the between-individual variability in outcomes (83). Lastly, strategic data sharing and generation will also help to improve the quality of research into both individual and public health benefits of food supplements.
7 Conclusions
Good nutrition is essential for health, resilience, and wellbeing. Food supplements are critical in bridging the gaps between insufficient dietary intake and requirements among populations and individuals. They can play an important role in enhancing individual and public health while supporting productivity and economic growth across the life-course. The under-recognition of micronutrient insufficiency among policymakers, public health officials, and healthcare providers hinders efforts to fully address this issue through easily available, cost-effective measures such as food supplements.
To effectively promote optimal health, it is crucial to recognize that nutritional needs cannot be met using a one-size-fits-all approach. As we face geoclimatic changes, evolving food systems, and varying micronutrient supplies in our diets, it is important to ensure that food supplements are adaptable to meet individual requirements, based on demographics, health conditions, and lifestyle choices. The need for flexible supplementation is underscored by the fact that micronutrient deficiencies and insufficiencies can vary widely across regions and populations. Policymakers and health professionals must focus on adaptive strategies that prioritize personalization in nutritional guidelines. This approach will involve ongoing research to better understand the interplay between genetics, lifestyle, and nutrition, enabling the development of tailored supplementation options that can effectively support diverse populations to achieve optimal health.
By incorporating food supplements into public health strategies, we can ensure better nutritional outcomes and reduce the risk of chronic diseases and strain on healthcare systems. A more comprehensive and integrated approach to nutrition policy and clinical training is needed, where food supplements are not seen as a replacement for dietary improvement, but as a necessary complement to foster healthier and a more resilient population and economy in Europe.
Author contributions
SC: Writing – original draft, Writing – review & editing. DC: Writing – original draft, Writing – review & editing. RT-S: Writing – original draft, Writing – review & editing. AG-W: Writing – original draft, Writing – review & editing. KM: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The services of the medical writer were funded by Food Supplements Europe (FSE). Bayer Consumer Care provided the Open Access fee.
Acknowledgments
We thank Patrizia Bohnhorst for her initiation of the manuscript and subsequent insightful feedback. The draft manuscript was prepared by Deborah Nock (Medical WriteAway, Norwich, UK), with full review and approval by all authors.
Conflict of interest
KM is an employee of Bayer. SC is Scientific Advisor and Consultant for the Council of Responsible Nutrition, UK. DC and RT-S are employees of Nestle Health Science. AG-W is an employee of Amway Corporation.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. European Food Safety Authority. Food Supplements (2025). Available online at: https://www.efsa.europa.eu/en/topics/topic/food-supplements (Accessed May 15, 2025).
2. van Ommen B, Fairweather-Tait S, Freidig A, Kardinaal A, Scalbert A, Wopereis S, et al. Network biology model of micronutrient related health. Br J Nutr. (2008) 99(Suppl 3):S72–80. doi: 10.1017/S0007114508006922
3. Coates PM, Bailey RL, Blumberg JB, El-Sohemy A, Floyd E, Goldenberg JZ, et al. The evolution of science and regulation of dietary supplements: past, present, and future. J Nutr. (2024) 154:2335–45. doi: 10.1016/j.tjnut.2024.06.017
4. Calder PC, Bach-Faig A, Bevacqua T, Caballero Lopez CG, Chen ZY, Connolly D, et al. Vital role for primary healthcare providers: urgent need to educate the community about daily nutritional self-care to support immune function and maintain health. BMJ Nutr Prev Health. (2023) 6:392–401. doi: 10.1136/bmjnph-2023-000755
5. Berger MM, Amrein K, Barazzoni R, Bindels L, Bretón I, Calder PC, et al. The science of micronutrients in clinical practice - report on the espen symposium. Clin Nutr. (2024) 43:268–83. doi: 10.1016/j.clnu.2023.12.006
6. Lepp HL, Amrein K, Dizdar OS, Casaer MP, Gundogan K, de Man AME, et al. Lll 44-module 3: micronutrients in chronic disease. Clin Nutr ESPEN. (2024) 62:285–95. doi: 10.1016/j.clnesp.2024.05.009
7. Mensink GB, Fletcher R, Gurinovic M, Huybrechts I, Lafay L, Serra-Majem L, et al. Mapping low intake of micronutrients across Europe. Br J Nutr. (2013) 110:755–73. doi: 10.1017/S000711451200565X
8. Giustina A, Bilezikian JP, Adler RA, Banfi G, Bikle DD, Binkley NC, et al. Consensus statement on vitamin D status assessment and supplementation: whys, whens, and hows. Endocr Rev. (2024) 45:625–54. doi: 10.1210/endrev/bnae009
9. Public Health England and the Food Standards Agency. Uk National Diet and Nutrition Survey Rolling Programme Years 9 to 11 (2016/2017 to 2018/2019) (2020). Available online at: https://www.gov.uk/government/statistics/ndns-results-from-years-9-to-11-2016-to-2017-and-2018-to-2019 (Accessed June 27, 2025).
10. Netherlands National Institute for Public Health and the Environment (RIVM). The Diet of the Dutch. Results of the Dutch National Food Consumption Survey 2019-2021 on Food Consumption and Evaluation with Dietary Guidelines (2025). Available online at: https://www.rivm.nl/en/dutch-national-food-consumption-survey/overview-surveys/dnfcs-2019-2021-1-79-years (Accessed June 27, 2025).
11. Irish Universities Nutrition Alliance (IUNA). National Adult Nutrition Survey (Nans) (2010). Available online at: https://www.iuna.net/surveyreports (Accessed June 27, 2025).
12. French French Agency on Food E Health O Safety Dubuisson C Carrillo S Dufour A . The french dietary survey on the general population (Inca3). EFSA Supporting Publications. (2017) 14:1351E. doi: 10.2903/sp.efsa.2017.EN-1351
13. Cashman KD, Dowling KG, Škrabáková Z, Gonzalez-Gross M, Valtueña J, De Henauw S, et al. Vitamin D deficiency in Europe: pandemic? Am J Clin Nutr. (2016) 103:1033–44. doi: 10.3945/ajcn.115.120873
14. Kaur J, Khare S, Sizar O, Givler A. Vitamin D deficiency. In: StatPearls. Treasure Island (FL): StatPearls Publishing (2025). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK532266/ (Accessed May 16, 2025).
15. Linus Pauling Institute. Micronutrient Information Center (2025). Available online at: https://lpi.oregonstate.edu/mic (Accessed 15 May 2025).
16. Beluska-Turkan K, Korczak R, Hartell B, Moskal K, Maukonen J, Alexander DE, et al. Nutritional gaps and supplementation in the first 1000 days. Nutrients. (2019) 11:20191127. doi: 10.3390/nu11122891
17. Hong S. Essential micronutrients in children and adolescents with a focus on growth and development: a narrative review. J Yeungnam Med Sci. (2025) 42:25. doi: 10.12701/jyms.2025.42.25
18. Maggini S, Pierre A, Calder PC. Immune function and micronutrient requirements change over the life course. Nutrients. (2018) 10:1531. doi: 10.3390/nu10101531
19. Mahadzir MDA, Tan S, Elena S, Chin EM, Garg V, Mantantzis K, et al. Towards defining optimal concentrations of micronutrients in adults to optimize health. Mech Ageing Dev. (2025) 225:112062. doi: 10.1016/j.mad.2025.112062
20. European Food Safety Authority. Drv Finder: Dietary Reference Values for the Eu (2024). Available online at: https://multimedia.efsa.europa.eu/drvs/index.htm (Accessed May 15, 2025).
21. Coppens P. The importance of food supplements for public health and well-being. World Rev Nutr Diet. (2020) 121:66–72. doi: 10.1159/000507524
23. Ljungqvist O, Man F. Under nutrition: a major health problem in Europe. Nutr Hosp. (2009) 24:369–70.
24. Yilmaz H, Yilmaz A. Hidden hunger in the age of abundance: the nutritional pitfalls of modern staple crops. Food Sci Nutr. (2025) 13:e4610. doi: 10.1002/fsn3.4610
25. Jaworowska A, Blackham T, Davies IG, Stevenson L. Nutritional challenges and health implications of takeaway and fast food. Nutr Rev. (2013) 71:310–8. doi: 10.1111/nure.12031
26. Berger MM, Shenkin A, Schweinlin A, Amrein K, Augsburger M, Biesalski HK, et al. Espen micronutrient guideline. Clin Nutr. (2022) 41:1357–424. doi: 10.1016/j.clnu.2022.02.015
27. Afshin A, Sur PJ, Fay KA, Cornaby L, Ferrara G, Salama JS, et al. Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2019) 393:1958–72. doi: 10.1016/S0140-6736(19)30041-8
28. Neufeld LM, Ho E, Obeid R, Tzoulis C, Green M, Huber LG, et al. Advancing nutrition science to meet evolving global health needs. Eur J Nutr. (2023) 62:1–16. doi: 10.1007/s00394-023-03276-9
29. European Commission. Food 2030 (2025). Available online at: https://research-and-innovation.ec.europa.eu/research-area/environment/bioeconomy/food-systems/food-2030_en (Accessed May 16, 2025).
30. Bhardwaj RL, Parashar A, Parewa HP, Vyas L. An alarming decline in the nutritional quality of foods: the biggest challenge for future generations' health. Foods. (2024) 13:877. doi: 10.3390/foods13060877
31. Mayer AB, Trenchard L, Rayns F. Historical changes in the mineral content of fruit and vegetables in the UK from 1940 to 2019: a concern for human nutrition and agriculture. Int J Food Sci Nutr. (2022) 73:315–26. doi: 10.1080/09637486.2021.1981831
32. Beal T, Ortenzi F, Fanzo J. Estimated micronutrient shortfalls of the eat-lancet planetary health diet. Lancet Planet Health. (2023) 7:e233–e7. doi: 10.1016/S2542-5196(23)00006-2
33. Bird JK, Barron R, Pigat S, Bruins MJ. Contribution of base diet, voluntary fortified foods and supplements to micronutrient intakes in the UK. J Nutr Sci. (2022) 11:e51. doi: 10.1017/jns.2022.47
34. Rippin HL, Hutchinson J, Jewell J, Breda JJ, Cade JE. Adult nutrient intakes from current national dietary surveys of European populations. Nutrients. (2017) 9:1288. doi: 10.3390/nu9121288
35. Kroner JDC, Sommer A, Fabri M. Vitamin D every day to keep the infection away? Nutrients. (2015) 7:4170–88. doi: 10.3390/nu7064170
36. Food Supplements Europe. Consumer Survey on Food Supplements in the Eu (2022). Available online at: https://foodsupplementseurope.org/wp-content/uploads/2022/07/FSE-Consumer_Survey-Ipsos-2022.pdf (Accessed May 16, 2025).
37. Cashman KD. Vitamin D and other micronutrient deficiency prevention: the role of data in informing national, regional and global policy. Proc Nutr Soc. (2024) 1–11. doi: 10.1017/S0029665124007626
38. Horizon: The EU Research & Innovation Magazine (European Commission). Hidden Hunger in Europe: Well Fed yet Undernourished (2025). Available online at: https://projects.research-and-innovation.ec.europa.eu/en/horizon-magazine/hidden-hunger-europe-well-fed-yet-undernourished (Accessed May 15, 2025).
39. Lepre B, Trigueiro H, Johnsen JT, Khalid AA, Ball L, Ray S. Global architecture for the nutrition training of health professionals: a scoping review and blueprint for next steps. BMJ Nutr Prev Health. (2022) 5:106–17. doi: 10.1136/bmjnph-2021-000354
40. Amoore BY, Gaa PK, Amalba A, Mogre V. Nutrition education intervention improves medical students' dietary habits and their competency and self-efficacy in providing nutrition care: a pre, post and follow-up quasi-experimental study. Front Nutr. (2023) 10:1063316. doi: 10.3389/fnut.2023.1063316
41. Nowson C. Opportunities for innovation in nutrition education for health professionals. BMJ Nutr Prev Health. (2020) 3:126–8. doi: 10.1136/bmjnph-2020-000135
42. Cashman KD, Kiely M. Contribution of nutrition science to the vitamin D field—clarity or confusion? J Steroid Biochem Mol Biol. (2019) 187:34–41. doi: 10.1016/j.jsbmb.2018.10.020
43. Liu J, Mantantzis K, Kaufmann L, Campos Goenaga Z, Gromova O, Kuroda K, et al. Clinical benefits and safety of multiple micronutrient supplementation during preconception, pregnancy and lactation: a review. Nutr Rev. (2025) 14:nuaf079. doi: 10.1093/nutrit/nuaf079
44. Grant WB, Wimalawansa SJ, Pludowski P, Cheng RZ. Vitamin D: evidence-based health benefits and recommendations for population guidelines. Nutrients (2025) 17:277. doi: 10.3390/nu17020277
45. Hyppönen E, Boucher BJ. Adiposity, Vitamin D requirements, and clinical implications for obesity-related metabolic abnormalities. Nutr Rev. (2018) 76:678–92. doi: 10.1093/nutrit/nuy034
46. gov.uk. Guidance. Healthy Eating: Applying All Our Health (2023–2025). Available online at: https://www.gov.uk/government/publications/healthy-eating-applying-all-our-health/healthy-eating-applying-all-our-health (Accessed May 16, 2025).
47. Leichsenring K, Sidorenko A. A Research Agenda for Ageing and Social Policy. Elgar Research Agendas (2024). doi: 10.4337/9781802208139
48. Sun X, Li X. Editorial: aging and chronic disease: public health challenge and education reform. Front Public Health. (2023) 11:1175898. doi: 10.3389/fpubh.2023.1175898
49. NHS. Rickets and Osteomalacia. Prevention (2021). Available online at: https://www.nhs.uk/conditions/rickets-and-osteomalacia/prevention/ (Accessed May 20, 2025).
50. Pludowski P, Grant WB, Karras SN, Zittermann A, Pilz S. Vitamin D supplementation: a review of the evidence arguing for a daily dose of 2000 international units (50 μg) of vitamin D for adults in the general population. Nutrients. (2024) 16:391. doi: 10.3390/nu16030391
51. Weaver CM, Bischoff-Ferrari HA, Shanahan CJ. Cost-benefit analysis of calcium and vitamin D supplements. Arch Osteoporos. (2019) 14:50. doi: 10.1007/s11657-019-0589-y
52. Jolliffe DA, Camargo CA Jr, Sluyter JD, Aglipay M, Aloia JF, Bergman P, et al. Vitamin D supplementation to prevent acute respiratory infections: systematic review and meta-analysis of stratified aggregate data. Lancet Diabetes Endocrinol. (2025) 13:307–20. doi: 10.1016/S2213-8587(24)00348-6
53. Angellotti E, Pittas AG. The role of vitamin D in the prevention of type 2 diabetes: to D or not to D? Endocrinology. (2017) 158:2013–21. doi: 10.1210/en.2017-00265
54. Jayedi A, Daneshvar M, Jibril AT, Sluyter JD, Waterhouse M, Romero BD, et al. Serum 25(Oh)D concentration, vitamin D supplementation, and risk of cardiovascular disease and mortality in patients with type 2 diabetes or prediabetes: a systematic review and dose-response meta-analysis. Am J Clin Nutr. (2023) 118:697–707. doi: 10.1016/j.ajcnut.2023.07.012
55. EFSA EFSA Panel on Dietetic Products N, Allergies. Dietary Reference Values for Vitamin D. EFSA J. (2016) 14:e04547. doi: 10.2903/j.efsa.2016.4547
56. Floreskul V, Juma FZ, Daniel AB, Zamir I, Rawdin A, Stevenson M, et al. Cost-effectiveness of vitamin D supplementation in pregnant woman and young children in preventing rickets: a modeling study. Front Public Health. (2020) 8:439. doi: 10.3389/fpubh.2020.00439
57. Zandieh N, Hemami MR, Darvishi A, Hasheminejad SM, Abdollahi Z, Zarei M, et al. Economic evaluation of a national vitamin D supplementation program among iranian adolescents for the prevention of adulthood type 2 diabetes mellitus. BMC Complement Med Ther. (2022) 22:1. doi: 10.1186/s12906-021-03474-0
58. Grimani A, Aboagye E, Kwak L. The effectiveness of workplace nutrition and physical activity interventions in improving productivity, work performance and workability: a systematic review. BMC Public Health. (2019) 19:1676. doi: 10.1186/s12889-019-8033-1
59. Rachmah Q, Martiana T, Mulyono M, Paskarini I, Dwiyanti E, Widajati N, et al. The effectiveness of nutrition and health intervention in workplace setting: a systematic review. J Public Health Res (2021) 11:2312. doi: 10.4081/jphr.2021.2312
60. McKinsey Global Institute. Prioritizing Health. A Prescription for Prosperity (2020–2025). Available online at: https://www.mckinsey.com/industries/healthcare/our-insights/prioritizing-health-a-prescription-for-prosperity (Accessed May 21, 2025).
61. Plotnikoff GA, Finch MD, Dusek JA. Impact of vitamin D deficiency on the productivity of a health care workforce. J Occup Environ Med. (2012) 54:117–21. doi: 10.1097/JOM.0b013e318240df1e
62. Zero Hidden Hunger EU. Reducing Micronutrient Deficiencies (2025). Available online at: https://www.zerohiddenhunger.eu/ (Accessed May 21, 2025).
63. Owino V, Kumwenda C, Ekesa B, Parker ME, Ewoldt L, Roos N, et al. The impact of climate change on food systems, diet quality, nutrition, and health outcomes: a narrative review. Front Clim. (2022) 4:941842. doi: 10.3389/fclim.2022.941842
64. Kam MYY. Hidden hunger: from a plant biologist's perspective. J Sci Food Agric. doi: 10.1002/jsfa.14164
65. US Department of Agriculture Economic Research Service. Consumers Balance Time and Money in Purchasing Convenience Foods (2018). Available online at: https://www.ers.usda.gov/publications/pub-details?pubid=89343 (Accessed June 26, 2025).
66. Wishart K. Increased micronutrient requirements during physiologically demanding situations: review of the current evidence. Vitamin Miner. (2017) 6:1–16. doi: 10.4172/2376-1318.1000166
67. Kaganov B, Caroli M, Mazur A, Singhal A, Vania A. Suboptimal micronutrient intake among children in Europe. Nutrients. (2015) 7:3524–35. doi: 10.3390/nu7053524
68. Donovan SM, Abrahams M, Anthony JC, Bao Y, Barragan M, Bermingham KM, et al. Personalized nutrition: perspectives on challenges, opportunities, and guiding principles for data use and fusion. Crit Rev Food Sci Nutr. (2025) 1–18. doi: 10.1080/10408398.2025.2461237
69. Ho E, Drake VJ, Michels AJ, Nkrumah-Elie YM, Brown LL, Scott JM, et al. Perspective: council for responsible nutrition science in session. Optimizing health with nutrition-opportunities, gaps, and the future. Adv Nutr. (2023) 14:948–58. doi: 10.1016/j.advnut.2023.05.015
70. Kehoe L, Walton J, Hopkins SM, McNulty BA, Nugent AP, Flynn A. Modelling the impact of mandatory folic acid fortification of bread or flour in ireland on the risk of occurrence of ntd-affected pregnancies in women of childbearing age and on risk of masking vitamin B(12) deficiency in older adults. Eur J Nutr. (2020) 59:2631–9. doi: 10.1007/s00394-019-02111-4
71. Nyakundi PN, Némethné Kontár Z, Kovács A, Járomi L, Zand A, Lohner S. Fortification of staple foods for household use with vitamin D: an overview of systematic reviews. Nutrients. (2023) 15:nu15173742. doi: 10.3390/nu15173742
72. Jääskeläinen T, Itkonen ST, Lundqvist A, Erkkola M, Koskela T, Lakkala K, et al. The positive impact of general vitamin D food fortification policy on vitamin D status in a representative adult finnish population: evidence from an 11-Y follow-up based on standardized 25-hydroxyvitamin D data. Am J Clin Nutr. (2017) 105:1512–20. doi: 10.3945/ajcn.116.151415
73. Leung AM, Braverman LE, Pearce EN. History of US iodine fortification and supplementation. Nutrients. (2012) 4:1740–6. doi: 10.3390/nu9090976
74. Food Standards Australia & New Zealand. Iodine Fortification (2019). Available online at: https://www.foodstandards.gov.au/consumer/food-fortification/iodine-fortification (Accessed June 26, 2025).
75. Guidelines Review Committee NaFSN. Guideline: Fortification of Food-Grade Salt with Iodine for the Prevention and Control of Iodine Deficiency Disorders. World Health Organization (2014). Available online at: https://www.who.int/publications/i/item/9789241507929 (Accessed May 21, 2025).
76. Prevention and Control of Iodine Deficiency in the Who European Region: Adapting to Changes in Diet and Lifestyle. Copenhagen. Licence: CC BY-NC-SA 3.0 IGO: WHO Regional Office for Europe (2024).
77. Hayes DP. Adverse effects of nutritional inadequacy and excess: a hormetic model. Am J Clin Nutr. (2008) 88:578s−81s. doi: 10.1093/ajcn/88.2.578S
78. National Institute for Health and Care Excellence. Vitamin D: Supplement Use in Specific Population Groups. Public Health Guideline Ph56 (2014–2025). Available online at: https://www.nice.org.uk/guidance/ph56 (Accessed May 21, 2025).
79. Laird E, Ward M, McSorley E, Strain JJ, Wallace J. Vitamin D and bone health: potential mechanisms. Nutrients. (2010) 2:693–724. doi: 10.3390/nu2070693
80. Méndez-Sánchez L, Clark P, Winzenberg TM, Tugwell P, Correa-Burrows P, Costello R. Calcium and vitamin D for increasing bone mineral density in premenopausal women. Cochrane Database Syst Rev. (2023) 1:CD012664. doi: 10.1002/14651858.CD012664.pub2
81. Griffin G, Hewison M, Hopkin J, Kenny RA, Quinton R, Rhodes J, et al. Perspective: vitamin D supplementation prevents rickets and acute respiratory infections when given as daily maintenance but not as intermittent bolus: implications for COVID-19. Clin Med. (2021) 21:e144–e9. doi: 10.7861/clinmed.2021-0035
82. Mazess RB, Bischoff-Ferrari HA, Dawson-Hughes B. Vitamin D: bolus is bogus-a narrative review. JBMR Plus. (2021) 5:e10567. doi: 10.1002/jbm4.10567
83. Sudfeld CR, Smith ER. What works and for whom? individual patient data meta-analyses in global nutrition research. Am J Clin Nutr. (2021) 114(Suppl 1):1s-2s. doi: 10.1093/ajcn/nqab316
84. Elmadfa I, Meyer A, Nowak V, Hasenegger V, Putz P, Verstraeten R, et al. European nutrition and health report 2009. Forum Nutr. (2009) 62:1–405. doi: 10.1159/000242367
85. Jouanne M, Oddoux S, Noël A, Voisin-Chiret AS. Nutrient requirements during pregnancy and lactation. Nutrients. (2021) 13:692. doi: 10.3390/nu13020692
86. Bradley M, Melchor J, Carr R, Karjoo S. Obesity and malnutrition in children and adults: a clinical review. Obesity Pillars. (2023) 8:100087. doi: 10.1016/j.obpill.2023.100087
87. Kehoe L, Walton J, Flynn A. Nutritional challenges for older adults in Europe: current status and future directions. Proc Nutr Soc. (2019) 78:221–33. doi: 10.1017/S0029665118002744
88. Stahl-Gugger A, de Godoi Rezende Costa Molino C, Wieczorek M, Chocano-Bedoya PO, Abderhalden LA, Schaer DJ, et al. Prevalence and incidence of iron deficiency in European community-dwelling older adults: an observational analysis of the do-health trial. Aging Clin Exp Res. (2022) 34:2205–15. doi: 10.1007/s40520-022-02093-0
89. Bakaloudi DR, Halloran A, Rippin HL, Oikonomidou AC, Dardavesis TI, Williams J, et al. Intake and adequacy of the vegan diet. A systematic review of the evidence. Clin Nutr. (2021) 40:3503–21. doi: 10.1016/j.clnu.2020.11.035
90. Welham S, Coneyworth L, Eveleigh E. The role of micronutrients and micronutrient supplements in vegetarian and vegan diets. In:Rao AV, Rao L, , editors. Dietary Supplements - Challenges and Future Research. Rijeka: IntechOpen (2023).
Keywords: Europe, food supplements, health resilience, micronutrients, nutritional gaps, nutrition policy, public health, vitamin and mineral insufficiency
Citation: Christie S, Crooks D, Thomson-Selibowitz R, Green-Woolard A and Mantantzis K (2025) Micronutrient inadequacy in Europe: the overlooked role of food supplements in health resilience. Front. Nutr. 12:1686365. doi: 10.3389/fnut.2025.1686365
Received: 15 August 2025; Accepted: 25 August 2025;
Published: 24 September 2025.
Edited by:
Luciane Bresciani Salaroli, Federal University of Espirito Santo, BrazilReviewed by:
Virginia Maria Muniz, Universidade Federal do Espírito Santo, BrazilCopyright © 2025 Christie, Crooks, Thomson-Selibowitz, Green-Woolard and Mantantzis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Konstantinos Mantantzis, a29zdGFzLm1hbnRhbnR6aXNAYmF5ZXIuY29t
 Samantha Christie
Samantha Christie David Crooks
David Crooks Rowena Thomson-Selibowitz
Rowena Thomson-Selibowitz Ashley Green-Woolard3
Ashley Green-Woolard3 Konstantinos Mantantzis
Konstantinos Mantantzis