- 1School of International Pharmaceutical Business, China Pharmaceutical University, Nanjing, China
- 2China Center for Health Economic Research, Peking University, Beijing, China
Background: The EQ-5D-5L is a generic preference-based questionnaire developed by the EuroQol Group to measure health-related quality of life (HRQoL) in 2005. Since its development, it has been increasingly applied in populations with various diseases and has been found to have good reliability and sensitivity. This study aimed to summarize the health utility elicited from EQ-5D-5L for patients with different diseases in cross-sectional studies worldwide.
Methods: Web of Science, MEDLINE, EMBASE, and the Cochrane Library were searched from January 1, 2012, to October 31, 2019. Cross-sectional studies reporting utility values measured with the EQ-5D-5L in patients with any specific disease were eligible. The language was limited to English. Reference lists of the retrieved studies were manually searched to identify more studies that met the inclusion criteria. Methodological quality was assessed with the Agency for Health Research and Quality (AHRQ) checklist. In addition, meta-analyses were performed for utility values of any specific disease reported in three or more studies.
Results: In total, 9,400 records were identified, and 98 studies met the inclusion criteria. In the included studies, 50 different diseases and 98,085 patients were analyzed. Thirty-five studies involving seven different diseases were included in meta-analyses. The health utility ranged from 0.31 to 0.99 for diabetes mellitus [meta-analysis random-effect model (REM): 0.83, (95% CI = 0.77–0.90); fixed-effect model (FEM): 0.93 (95% CI = 0.93–0.93)]; from 0.62 to 0.90 for neoplasms [REM: 0.75 (95% CI = 0.68–0.82); FEM: 0.80 (95% CI = 0.78–0.81)]; from 0.56 to 0.85 for cardiovascular disease [REM: 0.77 (95% CI = 0.75–0.79); FEM: 0.76 (95% CI = 0.75–0.76)]; from 0.31 to 0.78 for multiple sclerosis [REM: 0.56 (95% CI = 0.47–0.66); FEM: 0.67 (95% CI = 0.66–0.68)]; from 0.68 to 0.79 for chronic obstructive pulmonary disease [REM: 0.75 (95% CI = 0.71–0.80); FEM: 0.76 (95% CI = 0.75–0.77)] from 0.65 to 0.90 for HIV infection [REM: 0.84 (95% CI = 0.80–0.88); FEM: 0.81 (95% CI = 0.80–0.82)]; from 0.37 to 0.89 for chronic kidney disease [REM: 0.70 (95% CI = 0.48–0.92; FEM: 0.76 (95% CI = 0.74–0.78)].
Conclusions: EQ-5D-5L is one of the most widely used preference-based measures of HRQoL in patients with different diseases worldwide. The variation of utility values for the same disease was influenced by the characteristics of patients, the living environment, and the EQ-5D-5L value set.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/, identifier CRD42020158694.
Background
As a quantitative indicator of health-related quality of life (HRQoL), the health utility reflects people's preference for a given health state. The health utility is measured on a scale from zero to one, where zero represents death and one represents full health (1). The worse the perception of the health status is, the lower the utility value. It can be a negative value when a health state is perceived as being worse than death. There are several preference-based measurement tools for health utility, such as the EuroQol 5 dimensions (EQ-5D) family of instruments (2), the Short Form-6 Dimensions (SF-6D) (3), and the Health Utilities Index (HUI) (4). Health utility can be used as quality-of-life weight to calculate QALYs in cost-utility analysis (CUA). Thus, health utility plays an important role not only in the measurement of HRQoL but also in health economics evaluations (5, 6).
The EQ-5D, developed by the European Quality of Life Group (EuroQol Group), is currently one of the most widely used questionnaires in HRQoL research (7). The original version of the EQ-5D was introduced in 1990 and contains five dimensions: Mobility, Self-Care, Usual Activities, Pain/Discomfort, and Anxiety/Depression (2). For each dimension, there were three levels to describe the severity, namely, have no problems, have some problems, and have extreme problems, which could describe 243 different health states (2). However, there may be some issues when using the EQ-5D-3L to detect small changes in mild conditions, and the EQ-5D-3L had obvious ceiling effects (8). Therefore, in 2005, the EuroQol Group developed a new version of the EQ-5D based on the same five dimensions but with five rather than three severity levels (EQ-5D-5L); this instrument could detect 3,125 unique health states (8). Published studies have shown that compared with the EQ-5D-3L, the EQ-5D-5L was significantly more sensitive, with reduced ceiling effects (9, 10).
To derive health utility from the responses on the EQ-5D instruments, country-specific value sets need to be estimated (11). Since 2016, more than 20 countries and regions have published standard EQ-5D-5L value sets (Europe: 9; Asia: 9; Americas: 3; Africa: 1) (12). In 2012, before any standard EQ-5D-5L value set was established, van Hout et al. (13) developed a crosswalk project to map the EQ-5D-5L to the EQ-5D-3L, enabling researchers to obtain a crosswalk value set for the EQ-5D-5L based on published EQ-5D-3L standard value sets. Besides that, the psychometric properties of the EQ-5D-5L have been validated in both general and disease populations (12).
In recent years, with the availability of the EQ-5D-5L value sets, an increasing number of studies have used the EQ-5D-5L to measure the HRQoL of patients with different diseases and perform economic evaluations to support health decision-making (14, 15). At present, a comprehensive review of these studies is lacking. For HRQoL measured with EQ-5D-5L, cross-sectional studies mainly focus on the current health status of the patients while randomized controlled trials (RCTs) pay attention to the effects of different interventions on health outcomes. This study focuses on the use of the EQ-5D-5L to explore the variation in health utility in patients in different conditions, provide information to perform CUAs, and inform health policies.
Method
Search Strategy and Study Inclusion Criteria
This systematic review and meta-analysis was performed in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (16). The protocol was registered on PROSPERO with ID CRD42020158694 (https://www.crd.york.ac.uk/PROSPERO/). Literature searches were conducted in Medline via Ovid, Embase via Ovid, The Cochrane Library, and Web of Science from January 2012 to October 2019 with combinations of the following search terms: “quality of life,” “QoL,” “HRQoL,” “HRQL,” “EQ-5D,” “EQ-5D-5L,” “five level,” “EuroQol,” “five dimensions,” “randomized controlled trial,” “RCT,” and “diseases” (details in Supplementary Table 1).
According to the selection criteria, all studies were original cross-sectional studies reporting EQ-5D-5L utilities for any specific disease with or without comorbidities and using country-specific value sets or the crosswalk method (mapping from EQ-5D-3L). Due to the lack of EQ-5D-5L standard value sets in many countries, the crosswalk method is the most important value set to calculate utility measured by EQ-5D-5L. In addition, the crosswalk method is recommended by the National Institute for Health and Care Excellence (NICE) to perform CUA when EQ-5D-5L is used to measure health outcomes in England. Therefore, it is useful and necessary to include these articles in this review. Studies reported that multiple utility values using value sets from different countries in the same published article were also included. The language of publication was limited to English. This review excluded reviews, protocols, or abstracts; studies focused on the general population; longitudinal studies or effects evaluation studies of different interventions; studies that reported only synthetic utilities of multiple diseases, non-EQ-5D-5L utilities, or no utilities; and studies unrelated to HRQoL.
Data Collection and Quality Assessment
After removing duplicates, title and abstract screening was conducted by two authors independently. Following the application of the selection criteria, all eligible studies with full-texts were read, and the relevant references were checked manually. Two researchers independently collected the data using a predesigned data extraction table, including author, publication year, country or region, sample size, disease type, mean age, health utility, EQ-5D VAS score, proportions with problems in the five dimensions, value set, and administration method (i.e., face-to-face, telephone survey). When there was any discrepancy between the two researchers, it was resolved by discussion.
Quality assessment was conducted with the 11-item cross-sectional research checklist developed by the Agency for Healthcare Research and Quality (AHRQ) (17). According to the description in the study and the AHRQ checklist, the reviewer selects one of three options (“Yes,” “No,” and “Unclear”) for each item. “Yes” was assigned one point, while “No” or “Unclear” was assigned zero points. The quality level of each study was determined by summing all the item scores. For each assessed study, 0–3 points indicated low quality, 4–7 points indicated moderate quality, and 8–11 points indicated high quality.
Statistical Analysis
This review involved the analysis of the range of mean health utility values of the overall sample (or subgroups when there is no overall utility value reported) among different studies and value sets used in each study for a specific disease with or without comorbidities. In addition, this study reports the ranges in mean EQ-VAS scores and responses on each dimension of the EQ-5D-5L.
Meta-analysis was performed to synthesize utility data when three or more studies reported utility values and standard error/deviation for a specific disease. For any study that reported multiple utility values for the same sample using different EQ-5D-5L value sets, the average value or the utility calculated by using a local country-specific value set was applied in meta-analysis. Heterogeneity was assessed with the I2 statistic. Random-effect (DerSimonian–Laird estimator method) and fixed-effect (inverse variance method) models were both used to calculate the pooled utility for a specific disease. Sensitivity analysis was conducted by removing EQ-5D-5L utility values derived from crosswalk value sets. All analyses were performed with R (version 4.0.5).
Results
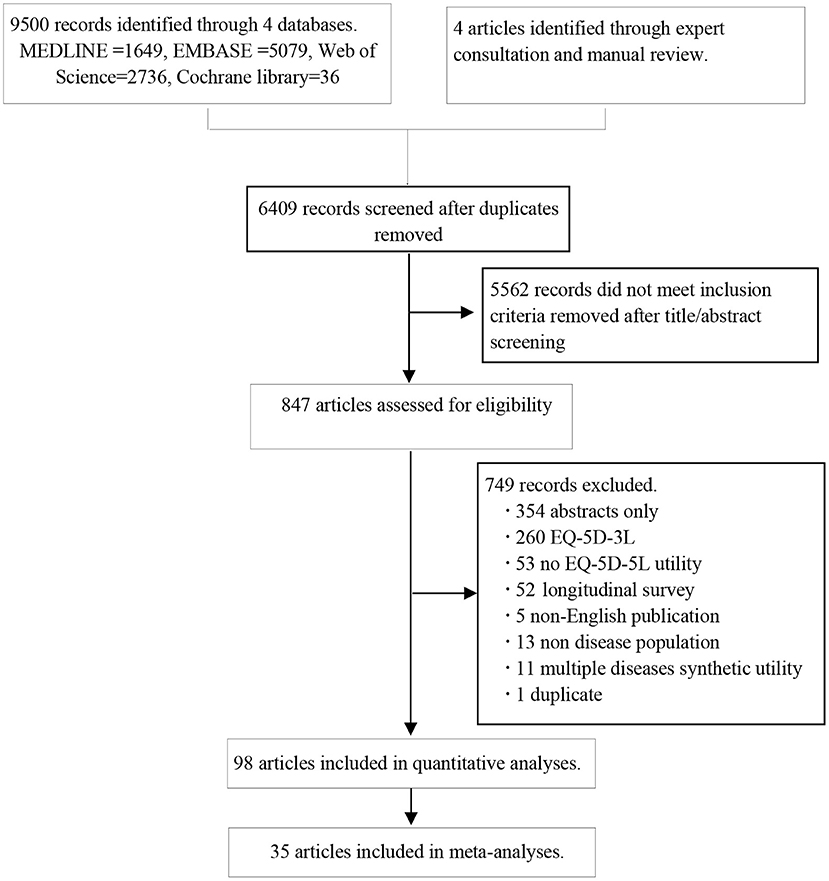
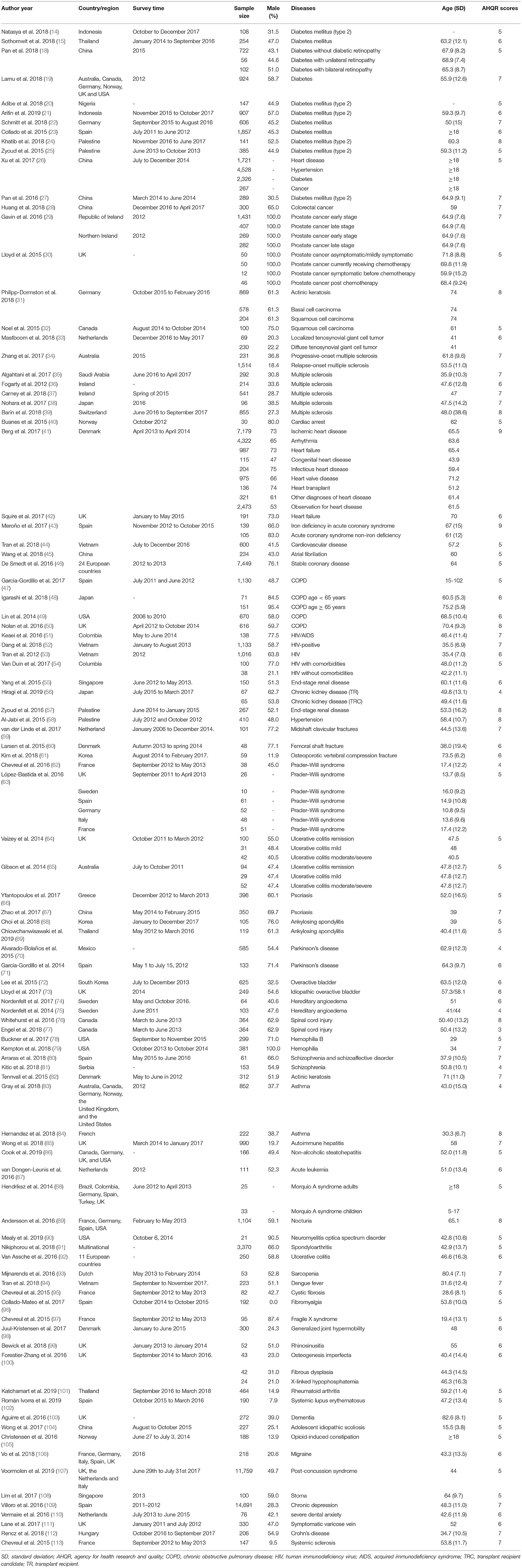
A total of 9,500 articles were identified from the four databases, and four additional studies were obtained from the manual search. After eliminating duplicates, 6,409 documents were screened to assess eligibility, of which 98 articles (15, 16, 18–113) were finally included in qualitative analyses and 35 studies were included in meta-analyses (Figure 1). Those 98 articles involved 98,085 patients. The included studies were published between January 2006 and March 2018 (Table 1). Except for three studies (29, 39, 79) that only included male patients and one study (96) that only included female patients, the rest of the studies included patients of both sexes. Twenty studies did not report the mode of administration. Of the remaining 78 studies, 47.4% involved the face-to-face administration of the survey, 47.4% involved self-administered surveys, and 5.2% involved telephone surveys. The AHRQ checklist scores ranged from four to nine points, the median was six points, and the mode was five points (details in Supplementary Table 2). There were no low-quality studies; 87 studies and 11 studies were of moderate and high quality, respectively. The data about the distributions of EQ-5D-5L are summarized in Supplementary Table 3.
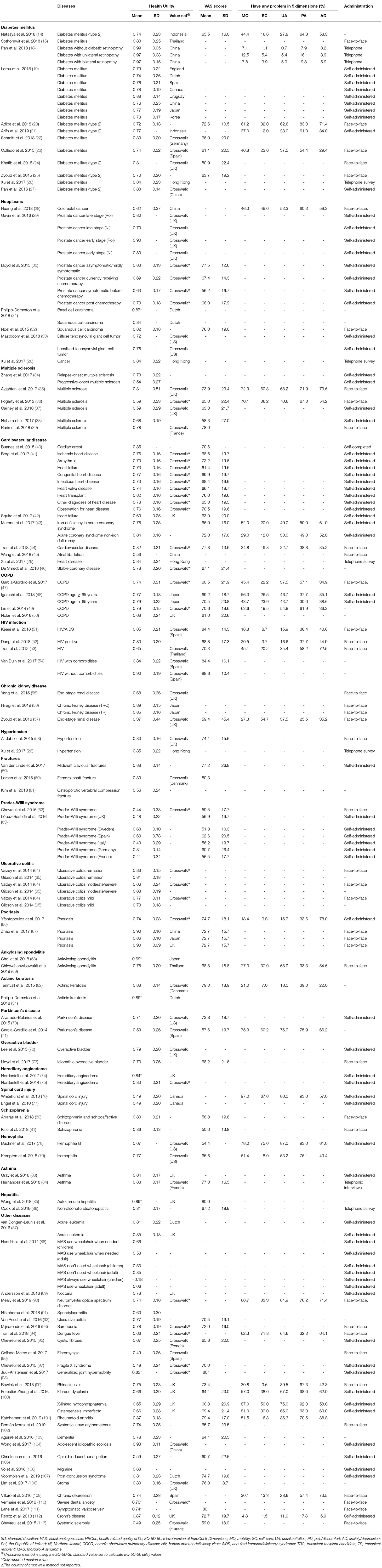
In this review, health utility values derived from the EQ-5D-5L were reported for 50 different diseases. Among these, diabetes mellitus, neoplasms, multiple sclerosis, cardiovascular disease, chronic obstructive pneumonia disease (COPD), human immunodeficiency virus (HIV) infection, chronic kidney disease, and fracture were reported in three or more studies and meta-analyses were performed for these diseases (fracture was not included in meta-analysis, because only two of the studies reported standard error/deviation). The sensitivity analysis results (remove all the utility values derived from the crosswalk value set) are presented in Supplementary Figure 1.
Diabetes Mellitus
For patients with diabetes mellitus (Table 2), 12 studies reported health utility values ranging from 0.31 to 0.99 (14, 15, 18–27). The Chinese standard EQ-5D-5L value set (18) and Crosswalk UK value set (24) were used to derive the utility values in the studies that reported the highest value and lowest value, respectively. The former focused on diabetes patients without diabetic retinopathy with a mean disease duration of 10.3 years and a mean age of 67.9 years (18), while the latter involved patients with severe comorbidities on hemodialysis, with a mean age of 60.3 years (24). Additionally, Lamu et al. (19) used eight country value sets (England, the Netherlands, Spain, Canada, Uruguay, China, Japan, and Korea) to analyze 924 diabetic patients from six countries. The results showed that the utility value calculated with the Uruguay value set was the highest at 0.880, while the lowest, 0.735, was derived with the value set from the Netherlands. The EQ-5D VAS scores were reported to range from 50.9 to 72.6 in six studies (14, 20, 22–25). Among the five dimensions of the EQ-5D-5L, pain/discomfort was the dimension with the most reported problems. The prevalence of diabetes comorbidities ranged from 55 to 100%, which was one of the most important factors negatively affecting the HRQoL of patients.
The meta-analytic utility estimate of diabetes mellitus was 0.83 (95% confidence interval (CI) = 0.77–0.90, heterogeneity I2 = 100%, P = 0.00) using the random-effect model, and it was 0.93 (95% CI = 0.93–0.93) using the fixed-effect model. The results are presented in Figure 2A.
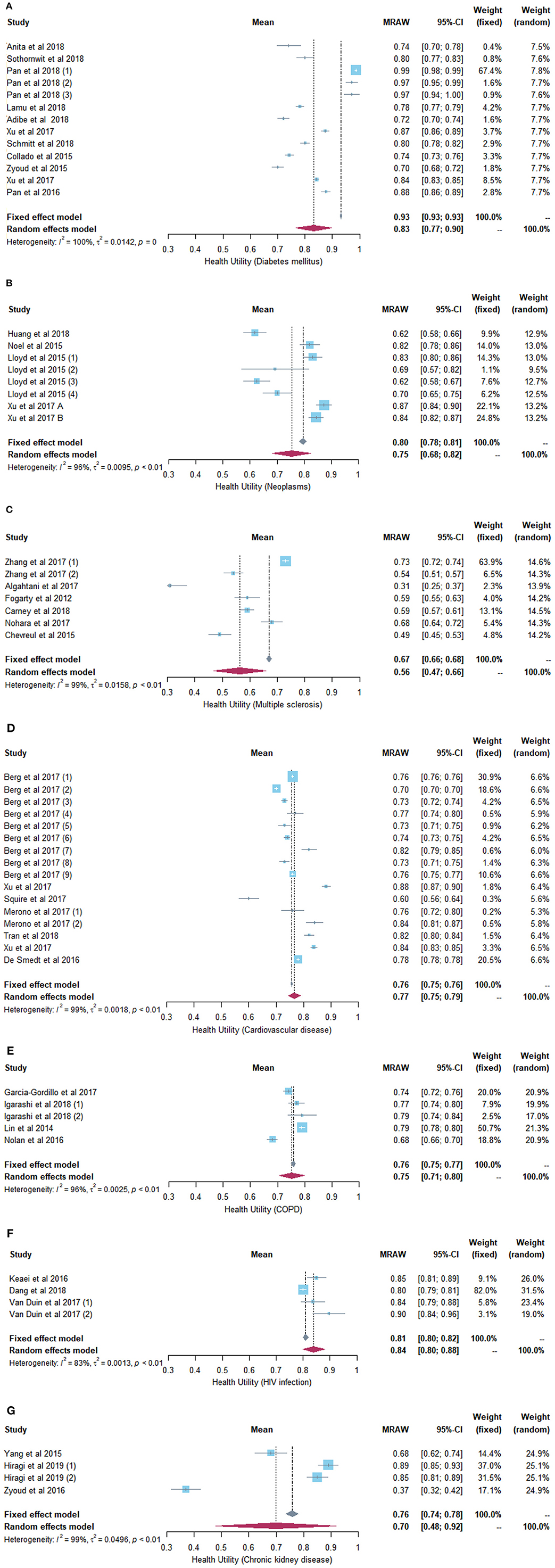
Figure 2. (A) Forest plot of the health utility of patients with diabetes mellitus. (B) Forest plot of the health utility of patients with neoplasms. (C) Forest plot of the health utility of patients with multiple sclerosis. (D) Forest plot of the health utility of patients with cardiovascular diseases. (E) Forest plot of the health utility of patients with chronic obstructive pneumonia disease. (F) Forest plot of the health utility of patients with human immunodeficiency virus infection. (G) Forest plot of the health utility of patients with chronic kidney disease.
Neoplasms
Seven studies reported health utility values for cancer patients ranging from 0.62 to 0.90 (26, 28–33). The highest utility value was in early-stage prostate cancer patients using the crosswalk UK value set (29), while the lowest value was in colorectal cancer patients, 49.7% of whom had stage III–IV disease, applying the China value set (28). The EQ-5D VAS scores ranged from 56.2 to 77.5 in two studies (30, 32). The decrease in health utility in cancer patients was mainly due to problems related to the pain/discomfort dimension of the EQ-5D-5L. As the cancer progressed, the health utility value decreased.
The pooled utility value of cancer patients was 0.75 (95% CI = 0.68–0.82, heterogeneity I2 = 96%, P < 0.01) using the random-effect model, and it was 0.80 (95% CI = 0.78–0.81) using the fixed-effect model (Figure 2B).
Multiple Sclerosis
The health utility ranged from 0.31 to 0.78 for multiple sclerosis patients in six studies (34–39). The upper and lower utility values were generated with the crosswalk France value set (35) and the crosswalk UK value set (39), respectively. The study with the highest value (39) reported a shorter disease duration (9 vs. 15 years) than the study with the lowest utility value (35). In addition, the former had a higher proportion of relapsing–remitting multiple sclerosis patients than the latter (71.5 vs. 52.8%). EQ-5D VAS scores ranged from 58.3 to 78.0 in five studies (35–39). Pain/discomfort and usual activities were the dimensions with the most reported problems among multiple sclerosis patients.
The meta-analytic utility estimate of multiple sclerosis patients was 0.56 (95% CI = 0.47–0.66, heterogeneity I2 = 99%, P < 0.01) using the random-effect model, and it was 0.67 (95% CI = 0.66–0.68) using the fixed-effect model (Figure 2C).
Cardiovascular Disease
For cardiovascular disease patients, the health utility values ranged from 0.56 to 0.85 in eight studies (26, 40–46). The lowest value was derived from the Chinese value set (45), while the study with the highest value did not report the value set used (40). In the study with the highest utility value (40), all patients were evaluated 4 years after cardiac arrest, and the proportion of men was 80%. In the study with the lowest value, the patients had atrial fibrillation; 43% of them were men, and 23% had diabetes mellitus (45). Berg et al. (41) compared utility values among nine subgroups of patients with different cardiovascular diseases. Among these subgroups, heart transplant patients had the highest value, which was 0.82, while arrhythmia patients had the lowest value, which was 0.70. The EQ-5D VAS scores ranged from 61.4 to 77.8 in six studies (26, 40–44). Anxiety/depression and pain/discomfort were the dimensions with the most reported problems among cardiovascular disease patients.
The pooled utility value of cardiovascular disease patients was 0.77 (95% CI = 0.75–0.79, heterogeneity I2 = 99%, P < 0.01) using the random-effect model, and it was 0.76 (95% CI = 0.75–0.76) using the fixed-effect model (Figure 2D).
COPD
For patients with COPD, the health utility values ranged from 0.68 to 0.79 in four studies (47–50). The crosswalk US value set and UK standard EQ-5D-5L value set were used in the studies that reported the highest utility value (49) and the lowest value (50), respectively. The mean age of COPD patients in the study reporting the lowest utility was 70.4 years, and the mean predicted forced expiratory volume in 1 s (FEV1) was 49.8% (50). Meanwhile, the patients in the study with the highest value had a younger mean age (68.5 years old) and a better predicted FEV1 (49). The EQ-5D VAS scores ranged from 60.5 to 70.6 in four studies (47–50). Mobility was the dimension with the most problems affecting the HRQoL of COPD patients based on EQ-5D-5L. In addition, as the predicted FEV1 decreased, the health utility value in COPD patients decreased.
The synthesized utility value of COPD patients was 0.75 (95% CI = 0.71–0.80, heterogeneity I2 = 96%, P < 0.01) using the random-effect model, and it was 0.76 (95% CI = 0.75–0.77) using the fixed-effect model (Figure 2E).
HIV Infection
The health utility values of patients infected with HIV ranged from 0.65 to 0.90 in four studies (51–54), and both extreme values were derived with a crosswalk value set [Thailand (53) and Spain (54)]. The study (54) with the highest utility value involved patients in relatively good condition and without any comorbidities, while the study (53), with the lowest value focused on patients who had symptomatic HIV infections. The EQ-5D VAS scores ranged from 68.8 to 88.6 in four studies (51–54). The decrease in utility in HIV-infected patients was mainly due to problems related to the anxiety/depression dimension of the EQ-5D-5L.
The pooled utility value of patients infected with HIV was 0.84 (95% CI = 0.80–0.88, heterogeneity I2 = 83%, P < 0.01) using the random-effect model, and it was 0.81 (95% CI = 0.80–0.82) using the fixed-effect model (Figure 2F).
Chronic Kidney Disease
For chronic kidney disease patients, the health utility values ranged from 0.37 to 0.89 in three studies (55–57). The Japan value set and crosswalk UK value set were used to calculate the highest utility value (56) and the lowest value (57), respectively. The mean age of chronic kidney disease patients in the study reporting the highest value was 49.8 years old, and all of them had received kidney transplants (56), while those in the study reporting the lowest value were 59.4 years old, and 33.7% of them had been on dialysis for 4 years or longer (57). One study (57) reported that the EQ-5D VAS score was 59.4. Among the five dimensions, self-care was the dimension with the most reported problems among chronic kidney disease patients.
The meta-analytic utility estimate of chronic kidney disease was 0.70 (95% CI = 0.48–0.92, heterogeneity I2 = 99%, P < 0.01) using the random-effect model, and it was 0.76 (95% CI = 0.74–0.78) using the fixed-effect model (Figure 2G).
Fracture
The health utility values of patients with fractures ranged from 0.56 to 0.88 in the three studies (59–61). However, neither of the studies that reported the maximum and minimum values described the value sets used (59, 61). The patients in the study reporting the highest value (59) had midshaft clavicular fractures and a much younger mean age (44.5 vs. 73.5 years old) than the osteoporotic vertebral compression fracture patients in the study reporting the lowest value (61). Two studies reported EQ-5D VAS scores of 80.3 (60) and 77.2 (59). No information was available for the dimensions that contributed the most to the HRQoL of fracture patients.
Other Diseases
For Prader–Willi syndrome, hypertension, ulcerative colitis, ankylosing spondylitis, psoriasis, actinic keratosis, Parkinson's disease, overactive bladder, hereditary angioedema, spinal cord injury, schizophrenia, hemophilia, asthma, and hepatitis, only two studies reported the health utility values for patients with each disease. For the remaining 29 diseases (87–113), the HRQoL and utility values were only reported by one study each. Patients with adolescent idiopathic scoliosis had the highest utility value of 0.93 (104), while children with Morquio A syndrome, who must use wheelchairs, had the lowest value of −0.18 (88).
Furthermore, two studies compared utility values calculated with different country-specific value sets in the same sample (67, 87). For patients with psoriasis living in central South China (67), value sets for Japan, China, and the UK were used separately to obtain the EQ-5D-5L utility values, and the results were 0.86, 0.90, and 0.90, respectively. van Dongen-Leunis et al. (87) used two EQ-5D-5L country-specific value sets to calculate the health utility of acute leukemia patients, and the value derived from the Dutch value set (0.81) was lower than that derived from the UK value set (0.85). The rest of the studies all used a single value set. Compared with other dimensions, pain/discomfort was the dimension with the most problems reported by patients in most of the studies.
Discussion
In this study, we reviewed the health utility values in patients with different diseases according to the EQ-5D-5L in cross-sectional surveys. We found that the EQ-5D-5L has been widely applied in populations with specific diseases, including various chronic non-communicable diseases, such as diabetes mellitus, neoplasms, multiple sclerosis, and cardiovascular disease, and infectious diseases, such as HIV and Dengue fever. The health utility values for a specific disease measured by the EQ-5D-5L differed based on patient characteristics, survey location, the use of country-specific value sets, and other factors. Meta-analyses were performed to synthesized utility data of any specific disease reported in three or more studies.
Health utility measures the preference of people for a given health state and reflects their status with regard to quality of life (1). Sex is one of the factors that affect health utilities (47). There are differences in the perception of health status between males and females, and in most of the included studies that reported sex-specific utilities, men had better HRQoL as measured by the EQ-5D-5L than women. For instance, the utility value was 0.80 for men with COPD and 0.69 for women with COPD, and the proportion of men who reported having problems on all five dimensions was lower than the proportion of women (47). In addition, health utility values decreased as the age of patients increased due to the deterioration of physical function and reduced disease tolerance. Among patients with COPD, for example, the utility value for patients under 65 years of age (0.77) was lower than that for patients who were 65 years old and older (0.79) (48).
In general, the severity of disease is reflected by the magnitude of the health utility value. The variation in values measured by EQ-5D-5L for the same disease under different conditions reflects its discriminative ability. As the disease progresses, the utility value decreases. Alvarado-Bolaños et al. (70) used Hoehn and Yahr staging to categorize Parkinson's disease patients into groups with mild, moderate, and severe disease, and the utility values were 0.77, 0.65, and 0.47, respectively. In addition, the number of comorbidities and the different types of comorbidities substantially affect the HRQoL of patents. Patients who have comorbidities usually report a lower utility value than those without comorbidities. Van Duin et al. (54) reported that the utility value was 0.90 in patients with HIV infections who did not have any comorbidities; however, it was reduced to 0.84 when patients had comorbid diseases. In Al-Jabi's study (58), for hypertension patients with one, two, and three or more comorbidities, the utility values were 0.81, 0.73, and 0.66, respectively.
Various living environments result in different lifestyles, which may influence HRQoL and health utility. Zyoud et al. (57) reported that among patients with end-stage renal disease in Palestine, those living in villages had a higher mean utility value than those living in cities (0.44 vs. 0.29). In another study (44), among patients with cardiovascular disease, the utility value was a little bit higher for those living in urban Vietnam than those in rural areas (0.82 vs. 0.81).
To calculate health utility, the target patients' responses to the EQ-5D-5L and a country-specific value set are needed. The health preferences of patients living in different countries are affected by their social environment, living standards, and health system. Therefore, the EQ-5D-5L value sets estimated based on residents' preferences for health states vary across countries or regions. Different results can be observed in the same sample when various country value sets are used to calculate health utility values. In the same sample of patients with acute leukemia, van Dongen-Leunis et al. (87) reported that the value obtained with the Dutch value set was higher than that obtained with the UK value set. In countries where the EQ-5D-5L utility value set has been estimated, it is more appropriate to use the local value set. Before any standard country-specific EQ-5D-5L value set was published, the crosswalk method developed by van Hout et al. (13) in 2012 was an alternative means of calculating health utility measured by EQ-5D-5L. For cost-utility analyses performed in England, the NICE recommends the use of the crosswalk method to obtain EQ-5D-5L utility values and calculate quality-adjusted life-years (QALYs) because there are some concerns about the current standard value set published by Devlin et al. (114). In this review, a crosswalk value set was used in half of the studies to calculate utility values due to the lack of a local standard EQ-5D-5L value set when the survey was conducted. Therefore, the crosswalk value set is still important for researchers to calculate health utility.
The heterogeneity of health utility derived from different studies for any specific disease is significant. Although, this may lead to some issues of the direct comparison among these studies, the trend of variation and the influence factors of health utility can be observed. In addition, to perform CUA, different sources of health utilities are need to be identified and applied in the model (1). The summarization and review of health utility for different diseases are helpful and useful.
There are some limitations of this study. Among the 50 different diseases analyzed in this review, nearly half of them were only discussed in one study each. The included studies were limited to those published in English. In addition, some of the studies did not describe the value set used. This review focused on health utility measured by the EQ-5D-5L in cross-sectional studies, and the comparison of different utility-based instruments (i.e., SF-6D, HUI) in populations with specific diseases needs further exploration.
A deeper understanding of the HRQoL and health utility of patients with different diseases facilitates the provision of a more appropriate range of services for disease management and treatment. In addition, health utility is used for HRQoL weighting when calculating QALYs. QALY is used as the outcome measure in CUA and plays an important role in health technology assessments (12). The summarization of health utility from various sources provides information to perform CUA which could inform health decision making and the reasonable allocation of health resources.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
TZ, HG, and AM designed this study protocol. HG, AM, and TZ conceived the literature strategies. LW and MR reviewed the title/abstract independently. TZ and LW performed the original study review. TZ, HG, and YZ extracted and analyzed the data from included studies. TZ and MR assessed the methodological quality with AHRQ checklists. TZ and YZ contributed to the writing of the manuscript. All the authors approved the final version of this systematic review.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.675523/full#supplementary-material
References
1. Brazier J, Ara R, Azzabi I, Busschbach J, Chevrou-Séverac H, Crawford B, et al. Identification, review, and use of health state utilities in cost-effectiveness models: an ISPOR good practices for outcomes research task force report. Value Health. (2019) 22:267–75. doi: 10.1016/j.jval.2019.01.004
2. Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. (2001) 33:337–43. doi: 10.3109/07853890109002087
3. Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. (2002) 21:271–92. doi: 10.1016/S0167-6296(01)00130-8
4. Horsman J, Furlong W, Feeny D, Torrance G. The Health Utilities Index (HUI): concepts, measurement properties and applications. Health Qual Life Outcomes. (2003) 1:54. doi: 10.1186/1477-7525-1-54
5. Ara R, Wailoo A. Using health state utility values in models exploring the cost-effectiveness of health technologies. Value Health. (2012) 15:971–74. doi: 10.1016/j.jval.2012.05.003
6. Wolowacz SE, Briggs A, Belozeroff V, Clarke P, Doward L, Goeree R, et al. Estimating health-state utility for economic models in clinical studies: an ISPOR good research practices task force report. Value Health. (2016) 19:704–19. doi: 10.1016/j.jval.2016.06.001
7. Wisløff T, Hagen G, Hamidi V, Movik E, Klemp M, Olsen JA. Estimating QALY gains in applied studies: a review of cost-utility analyses published in 2010. Pharmacoeconomics. (2014) 32:367–75. doi: 10.1007/s40273-014-0136-z
8. Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. (2011) 20:1727–36. doi: 10.1007/s11136-011-9903-x
9. Kim SH, Kim HJ, Lee SI, Jo MW. Comparing the psychometric properties of the EQ-5D-3L and EQ-5D-5L in cancer patients in Korea. Qual Life Res. (2012) 21:1065–73. doi: 10.1007/s11136-011-0018-1
10. Scalone L, Ciampichini R, Fagiuoli S, Gardini I, Fusco F, Gaeta L, et al. Comparing the performance of the standard EQ-5D 3L with the new version EQ-5D 5L in patients with chronic hepatic diseases. Qual Life Res. (2013) 22:1707–6. doi: 10.1007/s11136-012-0318-0
11. EuroQol Research Foundation. EQ-5D-5L User Guide. (2019). Available online at: https://euroqol.org/publications/user-guides (accessed January 01, 2021).
12. EuroQol Group. EQ-5D-5L Valuation: Standard Value Sets. Available online at: https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/valuation-standard-value-sets/ (accessed January 03, 2021).
13. van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. (2012) 15:708–15. doi: 10.1016/j.jval.2012.02.008
14. Natasya A, Andrajati R, Sauriasari R.Cross-sectional study of association between glycemic control and quality of life among diabetic patients. Int J Pharmaceut. (2018) 10:92–6. doi: 10.22159/ijap.2018.v10s1.19
15. Sothornwit J, Srisawasdi G, Suwannakin A, Sriwijitkamol A. Decreased health-related quality of life in patients with diabetic foot problems. Diabetes Metab Syndr Obes. (2018) 11:35–43. doi: 10.2147/DMSO.S154304
16. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
17. AHQR. Methods guide for effectiveness and comparative effectiveness reviews. In: Methods Guide for Effectiveness and Comparative Effectiveness Reviews. (2008). Available online at: https://effectivehealthcare.ahrq.gov/products/cer-methods-guide/overview/ (accessed February 02, 2021).
18. Pan CW, Wang S, Wang P, Xu CL, Song E. Diabetic retinopathy and health-related quality of life among Chinese with known type 2 diabetes mellitus. Qual Life Res. (2018) 27:2087–93. doi: 10.1007/s11136-018-1876-6
19. Lamu AN, Chen G, Gamst-Klaussen T, Olsen JA. Do country-specific preference weights matter in the choice of mapping algorithms? The case of mapping the Diabetes-39 onto eight country-specific EQ-5D-5L value sets. Qual Life Res. (2018) 27:1801–14. doi: 10.1007/s11136-018-1840-5
20. Adibe MO, Anosike C, Nduka SO, Isah A. Evaluation of health status of type 2 diabetes outpatients receiving care in a tertiary hospital in Nigeria. Pharmacoecon Open. (2018) 2:337–45. doi: 10.1007/s41669-017-0056-x
21. Arifin B, Idrus LR, van Asselt ADI, Purba FD, Perwitasari DA, Thobari JA, et al. Health-related quality of life in Indonesian type 2 diabetes mellitus outpatients measured with the Bahasa version of EQ-5D. Qual Life Res. (2019) 28:1179–90. doi: 10.1007/s11136-019-02105-z
22. Schmitt A, Reimer A, Kulzer B, Icks A, Paust R, Roelver KM, et al. Measurement of psychological adjustment to diabetes with the diabetes acceptance scale. J Diabetes Complications. (2018) 32:384–92. doi: 10.1016/j.jdiacomp.2018.01.005
23. Collado Mateo D, García Gordillo MA, Olivares PR, Adsuar JC. Normative values of EQ-5D-5L for diabetes patients from Spain. Nutr Hosp. (2015) 32:1595–602. doi: 10.3305/nh.2015.32.4.9605
24. Khatib ST, Hemadneh MK, Hasan SA, Khazneh E, Zyoud SH. Quality of life in hemodialysis diabetic patients: a multicenter cross-sectional study from Palestine. BMC Nephrol. (2018) 19:49. doi: 10.1186/s12882-018-0849-x
25. Zyoud SH, Al-Jabi SW, Sweileh WM, Arandi DA, Dabeek SA, Esawi HH, et al. Relationship of treatment satisfaction to health-related quality of life among Palestinian patients with type 2 diabetes mellitus: findings from a cross-sectional study. J Clin Transl Endocrinol. (2015) 2:66–71. doi: 10.1016/j.jcte.2015.03.002
26. Xu RH, Cheung AWL, Wong ELY. The relationship between shared decision-making and health-related quality of life among patients in Hong Kong SAR, China. Int J Qual Health Care. (2017) 29:534–40. doi: 10.1093/intqhc/mzx067
27. Pan CW, Sun HP, Zhou HJ, Ma Q, Xu Y, Luo N, et al. Valuing health-related quality of life in type 2 diabetes patients in China. Med Decis Making. (2016) 36:234–41. doi: 10.1177/0272989X15606903
28. Huang W, Yang J, Liu Y, Liu C, Zhang X, Fu W, et al. Assessing health-related quality of life of patients with colorectal cancer using EQ-5D-5L: a cross-sectional study in Heilongjiang of China. BMJ Open. (2018) 8:e022711. doi: 10.1136/bmjopen-2018-022711
29. Gavin AT, Donnelly D, Donnelly C, Drummond FJ, Morgan E, Gormley GJ, et al. Effect of investigation intensity and treatment differences on prostate cancer survivor's physical symptoms, psychological well-being and health-related quality of life: a two country cross-sectional study. BMJ Open. (2016) 6:e012952. doi: 10.1136/bmjopen-2016-012952
30. Lloyd AJ, Kerr C, Penton J, Knerer G. Health-related quality of life and health utilities in metastatic castrate-resistant prostate cancer: A Survey capturing experiences from a diverse sample of UK patients. Value Health. (2015) 18:1152–57. doi: 10.1016/j.jval.2015.08.012
31. Philipp-Dormston WG, Müller K, Novak B, Strömer K, Termeer C, Hammann U, et al. Patient-reported health outcomes in patients with non-melanoma skin cancer and actinic keratosis: results from a large-scale observational study analysing effects of diagnoses and disease progression. J Eur Acad Dermatol Venereol. (2018) 32:1138–46. doi: 10.1111/jdv.14703
32. Noel CW, Lee DJ, Kong Q, Xu W, Simpson C, Brown D, et al. Comparison of health state utility measures in patients with head and neck cancer. JAMA Otolaryngol Head Neck Surg. (2015) 141:696–703. doi: 10.1001/jamaoto.2015.1314
33. Mastboom MJ, Planje R, van de Sande MA. The patient perspective on the impact of tenosynovial giant cell tumors on daily living: crowdsourcing study on physical function and quality of life. Interact J Med Res. (2018) 7:e4. doi: 10.2196/ijmr.9325
34. Zhang Y, Taylor BV, Simpson S Jr, Blizzard L, van der Mei I. Patient-reported outcomes are worse for progressive-onset multiple sclerosis than relapse-onset multiple sclerosis, particularly early in the disease process. Eur J Neurol. (2019) 26:155–61. doi: 10.1111/ene.13786
35. Algahtani HA, Shirah BH, Alzahrani FA, Abobaker HA, Alghanaim NA, Manlangit JS Jr. Quality of life among multiple sclerosis patients in Saudi Arabia. Neurosciences. (2017) 22:261–6. doi: 10.17712/nsj.2017.4.20170273
36. Fogarty E, Walsh C, Adams R, McGuigan C, Barry M, Tubridy N. Relating health-related quality of life to disability progression in multiple sclerosis, using the 5-level EQ-5D. Mult Scler. (2013) 19:1190–96. doi: 10.1177/1352458512474860
37. Carney P, O'Boyle D, Larkin A, McGuigan C, O'Rourke K. Societal costs of multiple sclerosis in Ireland. J Med Econ. (2018) 21:425–37. doi: 10.1080/13696998.2018.1427100
38. Nohara C, Hase M, Liebert R, Wu N. The burden of multiple sclerosis in Japan. J Med Econ. (2017) 20:1290–98. doi: 10.1080/13696998.2017.1373653
39. Barin L, Salmen A, Disanto G, Babačić H, Calabrese P, Chan A, et al. The disease burden of Multiple sclerosis from the individual and population perspective: which symptoms matter most? Mult Scler Relat Disord. (2018) 25:112–21. doi: 10.1016/j.msard.2018.07.013
40. Buanes EA, Gramstad A, Søvig KK, Hufthammer KO, Flaatten H, Husby T, et al. Cognitive function and health-related quality of life four years after cardiac arrest. Resuscitation. (2015) 89:13–8. doi: 10.1016/j.resuscitation.2014.12.021
41. Berg SK, Rasmussen TB, Thrysoee L, Lauberg A, Borregaard B, Christensen AV, et al. DenHeart: differences in physical and mental health across cardiac diagnoses at hospital discharge. J Psychosom Res. (2017) 94:1–9. doi: 10.1016/j.jpsychores.2017.01.003
42. Squire I, Glover J, Corp J, Haroun R, Kuzan D, Gielen V. Impact of HF on HRQoL in patients and their caregivers in England: results from the ASSESS study. Br J Cardiol. (2017) 24:30–34. doi: 10.5837/bjc.2017.007
43. Meroño O, Cladellas M, Ribas-Barquet N, Poveda P, Recasens L, Bazán V, et al. Iron deficiency is a determinant of functional capacity and health-related quality of life 30 days after an acute coronary syndrome. Rev Esp Cardiol. (2017) 70:363–70. doi: 10.1016/j.rec.2016.10.004
44. Tran BX, Moir MP, Thai TPT, Nguyen LH, Ha GH, Nguyen THT, et al. Socioeconomic inequalities in health-related quality of life among patients with cardiovascular diseases in Vietnam. Biomed Res Int. (2018) 2018:2643814. doi: 10.1155/2018/2643814
45. Wang Z, Chen Z, Wang X, Zhang L, Li S, Tian Y, et al. The disease burden of atrial fibrillation in China from a national cross-sectional survey. Am J Cardiol. (2018) 122:793–98. doi: 10.1016/j.amjcard.2018.05.015
46. De Smedt D, Clays E, Höfer S, Oldridge N, Kotseva K, Maggioni AP, et al. Validity and reliability of the HeartQoL questionnaire in a large sample of stable coronary patients: The EUROASPIRE IV Study of the European Society of Cardiology. Eur J Prev Cardiol. (2016) 23:714–21. doi: 10.1177/2047487315604837
47. Garcia-Gordillo MÁ, Collado-Mateo D, Olivares PR, Adsuar JC, Merellano-Navarro E. A cross-sectional assessment of health-related quality of life among patients with chronic obstructive pulmonary disease. Iran J Public Health. (2017) 46:1046–53.
48. Igarashi A, Fukuchi Y, Hirata K, Ichinose M, Nagai A, Nishimura M, et al. COPD uncovered: a cross-sectional study to assess the socioeconomic burden of COPD in Japan. Int J Chron Obstruct Pulmon Dis. (2018) 13:2629–41. doi: 10.2147/COPD.S167476
49. Lin FJ, Pickard AS, Krishnan JA, Joo MJ, Au DH, Carson SS, et al. Measuring health-related quality of life in chronic obstructive pulmonary disease: properties of the EQ-5D-5L and PROMIS-43 short form. BMC Med Res Methodol. (2014) 14:78. doi: 10.1186/1471-2288-14-78
50. Nolan CM, Longworth L, Lord J, Canavan JL, Jones SE, Kon SS, et al. The EQ-5D-5L health status questionnaire in COPD: validity, responsiveness and minimum important difference. Thorax. (2016) 71:493–500. doi: 10.1136/thoraxjnl-2015-207782
51. Keaei M, Kuhlmann J, Conde R, Evers SM, Gonzalez J, Govers M, et al. Health-related quality of life of patients with HIV/AIDS in Bogotá, Colombia. Value Health Reg Issues. (2016) 11:68–72. doi: 10.1016/j.vhri.2016.05.001
52. Dang AK, Nguyen LH, Nguyen AQ, Tran BX, Tran TT, Latkin CA, et al. Physical activity among HIV-positive patients receiving antiretroviral therapy in Hanoi and Nam Dinh, Vietnam: a cross-sectional study. BMJ Open. (2018) 8:e020688. doi: 10.1136/bmjopen-2017-020688
53. Tran BX, Ohinmaa A, Nguyen LT. Quality of life profile and psychometric properties of the EQ-5D-5L in HIV/AIDS patients. Health Qual Life Outcomes. (2012) 10:132. doi: 10.1186/1477-7525-10-132
54. Van Duin MJ, Conde R, Wijnen B, Evers SM, Gonzalez-Rodriguez JL, Govers MJ, et al. The impact of comorbidities on costs, utilities and health-related quality of life among HIV patients in a clinical setting in Bogotá. Expert Rev Pharmacoecon Outcomes Res. (2017) 17:303–10. doi: 10.1080/14737167.2017.1246185
55. Yang F, Lau T, Lee E, Vathsala A, Chia KS, Luo N. Comparison of the preference-based EQ-5D-5L and SF-6D in patients with end-stage renal disease (ESRD). Eur J Health Econ. (2015) 16:1019–26. doi: 10.1007/s10198-014-0664-7
56. Hiragi S, Goto R, Tanaka Y, Matsuyama Y, Sawada A, SakaI K, et al. Estimating the net utility gains among donors and recipients of adult living donor kidney transplant. Transplant Proc. (2019) 51:676–83. doi: 10.1016/j.transproceed.2019.01.049
57. Zyoud SH, Daraghmeh DN, Mezyed DO, Khdeir RL, Sawafta MN, Ayaseh NA, et al. Factors affecting quality of life in patients on haemodialysis: a cross-sectional study from Palestine. BMC Nephrol. (2016) 17:44. doi: 10.1186/s12882-016-0257-z
58. Al-Jabi SW, Zyoud SH, Sweileh WM, Wildali AH, Saleem HM, Aysa HA, et al. Relationship of treatment satisfaction to health-related quality of life: findings from a cross-sectional survey among hypertensive patients in Palestine. Health Expect. (2015) 18:3336–48. doi: 10.1111/hex.12324
59. van der Linde RA, Beetz I, van Helden SH. Plating for midshaft clavicular fractures: the impact on quality of life and functional outcome. Injury. (2017) 48:2778–83. doi: 10.1016/j.injury.2017.10.032
60. Larsen P, Elsoe R, Graven-Nielsen T, Laessoe U, Rasmussen S. Decreased muscle strength is associated with impaired long-term functional outcome after intramedullary nailing of femoral shaft fracture. Eur J Trauma Emerg Surg. (2015) 41:673–81. doi: 10.1007/s00068-014-0488-2
61. Kim HJ, Park S, Park SH, Park J, Chang BS, Lee CK, et al. Prevalence of frailty in patients with osteoporotic vertebral compression fracture and its association with numbers of fractures. Yonsei Med J. (2018) 59:317–24. doi: 10.3349/ymj.2018.59.2.317
62. Chevreul K, Berg Brigham K, Clément MC, Poitou C, Tauber M, Members of the BURQOL-RD Research Network listed in the Online Appendix. Economic burden and health-related quality of life associated with Prader-Willi syndrome in France. J Intellect Disabil Res. (2016) 60:879–90. doi: 10.1111/jir.12288
63. López-Bastida J, Linertová R, Oliva-Moreno J, Posada-de-la-Paz M, Serrano-Aguilar P, Kanavos P, et al. Social/economic costs and health-related quality of life in patients with Prader-Willi syndrome in Europe. Eur J Health Econ. (2016) 17(Suppl 1):99–108. doi: 10.1007/s10198-016-0788-z
64. Vaizey CJ, Gibson PR, Black CM, Nicholls RJ, Weston AR, Gaya DR, et al. Disease status, patient quality of life and healthcare resource use for ulcerative colitis in the UK: an observational study. Frontline Gastroenterol. (2014) 5:183–9. doi: 10.1136/flgastro-2013-100409
65. Gibson PR, Vaizey C, Black CM, Nicholls R, Weston AR, Bampton P, et al. Relationship between disease severity and quality of life and assessment of health care utilization and cost for ulcerative colitis in Australia: a cross-sectional, observational study. J Crohns Colitis. (2014) 8:598–606. doi: 10.1016/j.crohns.2013.11.017
66. Yfantopoulos J, Chantzaras A, Kontodimas S. Assessment of the psychometric properties of the EQ-5D-3L and EQ-5D-5L instruments in psoriasis. Arch Dermatol Res. (2017) 309:357–70. doi: 10.1007/s00403-017-1743-2
67. Zhao Y, Li SP, Liu L, Zhang JL, Chen G. Does the choice of tariff matter?: a comparison of EQ-5D-5L utility scores using Chinese, UK, and Japanese tariffs on patients with psoriasis vulgaris in Central South China. Medicine. (2017) 96:e7840. doi: 10.1097/MD.0000000000007840
68. Choi JH, Lee SH, Kim HR, Lee KA. Association of neuropathic-like pain characteristics with clinical and radiographic features in patients with ankylosing spondylitis. Clin Rheumatol. (2018) 37:3077–86. doi: 10.1007/s10067-018-4125-z
69. Chiowchanwisawakit P, Thaweeratthakul P, Wattanamongkolsil L, Srinonprasert V, Koolvisoot A, Muangchan C, et al. Relationship between health-related quality of life and patient acceptable symptom state with disease activity and functional status in patients with ankylosing spondylitis in Thailand. J Clin Rheumatol. (2019) 25:16–23. doi: 10.1097/RHU.0000000000000750
70. Alvarado-Bolaños A, Cervantes-Arriaga A, Rodríguez-Violante M, Llorens-Arenas R, Calderón-Fajardo H, Millán-Cepeda R, et al. Convergent validation of EQ-5D-5L in patients with Parkinson's disease. J Neurol Sci. (2015) 358:53–7. doi: 10.1016/j.jns.2015.08.010
71. García-Gordillo M, del Pozo-Cruz B, Adsuar JC, Sánchez-Martínez FI, Abellán-Perpiñán JM. Validation and comparison of 15-D and EQ-5D-5L instruments in a Spanish Parkinson's disease population sample. Qual Life Res. (2014) 23:1315–26. doi: 10.1007/s11136-013-0569-4
72. Lee KS, Choo MS, Seo JT, Oh SJ, Kim HG, Ng K, et al. Impact of overactive bladder on quality of life and resource use: results from Korean Burden of Incontinence Study (KOBIS). Health Qual Life Outcomes. (2015) 13:89. doi: 10.1186/s12955-015-0274-9
73. Lloyd S, Crawford G, Mcskimming P, Grifi M, Greenwell TJ, Ockrim J. The impact of age, gender and severity of overactive bladder wet on quality of life, productivity, treatment patterns and satisfaction. J Clin Urol. (2017) 10:1–10. doi: 10.1177/2051415817710111
74. Nordenfelt P, Nilsson M, Lindfors A, Wahlgren CF, Björkander J. Health-related quality of life in relation to disease activity in adults with hereditary angioedema in Sweden. Allergy Asthma Proc. (2017) 38:447–55. doi: 10.2500/aap.2017.38.4087
75. Nordenfelt P, Dawson S, Wahlgren CF, Lindfors A, Mallbris L, Björkander J. Quantifying the burden of disease and perceived health state in patients with hereditary angioedema in Sweden. Allergy Asthma Proc. (2014) 35:185–90. doi: 10.2500/aap.2014.35.3738
76. Whitehurst DGT, Mittmann N, Noonan VK, Dvorak MF, Bryan S. Health state descriptions, valuations and individuals' capacity to walk: a comparative evaluation of preference-based instruments in the context of spinal cord injury. Qual Life Res. (2016) 25:2481–96. doi: 10.1007/s11136-016-1297-3
77. Engel L, Bryan S, Noonan VK, Whitehurst DGT. Using path analysis to investigate the relationships between standardized instruments that measure health-related quality of life, capability well-being and subjective well-being: an application in the context of spinal cord injury. Soc Sci Med. (2018) 213:154–64. doi: 10.1016/j.socscimed.2018.07.041
78. Buckner TW, Witkop M, Guelcher C, Sidonio R, Kessler CM, Clark DB, et al. Impact of hemophilia B on quality of life in affected men, women, and caregivers-Assessment of patient-reported outcomes in the B-HERO-S study. Eur J Haematol. (2018) 100:592–602. doi: 10.1111/ejh.13055
79. Kempton CL, Recht M, Neff A, Wang M, Buckner TW, Soni A, et al. Impact of pain and functional impairment in US adults with haemophilia: patient-reported outcomes and musculoskeletal evaluation in the pain, functional impairment and quality of life (P-FiQ) study. Haemophilia. (2018) 24:261–70. doi: 10.1111/hae.13377
80. Arraras JI, Ibañez B, Basterra I, Pereda N, Martin M, Iribarren S. Determinants of quality of life in Spanish outpatients with schizophrenia spectrum disorders. Eur J Psychiat. (2017) 32:113–21. doi: 10.1016/j.ejpsy.2017.11.001
81. Kitic AP, Jankovic S. Quality of life in institutionalized patients with schizophrenia. Psychiatr Psychol Klin. (2018) 18:5–11. doi: 10.15557/PiPK.2018.0001
82. Tennvall GR, Norlin JM, Malmberg I, Erlendsson AM, Hædersdal M. Health related quality of life in patients with actinic keratosis–an observational study of patients treated in dermatology specialist care in Denmark. Health Qual Life Outcomes. (2015) 13:111. doi: 10.1186/s12955-015-0295-4
83. Gray LA, Hernández Alava M, Wailoo AJ. Development of methods for the mapping of utilities using mixture models: mapping the AQLQ-S to the EQ-5D-5L and the HUI3 in patients with asthma. Value Health. (2018) 21:748–57. doi: 10.1016/j.jval.2017.09.017
84. Hernandez G, Dima AL, Pont À, Garin O, Martí-Pastor M, Alonso J, et al. Impact of asthma on women and men: comparison with the general population using the EQ-5D-5L questionnaire. PLoS ONE. (2018) 13:e0202624. doi: 10.1371/journal.pone.0202624
85. Wong LL, Fisher HF, Stocken DD, Rice S, Khanna A, Heneghan MA, et al. The impact of autoimmune hepatitis and its treatment on health utility. Hepatology. (2018) 68:1487–97. doi: 10.1002/hep.30031
86. Cook N, Geier A, Schmid A, Hirschfield G, Kautz A, Schattenberg JM, et al. The patient perspectives on future therapeutic options in nash and patient needs. Front Med. (2019) 6:61. doi: 10.3389/fmed.2019.00061
87. van Dongen-Leunis A, Redekop WK, Uyl-de Groot CA. Which questionnaire should be used to measure quality-of-life utilities in patients with acute leukemia? An evaluation of the validity and interpretability of the EQ-5D-5L and preference-based questionnaires derived from the EORTC QLQ-C30. Value Health. (2016) 19:834–43. doi: 10.1016/j.jval.2016.05.008
88. Hendriksz CJ, Lavery C, Coker M, Ucar SK, Jain M, Bell L, et al. Burden of disease in patients with Morquio A syndrome: results from an international patient-reported outcomes survey. Orphanet J Rare Dis. (2014) 9:32. doi: 10.1186/1750-1172-9-32
89. Andersson F, Anderson P, Holm-Larsen T, Piercy J, Everaert K, Holbrook T. Assessing the impact of nocturia on health-related quality-of-life and utility: results of an observational survey in adults. J Med Econ. (2016) 19:1200–06. doi: 10.1080/13696998.2016.1211136
90. Mealy MA, Boscoe A, Caro J, Levy M. Assessment of patients with neuromyelitis optica spectrum disorder using the EQ-5D. Int J MS Care. (2019) 21:129–34. doi: 10.7224/1537-2073.2017-076
91. Nikiphorou E, Ramiro S, van der Heijde D, Norton S, Moltó A, Dougados M, et al. Association of comorbidities in spondyloarthritis with poor function, work disability, and quality of life: results from the assessment of spondyloarthritis international society comorbidities in spondyloarthritis study. Arthritis Care Res. (2018) 70:1257–62. doi: 10.1002/acr.23468
92. Van Assche G, Peyrin-Biroulet L, Sturm A, Gisbert JP, Gaya DR, Bokemeyer B, et al. Burden of disease and patient-reported outcomes in patients with moderate to severe ulcerative colitis in the last 12 months - Multicenter European cohort study. Dig Liver Dis. (2016) 48:592–600. doi: 10.1016/j.dld.2016.01.011
93. Mijnarends DM, Schols JMGA, Halfens RJG, Meijers J, Luiking YC, Verlaan S, et al. Burden-of-illness of Dutch community-dwelling older adults with sarcopenia: health related outcomes and costs. Eur Geriatr Med. (2016) 7:276–84. doi: 10.1016/j.eurger.2015.12.011
94. Tran BX, Thu Vu G, Hoang Nguyen L, Tuan Le Nguyen A, Thanh Tran T, Thanh Nguyen B, et al. Cost-of-illness and the health-related quality of life of patients in the dengue fever outbreak in Hanoi in 2017. Int J Environ Res Public Health. (2018) 15:1174. doi: 10.3390/ijerph15061174
95. Chevreul K, Berg Brigham K, Michel M, Rault G, BURQOL-RD Research Network. Costs and health-related quality of life of patients with cystic fibrosis and their carers in France. J Cyst Fibros. (2015) 14:384–91. doi: 10.1016/j.jcf.2014.11.006
96. Collado-Mateo D, Chen G, Garcia-Gordillo MA, Iezzi A, Adsuar JC, Olivares PR, et al. Fibromyalgia and quality of life: mapping the revised fibromyalgia impact questionnaire to the preference-based instruments. Health Qual Life Outcomes. (2017) 15:114. doi: 10.1186/s12955-017-0690-0
97. Chevreul K, Berg Brigham K, Brunn M, des Portes V, BURQOL-RD Research Network. Fragile X syndrome: economic burden and health-related quality of life of patients and caregivers in France. J Intellect Disabil Res. (2015) 59:1108–20. doi: 10.1111/jir.12215
98. Juul-Kristensen B, Østengaard L, Hansen S, Boyle E, Junge T, Hestbaek L. Generalised joint hypermobility and shoulder joint hypermobility, - risk of upper body musculoskeletal symptoms and reduced quality of life in the general population. BMC Musculoskelet Disord. (2017) 18:226. doi: 10.1186/s12891-017-1595-0
99. Bewick J, Morris S, Hopkins C, Erskine S, Philpott CM. Health utility reporting in chronic rhinosinusitis patients. Clin Otolaryngol. (2018) 43:90–5. doi: 10.1111/coa.12903
100. Forestier-Zhang L, Watts L, Turner A, Teare H, Kaye J, Barrett J, et al. Health-related quality of life and a cost-utility simulation of adults in the UK with osteogenesis imperfecta, X-linked hypophosphatemia and fibrous dysplasia. Orphanet J Rare Dis. (2016) 11:160. doi: 10.1186/s13023-016-0538-4
101. Katchamart W, Narongroeknawin P, Chanapai W, Thaweeratthakul P. Health-related quality of life in patients with rheumatoid arthritis. BMC Rheumatol. (2019) 3:34. doi: 10.1186/s41927-019-0080-9
102. Román Ivorra JA, Fernández-Llanio-Comella N, San-Martín-Álvarez A, Vela-Casasempere P, Saurí-Ferrer I, González-de-Julián S, et al. Health-related quality of life in patients with systemic lupus erythematosus: a Spanish study based on patient reports. Clin Rheumatol. (2019) 38:1857–64. doi: 10.1007/s10067-019-04485-6
103. Aguirre E, Kang S, Hoare Z, Edwards RT, Orrell M. How does the EQ-5D perform when measuring quality of life in dementia against two other dementia-specific outcome measures? Qual Life Res. (2016) 25:45–9. doi: 10.1007/s11136-015-1065-9
104. Wong CKH, Cheung PWH, Samartzis D, Luk KD, Cheung KMC, Lam CLK, et al. Mapping the SRS-22r questionnaire onto the EQ-5D-5L utility score in patients with adolescent idiopathic scoliosis. PLoS ONE. (2017) 12:e0175847. doi: 10.1371/journal.pone.0175847
105. Christensen HN, Olsson U, From J, Breivik H. Opioid-induced constipation, use of laxatives, and health-related quality of life. Scand J Pain. (2016) 11:104–10. doi: 10.1016/j.sjpain.2015.12.007
106. Vo P, Fang J, Bilitou A, Laflamme AK, Gupta S. Patients' perspective on the burden of migraine in Europe: a cross-sectional analysis of survey data in France, Germany, Italy, Spain, and the United Kingdom. J Headache Pain. (2018) 19:82. doi: 10.1186/s10194-018-0907-6
107. Voormolen DC, Cnossen MC, Polinder S, Gravesteijn BY, Von Steinbuechel N, Real RGL, et al. Prevalence of post-concussion-like symptoms in the general population in Italy, The Netherlands and the United Kingdom. Brain Inj. (2019) 33:1078–86. doi: 10.1080/02699052.2019.1607557
108. Lim SH, He HG, Chan SWC. Psychometric properties of the Chinese version of the acceptance of Chronic Health Conditions (Stoma) Scale for patients with stoma. Cancer Nurs. (2017) 40:E42–9. doi: 10.1097/NCC.0000000000000411
109. Villoro R, Merino M, Hidalgo-Vega A. Quality of life and use of health care resources among patients with chronic depression. Patient Relat Outcome Meas. (2016) 7:145–55. doi: 10.2147/PROM.S101595
110. Vermaire JH, van Houtem CM, Ross JN, Schuller AA. The burden of disease of dental anxiety: generic and disease-specific quality of life in patients with and without extreme levels of dental anxiety. Eur J Oral Sci. (2016) 124:454–58. doi: 10.1111/eos.12290
111. Lane TRA, Varatharajan L, Fiorentino F, Shepherd AC, Zimmo L, Gohel MS, et al. Truncal varicose vein diameter and patient-reported outcome measures. Br J Surg. (2017) 104:1648–55. doi: 10.1002/bjs.10598
112. Rencz F, Lakatos PL, Gulácsi L, Brodszky V, Kürti Z, Lovas S, et al. Validity of the EQ-5D-5L and EQ-5D-3L in patients with Crohn's disease. Qual Life Res. (2019) 28:141–52. doi: 10.1007/s11136-018-2003-4
113. Chevreul K, Brigham KB, Gandré C, Mouthon L, BURQOL-RD Research Network. The economic burden and health-related quality of life associated with systemic sclerosis in France. Scand J Rheumatol. (2015) 44:238–46. doi: 10.3109/03009742.2014.976653
114. National Institute for Clinical Excellence. Position Statement on Use of the EQ-5D-5L Value Set for England (updated October 2019). Available online at: https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/technology-appraisal-guidance/eq-5d-5l (accessed February 03, 2021).
Keywords: HRQOL, health utility, EQ-5D-5L, disease, EuroQol
Citation: Zhou T, Guan H, Wang L, Zhang Y, Rui M and Ma A (2021) Health-Related Quality of Life in Patients With Different Diseases Measured With the EQ-5D-5L: A Systematic Review. Front. Public Health 9:675523. doi: 10.3389/fpubh.2021.675523
Received: 03 March 2021; Accepted: 24 May 2021;
Published: 29 June 2021.
Edited by:
Mihajlo Jakovljevic, Hosei University, JapanReviewed by:
Renata Linertová, Fundación Canaria de Investigación Sanitaria, SpainLong Hoang Nguyen, Hanoi Medical University, Vietnam
Georgi Iskrov, Plovdiv Medical University, Bulgaria
Copyright © 2021 Zhou, Guan, Wang, Zhang, Rui and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aixia Ma, YWl4aWF4YTE5NjFAMTYzLmNvbQ==
 Ting Zhou
Ting Zhou Haijing Guan2
Haijing Guan2 Luying Wang
Luying Wang Mingjun Rui
Mingjun Rui