Abstract
Background:
COVID-19 is a global concern due to its high transmission and mortality rates. Despite governments’ efforts worldwide to control its spread, many people were hesitant to adopt preventive measures. The effectiveness of these measures largely depends on public willingness, which is influenced by their knowledge and perception of risk. Therefore, this study aimed to examine the knowledge, risk perceptions, protection practices, and related factors concerning COVID-19 in the Dessie City Administration, Northeast Ethiopia.
Methodology:
This study employed a cross-sectional design. We selected seven hundred ninety participants using a systematic sampling technique. Data was collected face-to-face using an interviewer-administered questionnaire. Descriptive statistics, including frequency, percentage, mean, and standard deviation, were used to summarise the sample characteristics. Multivariable logistic regression analysis was conducted using SPSS (version 23), and the results were presented in the form of text, tables, and graphs.
Results:
Of the study participants, 498 (63%) had good knowledge of the pandemic, while 457 (58%) had a low-risk perception. Only 305 (39%) demonstrated good protection practices. The most trusted sources of information were healthcare personnel (686 participants, 86.8%), followed by the Ministry of Health websites (654 participants, 82.8%). Monthly income (>10,000 ETB), knowledge, and risk perceptions with AORs of 3.05 (CI: 1.51–6.14), 4.45 (CI: 2.81–7.04), 2.06 (CI: 1.38–3.08) were significantly associated with protection practices against the COVID-19 pandemic.
Conclusion:
More than two-thirds of the participants demonstrated good knowledge about COVID-19. However, over half perceived themselves to be at low risk and engaged in poor preventive practices. Control efforts will be challenging, especially among younger and less educated groups who consider themselves at low risk, requiring focused attention. Understanding people’s risk perceptions and beliefs about the effectiveness of COVID-19 prevention measures is essential for improving protective behaviours. Health education and active community engagement are key strategies in combating the spread of the virus.
1 Introduction
Coronavirus disease 2019 (COVID-19) is a contagious respiratory disease in humans that causes pneumonia-like infection (1). So far, seven human coronaviruses (HCoVs) have been identified. These include the highly pathogenic severe acute respiratory syndrome coronavirus (SARS-CoV), Middle East respiratory syndrome coronavirus (MERS-CoV), and the newly identified SARS-CoV-2. They are known to have caused global outbreaks, with SARS-CoV-2 being responsible for the current pandemic (2).
The COVID-19 pandemic emerged in Wuhan, China, in late December 2019 (3). Later, this disease was declared a global public health emergency (4). COVID-19 was declared a pandemic by WHO on March 11, 2020, due to an increase in the number of cases worldwide (5). On March 13, 2020, the first COVID-19 case in Ethiopia was confirmed (6).
Contaminated objects and respiratory droplets were the primary means of transmission for this pandemic (7). Asymptomatic patients serve as carriers of this pandemic (8). Old age and patients with pre-existing chronic illnesses were identified as risk factors for the severe form of the disease and mortality (9). Fever, dry cough, fatigue, respiratory illnesses, diarrhoea, vomiting, and headache were among the clinical manifestations (10).
Non-pharmaceutical interventions (NPIs) are key to controlling the spread of this virus (11), relying on public willingness, which is influenced by knowledge and risk perception (12). However, studies showed inconsistent knowledge about the pandemic. A study in Bangladesh showed that about 45% of participants had poor knowledge (13). A Chinese study showed that droplet infection was mentioned as a mode of transmission by only 66.6% of the participants, while 35.9 and 4.8% of the participants, respectively, mentioned people with ages greater than 65 and smokers as being at high risk of contracting COVID-19 (14).
Because of its high transmission rate, lack of definitive treatment, and high morbidity and mortality rate, this disease is a global concern (15). Controlling its spread was extremely difficult due to the lack of definitive treatments (16). Developed countries are adversely affected, despite their advancement in healthcare systems (17). Ethiopia is an African country with a low-skilled workforce and technological assets (18). Governments all over the world are working hard to keep it under control. However, a large number of people were reluctant to use preventive measures. To be effective, information is crucial to comprehend the relationships between demographic factors, risk perceptions, and prevention practices (19).
Several studies conducted in various countries revealed that the risk perception for this disease was low. A study done in Ghana showed that about 32% of participants had low-risk perceptions (20). A Myanmar study showed that approximately 22% of the participants wrongly perceived spontaneous recovery (14). According to a study conducted in Iraq, only 26.9, 29.7, and 41.7% of respondents, respectively, were concerned about contracting infection, serious illness, or death from this pandemic (21).
The number of COVID-19 cases and deaths in Ethiopia has increased over time. The Ethiopian Ministry of Health reported 102,720 cases as of December 14, 2020 (22). Ethiopia adapts basic intervention measures to reduce the spread of this virus (23). However, people’s adherence to preventive measures is critical, which is influenced primarily by their knowledge and risk perception (3).
Protection practices rely on the perceived risk of contracting a disease and efficacy beliefs for preventive modalities (24). Health models advocate risk perception as a motivator for change in behaviour (25). One of them is the extended parallel process model (EPPM), which advocates protection practice as a result of threat assessment and coping evaluation based on the concept of protection motivation theory (PMT). Threat assessment entails assessing the risk of contracting a disease (perceived vulnerability or susceptibility) and determining the severity of the disease (perceived severity) (26).
Several studies found that protection practices against this disease were not satisfactory. For instance, studies done in Myanmar (14) and Bangladesh (27) revealed that nearly 45.2 and 24.8% of participants, respectively, had poor hand hygiene practices. Studies in the Philippines (28) and Malaysia (29) showed that around 37 and 49% of participants were not avoiding crowded areas, respectively. A Bangladesh (27) study showed that around 30% of participants failed the regular mask-wearing practice. Studies done in Myanmar (14), Bangladesh (27), and Thailand (30) showed that 78, 50, and 83% of respondents had poor protection practices, respectively.
Males, younger age groups, and less educated individuals were less likely to implement preventive measures (31). The clarity of communication influences protection behaviour (32). Risk perception and beliefs about the efficacy of the preventive methods influenced the community’s engagement in realising precautionary measures (33). People with good knowledge and a high-risk perception of the pandemic respond positively to preventive methods (34, 35).
As a result, the purpose of this study was to assess knowledge, risk perceptions, and protection practices in Dessie City, Northeast Ethiopia, as well as investigate factors associated with protection practices.
2 Methods
2.1 Study area and period
The study was conducted among the population of Dessie City, North-East Ethiopia, between the end of July and mid-December 2020. Dessie is the main trading center in the Northeastern part of Ethiopia and is a part of the Wollo culture, thus having a style of close cultural relationship. The city is divided into 26 kebeles (the smallest administrative unit) for administrative purposes. The city has a number of publicly and privately owned health institutions. The city has one referral hospital that serves more than eight million people from all over the city and provinces. The city also serves as a COVID-19 treatment and quarantine center.
2.2 Population and study design
This community-based cross-sectional survey was done among the selected households in the study area. Adult members (>18 years) were selected by lottery from the participating households for an interview. Those with hearing and speaking problems and the inability to comprehend due to illness or age were excluded.
2.3 Variables
The outcome variable was protection practice. Its score was determined using a five-point Likert scale. On the scale, one point stands for never, two points for seldom, three points for occasionally, four points for frequently, and five points for always.
Sociodemographic, access to trusted health information, a member with chronic illness (such as diabetes, hypertension, and cancer), knowledge, belief in the efficacy of prevention, and risk perception variables were used as control covariates in the regression models.
Socio-demographic characteristics included sex, age, marital status, religion, education, occupation, family size, and economic status.
Knowledge was measured by 27 items. Furthermore, participants were asked about various sources of knowledge-based information, including social media platforms such as Facebook and others, official websites (WHO websites, MOH updates), official statements on radio and television, family members, and others. Their trust in health information obtained from such sources was also assessed.
Risk perception was measured using 12 items developed according to the framework of the EPPM and WHO COVID-19 survey tool and guidance (26, 36). Perceived efficacy to the desired protection measures addressed their belief in response to efficacy and self-efficacy for the novel COVID-19 (14, 26). The risk perception and belief in efficacy for preventive methods were assessed using a five-point Likert scale. On the scale, one point stands for strongly disagree, two points for disagree, three points for neutral, four points for agree, and five points for strongly agree.
2.4 Sample size determination and sampling procedures
The number of households was determined using the single population proportion formula. The sample size was calculated using Epi Info with a 5% margin of error, resulting in 376 participants. However, the sampling procedure involved two stages, and the design effect was considered in addition to a 5% contingency for non-response. The final sample size was 790 households.
In the sampling procedures, first, from the total of 26 “kebeles,” eight “kebeles” were randomly selected as the first sampling unit using the lottery method. Then the sampled households were proportionally divided into the selected “kebeles” according to their number of households. The household list was obtained from “kebele” health post extension workers and used as a sampling frame. The first household was selected randomly from the central location of the “kebeles.” Then household members from each “kebele” were selected through a systematic sampling (Figure 1).
Figure 1
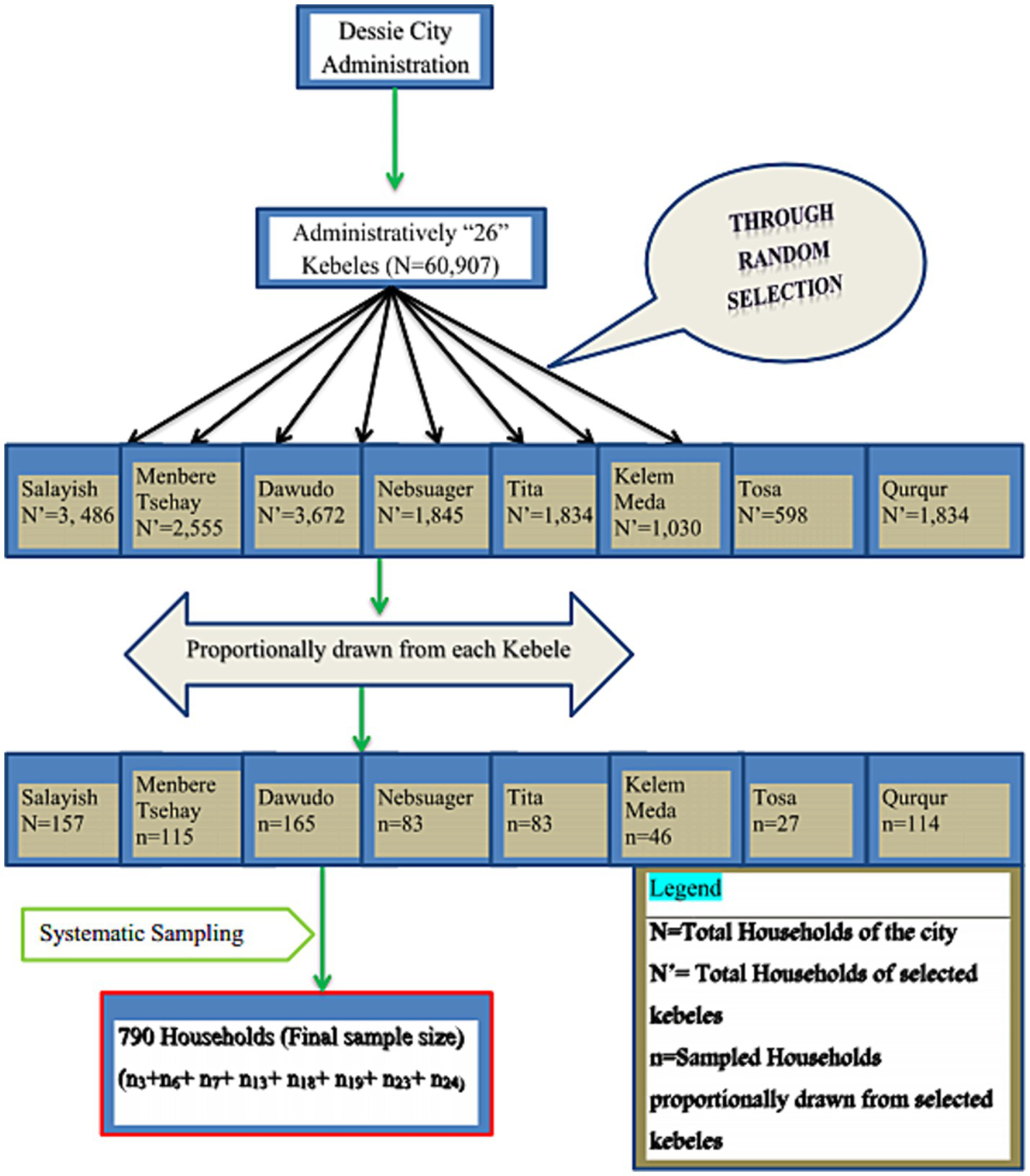
Sampling procedures for assessing risk perceptions, knowledge, and protection practices related to COVID-19, Dessie, Ethiopia, 2020.
2.5 Data collection tools and procedures
A structured interviewer-administered questionnaire was employed for the data collection. The questionnaire was adapted from a previous survey conducted in different settings (12, 14, 21, 37). It was prepared in English and translated to Amharic and back to English by a PhD English language expert for validity. It contained the following parts: (1) socio-demographic characteristics, (2) COVID-19 knowledge items, (3) health information knowledge items, (4) risk perception items, (5) belief in efficacy for the preventive methods, and (6) protection practice items.
The questionnaire contained 27 knowledge items (Table 1). These questions were answered on a yes/no basis, with an additional “I do not know” option.
Table 1
| COVID-19 knowledge items | Response options |
|---|---|
| K1. Do you think COVID-19 exists? | Yes, no, I do not know |
| K2. Is COVID-19 a viral infection? | Yes, no, I do not know |
| K3. Can COVID-19 be transmitted from person to person? | Yes, no, I do not know |
| K4. Could an asymptomatic person transmit the disease? | Yes, no, I do not know |
| K5. Do you know that COVID-19 has a vaccine? | Yes, no, I do not know |
| K6. Do you know that there is a cure for COVID-19? | Yes, no, I do not know |
| K7. Is COVID-19 spread through the air via respiratory droplets produced by infected people sneezing or coughing? | Yes, no, I do not know |
| K8. Does touching or shaking an infected person’s hands result in COVID-19 infection? | Yes, no, I do not know |
| K9. Is close contact with people increasing the virus’s spread? | Yes, no, I do not know |
| K10. Does touching an object and then touching your mouth, nose, or eyes with an unwashed hand result in COVID-19 virus infection? | Yes, no, I do not know |
| K11. Does using a public toilet result in COVID-19 virus infection? | Yes, no, I do not know |
| K12. Do people infected with COVID-19 get a fever? | Yes, no, I do not know |
| K13. Does COVID-19 infection cause dry cough? | Yes, no, I do not know |
| K14. Do COVID-19 infected people have trouble breathing? | Yes, no, I do not know |
| K15. Does COVID-19 infection cause headaches? | Yes, no, I do not know |
| K16. Is it possible to prevent the spread of the virus by washing hands with soap and water for at least 20 s or using an alcohol-based hand sanitizer (60%)? | Yes, no, I do not know |
| K17. Is contact isolation and quarantine of people infected with the COVID-19 virus effective in reducing virus spread? | Yes, no, I do not know |
| K18. Does limiting handshakes reduce the risk of infection? | Yes, no, I do not know |
| K19. Is it possible to prevent the virus from spreading by not touching the eyes, nose, or mouth with unwashed hands? | Yes, no, I do not know |
| K20. Does avoiding going to crowded places such as public transportation, religious places, hospitals, and workplaces prevent the spread of the virus? | Yes, no, I do not know |
| K21. Do you know that you should keep a safe distance of at least two meters when sitting with other people to protect yourself from the virus? | Yes, no, I do not know |
| K22. Do you know that staying at home can reduce your chances of contracting an infection? | Yes, no, I do not know |
| K23. Do you know that wearing facemasks when leaving the house can help prevent the virus from spreading? | Yes, no, I do not know |
| K24. Is the older adult (those over the age of 65) more vulnerable to coronavirus disease? | Yes, no, I do not know |
| K25. Are smokers more vulnerable to the coronavirus disease? | Yes, no, I do not know |
| K26. Are people with chronic diseases (like hypertension, diabetes, and cancer) more susceptible to coronavirus infection? | Yes, no, I do not know |
| K27. Are people in densely populated areas more susceptible to COVID-19? | Yes, no, I do not know |
COVID-19 knowledge items questionnaire, Dessie, Ethiopia, 2020.
This study used six items with five levels of agreement to assess belief in the efficacy of COVID-19 prevention methods. The questionnaire included 12 risk perception items: six for perceived susceptibility or risk of infection (R1–R6) and six for perceived severity (R7–R12) of COVID-19. Negative items were scored in reverse, and the sum of all items was calculated to get the perceived risk score. The questionnaires for risk perceptions, belief in the efficacy of preventive methods, and COVID-19 protection practices are shown in Table 2.
Table 2
| Risk perception items | Response options |
|---|---|
| R1: There is a lower risk of infection spreading to family members from the sick person® | SD, D, N, A, SA |
| R2: Healthy people have no chance of contracting an infection® | SD, D, N, A, SA |
| R3: Young people have a low risk of contracting an infection® | SD, D, N, A, SA |
| R4: People who work with unidentified strangers are vulnerable to infection. | SD, D, N, A, SA |
| R5: Crowded areas are at risk for disease transmission. | SD, D, N, A, SA |
| R6: A healthy lifestyle reduces the likelihood of infection. | SD, D, N, A, SA |
| R7: The COVID-19 virus will cause severe medical problems. | SD, D, N, A, SA |
| R8: I would not be able to survive if I became infected with COVID-19. | SD, D, N, A, SA |
| R9: I could have COVID-19 without showing any signs or symptoms® | SD, D, N, A, SA |
| R10: If I become infected with COVID-19, I will recover on my own® | SD, D, N, A, SA |
| R11: If I were infected with COVID-19, I could be treated® | SD, D, N, A, SA |
| R12: I'm worried about the recent COVID-19 outbreak. | SD, D, N, A, SA |
| Belief in the efficacy of preventive methods | Response options |
| E1: I can get trustworthy information about the effectiveness of COVID-19 control methods. | SD, D, N, A, SA |
| E2: A healthy diet effectively prevents COVID-19. | SD, D, N, A, SA |
| E3: Hand washing or the use of hand sanitizer effectively prevents COVID-19. | SD, D, N, A, SA |
| E4: I easily implemented self-care measures to prevent COVID-19. | SD, D, N, A, SA |
| E5: Avoiding crowded areas is an effective way to prevent COVID-19. | SD, D, N, A, SA |
| E6: When entering a crowded area, wearing a face mask effectively prevents COVID-19. | SD, D, N, A, SA |
| Participants' frequency of implementing protective measures | Response options |
| P1: How often do you avoid large crowds? | Nev,Sel,Occ,Freq,Al |
| P2: How frequently do you avoid touching your face, mouth, nose, and eyes? | Nev,Sel,Occ,Freq,Al |
| P3: How frequently do you limit contact (such as handshakes)? | Nev,Sel,Occ,Freq,Al |
| P4: How frequently do you avoid unnecessary travel or trips? | Nev,Sel,Occ,Freq,Al |
| P5: How frequently do you avoid close contact with sick or infectious people? | Nev,Sel,Occ,Freq,Al |
| P6: How frequently do you wash your hands for at least 20 seconds or use hand sanitizer with 60% alcohol? | Nev,Sel,Occ,Freq,Al |
| P7: When you sneeze or cough, how often do you use a tissue? | Nev,Sel,Occ,Freq,Al |
| P8: How frequently do you wear face masks in public? | Nev,Sel,Occ,Freq,Al |
| P9: How often do you throw away used masks or tissues in the trash? | Nev,Sel,Occ,Freq,Al |
| P10: When you're sick, how often do you stay at home? | Nev,Sel,Occ,Freq,Al |
| P11: How often do you practice "physical distancing" by standing 2 meters away from others? | Nev,Sel,Occ,Freq,Al |
Questionnaire on COVID-19 risk perceptions, belief in the efficacy of preventive methods, and protection practices, Dessie, Ethiopia, 2020.
SD = Strongly Disagree; D = Disagree; N = Neutral; A = Agree; SA = Strongly Agree Nev=Never; Sel=Seldom; Occ=Occasionally; Freq=Frequently; Al=Always.
Data was collected between the end of July and the middle of December 2020. Two trained data collectors collected the data using a structured one-on-one interview technique. During the data collection, respondents were educated on adherence to standard precautions and PPEs such as antiseptic fluids, face masks, and latex gloves. All necessary precautions were taken to prevent disease transmissibility during data collection.
2.6 Quality assurance
The study was pre-tested on 40 respondents before the actual data collection. The survey tool was amended for consistency. Trained data collectors with a diploma in pharmacy collected the data. The investigator provided comprehensive one-day training about the data collection instruments, approaches required for interaction, and securing respondents’ consent.
Cronbach’s alpha was used to assess the reliability of the interviewer-administered questionnaire, and values of 73.6, 71.5, and 81.9%, respectively, were obtained for the knowledge, risk perception, and protective practice item questionnaires. This indicates that the internal consistency is acceptable (38).
The logistic regression test assumptions were verified and met the criteria (a binary dependent variable, independent observations, multicollinearity, outliers, and a large sample size). The Box-Tidwell test was used to check the linearity assumptions. The model was fitted for the assumptions.
2.7 Statistical analysis and presentation
Descriptive analysis was used to generate sample characteristics. The data was summarised using frequency, percentage, mean, and standard deviation. First, the bivariable binary logistic regression analysis using SPSS (version 23) was used to determine the relationship between each independent variable and the outcome variable in order to identify factors associated with protection practice. The variables with a p-value < 0.2 in the bivariate analysis were entered into the multiple logistic regression model to identify the independent factors of the outcome variable. The associations between independent variables and protection practices were quantified using crude odds ratios (CORs) and adjusted odds ratios (AORs) with 95% confidence intervals (CIs). In the final model, variables with a p-value < 0.05 were significant. The findings of the study were then presented in the form of text, tables, and graphs.
2.8 Operational definitions
The mean value is used as a cut-off value when defining knowledge, risk perceptions, belief in the efficacy of preventive methods, and protection practices. The mean, which is the average value from each observation in the dataset, identifies the center of a dataset. As a result of these considerations, the mean was chosen as the cutoff value for the study. In addition, previous research has used the mean value as a cut-off point when categorising such variables (12, 39, 40).
2.8.1 Knowledge scores
When the scoring was greater than the mean score (18.9) of items, it indicated good knowledge, while scores below the mean indicated poor knowledge of the COVID-19 pandemic.
COVID-19 risk perception was measured using items for threat appraisal (susceptibility and severity). Susceptibility refers to respondents’ belief that they are infected with the disease. Severity refers to respondents’ perceptions of the seriousness of the disease if infected with COVID-19. If a risk perception score exceeded the mean score (36.03) of the items, it was considered high; when it was less, it was considered low.
2.8.2 Belief in efficacy for the preventive methods
The belief in efficacy of preventive methods was measured using items for efficacy appraisal (response efficacy and self-efficacy) of preventive modalities. Perceived efficacy refers to participants’ belief in the efficacy of preventive modalities and their ability to act.
2.8.3 Protection practice scores
A score greater than the mean score (29.06) of items indicated good practice, while a lower score indicated poor practice.
3 Results
3.1 Socio-demographic characteristics
Seven hundred ninety participants enrolled with a 100% response rate. Table 3 depicts the socio-demographic characteristics of the study’s participants. More than half, 433 (54.8%), of the study participants were female, and 464 (58.7%) were married. In terms of religion, Muslims made up more than half, 419 (53%), of the study participants, with Orthodox coming in second. The average age of the participants was 40.8 years, with ages ranging from 21 to 68 years. The most common age range, 338 (42.8%), was 31 to 40 years old. In terms of education, 461 (58.4%) of the study participants had a secondary education or less, while 191 (24.2%) had a bachelor’s degree or above. A large proportion, 268 (33.9%), of the participants’ monthly income ranged from 2,001 to 3,000 ETB. Regarding the medical conditions, 137 (17.3%) of the study participants had at least one or more chronic diseases such as diabetes, hypertension, or lung disease (Table 3).
Table 3
| Variables | Description | Frequency | % |
|---|---|---|---|
| Gender | Male | 357 | 45.2 |
| Female | 433 | 54.8 | |
| Age (years) | <31 | 136 | 17.2 |
| 31–40 | 338 | 42.8 | |
| 41–50 | 146 | 18.5 | |
| 51–60 | 111 | 14.1 | |
| >60 | 59 | 7.5 | |
| Religion | Islam | 419 | 53 |
| Orthodox | 322 | 40.8 | |
| Protestant | 49 | 6.2 | |
| Marital Status | Single | 223 | 28.2 |
| Widowed | 73 | 9.2 | |
| Divorced | 30 | 3.8 | |
| Married | 464 | 58.7 | |
| Education | No formal education | 152 | 19.2 |
| Primary school | 145 | 18.4 | |
| Secondary school | 164 | 20.8 | |
| Diploma | 138 | 17.5 | |
| Bachelor-degree or above | 191 | 24.2 | |
| Occupation | Unemployed | 112 | 14.2 |
| Student | 43 | 5.4 | |
| Private-employee | 299 | 37.8 | |
| Housewife | 68 | 8.6 | |
| Merchant | 103 | 13 | |
| Governmental employee | 165 | 20.9 | |
| Monthly income (ETB) | <2,000 | 148 | 18.7 |
| 2,001–3,000 | 268 | 33.9 | |
| 3,001–5,000 | 177 | 22.4 | |
| 5,001–10,000 | 104 | 13.2 | |
| >10,000 | 93 | 11.8 | |
| Chronic illness | No | 653 | 82.7 |
| Yes | 137 | 17.3 |
Socio-demographic characteristics of the study population, Dessie City, Ethiopia, 2020.
ETB, Ethiopian Birr.
3.2 Knowledge about COVID-19
COVID-19 was thought to exist in Ethiopia by 713 (90.3%) of participants, and the virus was mentioned as the cause of this disease by 691 (87.5%). Around nine to ten, or 710 (89.9%), of the respondents stated that it was transmitted from person to person. A large proportion of study participants, 540 (68%) and 615 (78%), stated that there was no vaccine or definitive treatment for COVID-19, respectively.
Seven hundred thirty-three (92.8%) and 655 (82.9%) of the study participants agreed that respiratory droplets from infected individuals during coughing, sneezing, or expiration, as well as close contact with the people, would result in the virus spreading, respectively. Shaking an infected person’s hand and touching a virus-infected object were also mentioned as ways of COVID-19 transmission by 624 (79%) and 596 (75.4%) of the participants, respectively.
Fever, dry cough, difficulty breathing, and headache were declared by study participants to be the most likely symptoms of infected individuals by 760 (96.2%), 707 (89.5%), 690 (87.3%), and 655 (82.9%), respectively. Six hundred seventy-seven (85.7%) and 635 (80.4%) participants stated that people in crowded places and those with chronic diseases were at high risk of contracting COVID-19, respectively.
Face masks and frequent hand hygiene were mentioned as important preventive measures by 710 (89.9%) and 699 (88.5%) of participants, respectively. Six hundred thirty-six (80.6%) and 612 (77.5%) participants reported that avoiding crowded places and contact isolation reduced the spread of the virus, respectively (Table 4).
Table 4
| Knowledge of COVID-19 preventive modalities | Frequency | Percentage |
|---|---|---|
| Put on face masks | 710 | 89.9 |
| Handwashing with soap and water every 20 s or using an alcohol-based hand sanitizer | 699 | 88.5 |
| Avoid crowded places such as public transportation, religious places, hospitals, and workplaces | 637 | 80.6 |
| Contact isolation and quarantine of infected individuals | 612 | 77.5 |
| Limiting handshakes | 610 | 77.2 |
| Avoid touching your eyes, nose, and mouth with unwashed hands | 593 | 75.1 |
| Staying at home | 550 | 69.6 |
| Maintain at least a two-meter safe distance | 531 | 67.2 |
Knowledge regarding preventive measures for COVID-19 among participants in Dessie, Ethiopia, 2020.
The study participants’ average knowledge score was 18.9 (range: 9 to 25). Approximately two-thirds of the participants in the study, 498 (63.0%) (95% CI (59.7–66.4%)), had a good level of knowledge (i.e., greater than the mean score of 18.9).
3.3 COVID-19 health information sources
The most common sources of health information about COVID-19 were television (662, 83.8%) and social media (415, 52.5%). Health care personnel were the most trusted sources, 686 (86.8%), followed by information obtained from MOHS websites, 654 (82.8%), and television, 516 (65.3%). Health professionals and MOH officials websites, on the other hand, were the least accessible source of information (Figure 2).
Figure 2
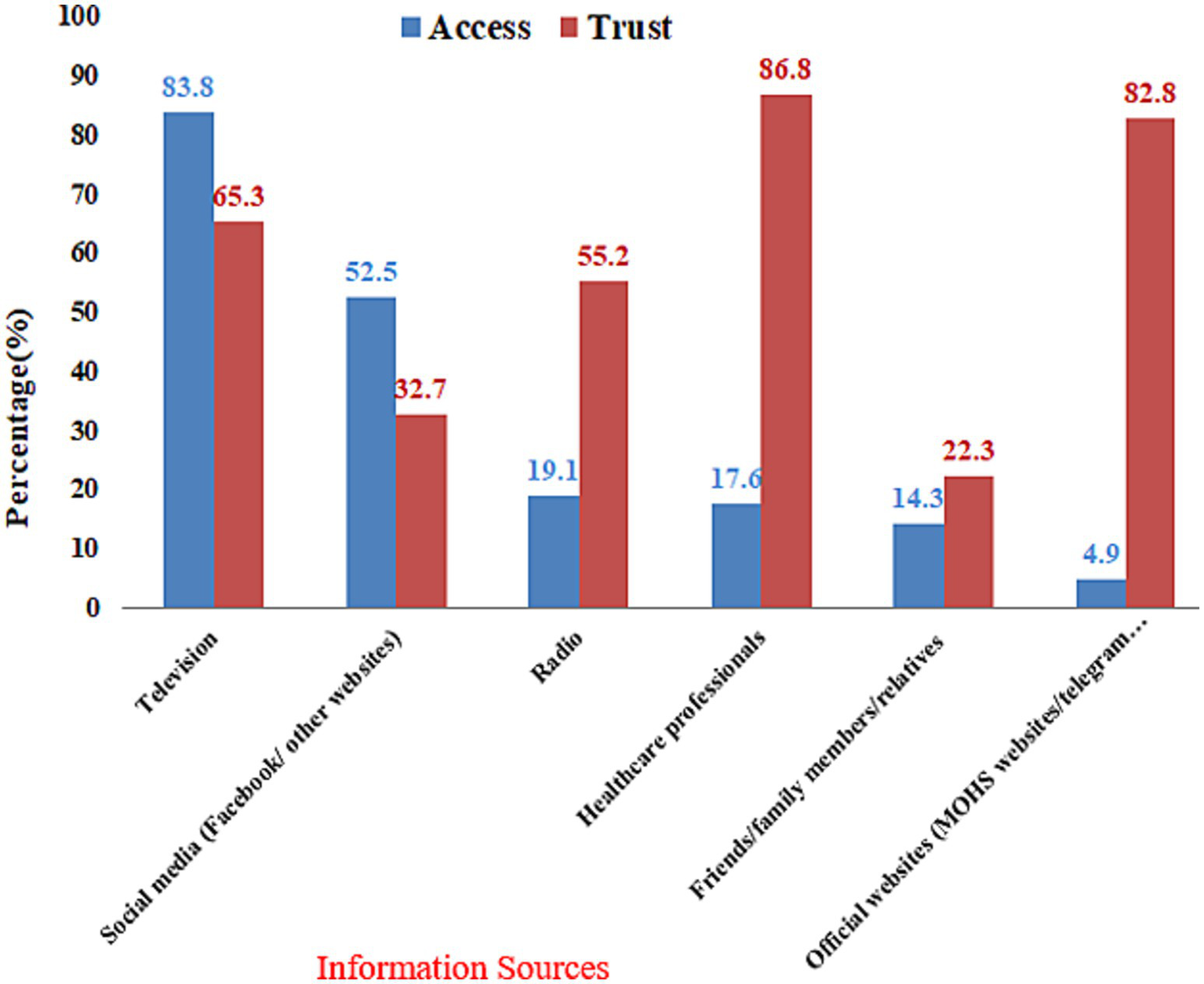
Sources of health information access and trust among the participants, Dessie City, Ethiopia, 2020.
3.4 Risk perceptions about COVID-19
The results revealed that 460 (57.8%) of respondents fell into the low-risk perception category, while the remaining fell into the high-risk perception category. Four hundred eight (51.6%) of the study participants perceived they were at low risk of getting an infection. Three hundred seventeen (40%) and 260 (33%) of the respondents incorrectly perceived that there was a low chance of infection among young people and no chance of infection among healthy people, respectively (Figure 3).
Figure 3
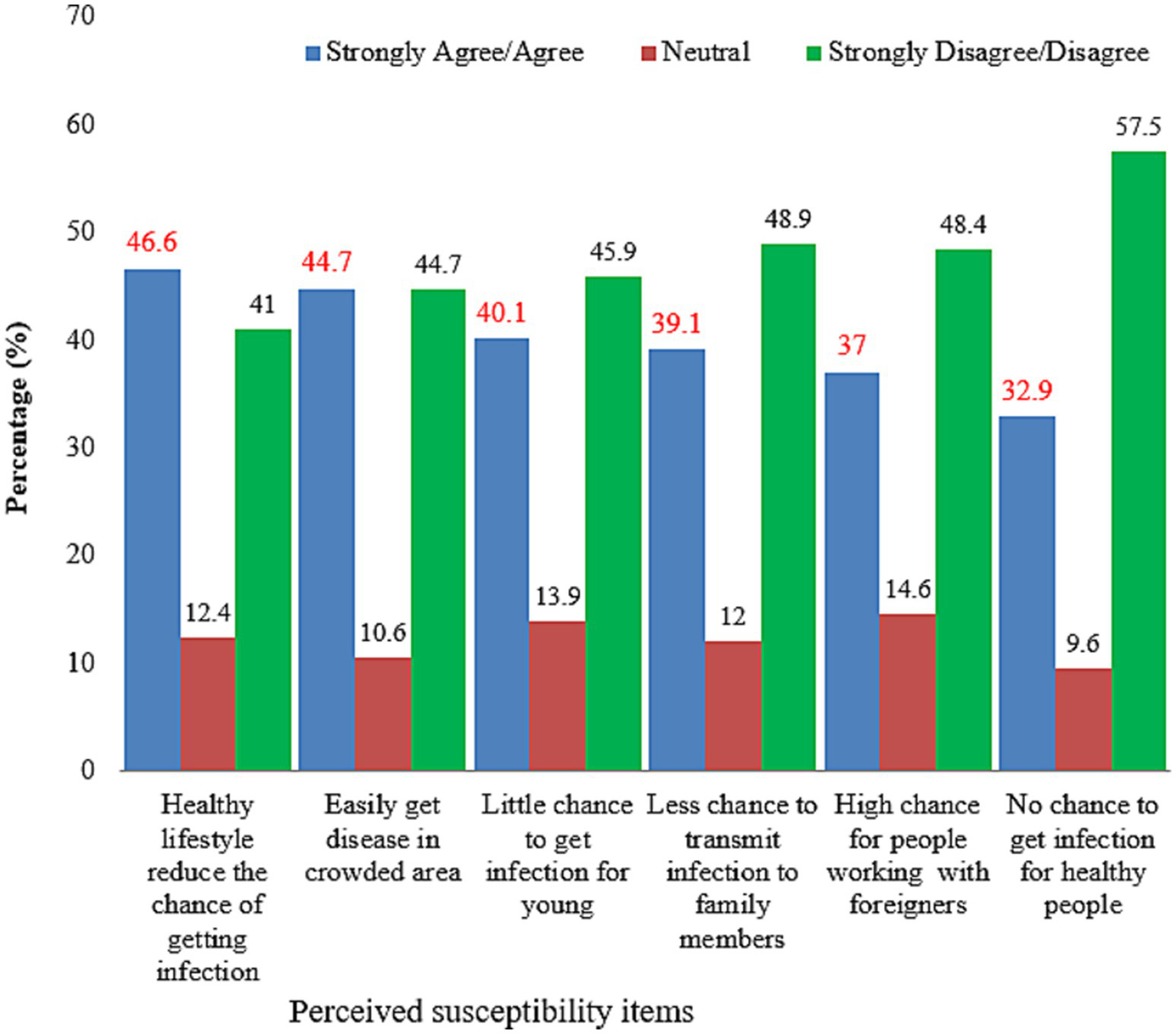
Perceived susceptibility to COVID-19 among participants, Dessie City, Ethiopia, 2020.
Only 266 (33.7%) participants believed COVID-19 would cause severe medical problems, while about 423 (53.5%) thought infected people could survive. Approximately two to five respondents, 337 (42.6%) and 367 (46.4%), believed that this disease was asymptomatic and spontaneous recovery was possible, respectively (Figure 4).
Figure 4
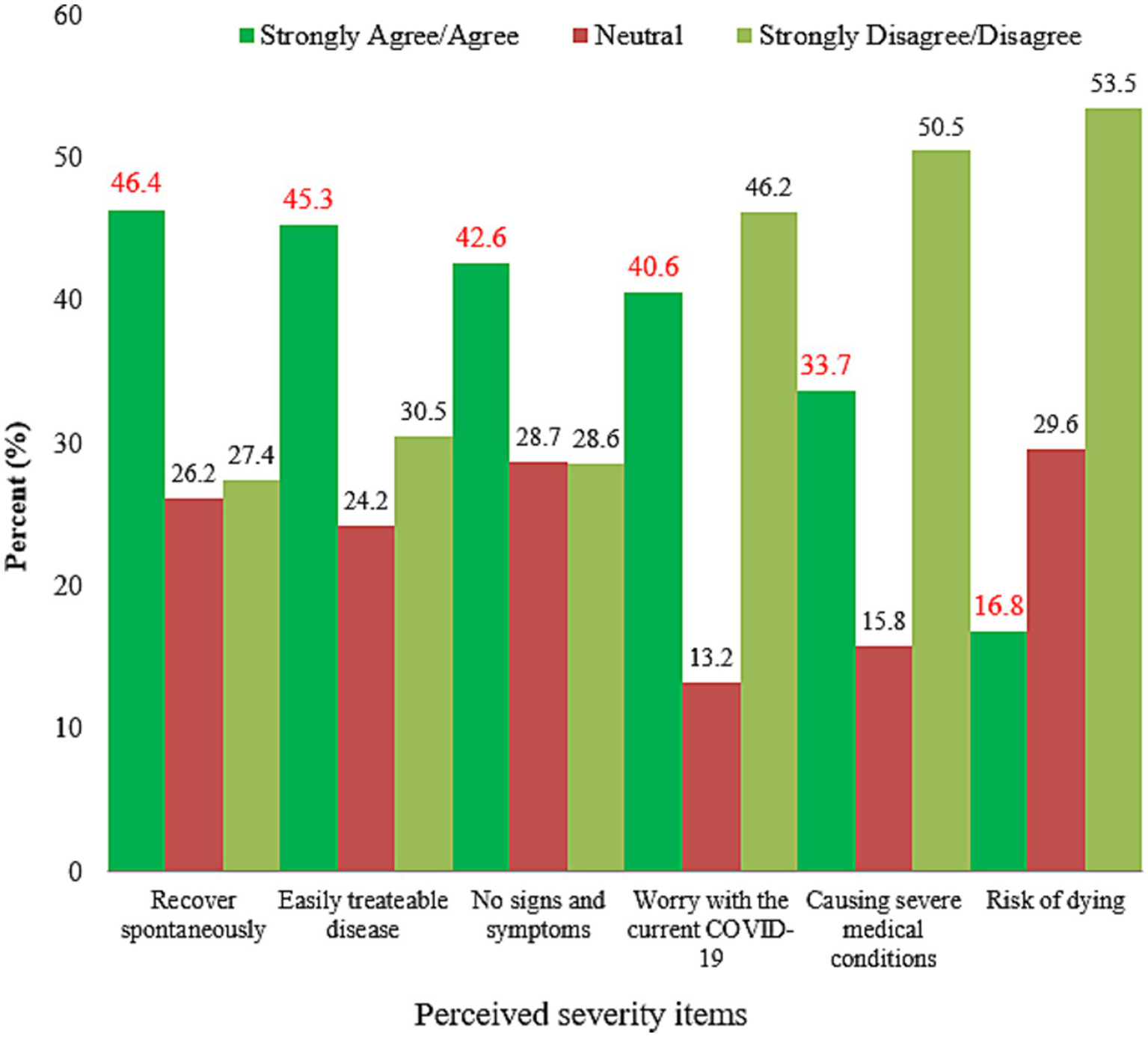
Perceived severity of COVID-19 among participants, Dessie City, Ethiopia, 2020.
3.5 Protection practices and associated factors
3.5.1 Belief in the efficacy of COVID-19 preventive methods
Two hundred forty-one (30.5%) of respondents believed they could access reliable health information regarding COVID-19 effective preventive methods. Only 303 (38.4%) of them were motivated to undertake self-care in controlling the spread of COVID-19 using preventive measures. Approximately half of the respondents, 380 (48.1%), were not concerned about their crowded area of visit (Figure 5).
Figure 5
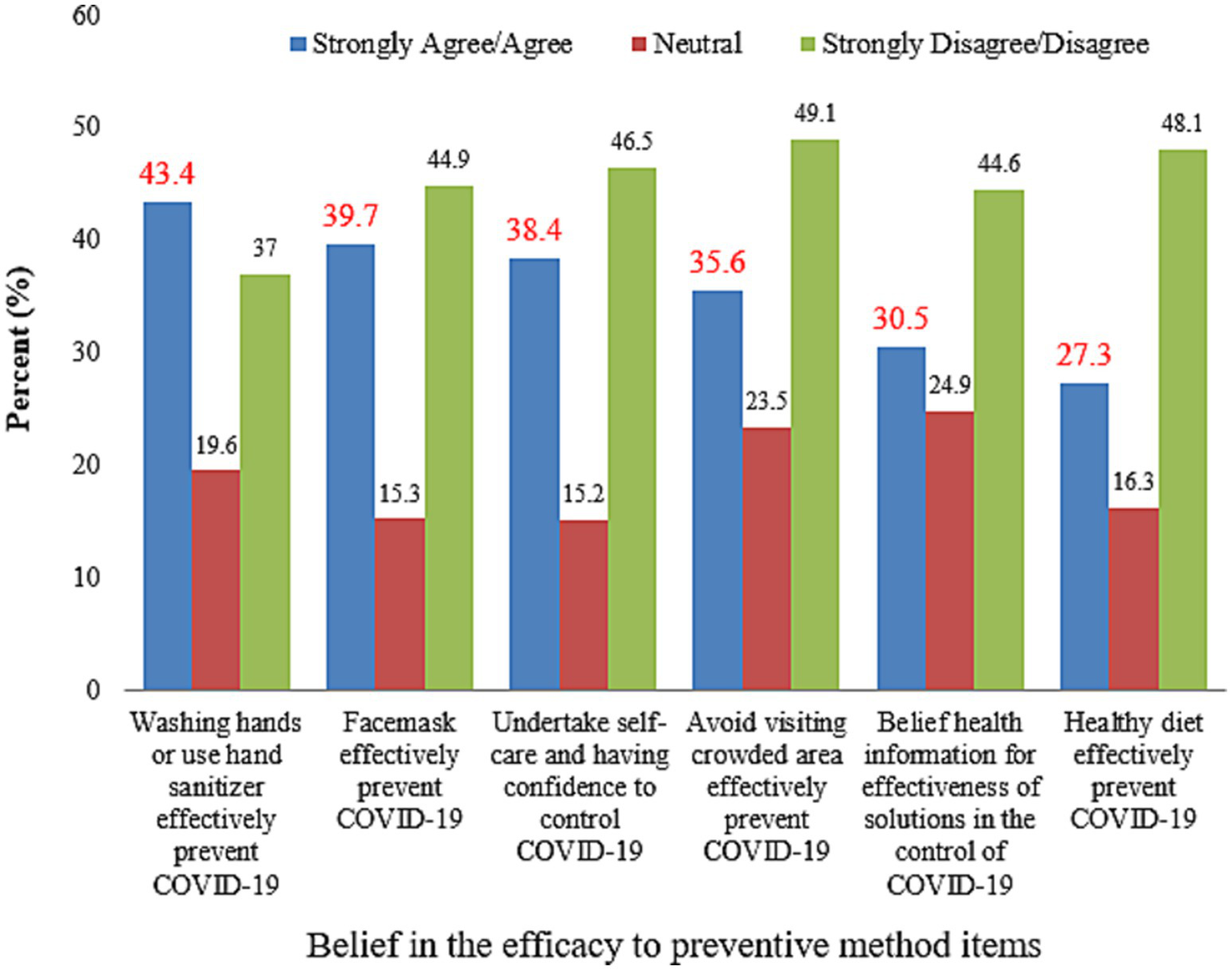
Belief in the efficacy of COVID-19 preventive methods among respondents, Dessie City, Ethiopia, 2020.
3.5.2 Protection practices
The prevalence of good practice was 305 (38.6%), with a 95% confidence interval of 35.0–42.0%. Four hundred sixty-three (58.6%) of participants stated that they wash their hands. The majority of the study participants, 579 (73.3%) and 574 (72.7%), did not stay at home when they were sick and did not wear face masks in public places, respectively (Figure 6).
Figure 6
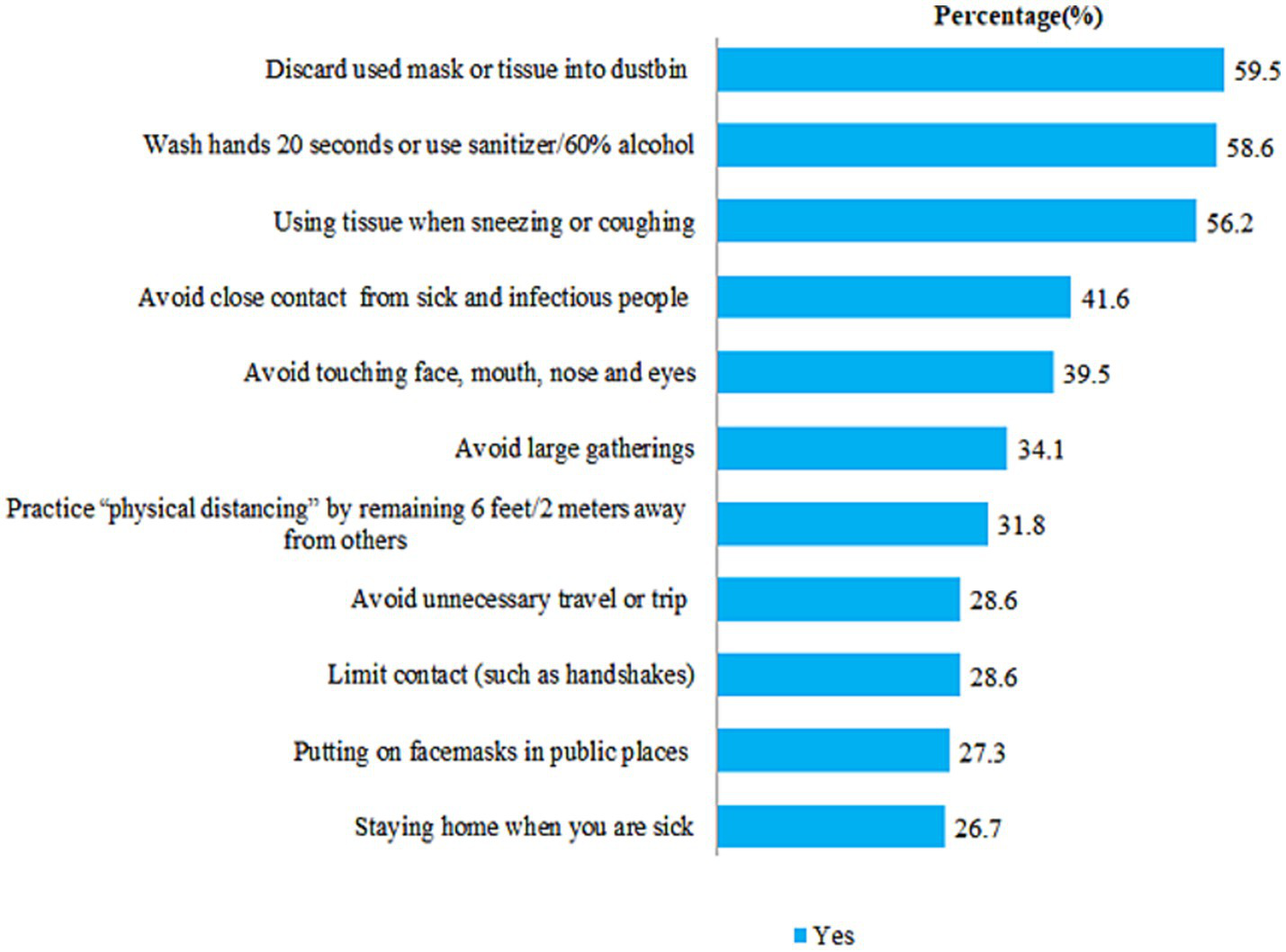
COVID-9 protection practices among participants, Dessie City, Ethiopia, 2020.
Only 284 (35.9%) and 274 (34.7%) of the participants frequently discarded used masks into the trash and washed their hands with soap and water, respectively. According to the frequency of use, only 245 (31%) of respondents used tissues when sneezing, and 200 (25.3%) avoided close contact with sick or infectious people (Figure 7).
Figure 7
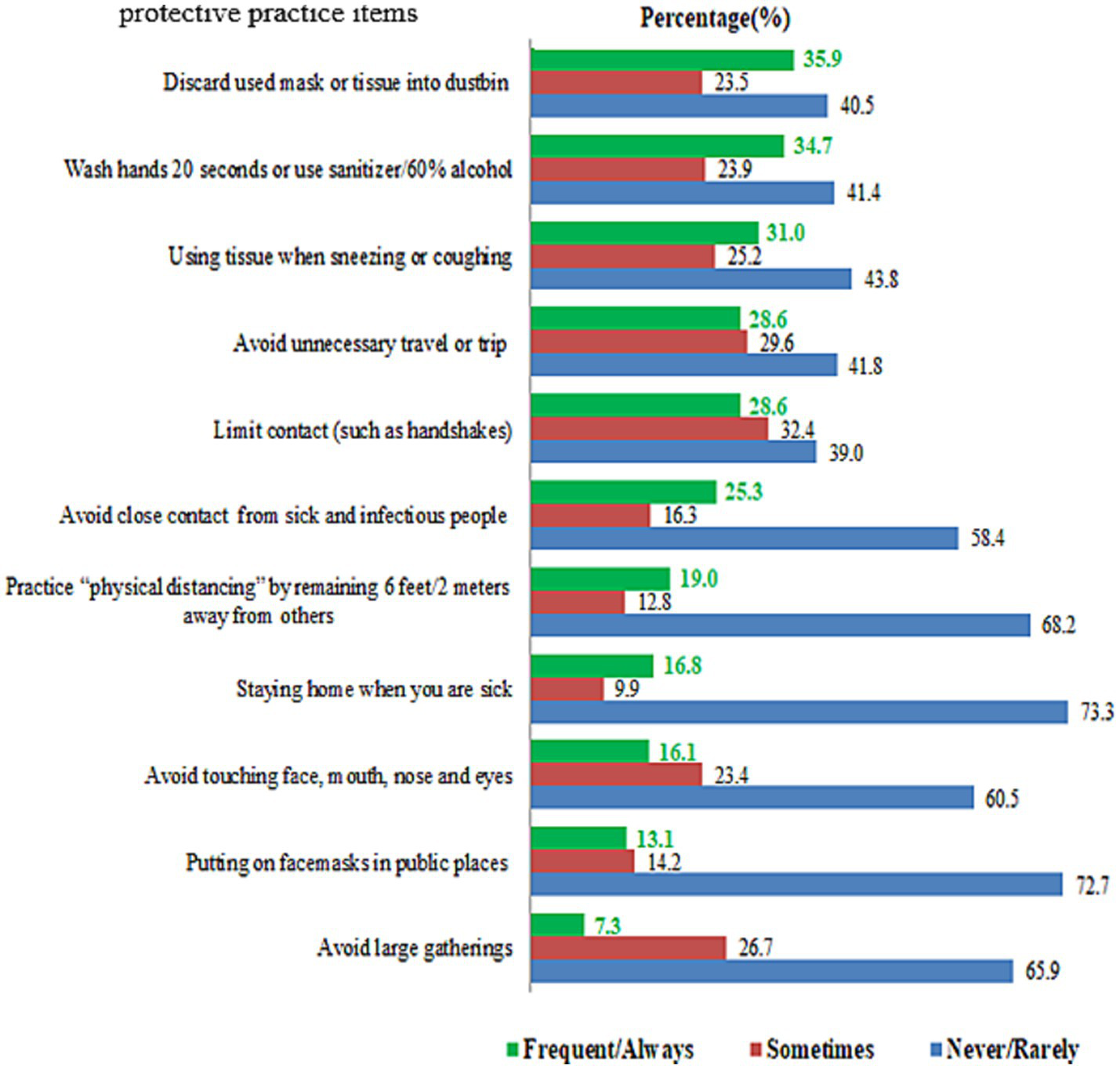
Frequency of protection practices in the community for COVID-19, Dessie City, Ethiopia, 2020.
3.5.3 Factors associated with the protection practices of COVID-19
Socio-demographic variables such as age, educational status, and monthly household income were found to be associated with good protection practices. Knowledge, risk perception, and belief in the efficacy of preventive methods were predictors of good protection practices. Participants with good knowledge levels and high-risk perceptions were more likely to exhibit good protective practices, with AORs of 4.45 (CI: 2.81–7.04) and 2.06 (CI: 1.38–3.08), respectively. Participants with “diploma level qualifications” and “degree or above level qualifications” were 2.04 times (CI: 1.08–3.83) and 2.94 times (CI: 1.64–5.28) more likely to have good protective practices than those with no formal education, respectively. The odds of good practice were 2.59 (AOR = 2.59, CI:1.31–5.15) and 3.05 (AOR = 3.05, CI:1.51–6.14) higher in study participants with household incomes of 5,001–10,000 ETB and ≥10,000 ETB than in participants with a low level of household income (i.e., <2000 ETB), respectively (Table 5).
Table 5
| Variables | Description | p-value | COR (CI) | p-value | AOR (CI) |
|---|---|---|---|---|---|
| Age (years) | <31 | 1 | 1 | ||
| 51–60 | 0.000 | 3.07 (1.82–5.16) | |||
| >60 | 0.000 | 3.52 (1.86–6.66) | 0.016 | 2.31 (1.17–4.59) | |
| Education | No formal education | 1 | 1 | ||
| Diploma-level | 0.000 | 3.97 (2.41–6.54) | 0.026 | 2.04 (1.08–3.83) | |
| Bachelor-level or above | 0.000 | 4.14 (2.59–6.59) | 0.000 | 2.94 (1.64–5.28) | |
| Family Size | <3.5 | 1 | |||
| >3.5 | 2.13 | 0.000 (1.59–2.86) | |||
| Income (ETB) | <2,000 | 1 | 1 | ||
| 5,001–10,000 | 0.000 | 2.82 (1.67–4.75) | 0.007 | 2.59 (1.31–5.15) | |
| ≥10,000 | 0.000 | 3.63 (2.11–6.25) | 0.002 | 3.05 (1.51–6.14) | |
| Knowledge | Poor | 1 | 1 | ||
| Good | 0.000 | 7.66 (5.22–11.24) | 0.000 | 4.45 (2.81–7.04) | |
| Risk perceptions | Low | 1 | 1 | ||
| High | 0.000 | 4.35 (3.21–5.91) | 0.000 | 2.06 (1.38–3.08) | |
| Belief in efficacy | Poor | 1 | 1 | ||
| High | 0.000 | 7.71 (5.54–10.74) | 0.000 | 5.22 (3.45–7.88) |
Factors associated with the practice of precautionary measures against COVID-19 among participants, Dessie City, Ethiopia, 2020.
AOR, Adjusted odds ratio; COR, crude odds ratio; ETB, Ethiopian Birr.
4 Discussion
COVID-19 poses a serious economic as well as public health threat. COVID-19 is effectively controlled by increasing public knowledge, perception, and prevention practices.
In line with the previous study (41), nearly nine out of ten participants believed that the virus caused this pandemic (87.5% vs. 96%). The majority of them reported fever, dry cough, difficulty breathing, and headache as symptoms of this pandemic. These findings agreed with those of Fang et al. (42).
The study found that 63% of the participants had good knowledge about the COVID-19 pandemic. This was comparable to findings from Bangladesh (63% vs. 61.4%) (27) but higher than in Myanmar, where the majority (87%) of the participants had poor knowledge (14), and lower than in India (43), Tanzania (44), China (12), and USA (45), where 80.64, 84.4, 90, and 80% of participants, respectively, had good knowledge. The variation in knowledge levels across studies may be due to differences in study population, timing of study, and access to information, highlighting the need for improved health education in the community.
Regarding the source of information, the majority of participants obtained COVID-19-related information from national TV, social media, and radio, with social media being a significant source, similar to studies in Myanmar (14) and Hong Kong (12), approximately half of participants obtained information about COVID-19 from social media. However, this finding differed from the Chinese study, in which the vast majority of participants (98%) obtained information about COVID-19 via social media (46). This shows a high proclivity for people to use social media in recent years. However, trust in the truthfulness of social media information was low. The most reliable information sources were health professionals, MOH official websites, and mass communication tools such as television or radio. These findings were imperative since they may indicate that more efforts should be made to deliver trustworthy information through the most popular and trusted communication channels.
Approximately two out of five participants thought they were at risk of COVID-19. This finding is lower than that of Thailand (75%) (30), Southwest Ethiopia (53.4%) (39), Ghana (68.3%) (20), and Sierra Leone (75%) (47). Furthermore, the study found a higher risk perception than 7.6% in India (48). This could be due to the differences in the study period, study population, and case count. The perceived severity of the disease was lower than in the Hong Kong (49) and Myanmar (14) studies, where almost all participants perceived the disease to be very severe. In this study only 16.8% of the participants thought COVID-19 was a deadly disease, whereas in Thailand, approximately 70% thought it was a severe and dangerous disease (30). Similarly, studies in China found that the majority of people thought COVID-19 was extremely severe (46, 50). In terms of survivorship, if infected, the communities in this study had a higher (53.5%) response rate than Myanmar (22%) (14) and Hong Kong (18%) (12). This explains why the people in this study setting become more hesitant to take preventive measures and require more convincing of the COVID-19 risk. According to a study conducted in Egypt (3), the majority of participants thought the disease was more dangerous for the older adult and those with chronic diseases. This could be because the risk of death from COVID-19 is higher in the older adult and those with medical conditions (51).
Perceived efficacy toward preventive measures such as hand hygiene, wearing face masks, and avoiding crowded areas was lower than in previous studies conducted in Myanmar and Hong Kong (i.e., 49.1% vs. 80 and 90%, respectively) (12, 14). The belief in the efficacy of preventive methods is important information for improving epidemic control. This indicates that more work is required to ratify belief in efficacy.
Handwashing practices were lower in studies conducted in the Philippines (28), Hong Kong (49), and Bangladesh (52) (58.6% vs. 89.9, 95.8, and 98.6%, respectively), but higher than a study conducted in Myanmar (14) (58.6% vs. 44.9%). Avoiding crowded places was lower in this study than in previous studies from Myanmar (14) and Hong Kong (49) (34.1% vs. 57.9 and 88.1%, respectively). Furthermore, the practice of avoiding crowded areas was lower than in a study conducted in the Philippines (28), Bangladesh (13), Tanzania (44), China (12), Nepal (53), and Malaysia (29), where 62.9, 87.97, 77, 96.4, 94.9, and 51.2% of people avoid social gatherings, respectively.
Only 26.7% of participants followed the principles of staying at home. This was much lower than in the Bangladesh study (52), where the majority (93.2%) of respondents followed the stay-at-home principle. Cough etiquette practice was markedly lower than in a Hong Kong study (49) (56.2% vs. 97.1%), but higher than in a Myanmar study (14) (56.2% vs. 47.3%). Only 27.3% of participants put on a face mask when leaving their home. It was much lower than in studies conducted in Bangladesh (13), Malaysia (29), Tanzania (44), China (12), and Nepal (53), where nearly 75, 83.4, 80, 98, and 88.2% of the participants used a face mask. This disparity was attributed to socioeconomic factors, culture, case count, beliefs in the efficacy of preventive measures, and perceptions of COVID-19 risk.
The practice of COVID-19 prevention measures in this study was 38.6%, which was much lower than the study conducted in Iran (54), 71%, and Bangladesh (27), 51.6% of participants had good COVID-19 prevention practices, but higher than the study conducted in Myanmar, 22% (14). The disparities could be explained by differences in information-seeking behaviour, case counts, death rates, misconceptions, and study time.
In line with the study done in Lebanon (41), Iran (55), India (43), Hong Kong (49), and Malaysia (56), education was a strong predictor of protection practices. Behavioural models advocate education is an influential determining factor of healthy behaviour (57). Education leads to better information-gathering habits and efficient use of health inputs (58). This may explain why more educated respondents engaged in precautionary behaviours. This underlines the importance of education in an attempt to raise protection.
In line with the study done in China (12), high income was associated with good practices. Economic status is the primary determinant of actions for maintaining one’s health (57). It has been demonstrated that the low-income households do not use preventive methods (59). In addition, income determines the likelihood of purchasing personal protective equipment, such as a face mask and hand sanitiser. Individuals with low income fail to observe preventive methods; instead, they prefer to continue their daily activities to satisfy their basic needs during the transmission period. This may explain why high-income groups had good preventive practices. Therefore, the government should recognise income discrepancies and provide targeted support to decline the transmission rate across the income spectrum.
Protective practices were predicted by knowledge, aligning with findings from other studies (12, 60). Knowledge enhances awareness, dispels misconceptions, and supports informed decision-making. However, its effectiveness can be shaped by cultural beliefs to the pandemic, socioeconomic conditions, and trust in health systems. Traditional practices, resources limitation, and distrust may hinder the adoption of scientific protective behaviours. In line with other studies (61), risk perception also strongly predicts protective behaviour. People with a low perception of risk should be a prime target for public health education. Additionally, belief in the effectiveness of preventive methods was the strongest predictor of adherence to protective behaviours during the pandemic.
These findings showed that protective behaviour implementation largely depends on community engagement in the prevention pathway. Public health education should focus on enhancing knowledge while addressing key barriers, particularly among individuals with low risk perception and limited belief in the effectiveness of preventive measures, to ensure effective control over the spread of this virus.
5 Strengths and limitations of the study
5.1 Strengths of the study
In the study setting, although studies had examined knowledge and protective practices for COVID-19, those comprising risk perception in their work were limited. Most previous studies were online application-based surveys; as a strong point, this research was a field-based study. The use of a field survey in the data collection process in this study may have resulted in an adequate representation of the less educated groups. This study solves the issue of representation and the methodological concerns of previous studies.
5.2 Limitations of the study
The cross-sectional nature of this study might make it tougher to establish a cause-and-effect relationship. Furthermore, the study is limited to one city administration in Northeast Ethiopia rather than the entire country, which is a limitation.
6 Conclusion
The study found that two-thirds of the participants had good knowledge. However, there was a low perception of the risk and poor practices for preventing COVID-19. There is an urgent need to fill the risk perception and knowledge gap to control the expansion of the COVID-19 outbreak.
This study revealed that COVID-19 knowledge, efficacy beliefs, and risk perception significantly predicted precautionary behaviour. Older people, people with a high income, a high level of education, and a large family size readily showed a high propensity toward protection practices. As a result, the young population, as well as lower-income and education groups, would be challenging to the control efforts and will require special attention. Risk communication and community engagement efforts should be considered in fighting against this pandemic.
The results of this study indicate the focus areas that need to be addressed and disclose the need for continued monitoring. The media should make it easier to get reliable health information. Moreover, future research would identify the possible barriers to adopting protective behaviours in fighting the pandemic disease and their solutions.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was obtained from the Ethics Review Committee of the College of Medicine and Health Sciences, Wollo University (CMHS-456/013/12), and informed consent was secured from each participant.
Author contributions
HNT: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. EMB: Data curation, Formal analysis, Investigation, Methodology, Software, Writing – review & editing. BDW: Data curation, Formal analysis, Investigation, Methodology, Writing – review & editing. TGF: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
COVID-19, Coronavirus disease 2019; EPHI, Ethiopian Public Health Institute; EPPM, Extended Parallel Process Model; NCoV, Novel Corona Virus; NPIs, Non-Pharmaceutical Interventions; PHM, Public Health Measures; PPE, Personal Protective Equipment; SARS, Severe Acute Respiratory Syndrome; SARS-CoV-2, Severe Acute Respiratory Syndrome Coronavirus 2; WHO, World Health Organization.
References
1.
Enitan SS Ibeh IN Oluremi AS Olayanju AO Itodo GE . The 2019 Novel coronavirus outbreak: current crises, controversies and global strategies to prevent a pandemic. Int J Pathog Res. (2020) 4:1–16. doi: 10.9734/ijpr/2020/v4i130099
2.
Ye Z-W Yuan S Yuen K-S Fung S-Y Chan C-P Jin D-Y . Zoonotic origins of human coronaviruses. Int J Biol Sci. (2020) 16:1686–97. doi: 10.7150/ijbs.45472
3.
Abdelhafiz AS Mohammed Z Ibrahim ME Ziady HH Alorabi M Ayyad M et al . Knowledge, perceptions, and attitude of egyptians towards the novel coronavirus disease (COVID-19). J Community Health. (2020) 45:881–90. doi: 10.1007/s10900-020-00827-7
4.
Shigemura J Ursano RJ Morganstein JC Kurosawa M Benedek DM . Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin Neurosci. (2020) 74:281–2. doi: 10.1111/pcn.12988
5.
Phelan AL Katz R Gostin LO . The novel coronavirus originating in Wuhan, China: challenges for global health governance. JAMA. (2020) 323:709–10. doi: 10.1001/jama.2020.1097
6.
Zikargae MH . COVID-19 in Ethiopia: assessment of how the Ethiopian government has executed administrative actions and managed risk communications and community engagement. Risk Manag Healthc Policy. (2020) 13:2803–10. doi: 10.2147/RMHP.S278234
7.
Singhal T . A review of coronavirus disease-2019 (COVID-19). Indian J Pediatr. (2020) 87:281–6. doi: 10.1007/s12098-020-03263-6
8.
Zhou C . Evaluating new evidence in the early dynamics of the novel coronavirus COVID-19 outbreak in Wuhan, China with real time domestic traffic and potential asymptomatic transmissions. medRxiv. (2020) 1–15. doi: 10.1101/2020.02.15.20023440
9.
Shi H Han X Jiang N Cao Y Alwalid O Gu J et al . Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. (2020) 20:425–34. doi: 10.1016/S1473-3099(20)30086-4
10.
Cao J Tu W-J Cheng W Yu L Liu Y-K Hu X et al . Clinical features and short-term outcomes of 102 patients with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. (2020) 71:748–55. doi: 10.1093/cid/ciaa243
11.
Khosravi M . Perceived risk of COVID-19 pandemic: the role of public worry and trust. Electron J Gen Med. (2020) 17:em203. doi: 10.29333/ejgm/7856
12.
Zhong B-L Luo W Li H-M Zhang Q-Q Liu X-G Li W-T et al . Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci. (2020) 16:1745–52. doi: 10.7150/ijbs.45221
13.
Haque T Hossain KM Bhuiyan MMR Ananna SA Chowdhury SH Islam MR et al . Knowledge, attitude and practices (KAP) towards COVID-19 and assessment of risks of infection by SARS-CoV-2 among the Bangladeshi population: An online cross sectional survey. North Carolina, United States: Research Square (2020). doi: 10.21203/rs.3.rs-24562/v2
14.
Mya Kyaw S Aye S Hlaing Win A Hlaing Su S Thida A . Awareness, perceived risk and protective behaviours of Myanmar adults on COVID-19. Int J Community Med Public Health. (2020) 7:1627. doi: 10.18203/2394-6040.ijcmph20201530
15.
Huang C Wang Y Li X Ren L Zhao J Hu Y et al . Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
16.
Lai C-C Shih T-P Ko W-C Tang H-J Hsueh P-R . Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. (2020) 55:105924. doi: 10.1016/j.ijantimicag.2020.105924
17.
Acter T Uddin N Das J Akhter A Choudhury TR Kim S . Evolution of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as coronavirus disease 2019 (COVID-19) pandemic: a global health emergency. Sci Total Environ. (2020) 730:138996. doi: 10.1016/j.scitotenv.2020.138996
18.
Tolu LB Ezeh A Feyissa GT . How prepared is Africa for the COVID-19 pandemic response? The case of Ethiopia. Risk Manag Healthc Policy. (2020) 13:771–6. doi: 10.2147/RMHP.S258273
19.
Betsch C Wieler LH Habersaat K . Monitoring behavioural insights related to COVID-19. Lancet. (2020) 395:1255–6. doi: 10.1016/S0140-6736(20)30729-7
20.
Serwaa D Lamptey E Appiah AB Senkyire EK Ameyaw JK . Knowledge, risk perception and preparedness towards coronavirus disease-2019 (COVID-19) outbreak among Ghanaians: a quick online cross-sectional survey. Pan Afr Med J. (2020) 35:44. doi: 10.11604/pamj.supp.2020.35.2.22630
21.
Shabu SA M-Amin K Mahmood KI Shabila NP . Risk perception and behavioral response to COVID-19: a survey of university students and staff in the Iraqi Kurdistan region. Soc Work Public Health. (2021) 36:474–85. doi: 10.1080/19371918.2021.1915909
22.
Ethiopia U . COVID-19 and operational update (14 December 2020). Ethiopia: ReliefWeb (2021).
23.
Baye K . COVID-19 prevention measures in Ethiopia: Current realities and prospects. Washington, D.C., United States: International Food Policy Research Institute (IFPRI) (2020). doi: 10.2499/p15738coll2.133729
24.
Zhang X Wang F Zhu C Wang Z . Willingness to self-isolate when facing a pandemic risk: model, empirical test, and policy recommendations. Int J Environ Res Public Health. (2020) 17:197. doi: 10.3390/ijerph17010197
25.
Pulcini C Pradier C Samat-Long C Hyvernat H Bernardin G Ichai C et al . Factors associated with adherence to infectious diseases advice in two intensive care units. J Antimicrob Chemother. (2006) 57:546–50. doi: 10.1093/jac/dki483
26.
Witte K . Fear control and danger control: a test of the extended parallel process model (EPPM). Commun Monogr. (1994) 61:113–34. doi: 10.1080/03637759409376328
27.
Banik R Rahman M Sikder MT Rahman QM Pranta MUR . Knowledge, attitudes, and practices related to COVID-19 outbreak among Bangladeshi young adults: A web-based cross-sectional analysis. England, United Kingdom: Journal of Public Health. (2023) 31:9–19. doi: 10.1007/s10389-020-01432-7
28.
Lau LL Hung N Go DJ Ferma J Choi M Dodd W et al . Knowledge, attitudes and practices of COVID-19 among income-poor households in the Philippines: a cross-sectional study. J Glob Health. (2020) 10:011007. doi: 10.7189/jogh.10.011007
29.
Azlan AA Hamzah MR Sern TJ Ayub SH Mohamad E . Public knowledge, attitudes and practices towards COVID-19: a cross-sectional study in Malaysia. PLoS One. (2020) 15:e0233668. doi: 10.1371/journal.pone.0233668
30.
Srichan P Apidechkul T Tamornpark R Yeemard F Khunthason S Kitchanapaiboon S et al . Knowledge, attitude and preparedness to respond to the 2019 novel coronavirus (COVID-19) among the bordered population of northern Thailand in the early period of the outbreak: a cross-sectional study. New Delhi, India: WHO South-East Asia Journal of Public Health (2020) 9. doi: 10.4103/2224-3151.294305
31.
Magdy DM Metwally A Magdy O . Assessment of community psycho-behavioral responses during the outbreak of novel coronavirus (2019-nCoV): a cross sectional study. Missouri, United States: AIMS Public Health (2020) 9:26–40. doi: 10.3934/publichealth.2022003
32.
Bish A Michie S . Demographic and attitudinal determinants of protective behaviours during a pandemic: a review. Br J Health Psychol. (2010) 15:797–824. doi: 10.1348/135910710X485826
33.
Rudisill C . How do we handle new health risks? Risk perception, optimism, and behaviors regarding the H1N1 virus. J Risk Res. (2013) 16:959–80. doi: 10.1080/13669877.2012.761271
34.
Zhong Y Liu W Lee T-Y Zhao H Ji J . Risk perception, knowledge, information sources and emotional states among COVID-19 patients in Wuhan, China. Nurs Outlook. (2021) 69:13–21. doi: 10.1016/j.outlook.2020.08.005
35.
Wise T Zbozinek TD Michelini G Hagan CC Mobbs D . Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States. R Soc Open Sci. (2020) 7:200742. doi: 10.1098/rsos.200742
36.
Kalaycioglu O . Guidance for research on the Covid-19 disease in times of pandemic. J Health Soc Sci. (2020) 5:177–86.
37.
Ning L Niu J Bi X Yang C Liu Z Wu Q et al . The impacts of knowledge, risk perception, emotion and information on citizens’ protective behaviors during the outbreak of COVID-19: a cross-sectional study in China. BMC Public Health. (2020) 20:1751. doi: 10.1186/s12889-020-09892-y
38.
Taber KS . The use of Cronbach’s alpha when developing and reporting research instruments in science education. Res Sci Educ. (2018) 48:1273–96. doi: 10.1007/s11165-016-9602-2
39.
Asefa A Qanche Q Hailemariam S Dhuguma T Nigussie T . Risk perception towards COVID-19 and its associated factors among waiters in selected towns of Southwest Ethiopia. Risk Manag Healthc Policy. (2020) 13:2601–10. doi: 10.2147/RMHP.S276257
40.
Islam S Emran GI Rahman E Banik R Sikder T Smith L et al . Knowledge, attitudes and practices associated with the COVID-19 among slum dwellers resided in Dhaka City: a Bangladeshi interview-based survey. J Public Health (Oxf). (2021) 43:13–25. doi: 10.1093/pubmed/fdaa182
41.
Sakr S Ghaddar A Sheet I Eid AH Hamam B . Knowledge, attitude and practices related to COVID-19 among young Lebanese population. BMC Public Health. (2021) 21:1–11. doi: 10.1186/s12889-021-10575-5
42.
Fang Y Nie Y Penny M . Transmission dynamics of the COVID-19 outbreak and effectiveness of government interventions: a data-driven analysis. J Med Virol. (2020) 92:645–59. doi: 10.1002/jmv.25750
43.
Tomar BS Singh P Nathiya D Suman S Raj P Tripathi S et al . Indian communitys knowledge, Attitude & Practice towards COVID-19. medRxiv. (2020) 1–20. doi: 10.1101/2020.05.05.20092122
44.
Byanaku A Ibrahim M . Knowledge, attitudes, and practices (KAP) towards COVID-19: a quick online cross-sectional survey among Tanzanian residents. medRxiv. (2020)
45.
Clements JM . Knowledge and behaviors toward COVID-19 among US residents during the early days of the pandemic: cross-sectional online questionnaire. JMIR Public Health Surveill. (2020) 6:e19161. doi: 10.2196/19161
46.
Chen Y Jin Y Zhu L Fang Z Wu N Du M et al . The network investigation on knowledge, attitude and practice about novel coronavirus pneumonia of the residents in Anhui Province. Zhonghua Yu Fang Yi Xue Za Zhi. (2020) 54:E004-E. doi: 10.3760/cma.j.issn.0253-9624.2020.0004
47.
Sengeh P Jalloh MB Webber N Ngobeh I Samba T Thomas H et al . Community knowledge, perceptions and practices around COVID-19 in Sierra Leone: a nationwide, cross-sectional survey. BMJ Open. (2020) 10:e040328. doi: 10.1136/bmjopen-2020-040328
48.
Kuang J Ashraf S Das U Bicchieri C . Awareness, risk perception, and stress during the COVID-19 pandemic in communities of Tamil Nadu, India. Int J Environ Res Public Health. (2020) 17:7177. doi: 10.3390/ijerph17197177
49.
Kwok KO Li KK Chan HH Yi YY Tang A Wei WI et al . Community responses during the early phase of the COVID-19 epidemic in Hong Kong: risk perception, information exposure and preventive measures. MedRxiv. (2020). 1–26. doi: 10.1101/2020.02.26.20028217
50.
Li J-B Yang A Dou K Wang L-X Zhang M-C Lin X-Q . Chinese public’s knowledge, perceived severity, and perceived controllability of COVID-19 and their associations with emotional and behavioural reactions, social participation, and precautionary behaviour: a national survey. BMC Public Health. (2020) 20:1589. doi: 10.1186/s12889-020-09695-1
51.
Ioannidis JPA Axfors C Contopoulos-Ioannidis DG . Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicenters. Environ Res. (2020) 188:109890. doi: 10.1016/j.envres.2020.109890
52.
Rahman A Sathi NJ . Knowledge, attitude, and preventive practices toward COVID-19 among Bangladeshi internet users. Electron J Gen Med. (2020) 17:em245. doi: 10.29333/ejgm/8223
53.
Hussain A Garima T Singh BM Ram R Tripti RP . Knowledge, attitudes, and practices towards COVID-19 among Nepalese residents: a quick online cross-sectional survey. Asian J Med Sci. (2020) 11:6–11. doi: 10.3126/ajms.v11i3.28485
54.
Jahangiry L Bakhtari F Sohrabi Z Reihani P Samei S Ponnet K et al . Risk perception and behavioral responses related to COVID-19 among the Iranian general population: An Application of the Extended Parallel Process Model. London, United Kingdom: BMC Public Health (2020) 20. doi: 10.1186/s12889-020-09681-7
55.
Erfani A Shahriarirad R Ranjbar K Mirahmadizadeh A Moghadami M . Knowledge, attitude and practice toward the novel coronavirus (COVID-19) outbreak: a population-based survey in Iran. Bull World Health Organ. (2020) 30:1–23. doi: 10.2471/BLT.20.256651
56.
Mohamad EM Azlan AA Hamzah MR Tham JS Ayub SH . Public knowledge, attitudes and practices towards COVID-19: a cross-sectional study in Malaysia. medRxiv. (2020) 1–15. doi: 10.1101/2020.04.29.20085563
57.
Mantwill S Monestel-Umaña S Schulz PJ . The relationship between health literacy and health disparities: a systematic review. PLoS One. (2015) 10:e0145455. doi: 10.1371/journal.pone.0145455
58.
Brunello G Fort M Schneeweis N Winter-Ebmer R . The causal effect of education on health: what is the role of health behaviors?Health Econ. (2016) 25:314–36. doi: 10.1002/hec.3141
59.
Braveman PA Cubbin C Egerter S Williams DR Pamuk E . Socioeconomic disparities in health in the United States: what the patterns tell us. Am J Public Health. (2010) 100:S186–96. doi: 10.2105/AJPH.2009.166082
60.
Kebede Y Yitayih Y Birhanu Z Mekonen S Ambelu A . Knowledge, perceptions and preventive practices towards COVID-19 among Jimma University medical center visitors, Southwest Ethiopia. California, United States: PLOS ONE (2020) 15:1–15. doi: 10.1371/journal.pone.0233744
61.
Chan EYY Huang Z Lo ESK Hung KKC Wong ELY Wong SYS . Sociodemographic predictors of health risk perception, attitude and behavior practices associated with health-emergency disaster risk Management for Biological Hazards: the case of COVID-19 pandemic in Hong Kong, SAR China. Int J Environ Res Public Health. (2020) 17:3869. doi: 10.3390/ijerph17113869
Summary
Keywords
COVID-19, knowledge, risk perception, protection practice, Dessie, Ethiopia
Citation
Toleha HN, Bayked EM, Workneh BD and Fenta TG (2025) Risk perceptions, knowledge and protection practices related to COVID-19 in Dessie City Administration, Northeast Ethiopia: a community-based study. Front. Public Health 13:1505621. doi: 10.3389/fpubh.2025.1505621
Received
03 October 2024
Accepted
21 April 2025
Published
09 May 2025
Volume
13 - 2025
Edited by
Roland Salmon, Public Health Wales, United Kingdom
Reviewed by
Kenesh O. Dzhusupov, International Higher School of Medicine, Kyrgyzstan
Douglas Bulafu, Makerere University, Uganda
Updates
Copyright
© 2025 Toleha, Bayked, Workneh and Fenta.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Husien Nurahmed Toleha, husen3431@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.