- 1Department of Nutritional Sciences, The Pennsylvania State University, University Park, PA, United States
- 2Department of Statistics, The Pennsylvania State University, University Park, PA, United States
- 3Department of Biobehavioral Health, The Pennsylvania State University, University Park, PA, United States
- 4Department of Nutrition Science, Purdue University, West Lafayette, IN, United States
Food insecurity (FI) is a dynamic phenomenon, and its association with daily affect is unknown. We explored the association between daily FI and affect among low-income adults during a 2-seasonal-month period that covered days both pre- and during the COVID-19 pandemic. A total of 29 healthy low-income adults were recruited during fall in 2019 or 2020, 25 of whom were followed in winter in 2020 or 2021. Daily FI (measured once daily) and affect (measured 5 times daily) were collected over the 2nd−4th week in each month. Time-Varying-Effect-Models were used to estimate the association between daily FI and positive/negative affect (PA/NA). Overall, 902 person-days of daily-level data were collected. Daily FI was associated with lower PA in the 3rd and 4th week of fall and winter and with higher NA in the second half of winter months. Similar patterns of FI-affect relations were found pre- and during COVID-19 in the second half of a given month, while unique patterns of positive affect scores in the 2nd week and negative scores in the 1st week were only observed during COVID days. Our study supports a time-varying association between FI and affect in low-income adults. Future large studies are needed to verify the findings; ultimately, better understanding such associations may help identify, target, and intervene in food insecure adults to prevent adverse mental health outcomes.
Introduction
Food insecurity is defined as having limited access to adequate food for active, healthy living due to lack of money and other resources, and it disproportionally affects vulnerable populations, including low-income households (1). In 2019, the prevalence of food insecurity in households with income < 185% of the federal poverty line (FPL) was nearly three times higher (27.6%) than the national average (10.5%) (1). During the COVID-19 pandemic, the prevalence of food insecurity increased dramatically to 44% in low-income adults (2). Low-income populations were more susceptible because pandemic lockdown, quarantine, and isolation measures lead to additional financial stress, loss of employment, and incapability to access sufficient food sources in low-income households, with additional anxiety and depression resulting from these stressors (3, 4).
Food insecurity is associated with a wide range of chronic conditions, including diabetes, obesity, cardiovascular diseases, and poor neurocognitive function (5–10). Rather than being static, food insecurity is believed to be a dynamic process that potentially follows a cyclical pattern. Fluctuations in food expenditure and dietary intake over the course of a given month have been observed in low-income adults (11, 12), households (13, 14) and communities (15). Changes in food insecurity by season are also possibly profound in low-income households, where other essential living expenses, such as heating costs in winter, may stress the limited resources for access to healthy foods (16) and create the seasonal “heat-or-eat” dilemma during winter times when heating costs compete with food costs (17).
In addition to its direct impact on diet, food insecurity is associated with increased adverse mental health outcomes (18). The directionality and mechanisms of the food insecurity-mental health relationship, however, are unclear. Prior longitudinal studies suggested a bidirectional association linking food insecurity measures (e.g., food insecurity experience over the past 12 months) and measures of mental health (primarily focused on depression and stress) (19, 20). Affective tendencies, such as positive or negative affect, can be determined by assessing and aggregating emotional states or people's recollections of their feelings, and can be used to predict a variety of health-behaviors and health outcomes (21–24). Affective reactivity to minor stressful events in daily life has received increasingly more attention because it can be an indicator of vulnerability vs. resilience; that is, the way people react emotionally to daily stressors may be indicative of long-term health and wellbeing (25, 26). Among the low-income population who are at higher risk of food insecurity, the ways in which daily food insecurity relates to everyday affect, and specifically, how the cyclical nature of food insecurity is associated with emotional wellbeing at different times in a given month, and in different times of the year, has not been extensively explored.
Ecological momentary assessment (EMA), using repeated collection of real-time data in subjects' natural living environments, is a useful tool for collecting dynamic data. Compared to the commonly used retrospective reporting, the concurrent behaviors and experience captured by EMA are believed to minimize recall bias and maximize ecological validity (27, 28). EMA has been widely used to assess human dietary intake (29) and affect (30). Using the EMA design on smartphones, we piloted a study designed to track daily food insecurity, dietary intake, and positive and negative affect in everyday life. Our aims were to study: (1) how food insecurity status within a given month in two seasons was associated with affect in predominantly rural, low-income adults on a daily basis; and (2) how the COVID pandemic may modify the association between daily food insecurity and affect. We hypothesized that food insecurity is associated with increased negative affect and decreased positive affect, and that the associations would be more evident in the 4th week than the 2nd week, in the winter than the fall season, and during the pandemic compared to pre-pandemic.
Materials and Methods
Subjects and Settings
The Food ‘N Mood study is a pilot study conducted in central Pennsylvania between September 2019 and March 2021. Participants were recruited via study flyers from selected communities and locations serving low-income populations, such as Women, Infants and Children (WIC) offices, county assistance offices, food banks, food pantries, and Head-Start childcare services. The inclusion criteria were healthy adults aged 20–50 years and household income below the 185% of the Federal Poverty Line (FPL). The exclusion criteria were adults who were Non-English-speaking, had diagnosed physical, mental or emotional disabilities, who had disabled family members in the household, and those who reported taking medications known to affect heart rate. Women who were pregnant or menopausal were also excluded. Data collection occurred at participants' homes over two 3-week-long waves (between the 2nd and 4th week), covering one fall month (September, October, or November) in 2019 or 2020, and one winter month (February or March) in 2020 or 2021. Data on food insecurity status and affective wellbeing were collected through an EMA framework on provided smartphones. Participants responded to 8 or 9 survey modules on a daily basis, including a morning survey (n = 1), notified surveys (n = 5), an evening survey (n = 1), and food records (Sunday, Monday, and Tuesday of each survey week). A written consent has been obtained from participants enrolled during in-person procedures. During the COVID-19 pandemic, a verbal consent form was filled out during virtual recruitment procedures and an electronic consent form was sent to participants for their records. Participants were provided with up to $140 cash compensation if they completed data collection in both fall and winter season. The study protocol was approved by the National Center for Advancing Translational Sciences (NCATS) and The Pennsylvania State University Institutional Review Board, University Park, Pennsylvania.
Daily Food Insecurity
Individual level food insecurity status was assessed using an adapted 6-item U.S. Adult Food Security Survey Module given our research interest in adult food insecurity and participants' affect (31). Each day, participants were asked whether or not they had any experience of food insecurity in the past 24 h. The experiences included: “worrying about food running out”, “could not afford to eat balanced meals”, “cutting meal size or skipping a meal because there wasn't enough money for food”, “eating less because there wasn't enough money for food”, “was hungry but did not eat because there wasn't enough money for food” and “did not eat for a whole day because there wasn't enough money for food”. In our study, the mean Cronbach's alpha for the continuous daily food insecurity score, calculated from the sum of the six questions, was 0.37. Given the low alpha value, we chose to generate a binary food insecurity status variable to indicate whether or not the adults experienced any food insecure situations (coded as “1” if participants experienced one or more of these food insecure situations; or “0” if participants did not affirm any of the food insecure experiences). As a set of sensitivity analyses, we applied the continuous food insecurity score in the analysis; results are presented in Supplementary Material.
Daily Affect
Momentary mood/affective states were assessed via an 11-item questionnaire, using items drawn from the Profile of Mood States (32), Positive and Negative Affect Schedule (33), and the modified Differential Emotions Scale (34) to incorporate items reflecting both activated and deactivated positive affect and negative affect. Positive affect was assessed with five items (happy, hopeful, excited, calm, and proud), and negative affect was assessed with six items (tense/anxious, lonely, annoyed, embarrassed, depressed, and tired). The smartphone randomly beeped around five anchor time points with survey reminders, and the participants were asked to rate their mood at the moment on a slider scale that ranged from “not at all” to “extremely” (and which equated to a 0–10 scale). These surveys were considered complete if all of the 11 items were rated. Daily positive and negative affect scores were calculated by computing means of the completed ratings within the same survey day of each participant. Following methods described by Cranford et al. (35), we calculated the reliability for within-person change for positive and negative affect. Both positive and negative affect showed good reliability (Rc = 0.98 for both affect measures).
Demographic and Socioeconomic Characteristics
A background survey was administered at enrollment to collect demographic, health and socioeconomic characteristics of participants, including age, gender, race and ethnicity, relationship status, weight, height, education, employment status, household size, number of children under 18 years in the household, total annual household income, and enrollment in food assistance programs. In addition to the main measure of daily food insecurity, we also measured household food insecurity over the past 12 month as part of the socioeconomic module, using the U.S. Adult Food Security Survey Module (31). Body mass index (BMI) was calculated as self-reported weight (kg)/height2 (m2). Poverty status was categorized per the Department of Health and Human Services' definition that considers the gross household income (<130% FPL or ≥130 and <185% FPL) and household size (36). To be able to examine whether findings were affected by the COVID-19 pandemic, we created a dummy code to differentiate between “pre-COVID-19 period” and “during COVID-19 period” based on whether data were collected before or after March 1, 2020.
Statistical Analysis
Time Varying Effect Models (TVEMs) (37, 38) were applied to estimate the association between daily food insecurity status and affect as a function of time. The TVEMs have no constraints on the shapes of coefficients and are free of model misspecification (39). TVEMs have been widely applied for estimating time-varying effects in human behavioral and health research (39–42). Because the coefficient functions for intercept terms were approximately constant (that is the population mean of positive and negative affect did not vary over the course of the month when the explanatory variables are set to be 0), we considered the TVEM model with fixed intercepts and with a coefficient function of daily food insecurity and time using the polynomial spline-based method (43–45). We set the degree of splines to be 3 and the number of knots to be 2 in our final model, which had the lowest Akaike Information Criterion (AIC) in comparison to alternative models. The “geeglm” function with correlation structure “ar1” in R was used to account for intrapersonal correlation of repeated measures in the affect measures. The specific model is described as the following:
Where yij is the expected daily affect (positive or negative) for subject i on day j; β0 is the fixed intercept (non-time varying) of daily affect; β1(tij) denotes the time-varying association between daily food insecurity and daily affect for subject i on day j. The 95% pointwise confidence interval for the adjusted β1(tij) was estimated across the 21 study days within a month to determine statistical significance. is the vector of parameters for covariates being adjusted in the model, including gender, race/ethnicity, employment, poverty status, and whether or not data collection occurred during COVID-19. These covariates were considered because of their known relationship to food insecurity and emotional health (46–48). γ is considered constant for different individuals over time. εij is the continuous error term that was not assumed to follow a normal distribution as suggested by previous work (41).
To examine the potential role of COVID-19 with the food-insecurity-affect associations, the observations of food insecurity and affect were stratified by data collection pre- or during the COVID-19 period, controlling for gender, race/ethnicity, employment, poverty status, and whether data were collected in fall or winter months in otherwise similar TVEMs.
Results
Overall, 29 participants were enrolled in the study. A sample of 28 participants were recruited in fall 2019/2020, of whom 25 participants were followed up in winter 2020/2021; one additional participant was recruited in winter 2020/2021. A total of 902 person-days (response rate = 78.1%) or an average of 30.1 days per participant of information on food insecurity and affect were collected. Table 1 presents the baseline demographic and socioeconomic characteristics of the 29 participants. The mean (SD) age of participants was 36.3 (7.1) years. The majority of adults enrolled were women (86.2%), White or Caucasian (69.0%), employed (72.4%), and had college or higher degrees (82.8%). Sixteen participants who were employed at baseline (n = 21) provided information about their payment schedule in the survey month, including two who were paid weekly, 8 who were paid bi-monthly, and 6 who were paid monthly. About half of the participants were married or living with partners (48.3%). Sixteen (55.2%) participants lived below the 130% FPL and thirteen (44.8%) lived between 130 and 185% FPL.
The proportion of daily food insecurity reported by participants is presented in Figure 1. In the fall months, the proportion of participants with any daily food insecurity experience ranged from 36.8 to 64.0%. There were 8 days in which over half of the participants affirmed that at least one food insecurity situation occurred (Figure 1A). In the winter months, the proportion range was 25.0–52.6% and there were 3 days in which more than half of the participants reported experiencing at least one food insecurity situation (Figure 1B). We observed a higher proportion of daily food insecurity reported during the COVID pandemic than the pre-pandemic period. The daily proportion range was 26.7–56.5% and 37.5–64.3%, respectively, for the pre- and during COVID periods. The number of days during which half or more participants had any food insecurity situation increased from 2 days in a given month pre-COVID to 10 days in a given month during the COVID pandemic (Figures 1C,D).
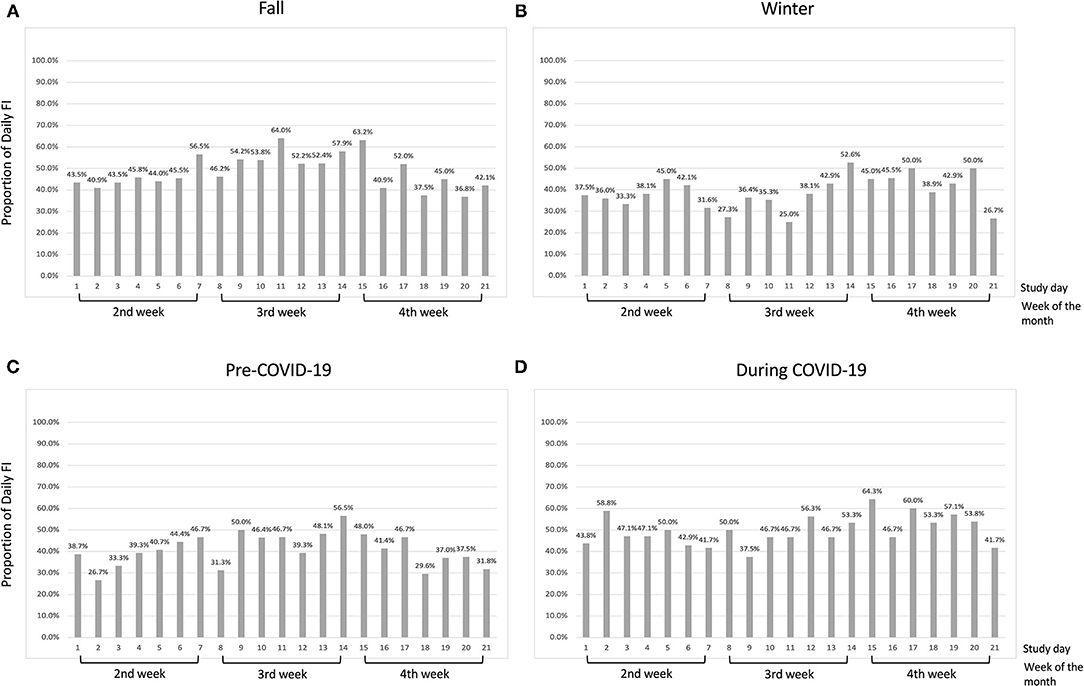
Figure 1. Proportion of daily food insecurity by study day in low-income participants (<185% of FPL) in (A) the fall months; (B) the winter months; (C) pre-COVID-19 period; and (D) during COVID-19 period.
As depicted in Figures 2, 3, daily positive and negative affect showed wide interpersonal variation each day. For positive affect, the median score was 23.0 in both fall and winter months (Figures 2A,B). The median score was 24.7 in the pre-COVID period and 17.3 during COVID (Figures 2C,D). For negative affect (Figure 3), the median for fall (Figure 3A), winter (Figure 3B), pre-COVID (Figure 3C) and COVID periods (Figure 3D) was 10.7, 10.6, 10.0, and 11.5, respectively. Out of the maximum reporting of 5 times per day, the average daily frequency of reporting was 3.4 for both positive and negative affect.
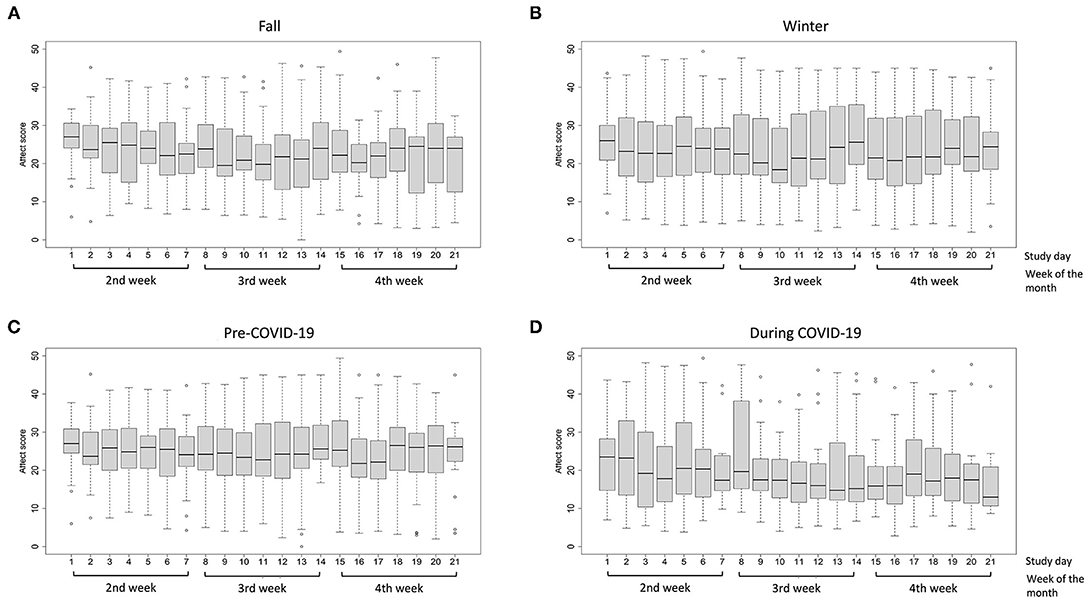
Figure 2. Distribution of positive affect scores in low-income participants (<185% of FPL) by study day (A) the fall months; (B) the winter months; (C) pre-COVID-19 period; and (D) during COVID-19 period. The boxplot indicates the minimum score (bottom line), 25th percentile (lower bound), median (middle bar), 75th percentile (upper bound), and maximum score (top line) of positive or negative affect on each study day. The circles below and above the boxplots indicate outliers.
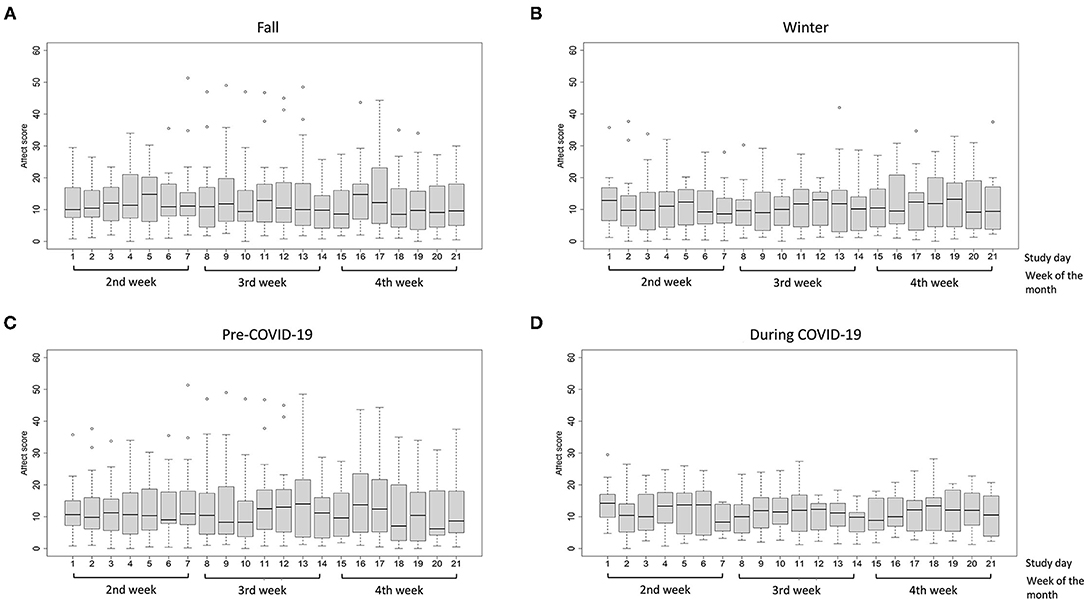
Figure 3. Distribution of negative affect scores in low-income participants (<185% of FPL) by study day (A) the fall months; (B) the winter months; (C) pre-COVID-19 period; and (D) during COVID-19 period. The boxplot indicates the minimum score (bottom line), 25th percentile (lower bound), median (middle bar), 75th percentile (upper bound), and maximum score (top line) of positive or negative affect on each study day. The circles below and above the boxplots indicate outliers.
The adjusted relationships were controlled for gender, race/ethnicity, employment, poverty status, and whether or not data assessment occurred during the COVID-19 pandemic. In the fall months, daily food insecurity was associated with lower positive affect scores between study days 10–21 and significant associations were seen between study days 13–17 (the end of the 3rd week and the beginning of the 4th week, beta-coefficient ranged from −2.37 to −1.83) and study days 20–21 (the end of the 4th week, beta-coefficient was −2.81 and −4.44, respectively) (Figure 4A). Experiencing daily food insecurity was significantly associated with lower positive affect scores and the coefficients decreased between study day 13–15, and slightly increased in study day 16–17. In the winter months, a similar negative association was observed for positive affect between study days 9–20 and the significant association was observed during study days 10–18 (most of the 3rd week and 4th week of the month, beta-coefficient ranged from −3.15 to −0.86) (Figure 4B). The coefficients decreased between study day 10–15 and slightly increased between study day 16–18. Contrary to the results observed for positive affect, there was no association between daily food insecurity and negative affect in the fall months (Figure 5A). Daily food insecurity was significantly associated with higher negative affect scores in the winter months during study days 8–17 (3rd and most of the 4th week of the month, beta-coefficient ranged from 1.53 to 2.39), where the coefficients increased first in study day 8–12, and then decreased in study day 13–on study day 17 (Figure 5B).
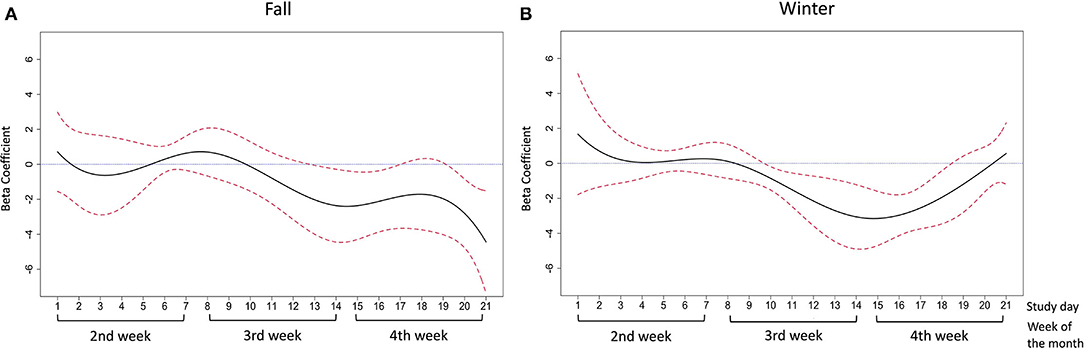
Figure 4. The association between daily food insecurity status and positive affect in (A) the fall months; (B) the winter months. The time-varying effect models were adjusted for gender, race/ethnicity, employment, poverty status, and data collection pre- or during covid-19. The solid line in black represents the estimated coefficients between daily food insecurity status and positive affect. The dashed lines in red are the pointwise 95% confidence intervals. The dotted blue line at zero represents null association between daily food insecurity and affective wellbeing.
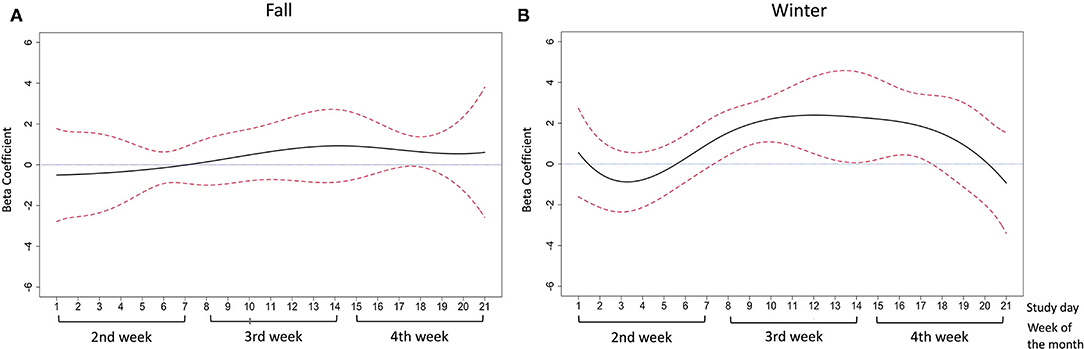
Figure 5. The association between daily food insecurity status and negative affect in (A) fall months; (B) winter months. The solid line in black represents the estimated coefficients between daily food insecurity status and negative affect. The dashed lines in red are the pointwise 95% confidence intervals. The dotted blue line at zero represents null association between daily food insecurity and affective wellbeing.
The adjusted associations between daily food insecurity status and affect pre- and during the COVID-19 pandemic are presented by study day in Figure 6 for positive affect and Figure 7 for negative affect. The detailed estimates are presented in Supplementary Tables 3, 4.
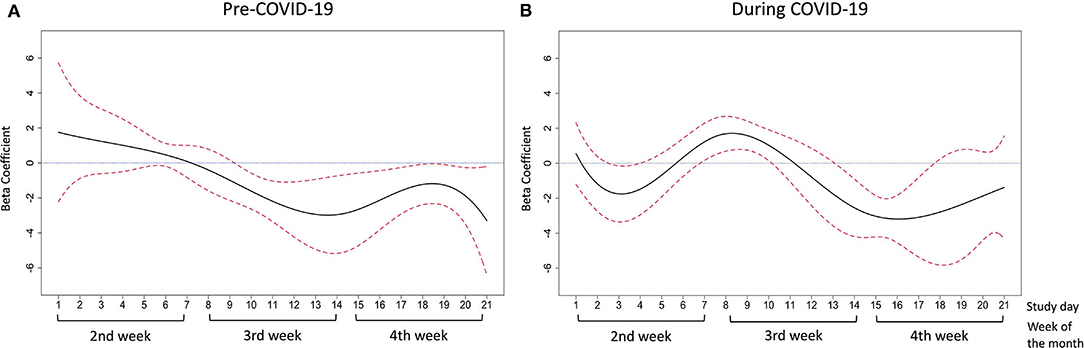
Figure 6. The association between daily food insecurity status and positive affect (A) in pre-COVID-19 days; (B) during COVID-19 days. The time-varying effect models were adjusted for gender, race/ethnicity, employment, poverty status, and season. The solid line in black represents the estimated coefficients between daily food insecurity status and positive affect. The dashed lines in red are the pointwise 95% confidence intervals. The dotted blue line at zero represents null association between daily food insecurity and affective wellbeing.

Figure 7. The association between daily food insecurity status and negative affect (A) in pre-COVID-19 days; (B) during COVID-19 days. The time-varying effect models were adjusted for gender, race/ethnicity, employment, poverty status, and season. The solid line in black represents the estimated coefficients between daily food insecurity status and negative affect. The dashed lines in red are the pointwise 95% confidence intervals. The dotted blue line at zero represents null association between daily food insecurity and affective wellbeing.
Prior to the COVID-19 pandemic, daily food insecurity was significantly associated with lower positive affect scores between study days 10–21 (the middle of the 3rd week to the end of the 4th week of the month, beta-coefficient ranged from −3.30 to −1.23) (Figure 6A). A decreasing trend of coefficients was observed between study day 10–14. Between study day 15–21, the coefficients increased first then deceased. During the COVID-19 pandemic, daily food insecurity was significantly associated with lower positive affect scores between study day 3–4 (the middle of the 2nd week of the month, beta-coefficient was −1.78 and −1.48, respectively) and study day 14–17 (the end of the 3rd week and the 4th week of the month, beta-coefficient ranged from −3.19 to −2.55) (Figure 6B). From study days 7–10 (the last day of the 1st week and the beginning of the 2nd week), experiencing food insecurity was associated with increased positive affect (beta-coefficients ranged between 1.03 and 1.69).
For negative affect in pre-pandemic days, daily food insecurity was significantly associated with higher negative affect scores from study day 10–13 and to study day 16 (most of the 3rd week of the month, beta-coefficient ranged 1.54–2.48) (Figure 7A). The coefficient increased between study day 5–13, and showed a decreasing trend afterwards until study day 21 (Figure 7A). During the pandemic, daily food insecurity was significantly associated with higher negative affect from study day 16–20 (most of the 4th week of the month, beta-coefficient ranged 1.38–1.94) (Figure 7B). However, during study days 1–4 (the first half of the 2nd week in the month), we also observed lower negative affect scores associated with daily food insecurity (beta-coefficient ranged −1.86 to −1.27; Figure 7B). Overall, the beta-coefficient for negative affect generally increased from day 2–20.
Using the continuous daily food insecurity, instead of the dichotomous daily food insecurity status, we found similar and robust results from similarly constructed TVEMs (Supplementary Figures 5, 6).
Discussion
In this pilot study, we measured daily food insecurity and affect among 29 low-income adults, 25 of whom were tracked for two 21-day periods over two seasons. We identified a time-varying association of daily food insecurity with daily affect within a given month. Regardless of season and whether the data were collected pre- or during the COVID-19 pandemic, we have observed a generally consistent association between daily food insecurity and lower positive affect and higher negative affect in the second half of a given month. Using intensive longitudinal data and an EMA design, our study was the first to track day-to-day food insecurity stressors and affect and demonstrate how low-income adults' affect fluctuates with food insecurity experiences in daily life. Given that prior research has focused more on chronic food insecurity in relation to mental health outcomes, findings from this study are novel and may suggest that psychological vulnerability to minor, possibly transient, stressors related to food insecurity are time-varying within a given month and across different times of the year.
Daily negative and positive affect were associated with daily food insecurity in certain weeks of the months. Both positive and negative affective reactivity to same-day stressful events, along with one's affective variability over time, seem to have independent health implications (49–53). Our study findings suggest that food insecurity may affect health in ways outside of diet-dependent pathways, with affect perhaps serving as an important mechanism in what has been termed the “cycle of food insecurity and chronic disease” model (54). However, caution is needed when interpreting our data, because the directionality of the associations cannot be confirmed and stress-related biomarkers were not incorporated in the present work. More research is needed to test the hypothesis that food insecurity affects physical health and to determine mechanisms of this potential relationship.
Although we did not see an increasing pattern of reported daily food insecurity over week (Figure 1), we did observe that the food insecurity-affect relationship became stronger in the expected direction in the latter half of the week (Figures 4–7). This phenomenon may be partially explained by the anticipated cycle of arrival and depletion of income/ benefits within a given month and the coping strategies available to “make ends meet”. Low-income adults may face higher economic strain near the end of the month if they get most of their income at the beginning or on the last day of the month. In addition, SNAP benefits in Pennsylvania are distributed to eligible low-income households within the first 10 days of each month (55). SNAP benefits are usually spent quickly within the first few days after receipt (13, 14), leaving the rest of the month less likely to be supported by SNAP benefits. In exploratory analyses to test how payment cycle may modify the relationship, we grouped people by whether or not they received money in the 4th week and observed decreased positive affect and increased negative affect in the 4th week among people who did not receive any payment in that week (n = 14). Similarly, for people who did receive payment in the 4th week (n = 8), similar decreased positive and increased negative affect scores were observed but were shifted to 1 week earlier (data not shown), suggesting the possibility that such individuals may have exhausted their resources by the week before the next payment. Because of the small sample size and missing data in payment cycle information, future studies are warranted to explore the role of payment cycle in the food insecurity and affect relationship.
In addition, low-income adults may have time-varying stress reactivity in response to food insecurity due to limited coping strategies in latter half of the months. Responsiveness to financial stress, characterized by both primary coping strategies (i.e., stressful situation management through problem solving, emotional expression, and emotion regulation) and secondary coping strategies (i.e., stressful situation adaptation through active acceptance, cognitive restructuring, distraction, and positive thinking) is related to how well low-income adults adapt to stress (56). Specifically, strategies for food budgeting that help stretch available food dollars, referred to as food management skills (57), were found to mitigate the impact of food insecurity in low-income adults and children (58–61). Coping with food insecurity using food management skills could be increasingly challenging when food dollars become limited at the end of the month. While low-income people may be able to secure food, they may have to sacrifice other critical resources in doing so, such as cost-related medication needs (62), in ways that may directly or indirectly influence their mental wellbeing. Findings are consistent with the possibility that food insecurity contributes to changes in affect. However, causality cannot be determined from the present research. It is possible that additional factors may have contributed to the observed time-varying relationships. For example, other stressors may be associated with both food insecurity and affect.
The COVID-19 pandemic appears to have modified the association between daily food insecurity and affect. While the associations in the pre-pandemic period largely mimicked what we saw in the fall and winter, some of the ups and downs in affect were in the unexpected direction during the COVID-19 pandemic. We do not fully understand why participants who reported having daily food insecurity experience appeared to feel more “hopeful” than their food-secure peers during the COVID-19 pandemic. This may be due to the additional COVID-19 relief benefits that they were eligible to receive or that they had already received. Unfortunately, we do not have the data necessary to verify this hypothesis. However, experiencing food insecurity was associated with increasingly worst affect in the 3rd and 4th week of the months, confirming the second half of the months as the most vulnerable time regardless of whether it was pre- or during the pandemic period.
Our study has several limitations. The small sample size prevented us from conducting an analysis by food security level or by subject characteristics. Participants tended to skip a few notified surveys within a day; however, the majority of participants (25/30 or 83.3%) completed at least 1 affect survey on each study day and the mean daily frequency was more than three times. The pandemic may have influenced patterns in the association between food insecurity and affect, although the pandemic indicator included in all of our adjusted models was not statistically significant. The findings by COVID-19 status revealed some different patterns when comparing the pre- and during the pandemic periods. The residual confounding may not be fully controlled for by adding whether or not data were collected before or after March 2020. For example, both food access and affect may have been impacted by the pandemic because of the change in self or family members' health conditions, employment status, income, and participation in food assistance programs and COVID-related financial assistance programs during the study period; however, our study did not collect these data, so we were not able to adjust for these factors. We did not assess every type of daily stressor that may contribute to affect variability. There may be unmeasured variables that account for the observed association. BMI data were missing in 9 (31%) of the participants, but sensitivity analysis with further adjustment of BMI revealed similar results (data not shown). Because of the potential residual confounding, our findings in this small pilot study should be interpreted with caution. Future observational studies with large sample size and detailed measures of daily stressors and behaviors are warranted to further explore the time-varying FI-affect associations. More than 80% of participants had a college degree or higher, which was much higher than the average in Pennsylvania (63). Although we followed the standard protocol strictly to screen for eligible low-income adults, potential for overreporting of educational attainment and/or underreporting of household income was possible. Future studies are needed to investigate the association between food insecurity and affect in low-income populations of lower educational attainment. The majority of the participants (86.7%) were female. Compared to males, females endure a higher burden of affect and stress related diseases (64). Our research findings, therefore, may not represent low-income adults as a whole. Lastly, our findings regarding seasonal differences may not be generalizable to other regions.
There are several strengths of the study to be recognized. Using an EMA model on smartphones, our study applied an intensive longitudinal design that assessed daily food insecurity status and multiple affective measures within a survey day, thus reducing measurement error and recall bias. Utilizing the USDA 6-item food insecurity module to assess the daily food insecure status was novel. Although further validation of the daily food insecurity measure is needed, data collected from the same pilot study suggested that daily food insecurity is associated with poor overall dietary quality (65), which provided some external validity of using the current daily FI indicator. The rigorous time-varying statistical models used in food insecurity research are a new extension and a strength. Albeit in a small sample, the overall trends of time-varying affect change in relation to daily food insecurity provide the first empirical evidence of the interplay between food insecurity and affect, and their potential association with the food insecurity cycle.
Conclusion
Food insecurity is prevalent among low-income adults and is associated with their day-to-day affective wellbeing. This pilot study provides empirical evidence of a time-varying association in the latter half of a month between daily food insecurity and positive mood in fall and winter months and between daily food insecurity and negative moods in winter months only. It also suggests that the COVID-19 pandemic may have influenced the associations between daily food insecurity and affect across the month. Larger observational studies are needed to further verify these preliminary findings. Such research holds promise to better identify at-risk populations and may eventually lead to more timely prevention and intervention efforts to minimize food insecurity and promote mental health in low-income populations.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the National Center for Advancing Translational Sciences (NCATS) and the Institutional Review Board of the Pennsylvania State University, University Park, Pennsylvania (Protocol code: STUDY00010715, Date of approval: 12/02/2018). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
MN, LF, JG-E, LM-K, and RL: conceptualization and methodology. MN: funding acquisition, project administration, and writing—original draft preparation. MN and ND: data collection and curation. ND, YL, and RL: formal analysis. MN, ND, YL, SJR, LF, JG-E, LM-K, and RL: writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
This project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1TR002014. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. MN's effort was also supported by the Broadhurst Career Development Professorship for the Study of Health Promotion and Disease Prevention, Penn State.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Naiwen Ji, Linna Shi, and Emma Louise Sharp for volunteering their time to help recruit participants.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.790519/full#supplementary-material
References
1. Coleman-Jensen A, Rabbitt MP, Gregory C, Singh A. Household Food Security in the United States in 2019. USDA Economic Research Service (2020).
2. Wolfson JA, Leung CW. Food Insecurity During COVID-19: an acute crisis with long-term health implications. Am J Public Health. (2020) 110:1763–5. doi: 10.2105/AJPH.2020.305953
3. Frasquilho D, Matos MG, Salonna F, Guerreiro D, Storti CC, Gaspar T, et al. Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health. (2015) 16:115. doi: 10.1186/s12889-016-2720-y
4. Fang D, Thomsen MR, Nayga RM. The association between food insecurity and mental health during the COVID-19 pandemic. BMC Public Health. (2021) 21:607. doi: 10.1186/s12889-021-10631-0
5. Gucciardi E, Vogt JA, Demelo M, Stewart DE. An exploration of the relationship between household food insecurity and diabetes mellitus in Canada. Diabetes Care. (2009) 32:2218–24. doi: 10.2337/dc09-0823
6. Eisenmann JC, Gundersen C, Lohman BJ, Garasky S, Stewart SD. Is food insecurity related to overweight and obesity in children and adolescents? A summary of studies, 1995–2009. Obes Rev. (2011) 12:e73–83. doi: 10.1111/j.1467-789X.2010.00820.x
7. Larson NI, Story MT. Food insecurity and weight status among US children and families: a review of the literature. Am J Prev Med. (2011) 40:166–73. doi: 10.1016/j.amepre.2010.10.028
8. Laraia BA. Food insecurity and chronic disease. Adv Nutr. (2013) 4:203–12. doi: 10.3945/an.112.003277
9. Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff. (2015) 34:1830–9. doi: 10.1377/hlthaff.2015.0645
10. Na M, Dou N, Ji N, Xie D, Huang J, Tucker KL, et al. Food insecurity and cognitive function in middle to older adulthood: a systematic review. Adv Nutr. (2019) 11:667–76. doi: 10.1093/advances/nmz122
11. Shapiro JM. Is there a daily discount rate? Evidence from the food stamp nutrition cycle. J Public Econ. (2005) 89:303–25. doi: 10.1016/j.jpubeco.2004.05.003
12. Tarasuk V, Mcintyre L, Li J. Low-income women's dietary intakes are sensitive to the depletion of household resources in one month. J Nutr. (2007) 137:1980–7. doi: 10.1093/jn/137.8.1980
13. Wilde PE, Andrews MS. The food stamp program in an era of welfare reform: Electronic benefits and changing sources of cash income. J Consumer Affairs. (2000) 34:31–46. doi: 10.1111/j.1745-6606.2000.tb00082.x
14. Wilde PE, Ranney CK. The monthly food stamp cycle: shooping frequency and food intake decisions in an endogenous switching regression framework. Am J Agric Econ. (2000) 82:200–13. doi: 10.1111/0002-9092.00016
15. Wycherley TP, Pekarsky BA, Ferguson MM, O'dea K, Brimblecombe JK. Fluctuations in money availability within an income cycle impacts diet quality of remote Indigenous Australians. Public Health Nutr. (2017) 20:1431–40. doi: 10.1017/S1368980016003360
16. Nord M, Kantor LS. Seasonal variation in food insecurity is associated with heating and cooling costs among low-income elderly Americans. J Nutr. (2006) 136:2939–44. doi: 10.1093/jn/136.11.2939
17. Bhattacharya J, Deleire T, Haider S, Currie J. Heat or eat? Cold-weather shocks and nutrition in poor American families. Am J Public Health. (2003) 93:1149–54. doi: 10.2105/AJPH.93.7.1149
18. Pourmotabbed A, Moradi S, Babaei A, Ghavami A, Mohammadi H, Jalili C, et al. Food insecurity and mental health: a systematic review and meta-analysis. Public Health Nutr. (2020) 23:1778–90. doi: 10.1017/S136898001900435X
19. Bruening M, Dinour LM, Chavez JBR. Food insecurity and emotional health in the USA: a systematic narrative review of longitudinal research. Public Health Nutr. (2017) 20:3200–8. doi: 10.1017/S1368980017002221
20. Dou N, Xie D, Gao X, Palacios N, Falcon LM, Tucker KL, et al. Psychosocial risk factors for food insecurity in puerto ricans living in the USA from baseline to 5-year follow-up. J Nutr. (2020) 150:2199–203. doi: 10.1093/jn/nxaa177
21. Kubzansky LD, Kawachi I. Going to the heart of the matter: do negative emotions cause coronary heart disease? J Psychosom Res. (2000) 48:323–37. doi: 10.1016/S0022-3999(99)00091-4
22. Pressman SD, Cohen S. Does positive affect influence health? Psychol Bull. (2005) 131:925. doi: 10.1037/0033-2909.131.6.925
23. Moller CI, Tait RJ, Byrne DG. Deliberate self-harm, substance use, and negative affect in nonclinical samples: a systematic review. Substance Abuse. (2013) 34:188–207. doi: 10.1080/08897077.2012.693462
24. Graham-Engeland JE, Sin NL, Smyth JM, Jones DR, Knight EL, Sliwinski MJ, et al. Negative and positive affect as predictors of inflammation: timing matters. Brain Behav Immun. (2018) 74:222–30. doi: 10.1016/j.bbi.2018.09.011
25. Almeida DM. Resilience and vulnerability to daily stressors assessed via diary methods. Curr Dir Psychol Sci. (2005) 14:64–8. doi: 10.1111/j.0963-7214.2005.00336.x
26. Charles ST, Piazza JR, Mogle J, Sliwinski MJ, Almeida DM. The wear and tear of daily stressors on mental health. Psychol Sci. (2013) 24:733–41. doi: 10.1177/0956797612462222
27. Schwarz N. Retrospective and concurrent self-reports: the rationale for real-time data capture. Sci Real Time Data Capture Self Rep Health Res. (2007) 11:26. doi: 10.1201/9781584888901.ch2
28. Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. (2008) 4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415
29. Schembre SM, Liao Y, O'connor SG, Hingle MD, Shen SE, Hamoy KG, et al. Mobile ecological momentary diet assessment methods for behavioral research: systematic review. JMIR Mhealth Uhealth. (2018) 6:e11170. doi: 10.2196/11170
30. Liu H, Xie QW, Lou VWQ. Everyday social interactions and intra-individual variability in affect: a systematic review and meta-analysis of ecological momentary assessment studies. Motiv Emot. (2019) 43:339–53. doi: 10.1007/s11031-018-9735-x
31. USDA. Adult Food Security Survey Module: Three-Stage Design, With Screeners. Washington, DC: Economic Research Service (2012).
32. Usala PD, Hertzog C. Measurement of affective states in adults: evaluation of an adjective rating scale instrument. Res Aging. (1989) 11:403–26. doi: 10.1177/0164027589114001
33. Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. (1988) 54:1063. doi: 10.1037/0022-3514.54.6.1063
34. Izard CE. Patterns of Emotions: A New Analysis of Anxiety and Depression. New York, NY: Academic Press (2013).
35. Cranford JA, Shrout PE, Iida M, Rafaeli E, Yip T, Bolger N. A procedure for evaluating sensitivity to within-person change: can mood measures in diary studies detect change reliably? Pers Soc Psychol Bull. (2006) 32:917–29. doi: 10.1177/0146167206287721
36. U.S. Department of Health and Human Services. 2019 Poverty Guidelines. (2019). Available online at: https://aspe.hhs.gov/2019-poverty-guidelines (accessed June 3, 2021).
37. Cleveland WS, Grosse E, Shyu WM, Chambers JM, Hastie T. Statistical Models in s. Local Regression Models (1992).
38. Hastie T, Tibshirani R. Varying-coefficient models. J R Stat Soc Series B. (1993) 55:757–79. doi: 10.1111/j.2517-6161.1993.tb01939.x
39. Shiyko MP, Lanza ST, Tan X, Li R, Shiffman S. Using the time-varying effect model (TVEM) to examine dynamic associations between negative affect and self confidence on smoking urges: differences between successful quitters and relapsers. Prev Sci. (2012) 13:288–99. doi: 10.1007/s11121-011-0264-z
40. Tan X, Shiyko MP, Li R, Li Y, Dierker L. A time-varying effect model for intensive longitudinal data. Psychol Methods. (2012) 17:61–77. doi: 10.1037/a0025814
41. Lanza ST, Vasilenko SA, Liu X, Li R, Piper ME. Advancing the understanding of craving during smoking cessation attempts: a demonstration of the time-varying effect model. Nicotine Tob Res. (2014) 16 (Suppl. 2):S127–34. doi: 10.1093/ntr/ntt128
42. Shiyko MP, Burkhalter J, Li R, Park BJ. Modeling nonlinear time-dependent treatment effects: an application of the generalized time-varying effect model (TVEM). J Consult Clin Psychol. (2014) 82:760–72. doi: 10.1037/a0035267
43. Huang JZ, Wu CO, Zhou L. Varying-coefficient models and basis function approximations for the analysis of repeated measurements. Biometrika. (2002) 89:111–28. doi: 10.1093/biomet/89.1.111
44. Huang JZ, Shen H. Functional coefficient regression models for non-linear time series: a polynomial spline approach. Scand J Stat. (2004) 31:515–34. doi: 10.1111/j.1467-9469.2004.00404.x
45. Huang JZ, Wu CO, Zhou L. Polynomial spline estimation and inference for varying coefficient models with longitudinal data. Stat Sin. (2004) 14:763–88.
46. Laraia BA, Siega-Riz AM, Gundersen C, Dole N. Psychosocial factors and socioeconomic indicators are associated with household food insecurity among pregnant women. J Nutr. (2006) 136:177–82. doi: 10.1093/jn/136.1.177
47. Dolatian M, Sharifi N, Mahmoodi Z. Relationship of socioeconomic status, psychosocial factors, and food insecurity with preterm labor: a longitudinal study. Int J Reprod Biomed. (2018) 16:563–70. doi: 10.29252/ijrm.16.9.563
48. Nagata JM, Seligman HK, Weiser SD. Perspective: the convergence of coronavirus disease 2019 (COVID-19) and food insecurity in the United States. Adv Nutr. (2020) 12:287–90. doi: 10.1093/advances/nmaa126
49. Buchanan TW, Al'absi M, Lovallo WR. Cortisol fluctuates with increases and decreases in negative affect. Psychoneuroendocrinology. (1999) 24:227–41. doi: 10.1016/S0306-4530(98)00078-X
50. Human LJ, Whillans AV, Hoppmann CA, Klumb P, Dickerson SS, Dunn EW. Finding the middle ground: curvilinear associations between positive affect variability and daily cortisol profiles. Emotion. (2015) 15:705–20. doi: 10.1037/emo0000071
51. Sin NL, Graham-Engeland JE, Ong AD, Almeida DM. Affective reactivity to daily stressors is associated with elevated inflammation. Health Psychol. (2015) 34:1154. doi: 10.1037/hea0000240
52. Chan DK, Zhang X, Fung HH, Hagger MS. Affect, affective variability, and physical health: Results from a population-based investigation in China. Int J Behav Med. (2016) 23:438–46. doi: 10.1007/s12529-015-9510-2
53. Jones DR, Smyth JM, Engeland CG, Sliwinski MJ, Russell MA, Sin NL, et al. Affect variability and inflammatory markers in midlife adults. Health Psychol. (2020) 39:655. doi: 10.1037/hea0000868
54. Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. (2010) 363:6–9. doi: 10.1056/NEJMp1000072
55. The Pennsylvania SNAP Deposit Schedule. (2020). Available online at: http://services.dpw.state.pa.us/oimpolicymanuals/snap/PA_855.pdf (accessed June 3, 2021).
56. Wadsworth ME, Rindlaub L, Hurwich-Reiss E, Rienks S, Bianco H, Markman HJ. A longitudinal examination of the adaptation to poverty-related stress model: Predicting child and adolescent adjustment over time. J Clin Child Adoles Psychol. (2013) 42:713–25. doi: 10.1080/15374416.2012.755926
57. USDA. SNAP-Ed Toolkit: Glossary Terms. (2020). Available online at: https://snapedtoolkit.org/glossary/#food_resource_management_frm (accessed March 10, 2020).
58. Hersey J, Anliker J, Miller C, Mullis RM, Daugherty S, Das S, et al. Food shopping practices are associated with dietary quality in low-income households. J Nutr Educ. (2001) 33:S16–26. doi: 10.1016/S1499-4046(06)60066-3
59. Eicher-Miller HA, Mason AC, Abbott AR, Mccabe GP, Boushey CJ. The effect of food stamp nutrition education on the food insecurity of low-income women participants. J Nutr Educ Behav. (2009) 41:161–8. doi: 10.1016/j.jneb.2008.06.004
60. Dollahite JS, Pijai EI, Scott-Pierce M, Parker C, Trochim W. A randomized controlled trial of a community-based nutrition education program for low-income parents. J Nutr Educ Behav. (2014) 46:102–9. doi: 10.1016/j.jneb.2013.09.004
61. Na M, Jomaa L, Eagleton SG, Savage JS. Head start parents with or without food insecurity and with lower food resource management skills use less positive feeding practices in preschool-age children. J Nutr. (2021) 151:1294–301. doi: 10.1093/jn/nxab001
62. Herman D, Afulani P, Coleman-Jensen A, Harrison GG. Food insecurity and cost-related medication underuse among nonelderly adults in a nationally representative sample. Am J Public Health. (2015) 105:e48–59. doi: 10.2105/AJPH.2015.302712
63. United States Census Bureau. QuickFacts Blair County, Pennsylvania; Clearfield County, Pennsylvania; Centre County, Pennsylvania. (2019). Available online at: https://www.census.gov/quickfacts/fact/table/blaircountypennsylvania,clearfieldcountypennsylvania,centrecountypennsylvania/PST045219 (accessed August 5, 2021).
64. Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, De Girolamo G, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. (2011) 9:90. doi: 10.1186/1741-7015-9-90
Keywords: food insecurity, mood, EMA, season, stress
Citation: Na M, Dou N, Liao Y, Rincon SJ, Francis LA, Graham-Engeland JE, Murray-Kolb LE and Li R (2022) Daily Food Insecurity Predicts Lower Positive and Higher Negative Affect: An Ecological Momentary Assessment Study. Front. Nutr. 9:790519. doi: 10.3389/fnut.2022.790519
Received: 06 October 2021; Accepted: 10 February 2022;
Published: 25 March 2022.
Edited by:
Shreela Sharma, University of Texas Health Science Center at Houston, United StatesReviewed by:
Fei Men, University of Alabama, United StatesTomas Cabeza De Baca, National Institute of Diabetes and Digestive and Kidney Diseases (NIH), United States
Copyright © 2022 Na, Dou, Liao, Rincon, Francis, Graham-Engeland, Murray-Kolb and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Muzi Na, bXV6aS5uYUBwc3UuZWR1
 Muzi Na
Muzi Na Nan Dou
Nan Dou Yujie Liao2
Yujie Liao2 Jennifer E. Graham-Engeland
Jennifer E. Graham-Engeland