- 1Department of Urology, Institute of Urology, West China Hospital, Sichuan University, Chengdu, China
- 2Department of Urology, Affiliated Hospital of North Sichuan Medical College, Nanchong, China
- 3Department of Respiratory and Critical Care Medicine, West China Hospital, Sichuan University, Chengdu, China
Objective: This study aims to examine the correlation between overactive bladder (OAB) and food insecurity.
Methods: We conducted a cross-sectional analysis utilizing extensive population data derived from the National Health and Nutrition Examination Survey 2007–2018. The status of Household food insecurity is evaluated by the US Food Security Survey Module. To explore the relationship between food insecurity and OAB, three multivariable logistic regression models were carried out. Additionally, interaction and stratified analyses were also performed to find whether some factors have the potential to alter the correlation.
Results: There were 29,129 participants enrolled in the study. Compared to the other three groups, individuals with full food security exhibited a lower proportion of nocturia, urinary urgency incontinence, and OAB. In the fully-adjusted model, it was found that people experiencing food insecurity have a significantly higher prevalence of OAB compared to those with food security in the fully-adjusted model (OR = 1.540, 95%CI 1.359–1.745). Additionally, there was a significant association between the levels of food insecurity and an increased risk of OAB prevalence was also observed (marginal food security: OR = 1.312, low food security: OR = 1.559, and very low food security: OR = 1.759). No significant interaction was seen in the fully-adjusted model.
Conclusion: There is a strong positive correlation between food insecurity and the prevalence of OAB. Similarly, the correlation between levels of food insecurity and OAB also indicates the same trend. Namely, the more insecure food, the higher risk of OAB prevalence in the population.
1 Introduction
Overactive bladder (OAB) is a condition marked by urinary urgency, often accompanied by nocturia and frequent urination, with or without urge urinary incontinence (1). In recent years, there has been an increase in the prevalence of OAB. A report from the Epidemiology of Incontinence study in five countries (Canada, Germany, Italy, Sweden, and the UK) indicates an overall OAB prevalence of 11.8%, with a higher prevalence in women (12.8%) than in men (10.8%). Moreover, the prevalence of OAB increases with age (2). Furthermore, it is evident that OAB imposes a substantial global burden on both economic and social medical security systems, in addition to significantly impacting the quality of life. Debra et.al has reported that the average annual direct cost of OAB worldwide ranges from €1.2 to 2.7 trillion, with an expected increase to €1.4 to 3.2 trillion in 2018 (3). In clinical practice, long-term comprehensive treatment is recommended for most individuals, with non-surgical therapies being the first line of treatment (4). However, the primary objective of treating OAB is to alleviate symptoms, as it is unable to reverse pathophysiological abnormalities. Research has established that involuntary contractions of the detrusor muscle are the characteristic urodynamic feature in patients, with other forms of urethra–bladder dysfunction being less prevalent. Additionally, several risk factors have been identified for OAB, including dietary, physical activity, chronic diseases (diabetes, obesity, cardiac failure, and chronic obstructive pulmonary diseases), as well as neurological diseases (5–7). Despite the proliferation of theories posited to elucidate the pathophysiology of OAB, a definitive doctrine that universally encompasses its multifactorial and intricate pathogenesis has not yet been established. Consequently, there is an exigent need to clarify the underlying mechanism and devise potential strategies for managing OAB.
Food insecurity is defined as the state of lacking social, economic, and physical access to sufficient and nutritious food for the purpose of maintaining an active and healthy lifestyle (8). Two cross-section analysis showed that people with food insecurity was likely to be accompanied by worse psychological status (depression and suicide ideation) and higher risk of metabolism disorders (9–11). In addition, a study with 3,632 people (≥60 years old) enrolled indicated that the people probably prefer to have sarcopenia (low grip strength) compared to those with full food security (12). Those diseases mentioned above make contribute to the development of OAB (13). Recent research has revealed that approximately 10.5% of households in the United States experience food insecurity, and this proportion has jumped to 38.8% due to the impact of the novel coronavirus disease 2019 (14). This highlights the significance of food insecurity as a major public health concern, not only in developing nations but also in developed countries. Recent studies find that unhealthy eating habits and dietary structure make the risk of OAB increase, and the Mediterranean diet is seen as a protective factor (6, 15). Despite extensive research on the impact of food components and diet on overactive bladder (OAB), no studies have explored the relationship between food insecurity and OAB. Thus, a cross-sectional analysis utilizing the large population data from the National Health and Nutrition Examination Survey (NHANES) to explore the relationship between food insecurity and OAB would be highly valuable, and it is hypothesized that a positive association exists between the two variables.
2 Methods
2.1 Study design and population
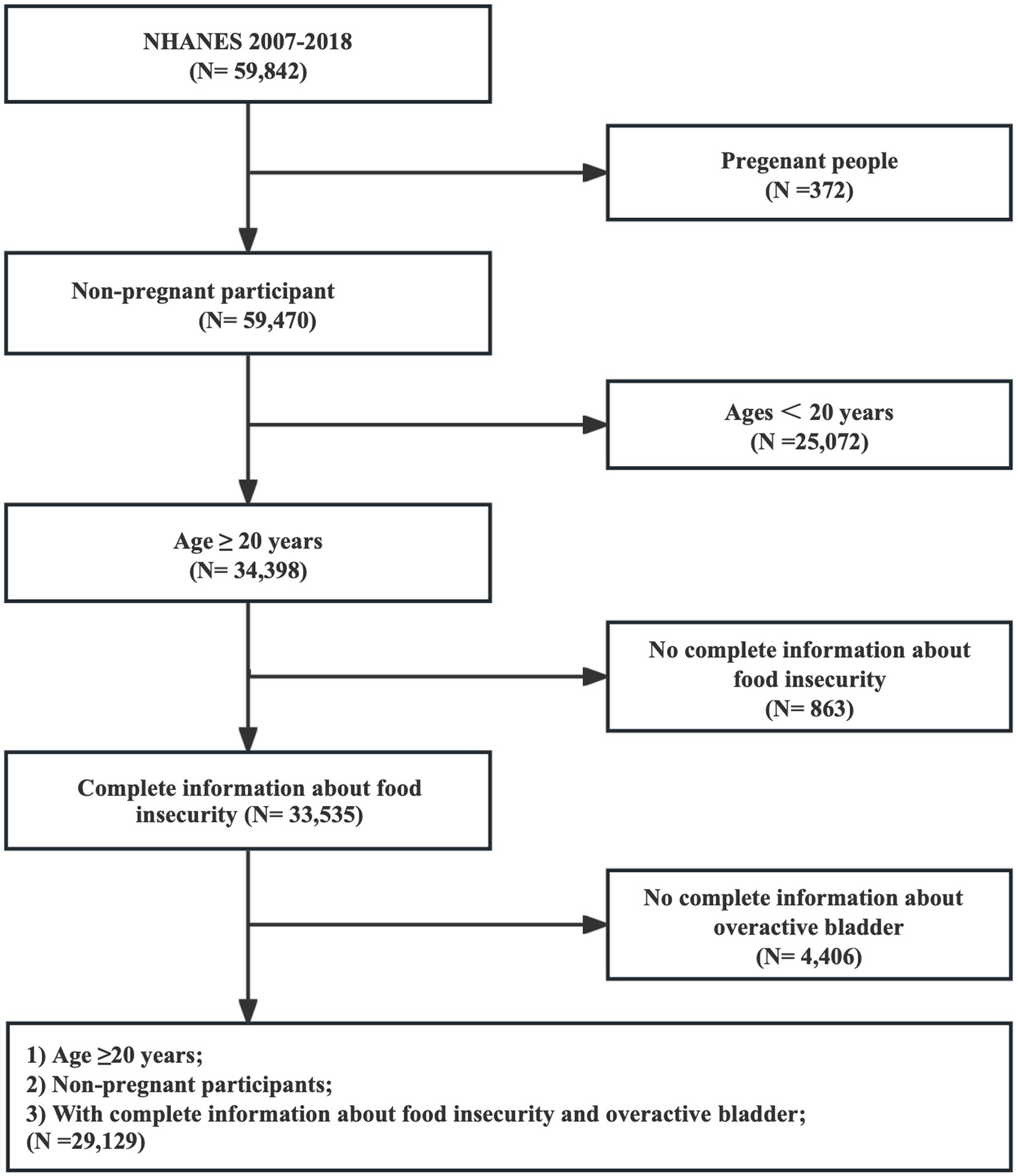
A cross-sectional analysis was conducted using data derived from the NHANES 2007–2018, which was designed by the National Center for Health Statistics (NCHS). NHANES is a nationally representative survey that aims to investigate the health and nutritional status of Americans by collecting information through physical examinations, laboratory tests, and interviews. Researchers are granted free access to NHANES, and the database has been updated biennially since 1999. The study initially involved 59,842 individuals, of which 372 pregnant individuals were not enrolled, and those under the age of 20 were excluded (n = 25,072). Furthermore, participants with incomplete information regarding food security (n = 863) and overactive bladder (n = 4,406) diagnoses were eliminated. Ultimately, the study comprised 29,129 individuals, as depicted in Figure 1.
2.2 Food security diagnosis
Household food security in the United States was assessed using the US Food Security Survey Module (FSSM), which is considered the standard for measuring food security. The FSSM consists of 10 questions for households with and without children.1 Food security status was determined based on the number of affirmative responses in the adult module. (I) Full food security was indicated by zero affirmative responses. (II) Marginal food security was indicated by 1–2 affirmative responses. (III) Low food security was indicated by 3–5 affirmative responses. (IV) Very low food security was indicated by 6–10 affirmative responses. Following USDA guidelines, food security was categorized as a binary variable: food security (full and marginal food security) and food insecurity (low and very low food security).
2.3 Overactive bladder diagnosis
The definition of OAB involves a frequent need to urinate, characterized by urinary urgency incontinence (UUI) and waking up at night to urinate (nocturia). The data for this study were collected through questionnaires administered in face-to-face interviews by trained research personnel. UUI was determined by asking participants “During the past 12 months, have you leaked or lost control of even a small amount of urine with an urge or pressure to urinate and you could not get to the toilet fast enough?” and the severity of the condition was evaluated by inquiring “How frequently does this occur?” Furthermore, nocturia was assessed by asking participants “During the past 30 days, how many times per night did you most typically get up to urinate, from the time you went to bed at night until the time you got up in the morning.” Additionally, the severity of OAB was measured using the Overactive Bladder Symptom Score (OABSS), as shown in Figure 2. An individual with an overall OABSS score of ≥3 was considered to have OAB (16).
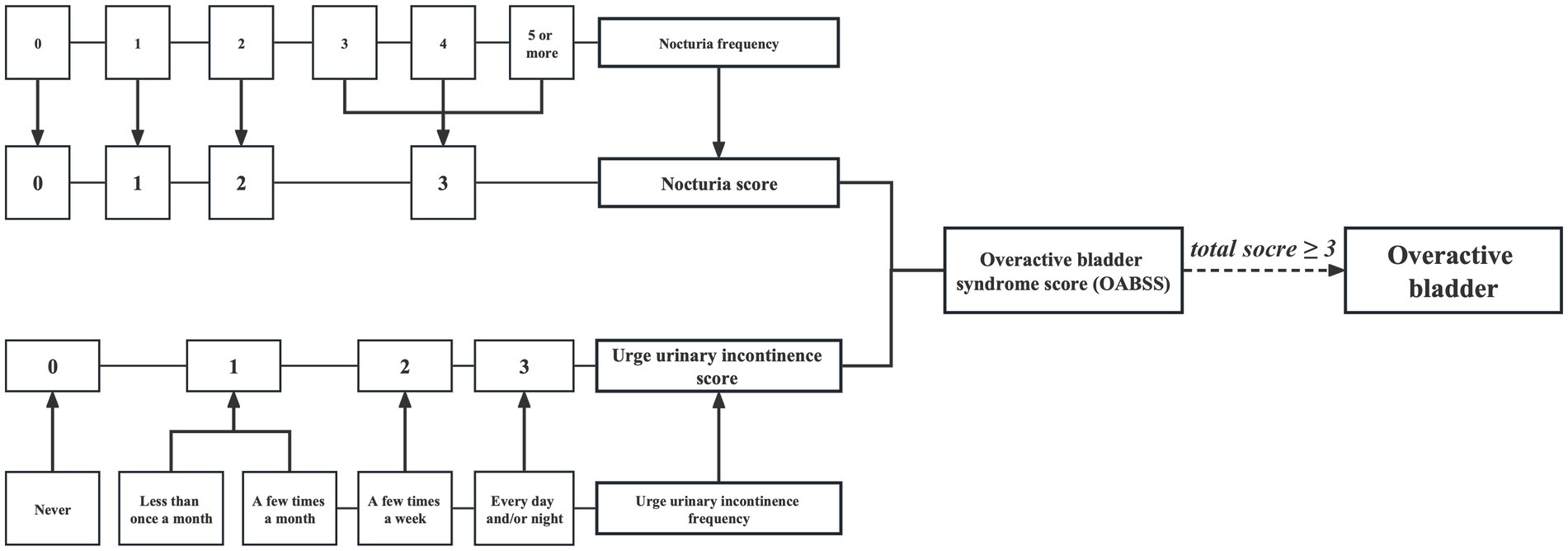
Figure 2. Flow diagram of the overactive bladder diagnosis based on overactive bladder syndrome score.
2.4 Covariates
Several methods were used to collect information about covariates, including questionnaires, examinations, and laboratory tests. The continuous variables included age, body mass index (BMI), and poverty income ratio (PIR). The categorical variables included gender (female and male), race (Mexican American, Non-Hispanic white, Non-Hispanic black, other Hispanic, other races), education level (less than 9th grade, 9–11th grade, high school graduate, some college, college graduate or above). marital status (married/living with a partner, divorced/separated/widowed, never married), alcohol, smoking (never, former, now), diabetes (no, borderline, yes), cardiovascular disease (CVD), hypertension, cancer (all no/yes).
2.5 Statistical analysis
Mean ± standard errors (SE) and proportions were used to describe the baseline characteristics of all participants. Among them, the correlation between continuous variables was analyzed by linear regression, and the correlation between categorical variables was analyzed by Chi-square analysis.
The study employed a stratification method based on the US FSSM to categorize participants into four groups, which were subsequently recoded into a dichotomous variable. To explore the association between food security and the prevalence of OAB, three multivariable logistic models were conducted. The non-adjusted model did not include any adjustments, while the minimally-adjusted model adjusted for age and race. The fully-adjusted model, on the other hand, accounted for age, race, gender, BMI, PIR, education, marital status, alcohol, smoking, diabetes, hypertension, CVD, and cancer were all adjusted. To explore potential modifiers of the relationship between food security and the prevalence of overactive bladder both interaction and stratified analyses were performed.
The sample weights recommended by the Centers for Disease Control and Prevention (CDC)2 were used in all analyses. This crucial step ensured the representativeness of the sample concerning the US civilian population and facilitated the generation of unbiased national estimates. Statistical analyses were conducted using R 4.0 (the R Foundation)3 and EmpowerStats (X&Y Solutions, Inc.).4 p value less than 0.05 (p < 0.05) was considered statistically significant.
3 Results
3.1 Baseline characteristics of the population
A total of 29,129 participants were enrolled across seven cycles of NHANES and subsequently categorized into four distinct groups, namely full food security (n = 19,883), marginal food security (n = 3,557), low food security (n = 3,243), and very low food security (n = 2,446), based on the establishment of US FSSM. Notably, all baseline characteristics exhibited significant differences across the aforementioned groups, as presented in Table 1. Compared to the other three groups, individuals with full food security exhibited a higher age (Mean ± SE, 49.5 ± 17.1 years) and a greater proportion of males (49.8%). The prevalence of UUI was lower (19.7%), as were occurrences of nocturia (64.9%) and overactive bladder (OAB) (14.8%) in this group. Additionally, the same trend was present in BMI (28.8 ± 6.6 kg/m2), smoking (15.3%), CVD (8.6%), and diabetes (14.2%). Conversely, these individuals exhibited higher levels of education (college graduate or above, 36.3%) and PIR, (3.4 ± 1.5) and a greater proportion of non-single status (married/living with a partner, 66.3%). In addition, the details of OABSS are showed in Supplementary Table S1.
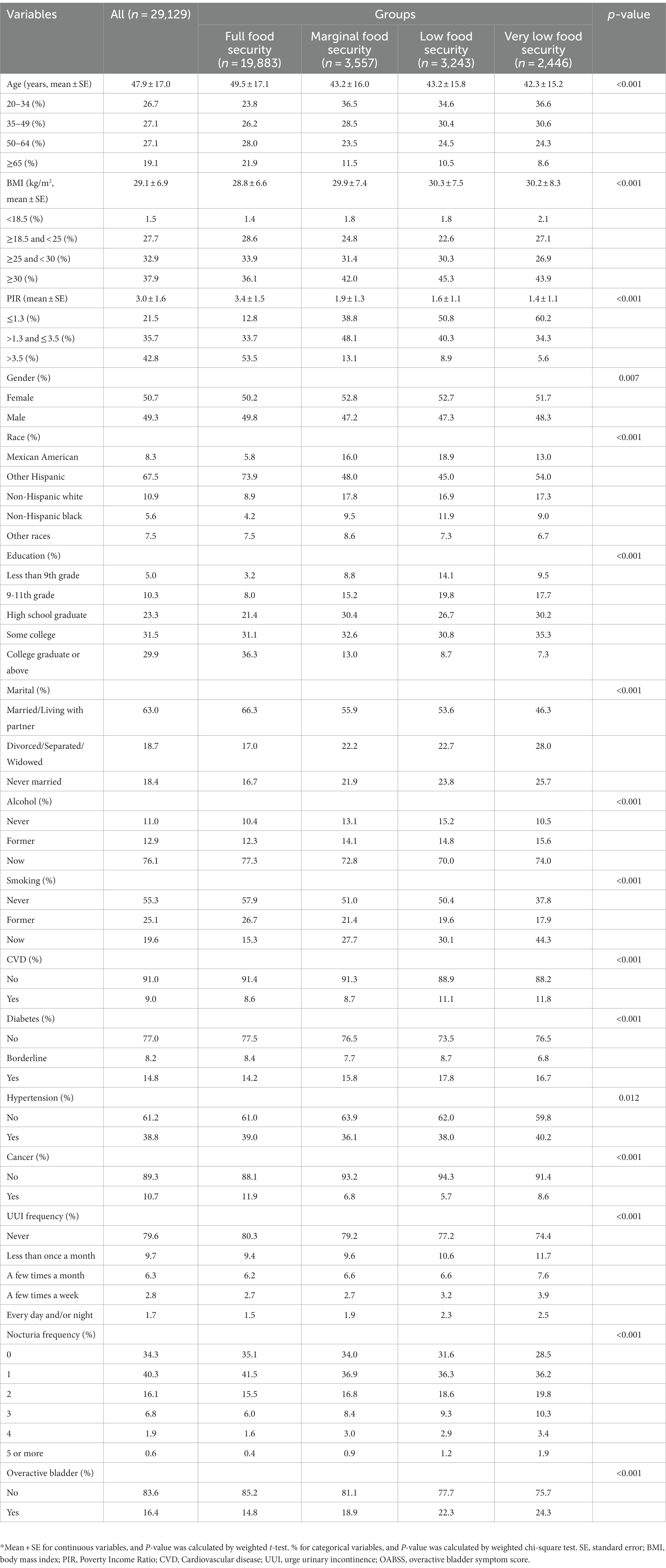
Table 1. Characteristics of participants by categories of the status of food insecurity: NHANES 2007–2018*.
3.2 Multivariable regression analysis
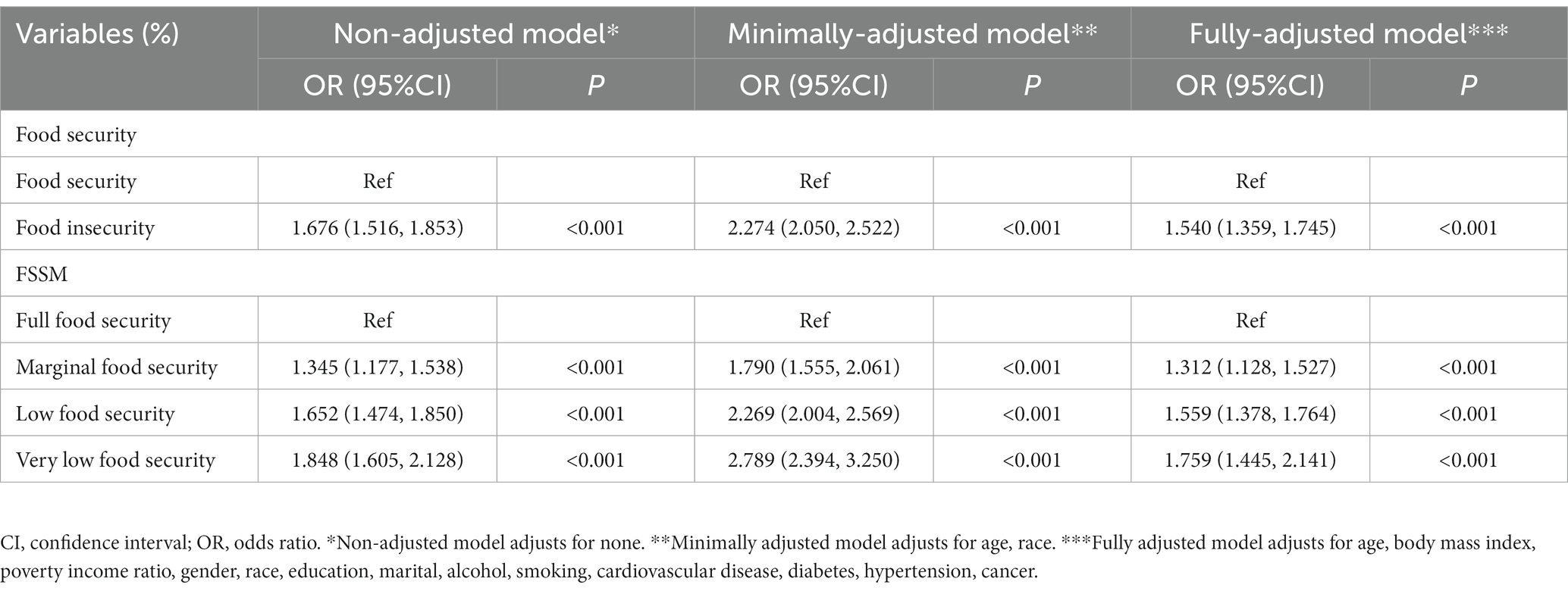
Three logistic models were employed to investigate the relationship between food security and OAB through multivariable logistic regression analysis. As evidenced by Table 2, a positive correlation was observed between food insecurity and the prevalence of OAB in the non-adjusted model (OR = 1.676, 95%CI 1.516–1.853, p < 0.001), in the minimally-adjusted model (OR = 2.274, 95%CI 2.050–2.522, p < 0.001), in the fully-adjusted model (OR = 1.540, 95%CI 1.359–1.745, p < 0.001). To provide additional clarification, a stratified multivariate logistic regression analysis was performed based on the US FSSM. The results indicated that there was a significant association between the levels of food insecurity and an increased risk of OAB prevalence, with odds ratios of 1.312 for marginal food security, 1.559 for low food security, and 1.759 for very low food security, all of which were statistically significant at p < 0.001.
3.3 Stratified and interaction analysis
To examine potential factors that may affect the relationship between food security and the prevalence of OAB, stratified and interaction analyses were conducted. The findings presented in Table 3 suggest that age, BMI, and race could have an impact on this association, with a stronger positive association observed. However, it is important to note that the direction of effect estimates remained consistent across all subgroups, and no additional interactions were found.
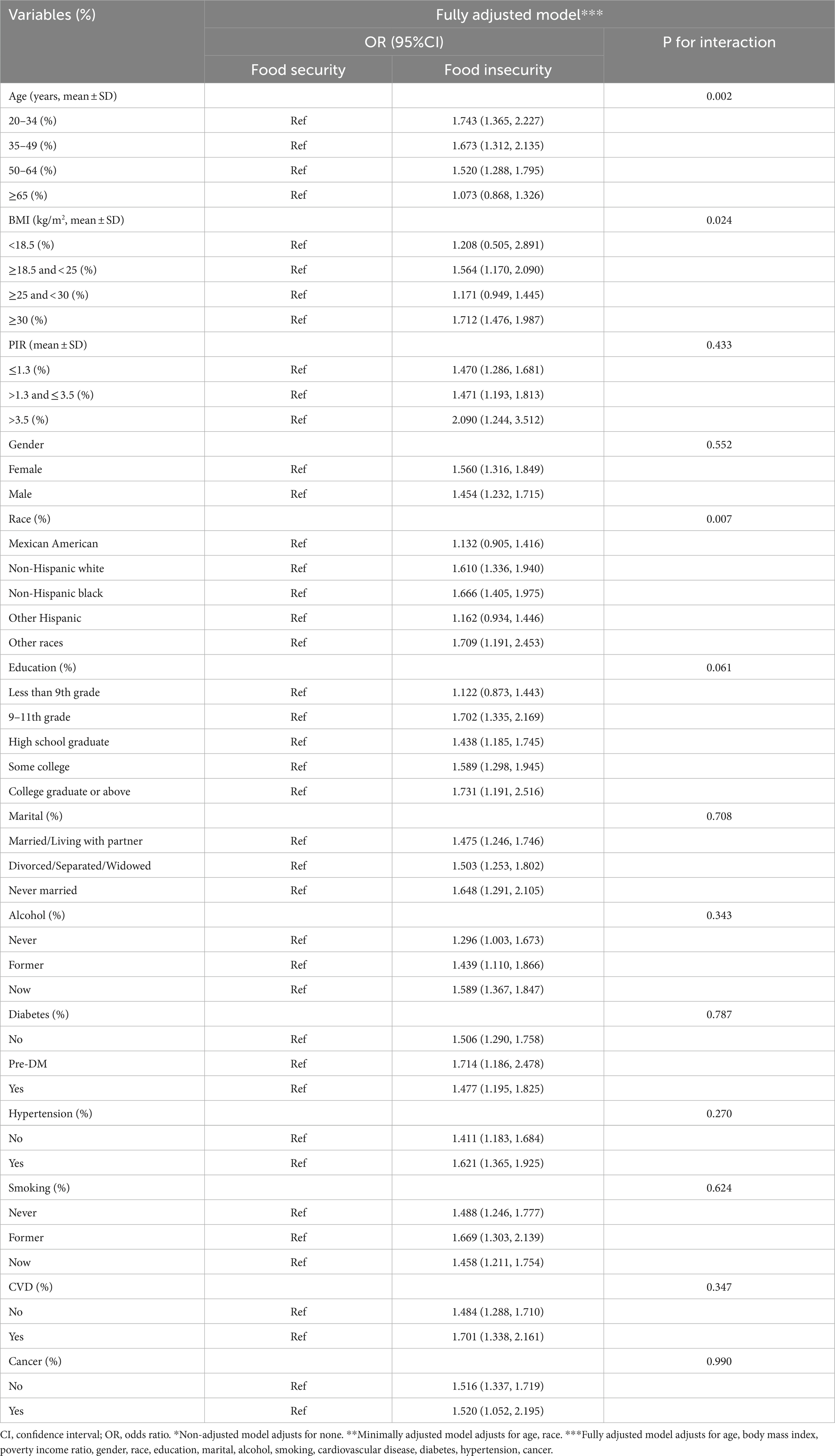
Table 3. Logistic regression analysis to identify variables that modify the correlation between food insecurity and the prevalence of overactive bladder.
4 Discussion
Our study reveals a significant positive correlation between food insecurity and the prevalence of OAB. Furthermore, we observe that higher levels of food insecurity are associated with an increased risk of OAB in the population. Importantly, this positive association remains consistent across various factors, suggesting the reliability of our findings.
Increasing evidence has demonstrated that diet plays a critical role in OAB management. Some research suggested that people with low vitamin D intake had a high risk of OAB via muscle atrophy (17). A clinical study revealed that low vitamin B6 and B12 often coupled with elevated plasma homocysteine concentrations resulting from impaired homocysteine metabolism, may contribute to the development of CVD and neurodegenerative disorders (18). Additionally, both inadequate and excessive levels of potassium have been found to impair bladder function and contribute to the manifestation of urinary storage symptoms (19). Apart from that, some circumstantial evidence agrees with our conclusion. Food insecurity is mainly characterized by the consumption of high-fat fast food, high-sugar contents, and reduced intake of vegetables and fruits. Thus, this type of high-calorie, low-nutrient diet is known to result in insufficient nutrient intake and an elevated risk of multiple nutritional deficiencies, thereby increasing the incidence of various chronic diseases (20). Several studies indicate that people with low fruit and vegetable intake often along with low dietary fiber intake, which serves as one of the contributing factors to the occurrence of chronic constipation and bowel straining (21). It is important to note that these aforementioned disorders exert an adverse effect on the neurological function of the pelvic floor. Furthermore, individuals experiencing food insecurity are more likely to exhibit higher rates of obesity in comparison to those who have access to adequate food resources (22). A prospective cohort study has suggested that obesity is a significant risk factor for the onset of OAB and stress incontinence, increased exposure of the pelvic floor to intraabdominal and intravesical pressure may explain this phenomenon (23). Additionally, people with dyslipidemia and diabetes are more common in these people with food insecurity, leading to a higher prevalence of arteriosclerosis and CVD (24, 25). Mountainous studies have identified that these are major contributors to OAB. Moreover, food insecurity is found to have the ability of pro-inflammatory potential, which results in neurodegenerative and neuropsychiatric illness (26, 27). Therefore, it is imperative to increase awareness of food security as a means of managing OAB and to explore its potential for clinical translation.
Food insecurity primarily arises from socio-economic and non-economic determinants, with socio-economic factors playing a dominant role in this regard. Previous studies supported that individuals with lower income levels are more susceptible to experiencing food insecurity, characterized by a higher prevalence of consumables containing saturated fats, added sugars, and refined carbohydrates, compared to those with middle or high-income levels (28). Moreover, apart from being predisposed to consuming low-quality food, the population facing food insecurity is also more inclined to encounter challenges in accessing substandard pharmaceuticals and experiencing limited availability of medical resources due to transportation constraints (29). According to several studies, individuals with higher incomes are more engaged in physical activity than those with poverty income (30). All of these mentioned above accelerate the OAB development. In another part, non-economic factors primarily contribute to the responsibility for food insecurity among older individuals. Several studies indicate that physical limitations in acquiring groceries (31.4%) or preparing meals (22.7%) pose more significant challenges for older adults than financial constraints (merely 14.6%) (31, 32). Moreover, the distressing nature of food insecurity or uncertainty regarding the availability of the next meal predisposes individuals to the development of anxiety and depression, which are the cause of suffering from OAB (33, 34). In turn, the presence of poor mental health conditions intensifies both the financial and physical hardships, thus establishing a detrimental cycle. Consequently, the matter of food security transcends mere governmental regulation and has evolved into a multifaceted concern encompassing social, economic, and livelihood aspects. Mitigating income inequality and implementing comprehensive food programs and services can potentially contribute to addressing food insecurity and preventing the onset of OAB.
In the study, we find that the positive association between food insecurity and the prevalence of OAB differed from age, and stratified and interaction analysis indicate the younger can amplify the association. During the COVID-19 pandemic, there was a noticeable increase in the consumption of ultra-processed foods (UPF) and a decrease in the consumption of fresh foods among young people (35). And mounting evidence shows that young individuals exhibit the highest intake of UPF in their dietary patterns, surpassing other demographic groups. Furthermore, it is essential to highlight that vitamin D deficiency is closely related to regular diet and physical activity, and irregular diet phenomenon which accelerates the disease is more common in the young (36, 37). These diseases will lead to the occurrence of some chronic diseases such as obesity, diabetes, and immunocompromised, making the risk of OAB prevalence increase (38). Therefore, the importance of food security publicity and education needs to be handled seriously, especially for young people.
The study has several notable strengths. Firstly, it utilizes a representative sample that includes a diverse population, allowing for the results to be more easily applied to the broader United States populace. Additionally, this study is the first to examine the association between food insecurity and the prevalence of OAB. The status of food insecurity is assessed using the validated and reliable FSSM. However, there are also some limitations that should be acknowledged. The cross-sectional design of the study prevents the establishment of causal relationships. Additionally, it is important to note that the NHANES does not include any relevant laboratory diagnostic tests (urodynamics, residual urine), although the OABSS scale is used for diagnosis in this study. Furthermore, certain confounding factors such as multiparous and parity were not adjusted for due to missing data in the database, despite the adjustment for many other confounders.
5 Conclusion
There is a significant association between food insecurity and the prevalence of OAB. Namely, food insecurity is positively associated with OAB development, and levels of food insecurity are also linked with the prevalence of OAB. However, owing to the cross-sectional analysis, a prospective cohort study is supposed to be conducted for further verification and exploration.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found at: https://www.cdc.gov/nchs/nhanes/index.htm.
Ethics statement
This study was performed using public data from the National Center for Health Statistics (NCHS) Program and the National Health and Nutrition Examination Survey (NHANES). The data have been de-identified and not merged or augmented in any way that has compromised the privacy of the participants. Therefore, the study requires no further approval and follows ethical guidelines.
Author contributions
YFX: Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Validation, Writing – original draft, Writing – review & editing. SY: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. YJB: Data curation, Formal analysis, Funding acquisition, Project administration, Supervision, Writing - review & editing. JHW: Data curation, Formal analysis, Methodology, Software, Supervision, Writing – original draft. JWC: Data curation, Investigation, Writing – original draft. YQY: Data curation, Investigation, Software, Writing – original draft. JW: Conceptualization, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Key Research and Development Projects of Sichuan Science and Technology Department (grant no. 2022YFS0306).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023.1329687/full#supplementary-material
Footnotes
References
1. Rogers, RG , Pauls, RN , Thakar, R , Morin, M , Kuhn, A , Petri, E, et al. An international Urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for the assessment of sexual health of women with pelvic floor dysfunction. Neurourol Urodyn. (2018) 37:1220–40. doi: 10.1002/nau.23508
2. Irwin, DE , Milsom, I , Hunskaar, S , Reilly, K , Kopp, Z , Herschorn, S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. (2006) 50:1306–15. discussion 1314–1305. doi: 10.1016/j.eururo.2006.09.019
3. Irwin, DE , Kopp, ZS , Agatep, B , Milsom, I , and Abrams, P . Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction. BJU Int. (2011) 108:1132–8. doi: 10.1111/j.1464-410X.2010.09993.x
4. Lightner, DJ , Gomelsky, A , Souter, L , and Vasavada, SP . Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline amendment 2019. J Urol. (2019) 202:558–63. doi: 10.1097/JU.0000000000000309
5. Ahmed, Z . Effects of cathodal trans-spinal direct current stimulation on lower urinary tract function in normal and spinal cord injury mice with overactive bladder. J Neural Eng. (2017) 14:056002. doi: 10.1088/1741-2552/aa76f2
6. Bozkurt, YE , Temeltaş, G , Müezzinoğlu, T , and Üçer, O . Mediterranean diet and overactive bladder. Int Neurourol J. (2022) 26:129–34. doi: 10.5213/inj.2142118.059
7. Hsu, LN , Hu, JC , Chen, PY , Lee, WC , and Chuang, YC . Metabolic syndrome and overactive bladder syndrome may share common pathophysiologies. Biomedicine. (2022) 10:1957. doi: 10.3390/biomedicines10081957
8. Nikolaus, CJ , An, R , Ellison, B , and Nickols-Richardson, SM . Food insecurity among college students in the United States: a scoping review. Adv Nutr. (2020) 11:327–48. doi: 10.1093/advances/nmz111
9. Himmelgreen, D , Romero-Daza, N , Heuer, J , Lucas, W , Salinas-Miranda, AA , and Stoddard, T . Using syndemic theory to understand food insecurity and diet-related chronic diseases. Soc Sci Med. (2022) 295:113124. doi: 10.1016/j.socscimed.2020.113124
10. Lee, J , and Pak, TY . Longitudinal associations between food insecurity and suicidal ideation among adults aged ≥65 in the Korean welfare panel study. Int J Public Health. (2023) 68:1605618. doi: 10.3389/ijph.2023.1605618
11. Umutoniwase, S , Nshimyiryo, A , Barnhart, DA , Dusabeyezu, S , Mpanumusingo, E , Nahimana, E, et al. Food insecurity and level of depression among patients with chronic diseases, and associated factors during the COVID-19 lockdown: a cross-sectional study in rural Rwanda. BMJ Open. (2022) 12:e054137. doi: 10.1136/bmjopen-2021-054137
12. Lynch, DH , Petersen, CL , Van Dongen, MJ , Spangler, HB , Berkowitz, SA , and Batsis, JA . Association between food insecurity and probable sarcopenia: data from the 2011-2014 National Health and Nutrition Examination Survey. Clin Nutr. (2022) 41:1861–73. doi: 10.1016/j.clnu.2022.07.002
13. Marinkovic, SP , Rovner, ES , Moldwin, RM , Stanton, SL , Gillen, LM , and Marinkovic, CM . The management of overactive bladder syndrome. BMJ. (2012) 344:e2365. doi: 10.1136/bmj.e2365
14. Wolfson, JA , and Leung, CW . Food insecurity and COVID-19: disparities in early effects for US adults. Nutrients. (2020) 12:1648. doi: 10.3390/nu12061648
15. Zhang, Q , Zhang, Z , He, X , Liu, Z , Shen, L , Long, C, et al. Vitamin D levels and the risk of overactive bladder: a systematic review and meta-analysis. Nutr Rev. (2023):nuad049. doi: 10.1093/nutrit/nuad049 [Epub ahead of print].
16. Zhu, S , Wang, Z , Tao, Z , Wang, S , and Wang, Z . Relationship between marijuana use and overactive bladder (OAB): a cross-sectional research of NHANES 2005 to 2018. Am J Med. (2023) 136:72–8. doi: 10.1016/j.amjmed.2022.08.031
17. Markland, AD , Vaughan, CP , Huang, AJ , Kim, E , Bubes, VY , Tangpricha, V, et al. Effect of vitamin D supplementation on overactive bladder and urinary incontinence symptoms in older men: ancillary findings from a randomized trial. J Urol. (2023) 209:243–52. doi: 10.1097/JU.0000000000002942
18. Lai, JS , Pang, WW , Cai, S , Lee, YS , Chan, JKY , Shek, LPC, et al. High folate and low vitamin B12 status during pregnancy is associated with gestational diabetes mellitus. Clin Nutr. (2018) 37:940–7. doi: 10.1016/j.clnu.2017.03.022
19. Li, N , Ding, H , Li, Z , Liu, Y , and Wang, P . Effect of high-fat diet-induced obesity on the small-conductance Ca(2+)-activated K(+) channel function affecting the contractility of rat detrusor smooth muscle. Int Urol Nephrol. (2019) 51:61–72. doi: 10.1007/s11255-018-2016-5
20. Christian, VJ , Miller, KR , and Martindale, RG . Food insecurity, malnutrition, and the microbiome. Curr Nutr Rep. (2020) 9:356–60. doi: 10.1007/s13668-020-00342-0
21. Okada, C , Kim, JI , Melamed, ML , Abraham, N , and Halani, PK . The relationship between fecal incontinence and food insecurity in United States women: an analysis of 2005-2010 National Health and nutrition examination survey. Am J Obstet Gynecol. (2023) 228:449.e1–449.e13. doi: 10.1016/j.ajog.2022.12.007
22. Keenan, GS , Christiansen, P , and Hardman, CA . Household food insecurity, diet quality, and obesity: An explanatory model. Obesity. (2021) 29:143–9. doi: 10.1002/oby.23033
23. Dallosso, HM , Mcgrother, CW , Matthews, RJ , and Donaldson, MM . The association of diet and other lifestyle factors with overactive bladder and stress incontinence: a longitudinal study in women. BJU Int. (2003) 92:69–77. doi: 10.1046/j.1464-410X.2003.04271.x
24. Berkowitz, SA , Karter, AJ , Corbie-Smith, G , Seligman, HK , Ackroyd, SA , Barnard, LS, et al. Food insecurity, food "deserts," and glycemic control in patients with diabetes: a longitudinal analysis. Diabetes Care. (2018) 41:1188–95. doi: 10.2337/dc17-1981
25. Sun, Y , Liu, B , Rong, S , Du, Y , Xu, G , Snetselaar, LG, et al. Food insecurity is associated with cardiovascular and all-cause mortality among adults in the United States. J Am Heart Assoc. (2020) 9:e014629. doi: 10.1161/JAHA.119.014629
26. Bergmans, RS , Palta, M , Robert, SA , Berger, LM , Ehrenthal, DB , and Malecki, KM . Associations between food security status and dietary inflammatory potential within lower-income adults from the United States National Health and nutrition examination survey, cycles 2007 to 2014. J Acad Nutr Diet. (2018) 118:994–1005. doi: 10.1016/j.jand.2017.12.003
27. Khansari, PS , and Sperlagh, B . Inflammation in neurological and psychiatric diseases. Inflammopharmacology. (2012) 20:103–7. doi: 10.1007/s10787-012-0124-x
28. Jia, J , Fung, V , Meigs, JB , and Thorndike, AN . Food insecurity, dietary quality, and health care utilization in lower-income adults: a cross-sectional study. J Acad Nutr Diet. (2021) 121:2177–2186.e3. doi: 10.1016/j.jand.2021.06.001
29. Smith, MD , and Coleman-Jensen, A . Food insecurity, acculturation and diagnosis of CHD and related health outcomes among immigrant adults in the USA. Public Health Nutr. (2020) 23:416–31. doi: 10.1017/S1368980019001952
30. Sfm, C , Van Cauwenberg, J , Maenhout, L , Cardon, G , Lambert, EV , and Van Dyck, D . Inequality in physical activity, global trends by income inequality and gender in adults. Int J Behav Nutr Phys Act. (2020) 17:142. doi: 10.1186/s12966-020-01039-x
31. Locher, JL , Ritchie, CS , Roth, DL , Sen, B , Vickers, KS , and Vailas, LI . Food choice among homebound older adults: motivations and perceived barriers. J Nutr Health Aging. (2009) 13:659–64. doi: 10.1007/s12603-009-0194-7
32. Vaudin, AM , Moshfegh, AJ , and Sahyoun, NR . Measuring food insecurity in older adults using both physical and economic food access, NHANES 2013-18. J Nutr. (2022) 152:1953–62. doi: 10.1093/jn/nxac058
33. Davis, HA , Kells, M , Todorov, S , Kosmas, J , and Wildes, JE . Comorbid eating, depressive, and anxiety psychopathology is associated with elevated shame in women with food insecurity. Int J Eat Disord. (2023) 56:1087–97. doi: 10.1002/eat.23913
34. Reeder, N , Tolar-Peterson, T , Bailey, RH , Cheng, WH , and Evans, MW Jr. Food insecurity and depression among US adults: NHANES 2005-2016. Nutrients. (2022) 14:3081. doi: 10.3390/nu14153081
35. Dezanetti, T , Quinaud, RT , Caraher, M , and Jomori, MM . Meal preparation and consumption before and during the COVID-19 pandemic: the relationship with cooking skills of Brazilian university students. Appetite. (2022) 175:106036. doi: 10.1016/j.appet.2022.106036
36. Cuomo, A , Maina, G , Bolognesi, S , Rosso, G , Beccarini Crescenzi, B , Zanobini, F, et al. Prevalence and correlates of vitamin D deficiency in a sample of 290 inpatients with mental illness. Front Psych. (2019) 10:167. doi: 10.3389/fpsyt.2019.00167
37. Roshanmehr, F , Hayashi, K , Tahara, Y , Suiko, T , Nagamori, Y , Iwai, T, et al. Association between breakfast meal categories and timing of physical activity of Japanese workers. Foods. (2022) 11:2609. doi: 10.3390/foods11172609
Keywords: food insecurity, overactive bladder, nocturia, urinary urgency incontinence, NHANES
Citation: Xiao Y, Yin S, Bai Y, Wang J, Cui J, Yang Y and Wang J(2024) A positive association between food insecurity and the prevalence of overactive bladder in U.S. adults. Front. Nutr. 10:1329687. doi: 10.3389/fnut.2023.1329687
Edited by:
Zhaohui Chen, Huazhong University of Science and Technology, ChinaReviewed by:
Xiao-qiang Liu, Tianjin Medical University General Hospital, ChinaFa Sun, Guizhou Provincial People's Hospital, China
Copyright © 2024 Xiao, Yin, Bai, Wang, Cui, Yang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jia Wang, d2FuZ2ppYXdjaEAxNjMuY29t
†These authors have contributed equally to this work
 Yunfei Xiao
Yunfei Xiao Shan Yin
Shan Yin Yunjin Bai1
Yunjin Bai1 Jiahao Wang
Jiahao Wang Jianwei Cui
Jianwei Cui Yaqing Yang
Yaqing Yang Jia Wang
Jia Wang