- University Clinic for Psychosomatic Medicine and Psychotherapy, Medical Faculty, Campus East-Westphalia, Ruhr-University Bochum, Bochum, North Rhine-Westphalia, Germany
Context: The COVID-19 pandemic intensified mental health issues and increased emotional eating (EE), a coping mechanism, where food is consumed in response to emotions rather than hunger. During the pandemic, gender-specific EE patterns were observed, with women reporting elevated EE levels in response to stress, anxiety, and depression due to various social and psychological factors.
Objectives: This study primarily focused on examining gender differences in EE during the COVID-19 pandemic. As a secondary outcome, it aimed to explore predictors of EE.
Data sources and extraction: This systematic review was pre-registered (PROSPERO CRD42023421727) and adhered to PRESS and PRISMA guidelines. Studies published between March 2020 and August 2024 were identified across Scopus, Web of Science, PubMed, and PsycINFO. The quality assessment was performed using the “Critical Appraisal Checklist for Analytical Cross-Sectional Studies.” The meta-analysis was conducted following MOOSE guidelines.
Data analysis: Of 14,347 studies identified, 30 met inclusion criteria (only if population ≥18 years, without clinical diagnoses, gender-specific analysis regarding EE, observational studies with original data collection during COVID-19 pandemic), with 16 incorporated into the meta-analysis. Gender significantly moderated pandemic-related stress. Higher EE scores in women were linked to isolation and caregiving responsibilities, while men’s EE often appeared as reward-seeking. Across diverse measures and regions, women consistently exhibited higher EE scores (Cohen’s d = 0.39). Young adults and students showed a stronger association with EE, suggesting heightened vulnerability. Key predictors included increased food intake, COVID-19-related stress and lifestyle changes, sleep quality, and physical activity.
Conclusion: The predominance of cross-sectional designs limits the ability to draw causal conclusions, and selection bias in studies, often targeting specific groups, restricts generalizability. Future longitudinal studies are needed to assess causality and explore the inferences to additional factors, such as socioeconomic status and mental health. Gender-sensitive interventions are suggested to address EE risks, particularly in women.
Systematic review registration: PROSPERO (CRD42023421727). https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023421727.
1 Introduction
In March 2020, the World Health Organization officially recognized the COVID-19 outbreak as a global pandemic (1), which led to the widespread implementation of various safety measures, including lockdowns, social distancing mandates, and home confinements (2). These measures disrupted daily routines and lifestyles (3) and posed significant economic challenges for many individuals (4). Extended lockdowns and prolonged uncertainty significantly increased global stress and anxiety levels (5), intensifying existing mental health challenges, including disordered eating behaviors (DEB) and emotional eating (EE) (6, 7).
1.1 Emotional eating
EE has been defined as the tendency to consume food in response to emotions, both positive and negative, rather than to satisfy physical hunger (8). Given the societal health risks associated with obesity, the link between EE and excess weight underscores the importance of addressing this behavior as a public health issue (9, 10). EE is strongly connected with other DEB, such as loss of control over eating, binge-eating, and food cravings (11, 12), which also often lead to obesity (13).
Research shows that individuals prone to EE have distinct dietary patterns compared to non-emotional eaters, including higher consumption of sweet and high-fat meals (14) and more frequent snacking (15). Many individuals also experience low levels of interoceptive awareness (16), leading to difficulties in identifying hunger, satiety, and emotional states (17). This reduced awareness is often linked with alexithymia, a condition characterized by difficulties in recognizing and expressing emotions (18).
EE may function as a form of escapism from negative emotions (19), given the stress-relieving effect of consuming energy-dense foods that activate reward pathways and release dopamine (20). The EE pattern creates a feedback loop in which EE provides temporary relief from distressing emotions but may lead to feelings of shame and guilt when the individuals reflect on their past behavior, which reinforces the negative emotions and may thus further perpetuate EE (19, 21). Research indicates that certain emotional states—such as anxiety, sadness, tension, and boredom—are more likely to result in EE than other negative emotions (22, 23). Accordingly, an experimental study found that anxiety, but not anger, is associated with greater food consumption (24). Furthermore, EE has been shown to be highly correlated with perceived stress (25). Increased stress levels are associated with a reduced ability to accurately perceive internal signals of hunger and satiety, along with alterations in the body’s natural hunger cues (26).
1.2 Eating behaviors in the pandemic context
Limited access to healthcare services during the COVID pandemic exacerbated anxiety and affected treatment compliance, particularly impacting individuals with ongoing health needs (27). Stress associated with confinement was further linked to sleep disturbances, which, in turn, were associated with higher food consumption (28). The prolonged lockdowns and restrictions during the pandemic intensified social isolation and heightened levels of stress, anxiety, and fear (29). This has led to an increase in the consumption of high-caloric “comfort foods” as a coping mechanism for negative emotions (30). Continuous media exposure to COVID-19-related news also acted as a chronic stressor, further fueling overeating behaviors (31). Additional pandemic-driven changes, such as disruptions to physical activity routines and increased preoccupation with weight and body image, exacerbated DEB (27, 32–34). Notably, these pandemic-related stressors appear to have impacted DEB in a gender-specific way; the systematic analysis by Laskowski et al. (35) found that women exhibited higher levels of disordered eating compared to men.
1.3 Gender differences in emotional eating
Research highlights that stress responses differ by gender, with women showing a greater propensity for stress-induced EE (36). Studies consistently demonstrate that EE levels are higher in women than in men (37, 38). In particular, women more often report eating as a response to emotional states such as depression, anxiety, or anger, especially during periods of elevated stress (26, 37, 39, 40). This pattern suggests that women may be more inclined to rely on EE as a coping mechanism during times of emotional distress (41).
A contributing factor to the observed gender disparity in EE is its association with depressive symptoms, which are more commonly reported by women (42–44). The higher prevalence of depressive symptoms may make women more likely to engage in EE as a means of managing their emotional distress. This aligns with patterns observed in other DEB, such as binge eating (45), where women are also overrepresented (46). Research suggests that men and women often differ in their ability to identify and express emotions, potentially leading to higher self-reported EE in women (37, 47).
Pandemic-induced stress and its impact on emotional regulation also appear to have differed between men and women. Evidence suggests that women are more likely to use self-distraction, including EE, as a coping strategy in response to heightened stressors (48, 49). This gender-specific vulnerability reflects a combination of psychological (50), social (51), and biological factors (52, 53) that influence stress processing and emotional responses. Current research suggests differences in hypothalamic-pituitary-adrenal (HPA) axis activation (54), immune function (55) and brain regions associated with emotional processing (53). In addition, women reported higher levels of rumination during negative affect (56, 57), which can exacerbate feelings of loss of control, leading to increased depressive and anxious symptoms (58).
The persistent stressors of the pandemic—including caregiving responsibilities, work-life balance challenges, and frequent exposure to anxiety-provoking media—may have exacerbated these tendencies in women (21). Prolonged isolation, increased anxiety, and constant exposure to distressing news may amplify negative emotions and disrupt emotion regulation, potentially leading to more pronounced gender-specific eating responses (59–61). This highlights the complex dynamics between stress processing, emotional regulation (62), and societal pressures that differentially affect genders (62, 63).
Although several reviews have examined eating behaviors during the COVID-19 pandemic, there is a lack of systematic reviews with meta-analytic synthesis focusing specifically on gender differences in EE. Previous reviews either addressed broader DEB or reported gender as a secondary outcome, leaving the precise magnitude and moderators of gender-specific EE during the pandemic insufficiently clarified. Despite several reviews on eating behaviors during COVID-19, a quantitative synthesis focusing specifically on gender differences in emotional eating is thus still lacking.
1.4 Objectives of the study
Evidence indicates that EE is shaped by gender-specific patterns and the distinct stressors introduced by the COVID-19 pandemic (64, 65), highlighting the need for an in-depth investigation into these dynamics. This systematic review and meta-analysis aimed to synthesize evidence on gender differences in EE during the COVID-19 pandemic. Specifically, we sought to quantify effect sizes across studies to provide a precise estimate of gender-specific patterns and to explore potential moderators of these differences. By clarifying the magnitude and consistency of gender differences in EE, this study addresses a gap in the literature and provides evidence relevant for designing gender-sensitive interventions.
2 Methods
2.1 Criteria for inclusion and exclusion
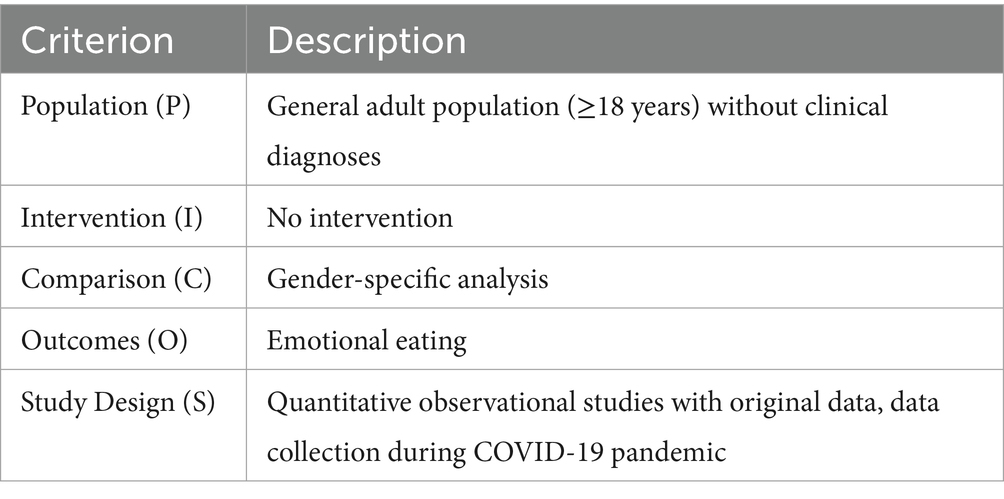
We included original research articles written in English or German, with no geographical limitations. Eligible studies focused on the general adult population, regardless of gender, while studies involving children, adolescents (<18 years), or clinical populations were excluded. Studies were required to address outcomes explicitly related to EE with a clear gender-specific analysis. Publications before March 2020 and those written in languages other than English or German, were excluded. Research on general eating behavior or emotion regulation without a specific focus on EE, as well as studies lacking gender comparisons, were excluded. Excluded publication types comprised (systematic) reviews, meta-analyses, case reports, qualitative studies, commentaries, conference papers, opinion pieces, letters, and editorials. The inclusion and exclusion criteria according to the population, intervention, comparison, outcomes, study design (PICOS) scheme are shown in Table 1.
During screening, we verified that all included studies reported at least one measurement collected during the COVID-19 pandemic (March 2020 onward). Studies that also contained pre-pandemic data were eligible only if pandemic-period data were available and analyzed.
2.2 Literature search
This review was preregistered with the National Institute for Health and Care Research on the “Prospero International Prospective Register of Systematic Reviews” (registration number: CRD42023421727). No additional protocol document beyond the PROSPERO registration form was developed or published. An evidence-based electronic search was conducted following the “Peer Review of Electronic Search Strategies” (PRESS) guidelines to guarantee a rigorous and reproducible approach. Additionally, the review adhered to the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” (PRISMA 2020) guidelines (66) (see Supplementary material for checklist), ensuring a transparent, structured, and comprehensive reporting process.
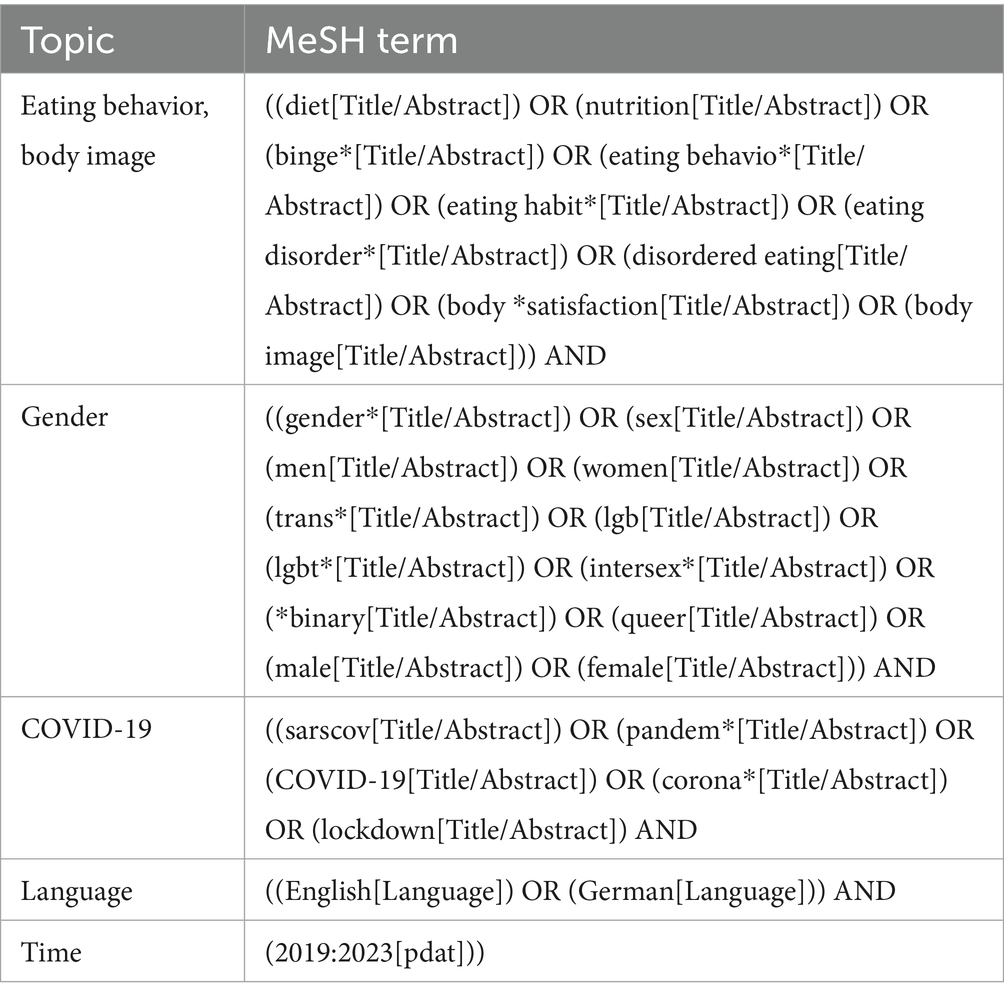
A comprehensive search of the literature was performed across four major databases—Scopus, Web of Science (WOS), PubMed MEDLINE, and PsycINFO—covering the period from March 2020 to August 8, 2024. The initial search was conducted on July 13, 2023, and updated and finalized on August 8, 2024. Although the initial search syntax formally included records from 2019 onwards, only studies published from March 2020 onwards and reporting data collected during the COVID-19 pandemic were eligible for inclusion. The search query used for PubMed is displayed in Table 2, with search terms adapted as needed for each database. The complete search strategy for all databases is available at https://www.crd.york.ac.uk/PROSPEROFILES/421727_STRATEGY_20230713.pdf. The Covidence software (67) was employed to organize and manage the studies, including deduplication, title/abstract screening, and full-text review. We did not systematically search the grey literature, which may have limited the inclusion of non-indexed studies.
2.3 Study evaluation
A two-stage procedure was employed for study selection. In the first stage, titles and abstracts were screened independently by two reviewers, with assignments rotated among six investigators (CZ, MP, GB, CR, LS, and NL). In the second stage, two reviewers independently examined each full text using the same assignment procedure, with particular attention to whether questionnaires assessed and reported EE. If the two reviewers agreed, the decision was accepted; in case of disagreement, consensus was sought through discussion with the broader review team, and unresolved cases were adjudicated by the first author (CZ), in consultation with the senior authors (NL and GP) if needed. The final set of included studies was verified by the senior authors (NL and GP). The synthesis of outcomes was conducted by the first (CZ) and second (MP) author, and NL, who provided methodological oversight.
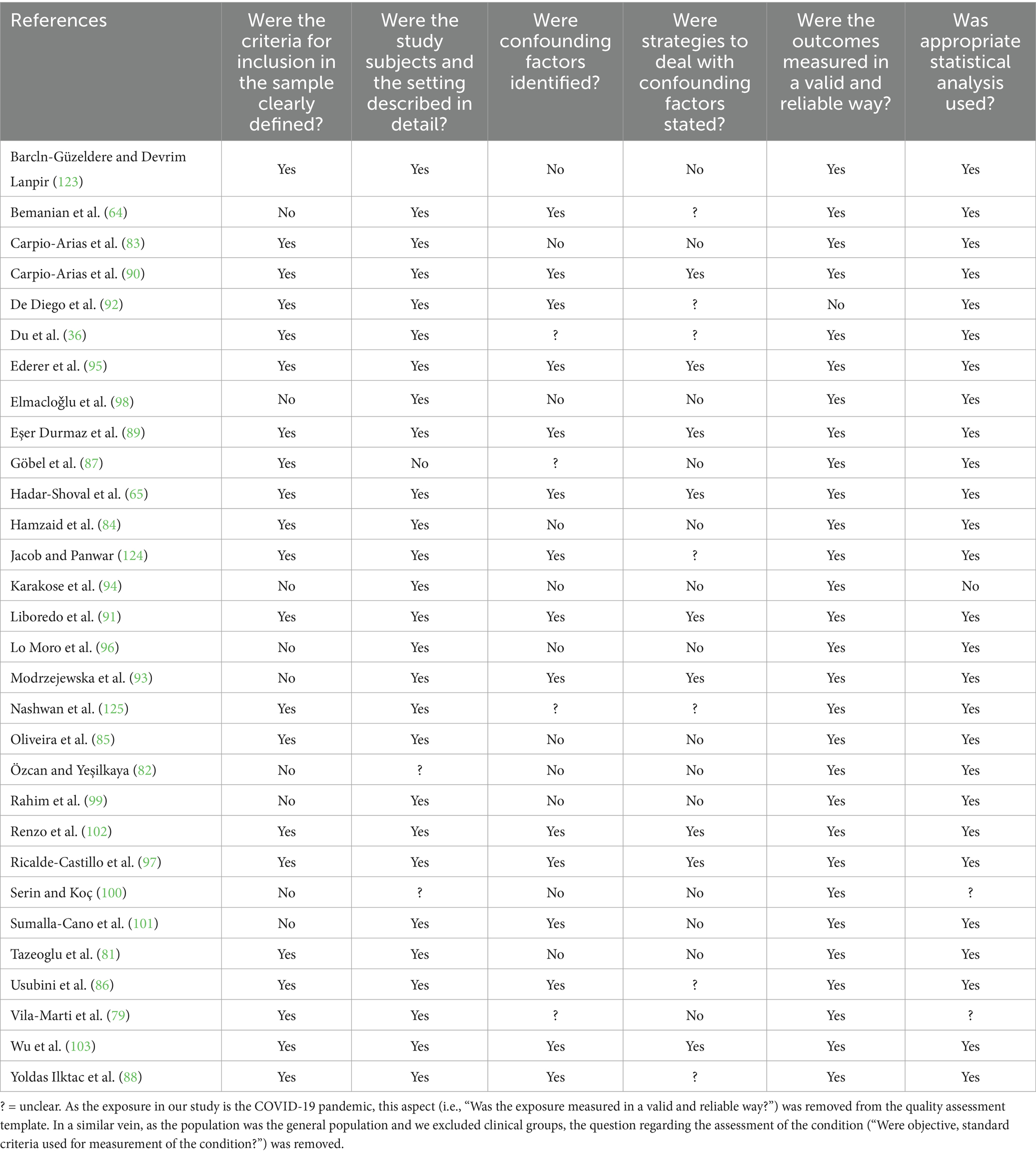
The quality assessment was performed using the “Critical Appraisal Checklist for Analytical Cross-Sectional Studies” developed by the Joanna Briggs Institute (68), following recommendations by Ma et al. (69). The checklist comprises eight items evaluated as “Yes,” “No,” “Unclear,” or “Not Applicable,” with an overall appraisal categorized as “Include,” “Exclude,” “Seek Further Information,” and “Comments.” Two authors independently conducted the quality assessment of included studies, with CZ making the final decision on assessments.
2.4 Statistical methods for meta-analysis
All statistical analyses were performed using the open-source software R version 4.4.1 (70), with the metafor package version 4.6.0 (71) employed to calculate Cohen’s d, perform the sensitivity analysis, and conduct subgroup analyses. In accordance with Cochrane’s recommendations for observational data, we followed the MOOSE guidelines (see Supplementary material for checklist) for conducting and reporting this meta-analysis of observational studies (72). In this meta-analysis, Cohen’s d was calculated as the standardized mean difference effect size based on mean values (M) and standard deviations (SD), either directly extracted from the included studies (n = 9) or obtained by contacting the corresponding authors (n = 21) to request (additional) data. These inquiries were conducted between September, 15th 2024 and October, 18th 2024. If no response was received, additional co-authors of the respective articles were contacted. If no extractable statistics were obtained after these attempts, the study was retained for the qualitative synthesis but excluded from the meta-analysis. The data associated with this study can be requested from the corresponding author.
We calculated the overall effect size and created a forest plot to visually summarize the findings across studies. To assess the robustness of our results, we performed a sensitivity analysis using the “leave-one-out” method, systematically removing one study at a time that had the greatest impact on heterogeneity, and recalculating the effect size for each iteration.
To gain deeper insights and identify potential moderators contributing to the observed variability, we conducted subgroup analyses targeting specific factors. The following data was extracted for this purpose: (1) measurement instruments: Emotional Eater Questionnaire (EEQ) (73), Emotional Eating Scale (EES) (8), Three-Factor-Eating Questionnaire (TFEQ) (74, 75), Eating Behavior Pattern Questionnaire (EBPQ) (76), Dutch Eating Behavior Questionnaire (DEBQ) (77), Emotional Overeating Questionnaire (EOQ-5) (78), self-developed; (2) percentage of women (<50%, 50–70, >70%); and (3) sample characteristics (young adults and university students, general population, and professionals). Finally, we examined (4) geographical regions, including Middle East, Europe, Latin America, South Asia, East Asia, cross-regional, and cross-regional Spanish-speaking. In this context, the “cross-regional” category includes one (36) study that evaluated participants from several different regions, while “cross-regional Spanish-speaking” refers to a study (79) that specifically included multiple Spanish-speaking countries across regions.
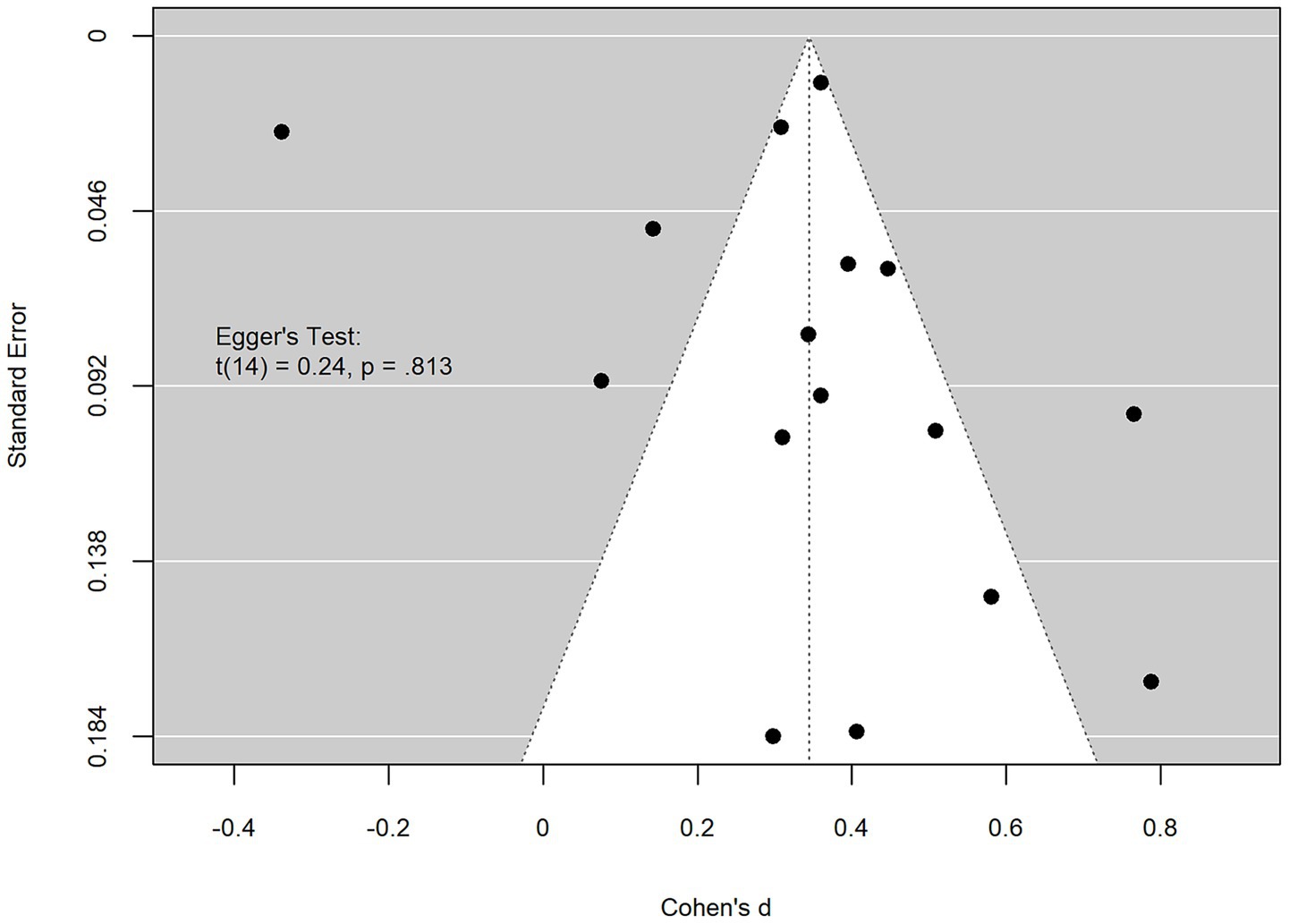
To assess heterogeneity, we calculated the I2 statistic and Cochran’s Q, with a significant p-value for Cochran’s Q indicating heterogeneity beyond chance. Publication bias was evaluated using Egger’s test and a funnel plot; a significant p-value for Egger’s test would suggest asymmetry, indicating potential publication bias. We applied a random-effects model to account for variability across studies, representing effect sizes as Cohen’s d. Forest plots were used to display both individual and overall Cohen’s d values.
3 Results
3.1 Extracted studies
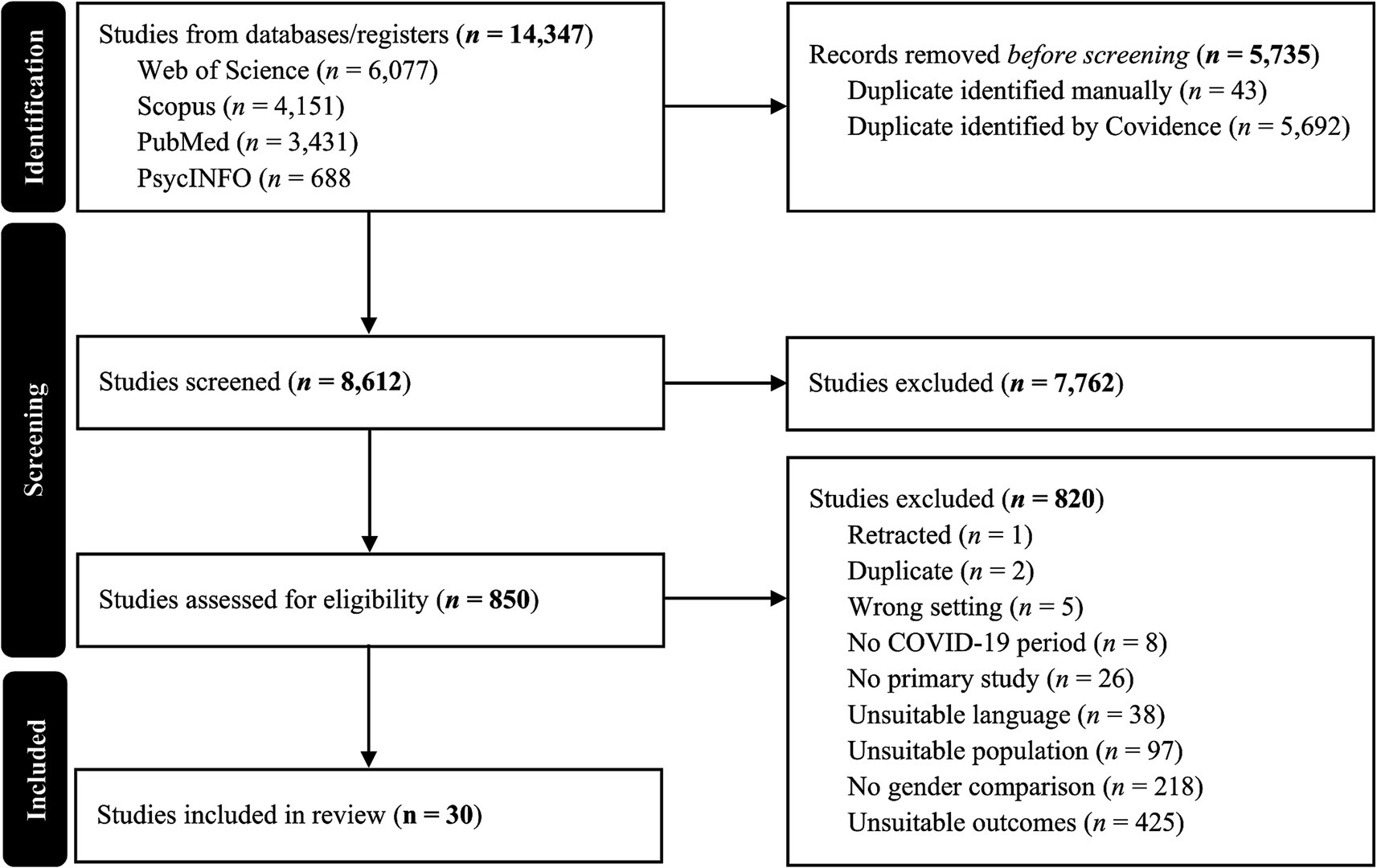
The literature search yielded 14,347 records. Following the selection process, 30 studies met the inclusion criteria and were included in the final synthesis (see PRISMA diagram, Figure 1). Of these, 16 studies were included in the meta-analysis. Studies entered the meta-analysis when they reported gender-disaggregated means and standard deviations (or convertible statistics) for emotional eating outcomes during the pandemic. The remaining studies (n = 14) did not provide sufficient quantitative information and were therefore retained in the narrative synthesis only.
3.2 Results regarding emotional eating
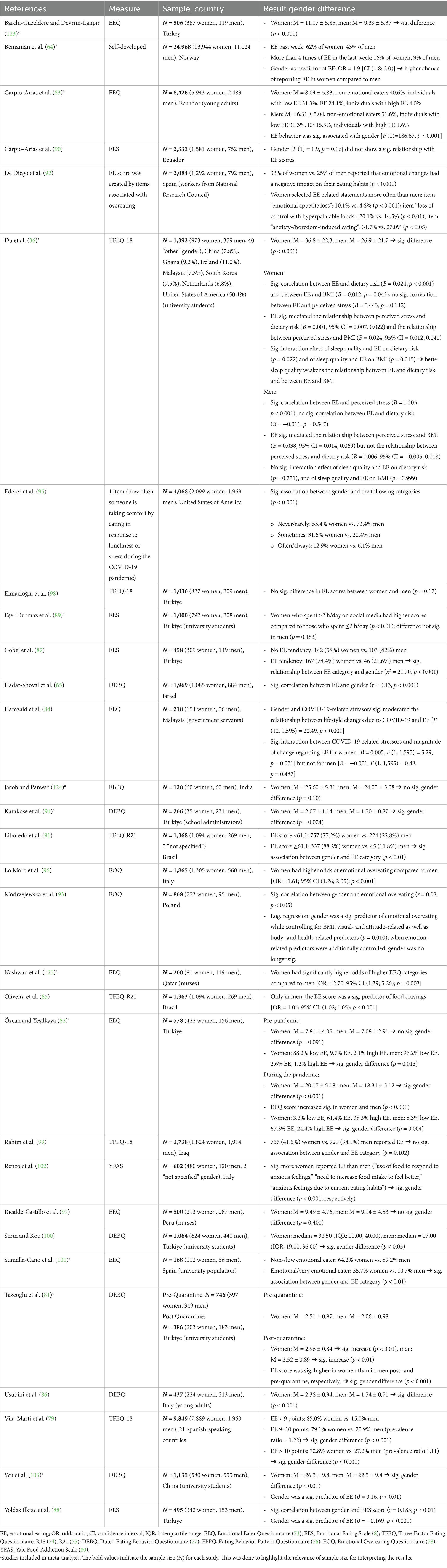
Thirty studies examining EE (see Table 3) were included in this review. Among these studies, 27 reported binary categories of women and men, while three also included “other” and “not specified” genders. The total sample size across all studies was 73,812 participants, comprising 46,935 women (63.6%), 26,830 men (36.3%), and 47 individuals (0.1%) classified as “other” or “not specified.” However, none of the studies provided detailed analyses for the “other” and “not specified” gender categories. Sample sizes in individual studies ranged from 120 to 24,968 participants.
The most frequently used tools for assessing EE included the EEQ (73); n = 7, the TFEQ in its 18-item (TFEQ-R18) (74) or 21-item version (TEFQ-R21) (75); n = 6, and the DEBQ (77); n = 6. The EES (8) was used in four studies, while self-developed questions were employed in three. Two studies used the EOQ-5 (78), and one study each used the EBPQ (76), and the Yale Food Addiction Scale (YFAS) (80).
Among the studies, one was longitudinal (81), while the remaining 29 employed cross-sectional designs. Nonetheless, one cross-sectional study (82) included retrospective (pre-pandemic) and prospective (i.e., during the pandemic) assessments of EE. Study samples were primarily drawn from the general population (n = 17), with no specific age or profession criteria. Additional groups included university populations (n = 6), young adults (n = 2), nurses (n = 2), workers from the National Research Council (n = 1), government servants (n = 1), and school administrators (n = 1).
3.2.1 Gender differences
Significant gender differences in EE behaviors were consistently observed across studies, with women typically reporting higher EE scores than men.
Multiple studies using the EEQ observed significant gender differences, with women scoring higher than men. For example, in Turkey, Özcan and Yeşilkaya (82) reported that women exhibited significantly higher EEQ scores during the COVID-19 pandemic, although no such difference was observed pre-pandemic, reflecting an increase in EE for both genders, with more pronounced changes among women. Similarly, in Ecuador (83), a significant association between gender and EE was found, with women again scoring higher than men. In Malaysia, Hamzaid et al. (84) demonstrated that gender and pandemic-related stressors significantly moderated the relationship between lifestyle changes and EE, particularly among women.
Studies employing the TFEQ also identified substantial gender differences in EE scores. In large multinational studies (36, 79), women consistently had higher EE scores and were more likely to report EE behaviors than men. At the same time, in Brazil, Oliveira et al. (85) found that EE scores significantly predicted food cravings in men, but not in women, highlighting potential gender differences in EE-related sequelae.
The DEBQ also revealed gender disparities in EE. For example, Usubini et al. (86) found that Italian women scored significantly higher than men. Similarly, in Israel (65), higher emotional eating in women compared to men was observed. Tazeoglu et al. (81) found that EE scores increased significantly post-quarantine for both genders in Turkey, with women consistently scoring higher.
Findings from studies using the EES showed more heterogeneous results concerning gender differences. In Turkey, Göbel et al. (87) and Yoldas Ilktac et al. (88) reported significantly higher EES scores in women and a stronger association between gender and EE tendencies. Additionally, Eşer Durmaz et al. (89) found that Turkish women who spent more time on social media exhibited higher EES scores, while no significant differences were noted for men. Conversely, Carpio-Arias et al. (90) found no significant relationship between gender and EE scores in Ecuador.
Studies utilizing either self-developed questions, the EBPQ, or the YFAS also supported the trend of higher EE prevalence in women. For instance, in a large Norwegian study with self-developed questions (64), women were nearly twice as likely as men to report EE, with gender serving as a significant predictor of EE.
Overall, across various measurement tools, women demonstrated higher EE tendencies than men, with gender frequently acting as a significant predictor of EE. A summary of gender differences in EE is presented in Table 3.
3.2.2 Associations between emotional eating and contributing factors during the COVID-19 pandemic
This section examines the associations between EE and various contributing factors during the COVID-19 pandemic, without emphasizing gender-specific outcomes.
Several studies found strong associations between changes in food intake during the pandemic and EE. For example, Liboredo et al. (91) identified increased food intake as a significant predictor of EE, with an odds ratio of 3.6 [95% CI (1.8; 3.7)], indicating a substantial rise in EE linked to higher food consumption. Similarly, De Diego et al. (92) reported that greater consumption of savory snacks, bakery products, and sweet snacks was significantly associated with higher EE behaviors (p < 0.001, respectively), highlighting the impact of altered dietary habits on EE during the pandemic.
COVID-19-related stress also emerged as a significant factor influencing EE. Hadar-Shoval et al. (65) found a notable correlation between pandemic-related stressors and EE (r = 0.24; p < 0.001). Participants who experienced positive changes in alcohol consumption, sleep quality, or smoking showed significantly less EE than those with negative changes, though no significant association was found with changes in physical activity. Similarly, Modrzejewska et al. (93) identified pandemic-related stress as a predictor of emotional overeating, even when controlling for variables such as gender, BMI, and affect regulation. These findings underscore the role of pandemic-induced stress in EE behaviors.
Fear of COVID-19 was another factor linked to EE. Karakose et al. (94) demonstrated a significant association between fear of the virus and EE (r = 0.35; p < 0.01), with fear of COVID-19 serving as a significant predictor of EE. Similarly, Yoldas Ilktac et al. (88) found an association between fear of COVID-19 and EE (r = 0.09; p = 0.046). However, fear did not remain a significant predictor after controlling for variables such as sleep quality, BMI, age, and gender.
Additional pandemic-specific factors included quarantine duration and lifestyle changes. Özcan and Yeşilkaya (82) found a significant association between the length of quarantine and EE scores (r = 0.61; p = 0.025), suggesting that prolonged quarantine correlated with increased EE. Vila-Marti et al. (79) reported that lower sleep quality, reduced physical activity, higher screen time, and changes in the relationship with food were negatively linked with medium and high EE scores (p < 0.05, respectively). Among these, changes in sleep quality were key predictors of high EE scores, emphasizing the critical role of sleep in managing EE.
Finally, Ederer et al. (95) explored EE in response to loneliness or stress, finding a significant association between EE and weight changes during the pandemic. Those who frequently engaged in EE due to loneliness or stress had increased odds of both weight loss and weight gain (odds-ratios ranging from 1.62 to 4.61), suggesting a strong link between EE behaviors and weight fluctuations during this period.
3.3 Meta-analytic findings on emotional eating across genders
The meta-analysis included 16 studies (see Table 3) on EE, with a combined sample size of 53,381 participants, comprising 34,137 women and 19,244 men. The initial random-effects model (see Supplementary Figure 1) revealed a moderate overall effect size [Cohen’s d = 0.34, 95% CI (0.21, 0.48), p < 0.001], suggesting that EE significantly differed by gender across studies. However, this initial model exhibited a high level of heterogeneity (I2 = 96.99%), indicating substantial variability between the included studies. The Q-test for heterogeneity was also significant [Q (15) = 700.30, p < 0.001], further highlighting unexplained variability across studies (see Supplementary Figure 1).
To better understand and address the observed heterogeneity, a leave-one-out sensitivity analysis was conducted. In this stepwise approach, the study by Vila-Marti et al. (79) was excluded first, slightly reducing heterogeneity to I2 = 90.32%, with a comparable effect size estimate [Cohen’s d = 0.39, 95% CI (0.30, 0.48), p < 0.001]. As additional studies with a strong influence on heterogeneity were removed—specifically, Usubini et al. (86), Lo Moro et al. (96), and Ricalde-Castillo et al. (97)—the heterogeneity dropped substantially, reaching I2 = 41.87% with 12 remaining studies. At this point, heterogeneity was no longer statistically significant (p = 0.078). The effect size estimate at this stage remained significant [Cohen’s d = 0.38, 95% CI (0.33, 0.42), p < 0.001], indicating that the effect of gender on EE is robust across these relatively homogeneous studies.
The final exclusion involved omitting Carpio-Arias et al. (83), leaving a subset of 11 studies, which further reduced heterogeneity to I2 = 15.60%, while maintaining a stable effect size estimate [Cohen’s d = 0.39, 95% CI (0.35, 0.43), p < 0.001]. However, given the stability of the effect size and the lack of statistically significant heterogeneity (p = 0.078) with 12 studies, further reductions were deemed unnecessary. We selected the 12-study subset as the final analysis group (see Figure 2) to balance statistical homogeneity with the inclusion of a broader evidence base. This subset reflects a relatively homogeneous group of studies with consistent effect sizes, underscoring the reliability of the gender difference in EE across diverse study contexts and populations.
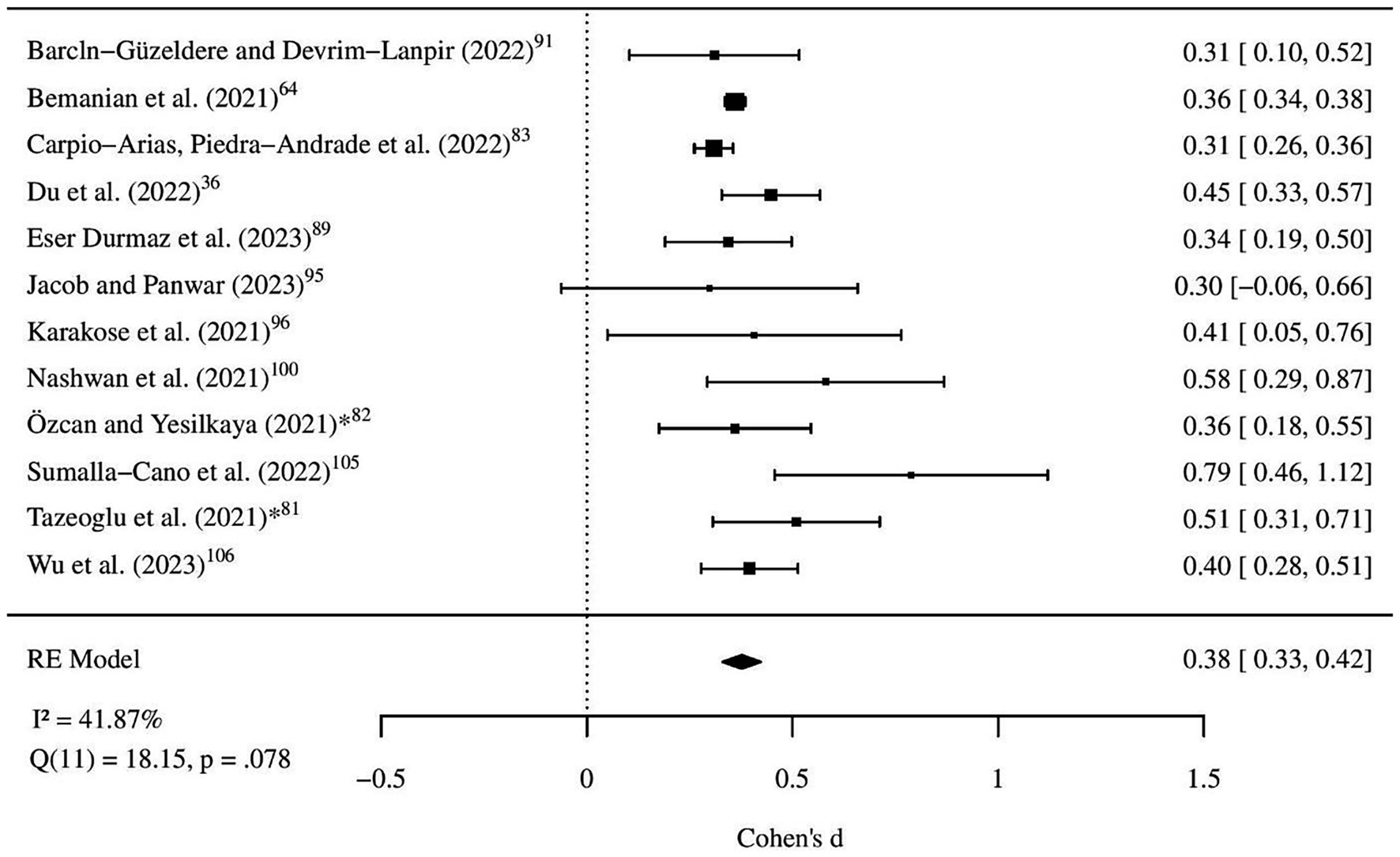
Figure 2. Forest plot of final random-effects model. All studies represent data collected during the COVID-19 pandemic. *Indicates the second measurement point for Özcan and Yeşilkaya (82) and for Tazeoglu et al. (81).
Subgroup analyses explored potential moderators to further explain variability in effect size across studies. When examining region as a moderator, this model accounted for 47.38% of the between-study heterogeneity. Notably, the “cross-regional Spanish-speaking” subgroup, represented solely by Vila-Marti et al. (79), showed a significant negative effect [estimate = −0.73, 95% CI (−1.26, −0.20), p = 0.007], indicating a reversal of the typical gender effect on EE, with men reporting higher levels than women. Importantly, other regional subgroups, such as studies from Spain categorized under “Europe” or studies from Latin America, did not yield significant effects when examined separately.
Analyses by sample type showed that samples consisting of young adults and university students had a significantly higher association with EE [estimate = 0.27, 95% CI (0.03, 0.51), p = 0.028] compared to the general population and professionals, suggesting that this demographic may be more susceptible to EE behaviors. Instrument type was also examined but did not significantly influence effect size, indicating that between-study variability was not strongly dependent on the measurement approach [QM (6) = 4.78, p = 0.573]. Full subgroup estimates (k, Cohen’s d, 95% CIs, p-values, R2/I2) are reported in Supplementary Table S1.
To investigate the combined effects of moderators on EE, a mixed-effects meta-regression was conducted. This model, which included both region and sample type as moderators, significantly reduced residual heterogeneity, explaining 71.10% of the variability. Within this model, the study from the Spanish-speaking subgroup Vila-Marti et al. (79) exhibited a significantly negative effect size (estimate = −0.49, p = 0.029), whereas young adults and university students showed a significantly higher effect size (estimate = 0.24, p = 0.016), consistent with findings from the subgroup analyses. The residual heterogeneity in this combined model remained modest (I2 = 77.61%, p < 0.001), indicating that while a substantial portion of variability is explained by these moderators, additional unmeasured factors may still contribute to differences across studies.
Lastly, an examination of a potential publication bias was conducted. A funnel plot analysis, along with Egger’s test for funnel plot asymmetry [t (14) = 0.241, p = 0.813], suggested no evidence of publication bias in the included studies, indicating that the observed results are unlikely to be influenced by selective publication practices (see Figure 3).
3.4 Quality assessment
The quality assessment of the included studies revealed variations in adherence to established evaluation criteria. Most studies met key quality standards, including clear definitions of the study population, detailed descriptions of participants and settings, identification of confounding factors, valid and reliable outcome measurements, and the use of appropriate statistical methods.
However, specific shortcomings were identified in several studies. Notably, some studies lacked explicit definitions of sample inclusion criteria, including those by Bemanian et al. (64), Özcan and Yeşilkaya (82), Elmacloǧlu et al. (98), Karakose et al. (94), Lo Moro et al. (96), Modrzejewska et al. (93), Rahim et al. (99), Serin and Koç (100), and Sumalla-Cano et al. (101). Additionally, deficiencies in the identification and management of confounding variables were common. On the other hand, the following studies fulfilled both quality criteria: Hadar-Shoval et al. (65), Eşer Durmaz et al. (89), Carpio-Arias et al. (90), Ederer et al. (95), Liboredo et al. (91), Modrzejewska et al. (93), Renzo et al. (102), Ricalde-Castillo et al. (97), and Wu et al. (103).
Concerns regarding the validity and reliability of outcome measurements were limited, with only De Diego et al. (92) showing notable issues in this area. A detailed summary of the quality assessment for each study is presented in Table 4.
4 Discussion
4.1 General findings
This systematic review and meta-analysis aimed to provide a comprehensive evaluation of gender differences in EE during the COVID-19 pandemic within an adult general population. Our study provides robust evidence for significant gender differences in EE during the COVID-19 pandemic. Across the large majority of the included studies, women reported higher levels of EE than men, a trend intensified by pandemic-specific stressors such as increased anxiety, fear, loneliness, and disrupted routines (65, 82, 95). While most studies supported the evidence of gender disparities, exceptions were noted. For instance, Carpio-Arias et al. (90) found no significant gender differences in the general population, and Elmacloǧlu et al. (98) observed no changes in EE due to social isolation. However, the overall trend indicates that women were disproportionately affected by EE during the pandemic.
Several studies, e.g., Hadar-Shoval et al. (65), Vila-Marti et al. (79), Özcan and Yeşilkaya (82), Hamzaid et al. (84), Ederer et al. (95), Karakose et al. (94), and Modrzejewska et al. (93), reported that gender and pandemic-related stressors such as increased anxiety and fear, sleep disturbances and loneliness, were significant moderators of EE behavior. Women’s tendency to rely on EE as a coping mechanism is consistent with previous research highlighting their greater predisposition toward emotion-focused coping strategies when faced with stressors (37).
The regional aspect of these studies further highlights the complexity of gender differences in EE. One notable finding was from Vila-Marti et al. (79), which uniquely identified a reversal of the typical gender effect on EE within Spanish-speaking populations spanning Spain and Latin America. In this study, men reported higher mean levels of EE than women; however, women were still more likely to be categorized in the high EE group. This result underscores the potential influence of cultural factors, such as differences in emotional expression or dietary habits, on EE behaviors. Importantly, the other regional subgroups, such as Europe and Latin America examined separately, did not yield significant effects, suggesting that geographic (i.e., cultural) region may not uniformly influence gender differences in EE. Nonetheless, our study encompasses a diverse range of geographical contexts, including the Middle East, East Asia, South Asia, and cross-regional datasets, providing a broad perspective on EE behaviors. This geographical diversity strengthens the generalizability of the findings while highlighting areas for further exploration of cultural moderators of EE.
In addition, Oliveira et al. (85) identified EE as a significant predictor of food cravings in men but not in women in a Brazilian sample, highlighting further the nuanced ways in which EE may manifest across genders. This finding may reflect the distinction between EE and food cravings, where EE involves eating in response to emotional triggers like stress or anxiety, while food cravings are characterized by intense, specific desires for particular foods, often driven by physiological or sensory cues. Therefore, the results reported by Oliveira et al. (85) suggest that men’s EE might be more closely linked to food cravings, potentially due to gender differences in how emotional and physiological responses to food are processed.
The observed gender differences in EE during the COVID-19 pandemic can be partly explained by divergent stress-coping strategies. Women are more likely to engage in avoidant, passive, and emotion-focused coping mechanisms, such as self-blame and behavioral disengagement (104, 105), which can increase anxiety (58). Consequently, women are more inclined to engage in EE as a way to temporarily alleviate negative emotions such as stress, anger, anxiety, or sadness (21, 37). While this behavior may offer momentary relief, it fails to address the root causes of these stressors. Pandemic-related stressors, such as social isolation, increased caregiving responsibilities, and economic uncertainty (106), likely intensified this reliance on EE. In contrast, men tend to use more problem-focused strategies, such as active planning, seeking instrumental support, and directly confronting challenges, which are generally linked to better mental health outcomes (104, 105). However, when men do engage in EE, it tends to manifest as reward-seeking behavior, where consuming calorie-dense foods satisfies cravings and provides immediate satisfaction (85). This is consistent with physiological evidence suggesting gender differences in appetite responses to negative emotions, with women reporting increased appetite and men experiencing appetite suppression (107, 108), which may partly explain their lower EE scores.
It is challenging to determine the extent to which observed changes were directly caused by the pandemic. Only a limited number of studies were able to assess changes in gender differences in EE over time. For instance, Tazeoglu et al. (81) observed that both men and women significantly increased their EE during the quarantine period, with women consistently scoring higher than men both before and after the quarantine. Notably, this study did not find evidence of a significant exacerbation of the gender gap in EE scores during this specific period. In contrast, Özcan and Yeşilkaya (82), by comparing EE behaviors before and during the pandemic, identified a trend toward gender-specific changes. Their findings suggest that EE increased for both men and women, with a more pronounced rise in women, indicating that the pandemic may have intensified pre-existing gender-specific coping tendencies. Elmacloǧlu et al. (98) found no significant gender differences in changes in EE due to social isolation, while Hamzaid et al. (84) demonstrated a significant interaction between COVID-19-related stressors and the extent of change in EE for women (p = 0.021) but not for men (p = 0.487).
Preexisting mental health conditions likely intensified EE among women during the pandemic. Reflecting the overall higher prevalence of depression and anxiety in women (109, 110), research indicates that women experienced significantly higher levels of depression, anxiety, and stress during the first wave of the pandemic (111). This increase was partly due to heightened concerns for family well-being and increased caregiving responsibilities, which disproportionately impacted women (112). Additionally, restricted access to healthcare services during the pandemic contributed to increased anxiety and a general worsening of mental health conditions. This combination of heightened psychological stress and limited support may have led women with preexisting mental health conditions to engage in EE more frequently as a coping mechanism.
The meta-analytic findings— including 16 studies—revealed that the gender differences (with a stable effect size of Cohen’s d = 0.4) in EE were more pronounced in studies focusing on young adults and students compared to those investigating the general population and professionals. Several interconnected factors may explain this heightened effect among younger adults. Developmentally, young adulthood is a critical period marked by heightened emotional reactivity and limited impulse control, which may predispose individuals to maladaptive coping mechanisms such as EE (113, 114). For young women in particular, societal pressures related to body image and appearance, combined with greater tendencies toward emotion-focused coping strategies, may amplify their susceptibility to EE compared to young men (62, 63). Moreover, pandemic-specific stressors, such as disruptions to education, early career paths, and social connections, disproportionately impacted younger adults (115, 116). These combined biological, psychological, and sociocultural factors likely contributed to the observed intensified gender differences in EE within younger adult populations, underscoring the need for targeted interventions tailored to this demographic.
Based on the results of this study, important implications arise for public health strategies designed to mitigate the long-term health risks associated with EE. The elevated gender disparities observed in young adult samples emphasize the urgency of developing tailored, gender-specific interventions aimed at improving emotion regulation and stress management. Women’s heightened reliance on EE as a coping mechanism highlights the need for targeted interventions during crises, addressing both immediate emotional needs and the underlying stressors. Given the established link between EE and obesity, as well as the greater burden of obesity-related health conditions on women (117), such strategies are crucial for reducing health disparities and promoting equitable health outcomes (118).
Young adults and university students, identified as particularly vulnerable to EE, require special consideration in public health initiatives. The greater gender disparities observed in this demographic suggest that age-related developmental factors, such as higher emotional reactivity and less effective impulse control, may exacerbate the tendency toward EE (119), particularly in young adults (120). These findings point to the necessity of resilience-building programs that integrate gender-sensitive approaches, providing education on stress management, emotion regulation, and healthy coping strategies. Establishing support networks and increasing access to mental health services tailored for this age group could mitigate the negative impacts of EE, reduce gender disparities, and foster healthier long-term behaviors.
Our findings also point to the importance of tailoring interventions to gender-specific needs. For women, who more frequently report EE as a coping strategy, interventions may focus on strengthening adaptive coping mechanisms and stress regulation. For men, however, the lower reported levels of EE might partly reflect difficulties in perceiving, labeling, or acknowledging emotional states. This suggests that interventions for men may benefit from emphasizing emotional literacy and recognition, ensuring that maladaptive eating patterns are not overlooked simply because they are not self-identified as “emotional eating.” By addressing both coping and awareness, gender-sensitive programs can more effectively reduce EE-related health risks and promote equitable outcomes.
4.2 Limitations and future directions
Several limitations should be noted when interpreting the findings of this systematic review and meta-analysis. First, most of the included studies were cross-sectional, which limits the ability to establish causal relationships between pandemic conditions and changes in EE. Cross-sectional designs capture data at a single point in time and cannot account for changes in eating behaviors compared to pre-pandemic baselines, potentially introducing bias (121, 122). Longitudinal research during times of crises is essential to elucidate the causal and gender-specific pathways linking pandemic-related stressors to psychopathology, e.g., EE behaviors. In addition, we did not systematically search the grey literature (e.g., dissertations, reports, preprints). This may have excluded relevant non-indexed studies and increased the risk of publication bias. However, we formally assessed publication bias (funnel plot and Egger’s test), and the results did not indicate substantial bias, which mitigates this concern. Another limitation is the potential selection bias within the studies included in the meta-analysis, as many focused on specific populations, such as students, certain geographic regions, or professional groups, which may limit their representativeness for the general population. This limits the generalizability of the findings to broader or more diverse groups. Furthermore, the over-representation of certain demographic groups, such as younger adults, may have influenced the results, as EE is often more prevalent in these populations. To address this limitation, we conducted subgroup analyses to explore potential variations across different demographic groups and regions.
The quality assessment identified variations in adherence to the defined evaluation criteria. While most studies fulfilled key quality standards, notable shortcomings were observed. The most prevalent issues included unclear inclusion criteria and inadequate consideration of confounding factors, which may have implications for the robustness of the findings.
Self-report measures used in the included studies, such as the EEQ, TFEQ, DEBQ, and EES may also be subject to bias. Participants may underreport or overreport their behaviors due to social desirability or recall bias, particularly in the context of sensitive topics such as EE. This may affect the accuracy of the reported gender differences and undermine the reliability of the conclusions. The variation in measurement tools across studies is another limitation. Different instruments assess EE in slightly different ways, which may contribute to variability in the results. While tools like the EEQ, TFEQ, DEBQ, and EES are widely used, inconsistencies in how EE is conceptualized and measured could affect the comparability of the findings across studies. To mitigate this limitation, again, we conducted subgroup analyses to examine the potential impact of different measurement tools on the results.
Moreover, pandemic-related stressors, such as social isolation and caregiving responsibilities, were found to exacerbate EE in women (84, 95), however, the role of other psychological and social factors, such as pre-existing mental health conditions and socioeconomic status, has not been fully explored. Future research should consider these factors, as they may further contribute to gender differences in EE during stressful events like a pandemic.
Finally, although some included studies mentioned categories beyond the binary gender classification (e.g., “other” or “not specified” gender), none provided detailed analyses for these groups. As a result, our meta-analysis could only address gender differences between women and men. This limitation highlights the urgent need for future studies to systematically include and analyze data from individuals with diverse gender identities to better capture the full spectrum of EE behaviors.
5 Conclusion
This review provides valuable insights into gender differences in EE in the general population during the COVID-19 pandemic, combining a robust narrative synthesis with a meta-analysis that spans diverse populations and geographical regions. By examining cross-country data and emphasizing gender-specific differences, this study contributes to a deeper understanding of how pandemic-related stressors have uniquely affected EE. The inclusion of studies utilizing a variety of methodologies further strengthens the reliability of the findings. Despite these contributions, several limitations highlight the need for further research, particularly longitudinal studies, to better understand causal pathways and gender-specific responses to stressors. Addressing these gaps in future research will be crucial to developing more effective, gender-sensitive approaches to manage EE and its associated health risks.
Data availability statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request. Access to some data may be restricted due to copyright or data protection regulations. Requests to access these datasets should be directed to christopher.zaiser@ruhr-uni-bochum.de.
Author contributions
CZ: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Software, Visualization, Writing – original draft, Writing – review & editing. MP: Data curation, Formal analysis, Software, Writing – original draft, Writing – review & editing. GB: Software, Writing – original draft, Writing – review & editing. CB: Software, Writing – original draft, Writing – review & editing. LS: Software, Writing – original draft, Writing – review & editing. NL: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Software, Writing – original draft, Writing – review & editing. GP: Funding acquisition, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This publication was supported by the German Federal Ministry of Education and Research (BMBF) Network of University Medicine 2.0: “NUM 2.0”, Grant No. 01KX2121, Project: (Collateral Effects in Pandemics-CollPan).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2025.1680872/full#supplementary-material
References
1. Cucinotta, D, and Vanelli, M. Who declares COVID-19 a pandemic. Acta Biomed. (2020) 91:157–60. doi: 10.23750/abm.v91i1.9397
2. Harder, T, Külper-Schiek, W, Reda, S, Treskova-Schwarzbach, M, Koch, J, Vygen-Bonnet, S, et al. Effectiveness of COVID-19 vaccines against SARS-CoV-2 infection with the Delta (B.1.617.2) variant: second interim results of a living systematic review and meta-analysis, 1 January to 25 August 2021. Euro Surveill. (2021) 26:2100920. doi: 10.2807/1560-7917.ES.2021.26.41.2100920
3. Caroppo, E, Mazza, M, Sannella, A, Marano, G, Avallone, C, Claro, AE, et al. Will nothing be the same again?: changes in lifestyle during COVID-19 pandemic and consequences on mental health. Int J Environ Res Public Health. (2021) 18:8433. doi: 10.3390/ijerph18168433
4. Ashraf, BN. Economic impact of government interventions during the COVID-19 pandemic: international evidence from financial markets. J Behav Exp Finance. (2020) 27:100371. doi: 10.1016/j.jbef.2020.100371
5. Manchia, M, Gathier, AW, Yapici-Eser, H, Schmidt, MV, de Quervain, D, van Amelsvoort, T, et al. The impact of the prolonged COVID-19 pandemic on stress resilience and mental health: a critical review across waves. Eur Neuropsychopharmacol. (2022) 55:22–83. doi: 10.1016/j.euroneuro.2021.10.864
6. Gao, Y, Bagheri, N, and Furuya-Kanamori, L. Has the COVID-19 pandemic lockdown worsened eating disorders symptoms among patients with eating disorders? A systematic review. J Public Health. (2022) 30:2743–52. doi: 10.1007/s10389-022-01704-4
7. Ramalho, SM, Trovisqueira, A, de Lourdes, M, Gonçalves, S, Ribeiro, I, Vaz, AR, et al. The impact of COVID-19 lockdown on disordered eating behaviors: the mediation role of psychological distress. Eat Weight Disord. (2022) 27:179–88. doi: 10.1007/s40519-021-01128-1
8. Arnow, B, Kenardy, J, and Agras, WS. The emotional eating scale: The development of a measure to assess coping with negative affect by eating. Int J Eat Disord. (1995) 18:79–90. doi: 10.1002/1098-108X(199507)18:1<79::AID-EAT2260180109>3.0.CO;2-V
9. Madalı, B, Alkan, ŞB, Örs, ED, Ayrancı, M, Taşkın, H, and Kara, HH. Emotional eating behaviors during the COVID-19 pandemic: a cross-sectional study. Clin Nutr ESPEN. (2021) 46:264–70. doi: 10.1016/j.clnesp.2021.09.745
10. Varela, C, Andrés, A, and Saldaña, C. The behavioral pathway model to overweight and obesity: coping strategies, eating behaviors and body mass index. Eat Weight Disord. (2020) 25:1277–83. doi: 10.1007/s40519-019-00760-2
11. Chao, A, Grey, M, Whittemore, R, Reuning-Scherer, J, Grilo, CM, and Sinha, R. Examining the mediating roles of binge eating and emotional eating in the relationships between stress and metabolic abnormalities. J Behav Med. (2016) 39:320–32. doi: 10.1007/s10865-015-9699-1
12. Wiedemann, AA, Ivezaj, V, and Grilo, CM. An examination of emotional and loss-of-control eating after sleeve gastrectomy surgery. Eat Behav. (2018) 31:48–52. doi: 10.1016/j.eatbeh.2018.07.008
13. Crowley, N, Madan, A, Wedin, S, Correll, JA, Delustro, LM, Borckardt, JJ, et al. Food cravings among bariatric surgery candidates. Eat Weight Disord. (2014) 19:371–6. doi: 10.1007/s40519-013-0095-y
14. Camilleri, GM, Méjean, C, Kesse-Guyot, E, Andreeva, VA, Bellisle, F, Hercberg, S, et al. The associations between emotional eating and consumption of energy-dense snack foods are modified by sex and depressive symptomatology. J Nutr. (2014) 144:1264–73. doi: 10.3945/jn.114.193177
15. O’Connor, DB, Jones, F, Conner, M, Mcmillan, B, and Ferguson, E. Effects of daily hassles and eating style on eating behavior. Health Psychol. (2008) 27:S20–31. doi: 10.1037/0278-6133.27.1.S20
16. Bullock, AJ, and Goldbacher, EM. Interoceptive awareness and emotional eating in college women: the role of appetite and emotional awareness. J Am Coll Heal. (2023) 71:2445–50. doi: 10.1080/07448481.2021.1970566
17. Jenkinson, PM, Taylor, L, and Laws, KR. Self-reported interoceptive deficits in eating disorders: a meta-analysis of studies using the eating disorder inventory. J Psychosom Res. (2018) 110:38–45. doi: 10.1016/j.jpsychores.2018.04.005
18. Brewer, R, Cook, R, and Bird, G. Alexithymia: a general deficit of interoception. R Soc Open Sci. (2016) 3:150664. doi: 10.1098/rsos.150664
19. Heatherton, TE, and Baumeister, RF. Binge eating as escape from self-awareness. Psychol Bull. (1991) 110:8–108. doi: 10.1037/0033-2909.110.1.86
20. Finch, LE, and Tomiyama, AJ. Stress-induced eating dampens physiological and behavioral stress responses In: Nutrition in the prevention and treatment of abdominal obesity. 2nd ed. Amsterdam: Elsevier Inc. (2014). 189–95.
21. Klatzkin, RR, Nolan, LJ, and Kissileff, HR. Self-reported emotional eaters consume more food under stress if they experience heightened stress reactivity and emotional relief from stress upon eating. Physiol Behav. (2022) 243:113638. doi: 10.1016/j.physbeh.2021.113638
22. Altheimer, G, and Urry, HL. Do emotions cause eating? The role of previous experiences and social context in emotional eating. Curr Dir Psychol Sci. (2019) 28:234–40. doi: 10.1177/0963721419837685
23. Jackson, A, Anderson, A, Weybright, E, and Lanigan, J. Differing experiences of boredom during the pandemic and associations with dietary behaviors. J Nutr Educ Behav. (2021) 53:706–11. doi: 10.1016/j.jneb.2021.04.005
24. Schneider, KL, Appelhans, BM, Whited, MC, Oleski, J, and Pagoto, SL. Trait anxiety, but not trait anger, predisposes obese individuals to emotional eating. Appetite. (2010) 55:701–6. doi: 10.1016/j.appet.2010.10.006
25. Dakanalis, A, Mentzelou, M, Papadopoulou, SK, Papandreou, D, Spanoudaki, M, Vasios, GK, et al. The association of emotional eating with overweight/obesity, depression, anxiety/stress, and dietary patterns: a review of the current clinical evidence. Nutrients. (2023) 15:1173. doi: 10.3390/nu15051173
26. Tan, CC, and Chow, CM. Stress and emotional eating: the mediating role of eating dysregulation. Pers Individ Dif. (2014) 66:1–4. doi: 10.1016/j.paid.2014.02.033
27. Miniati, M, Marzetti, F, Palagini, L, Marazziti, D, Orrù, G, Conversano, C, et al. Eating disorders spectrum during the COVID pandemic: a systematic review. Front Psychol. (2021) 12:663376. doi: 10.3389/fpsyg.2021.663376
28. Muscogiuri, G, Barrea, L, Aprano, S, Framondi, L, di Matteo, R, Laudisio, D, et al. Sleep quality in obesity: does adherence to the Mediterranean diet matter? Nutrients. (2020) 12:1364. doi: 10.3390/nu12051364
29. Rodríguez-Hidalgo, AJ, Pantaleón, Y, Dios, I, and Falla, D. Fear of COVID-19, stress, and anxiety in university undergraduate students: a predictive model for depression. Front Psychol. (2020) 11:591797. doi: 10.3389/fpsyg.2020.591797
30. Moynihan, AB, van Tilburg, WAP, Igou, ER, Wisman, A, Donnelly, AE, and Mulcaire, JB. Eaten up by boredom: consuming food to escape awareness of the bored self. Front Psychol. (2015) 6:369. doi: 10.3389/fpsyg.2015.00369
31. Yılmaz, C, and Gökmen, V. Neuroactive compounds in foods: occurrence, mechanism and potential health effects. Food Res Int. (2020) 128:108744. doi: 10.1016/j.foodres.2019.108744
32. Richardson, C, Patton, M, Phillips, S, and Paslakis, G. The impact of the COVID-19 pandemic on help-seeking behaviors in individuals suffering from eating disorders and their caregivers. Gen Hosp Psychiatry. (2020) 67:136–40. doi: 10.1016/j.genhosppsych.2020.10.006
33. Richardson, C, Phillips, S, and Paslakis, G. One year in: The impact of the COVID-19 pandemic on help-seeking behaviors among youth experiencing eating disorders and their caregivers. Psychiatry Res. (2021) 306:114263. doi: 10.1016/j.psychres.2021.114263
34. Devoe, DJ, Anderson, A, Bahji, A, Singh, M, Patten, SB, Soumbasis, A, et al. The prevalence of impulse control disorders and behavioral addictions in eating disorders: a systematic review and meta-analysis. Front Psychiatry. (2022) 12:724034. doi: 10.3389/fpsyt.2021.724034
35. Laskowski, NM, Brandt, G, Reque, CB, Sabel, L, Pahlenkemper, M, Zaiser, C, et al. The collateral effects of the COVID-19 pandemic: a gender-specific systematic review of disordered eating behaviour in the general population. Eur Eat Disord Rev. (2024) 33:254–88. doi: 10.1002/erv.3141
36. Du, C, Adjepong, M, Zan, MCH, Cho, MJ, Fenton, JI, Hsiao, PY, et al. Gender differences in the relationships between perceived stress, eating behaviors, sleep, dietary risk, and body mass index. Nutrients. (2022) 14:1045. doi: 10.3390/nu14051045
37. Guerrero-Hreins, E, Stammers, L, Wong, L, Brown, RM, and Sumithran, P. A comparison of emotional triggers for eating in men and women with obesity. Nutrients. (2022) 14:4144. doi: 10.3390/nu14194144
38. Larsen, JK, Van Strien, T, Eisinga, R, and Engels, RCME. Gender differences in the association between alexithymia and emotional eating in obese individuals. J Psychosom Res. (2006) 60:237–43. doi: 10.1016/j.jpsychores.2005.07.006
39. Thompson, S. Gender and racial differences in emotional eating, food addiction symptoms, and body weight satisfaction among undergraduates. J Diabetes Obes. (2015) 2:1–6. doi: 10.15436/2376-0494.15.035
40. Smith, JM, Serier, KN, Belon, KE, Sebastian, RM, and Smith, JE. Evaluation of the relationships between dietary restraint, emotional eating, and intuitive eating moderated by sex. Appetite. (2020) 155:104817. doi: 10.1016/j.appet.2020.104817
41. Rosenqvist, E, Kiviruusu, O, Berg, N, and Konttinen, H. Stress-induced eating and drinking and their associations with weight among women and men during 30-year follow-up. Psychol Health. (2023) 40:1–16. doi: 10.1080/08870446.2023.2192240
42. Braden, A, Musher-Eizenman, D, Watford, T, and Emley, E. Eating when depressed, anxious, bored, or happy: are emotional eating types associated with unique psychological and physical health correlates? Appetite. (2018) 125:410–7. doi: 10.1016/j.appet.2018.02.022
43. Wang, L, Shi, C, Zhang, K, and Xu, Q. The gender-specific association of EHD3 polymorphisms with major depressive disorder. Neurosci Lett. (2014) 567:11–4. doi: 10.1016/j.neulet.2014.02.055
44. Wong, L, Stammers, L, Churilov, L, Price, S, Ekinci, E, and Sumithran, P. Emotional eating in patients attending a specialist obesity treatment service. Appetite. (2020) 151:104708. doi: 10.1016/j.appet.2020.104708
45. Araujo, DMR, da Silva Santos, GF, and Nardi, AE. Binge eating disorder and depression: a systematic review. World J Biol Psychiatry. (2010) 11:199–207. doi: 10.3109/15622970802563171
46. Brandt, G, Halbeisen, G, Braks, K, Huber, TJ, and Paslakis, G. Gender differences in individuals with obesity and binge eating disorder: a retrospective comparison of phenotypical features and treatment outcomes. Eur Eat Disord Rev. (2023) 31:413–24. doi: 10.1002/erv.2972
47. Fischer, AH, Kret, ME, and Broekens, J. Gender differences in emotion perception and self-reported emotional intelligence: a test of the emotion sensitivity hypothesis. PLoS One. (2018) 13:e0190712. doi: 10.1371/journal.pone.0190712
48. Cholankeril, R, Xiang, E, and Badr, H. Gender differences in coping and psychological adaptation during the COVID-19 pandemic. Int J Environ Res Public Health. (2023) 20:993. doi: 10.3390/ijerph20020993
49. Ling, J, and Zahry, NR. Relationships among perceived stress, emotional eating, and dietary intake in college students: eating self-regulation as a mediator. Appetite. (2021) 163:105215. doi: 10.1016/j.appet.2021.105215
50. Troisi, A. Gender differences in vulnerability to social stress a Darwinian perspective. Physiol Behav. (2001) 73:443–9. doi: 10.1016/s0031-9384(01)00459-0
51. Dedovic, K, Wadiwalla, M, Engert, V, and Pruessner, JC. The role of sex and gender socialization in stress reactivity. Dev Psychol. (2009) 45:45–55. doi: 10.1037/a0014433
52. Juster, RP, de Torre, MB, Kerr, P, Kheloui, S, Rossi, M, and Bourdon, O. Sex differences and gender diversity in stress responses and allostatic load among workers and LGBT people. Curr Psychiatry Rep. (2019) 21:110. doi: 10.1007/s11920-019-1104-2
53. Wang, J, Korczykowski, M, Rao, H, Fan, Y, Pluta, J, Gur, RC, et al. Gender difference in neural response to psychological stress. Soc Cogn Affect Neurosci. (2007) 2:227–39. doi: 10.1093/scan/nsm018
54. Heck, AL, and Handa, RJ. Sex differences in the hypothalamic–pituitary–adrenal axis’ response to stress: an important role for gonadal hormones. Neuropsychopharmacology. (2019) 44:45–58. doi: 10.1038/s41386-018-0167-9
55. Martinez-Muniz, GA, and Wood, SK. Sex differences in the inflammatory consequences of stress: implications for pharmacotherapy. J Pharmacol Exp Ther. (2020) 375:161–74. doi: 10.1124/JPET.120.266205
56. Butler, LD, and Nolen-Hoeksema, S. Gender differences in responses to depressed mood in a college sample. Sex Roles. (1994) 30:331–46. doi: 10.1007/BF01420597
57. Thomsen, DK, Mehlsen, MY, Viidik, A, Sommerlund, B, and Zachariae, R. Age and gender differences in negative affect—is there a role for emotion regulation? Pers Individ Dif. (2005) 38:1935–46. doi: 10.1016/j.paid.2004.12.001
58. Kelly, MM, Tyrka, AR, Price, LH, and Carpenter, LL. Sex differences in the use of coping strategies: predictors of anxiety and depressive symptoms. Depress Anxiety. (2008) 25:839–46. doi: 10.1002/da.20341
59. Cecchetto, C, Aiello, M, Gentili, C, Ionta, S, and Osimo, SA. Increased emotional eating during COVID-19 associated with lockdown, psychological and social distress. Appetite. (2021) 160:105122. doi: 10.1016/j.appet.2021.105122
60. Waterschoot, J, Morbée, S, Vermote, B, Brenning, K, Flamant, N, Vansteenkiste, M, et al. Emotion regulation in times of COVID-19: a person-centered approach based on self-determination theory. Curr Psychol. (2023) 42:20211–25. doi: 10.1007/s12144-021-02623-5
61. Xu, F, and Huang, L. Impacts of stress response and negative emotion on mental health of college students during the COVID-19 outbreak. Front Psychiatry. (2022) 12:784661. doi: 10.3389/fpsyt.2021.784661
62. Ata, RN, Ludden, AB, and Lally, MM. The effects of gender and family, friend, and media influences on eating behaviors and body image during adolescence. J Youth Adolesc. (2007) 36:1024–37. doi: 10.1007/s10964-006-9159-x
63. Shriver, LH, Dollar, JM, Calkins, SD, Keane, SP, Shanahan, L, and Wideman, L. Emotional eating in adolescence: effects of emotion regulation, weight status and negative body image. Nutrients. (2021) 13:79. doi: 10.3390/nu13010079
64. Bemanian, M, Mæland, S, Blomhoff, R, Rabben, ÅK, Arnesen, EK, Skogen, JC, et al. Emotional eating in relation to worries and psychological distress amid the COVID-19 pandemic: a population-based survey on adults in Norway. Int J Environ Res Public Health. (2021) 18:130. doi: 10.3390/ijerph18010130
65. Hadar-Shoval, D, Alon-Tirosh, M, Asraf, K, Tannous-Haddad, L, and Tzischinsky, O. Lifestyle changes, emotional eating, gender, and stress during COVID-19 lockdown. Nutrients. (2022) 14:3868. doi: 10.3390/nu14183868
66. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. Statement: an updated guideline for reporting systematic reviews. BMJ. (2020) 372:372. doi: 10.1136/bmj.n71
67. Veritas Health Innovation. (2024). Covidence. Available online at: https://www.covidence.org/. (Accessed September 18, 2024)
68. Joanna Briggs Institute. (2017). Checklist for analytical cross sectional studies. Available online at: https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Analytical_Cross_Sectional_Studies2017_0.pdf (Accessed October 9, 2025).
69. Ma, LL, Wang, YY, Yang, ZH, Huang, D, Weng, H, and Zeng, XT. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: What are they and which is better? Mil Med Res. (2020) 7:7. doi: 10.1186/s40779-020-00238-8
70. R Core Team. (2021). R: a language and environment for statistical computing. Available online at: https://www.r-project.org/. (Accessed November 11, 2024)
71. Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J Stat Softw. (2010) 36:1–48. doi: 10.18637/jss.v036.i03
72. Stroup, DF. Meta-analysis of observational studies in epidemiology. JAMA. (2000) 283:2008. doi: 10.1001/jama.283.15.2008
73. Garaulet, M, Canteras, M, Morales, E, López-Guimera, G, Sánchez-Carracedo, D, and Corbalán-Tutau, MD. Validation of a questionnaire on emotional eating for use in cases of obesity: the Emotional Eater Questionnaire (EEQ). Nutr Hosp. (2012) 27:645–51. doi: 10.1590/S0212-16112012000200043
74. Karlsson, J, Persson, LO, Sjöström, L, and Sullivan, M. Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish obese subjects (SOS) study. Int J Obes. (2000) 24:1715–25. doi: 10.1038/sj.ijo.0801442
75. Cappelleri, JC, Bushmakin, AG, Gerber, RA, Leidy, NK, Sexton, CC, Lowe, MR, et al. Psychometric analysis of the Three-Factor Eating Questionnaire-R21: results from a large diverse sample of obese and non-obese participants. Int J Obes. (2009) 33:611–20. doi: 10.1038/ijo.2009.74
76. Schlundt, DG, Hargreaves, MK, and Buchowski, MS. The Eating Behavior Patterns Questionnaire predicts dietary fat intake in African American women. J Am Diet Assoc. (2003) 103:338–45. doi: 10.1053/jada.2003.50049
77. van Strien, T, Frijters, JER, Bergers, GPA, and Defares, PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional and external eating behavior. Int J Eat Disord. (1986) 5:295–315. doi: 10.1002/1098-108X(198602)5:2<>3.0.CO;2-T
78. Masheb, RM, and Grilo, CM. Emotional overeating and its associations with eating disorder psychopathology among overweight patients with Binge eating disorder. Int J Eat Disord. (2006) 39:141–6. doi: 10.1002/eat.20221
79. Vila-Marti, A, Ramírez-Contreras, C, Apolinar-Jiménez, E, Rojas-Cárdenas, P, Valera-Gran, D, Almendra-Pegueros, R, et al. Factors associated with dietary restriction and emotional and uncontrolled eating in adults from Spanish-speaking countries during the COVID-19 confinement: results of the CoV-Eat Project. Nutrients. (2022) 14:4866. doi: 10.3390/nu14224866
80. Gearhardt, AN, Corbin, WR, and Brownell, KD. Preliminary validation of the Yale Food Addiction Scale. Appetite. (2009) 52:430–6. doi: 10.1016/j.appet.2008.12.003
81. Tazeoglu, A, Bozdogan, FBK, and Idiz, C. Evaluation of osmaniye korkut ata university students’ eating behaviors during the quarantine period during the COVID-19 pandemic period. Nutr Clin Diet Hosp. (2021) 41:86–93. doi: 10.12873/412tazeoglu
82. Özcan, BA, and Yeşilkaya, B. Adverse effect of emotional eating developed during the COVID-19 pandemic on healthy nutrition, a vicious circle: a cross-sectional descriptive study. Rev Esp Nutr Hum Diet. (2021):25. doi: 10.14306/renhyd.25.S2.1144
83. Carpio-Arias, TV, Piedra-Andrade, JS, Nicolalde-Cifuentes, TM, Padilla-Samaniego, MV, Tapia-Veloz, EC, and Vinueza-Veloz, MF. Mobility restrictions and mental health among young adults during the COVID-19 pandemic in Ecuador. Gac Sanit. (2022) 36:512–9. doi: 10.1016/j.gaceta.2021.12.008
84. Hamzaid, NH, Gumisi, ZGR, Ahmad Helme, SK, Azmi, N, and Shahril, MR. Lifestyle and psychological factors affecting eating habits and physical activity among government servants in the states with the highest cumulative cases in Malaysia during the COVID-19 pandemic. Front Public Health. (2022) 10:816530. doi: 10.3389/fpubh.2022.816530
85. Oliveira, LA, Della Lucia, CM, Rezende, FAC, Ferreira, LG, Anastácio, LR, Souza, TC d M, et al. Food craving and its associated factors during COVID-19 outbreak in Brazil. Am J Health Educ. (2022) 53:207–18. doi: 10.1080/19325037.2022.2071360
86. Usubini, AG, Cattivelli, R, Varallo, G, Guerrini Usubini, A, Castelnuovo, G, Molinari, E, et al. The relationship between psychological distress during the second wave lockdown of COVID-19 and emotional eating in Italian young adults: the mediating role of emotional dysregulation. J Pers Med. (2021) 11:569. doi: 10.3390/jpm11060569
87. Göbel, P, Sanlier, N, Yilmaz, S, Açikalin, B, and Kocabaş, Ş. The correlation between social media addiction and emotional eating during the COVID-19 quarantine period. Ecol Food Nutr. (2023) 62:60–74. doi: 10.1080/03670244.2023.2179044
88. Yoldas Ilktac, H, Savci, C, and Cil Akinci, A. Nutritional behavior during the COVID-19 pandemic: the association of fear and sleep quality with emotional eating. Eat Weight Disord. (2022) 27:2673–83. doi: 10.1007/s40519-022-01409-3
89. Eşer Durmaz, S, Keser, A, and Tunçer, E. Effect of emotional eating and social media on nutritional behavior and obesity in university students who were receiving distance education due to the COVID-19 pandemic. J Public Health. (2023) 31:1645–54. doi: 10.1007/s10389-022-01735-x
90. Carpio-Arias, TV, Solís Manzano, AM, Sandoval, V, Vinueza-Veloz, AF, Rodríguez Betancourt, A, Betancourt Ortíz, SL, et al. Relationship between perceived stress and emotional eating. A cross sectional study. Clin Nutr ESPEN. (2022) 49:314–8. doi: 10.1016/j.clnesp.2022.03.030
91. Liboredo, JC, Anastácio, LR, Ferreira, LG, Oliveira, LA, and Della Lucia, CM. Quarantine during COVID-19 outbreak: eating behavior, perceived stress, and their independently associated factors in a Brazilian sample. Front Nutr. (2021) 8:704619. doi: 10.3389/fnut.2021.704619
92. De Diego, EH, Zapatera, B, Frías, J, and Gómez-Martínez, S. Healthy habits in CSIC workers during COVID-19 lockdown in Spain. Arbor. (2022) 198:a681. doi: 10.3989/arbor.2022.806011
93. Modrzejewska, A, Czepczor-Bernat, K, Modrzejewska, J, and Matusik, P. Eating motives and other factors predicting emotional overeating during COVID-19 in a sample of Polish adults. Nutrients. (2021) 13:1658. doi: 10.3390/nu13051658
94. Karakose, T, Yirci, R, Basyigit, H, and Kucukcakir, A. Investigation of associations between the effects of COVID-19 fear on school administrators and nutrition and problematic eating behaviors. Prog Nutr. (2021) 23:e2021187. doi: 10.23751/pn.v23i2.11656
95. Ederer, DJ, Lee, SH, Belay, B, Boutelle, K, and Park, S. Associations between comfort eating and weight change during the COVID-19 pandemic among U.S. adults. Human Nutr Metab. (2023) 33:200212. doi: 10.1016/j.hnm.2023.200212
96. Lo Moro, G, Bert, F, Catozzi, D, Scacchi, A, and Siliquini, R. Emotional eating and depression during the pandemic: QuarantEat, an Italian nationwide survey. Nutrition. (2022) 103-104:111825–104. doi: 10.1016/j.nut.2022.111825
97. Ricalde-Castillo, Y, Celis-Mendoza, M, Morales-García, M, Huancahuire-Vega, S, Calizaya-Milla, YE, Saintila, J, et al. Sociodemographic factors, mental health, and emotional eating associated with concern for COVID-19 contagion in nurses: a cross-sectional study. J Prim Care Community Health. (2023) 14:21501319231200400. doi: 10.1177/21501319231200400
98. Elmacloǧlu, F, Emiroǧlu, E, Ülker, MT, Özyllmaz Klrcali, B, and Oruç, S. Evaluation of nutritional behaviour related to COVID-19. Public Health Nutr. (2021) 24:512–8. doi: 10.1017/S1368980020004140
99. Rahim, HA, Hoseini, R, Hoseini, Z, Abbas, EN, and Kareem, DA. Health-related factors of the Iraqi adult population during the 2020 COVID-19 pandemic: physical activity, eating behavior, quality of life, general health, and mood states cross-talk. BMC Public Health. (2023) 23:1046. doi: 10.1186/s12889-023-15898-z
100. Serin, E, and Koç, MC. Examination of the eating behaviours and depression states of the university students who stay at home during the coronavirus pandemic in terms of different variables. Prog Nutr. (2020) 22:33–43. doi: 10.23751/pn.v22i1-S.9780
101. Sumalla-Cano, S, Forbes-Hernández, T, Aparicio-Obregón, S, Crespo, J, Eléxpuru-Zabaleta, M, Gracia-Villar, M, et al. Changes in the lifestyle of the Spanish university population during confinement for COVID-19. Int J Environ Res Public Health. (2022) 19:2210. doi: 10.3390/ijerph19042210
102. Di, RL, Gualtieri, P, Cinelli, G, Bigioni, G, Soldati, L, Attinà, A, et al. Psychological aspects and eating habits during COVID-19 home confinement: results of EHLC-COVID-19 Italian online survey. Nutrients. (2020) 12:2152. doi: 10.3390/nu12072152
103. Wu, C, Hao, M, Liu, X, Yang, D, Liu, B, Yan, W, et al. The effects of body dissatisfaction and depression levels on the dietary habits of university students in southern China during COVID-19. Front Nutr. (2023) 10:1103724. doi: 10.3389/fnut.2023.1103724
104. Smriti Sinha, LG. Coping response to same stressors varies with gender. Natl J Physiol Pharm Pharmacol. (2018) 8:1053–6. doi: 10.5455/njppp.2018.8.0206921032018
105. Braun-Lewensohn, O. Coping strategies as mediators of the relationship between chronic exposure to missile attacks and stress reactions. J Child Adolesc Trauma. (2012) 5:315–26. doi: 10.1080/19361521.2012.719596
106. United Nations. UN Secretary-General’s policy brief: the impact of COVID-19 on women. New York: UN Women Office Publishing (2020).
107. Marcus, SM, Young, EA, Kerber, KB, Kornstein, S, Farabaugh, AH, Mitchell, J, et al. Gender differences in depression: findings from the STAR*D study. J Affect Disord. (2005) 87:141–50. doi: 10.1016/j.jad.2004.09.008
108. Alexandrino-Silva, C, Wang, YP, Carmen Viana, M, Bulhões, RS, Martins, SS, and Andrade, LH. Gender differences in symptomatic profiles of depression: results from the São Paulo megacity mental health survey. J Affect Disord. (2013) 147:355–64. doi: 10.1016/j.jad.2012.11.041
109. McLean, CP, Asnaani, A, Litz, BT, and Hofmann, SG. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. (2011) 45:1027–35. doi: 10.1016/j.jpsychires.2011.03.006
110. Albert, PR. Why is depression more prevalent in women? J Psychiatry Neurosci. (2015) 40:219–21. doi: 10.1503/jpn.150205
111. Opanković, A, Latas, M, Jerotić, S, Ristić, I, and Milovanović, S. Gender differences in depression, anxiety, and stress during the first wave of the COVID-19 pandemic in Serbia—results from an online survey. Eur Psychiatry. (2021) 64:S270. doi: 10.1192/j.eurpsy.2021.724
112. Queen, C, Pasupathy, R, and Reine, I. Multi-method analysis of gender differences in psychological distress among the elderly during COVID. Eur J Pub Health. (2022) 32:ckac130.207. doi: 10.1093/eurpub/ckac130.207
113. Elran Barak, R, Shuval, K, Li, Q, Oetjen, R, Drope, J, Yaroch, AL, et al. Emotional eating in adults: the role of sociodemographics, lifestyle behaviors, and self-regulation—findings from a U.S. national study. Int J Environ Res Public Health. (2021) 18:1744. doi: 10.3390/ijerph18041744
114. Lamichhane, B, Di Rosa, E, and Braver, TS. Delay of gratification dissociates cognitive control and valuation brain regions in healthy young adults. Neuropsychologia. (2022) 173:108303. doi: 10.1016/j.neuropsychologia.2022.108303
115. Glowacz, F, and Schmits, E. Psychological distress during the COVID-19 lockdown: the young adults most at risk. Psychiatry Res. (2020) 293:113486. doi: 10.1016/j.psychres.2020.113486
116. Lee, J, Jeong, HJ, and Kim, S. Stress, anxiety, and depression among undergraduate students during the COVID-19 pandemic and their use of mental health services. Innov High Educ. (2021) 46:519–38. doi: 10.1007/s10755-021-09552-y
117. Muennig, P, Lubetkin, E, Jia, H, and Franks, P. Gender and the burden of disease attributable to obesity. Am J Public Health. (2006) 96:1662–8. doi: 10.2105/AJPH.2005.068874
118. Kapoor, N, Arora, S, and Kalra, S. Gender disparities in people living with obesity—an unchartered territory. J Midlife Health. (2021) 12:103–7. doi: 10.4103/jmh.jmh_48_21
119. Van Blyderveen, S, Lafrance, A, Emond, M, Kosmerly, S, O’Connor, M, and Chang, F. Personality differences in the susceptibility to stress-eating: the influence of emotional control and impulsivity. Eat Behav. (2016) 23:76–81. doi: 10.1016/j.eatbeh.2016.07.009
120. Yang, H, Zhou, X, Xie, L, and Sun, J. The effect of emotion regulation on emotional eating among undergraduate students in China: the chain mediating role of impulsivity and depressive symptoms. PLoS One. (2023) 18:e0280701. doi: 10.1371/journal.pone.0280701
121. Chew, HSJ, and Lopez, V. Global impact of COVID-19 on weight and weight-related behaviors in the adult population: a scoping review. Int J Environ Res Public Health. (2021) 18:1876. doi: 10.3390/ijerph18041876
122. Neira, C, Godinho, R, Rincón, F, Mardones, R, and Pedroso, J. Consequences of the COVID-19 syndemic for nutritional health: a systematic review. Nutrients. (2021) 13:1168. doi: 10.3390/nu13041168
123. Barcln-Güzeldere, HK, and Devrim-Lanpir, A. The association between body mass index, emotional eating and perceived stress during COVID-19 partial quarantine in healthy adults. Public Health Nutr. (2022) 25:43–50. doi: 10.1017/S1368980021002974
124. Jacob, JS, and Panwar, N. Effect of age and gender on dietary patterns, mindful eating, body image and confidence. BMC Psychol. (2023) 11:264. doi: 10.1186/s40359-023-01290-4
125. Nashwan, AJ, Villar, RC, Al-Qudimat, AR, Kader, N, Alabdulla, M, Abujaber, AA, et al. Quality of life, sleep quality, depression, anxiety, stress, eating habits, and social bounds in nurses during the coronavirus disease 2019 pandemic in Qatar (The PROTECTOR study): a cross-sectional, comparative study. J Pers Med. (2021) 11:918. doi: 10.3390/jpm11090918
Keywords: COVID-19, coronavirus, emotional eating, gender differences, systematic review, health inequalities, meta-analysis, mental health
Citation: Zaiser C, Pahlenkemper M, Brandt G, Ballero Reque C, Sabel L, Laskowski NM and Paslakis G (2025) Feeding the feelings: gender differences in emotional eating during COVID-19: a systematic review and meta-analysis. Front. Nutr. 12:1680872. doi: 10.3389/fnut.2025.1680872
Edited by:
Monica Tarcea, George Emil Palade University of Medicine, Pharmacy, Sciences and Technology of Târgu Mureş, RomaniaReviewed by:
Vasile Constantin, University of Bucharest, RomaniaSimone Gonzaga Do Carmo, University of Brasilia, Brazil
Copyright © 2025 Zaiser, Pahlenkemper, Brandt, Ballero Reque, Sabel, Laskowski and Paslakis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christopher Zaiser, Y2hyaXN0b3BoZXIuemFpc2VyQHJ1aHItdW5pLWJvY2h1bS5kZQ==
†ORCID: Christopher Zaiser, https://orcid.org/0009-0002-7643-5425
Marie Pahlenkemper, https://orcid.org/0009-0003-5111-3830
Gerrit Brandt, https://orcid.org/0000-0002-4895-1599
Cristina Ballero Reque, https://orcid.org/0000-0003-0097-7594
Luisa Sabel, https://orcid.org/0009-0003-1589-2785
Nora M. Laskowski, https://orcid.org/0000-0003-0213-5171
Georgios Paslakis, https://orcid.org/0000-0002-2069-0024
 Christopher Zaiser
Christopher Zaiser Marie Pahlenkemper
Marie Pahlenkemper Gerrit Brandt
Gerrit Brandt Cristina Ballero Reque
Cristina Ballero Reque Luisa Sabel
Luisa Sabel Nora M. Laskowski
Nora M. Laskowski Georgios Paslakis
Georgios Paslakis