- 1Department of Health Management, College of Public Health and Health Informatics, University of Ha’il, Ha’il, Saudi Arabia
- 2Department of Management and Information Systems, College of Business Administration, University of Ha’il, Ha’il, Saudi Arabia
- 3Department of Public Health, College of Public Health and Health Informatics, University of Ha’il, Ha’il, Saudi Arabia
- 4School of Management, Doon University, Dehradun, Uttarakhand, India
- 5Department of Management Studies, Graphic Era Deemed to be University, Dehradun, Uttarakhand, India
In recent years, Artificial Intelligence (AI) is transforming healthcare systems globally and improved the efficiency of its delivery. Countries like Saudi Arabia are facing unique adoption challenges in their public healthcare, these challenges are specific to AI literacy, understanding and effective usage of AI technologies. In addition, cultural, regulatory and operational barriers increase the complication of integrating AI literacy into public healthcare operations. In spite of its critical contribution in enabling sustainable healthcare development, limited studies have addressed these adoption challenges. Our study explores the AI literacy adoption barriers in context to Saudi Arabian public healthcare sector, focusing on its relevance for advancing healthcare operations and achieving Sustainable Development Goals (SDGs). The research aims to identifying and addressing the adoption challenges of Artificial Intelligence literacy within the public healthcare in Saudi Arabia. The research aims to enhance the understanding of AI literacy, its necessity for enhancing healthcare operations, and the specific hurdles that impede its successful AI adoption in Saudi Arabia’s public healthcare ecosystem. The research employs a qualitative analysis using the T-O-E framework to explore the adoption challenges of AI literacy. Additionally, the Best-Worse Method (BWM) is applied to evaluate the adoption challenges to AI literacy adoption across various operational levels within Saudi Arabia’s public healthcare supply chain. The study uncovers substantial adoption challenges at operational, tactical, and strategic level, including institutional readiness, data privacy, and compliance with regulatory frameworks. These challenges complicate the adoption of AI literacy in the Saudi public healthcare supply chains. The research offers critical insights into the various issues affecting the promotion of AI literacy in Saudi Arabia’s public healthcare sector. This evidence-based study provides essential commendations for healthcare professionals and policymakers to effectively address the identified challenges, nurturing an environment beneficial to the integration of AI literacy and advancing the goals of sustainable healthcare development.
1 Introduction
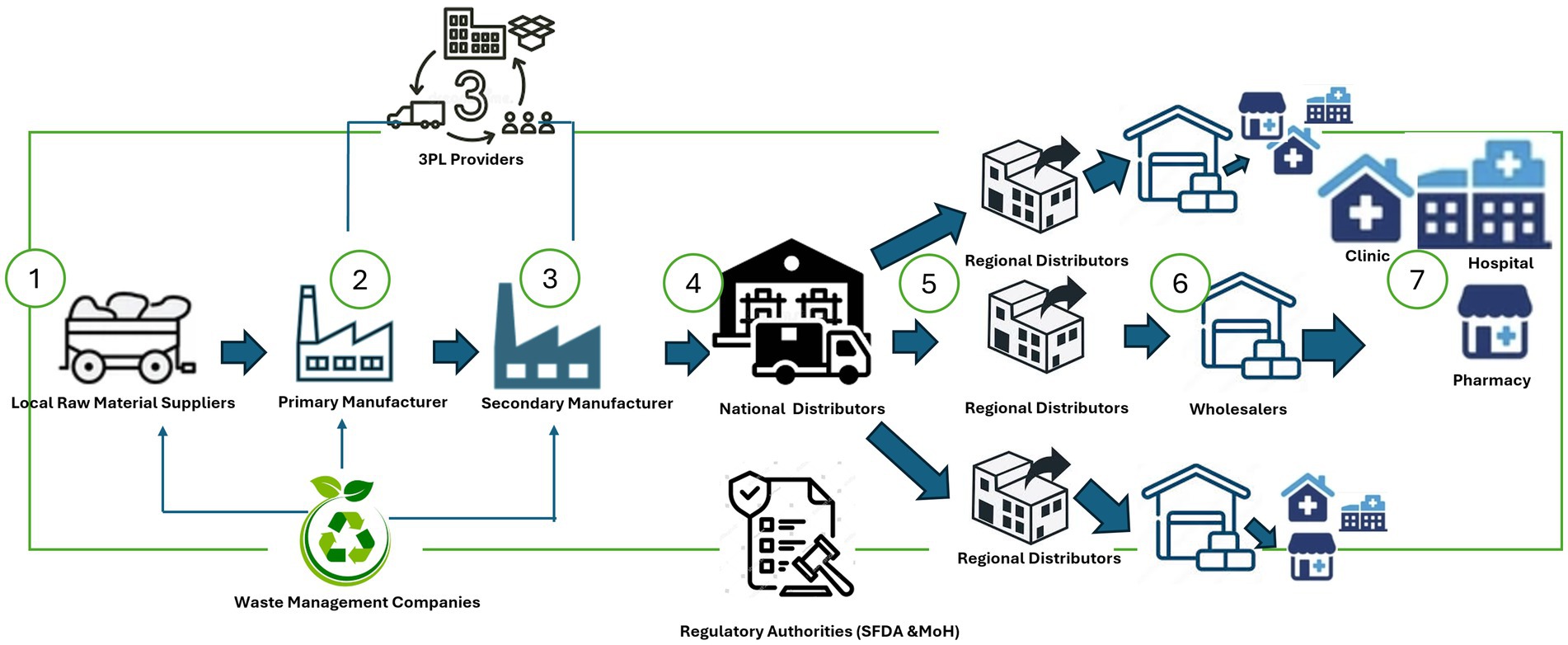
Artificial Intelligence (AI) is reshaping public healthcare systems, enhancing the prediction, treatment, and management of health conditions (1). In line with Vision 2030, Saudi Arabia is committed to advancing technological integration, particularly AI, within its public healthcare, offering substantial promise while facing formidable challenges (2). As depicted in Figure 1, A typical public healthcare system (PHS) consists of key Supply Chain players, including Local Raw Material Suppliers, Primary and Secondary Manufacturers (medical suppliers, pharmaceuticals, essential healthcare equipment makers), Logistics providers, National and Regional Distributors, public health service providers (Government hospitals and clinics) and essentially the regulatory bodies (including SFDA and MoH) (3).
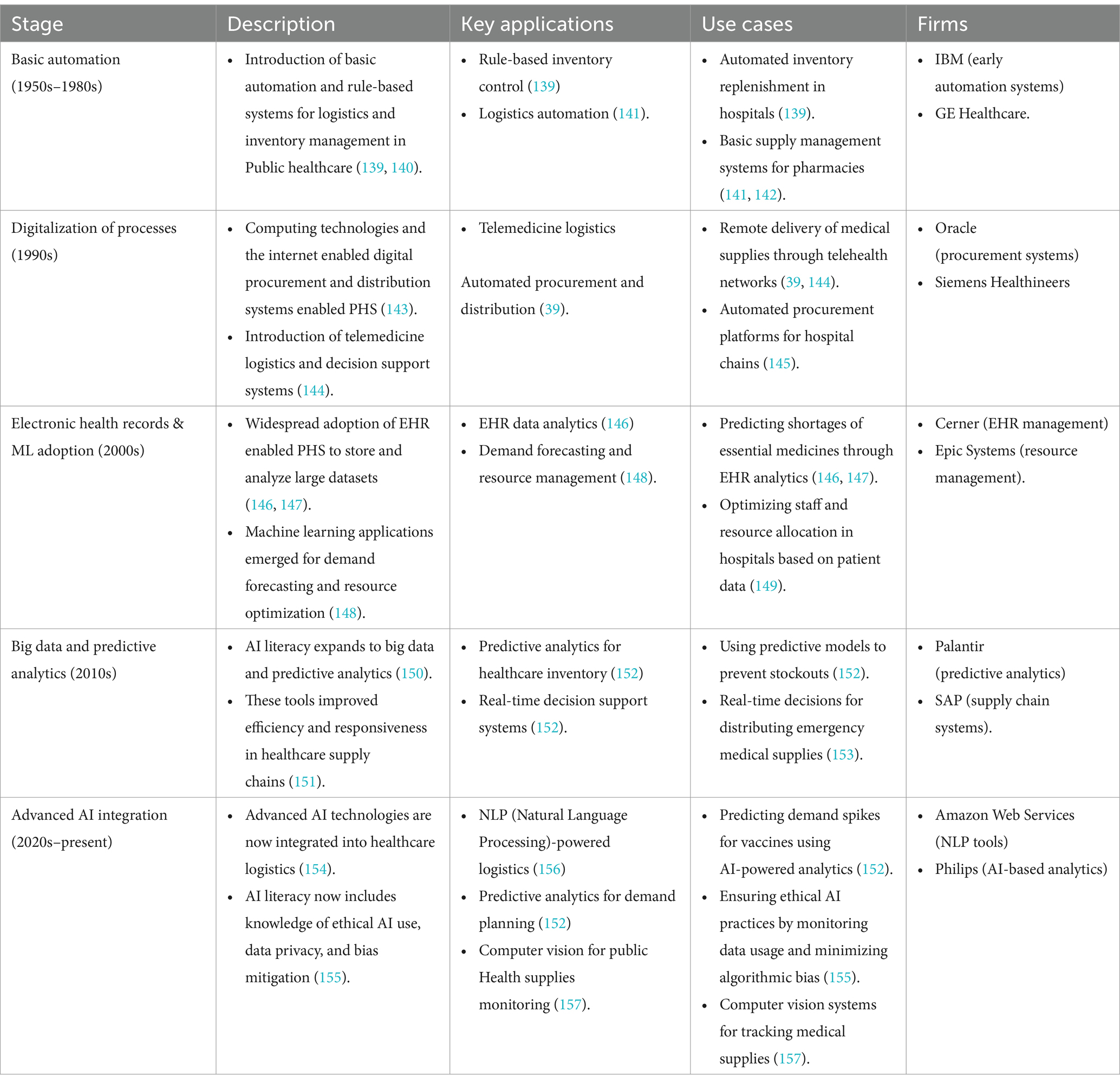
To unleash the capacity of AI in enhancing healthcare delivery, it is critical to identify and develop strategies that promote AI literacy among critical stakeholders, addressing the challenges hindering its effective implementation (4, 5). AI has tremendous potential to analyze electronic health data, uncover patterns, and offer valuable insights for decision-making (6, 7). Traditionally, the healthcare industry generates vast amounts of data through clinical health records, image data, and patient monitoring (8, 9). Over the decades, AI literacy in healthcare supply chains has evolved significantly while harnessing the data to improve diagnostics, treatments, and patient outcomes (10). In the 1950s, basic automation and rule-based logistics and inventory management systems of healthcare inventory were introduced (11). By the 1990s, the rise of computing technologies and the internet facilitated the digitalization of supply chain processes. Also, it introduced the need for AI literacy in areas like telemedicine, logistics and decision support systems (11). In the 2000s, the adoption of Electronic Health Records (EHR) enabled healthcare supply chains to analyze large datasets for demand forecasting and resource optimization (11). By the 2010s, AI literacy expanded to include knowledge of data decision making, which became essential for efficiency and responsiveness in the Supply Chains (10, 11). Today, AI literacy in public healthcare encompasses advanced digital technologies for managing complex logistics, predictive analytics for inventory and demand planning, and the ethical use of AI to ensure transparency, mitigate bias, and maintain data privacy in the increasingly interconnected public healthcare ecosystem (12–14). Table 1 explained the evolution of AI Literacy.
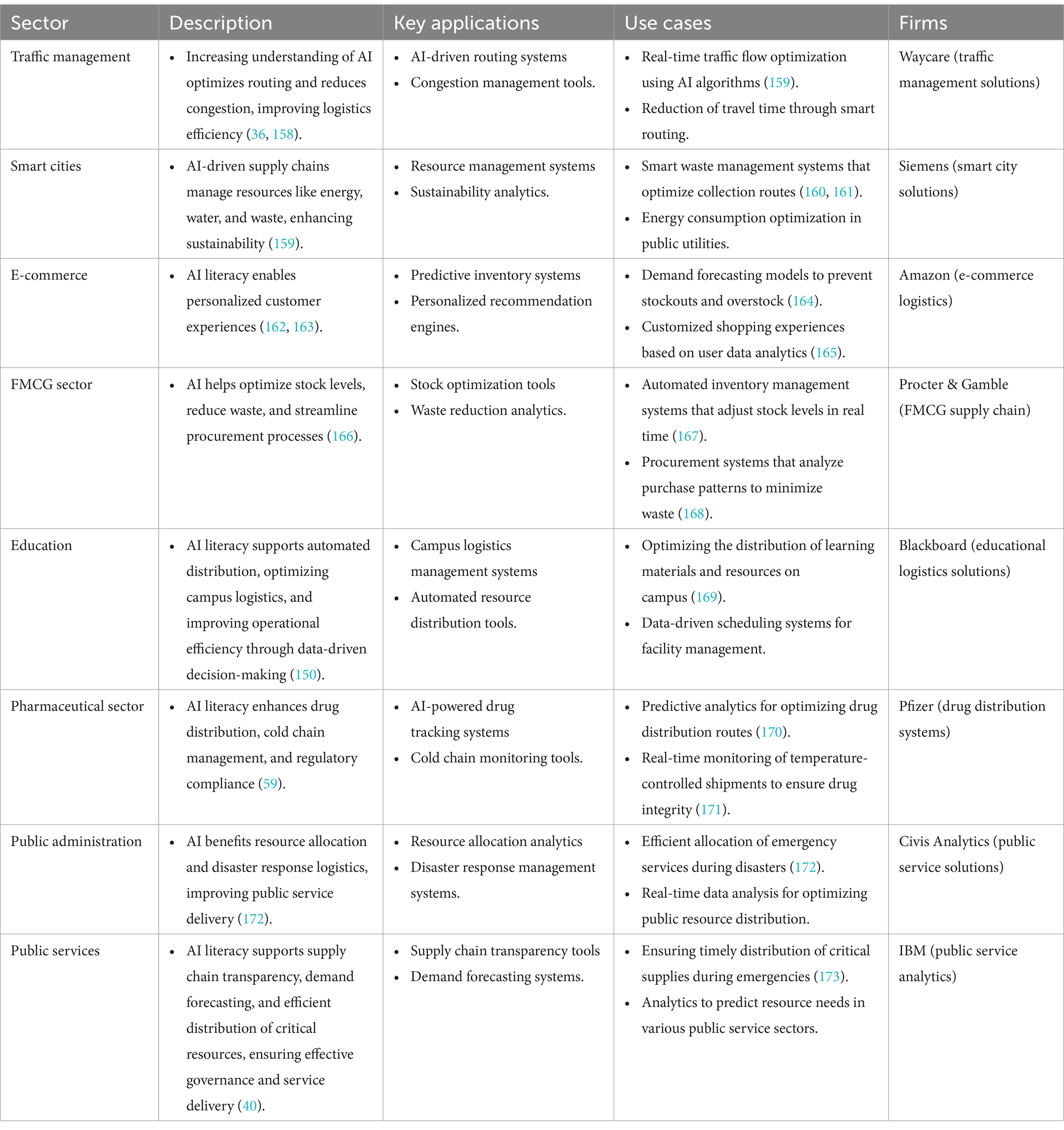
AI literacy has recently advanced beyond basic automation comprehension, integrating big data analytics for predictive insights (15, 16). This progression has profoundly impacted PHS through data-driven decisions, predictive resource allocation, and improved patient outcomes (16). Identically, AI literacy significantly enhances operational and Supply Chain activities across various sectors while better adoption and implementation and strengthening the capabilities of users. In traffic management, the Increasing understanding of AI optimizes routing and reduces congestion, improving logistics efficiency (4, 17). For smart cities, AI-driven systems manage energy, water, and waste resources, enhancing sustainability (18). In e-commerce, AI literacy enables predictive analytics for demand forecasting, inventory management, personalized customer experiences, driving efficiency (19). In the FMCG (Fast-moving consumer goods) sector, AI helps optimize stock levels, reduce waste, and streamline procurement processes (20). In education, AI literacy can support automated distribution, optimize campus logistics, and improve operational efficiency using data-driven decision-making (21). AI literacy can significantly influence the pharmaceutical sector by enhancing the effectiveness in drug distribution, cold chain management, and regulatory compliance (22). Public administration benefits from AI in resource allocation and disaster response logistics, improving public services delivery (23). In public services, AI literacy supports supply chain transparency, demand forecasting, and efficient distribution of critical resources, ensuring effective governance and service delivery (24). Table 2 demonstrates role of AI literacy in improving the operational efficiency in various industries.
Thus, across all sectors, even with slow adoption, organizations can enhance operations, optimize costs, and enhance decision making. The AI advancements are particularly relevant in Saudi Arabia to implement AI-driven solutions, aligning with Sustainable Development Goals (SDGs) to enhance healthcare sustainability, efficiency, and equity (25, 26). However, challenges remain in ensuring widespread AI literacy among stakeholders to leverage these technologies for sustainable public health improvements fully. Thus, the research aims to address research questions and objectives are as follows:
RQ1: What are the major adoption challenges to AI literacy in PHS, in Saudi Arabia?
RO1: To identify the key adoption challenges while adopting AI in PHS, in Saudi Arabia.
RQ2: What are the extremely critical AI literacy adoption challenges in PHS, in Saudi Arabia?
RO2: To identify extremely AI adoption challenges and discuss the roadmap to reduce AI adoption barriers in PHS, in Saudi Arabia.
RQ3: What is the strategic roadmap to AI adoption in PHS.
RO3: To suggest the framework for exploring AI adoption challenges, emphasizing the prioritization of critical barriers and strategic roadmap development.
The organization of the research paper as: Section 2 provides comprehensive review on AI literacy within Public Healthcare System, examined through the lens of SDGs, and presents the foundational theories underpinning the study. Section 3 explained methodology employed in the current research. Section 4 introduces a comprehensive framework for AI implementation. Section 5 details the main outcomes of the study. Section 6 proposes a strategic roadmap to mitigate the challenges hindering AI adoption in PHS. Finally, Section 7 explains limitations and highlights areas for further studies.
2 Literature review
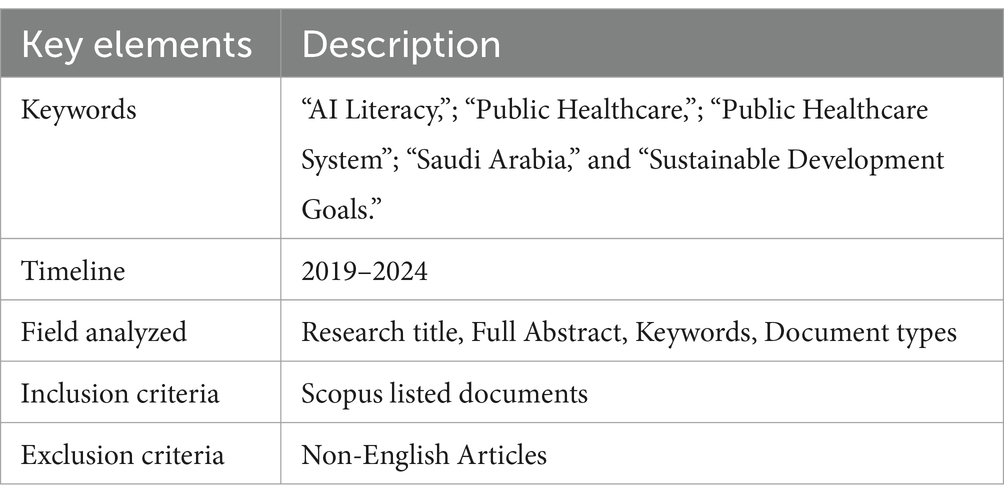
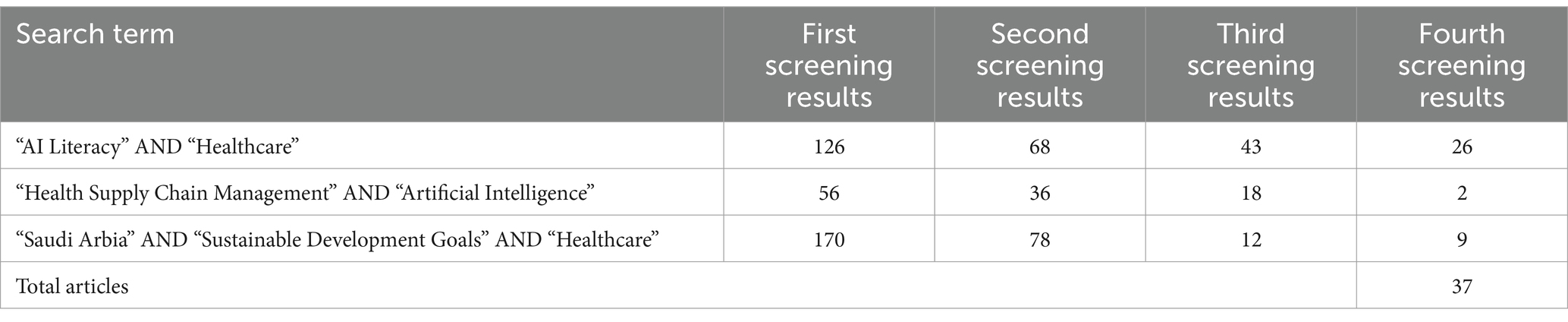
The Systematic Literature Review (SLR) has been carried out on relevant literature from Scopus database. SLR process conducted using multiple keywords, including “AI Literacy,”; “Public Healthcare,”; “Public Healthcare System,”; “Saudi Arabia,” and “Sustainable Development Goals.” The SLR used a timeline between 2019 and 2024. The search yielded 518 articles. Table 3 depicts the search protocol used for this study.
In the first screening results into the removal of duplicate articles, 352 publications that meet with the research objectives. Further, in next level of screening, working papers, conference papers, and conference proceedings were also omitted and 183 articles where retrieved. After further investigation in the third screening, it was determined that 73 papers were pertinent to the study questions. In the fourth screening A cross-referencing method was used to finalize the paper selection process, and 37 papers were ultimately chosen. The SLR procedure used by the authors for this investigation (Table 4).
2.1 AI in public healthcare in Saudi Arabia
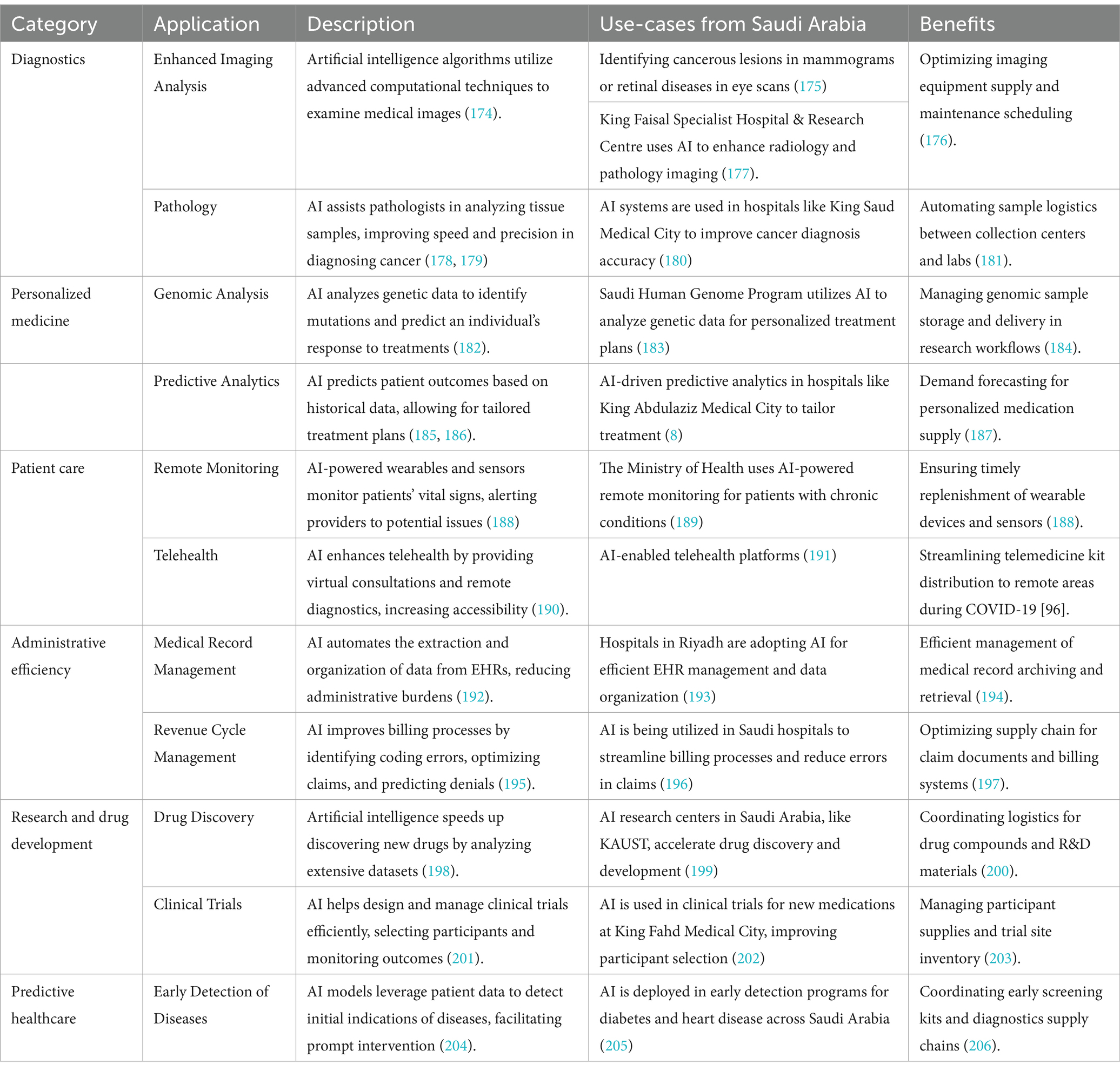
In Saudi Arabia, development of AI in public services is primarily driven by the Vision 2030 initiative (26). The key aim of Vision 2030 is to transform and develop the country toward a digitally empowered, diversified, self-reliant and sustainable economy (27). The application of AI in the government has helped in enhancing government services and key decision-making processes and efficiency in the allocation of the available resources (28). Recent strategic initiatives in Saudi Arabia, viz., Vision 2030, were inducted to achieve United Nation’s SDGs and to drive the AI adoption process in various public sectors (29). The National Strategy uses AI for economic growth, healthcare improvements, environmental sustainability, and better citizen services, aligning with Vision 2030 goals (30). These strategic goals aim to project Saudi Arabia as a global AI leader by 2030 while emphasizing data-driven approaches for governance and public services for the masses (31, 32). AI is increasingly adopted across Saudi Arabia’s PHS to enhance patients’ treatment, diagnostic methods, and hospital administration (30). Table 5 depicts various potential areas of AI applications in PHS.
2.2 Relevance of AI literacy for sustainable performance of public healthcare system
AI literacy becomes relevant for sustainable performance of public healthcare, especially with the adoption of AI technologies with the aim to optimize operations and sustain performance (33). AI literacy among stakeholders (including policymakers and supply chain managers) ensures responsible usage of AI (34). The recent advancement emphasized focusing on AI literacy to improve decision-making in supply chains. AI can enhance SC performance by predicting demand, optimizing inventory, and identifying bottlenecks, ultimately reducing costs and waste (35). In healthcare logistics, using deep reinforcement learning models substantially improved economic, environmental and social outcomes while selecting sustainable chain modes more efficiently than traditional methods (36). Additionally, AI literacy significantly mitigates data-driven risks, including algorithmic bias, privacy infringements, and poor data governance. Such issues are critical for AI-driven systems to align with patient-centric and ethical standards (37). In addition to data-driven decision-making, the role of AI literacy in catering to public health crisis activities, including improving resource distribution during emergencies by leveraging underlined technologies (38). Also, using digital AI literacy using predictive algorithms and big data analytics in the healthcare supply chain as its consumption reduces the error rate and enhances productivity (39, 40). Public healthcare systems use multiple literacy programs that aim at improving digital and health AI competencies, including familiarity with predictive algorithms and big data analytics, which are necessary to foster trust and smooth integration of AI in healthcare settings. Through AI adoption, public healthcare systems remain sustainable and adaptive to evolving challenges (41).
The growing need for AI literacy is also linked to the ability to interpret AI-driven insights accurately and act upon them (42). Therefore, embedding AI literacy as a critical skill among healthcare professionals and supply chain managers will be vital in driving sustainable performance in public healthcare systems (43). These developments underline the importance of continuous training and strategic frameworks to improve AI literacy, ensuring the long-term success of public healthcare systems (44). The significance of taking interests of all parties involved in organization’s activities is emphasized by stakeholder theory (45). In the context of public healthcare systems, AI literacy becomes critical for ensuring sustainable and effective collaboration among stakeholders such as health service providers, policymakers, suppliers, patients, and regulators (10).
(a) Healthcare providers as stakeholders: AI literacy among healthcare professionals ensures they can leverage AI-driven tools to enhance decision-making, streamline inventory management, and predict resource needs effectively. With better understanding, providers can work collaboratively to use AI for predictive diagnostics, patient data management, and optimizing logistics during emergencies, fostering sustainable healthcare delivery (46).
(b) Policymakers and regulators: Policymakers participation has a crucial role in creating frameworks that ensure the responsible use of AI. An AI-literate policymaker can promote transparency, data privacy, and address ethical concerns around AI-driven healthcare systems through a sustainable policy framework. AI literacy enables stakeholder alignment by bridging communication gaps between technical teams, regulators, and healthcare practitioners, ensuring AI solutions are both compliant and practical (47).
(c) Patients and the public: Patients, as indirect stakeholders, benefit from AI-driven supply chains through improved service delivery, faster diagnostics, and better resource availability. AI literacy among the public encourages trust in AI tools and ensures acceptance of innovations such as AI-powered telemedicine platforms or automated drug delivery systems (48).
(d) Suppliers and partners: AI-literate suppliers can optimize their processes by utilizing predictive analytics for inventory planning, reducing waste, and ensuring timely deliveries (49). AI literacy enhances cold chain management in the pharmaceutical sector, ensuring that temperature-sensitive products are delivered effectively and sustainably.
(e) Governance and collaboration among stakeholders: AI-driven governance mechanisms that align the interests of multiple stakeholders are critical for the sustainability of healthcare supply chains (50). AI literacy fosters collaborative efforts between public and private stakeholders to ensure efficient logistics management during public health emergencies (51). For example, understanding predictive algorithms and big data analytics allows stakeholders to collaborate effectively on disaster response logistics and resource allocation (52).
(f) Social and environmental impact: AI literacy helps healthcare stakeholders align their operations with broader sustainability goals by reducing carbon footprints through optimized transportation and supply chain routes (53). It enables organizations to adopt circular economic practices, ensuring waste management through effective resource utilization.
AI literacy within and among healthcare stakeholders strengthens sustainable performance by ensuring all parties can collaborate effectively. It mitigates algorithmic bias, poor data governance, and compliance risks. Furthermore, it helps align stakeholders’ interests toward better patient outcomes, resource optimization, and environmental sustainability, ensuring public health systems are resilient, adaptive, and equitable (54).
2.3 Rise of AI literacy
A surge in AI literacy facilitates the use of AI tools in PHS in Saudi Arabia (55). Beyond operational benefits, AI literacy aligns with the SDGs driving healthcare innovation and contributing to sustainable development in several ways (56). AI literacy empowers healthcare professionals and supply chain managers to utilize advanced AI tools effectively, enhancing healthcare supply chains across multiple dimensions (33). It enables predictive analytics, demand forecasting, and inventory management to prevent stockouts or overstocking, ensuring optimal resource utilization (57). Automated AI-driven systems reduce human errors and provide real-time monitoring, ensuring timely delivery of essential supplies, even to remote or underserved areas (58). Additionally, AI integrated with blockchain enhances transparency and traceability in tracking pharmaceuticals and vaccines, mitigating counterfeit risks and safeguarding patient safety (59). Furthermore, AI literacy promotes sustainable operations by minimizing waste, improving recycling, enabling energy-efficient logistics, driving cost-effectiveness and reducing the sector’s carbon footprint in alignment with broader sustainability goals (60). AI literacy aligns with multiple SDGs by enabling stakeholders to leverage AI for sustainable healthcare development (61). It supports SDG 3 (Good Health and Wellbeing) by optimizing the availability of essential medical supplies, enhancing healthcare outcomes, and ensuring effective responses to public health crises across Saudi Arabia (55). In line with SDG 9, AI literacy fosters innovation and resilient healthcare infrastructure, advancing the digital transformation goals of Vision 2030 (62). It also promotes SDG 12 by enhancing resource optimization, reducing waste, and encouraging sustainable use of pharmaceuticals and medical equipment (63). By creating high-skilled jobs in healthcare technology and logistics, AI literacy contributes to SDG 8, driving economic diversification and operational efficiency (64). Additionally, AI literacy advances SDG 17 by facilitating collaborations among technology providers, healthcare organizations, and government agencies, ensuring scalable AI solutions for local and global healthcare systems (65). There are some major challenges that need to be raised concerning the general concept and practice of AI literacy (35). Professionals must understand data privacy and security measures to safeguard sensitive health information, aligning AI use with regulatory frameworks and SDG privacy standards (66). Additionally, adapting AI systems to Saudi Arabia’s cultural context and regulatory environment requires literacy in both AI technology and local healthcare laws to ensure smooth integration into clinical workflows (67). AI literacy should also encompass knowledge of the environmental impact of AI systems, such as energy consumption, to align adoption with SDG 13, promoting a balance between innovation and sustainability (68). Development of AI literacy among healthcare professionals, supply chain managers, and policymakers enables Saudi Arabia to unlock the full potential of AI-powered public health systems, improving healthcare services while advancing the country’s contribution to the SDGs (12). Saudi Arabia’s Vision 2030 offers a strategic framework for the sustainable integration of AI solutions, ensuring healthcare transformation aligns with global development objectives (55). Emphasizing AI literacy ensures that these technologies drive more than just automation, promoting informed decision-making, sustainable consumption, and economic growth while safeguarding societal wellbeing and environmental sustainability (69). The rise of AI in Public Healthcare Systems in Saudi Arabia presents significant potential for advancing the country’s healthcare sector while contributing to Sustainable Development Goals (SDGs) (70). AI enhances the efficiency of operations through predictive analytics, demand forecasting, and inventory management. By predicting the demand for medical supplies and pharmaceuticals, AI helps avoid shortages or overstocking, optimizing resource utilization (48, 71). AI-powered automation reduces manual errors and enables real-time monitoring of supply chain processes. This ensures that critical supplies reach hospitals and healthcare centers promptly, particularly in remote or under-served areas (72). AI combined with blockchain technology to ensures transparency in the supply chain, particularly for pharmaceuticals and vaccines. This is critical in preventing counterfeit drugs and ensuring patient safety (72). AI helps minimize waste by analyzing data on consumption patterns, improving recycling, and implementing energy-efficient logistics. It contributes to lowering carbon footprints and healthcare costs (73).
AI literacy, use Artificial Intelligence for transforming healthcare supply chains in ways that align with sustainable development (74). Empowering healthcare professionals, policymakers, and supply chain managers with AI knowledge ensures that advanced tools are adopted strategically, enhancing healthcare systems, improving sustainability, and advancing the United Nations SDGs (75). AI literacy enables healthcare personnel to use AI enabled algorithms in demand forecasting for medical supplies, vaccines, and pharmaceuticals (76). Informed decisions based on AI insights ensure consistent availability of essential drugs and equipment, reducing stockouts and delays (48). With AI tools integrated into the supply chain, professionals can act faster and more effectively in public health crises, ensuring a high standard of care across the country (77). Understanding how AI can improve supply chain operations empowers healthcare leaders to adopt innovations like real-time tracking, predictive maintenance, and automated inventory systems (78). AI literacy enables organizations to optimize resource planning, leading to more resilient healthcare infrastructure (79). In alignment with Vision 2030, AI-literate professionals can spearhead digital transformation, positioning Saudi Arabia as a hub for healthcare infrastructure development (80). AI-literate supply chain managers can leverage machine learning models to minimize waste and promote responsible use of medical resources (81). By accurately forecasting demand and managing inventory, they avoid overstocking and the expiration of pharmaceuticals, reducing environmental impact. Increased awareness of AI tools also allows professionals to track and recycle equipment, fostering a circular economy in healthcare (82). Developing AI literacy creates pathways for new job roles in healthcare logistics, data analytics, and AI system management (83). As AI automates routine tasks, workers can transition to high-value roles, driving operational efficiency and economic growth (84). The expansion of AI-powered healthcare systems also offers opportunities for collaboration between industries, contributing to the diversification with Vision 2030 (85). AI literacy strengthens multi-stakeholder collaboration by enhancing the ability of healthcare providers, policymakers, and private-sector partners to deploy AI solutions. Informed stakeholders are more capable of fostering public-private partnerships and aligning AI-driven supply chains with national and global development priorities (86). Cross-border knowledge-sharing initiatives are also facilitated by AI literacy, promoting global healthcare advancements (87). By promoting AI literacy across the healthcare supply chain, Saudi Arabia enhances its capacity to achieve the SDGs through sustainable innovation. Trained professionals can effectively harness AI to address healthcare challenges, optimize supply chains, and foster collaboration among stakeholders (88). Vision 2030 provides the strategic direction for building a digitally literate workforce, integrating AI seamlessly into healthcare infrastructure, and promoting long-term sustainability (89). Ultimately, AI literacy ensures that technological advancements in healthcare supply chain management are implemented thoughtfully, fostering economic growth, improving wellbeing, and promoting responsible consumption and production (33).
2.4 AI literacy challenges in Saudi Arabia in comparison to other nations
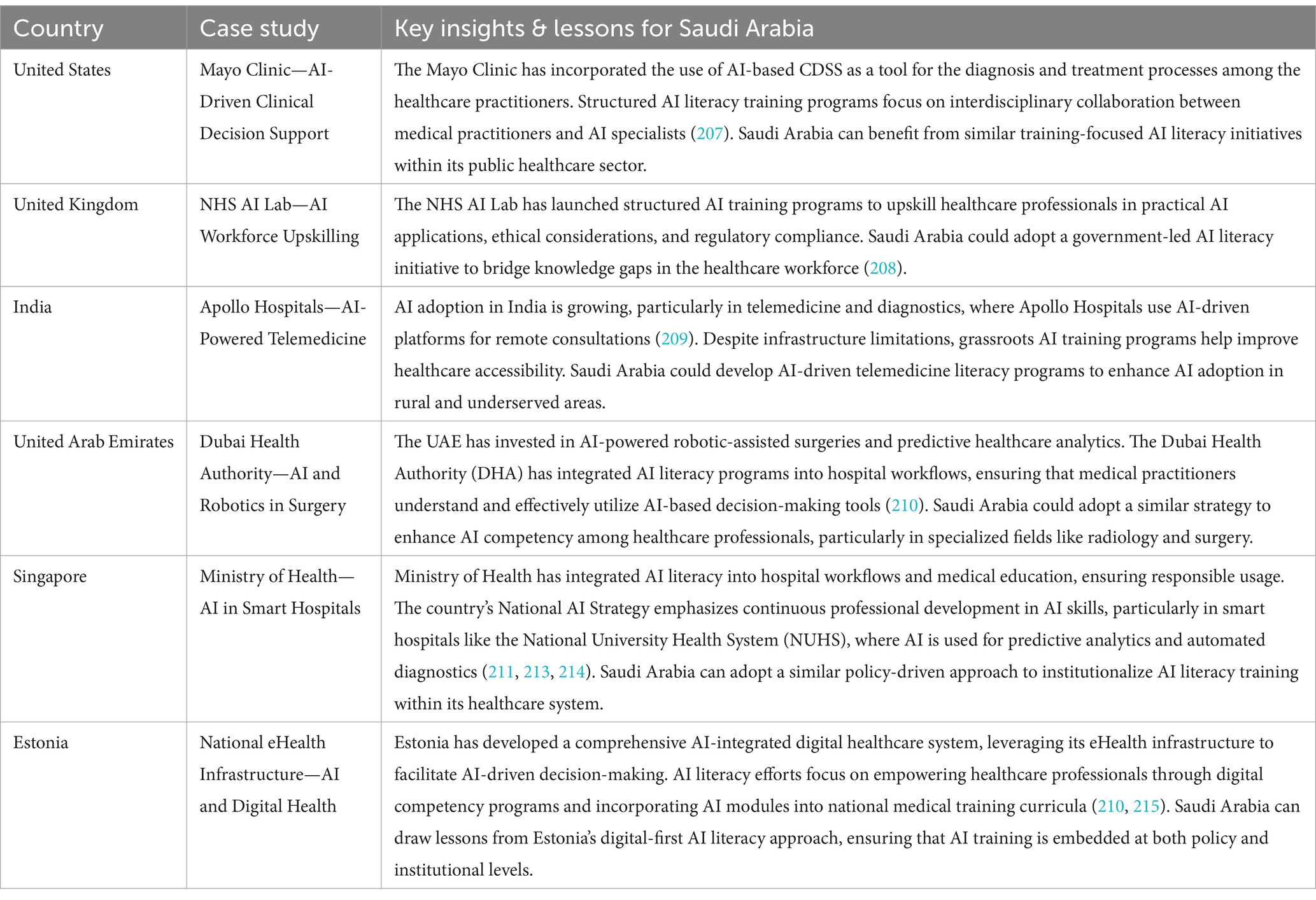
AI literacy adoption in public healthcare varies across nations due to differences in technological infrastructure, regulatory policies, and workforce preparedness. Saudi Arabia, under its Vision 2030 initiative, is making significant strides in AI integration, particularly in healthcare. However, challenges such as a shortage of AI-trained professionals, resistance to change, and concerns about ethical AI implementation persist. Table 6 explains a comparative analysis with other countries provides valuable insights into how these challenges manifest globally.
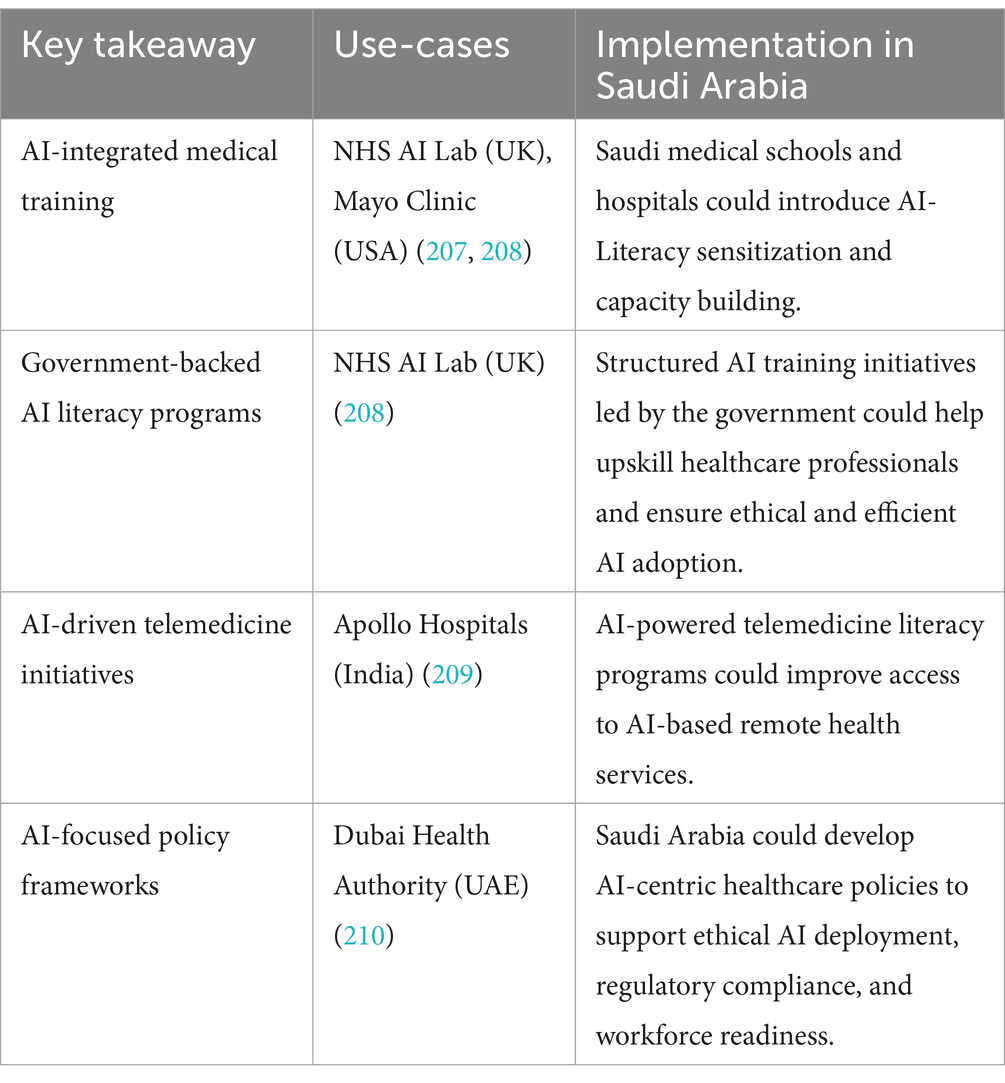
Table 7 explained various takeaways for Saudi Arabia.
2.5 Challenges to AI literacy in public healthcare systems
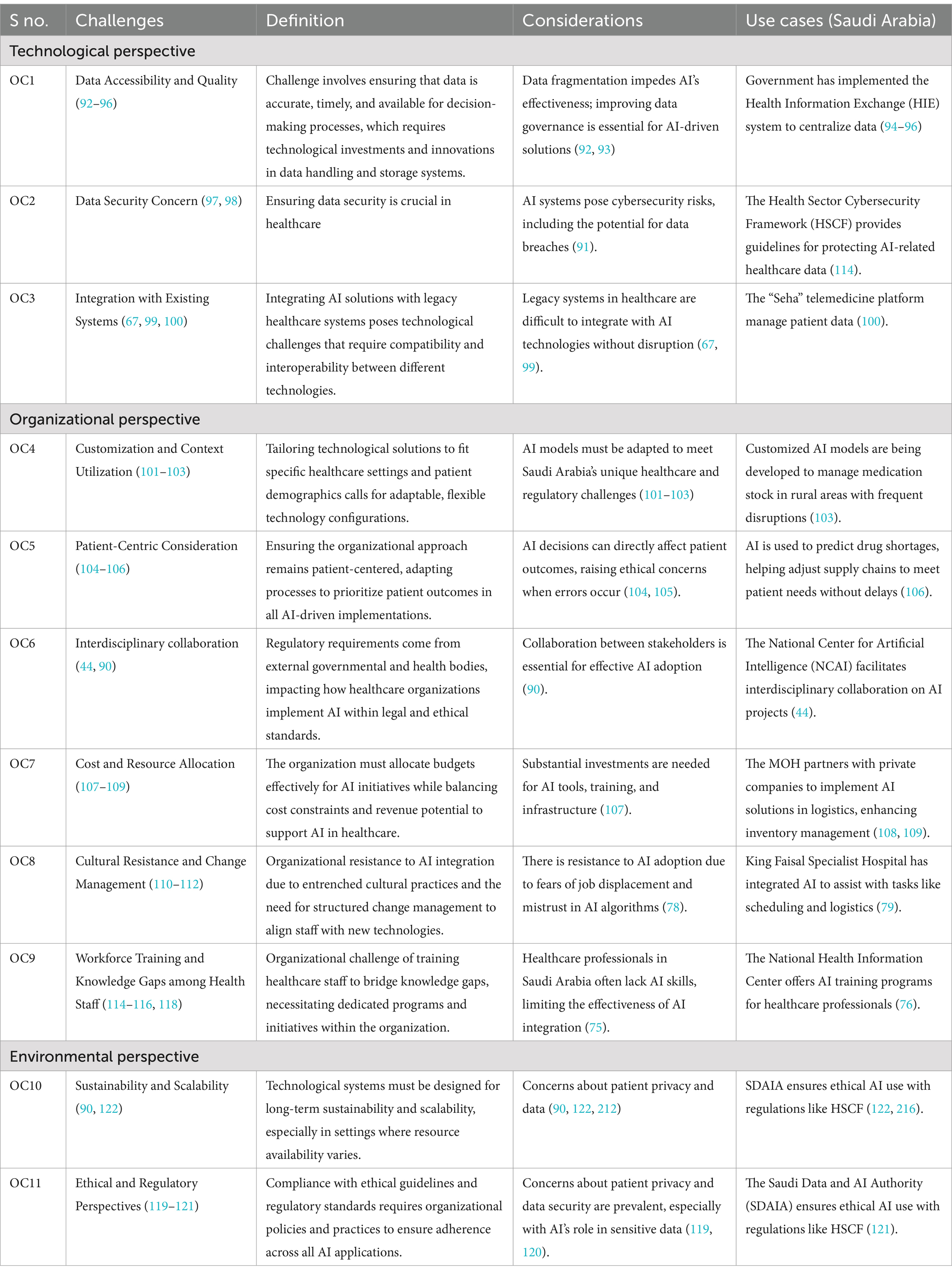
Building AI literacy in public healthcare systems, especially in Saudi Arabia, presents unique challenges and considerations due to the Saudi Arabia’s rapid adoption of AI as part of its Vision 2030 agenda (90). AI is being positioned as a tool to advance quality of healthcare services (91). Below are key challenges, considerations, and specific use cases from Saudi Arabia, supported by literature. Based on the literature, authors have identified various operational challenges (OC) in building AI literacy, which is the critical enabler for sustainable public health healthcare systems in developing countries, including Saudi Arabia.
OC1-Data accessibility and quality: AI systems in healthcare depend heavily on large datasets, yet data quality and accessibility remain challenges (92, 93). Public healthcare systems in Saudi Arabia still face issues with data fragmentation, impeding AI’s effectiveness (94). Improving data governance and ensuring data interoperability across various healthcare facilities will be key to unlocking AI’s potential (95). Saudi Arabia’s Ministry of Health (MOH) has introduced a Health Information Exchange (HIE) system aimed at centralizing patient data, improving data access and quality for AI-driven systems in supply chains (96).
OC2-Data security concern: As AI is adopted more widely in Saudi healthcare supply chains, there are growing concerns about data safety (97). AI literacy programs should include cybersecurity training that addresses specific threats related to AI systems. The public health systems include stringent guidelines for protecting healthcare data used by AI systems, ensuring that staff across the supply chain are aware of and follow cybersecurity best practices (98).
OC3-Integration with existing system: Public Healthcare in Saudi Arabia often rely on legacy systems that are difficult to integrate with modern AI technologies (67). AI literacy programs should focus on how to gradually integrate AI tools with these existing systems without causing disruption (99). Saudi Arabia’s digitization efforts under Vision 2030 include projects like the “Seha” telemedicine platform, which leverages AI to optimize patient data management, demonstrating how AI can be integrated into existing healthcare infrastructure (100).
OC4-Customization and context utilization: AI models developed in other regions may not fit Saudi Arabia’s specific healthcare challenges, especially in the context of its supply chains (101). Training programs should customize AI solutions that account for Saudi Arabia’s unique healthcare requirements and regulations (102). AI models are being customized for the Saudi healthcare system, especially in rural areas where supply chain disruptions are common. Customized AI systems predict and manage medication stock levels in these areas (103).
OC5-Patient-centric consideration: AI decisions in healthcare supply chains can have direct implications for patient outcomes, creating ethical concerns if AI systems make errors (104). AI literacy programs must emphasize patient-centered approaches, ensuring that healthcare workers understand how AI can improve patient care through efficient supply chain management (105). AI-driven systems in Saudi Arabia are being used to predict drug shortages and adjust supply chains, accordingly, ensuring that patients receive the medications they need without delay (106). The Table 8 consolidates the challenges, considerations, and specific use-cases from Saudi Arabia to provide a structured overview of building AI literacy in public health systems.
OC6-Interdiscplinary collaboration: AI literacy in Saudi Arabia’s healthcare sector requires not only technical knowledge but also collaboration between stakeholders (90). AI literacy efforts must promote interdisciplinary knowledge exchange between them to ensure sustainable health systems (44). The National Center for Artificial Intelligence (NCAI) fosters collaboration between healthcare institutions and AI companies, ensuring that supply chain innovations are driven by both medical expertise and AI technology (44).
OC7-Cost and resource allocation: AI implementation in Saudi Arabia’s public health systems requires substantial investments, especially for training, infrastructure, and AI tools (107). Government funding and public-private partnerships are essential to developing AI literacy and sustaining AI initiatives across the healthcare system (108). The MOH in Saudi Arabia has partnered with private tech companies to implement AI-based solutions in healthcare logistics, ensuring more efficient inventory management, while also training staff to utilize these tools (109).
OC8-Cultural resistance and change management: Resistance to AI adoption is common among healthcare professionals in Saudi Arabia, particularly due to concerns over job displacement and mistrust in AI algorithms (110). AI literacy programs need to emphasize AI’s role to assist public healthcare partners (111). In Saudi hospitals, AI is gradually being used to assist with repetitive tasks, such as scheduling and supply chain logistics (112). King Faisal Specialist Hospital and Research Centre has integrated AI-powered systems that automate administrative tasks, leading to cost reductions and improved efficiency (113).
OC9-Workforce training and knowledge gaps among health staff: Many healthcare professionals in Saudi Arabia lack the necessary AI skills (114). As AI becomes more integrated into healthcare supply chains, professionals must understand how AI models function and how they can be leveraged for tasks like inventory management and demand forecasting (115). Saudi Arabia has initiated training programs to enhance AI literacy among healthcare professionals as part of broader digital health strategies (116, 117). The Saudi Arabia has launched initiatives such as the National Health Information Center to provide training on AI applications in healthcare, emphasizing AI-based decision support systems for medical staff (118).
OC10-Ethical and regulatory perspectives: In Saudi Arabia, as in many countries, concerns arise about how AI impacts patient privacy, especially regarding sensitive health data (119). AI literacy must include training on compliance with Saudi-specific regulations, like the Health Sector Cybersecurity Framework (HSCF), which focuses on safeguarding patient data (120). The Saudi Data and AI Authority (SDAIA) plays a significant role in ensuring AI’s ethical use, setting guidelines that healthcare supply chains must follow to protect patient privacy and ensure transparency in decisions (121).
OC11-Sustainability and scalability: While pilot AI projects in Saudi healthcare have shown success, scaling them across the entire public health system remains a challenge (90). AI literacy programs must focus on scalability, helping professionals learn how to expand AI solutions from pilots to wider use cases (122).
3 Methodology
The research used a qualitative analysis employing the T-O-E framework to identify the adoption challenges of AI literacy.
The Technology-Organization-Environment (T-O-E) framework was chosen for this study as it provides a holistic perspective on AI literacy adoption in public healthcare by considering multiple influencing factors. Unlike individual-centric models such as the Technology Acceptance Model (TAM) (123) and the Unified Theory of Acceptance and Use of Technology (UTAUT) (124), which primarily focus on user perceptions and behavioral intent, the T-O-E framework captures broader institutional and contextual determinants. Drazin (125) emphasize that the T-O-E model effectively integrates technological capabilities, organizational structures, and environmental influences, making it particularly useful for studying technology adoption at the institutional level. Moreover, Baker (126) highlights that the framework is adaptable across various industries, including healthcare, due to its ability to incorporate external policy and regulatory constraints. Given that AI literacy adoption in public healthcare is shaped by multi-level barriers—including technological capabilities, organizational readiness, and external policy dynamics, the T-O-E framework provides a comprehensive analytical lens for this study.
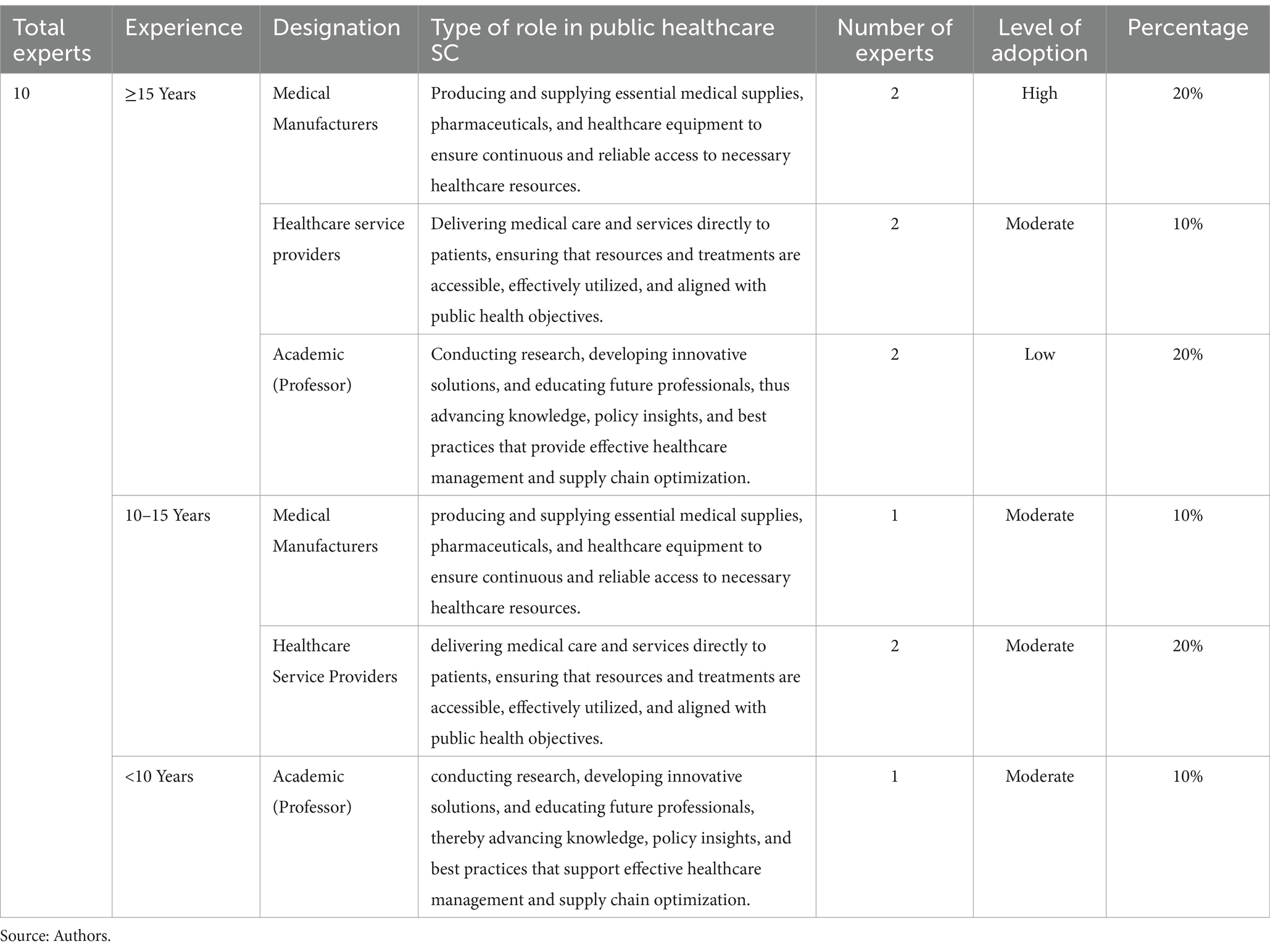
To ensure depth and relevance of data, the study strategically selected 10 experts from the healthcare sector based on strict inclusion and exclusion criteria. Experts were included if they held decision-making roles in healthcare and AI technologies, possessed at least 5 years of experience in healthcare technology integration, and worked directly in healthcare settings. Those primarily involved in unrelated IT services or administrative roles, or with less than 5 years in the field, were excluded. Authors have deployed Best-Worst Method (BWM) approach to identify the critical AI adoption challenges in public health systems. BWM is a multi-criterion decision making method that rates the options according to the ordinal ranking of criteria based on the relative importance of the criteria (127). Depending on the objectives and environments of decision makers, the most preferable and least desirable criteria are selected first, followed by the pairwise comparisons that are essential for obtaining the optimal weights which also guarantee the consistency of the judgments made. The BWM has been used widely in different fields for its reliability and validity in other related areas. In supply chain and logistics, BWM assists in the selection of a supplier by ranking necessary criteria such as cost and quality (128). In energy planning, BWM assesses potential resources by their environmental influence and effectiveness (129, 130). The healthcare sectors utilize BWM to allocate resources, and the urban planners have integrated it with the priority of smart city projects allocating supports decision-making in product development evaluation of environments, and risk evaluation because the system allows the organization to sort out factors such as customer preference, social issues or risk probability (131). Due to the accurate balance of weights assigned to criteria, BWM is an ideal tool for strategic decision-making (132). The Best Worst Method (BWM) involves a structured pairwise comparison process that typically requires fewer comparisons than the Analytic Hierarchy Process (AHP) (133). Firstly, it operates by identifying the most and least important criteria from a set, thus making it a focused comparison approach that reduces the cognitive load and potential bias compared to AHP. Secondly, by specifically comparing all criteria to these two reference points (best and worst), the method effectively minimizes anchoring bias, as it anchors the scale on identified extremes rather than arbitrary judgments. Thirdly, the results obtained from BWM are generally more consistent and reliable due to its systematic reduction of comparison complexity and clearer decision framework (134–136).
3.1 Calculation of the weight of challenges using BWM method
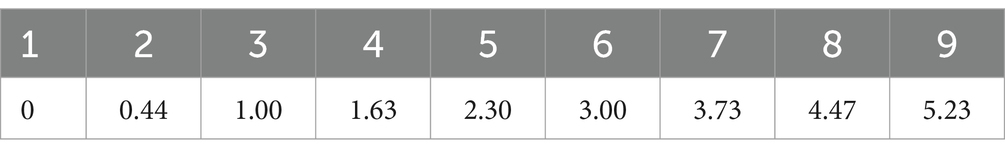
In this step, the relative importance of 11 problems were determined. The stars for each criterion were made through usage of a 1–9 point scale on pairwise comparisons. To derive the weights of criteria and sub-criteria, the BWM optimization model as suggested by Razaei (127). This strategy helps decision-makers in decision-making since the results obtained are so reliable. Annexure I discussed step involved in BWM Method. Table 9 displays the Consistency Index for Best-Worst Method models with varying criteria counts.
4 Results
The medical manufacturers, healthcare service providers, and academic (Professor) were the experts who participated in this study. Participants’ demographic details are given in Table 10.
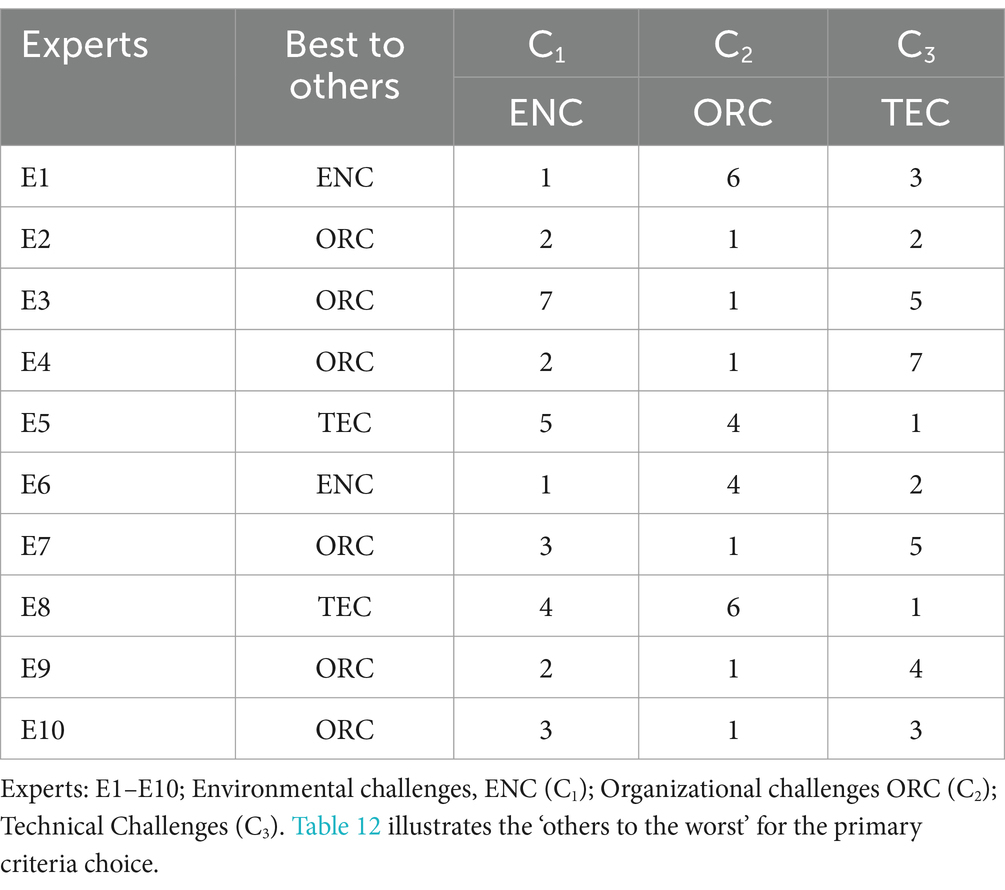
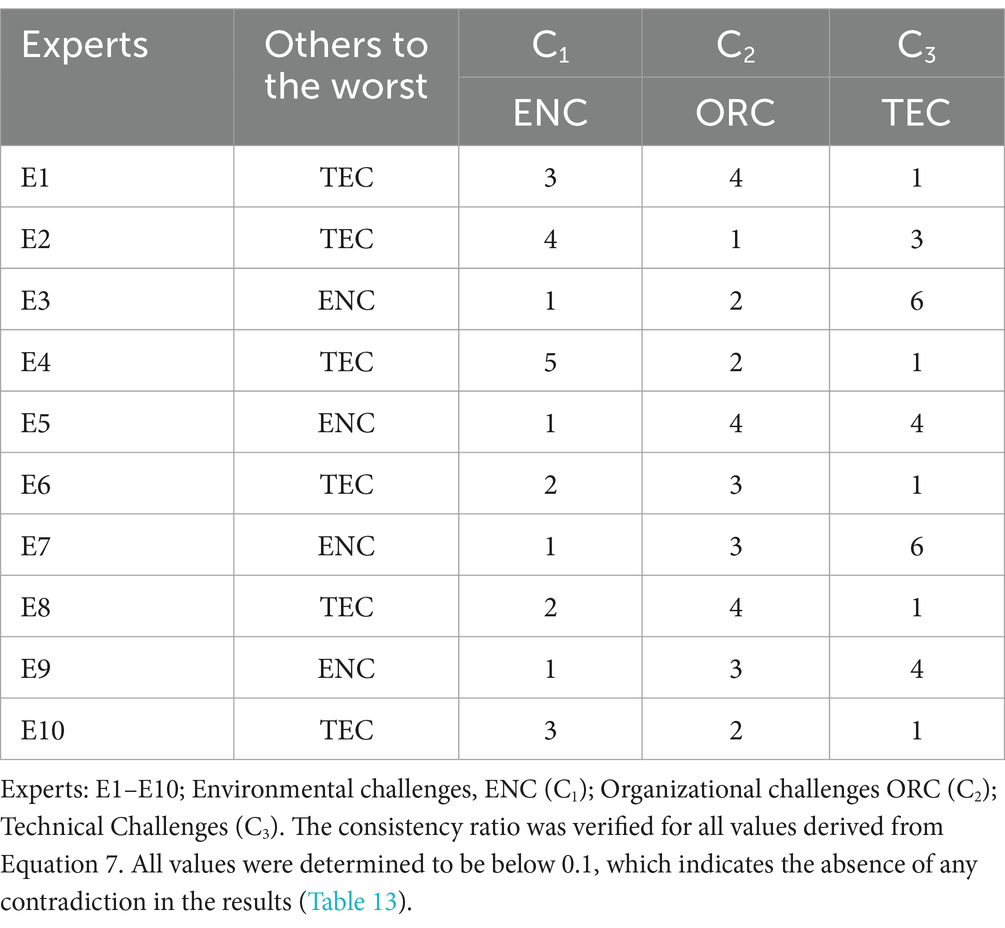
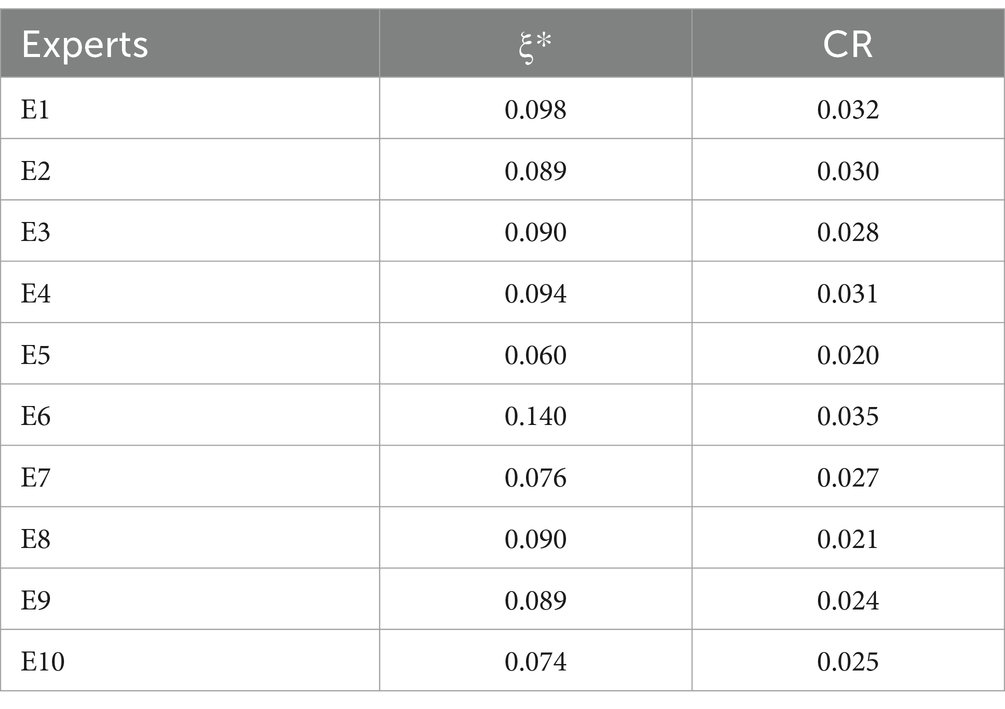
Tables 9, 10 show the best-to-others and worst-to-worst results, respectively. Weights and consistency rates are derived from a non-linear mathematical model of BWM, as presented in Tables 11, 12. Expert evaluations indicate that the BWM results demonstrate ‘C2’ as the most critical criterion. Experts E2, E3, E4, E7, E9, and E10 selected Criterion C2 as the ‘best to others’ criterion (Table 9) (Table 13).
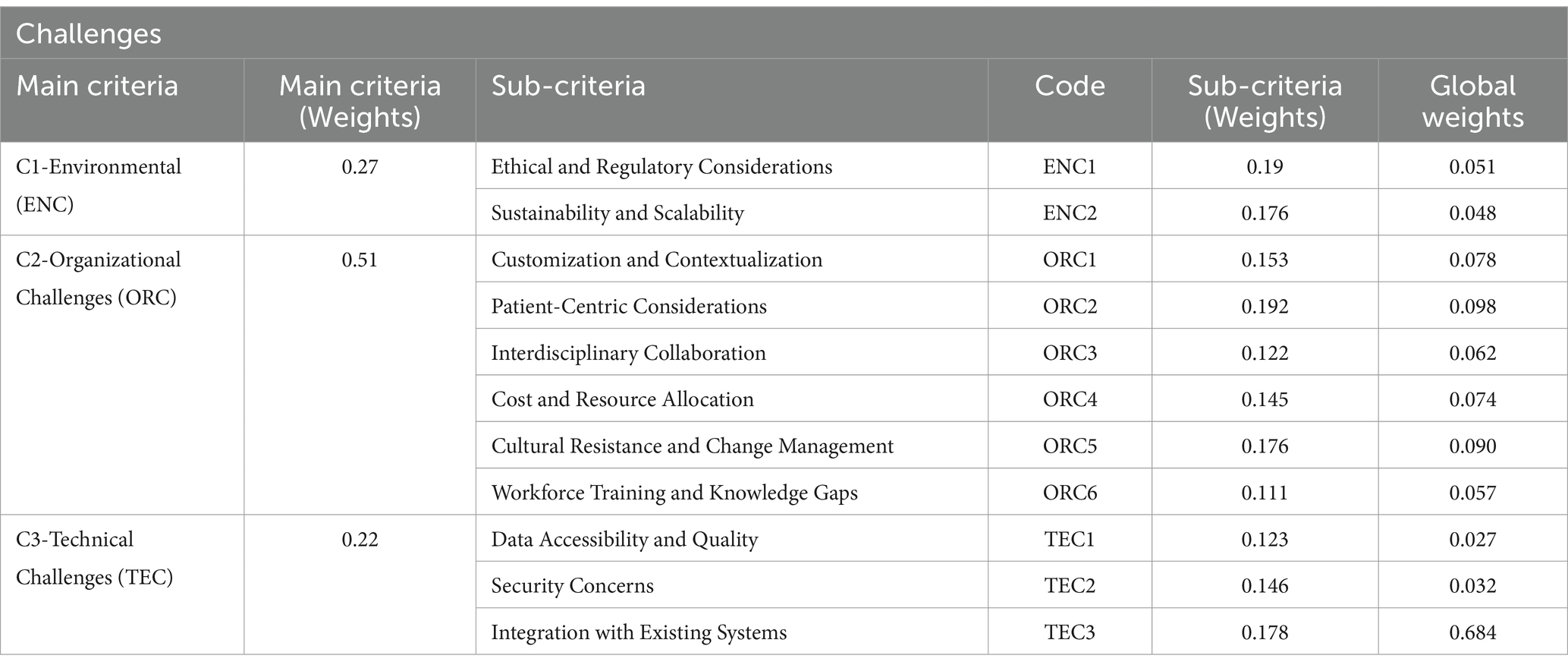
Likewise, the BWM solver was employed to calculate the weights for the sub-criteria. The global weights of the primary criteria were also computed. The ranking was conducted utilizing global weights and is shown in Table 14.
The weights for each criterion were calculated based on the average means of the values provided by the experts. The conclusive ‘Best to others’ and ‘others to the worst’ outcomes derived from the experts for primary criteria. The scores are displayed in Table 14.
The use of the Best-Worst Method (BWM) in this research outlines the main issues arising from the development of AI literacy to support sustainable public health supply chains in Saudi Arabia. The results revealed that the type of implementation challenges in the context of organizational perspective (ORC) has the highest weight of 0.51 as the main criteria. This points to the idea that implementation Challenges such as Customization and Contextualization, Patient Centered Considerations, Cultural Resistance and Change Management, Cost and resource allocation are paramount to achievement of AI literacy. These criteria reflect the concerns closely with the contextual aspects of leveraging different AI tools in the local environment, cultural adaptation, and patient-centeredness that are crucial for creating a more significant impact of AI in the sphere. The focus on organizational Challenges goes well with the context of scope and intricate environment in the Saudi healthcare sector where engagement of stakeholders and their acceptance is most important. The research results further reveal Environmental Challenges (ENC) with a threat weight of 0.27 as another implementation challenge. Ethical standards and Regularity norms, ensuring sustainability and scalability are important concerns to be considered during the transformation planning in healthcare ecosystem. With Saudi Arabia’s Vision 2030 emphasizing technological transformation, the economic burden of AI adoption necessitates careful allocation of resources and strategic investment, especially when scaling AI projects from pilot phases to broader implementation across healthcare institutions. Technical Challenges (TEC), accounting for a weight of 0.22, emphasize the importance of Data Accessibility and Quality, Security Concerns, and Integration with Existing Systems. As AI in healthcare relies on vast and often sensitive datasets, ensuring data accessibility and quality is crucial. Moreover, the integration of AI with existing legacy systems is challenging yet essential to maximize the effectiveness of AI tools without disrupting current workflows. These technical issues, if unaddressed, could hinder the scalability and efficacy of AI-driven supply chain solutions. In addition to identifying these main challenges, the study also highlights sub-criteria with high global weights, such as Patient-Centric Considerations (0.098) and Cultural Resistance and Change Management (0.090) within the organizational challenges. These findings reinforce the importance of prioritizing stakeholder buy-in and cultural adaptability in AI literacy programs. Addressing these factors is critical for fostering trust and acceptance among healthcare professionals, patients, and other stakeholders. The consistency ratio (CR) analysis confirmed the reliability of expert judgments, with all CR values below the acceptable threshold of 0.1. This indicates a high level of agreement among experts regarding the significance of these criteria, validating the robustness of the BWM model in assessing AI literacy challenges within Saudi Arabia’s healthcare sector. Overall, the research study emphasizes the multifaceted nature of building AI literacy, involving organizational, environmental, and technical dimensions. Effective strategies must address each of these areas to foster sustainable PHSC that align with Saudi Arabia’s Vision 2030 objectives and broader Sustainable Development Goals. This research contributes to strategic and practical considerations needed to support AI integration in healthcare, laying the groundwork for further studies and the development of targeted AI literacy programs.
5 Conclusion and future research directions
5.1 Conclusion
The strategic roadmap for AI implementation in PHS, based on the TOE framework, provides a comprehensive approach to fostering a resilient and sustainable healthcare ecosystem in alignment with Saudi Vision 2030 and SDGs. By addressing organizational, environmental, and technical dimensions, this framework outlines essential actions to overcome the critical barriers to AI adoption. Organizational strategies emphasize cultural adaptation, stakeholder engagement, and literacy development; economic strategies focus on resource allocation, public-private partnerships, and scalable pilot projects; and technical strategies highlight data governance, interoperability, and cybersecurity. Collectively, these elements lay the foundation for a robust, inclusive, and sustainable healthcare AI infrastructure that supports national and global health objectives.
5.2 Limitations
Besides the strengths of this research framework, the study has several limitations. First, the study’s focus on Saudi Arabia limits the direct applicability of findings to other contexts with different cultural, regulatory, and healthcare environments. Second, while the TOE framework provides a structured approach, the complex and evolving nature of AI technology means that some aspects, especially regulatory compliance and cybersecurity, may require continuous updates. Additionally, the study relies on existing data and stakeholder insights, which may not fully capture the dynamic challenges and emerging technologies that could influence future AI adoption in healthcare.
5.3 Areas for future research
Future research should explore longitudinal studies to assess the long-term impacts of AI implementation within Saudi Arabia’s healthcare system, especially concerning patient outcomes and healthcare provider efficiency. Comparative studies between different regions and countries could offer further insights into how the TOE framework might be adapted to diverse contexts. Moreover, further research could investigate specific technical challenges such as data privacy, algorithmic transparency, and the integration of AI with emerging technologies like blockchain and the Internet of Medical Things (IoMT). Additional studies on the socio-cultural impacts of AI in healthcare focusing on ethical considerations, patient perceptions, and workforce adaptation would enrich our understanding of sustainable AI adoption in Saudi Arabia and beyond.
Table 15 discussed Future research on AI literacy adoption in public healthcare can explore several key areas:
Regulatory compliance and governance are essential to ensuring adherence to data protection for safeguarding patient data while promoting ethical AI deployment. Future research should explore strategies for effective deployment in clinical settings and enhance regulatory frameworks that balance innovation with privacy concerns. Public-private collaboration is also crucial in shaping AI ethics, with studies needed to examine how cooperation between policymakers, healthcare providers, and AI developers can establish standardized governance frameworks for ethical AI deployment. Past studies including, Dwivedi et al. (137) highlight institutional barriers to AI adoption and advocates for a multi-stakeholder approach to AI literacy, while Morley et al. (104) stresses the significance of interdisciplinary AI training to mitigate ethical risks in AI-driven healthcare. Reddy et al. (138) examine AI literacy gaps among clinicians and propose structured AI education programs to bridge these deficiencies. Future research should expand upon these perspectives, exploring region-specific AI literacy initiatives that address the unique challenges of healthcare systems while ensuring alignment with global best practices. By integrating these insights, future studies can contribute to a more comprehensive understanding of AI literacy, ethics, and governance, ultimately fostering responsible AI adoption in healthcare.
5.4 Strategic framework
For implementing AI in Saudi Arabia’s public healthcare systems, a strategic roadmap grounded in the TOE (Technology-Organization-Environment) framework is recommended. This roadmap promotes an inclusive and sustainable environment consistent with Saudi Vision 2030 and the Sustainable Development Goals (SDGs). The framework is designed to foster a resilient, inclusive, and sustainable ecosystem by addressing technological, organizational, and environmental aspects, thus overcoming key barriers identified in the study. These strategic pillars, Organizational Strategy, Environmental Strategy, and Technical Strategy, target the essential enablers and barriers to AI adoption, as illustrated in Figure 2. The strategic AI adoption leads to Sustainable performance of public healthcare systems.
The technical dimension addresses the need for robust data governance frameworks to ensure compliance with local regulations, facilitate secure data sharing, and maintain interoperability across healthcare entities. This approach supports SDG 9 by fostering innovation and infrastructure resilience. Enhanced cybersecurity and phased integration with existing systems are crucial to secure sensitive data, promoting sustainable and resilient healthcare aligned with the SDGs. From an organizational perspective, AI solutions should be adapted to Saudi Arabia’s healthcare structure and cultural context.
This involves co-designing AI tools with input from patients and healthcare providers to enhance care delivery, aligning with SDG 3 on health and wellbeing. The strategy includes comprehensive training to build AI literacy among healthcare professionals, along with stakeholder engagement through workshops and awareness initiatives to mitigate cultural resistance and ensure sustainable adoption. In terms of the economic dimension, resource allocation and partnerships with local and international technology firms, along with Public-Private Partnerships (PPPs), are vital. These partnerships provide the financial and technical support needed to scale AI adoption sustainably. By supporting pilot projects and phased expansions, these initiatives align with SDG 17, emphasizing partnerships for sustainable development. Through the TOE framework, this roadmap provides actionable strategies that uphold Saudi Arabia’s goals for a technologically advanced, sustainable healthcare ecosystem, contributing meaningfully to the nation’s broader Vision 2030 and SDG commitments.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
Ethics statement
The studies involving humans were approved by Research Ethics Committee (REC), University of Hail (Permission number: H-2024-351). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
RK: Writing – original draft, Writing – review & editing, Conceptualization, Formal analysis, Funding acquisition, Methodology, Project administration, Software, Supervision. AS: Conceptualization, Data curation, Methodology, Validation, Writing – original draft, Writing – review & editing. AK: Data curation, Investigation, Project administration, Resources, Validation, Writing – review & editing, Writing – original draft. MH: Data curation, Investigation, Project administration, Resources, Validation, Writing – review & editing, Writing – original draft. SJ: Data curation, Formal analysis, Investigation, Resources, Software, Writing – original draft, Writing – review & editing. MS: Data curation, Investigation, Resources, Software, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research has been funded by Scientific Research Deanship at University of Ha’il—Saudi Arabia through project number—RG-23 251.
Acknowledgments
The authors would like to thank all the participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bekbolatova, M, Mayer, J, Ong, CW, and Toma, M. Transformative potential of AI in healthcare: definitions, applications, and navigating the ethical landscape and public perspectives. Healthcare. (2024) 12:125. doi: 10.3390/healthcare12020125
2. Rahman, R, and Al-Borie, HM. Strengthening the Saudi Arabian healthcare system: role of vision 2030. Int J Healthc Manag. (2021) 14:1483–91. doi: 10.1080/20479700.2020.1788334
3. Almutairi, AM, Salonitis, K, and Al-Ashaab, A. A framework for implementing lean principles in the supply chain management at health-care organizations: Saudi’s perspective. Int J Lean Six Sigma. (2020) 11:463–92. doi: 10.1108/IJLSS-01-2019-0002
4. Ng, DTK, Leung, JKL, Chu, SKW, and Qiao, MS. Conceptualizing AI literacy: an exploratory review. Comput Educ Artif Intell. (2021) 2:100041. doi: 10.1016/j.caeai.2021.100041
5. Chew, HSJ, and Achananuparp, P. Perceptions and needs of artificial intelligence in health care to increase adoption: scoping review. J Med Internet Res. (2022) 24:e32939. doi: 10.2196/32939
6. Xiao, C, Choi, E, and Sun, J. Opportunities and challenges in developing deep learning models using electronic health records data: a systematic review. J Am Med Inform Assoc. (2018) 25:1419–28. doi: 10.1093/jamia/ocy068
7. Kumar, S, and Singh, M. Big data analytics for healthcare industry: impact, applications, and tools. Big Data Mining Anal. (2018) 2:48–57. doi: 10.26599/BDMA.2018.9020031
8. Alowais, SA, Alghamdi, SS, Alsuhebany, N, Alqahtani, T, Alshaya, AI, Almohareb, SN, et al. Revolutionizing healthcare: the role of artificial intelligence in clinical practice. BMC Med Educ. (2023) 23:689. doi: 10.1186/s12909-023-04698-z
9. Saha, E, and Rathore, P. The impact of healthcare 4.0 technologies on healthcare supply chain performance: extending the organizational information processing theory. Technol Forecast Soc Chang. (2024) 201:123256. doi: 10.1016/j.techfore.2024.123256
10. Esmaeilzadeh, P. Challenges and strategies for wide-scale artificial intelligence (AI) deployment in healthcare practices: a perspective for healthcare organizations. Artif Intell Med. (2024) 151:102861. doi: 10.1016/j.artmed.2024.102861
11. Mehta, N, Pandit, A, and Shukla, S. Transforming healthcare with big data analytics and artificial intelligence: a systematic mapping study. J Biomed Inform. (2019) 100:103311. doi: 10.1016/j.jbi.2019.103311
12. Kimiafar, K, Sarbaz, M, Tabatabaei, SM, Ghaddaripouri, K, Mousavi, AS, Mehneh, MR, et al. Artificial intelligence literacy among healthcare professionals and students: a systematic review. Front Health Inf. (2023) 12:168. doi: 10.30699/fhi.v12i0.524
13. Umer, M, Naveed, A, Maryam, Q, Malik, AR, Bashir, N, and Kandel, K. Investigating awareness of artificial intelligence in healthcare among medical students and professionals in Pakistan: a cross-sectional study. Ann Med Surg. (2024) 86:2606–11. doi: 10.1097/MS9.0000000000001957
14. Endalamaw, A, Zewdie, A, Wolka, E, and Assefa, Y. A scoping review of digital health technologies in multimorbidity management: mechanisms, outcomes, challenges, and strategies. BMC Health Serv Res. (2025) 25:382. doi: 10.1186/s12913-025-12548-5
15. Shiri, A. Artificial intelligence literacy: a proposed faceted taxonomy. Digit Libr Perspect. (2024) 40:681–99. doi: 10.1108/DLP-04-2024-0067
16. Adeniran, IA, Efunniyi, CP, Osundare, OS, and Abhulimen, AO. Data-driven decision-making in healthcare: improving patient outcomes through predictive modeling. Eng Sci Technol J. (2024) 5:059–67. doi: 10.56781/ijsrms.2024.5.1.0040
17. Wagner, DN. Economic AI literacy: a source of competitive advantage In: Handbook of research on applied AI for international business and marketing applications. Hershey, Pennsylvania, USA: IGI Global (2021). 135–52.
18. Al-Raeei, M. The smart future for sustainable development: artificial intelligence solutions for sustainable urbanization. Sustain Dev. (2024) 33:508–17. doi: 10.1002/sd.3131
19. Raji, MA, Olodo, HB, Oke, TT, Addy, WA, Ofodile, OC, and Oyewole, AT. E-commerce and consumer behavior: a review of AI-powered personalization and market trends. GSC Adv Res Rev. (2024) 18:066–77. doi: 10.30574/gscarr.2024.18.3.0090
20. Igwe, A. N., Eyo-Udo, N. L., and Stephen, A. Technological innovations and their role in enhancing sustainability in food and FMCG supply chains. Int J Eng Inventions (2024) 13:176–88.
21. Mutambik, I. The use of AI-driven automation to enhance student learning experiences in the KSA: an alternative pathway to sustainable education. Sustain For. (2024) 16:5970. doi: 10.3390/su16145970
22. Srivastava, N, Verma, S, Singh, A, Shukla, P, Singh, Y, Oza, AD, et al. Advances in artificial intelligence-based technologies for increasing the quality of medical products. DARU J Pharm Sci. (2025) 33:1–21. doi: 10.1007/s40199-024-00548-5
23. Henman, P. Improving public services using artificial intelligence: possibilities, pitfalls, governance. Asia Pacific J Public Admin. (2020) 42:209–21. doi: 10.1080/23276665.2020.1816188
24. Madan, R, and Ashok, M. AI adoption and diffusion in public administration: a systematic literature review and future research agenda. Gov Inf Q. (2023) 40:101774. doi: 10.1016/j.giq.2022.101774
25. Nahar, S. Modeling the effects of artificial intelligence (AI)-based innovation on sustainable development goals (SDGs): applying a system dynamics perspective in a cross-country setting. Technol Forecast Soc Chang. (2024) 201:123203. doi: 10.1016/j.techfore.2023.123203
26. AlGosaibi, AA, Sait, ARW, AlOthman, AF, and AlHamed, S. Developing an intelligent framework for improving the quality of service in the government organizations in the Kingdom of Saudi Arabia. Int J Adv Comput Sci Appl. (2020) 11:260–68. doi: 10.14569/IJACSA.2020.0111233
27. Kjaer, AL. Major trends to 2030+ In: The trend management toolkit: a practical guide to the future. London: Palgrave Macmillan UK (2014). 116–56.
28. Caiza, G, Sanguña, V, Tusa, N, Masaquiza, V, Ortiz, A, and Garcia, MV. Navigating governmental choices: a comprehensive review of artificial Intelligence’s impact on decision-making. Informatics. (2024) 11:64. doi: 10.3390/informatics11030064
29. Bedamatta, R, Laishram, B, and Johari, S. Research and innovation for sustainable development goals Springer (2024) 210.
30. Bendary, MG, and Rajadurai, J. Emerging technologies and public innovation in the Saudi public sector: an analysis of adoption and challenges amidst vision 2030. Innov J. (2024) 29:1–42.
31. Abedalrhman, K., and Alzaydi, A. Saudi Arabia's strategic leap towards a diversified economy and technological innovation. (2024). doi: 10.2139/ssrn.5048258
32. Al-Hajri, A, Abdella, GM, Al-Yafei, H, Aseel, S, and Hamouda, AM. A systematic literature review of the digital transformation in the Arabian Gulf’s oil and gas sector. Sustain For. (2024) 16:6601. doi: 10.3390/su16156601
33. Damoah, IS, Ayakwah, A, and Tingbani, I. Artificial intelligence (AI)-enhanced medical drones in the healthcare supply chain (HSC) for sustainability development: a case study. J Clean Prod. (2021) 328:129598. doi: 10.1016/j.jclepro.2021.129598
34. Miao, F, Holmes, W, Huang, R, and Zhang, H. AI and education: a guidance for policymakers. Paris, France: Unesco Publishing (2021).
35. Dwivedi, YK, Hughes, L, Ismagilova, E, Aarts, G, Coombs, C, Crick, T, et al. Artificial intelligence (AI): multidisciplinary perspectives on emerging challenges, opportunities, and agenda for research, practice and policy. Int J Inf Manag. (2021) 57:101994. doi: 10.1016/j.ijinfomgt.2019.08.002
36. Chen, W, Men, Y, Fuster, N, Osorio, C, and Juan, AA. Artificial intelligence in logistics optimization with sustainable criteria: a review. Sustain For. (2024) 16:9145. doi: 10.3390/su16219145
37. Williamson, SM, and Prybutok, V. Balancing privacy and progress: a review of privacy challenges, systemic oversight, and patient perceptions in AI-driven healthcare. Appl Sci. (2024) 14:675. doi: 10.3390/app14020675
38. Schmarzo, B. AI & data literacy: empowering citizens of data science. Birmingham, UK: Packt Publishing Ltd. (2023).
39. Avinash, B, and Joseph, G. Reimagining healthcare supply chains: a systematic review on digital transformation with specific focus on efficiency, transparency and responsiveness. J Health Organ Manag. (2024) 38:1255–79. doi: 10.1108/JHOM-03-2024-0076
40. Khoa, BQ, Nguyen, HT, Anh, DBH, and Ngoc, NM. Impact of artificial intelligence's part in supply chain planning and decision making optimization. Int J Multidis Res Growth Eval. (2024) 5:837–56. doi: 10.54660/.IJMRGE.2024.5.6.837-856
41. Paasche-Orlow, MK, Schillinger, D, Greene, SM, and Wagner, EH. How health care systems can begin to address the challenge of limited literacy. J Gen Intern Med. (2006) 21:884–7. doi: 10.1111/j.1525-1497.2006.00544.x
42. Celik, I. Exploring the determinants of artificial intelligence (Ai) literacy: digital divide, computational thinking, cognitive absorption. Telematics Inform. (2023) 83:102026. doi: 10.1016/j.tele.2023.102026
43. Pesqueira, A, Sousa, MJ, and Rocha, Á. Big data skills sustainable development in healthcare and pharmaceuticals. J Med Syst. (2020) 44:197. doi: 10.1007/s10916-020-01665-9
44. Abulibdeh, A, Zaidan, E, and Abulibdeh, R. Navigating the confluence of artificial intelligence and education for sustainable development in the era of industry 4.0: challenges, opportunities, and ethical dimensions. J Clean Prod. (2024) 437:140527. doi: 10.1016/j.jclepro.2023.140527
45. Jensen, MC. Value maximization, stakeholder theory, and the corporate objective function. J Appl Corp Financ. (2010) 22:32–42. doi: 10.1111/j.1745-6622.2010.00259.x
46. Adegboye, M. Impact of artificial intelligence on health information literacy: guidance for healthcare professionals. Library Hi Tech News. (2024) 41:1–5. doi: 10.1108/LHTN-03-2024-0048
47. de Almeida, PGR, dos Santos, CD, and Farias, JS. Artificial intelligence regulation: a framework for governance. Ethics Inf Technol. (2021) 23:505–25. doi: 10.1007/s10676-021-09593-z
48. Ugwu, OI, Clarksville, TN, Hassan, OF, Clarksville, TN, Sanusi, MA, Odukoya, O, et al. Artificial intelligence in healthcare supply chains: enhancing resilience and reducing waste. Int J Adv Res Ideas Innov Technol. (2024) 10:203–17.
49. Menzies, J, Sabert, B, Hassan, R, and Mensah, PK. Artificial intelligence for international business: its use, challenges, and suggestions for future research and practice. Thunderbird Int Bus Rev. (2024) 66:185–200. doi: 10.1002/tie.22370
50. Hao, X, and Demir, E. Artificial intelligence in supply chain decision-making: an environmental, social, and governance triggering and technological inhibiting protocol. J Model Manag. (2024) 19:605–29. doi: 10.1108/JM2-01-2023-0009
51. Khorram-Manesh, A, Goniewicz, K, and Burkle, FMJr. Unleashing the global potential of public health: a framework for future pandemic response. J Infect Public Health. (2024) 17:82–95. doi: 10.1016/j.jiph.2023.10.038
52. Papadopoulos, T, Gunasekaran, A, Dubey, R, Altay, N, Childe, SJ, and Fosso-Wamba, S. The role of big data in explaining disaster resilience in supply chains for sustainability. J Clean Prod. (2017) 142:1108–18. doi: 10.1016/j.jclepro.2016.03.059
53. Olawade, DB, Wada, OZ, David-Olawade, AC, Fapohunda, O, Ige, AO, and Ling, J. Artificial intelligence potential for net zero sustainability: current evidence and prospects. Next Sustainability. (2024) 4:100041. doi: 10.1016/j.nxsust.2024.100041
54. Zhang, J, and Zhang, ZM. Ethics and governance of trustworthy medical artificial intelligence. BMC Med Inform Decis Mak. (2023) 23:7. doi: 10.1186/s12911-023-02103-9
55. Mani, ZA, and Goniewicz, K. Transforming healthcare in Saudi Arabia: a comprehensive evaluation of vision 2030’s impact. Sustain For. (2024) 16:3277. doi: 10.3390/su16083277
56. Adel, A, and Alani, NH. Human-centric collaboration and industry 5.0 framework in smart cities and communities: fostering sustainable development goals 3, 4, 9, and 11 in society 5.0. Smart. Cities. (2024) 7:1723–75. doi: 10.3390/smartcities7040068
57. Mitta, NR. Leveraging AI for smart inventory management in retail: developing machine learning models for predictive replenishment, stock optimization, and demand-supply balancing. Austral J Mach Learn Res Appl. (2024) 4:113–46.
58. Kudrenko, I. Navigating the future: AI-driven healthcare supply chains In: Hospital supply chain: challenges and opportunities for improving healthcare. Springer Nature Switzerland: Cham (2024). 553–70.
59. Das, SR, Jhanjhi, NZ, Asirvatham, D, Rizwan, F, and Javed, D. Securing AI-based healthcare systems using blockchain technology In: AI techniques for securing medical and business practices. Hershey, Pennsylvania, USA: IGI Global (2025). 333–56.
60. Bhatia, M, Meenakshi, N, Kaur, P, and Dhir, A. Digital technologies and carbon neutrality goals: an in-depth investigation of drivers, barriers, and risk mitigation strategies. J Clean Prod. (2024) 451:141946. doi: 10.1016/j.jclepro.2024.141946
61. Koebe, P. How digital technologies and AI contribute to achieving the health-related SDGs. Int J Inf Manag Data Insights. (2025) 5:100298. doi: 10.1016/j.jjimei.2024.100298
62. Kasinathan, P, Pugazhendhi, R, Elavarasan, RM, Ramachandaramurthy, VK, Ramanathan, V, Subramanian, S, et al. Realization of sustainable development goals with disruptive technologies by integrating industry 5.0, society 5.0, smart cities and villages. Sustain For. (2022) 14:15258. doi: 10.3390/su142215258
63. Yadav, M, Agashe, P, Dhanshetti, P, and Pargoankar, P. Towards sustainable pharma: assessing contribution to sustainable development goals (Sdgs) of leading companies. Educ Admin Theory Pract. (2024) 30:2315–20. doi: 10.61093/sec.8(2).273-286.2024
64. Koh, JM. Cooperative firms and the sustainable development goals: pursuing decent work and reducing inequality. Oxfordshire, UK: Taylor & Francis (2023).
65. Baig, M. A. A., Huang, J., and Xu, J. AI for United Nations sustainable development goals: AI for UNSDGs. (2024).
66. Layode, O, Naiho, HNN, Adeleke, GS, Udeh, EO, and Labake, TT. Data privacy and security challenges in environmental research: approaches to safeguarding sensitive information. Int J Appl Res Soc Sci. (2024) 6:1193–214. doi: 10.51594/ijarss.v6i6.1210
67. Uraif, A. Developing healthcare infrastructure in Saudi Arabia using smart technologies: challenges and opportunities. Commun Netw. (2024) 16:51–73. doi: 10.4236/cn.2024.163003
68. Lainjo, B. The role of artificial intelligence in achieving the United Nations sustainable development goals. J Sustain Dev. (2024) 17:30. doi: 10.5539/jsd.v17n5p30
69. Kulkov, I, Kulkova, J, Rohrbeck, R, Menvielle, L, Kaartemo, V, and Makkonen, H. Artificial intelligence-driven sustainable development: examining organizational, technical, and processing approaches to achieving global goals. Sustain Dev. (2024) 32:2253–67. doi: 10.1002/sd.2773
70. Alsari, SM, Alzamanan, MMM, Salem, HA, Almutyif, QH, Al-Masad, AMS, Alabbas, MS, et al. The impact of vision 2030 on the healthcare system in Saudi Arabia. J Int Crisis Risk Commun Res. (2024) 7:2262–79. doi: 10.63278/jicrcr.vi.1393
71. Kumar, P, Choubey, D, Amosu, OR, and Ogunsuji, YM. AI-enhanced inventory and demand forecasting: using AI to optimize inventory management and predict customer demand. World J Adv Res Rev. (2024) 23:1931–44.
72. Haji, M, Kerbache, L, Sheriff, KM, and Al-Ansari, T. Critical success factors and traceability technologies for establishing a safe pharmaceutical supply chain. Methods Protocols. (2021) 4:85. doi: 10.3390/mps4040085
73. Das, KP, and Chandra, J. A survey on artificial intelligence for reducing the climate footprint in healthcare. Energy Nexus. (2023) 9:100167. doi: 10.1016/j.nexus.2022.100167
74. Di Vaio, A, Palladino, R, Hassan, R, and Escobar, O. Artificial intelligence and business models in the sustainable development goals perspective: a systematic literature review. J Bus Res. (2020) 121:283–314. doi: 10.1016/j.jbusres.2020.08.019
75. Bag, S, Dhamija, P, Singh, RK, Rahman, MS, and Sreedharan, VR. Big data analytics and artificial intelligence technologies based collaborative platform empowering absorptive capacity in health care supply chain: an empirical study. J Bus Res. (2023) 154:113315. doi: 10.1016/j.jbusres.2022.113315
76. Bhattamisra, SK, Banerjee, P, Gupta, P, Mayuren, J, Patra, S, and Candasamy, M. Artificial intelligence in pharmaceutical and healthcare research. Big Data Cogn Comput. (2023) 7:10. doi: 10.3390/bdcc7010010
77. Jabarulla, MY, and Lee, HN. A blockchain and artificial intelligence-based, patient-centric healthcare system for combating the COVID-19 pandemic: opportunities and applications. Healthcare. (2021) 9:1019. doi: 10.3390/healthcare9081019
78. Adeniran, IA, Efunniyi, CP, Osundare, OS, and Abhulimen, AO. Optimizing logistics and supply chain management through advanced analytics: insights from industries. Eng Sci Technol J. (2024) 5:52–61.
79. Wiljer, D, and Hakim, Z. Developing an artificial intelligence–enabled health care practice: rewiring health care professions for better care. J Med Imag Radiat Sci. (2019) 50:S8–S14. doi: 10.1016/j.jmir.2019.04.005
80. Tadimalla, S. Y., and Maher, M. L. AI literacy for all: adjustable interdisciplinary socio-technical curriculum. arXiv preprint arXiv:2409.10552. (2024). doi: 10.48550/arXiv.2409.10552
81. Asrifan, A, Said, UMR, Jakob, JC, and Wanci, R. AI literacy: foundations, importance, and broader implications In: Transforming vocational education and training using AI. Hershey, Pennsylvania, USA: IGI Global Scientific Publishing (2025). 17–48.
82. Cheah, CG, Chia, WY, Lai, SF, Chew, KW, Chia, SR, and Show, PL. Innovation designs of industry 4.0 based solid waste management: machinery and digital circular economy. Environ Res. (2022) 213:113619. doi: 10.1016/j.envres.2022.113619
83. Chauhan, P, Yadav, RK, and Simon, R. Decoding AI’s impact on the workforce: a comprehensive analysis of opportunities, challenges, and strategic adaptations in job markets. Glob J Enterpr Inf Syst. (2024) 16:40–7.
84. George, AS. Artificial intelligence and the future of work: job shifting not job loss. Partners Univ Innov Res Publ. (2024) 2:17–37. doi: 10.5281/zenodo.10936490
85. Rashid, AB, and Kausik, AK. AI revolutionizing industries worldwide: a comprehensive overview of its diverse applications. Hybrid Adv. (2024) 7:100277. doi: 10.1016/j.hybadv.2024.100277
86. Dreier, V, Gelissen, T, Oliveira, M, Riezebos, S, Saxena, R, Sibal, P, et al. Multi-stakeholder AI development: 10 building blocks for inclusive policy design. Paris, France: UNESCO Publishing (2022).
87. Kumar, A. Knowledge transfer in the digital age: investigating the mechanisms and challenges. A, Knowl Transf Digital Age Invest Mech Challeng. (2024) 1–16. doi: 10.2139/ssrn.4809874
88. Eyo-Udo, N. Leveraging artificial intelligence for enhanced supply chain optimization. Open Access Res J Multidis Stud. (2024) 7:001–15.
89. Gavino, S., and Sobhani, S. E. Fostering mission-oriented innovation and AI for sustainable cities and communities: advancing collaboration and synergistic progress towards the 2030 agenda (2023) Departement Omgeving. doi: 10.53022/oarjms.2024.7.2.0044
90. Muafa, AM, Al-Obadi, SH, Al-Saleem, N, Taweili, A, and Al-Amri, A. The impact of artificial intelligence applications on the digital transformation of healthcare delivery in Riyadh, Saudi Arabia (opportunities and challenges in alignment with vision 2030). Acad J Res Sci Publ. (2024) 5, 61–102.
91. Aggarwal, N, Ahmed, M, Basu, S, Curtin, JJ, Evans, BJ, Matheny, ME, et al. Advancing artificial intelligence in health settings outside the hospital and clinic. NAM Perspectives. (2020) 2020. doi: 10.31478/202011b
92. Liang, W, Tadesse, GA, Ho, D, Fei-Fei, L, Zaharia, M, Zhang, C, et al. Advances, challenges and opportunities in creating data for trustworthy AI. Nat Mach Intell. (2022) 4:669–77. doi: 10.1038/s42256-022-00516-1
93. Norori, N, Hu, Q, Aellen, FM, Faraci, FD, and Tzovara, A. Addressing bias in big data and AI for health care: a call for open science. Patterns. (2021) 2:100347. doi: 10.1016/j.patter.2021.100347
94. Al-Saggaf, L, Al-Hadrami, AH, and Aoun, M. Healthcare sector in Saudi Arabia: initiatives and challenges In: Achieving sustainable business through AI, technology education and computer science: Volume 1: Computer science, business sustainability, and competitive advantage. Springer Nature Switzerland: Cham (2024). 203–14.
95. Tariq, MU. Revolutionizing health data management with blockchain technology: enhancing security and efficiency in a digital era In: Emerging Technologies for Health Literacy and Medical Practice. Hershey, Pennsylvania, USA: IGI Global (2024). 153–75.
96. Kreiri, AM, Shajiri, TM, Qaeari, BMA, Alnayif, BSA, Albloshi, FSH, Aseeri, RA, et al. Advancing health information Management in Saudi Arabia: challenges and opportunities. J Int Crisis Risk Commun Res. (2024) 7:1503–13.
97. Alkraiji, AI, Jackson, T, and Murray, I. Factors impacting the adoption decision of health data standards in tertiary healthcare organisations in Saudi Arabia. J Enterp Inf Manag. (2016) 29:650–76. doi: 10.1108/JEIM-11-2014-0111
98. Kallonas, C, Piki, A, and Stavrou, E. Empowering professionals: a generative AI approach to personalized cybersecurity learning In: 2024 IEEE global engineering education conference (EDUCON), Kos Island, Greece: IEEE (2024). 1–10.
99. Long, D., and Magerko, B. What is AI literacy? Competencies and design considerations. In Proceedings of the 2020 CHI conference on human factors in computing systems (pp. 1–16). (2020).
100. Sheerah, HA, AlSalamah, S, Alsalamah, SA, Lu, CT, Arafa, A, Zaatari, E, et al. The rise of virtual health care: transforming the health care landscape in the Kingdom of Saudi Arabia: a review article. Telemedicine and e-Health. (2024) 30:2545–54. doi: 10.1089/tmj.2024.0114
101. Hussain, M, Ajmal, M, Subramanian, G, Khan, M, and Anas, S. Challenges of big data analytics for sustainable supply chains in healthcare–a resource-based view. BIJ. (2024) 31:2897–918. doi: 10.1108/BIJ-06-2022-0390
102. AlRuthia, Y, Almutiri, NM, Almutairi, RM, Almohammed, O, Alhamdan, H, El-Haddad, SA, et al. Local causes of essential medicines shortages from the perspective of supply chain professionals in Saudi Arabia. Saudi Pharm J. (2023) 31:948–54. doi: 10.1016/j.jsps.2023.04.019
103. Aljarboa, SS, Alaya, B, Al-Ajlan, A, and Miah, SJ. CDSS adoption and the role of artificial intelligence in Saudi Arabian primary healthcare. Inf Med Unlock. (2024):101596 (In Press). doi: 10.1016/j.imu.2024.101596
104. Morley, J, Machado, CC, Burr, C, Cowls, J, Joshi, I, Taddeo, M, et al. The ethics of AI in health care: a mapping review. Soc Sci Med. (2020) 260:113172. doi: 10.1016/j.socscimed.2020.113172
105. Božić, V., and Poola, I. The role of artificial intelligence in increasing the digital literacy of healthcare workers and standardization of healthcare. (2023) 4:1–13. Preprint.
106. Alsanosi, SM, and Padmanabhan, S. Potential applications of artificial intelligence (AI) in managing polypharmacy in Saudi Arabia: a narrative review. Healthcare. (2024) 12:788. doi: 10.3390/healthcare12070788
107. Saeed, A, Saeed, AB, and AlAhmri, FA. Saudi Arabia health systems: challenging and future transformations with artificial intelligence. Cureus. (2023) 15:e37826. doi: 10.7759/cureus.37826
108. Morley, J, Murphy, L, Mishra, A, Joshi, I, and Karpathakis, K. Governing data and artificial intelligence for health care: developing an international understanding. JMIR Format Res. (2022) 6:e31623. doi: 10.2196/31623
109. Al Yousuf, M, Akerele, TM, and Al Mazrou, YY. Organization of the Saudi health system. EMHJ-Eastern Mediter Health J. (2002) 8:645–53. doi: 10.26719/2002.8.4-5.645
110. Mansour, H. The impediments to advancing artificial intelligence in healthcare within the middle eastern context: a critical examination. J Adv Anal Healthc Manag. (2022) 6:58–65.
111. Moldt, JA, Festl-Wietek, T, Fuhl, W, Zabel, S, Claassen, M, Wagner, S, et al. Assessing AI awareness and identifying essential competencies: insights from key stakeholders in integrating AI into medical education. JMIR Med Educ. (2024) 10:e58355. doi: 10.2196/58355
112. Xia, H, Sun, Z, Wang, Y, Zhang, JZ, Kamal, MM, Jasimuddin, SM, et al. Emergency medical supplies scheduling during public health emergencies: algorithm design based on AI techniques. Int J Prod Res. (2025) 63:628–50. doi: 10.1080/00207543.2023.2267680
113. Alyami, MAM, Atti, NSA, Masmali, FMM, Oraibi, MH, Alruwaili, MA, Mahdi, ZMA, et al. The role of artificial intelligence in transforming healthcare leadership: a systematic review of current trends and future directions. J Namib Stud Hist Polit Cult. (2022) 31:86–106.
114. Ramadan, OME, Alruwaili, MM, Alruwaili, AN, Elsehrawy, MG, and Alanazi, S. Facilitators and barriers to AI adoption in nursing practice: a qualitative study of registered nurses' perspectives. BMC Nurs. (2024) 23:891. doi: 10.1186/s12912-024-02571-y
115. Dasaklis, TK, and Tsoulfas, GT. The future of healthcare supply chains: integrating industry 4.0 technologies for improved resilience and sustainability In: Hospital supply chain: challenges and opportunities for improving healthcare. Cham: Springer Nature Switzerland (2024). 533–51.
116. Habbash Saleh Almansour, S, and Almansour, MHH. The role of health technology in improving healthcare services in Saudi Arabia. J Int Crisis Risk Commun Res. (2024) 7:812–31.
117. Maita, KC, Maniaci, MJ, Haider, CR, Avila, FR, Torres-Guzman, RA, Borna, S, et al. The impact of digital health solutions on bridging the health care gap in rural areas: a scoping review. Perm J. (2024) 28:130–43. doi: 10.7812/TPP/23.134
118. Al Baalharith, I. M., and Aboshaiqah, A. E. A Delphi study on identifying competencies in virtual healthcare for healthcare professionals. Healthcare (2024) 12:739. doi: 10.3390/healthcare12070739
119. Chikhaoui, E, Alajmi, A, and Larabi-Marie-Sainte, S. Artificial intelligence applications in healthcare sector: ethical and legal challenges. Emerg Sci J. (2022) 6:717–38. doi: 10.28991/ESJ-2022-06-04-05
120. Tash, AA, and Al-Bawardy, RF. Cardiovascular disease in Saudi Arabia: facts and the way forward. J Saudi Heart Assoc. (2023) 35:148–62. doi: 10.37616/2212-5043.1336
121. Memish, ZA, Altuwaijri, MM, Almoeen, AH, and Enani, SM. The Saudi Data & Artificial Intelligence Authority (SDAIA) vision: leading the kingdom’s journey toward global leadership. J Epidemiol Global Health. (2021) 11:140–2. doi: 10.2991/jegh.k.210405.001
122. Leoste, J, Õun, T, Loogma, K, and San Martín López, J. Designing training programs to introduce emerging technologies to future workers—a pilot study based on the example of artificial intelligence enhanced robotics. Mathematics. (2021) 9:2876. doi: 10.3390/math9222876
123. Davis, FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. (1989) 13:319. doi: 10.2307/249008
124. Venkatesh, V, Morris, MG, Davis, GB, and Davis, FD. User acceptance of information technology: toward a unified view. MIS Q. (2003) 27:425. doi: 10.2307/30036540
125. Drazin, R. The processes of technological innovation: David A. Tansik book review editor Louis G. Tornatzky and Mitchell Fleischer. Lexington, MA: DC Heath & Company (1991) 1990. 298 pages.£ 44.95.
126. Baker, J. The technology–organization–environment framework. Inf Syst Theory Explain Predict Our Digital Soc. (2011) 28:231–45. doi: 10.1007/978-1-4419-6108-2_12
127. Rezaei, J. Best-worst multi-criteria decision-making method. Omega. (2015) 53:49–57. doi: 10.1016/j.omega.2014.11.009
128. Gunduz, MA, Demir, S, and Paksoy, T. Matching functions of supply chain management with smart and sustainable tools: a novel hybrid BWM-QFD based method. Comput Ind Eng. (2021) 162:107676. doi: 10.1016/j.cie.2021.107676
129. Kolagar, M, Hosseini, SMH, Felegari, R, and Fattahi, P. Policy-making for renewable energy sources in search of sustainable development: a hybrid DEA-FBWM approach. Environ Syst Decis. (2020) 40:485–509. doi: 10.1007/s10669-019-09747-x
130. Ecer, F. Sustainability assessment of existing onshore wind plants in the context of triple bottom line: a best-worst method (BWM) based MCDM framework. Environ Sci Pollut Res. (2021) 28:19677–93. doi: 10.1007/s11356-020-11940-4
131. Rowshan, M, Shojaei, P, Askarifar, K, and Rahimi, H. Identifying and prioritizing effective factors on outsourcing in public hospitals using fuzzy BWM. Hosp Top. (2020) 98:16–25. doi: 10.1080/00185868.2019.1711482
132. Hao, Y., Liu, Z., Riter, R. N., and Kalantari, S. Advancing patient-centered shared decision-making with AI systems for older adult cancer patients. In Proceedings of the CHI conference on human factors in computing systems (pp. 1–20). (2024).
133. Srdjevic, B, Srdjevic, Z, Reynolds, KM, Lakicevic, M, and Zdero, S. Using analytic hierarchy process and best–worst method in group evaluation of urban park quality. Forests. (2022) 13:290. doi: 10.3390/f13020290
134. Sharma, H, Sohani, N, and Yadav, A. Comparative analysis of ranking the lean supply chain enablers: an AHP, BWM and fuzzy SWARA based approach. Int J Qual Reliab Manag. (2022) 39:2252–71. doi: 10.1108/IJQRM-04-2021-0114
135. Sharma, M, Luthra, S, Joshi, S, and Kumar, A. Accelerating retail supply chain performance against pandemic disruption: adopting resilient strategies to mitigate the long-term effects. J Enterp Inf Manag. (2021) 34:1844–73. doi: 10.1108/JEIM-07-2020-0286
136. Sharma, M, Joshi, S, and Govindan, K. Overcoming barriers to implement digital technologies to achieve sustainable production and consumption in the food sector: a circular economy perspective. Sustain Prod Consum. (2023) 39:203–15. doi: 10.1016/j.spc.2023.04.002
137. Dwivedi, YK, Hughes, DL, Ismagilova, E, Aarts, G, and Coombs, C. Artificial intelligence (AI): multidisciplinary perspectives on emerging challenges, opportunities, and agenda for research, practice, and policy. Int J Inf Manag. (2021) 57:102261. doi: 10.1016/j.ijinfomgt.2020.102261
138. Reddy, S, Allan, S, Coghlan, S, and Cooper, P. A governance model for the application of AI in health care. Lancet Digital Health. (2019) 1:e35–7. doi: 10.1016/S2589-7500(19)30020-5
139. Harihara, CG. Optimization and rule-based models for hospital inventory management (Doctoral dissertation) Massachusetts Institute of Technology (2024).
140. Nugraha, JAM, Suryono, S, and Suseno, JE. Rule based system for medicine inventory control using radio frequency identification (RFID) In: 2nd International conference on energy, environment and information system. Semarang, Universitas Diponegoro: (2017)
141. Jebbor, S, Chiheb, R, El Afia, A, and Gallab, M. Designing a fully automated and integrated inventory and replenishment system for hospitals. Int J Syst Sci: Oper Logist. (2023) 10:1962429. doi: 10.1080/23302674.2021.1962429
142. Granlund, A, and Wiktorsson, M. Automation in healthcare internal logistics: a case study on practice and potential. Int J Innov Technol Manag. (2013) 10:1340012. doi: 10.1142/S0219877013400129
143. Mackey, TK, and Cuomo, RE. An interdisciplinary review of digital technologies to facilitate anti-corruption, transparency and accountability in medicines procurement. Glob Health Action. (2020) 13:1695241. doi: 10.1080/16549716.2019.1695241
144. Kindle, RD, Badawi, O, Celi, LA, and Sturland, S. Intensive care unit telemedicine in the era of big data, artificial intelligence, and computer clinical decision support systems. Crit Care Clin. (2019) 35:483–95. doi: 10.1016/j.ccc.2019.02.005
145. Omar, IA, Jayaraman, R, Debe, MS, Salah, K, Yaqoob, I, and Omar, M. Automating procurement contracts in the healthcare supply chain using blockchain smart contracts. IEEE Access. (2021) 9:37397–409. doi: 10.1109/ACCESS.2021.3062471
146. Kruse, CS, Stein, A, Thomas, H, and Kaur, H. The use of electronic health records to support population health: a systematic review of the literature. J Med Syst. (2018) 42:214. doi: 10.1007/s10916-018-1075-6
147. Shafqat, S, Kishwer, S, Rasool, RU, Qadir, J, Amjad, T, and Ahmad, HF. Big data analytics enhanced healthcare systems: a review. J Supercomput. (2020) 76:1754–99. doi: 10.1007/s11227-017-2222-4
148. Iqbal, K. Resource optimization and cost reduction for healthcare using big data analytics. Int J Soc Anal. (2023) 8:13–26.
149. Yinusa, A, and Faezipour, M. Optimizing healthcare delivery: a model for staffing, patient assignment, and resource allocation. Appl Syst Innov. (2023) 6:78. doi: 10.3390/asi6050078
150. Lazaroiu, G, Androniceanu, A, Grecu, I, Grecu, G, and Neguriță, O. Artificial intelligence-based decision-making algorithms, internet of things sensing networks, and sustainable cyber-physical management systems in big data-driven cognitive manufacturing. Oeconomia Copernicana. (2022) 13:1047–80. doi: 10.24136/oc.2022.030
151. Srivastava, S, Garg, D, and Agarwal, A. Responsive supply chain management in healthcare industry: an overview. Glob J Enterpr Inf Syst. (2020) 12:46–53.
152. Galli, L, Levato, T, Schoen, F, and Tigli, L. Prescriptive analytics for inventory management in health care. J Oper Res Soc. (2021) 72:2211–24. doi: 10.1080/01605682.2020.1776167
153. Liu, Y, Wang, M, and Wang, Y. Location decision of emergency medical supply distribution centers under uncertain environment. Int J Fuzzy Syst. (2024) 26:1567–603. doi: 10.1007/s40815-024-01689-0
154. Piffari, C, Lagorio, A, and Cagliano, AC. AI applications in the healthcare logistics and supply chain sectors In: IFIP international conference on advances in production management systems. Cham: Springer (2024). 61–75.
155. Yi, Y. Establishing the concept of AI literacy. Jahr–European J Bioethics. (2021) 12:353–68. doi: 10.21860/j.12.2.8
156. Jerfy, A, Selden, O, and Balkrishnan, R. The growing impact of natural language processing in healthcare and public health. INQUIRY J Health Care Org Provision Financ. (2024) 61:00469580241290095. doi: 10.1177/00469580241290095
157. Feng, D, and Feng, MQ. Computer vision for structural dynamics and health monitoring. Hoboken, New Jersey, USA: John Wiley & Sons (2021).
158. Meduri, K, Nadella, GS, Gonaygunta, H, and Meduri, SS. Developing a fog computing-based AI framework for real-time traffic management and optimization. Int J Sustain Dev Comput Sci. (2023) 5:1–24.
159. Jose, R, Panigrahi, SK, Patil, RA, Fernando, Y, and Ramakrishna, S. Artificial intelligence-driven circular economy as a key enabler for sustainable energy management. Mater Circ Econ. (2020) 2:1–7. doi: 10.1007/s42824-020-00009-9
160. Sharma, M, Joshi, S, Kannan, D, Govindan, K, Singh, R, and Purohit, HC. Internet of things (IoT) adoption barriers of smart cities’ waste management: an Indian context. J Clean Prod. (2020) 270:122047. doi: 10.1016/j.jclepro.2020.122047
161. Sharma, M, Joshi, S, and Kumar, A. Assessing enablers of e-waste management in circular economy using DEMATEL method: an Indian perspective. Environ Sci Pollut Res. (2020) 27:13325–38. doi: 10.1007/s11356-020-07765-w
162. Okeleke, PA, Ajiga, D, Folorunsho, SO, and Ezeigweneme, C. Predictive analytics for market trends using AI: a study in consumer behavior. Int J Eng Res Updat. (2024) 7:036–49. doi: 10.53430/ijeru.2024.7.1.0032
163. Ara, A, Maraj, MAA, Rahman, MA, and Bari, MH. The impact of machine learning on prescriptive analytics for optimized business decision-making. Int J Manag Inf Syst Data Sci. (2024) 1:7–18. doi: 10.62304/ijmisds.v1i1.112
164. Beutel, AL, and Minner, S. Safety stock planning under causal demand forecasting. Int J Prod Econ. (2012) 140:637–45. doi: 10.1016/j.ijpe.2011.04.017
165. Gonzalez, M, and Rabbi, F. Evaluating the impact of big data analytics on personalized E-commerce shopping experiences and customer retention strategies. J Comput Soc Dyn. (2023) 8:13–25.
166. Ogundipe, OB, Okwandu, AC, and Abdulwaheed, SA. Optimizing construction supply chains through AI: streamlining material procurement and logistics for project success. GSC Adv Res Rev. (2024) 20:147–58. doi: 10.30574/gscarr.2024.20.1.0258
167. Roosevelt, SC, Veemaraj, E, and Kirubakaran, S. Real time stock inventory management system In: 2024 8th international conference on inventive systems and control (ICISC), Coimbatore, India: IEEE (2024, July). 156–62.
168. Zsidisin, GA, and Siferd, SP. Environmental purchasing: a framework for theory development. Eur J Purchas Supply Manag. (2001) 7:61–73. doi: 10.1016/S0969-7012(00)00007-1
169. Zhao, L, and Wang, Y. Research on optimizing human resource expenditure in the allocation of materials in universities. Information. (2024) 15:522. doi: 10.3390/info15090522
170. Vora, LK, Gholap, AD, Jetha, K, Thakur, RRS, Solanki, HK, and Chavda, VP. Artificial intelligence in pharmaceutical technology and drug delivery design. Pharmaceutics. (2023) 15:1916. doi: 10.3390/pharmaceutics15071916
171. Kartoglu, U, and Ames, H. Ensuring quality and integrity of vaccines throughout the cold chain: the role of temperature monitoring. Expert Rev Vaccines. (2022) 21:799–810. doi: 10.1080/14760584.2022.2061462
172. Abid, SK, Sulaiman, N, Chan, SW, Nazir, U, Abid, M, Han, H, et al. Toward an integrated disaster management approach: how artificial intelligence can boost disaster management. Sustain For. (2021) 13:12560. doi: 10.3390/su132212560
173. Hale, T, and Moberg, CR. Improving supply chain disaster preparedness: a decision process for secure site location. Int J Phys Distrib Logist Manag. (2005) 35:195–207. doi: 10.1108/09600030510594576
174. Krzywanski, J, Sosnowski, M, Grabowska, K, Zylka, A, Lasek, L, and Kijo-Kleczkowska, A. Advanced computational methods for modeling, prediction and optimization—a review. Materials. (2024) 17:3521. doi: 10.3390/ma17143521
175. Kundel, HL, Nodine, CF, Conant, EF, and Weinstein, SP. Holistic component of image perception in mammogram interpretation: gaze-tracking study. Radiology. (2007) 242:396–402. doi: 10.1148/radiol.2422051997
176. Marmolejo-Correa, D, Juarez-Valdivia, RG, and Rodriguez-Navarro, A. Optimization of preventive maintenance program for imaging equipment in hospitals In: Computer aided chemical engineering, vol. 38. Amsterdam, Netherlands: Elsevier (2016). 1833–8.
177. AlFawaz, I, Ahmed, B, Ali, A, Ayas, M, AlKofide, A, Habib, Z, et al. Experience of treating pediatric hepatoblastoma at King Faisal Specialist Hospital and research center, Riyadh, Saudi Arabia - timely surgical intervention playing a key role. Int J Pediatr Adolescent Med. (2021) 8:39–43. doi: 10.1016/j.ijpam.2020.11.001
178. Dlamini, Z, Francies, FZ, Hull, R, and Marima, R. Artificial intelligence (AI) and big data in cancer and precision oncology. Comput Struct Biotechnol J. (2020) 18:2300–11. doi: 10.1016/j.csbj.2020.08.019
179. Ahmad, Z, Rahim, S, Zubair, M, and Abdul-Ghafar, J. Artificial intelligence (AI) in medicine, current applications and future role with special emphasis on its potential and promise in pathology: present and future impact, obstacles including costs and acceptance among pathologists, practical and philosophical considerations. A comprehensive review. Diagn Pathol. (2021) 16:1–16. doi: 10.1186/s13000-021-01085-4
180. Aljondi, R, Alghamdi, SS, Tajaldeen, A, Alassiri, S, Alkinani, MH, and Bertinotti, T. Application of artificial intelligence in the mammographic detection of breast cancer in Saudi Arabian women. Appl Sci. (2023) 13:12087. doi: 10.3390/app132112087
181. Courtney, P, and Royall, PG. Using robotics in laboratories during the covid-19 outbreak: a review. IEEE Robot Automat Mag. (2021) 28:28–39. doi: 10.1109/MRA.2020.3045067
182. Abdallah, S, Sharifa, M, Almadhoun, MKI, Khawar, MMSr, Shaikh, U, Balabel, KM, et al. The impact of artificial intelligence on optimizing diagnosis and treatment plans for rare genetic disorders. Cureus. (2023) 15:e46860. doi: 10.7759/cureus.46860
183. Abu-Elmagd, M, Assidi, M, Schulten, HJ, Dallol, A, Pushparaj, PN, Ahmed, F, et al. Individualized medicine enabled by genomics in Saudi Arabia. BMC Med Genet. (2015) 8:1–17. doi: 10.1186/1755-8794-8-S1-S1
184. Hall, D, Miller, JA, Arnold, J, Kochut, KJ, Sheth, AP, and Weise, MJ. Using workflow to build an information management system for a geographically distributed genome sequencing initiative In: Genomics of plants and Fungi. Boca Raton, Florida, USA: CRC Press (2003). 359–71.
185. Henry, E. Ai-driven optimization in healthcare: machine learning models for predictive diagnostics and personalized treatment strategies. Well Test J. (2024) 33:10–33.
186. Pattyam, SP. AI in data science for healthcare: advanced techniques for disease prediction, treatment optimization, and patient management. Distrib Learn Broad Appl Sci Res. (2019) 5:417–55.
187. da Costa, LS. Applying artificial intelligence to improve the effectiveness of the demand forecasting in a specialty pharmacy (Doctoral dissertation) University of Cincinnati (2023).
188. Kanakaprabha, S, Kumar, GG, Reddy, BP, Raju, YR, and Rai, PCM. Wearable devices and health monitoring: big data and AI for remote patient care In: Intelligent data analytics for bioinformatics and biomedical systems, Wiley, Hoboken, New Jersey, USA (2024). 291–311.
189. Murala, DK, Panda, SK, and Dash, SP. MedMetaverse: medical care of chronic disease patients and managing data using artificial intelligence, blockchain, and wearable devices state-of-the-art methodology. IEEE Access. (2023) 11:138954–85. doi: 10.1109/ACCESS.2023.3340791
190. Chintala, S. Improving healthcare accessibility with AI-enabled telemedicine solutions. Int J Res Rev Tech. (2023) 2:75–81.
191. Andrikopoulou, E. The rise of AI in telehealth In: Emerging practices in telehealth. Cambridge, Massachusetts, USA: Academic Press (2023). 183–207.
192. Prabhod, KJ. The role of artificial intelligence in reducing healthcare costs and improving operational efficiency. Quart J Emerg Technol Innov. (2024) 9:47–59.
193. Alanazi, SA, Alanazi, AO, Alanazi, HS, Alanazi, TG, Almutiri, MH, Alharbi, AAS, et al. Integrating digital technologies and artificial intelligence into electronic health records to enhance healthcare outcomes. J Int Crisis Risk Commun Res. (2024) 7:976–83.
194. Anjum, S, Ramaguru, R, and Sethumadhavan, M. Medical records management using distributed ledger and storage In: International conference on advances in computing and data sciences. Cham: Springer International Publishing (2021). 52–62.
195. Johnson, M, Albizri, A, and Harfouche, A. Responsible artificial intelligence in healthcare: predicting and preventing insurance claim denials for economic and social wellbeing. Inf Syst Front. (2023) 25:2179–95. doi: 10.1007/s10796-021-10137-5
196. Abidi, MH, Rehman, AU, Mian, SH, Alkhalefah, H, and Usmani, YS. The role of AI in elevating hospital service quality: framework, development, and applications In: Modern healthcare marketing in the digital era. Hershey, Pennsylvania, USA: IGI Global (2024). 211–24.
197. Poirier, CC, and Reiter, SE. Supply chain optimization: building the strongest total business network. Oakland, California: Berrett-Koehler Publishers (1996).
198. Gupta, R, Srivastava, D, Sahu, M, Tiwari, S, Ambasta, RK, and Kumar, P. Artificial intelligence to deep learning: machine intelligence approach for drug discovery. Mol Divers. (2021) 25:1315–60. doi: 10.1007/s11030-021-10217-3
199. Kazim, SM, AlGhamdi, SA, Lytras, MD, and Alsaywid, BS. Nurturing future leaders: cultivating research and innovation skills in Saudi scientific community In: Transformative leadership and sustainable innovation in education: interdisciplinary perspectives. Leeds, England: Emerald Publishing Limited (2024). 231–65.
200. Ding, B. Pharma industry 4.0: literature review and research opportunities in sustainable pharmaceutical supply chains. Process Saf Environ Prot. (2018) 119:115–30. doi: 10.1016/j.psep.2018.06.031
201. Harrer, S, Shah, P, Antony, B, and Hu, J. Artificial intelligence for clinical trial design. Trends Pharmacol Sci. (2019) 40:577–91. doi: 10.1016/j.tips.2019.05.005
202. Gunasekeran, DV, Tham, YC, Ting, DSW, Tan, GSW, and Wong, TY. Digital health during COVID-19: lessons from operationalising new models of care in ophthalmology. Lancet Digit Health. (2021) 3:e124–34. doi: 10.1016/S2589-7500(20)30287-9
203. Hardter, E, Collins, J, Shmueli-Blumberg, D, and Armstrong, G. Procurement and distribution of study medicines In: Principles and practice of clinical trials, Emmes, Karnataka, India, Berlin: Springer, (2022). 169–89.
204. Dogheim, GM, and Hussain, A. Patient care through AI-driven remote monitoring: analyzing the role of predictive models and intelligent alerts in preventive medicine. J Contemp Healthc Anal. (2023) 7:94–110.
205. Binhowemel, S, Alfakhri, M, AlReshaid, K, and Alyani, A. Role of artificial intelligence in diabetes research diagnosis and prognosis: a narrative review. J Health Inf Dev Countr. (2023) 17, pp. 1–12.
206. Maluleke, K, Musekiwa, A, Kgarosi, K, Gregor, EM, Dlangalala, T, Nkambule, S, et al. A scoping review of supply chain management systems for point of care diagnostic services: optimising COVID-19 testing capacity in resource-limited settings. Diagnostics. (2021) 11:2299. doi: 10.3390/diagnostics11122299
207. Topol, E. Deep medicine: how artificial intelligence can make healthcare human again. London, England: Hachette UK (2019).
208. Lords, H. O. AI in the UK: ready, willing and able?. House of lords select committee on artificial intelligence report of session 2017–19. Retrieved August, 13, 2021. (2018) 1–183.
209. Joshi, S, Sharma, M, Das, RP, Rosak-Szyrocka, J, Żywiołek, J, Muduli, K, et al. Modeling conceptual framework for implementing barriers of AI in public healthcare for improving operational excellence: experiences from developing countries. Sustain For. (2022) 14:11698. doi: 10.3390/su141811698
210. Estonian Business and Innovation Agency. E-health. E-Estonia. (2025). Available online at: https://e-estonia.com/solutions/e-health/e-health-records/ (Accessed Feburary 14, 2025).
211. Ngiam, KY, and Khor, W. Big data and machine learning algorithms for health-care delivery. Lancet Oncol. (2019) 20:e262–73. doi: 10.1016/S1470-2045(19)30149-4
212. Rehman, A, Naz, S, and Razzak, I. Leveraging big data analytics in healthcare enhancement: trends, challenges and opportunities. Multimedia Systems. (2022) 28:1339–71. doi: 10.1007/s00530-020-00736-8
213. Gunasekeran, DV, Tseng, RMWW, Tham, YC, and Wong, TY. Applications of digital health for public health responses to COVID-19: a systematic scoping review of artificial intelligence, telehealth and related technologies. NPJ Digit Med. (2021) 4:40. doi: 10.1038/s41746-021-00412-9
214. Allahham, M, Sharabati, AAA, Hatamlah, H, Ahmad, AYB, Sabra, S, and Daoud, MK. Big data analytics and AI for green supply chain integration and sustainability in hospitals. WSEAS Trans Environ Dev. (2023) 19:1218–30. doi: 10.37394/232015.2023.19.111
215. Juliet, AH, and Kalaiselvi, K. Role of technology in healthcare systems In: Artificial intelligence-based system models in healthcare. eds. Anand, AJ, Kalaiselvi, K, and Chatterje, JM. (2024). 1–30. doi: 10.1002/9781394242528.ch1
216. Zolfani, SH, and Chatterjee, P. Comparative evaluation of sustainable design based on step-wise weight assessment ratio analysis (SWARA) and best worst method (BWM) methods: a perspective on household furnishing materials. Symmetry. (2019) 11:74. doi: 10.3390/sym11010074
Annexure I
Step 1: The experts outline and give details of a set of parameters.
Step 2: Evaluation of super-optimal (B) and unsuitable (W) criteria by the specialists.
Step 3: A pairwise comparison has been carried out for each criterion using a 9-point scale to determine the preferred criterion in relation to others. The comparative results are illustrated as a vector ordered from the highest to the other vectors.
where represents the preferences of the best criterion B over the criterion j.
Step 4: The preferences for the remaining criteria in relation to the least favorable criterion are determined using a vector scale of 1 to 9.
where denotes the preference of criteria j over the least favorable criterion W.
Step 5: Mathematical model 1 is utilized to compute the weights of the criterion (Equation 1).
(w1*, w2*, … wn*)
Model 1
s.t:
To determine the weigts of the criteria (w1*, w2*, … wn*), model 1 can be converted into model 2 (Equation 2),
Min
s.t.
The consistency ratio (CR) of the Best-Worst Method (BWM) is denoted by ξ*, and the associated consistency index (CI) values are calculated using Equation 3.
A smaller ξ* corresponds to a lower CR value and greater consistency among the vectors.
Keywords: artificial intelligence, AI literacy, adoption challenges, public healthcare, Sustainable Development Goals, Saudi Arabia
Citation: Kumar R, Singh A, Kassar ASA, Humaida MI, Joshi S and Sharma M (2025) Adoption challenges to artificial intelligence literacy in public healthcare: an evidence based study in Saudi Arabia. Front. Public Health. 13:1558772. doi: 10.3389/fpubh.2025.1558772
Edited by:
Suraiya Jabin, Jamia Millia Islamia, IndiaReviewed by:
Dinesh Gunasekeran, National University of Singapore, SingaporeSaba Sarwar, Jamia Millia Islamia, India
Copyright © 2025 Kumar, Singh, Kassar, Humaida, Joshi and Sharma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rakesh Kumar, cmEua3VtYXJAdW9oLmVkdS5zYQ==
 Rakesh Kumar
Rakesh Kumar Ajay Singh
Ajay Singh Ahmed Subahi Ahmed Kassar
Ahmed Subahi Ahmed Kassar Mohammed Ismail Humaida
Mohammed Ismail Humaida Sudhanshu Joshi
Sudhanshu Joshi Manu Sharma
Manu Sharma