- 1Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
- 2Department of Community Medicine, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
- 3Environmental Medicine and Occupational Medicine Excellent Center, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
- 4Department of Psychiatry, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
Objective: This study aimed to determine the prevalence of Imposter Syndrome (IP) and its associated factors among Thai medical students.
Methods: Thai medical students voluntarily participated in this cross-sectional survey conducted from September to October 2022. The completed online questionnaires included the Clance Imposter Phenomenon Scale (CIPS) to assess IP Status, along with several other factors from different questionnaires: the Single-Item Measurement of Suicidal Behaviors, the Patient Health Questionnaire, the Resilience Inventory, and the Rosenberg Self-Esteem Scale. Linear regression analyses were conducted to examine the associations between these factors and IP.
Results: A study involving 477 medical students revealed that 47.1% of Thai participants reported experiencing frequent IP, while 7.1% identified at an intense level. Notably, students in their 2nd year, along with those exhibiting high resilience, demonstrated lower CIPS scores when compared to their 1st-year counterparts, with regression coefficients of −4.72 and −9.66, respectively. Conversely, factors such as moderate and high self-esteem, as well as indicators of depression, were significantly associated with an increased severity of IP.
Conclusion: Approximately 50% of Thai medical students experience Impostor Syndrome, which is associated with higher rates of depression. Additionally, high self-esteem may worsen IP. Promoting resilience through structured curricula and group therapy overseen by medical schools could be an effective approach to address this issue.
1 Introduction
Impostor Syndrome (IP), also known as the impostor phenomenon, is a psychological experience characterized by persistent self-doubt despite objective successes and a fear of being discovered as a fraud. IP is commonly observed among medical students. Additionally, organizational culture plays a significant role in the emergence of IP, and the prevailing culture in medicine, which fosters a fear of failure, can be detrimental (1, 2). IP can have various implications for medical education, potentially leading to differences in learning styles. This highlights the need to tailor curricula to accommodate the considerable number of learners experiencing IP.
The prevalence of IP varies across different professions, with rates ranging from 23.7 to 50.0%. Graduate students experience IP rates between 25.8 to 33.3% (3–5), while college students report rates between 40.0 and 50.0% (6, 7). Medical students experience IP prevalence from 23.7 to 49.4% (8–10), and other professions have rates between 24.0 to 39.0% (11–14). Factors contributing to these variations include internal elements like self-evaluation and self-perception (15), and external influences such as family dynamics and workplace culture (16). IP can lead to physical symptoms, including headaches, stomach aches, and insomnia, as well as mental health issues such as psychological distress, low self-esteem, depression, and burnout (8, 17, 18).
The IP can lead to significant consequences such as anxiety, self-criticism (19, 20), and even suicidal ideation in severe cases (15, 21). In medical schools, IP is associated with decreased performance, poor professional identity, and lack of confidence, all of which increase stress in a competitive environment (22, 23). To cope, processes like self-reflection and self-evaluation can foster resilience and self-confidence (24). Effective strategies include reflective journaling, structured supervision, and group workshops, which can reduce scores on the Clance Impostor Phenomenon Scale (CIPS) and enhance self-awareness and self-confidence (25).
Despite the notable prevalence of IP among medical students, there is a significant gap in research concerning Thai medical colleges. This study aims to assess the prevalence of IP among this population and identify the factors associated with it.
2 Materials and methods
2.1 Participants, study design, and data collection
This study was conducted as a cross-sectional survey involving Thai medical students from their first to sixth year, between September and October 2022. Data were collected through a secure website accessible only to authorized personnel. Participants volunteered after being informed via Facebook (Overcoming Imposter Project), Instagram (imposter.syndrome.bootcamp2022), and a Line® application group, the most popular instant messaging and voice-over-IP service in Thailand. In collaboration with the Society of Medical Students of Thailand, letters were also sent to Thai medical institutions to inform them about the study. Participants provided informed consent before completing Thai-language questionnaires anonymously, which included their region, year of study, and academic performance. The survey assessed factors such as the CIPS, the Single-Item Measurement of Suicidal Behaviors, the Patient Health Questionnaire (PHQ-9) for depression, the Resilience Inventory (RI-9), and the Rosenberg Self-Esteem Scale (RSES).
Upon completing the survey, participants received automatically generated results for the CIPS, the Single-Item Measurement of Suicidal Behaviors, PHQ-9, RI-9, and RSES, along with individualized feedback for each measure provided by a psychiatrist. They were also given contact information for free psychological services available to all Thai medical students, including a website, hotline, and Facebook page for the Department of Mental Health. The study’s sample size was calculated using Biostatistics, yielding a total of 384 participants, based on parameters d = 0.05, p = 0.474, and alpha = 0.05, from a cross-sectional study on the Impostor Phenomenon among medical students in Thailand (26). Participants needed to be medical students in their 1st to 6th years in 2022, have internet access, and be able to read Thai, while those studying outside Thailand were excluded. Eligibility was confirmed through two questions: “Are you a 1st to 6th year medical student?” and “Are you a medical student studying in Thailand?” Only those who answered “Yes” to both could proceed with the survey.
2.2 Study variables
The prevalence of IP among the students, as the outcome variable, was determined using the CIPS, originally developed by Clance and Imes (27) and validated in Thai by Chaisaen (18). The CIPS consists of 20 items rated on a six-point scale (0 = strongly disagree to 5 = strongly agree), with the total score ranging from 0 to 100. Scores were categorized into four levels of IP: mild (0–40), moderate (41–60), frequent (61–80), and intense (81–100) (28). A score of 61 or higher indicates that the individual has experienced IP (28). The overall Cronbach’s alpha for this scale was 0.96, which indicated good internal consistency (29).
The study identified factors affecting IP severity as indicated by CIPS scores, including student region, age, medical year, and GPA, as well as suicidal ideation, depressive disorder, resilience, and self-esteem.
Data from the Single-Item Measurement of Suicidal Behaviors were utilized to evaluate participants’ experiences of suicidal feelings over the past year (30). Participants indicated “yes” or “no” to whether they had experienced suicidal thoughts in the last 12 months. This measurement indicated a false positive rate of 10.7% and a false negative rate of 6.39% (31).
The depressive status was assessed using the PHQ-9, a validated nine-item tool for screening and monitoring major depressive disorder (MDD). Participants rated their symptoms on a 4-point scale from 0 (“Not at all”) to 3 (“Almost every day”), with total scores ranging from 0 to 27. A score of 9 or higher indicated potential major depression, with a sensitivity of 0.84 and specificity of 0.77 compared to the Thai Mini International Neuropsychiatric Interview (32). Depression severity was categorized as mild (9–14 points), moderate (15–19 points), and severe (≥20 points) (33).
The RI-9, a validated nine-item instrument, was used to assess an individual’s ability to cope with adversity. Participants responded on a 5-point Likert scale, where 1 point means “does not describe me at all” and 5 points mean “describes me very well.” Total scores range from 9 to 45. Participants were categorized based on their scores: below the 25th percentile reflects low resilience, between the 25th and 75th percentile indicates average resilience, and above the 75th percentile indicated high resilience (34). The instrument has a strong reliability with a Cronbach’s alpha of 0.90 (35).
The RSES is a validated 10-item instrument designed to measure an individual’s self-worth and self-esteem. Participants rated their level of agreement with each statement using a 4-point Likert scale: 1 point for “strongly disagree,” 2 points for “disagree,” 3 points for “agree,” and 4 points for “strongly agree.” Scores ranged from 10 to 40, with the following interpretations: low self-esteem (10–25), medium self-esteem (26–29), and high self-esteem (30–40) (36). The Cronbach’s alpha for the Thai version of the RSES was found to be 0.86 (37), and this version was utilized in the present study.
The study followed the Declaration of Helsinki, and the protocol received approval from the Research Ethics Committee of the Faculty of Medicine at Chiang Mai University, Thailand (Study code: FAC-MED-2565-09115).
2.3 Statistical analysis
Data are presented as counts and percentages for categorical variables, and as means and standard deviations or medians and interquartile ranges (IQR) for continuous variables, depending on normality. Normality was assessed using Q–Q plots and histograms. The prevalence of IP is calculated as the number of individuals with IP in each category divided by the total number of participants. The numerical CIPS score from each student served as the outcome variable to evaluate IP severity in simple linear regression models, which examined factors like student demographics, suicidal ideation, depressive disorders, resilience, and self-esteem. Each academic year was treated separately as a categorical variable due to its unique context. Established cut points for the RSES, RI-9, and PHQ-9 were also used. The regression coefficients indicated the relationship between IP severity and associated factors.
The study findings adhered to the Strengthening the Reporting of Observational Studies in Epidemiology statement guidelines (38). After data collection, the missingness patterns were reviewed. Observations with completely at random missing data (MCAR) were excluded, and a frequency-based inverse probability weighting was used to account for missing data at random (MAR) from the sampling variability across pre-clinical and clinical years. For missing data not at random (MNAR), we did not perform imputation. A sensitivity analysis was conducted using the difference in beta (dfbeta) method to assess influential observations and result robustness. Robust variance correction was applied for highly influential observations, and all analyses were conducted using STATA version 16.0.
3 Results
3.1 Data description
The study flow diagram of participants is shown in Figure 1. A total of 477 completed all questionnaires. The distribution of respondents is as follows: North (57.2%), Bangkok (18.0%), Northeast (15.7%), Central-West–East (7.3%), and South (1.6%). The demographic characteristics of the participants are summarized in Table 1. The mean ± SD age of the participants was 21.0 ± 2.0 years, with a minimum age of 18 years and a maximum age of 44 years. Most participants (76.5%) were in their preclinical years (1st–3rd years), with approximately 20% in each of these years. The number of respondents in the clinical years (4th–6th year students) was lower than in the preclinical years. Based on the multiple-choice questions with a 0.5-grade interval of academic grades, over half (54.1%) of the participants reported high academic performance scores (3.51–4.00), while the 25th percentile fell between 3.01 and 3.5. The scores for resilience, self-esteem, and depression were reported as medians of 33 (IQR 29-37), 26 (IQR 25-27), and 8 (IQR 5-13), respectively. Many participants reported moderate levels of resilience and self-esteem. Interestingly, almost half reported experiencing depression within the past 2 weeks, and one-fifth indicated having thoughts of suicide. Data was initially assumed to be MNAR in the first section, which included age and academic year. After the CIPS section, the data was considered MCAR due to a loss of 2% (9 out of 486) across the sections of the questionnaire, which comprised the RSES, RI-9, PHQ-9, and measures of suicidal ideation. As a result, no imputation for missing data imputation was performed.
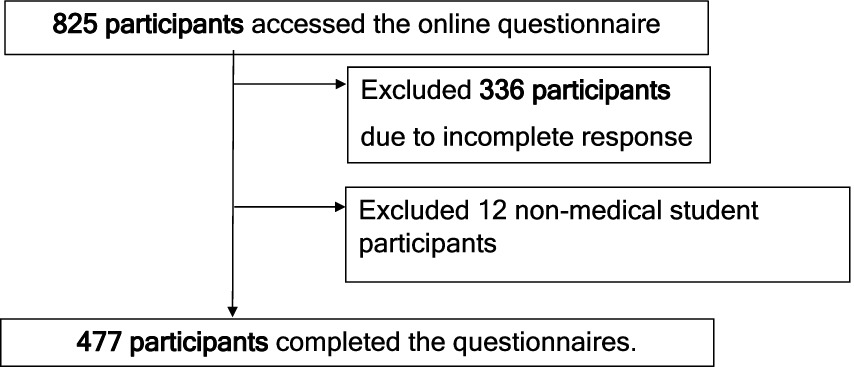
Figure 1. Study flow diagram demonstrating the recruitment process in the 1st – 6th year medical students across Thailand from September to October 2022.
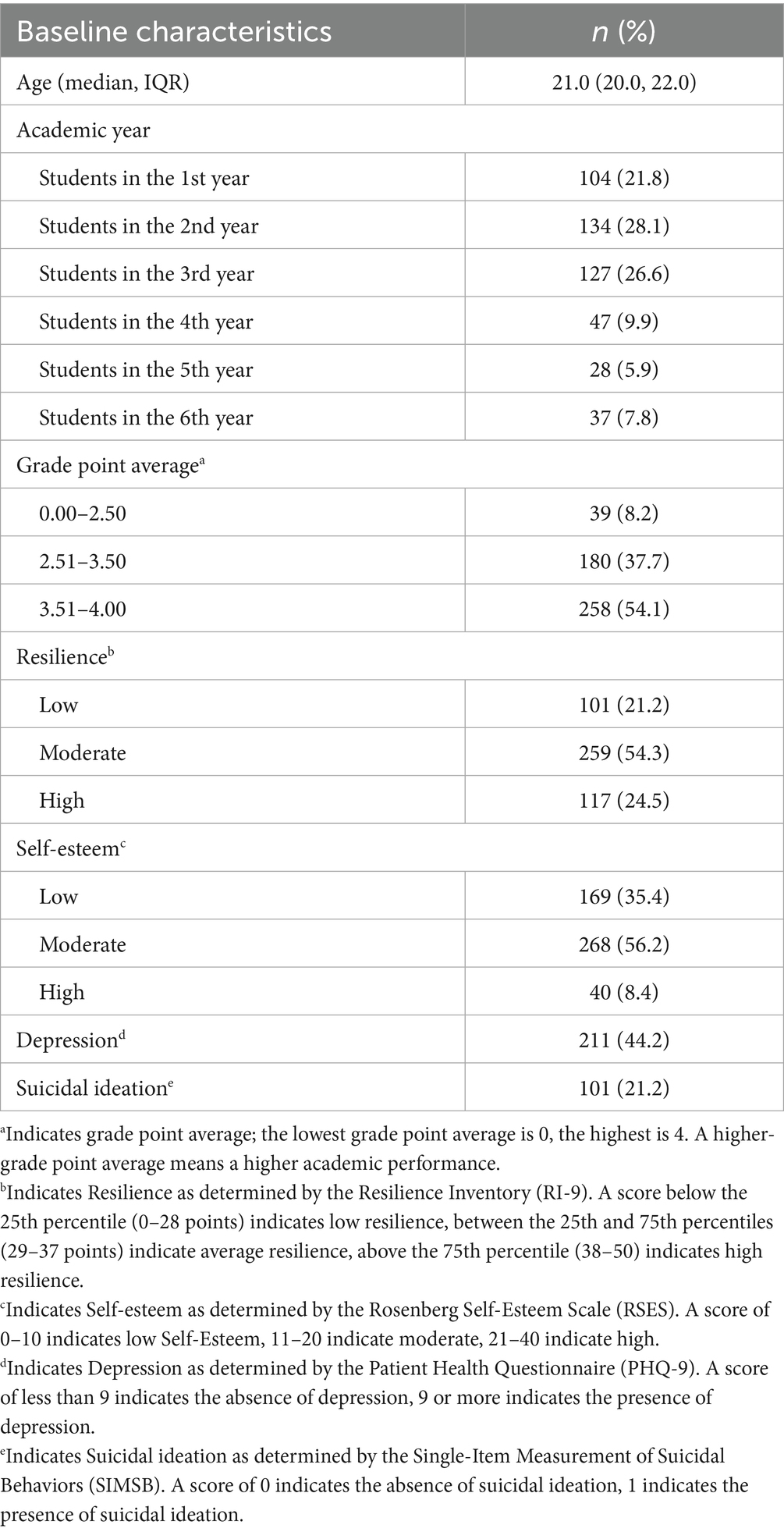
Table 1. Descriptive baseline and sociodemographic characteristics of participating 1st – 6th year medical students across Thailand (September to October 2022).
3.2 Imposter syndrome
The overall mean and SD of the CIPS score were 58.3 and 16.0, respectively. As shown in Table 2, 40% of Thai medical students reported frequently experiencing IP, while only 7.1% reported intense IP.

Table 2. Mean (standard deviation) and frequency and proportion across severity categories of imposter syndrome scores in the 1st – 6th year medical students across Thailand (September to October 2022).
3.3 Factors associated with imposter syndrome
The results from exploratory multivariable linear regression models, which included robust standard error correction, are presented in Table 3. Students in their 2nd exhibited lower levels of IP severity compared to 1st-year students, with CIPS regression coefficients of −4.72 (95% CI: −7.97, −1.47). No differences were found among students in other academic years. Additionally, higher levels of resilience were associated with less severe IP. Students with high resilience showed a notably greater decrease in severity, with a regression coefficient of −9.66 (95% CI: −15.40, −3.91) compared to those with low resilience.
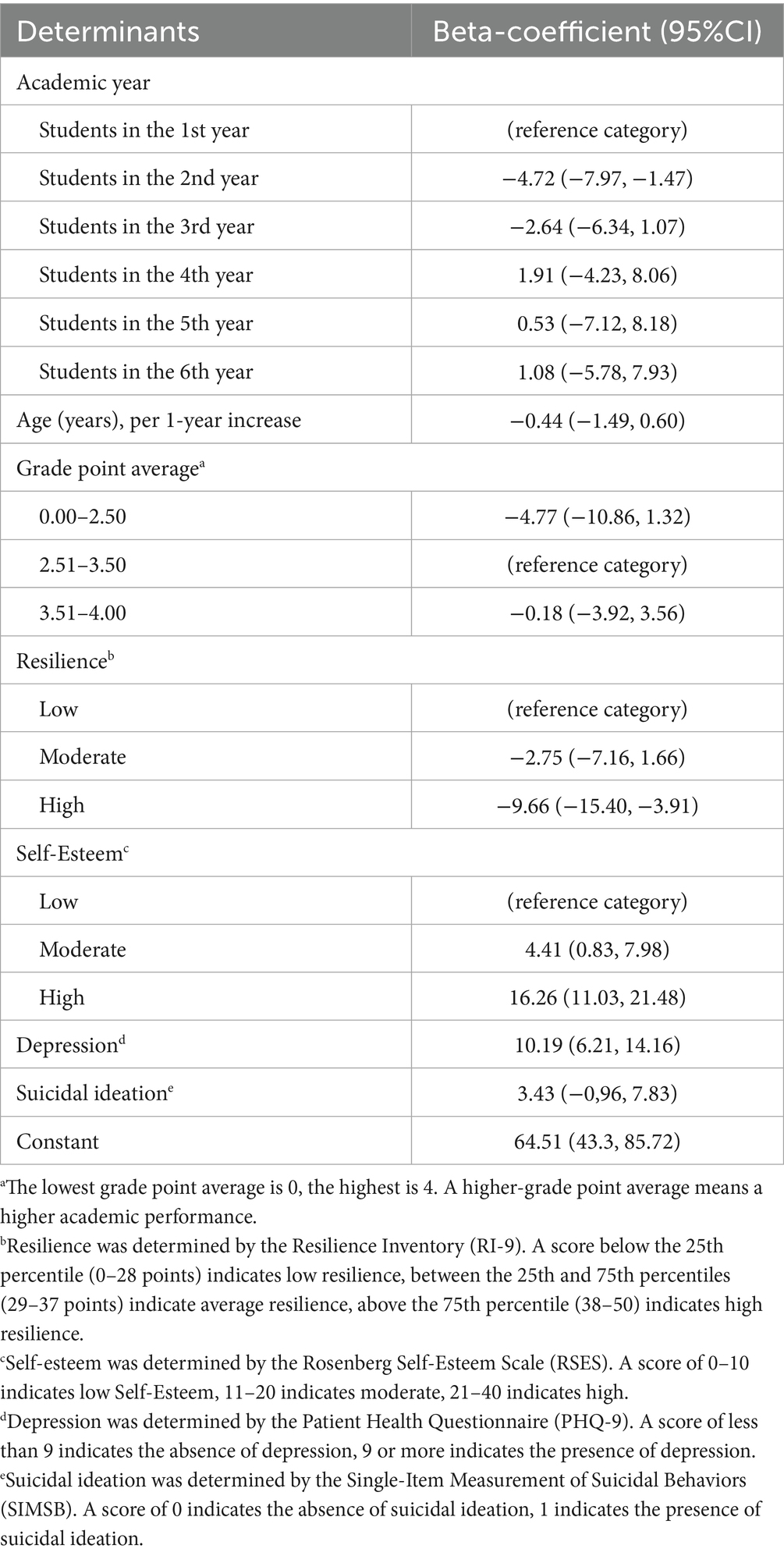
Table 3. Multivariable linear regression demonstrating factors associated with imposter syndrome, using CIPS scores, the dependent variable, in the 1st – 6th year medical students across Thailand (September to October 2022).
Higher self-esteem and depression were linked to an increase in the severity of IP. Students with moderate self-esteem experienced a 4.41 regression coefficient (95% CI: 0.83, 7.98) increase in severity compared to those with low self-esteem. In contrast, students with high self-esteem showed a significant regression coefficient increase of 16.26 (95% CI: 11.03, 21.48) in severity. Additionally, students reporting depression had a 10.19 regression coefficient (95% CI: 6.21, 14.16) increase.
4 Discussion
4.1 Prevalence
This study found that 42.8% of Thai medical students surveyed experienced IP using a cutoff CIPS score of 61. The prevalence of IP among medical students worldwide ranges from 30.6 to 87% (22, 39–41). For example, 30.6% of individuals are affected in Peru, and 45.2% in the Middle East (22). In the USA, prevalence rates range from 58 to 87%, while in Canada, it is reported at 73% (42). Although IP has not been widely reported in Asia, our findings suggest that Thai medical students also experience it. The prevalence among these students is similar to that in South America and the Middle East, though it may be lower than in higher-income countries like the USA and Canada. Most studies on IP have been conducted outside of Asia. One Asian study linked high parental expectations, common in many Asian families, to IP. However, the prevalence we found is not excessively high, indicating that other factors may reduce imposter feelings. Future research should explore this with a larger sample size and a wider range of factors.
4.2 Factors associated with the severity of imposter syndrome
4.2.1 Demographics
This study found that 2nd-year medical students had a CIPS regression coefficient decrease of −4.72 (95% CI: −7.97, −1.47), compared to 1st-year students. A study from the United Kingdom (43) indicates that feelings of impostor syndrome often intensify during critical transitional life phases, such as the transition to university. Therefore, the score reduction observed in the 2nd-year could be attributed to the relatively stable environment of preclinical years, which minimized the need for constant adaptation and, in turn, resulted in lowered impostor syndrome scores. However, the prevalence of impostor syndrome among medical students remains controversial across various social contexts. Studies conducted in Brazil (44) and Ireland (22) have shown no significant differences in the prevalence of impostor syndrome among students across different academic years. Conversely, a study conducted in the USA (39) reported a significant increase in impostor scores during the final year compared to the first year when students entered university. Unlike findings related to the academic year, our study found that age differences did not affect the severity of IP. Other studies have also reported no differences in the severity of IP between age groups (22, 45, 46).
4.2.2 Psychological issues
This study found that depression were linked to increased IP severity, with CIPS regression coefficients of 10.19. IP. Researchers have also established positive connections between IP and depression in Peruvian medical students (41), Thai medical students (26), and Egyptian nursing students (47). Experiencing stress and being surrounded by more successful peers can intensify these feelings (41, 48). While IP is not a mental illness, it can contribute to mental health issues by increasing stress and negative self-perception. Conversely, depression may also evoke feelings of inadequacy similar to IP. Recognizing the bidirectional relationship between IP and depression is essential, as they can reinforce each other.
4.2.3 Self-esteem
According to Table 3, 1st to 6th years students with high self-esteem in this study exhibited higher scores for IP. This is the first report of the positive relationship between high self-esteem and more severe IP in Thailand. In contrast, most previous studies involving medical students in other regions have found a relationship between low self-esteem and IP (22, 40, 41, 48). Differences in the population’s culture, lifestyle, and mental health may explain this finding. Additionally, Asian individuals with lower self-esteem often adopt an emotionally driven coping style to manage stressors, and lower self-esteem is associated with reduced anxiety in the Asian population (49).
While high self-esteem and IP may initially appear to be contradictory (22, 40, 41, 48, 50), they can coexist. In fact, high self-esteem can sometimes lead to IP due to the pressure of high expectations (51), competition (17, 52), fear of judgment (53, 54), and the need to maintain a positive self-image. The occurrence of high expectations starts before entering medical school, with impressive academic records and achievements that significantly contribute to their acceptance. As a result, they tend to set very high standards for themselves (55). They encounter substantial academic and professional pressures due to the demanding medical curriculum, exposure to extensive and complex information, and constant evaluations by professors, preceptors, and peers. This pressure can lead to feelings of inadequacy, as students may feel overwhelmed and doubt their ability to master all aspects of their studies. Such feelings can threaten their self-image and self-worth (56–58). In the medical school environment, students find themselves surrounded by exceptionally motivated and talented peers (59). Individuals with high self-esteem often engage in a cycle of self-comparison with their classmates, which can lead to feelings of inadequacy when they perceive others excelling. This ongoing self-evaluation can intensify the impact of IP. Students with high self-esteem may feel increased anxiety about receiving negative feedback (60, 61). This anxiety can worsen IP when they receive criticism or constructive input (53, 62), making them question the legitimacy of their admission and attributing their success to luck or external factors rather than recognizing their abilities. In addition, individuals with high self-esteem tend to have a fear of judgment and often strongly desire to maintain a positive self-image (63). They may worry that admitting gaps in their knowledge or seeking help could diminish how competent their peers perceive them to be. This fear of potential judgment can trigger IP when they face challenges or make mistakes (17).
4.2.4 Resilience
Our results indicate that higher resilience was associated with lower CIPS scores. Participants with high resilience experienced a significant reduction in IP severity, with a CIPS regression coefficient of −9.66. Similarly, a study conducted in Saudi Arabia identified a negative correlation between two factors among undergraduate nursing and medical students, evidenced by a significant correlation coefficient of r = −0.220 (64). This correlation was also observed in a study among Brazilian medical students (65). Resilience, the ability to adapt to stress, serves as a protective factor against IP, leading to fewer depressive symptoms and burnout (65).
4.3 Strengths and limitations
This study is one of the few to investigate the impact of IP on Thai medical students, revealing both negative factors like depression as well as positive aspects such as resilience. These findings could inform positive psychology policies for medical students. However, this study has some limitations. First, there are challenges in measuring IP prevalence through online surveys, as satisfied individuals may opt out. Statistical methods, sample size calculation, and an approach to informing students on a variety of platforms were used to address imbalances and enhance the integrity of our findings. A more standardized sampling approach could be implemented to improve sample representation. Second, the cross-sectional nature of the study limits the ability to establish causal relationships. Most parameters related to behavior were presented some time before the study was performed. However, the time occurrence of some parameters and outcomes is uncertain. Therefore, the result of our study must be carefully applied, and adopting longitudinal designs in future studies could clarify the relationship. Finally, as the questionnaire-based survey cannot collect qualitative information, future research should consider exploring alternative methods, such as interviews or focus groups, that could provide more insight into the field.
4.4 Practice implications and intervention suggestions for medical schools
This study found that high self-esteem correlates with high IP, indicating that even confident, high-performing students can experience self-doubt. Therefore, educators should not assume students are immune to psychological struggles. Medical schools should routinely assess students’ mental health, provide accurate and constructive feedback, normalize conversations about mental health, offer support, and integrate resilience-building programs into the curriculum, as these have been shown to enhance resilience (66, 67).
5 Conclusion
Almost half of Thai medical students face IP, similar to medical students in other countries. This condition is linked to higher risks of other mental health issues, including depression. This study found that individuals with higher self-esteem may also experience the impostor phenomenon. Future studies should implement a more standardized sampling approach to improve representation and adopt longitudinal designs to clarify the relationship. Medical educators and schools should regularly assess students for stress and insecurity, monitor their psychological health, provide follow-up care for those showing signs of depression, and integrate resilience-building programs into the curriculum to better support them.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The study followed the Declaration of Helsinki, and the protocol received approval from the Research Ethics Committee of the Faculty of Medicine at Chiang Mai University, Thailand (Study code: FAC-MED-2565-09115). The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because this is an online questionnaire, the research participants will read the Inform consent document carefully. Then, if the participants agree to take the questionnaire, you will be able to press enter to do it immediately without having to sign (Consent by action).
Author contributions
AS: Conceptualization, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. VS: Conceptualization, Formal analysis, Methodology, Project administration, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing. NK: Conceptualization, Formal analysis, Methodology, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing. RA: Conceptualization, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. DD: Conceptualization, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. WK: Data curation, Formal analysis, Software, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We sincerely thank Barbara Metzler and Ruth Leatherman, RN, for their invaluable assistance in proofreading this manuscript. Their attention to detail and expertise greatly enhanced its clarity and quality.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CIPS, Clance Imposter Phenomenon Scale; IP, Imposter Syndrome; PHQ-9, Patient Health Questionnaire; RI-9, Resilience Inventory; RSES, Rosenberg Self-Esteem Scale.
References
1. Huecker, MR, Shreffler, J, McKeny, PT, and Davis, D. Imposter phenomenon. Treasure Island, Florida: StatPearls (2023).
2. Harvey, JC, and Katz, C. If I'm so successful, why do I feel like a fake?: The impostor phenomenon. New York: St. Martin's Press (1985).
3. Jöstl, G, Bergsmann, E, Lüftenegger, M, Schober, B, and Spiel, C. When will they blow my cover? Z Psychol. (2015) 220:109–20. doi: 10.1027/2151-2604/a000102
4. Ferrari, JR. Impostor tendencies and academic dishonesty: do they cheat their way to success? Soc Behav Pers. (2005) 33:11–8. doi: 10.2224/sbp.2005.33.1.11
5. Selby, CL, and Mahoney, MJ. Psychological and physiological correlates of self-complexity and authenticity. Construct Hum Sci. (2002) 7:39–52.
6. Patzak, A, Kollmayer, M, and Schober, B. Buffering impostor feelings with kindness: the mediating role of self-compassion between gender-role orientation and the impostor phenomenon. Front Psychol. (2017) 8:1289. doi: 10.3389/fpsyg.2017.01289
7. Sonnak, C, and Towell, T. The impostor phenomenon in British university students: relationships between self-esteem, mental health, parental rearing style and socioeconomic status. Pers Individ Differ. (2001) 31:863–74. doi: 10.1016/S0191-8869(00)00184-7
8. Villwock, JA, Sobin, LB, Koester, LA, and Harris, TM. Impostor syndrome and burnout among American medical students: a pilot study. Int J Med Educ. (2016) 7:364–9. doi: 10.5116/ijme.5801.eac4
9. Legassie, J, Zibrowski, EM, and Goldszmidt, MA. Measuring resident well-being: impostorism and burnout syndrome in residency. J Gen Intern Med. (2008) 23:1090–4. doi: 10.1007/s11606-008-0536-x
10. Henning, K, Ey, S, and Shaw, D. Perfectionism, the impostor phenomenon, and psychological adjustment in medical, dental, nursing, and pharmacy students. Med Educ. (1998) 32:456–64. doi: 10.1046/j.1365-2923.1998.00234.x
11. Vergauwe, J, Wille, B, Feys, M, De Fruyt, F, and Anseel, F. Fear of being exposed: the trait-relatedness of the impostor phenomenon and its relevance in the work context. J Bus Psychol. (2015) 30:565–81. doi: 10.1007/s10869-014-9382-5
12. Castro, DM, Jones, RA, and Mirsalimi, H. Parentification and the impostor phenomenon: an empirical investigation. Am J Fam Ther. (2010) 32:205–16. doi: 10.1080/01926180490425676
13. Chae, J-H, Piedmont, RL, Estadt, BK, and Wicks, RJ. Personological evaluation of Clance's imposter phenomenon scale in a Korean sample. J Pers Assess. (2010) 65:468–85. doi: 10.1207/s15327752jpa6503_7
14. Cromwell, B, Brown, N, and Adair, FL. The impostor phenomenon and personality characteristics of high school honor students. Soc Behav Pers. (1990) 5:563–73.
15. Thomas, M, and Bigatti, S. Perfectionism, impostor phenomenon, and mental health in medicine: a literature review. Int J Med Educ. (2020) 11:201–13. doi: 10.5116/ijme.5f54.c8f8
16. Baumann, N, Faulk, C, Vanderlan, J, Chen, J, and Bhayani, RK. Small-group discussion sessions on imposter syndrome. MedEdPORTAL. (2020) 16:11004. doi: 10.15766/mep_2374-8265.11004
17. Lin, E, Crijns, TJ, Ring, D, and Jayakumar, PThe Science of Variation Group. Imposter syndrome among surgeons is associated with intolerance of uncertainty and lower confidence in problem-solving. Clin Orthop Relat Res. (2023) 481:664–71. doi: 10.1097/corr.0000000000002390
18. Chaisaen, A. Causal factors and the consequences of the impostor phenomenon in Thai doctoral students. Bangkok: Srinakharinwirot University (2016).
19. Chrisman, SM, Pieper, W, Clance, PR, Holland, C, and Glickauf-Hughes, C. Validation of the Clance imposter phenomenon scale. J Pers Assess. (1995) 65:456–67. doi: 10.1207/s15327752jpa6503_6
20. Cozzarelli, C, and Major, B. Exploring the validity of the impostor phenomenon. J Soc Clin Psychol. (1990) 9:401–17. doi: 10.1521/jscp.1990.9.4.401
21. Alrayyes, S, Dar, UF, Alrayes, M, Alghutayghit, A, and Alrayyes, N. Burnout and imposter syndrome among Saudi young adults. The strings in the puppet show of psychological morbidity. Saudi Med J. (2020) 41:189–94. doi: 10.15537/smj.2020.2.24841
22. Naser, MJ, Hasan, NE, Zainaldeen, MH, Zaidi, A, Mohamed, Y, and Fredericks, S. Impostor phenomenon and its relationship to self-esteem among students at an international medical college in the Middle East: a cross-sectional study. Front Med. (2022) 9:850434. doi: 10.3389/fmed.2022.850434
23. Khan, M. Imposter syndrome—a particular problem for medical students. BMJ. (2021) 375:3048. doi: 10.1136/bmj.n3048
24. Chapman, A. Using the assessment process to overcome imposter syndrome in mature students. J Furth High Educ. (2015) 41:1–8. doi: 10.1080/0309877X.2015.1062851
25. Siddiqui, ZK, Church, HR, Jayasuriya, R, Boddice, T, and Tomlinson, J. Educational interventions for imposter phenomenon in healthcare: a scoping review. BMC Med. (2024) 24:43. doi: 10.1186/s12909-023-04984-w
26. Shinawatra, P, Kasirawat, C, Khunanon, P, Boonchan, S, Sangla, S, and Maneeton, B. Exploring factors affecting impostor syndrome among undergraduate clinical medical students at Chiang Mai University, Thailand: a cross-sectional study. Behav Sci. (2023) 13:976. doi: 10.3390/bs13120976
27. Clance, PR, and Imes, SA. The imposter phenomenon in high achieving women: dynamics and therapeutic intervention. Psychol Psychother. (1978) 15:241–7. doi: 10.1037/h0086006
28. Clance, PR. The impostor phenomenon: When success makes you feel like a fake. Toronto: Bantam Book (1985).
29. Freeman, KJ, Houghton, S, Carr, SE, and Nestel, D. Measuring impostor phenomenon in healthcare simulation educators: a validation of the Clance impostor phenomenon scale and Leary impostorism scale. BMC Med. (2022) 22:139. doi: 10.1186/s12909-022-03190-4
30. Meehan, PJ, Lamb, JA, Saltzman, LE, and O'Carroll, PW. Attempted suicide among young adults: progress toward a meaningful estimate of prevalence. Am J Psychiatry. (1992) 149:41–4. doi: 10.1176/ajp.149.1.41
31. Millner, AJ, Lee, MD, and Nock, MK. Single-item measurement of suicidal behaviors: validity and consequences of misclassification. PLoS One. (2015) 10:e0141606. doi: 10.1371/journal.pone.0141606
32. Lotrakul, M, Sumrithe, S, and Saipanish, R. Reliability and validity of the Thai version of the PHQ-9. BMC Psychiatry. (2008) 8:46. doi: 10.1186/1471-244X-8-46
33. Kaewporndawan, T, and Chaiudomsom, C. The prevalence and associated factors of depression among residents in training at faculty of medicine, Siriraj hospital. J Psychiatr Assoc Thai. (2013) 59:41–50.
34. Wongpakaran, N, Wongpakaran, T, and Kuntawong, P. Development and validation of the (inner) strength-based inventory. Ment Health Relig Cult. (2020) 23:263–73. doi: 10.1080/13674676.2020.1744310
35. Wongpakaran, T, Yang, T, Varnado, P, Siriai, Y, Mirnics, Z, Kövi, Z, et al. The development and validation of a new resilience inventory based on inner strength. Sci Rep. (2023) 13:2506. doi: 10.1038/s41598-023-29848-7
36. Álvarez-Pardo, S, De Paz, JA, Montserrat Romero-Pérez, E, Portilla-Cueto, KM, Horta-Gim, MA, González-Bernal, JJ, et al. Factors associated with body image and self-esteem in mastectomized breast cancer survivors. Int J Environ Res Public Health. (2023) 20:5154. doi: 10.3390/ijerph20065154
37. Wongpakaran, T, and Wongpakaran, N. A comparison of reliability and construct validity between the original and revised versions of the Rosenberg self-esteem scale. Psychiatry Investig. (2012) 9:54–8. doi: 10.4306/pi.2012.9.1.54 42
38. Von Elm, E, Altman, DG, Egger, M, Pocock, SJ, Gøtzsche, PC, and Vandenbroucke, JP. The strengthening the reporting of observational studies in epidemiology statement: guidelines for reporting observational studies. J Clin Epidemiol. (2008) 61:344–9. doi: 10.1016/j.jclinepi.2007.11.008
39. Rice, J, Rosario-Williams, B, Williams, F, West-Livingston, L, Savage, D, Wilensky, JA, et al. Impostor syndrome among minority medical students who are underrepresented in medicine. J Natl Med Assoc. (2023) 115:191–8. doi: 10.1016/j.jnma.2023.01.012
40. Rosenthal, S, Schlussel, Y, Yaden, MB, DeSantis, J, Trayes, K, Pohl, C, et al. Persistent impostor phenomenon is associated with distress in medical students. Fam Med. (2021) 53:118–22. doi: 10.22454/FamMed.2021.799997
41. Vilchez-Cornejo, J, Romani, L, Chávez-Bustamante, SG, Copaja-Corzo, C, Sánchez-Vicente, JC, Viera-Morón, RD, et al. Imposter syndrome and its associated factors in medical students in six Peruvian faculties. Rev Colomb Psiquiatr. (2021) 28:S0034-7450(21)00088-3. doi: 10.1016/j.rcp.2021.04.011
42. Neufeld, A, Babenko, O, Lai, H, Svrcek, C, and Malin, G. Why do we feel like intellectual frauds? A self-determination theory perspective on the impostor phenomenon in medical students. Teach Learn Med. (2023) 35:180–92. doi: 10.1080/10401334.2022.2056741
43. Ogunyemi, D, Lee, T, Ma, M, Osuma, A, Eghbali, M, and Bouri, N. Improving wellness: defeating impostor syndrome in medical education using an interactive reflective workshop. PLoS One. (2022) 17:e0272496. doi: 10.1371/journal.pone.0272496
44. Campos, IFS, Camara, GF, Carneiro, AG, Kubrusly, M, Peixoto, RAC, and Peixoto Junior, AA. Impostor syndrome and its association with depression and burnout among medical students. Rev Bras Educ Med. (2022) 46:e068. doi: 10.1590/1981-5271v46.2-20200491.ING
45. Brauer, K, and Proyer, RT. The impostor phenomenon and causal attributions of positive feedback on intelligence tests. Pers Individ Differ. (2022) 194:111663. doi: 10.1016/j.paid.2022.111663
46. Shreffler, J, Weingartner, L, Huecker, M, Shaw, MA, Ziegler, C, Simms,, et al. Association between characteristics of impostor phenomenon in medical students and step 1 performance. TLM. (2021) 33:36–48. doi: 10.1080/10401334.2020.1784741
47. El-Ashry, AM, Taha, SM, Elhay, ESA, Hammad, HA, Khedr, MAK, and El-Sayed, MM. Prevalence of imposter syndrome and its association with depression, stress, and anxiety among nursing students: a multi-center cross-sectional study. BMC Nurs. (2024) 23:862. doi: 10.1186/s12912-024-02414-w
48. Gottlieb, M, Chung, A, Battaglioli, N, Sebok-Syer, SS, and Kalantari, A. Impostor syndrome among physicians and physicians in training: a scoping review. Med Educ. (2020) 54:116–24. doi: 10.1111/medu.13956
49. Amorim, F. E. S., and Lam, M. K. G.. (2013). Self-esteem and anxiety among Asian and European students [dissertation/master's thesis]. Umeå: Umeå University. Available online at: https://www.diva-portal.org/smash/get/diva2:635116/fulltext01.pdf (accessed May 20, 2024).
50. Sawant, NS, Kamath, Y, Bajaj, U, Ajmera, K, and Lalwani, D. A study on impostor phenomenon, personality, and self-esteem of medical undergraduates and interns. Ind Psychiatry J. (2023) 32:136–41. doi: 10.4103/ipj.ipj_59_22
51. Dudău, DP. The relation between perfectionism and impostor phenomenon. Procedia Soc Behav Sci. (2014) 127:129–33. doi: 10.1016/j.sbspro.2014.03.226
52. Cader, FA, Gupta, A, Han, JK, Ibrahim, NE, Lundberg, GP, Mohamed, A, et al. How feeling like an imposter can impede your success. JACC Case Reports. (2021) 3:347–9. doi: 10.1016/j.jaccas.2021.01.003
53. Badawy, RL, Gazdag, BA, Bentley, JR, and Brouer, RL. Are all impostors created equal? Exploring gender differences in the impostor phenomenon-performance link. Pers Individ Differ. (2018) 131:156–63. doi: 10.1016/j.paid.2018.04.044
54. McLean, MC. The impostor syndrome: An obstacle to women's pursuit of power. Rutgers the State University of new Jersey, School of Graduate Studies ProQuest Dissertations and Theses (2017). 10799978 p.
55. Foong, CC, Bashir Ghouse, NL, Lye, AJ, Pallath, V, Hong, WH, and Vadivelu, J. Differences between high- and low-achieving pre-clinical medical students: a qualitative instrumental case study from a theory of action perspective. Ann Med. (2022) 54:195–210. doi: 10.1080/07853890.2021.1967440
56. Makowska, M, and Wyleżałek, J. A qualitative study of the mistreatment of medical students by their lecturers in polish medical schools. Int J Environ Res Public Health. (2021) 18:12271. doi: 10.3390/ijerph182312271
57. Nguyen, DT, Wright, EP, Dedding, C, Pham, TT, and Bunders, J. Low self-esteem and its association with anxiety, depression, and suicidal ideation in Vietnamese secondary school students: a cross-sectional study. Front Psych. (2019) 10:698. doi: 10.3389/fpsyt.2019.00698
58. Berjot, S, and Gillet, N. Stress and coping with discrimination and stigmatization. Front Psychol. (2011) 2:33. doi: 10.3389/fpsyg.2011.00033
59. Klingenberg, M., Gwozdz, A., and Gill, D.. The competitive environment in undergraduate medical education: Is it a barrier to becoming a “good doctor”? (2011). Available online at: https://www.researchgate.net/publication/258364114_Group_defenses_in_medical_education_-_a_psychoanalytic_examination (accessed March 16, 2024).
60. Fernandes, B, Newton, J, and Essau, CA. The mediating effects of self-esteem on anxiety and emotion regulation. Psychol Rep. (2022) 125:787–803. doi: 10.1177/0033294121996991
61. Brockner, J, Derr, WR, and Laing, WN. Self-esteem and reactions to negative feedback: toward greater generalizability. J Res Pers. (1987) 21:318–33. doi: 10.1016/0092-6566(87)90014-6
62. Gadsby, S, and Hohwy, J. Negative performance evaluation in the imposter phenomenon. Curr Psychol. (2024) 43:9300–8. doi: 10.1007/s12144-023-05030-0
63. Laws, VL, and Rivera, LM. The role of self-image concerns in discrepancies between implicit and explicit self-esteem. Personal Soc Psychol Bull. (2012) 38:1453–66. doi: 10.1177/0146167212452613
64. Khalil, AI, Alharbi, R, Qtame, HA, Bena, RA, and Khan, MA. Investigating the association between resilience and impostor syndrome in undergraduate nursing and medical students: a cross-sectional study. J Med Life. (2024) 17:868–79. doi: 10.25122/jml-2024-0160
65. Camara, GF, de Santiago Campos, IF, Carneiro, AG, de Sena Silva, IN, de Barros Silva, PG, Peixoto, RAC, et al. Relationship between resilience and the impostor phenomenon among undergraduate medical students. J Med Educ. (2022) 9:23821205221096105. doi: 10.1177/23821205221096105
66. Bravata, DM, Watts, SA, Keefer, AL, Madhusudhan, DK, Taylor, KT, Clark, DM, et al. Prevalence, predictors, and treatment of impostor syndrome: a systematic review. J Gen Intern Med. (2019) 35:1252–75. doi: 10.1007/s11606-019-05364-1
Keywords: imposter syndrome, resilience, self-esteem, depression, medical student
Citation: Suriyasathaporn A, Surawattanasakul V, Karawekpanyawong N, Aungkasuraphan R, Dejvajara D and Kiratipaisarl W (2025) Severity of imposter syndrome associated with resilience, self-esteem, and depression among medical students in Thailand. Front. Public Health. 13:1577184. doi: 10.3389/fpubh.2025.1577184
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
Alejandro Hernández Chávez, National Autonomous University of Mexico, MexicoSuppachai Lawanaskol, Chaiprakarn Hospital, Thailand
Copyright © 2025 Suriyasathaporn, Surawattanasakul, Karawekpanyawong, Aungkasuraphan, Dejvajara and Kiratipaisarl. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vithawat Surawattanasakul, dml0aGF3YXQuc3VyYXdhdEBjbXUuYWMudGg=
 Arpunna Suriyasathaporn
Arpunna Suriyasathaporn Vithawat Surawattanasakul
Vithawat Surawattanasakul Nuntaporn Karawekpanyawong
Nuntaporn Karawekpanyawong Ranlaphat Aungkasuraphan1
Ranlaphat Aungkasuraphan1 Wuttipat Kiratipaisarl
Wuttipat Kiratipaisarl