- 1Dongzhimen Hospital, Beijing University of Chinese Medicine, Beijing, China
- 2Graduate School, Beijing University of Chinese Medicine, Beijing, China
- 3Tongzhou District of Dongzhimen Hospital, Beijing University of Chinese Medicine, Beijing, China
Objective: Air pollution is a major environmental risk to human health, with increasing evidence linking it to non-alcoholic fatty liver disease (NAFLD). However, findings remain inconsistent. This meta-analysis aimed to assess the relationship between air pollutants and the risk of NAFLD.
Methods: PubMed, Embase, and Web of Science were systematically searched for studies published up to March 20, 2025. A random effects model was used to estimate combined odds ratios (ORs) and 95% confidence intervals (95% CIs). Subgroup analysis, sensitivity analysis, funnel plots, and Egger's test were conducted.
Results: A total of 12 studies, including 49,549,903 participants (published between 2022 and 2024), were analyzed. For each 10 μg/m3 increase in pollutants, the ORs were 1.22 (1.16–1.29) for particulate matter with aerodynamic diameter ≤ 2.5 μm (PM2.5), 1.15 (0.95–1.40) for particulate matter between 2.5 and 10 μm in aerodynamic diameter (PM2.5 − 10), and 1.07 (1.01–1.13) for particulate matter with aerodynamic diameter ≤ 10 μm (PM10). For gaseous pollutants, the ORs were 1.45 (0.92–2.28) for sulfur dioxide (SO2) and 1.10 (1.06–1.14) for nitrogen dioxide (NO2). No notable connection emerged between ozone (O3) or carbon monoxide (CO) and NAFLD. Subgroup analysis revealed stronger associations for PM2.5, PM10, and NO2 with NAFLD in developed countries, Europe, and cohort studies, compared to developing countries, Asia, and cross-sectional studies.
Conclusion: This analysis supports a positive relationship between air pollution and NAFLD risk. Geographic region and economic development appear to moderate this association.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD42024594146, Identifier: CRD42024594146.
1 Introduction
Non-alcoholic fatty liver disease (NAFLD) ranks among the foremost causes of chronic liver conditions globally, encompassing a progression from simple steatosis and steatohepatitis to severe outcomes like fibrosis and cirrhosis (1). Currently affecting 32.4% of people globally, this condition is expected to see a notable surge in prevalence over the next 10 years (2–4). Beyond its toll on liver function and survival, NAFLD is connected to various extrahepatic disorders, such as cardiovascular disease, type 2 diabetes mellitus, chronic kidney disease, and select cancers (5–7), posing a growing public health challenge (4). Understanding the risk factors for NAFLD is crucial for early prevention and management.
Air pollution, a major environmental health threat, contributes to an estimated 7 million premature deaths annually (8) and is linked to chronic diseases including cardiovascular disease, respiratory disorders, and cancer (9–12). Key pollutants include particulate matter (PM), ozone (O3), nitrogen dioxide (NO2), sulfur dioxide (SO2), and carbon monoxide (CO) (13). Recent evidence suggests that air pollutants may also increase NAFLD risk, though findings remain inconsistent (14–16). For instance, some studies have reported a significant association between particulate matter with aerodynamic diameter ≤ 2.5 μm (PM2.5) and the risk of NAFLD (17, 18), whereas others have found little to no relationship (19, 20). Experimental studies indicate that the underlying mechanisms may involve oxidative stress, inflammation, and insulin resistance induced by air pollutant exposure (21–23).
A prior meta-analysis (24) focused on NAFLD risk included a limited subset of studies and failed to standardize effect sizes across studies, leading to potential bias. Furthermore, several large, high-quality cohort and cross-sectional studies in recent years have added new insights into the relationship between air pollution and NAFLD risk (17, 20, 25, 26). To address these gaps, we conducted an updated meta-analysis to comprehensively evaluate the relationship between multiple air pollutants (e.g., PM, NO2, SO2, CO, O3) and NAFLD risk, incorporating recent high-quality studies and standardizing effect estimates for improved comparability.
2 Methods
This meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (27) and was registered with PROSPERO (CRD42024594146) before initiation.
2.1 Data sources and searches
PubMed, Embase, and Web of Science were explored for pertinent studies released by March 20, 2025. The search was limited to English-language publications and utilized a blend of medical subject headings (MeSH) and terms associated with liver conditions (e.g., “fatty liver,” “steatohepatitis*,” “Visceral Steatos*,” “liver steatosis*”) and atmospheric pollutants (e.g., “air pollution,” “particulate matter,” “nitrogen oxides,” “ozone,” “sulfur dioxide,” “carbon monoxide”). The detailed search strategy is provided in Supplementary Tables S1–S3.
2.2 Selection criteria
The meta-analysis included studies that met the following Population, Exposure, Comparison, Outcome, Study Design (PECOS) criteria:
Population: general population, including adults and children.
Exposure: air pollutants, including PM2.5, particulate matter between 2.5 and 10 μm in aerodynamic diameter (PM2.5 − 10), particulate matter with aerodynamic diameter ≤ 10 μm (PM10), NO2, SO2, CO, and O3.
Comparator: non-exposed or less-exposed populations.
Outcome: NAFLD, metabolic-associated fatty liver disease (MAFLD), or metabolic dysfunction-associated steatotic liver disease (MASLD). NAFLD diagnoses were based on ICD-10 codes K75.8 and K76.0, or ultrasonography of hepatic steatosis with complications such as obesity, type 2 diabetes mellitus, or metabolic disorders (MAFLD) (28), or MASLD as defined by hepatic steatosis plus one of five cardiometabolic criteria (29).
Study design: observational studies, including cohort, cross-sectional, and case-control designs.
Studies that reported odds ratios (ORs), risk ratios (RRs), or hazard ratios (HRs) with 95% confidence intervals (CIs), or provided sufficient data for these estimates, were included. Recent or comprehensive studies were prioritized when datasets overlapped (30).
Exclusion criteria included conference abstracts, protocols, reviews, and duplicate publications.
2.3 Study selection
Titles and abstracts were independently reviewed by two authors (XZ and LSH) based on pre-set inclusion and exclusion guidelines. Full texts of potentially qualifying studies were then evaluated to confirm their suitability. Any differences of opinion were settled by involving a third author (XZY) as a mediator.
2.4 Data extraction
Data were independently gathered by two authors (XZ and LSH), with a third author (XZY) addressing any inconsistencies. Collected details included the first author, year of publication, study design, region, survey period, sample size, mean age, female proportion, air pollutants measured, outcome, statistical model, and effect estimates with corresponding 95% CIs.
2.5 Quality assessment
Quality assessments were independently performed by two authors (XZ and LSH). Discrepancies were resolved through discussion. The quality of cohort studies was assessed using the Newcastle-Ottawa Scale (NOS) (31), with scores categorized as: low (0–3), moderate (4–6), or high (7–9) quality. Cross-sectional study quality was assessed using the American Agency for Healthcare Research and Quality criteria (32), with scores classified as: low (0–3), moderate (4–7), or high (8–11).
2.6 Statistical analysis
Adjusted ORs and their 95% CIs were relied upon to evaluate the link between air pollutants and NAFLD risk. Studies reporting RRs or HRs were considered equivalent to ORs (33). Pollutant levels reported in parts per billion (ppb) were transformed to μg/m3 using conversion rates: 1.88 for NO2, 2.62 for SO2, 1.96 for O3, and 1.15 for CO. Due to varying increments of air pollutant exposure, ORs and 95% CIs were standardized to a 10 μg/m3 increase using the formula (34):
A random-effects model was employed to derive pooled ORs linking NAFLD with pollutant exposure. Heterogeneity was examined using Cochran's Q test and the I2 metric, where I2 exceeding 50% denoted substantial variability. Subgroup analyses explored heterogeneity sources, considering factors like study type, sample size, female ratio, economic context, smoking prevalence, region, education, and outcome classification. Sensitivity tests verified the stability of results. Funnel plots and Egger's regression test were used to detect publication bias (35), with a minimum of 10 studies required for this analysis (36). Statistical analyses were performed using Stata version 14.0.
3 Results
3.1 Literature selection
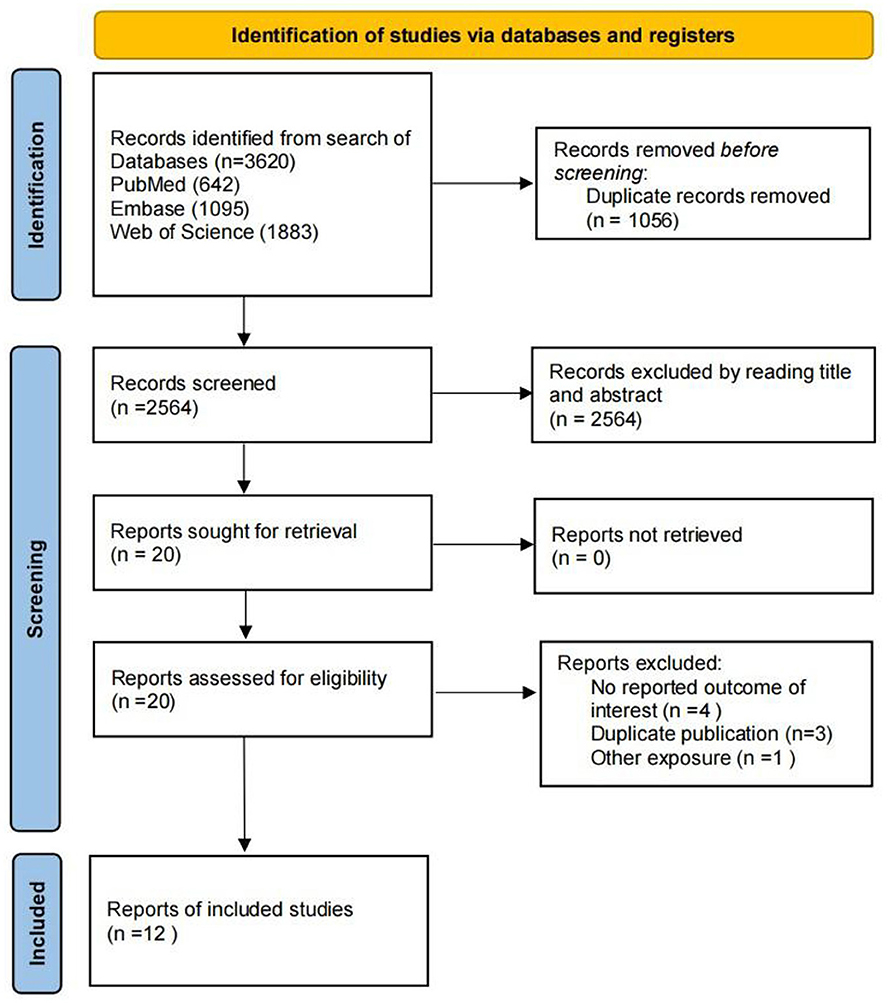
The search strategy identified 3,620 relevant articles. After removing duplicates, 2,564 records underwent title and abstract evaluation. Full-text assessment was performed on 20 articles, of which eight were excluded: four for lack of relevant results, three for duplication, and one for addressing a different exposure. Ultimately, 12 studies were retained for the meta-analysis (Figure 1).
3.2 Study characteristics
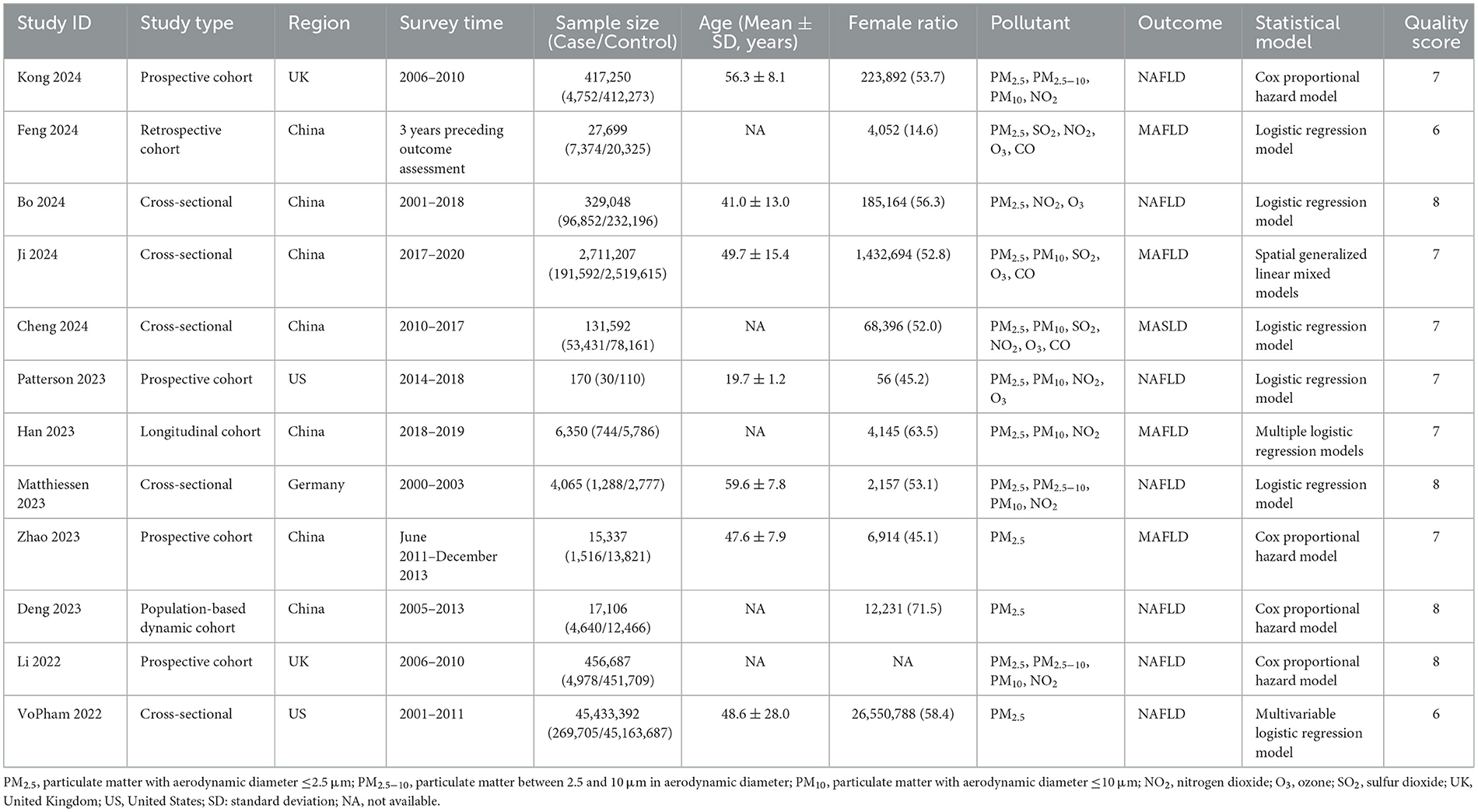
The 12 included studies (14–18, 20, 25, 26, 37–40), published between 2022 and 2024, involved a total of 49,549,903 participants. Of these, seven were cohort studies (17, 18, 20, 25, 37, 39, 40) and five were cross-sectional (14–16, 26, 38). Sample sizes ranged from 170 to 45,433,392. Studies focused on various air pollutants: 12 on PM2.5, three on PM2.5 − 10, seven on PM10, three on SO2, eight on NO2, five on O3, and three on CO. Geographically, seven studies were conducted in Asia, three in Europe, and two in North America. Confounders adjusted for in the studies varied slightly. Quality assessment revealed eight studies rated as high quality and four as medium quality (Supplementary Tables S4, S5). Detailed study characteristics are provided in Table 1.
3.3 Exposure of air pollution and NAFLD
Table 2 presents the ORs linking air pollutants to NAFLD, with forest plots for analyses involving over five studies shown in Figures 2–4. A 10 μg/m3 rise in PM2.5, PM10, and NO2 levels was notably tied to elevated NAFLD risk (PM2.5 OR = 1.22, 95% CI: 1.16–1.29; PM10 OR = 1.07, 95% CI: 1.01–1.13; NO2 OR = 1.10, 95% CI: 1.06–1.14; Figures 2–4). However, significant heterogeneity was observed across studies (PM2.5 I2 = 91.4%, P < 0.001; PM10 I2 = 86.9%, P < 0.001; NO2 I2 = 92.9%, P < 0.001). For PM2.5 − 10 and SO2, a 10 μg/m3 increase suggested increased NAFLD likelihood, though these findings did not achieve statistical significance (PM2.5 − 10 OR = 1.15, 95% CI: 0.95–1.40, P = 0.15; SO2 OR = 1.45, 95% CI: 0.92–2.28, P = 0.113), with SO2 showing marked heterogeneity (I2 = 98.4%, P < 0.001). No notable connection emerged between O3 or CO and NAFLD.
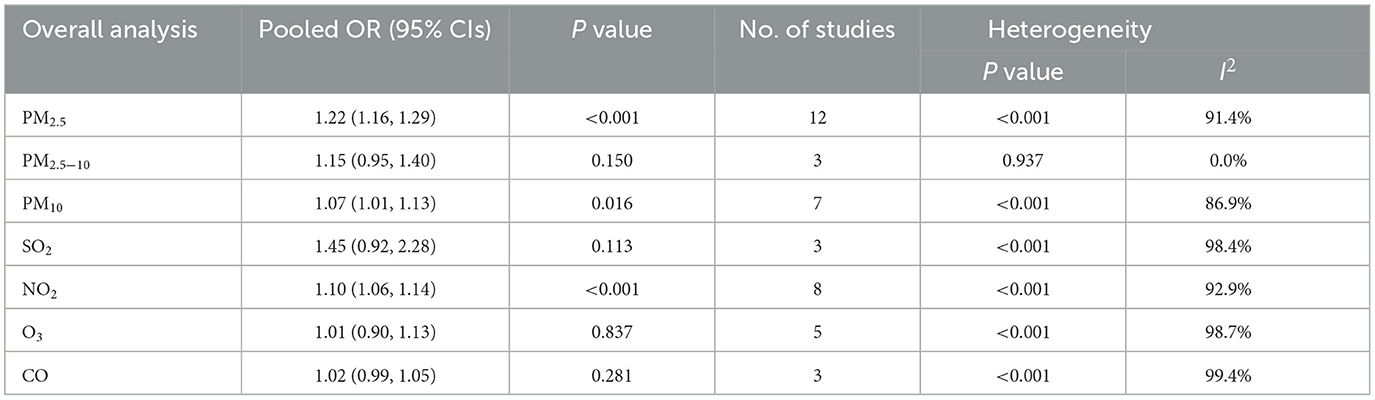
Table 2. Meta-analysis of NAFLD in association with a 10 μg/m3 increase in PM2.5, PM2.5 − 10, PM10, SO2, NO2, O3, and CO.
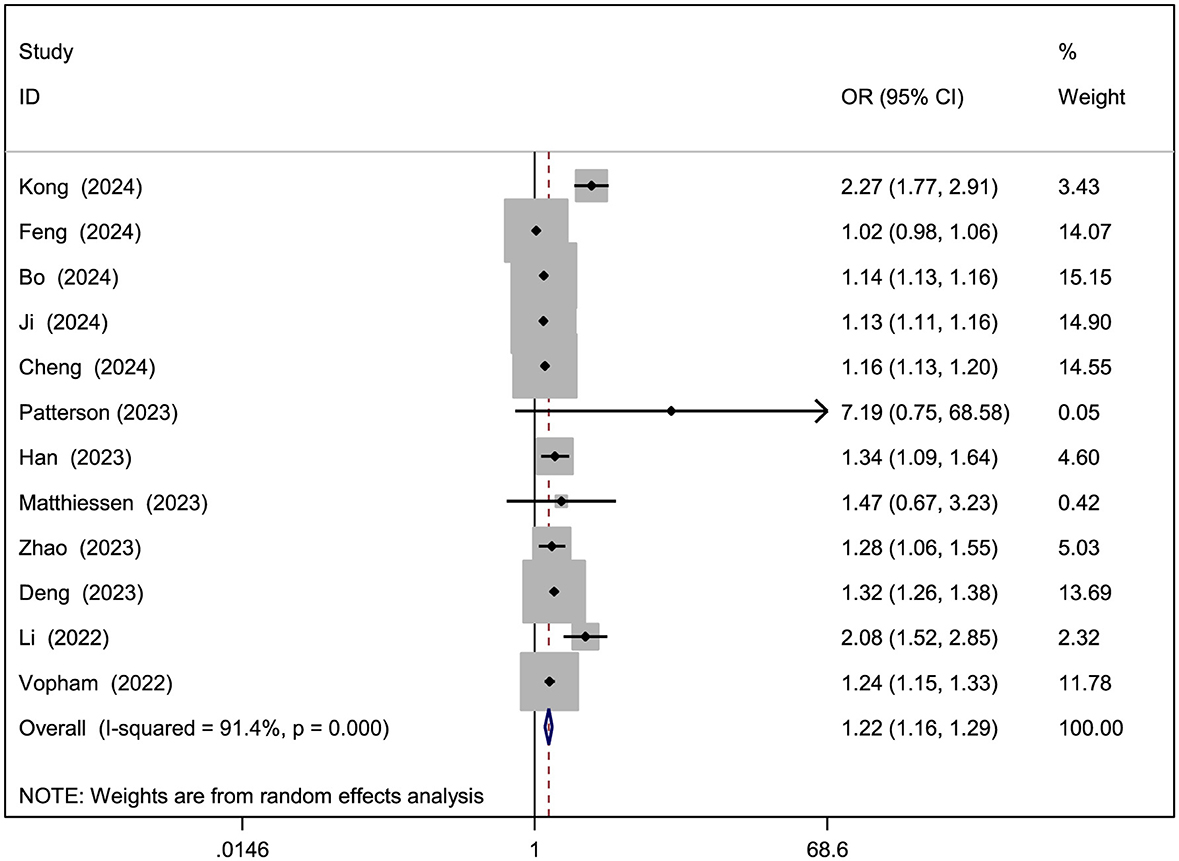
Figure 2. Forest plot of the association between PM2.5 exposure (per 10 μg/m3 increment) and risk of NAFLD.
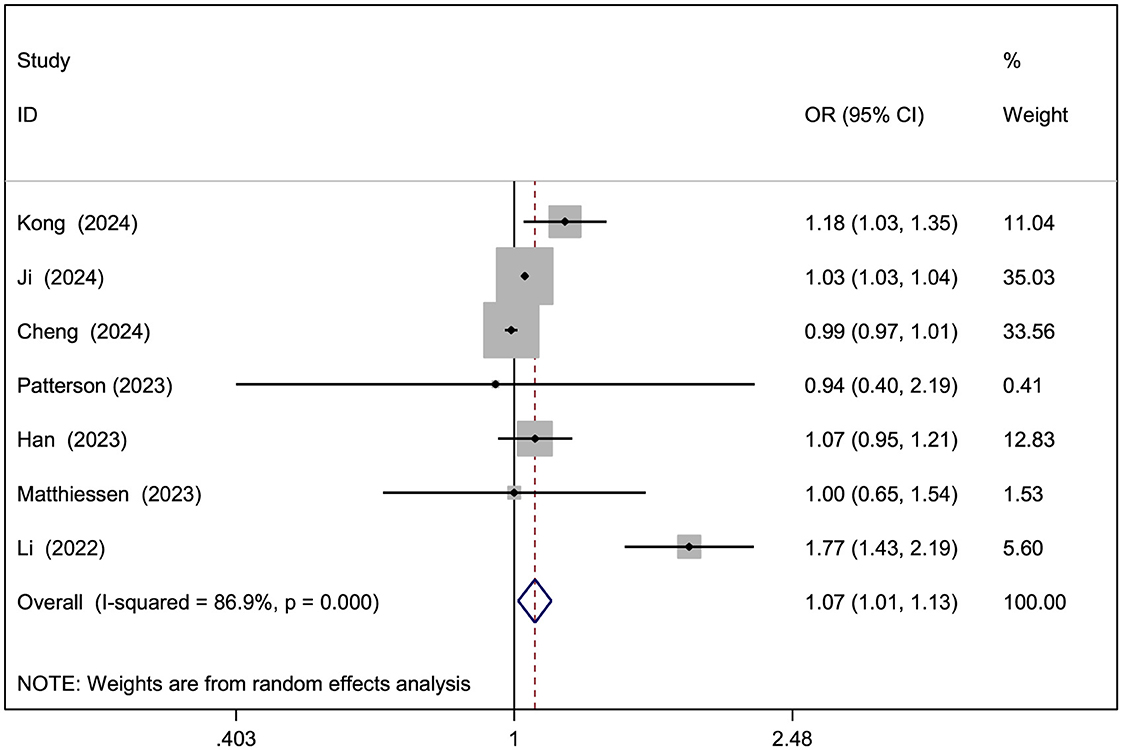
Figure 3. Forest plot of the association between PM10 exposure (per 10 μg/m3 increment) and risk of NAFLD.
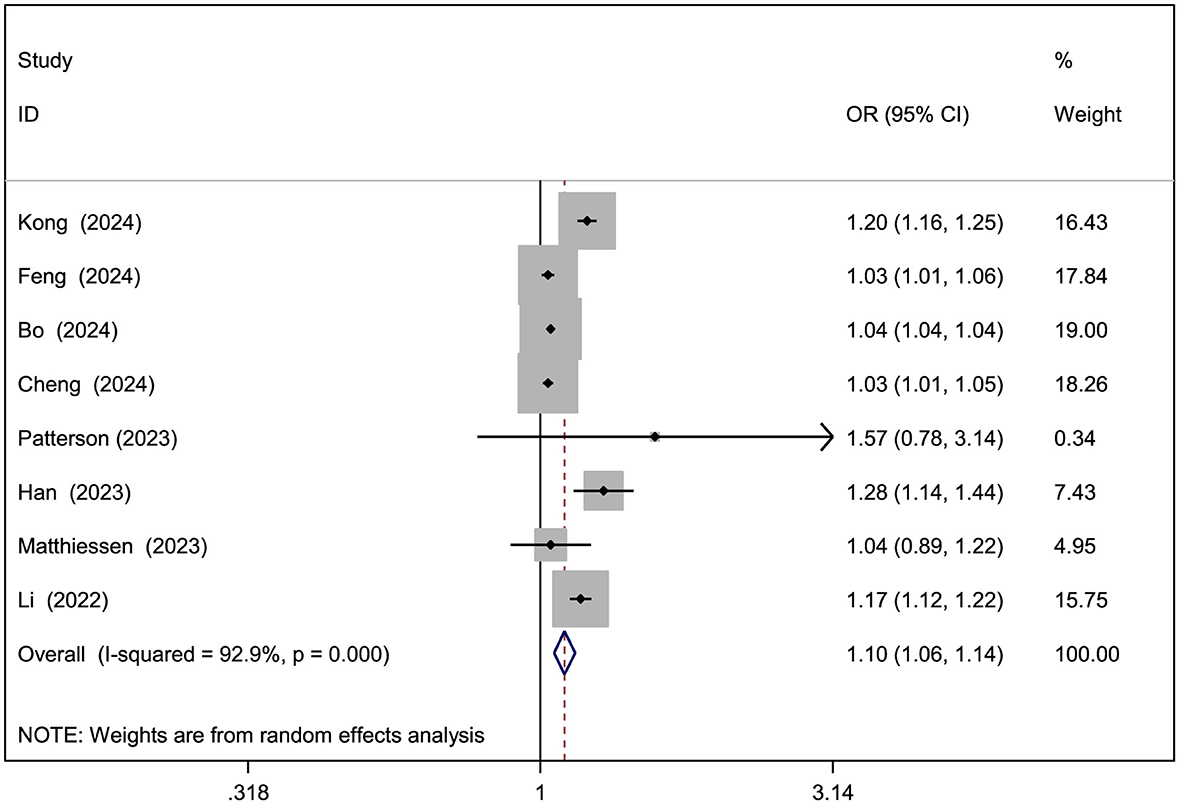
Figure 4. Forest plot of the association between NO2 exposure (per 10 μg/m3 increment) and risk of NAFLD.
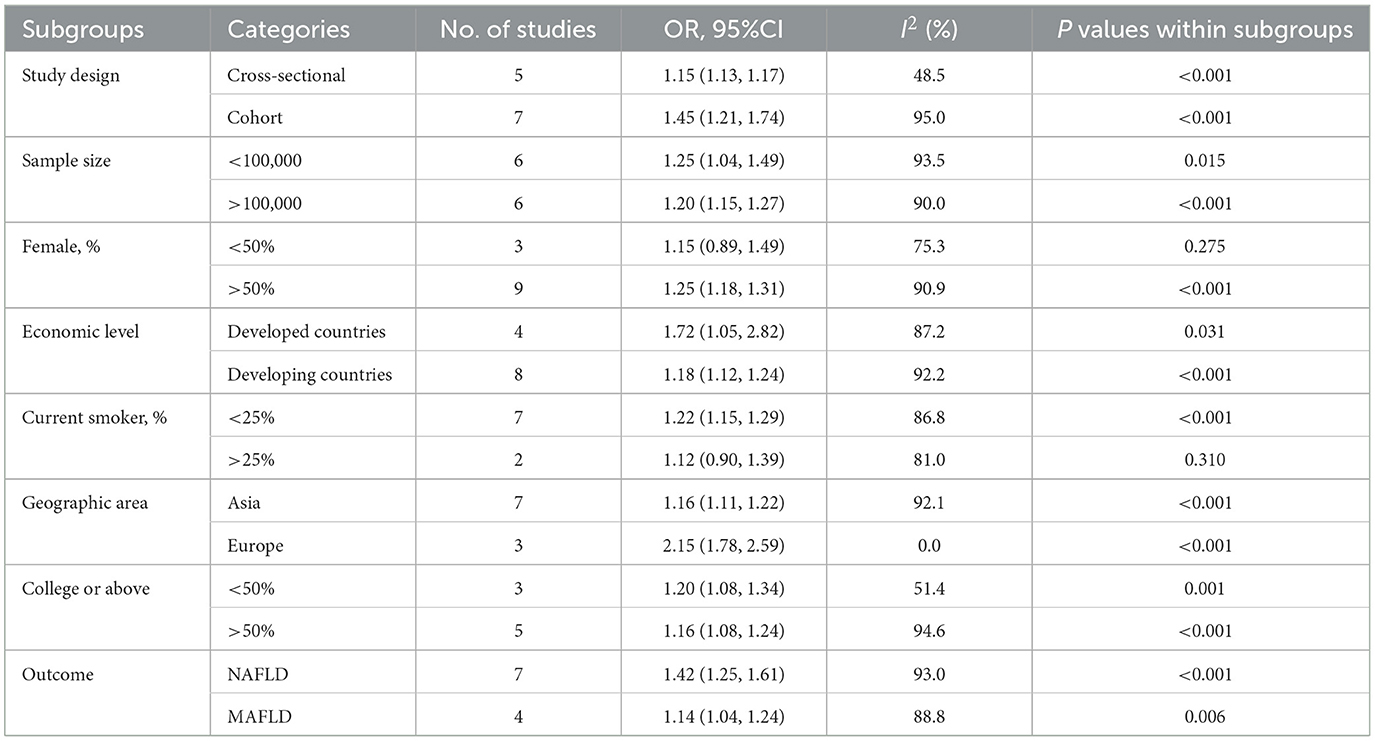
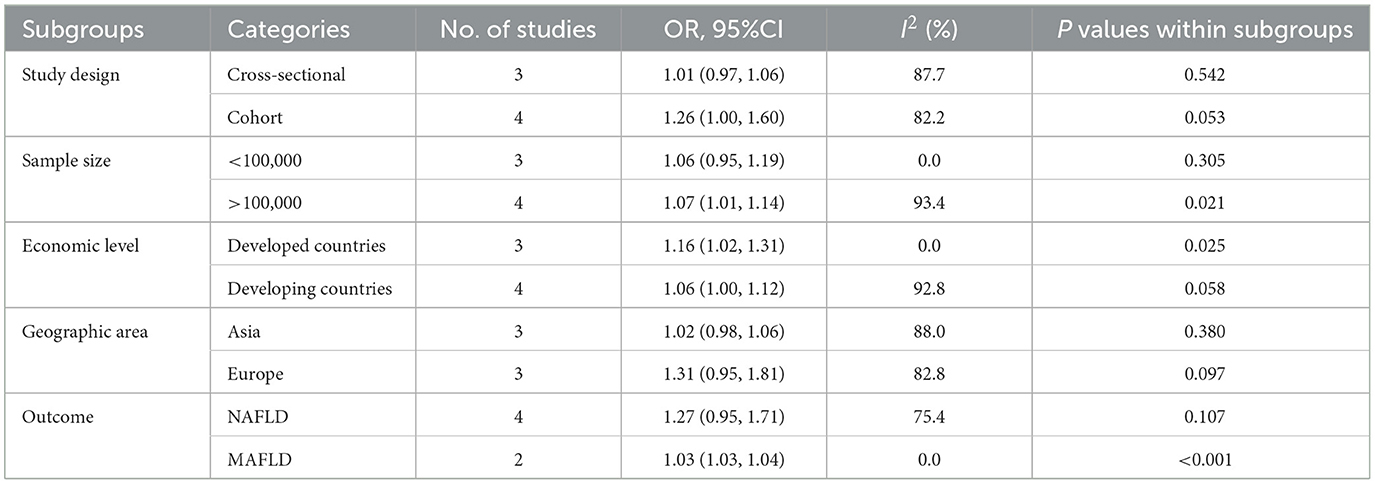
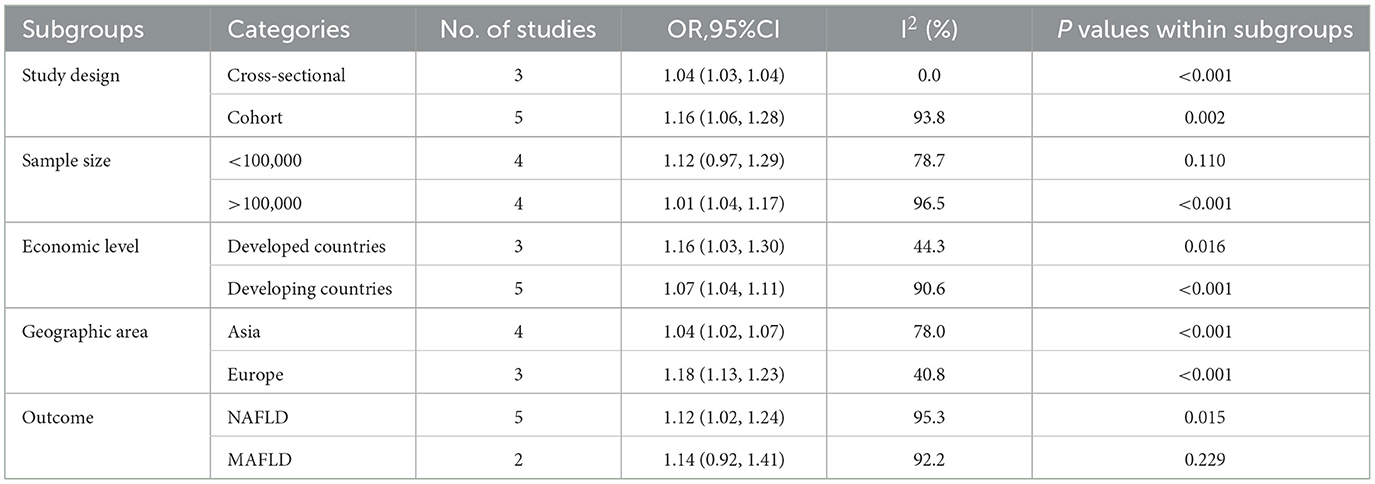
3.4 Subgroup analysis
Given the scarcity of studies, subgroup analyses were not feasible for PM2.5 − 10, SO2, O3, or CO. Subgroup analyses for PM2.5, PM10, and NO2 are presented in Tables 3–5. In most subgroups, exposure to these pollutants remained positively associated with NAFLD, although heterogeneity remained at moderate to high levels. Stronger associations were observed in studies from developed countries, Europe, and cohort studies compared to those from developing countries, Asia, and cross-sectional studies. Specifically, a significant and robust association was found for PM2.5 in Europe (OR = 2.15, 95% CI: 1.78–2.59, P < 0.001, I2 = 0%). Stratified analysis of PM10 in developed countries, with sample sizes < 100,000, showed I2 = 0%, as did stratified analysis of NO2 in cross-sectional studies.
3.5 Sensitivity analysis and publication bias
Sensitivity analysis, conducted by excluding one study at a time, indicated that the results for most air pollutants were stable (Supplementary Figure S1). Publication bias tests were not conducted for exposures with fewer than 10 studies. Visual inspection of the funnel plot for PM2.5 indicated no significant publication bias (Figure 5). Additionally, Egger's regression test (P = 0.069) supported the absence of publication bias.
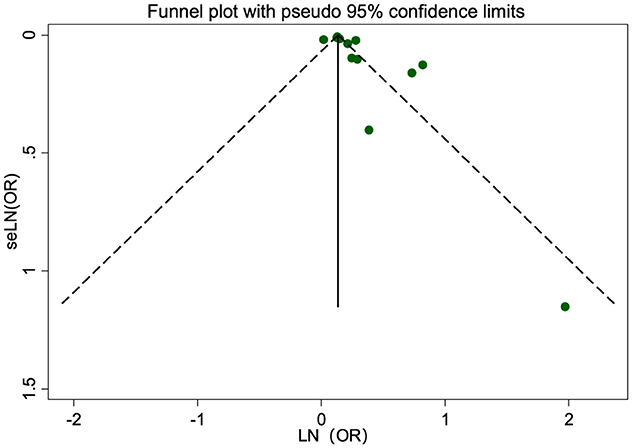
Figure 5. Funnel plot of the association between PM2.5 exposure (per 10 μg/m3 increment) and risk of NAFLD.
4 Discussion
Based on 12 studies involving 49,549,903 participants, the results indicate that exposure to air pollutants, including PM2.5, PM2.5 − 10, PM10, SO2, NO2, O3, and CO, correlates with an increased risk of NAFLD. However, considerable heterogeneity was observed across studies, with the associations for PM2.5 − 10 and SO2 not reaching statistical significance. Subgroup and sensitivity analyses supported these overall findings, with consistent associations observed across most subgroups.
A prior meta-analysis by He et al. reported that PM2.5, NOx, PM10, and PM2.5 − 10 elevate NAFLD risk, while suggesting a protective role for O3 (24). That review, however, was limited to a subset of earlier studies on air pollution and MAFLD risk, introducing potential selection bias. In addition, the meta-analysis did not normalize effect sizes to the same increments across studies. In contrast, this work involved an exhaustive review of research linking air pollution to NAFLD, MAFLD, or MASLD, included several recent, large-sample, high-quality studies, and standardized effect sizes to 10 μg/m3 increments. Therefore, this research has more advantages in timeliness and comparability. In addition, instead of including the cross-sectional study by Guo et al. (41), the same sample, the latest cohort study by Han et al. (25), was chosen, which contributes to the reliability of causal inference. Notably, unlike the results from He et al., no significant association was found between O3 and NAFLD. Stronger associations were observed between PM2.5, PM10, NO2, and NAFLD in developed countries, particularly in Europe, and in cohort studies.
Subgroup analysis indicated a stronger association between PM2.5, PM10, and NO2 with NAFLD in cohort studies, which offer greater reliability for inferring correlation compared to cross-sectional studies. Additionally, a more pronounced and statistically significant association was found for PM2.5 in women over 50%. This may be linked to sex-specific differences in susceptibility to air pollution, as previous studies have suggested women may have a higher susceptibility to respiratory and cardiovascular issues related to PM2.5 exposure (42, 43). Furthermore, estrogen has been shown to regulate liver lipid metabolism, potentially offering protective effects in women (44–47). The decline in estrogen levels post-menopause may increase susceptibility to NAFLD in women exposed to air pollution, contributing to the observed gender differences. Gender differences in NAFLD risk may, therefore contribute to heterogeneity in the results. Regional variations were also evident, with stronger associations found in studies from developed countries, particularly Europe, for PM2.5 and NO2, possibly reflecting economic and environmental influences—though limited study numbers constrain broader conclusions.
In stratified analysis comparing NAFLD and MAFLD outcomes, no significant differences were observed regarding their associations with PM2.5, PM10, and NO2. Notably, a study by the European LITMUS “Liver Investigation: Testing Marker Utility in Steatohepatitis” Consortium found that 98% of NAFLD cases met the MASLD criteria (29), and data from Song et al. indicated that most NAFLD patients met the metabolic criteria for MAFLD and MASLD (48). This suggests that findings for NAFLD are applicable under both the MAFLD and MASLD definitions.
The mechanisms by which air pollution contributes to NAFLD remain incompletely understood, though animal studies offer valuable insights. Chronic exposure to PM2.5 has been demonstrated to cause liver inflammation, oxidative stress, and insulin resistance, which are pivotal factors in the pathogenesis of NAFLD (49–52). Experimental studies also suggest that PM2.5 disrupts liver glycogen storage, causes glucose intolerance, and contributes to non-alcoholic steatohepatitis (53, 54). Furthermore, PM2.5 exposure activates hepatic stellate cells, promoting liver fibrosis (55, 56). NO2 and O3 exposure may also impair lipid metabolism and trigger insulin resistance, potentially exacerbating NAFLD risk (57–59). However, this analysis did not show a significant correlation between O3 and NAFLD, possibly due to differences in species, exposure levels, or study design. The effects of SO2 and CO on NAFLD remain unclear and warrant further research.
Given the global health burden of air pollution and rising NAFLD prevalence, our findings highlight the urgent need for improved air quality, which may help prevent NAFLD and other related non-communicable diseases, like cardiovascular and respiratory conditions (60, 61).
This study has several limitations. First, methodological and clinical heterogeneity was observed due to variations in confounder adjustment and study designs. Although subgroup analyses were conducted to explore potential sources of heterogeneity, the limited number of studies restricted a comprehensive identification of contributing factors. Second, the analysis focused on individual pollutants, despite the potential for combined effects of air pollutants on health outcomes. The complexity of joint effects and the scarcity of relevant studies precluded their inclusion in this meta-analysis. Third, the included studies did not consistently stratify NAFLD by severity (e.g., simple steatosis vs. non-alcoholic steatohepatitis or fibrosis), limiting the ability to assess the impact of air pollution on non-reversible forms of the disease. Future studies stratifying outcomes by NAFLD severity could reduce heterogeneity and provide clearer insights into the role of air pollution. Finally, given the heterogeneity and limited number of studies for certain pollutants, caution is warranted when interpreting the findings. Larger-scale cohort studies are needed to validate these results and further elucidate the relationship between air pollution and NAFLD risk.
5 Conclusion
This meta-analysis provides evidence that exposure to air pollutants, particularly PM2.5, PM10, and NO2, is associated with an increased risk of NAFLD. These findings underscore the importance of improving air quality to mitigate the burden of NAFLD and related diseases. However, it remains to be determined whether air pollutants directly target the liver or contribute to NAFLD by aggravating obesity and insulin resistance in air-polluted environments. Future research should focus on large-scale, longitudinal cohort studies that stratify NAFLD by severity, evaluate the combined effects of multiple air pollutants, and explore underlying biological mechanisms.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
XZ: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. XY: Conceptualization, Funding acquisition, Supervision, Validation, Writing – review & editing. LH: Data curation, Methodology, Software, Writing – original draft. LT: Data curation, Investigation, Writing – original draft. XL: Data curation, Writing – original draft. YC: Formal analysis, Writing – original draft. SR: Conceptualization, Data curation, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The research reported in this publication was supported by the Fundamental Research Funds for the Central Universities, Beijing University of Chinese Medicine (No. 2020-JYB-ZDGG-115) and Beijing Traditional Chinese Medicine New Era 125 project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1606959/full#supplementary-material
References
1. Rinella ME, Neuschwander-Tetri BA, Siddiqui MS, Abdelmalek MF, Caldwell S, Barb D, et al. AASLD practice guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology. (2023) 77:1797–835. doi: 10.1097/HEP.0000000000000323
2. Perumpail BJ, Khan MA, Yoo ER, Cholankeril G, Kim D, Ahmed A. Clinical epidemiology and disease burden of nonalcoholic fatty liver disease. World J Gastroenterol. (2017) 23:8263–76. doi: 10.3748/wjg.v23.i47.8263
3. Riazi K, Azhari H, Charette JH, Underwood FE, King JA, Afshar EE, et al. The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. (2022) 7:851–61. doi: 10.1016/S2468-1253(22)00165-0
4. Younossi ZM. Non-alcoholic fatty liver disease – a global public health perspective. J Hepatol. (2019) 70:531–44. doi: 10.1016/j.jhep.2018.10.033
5. Duell PB, Welty FK, Miller M, Chait A, Hammond G, Ahmad Z, et al. Nonalcoholic fatty liver disease and cardiovascular risk: a scientific statement from the American Heart Association. Arterioscler Thromb Vasc Biol. (2022) 42:e168–85. doi: 10.1161/ATV.0000000000000153
6. Thomas JA, Kendall BJ, El-Serag HB, Thrift AP, Macdonald GA. Hepatocellular and extrahepatic cancer risk in people with non-alcoholic fatty liver disease. Lancet Gastroenterol Hepatol. (2024) 9:159–69. doi: 10.1016/S2468-1253(23)00275-3
7. Adams LA, Anstee QM, Tilg H, Targher G. Non-alcoholic fatty liver disease and its relationship with cardiovascular disease and other extrahepatic diseases. Gut. (2017) 66:1138–53. doi: 10.1136/gutjnl-2017-313884
9. Feigin VL, Abate MD, Abate YH, Abd ElHafeez S, Abd-Allah F, Abdelalim A, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol. (2024) 23:973–1003. doi: 10.1016/S1474-4422(24)00369-7
10. Yang IA, Jenkins CR, Salvi SS. Chronic obstructive pulmonary disease in never-smokers: risk factors, pathogenesis, and implications for prevention and treatment. Lancet Respir Med. (2022) 10:497–511. doi: 10.1016/S2213-2600(21)00506-3
11. Turner MC, Andersen ZJ, Baccarelli A, Diver WR, Gapstur SM, Pope CA III, et al. Outdoor air pollution and cancer: an overview of the current evidence and public health recommendations. CA Cancer J Clin. (2020) 70:460–79. doi: 10.3322/caac.21632
12. Simon TG, Roelstraete B, Hagström H, Sundström J, Ludvigsson JF. Non-alcoholic fatty liver disease and incident major adverse cardiovascular events: results from a nationwide histology cohort. Gut. (2022) 71:1867–75. doi: 10.1136/gutjnl-2021-325724
13. Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. (2017) 389:1907–18. doi: 10.1016/S0140-6736(17)30505-6
14. Bo Y, Lin C, Guo C, Wong M, Huang B, Lau A, et al. Chronic exposure to ambient air pollution and the risk of non-alcoholic fatty liver disease: a cross-sectional study in Taiwan and Hong Kong. Ecotoxicol Environ Saf. (2024) 275:116245. doi: 10.1016/j.ecoenv.2024.116245
15. Ji W, Cheng Y, Tang S, Gu K, Liao H, Li, et al. Exposure to ambient air pollution and metabolic dysfunction-associated fatty liver disease: findings from over 27 million adults in Northwestern China. Ecotoxicol Environ Saf . (2024) 272:116109. doi: 10.1016/j.ecoenv.2024.116109
16. VoPham T, Kim NJ, Berry K, Mendoza JA, Kaufman JD, Ioannou GN. PM2.5 air pollution exposure and nonalcoholic fatty liver disease in the Nationwide Inpatient Sample. Environ Res. (2022) 213:113611. doi: 10.1016/j.envres.2022.113611
17. Kong X, Huang R, Geng R, Wu J, Li J, Wu Y, et al. Associations of ambient air pollution and lifestyle with the risk of NAFLD: a population-based cohort study. BMC Public Health. (2024) 24:2354. doi: 10.1186/s12889-024-19761-7
18. Li F-R, Liao J, Zhu B, Li X, Cheng Z, Jin C, et al. Long-term exposure to air pollution and incident non-alcoholic fatty liver disease and cirrhosis: a cohort study. Liver Int. (2023) 43:299–307. doi: 10.1111/liv.15416
19. Song Q, Pan J, Pan M, Zheng C, Fan W, Zhen J, et al. Exploring the relationship between air pollution, non-alcoholic fatty liver disease, and liver function indicators: a two-sample Mendelian randomization analysis study. Front Endocrinol. (2024) 15:1396032. doi: 10.3389/fendo.2024.1396032
20. Feng C, Yang B, Wang Z, Zhang J, Fu Y, Yu B, et al. Relationship of long-term exposure to air pollutant mixture with metabolic-associated fatty liver disease and subtypes: a retrospective cohort study of the employed population of Southwest China. Environ Int. (2024) 188:108734. doi: 10.1016/j.envint.2024.108734
21. Sepehri B, Darbani R, Mesgari-Abbasi M, Kheirouri S, Shanehbandi D, Khordadmehr M, et al. The effects of short-time air pollution, SO2, and ozone on biochemical, histo-pathological, oxidative stress, and carcinogenesis related genes expressions in the liver of the rats. Hum Exp Toxicol. (2024) 43:9603271241263569. doi: 10.1177/09603271241263569
22. Liu C, Xu X, Bai Y, Wang T-Y, Rao X, Wang A, et al. Air pollution–mediated susceptibility to inflammation and insulin resistance: influence of CCR2 pathways in mice. Environ Health Perspect. (2014) 122:17–26. doi: 10.1289/ehp.1306841
23. Sun Q, Yue P, Deiuliis JA, Lumeng CN, Kampfrath T, Mikolaj MB, et al. Ambient air pollution exaggerates adipose inflammation and insulin resistance in a mouse model of diet-induced obesity. Circulation. (2009) 119:538–46. doi: 10.1161/CIRCULATIONAHA.108.799015
24. He X, Zhang S, Bai Q, Pan M, Jiang Y, Liu W, et al. Air pollution exposure and prevalence of non-alcoholic fatty liver disease and related cirrhosis: a systematic review and meta-analysis. Ecotoxicol Environ Saf. (2025) 289:117469. doi: 10.1016/j.ecoenv.2024.117469
25. Han X, Guo B, Wang L, Chen K, Zhou H, Huang S, et al. The mediation role of blood lipids on the path from air pollution exposure to MAFLD: a longitudinal cohort study. Sci Total Environ. (2023) 904:166347. doi: 10.1016/j.scitotenv.2023.166347
26. Cheng W-C, Wong P-Y, Wu C-D, Cheng P-N, Lee P-C, Li C-Y. Non-linear association between long-term air pollution exposure and risk of metabolic dysfunction-associated steatotic liver disease. Environ Health Prev Med. (2024) 29:7–7. doi: 10.1265/ehpm.23-00271
27. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
28. Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. (2020) 73:202–9. doi: 10.1016/j.jhep.2020.07.045
29. Rinella ME, Lazarus JV, Ratziu V, Francque SM, Sanyal AJ, Kanwal F, et al. A multi-society Delphi consensus statement on new fatty liver disease nomenclature. J Hepatol. (2023) 79:1542–56 doi: 10.1097/HEP.0000000000000696
30. Bai W, Chen P, Cai H, Zhang Q, Su Z, Cheung T, et al. Worldwide prevalence of mild cognitive impairment among community dwellers aged 50 years and older: a meta-analysis and systematic review of epidemiology studies. Age Ageing. (2022) 51:afac173. doi: 10.1093/ageing/afac173
31. Wells G, Shea BJ, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Wwwohrica (2021). Available online at: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (Accessed April 5, 2025).
32. Rostom A, Dubé C, Cranney A, Saloojee N, Sy R, Garritty C, et al. Appendix D. Quality Assessment Forms. Agency for Healthcare Research and Quality (2004). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK35156/ (Accessed April 5, 2025).
33. Ou X-X, Wang X, Zhan X-L, Shen S-L, Karatela S, Jing J, et al. The associations of secondhand smoke exposure with neurodevelopmental disorders and critical time window identification: a systematic review and meta-analysis. Sci Total Environ. (2024) 913:169649. doi: 10.1016/j.scitotenv.2023.169649
34. Yang B-Y, Qian Z, Howard SW, Vaughn MG, Fan S-J, Liu K-K, et al. Global association between ambient air pollution and blood pressure: a systematic review and meta-analysis. Environ Pollut. (2018) 235:576–88. doi: 10.1016/j.envpol.2018.01.001
35. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
36. Higgins J, Thomas J. Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed. Chichester, UK: Wiley-Blackwell (2019). doi: 10.1002/9781119536604
37. Patterson WB, Holzhausen E, Chalifour B, Goodrich J, Costello E, Lurmann F, et al. Exposure to ambient air pollutants, serum miRNA networks, lipid metabolism, and non-alcoholic fatty liver disease in young adults. Ecotoxicol Environ Saf. (2023) 264:115486. doi: 10.1016/j.ecoenv.2023.115486
38. Matthiessen C, Glaubitz L, Lucht S, Kälsch J, Luedde T, Erbel R, et al. Long-term exposure to air pollution and prevalent nonalcoholic fatty liver disease. Environ Epidemiol. (2023) 7:e268. doi: 10.1097/EE9.0000000000000268
39. Zhao Y, Peng Y, Wang M, Zhao Y, He Y, Zhang, et al. Exposure to PM2.5 and its constituents is associated with metabolic dysfunction-associated fatty liver disease: a cohort study in Northwest of China. Environ Geochem Health. (2023) 46:304. doi: 10.1007/s10653-024-02071-7
40. Deng P, Tang H, Zhu L, Duan J, Li F, Li Y, et al. Association of long-term ambient fine particulate matter (PM2.5) and incident non-alcoholic fatty liver disease in Chinese adults. Environ Pollut. (2023) 329:121666. doi: 10.1016/j.envpol.2023.121666
41. Guo B, Guo Y, Nima Q, Feng Y, Wang Z, Lu R, et al. Exposure to air pollution is associated with an increased risk of metabolic dysfunction-associated fatty liver disease. J Hepatol. (2022) 76:518–25. doi: 10.1016/j.jhep.2021.10.016
42. Bell ML, Son J-Y, Peng RD, Wang Y, Dominici F. Ambient PM2.5 and risk of hospital admissions: do risks differ for men and women? Epidemiology. (2015) 26:575–9. doi: 10.1097/EDE.0000000000000310
43. Swieczkowski M, Lip GYH, Kurasz A, Dabrowski EJ, Tomaszuk-Kazberuk A, Kamiński JW, et al. Association between exposure to air pollution and increased ischemic stroke incidence: a retrospective population-based cohort study (EP-PARTICLES study). Eur J Prev Cardiol. (2024) 32:276–87. doi: 10.1093/eurjpc/zwae301
44. Ministrini S, Montecucco F, Sahebkar A, Carbone F. Macrophages in the pathophysiology of NAFLD: the role of sex differences. Eur J Clin Invest. (2020) 50:e13236. doi: 10.1111/eci.13236
45. Sommerauer C, Gallardo-Dodd CJ, Savva C, Hases L, Birgersson M, Indukuri R, et al. Estrogen receptor activation remodels TEAD1 gene expression to alleviate hepatic steatosis. Mol Syst Biol. (2024) 20:374–402. doi: 10.1038/s44320-024-00024-x
46. Naville D, Labaronne E, Vega N, Pinteur C, Canet-Soulas E, Vidal H, et al. Metabolic outcome of female mice exposed to a mixture of low-dose pollutants in a diet-induced obesity model. PLoS ONE. (2015) 10:e0124015. doi: 10.1371/journal.pone.0124015
47. Le Magueresse-Battistoni B. Endocrine disrupting chemicals and metabolic disorders in the liver: what if we also looked at the female side? Chemosphere. (2021) 268:129212. doi: 10.1016/j.chemosphere.2020.129212
48. Song SJ, Lai JC, Wong GL, Wong VW, Yip TC. Can we use old NAFLD data under the new MASLD definition? J Hepatol. (2023) 80:e54–6. doi: 10.1016/j.jhep.2023.07.021
49. Chen J, Wu L, Yang G, Zhang C, Liu X, Sun X, et al. The influence of PM2.5 exposure on non-alcoholic fatty liver disease. Life Sci. (2021) 270:119135. doi: 10.1016/j.lfs.2021.119135
50. Xu M-X, Ge C-X, Qin Y-T, Gu T-T, Lou D-S, Li Q, et al. Prolonged PM2.5 exposure elevates risk of oxidative stress-driven nonalcoholic fatty liver disease by triggering increase of dyslipidemia. Free Radic Biol Med. (2019) 130:542–56. doi: 10.1016/j.freeradbiomed.2018.11.016
51. Du Z, Liang S, Li Y, Zhang J, Yu Y, Xu Q, et al. Melatonin alleviates PM25-induced hepatic steatosis and metabolic-associated fatty liver disease in ApoE-/- mice. Oxid Med Cell Longev. (2022) 2022:1–24. doi: 10.1155/2022/8688643
52. Alderete TL, Habre R, Toledo-Corral CM, Berhane K, Chen Z, Lurmann FW, et al. Longitudinal associations between ambient air pollution with insulin sensitivity, β-cell function, and adiposity in Los Angeles Latino Children. Diabetes. (2017) 66:1789–96. doi: 10.2337/db16-1416
53. Tarantino G, Capone D, Finelli C. Exposure to ambient air particulate matter and non-alcoholic fatty liver disease. World J Gastroenterol. (2013) 19:3951. doi: 10.3748/wjg.v19.i25.3951
54. Zheng Z, Xu X, Zhang X, Wang A, Zhang C, Hüttemann M, et al. Exposure to ambient particulate matter induces a NASH-like phenotype and impairs hepatic glucose metabolism in an animal model. J Hepatol. (2013) 58:148–54. doi: 10.1016/j.jhep.2012.08.009
55. Zheng Z, Zhang X, Wang J. Exposure to fine airborne particulate matters induces hepatic fibrosis in murine models. J Hepatol. (2015) 63:1397–404. doi: 10.1016/j.jhep.2015.07.020
56. Wang Z-J, Yu H, Hao J-J, Peng Y, Yin, T-T. Qiu, Y-N. PM25 promotes Drp1-mediated mitophagy to induce hepatic stellate cell activation and hepatic fibrosis via regulating miR-411. Exp Cell Res. (2021) 407:112828. doi: 10.1016/j.yexcr.2021.112828
57. Guo Y, Ji S, Li D, Sang N. Ambient NO2 exposure affects hepatic glycolipid metabolism in mice with a sex-dependent property. J Hazard Mater. (2022) 441:129957. doi: 10.1016/j.jhazmat.2022.129957
58. Miller DB, Snow SJ, Henriquez A, Schladweiler MC, Ledbetter AD, Richards JE, et al. Systemic metabolic derangement, pulmonary effects, and insulin insufficiency following subchronic ozone exposure in rats. Toxicol Appl Pharmacol. (2016) 306:47–57. doi: 10.1016/j.taap.2016.06.027
59. Vella RE, Pillon NJ, Zarrouki B, Croze ML, Koppe L, Guichardant M, et al. Ozone exposure triggers insulin resistance through muscle c-Jun N-terminal kinase activation. Diabetes. (2015) 64:1011–24. doi: 10.2337/db13-1181
60. Rajagopalan S, Al-Kindi SG, Brook RD. Air Pollution and Cardiovascular Disease. J Am Coll Cardiol. (2018) 72:2054–70. doi: 10.1016/j.jacc.2018.07.099
Keywords: air pollution, particulate matter, non-alcoholic fatty liver disease, systematic review, meta-analysis
Citation: Zhang X, Yang X, Hu L, Tan L, Li X, Chai Y and Ru S (2025) Association between air pollution and risk of non-alcoholic fatty liver disease: an updated meta-analysis. Front. Public Health 13:1606959. doi: 10.3389/fpubh.2025.1606959
Received: 06 April 2025; Accepted: 28 July 2025;
Published: 19 August 2025.
Edited by:
Kaijian Hou, Shantou University, ChinaReviewed by:
Brigitte Le Magueresse-Battistoni, INSERM U1060 Laboratoire de Recherche en Cardiovasculaire, Métabolisme, diabétologie et Nutrition, FranceWang Miyuan, Huazhong University of Science and Technology, China
Copyright © 2025 Zhang, Yang, Hu, Tan, Li, Chai and Ru. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xianzhao Yang, eWFuZ3hpYW56aGFvQGJ1Y20uZWR1LmNu; Shuying Ru, cnN5XzIwMDhAMTYzLmNvbQ==
 Xu Zhang
Xu Zhang Xianzhao Yang
Xianzhao Yang Lanshuo Hu
Lanshuo Hu Lingjie Tan
Lingjie Tan Xiaoyang Li
Xiaoyang Li Yijie Chai
Yijie Chai Shuying Ru
Shuying Ru