- 1Department of Cardiology, The First Hospital of Qinhuangdao, Qinhuangdao, Hebei, China
- 2Department of Operating Room, The First Hospital of Qinhuangdao, Qinhuangdao, Hebei, China
Background: Cardiovascular disease, obesity, high blood pressure, and abnormal lipid profiles are public health issues. Dietary therapies like the DASH diet and omega-3 supplements show cardiometabolic advantages in Western populations. Few Asian cohort studies have examined the effects on obese people with dyslipidemia and hypertension.
Objective: The study aims to evaluate the associations of omega-3 supplementation and DASH diet adherence, individually and in combination on lipid profiles, blood pressure, and metabolic outcomes among Chinese obese adults.
Methods: This retrospective analysis examined data from 3,350 obese adults (BMI ≥ 28 kg/m2) with hyperlipidemia and hypertension, recruited at First Hospital of Qinhuangdao City from March 2023 to February 2025. Validated food frequency surveys and structured self-reports examined dietary adherence, while prescriptions and self-reports confirmed omega-3 consumption. LDL-C, HDL-C, triglycerides, total cholesterol, and systolic and diastolic blood pressure were the main results. Weight loss, glycemic control, and lipid/blood pressure targets were secondary outcomes. Multivariable linear, logistic, and mixed-effects regression models were used for statistical analysis.
Results: Among participants, 42.7% used omega-3 supplements, 35.2% adhered to the DASH diet, and 22.1% followed both interventions. Combined adherence was associated with the greatest improvements: LDL-C reduction (−31.7 mg/dL), HDL-C increase (+5.8 mg/dL), triglyceride reduction (−45.3 mg/dL), and systolic/diastolic BP reduction (−14.7 mmHg, all p < 0.001). Participants with combined adherence were significantly more likely to achieve both lipid and BP targets (68.6%; OR = 3.74, 95% CI: 3.20–4.40) than those with single interventions. Subgroup analyses revealed stronger benefits among older adults, women, individuals with longer obesity duration, and those with diabetes. Time-dependent analyses confirmed sustained improvements over 24 months. Adverse events were generally mild, with overall adherence remaining above 80%.
Conclusion: Combined omega-3 supplementation and DASH diet adherence was associated with synergistic improvements in lipid and blood pressure control, weight reduction, and glycemic outcomes. These findings support the implementation of integrated dietary and supplement-based strategies for cardiometabolic risk reduction in obese adults, particularly in Asian populations.
1 Introduction
Obesity is a chronic and multifactorial disorder characterized by excessive adiposity, metabolic dysregulation, and low-grade systemic inflammation. It is strongly associated with the development of hyperlipidemia, hypertension, and cardiovascular disease (1, 2). Since 1975, obesity has nearly tripled, leaving over 650 million individuals obese worldwide. Over the previous few decades, China’s obese population has grown. About 16–18% of US individuals are obese, while over 50% are overweight or obese. Along with this epidemiological shift, obesity-related comorbidities have increased significantly. About 35–40% of Chinese individuals have hyperlipidemia, and nearly 27.5%, or 245 million people, have hypertension. Since obesity, dyslipidemia, and hypertension cause cardiovascular morbidity and mortality, this disrupts public health (3, 4). The metabolic, hormonal, and circulatory pathways linking obesity, dyslipidemia, and hypertension are complex. Adipose tissue liberates fatty acids. Triglycerides and VLDL are overproduced by the liver. The liver requires time to balance them, so the cycle continues. Reduced lipoprotein lipase activity and hypertriglyceridemia result from obesity-induced insulin resistance (5). Obesity increases blood pressure through renin–angiotensin–aldosterone system activation, sympathetic nervous system overactivity, endothelial dysfunction, and vascular remodeling. Additionally, adipose-derived cytokines like TNF-α and interleukin-6 cause vascular stiffness and inflammation, worsening hyperlipidemia and hypertension in obese persons (6).
Nutritional adjustments are needed for non-pharmacological cardiometabolic disease treatment. Numerous diets lower blood pressure and enhance lipids, including DASH. The DASH diet limits salt, saturated fat, and added sugar and promotes fruits, vegetables, whole grains, legumes, nuts, and low-fat dairy. High fiber and antioxidant intakes improve insulin sensitivity, reduce oxidative stress, and change lipid metabolism, while potassium, magnesium, and calcium increase vasodilation and sodium excretion (7, 8). Several meta-analyses showed that the DASH diet improves cardiovascular health and cholesterol markers by lowering lipids and improving blood vessel function. Inhibiting diacylglycerol acyltransferase decreases liver triglyceride production. They also increase lipoprotein lipase activity. The ultimate benefit is improved β-oxidation of fatty acids (9). In addition, omega-3 fatty acids compete with arachidonic acid in eicosanoid pathways, creating resolvins and protectins. These molecules are formed by anti-inflammatory and vasodilatory mediators. All of these effects lower plasma lipids, vascular inflammation, endothelial nitric oxide bioavailability, and arterial stiffness. Clinical research indicated that high dosages of eicosapentaenoic acid reduced triglycerides by 20–30% and serious adverse cardiovascular events by 25% (10).
Omega-3 fatty acids and the DASH diet alleviate metabolic problems that cause high blood pressure and cholesterol. Nutrients and antioxidants lower blood pressure and cholesterol in the DASH diet. However, omega-3 s greatly lower triglycerides and inflammation. Combining these drugs may show their synergistic impact in cardiometabolic control. This study focused on obese adults since obesity worsens dyslipidemia and hypertension and increases treatment resistance. Obese patients have insulin resistance, chronic inflammation, and endothelial dysfunction, making them appropriate for testing combined dietary and supplemental therapy. Most large-scale research on the DASH diet and omega-3 fatty acids has been done in Western cultures, whereas Asian cohorts have provided little evidence. These populations may benefit differently due to genetics, nutrition, and supplement use. Data on their uptake and applicability in obese people with hyperlipidemia and hypertension are lacking (7, 11). Therefore, the present study aimed to conduct a retrospective analysis of omega-3 fatty acid supplementation and DASH diet adherence in the management of hyperlipidemia and hypertension among obese individuals. By evaluating sociodemographic, clinical, and lifestyle characteristics in a large Chinese cohort, this study seeks to generate population-specific evidence on the role of nutritional interventions in cardiometabolic disease prevention and management.
2 Materials and methods
2.1 Study design and source of data
This retrospective study was approved by the Ethics Committee of the First Hospital of Qinhuangdao City (Approval No. 2021C017) complies with the ethical principles proposed by the Declaration of Helsinki. The study description follows the guidelines for Strengthening and Reporting in Observational Studies (STROBE).
2.2 Study design and setting
This cross-sectional implementation research study incorporated retrospective outcome data collection to evaluate the impact of omega-3 fatty acid supplementation and adherence to the Dietary Approaches to Stop Hypertension (DASH) diet on the management of hyperlipidemia and hypertension among obese adults. The study was undertaken at Qinhuangdao’s First Hospital from March 2023 to February 2025. To assess how nutritional intervention quality affects cardiometabolic system health, the study quantified dietary adherence, supplement use, and clinical results.
2.3 Participants
Participants were sequentially enrolled in the endocrinology and cardiology clinic. Participants had to be obese (28 kg/m2), 30–70 years old, and have hyperlipidemia and/or hypertension for 6 months. Participants were excluded from the trial due to secondary hypertension, familial hypercholesterolemia, chronic kidney disease (stage ≥3), terminal illness, and insufficient clinical and dietary data. From March 2023 to February 2025, 3,350 registered and selected after the inclusion criteria. Selectivity bias was avoided by analyzing participant demographics throughout enrollment. The sample size was sufficient to detect a 5 mmHg systolic blood pressure change or a 10 mg/dL LDL cholesterol difference between intervention and non-intervention groups with 80% power and α = 0.05 significance. Successful cohorts provide primary and subgroup analyses with statistical power. DASH diet adherence was assessed using a validated food frequency questionnaire. The questionnaire assessed fruit, vegetable, whole grain, low-fat dairy, lean protein, salt, and saturated fat intake. The highest tertile was “high adherence.” Prescription records, supplement purchase verification, and structured patient self-reports assessed omega-3 supplementation. Regular use was 1 g of combined EPA and DHA daily for 6 months before effect testing.
2.4 Fidelity and exposure assessment
Implementation adherence (degree to which patients followed DASH guidelines), dose (frequency and duration of omega-3 supplementation), quality of delivery (accuracy of dietary counseling and supplement prescription by healthcare providers), and patient responsiveness were assessed to determine fidelity of dietary interventions. Fidelity grading took into account nutritional intake, medical records, and patient adherence. Dual coding of 20% of food recollections yielded 0.87–0.93 reliability coefficients. Weighted averages of standardized domain scores yielded composite adherence scores.
2.5 Data collection and measures
The study measured BMI, lifestyle factors, comorbidities, medication use, and standardized lipid and blood pressure markers. Verified nutritional adherence and retrospective healthcare data enabled cross-sectional analyses.
2.6 Statistical analysis
All data were analyzed using standard statistical methods (SPSS version 25), using categorical variables as frequencies (%) and continuous variables as mean ± SD or median (IQR). Tests for group differences included Chi-square, ANOVA, Kruskal–Wallis, p-trend, and subgroup/multivariable regression analyses, identifying treatment interactions and independent predictors (p < 0.05).
3 Results
3.1 Sociodemographic, clinical, and dietary characteristics
The present study included 3,350 people with an average age of 51.8 ± 9.2 years. 52.7% of participants were female. About 31.9% of the population had completed elementary school, 38.6% had completed middle school, and 29.4% had completed high school. 32% of participants reported a moderate family income, 53% reported a low family income, and 13% reported a high income. 45.1% of married adults were married. Clinically, the average BMI was 32.8 kg/m2 with a standard deviation of 4.4 kg/m2. 46.9% had Class I obesity, 31.2% Class II, and 18.8% Class III. Seventy-one percent of patients had hypertension, with mean systolic and diastolic blood pressures of 147.2 ± 16.5 and 91.9 ± 9.6 mmHg, respectively. Hyperlipidemia was observed in 74.8% of participants, with mean total cholesterol, LDL-C, HDL-C, and triglyceride levels of 241.3 ± 40.6 mg/dL, 151.8 ± 35.7 mg/dL, 42.1 ± 8.7 mg/dL, and 211.6 ± 58.5 mg/dL, respectively. This study shows that 46.8% had a family history of cardiovascular disease, and 32.1% smoked. The DASH diet was followed by 35.5% of individuals, while 42.2% used omega-3 supplements. Also, 22.3% followed both therapies. Participants’ nutrition and treatment practices are the subject of this study. Similar to the prior study, 42.1% of the population received no treatments. The DASH diet was followed for an average of 2.2 years. However, the average period they took omega-3 supplements was 2.3 ± 1.4 years (Table 1).
3.2 Dietary adherence and use of supplements
Dietary adherence and supplement use indicate how well people follow diets with nutritional assistance. In the study group (n = 3,350), 42.2% reported Omega-3 supplementation compliance, with no significant difference between males (41.2%) and females (43.1%; p = 0.26). Overall, the Omega-3 adherence score was 6.7 ± 1.8, with females achieving higher adherence than males (7.0 ± 1.8 vs. 6.4 ± 1.9; p = 0.01). The median Omega-3 use was 2.0 years (IQR 1.0–3.0) and similar between genders (p = 0.41). The DASH diet was adhered to by 35.5% of participants, with a larger proportion of females (37.0% vs. 33.9%; p < 0.001) than males. A mean DASH adherence score of 5.8 ± 2.0 was observed, with females scoring higher than males (6.0 ± 2.1 vs. 5.5 ± 1.9; p < 0.00). The median DASH diet adherence was 1.8 years (IQR 1.0–2.5), with no significant gender difference (p = 0.09). Omega-3 supplementation and the DASH diet were followed by 22.3% of individuals, with 24.9% of men and 19.9% of women (p = 0.004). The mean total adherence lasted 1.9 ± 1.1 years, with females having a significantly longer duration (2.1 ± 1.1 vs. 1.8 ± 1.0; p = 0.03) (Table 2).
3.3 Lipid profile outcomes among participants
Healthy lipids reduce cardiovascular risk, while excessive levels raise heart disease and stroke risk. The combined Omega-3 supplementation and DASH diet group had the best lipid profile and blood pressure improvements at follow-up. Mean total cholesterol was lowest in the combined group (199.1 ± 30.1 mg/dL; median 199 mg/dL, IQR 180–222), compared with 211.2 ± 31.9 mg/dL in the Omega-3 only group and 207.8 ± 31.2 mg/dL in the DASH-only group (p < 0.001). LDL-C followed a similar pattern, with the combined group achieving the lowest levels (119.1 ± 22.6 mg/dL; median 119 mg/dL, IQR 104–137) versus 135.1 ± 25.6 mg/dL and 130.8 ± 24.9 mg/dL in the Omega-3 and DASH-only groups, respectively (p < 0.001). HDL-C was highest in the combined group (51.6 ± 8.7 mg/dL; median 53 mg/dL, IQR 47–59), reflecting a greater cardioprotective effect, while triglycerides were lowest (156.7 ± 44.3 mg/dL; median 155 mg/dL, IQR 135–180) compared with the other groups (p < 0.001 for both). The combined group had lower systolic blood pressure (136.3 ± 14.1 mmHg; median 141 mmHg, interquartile range 132–150) than the omega-3 fatty acid (141.9 ± 15.2 mmHg) and DASH (140.4 ± 14.8 mmHg) groups. The combined group had comparable diastolic blood pressure patterns, with a mean of 85.1 ± 8.2 mmHg (median of 89, interquartile range of 83–85 mmHg), compared to Omega-3 and DASH-only groups that reached 89.8 ± 9.2 and 89.1 ± 8.9 mmHg (p < 0.001) (Table 3).
3.4 Anthropometric measurements among participants
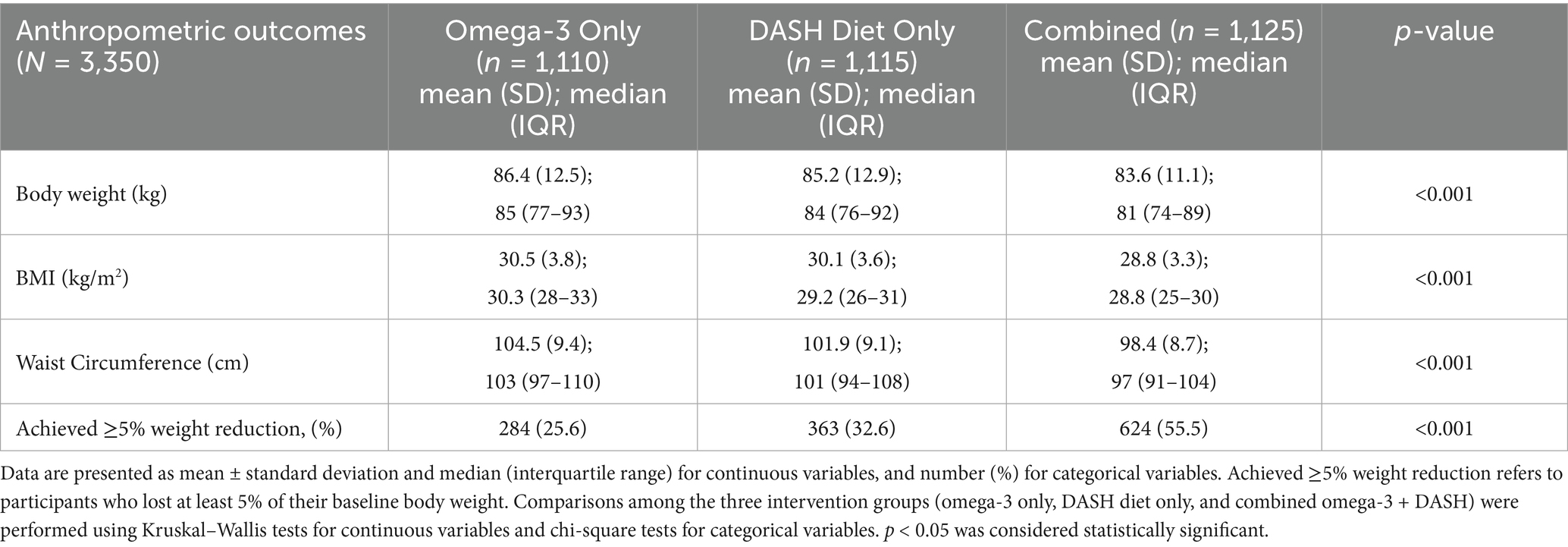
Anthropometric measurements are physical assessments of body size, shape, and composition, such as height, weight, BMI, and waist circumference. At the 24-month follow-up, participants in the combined Omega-3 and DASH diet group exhibited the most significant improvements in anthropometric measures compared to those in the Omega-3 only and DASH diet only groups. The mean body weight was lowest in the combined group (83.6 ± 11.1 kg; median 81 kg, IQR 74–89), followed by the DASH diet only group (85.2 ± 12.9 kg; median 84 kg, IQR 76–92), and the Omega-3 only group (86.4 ± 12.5 kg; median 85 kg, IQR 77–93) (p < 0.001). Similarly, the mean BMI was lowest in the combined group (28.8 ± 3.3 kg/m2; median 28.8 kg/m2, IQR 25–30), compared to the DASH diet only group (30.1 ± 3.6 kg/m2; median 29.2 kg/m2, IQR 26–31), and the Omega-3 only group (30.5 ± 3.8 kg/m2; median 30.3 kg/m2, IQR 28–33) (p < 0.001). Waist circumference also showed the greatest reduction in the combined group (98.4 ± 8.7 cm; median 97 cm, IQR 91–104), followed by the DASH diet only group (101.9 ± 9.1 cm; median 101 cm, IQR 94–108), and the Omega-3 only group (104.5 ± 9.4 cm; median 103 cm, IQR 97–110) (p < 0.001). Notably, the combined intervention group achieved the highest proportion of participants with ≥5% weight reduction (55.5%), compared to 32.6% in the DASH diet only group and 25.6% in the Omega-3 only group (p < 0.001) (Table 4).
3.5 Glycemic and metabolic outcomes among participants
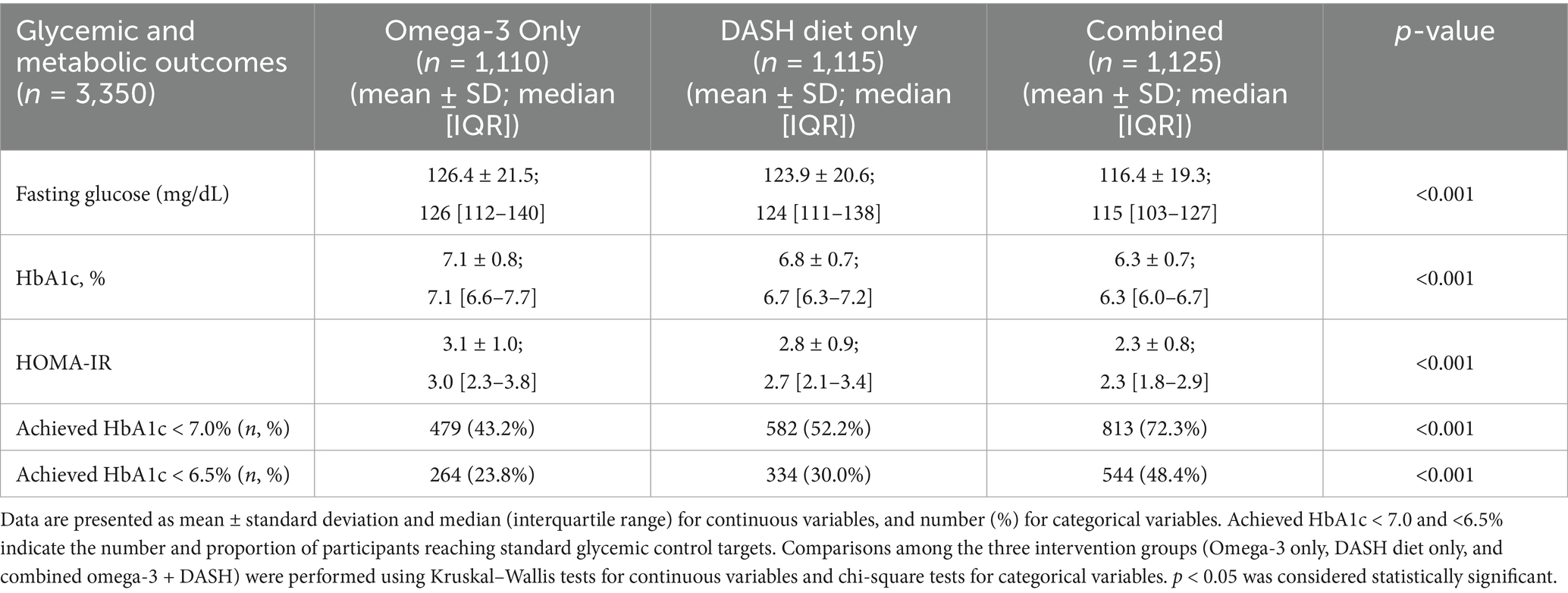
Glycemic and metabolic outcomes refer to the effects of diet or interventions on blood sugar control, insulin response, and overall metabolic health. Participants in the combined Omega-3 supplementation and DASH diet group showed the most substantial improvements in glycemic and metabolic parameters compared with the Omega-3 only and DASH-only groups. The mean fasting glucose was lowest in the combined group (116.4 ± 19.3 mg/dL; median 115 mg/dL, IQR 103–127), compared with 126.4 ± 21.5 mg/dL in the Omega-3 only group and 123.9 ± 20.6 mg/dL in the DASH-only group (p < 0.001). Similarly, mean HbA1c was lowest in the combined group (6.3 ± 0.7%; median 6.3%, IQR 6.0–6.7) versus 7.1 ± 0.8% in the Omega-3 group and 6.8 ± 0.7% in the DASH-only group (p < 0.001). Insulin resistance, measured by HOMA-IR, was also significantly reduced in the combined group (2.3 ± 0.8; median 2.3, IQR 1.8–2.9) compared with the Omega-3 only (3.1 ± 1.0) and DASH-only groups (2.8 ± 0.9; p < 0.001). The combined group had the largest proportion of patients meeting target HbA1c levels, with 72.3% obtaining <7.0 and 48.4% achieving <6.5%, compared to 43.2 and 23.8% in the Omega-3 only group and 52.2 and 30.0% in the DASH-only group (p < 0.001) (Table 5).
3.6 Combined effects of omega-3 and DASH diet on lipid and blood pressure
Participants receiving both Omega-3 supplementation and DASH diet adherence demonstrated the most pronounced improvements in lipid and blood pressure outcomes compared with either intervention alone. Mean LDL-C reduction was greatest in the combined group (−31.7 ± 9.1 mg/dL; β = −31.3, 95% CI –32.5 to −30.1) compared with −18.7 ± 7.3 mg/dL in the Omega-3 only group and −22.3 ± 8.1 mg/dL in the DASH-only group (p < 0.001; interaction p = 0.012). HDL-C increased most in the combined group (+5.8 ± 2.0 mg/dL; β = +5.6, 95% CI 5.3–5.9) versus +3.3 ± 1.9 mg/dL and +3.7 ± 2.0 mg/dL in the Omega-3 only and DASH-only groups, respectively (p < 0.001; interaction p = 0.021). Triglyceride reduction was also largest in the combined group (−45.3 ± 14.0 mg/dL; β = −44.9, 95% CI –46.7 to −43.1) compared with −28.3 ± 12.1 mg/dL and −31.7 ± 13.0 mg/dL in the Omega-3 and DASH-only groups (p < 0.001; interaction p = 0.009). Observable improvements occurred in blood pressure as well. The combined group showed the greatest reduction in systolic and diastolic BP (−14.7 ± 4.7 mmHg; β = −14.4, 95% CI –15.1 to −13.9), which is significantly greater than Omega-3 or DASH-only interventions (p < 0.001; interaction p = 0.015 and 0.022, respectively). Participants in the combined group achieved higher lipid and blood pressure targets (772/1125, 68.6%; OR = 3.74, 95% CI 3.20–4.40) in comparison to DASH-only (43.7%; OR = 1.31) and Omega-3-only (38.9%; reference), indicating a harmonious effect on cardiometabolic outcomes (p < 0.001) (Table 6).
3.7 Subgroup analyses of combined omega-3 and DASH diet effects on lipid and blood pressure
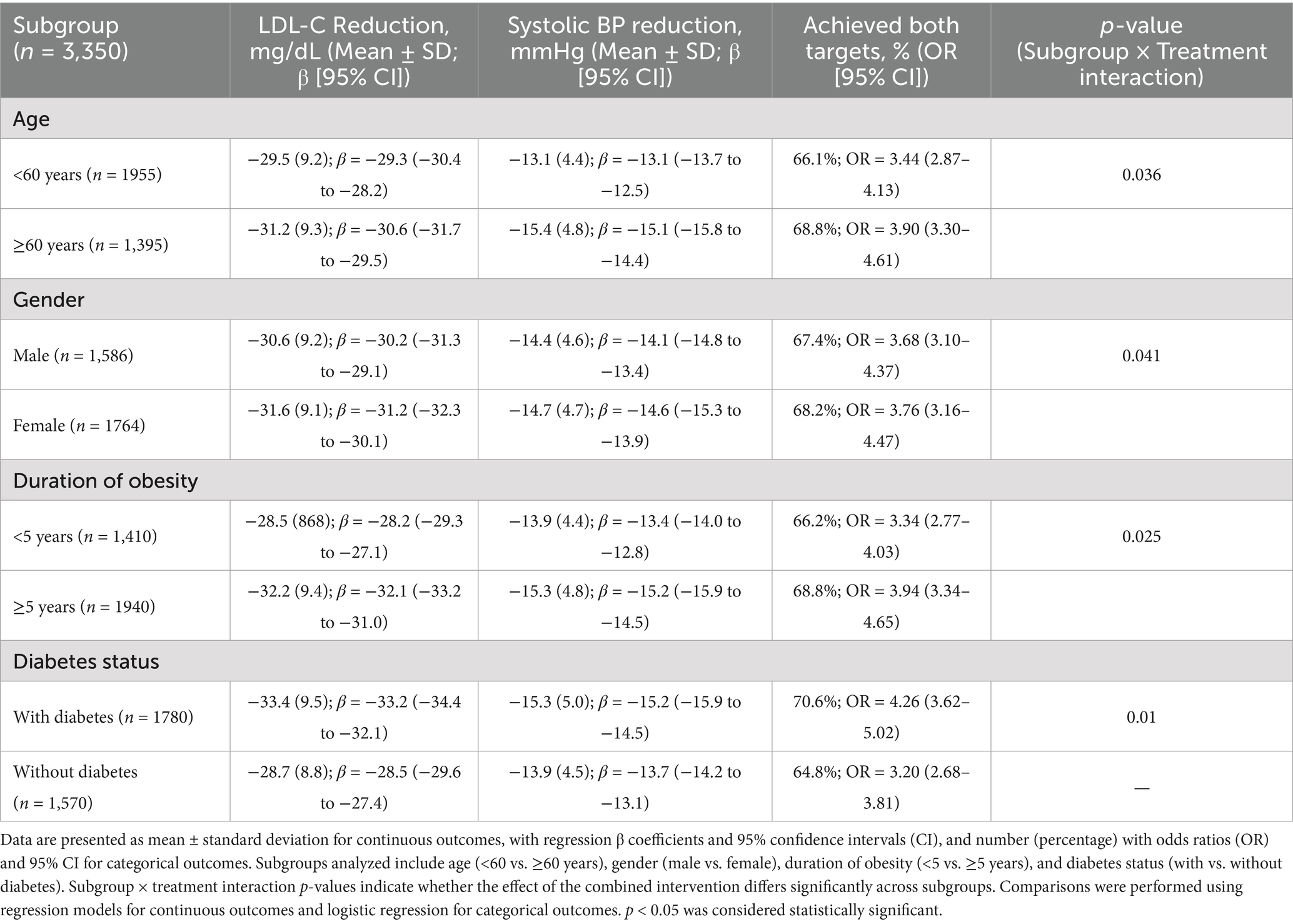
Omega-3 supplementation and DASH diet intervention reduced LDL-C, systolic blood pressure, and met both targets in all categories, with considerable variation in degree. Participants aged ≥60 years experienced slightly greater LDL-C reduction (−31.2 ± 9.3 mg/dL; β = −30.6, 95% CI –31.7 to −29.5) and systolic BP reduction (−15.4 ± 4.8 mmHg; β = −15.1, 95% CI –15.8 to −14.4) compared with those <60 years, and a higher proportion achieved both targets (68.8% vs. 66.1%; OR = 3.90 vs. 3.44; interaction p = 0.036). Gender-based analysis showed slightly greater improvements among females, with LDL-C reduction of −31.6 ± 9.1 mg/dL (β = −31.2, 95% CI –32.3 to −30.1) and systolic BP reduction of −14.7 ± 4.7 mmHg (β = −14.6, 95% CI –15.3 to −13.9), resulting in 68.2% achieving both targets (OR = 3.76; interaction p = 0.041). Duration of obesity influenced outcomes, with participants obese ≥5 years demonstrating larger LDL-C reductions (−32.2 ± 9.4 mg/dL; β = −32.1, 95% CI –33.2 to −31.0) and systolic BP decreases (−15.3 ± 4.8 mmHg; β = −15.2, 95% CI –15.9 to −14.5) compared with those obese <5 years, and a higher proportion achieving both targets (68.8% vs. 66.2%; interaction p = 0.025). Diabetes status was a strong modifier of intervention effectiveness: participants with diabetes achieved the greatest LDL-C reduction (−33.4 ± 9.5 mg/dL; β = −33.2, 95% CI –34.4 to −32.1), systolic BP reduction (−15.3 ± 5.0 mmHg; β = −15.2, 95% CI –15.9 to −14.5), and proportion achieving both targets (70.6%; OR = 4.26) compared with non-diabetic participants (64.8%; OR = 3.20; interaction p = 0.01) (Table 7).
3.8 Time-dependent trends in lipid, blood pressure, and weight outcomes by intervention
All intervention groups showed improvement in weight, blood pressure, and lipids at 24 months interval. Total cholesterol steadily decreased, with the Omega-3 + DASH group showing the greatest reduction from baseline (239.4 ± 32.1 mg/dL) to 24 months (201.5 ± 25.2 mg/dL). The combined group’s LDL-C reduced from 148.8 ± 24.7 mg/dL at baseline to 113.9 ± 20.1 at 24 months. HDL-C levels increased in all groups, especially the combination group (from 38.7 ± 8.3 to 44.6 ± 8.0 mg/dL). The combo intervention was the most effective in lowering triglycerides (from 186.5 ± 43.1 to 153.9 ± 36.1 mg/dL). The combined group had the greatest decrease in systolic and diastolic blood pressures over time (systolic BP: 148.4 ± 12.7 mmHg at baseline to 131.2 ± 9.4 at 24 months; diastolic BP: 92.5 ± 82.6 ± 7.1 mmHg). The combined group experienced the most weight decrease (≥5%) at 24 months (46.6%). 58.7% met cholesterol and blood pressure objectives at 24 months. Combining Omega-3 supplementation with the DASH diet led to sustained cardiometabolic advantages (p-trend < 0.001) (Table 8).
3.9 Adverse events and safety outcomes in omega-3 and DASH diet interventions
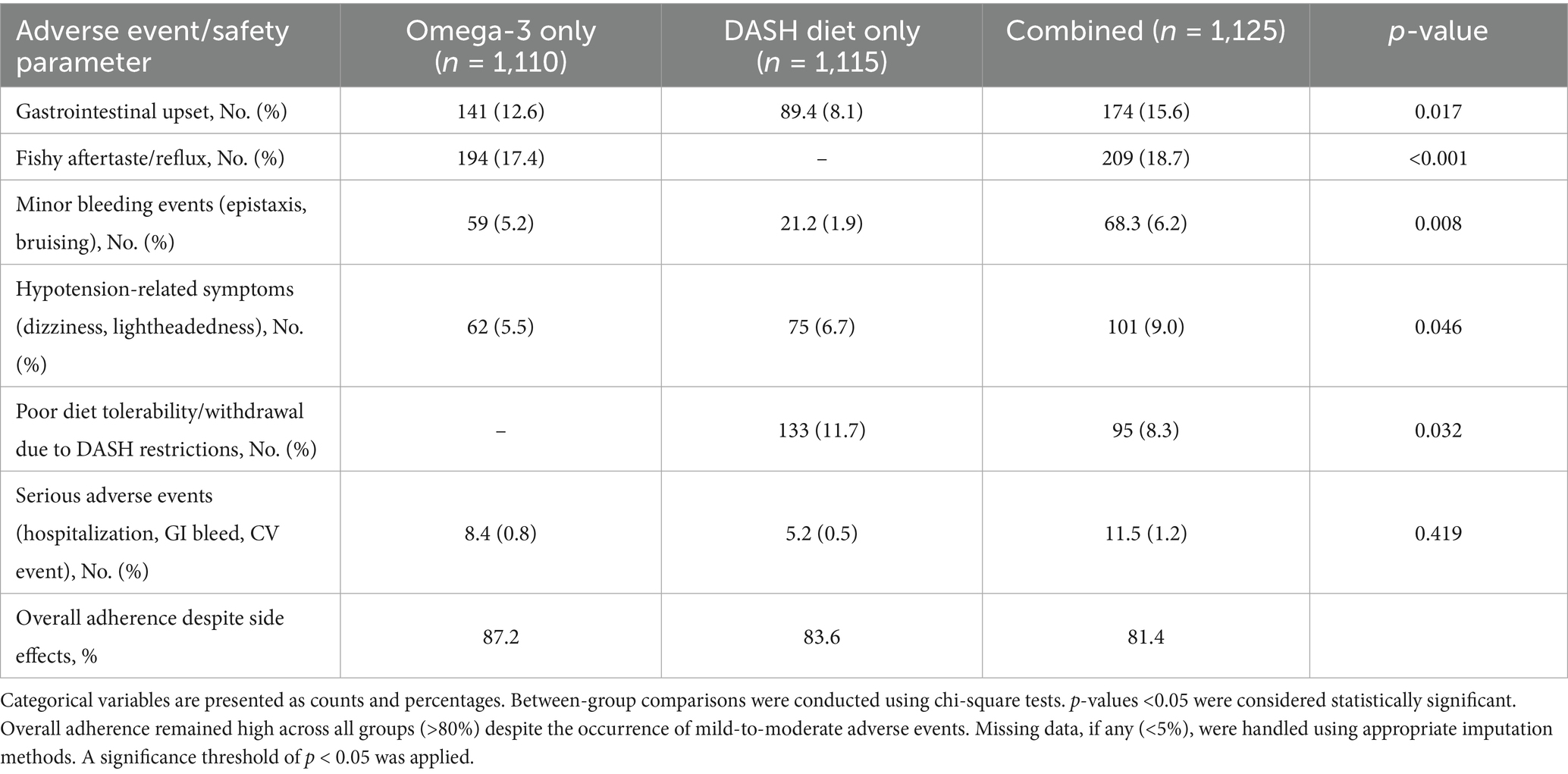
Adverse events and safety outcomes evaluate the risks, side effects, and overall tolerability of omega-3 and DASH diet interventions. Table 9 summarizes adverse events and safety outcomes for participants receiving omega-3 supplementation, the DASH diet, or a combination of both interventions. Gastrointestinal upset was reported in 12.6% of the omega-3 group, 8.1% of the DASH diet group, and 15.6% of the combined group, showing a statistically significant difference (p = 0.017). Fishy aftertaste or reflux occurred in 17.4% of the omega-3 group and 18.7% of the combined group, with no data available for the DASH diet group, and this difference was highly significant (p < 0.001). Minor bleeding events were observed in 5.2% of the omega-3 group, 1.9% of the DASH diet group, and 6.2% of the combined group, with a significant difference across groups (p = 0.008). Hypotension-related symptoms were reported in 5.5% of the omega-3 group, 6.7% of the DASH diet group, and 9.0% of the combined group (p = 0.046). Poor diet tolerability or withdrawal due to DASH diet restrictions was 11.7% in the DASH diet group and 8.3% in the combined group, while not applicable to the omega-3 group, with a significant difference (p = 0.032). Hospitalization, gastrointestinal bleeding, and cardiovascular events were rare: 0.8% in the omega-3 group, 0.5% in the DASH diet group, and 1.2% in the combination group (p = 0.419). Omega-3 had 87.2% adherence, DASH 83.6%, and the combined group 81.4% despite adverse effects.
3.10 Multivariable regression analysis of lipid and blood pressure
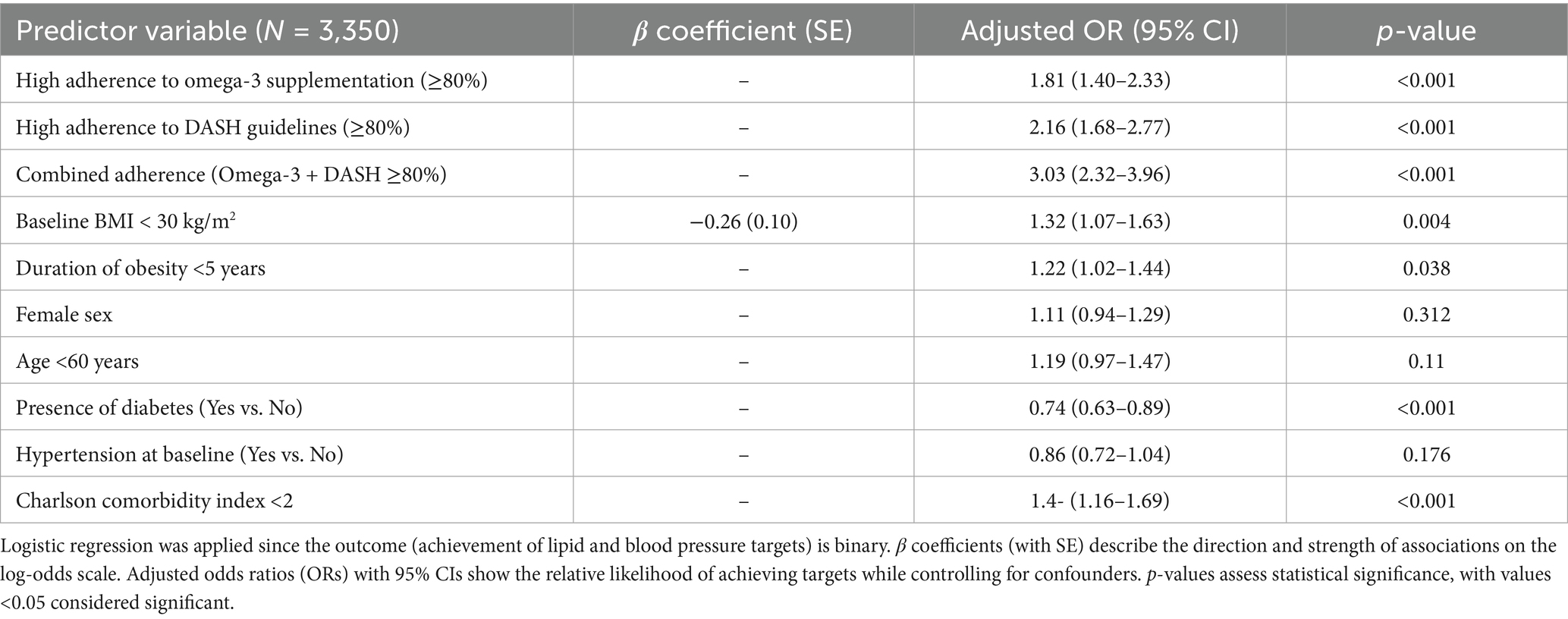
Multivariable regression showed that adherence considerably affects outcomes. High omega-3 supplementation adherence (≥80%) significantly enhanced odds of attaining cholesterol and blood pressure targets (OR: 1.81, 95% CI: 1.40–2.33, p < 0.001), while high DASH diet adherence alone had even greater odds (OR: 2.16, 95% CI: 1.68–2.77, p < 0.001) Adherence to both medications resulted in the best success rate (OR: 3.03, 95% CI: 2.32–3.96, p < 0.001). Among baseline characteristics, participants with BMI < 30 kg/m2 (β = −0.26, SE = 0.10; OR: 1.32, 95% CI: 1.07–1.63, p = 0.004), obesity duration <5 years (OR: 1.22, 95% CI: 1.02–1.44, p = 0.038), and a Charlson comorbidity index <2 (OR: 1.40, 95% CI: 1.16–1.69, p < 0.001) showed significantly greater odds of achieving targets. In contrast, female sex (OR: 1.11, 95% CI: 0.94–1.29, p = 0.312), younger age <60 years (OR: 1.19, 95% CI: 0.97–1.47, p = 0.11), and baseline hypertension (OR: 0.86, 95% CI: 0.72–1.04, p = 0.176) were not significant predictors. Diabetes was found to be negatively linked with outcomes (OR: 0.74, 95% CI: 0.63–0.89, p < 0.001), indicating a lower likelihood of achieving cholesterol and BP control (Table 10).
4 Discussion
This study investigates the comparative and combined effects of Omega-3 fatty acids and the DASH diet on lipid profile and blood pressure regulation in obese individuals with hyperlipidemia and hypertension. According to previous studies, obesity is strongly linked to hypertension and dyslipidemia (11, 12). The Dietary Approaches to Stop Hypertension (DASH) trial found that diet changes help to lower blood pressure (13, 14). Many patients did not follow DASH guidelines, showing an implementation gap similar to those in other Asian nations where cultural eating patterns and minimum nutritional guidance are not widely accepted (15). Our study showed that people are more adherent to omega-3 supplements than the DASH diet, which is consistent with international trends in triglyceride lowering (16). High-risk patients may benefit from dose-dependent Omega-3 fatty acid triglyceride and cardiovascular event reduction. Due to our mean triglyceride level of 212 mg/dL, omega-3 intervention is necessary. VLDL, triglycerides, inflammation, and atherosclerotic plaques decrease in the liver (17, 18). Limiting sodium, increasing potassium, magnesium, and fiber, and reducing saturated fat may improve endothelial function, insulin sensitivity, and vascular tone, according to previous studies (7, 19). A subset of participants using DASH and omega-3 simultaneously may have caused the combined group’s synergistic improvements in lipid and blood pressure outcomes, supporting controlled studies that show multi-targeted lifestyle and nutraceutical interventions work better than isolated interventions (12, 20). Recently, a national survey in China demonstrated that obesity prevalence has consistently increased over the previous decade (4). This study indicated that our community has high hypertension and hyperlipidemia and low evidence-based diet adherence, suggesting public health programs should improve. Practical adherence and obesity-related cardiovascular disease combination methods are stressed. This study proves DASH and omega-3 therapy’s cardiometabolic benefits. According to US and European data, women had greater diet quality and cardioprotective diet engagement than men (21). For instance, analysis from the Nurses’ Health Study and Health Professionals Follow-Up Study indicated that women were more likely to sustain adherence to DASH and Mediterranean-style diets over long-term follow-up (22). Asian women are more likely to use omega-3 supplements for weight and cardiovascular risk. Our omega-3 compliance rate was 42.2%, compared to 20–35% in Western trials. Our findings are consistent with urban Chinese groups with high nutraceutical therapy awareness (23–25). Similar to Chinese data, DASH diet acceptance has remained below 40% despite its proven benefits in lowering blood pressure and improving cardiometabolic outcomes (26). The low total adherence rate (22.3%) suggests that multiple concurrent dietary treatments are difficult to apply, validating recent studies that suggest dietary complexity may affect compliance in real life (27). Furthermore, females may have longer combined adherence as they are more health-conscious and adopt proactive preventative approaches (28). These findings show that obese people may need gender-specific interventions to increase long-term omega-3 supplementation and DASH dietary recommendations.
It is generally known that omega-3 fatty acids decrease triglycerides and enhance HDL-C. Meta-analyses suggest a 20–30% decline in triglycerides and a 5–10% increase in HDL-C (18, 29). Similarly, the DASH diet has also been associated with reductions in total cholesterol and LDL-C, as demonstrated in the PREMIER and OmniHeart trials, which reported LDL-C reductions of 10–15 mg/dL over 6 months (26, 30). Omega-3 and DASH may cooperate. Omega-3 s target triglyceride-rich lipoproteins, while DASH reduces saturated fat, salt, LDL-C, and total lipids. Recent observational and interventional research support multi-target diets. Recent studies found that fish-based and DASH diets regulated lipids better than either alone (31). A meta-analysis found that multi-component diets improved cardiometabolic outcomes over single-therapy (32). Previous researches showed that obese people with hyperlipidemia and hypertension benefit from a combined strategy (14, 20, 33, 34). Recent studies found that multi-component diet and lifestyle treatments could lower SBP by 10 mmHg, improving hypertension management (7, 14). Omega-3 supplementation with DASH diet adherence improved weight, BMI, and waist circumference more than either alone. Research shows DASH fruits, veggies, healthy grains, and low-fat dairy prevent belly obesity and small weight loss. Omega-3 s lower inflammation, regulate lipids, and improve insulin sensitivity (26, 35). The combined intervention may result in ≥5% weight loss due to synergistic effects such enhanced satiety, reduced calorie intake, and improved metabolic regulation. Omega-3 supplementation with the DASH diet permanently reduces weight and improves central adiposity in overweight and obese persons.
The DASH diet also improves glycemic control and insulin sensitivity in patients with metabolic syndrome. According to randomized controlled studies and meta-analyses, the DASH diet decreases fasting glucose and HbA1c by emphasizing high fiber, low sodium, and reduced refined carbs (36, 37). Omega-3 fatty acids reduce inflammation and increase cell membrane fluidity, which may stimulate insulin signaling, while the DASH diet lowers food glycemic load to optimize postprandial glucose levels. A recent study found that Mediterranean-style diets with omega-3-rich foods improved glycemic results more than either alone (38). A systematic study found that DASH diet adherence lowered HbA1c and insulin resistance, especially when paired with weight loss and nutrient-specific supplementation (39). The current study found that omega-3 fatty acid supplementation with the DASH diet improves glycemic and metabolic outcomes more than either alone. This comprehensive metabolic control and cardiovascular risk reduction approach may assist type 2 diabetes and prediabetes patients. Omega-3 fatty acids and the DASH diet enhance cardiometabolic risk factors individually and synergistically, according to this study. Hypertensive and metabolic syndrome patients’ cholesterol and blood pressure drop on the DASH diet (22, 35, 40). Meanwhile, omega-3 fatty acids are well documented to reduce triglycerides and modestly increase HDL-C, though their effect on LDL-C and blood pressure is less robust (7, 13, 33). Synergistic benefits of DASH, omega-3 s, and mixed diets, such as Mediterranean diets with omega-3, improve lipid indicators and endothelial function (7, 16, 20, 38, 41). The REDUCE-IT trial found that omega-3 fatty acid therapy improved triglyceride reduction and cardiovascular outcomes (42, 43). A study showed weight loss in the first year, partial weight rebound, and weak dietary and supplement adherence (35). This study shows that omega-3 supplementation within a DASH framework may be the optimal nutritional therapy for cardiovascular disease patients, delivering clinically significant benefits. Despite strong adherence, omega-3 supplementation caused gastrointestinal discomfort (44), fishy taste, and slight bleeding. The DASH diet lowers blood pressure, which may worsen hypotension. The strict diet raised withdrawal rates, emphasizing long-term adherence issues (14, 45).
This study validates prior findings that adherence improves cardiometabolic health. The DASH and PREMIER studies found that diet compliance reduced blood pressure and cholesterol more (46). Similarly, meta-analyses of omega-3 supplementation show that dose and adherence strongly influence lipid and blood pressure outcomes (47, 48). The synergistic advantage of omega-3 and DASH here matches evidence showing multi-component lifestyle therapies improve cardiovascular risk variables more than single programs (7, 36). Diabetics responded less, corroborating prior results that severe metabolic dysfunction degrades lifestyle-only therapy and typically requires pharmacological co-management (49, 50). These data underline the need of adherence and early intervention in improving cardiometabolic outcomes with the Dash diet and Omega-3 supplementation.
5 Conclusion
DASH diet and omega-3 fatty acid supplementation improve lipid metabolism, blood pressure regulation, glycemic control, and anthropometrics among obese adults having hyperlipidemia and hypertension. Omega-3 fatty acids with the DASH diet may reduce hepatic triglyceride synthesis, increase β-oxidation, and minimize vascular inflammation. The DASH diet is enriched with fiber and antioxidants, which improve endothelial function, vasodilation, and insulin sensitivity. Combining interventions increased the likelihood of meeting dual cholesterol and blood pressure targets three times, highlighting its therapeutic importance for cardiometabolic risk reduction. Subgroup studies show that older adults, women, people with long-term obesity, and diabetics are more affected, suggesting precision nutrition interventions may be stratified. Prospective, multicenter, randomized trials are needed to demonstrate causality and identify omega-3 supplement content, dosage, and duration in conjunction with DASH adherence. Synergistic effects will be explained by mechanistic studies using biomarkers of inflammation, endothelial function, and lipid kinetics. Digital health tools, behavioral interventions, and culturally specific education may improve long-term adherence and clinical effectiveness. Expanding the study to other Asian communities with different genetic and dietary origins can help produce population-specific, evidence-based nutritional advice to reduce obesity-related cardiovascular disease.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving humans were approved by Ethics Committee of the First Hospital of Qinhuangdao City. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
HY: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. YQZ: Writing – original draft, Writing – review & editing. YJZ: Formal analysis, Writing – original draft, Writing – review & editing. LR: Data curation, Visualization, Writing – original draft, Writing – review & editing. LM: Conceptualization, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Financial support for this project was provided by the Hebei Medical Science Research Project Plan (Approval No. 20231885).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Guerra, JV, Dias, MM, Brilhante, AJ, Terra, MF, Garcia-Arevalo, M, and Figueira, ACM. Multifactorial basis and therapeutic strategies in metabolism-related diseases. Nutrients. (2021) 13:2830. doi: 10.3390/nu13082830
2. Masood, I, Noreen, S, Raza, K, Khalid, W, Rahim, MA, and Mohamedahmed, KA. Effect of ketogenic diet and hypocaloric Mediterranean diet on metabolic and endocrine parameter in women suffering from polycystic ovary syndrome. Int J Food Prop. (2023) 26:3187–96. doi: 10.1080/10942912.2023.2275528
3. Lu, X, Jin, Y, Li, D, Zhang, J, Han, J, and Li, Y. Multidisciplinary progress in obesity research. Genes. (2022) 13:1772. doi: 10.3390/genes13101772
4. Zhang, Y, Zhang, W-Q, Tang, W-W, Zhang, W-Y, Liu, J-X, Xu, R-H, et al. The prevalence of obesity-related hypertension among middle-aged and older adults in China. Front Public Health. (2022) 10:865870. doi: 10.3389/fpubh.2022.865870
5. Qureshi, K, and Abrams, GA. Metabolic liver disease of obesity and role of adipose tissue in the pathogenesis of nonalcoholic fatty liver disease. World J Gastroenterol: WJG. (2007) 13:3540–53. doi: 10.3748/wjg.v13.i26.3540
6. Kawarazaki, W, and Fujita, T. The role of aldosterone in obesity-related hypertension. Am J Hypertens. (2016) 29:415–23. doi: 10.1093/ajh/hpw003
7. Akhlaghi, M. Dietary approaches to stop hypertension (DASH): potential mechanisms of action against risk factors of the metabolic syndrome. Nutr Res Rev. (2020) 33:1–18. doi: 10.1017/S0954422419000155
8. Altawili, AA, Altawili, M, Alwadai, AM, Alahmadi, AS, Alshehri, AMA, Muyini, BH, et al. An exploration of dietary strategies for hypertension management: a narrative review. Cureus. (2023) 15:e50130. doi: 10.7759/cureus.50130
9. Xu, R, Molenaar, AJ, Chen, Z, and Yuan, Y. Mode and mechanism of action of Omega-3 and Omega-6 unsaturated fatty acids in chronic diseases. Nutrients. (2025) 17:1540. doi: 10.3390/nu17091540
10. Rosenson, RS, Davidson, MH, Hirsh, BJ, Kathiresan, S, and Gaudet, D. Genetics and causality of triglyceride-rich lipoproteins in atherosclerotic cardiovascular disease. J Am Coll Cardiol. (2014) 64:2525–40. doi: 10.1016/j.jacc.2014.09.042
11. Ravera, A, Carubelli, V, Sciatti, E, Bonadei, I, Gorga, E, Cani, D, et al. Nutrition and cardiovascular disease: finding the perfect recipe for cardiovascular health. Nutrients. (2016) 8:363. doi: 10.3390/nu8060363
12. Tang, N, Ma, J, Tao, R, Chen, Z, Yang, Y, He, Q, et al. The effects of the interaction between BMI and dyslipidemia on hypertension in adults. Sci Rep. (2022) 12:927. doi: 10.1038/s41598-022-04968-8
13. Conlin, PR, Chow, D, Miller, ER, Svetkey, LP, Lin, P-H, Harsha, DW, et al. The effect of dietary patterns on blood pressure control in hypertensive patients: results from the dietary approaches to stop hypertension (DASH) trial. Am J Hypertens. (2000) 13:949–55. doi: 10.1016/s0895-7061(99)00284-8
14. Filippou, CD, Tsioufis, CP, Thomopoulos, CG, Mihas, CC, Dimitriadis, KS, Sotiropoulou, LI, et al. Dietary approaches to stop hypertension (DASH) diet and blood pressure reduction in adults with and without hypertension: a systematic review and meta-analysis of randomized controlled trials. Adv Nutr. (2020) 11:1150–60. doi: 10.1093/advances/nmaa041
15. Kwan, MW-M, Wong, MC-S, Wang, HH-X, Liu, KQ-L, Lee, CL-S, Yan, BP-Y, et al. Compliance with the dietary approaches to stop hypertension (DASH) diet: a systematic review. PLoS One. (2013) 8:e78412. doi: 10.1371/journal.pone.0078412
16. Nayda, NC, Thomas, JM, Delaney, CL, and Miller, MD. The effect of omega-3 polyunsaturated fatty acid intake on blood levels of omega-3s in people with chronic atherosclerotic disease: a systematic review. Nutr Rev. (2023) 81:1447–61. doi: 10.1093/nutrit/nuad020
17. Wang, T, Zhang, X, Zhou, N, Shen, Y, Li, B, Chen, BE, et al. Association between omega-3 fatty acid intake and dyslipidemia: a continuous dose–response meta-analysis of randomized controlled trials. J Am Heart Assoc. (2023) 12:e029512. doi: 10.1161/JAHA.123.029512
18. Yan, J, Liu, M, Yang, D, Zhang, Y, and An, F. Efficacy and safety of omega-3 fatty acids in the prevention of cardiovascular disease: a systematic review and meta-analysis. Cardiovasc Drugs Ther. (2024) 38:799–817. doi: 10.1007/s10557-022-07379-z
19. Shibabaw, T. Omega-3 polyunsaturated fatty acids: anti-inflammatory and anti-hypertriglyceridemia mechanisms in cardiovascular disease. Mol Cell Biochem. (2021) 476:993–1003. doi: 10.1007/s11010-020-03965-7
20. Wang, H, Li, Q, Zhu, Y, and Zhang, X. Omega-3 polyunsaturated fatty acids: versatile roles in blood pressure regulation. Antioxid Redox Signal. (2021) 34:800–10. doi: 10.1089/ars.2020.8108
21. Imamura, F, Micha, R, Khatibzadeh, S, Fahimi, S, Shi, P, Powles, J, et al. Dietary quality among men and women in 187 countries in 1990 and 2010: a systematic assessment. Lancet Glob Health. (2015) 3:e132–42. doi: 10.1016/S2214-109X(14)70381-X
22. Arayici, ME, Kilic, ME, and Yilmaz, MB. High and low adherence to Mediterranean and DASH diet patterns and the risk of heart failure: a Meta-analysis of observational studies. Life. (2025) 15:63. doi: 10.3390/life15010063
23. Parmenter, BH, Bumrungpert, A, and Thouas, GA. Socio-demographic factors, beliefs and health perceptions associated with use of a commercially available Ω-3 fatty acid supplement: a cross-sectional study in Asian countries. PharmaNutrition. (2021) 15:100237. doi: 10.1016/j.phanu.2020.100237
24. Shi, J, Hu, H, Harnett, J, Zheng, X, Liang, Z, Wang, Y-T, et al. An evaluation of randomized controlled trials on nutraceuticals containing traditional Chinese medicines for diabetes management: a systematic review. Chin Med. (2019) 14:54. doi: 10.1186/s13020-019-0276-3
25. Thuppal, SV, Von Schacky, C, Harris, WS, Sherif, KD, Denby, N, Steinbaum, SR, et al. Discrepancy between knowledge and perceptions of dietary omega-3 fatty acid intake compared with the omega-3 index. Nutrients. (2017) 9:930. doi: 10.3390/nu9090930
26. Yi, K, Cui, S, Tang, M, Wu, Y, Xiang, Y, Yu, Y, et al. Adherence to DASH dietary pattern and its association with incident hyperuricemia risk: a prospective study in Chinese community residents. Nutrients. (2022) 14:4853. doi: 10.3390/nu14224853
27. Gibson, AA, and Sainsbury, A. Strategies to improve adherence to dietary weight loss interventions in research and real-world settings. Behav Sci. (2017) 7:44. doi: 10.3390/bs7030044
28. Uwizeye, G, Mwali, AK, and Radeny, S. Engaging communities and promoting health-seeking behavior through strategic social and behavior change Raleigh, NC: IntraHealth International (2022).
29. Kounatidis, D, Tentolouris, N, Vallianou, NG, Mourouzis, I, Karampela, I, Stratigou, T, et al. The pleiotropic effects of lipid-modifying interventions: exploring traditional and emerging hypolipidemic therapies. Meta. (2024) 14:388. doi: 10.3390/metabo14070388
30. Champagne, CM, Bergeron, N, Siri-Tarino, PW, Bray, GA, and Krauss, RM. The DASH Diet In: Bergeron N., Siri-Tarino P.W., Bray G.A., Krauss R.M., editors. Nutrition and Cardiometabolic Health. Boca Raton, FL: CRC Press (2017). 431–47.
31. Habumugisha, T, Engebretsen, IMS, Måren, IE, Kaiser, CWM, and Dierkes, J. Reducing meat and/or dairy consumption in adults: a systematic review and meta-analysis of effects on protein intake, anthropometric values, and body composition. Nutr Rev. (2024) 82:277–301. doi: 10.1093/nutrit/nuad055
32. Huang, Z, Li, J, Liu, Y, and Zhou, Y. Effects of different exercise modalities and intensities on body composition in overweight and obese children and adolescents: a systematic review and network meta-analysis. Front Physiol. (2023) 14:1193223. doi: 10.3389/fphys.2023.1193223
33. Musazadeh, V, Kavyani, Z, Naghshbandi, B, Dehghan, P, and Vajdi, M. The beneficial effects of omega-3 polyunsaturated fatty acids on controlling blood pressure: An umbrella meta-analysis. Front Nutr. (2022) 9:985451. doi: 10.3389/fnut.2022.985451
34. Qian, F, Ardisson Korat, AV, Imamura, F, Marklund, M, Tintle, N, Virtanen, JK, et al. N-3 fatty acid biomarkers and incident type 2 diabetes: an individual participant-level pooling project of 20 prospective cohort studies. Diabetes Care. (2021) 44:1133–42. doi: 10.2337/dc20-2426
35. Soltani, S, Shirani, F, Chitsazi, MJ, and Salehi-Abargouei, A. The effect of dietary approaches to stop hypertension (DASH) diet on weight and body composition in adults: a systematic review and meta-analysis of randomized controlled clinical trials. Obes Rev. (2016) 17:442–54. doi: 10.1111/obr.12391
36. Bayram, SŞ, and Kızıltan, G. The role of Omega-3 polyunsaturated fatty acids in diabetes mellitus management: a narrative review. Curr Nutr Rep. (2024) 13:527–51. doi: 10.1007/s13668-024-00561-9
37. Valenzuela-Fuenzalida, JJ, Bravo, VS, Valarezo, LM, Delgado Retamal, MF, Leiva, JM, Bruna-Mejías, A, et al. Effectiveness of DASH diet versus other diet modalities in patients with metabolic syndrome: a systematic review and meta-analysis. Nutrients. (2024) 16:3054. doi: 10.3390/nu16183054
38. O’Keefe, JH, and Abuannadi, M. Dietary strategies for the prevention & treatment of metabolic syndrome. Mo Med. (2010) 107:406.
39. Nilghaz, M, Sadeghi, A, Koochakpoor, G, Poustchi, H, Khodadadi, N, Narimani, B, et al. The efficacy of DASH combined with time-restricted feeding (16/8) on metabolic associated fatty liver disease management: a randomized controlled trial. Sci Rep. (2025) 15:7020. doi: 10.1038/s41598-025-88393-7
40. Sahebkar, A, Heidari, Z, Kiani, Z, Atefi, M, Zareie, A, Shojaei, M, et al. The efficacy of dietary approaches to stop hypertension (DASH) diet on lipid profile: a systematic review and meta-analysis of clinical controlled trials. Curr Med Chem. (2025) 32:563–78. doi: 10.2174/0929867331666230706102406
41. Esposito, K, Kastorini, C-M, Panagiotakos, DB, and Giugliano, D. Mediterranean diet and weight loss: meta-analysis of randomized controlled trials. Metab Syndr Relat Disord. (2011) 9:1–12. doi: 10.1089/met.2010.0031
42. Chaddha, A, and Eagle, KA. Omega-3 fatty acids and heart health. Circulation. (2015) 132:e350–2. doi: 10.1161/CIRCULATIONAHA.114.015176
43. Juraschek, SP, Miller, ER, Weaver, CM, and Appel, LJ. Effects of sodium reduction and the DASH diet in relation to baseline blood pressure. J Am Coll Cardiol. (2017) 70:2841–8. doi: 10.1016/j.jacc.2017.10.011
44. Javaid, M, Kadhim, K, Bawamia, B, Cartlidge, T, Farag, M, and Alkhalil, M. Bleeding risk in patients receiving Omega-3 polyunsaturated fatty acids: a systematic review and meta-analysis of randomized clinical trials. J Am Heart Assoc. (2024) 13:e032390. doi: 10.1161/JAHA.123.032390
45. Ishaq, I, Noreen, S, Maduabuchi Aja, P, and Atoki, AV. Role of protein intake in maintaining muscle mass composition among elderly females suffering from sarcopenia. Front Nutr. (2025) 12:1547325. doi: 10.3389/fnut.2025.1547325
46. Lin, P-H, Appel, LJ, Funk, K, Craddick, S, Chen, C, Elmer, P, et al. The PREMIER intervention helps participants follow the dietary approaches to stop hypertension dietary pattern and the current dietary reference intakes recommendations. J Am Diet Assoc. (2007) 107:1541–51. doi: 10.1016/j.jada.2007.06.019
47. Ali, HM, Attia, MH, and Rashed, EN. Enhancing the stability of strawberry anthocyanins complexed to β-cyclodextrin and starch toward heat, oxidation, and irradiation. Acs Omega. (2024) 9:5319–29. doi: 10.1021/acsomega.3c06311
48. Noreen, S, Shehzadi, S, Egbuna, C, and Aja, PM. Lycopene alleviates lipid dysregulation, oxidative stress, and hypercholesterolemia in obese rats subjected to a high-fat diet. Food Sci Nutr. (2025) 13:e70549. doi: 10.1002/fsn3.70549
49. Popescu, C, Matei, D, Amzolini, AM, and Trăistaru, MR. Inflammation and physical performance in overweight and obese schoolchildren. Life. (2024) 14:1583. doi: 10.3390/life14121583
Keywords: obesity, DASH diet, omega-3 fatty acids, hyperlipidemia, hypertension, cardiometabolic health
Citation: Yin H, Zhou Y, Zhou Y, Ren L and Ma L (2025) Retrospective analysis of omega-3 fatty acids and the DASH diet in hyperlipidemia and hypertension management among obese individuals. Front. Nutr. 12:1704552. doi: 10.3389/fnut.2025.1704552
Edited by:
Adriana Coppola, Clinical Institute Beato Matteo -GSD, ItalyReviewed by:
Tatiana Palotta Minari, Federal University of São Paulo, BrazilPeng Hu, Sun Yat-sen University, China
Copyright © 2025 Yin, Zhou, Zhou, Ren and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lixiang Ma, bGl4aWFuZ204ODY2QDE2My5jb20=
 Hongtao Yin
Hongtao Yin Yanqing Zhou2
Yanqing Zhou2 Lixiang Ma
Lixiang Ma