- 1Department of Global and International Health, School of Public Health, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
- 2Department of Health Promotion and Disability Studies, School of Public Health, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
Background: School-based interventions have been widely used in the prevention and control of childhood obesity. Teachers, as pivotal figures in child development, are strategically situated to aid in this process. Nonetheless, there is limited evidence regarding their role, awareness, and contribution to childhood obesity in Ghana. This study evaluated the role of teachers in the prevention and management of childhood obesity in Ghana.
Materials and methods: This quantitative, cross-sectional study included 74 teachers selected through convenience sampling from public schools in the Oforikrom Municipality of Kumasi, the capital of Ghana’s Ashanti Region. Data were gathered using a structured pre-tested questionnaire and analyzed using the R programming software. Binary logistic regression was performed to identify the factors associated with teacher’s participation in childhood obesity prevention programs.
Results: The study revealed that 46% of teachers were familiar with childhood obesity with only 33.8% of teachers familiar with its causes. Significant institutional hurdles included resource restrictions (46%), insufficient training (24.3%), and time constraints (12.2%). Chi-square analysis revealed that teachers’ participation in childhood obesity prevention was significantly associated with socioeconomic conditions (p = 0.016), challenges faced (p = 0.022), perception of physical activity (p = 0.012), physical education practices (p = 0.006), outdoor play promotion (p = 0.026), health screenings (p = 0.002), healthy eating education (p = 0.002), and counseling practices (p < 0.001). However, the multivariable logistic regression analysis revealed no statistically significant determinants of teachers’ participation.
Conclusion: The results highlight the necessity for specific measures, including professional development initiatives, institutional policy modifications, and resource distribution, to improve teachers’ ability to combat childhood obesity. Policymakers ought to incorporate comprehensive school health initiatives into the curriculum, prioritizing physical exercise and nutritious food.
Introduction
Obesity is a significant risk factor for non-communicable diseases (NCDs), including hypertension, cardiovascular illnesses, and certain malignancies (1). Over the last four decades, obesity has intensified into a global public health emergency, substantially exacerbating the prevalence of non-communicable diseases worldwide (2). The World Health Organization (WHO) categorizes overweight as a body mass index (BMI) of 25–29 kg/m2 and obesity as a BMI of 30 kg/m2 or more (3). Current figures indicate that 38% of the global population is classified as overweight or obese, with forecasts suggesting a significant rise in prevalence by 2030 (4, 5).
Childhood obesity is increasing, with more than 340 million children and adolescents aged 5–19 classified as overweight or obese in 2020, alongside 39 million children under 5 years old (6). Low- and middle-income countries (LMICs) have experienced a swift rise in obesity prevalence. In Tanzania, childhood obesity among school-aged children aged 6–9 ranges from 5.6% in Dodoma to 6.3% in Kinondoni (7). In Ghana, childhood obesity is an emerging public health issue, particularly in the urban areas (8) with 5% of school children in Cape Coast considered as obese, an additional 9% at high risk (9), and 2.3% in Kumasi, considered overweight and obese (10). Contributing factors include urbanization, industrialization, dietary shifts, and sedentary lifestyles (11, 12).
School-based interventions such as nutrition programs, physical activity promotion, and behavioral change initiatives have demonstrated potential in LMICs (13). These strategies aim to enhance nutritional status and promote healthier behaviors in children by utilizing schools as delivery platforms (14). Successful implementation requires collaboration with teachers, who are essential partners in executing effective obesity prevention measures. Teachers recognize the importance of health promotion in schools, as healthy students often achieve superior academic outcomes (15). Despite this awareness, societal prejudices and classroom-based constraints limit their effectiveness (16). Engaging teachers in program development improves both ownership and impact (17).
The Ghana Education Service (GES) introduced the School Health Education Programme (SHEP) in 1992 to promote health education in schools, aiming to equip students with life skills for healthy behaviors (18). However, evidence suggests that teachers often lack the training, knowledge, and resources necessary to address childhood obesity (9, 19). Although studies have been conducted to assess the role of teachers internationally (15, 17), limited research has been carried out in Ghana. Given the increasing rates of childhood obesity in Ghana and the essential role of teachers, this study seeks to assess their understanding of childhood obesity, available resources, policy frameworks, and the challenges they face. The findings will help develop targeted interventions and capacity-building programs for teachers in the country, with the broader aim of reducing childhood obesity rates, improving health outcomes for school-aged children, and supporting Ghana’s efforts to curb NCDs in its young population. This study therefore assessed the role of teachers in preventing and managing childhood obesity and identified the barriers and facilitators affecting their participation in obesity prevention among school-aged children in Kumasi, Ghana.
Materials and methods
Study design
Using a quantitative approach, we employed a cross-sectional study design to assess teachers’ awareness, challenges, and strategies in childhood obesity prevention in Ghana.
Study setting
The study was conducted in selected schools within the Oforikrom Municipality, Kumasi in the Ashanti Region of Ghana (between longitude 6.35°–6.40° and longitude 1.30°–1.35°). The municipality covers a land area of 54.1 km2 with a population of 303,016 people with a population density of 5,601 persons per km2. This urban municipality encompasses diverse educational institutions, providing a representative environment to study the role of teachers in managing childhood obesity. There are 24 public schools with 410 teachers in basic or primary and junior high schools under the Ghana Education Service in Oforikrom Municipal.
Study population and sampling
The target population is comprised of teachers in basic (lower primary, upper primary), and junior high schools within the municipality. The convenience sampling method was used to recruit participants due to time and logistical constraints, allowing the inclusion of teachers that were readily accessible. Teachers at these levels were deemed appropriate respondents due to their daily interactions with school-aged children and their potential role in childhood obesity prevention.
Inclusion and exclusion criteria
The study included teachers actively engaged in teaching at the time of data collection, as well as those who were willing to participate and thus provided informed consent. Teachers on leave or who were absent during the data collection period were excluded from the study.
Sample size determination
A sample size of 74 teachers was used in this study. This size was obtained using a power-based approach to detect a 20% difference in the proportion of teachers participating in childhood obesity prevention initiatives based on awareness (40% for aware teachers vs. 20% for non-aware teachers). The calculation assumed a 95% confidence level (α = 0.05, two-sided test), 70% power (β = 0.30), and a standard normal approximation for proportions (20). The relatively lower power was chosen due to the limited population of available teachers and the exploratory nature of the study. Standard normal approximations for proportions were used and no design effect or continuity correction was applied (20).
Data collection
A structured questionnaire, which included both closed-ended and open-ended questions, was developed to obtain demographic details, awareness, and perceptions of childhood obesity. Data on institutional strategies toward prevention and challenges and facilitators to teachers’ participation in childhood obesity prevention were also collected (Supplementary File 1).
The demographic details captured included age, gender, educational level, teaching experience, and grade level taught. The second section assessed teachers’ awareness and perceptions of childhood obesity through items on familiarity with obesity and its causes, recognition of associated health risks (e.g., type 2 diabetes, hypertension, and psychological effects), and sources of information. The third section examined school-level systems and prevention strategies, with items assessing whether schools had policies on healthy eating, physical activity programs, healthy snack initiatives, or nutritional education activities. The final section explored barriers and facilitators to teachers’ participation in childhood obesity prevention and management, including items on challenges such as limited resources, lack of training, time constraints, and parental support. Enabling factors such as allocated time for health education, professional training, curriculum support, and collaboration with healthcare staff were also captured.
The questionnaires were self-administered by study participants in selected schools, with teachers spending about 30 min to complete them. Data were collected over a four-week period. Respondents were given sufficient time to complete the questionnaire, and all forms were completed on-site to ensure data integrity.
Ethics approval
Ethical approval (CHRPE/AP/983/24) for the study was obtained from the Committee for Human Research and Publication Ethics (CHRPE), at the Kwame Nkrumah University of Science and Technology (KNUST).
Questionnaire validity and reliability
Reliability analysis was conducted to assess the internal consistency of the items in the questionnaire using Cronbach’s alpha. The calculated Cronbach’s alpha was 0.83, suggesting questionnaire reliability in consistently assessing the study objectives.
Data management and analysis
Data were cleaned and managed using Microsoft Excel 2019 and analyzed using R programming statistical software (R 4.4.1), at a significance level set at p < 0.05 and a confidence level set at 95%. Descriptive statistics such as frequencies and percentages were used to summarize the distribution of study variables. Inferential statistics, such as the chi-square test or Fischer’s exact test, were employed to examine associations between demographic and other teacher characteristics and their participation toward the prevention and management of childhood obesity in schools. Univariable and multivariate binary logistic regression analyses were also utilized to identify the independent predictors that influence teacher’s participation to prevent and manage childhood obesity.
Results
Sociodemographic characteristics of study participants
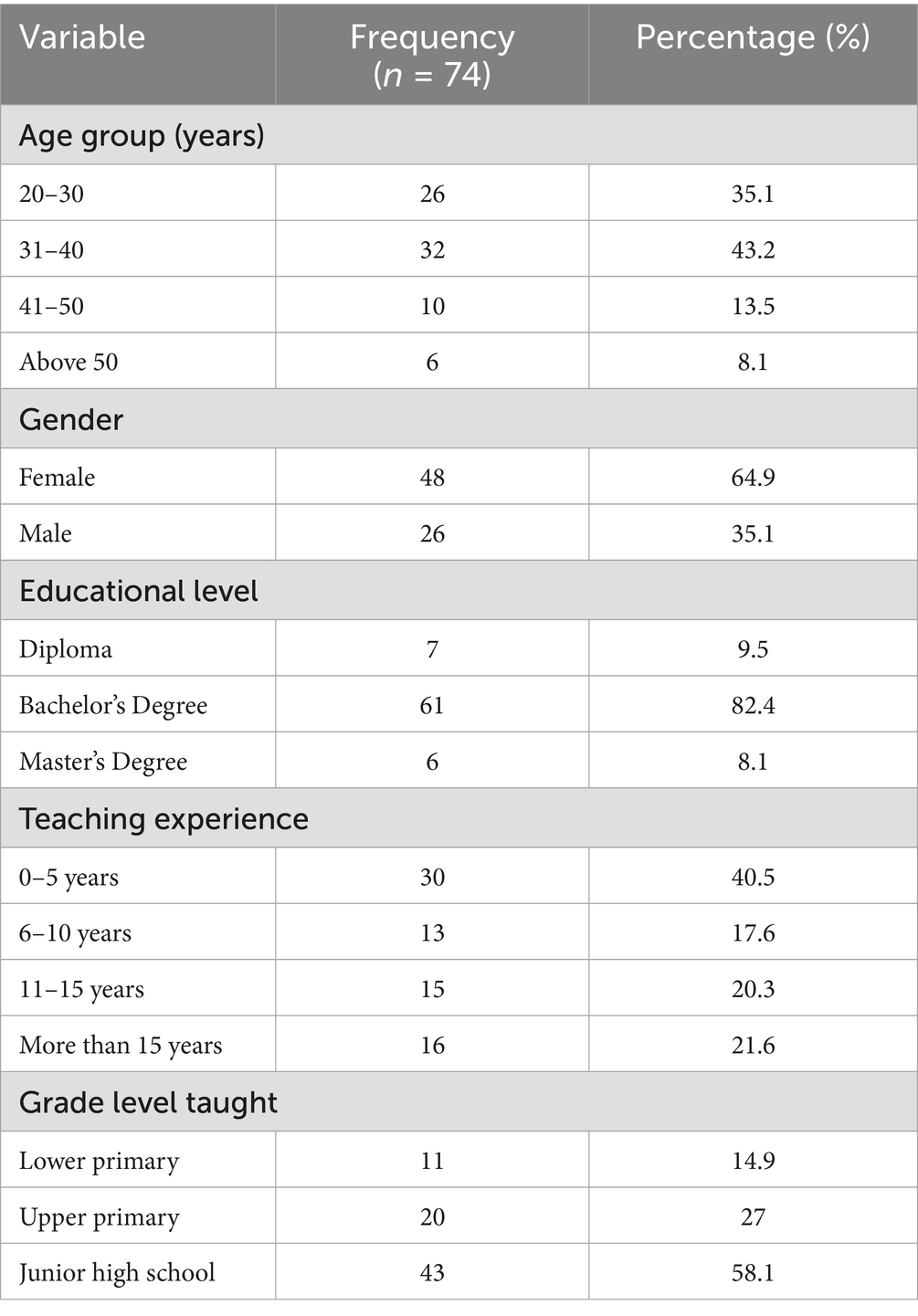
The socio-demographic characteristics of the 74 teachers involved in the study are summarized in Table 1. Many participants were aged between 31 and 40 years (43.2%), followed by those aged 20–30 years (35.1%). Females made up most of participants (64.9%), while males accounted for 35.1%. The vast majority of participants (82.4%) held a bachelor’s degree, while 9.5% had a Diploma, and 8.1% had attained a master’s degree. A substantial proportion (40.5%) had 0–5 years of teaching experience. Participants with 6–10 years of experience accounted for 17.6%, 11–15 years for 20.3%, and those with more than 15 years made up 21.6%. Most participants (58.1%) taught at the Junior High School level, followed by Upper Primary (27.0%) and Lower Primary (14.9%) (Table 1).
Level of awareness of childhood obesity among teachers
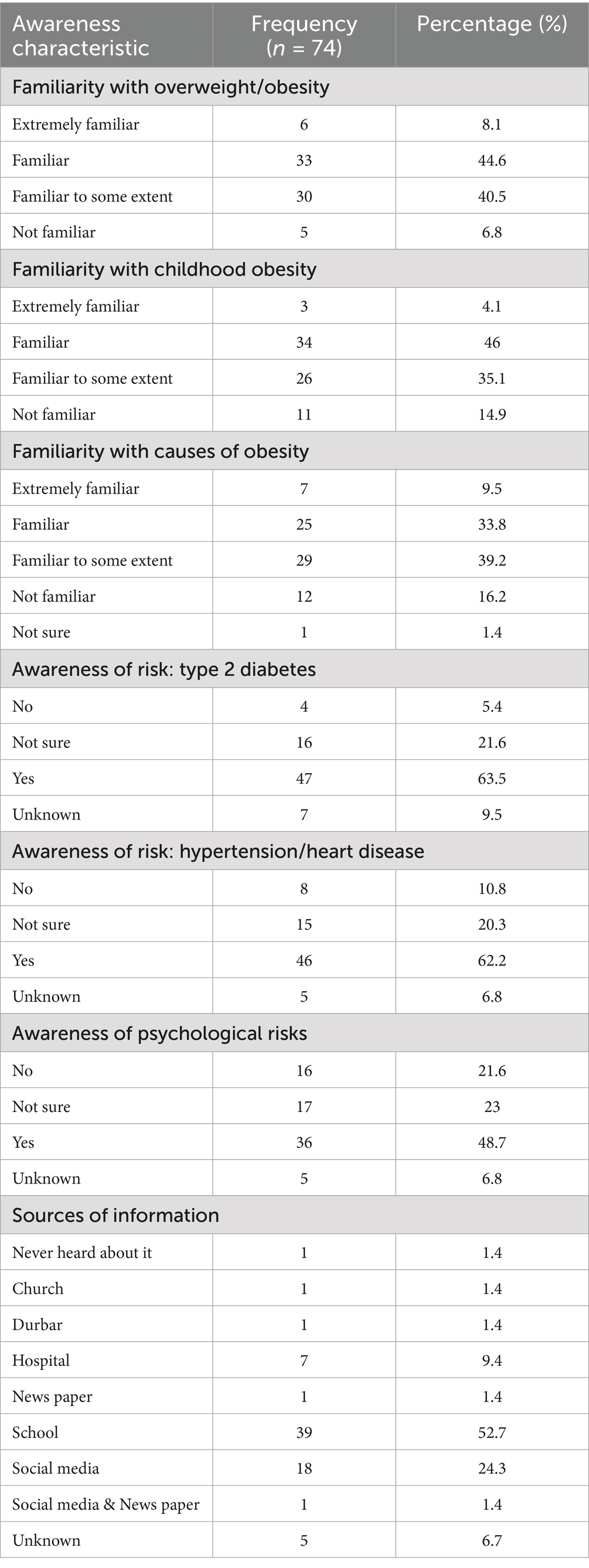
Findings on teachers’ awareness of childhood obesity, associated health risks, and sources of information are presented in Table 2. Most teachers reported being familiar with being overweight and obesity, with 44.6% indicating they were “familiar” and 40.5% “familiar to some extent.” Similarly, 46% were “familiar” with childhood obesity, although 14.9% reported no familiarity. Awareness of the causes of obesity was generally moderate, with 39.2% “familiar to some extent” and 33.8% “familiar,” while 16.2% were not familiar and 1.4% were unsure. Regarding associated health risks, 63.5% recognized type 2 diabetes as a potential consequence of childhood obesity, while 62.2% identified hypertension or heart disease. Awareness of psychological risks was relatively lower, with 48.7% acknowledging this association. The most common source of information on childhood obesity was the school setting (52.7%), followed by social media (24.3%), while few cited hospitals, community gatherings, or print media (Table 2).
Perceptions of childhood obesity as a public health issue
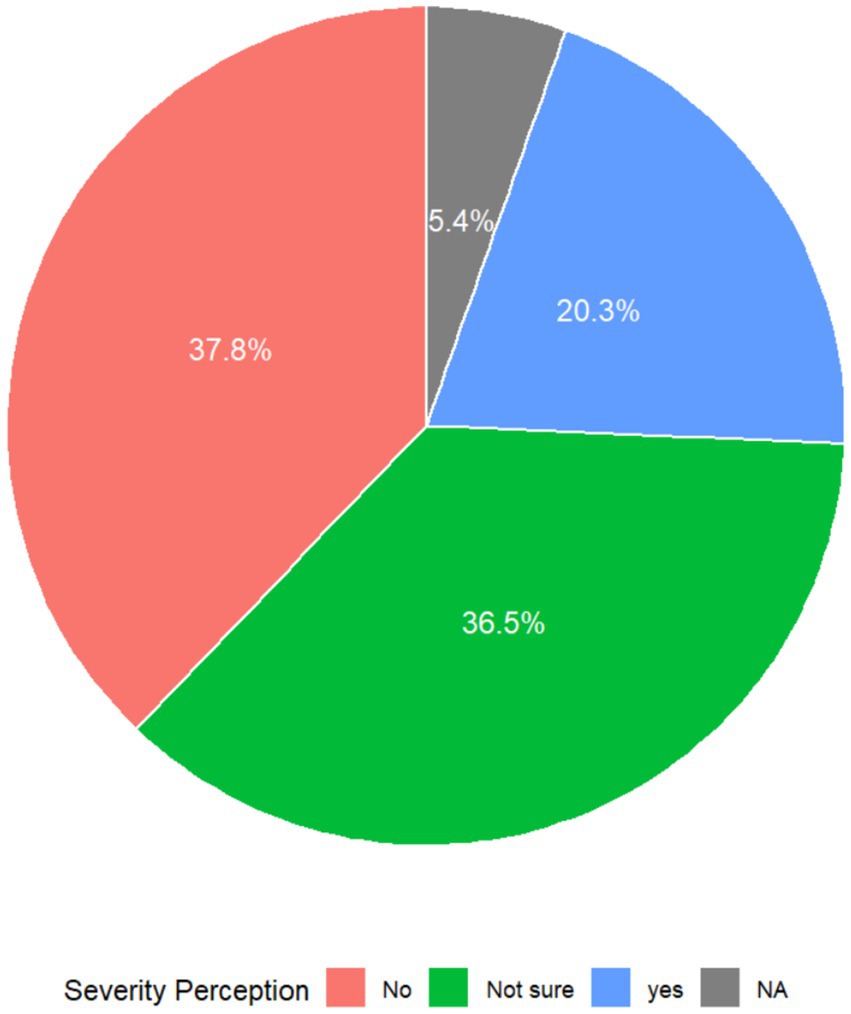
Respondents’ perceptions regarding childhood obesity as a public health issue are illustrated in Figure 1. About 37.8% of the respondents did recognize childhood obesity as a public health issue while 36.5% were unsure. Only 20.3% of respondents recognized childhood obesity as a public health concern, highlighting a minority that indicates potential health risks and societal impact (Figure 1).
Institutional systems and strategies
The institutional systems and strategies implemented in schools to address childhood obesity among school-aged children are summarized in Table 3. The presence of school policies promoting healthy eating and physical activity was limited, with 67.6% of participants indicating the absence of such policies. Few teachers reported having these policies (14.9%), while 17.6% were unsure about their existence. Over half (54.1%) of the participants indicated that their schools lacked initiatives that were targeted at addressing childhood obesity, and 20.3% were uncertain about their implementation. Only a quarter (25.6%) of participants acknowledged having these initiatives in place. Physical activity programs were available in all participating schools, with 73.0% reporting the presence of such programs. However, 16.2% reported that such programs were not implemented in their schools, and 10.8% were unsure about their availability. Healthy diets programs were reported to be present by 60.8% of teachers. However, 18.9% of participants reported the absence of healthy diet programs in their schools (Table 3).
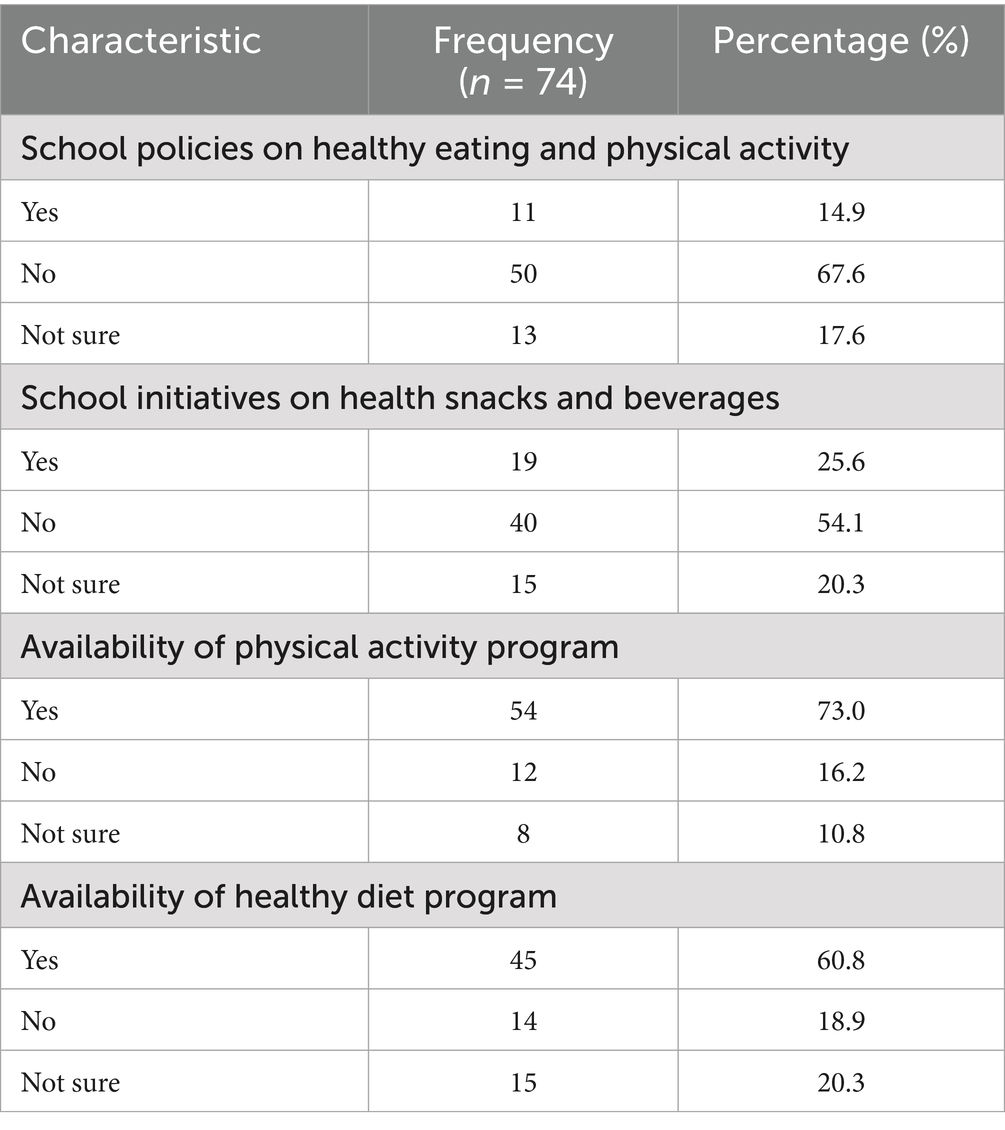
Table 3. Institutional systems and strategies for preventing and managing childhood obesity in schools.
Types of preventive measures available in schools
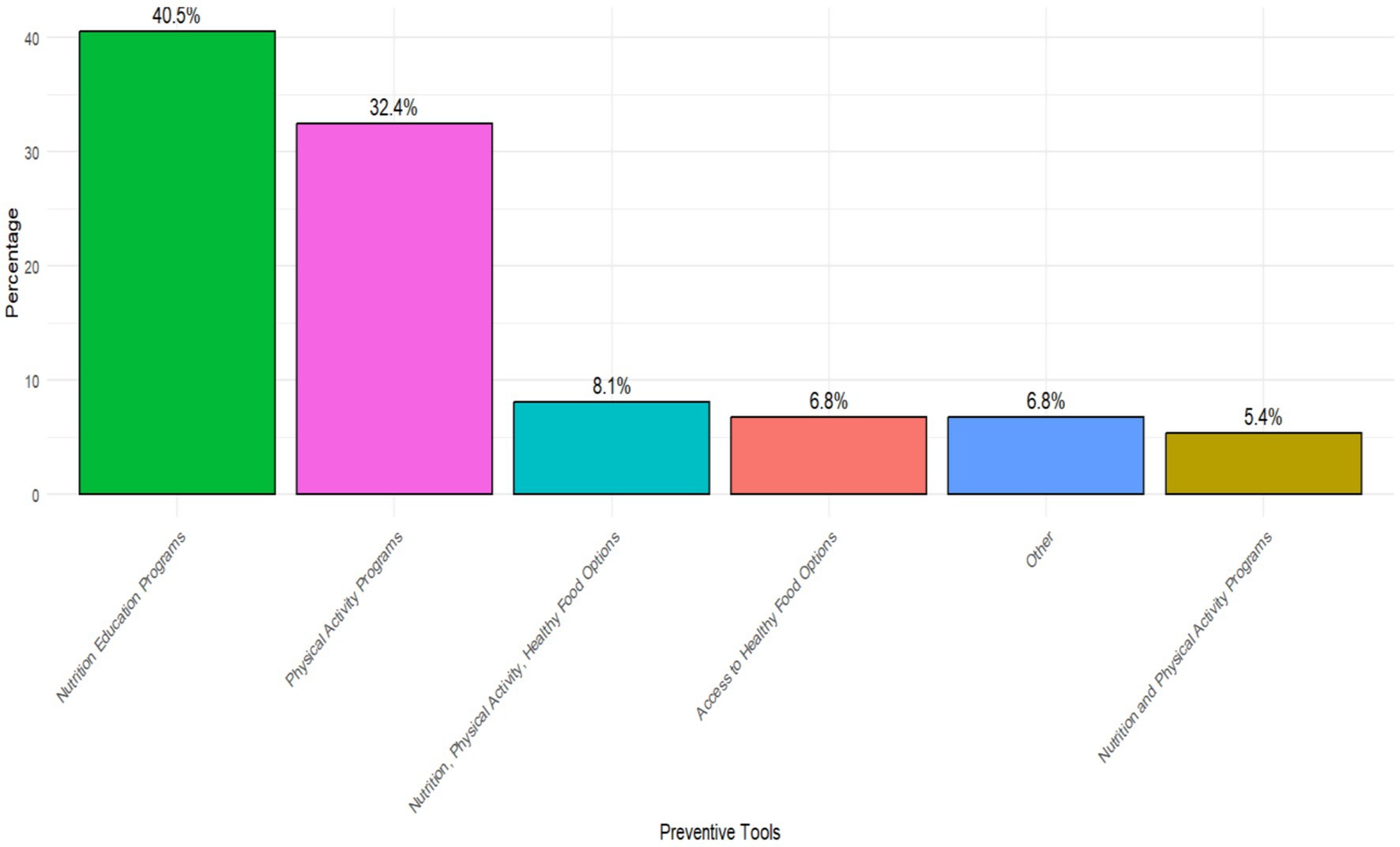
The study identified various preventive measures implemented in schools to address childhood obesity (Figure 2). Nutritional education programs were the most frequently reported measure, implemented by 40.5% of participants with physical activity programs accounting for 32.4%. Nutrition, physical activity, and healthy food options, as a comprehensive approach combining multiple strategies, were reported by 8.1% of participants. 6.8% of teachers reported that efforts were made to provide nutritious food alternatives within the school environment. An integrated approach combining nutrition and physical activity programs was implemented in 5.4% of schools. Miscellaneous measures, reported by 6.8% of teachers, included less conventional or unspecified interventions (Figure 2).
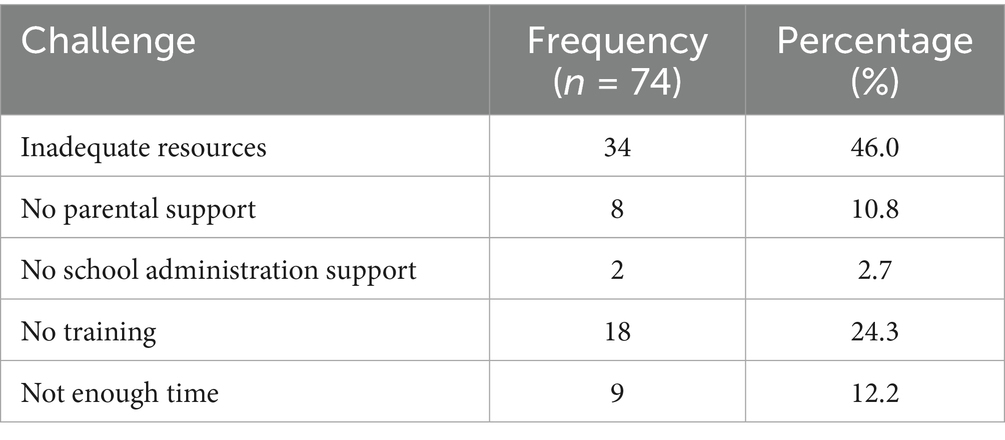
Hindrances and facilitators to teachers’ participation in prevention and management of childhood obesity
The key factors that hindered teachers’ participation in the prevention and management of childhood obesity are presented in Table 4. Inadequate resources emerged as the most common barrier, reported by 46% of respondents. A lack of training was also notable, cited by 24.3% of teachers, while 12.2% indicated insufficient time as a constraint. Additionally, 10.8% reported a lack of parental support, and 2.7% pointed out limited support from school administration (Table 4).
Factors facilitating teachers’ participation in prevention and management of childhood obesity
The various factors that facilitated teachers’ involvement in addressing childhood obesity prevention and management are summarized in Figure 3. Overall, relatively fewer teachers reported the existence of facilitators. The most frequently reported facilitator was having adequate time allocated for health education and physical activity, with only 27.0 and 21.6% of teachers identifying these as key enabling factors, respectively. Professional training was identified by 14.9% of teachers as a critical facilitator, with a smaller proportion of teachers (12.2%) emphasizing the importance of having access to structured teaching curricula. Other facilitators included parental participation (10.8%), working with healthcare workers (5.41%), and support from the school administration (1.35%) (Figure 3).
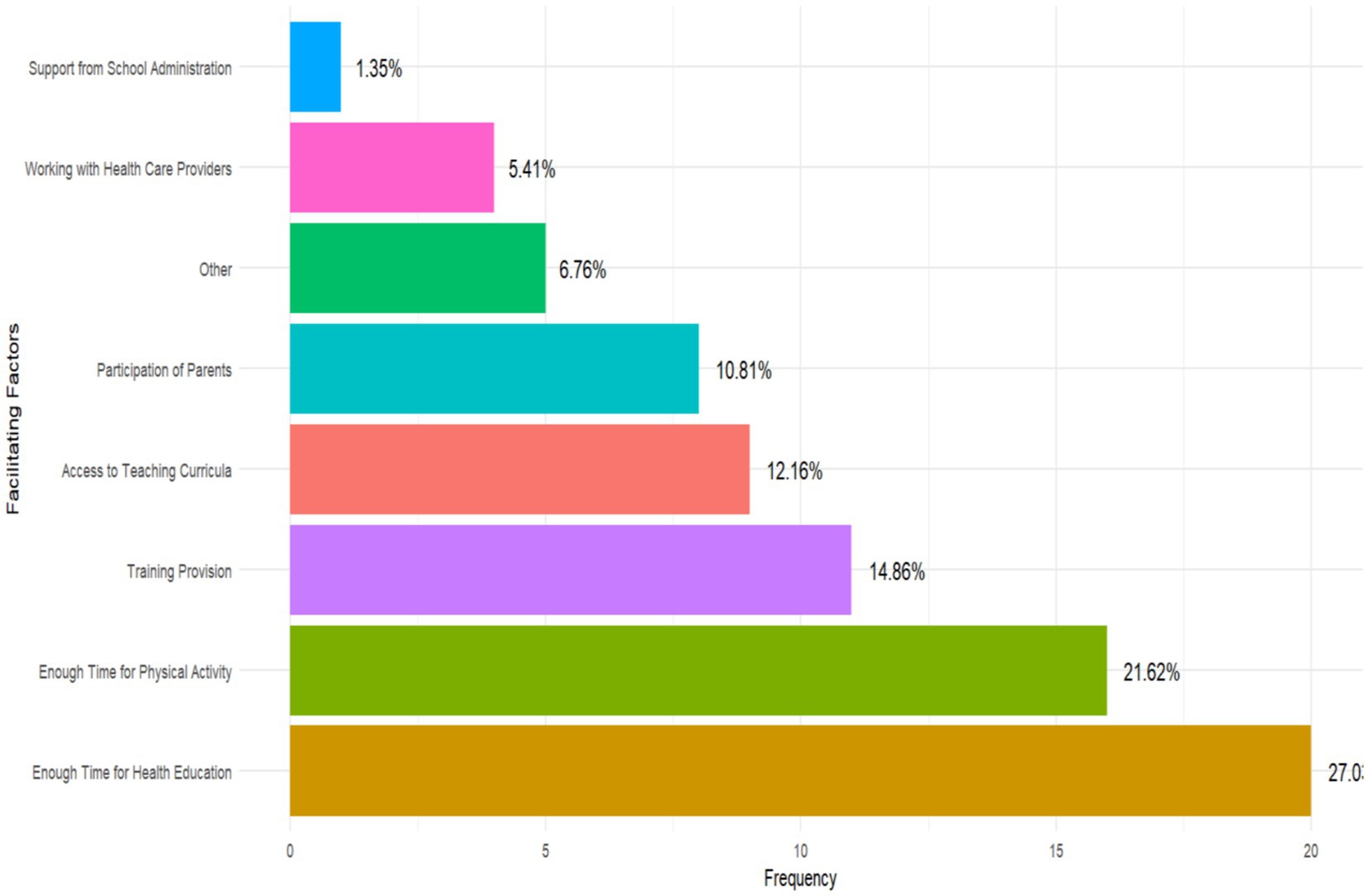
Figure 3. Factors facilitating teachers’ participation in prevention and management of childhood obesity.
Association between teacher characteristics, challenges and type of prevention practice and participation in childhood obesity prevention
A chi-square analysis examining the factors associated with teachers’ participation in the prevention and management of childhood obesity is presented in Table 5. Awareness status, age group, gender, educational level, and perception of healthy eating were not significantly associated with participation (p > 0.050). However, teachers’ socioeconomic conditions were significantly associated (p = 0.016), with a higher proportion of participants reporting no socioeconomic influence (39%) compared to non-participants (5.6%).
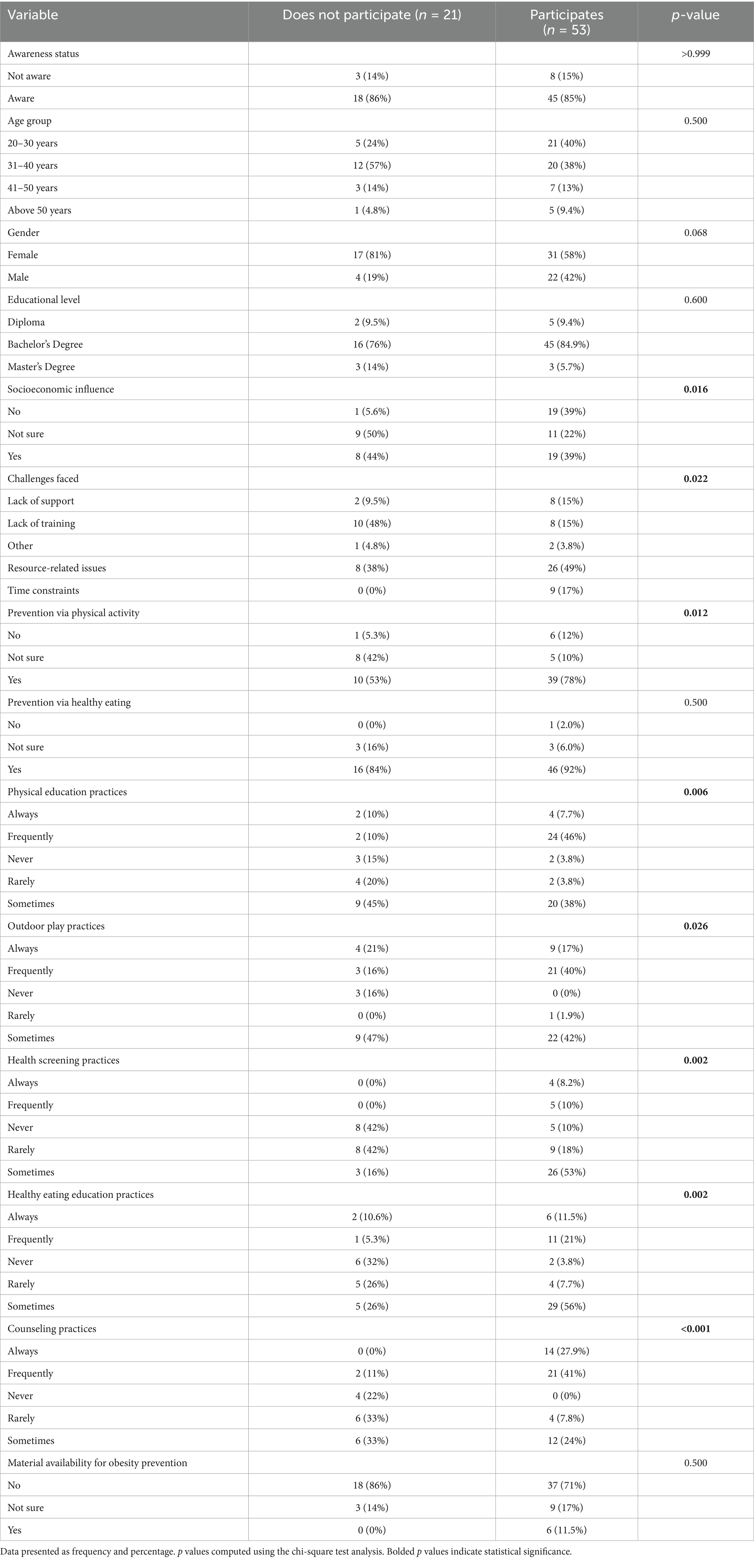
Table 5. Association between teachers’ characteristics, challenges and prevention practices with participation in obesity prevention programs.
Significant associations were also observed between participation and several challenges, including lack of training, time constraints, and resource-related issues (p = 0.022). Perceptions of physical activity as a preventive strategy were significantly associated with participation (p = 0.012), with 78% of participants endorsing it compared to 53% of non-participants. Similarly, physical education practices (p = 0.006), outdoor play (p = 0.026), health screening (p = 0.002), healthy eating education (p = 0.002), and counseling practices (p < 0.001) showed significant associations with participation. No significant association was found between the availability of obesity prevention materials and participation (p = 0.500) (Table 5).
Predictors for teachers participation in childhood obesity prevention programs
The univariable and multivariable logistic regression analyses of predictors for participation in childhood obesity prevention programs is illustrated in Table 6. At the univariable level, teachers who were unsure about the influence of their socioeconomic conditions were significantly less likely to participate (cOR = 0.06, 95% CI: 0.01–0.58, p = 0.014), though this association was not significant after adjustment (aOR = 0.10, 95% CI: 0.00–1.28, p = 0.100). A similar trend was observed among those uncertain about the role of physical activity (cOR = 0.10, p = 0.064; aOR = 0.05, p = 0.150). Frequent engagement in physical education and healthy eating practices was associated with higher odds of participation, but none reached statistical significance in the adjusted models. Overall, no predictors remained statistically significant after adjusting for cofounding factors (Table 6).
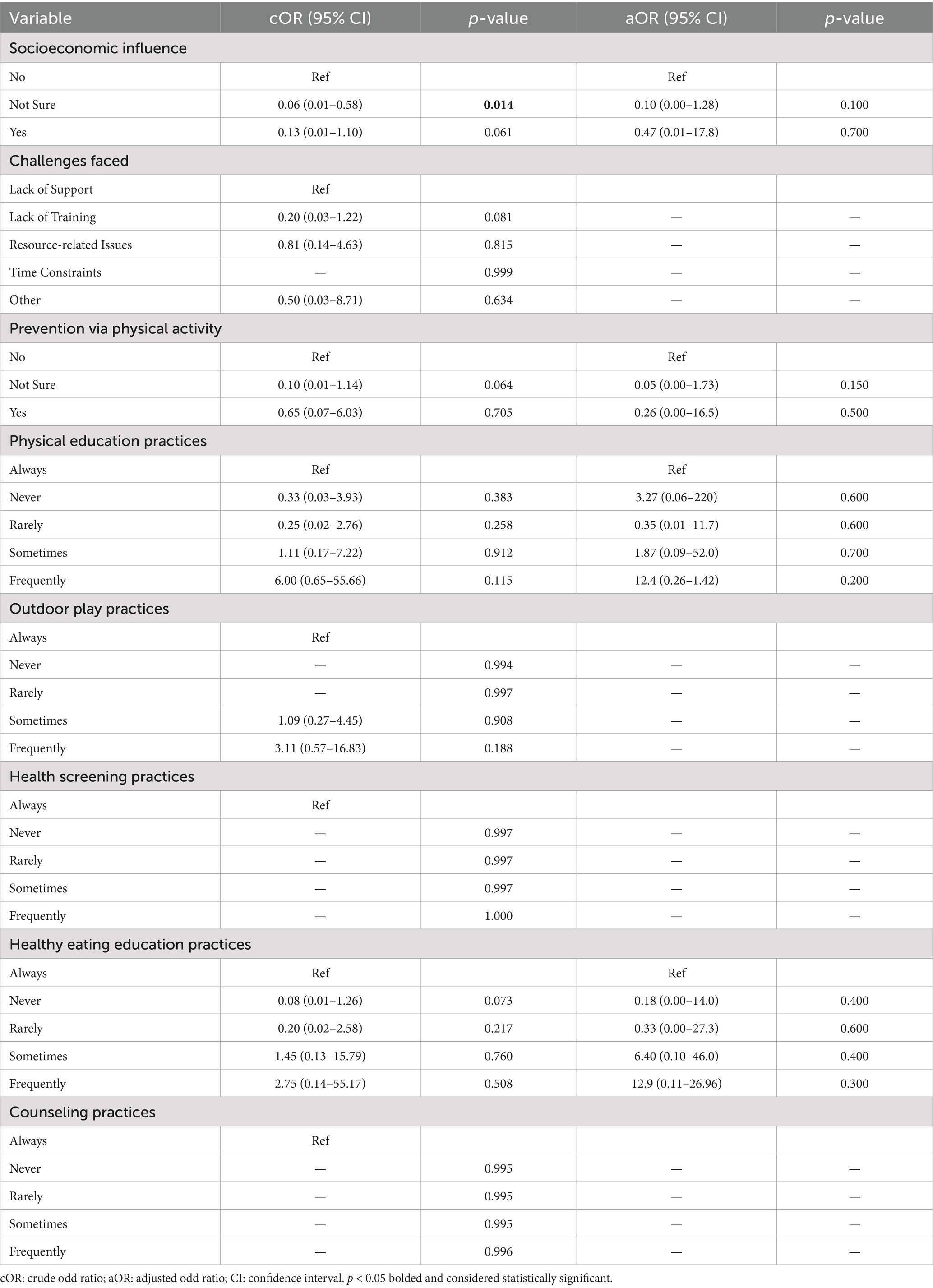
Table 6. Univariable and multivariable logistic regression analysis of statistically significant predictors for participation in childhood obesity prevention programs.
Discussion
The increase in childhood obesity worldwide has emerged as a critical public health issue. School-based programs have long been central to childhood obesity prevention, with efforts focused on promoting physical activity, providing nutrient-dense food options, and offering nutrition education. Schools provide a unique setting for health promotion, as they have direct access to children during their formative years, where lifelong habits are established. Teachers are thus pivotal in integrating nutrition education into the curriculum, promoting physical activity, and fostering a supportive school environment. However, limited research exists in Ghana on teachers’ actual participation and the factors influencing their engagement in school-based obesity prevention efforts. This study assessed the role of teachers in the prevention and management of childhood obesity among school aged children in Kumasi, Ghana.
The findings indicate that teachers generally possessed a high level of familiarity with childhood obesity, its related health risks and causes. Additionally, there was significant awareness of the health risks related to childhood obesity, specifically type 2 diabetes, hypertension, and heart disease among the teachers. These findings align with prior research indicating that teachers recognize these risks, potentially influenced by media campaigns and public health communications. The lower awareness of the psychological risks associated with obesity (52%) indicated a knowledge gap that future training programs for teachers should address (21). The psychological effects, among which are low self-esteem, depression, and stigmatization, are commonly not emphasized in public discussions, but these contribute significantly to the overall development of a child. Addressing this gap might better enable teachers to provide students with holistic support and advocate for more comprehensive school-based health efforts (22).
A notable percentage of respondents (37.8%) did not perceive childhood obesity as a public health concern, while 36.5% expressed uncertainty. This ambiguity in perception underscores a possible deficiency in comprehending the gravity of childhood obesity as a public health concern. The minimal number (20.3%) of respondents identifying it as a significant concern may be associated with widespread underappreciation of the long-term ramifications of pediatric obesity, including an elevated risk for chronic diseases (23). The results are troubling, indicating that many teachers lack comprehensive awareness of the overall public health challenges of childhood obesity, potentially obstructing effective prevention initiatives in schools. There is therefore the need for more focused initiatives designed to alter teachers’ attitudes toward juvenile obesity as a critical health problem. Training workshops, curriculum enhancements, and collaboration with health professionals could play a crucial role in shaping more informed attitudes and encouraging proactive involvement. The failure to acknowledge pediatric obesity as a public health concern is not exclusive to Ghana; similar trends have been noted in other LMICs, where health education frequently lacks emphasis in the curriculum (24–26). This is indicative of a global institutional issue where rampant communicable diseases in LMICs are often prioritized over the growing non-communicable health challenges such as childhood obesity. Moreover, non-communicable diseases (NCDs) are often associated with adults and the people over 65, despite their increasing prevalence in children, which contributes to missed opportunities for prevention and control among younger populations (27). Addressing this gap will require national policy changes to make health promotion a central core element of educational systems.
The research revealed that institutional frameworks and strategies for the prevention and management of childhood obesity in schools were inadequate. Most participants indicated that their schools did not have policies to encourage healthy food and physical activity. These findings reflect widespread concerns over the absence of comprehensive, school-wide health measures to address childhood obesity (28, 29). The limited occurrence of efforts advocating healthy snacks and physical activity programs emphasize the necessity for more institutional support for obesity prevention. These findings are similar to reports from other studies conducted in other African schools, where resources and institutional support for obesity prevention are often insufficient (30). Schools without policies and programs to address childhood obesity may be fostering an environment in which unhealthy habits are acceptable among youngsters. Bastida et al. (31) assert that comprehensive school health programs are essential for modifying children’s behaviors and enhancing their overall health outcomes. The availability of physical activity programs, even if not universally implemented, suggests that there is potential for schools to incorporate more structured and comprehensive obesity prevention measures into their daily routines.
The current study also identified major obstacles encountered by teachers in the prevention and management of childhood obesity including the lack of resources, unavailability of training, and insufficient time. These constraints correspond with prior research in other contexts that emphasize structural challenges, such as insufficient resources and training, as significant impediments to teachers’ successful participation in health promotion initiatives (30, 32). This is unsurprising, considering that school-based policies and programs have not been widely implemented in low-and middle-income countries and therefore the required resources and training that would be part of such programs are not adequately provided. The data clearly indicates the necessity for professional development and organized programs for teachers to improve their understanding and ability to address childhood obesity. Providing adequate time for health education and physical activity, together with professional training, were considered essential facilitators for teachers’ involvement in obesity prevention initiatives. This indicates that, given appropriate assistance and resources, teachers are prepared and capable of supporting the prevention and treatment of childhood obesity within educational institutions. However, parents’ involvement cannot be underestimated, as dietary and lifestyle modifications have been shown to reduce childhood obesity. Teachers’ knowledge and parents’ involvement are therefore key facilitators to the prevention and management of childhood obesity.
Teachers’ awareness status, along with various factors such as social economic influence, types of challenges faced by teachers, physical education practices, health screening practices, healthy eating education practices, and counseling practices, demonstrated statistically significant relationships with the prevention and management of childhood obesity. These associations suggest that both knowledge and practical implementation of health-promoting strategies are key components influencing teachers’ engagement in obesity-related initiatives. Conversely, age, gender, and educational level were found to be statistically non-significant, indicating that demographic characteristics may play a limited role in influencing teachers’ participation in such programs. As such, all teachers have the potential to lead such prevention and management measures. Subsequently, a lack of statistically significant predictors of teachers’ participation in childhood obesity prevention programs highlights the complexity of engaging teachers in these initiatives, as numerous factors may influence participation without achieving the desired threshold for statistical significance (33). Teachers who regularly participated in health education or physical activity programs demonstrated a higher likelihood of involvement, suggesting the influence of continuous engagement with health-related curricula and physical education initiatives.
Strengths, limitations and future directions
This study provides key findings into the role of teachers in preventing and managing childhood obesity, offering insights that are valuable for both individual and institutional stakeholders. However, these insights are tempered by a number of limitations. The study is limited to a single municipality and public schools in an urban area, which constrains the applicability of its findings to other districts, rural areas, or private schools, limiting the study’s generalizability and reducing the relevance for broader policy or program design. The convenience sampling technique employed may have introduced a risk of selection bias, which may also limit the generalizability of the findings to the broader population. Overlapping predictors, such as physical activity and healthy eating education, may obscure independent effects due to their interrelated nature, resulting in non-significant results in the adjusted logistic regression model. Additionally, measurement errors from self-reported data may have introduced bias, weakening associations. Moreover, contextual barriers, including socioeconomic challenges, lack of training, and resource limitations, may have overshadowed individual predictors, highlighting the need for larger, more robust studies with objective measures and context-specific analyses to further strengthen these findings.
Future research should include multiple districts encompassing both urban and rural settings across the country, as well as private and public schools to enhance the generalizability of findings and provide more comprehensive evidence to guide national policy and program development. Additionally, longitudinal and intervention-based research could evaluate the effectiveness of teacher-led obesity prevention programs, while examining the impact of comprehensive training, parental engagement, and policy implementation on children’s long-term health and behavioral outcomes.
Conclusion
Teachers showed general awareness of childhood obesity but limited understanding of its public health impact. Gender disparities, inadequate institutional support, and resource constraints hinder effective engagement. Findings also revealed deficiencies in school policies, low access to preventive programs, and inadequate training, stressing the necessity to strengthen both education and healthcare systems in Ghana. Targeted teacher training, adequate institutional support, and stronger school-community collaborations should be prioritized to enhance teachers’ effectiveness in the prevention and management of childhood obesity in Ghana. The study offers actionable recommendations to policymakers, educators, and school administrators, highlighting the critical role of incorporating structured health curricula, increasing opportunities for physical exercise, and partnering with healthcare professionals to sustain childhood obesity prevention efforts.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval (CHRPE/AP/983/24) for the study was obtained from the Committee for Human Research and Publication Ethics (CHRPE), at the Kwame Nkrumah University of Science and Technology (KNUST). Informed consent was obtained from all participants, confirming their voluntary participation. Anonymity and confidentiality were ensured throughout the study.
Author contributions
CK: Writing – original draft, Formal analysis, Software, Visualization, Methodology, Investigation, Validation, Writing – review & editing, Data curation, Conceptualization. NT: Conceptualization, Supervision, Writing – review & editing, Project administration, Visualization, Validation. PA: Visualization, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by funding from Mastercard Foundation Africa Higher Health Education Collaborative.
Acknowledgments
The authors are grateful to all teachers and selected schools for their time, willingness to participate and contributions to the successful implementation of the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1724617/full#supplementary-material
References
1. Bray, GA, Kim, K-K, Wilding, JP, and Federation, WO. Obesity: a chronic relapsing progressive disease process. A position statement of the world obesity Federation. Obes Rev. (2017) 18:715–23. doi: 10.1111/obr.12551
2. Mohajan, D, and Mohajan, HK. Obesity and its related diseases: a new escalating alarming in global health. J Innov Med Res. (2023) 2:12–23. doi: 10.56397/JIMR/2023.03.04
3. Flegal, KM, Kit, BK, and Graubard, BI. Body mass index categories in observational studies of weight and risk of death. Am J Epidemiol. (2014) 180:288–96. doi: 10.1093/aje/kwu111
4. Lobstein, T, Jackson-Leach, R, Powis, J, Brinsden, H, and Gray, M. World obesity atlas 2023. (2023). London: World Obesity Federation.
5. Ward, ZJ, Bleich, SN, Cradock, AL, Barrett, JL, Giles, CM, Flax, C, et al. Projected US state-level prevalence of adult obesity and severe obesity. N Engl J Med. (2019) 381:2440–50. doi: 10.1056/NEJMsa1909301
6. Bovet, P, Farpour-Lambert, N, Banatvala, N, and Baur, L. Obesity: burden, epidemiology and priority interventions In: Editors N. Banatvala, P. Bovet Noncommunicable diseases. London, UK: Routledge (2023). 74–82.
7. Mosha, T, and Fungo, S. Prevalence of overweight and obesity among children aged 6-12 years in Dodoma and Kinondoni municipalities, Tanzania. Tanzan J Health Res. (2010) 12:6–16. doi: 10.4314/thrb.v12i1.56202
8. Amissah, I, and Amoako-Boateng, M. Prevalence of diabetes mellitus complications among people with type 2 diabetes mellitus attending a teaching hospital in Ghana: a clinical audit. Int J Sci Res. (2014) 3:2104–9. doi: 10.21275/v5i6.21061602
9. Whyte, N. S., Amissah, A. A., and Mensah, J. Strategies for managing childhood obesity in primary schools in the Cape Coast Metropolis of Ghana Asian J Contemp. Educ. Karachi, Pakistan (2020).
10. Obirikorang, C, Anto, E, Ngala, R, and Gyamfi, E. The prevalence of childhood obesity and lifestyle-associated risk factors using anthropometric measurements among primary schools in the Kumasi metropolis, Ghana. Innovative J Med Health Sci. (2015) 4:13–23.
11. Konkor, I, and Kuuire, VZ. Epidemiologic transition and the double burden of disease in Ghana: what do we know at the neighborhood level? PLoS One. (2023) 18:e0281639. doi: 10.1371/journal.pone.0281639
12. Shetty, P. Nutrition transition and its health outcomes. Indian J Pediatrics. (2013) 80:21–7. doi: 10.1007/s12098-013-0971-5
13. Verstraeten, R, Roberfroid, D, Lachat, C, Leroy, JL, Holdsworth, M, Maes, L, et al. Effectiveness of preventive school-based obesity interventions in low-and middle-income countries: a systematic review. Am J Clin Nutr. (2012) 96:415–38. doi: 10.3945/ajcn.112.035378
14. Martínez-López, E, Pérez-Guerrero, EE, Torres-Carrillo, NM, López-Quintero, A, Betancourt-Núñez, A, and Gutiérrez-Hurtado, IA. Methodological aspects in randomized clinical trials of nutritional interventions. Nutrients. (2022) 14:2365. doi: 10.3390/nu14122365
15. Nga, VT, Dung, VNT, Chu, D-T, Tien, NLB, Van Thanh, V, Ngoc, VTN, et al. School education and childhood obesity: a systemic review. Diabetes Metab Syndr Clin Res Rev. (2019) 13:2495–501. doi: 10.1016/j.dsx.2019.07.014
16. Lee, A, Lo, ASC, Keung, MW, Kwong, CMA, and Wong, KK. Effective health promoting school for better health of children and adolescents: indicators for success. BMC Public Health. (2019) 19:1–12. doi: 10.1186/s12889-019-7425-6
17. Snelling, A, Hawkins, M, McClave, R, and Irvine Belson, S. The role of teachers in addressing childhood obesity: a school-based approach. Nutrients. (2023) 15:3981. doi: 10.3390/nu15183981
18. Adu-Mireku, S. Schools and health: a district-level evaluation of school health education in Ghana. Children. (2003) 18:105–20. doi: 10.4314/jsda.v18i2.23828
19. Adomako Gyasi, P, Zhou, L, Chen, Z, Numawoseh, E, and Opoku-Agyemang, A. Barriers to school-based health programs implementation in basic schools in Ghana: education stakeholders’ perspective. Health Educ Res. (2024) 39:55–67. doi: 10.1093/her/cyad045
20. Fleiss, JL, Levin, B, and Paik, MC. Statistical methods for rates and proportions. Hoboken, NJ, USA: john wiley & sons (2013).
21. Pulgarón, ER. Childhood obesity: a review of increased risk for physical and psychological comorbidities. Clin Ther. (2013) 35:A18–32. doi: 10.1016/j.clinthera.2012.12.014
22. Cavioni, V, Grazzani, I, and Ornaghi, V. 2020. Mental health promotion in schools: a comprehensive theoretical framework. Msida, Malta: International Journal of Emotional Education.
23. Coupe, N, Peters, S, Ayres, M, Clabon, K, Reilly, A, and Chisholm, A. Educators’ experiences and perspectives of child weight discussions with parents in primary school settings. BMC Public Health. (2022) 22:808. doi: 10.1186/s12889-022-13210-z
24. Ali, SA, Ali, SA, Suhail, N, Tikmani, SS, and Bano, G. Childhood obesity, a public health crisis: narrative review of public health interventions for childhood obesity. J Universal Surgery. (2016) 4:1
25. Baggio, MA, Alves, KR, Cavalheiro, RF, Matias, L, Hirano, AR, Machineski, GG, et al. Childhood obesity in the perception of children, families and health and education professionals. Texto & Contexto-Enfermagem. (2021) 30:e20190331. doi: 10.1590/1980-265x-tce-2019-0331
26. Suiraoka, IP, Duarsa, DPP, Wirawan, IDN, and Bakta, IM. Perception of parents, teachers, and nutritionist on childhood obesity and barriers to healthy behavior: a phenomenological study. Int J Health Sci. (2017) 1:1–11. doi: 10.21744/ijhs.v1i2.25
27. Akseer, N, Mehta, S, Wigle, J, Chera, R, Brickman, Z, Al-Gashm, S, et al. Non-communicable diseases among adolescents: current status, determinants, interventions and policies. BMC Public Health. (2020) 20:1–20. doi: 10.1186/s12889-020-09988-5
28. Akowuah, PK, and Kobia-Acquah, E. Childhood obesity and overweight in Ghana: a systematic review and Meta-analysis. J Nut Metabol. (2020) 2020:1–11. doi: 10.1155/2020/1907416
29. Wang, Y, Cai, L, Wu, Y, Wilson, R, Weston, C, Fawole, O, et al. What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes Rev. (2015) 16:547–65. doi: 10.1111/obr.12277
30. Adom, T, De Villiers, A, Puoane, T, and Kengne, AP. School-based interventions targeting nutrition and physical activity, and body weight status of African children: a systematic review. Nutrients. (2019) 12:95. doi: 10.3390/nu12010095
31. Bastida, L, Cea, G, Moya, A, Gallego, A, Gaeta, E, Sillaurren, S, et al. Promoting obesity prevention and healthy habits in childhood: the OCARIoT experience. IEEE J Trans Eng Health Med. (2023) 11:261–70. doi: 10.1109/JTEHM.2023.3261899
32. Saleh, M, Ba-Break, M, and Abahussin, A. Barriers and facilitators of school-based obesity prevention interventions: a qualitative study from the perspectives of primary school headteachers. J Health Popul Nutr. (2024) 43:217. doi: 10.1186/s41043-024-00713-1
33. Ganle, JK, Boakye, PP, and Baatiema, L. Childhood obesity in urban Ghana: evidence from a cross-sectional survey of in-school children aged 5–16 years. BMC Public Health. (2019) 19:1–12. doi: 10.1186/s12889-019-7898-3
Abbreviations
NCDs, Non-Communicable Diseases; WHO, World Health Organization; LMICs, Low- and middle-income countries; GES, Ghana Education Service; SHEP, School Health Education Programme.
Keywords: childhood obesity, school-based interventions, teachers, public health, Ghana
Citation: Kayitesi C, Tagoe N and Acheampong PR (2025) The role of teachers in the prevention and management of childhood obesity among school-aged children in Ghana: a cross-sectional study. Front. Public Health. 13:1724617. doi: 10.3389/fpubh.2025.1724617
Edited by:
Souhail Hermassi, Qatar University, QatarReviewed by:
Ferman Konukman, Qatar University, QatarAmani Alhazmi, King Khalid University, Saudi Arabia
Bela Jozsef Balla, University of Babeș-Bolyai, Romania
Copyright © 2025 Kayitesi, Tagoe and Acheampong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chantal Kayitesi, a2F5aXRlc2ljMzQ4QGdtYWlsLmNvbQ==
 Chantal Kayitesi
Chantal Kayitesi Nadia Tagoe
Nadia Tagoe Princess Ruhama Acheampong
Princess Ruhama Acheampong