- 1Department of Health Management, College of Public Health, Zhengzhou University, Zhengzhou, Henan, China
- 2Grassroots Health and Health Department, Health Commission of Henan Province, Zhengzhou, Henan, China
- 3Henan Key Laboratory for Health Management of Chronic Diseases, Central China Fuwai Hospital, Central China Fuwai Hospital of Zhengzhou University, Zhengzhou, Henan, China
- 4Department of Science and Laboratory Technology, Dar es salaam Institute of Technology, Dar es Salaam, Tanzania
Introduction: While adopting multiple healthy lifestyle behaviors has been shown to significantly reduce the risk of ischemic stroke (IS) in the general adult population, there is limited evidence on whether such benefits extend to older adults with hypertension. This study aimed to examine how a combination of modifiable healthy lifestyle behaviors is associated with the risks of IS among hypertensive patients aged 65 years and older.
Methods: This population-based study was conducted in Jia County, Henan Province, from 1 July, 2023 to 31 August, 2023. Data on participants’ lifestyles were collected through structured, face-to-face interviews. A composite lifestyle score was generated using five modifiable behaviors: non-smoking, non-drinking, ideal sleep duration, adherence to a healthy diet, and engagement in regular physical activity. The relationship between lifestyle and IS was determined using logistic regression models, with results presented as odds ratios (ORs) and 95% confidence intervals (CIs). To identify optimal interaction patterns among multiple factors, we applied generalized multifactor dimensionality reduction (GMDR) analysis.
Results: A total of 17,747 participants were included (42.11% male, mean age 73.39 years), 31.20% of whom had a history of IS. In multivariable-adjusted models, maintaining a healthy diet, never smoking, getting adequate sleep, and never drinking were each independently associated with a lower risk of IS. There was a clear inverse relationship between the number of healthy lifestyle behaviors and IS risk. After adjusting for covariates, participants who adopted all five healthy lifestyle behaviors had the lowest prevalence of IS, with a 58.5% reduction compared to those who reported none of the healthy behaviors. For every additional point gained in the healthy lifestyle score, the risk of IS dropped by 11.2%. The GMDR analysis showed that sleep, diet, and smoking had the most significant interaction with the risk of IS.
Conclusion: Embracing healthy lifestyle habits can significantly lower the risk of IS among older adults with hypertension in China. These findings offer valuable guidance for designing targeted lifestyle interventions aimed at preventing stroke in this high-risk population.
1 Introduction
The global population is aging at a rapid pace, driven by increaing life expectancy and improved survival among older adults, largely attributable to advances in healthcare and broader socioeconomic development (1). By 2050, an estimated 20% of the global population will be aged 65 years and older, with approximately 80% of older adults residing in low- and middle-income countries, posing substantial public health challenges (2). In China, individuals aged 65 years and older currently account for 15.4% of the total population (3). The rapid aging of the population has been accompanied by a rise in chronic diseases such as hypertension, imposing a significant burden on health systems. Hypertension is a leading cause of cardiovascular disease and premature deaths worldwide, with its global prevalence estimated to exceed 40% (4). In China, an estimated 245 million people are living with hypertension, with its prevalence increasing markedly with age and affecting more than half of those aged 65 years and older (5). Developing effective strategies to address health issues related to population aging has therefore become both urgent and unavoidable.
Ischemic stroke (IS) poses a substantial burden on global health and remains the second leading cause of death worldwide, posing a serious threat to health and quality of life (6). By 2030, the global age-standardized IS incidence rate is projected to rise to 89.32 per 100,000 persons (6). The prevalence of stroke in China is severe and continues to increase. Currently, the average age of stroke patients has reached 65 years, and IS accounts for 81.90% of all stroke events (7). Emerging evidence indicates that older adults with hypertension exhibit a substantially greater risk of cardio-cerebrovascular disease (8). Another study showed that blood pressure was independently associated with IS risk and served as a significant contributing factor for IS recurrence (9). Therefore, it is essential to constantly emphasize the significance of preventing IS among hypertensive patients aged 65 and older.
Evidence from previous studies has identified several factors that may help lower the risk of IS, with growing attention focused on lifestyle choices as key modifiable behaviors in prevention efforts (10, 11). Healthy lifestyles can significantly reduce the risk of IS by strengthening the body’s immunity and achieving optimal metabolic function. Compelling evidence suggested that adhering to healthy lifestyles, such as not smoking, avoiding alcohol, getting adequate sleep, engaging in regular physical activity, and following a healthy diet, can significantly lower the risk of IS (12, 13). This is attributable to the fact that healthy lifestyles can enhance the body’s immunity and optimize metabolic functions, thereby significantly reducing the risk of IS. In addition, up to 90% of stroke cases may be prevented in the early stages, with half of these cases attributable to lifestyle modification. A study found that individuals who followed none or only one healthy lifestyle behavior had a 66% higher risk of stroke compared to those who adopted three or four healthy lifestyle practices (14). Nonetheless, a significant research gap persists concerning elderly patients with hypertension, especially those aged 65 years and above. The effect of both individual and composite lifestyle behaviors in this demographic on the risk of IS has yet to be thoroughly investigated.
Our study aimed to examine the effect of both individual and combined lifestyle behaviors on IS risk in hypertensive adults aged 65 years and older. Additionally, we aimed to identify significant and optimal multifactorial interaction patterns among five key lifestyle factors using generalized multifactor dimensionality reduction (GMDR). The findings of this study are expected to offer valuable insights into the development of targeted lifestyle interventions for older hypertensive individuals, ultimately supporting improved health outcomes and wellbeing in this population.
2 Materials and methods
2.1 Study design and participants
We used data from a cross-section survey of 18,963 patients with primary hypertension aged 65 and above in Jia County, Henan Province, from 1 July to 31 August, 2023, selected through a cluster sampling method. All recruited participants were drawn from the National Basic Public Health Service Project (NBPHSP) and had received a confirmed diagnosis from qualified medical professionals. Questionnaire information was obtained through face-to-face interviews. Participants were included in the study if they provided informed consent, completed the questionnaire, and underwent a physical examination conducted by professionally trained investigators. We excluded participants with missing information on healthy lifestyle behaviors (n = 679), missing physical examination data (n = 413), or missing information on the duration of hypertension (n = 316). After these exclusions, 17,747 participants remained for analysis. The flowchart of participant selection is shown in Figure 1. Investigators received training in face-to-face interviewing, physical measurement tools, and questionnaire quality control and passed the examination. The study was approved by the Zhengzhou University Medical Ethics Committee (Approval number: 2023-318).
2.2 Assessment of lifestyle behaviors
We assessed five modifiable lifestyle behaviors, including smoking, drinking, sleep, diet, and physical activity. As for smoking, participants were categorized as current smokers and never smokers, with never smokers defined as those who had never smoked or had quit smoking for at least 30 years (15). Never smoking was defined as a healthy lifestyle. Participants’ alcohol consumption was categorized as current drinkers or never drinkers, with never drinking defined as having a healthy lifestyle (16). Dietary information was collected by recording how frequently participants consumed three key food items: fruits, vegetables, and red meat. A healthy diet was defined as meeting the following three criteria: fruits: ≥7times/week; vegetables: ≥7times/week; red meats: ≤6 times/week. Sleep information was based on participants’ reported actual sleep duration per night. An ideal sleep duration, defined as 6 to 8 h per night, was considered a healthy lifestyle behavior, in line with cutoffs commonly used in previous studies to ensure comparability (17). For physical activity, data on the weekly frequency and duration of exercise were collected. Regular exercise was defined as engaging in at least 3.5 h/week of moderate to vigorous–intensity exercise (≥30 min/day) as a healthy lifestyle, in accordance with the WHO guidelines.
We evaluated the association of each single lifestyle behavior with the risk of IS. For further investigation of the combined effect of lifestyle behaviors on the risk of IS, the participant received a score of 1 if they met the criterion for healthy lifestyle behavior and a score of 0 if otherwise. The scores on all lifestyle components were summed to yield a healthy lifestyle score ranging from 0 to 5, with a higher index indicating a healthier lifestyle.
2.3 Outcome
In this study, the prevalence of IS in this population was obtained from the NBPHSP. The classification of diseases was adopted in the International Classification of Diseases (ICD-10), and IS [codes I63] was used as the outcome variable in this study to investigate whether and how lifestyle influenced the risk of IS in hypertensive patients.
2.4 Covariates
Based on the existing literature, we identified a series of covariates. Sociodemographic information included age based on median (≤72 years, >72 years), sex (male or female), ethnicity (Han or Hui), marital status (married, widowed, or divorced/single/other status), years of education (≤6 year, 7–9years, ≥10years), and yearly household income (≤CNY¥30,000, >CNY¥30,000).
Health-related covariates were also collected, including hypertension duration, body mass index (BMI), and blood pressure. All participants’ height and weight were measured twice following a standard protocol, and the mean was used for analysis. BMI was weight divided by height squared. According to Chinese BMI classification standards, a normal body mass index (BMI) was defined as ranging from 18.5 to 23.99 kg/m2, while values outside this range were considered abnormal (18). Blood pressure was measured after the participant sat still for 5 min. The measurement of blood pressure was repeated three times, and the average value was adopted as the blood pressure. In accordance with the Chinese guidelines for the management of hypertension, hypertension was defined as having a systolic blood pressure (SBP) ≥140 mmHg (18.6 kPa) and/or a diastolic blood pressure (DBP) ≥90 mmHg (12.0 kPa) in the absence of antihypertensive medication, or having a documented history of hypertension, or currently taking antihypertensive drugs (19). All measurements were carried out by trained staff using standard instruments.
2.5 Statistical analysis
Characteristics of participants were described as counts (percentages) for categorical variables. Missing values are summarized in Supplementary Table S1. A multiple imputation chain-equation was applied to address missing demographic data. The chi-squared test was used to compare the differences in categorical variables between the IS group and non-ischemic stroke group. A binary logistic regression model was deployed to examine the associations between the prevalence of IS and each sociodemographic factor, lifestyle behaviors, and the healthy lifestyle score. Three models were used to examine the associations between healthy lifestyle scores and the prevalence of IS. Model 1 included no covariate adjustments. Model 2 was adjusted for sociodemographic factors, including age, sex, ethnicity, marital status, years of education, and household income. Model 3 further accounted for clinical variables such as the duration of hypertension, body mass index (BMI), and blood pressure. We implemented the trend test by adopting the categorical variable of a healthy lifestyle as a continuous variable. Using GMDR, the study identified statistically significant and optimal interaction models among the five healthy lifestyle behaviors. Parameters consisted of the sign test p-value, cross-validation consistency (CVC), and test balance accuracy (TBA). The optimal model was determined to be the one with the highest TBA, a low symbolic test p-value (≤0.05), and the highest CVC score.
A subgroup analysis based on participants’ age was conducted to explore the differences in the effect of lifestyle scores on health outcomes in different subgroups. In each subgroup, the reference group was set as the participants with the least healthy lifestyle behavior. To check the robustness of the results, we performed two sensitivity analyses. First, we redefined physical exercise; at least 150 min of moderate or 75 min of vigorous activity per week was considered a healthy behavior according to American adult physical activity guidelines (20). Second, as some studies treat BMI as a lifestyle factor (21), we incorporated BMI into the lifestyle score to re-evaluate the association between combined lifestyle factors and the risk of IS. All statistical analyses were conducted with SPSS software (version 26), R software (version 4.3.3), and GMDR (version 1.0). A two-sided p-value of < 0.05 was considered statistically significant.
3 Results
3.1 Characteristics of study participants
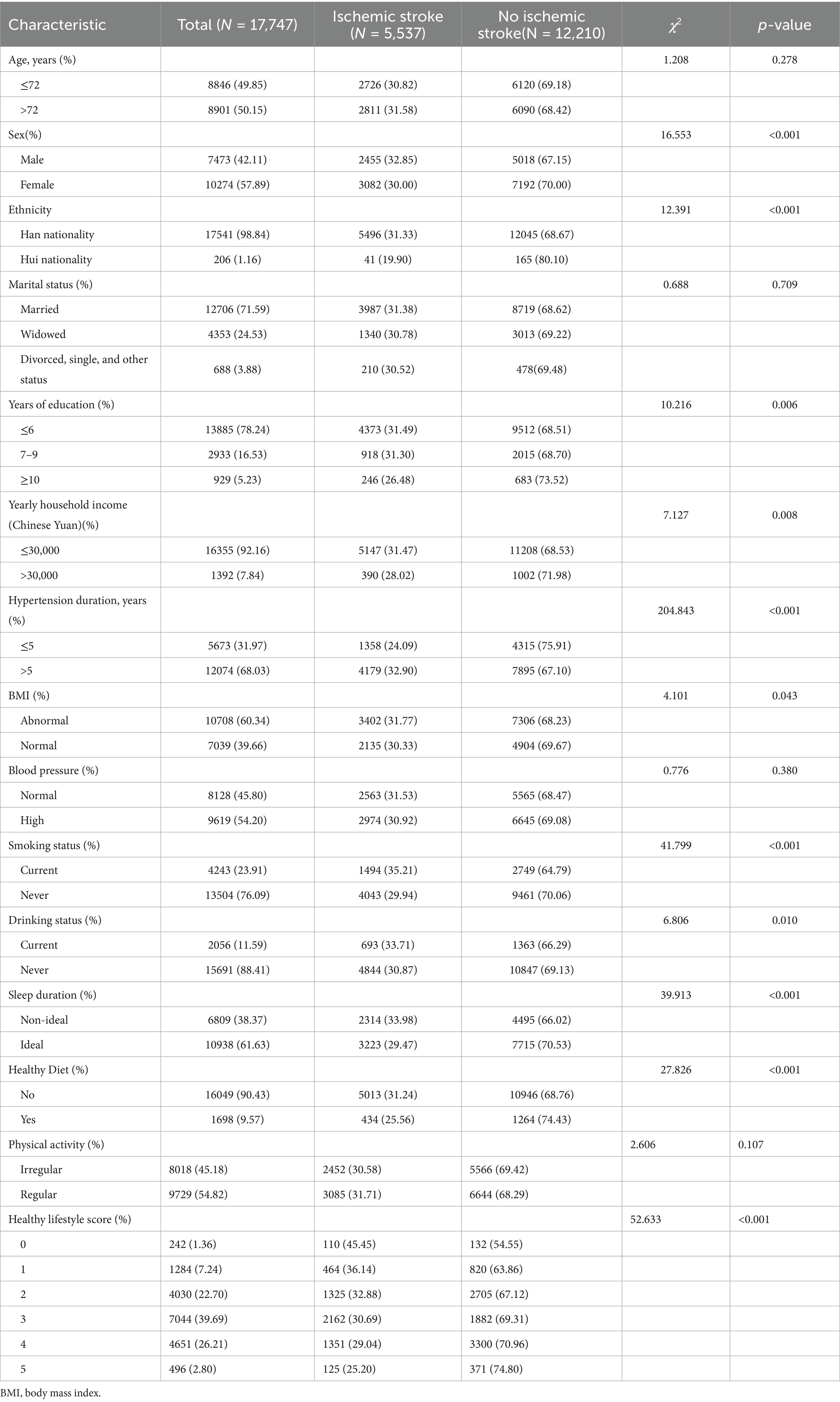
A total of 17,747 participants were screened for eligibility (Figure 1). Table 1 presents the participants’ demographic characteristics stratified by IS status. The median age of the participants was 72 years, and 42.11% were male. Among all participants with hypertension, 5,537 (31.20%) of them had a history of IS. The prevalence of IS was significantly higher among men (32.85%), individuals with lower income (31.47%), participants with >5 years of hypertension (32.90%), and participants with an abnormal BMI (31.77%) (p < 0.001). No statistically significant differences were observed with respect to age, marital status, or blood pressure (p > 0.05).
A total of 13,504 (76.09%) participants reported never smoking, 15,691 (88.41%) participants reported never drinking, 10,938 (61.63%) participants reported ideal sleep duration, 1,698 (9.57%) participants reported a healthy diet, and 9,729 (54.82%) participants reported regular physical activity. The proportions of participants with a healthy lifestyle score of 0, 1, 2, 3, 4, and 5 were 242 (1.36%), 1,284 (7.24%), 4,030 (22.70%), 7,044 (39.69%), 4,651 (26.21%), and 496 (2.80%), respectively.
3.2 Associations of demographic information with IS
The multivariate regression analysis indicated that being female (OR = 0.876; 95% CI = 0.822–0.934), belonging to the Hui ethnic group (OR = 0.545; 95% CI = 0.386–0.768), having a higher income level (annual income >30,000) (OR = 0.848; 95% CI = 0.751–0.957), and having a normal BMI (OR = 0.935; 95% CI = 0.876–0.998) were associated with a protective effect against IS. Conversely, a hypertension duration of more than 5 years (OR = 1.682; 95% CI = 1.566–1.807) was associated with an increased risk of IS. Additionally, educational attainment appeared to have a potential impact on the risk of IS (Figure 2).
3.3 Associations of individual healthy lifestyle behaviors with the risk of IS
The findings indicated that, among lifestyle factors, maintaining a healthy diet had the strongest protective effect against IS (OR = 0.736; 95% CI = 0.657–0.825), followed by never smoking (OR = 0.786; 95% CI = 0.731–0.846), achieving an ideal sleep duration (OR = 0.812; 95% CI = 0.761–0.866), and never drinking (OR = 0.878; 95% CI = 0.797–0.968). A healthy diet, compared with insufficient intake of fruits, vegetables, and meat; never smoking, compared with current smoking; ideal sleep duration, compared with sleeping more than 8 h or less than 6 h; and never drinking, compared with current drinking, emerged as protective factors against the risk of IS in hypertensive patients (Figure 2; Supplementary Table S2).
3.4 Associations of the healthy lifestyle score with IS
In the analysis where the five healthy lifestyle behaviors were considered jointly using a healthy lifestyle score, a higher score was significantly associated with a lower risk of IS, showing a non-linear dose-response relationship after adjusting for confounders (all p < 0.05, Table 2). After adjusting for the potential confounding factors in model 2 (age, gender, nation, marital status, education, and household income), the prevalence of IS was found to be lowest when the score of healthy lifestyle behaviors reached 5, with a decrease of 57.9% (OR = 0.85; 95% CI = 0.303–0.584) compared to a healthy lifestyle behavior score of 0. In model 3, which additionally controlled for hypertension duration, BMI, and blood pressure, the results remained robust. Compared to participants who had a healthy lifestyle behavior score of 0, the risk of IS decreased by 32.3% (OR = 0.677; 95% CI = 0.512–0.896) among participants with a healthy lifestyle behavior scored of 1, 40.1% (OR = 0.599; 95% CI = 0.459–0.781) among participants who had a healthy lifestyle behavior scored of 2, 45.7% (OR = 0.543; 95% CI = 0.417–0.708) among participants who had a healthy lifestyle behavior scored of 3, 49.7% (OR = 0.503; 95% CI = 0.386–0.661) among participants who had a healthy lifestyle behavior scored of 4, and 58.5% (OR = 0.415; 95% CI = 0.298–0.579) among participants who had a healthy lifestyle behavior scored of 5 (Table 2).
Furthermore, each point gained in the healthy lifestyle score was accompanied by an 11.2% reduction in the risk of IS in hypertensive patients (OR = 0.888; 95% CI = 0.860–0.916). As shown in Supplementary Table S2, a higher healthy lifestyle score was inversely associated with the risk of stroke.
3.5 High-Order Interaction
The GMDR analysis was conducted to explore potential interactions among the five healthy lifestyle factors in this study. After constructing higher-order interaction models, the three-factor model, including sleep, diet, and smoking, showed a significant replacement test (p < 0.05), and a CVC of 10/10, with the highest balanced accuracy of 0.5350, making it the optimal model (Table 3; Supplementary Figure S1). These results suggest that sleep, diet, and smoking have the strongest interaction effect on the risk of cerebral infarction.
3.6 Subgroup and sensitivity analyses
Supplementary Table S3 shows stratification by age group. The inverse associations between multiple healthy lifestyle behaviors and the risk of IS remained significant among both age groups. Two sensitivity analyses were conducted to examine the relationship between the healthy lifestyle score and the risk of IS in hypertensive patients. The results indicated that the findings from each sensitivity analysis were basically consistent with the primary analysis results (Supplementary Tables S4, S5).
4 Discussion
In our study, we observed that approximately 31.20% of the 17,747 participants aged 65 years and above experienced IS. Our findings revealed that adhering to healthy lifestyles (never smoking, never drinking, ideal sleep duration, and a healthy diet) was associated with a significantly reduced risk of IS, and a healthy diet had the greatest effect on reducing the risk of IS. The prevalence of IS decreased by 58.5% among individuals with a healthy lifestyle behavior score of 5 compared to those with a score of 0. In addition, each additional lifestyle factor was associated with an 11.2% lower prevalence of IS.
Our findings are consistent with previous studies, showing that the risk of IS decreases with increasing scores of healthy lifestyle behaviors (12, 22). A representative population-based prospective cohort study of 60-year-olds showed a 61% lower risk of cardiovascular disease among those with 6–7 healthy behaviors than among those with 0–2 healthy lifestyles (22). Similarly, another prospective cohort study revealed that adopting a healthier lifestyle was associated with a reduced risk of developing IS (23). The results of our study further support the importance of continuous exploration and intensive healthy lifestyle management, with a view to guiding the health management of this population more accurately, reducing the development of cerebral infarction events, and improving overall population health.
In the present study, adhering to the recommendations of ideal sleep duration was shown to have a protective effect on IS in our population. Findings from meta-analyses have shown a statistically significant linear association between short (less than 6 h) and long (more than 9 h) sleep duration and cardiovascular disease and mortality (24, 25). We also observed a higher prevalence of IS among individuals who smoked or consumed alcohol compared to those who had never smoked or never drank. Previous studies have found that smoking and drinking increased the risk of IS, and lifestyle modifications have the potential to reduce IS risk (26, 27), which is in line with our study.
In our study, only 1,698 (9.6%) participants adhered to a healthy diet, which is quite low and consistent with previous studies (28). Previous multiple studies have confirmed that dietary patterns are closely associated with the risk of developing IS. Specifically, high consumption of processed meats, unprocessed red meats, or poultry was significantly related to an increased risk of IS (29). Moreover, a study involving 23,797 participants clearly demonstrated that a high-quality dietary pattern characterized by high intake of fruits and vegetables and low intake of red meat and processed meats was associated with a lower risk of IS (30). Basic medical research suggested that vegetables and fruits are rich in dietary fiber, phytochemicals, vitamins, and other substances. These components can not only inhibit the oxidation of low-density lipoprotein (LDL), thereby reducing atherosclerotic plaques, but also reduce the release of inflammatory factors, inhibit platelet aggregation, prevent thrombosis, and thus slow down the occurrence and development of cerebral infarction (31–33). The results of this study suggested that we should pay close attention to the popularization of dietary knowledge in this group and further optimize the dietary guidelines according to their nutritional needs and dietary characteristics so as to improve their dietary health level and reduce the risk of IS.
However, no significant association was observed between regular physical activity and the risk of IS in this study. The relationship between the intensity of physical activity and the risk of cardio-cerebrovascular disease was controversial in the previous study. A longitudinal study involving 49,060 adults indicated that 150–300 min/week of moderate-intensity physical activity or more was significantly associated with decreased risk of stroke; however, 75–150 min/week of vigorous-intensity physical activity was found to be associated with few further benefits, and it may even weaken the cardiovascular benefits (34). Prestroke physical activity was associated with milder stroke; both light physical activity (such as walking for at least 4 h/week) and moderate physical activity (2–3 h/week) appeared to be beneficial(35). Moreover, another study reported no association between self-reported moderate-to-vigorous physical activity, accelerometer-based physical activity, sedentary behavior, and IS (36). This discrepancy may be due to the insufficient consideration of other potential confounding factors, such as hereditary factors or comorbidity, which can significantly influence IS (16). Additionally, short-term changes in physical activity may not be sufficient to have a significant effect on IS.
Previous GMDR studies focused on the effects of gene-gene and gene-environment interactions on disease (37). To the best of our knowledge, this is the first study to use GMDR to explore possible higher-order interactions between different lifestyle factors and found that the three factors of sleep, diet, and smoking interacted with each other and had the strongest interactions. Our analysis identified a significant three-way interaction involving sleep, diet, and smoking, which exhibited the strongest effect among the models tested. Methodologically, the GMDR approach, utilizing cross-validation and permutation testing, strengthens the reliability of these findings by mitigating the risk of overfitting, a common limitation in traditional additive or multiplicative interaction models (38). These findings deepen our understanding of the complex relationship between health behaviors and IS risk. The significant interplay observed among these modifiable factors underscores that public health interventions must evolve from promoting isolated behavioral changes toward implementing integrated, multi-dimensional strategies. For instance, simultaneously addressing sleep quality, dietary habits, and smoking cessation may yield synergistic effects, amplifying the benefits of primary prevention beyond what could be achieved by targeting each factor individually. Furthermore, our results aid in identifying population subgroups with specific risk profiles, enabling the design of targeted and personalized preventive measures. This approach is anticipated to enhance the precision, efficiency, and overall effectiveness of resource allocation in health programs targeting aging populations with hypertension.
To our knowledge, this is the first study to comprehensively examine health lifestyle behaviors in relation to the prevalence of IS among hypertensive participants aged 65 years and above, emphasizing the potential role of healthy lifestyles in IS.
Moreover, owing to the large, population-based sample, the findings are likely to be generalizable to individuals with primary hypertension residing in low-and middle-income countries. This study also had several limitations. First, the cross-sectional design of the study restricted the exploration of changes in lifestyles or the determination of causality, despite providing insights into the prevalence of IS among older hypertensive patients and its correlation with lifestyle behaviors. Second, the reliance on self-reported information about lifestyle behaviors may introduce information bias. The accuracy of responses from elderly participants with hypertension might be affected by memory decline, despite efforts to mitigate this through questionnaire design and interviewer assistance. Third, despite adjusting for recognized potential factors, the possibility of unmeasured confounders and reverse causation cannot be excluded.
5 Conclusion
In conclusion, our findings suggest that a higher healthy lifestyle score, including never smoking, never drinking, ideal sleep duration, a healthy diet, and regular physical activity, is associated with a substantially lower risk of IS among hypertensive patients aged 65 years and above. In particular, sleep, diet, and smoking emerged as the most significant interactive influences on IS risk. These insights provide important evidence to inform the development of tailored guidelines and public health interventions aimed at lowering stroke risk through lifestyle modification in this high-risk demographic.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Zhengzhou University Medical Ethics Committee (number:2023-318). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
JW: Writing – original draft, Funding acquisition. XJ: Software, Writing – original draft, Methodology, Funding acquisition, Investigation. WQ: Methodology, Investigation, Writing – review & editing. LZ: Supervision, Writing – review & editing, Formal analysis, Investigation. XG: Software, Investigation, Methodology, Writing – review & editing. ND: Investigation, Writing – review & editing. RL: Investigation, Writing – review & editing, Project administration. QZ: Investigation, Writing – review & editing, Project administration. YM: Project administration, Investigation, Writing – review & editing, Supervision. CT: Writing – review & editing. BY: Investigation, Writing – review & editing, Validation, Funding acquisition.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the Henan Provincial Major Science and Technology Project (241100310200), the Humanities and Social Science Fund project of the Ministry of Education, China (24YJAZH174), the Natural Science Foundation of Henan Province (252300423905), the Graduate Education Research Project of Zhengzhou University (YJSJY2025152), the General Projects of Humanities and Social Sciences Research in Henan Provincial Universities (2026-ZDJH-148), and the 2025 Graduate Independent Innovation Project of Zhengzhou University (20250432).
Acknowledgments
We are deeply grateful to all participants and their families for their contributions to this study. All authors confirm that this manuscript is a transparent and honest account of the research conducted. This research builds upon our previous study titled “Association between lifestyle behaviors and body mass index with blood pressure classifications among older adults with hypertension in China”. That earlier research examined how lifestyle behaviors and body mass index, along with their potential interactions, were associated with the severity of blood pressure classifications among older adults with hypertension. In contrast, the current submission focuses on examining how a combination of modifiable healthy lifestyle behaviors is associated with the risks of ischemic stroke (IS) among hypertensive patients aged 65 and older. We also used the generalized multifactor dimensionality reduction (GMDR) analysis to identify the best interaction patterns among multiple factors. The study methods are detailed in Section 2, “Materials and Methods”.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2025.1677786/full#supplementary-material
References
1. Partridge, L, Deelen, J, and Slagboom, PE. Facing up to the global challenges of ageing. Nature. (2018) 561:45–56. doi: 10.1038/s41586-018-0457-8
2. DDogra, S, Dunstan, DW, Sugiyama, T, Stathi, A, Gardiner, PA, and Owen, N. Active aging and public health: evidence, implications, and opportunities. Annu Rev Public Health. (2022) 43:439–59. doi: 10.1146/annurev-publhealth-052620-091107
3. National Bureau of Statistics of China E. coli. (2024) Available online at: https://www.gov.cn/lianbo/bumen/202402/content_6934935.htm. (Accessed February 29, 2024).
4. Mills, KT, Stefanescu, A, and He, J. The global epidemiology of hypertension. Nat Rev Nephrol. (2020) 16:223–37. doi: 10.1038/s41581-019-0244-2
5. Wang, JG, Zhang, W, Li, Y, and Liu, L. Hypertension in China: epidemiology and treatment initiatives. Nat Rev Cardiol. (2023) 20:531–45. doi: 10.1038/s41569-022-00829-z
6. Pu, L, Wang, L, Zhang, R, Zhao, T, Jiang, Y, and Han, L. Projected global trends in ischemic stroke incidence, deaths and disability-adjusted life years from 2020 to 2030. Stroke. (2023) 54:1330–9. doi: 10.1161/strokeaha.122.040073
7. Tu, WJ, and Wang, LD. China stroke surveillance report 2021. Mil Med Res. (2023) 10:33. doi: 10.1186/s40779-023-00463-x
8. Cao, X, Zhao, Z, Kang, Y, Tian, Y, Song, Y, Wang, L, et al. The burden of cardiovascular disease attributable to high systolic blood pressure across China, 2005-18: a population-based study. Lancet Public Health. (2022) 7:e1027–40. doi: 10.1016/s2468-2667(22)00232-8
9. Cipolla, MJ, Liebeskind, DS, and Chan, SL. The importance of comorbidities in ischemic stroke: impact of hypertension on the cerebral circulation. J Cereb Blood Flow Metab. (2018) 38:2129–49. doi: 10.1177/0271678x18800589
10. Zhu, X, Zhang, F, Luo, Z, Liu, H, Lai, X, Hu, X, et al. Effect of the number of unhealthy lifestyles in middle-aged and elderly people on hypertension and the first occurrence of ischemic stroke after the disease. Front Cardiovasc Med. (2023) 10:1152423. doi: 10.3389/fcvm.2023.1152423
11. Zhang, C, Li, M, Yang, M, Lin, J, Huang, J, Lin, Y, et al. Plasma metabolites, systolic blood pressure, lifestyle, and stroke risk: a prospective cohort study. Int J Stroke. (2025) 20:486–96. doi: 10.1177/17474930241293408
12. Wu, J, Feng, Y, Zhao, Y, Guo, Z, Liu, R, Zeng, X, et al. Lifestyle behaviors and risk of cardiovascular disease and prognosis among individuals with cardiovascular disease: a systematic review and meta-analysis of 71 prospective cohort studies. Int J Behav Nutr Phys Act. (2024) 21:42. doi: 10.1186/s12966-024-01586-7
13. Besseau, S, Sartori, E, Larnier, P, Paillard, F, Laviolle, B, and Mahé, G. Impact of dietary intervention on eating behavior after ischemic stroke. Front Nutr. (2023) 10:1067755. doi: 10.3389/fnut.2023.1067755
14. Rutten-Jacobs, LC, Larsson, SC, Malik, R, Rannikmäe, K, Sudlow, CL, Dichgans, M, et al. Genetic risk, incident stroke, and the benefits of adhering to a healthy lifestyle: cohort study of 306 473 UK Biobank participants. BMJ. (2018) 363:k4168. doi: 10.1136/bmj.k4168
15. Zhu, M, Wang, T, Huang, Y, Zhao, X, Ding, Y, Zhu, M, et al. Genetic risk for overall cancer and the benefit of adherence to a healthy lifestyle. Cancer Res. (2021) 81:4618–27. doi: 10.1158/0008-5472
16. Boehme, AK, Esenwa, C, and Elkind, MS. Stroke risk factors, genetics, and prevention. Circ Res. (2017) 120:472–95. doi: 10.1161/circresaha.116.308398
17. Guasch-Ferré, M, Li, Y, Bhupathiraju, SN, Huang, T, Drouin-Chartier, JP, Manson, JE, et al. Healthy lifestyle score including sleep duration and cardiovascular disease risk. Am J Prev Med. (2022) 63:33–42. doi: 10.1016/j.amepre.2022.01.027
18. Chen, Y, Peng, Q, Yang, Y, Zheng, S, Wang, Y, and Lu, W. The prevalence and increasing trends of overweight, general obesity, and abdominal obesity among Chinese adults: a repeated cross-sectional study. BMC Public Health. (2019) 19:1293. doi: 10.1186/s12889-019-7633-0
19. Wang, Z, Chen, Z, Zhang, L, Wang, X, Hao, G, Zhang, Z, et al. Status of hypertension in China: results from the China hypertension survey, 2012-2015. Circulation. (2018) 137:2344–56. doi: 10.1161/circulationaha.117.032380
20. Piercy, KL, Troiano, RP, Ballard, RM, Carlson, SA, Fulton, JE, Galuska, DA, et al. The Physical Activity Guidelines for Americans. JAMA. (2018) 320:2020–8. doi: 10.1001/jama.2018.14854
21. Lv, J, Yu, C, Guo, Y, Bian, Z, Yang, L, Chen, Y, et al. Adherence to healthy lifestyle and cardiovascular diseases in the Chinese population. J Am Coll Cardiol. (2017) 69:1116–25. doi: 10.1016/j.jacc.2016.11.076
22. Carlsson, AC, Wändell, PE, Gigante, B, Leander, K, Hellenius, ML, and de Faire, U. Seven modifiable lifestyle factors predict reduced risk for ischemic cardiovascular disease and all-cause mortality regardless of body mass index: a cohort study. Int J Cardiol. (2013) 168:946–52. doi: 10.1016/j.ijcard.2012.10.045
23. Myint, PK, Luben, RN, Wareham, NJ, Bingham, SA, and Khaw, KT. Combined effect of health behaviours and risk of first ever stroke in 20,040 men and women over 11 years’ follow-up in Norfolk cohort of European Prospective Investigation of Cancer (EPIC Norfolk): prospective population study. BMJ. (2009) 338:b349. doi: 10.1136/bmj.b349
24. Itani, O, Jike, M, Watanabe, N, and Kaneita, Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med. (2017) 32:246–56. doi: 10.1016/j.sleep.2016.08.006
25. Jike, M, Itani, O, Watanabe, N, Buysse, DJ, and Kaneita, Y. Long sleep duration and health outcomes: a systematic review, meta-analysis and meta-regression. Sleep Med Rev. (2018) 39:25–36. doi: 10.1016/j.smrv.2017.06.011
26. Harshfield, EL, Georgakis, MK, Malik, R, Dichgans, M, and Markus, HS. Modifiable lifestyle factors and risk of stroke: a mendelian randomization analysis. Stroke. (2021) 52:931–6. doi: 10.1161/strokeaha.120.031710
27. Millwood, IY, Walters, RG, Mei, XW, Guo, Y, Yang, L, Bian, Z, et al. Conventional and genetic evidence on alcohol and vascular disease aetiology: a prospective study of 500 000 men and women in China. Lancet. (2019) 393:1831–42. doi: 10.1016/s0140-6736(18)31772-0
28. Fu, L, Shi, Y, Li, S, Jiang, K, Zhang, L, Wen, Y, et al. Healthy diet-related knowledge, attitude, and practice (KAP) and related socio-demographic characteristics among middle-aged and older adults: a cross-sectional survey in Southwest China. Nutrients. (2024) 16. doi: 10.3390/nu16060869
29. Zhong, VW, Van Horn, L, Greenland, P, Carnethon, MR, Ning, H, Wilkins, JT, et al. Associations of processed meat, unprocessed red meat, poultry, or fish intake with incident cardiovascular disease and all-cause mortality. JAMA Intern Med. (2020) 180:503–12. doi: 10.1001/jamainternmed.2019.6969
30. Johansson, A, Acosta, S, Mutie, PM, Sonestedt, E, Engström, G, and Drake, I. Components of a healthy diet and different types of physical activity and risk of atherothrombotic ischemic stroke: a prospective cohort study. Front Cardiovasc Med. (2022) 9:993112. doi: 10.3389/fcvm.2022.993112
31. Ahmadzadeh, AM, Pourbagher-Shahri, AM, and Forouzanfar, F. Neuroprotective effects of phytochemicals through autophagy modulation in ischemic stroke. Inflammopharmacology. (2025) 33:729–57. doi: 10.1007/s10787-024-01606-9
32. Evans, CEL. Dietary fibre and cardiovascular health: a review of current evidence and policy. Proc Nutr Soc. (2020) 79:61–7. doi: 10.1017/s0029665119000673
33. Xu, Q, Qian, X, Sun, F, Liu, H, Dou, Z, and Zhang, J. Independent and joint associations of dietary antioxidant intake with risk of post-stroke depression and all-cause mortality. J Affect Disord. (2023) 322:84–90. doi: 10.1016/j.jad.2022.11.013
34. Xiang, B, Zhou, Y, Wu, X, and Zhou, X. Association of device-measured physical activity with cardiovascular outcomes in individuals with hypertension. Hypertension. (2023) 80:2455–63. doi: 10.1161/hypertensionaha.123.21663
35. Reinholdsson, M, Palstam, A, and Sunnerhagen, KS. Prestroke physical activity could influence acute stroke severity (part of PAPSIGOT). Neurology. (2018) 91:e1461–7. doi: 10.1212/wnl.0000000000006354
36. Bahls, M, Leitzmann, MF, Karch, A, Teumer, A, Dörr, M, Felix, SB, et al. Physical activity, sedentary behavior and risk of coronary artery disease, myocardial infarction and ischemic stroke:a two-sample Mendelian randomization study. Clin Res Cardiol. (2021) 110:1564–73. doi: 10.1007/s00392-021-01846-7
37. Galimova, E, Rätsep, R, Traks, T, Kingo, K, Escott-Price, V, and Kõks, S. Interleukin-10 family cytokines pathway: genetic variants and psoriasis. Br J Dermatol. (2017) 176:1577–87. doi: 10.1111/bjd.15363
Keywords: elderly, ischemic stroke, hypertensive patients, healthy lifestyle, GMDR
Citation: Wu J, Jiao X, Qi W, Zhao L, Guo X, Dai N, Liu R, Zhao Q, Miao Y, Tarimo CS and Ye B (2025) Association between healthy lifestyle and the risk of ischemic stroke among elderly adults with hypertension: a cross-sectional study in China. Front. Nutr. 12:1677786. doi: 10.3389/fnut.2025.1677786
Edited by:
Sisi Cao, Mead Johnson Nutrition Company, United StatesReviewed by:
Yong Gan, Huazhong University of Science and Technology, ChinaFang Wang, Xuzhou Medical University, China
Copyright © 2025 Wu, Jiao, Qi, Zhao, Guo, Dai, Liu, Zhao, Miao, Tarimo and Ye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Beizhu Ye, eWViZWl6aHVAenp1LmVkdS5jbg==
 Jian Wu
Jian Wu Xiaoyu Jiao1
Xiaoyu Jiao1 Wenzhe Qi
Wenzhe Qi Lipei Zhao
Lipei Zhao Xinghong Guo
Xinghong Guo Qiuping Zhao
Qiuping Zhao Yudong Miao
Yudong Miao Beizhu Ye
Beizhu Ye