- Department of Clinical Laboratory, Zhengzhou Key Laboratory of Children’s Infection and Immunity, Children’s Hospital Affiliated to Zhengzhou University, Henan Children’s Hospital, Zhengzhou Children’s Hospital, Zhengzhou, China
Background: Vitamins are vital for children’s health, and deficiencies can cause disorders, compromising quality of life and survival. This study systematically assesses multivitamin levels, nutritional status, and associated factors in children from Henan, China. It aims to provide robust evidence to improve pediatric nutrition and inform policies for local governments and institutions.
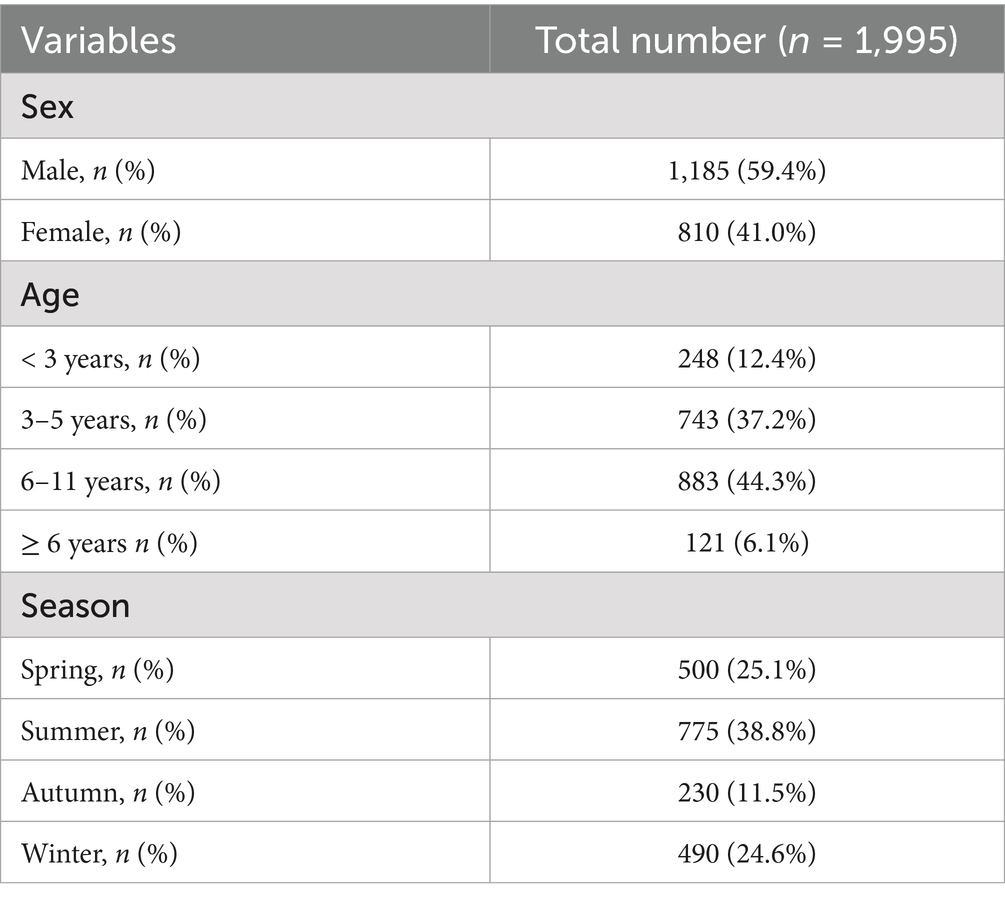
Methods: This retrospective study analyzed data from 1,995 healthy children who underwent routine physical examinations between March 1, 2022, and May 20, 2024. General clinical information and vitamin test results, including vitamins A, D, B1, B2, B3, B5, B7, and C, were retrieved from electronic medical records. Participants were categorized into four age groups: under 3 years, 3–5 years, 6–11 years and 12–18 years. Seasonal classification comprised spring, summer, autumn, and winter.
Results: The cohort consisted of 1,185 males and 810 females. Age distribution included 248 children under 3 years, 743 children aged 3 to 5 years, 883 children aged 6 to 11 years and 121 children aged 12 years or older. Analysis of vitamin insufficiency revealed the highest insufficiency rates for vitamin B7 (58.8%), followed by vitamin D (28.5%), A (28.0%), B1 (11.8%), C (9.1%), E (2.2%), and B3 (0.1%). Notable sex-specific differences were identified in vitamin D, E, B2, B5, and C levels. Age-dependent variations were observed for vitamin A, D, E, B1, B2, B3, B5, B7, and C, while seasonal fluctuations impacted vitamin A, D, E, B1, B3, B5, B7, and C. Sex-based analysis indicated a higher prevalence of vitamin A and C insufficiencies in males and a greater incidence of vitamin D insufficiency in females. Preschool children exhibited the highest vitamin A insufficiency rates, whereas adolescent aged children demonstrated the highest insufficiencies in vitamin D, E, B1, B7, and C. Seasonal analysis revealed increased vitamin A and C insufficiencies during summer, heightened vitamin D and B7 insufficiencies in winter, vitamin E insufficiencies in spring, and vitamin B1 deficiencies in autumn.
Conclusion: A high prevalence of vitamin insufficiencies, particularly in vitamins B7, D, A, and C, was observed among children in Henan, China, with variation rates associated with sex, age, and season.
Introduction
Vitamins are essential micronutrients indispensable for sustaining human health (1). They are classified into water-soluble vitamins (including vitamin C and B-complex vitamins) and fat-soluble vitamins (such as vitamins A, D, E, and K). These nutrients are integral to numerous physiological processes, including energy metabolism, antioxidant defense, immune modulation, and blood coagulation. Vitamin deficiencies can precipitate a range of adverse health outcomes, including compromised immune function, skeletal abnormalities, and cognitive impairments (2–6).
Childhood vitamin insufficiencies/deficiencies represent a significant global public health concern. Current evidence indicates that approximately 25% of children worldwide experience subclinical vitamin A (VA) deficiency, with nearly 250 million children annually at risk of blindness due to inadequate VA intake (7). In China, the prevalence of pediatric vitamin deficiencies, particularly VA and vitamin D (VD), has shown a rising trend. A cross-sectional survey conducted in Jiangsu Province between 2016 and 2017 reported a 0.8% prevalence of VA deficiency among children, with an additional 15.8% classified as marginally deficient (8). Notably, geographic disparities persist, with rural children displaying a significantly elevated risk of VA deficiency compared to their urban counterparts (9). VD deficiency is similarly concerning, affecting 23.2% of children with deficient levels and 54.2% with insufficient levels. The pediatric VD status is influenced by a range of factors, including sex, age, geographical location, duration of sunlight exposure, and maternal education (10). In northern China, children exhibit increased rates of VD deficiency during winter due to reduced ultraviolet radiation exposure (9). Moreover, deficiencies in B vitamins among children constitute a substantial global public health challenge (11). As children age, their physiological demand for B vitamins increases; however, dietary practices in many households fail to meet these requirements, resulting in significant nutritional gaps (12).
Currently, evidence suggests an age-dependent increase in the prevalence of vitamin deficiencies among children (13). Children’s nutritional status directly impacts their future health and developmental potential. However, comprehensive investigations into the vitamin nutritional levels and status of children in Henan, China are still lacking. This study aims to systematically assess the nutritional status of various vitamins among children in Henan, China and identify key influencing factors through epidemiological surveys. The outcomes are intended to inform public health policy, support clinicians in identifying high-risk groups, and guide the development of targeted intervention strategies. Additionally, the findings will provide practical insights into pediatric healthcare and nutrition, promoting a more evidence-based and standardized approach to managing child health.
Materials and methods
Study design and population
A retrospective study was conducted at Henan Provincial Children’s Hospital (Children’s Hospital Affiliated to Zhengzhou University). Henan Provincial Children’s Hospital is a tertiary hospital located in a major city in Henan, China. It is designated as a National Regional Medical Center for Children and is recognized as the Henan Provincial Children’s Medical Center. Thanks to the country’s comprehensive child health insurance system, children from diverse socioeconomic backgrounds can receive treatment at this center. As one of the largest children’s hospitals in Henan, China, it serves patients from Henan Province, making its patient population a representative sample of the pediatric population in Henan, China. From March 1, 2022, to May 20, 2024, 1,995 healthy children who underwent routine physical examinations at the Department of Child Health Care and Health Management Center were enrolled in this study. The inclusion criteria encompassed: (1) age below 18 years; (2) availability of complete electronic medical records containing age, sex, and vitamin assay results. Exclusion criteria comprised: (1) diagnosis of infectious diseases; (2) history of congenital anomalies; (3) presence of growth and developmental disorders; (4) hematological diseases or dysfunctions of the liver, kidneys, or heart.
The selection of vitamins was based on their established roles in child development and emerging regional concerns regarding suboptimal micronutrient status, particularly in areas undergoing dietary transition. While vitamins such as A, D, and C are widely recognized for their clinical significance, other B-vitamins (e.g., B1, B2, B3, B5, B7) were included to provide a comprehensive nutritional overview and support public health surveillance, given limited contemporary data in this population. It should be noted that biochemical deficiency does not invariably correspond to overt clinical disease; rather, it identifies populations at potential risk or with suboptimal status.
The study protocol adhered to the principles of the Declaration of Helsinki and was approved by the Ethics Review Committee of Henan Children’s Hospital (Approval No. 2022-K-L045). As the study employed anonymized retrospective data obtained during standard clinical practice, the requirement for informed consent was waived, as verified by the Ethics Review Board of Henan Children’s Hospital (Approval No. 2022-K-L045).
Data collection
Demographic data and laboratory parameters were systematically extracted from the electronic medical record system for children undergoing routine health examinations. Demographic variables included age, sex, examination date, and clinical diagnoses. The primary laboratory indicators encompassed vitamin assay results, specifically targeting retinol (VA), 25-(OH)-vitamin D2, 25-(OH)-vitamin D3, vitamin E (VE), vitamin B1 (VB1), vitamin B2 (VB2), vitamin B3 (VB3), vitamin B5 (VB5), vitamin B7 (VB7), and vitamin C (VC). Total VD level was calculated by 25-(OH)-vitamin D2 plus 25-(OH)-vitamin D3. Serum vitamin levels were determined using the ultra-performance liquid chromatography–tandem mass spectrometry (UPLC-MS/MS) system (Waters Corp, Milford, MA). Sample preparation was performed following the manufacturer’s protocol outlined in the commercial reagent kit (Shanghai Kehua Biological Technology Co., Ltd.).
Operational definitions
1) Age Stratification
Children under 18 years were stratified into three developmental stages:
(a) Infancy/Toddler Period: < 3 years.
(b) Preschool Age: 3–5 years.
(e) School Age: 6 to 11 years.
(f) Adolescent age: ≥ 12 years
2) Seasonal Classification
The calendar year was segmented into four meteorological seasons:
(a) Spring: March–May.
(b) Summer: June–August.
(c) Autumn: September–November.
(d) Winter: December–February of the following year.
3) Vitamin insufficiency criteria
According to the Chinese Expert Consensus on Clinical Applications of VA and VD in Children (2024) (14):
(i) VA (retinol) insufficiency: < 300 ng/mL.
(ii) VD insufficiency: < 20 ng/mL.
For vitamins without established guidelines, insufficiency thresholds were determined based on reference ranges from Mayo Clinic, Labcorp, and Quest Diagnostics:
(a) VE insufficiency: < 3.8 μg/mL (Mayo Clinic).
(b) VB1 insufficiency: < 2.12 ng/mL (Quest Diagnostics).
(c) VB2 insufficiency: < 1 ng/mL (Mayo Clinic).
(d) VB3 insufficiency: < 5.2 ng/mL (Labcorp).
(e) VB5 insufficiency (Mayo Clinic):
(i) Ages 0–10 years: < 3.45 ng/mL.
(ii) Ages > 10 years: < 37 ng/mL.
(f) VB7 insufficiency (Mayo Clinic):
(i) iAges < 12 years: < 0.1 ng/mL.
(ii) Ages ≥ 12 years: < 0.22 ng/mL
(g) VC insufficiency: < 4 μg/mL (Mayo Clinic).
Statistical analysis
All statistical analyses were performed using SPSS version 24.0. Continuous variables with non-normal distribution were expressed as median values along with interquartile ranges (25th–75th percentiles) and compared using the Mann–Whitney U test. Categorical variables were presented as numerical counts (percentages) and analyzed using the chi-square test. A two-tailed p-value < 0.05 was considered statistically significant.
Results
Study population characteristics
Between March 1, 2022, and May 20, 2024, a total of 1,995 pediatric patients who underwent routine health examinations were included in this study. As outlined in Table 1, the cohort comprised 1,185 males (59.4%) and 810 females (40.6%). The age distribution included 248 infants/toddlers (aged < 3 years, 12.4%), 743 preschool-aged children (aged 3 to 5 years, 37.2%), 883 school-aged children (aged 6 to 11 years, 44.3%) and 121 adolescents (aged ≥ 12 years, 6.1%). The seasonal distribution of health examinations was as follows: 500 examinations conducted in spring (25.1%), 775 in summer (38.8%), 230 in autumn (11.5%), and 490 in winter (24.6%).
Vitamin levels and nutritional status of healthy examined children
As presented in Table 2, the median concentrations (25th percentile, 75th percentile) for VA, VD, VE, VB1, VB2, VB3, VB5, VB7, and VC were as follows: VA: 349.8 (293.7, 414.2) ng/mL; VD: 25.2 (19.0, 32.0) ng/mL; VE: 7.0 (5.7, 8.4) μg/mL; VB1: 3.4 (2.6, 4.7) ng/mL; VB2: 9.2 (6.4, 13.0) ng/mL; VB3: 32.8 (21.9, 50.9) ng/mL; VB5: 52.6 (42.2, 72.0) ng/mL; VB7: 0.085 (0.043, 0.137) ng/mL; and VC: 11.3 (7.5, 15.4) μg/mL. Analysis of vitamin nutritional status revealed that VB7 exhibited the highest insufficiency rate at 58.8%, followed by VD (28.6%), VA (28.0%), VB1 (11.8%), VC (9.1%), VE (2.2%), and VB3 (0.1%). Notably, the insufficiency rates for VB2 and VB5 among the healthy pediatric population were both 0% (Supplementary Table 1).
Sex-specific variations in pediatric vitamins levels and nutritional status
Male participants demonstrated significantly higher peripheral blood levels of VD and VB5 compared to their female counterparts. In contrast, female participants exhibited markedly elevated levels of VE, VB2, and VC. No statistically significant differences between sex were observed for VA, VB1, VB3, and VB7 (Table 3). Analysis of vitamin nutritional status indicated a significantly greater prevalence of VC insufficiency among male children, whereas VD insufficiency was significantly more prevalent among female children (Supplementary Table 2).
Age-specific variations in pediatric vitamin levels and nutritional status
Serum concentrations of VA, VD, VE, and B-complex vitamins (B1, B2, B3, B5, B7), as well as VC, exhibited significant age-dependent variations among children. VA levels were notably lowest within the 3–5-year age group, while VD, VE, and all analyzed B vitamins (B1, B2, B3, B5, B7), as well as VC, demonstrated progressive declines with increasing age (Table 4). Vitamin nutritional status analysis revealed distinct age-related insufficiency patterns. The highest prevalence of VA insufficiency (31.1%) occurred in the 3–5-year group. In contrast, the insufficiency rates of VD, VE, VB1, VB7, and VC displayed significant positive correlations with age, peaking at 60.3, 5.0, 33.9, 100.0, and 24.8%, respectively, among children aged ≥ 12 years (Supplementary Table 3).
Season-specific variations in pediatric vitamins levels and nutritional status
Analysis of vitamin levels in pediatric subjects undergoing health examinations identified significant seasonal variations in VA, VD, VE, VB1, VB3, VB5, VB7, and VC. VA, VB1, VB5, and VC levels reached their lowest values during summer, while VD and VB7 levels were minimized in winter. VE and VB3 levels were lowest in spring (Table 5). Evaluation of vitamin nutritional status revealed pronounced seasonal disparities in insufficiency rates for VA, VD, VE, and VC. The highest insufficiency rates for VA (32.9%) and VC (13.7%) occurred in summer, whereas VD (42.2%) and VB7 (61.6%) insufficiency rates were most prevalent in winter. Additionally, VE insufficiency reached its peak in spring (4.4%), and VB1 demonstrated the highest insufficiency rate in autumn (16.5%) (Supplementary Table 4).
Discussion
Vitamins are fundamental nutrients essential for maintaining normal physiological functions, particularly during key stages of growth and development in childhood. Adequate vitamin intake is crucial for both physical and cognitive maturation. Vitamin deficiencies in children constitute a major global public health issue, exacerbated by the rapid progression of globalization and urbanization, particularly in low- and middle-income countries. Insufficient vitamin intake during childhood is associated with stunted growth, compromised immunity, and impaired cognitive abilities. Deficiencies in VA are linked to a range of visual impairments, including night blindness, xerophthalmia, and severe complications such as corneal ulceration and potential blindness (15). According to the World Health Organization, approximately 200 million children worldwide experience VA deficiency, directly affecting growth and immune function (16). VD deficiency is associated with skeletal abnormalities, including rickets (17), and recent studies have identified correlations between VD deficiency and increased risks of infectious diseases, cardiovascular conditions, and neurological disorders (5, 18, 19). Additionally, VE deficiency is linked to neurological impairments and immune dysfunction (20), while B vitamin deficiencies are implicated in various cardiovascular, neurological, and dermatological conditions (21–24).
Henan Province, situated in Henan, China, is the cradle of Huaxia civilization with over 3,200 years of recorded history. It served as the cultural, economic, and political center of China until approximately 1,000 years ago. Henan has a substantial child population; according to data from the Henan Provincial Government at the end of 2024, children under 15 years old numbered 20.71 million, constituting 21.2% of the total population. Furthermore, Henan Provincial Children’s Hospital, as the sole National Regional Medical Center for Children in Henan, China, provides services to children from Henan and neighboring provinces. However, the prevalence of vitamin deficiency disorders among children is increasing, and children’s nutritional status directly impacts their future health and developmental potential. Therefore, it is imperative to investigate the vitamin nutritional levels and status of children in Henan, China.
This study provides the first comprehensive assessment of multiple vitamin levels and nutritional status among children in Henan, China. It found that female children exhibited a higher prevalence of VD insufficiency. This disparity may be attributed to reduced sunlight exposure, thereby limiting endogenous VD synthesis. In contrast, female children typically present with higher levels of VE, VB2, VB5, and VC, accompanied by lower insufficiency rates compared to males. Sex-specific variations in vitamin requirements are evident; adolescent males generally exhibit higher energy and vitamin demands, which are attributed to accelerated growth rates, increased weight gain, and higher physical activity levels. Moreover, dietary patterns differ between sex, with females tending to adopt more balanced nutritional practices. In contrast, males are more likely to engage in selective eating, increasing the risk of micronutrient deficiencies.
Vitamin requirements also vary significantly across developmental stages. Infants necessitate increased VD intake to support proper skeletal growth, while adolescents require higher levels of VA and VC to facilitate immune system maturation (25). Changes in dietary habits, nutrient consumption, and physiological demands with age can result in vitamin deficiencies, adversely affecting health outcomes (26). The analysis identified distinct age-related trends, with levels of VD, VE, VB1, VB2, VB3, VB5, VB7, and VC progressively declining as age increases. Correspondingly, insufficiency rates for VD, VE, VB1, VB7, and VC rise with age, reaching their lowest levels in infants under 2 years and peaking in adolescent age over 12 years. This pattern likely reflects optimal nutrition during infancy, characterized by breastfeeding, fortified formulas, and routine VD supplementation to prevent rickets, contrasted with decreased dietary regulation and reduced outdoor activities as children grow older.
Seasonal fluctuations in vitamin levels arise from a complex interplay of factors, including sunlight exposure, dietary patterns, and physiological adaptations. VD levels exhibit pronounced seasonal variability, with deficiency risk significantly increasing during winter due to reduced daylight and lower UVB radiation (27). This study corroborates these findings, identifying the lowest VD levels and the highest insufficiency rates during winter. Seasonal variations also significantly affect VA, VE, VB1, VB3, VB5, VB7, and VC levels. Data analysis reveals that insufficiency rates for VA and VC peak during summer, while VE insufficiency is most prevalent in spring, and VC insufficiency rates increase in summer. These seasonal differences are likely influenced by the variable availability of fresh fruits and vegetables throughout the year (28).
This comprehensive analysis identifies significant associations between vitamin insufficiency rates and factors such as sex, age, and seasonal variations. However, several limitations should be considered. First, the single-center design may restrict the generalizability of our findings, and future multicenter studies are warranted for validation. Second, the lack of data on dietary habits, lifestyle factors, and socioeconomic status may introduce residual confounding. Furthermore, the limited sample size in certain subgroups—particularly within the broadly defined 12-18-year age group encompassing diverse pubertal stages—restricted finer age stratification and may have obscured more nuanced developmental trends. Additionally, the assessment of thiamine status relied solely on total blood thiamine levels rather than more sensitive functional assays, which may reduce the sensitivity to detect functional thiamine insufficiency.
Conclusion
In conclusion, this study reveals a high prevalence of vitamin insufficiencies, particularly vitamins B7, D, A, and C among children in Henan, China, with variations significantly associated with sex, age, and season. These findings provide critical evidence to guide public health policy formulation and support the implementation of targeted nutritional interventions, such as age-specific supplementation and seasonal dietary recommendations, to improve pediatric health outcomes in this population.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Ethics Review Committee of Henan Children’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because as the study employed anonymized retrospective data obtained during standard clinical practice, the requirement for informed consent was waived, as verified by the Ethics Review Board of Henan Children’s Hospital (Approval No. 2022-K-L045).
Author contributions
XL: Software, Writing – original draft, Conceptualization, Data curation, Formal analysis, Methodology. NC: Writing – review & editing, Validation, Resources, Data curation. LG: Data curation, Validation, Writing – review & editing, Resources. YL: Resources, Writing – review & editing, Data curation, Validation. ZJ: Funding acquisition, Writing – review & editing, Visualization, Project administration, Supervision. JY: Funding acquisition, Project administration, Visualization, Writing – review & editing, Supervision. TL: Supervision, Project administration, Methodology, Funding acquisition, Conceptualization, Software, Visualization, Formal analysis, Writing – review & editing, Resources, Writing – original draft, Data curation.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the National Natural Science Foundation of China (82200097), the Key Research, Development, and Promotion Projects of Henan Province (252102310054 and 232102310122), the Medical Science and Technology Project of Henan Province (LHGJ20220774), and the Zhengzhou Medical Research Project (ZZYK2024086, and ZZYK2024087).
Acknowledgments
We would like to thank Bullet Edits for their assistance with the linguistic editing of this work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2025.1657153/full#supplementary-material
References
1. Pham, VT, Dold, S, Rehman, A, Bird, JK, and Steinert, RE. Vitamins, the gut microbiome and gastrointestinal health in humans. Nutr Res. (2021) 95:35–53. doi: 10.1016/j.nutres.2021.09.001
2. Sirbe, C, Rednic, S, Grama, A, and Pop, TL. An update on the effects of vitamin D on the immune system and autoimmune diseases. Int J Mol Sci. (2022) 23:9784. doi: 10.3390/ijms23179784
3. Charoenngam, N, Shirvani, A, and Holick, MF. Vitamin D for skeletal and non-skeletal health: what we should know. J Clin Orthop Trauma. (2019) 10:1082–93. doi: 10.1016/j.jcot.2019.07.004
4. Stevens, SL. Fat-Soluble Vitamins. Nurs Clin North Am. (2021) 56:33–45. doi: 10.1016/j.cnur.2020.10.003
5. Ismailova, A, and White, JH. Vitamin D, infections and immunity. Rev Endocr Metab Disord. (2022) 23:265–77. doi: 10.1007/s11154-021-09679-5
6. Brenner, B, Kuperman, AA, Watzka, M, and Oldenburg, J. Vitamin K-dependent coagulation factors deficiency. Semin Thromb Hemost. (2009) 35:439–46. doi: 10.1055/s-0029-1225766
7. Han, X, Ding, S, Lu, J, and Li, Y. Global, regional, and national burdens of common micronutrient deficiencies from 1990 to 2019: a secondary trend analysis based on the global burden of disease 2019 study. EClinicalMedicine. (2022) 44:101299. doi: 10.1016/j.eclinm.2022.101299
8. Tian, T, Zhang, JX, and Xie, W. Vitamin a and vitamin D nutritional status among children and adolescents aged 6-17 in Jiangsu Province, 2016-2017. J. Hyg Res. (2023) 52:930–5. doi: 10.19813/j.cnki.weishengyanjiu.2023.06.012
9. Liu, R, Chen, Y, Wu, H, Xiong, F, Li, Y, and He, F. Serum vitamin a, D and E concentrations and status in children in Shaanxi Province, Northwest China. Asia Pac J Clin Nutr. (2021) 30:687–95. doi: 10.6133/apjcn.202112_30(4).0015
10. Li, LL, Li, XN, Jia, FY, Chi, MZ, Wen, ZH, Yang, F, et al. Analysis of vitamin D nutritional status in children under 7 years old in some regions of China. Chinese J. Pediatr. (2022) 60:413–20. doi: 10.3760/cma.j.cn112140-20220126-00087
11. Stevens, GA, Beal, T, Mbuya, MNN, Luo, H, Neufeld, LM, Addo, OY, et al. Micronutrient deficiencies among preschool-aged children and women of reproductive age worldwide: a pooled analysis of individual-level data from population-representative surveys. Lancet Glob Health. (2022) 10:e1590–9. doi: 10.1016/S2214-109X(22)00367-9
12. Chen, L, Li, Q, Fang, X, Wang, X, Min, J, and Wang, F. Dietary intake of homocysteine metabolism-related B-vitamins and the risk of stroke: a dose-response Meta-analysis of prospective studies. Adv Nutr. (2020) 11:1510–28. doi: 10.1093/advances/nmaa061
13. Li, T, Li, X, Chen, N, Yang, J, Yang, J, and Bi, L. Influence of the COVID-19 pandemic on the vitamin D status of children: a cross-sectional study. J Med Virol. (2023) 95:e28438. doi: 10.1002/jmv.28438
14. Society of Child Health Care. Chinese expert consensus on the clinical application of vitamin a and vitamin D for children. Chin J Child Health Care. (2021) 29:110–6. doi: 10.11852/zgetbjzz2024-0279
15. Sajovic, J, Meglic, A, Glavac, D, Markelj, Š, Hawlina, M, and Fakin, A. The role of vitamin a in retinal diseases. Int J Mol Sci. (2022) 23:14. doi: 10.3390/ijms23031014
16. WHO. Global prevalence of vitamin A deficiency in populations at risk 1995–2005 WHO global database on vitamin A deficiency. Geneva: World Health Organization (2009).
17. Ncayiyana, JR, Martinez, L, Goddard, E, Myer, L, and Zar, HJ. Prevalence and correlates of vitamin D deficiency among Young south African infants: a birth cohort study. Nutrients. (2021) 13:500. doi: 10.3390/nu13051500
18. Cosentino, N, Campodonico, J, Milazzo, V, de Metrio, M, Brambilla, M, Camera, M, et al. Vitamin D and cardiovascular disease: current evidence and future perspectives. Nutrients. (2021) 13:603. doi: 10.3390/nu13103603
19. Plantone, D, Primiano, G, Manco, C, Locci, S, Servidei, S, and de Stefano, N. Vitamin D in neurological diseases. Int J Mol Sci. (2022) 24:87. doi: 10.3390/ijms24010087
20. Terada, Y, Ohashi, H, Otani, Y, Tokunaga, K, and Takenaka, A. Increased anxiety-like behaviour is an early symptom of vitamin E deficiency that is suppressed by adrenalectomy in rats. Br J Nutr. (2021) 125:1310–9. doi: 10.1017/S0007114520001889
21. Yoshii, K, Hosomi, K, Sawane, K, and Kunisawa, J. Metabolism of dietary and microbial vitamin B family in the regulation of host immunity. Front Nutr. (2019) 6:48. doi: 10.3389/fnut.2019.00048
22. Pourie, G, Martin, N, Daval, JL, Alberto, JM, Umoret, R, Gueant, JL, et al. The stimulation of neurogenesis improves the cognitive status of aging rats subjected to gestational and perinatal deficiency of B9-12 vitamins. Int J Mol Sci. (2020) 21:8008. doi: 10.3390/ijms21218008
23. Uebanso, T, Shimohata, T, Mawatari, K, and Takahashi, A. Functional roles of B-vitamins in the gut and gut microbiome. Mol Nutr Food Res. (2020) 64:e2000426. doi: 10.1002/mnfr.202000426
24. Rudzki, L, Stone, TW, Maes, M, Misiak, B, Samochowiec, J, and Szulc, A. Gut microbiota-derived vitamins - underrated powers of a multipotent ally in psychiatric health and disease. Prog Neuro-Psychopharmacol Biol Psychiatry. (2021) 107:110240. doi: 10.1016/j.pnpbp.2020.110240
25. Palumbo, AM, Kirkwood, D, Borkhoff, CM, Keown-Stoneman, CDG, Muraca, GM, Fuller, A, et al. Validation of parent-reported gestational age categories for children less than 6 years of age. Epidemiology. (2023) 34:767–73. doi: 10.1097/EDE.0000000000001645
26. Hosseinzadeh, P, Mohseni, M, and Minaie, A. Vitamin D status in children with forearm fractures: incidence and risk factors. J Am Acad Orthop Surg Glob Res Rev. (2020) 4:e20.00150–5. doi: 10.5435/JAAOSGlobal-D-20-00150
27. Wang, C, Li, H, Huo, L, Wang, Q, Zhang, T, He, X, et al. Serum 25-Hydroxyvitamin D levels in type 2 diabetes patients in North China: seasonality and the association between vitamin D status and glycosylated hemoglobin levels. Int J Clin Pract. (2023) 2023:1–10. doi: 10.1155/2023/4151224
Keywords: children, vitamin status, age, sex, season
Citation: Li X, Chen N, Guo L, Luan Y, Jin Z, Yang J and Li T (2025) The nutritional levels and status of vitamins among children in Henan, China. Front. Nutr. 12:1657153. doi: 10.3389/fnut.2025.1657153
Edited by:
Aslam Khan, Riphah International University, PakistanReviewed by:
Phil Fischer, Mayo Clinic, United StatesKun Huang, Huazhong University of Science and Technology, China
Copyright © 2025 Li, Chen, Guo, Luan, Jin, Yang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhipeng Jin, amluemhpcGVuZzU1QDE2My5jb20=; Tiewei Li, bGl0aWV3ZWluZEAxNjMuY29t; Junmei Yang, eWFuZ2p1bm1laTc2ODNAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Xiaojuan Li†
Xiaojuan Li† Yusheng Luan
Yusheng Luan Junmei Yang
Junmei Yang Tiewei Li
Tiewei Li