- 1School of Nursing, Shanxi University of Chinese Medicine, Yuci, China
- 2Department of Central Operating Room, Shanxi Bethune Hospital Shanxi Academy of Medical Sciences, Tongji Shanxi Hospital, Third Hospital of Shanxi Medical University, Taiyuan, China
- 3Department of Nursing, Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences, Tongji Shanxi Hospital, Third Hospital of Shanxi Medical University, Taiyuan, China
Background: Type 2 Diabetes Mellitus (T2DM) poses a significant global health challenge. Propolis, a natural bioactive compound, is proposed to modulate glucose and lipid metabolism and exert anti-inflammatory effects. However, previous reviews have limited scope, and the effects of propolis on T2DM remain debated, particularly concerning lipid profiles, glycemic control, inflammation, and oxidative stress.
Methods: A systematic search was conducted across Chinese National Knowledge Infrastructure (CNKI), VIP, SinoMed, Wanfang Data, PubMed, Cochrane Library, Embase, Scopus, and Web of Science, with the search time limit set from the establishment of the databases to 20 May 2025. Study quality was assessed using the Cochrane Risk of Bias Assessment Tool version 2 (ROB 2); evidence quality was evaluated via the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach; and meta-analysis was performed using RevMan 5.4.
Results: In total, 12 randomized controlled trials (RCTs) with 731 participants were included in this study. Propolis supplementation significantly increased high-density lipoprotein cholesterol (HDL-C) levels (mean difference (MD) = 0.13, 95% CI 0.10–0.16, p < 0.00001), and reduced low-density lipoprotein cholesterol (LDL-C) (MD = −0.32, 95% CI: −0.56 to −0.08; p = 0.009) and triglyceride (TG) levels (MD = −0.15, 95% CI: −0.30 to −0.01; p = 0.04). It also improved glycemic control, lowering fasting blood sugar (FBS) (MD = −1.13, 95% CI: −2.00 to −0.27, p = 0.01), homeostasis model assessment of insulin resistance (HOMA-IR) (MD = −0.95, 95% CI: −1.36 to −0.55, p < 0.00001), and glycosylated hemoglobin (HbA1c) (MD = −0.44, 95% CI: −0.78 to −0.11, p = 0.01). Furthermore, propolis significantly reduced C-reactive protein (CRP) (MD = −2.68, 95% CI: −3.48 to −1.89, p < 0.00001). However, no significant effects were observed for total cholesterol (TC), tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), superoxide dismutase (SOD), or malondialdehyde (MDA).
Conclusion: Propolis may improve lipid and glucose profiles and reduce inflammation in T2DM. While current evidence does not confirm significant effects on oxidative stress markers, considering the limitations of existing clinical studies and positive basic research findings, its potential antioxidant effects require validation through high-quality RCTs.
Systematic review resistration: This study was registered with PROSPERO (registration number: CRD42024577722) https://www.crd.york.ac.uk/PROSPERO/#loginpage.
Introduction
Type 2 Diabetes Mellitus (T2DM) is a chronic metabolic disorder characterized by insulin resistance and dysfunction of pancreatic β-cells. It accounts for over 90% of global diabetes cases and exhibits a trend toward younger onset, and represents a major public health burden (1, 2). Globally, 537 million adults live with diabetes, a number projected to exceed 700 million by 2045. Approximately 40% of these individuals may develop chronic kidney disease (CKD) (3). The World Health Organization (WHO) reports that over half of patients do not adhere to regular medication, particularly in low- and middle-income countries with poor treatment coverage, increasing risks for complications like blindness, renal failure, and cardiovascular disease (4).
Current T2DM management relies heavily on pharmacological glucose control, but this approach carries significant safety concerns (5–8). For example, a regional study in Asia found that 35.8% of T2DM patients using oral hypoglycemic agents experienced hypoglycemia within 6 months (6). Sulfonylurea medications can impair hypoglycemia awareness and potentially cause severe complications such as cognitive dysfunction and arrhythmias (7). Thiazolidinediones are also linked to an increased risk of fractures and bladder cancer (9). Therefore, exploring safe, cost-effective, and efficient complementary therapies for T2DM is crucial.
Various plant-derived bioactive compounds have been investigated for T2DM adjunctive treatment, yet many show limited efficacy or practical application issues. For instance, curcumin has notable anti-inflammatory and antioxidant properties and demonstrated hypoglycemic potential in clinical trials, but its low oral bioavailability severely restricts clinical translation (10). Similarly, while okra may temporarily lower fasting blood glucose, it does not significantly improve glycated hemoglobin (HbA1c) levels (11). In contrast, propolis, as a natural nutraceutical with historical medicinal applications (12), appears more promising for T2DM intervention. It shows potential for improving insulin resistance, protecting pancreatic β-cell function, and has comparatively better absorption/utilization (13), possibly addressing current treatment limitations.
Propolis (14) is a natural substance collected by bees from plant sources like bark crevices and leaf buds, used by humans since ancient times and documented in pharmacopeias 4 centuries ago (15, 16). It is rich in beneficial bioactive non-nutrients, including flavonoids, polyphenols, and terpenes, with flavonoids being the most abundant and primary bioactive components (17, 18). It finds numerous applications in the treatment of various diseases (13, 19–22). Propolis has numerous applications, including antibacterial, antiviral, and anti-inflammatory effects, improving gut microbiota, promoting wound healing, and immune modulation (22–24).
While previous systematic reviews have investigated propolis effects on specific parameters such as blood glucose or lipids (25–28), they were often limited by a narrow focus on single outcomes or considerable heterogeneity among included populations. Consequently, a comprehensive assessment of its efficacy specifically in patients with T2DM is still lacking. Moreover, existing studies examining the effects of propolis on blood lipids (29–34), blood glucose (31–35), inflammatory markers (31, 32), and oxidative stress markers (35–38) in T2DM have reported inconsistent results. To address these gaps, this study systematically reviewed randomized controlled trials (RCTs) from Chinese and English databases. It aims to comprehensively evaluate the overall effects of propolis supplementation on multiple metabolic indicators in T2DM and to analyze the influence of factors such as dosage and intervention duration on therapeutic outcomes, thereby providing robust evidence to support its clinical application in diabetes management.
Materials and methods
This study was registered with PROSPERO (registration number: CRD42024577722).1 During the compilation of this manuscript, it strictly abided by the guidelines outlined in the Primary Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (39).
Inclusion criteria
Participants: Adults aged ≥18 years diagnosed with T2DM based on clinical criteria (40).
Interventions: The intervention group was treated with propolis (capsules, tablets, etc.).
Control: The control group received a conventional intervention or placebo.
Outcome: The primary outcomes were as follows: lipid indicators, including low-density lipoprotein cholesterol (LDL-C), total cholesterol (TC), triglycerides (TG), and high-density lipoprotein cholesterol (HDL-C); and glycemic markers, namely fasting blood sugar (FBS), glycosylated hemoglobin (HbA1c), and homeostasis model assessment of insulin resistance (HOMA-IR). The secondary outcomes were as follows: inflammatory markers such as C-reactive protein (CRP), tumor necrosis factor alpha (TNF-α), interleukin-6 (IL-6); and oxidative stress markers, including superoxide dismutase (SOD) and malondialdehyde (MDA). The studies must provide data on at least one outcome parameter.
Study design: Randomized controlled trials (RCTs).
Exclusion criteria
(1) Studies on propolis combined with other drugs/active substances; (2) Studies that are replications of published studies; (3) Studies for which the full text or incomplete data were unavailable; (4) Reviews, conference abstracts, animal experimental studies, etc.
Search strategy
Two researchers independently searched nine databases (China National Knowledge Infrastructure (CNKI), Wanfang Data, VIP, SinoMed, PubMed, Cochrane Library, Embase, Scopus, and Web of Science) from inception to 20 May 2025. A hybrid search strategy combining subject headings with free terms was employed. The detailed search strategy is provided in Additional File 1.
Literature screening and data extraction
Two researchers independently conducted literature searches and imported the retrieved records into EndNote 21 reference management software to remove duplicates. Subsequently, titles and abstracts were screened to exclude irrelevant studies. Full-texts were then assessed against the inclusion and exclusion criteria to identify eligible studies. Data extraction was performed independently by the two researchers, with information including publication year, first author, sample size, participant characteristics, propolis dosage, propolis formulation, intervention duration, and outcome measures.
Literature quality assessment
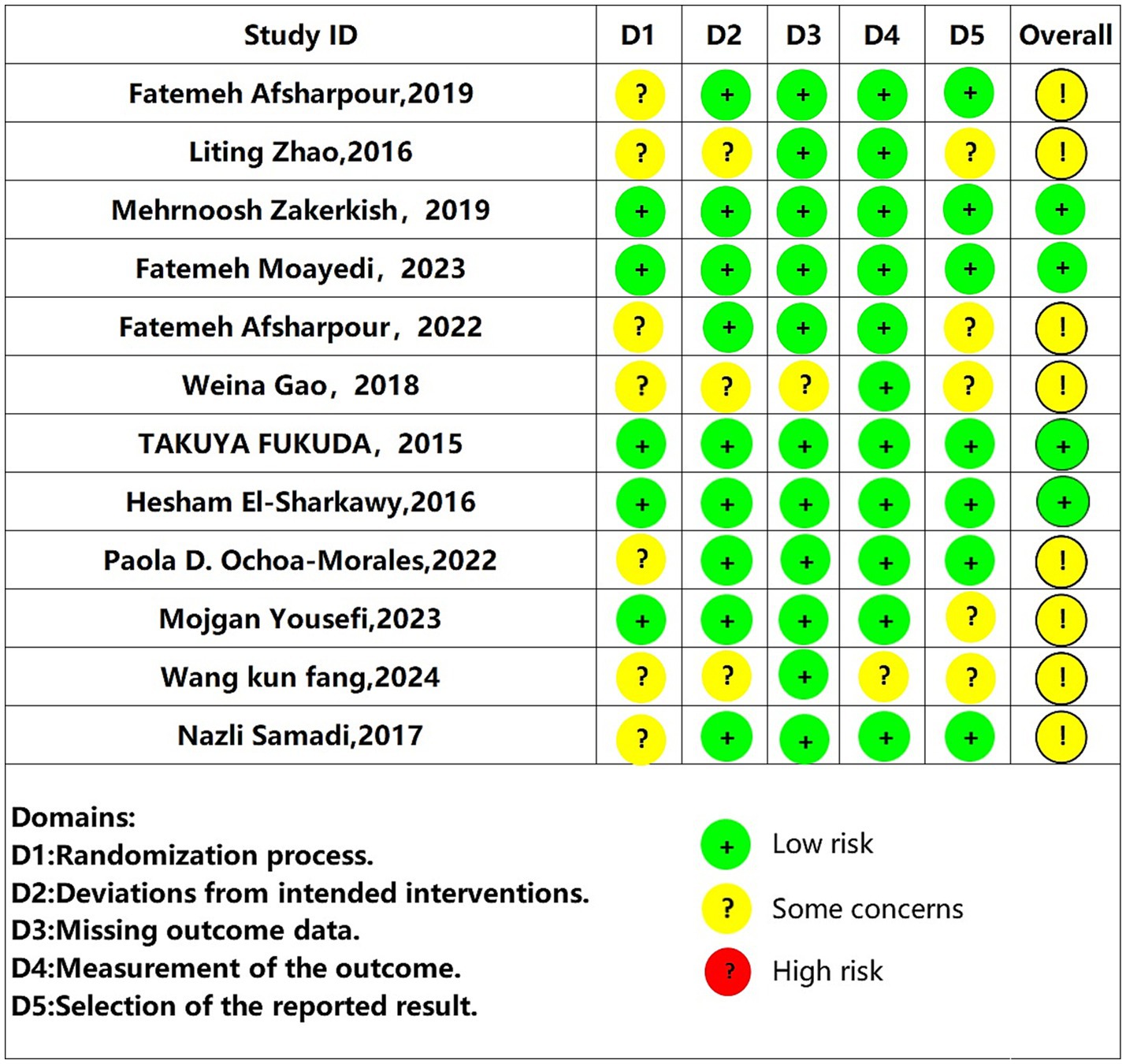
The quality of the included studies was assessed using the Cochrane Risk of Bias tool for Randomized Trials, version 2 (RoB 2) (39). The evaluation dimensions included the randomization process, deviation from the intended interventions, missing outcome data, measurement of outcomes, and selection of reported results. The assessment results were presented in the form of a risk of bias graph. Based on the risk of bias results, each study was categorized as “high risk,” “some concerns,” or “low risk.” In cases of disagreement during this process, a third researcher acted as an arbiter to reach a final consensus.
Evidence quality assessment
The certainty of evidence was evaluated using the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) framework. According to GRADE, the initial quality of evidence from randomized controlled trials (RCTs) was classified as high. This rating could be downgraded to moderate, low, or very low if limitations were identified in any of the five domains: Risk of bias, Inconsistency, Indirectness, Imprecision, or Publication bias. Conversely, evidence quality could be upgraded in cases of substantial effect magnitudes or observed dose–response gradients. Disagreements during assessment were resolved through arbitration by a third researcher to achieve consensus.
Data analysis methods
Meta-analysis of included studies was performed using Review Manager 5.4. Results were presented in forest plots. Heterogeneity was assessed; a fixed-effects model was utilized if p ≥ 0.1 and I2 ≤ 50%; otherwise, a random-effects model was adopted. To identify potential sources of heterogeneity, subgroup analyses were performed based on intervention dosage and duration. A sensitivity analysis, in which each study was sequentially removed, confirmed the robustness of the pooled estimates. Publication bias was assessed with funnel plots and Egger’s test for outcomes involving 10 or more studies; for outcomes with fewer studies, these tests were considered underpowered. All outcome measures were standardized continuous variables, and the effect size was expressed as the weighted mean difference (MD) with 95% confidence interval (CI). A p-value less than 0.05 was considered statistically significant.
Results
Literature search results
A total of 1,086 relevant literature was obtained from the preliminary search database, and after excluding 489 duplicate literatures, 597 literatures remained. After the titles and abstracts were assessed, 564 studies that failed to meet the inclusion criteria were eliminated. Yielding 23 potentially eligible publications. Upon further evaluation of the full texts, 11 publications were excluded. Consequently, a total of 12 publications were incorporated into the final analysis. The details of the literature selection process and outcomes are presented in Figure 1.
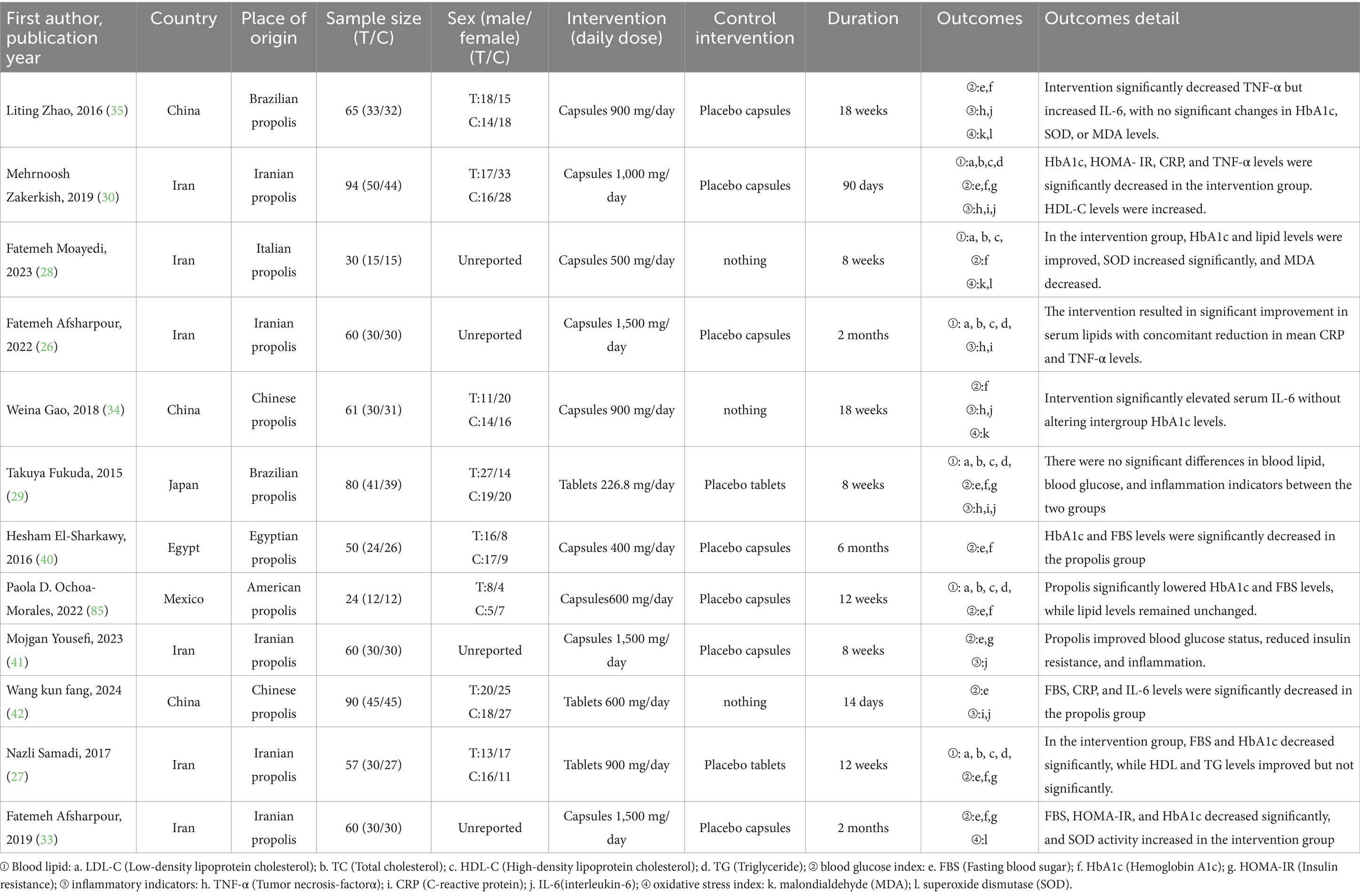
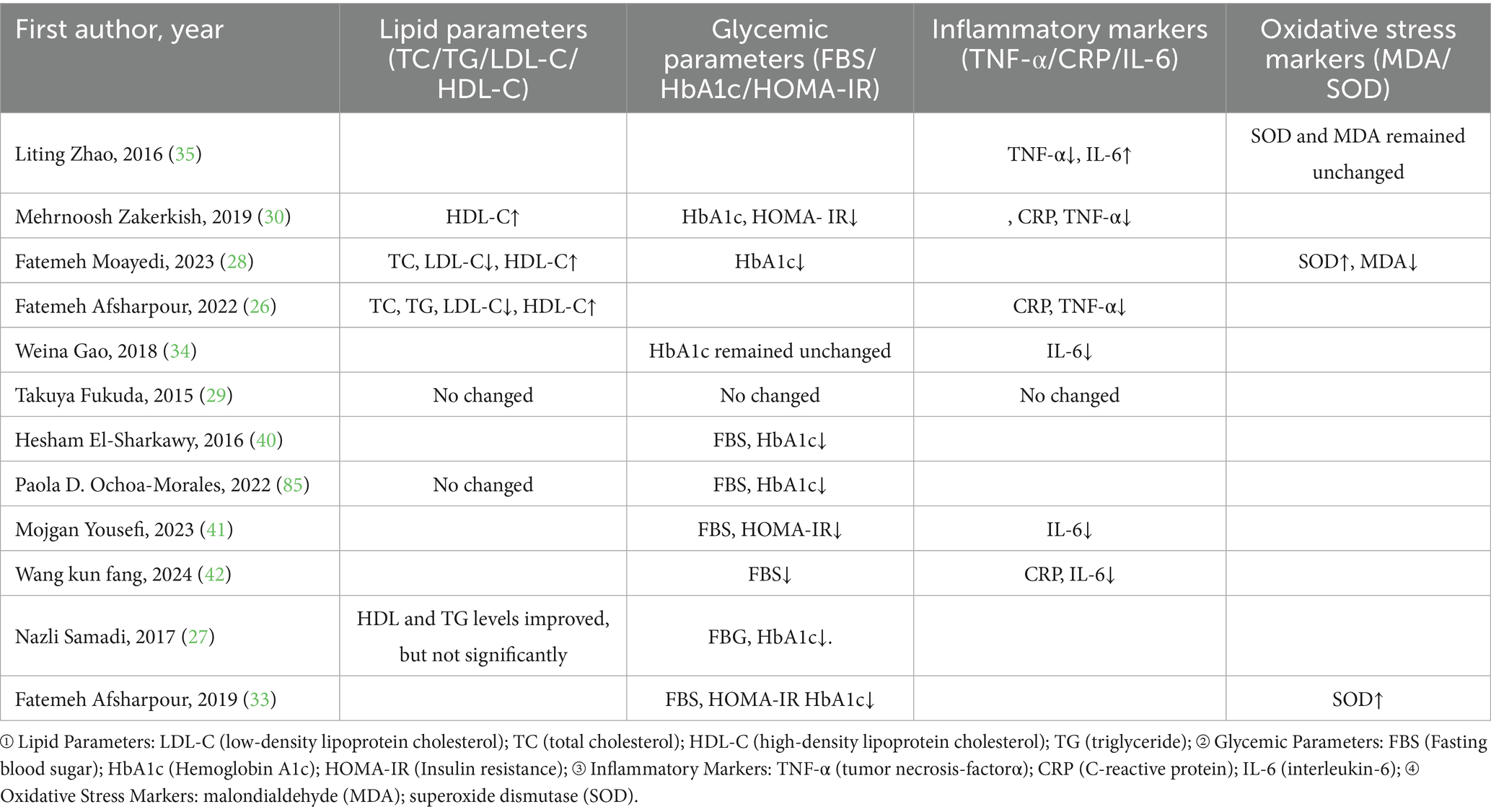
Basic characteristics of the included studies
This study included a total of 12 trials involving 731 patients, comprising 371 in the propolis experimental group and 360 in the placebo control group. All included studies provided descriptions of the baseline characteristics for both groups and reported the outcome measures, ensuring comparability. The basic information of the included studies is presented in Tables 1, 2.
Methodological quality of the included studies
The quality of the methodologies employed in the 12 included studies was systematically reviewed via the Cochrane Risk of Bias Assessment Tool, version 2 (RoB 2) (39). All studies were randomized controlled trials (RCTs), but evidence of bias was identified in their randomization procedures. Notably, five studies (28–30, 40, 41) implemented detailed randomization methods with allocation concealment. The methodological quality assessment results are presented in Figure 2 and Table 3.
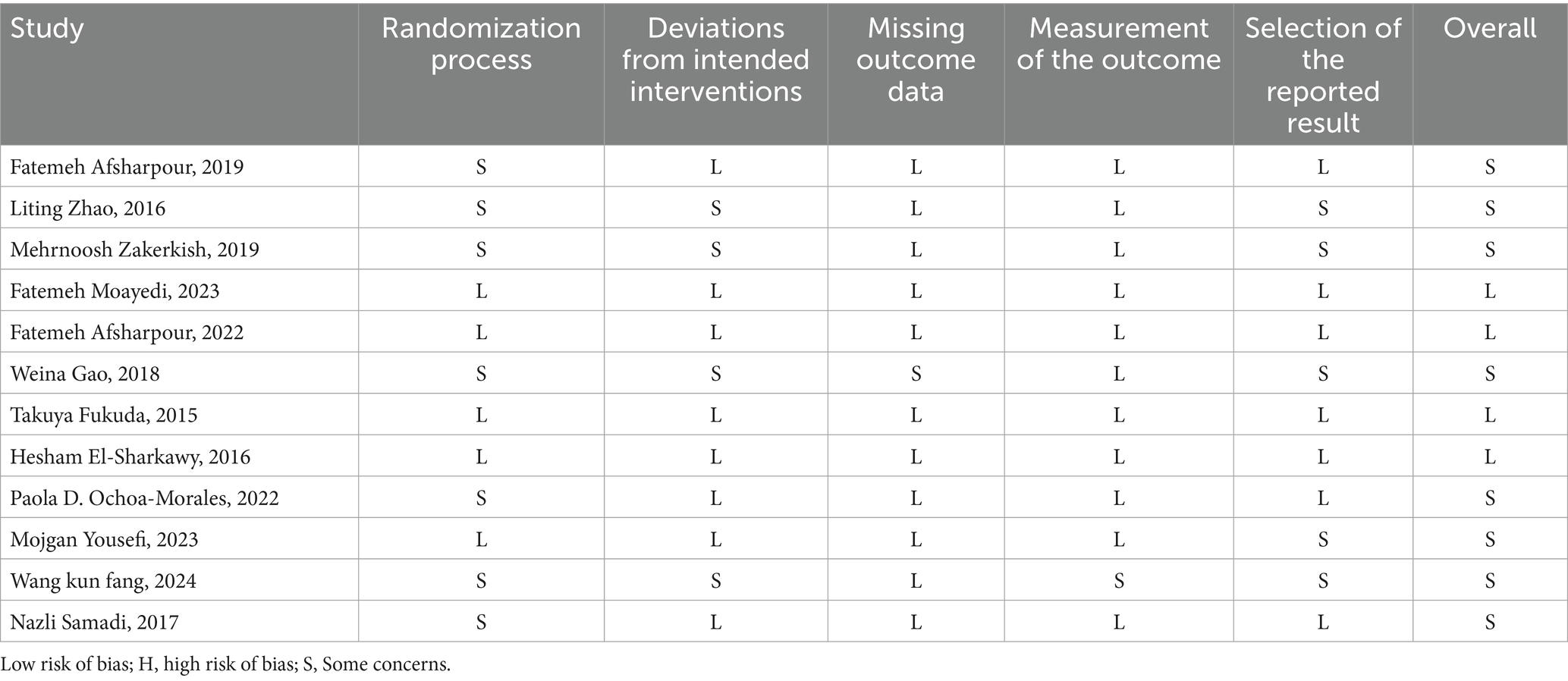
Table 3. Risk of bias summary of the included randomized controlled trials on propolis supplementation for type 2 diabetes mellitus.
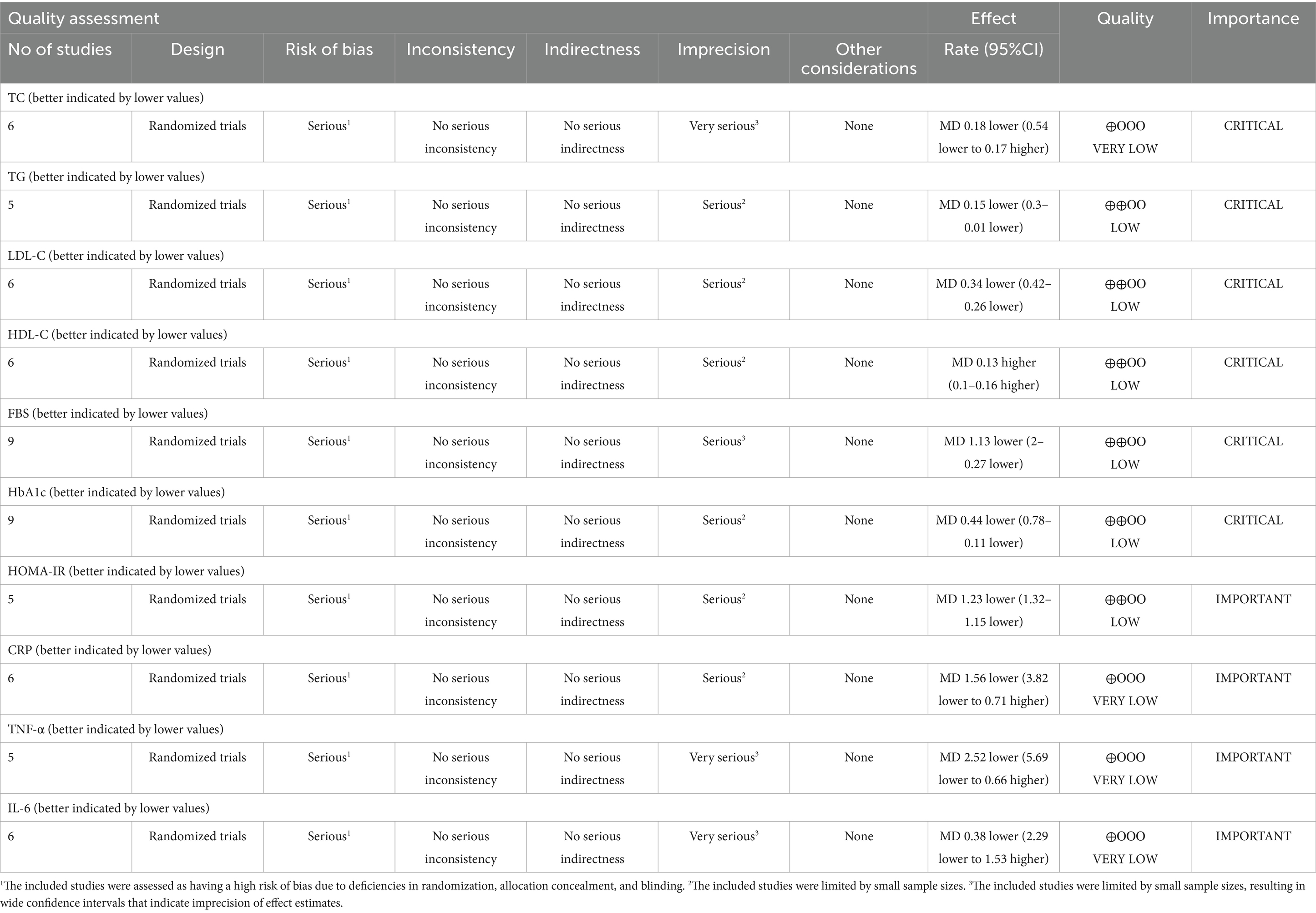
Quality of evidence
The certainty of evidence for propolis supplementation’s effects on metabolic and inflammatory biomarkers was evaluated using the GRADE framework. Evidence for TG, LDL-C, HDL-C, FBS, HbA1c, and HOMA-IR was rated as low certainty, primarily due to serious risk of bias and imprecision. For TC, IL-6, CRP, and TNF-α, the evidence was of very low certainty, attributed to very serious imprecision (wide confidence intervals crossing the null value) alongside serious risk of bias, precluding definitive conclusions. Key downgrading factors included inadequate randomization, lack of allocation concealment, insufficient blinding, and small sample sizes. The full GRADE evidence profile is detailed in Table 4.
Effect of propolis on blood lipids in patients with T2DM
A total of six studies (30–34, 42) reported the effect of propolis on total cholesterol (TC) in patients with T2DM. Heterogeneity was observed among these studies (p < 0.00001, I2 = 86%). Thus, a random-effects model was employed for the analysis. The pooled results showed no significant improvement in TC levels following propolis intervention (MD = −0.18, 95% CI: −0.54–0.17, p = 0.32). Further subgroup analysis revealed that neither intervention dosage nor duration significantly influenced TC outcomes (Figures 3a,b and Table 5).
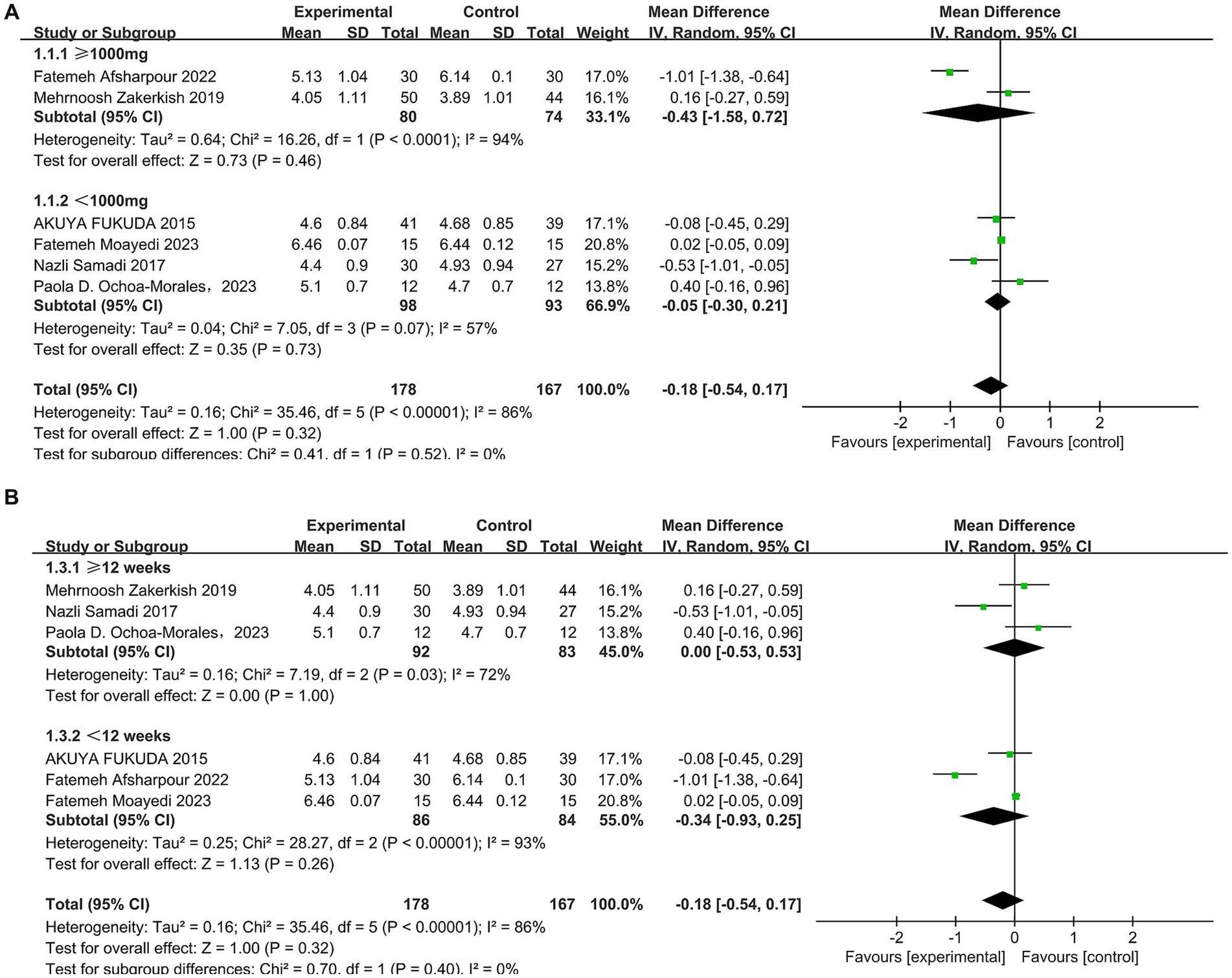
Figure 3. Subgroup analysis of propolis intervention on TC in T2DM patients stratified by dose (A) and duration (B).
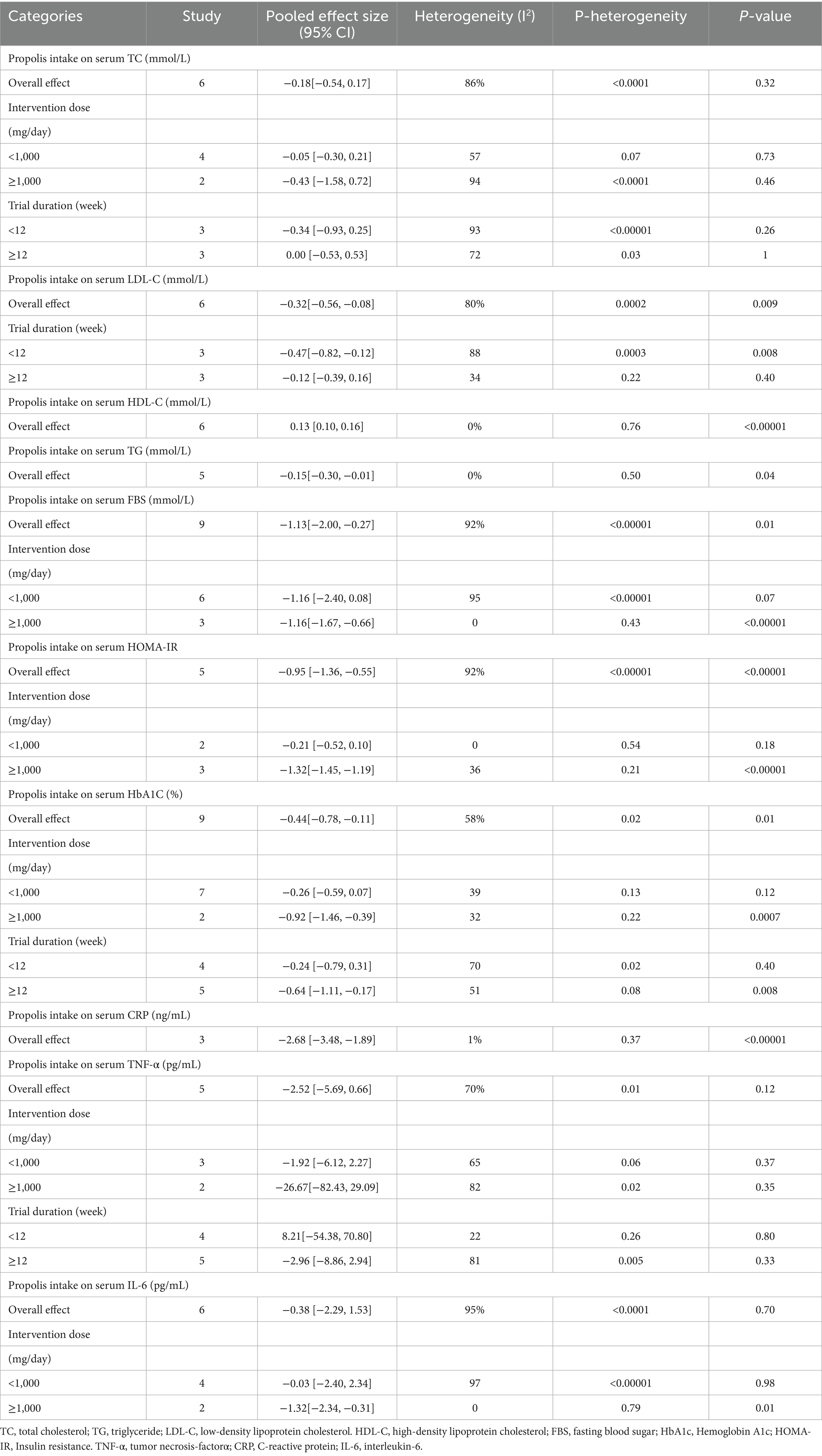
Table 5. Risk of bias summary of the included randomized controlled trials on propolis supplementation for type 2 diabetes mellitus.
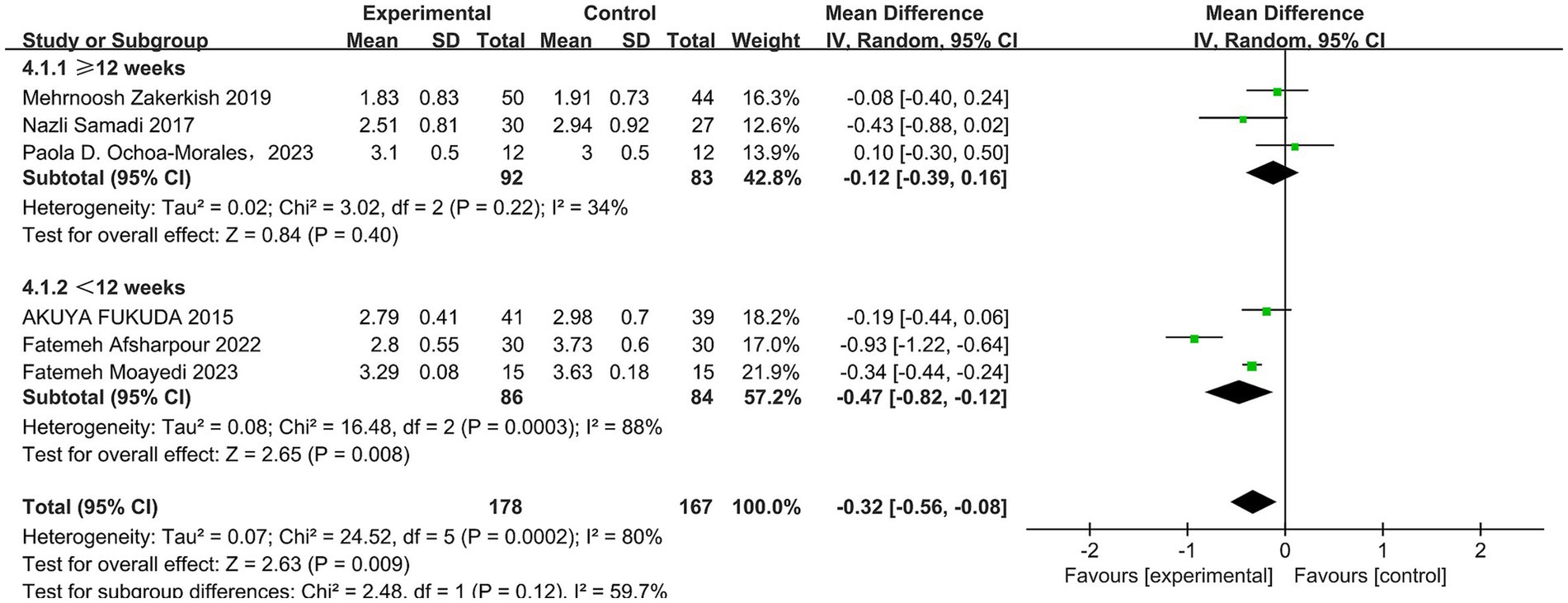
A total of six studies (30–34, 42) reported the effect of propolis on low-density lipoprotein cholesterol (LDL-C) in patients with T2DM. Heterogeneity was observed among these studies (p = 0.0002, I2 = 80%). Thus, a random-effects model was employed for the analysis. The pooled results showed propolis significantly reduced LDL-C levels, with statistical significance (MD = −0.32, 95% CI: −0.56 to −0.08, p = 0.009). Subgroup analysis revealed that when the intervention duration was less than 12 weeks, propolis significantly lowered LDL-C levels in T2DM patients (MD = −0.47, 95% CI: −0.82 to −0.12, p = 0.0008) (see Figure 4 and Table 5).
A total of six studies (30–34, 42) reported the effect of propolis on high-density lipoprotein cholesterol (HDL-C) in T2DM patients, and there was no significant heterogeneity among the studies (p = 0.76, I2 = 0%). A fixed effect model was used, and the results revealed that propolis could improve HDL-C levels in T2DM patients, with the observed difference reaching statistical significance (MD = 0.13, 95% CI: 0.10–0.16, p < 0.00001) (see Figure 5 and Table 5).
A total of five studies (30, 31, 33, 34, 42) reported the effect of propolis on triglyceride (TG) levels in T2DM patients, and there was no significant heterogeneity among the studies (p = 0.50, I2 = 0%). The differences were statistically significant when a fixed effects model was used (MD = −0.15, 95% CI: −0.30 to −0.01, p = 0.04) (see Figure 6 and Table 5).
Effect of propolis on blood glucose in T2DM patients
In total, nine studies (31, 33–35, 37, 41–44) evaluated the effects of propolis on fasting blood sugar (FBS) in T2DM patients. Substantial heterogeneity was observed (p < 0.00001, I2 = 92%). Thus, a random-effects model was used for the meta-analysis. The results indicated that propolis significantly reduced FBS levels in T2DM patients (MD = −1.13, 95% CI: −2.0 to −0.27, p = 0.01). Subgroup analysis revealed a dose-dependent effect: a significant reduction in FBS was observed at doses ≥ 1,000 mg/day (MD = −1.16, 95% CI: −1.67 to −0.66, p < 0.00001). To further explore sources of heterogeneity, a subgroup analysis was performed for studies using doses <1,000 mg/day, stratified by geographic region. Among studies conducted in the Middle East, which showed low heterogeneity (I2 = 22%), propolis significantly improved FBS (MD = −0.99, 95% CI: −1.67 to −0.32, p = 0.004). In contrast, trials from East Asia showed no significant effect on FBS (MD = −0.93, 95% CI: −3.38–1.52, p = 0.46) (Figures 7a,b and Table 5).
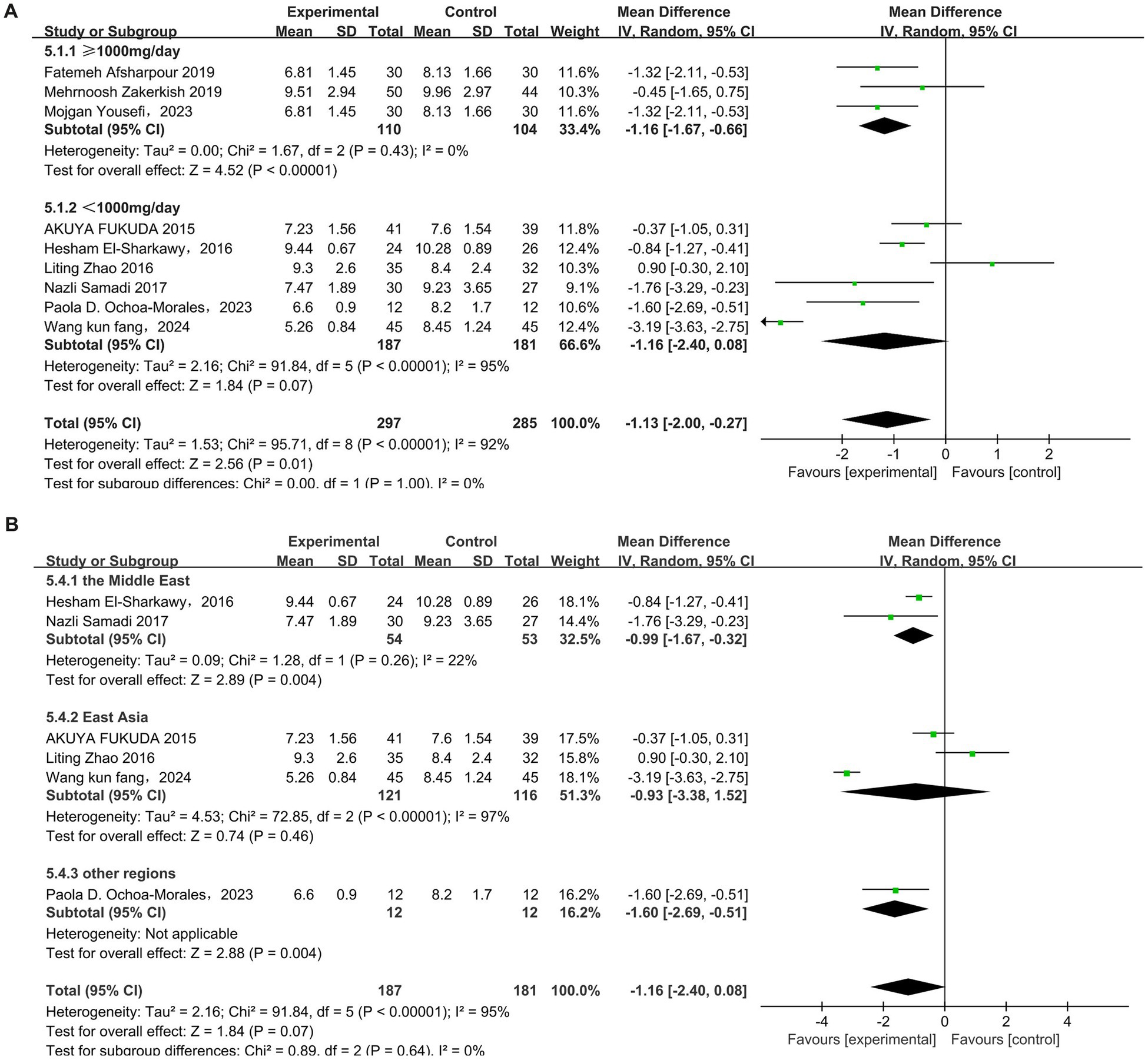
Figure 7. Subgroup analysis of propolis intervention on FBS in T2DM patients stratified by dose (A) and geographic region (B).
A total of five studies (31, 33–35, 43) reported the effect of propolis on insulin resistance (HOMA-IR) in T2DM patients, with heterogeneity among the studies (p < 0.00001, I2 = 92%), and a random-effects model was used. The results revealed that propolis can improve the level of HOMA-IR in T2DM patients, and the difference was statistically significant (MD = −0.95, 95% CI: −1.36 to −0.55, p < 0.00001). Subgroup analysis further showed a significant reduction only at doses ≥ 1,000 mg/day (MD = −1.32, 95% CI: −1.45 to −1.19, p < 0.00001) (Figure 8 and Table 5).
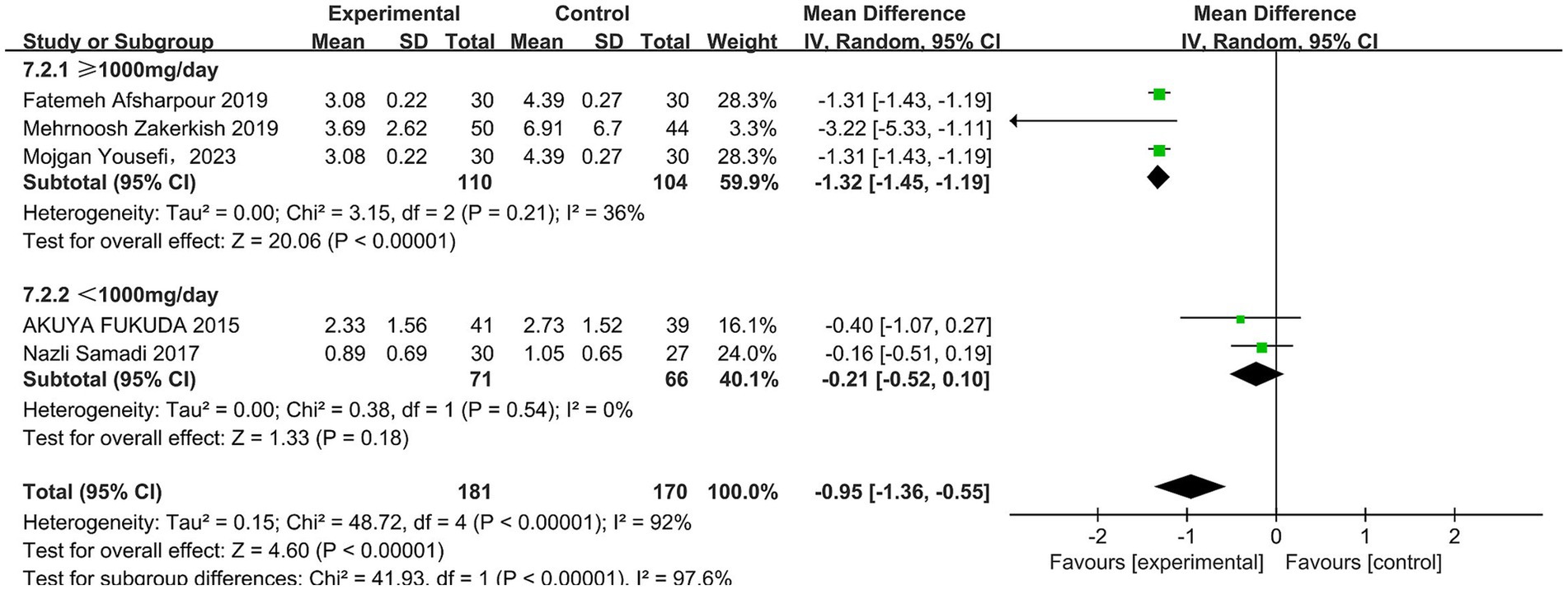
Figure 8. Subgroup analysis of propolis intervention on HOMA-IR in T2DM patients stratified by dose.
In total, nine studies (31–37, 41, 42) reported the effect of propolis on glycosylated hemoglobin (HbA1c) in T2DM patients. Significant heterogeneity was detected across the studies (p = 0.02, I2 = 58%), and a random-effects model was used, which showed that propolis can significantly reduce the HbA1c levels (MD = −0.44, 95%CI: −0.78 to −0.11, p = 0.01). Subgroup analyses revealed a dose- and time-dependent effect: significant reductions were observed with doses ≥ 1,000 mg/day (MD = −0.92, 95% CI: −1.46 to −0.39, p = 0.0007) and durations ≥12 weeks (MD = −0.64, 95% CI: −1.11 to −0.17, p = 0.008) (Figure 9 and Table 5).
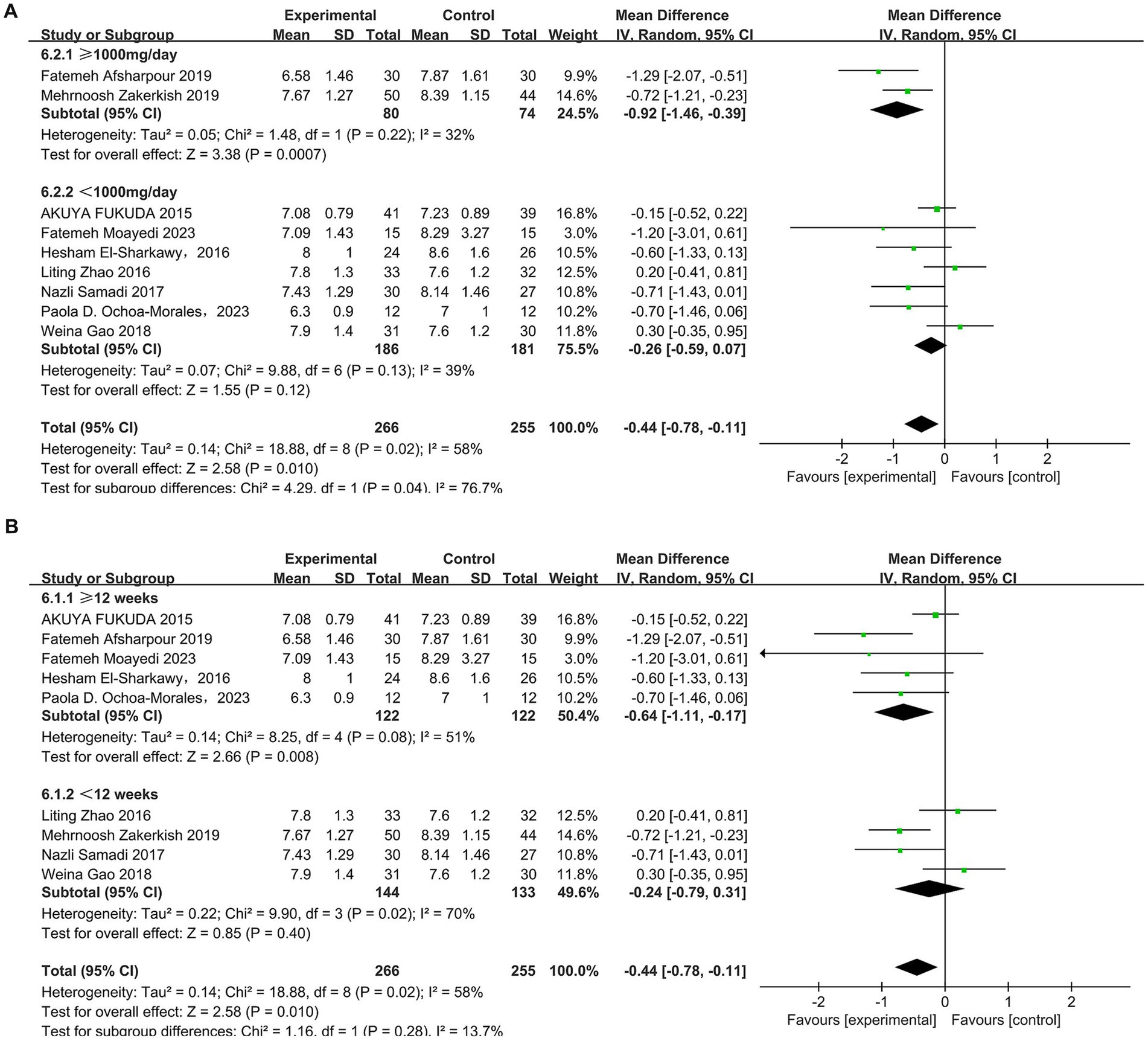
Figure 9. Subgroup analysis of propolis intervention on HbA1c in T2DM patients stratified by dose (A) and duration (B).
Effect of propolis on inflammatory indicators in T2DM patients
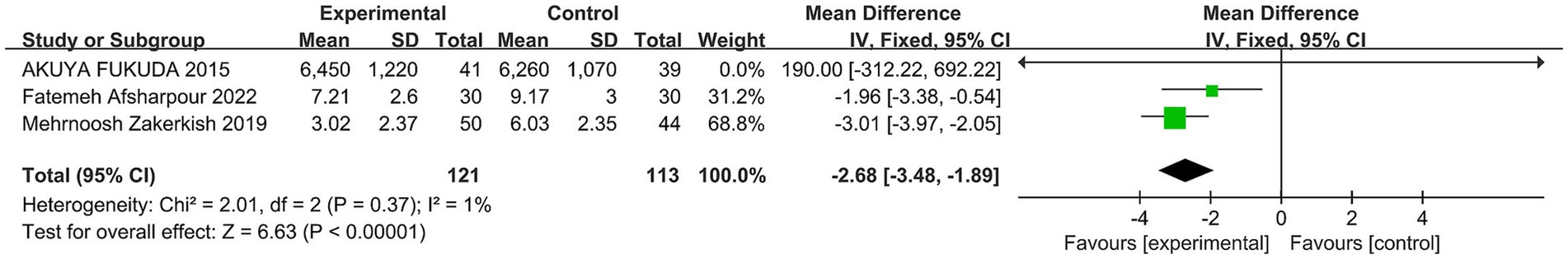
A total of four studies (30, 33, 34, 44) reported the effect of propolis on C-reactive protein (CRP) in T2DM patients. One study (44) was excluded from the meta-analysis due to the inclusion of inflammatory/infective patients, which could bias results. The remaining three showed low heterogeneity (p = 0.37, I2 = 1%), so a fixed-effect model was used. Meta-analysis found propolis significantly reduced CRP (MD = −2.68, 95% CI: −3.48 to −1.89, p < 0.00001) (Figure 10 and Table 5).
In total, five studies (30, 33, 34, 36, 37) reported the effect of propolis on TNF-α in T2DM patients. Significant heterogeneity was detected (p = 0.01, I2 = 70%); a random effects model was used. Meta-analysis showed no statistically significant effect of propolis on TNF-α levels (MD = −2.52, 95% CI: −5.69–0.66, p = 0.12). Subgroup analyses for intervention duration and dosage also found no significant differences (Figure 11 and Table 5).
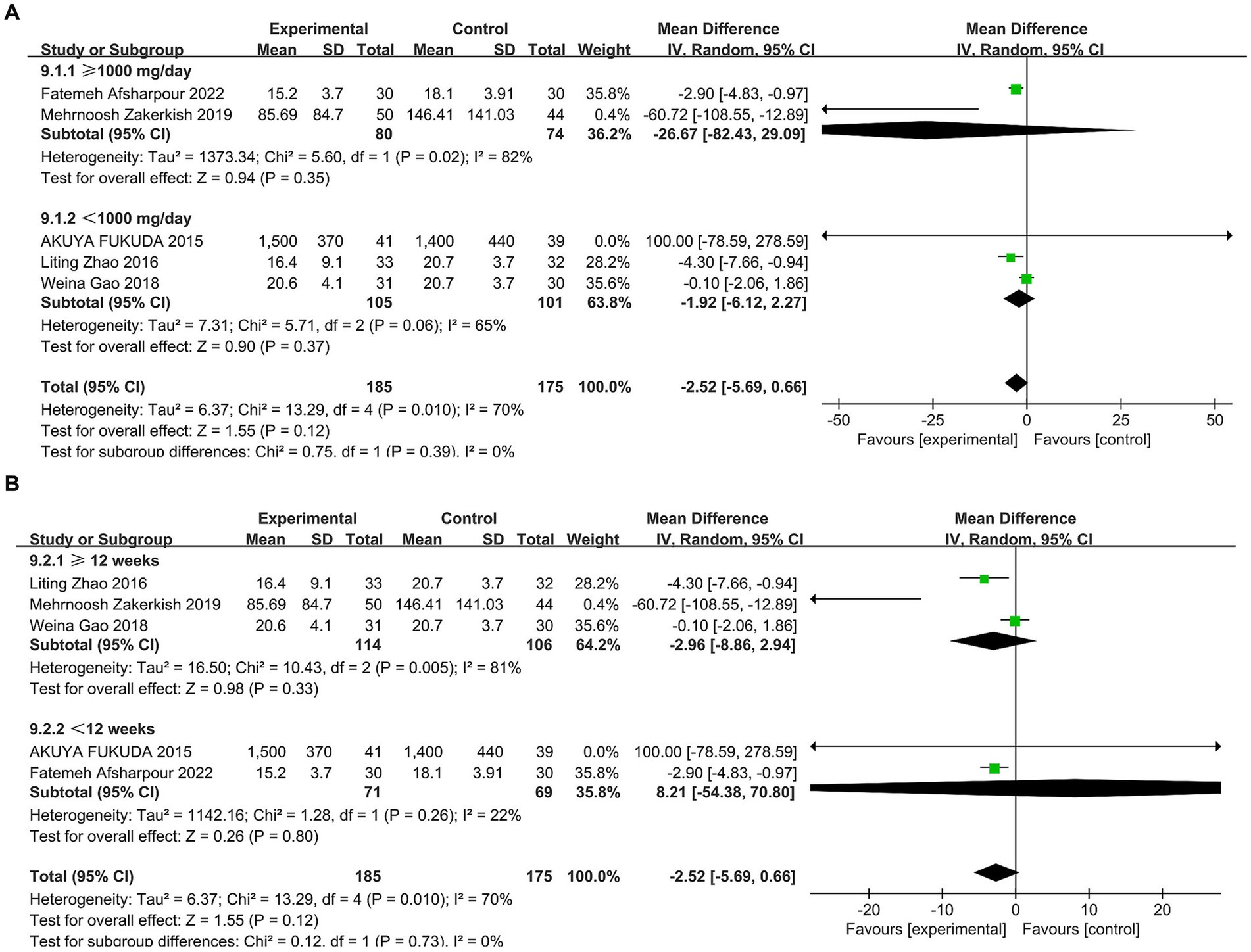
Figure 11. Subgroup analysis of propolis intervention on TNF-α in T2DM patients stratified by dose (A) and duration (B).
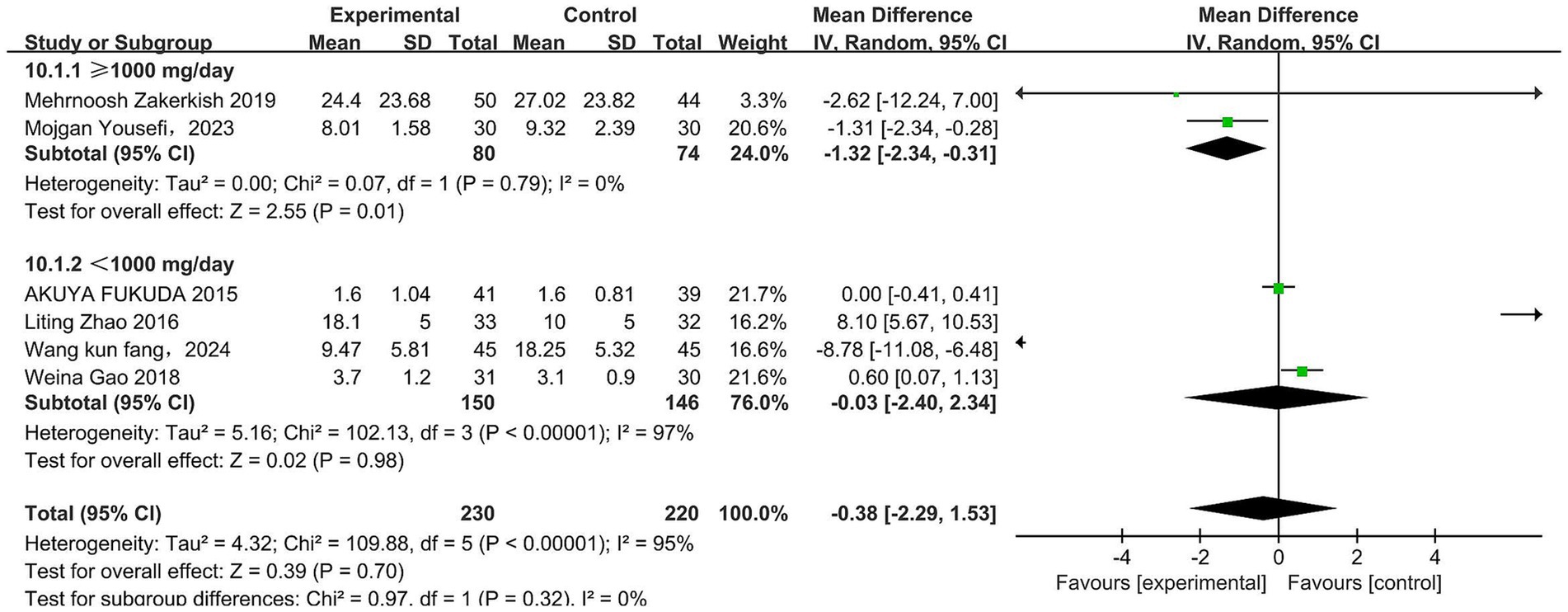
In total, six studies (33, 34, 36, 37, 43, 44) reported the effect of propolis on IL-6 in T2DM patients. Significant heterogeneity was detected (p < 0.00001, I2 = 95%). A random effects model was used, which revealed that propolis did not significantly alter IL-6 levels (MD = −0.38, 95% CI −2.29–1.53, p = 0.70). However, subgroup analysis showed a significant reduction at doses ≥1,000 mg/day (MD = −1.32, 95% CI −2.34 to −0.31, p = 0.01) (Figure 12 and Table 5).
Effect of propolis on the oxidative stress status of T2DM patients
A total of two studies (36, 37) found no effect of propolis on MDA levels in T2DM patients. Three studies (35–37) examined SOD levels, but unit differences precluded direct comparison. One study (35) reported a significant increase in SOD post-intervention, whereas the other two (36, 37) found no significant change.
Sensitivity analysis
Sensitivity analysis by sequential exclusion revealed stable pooled effects for TC, TG, HDL-C, LDL-C, FBS, HbA1c, HOMA-IR, CRP, and TNF-α, with confidence intervals remaining above the clinical significance threshold, confirming high robustness. However, the result for IL-6 demonstrated marked sensitivity. The initial meta-analysis, including all studies, showed no significant effect of propolis on IL-6 levels. However, after the removal of the study by Zhao et al. (37), the pooled effect became statistically significant (MD = −1.84, 95% CI −3.53 to −0.15, p = 0.03), suggesting a potential role of propolis in reducing IL-6. This study was identified as a key source of heterogeneity that might have masked the anti-inflammatory effect of propolis. Nevertheless, considerable heterogeneity persisted among the remaining studies (I2 = 94%), which precludes firm conclusions regarding its effect on IL-6.
Discussion
This meta-analysis of 12 randomized controlled trials (RCTs) comprising 731 participants demonstrates that propolis supplementation significantly improves lipid profiles [low-density lipoprotein cholesterol (LDL-C), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C)], glycemic control [fasting blood sugar (FBS), insulin resistance (HOMA-IR), hemoglobin (HbA1c)], and inflammation [C-reactive protein (CRP)] in patients with T2DM. However, current evidence is insufficient to confirm a significant effect of propolis on oxidative stress markers. This finding highlights an important direction for future research and warrants further in-depth investigation.
The present study demonstrated a downward trend in FBS, HOMA-IR, and HbA1c levels following propolis intervention, which is partially consistent with the conclusions of Karimian et al. (28). A key distinction, however, is that their research failed to detect a significant change in HOMA-IR and did not investigate the influence of dosage and intervention duration. This study not only revealed a significant reduction in HOMA-IR but also identified a dose-dependent effect, with the most pronounced improvements observed at dosages of 1,000 mg/day or higher. Similarly, while Hallajzadeh et al. (25) reported benefits for glycemic and inflammatory markers, they found no improvement in lipids and did not analyze dosage. In contrast, this study demonstrated concurrent improvements in lipid profiles, glycemic control, and inflammatory markers, and clarified the modulatory roles of both dosage and duration. Unlike previous meta-analyses (25–28), this study provides a more comprehensive evaluation by including oxidative stress and inflammatory markers. Subgroup analyses revealed that propolis at ≥1,000 mg/day significantly improved FBS, HOMA-IR, HbA1c, and IL-6 levels, with particularly pronounced HbA1c improvement at ≥12 weeks. These findings support the use of propolis as an adjunctive therapy in T2DM management.
Effects of propolis on blood lipids in T2DM patients
This meta-analysis demonstrated that propolis supplementation significantly reduced LDL-C and TG while increasing HDL-C, but had no significant effect on TC. Compared with previous meta-analyses, the results of the present study exhibit certain discrepancies. For instance, Salehi-Sahlabadi et al. (45) reported that propolis significantly reduced TG and increased HDL-C, but had no effect on LDL-C. In contrast, two other meta-analyses (25, 46) reported no significant effects of propolis on any lipid parameters. This discrepancy is likely attributable to the differing study populations; this study was limited to patients with T2DM, whereas prior studies included non-diabetic individuals.
Currently, the mechanisms of how propolis regulates lipids are not fully clear. Lipid peroxidation, a key outcome of oxidative stress, may be mitigated by propolis flavonoids, which protect lipids from oxidative damage through multiple pathways (47). Propolis can promote the expression of the ABCA1 and ABCG1 genes, promote reverse cholesterol transport, and stimulate HDL particle formation, thereby increasing HDL-C levels (48). Study (49) indicated that upregulation of ABCA1 may be a crucial way to improve HDL-C. Propolis contains polyphenols that inhibit intestinal cholesterol absorption, reduce ox-LDL, and downregulate CD36 receptor expression, thereby decreasing macrophage uptake of ox-LDL and suppressing atherosclerotic plaque formation (13, 48). Furthermore, propolis activates PPARα in the liver to balance lipid metabolism (50), and its active component, caffeic acid phenethyl ester (CAPE), can upregulate PPARα and downregulate PPARγ to relieve fat accumulation and metabolic disorders (51).
Effect of propolis on blood glucose in T2DM patients
This meta-analysis demonstrates that propolis supplementation significantly improves glycemic control in patients with T2DM. Subgroup analyses revealed that intervention dosage and duration are critical effect modifiers. Significant reductions in FBS, HOMA-IR, and HbA1c were observed only at dosages ≥1,000 mg/day, while a clinically meaningful HbA1c reduction required an intervention duration of ≥12 weeks. Given that elevated HbA1c is a primary risk factor for diabetic microvascular complications (52, 53), the observed HbA1c-lowering effect suggests that propolis, as an adjunctive therapy, holds potential for improving long-term patient prognosis. One study (25) observed reductions in FBS and HbA1c levels following propolis supplementation, but no improvement in HOMA-IR, which is inconsistent with our findings. This discrepancy may be attributed to the heterogeneity in metabolic characteristics of the study populations. Propolis enhances glucose uptake by increasing insulin sensitivity in skeletal muscle cells, boosting GLUT4 activity, and activating the PI3K and AMPK pathways (54). It may also stimulate insulin secretion or sensitivity and inhibit intestinal α-glucosidase to slow carbohydrate digestion (55, 56). Compounds like galangin and pinocembrin modulate glucose metabolism in IR-HepG2 cells, improving insulin resistance (57), while total flavonoids enhance HK and PK activity, promoting glucose absorption and glycogen synthesis (58, 59).
Effect of propolis on inflammatory indicators in T2DM patients
This meta-analysis found that propolis supplementation significantly lowers CRP levels in T2DM patients, but showed no significant overall effect on IL-6 or TNF-α. Notably, subgroup analysis revealed a clear dose−response relationship: IL-6 levels were significantly reduced at propolis doses ≥1,000 mg/day. Compared with previous meta-analyses (25, 60, 61), these findings are partially consistent for CRP but differ for IL-6 and TNF-α. Specifically, this study found that higher-dose propolis significantly reduced IL-6, aligning with the findings of Gholami et al. (61). However, no significant change in TNF-α levels was observed in this analysis.
Several factors may account for these discrepancies. First, the present analysis was strictly limited to T2DM patients, whereas prior studies (25, 60, 61) included non-diabetic individuals and healthy participants. As noted in study (61), the anti-inflammatory effects of propolis appear to be population-specific, with more pronounced reductions in IL-6 and TNF-α observed in Asian cohorts compared to American ones—a difference potentially attributable to geographical variations in propolis composition. This notion is supported by research (62) indicating that although both Chinese and Brazilian propolis possess anti-inflammatory properties, they differ significantly in the content of key active compounds, such as total flavonoids. Furthermore, the analysis of TNF-α in this study included only five trials, rendering it underpowered compared to the meta-analysis by Gholami et al. (61), which pooled data from 13 studies. Therefore, these results should be interpreted with caution and warrant further validation in future high-quality primary studies.
The anti-inflammatory effects of propolis are attributed to the synergistic regulation of multiple signaling pathways. A key mechanism involves the inhibition of inducible nitric oxide synthase (iNOS) by propolis, which reduces excess nitric oxide (NO) production and mitigates oxidative/nitrosative stress and subsequent tissue damage (13). The principal component, caffeic acid phenethyl ester (CAPE), is central to this action, directly suppressing iNOS transcription via NF-κB binding sites (63). CAPE, along with other flavonoids and phenolic acids, also downregulates LOX/COX-1/COX-2 in the arachidonic acid pathway, thereby blocking the synthesis of pro-inflammatory mediators like prostaglandins and leukotrienes (64, 65). Additionally, CAPE reduces pro-inflammatory cytokine mRNA levels in activated macrophages, alleviating chronic inflammation (66).
Effect of propolis on oxidative stress in T2DM patients
The limited number of studies on oxidative stress markers prevents definitive conclusions regarding propolis’s antioxidant effects. Existing evidence remains inconsistent, with one systematic review (25) reporting no benefit, while others (27, 67) suggest positive effects. This heterogeneity may be largely attributed to variations in dosage and methodology. Subgroup analyses from previous trials (27, 67) indicated that propolis supplementation ≥1,000 mg/day significantly reduces MDA and increases SOD activity, whereas lower doses exhibit no effect, thereby highlighting dosage as a critical moderating factor. Methodological variations further complicate the comparability of results. Although all included studies (35–37) employed the thiobarbituric acid (TBA) colorimetric assay to quantify MDA, this method is known to lack specificity. The TBA reagent reacts non-specifically with other serum aldehydes, potentially leading to a systematic overestimation of MDA concentrations (68). Therefore, future studies should prioritize the standardization of more specific detection methods to enhance the reliability and comparability of research findings.
Phenolic compounds, established as the primary active and non-nutritive constituents of propolis, exhibit inherent antioxidant properties (13). These compounds mitigate oxidative stress through multiple mechanisms: they inhibit ROS-generating enzymes (e.g., phospholipase A2), scavenge free radicals, and enhance the overall antioxidant capacity (25, 47). Consequently, propolis supplementation leads to reduced MDA levels and elevated activity of antioxidant enzymes, including SOD, catalase (CAT), and glutathione peroxidase (GSH-Px), thereby alleviating oxidative stress (55, 69). Furthermore, flavonoids in propolis activate the antioxidant regulator Nrf2, bolstering cellular defenses (70, 71). Polyphenolic components such as CAPE contribute to ROS reduction by inhibiting the NF-κB pathway, which aids in protecting endothelial function (72), and by suppressing the PI3K/Akt/mTOR pathway to downregulate LOX-1 and p38 MAPK, thereby attenuating oxidative damage (73).
In recent years, non-nutrient bioactive compounds have garnered significant attention for their potential in preventing and managing diabetes (74). These compounds, which are prevalent in plant-based foods and herbs, are structurally distinct from traditional nutrients and are typically soluble in water or ethanol (75). A research team (75) proposed the “theoretical model of family nurse diet therapy,” emphasizing that polyphenols and flavonoids act synergistically to prevent and treat chronic diseases via anti-inflammatory, antioxidant, and metabolic regulatory pathways. Supporting this, additional research (70) confirmed that diets rich in polyphenolic non-nutrients can modulate metabolism and ameliorate oxidative stress, thereby helping prevent hyperlipidemia.
This theoretical framework underpins the clinical application of propolis. As a natural product abundant in polyphenols and flavonoids, propolis has generated considerable interest owing to its notable antioxidant (76), anti-inflammatory (77), anticancer (78), and antibacterial properties (79). Its efficacy stems from the synergistic interactions among its non-nutritive components, such as flavonoids and phenolic acids (73), which align closely with the core principles of the “theoretical model of family nurse diet therapy.” This alignment not only strengthens the rationale for using propolis clinically but also underscores the potential of non-nutrient components in developing natural therapeutics for diabetes.
Regarding safety, propolis, as a resinous substance, exhibits a relatively low incidence of allergic reactions. A large-scale study involving 2,007 cases reported that only 3.8% of participants experienced allergic symptoms (80). In the present analysis, two studies (36, 37) documented allergic events, leading to the withdrawal of six participants due to propolis-related allergies. The primary allergens identified are caffeic acid and its esters (81). Fortunately, bacterial biotransformation techniques have been developed to effectively remove these allergenic compounds (82), indicating that advances in processing technology may further enhance the safety profile of edible propolis products.
Practical implications
Propolis, a natural product abundant in non-nutritive bioactive components, demonstrates potential for improving glycemic control, lipid profiles, and inflammatory markers in T2DM patients. Notably, elevated CRP levels constitute an independent risk factor for cardiovascular mortality, irrespective of diabetic status (83). The significant reduction in CRP levels associated with propolis supplementation suggests its promise as a novel adjunctive strategy for the prevention and management of both diabetes and cardiovascular disease.
This study indicates that the effects of propolis are dose- and time-dependent, with superior outcomes observed at higher doses (≥1,000 mg/day) and longer intervention durations (≥12 weeks). Consequently, for patients with inadequate glycemic control, optimizing propolis dosage and treatment duration under medical supervision may enhance therapeutic efficacy. Such individualized regimens should account for patient-specific factors, including diet, physical activity, concomitant medications, and the pharmacokinetic properties of its bioactive compounds.
Although generally safe, propolis can trigger allergic reactions in susceptible individuals (80). Pre-use allergy screening and consultation with a healthcare provider are recommended. Future research should prioritize elucidating the mechanisms of action of key bioactive constituents, establishing precise dose–response relationships, and evaluating long-term safety. To improve the synthesis of future evidence, we recommend that RCTs on propolis undergo prospective registration and adopt standardized outcome sets with uniform measurement units to reduce methodological heterogeneity.
Strengths and limitations
To clarify the comprehensive efficacy of propolis in the management of T2DM and to address the limitations of previous research, this study conducted a systematic update and in-depth analysis. We searched both Chinese and English databases and included 12 of the latest RCTs. The quality of the included studies was assessed using the Cochrane Risk of Bias tool two. This study provides a systematic and multi-faceted review of propolis intervention in T2DM, assessing its impact not only on glycemic control but also on dyslipidemia, inflammation, and oxidative stress. By situating the findings within a theoretical framework focusing on non-nutritive compounds in chronic disease management, the study offers novel mechanistic insights into the metabolic benefits of propolis. These results not only strengthen the scientific basis for incorporating propolis into diabetes care but also have practical implications for this theoretical model in the context of chronic disease management.
The study also has several limitations. Significant heterogeneity among the included studies—stemming from variations in propolis source, dosage, intervention duration, and sample size—persisted despite statistical adjustments. The feasibility of meta-analysis for oxidative stress markers and the assessment of publication bias were precluded by an insufficient number of studies. Moreover, the generalizability of this study may be limited by the geographical homogeneity of the included research, most of which originated from Iran (30–32, 34, 35). Given that the chemical composition and biological activity of propolis vary with geographical and botanical origin (84), caution should be exercised when extrapolating these findings to propolis from other regions. The applicability of these results to other populations and healthcare settings warrants further validation.
Conclusion
This study demonstrates that propolis significantly improves lipid, glycemic, and inflammatory parameters in patients with T2DM. These metabolic benefits are enhanced at doses ≥1,000 mg/day or intervention durations ≥12 weeks. Although no significant effect on oxidative stress markers was observed (likely due to methodological limitations such as study heterogeneity and limited sample sizes), the antioxidant potential of propolis should not be disregarded. Given the limited number of studies and the inability to assess publication bias, these findings should be interpreted cautiously. Further large-scale, multicenter randomized controlled trials are needed to confirm its clinical efficacy.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
YZ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Writing – original draft, Writing – review & editing. SD: Formal analysis, Investigation, Software, Writing – review & editing. WL: Investigation, Software, Writing – review & editing. XW: Conceptualization, Supervision, Writing – review & editing. JL: Conceptualization, Writing – review & editing. QN: Conceptualization, Writing – review & editing. QZ: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This project was supported by “2024 Annual Nursing Research Fund Project of Shanxi Bethune Hospital +2024YH21.”
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2025.1653730/full#supplementary-material
Footnotes
References
1. Ma, CX, Ma, XN, Guan, CH, Li, YD, Mauricio, D, and Fu, SB. Cardiovascular disease in type 2 diabetes mellitus: progress toward personalized management. Cardiovasc Diabetol. (2022) 21:74. doi: 10.1186/s12933-022-01516-6
2. Valabhji, J, and Kar, P. Rise in type 2 diabetes shows that prevention is more important than ever. BMJ. (2023) 381:910. doi: 10.1136/bmj.p910
3. Home, Resources, Diabetes Diabetes and kidney disease IDF Diabetes Atlas. (2024) Available online at: https://diabetesatlas.org/atlas/diabetes-and-kidney-disease/.
4. World Health Organization. Diabetes[EB/OL]//Diabetes. (2024). Available online at: https://www.who.int/news-room/fact-sheets/detail/diabetes.
5. Sheu, WHH, Ji, LN, Nitiyanant, W, Sheu, WH, Baik, SH, Yin, D, et al. Hypoglycemia is associated with increased worry and lower quality of life among patients with type 2 diabetes treated with oral antihyperglycemic agents in the Asia-Pacific region. Diabetes Res Clin Pract. (2012) 96:141–8. doi: 10.1016/j.diabres.2011.12.027
6. Cheng, HJ, Weng, SH, Wu, JL, Yeh, ST, Chen, HF, Novida, H, et al. Long-term sulfonylurea use and impaired awareness of hypoglycemia among patients with type 2 diabetes in Taiwan. Ann Fam Med. (2024) 22:309–16. doi: 10.1370/afm.3129
7. Bailey, CJ. Metformin: therapeutic profile in the treatment of type 2 diabetes. Diabetes Obes Metab. (2024) 26:3–19. doi: 10.1111/dom.15663
8. Longo, M, Bellastella, G, Maiorino, MI, Meier, JJ, Esposito, K, and Giugliano, D. Diabetes and aging: from treatment goals to pharmacologic therapy. Front Endocrinol. (2019) 10:45. doi: 10.3389/fendo.2019.00045
9. International Hypoglycaemia Study Group. Hypoglycaemia, cardiovascular disease, and mortality in diabetes: epidemiology, pathogenesis, and management. Lancet Diabetes Endocrinol. (2019) 7:385–96. doi: 10.1016/S2213-8587(18)30315-2
10. Mokgalaboni, K, Mashaba, RG, Phoswa, WN, and Lebelo, SL. Curcumin attenuates hyperglycemia and inflammation in type 2 diabetes mellitus: quantitative analysis of randomized controlled trial. Nutrients. (2024) 16:4177. doi: 10.3390/nu16234177
11. Mokgalaboni, K, Lebelo, SL, Modjadji, P, and Ghaffary, S. Okra ameliorates hyperglycaemia in pre-diabetic and type 2 diabetic patients: a systematic review and meta-analysis of the clinical evidence. Front Pharmacol. (2023) 14:1132650. doi: 10.3389/fphar.2023.1132650
12. Han, SM, Yuan, ZL, Liu, JP, He, WL, and Fang, C. Propolis is safe for consumption as both food and medicine. J Bee. (2004) 24, 30–1. Available online at: https://kns.cnki.net/kcms2/article/abstract?v=dTSX2bdXfeByVNM33NStHUhRvqgKF3KIckSGmfI1FjlUmf4QrWBhsWXmAJYMdUXhe0OkEaYA_RRv9GHEFGF_X3Hiy-MIlTSeV2yR-iqyQF4GP5SUcymXKSvEG4N_lPrjwVS5eqEMTpMyn9HjJfVXZlSokN50j7fnDBQj-vCGHYzsOuWsujkktA==&uniplatform=NZKPT&language=CHS
13. Chavda, VP, Vuppu, S, Balar, PC, Mishra, T, Bezbaruah, R, Teli, D, et al. Propolis in the management of cardiovascular disease. Int J Biol Macromol. (2024) 266:131219. doi: 10.1016/j.ijbiomac.2024.131219
14. Aminimoghadamfarouj, N, and Nematollahi, A. Propolis diterpenes as a remarkable bio-source for drug discovery development: a review. Int J Mol Sci. (2017) 18:1290. doi: 10.3390/ijms18061290
15. Bankova, VS, Popov, SS, and Marekov, NL. Isopentenyl cinnamates from poplar buds and propolis. Phytochemistry. (1989) 28:871–3. doi: 10.1016/0031-9422(89)80133-5
16. Sforcin, JM, and Bankova, V. Propolis: is there a potential for the development of new drugs? J Ethnopharmacol. (2011) 133:253–60. doi: 10.1016/j.jep.2010.10.032
17. Sforcin, JM. Biological properties and therapeutic applications of propolis. Phytothe Res. (2016) 30:894–905. doi: 10.1002/ptr.5605
18. Huang, S, Zhang, CP, Wang, K, Li, G, and Hu, F-L. Recent advances in the chemical composition of propolis. Molecules. (2014) 19:19610–32. doi: 10.3390/molecules191219610
19. Rivera-Yañez, N, Rivera-Yañez, CR, Pozo-Molina, G, Méndez-Catalá, CF, Méndez-Cruz, AR, and Nieto-Yañez, O. Biomedical properties of propolis on diverse chronic diseases and its potential applications and health benefits. Nutrients. (2020) 13:78. doi: 10.3390/nu13010078
20. Okamura, T, Hamaguchi, M, Bamba, R, Nakajima, H, Yoshimura, Y, Kimura, T, et al. Brazilian green propolis improves gut microbiota dysbiosis and protects against sarcopenic obesity. J Cachexia Sarcopenia Muscle. (2022) 13:3028–47. doi: 10.1002/jcsm.13076
21. Luque-Bracho, A, Rosales, Y, and Vergara-Buenaventura, A. The benefits of propolis in periodontal therapy. A scoping review of preclinical and clinical studies. J Ethnopharmacol. (2023) 303:115926. doi: 10.1016/j.jep.2022.115926
22. Pasupuleti, VR, Sammugam, L, Ramesh, N, and Gan, SH. Honey, propolis, and royal jelly: a comprehensive review of their biological actions and health benefits. Oxidative Med Cell Longev. (2017) 2017:1259510. doi: 10.1155/2017/1259510
23. Khalil, MI, and Sulaiman, SA. The potential role of honey and its polyphenols in preventing heart diseases: a review. Afr J Tradit Complement Altern Med. (2010) 7:315–21. doi: 10.4314/ajtcam.v7i4.56693
24. Ruiz-Bustos, P, Alday, E, Garibay-Escobar, A, Sforcin, JM, Lipovka, Y, Hernandez, J, et al. Propolis: antineoplastic activity, constituents, and mechanisms of action. Curr Top Med Chem. (2023) 23:1753–64. doi: 10.2174/1568026623666230321120631
25. Hallajzadeh, J, Milajerdi, A, Amirani, E, Attari, VE, Maghsoudi, H, and Mirhashemi, SM. Effects of propolis supplementation on glycemic status, lipid profiles, inflammation and oxidative stress, liver enzymes, and body weight: a systematic review and meta-analysis of randomized controlled clinical trials. J Diabetes Metab Disord. (2021) 20:831–43. doi: 10.1007/s40200-020-00696-w
26. Jalali, M, Ranjbar, T, Mosallanezhad, Z, Mahmoodi, M, Moosavian, SP, Ferns, GA, et al. Effect of propolis intake on serum C-reactive protein (CRP) and tumor necrosis factor-alpha (TNF-α) levels in adults: a systematic review and meta-analysis of clinical trials. Complement Ther Med. (2020) 50:102380. doi: 10.1016/j.ctim.2020.102380
27. Nazari-Bonab, H, Jamilian, P, Radkhah, N, Zarezadeh, M, and Ebrahimi-Mameghani, M. The effect of propolis supplementation in improving antioxidant status: a systematic review and meta-analysis of controlled clinical trials. Phytother Res. (2023) 37:3712–23. doi: 10.1002/ptr.7899
28. Karimian, J, Hadi, A, Pourmasoumi, M, Najafgholizadeh, A, and Ghavami, A. The efficacy of propolis on markers of glycemic control in adults with type 2 diabetes mellitus: a systematic review and meta-analysis. Phytothe Res. (2019) 33:1616–26. doi: 10.1002/ptr.6356
29. Fuliang, HU, Hepburn, HR, Xuan, H, Chen, M, Daya, S, and Radloff, SE. Effects of propolis on blood glucose, blood lipid and free radicals in rats with diabetes mellitus. Pharmacol Res. (2005) 51:147–52. doi: 10.1016/j.phrs.2004.06.011
30. Afsharpour, F, Javadi, M, Hashemipour, S, Koushan, Y, and Khadem Haghighian, H. Changes in lipid profile, liver enzymes and inflammatory factors following oral supplementation with propolis in patients with type 2 diabetes. Clin Diabetol. (2022) 11:224–31. doi: 10.5603/DK.a2022.0033
31. Samadi, N, Mozaffari-Khosravi, H, Rahmanian, M, and Askarishahi, M. Effects of bee propolis supplementation on glycemic control, lipid profile and insulin resistance indices in patients with type 2 diabetes: a randomized, double-blind clinical trial. J Integr Med. (2017) 15:124–34. doi: 10.1016/S2095-4964(17)60315-7
32. Moayedi, F, Taghian, F, Dehkordi, KJ, Jalali Dehkordi, K, and Hosseini, SA. Cumulative effects of exercise training and consumption of propolis on managing diabetic dyslipidemia in adult women: a single-blind, randomized, controlled trial with pre-post-intervention assessments. J Physiol Sci. (2023) 73:17. doi: 10.1186/s12576-023-00872-6
33. Fukuda, T, Fukui, M, Tanaka, M, Senmaru, TAKAFUMI, Iwase, HIROYA, Yamazaki, MASAHIRO, et al. Effect of Brazilian green propolis in patients with type 2 diabetes: a double-blind randomized placebo-controlled study. Biomed Rep. (2015) 3:355–60. doi: 10.3892/br.2015.436
34. Zakerkish, M, Jenabi, M, Zaeemzadeh, N, Hemmati, AA, and Neisi, N. The effect of Iranian propolis on glucose metabolism, lipid profile, insulin resistance, renal function and inflammatory biomarkers in patients with type 2 diabetes mellitus: a randomized double-blind clinical trial. Sci Rep. (2019) 9:7289. doi: 10.1038/s41598-019-43838-8
35. Afsharpour, F, Javadi, M, Hashemipour, S, Koushan, Y, and haghighian, HK. Propolis supplementation improves glycemic and antioxidant status in patients with type 2 diabetes: a randomized, double-blind, placebo-controlled study. Complement Ther Med. (2019) 43:283–8. doi: 10.1016/j.ctim.2019.03.001
36. Gao, W, Pu, L, Wei, J, Yao, Z, Wang, Y, Shi, T, et al. Serum antioxidant parameters are significantly increased in patients with type 2 diabetes mellitus after consumption of Chinese propolis: a randomized controlled trial based on fasting serum glucose level. Diabetes Ther. (2018) 9:101–11. doi: 10.1007/s13300-017-0341-9
37. Zhao, L, Pu, L, Wei, J, Li, J, Wu, J, Xin, Z, et al. Brazilian green Propolis improves antioxidant function in patients with type 2 diabetes mellitus. Int J Environ Res Public Health. (2016) 13:498. doi: 10.3390/ijerph13050498
38. Hesami, S, Hashemipour, S, Shiri-Shahsavar, MR, Koushan, Y, and Khadem Haghighian, H. Administration of Iranian Propolis attenuates oxidative stress and blood glucose in type II diabetic patients: a randomized, double-blind, placebo-controlled, clinical trial. Casp J Intern Med. (2019) 10:48–54. doi: 10.22088/cjim.10.1.48
39. Page, MJ, Mckenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
40. Harreiter, J, and Roden, M. Diabetes mellitus: definition, classification, diagnosis, screening and prevention (update 2023). Wien Klin Wochenschr. (2023) 135:7–17. doi: 10.1007/s00508-022-02122-y
41. El-Sharkawy, HM, Anees, MM, and Van Dyke, TE. Propolis improves periodontal status and glycemic control in patients with type 2 diabetes mellitus and chronic periodontitis: a randomized clinical trial. J Periodontol. (2016) 87:1418–26. doi: 10.1902/jop.2016.150694
42. Ochoa-Morales, PD, González-Ortiz, M, Martínez-Abundis, E, Pérez-Rubio, KG, and Patiño-Laguna, ADJ. Anti-hyperglycemic effects of propolis or metformin in type 2 diabetes mellitus. Int J Vitam Nutr Res. (2023) 93:498–506. doi: 10.1024/0300-9831/a000760
43. Yousefi, M, Hashemipour, S, Shiri-Shahsavar, MR, Koushan, Y, and Haghighian, HK. Reducing the inflammatory interleukins with anti-inflammatory and antioxidant effects of Propolis in patients with type 2 diabetes: double-blind, randomized controlled, clinical trial. Clin Diabetol. (2023) 12:327–35. doi: 10.5603/cd.96910
44. Wang, KF, Xu, SH, Xie, X, Yu, KN, and Lv, HQ. Effects of propolis supplementation on efficacy, inflammatory factors and immune function in type 2 diabetes patients with pulmonary infection. J Transl Med. (2024) 13:264–7. Available online at: https://kns.cnki.net/kcms2/article/abstract?v=dTSX2bdXfeBF87evRF4_f8MRqO_Up5i5rIIDYwRa1CwFR6QS66my4y7-OQQykwWCWV3TEXDzSM6iMoKO0xX7zkdrHi94s4BJ0yxOdxluTL85h2n5qyG6iyNKcdtgSOImV_fJEEJNqDGBFQ57qY6cYE7t7sa2J1C8rsJ_VmIg6wYDYV27XeiYKQ==&uniplatform=NZKPT&language=CHS
45. Salehi-Sahlabadi, A, Chhabra, M, Rahmani, J, Momeni, A, Karam, G, Nattagh-Eshtivani, E, et al. The effect of propolis on anthropometric indices and lipid profile: a systematic review and meta-analysis of randomized controlled trials. J Diabetes Metab Disord. (2020) 19:1835–43. doi: 10.1007/s40200-020-00604-2
46. Gheflati, A, Dehnavi, Z, Ghannadzadeh Yazdi, A, Khorasanchi, Z, Raeisi-Dehkordi, H, and Ranjbar, G. The effects of propolis supplementation on metabolic parameters: a systematic review and meta-analysis of randomized controlled clinical trials. Avicenna J Phytomed. (2021) 11:551–65. doi: 10.22038/AJP.2021.18046
47. Kumar, S, and Pandey, AK. Chemistry and biological activities of flavonoids: an overview. TheScientificWorldJournal. (2013) 2013:162750. doi: 10.1155/2013/162750
48. Yu, Y, Si, Y, Song, G, Luo, T, Wang, J, and Qin, S. Ethanolic extract of propolis promotes reverse cholesterol transport and the expression of ATP-binding cassette transporter A1 and G1 in mice. Lipids. (2011) 46:805–11. doi: 10.1007/s11745-011-3568-7
49. Daleprane, JB, Freitas, V d S, Pacheco, A, Rudnicki, M, Faine, LA, Dörr, FA, et al. Anti-atherogenic and anti-angiogenic activities of polyphenols from propolis. J Nutr Biochem. (2012) 23:557–66. doi: 10.1016/j.jnutbio.2011.02.012
50. Lh, C, Yw, C, Ml, C, CC, H, CH, C, HW, T, et al. Taiwanese green propolis ethanol extract delays the progression of type 2 diabetes mellitus in rats treated with streptozotocin/high-fat diet. Nutrients. (2018) 10:503. doi: 10.3390/nu10040503
51. Kong, L, Zhang, Y, Feng, Z, Dong, J, and Zhang, H. Phenolic compounds of propolis alleviate lipid metabolism disorder. Evid Based Complementary Altern Med. (2021) 2021:7615830. doi: 10.1155/2021/7615830
52. Guo, G, Guan, Y, Chen, Y, Ye, Y, Gan, Z, Cao, X, et al. HbA1c and the risk of lower limb ulcers among diabetic patients: an observational and genetics study. J Diabetes Res. (2025):2025: 4744194. doi: 10.1155/jdr/4744194
53. Ling, J, Xie, Z, Chen, X, Ling, D, and Luo, X. Inverted U-shaped relationship between HbA1c and diabetic retinopathy in diabetic patients: a cross-sectional study. BMC Ophthalmol. (2025) 25:289. doi: 10.1186/s12886-025-04079-8
54. Ueda, M, Hayashibara, K, and Ashida, H. Propolis extract promotes translocation of glucose transporter 4 and glucose uptake through both PI3K- and AMPK-dependent pathways in skeletal muscle. BioFactors. (2013) 39:457–66. doi: 10.1002/biof.1085
55. Mujica, V, Orrego, R, Pérez, J, Romero, P, Ovalle, P, Zúñiga-Hernández, J, et al. The role of propolis in oxidative stress and lipid metabolism: a randomized controlled trial. Evid Based Complement Alternat Med. (2017) 2017:4272940. doi: 10.1155/2017/4272940
56. Wei, P, Ding, Y, Lu, Q, Tan, J, and Liu, R. Flavonoid components in propolis and poplar resin and their inhibitory activity on α-glucosidase. J Huazhong Agric Univ. (2018) 37:92–9. doi: 10.13300/j.cnki.hnlkxb.2018.03.014
57. Liang, XL, Zhao, YZ, Zhang, HC, and Peng, WJ. Improvement effects of four flavonoids from propolis on insulin resistance in HepG2 cells. J Agric Sci Technol. (2017) 19:74–80. doi: 10.13304/j.nykjdb.2017.0020
58. Yang, M, Sui, DJ, Chen, WX, Yang, M, and Yu, DW. Hypoglycemic mechanism of total flavonoids from propolis in STZ-induced diabetic rats. J Chin Med Mater. (2014) 37:1623–6. doi: 10.13863/j.issn1001-4454.2014.09.030
59. Liu, Y, Liang, X, Zhang, G, Kong, L, Peng, W, and Zhang, H. Galangin and pinocembrin from Propolis ameliorate insulin resistance in HepG2 cells via regulating Akt/mTOR signaling. Evid Based Complement Alternat Med. (2018) 2018:7971842. doi: 10.1155/2018/7971842
60. Shang, H, Srikanth Bhagavathula, A, Ali Aldhaleei, W, Rahmani, J, Karam, G, Rinaldi, G, et al. Effect of propolis supplementation on C-reactive protein levels and other inflammatory factors: a systematic review and meta-analysis of randomized controlled trials. J King Saud Univ Sci. (2020) 32:1694–701. doi: 10.1016/j.jksus.2020.01.003
61. Gholami, A, Dinarvand, N, and Hariri, M. Propolis supplementation can reduce serum level of interleukin-6, C-reactive protein, and tumor necrosis factor-α: an updated systematic review and dose-response meta-analysis on randomized clinical trials. J Health Popul Nutr. (2024) 43:119. doi: 10.1186/s41043-024-00600-9
62. Yuan, M, Yuan, XJ, Pineda, M, Liang, Z-Y, He, J, Sun, S-W, et al. A comparative study between Chinese propolis and Brazilian green propolis: metabolite profile and bioactivity. Food Funct. (2020) 11:2368–79. doi: 10.1039/c9fo02051a
63. Li, D, Wang, X, Huang, Q, Li, S, Zhou, Y, and Li, Z. Cardioprotection of CAPE-oNO2 against myocardial ischemia/reperfusion induced ROS generation via regulating the SIRT1/eNOS/NF-κB pathway in vivo and in vitro. Redox Biol. (2018) 15:62–73. doi: 10.1016/j.redox.2017.11.023
64. Mirzoeva, OK, and Calder, PC. The effect of propolis and its components on eicosanoid production during the inflammatory response. Prostaglandins Leukot Essent Fatty Acids. (1996) 55:441–9. doi: 10.1016/s0952-3278(96)90129-5
65. Funk, CD. Prostaglandins and leukotrienes: advances in eicosanoid biology. Science. (2001) 294:1871–5. doi: 10.1126/science.294.5548.1871
66. Juman, S, Yasui, N, Ikeda, K, Ueda, A, Sakanaka, M, Negishi, H, et al. Caffeic acid phenethyl ester suppresses the production of pro-inflammatory cytokines in hypertrophic adipocytes through lipopolysaccharide-stimulated macrophages. Biol Pharm Bull. (2012) 35:1941–6. doi: 10.1248/bpb.b12-00317
67. Bahari, H, Shahraki Jazinaki, M, Aliakbarian, M, Rashidmayvan, M, Golafrouz, H, Rahnama, I, et al. Propolis supplementation on inflammatory and oxidative stress biomarkers in adults: a systematic review and meta-analysis of randomized controlled trials. Front Nutr. (2025) 12:1542184. doi: 10.3389/fnut.2025.1542184
68. Papastergiadis, A, Mubiru, E, VAN Langenhove, H, and De Meulenaer, B. Malondialdehyde measurement in oxidized foods: evaluation of the spectrophotometric thiobarbituric acid reactive substances (TBARS) test in various foods. J Agric Food Chem. (2012) 60:9589–94. doi: 10.1021/jf302451c
69. Yangi, B, Cengiz Ustuner, M, Dincer, M, Ozbayer, C, Tekin, N, Ustuner, D, et al. Propolis protects endotoxin induced acute lung and liver inflammation through attenuating inflammatory responses and oxidative stress. J Med Food. (2018) 21:1096–105. doi: 10.1089/jmf.2017.0151
70. Lee, Y, Shin, DH, Kim, JH, Hong, S, Choi, D, Kim, Y-J, et al. Caffeic acid phenethyl ester-mediated Nrf2 activation and IkappaB kinase inhibition are involved in NFkappaB inhibitory effect: structural analysis for NFkappaB inhibition. Eur J Pharmacol. (2010) 643:21–8. doi: 10.1016/j.ejphar.2010.06.016
71. Levonen, AL, Inkala, M, Heikura, T, Jauhiainen, S, Jyrkkänen, H-K, Kansanen, E, et al. Nrf2 gene transfer induces antioxidant enzymes and suppresses smooth muscle cell growth in vitro and reduces oxidative stress in rabbit aorta in vivo. Arterioscler Thromb Vasc Biol. (2007) 27:741–7. doi: 10.1161/01.ATV.0000258868.80079.4d
72. Natarajan, K, Singh, S, Burke, TR, Grunberger, D, and Aggarwal, BB. Caffeic acid phenethyl ester is a potent and specific inhibitor of activation of nuclear transcription factor NF-kappa B. Proc Natl Acad Sci USA. (1996) 93:9090–5. doi: 10.1073/pnas.93.17.9090
73. Chang, H, Yuan, W, Wu, H, Yin, X, and Xuan, H. Bioactive components and mechanisms of Chinese poplar propolis alleviates oxidized low-density lipoprotein-induced endothelial cells injury. BMC Complement Altern Med. (2018) 18:142. doi: 10.1186/s12906-018-2215-8
74. Jugran, AK, Rawat, S, Devkota, HP, Bhatt, ID, and Rawal, RS. Diabetes and plant-derived natural products: from ethnopharmacological approaches to their potential for modern drug discovery and development. Phytother Res. (2021) 35:223–45. doi: 10.1002/ptr.6821
75. Han, SF, Feng, YQ, and Gao, WQ. Theoretical model of non-nutrient diet therapy for prevention and treatment of chronic diseases. Chin Nurs Res. (2023) 37:565–9. doi: 10.12102/j.issn.1009-6493.2023.04.001
76. Solorzano, ER, Roverso, M, Bogialli, S, Bortoli, M, Orian, L, Badocco, D, et al. Antioxidant activity of Zuccagnia-type propolis: a combined approach based on LC-HRMS analysis of bioanalytical-guided fractions and computational investigation. Food Chem. (2024) 461:140827. doi: 10.1016/j.foodchem.2024.140827
77. Li, Z, Liu, Z, Guo, Y, Gao, S, Tang, Y, Li, T, et al. Propolis alleviates acute lung injury induced by heat-inactivated methicillin-resistant Staphylococcus aureus via regulating inflammatory mediators, gut microbiota and serum metabolites. Nutrients. (2024) 16:1598. doi: 10.3390/nu16111598
78. Guo, Y, Liu, Z, Wu, Q, Li, Z, Yang, J, and Xuan, H. Integration with transcriptomic and metabolomic analyses reveals the in vitro cytotoxic mechanisms of Chinese poplar propolis by triggering the glucose metabolism in human hepatocellular carcinoma cells. Nutrients. (2023) 15:4329. doi: 10.3390/nu15204329
79. Magnavacca, A, Sangiovanni, E, Racagni, G, and Dell'Agli, M. The antiviral and immunomodulatory activities of propolis: an update and future perspectives for respiratory diseases. Med Res Rev. (2022) 42:897–945. doi: 10.1002/med.21866
80. Jian, XD. Attention to propolis allergy. J Bee. (2014) 34:47. Available online at: https://kns.cnki.net/kcms2/article/abstract?v=dTSX2bdXfeDKKTWzGxIiBrt9ExgRI_Tt_6VE6RQkW-vBPuMgTQ3c_0nlqHjW-WGqPwnYtlNjR8ObcwZMZIluRTyiUrw5xBNMeupVFzBSihmLaC7wZpYjaIEESW6GPUkgas9DOanv7EQxIGYnXjODMhxsZx_6SrNvQp1JEIc0GtGVHkvEXvXcGg==&uniplatform=NZKPT&language=CHS
81. Ndreu, L, Hurben, AK, Nyman, GSA, Tretyakova, NY, Karlsson, I, and Hagvall, L. Investigation into propolis components responsible for inducing skin allergy: air oxidation of caffeic acid and its esters contribute to hapten formation. Chem Res Toxicol. (2023) 36:859–69. doi: 10.1021/acs.chemrestox.2c00386
82. Chen, JW, Shen, XG, and Hu, FL. Bioconversion technology for reducing allergens in propolis. China Beekeeping. (2016) 67:62. Available online at: https://kns.cnki.net/kcms2/article/abstract?v=dTSX2bdXfeBPqFm9FHD9yXT8ZV0pJblwdh6AM9O130hlYvzuMKK92nqjP56meO4ea5YEUm7F4nGpfDCIHvannP9gjcQZROedYPrYDqo8ci_b1eK8Wm8X8ZRJqa1dJY1H238GrEm9OlbXL9wTNL4ZBWjvIs5Fe83jIsYkXYavfOp3m48TE6vhnQ==&uniplatform=NZKPT&language=CHS
83. Rolver, MG, Emanuelsson, F, Nordestgaard, BG, and Benn, M. Contributions of elevated CRP, hyperglycaemia, and type 2 diabetes to cardiovascular risk in the general population: observational and Mendelian randomization studies. Cardiovasc Diabetol. (2024) 23:165. doi: 10.1186/s12933-024-02207-0
84. Socha, R, Gałkowska, D, Bugaj, M, and Juszczak, L. Phenolic composition and antioxidant activity of propolis from various regions of Poland. Nat Prod Res. (2015) 29:416–22. doi: 10.1080/14786419.2014.949705
Keywords: propolis, type 2 diabetes mellitus, glycolipid metabolism, inflammatory markers, oxidative stress, systematic review
Citation: Zhang Y, Ding S, Li W, Wang X, Lv J, Niu Q and Zhang Q (2025) Propolis effects on blood sugar and lipid metabolism, inflammatory indicators, and oxidative stress in people with type 2 diabetes: a systematic review and meta-analysis. Front. Nutr. 12:1653730. doi: 10.3389/fnut.2025.1653730
Edited by:
Shaohua Qi, Houston Methodist Research Institute, United StatesReviewed by:
Jin-Long Tian, Shenyang Agricultural University, ChinaMohammed Faris Abdulghani, University of Nineveh, Iraq
Ahmed S. El Newehy, King Saud University, Saudi Arabia
Copyright © 2025 Zhang, Ding, Li, Wang, Lv, Niu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qian Zhang, emhhbmdxaWFuQHN4YnFlaC5jb20uY24=
 Yihua Zhang
Yihua Zhang Shuo Ding1
Shuo Ding1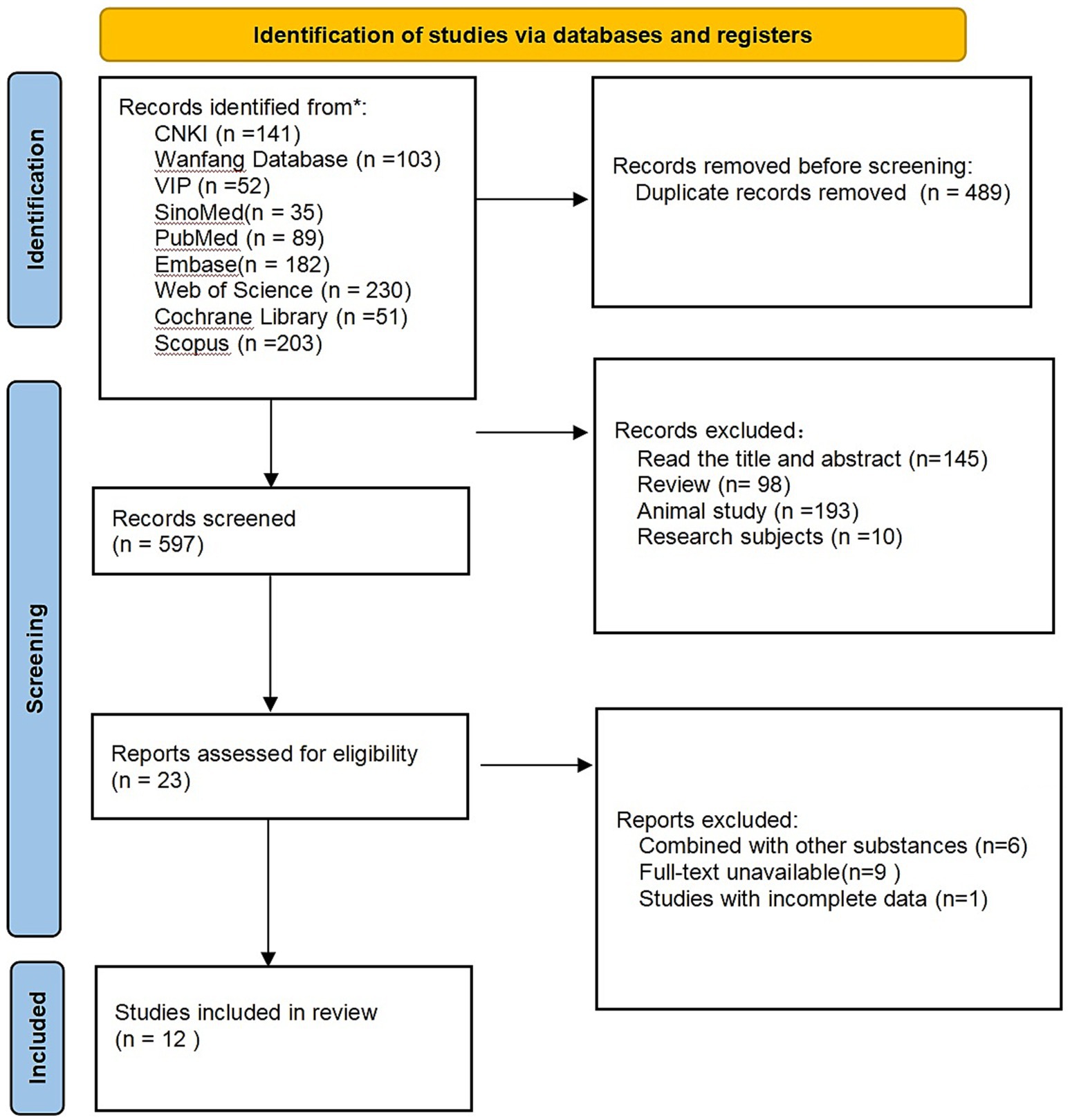
![Forest plot showing mean differences between experimental and control groups across six studies. Each study is represented by a square, with size indicating weight, and lines showing confidence intervals. The overall effect is represented by a diamond. The total mean difference is 0.13 with a 95% confidence interval of [0.10, 0.16]. Heterogeneity is low, with Chi² = 2.59, df = 5, and I² = 0%. The overall effect is statistically significant (Z = 9.77, P < 0.00001), favoring the experimental group.](https://www.frontiersin.org/files/Articles/1653730/fnut-12-1653730-HTML/image_m/fnut-12-1653730-g005.jpg)
![Forest plot showing a meta-analysis comparing experimental and control groups across five studies. Each study is represented with a green square indicating the effect size and a horizontal line representing the confidence interval. The diamond at the bottom represents the overall effect size, showing a mean difference of -0.15 with a 95% confidence interval of [-0.30, -0.01], favoring the experimental group. Heterogeneity is low with I² = 0%.](https://www.frontiersin.org/files/Articles/1653730/fnut-12-1653730-HTML/image_m/fnut-12-1653730-g006.jpg)