- 1Centre of Excellence for Korsakoff and Alcohol Related Cognitive Dysfunctions/Addiction Care, Vincent van Gogh Institute for Psychiatry, Venray, Netherlands
- 2Behavioural Science Institute, Radboud University Nijmegen, Nijmegen, Netherlands
- 3Kentalis Academy, Royal Dutch Kentalis, Sint-Michielsgestel, Netherlands
- 4Centre of Excellence for Neuropsychiatry, Vincent van Gogh Institute for Psychiatry, Venray, Netherlands
- 5Donders Institute for Brain, Cognition and Behaviour, Radboud University Nijmegen, Nijmegen, Netherlands
- 6Pompe Institute for Forensic Psychiatry, Pro Persona, Nijmegen, Netherlands
In mental health, the term dual-diagnosis is used for the co-occurrence of Substance Use Disorder (SUD) with another mental disorder. These co-occurring disorders can have a shared cause, and can cause/intensify each other’s expression. Forming a threat to health and society, dual-diagnosis is associated with relapses in addiction-related behavior and a destructive lifestyle. This is due to a persistent failure to control impulses and the maintaining of inadequate self-regulatory behavior in daily life. Thus, several aspects of executive functioning like inhibitory, shifting and updating processes seem impaired in dual-diagnosis. Executive (dys-)function is currently even seen as a shared underlying key component of most mental disorders. However, the number of studies on diverse aspects of executive functioning in dual-diagnosis is limited. In the present review, a systematic overview of various aspects of executive functioning in dual-diagnosis is presented, striving for a prototypical profile of patients with dual-diagnosis. Looking at empirical results, inhibitory and shifting processes appear to be impaired for SUD combined with schizophrenia, bipolar disorder or cluster B personality disorders. Studies involving updating process tasks for dual-diagnosis were limited. More research that zooms in to the full diversity of these executive functions is needed in order to strengthen these findings. Detailed insight in the profile of strengths and weaknesses that underlies one’s behavior and is related to diagnostic classifications, can lead to tailor-made assessment and indications for treatment, pointing out which aspects need attention and/or training in one’s self-regulative abilities.
Introduction
In dual-diagnosis, a Substance Use Disorder (SUD) co-occurs with another psychiatric condition such as psychotic disorder, mood disorder, anxiety disorder or personality disorder (Ziedonis and Brady, 2005). The Epidemiologic Catchment Area study, a comprehensive study of comorbidity, showed that the lifetime SUDs-rate in the general population was 17%, compared to 48% for persons with schizophrenia and 56% for persons with bipolar disorder (Regier et al., 1990). SUD is described in respectively 27 and 24% of patients with a depressive disorder or an anxiety disorder (Mueser et al., 2011; Dom et al., 2013). Studying a dual-diagnosis population is relevant, because of the threat that SUD and dual-diagnosis form to health, society, and the presence of relapses in addiction-related behavior and destructive lifestyles (De Jong et al., 2006; World Health Organisation [WHO], 2011). In clinical practice dual-diagnosis frequently occurs whereas ideally distinguishable single disorder groups are rare. Disorders in dual-diagnosis can have a shared cause, or can cause/intensify each other’s expression (Mueser et al., 1998). It is not always easy or possible to distinguish in which way the disorders causally interact or influence each other.
In most SUDs and other mental disorders self-regulatory behavior to manage daily life situations (involving work and relationships) falls short. Coping strategies are impaired, resulting in affective breakdowns (American Psychiatric Association, 2013). These frequently observed symptoms of psychiatric disorders point directly to deficits in executive functioning (EF) (among others: Barkley, 2001; Egger et al., 2007; Fernandez-Serrano et al., 2010; Wiers et al., 2012; Janssen, 2013; Luijten et al., 2013; Thoma and Daum, 2013; Goschke, 2014; Smith et al., 2014; Snyder et al., 2015). Executive (dis)-functioning is currently even seen as a shared underlying key component of most mental disorders (Egger et al., 2007; Janssen, 2013; Goschke, 2014; Snyder et al., 2015).
Executive functioning can be defined as all cognitive processes that regulate behavior in such a manner that it can be efficient and goal-orientated (Miyake et al., 2000; Barkley, 2001; Friedman et al., 2008; Miyake and Friedman, 2012; Snyder et al., 2015). Barkley (2001) describes EF as serving to “shift the control of behavior from the immediate context, social others, and the temporal now to self-regulation by internal representations regarding the hypothetical social future”. Miyake et al. (2000) introduced a model of EF in which three key EF aspects were presented. Firstly, Shifting concerns the switch of attention between tasks/operations and/or mental sets. Translated into daily life, it involves mental flexibility to repeatedly let go of irrelevant and/or inappropriate behaviors (for example, drug use or attention bias to alcohol related cues) and switch to more adequate/relevant behaviors (like sporting or switch of television-channel). Secondly, Updating involves the process of actively manipulating and monitoring relevant information in working memory, in order to keep track of information that is old and needs actualization (Miyake et al., 2000). For SUD, it can involve craving. When longing for drugs, a patient may usually tend to call the drug dealer. But, in a recent relapse prevention session he or she learned about putting the numbers of supporting friends in their phone. As this is the first moment of intense craving after the session and intrusive substance-use thoughts already come to mind, the patient has to monitor his or her own behavior and promptly update these thoughts by thinking of the newly learned information and healthier thoughts. He or she needs to replace the old information about the drug dealer with the new information regarding their supportive friend’s phone number. Inhibition is also needed in this scenario, and it is defined as the ability to inhibit dominant, automatic responses when necessary (Miyake et al., 2000; Barkley, 2001). Inhibition is, for instance, the suppression of approaching alcohol/drugs and/or calling the drug dealer. Shifting, updating and inhibition are all needed to some extent when making daily life decisions. For instance, when one wants to succeed in arriving at work on time tomorrow, thereby stopping destructive-avoidant behavior that was linked to one’s SUD lifestyle: (i) shifting is needed to get up earlier than before and to repeatedly let go of attention biases triggering late night out fantasies, (ii) inhibition is needed to prevent this late night ‘going out’ with friends by stopping yourself from drinking/using and going home, (iii) updating is involved in checking an alternative work-route, thereby avoiding and replacing the old, coffee-shop route that would trigger craving. The interplay between EF aspects can influence self-regulation in daily life by reducing problem-behavior and raising more goal-directed behavior. In addition, EF can facilitate one’s controlled coping with negative feelings and externalizing problem behaviors like substance-abuse/aggressive outbursts. On the contrary part, executive dysfunction can cause/aggravate negative feelings/behavioral outbursts by the perceived lack of control (Goschke, 2014).
The both unified and diverse aspects of EF can be placed in a model (Snyder et al., 2015, p. 13). EF can be assessed by global or more specific neurocognitive tasks (Figure 1 for specific tasks). If severe executive dysfunctioning is expected, the use of both global and specific EF tasks is recommended by Snyder et al. (2015). Inhibition can be measured by Go–NoGo, Stop Signal, Approach Avoidance Tasks, the Stroop, Anti-saccade, Event Related Potential components like P300, self-report/rating measures such as the Frontal Systems Behavioral Scale, BIS-BAS scales (Behavioral Inhibition System-Behavioral Approach System) and by the MMPI-2 Impulse-Control index1 (Stroop, 1935; Hallett, 1978; Butcher et al., 1989; Carver and White, 1994; Robbins et al., 1994; Roberts et al., 1994; Rogers and Monsell, 1995; Mayr and Kliegl, 2000; Grace and Malloy, 2001; Miyake et al., 2004; Handy, 2005; Franken et al., 2006; Friedman et al., 2008; Wiers et al., 2009; Wiers et al., 2010). Shifting can be measured by the Trail Making Test (Reitan, 1958), the Wisconsin Card Sorting Test (Berg, 1948), and other Category Switching Tasks. Updating can be measured by the letter memory task (Morris and Jones, 1990), keep track task (Yntema, 1963) or spatial n-back task.1 Updating tasks involve monitoring of incoming information to check task-relevance, and replacement, update, of old non-relevant information by new information1 (Snyder et al., 2015).
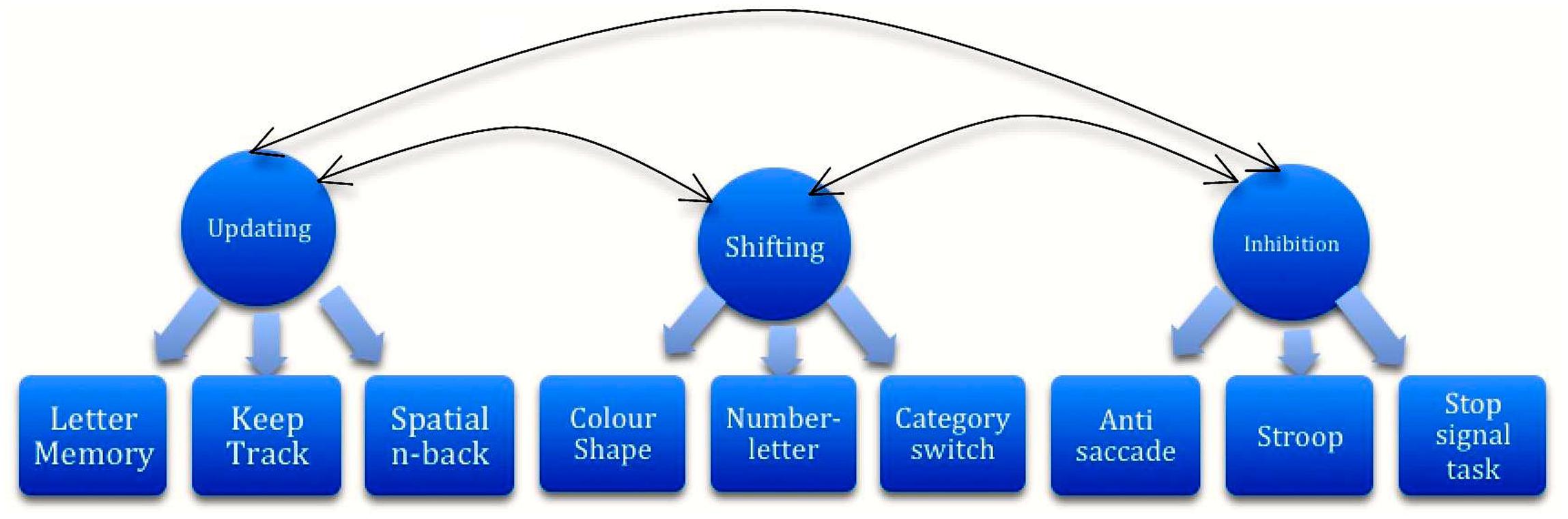
FIGURE 1. Unified and diverse aspects of executive functioning (Snyder et al., 2015.)
Impairments in EF aspects can trigger the appearance of mental disorders by several mechanisms such as (i) a failure to maintain goals when confronted with interfering desires that are difficult to inhibit and/or complicate shifting to more healthy goals, (ii) inhibitory impairment of impulsive responses, (iii) sticking attention to disorder-linked cues like substances that interfere with adequate shifting, (iv) impaired cognitive control (inhibition) and distorted anticipational planning, (v) reduced (emotional) stress regulation, and (vi) cognitive inflexibility (Goschke, 2014). These mechanisms negatively interfere with adequate impulse control and decision making, consequently also thwarting proper self-regulatory behavior in daily life.
Executive functioning impairments were described in several mental conditions like schizophrenia, bipolar-, anxiety-, personality-, developmental disorder, and SUD. For the separate disorders, a high number of studies have been undertaken and multiple reviews are present (see, among others, Verdejo-Garcia et al., 2006; Egger et al., 2007; Fernandez-Serrano et al., 2010; Wiers et al., 2012; Luijten et al., 2013; Thoma and Daum, 2013; Goschke, 2014; Smith et al., 2014; Snyder et al., 2015). Elaborating on this, one can expect that in dual-diagnosis EF will also be impaired. The majority of SUD-patients and half of schizophrenia/bipolar disorder patients are dually diagnosed. That makes insight into EF profiles for dual-diagnosis highly relevant, striving to unravel strengths and pitfalls for daily life behavior. For instance, the indications for treatment differ if one’s pitfall primarily is the inhibition of undesired responses, or a flexible shift from one behavioral strategy to another. Recommendations for treatment can be formed when one oversees the differentiated profile of strengths and weaknesses, particularly in EF.
This article presents an overview of EF studies in dual-diagnosis.
Materials and Methods
The inclusion criteria for studies were as follows: (i) A Method section that contains information concerning: (a) gender, age, test-materials and pre-assessment abstinence period of patients, and (b) diagnostic procedures that were used to determine if a dual-diagnosis was present or not; (ii) Comparisons by use of a healthy control group and/or a group without dual-diagnosis; and (iii) An abstinence period involving less risk for interfering influence of (sub-) acute substance effects, in order to only measure residual effects. The substance of study should not be traceable anymore. Studies with an abstinence period of at least one week were included. For cannabis, a period of four weeks was adhered to (for substance detection times see Verstraete, 2004; for interfering effects see Walvoort et al., 2013). Guidelines for PRISMA analysis were used to select papers (Moher et al., 2009). PRISMA analysis for Web of Science and PubMed resulted in 155 papers including the primary search terms of Executive Functioning AND dual-diagnosis. Four additional papers were found using other search term-combinations, and two additional papers were found by other sources such as on topic reviews (Rabin et al., 2011; Benaiges et al., 2010; Balanza-Martinez et al., 2015). Consequently, a total of 161 papers were screened (including duplicates). After screening, 131 papers were excluded for the following reasons: 121 papers involved the use of search terms in off-topic contexts: for instance, “dual” in “dual-task”. Five studies concerned theoretical/qualitative research/reviews and five papers involved medical/different use of the dual-diagnosis term. 30 articles were assessed for eligibility. Of these, 19 were excluded after analysis, for the following reasons: 12 papers did not mention abstinence periods, two papers’ method-sections did not contain gender/age/test materials, one paper was not found in full-text despite contacting authors and four papers were duplicates between searches. Finally, a total of 11 studies were selected based on the criteria (Table 1). Search terms were Executive Functioning, dual-diagnosis, Substance Use Disorder, alcohol use disorder, inhibition, updating, shifting, comorbidity, schizophrenia, bipolar disorder, personality disorder, anxiety disorder, mood disorder, developmental disorder, and addiction. The independent variable was the dual-diagnosis; the dependent variable was the level of functioning on EF tasks.
Results
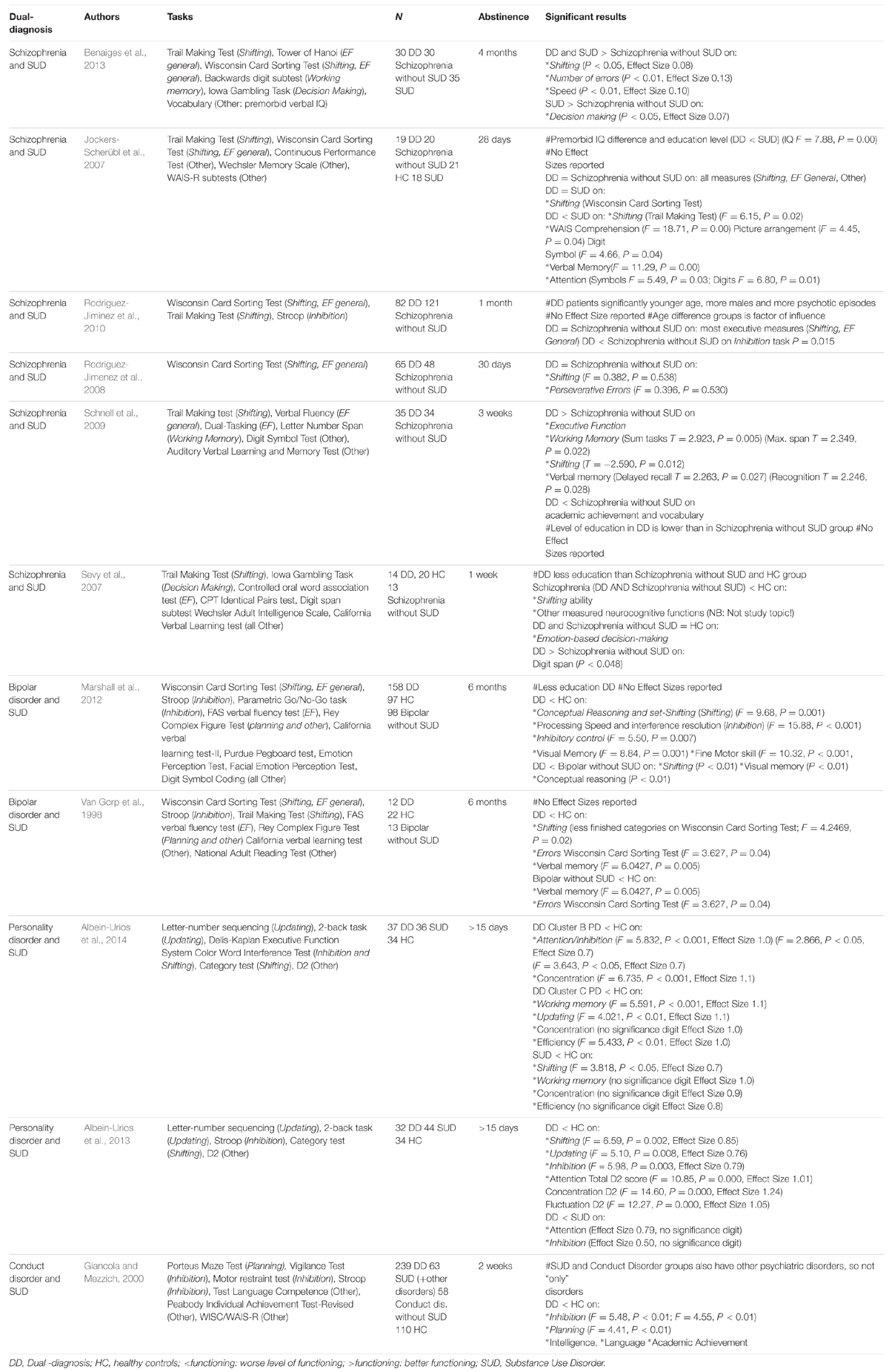
Findings are presented for 11 studies that involve the dual-diagnoses of SUD-Schizophrenia (six), SUD-Bipolar disorder (two), SUD-Personality disorders (two) and SUD-Conduct disorder (one). For SUD-Anxiety and SUD-Developmental disorder no studies were found. Results are organized by disorder, tasks and EF aspect. Significance levels and effect sizes are described if present (Table 1).
SUD-Schizophrenia
Rodriguez-Jiminez et al. (2010) performed the largest schizophrenia-SUD dual-diagnosis study, involving 82 patients with dual-diagnosis (Sch+) and 121 patients with Schizophrenia without SUD (Sch-). Results mostly showed comparable Shifting and EF general abilities for Sch+ and Sch-. The Sch+ group only functioned less at Inhibitory control as compared to the Sch- group. In two more studies, patients with Sch+ and patients with Sch- had similar results for several shifting tasks (Jockers-Scherübl et al., 2007; Rodriguez-Jimenez et al., 2008). Contradictory to those findings, two studies showed better functioning for patients with Sch+ as compared to Sch- on shifting abilities (Schnell et al., 2009; Benaiges et al., 2013). Furthermore, in one study, patients with Sch+ functioned less adequate at shifting (Trail Making Test) and inhibition tasks than patients with Sch- (Jockers-Scherübl et al., 2007). Lastly, Sevy et al., 2007; including a healthy control group) showed worse shifting abilities for Sch+ patients (schizophrenia-cannabis) as compared to healthy controls.
SUD-Bipolar Mood Disorder
Patients with SUD-bipolar disorder showed poorer functioning on mental shifting ability as compared to healthy controls, measured by the Wisconsin Card Sorting Test. That is, dual-diagnosis patients completed fewer categories than controls (Van Gorp et al., 1998). Marshall et al. (2012) described that patients with SUD-bipolar disorder had more executive (inhibitory control, set-shifting, and interference resolution) dysfunctions than controls and patients with bipolar disorder without SUD.
SUD-Personality Disorders
In 2013 and 2014, cocaine abusing patients with cluster B (borderline, narcissistic, histrionic, and anti-social) and cluster C (avoidant, dependent, and obsessive compulsive) personality disorders were studied at diverse EF. Patients with SUD-cluster B personality disorders, that is, more impulsive personality types, showed impairments in nearly all EF aspects as compared to controls and most specifically in inhibitory control. Patients with SUD-cluster C personality disorders, that is, more inhibited and obsessive personality types, showed more problems in working memory and updating ability. Patients with SUD as compared to the dual-diagnosis group had a better inhibitory control. However, compared to healthy controls, the SUD group also showed impairments in shifting and working memory. Patients with dual-diagnosis SUD-Personality disorders as a group consistently functioned less on shifting, updating and inhibitory abilities as compared to healthy controls (Albein-Urios et al., 2013; Albein-Urios et al., 2014).
SUD-Conduct Disorder
One study compared 239 females with dual-diagnosis to healthy controls. Impairments were shown for the dual-diagnosis group on inhibition and planning ability as compared to healthy controls (Giancola and Mezzich, 2000).
SUD-Anxiety Disorders, Developmental Disorders
Despite frequent co-occurrence of SUD-anxiety or SUD-developmental disorders (for prevalence numbers see Dom et al., 2013), we found no studies on EF for these groups.
Discussion
Aim and Model
Aim and Model Gaining a prototypical profile of EF for dual-diagnosis. This is expected to contribute to tailor-made directions for treatment.
Findings
Findings Shifting and inhibitory control mostly are compromised in patients with dual-diagnosis as compared to healthy controls. If one were to think of dual-diagnosis and its overt behavioral symptoms, it is quite conceivable that dual-diagnosis implicates a high amount of (affective) turbulence and sensory sensitivity, since both substances and psychotic/bipolar/other symptoms have an interfering influence on the balance of several brain processes. Elaborating on this, maintaining a realistic view of daily life situations with flexible participation and properly timed inhibition when needed, is likely to be impaired. As compared to Sch-, patients with Sch+ show less inhibitory control. One possible explanation for this difference may be that patients with a SUD-combination show relatively more impulsivity, partly because the use of substances may negatively influence their dopaminergic inhibitory brain processes. Thereby, they seem to be less capable of inhibiting desires than patients without SUD. Furthermore, with a view to negative symptomatology, the schizophrenia patient-group is possibly more avoidant/inhibited than approaching in behavior manner. In terms of impulsivity, this hypothetical explanation also applies to the finding that patients with cluster B (impulsive type) personality disorder and SUD perform inhibitory control tasks less adequately than patients with only SUD. Whereas impulsive behavior has shown to negatively interfere with inhibitory control, it can also be influenced vice versa: common impulsive behavior in dual-diagnoses such as SUD-Bipolar disorder, SUD-cluster B Personality disorder and SUD-Conduct disorder (American Psychiatric Association, 2013) may be maintained or even urged by executive impairments. Impulsivity however seems to have a positive counterpart as well: the finding that Sch+ patients function slightly better on shifting abilities than Sch- patients may be linked to a higher tendency for impulsiveness and search for novelty in patients with SUD-combinations. This means that a flexible switch from familiar pathways to other routes may be easier for persons that are more impulsive and less rigid in behavior than for more avoidant persons that may seek and/or persevere in familiar styles of behavior.
Limitations Concerning Dual-Diagnosis Research
Some conflicting findings reduce the certainty with which conclusions can be stated. These contradictions may be partly caused by factors that influenced several studies, and that may have restricted the validity and reliability of the observed empirical findings in those studies. For instance, the study of Jockers-Scherübl et al. (2007), that of Schnell et al. (2009) and that of Sevy et al. (2007) involved differences in education levels between the Sch+ (lower education level) and Sch- group. Furthermore, in one study the Sch+ group included younger patients and involved more males than the Sch- group. The differences in age actually showed to be a factor in differences found between the groups; so the observed weakened inhibitory control may be affected by the younger age of the dual-diagnosis group (study of Rodriguez-Jiminez et al., 2010). Complications in dual-diagnosis research are possibly due to several reasons. Sample sizes are mostly modest because it is difficult to recruit patients that (i) are in a mild psychiatric state needed for sufficient testability, (ii) are motivated to cooperate and stop using substances, and (iii) have achieved substance-abstinence for a reasonable time prior to assessment, ideally confirmed by tests. A pre-assessment abstinence period of at least six weeks is best, in case of alcohol, but probably for other substances as well, due to the recovery that the body undergoes in this period of time (Weeda et al., 2006; Walvoort et al., 2013). The length of substance abstinence and methods are not always clearly documented, which reduces the validity and reliability of conclusions. Furthermore, when testing patients with dual-diagnosis, it is not clear which disorder and/or substance contributes to which specific empirical finding (Balanza-Martinez et al., 2015). Partly for that reason, disorders and substances are usually studied “separately”. But procedures for dual-diagnosis presence are not always described. This makes it ambiguous whether separate disorders or dual-diagnosis is studied. For example, Giancola and Mezzich (2000) described a “SUD without dual-diagnosis” group in which no Conduct Disorder was present (2000); however, other psychiatric diagnoses were present in this “SUD” group, making it still a “dual-diagnosis” group.
Future Research
Findings lead to the following future research recommendations. Firstly, studying dual-diagnosis has value, when methods are described in a valid manner. Secondly, sufficiently long abstinence periods before assessment, preferably approximately 6 weeks, should be attained to prevent findings from being influenced by acute or sub-acute substance use effects (Weeda et al., 2006; Walvoort et al., 2013). Thirdly, the use of healthy control groups is highly recommended to enable valid comparisons. Fourthly, studies need to be performed in patient groups that also exist in clinical practice, such as dual-diagnosis involving anxiety and developmental disorders. Fifthly, research on all diverse aspects of EF is recommended, also involving Updating processes/working memory. Impairments in flexible shifting abilities, updating processes, or impairments in inhibitory control over undesired responses will most probably lead to different indications for treatment. Finally, findings as described should get more strength through follow up research, including the test of the stated impulsivity hypothesis. Elaborating on these recommendations, there are promising results regarding EF treatment interventions, for instance with Dys-executive Syndrome Treatment Programs and Approach-Avoidance/Inhibitory Intervention Training (among others, Boelen et al., 2012; Rinck et al., 2013; Sharbanee et al., 2014). Hence, unraveling EF in dual-diagnosis has great value for coaching and treatment of patients, and it illustrates how the gap between neuroscience and psychotherapy can be bridged.
Author Contributions
JD was first and corresponding author. She performed the literature search for this mini-review and wrote several concepts of the manuscript. She consulted CV on a regular basis as second author to revise concept manuscript versions and sharpen the described theoretical and empirical issues. CV revised concept versions and JE as last author was available for consultation during the project and revised the final concept version of the manuscript. In the end, the final manuscript and cover letter to be submitted was carefully revised by all three authors en JD eventually submitted the manuscript as first author.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors express their thanks to Mr. Remco. J. Somers, Mrs. Ingeborg L. Kiers, MSc, and Mrs. Anja J. C. M. Haaze-Schoof for english language evaluation of the manuscript.
Footnotes
- ^Most of the tasks are described and categorized in a review by Snyder et al. (2015).
References
Albein-Urios, N., Martinez-Gonzalez, J. M., Lozano, O., Moreno-Lopez, L., Soriano-Mas, C., and Verdejo-Garcia, A. (2013). Negative urgency, disinhibition and reduced temporal pole gray matter characterize the comorbidity of cocaine dependence and personality disorders. Drug. Alcohol Depend. 132, 131–137. doi: 10.1016/j.drugalcdep2013.02.008
Albein-Urios, N., Martinez-Gonzalez, J. M., Lozano-Royas, O., and Verdejo-Garcia, A. (2014). Executive functions in cocaine-dependent patients with cluster B and cluster C personality disorders. Neuropsychology 28, 84–90. doi: 10.1037/neu0000007
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders, DSM-5, 5th Edn. Arlington: American Psychiatric Association.
Balanza-Martinez, V., Crespo-Facorro, B., Gonzalez-Pinto, A., and Vieta, E. (2015). Bipolar disorder comorbid with alcohol use disorder: focus on neurocognitive correlates. Front. Physiol. 6:108. doi: 10.3389/fphys.2015.00108
Barkley, R. A. (2001). The executive functions and self-regulation: an evolutionary neuropsychological perspective. Neuropsychol. Rev. 11, 1–29. doi: 10.1023/A:1009085417776
Benaiges, I., Prat, G., and Adan, A. (2010). Neuropsychological aspects of dual diagnosis. Curr. Drug Abuse Rev. 3, 175–188. doi: 10.2174/1874473711003030175
Benaiges, I., Serra-Grabulosa, J. M., Prat, G., and Adan, A. (2013). Executive functioning in individuals with schizophrenia and/or cocaine dependence. Hum. Psychopharmacol. 28, 29–39. doi: 10.1002/hup.2279
Berg, E. A. (1948). A simple objective technique for measuring flexibility in thinking. J. Gen. Psychol. 39, 15–22. doi: 10.1080/00221309.1948.9918159
Boelen, D., Spikman, J. M., Lamberts, K., Brouwer, W. H., and Fasotti, L. (2012). Behandeling Van het Ddysexecutief Syndroom. Amsterdam: Boom.
Butcher, J. N., Dahlstrom, W. G., Graham, J. R., Tellegen, A., and Kaemmer, B. (1989). The Minnesota Multiphasic Personality Inventory-2 (MMPI-2): Manual for administration and scoring. Minneapolis, MN: University of Minnesota Press.
Carver, C. S., and White, T. L. (1994). Behavioural inhibition, behavioural activation, and affective responses to impending reward and punishment: the BIS/BAS scales. J. Pers. Soc. Psychol. 62, 319–333. doi: 10.1037/0022-3514.67.2.319
De Jong, C. A. J., Schellekens, A. F. A., Ellenbroek, B., Franke, B., and Verkes, R.-J. (2006). The Course of Addiction: Neurobiological Predictors of Chronicity. Cambridge, MA: Academic publications.
Dom, G., Dijkhuizen, A., van der Hoorn, B., Kroon, H., Muusse, C., van Rooijen, S., et al. (2013). Handboek Dubbele Diagnose. Utrecht: de Tijdstroom.
Egger, J. I. M., De Mey, H. R. A., and Janssen, G. T. L. (2007). Assessment of executive functioning in psychiatric disorders: functional diagnosis as the ouverture of treatment. Clin. Neuropsychiatry 4, 111–116.
Fernandez-Serrano, M. J., Perez-Garcia, M., Schmidt Rio-Valle, J., and Verdejo-Garcia, A. (2010). Neuropsychological consequences of alcohol and drug abuse on different components of executive functions. J. Psychopharmacol. 24, 1317–1332. doi: 10.1177/0269881109349841
Franken, I. H. A., Muris, P., and Georgieva, I. (2006). Gray’s model of personality and addiction. Addict. Behav. 31, 399–403. doi: 10.1016/j.addbeh.2005.05.022
Friedman, N. P., Miyake, A., Young, S. E., Defries, J. C., Corley, R. P., and Hewitt, J. K. (2008). Individual differences in executive functions are almost entirely genetic in origin. Gen. J. Exp. Psychol. 137, 201–225. doi: 10.1037/0096-3445.137.2.201
Giancola, P. R., and Mezzich, A. C. (2000). Neuropsychological deficits in female adolescents with a substance use disorder: better accounted for by conduct disorder? J. Stud. Alcohol 61, 809–817. doi: 10.15288/jsa.2000.61.809
Goschke, T. (2014). Dysfunctions of decision-making and cognitive control as transdiagnostic mechanisms of mental disorders: advances, gaps and needs in current research. Int. J. Methods Psychiatr. Res. 23, 41–57. doi: 10.1002/mpr.1410
Grace, J., and Malloy, P. F. (2001). Frontal Systems Behavioral Scale (FrSBe): Professional Manual. Lutz, FL: Psychological Assessment Resources.
Hallett, P. E. (1978). Primary and secondary saccades to goals defined by instructions. Vision Res. 18, 1279–1296. doi: 10.1016/0042-6989(78)90218-3
Janssen, G. T. L. (2013). Diagnostic Assessment of Psychiatric Patients: A Contextual Perspective on Executive Functioning. Nijmegen: Donders Series.
Jockers-Scherübl, M. C., Wolf, T., Radzei, N., Schlattmann, P., Rentzsch, J., Gomez-Carrillo de Castro, A., et al. (2007). Cannabis induces different cognitive changes in schizophrenic patients and in healthy controls. Prog. Neuropsychopharmacol. Biol. Psychiatry 31, 1054–1063. doi: 10.1016/j.pnpbp.2007.03.006
Luijten, M., Machielsen, M. W. J., Veltman, D. J., Hester, R., de Haan, L., and Franken, I. H. A. (2013). Systematic review of ERP and fMRI studies investigating inhibitory control and error processing in people with substance dependence and behavioural addictions. J. Psychiatry Neurosci. 39, 149–169. doi: 10.1503/jpn.130052
Marshall, D. F., Walker, S. J., Ryan, K. A., Kamali, M., Saunders, E. F. H., Weldon, A. L., et al. (2012). Greater executive and visual memory dysfunction in comorbid bipolar disorder and substance use disorder. Psychiatry Res. 200, 252–257. doi: 10.1016/j.psychres.2012.06.013
Mayr, U., and Kliegl, R. (2000). Task-set switching and long-term memory retrieval. J. Exp. Psychol. Learn. Mem. Cogn. 26, 1124–1140. doi: 10.1037//0278-7393.26.5.1124
Miyake, A., Emerson, M. J., Padilla, F., and Ahn, J. C. (2004). Inner speech as a retrieval aid for task goals: the effects of cue type and articulatory suppression in the random task cuing paradigm. Acta Psychol. 115, 123–142. doi: 10.1016/j.actpsy.2003.12.004
Miyake, A., and Friedman, N. P. (2012). The nature and organization of individual differences in executive functions: four general conclusions. Curr. Dir. Psychol. Sci. 21, 8–14. doi: 10.1177/0963721411429458
Miyake, A., Friedman, N. P., Emerson, M. J., Witzki, A. H., and Howerter, A. (2000). The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: a latent variable analysis. Cogn. Psychol. 41, 49–100. doi: 10.1006/cogp.1999.0734
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., and The Prisma Group (2009). Preferred reporting items for systematic reviews and meta analyses: the PRISMA statement. PLoS Med. 6:e1000097. doi: 10.1371/journal.pmed1000097
Morris, N., and Jones, D. M. (1990). Memory updating in working memory: the role of the central executive. Br. J. Psychol. 81, 111–121. doi: 10.1111/j.2044-8295.1990.tb02349.x
Mueser, K. T., Drake, R. E., and Wallach, M. A. (1998). Dual diagnosis: a review of etiological theories. Addict. Behav. 23, 717–734. doi: 10.1016/S0306-4603(98)00073-2
Mueser, K. T., Noordsy, D. L., Drake, R. E., and Fox, L. (2011). Geïntegreerde Behandeling Van Dubbele Diagnose. Een Richtlijn Voor Effectieve Behandeling. Utrecht: de Tijdstroom.
Rabin, R. A., Zakzanis, K. K., and George, T. P. (2011). The effects of cannabis use on neurocognition in schizophrenia: a meta-analysis. Schizophr. Res. 128, 111–116. doi: 10.1016/j.schres.2011.02.017
Regier, D. A., Farmer, M. E., Rae, D. S., Locke, B. Z., Keith, S. J., Judd, L. L., et al. (1990). Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area study. JAMA 264, 2511–2518. doi: 10.1001/jama.264.19.2511
Reitan, R. M. (1958). Validity of the trail making test as an indicator of organic brain damage. Percept. Motor Skills 8, 271–276. doi: 10.1080/13803395.2015.1052732
Rinck, M., Telli, S., Kampmann, I. L., Woud, M. L., Kerstholt, M., Velthuis te, S., et al. (2013). Training approach-avoidance of smiling faces affects emotional vulnerability in socially anxious individuals. Front. Hum. Neurosci. 7:481. doi: 10.3389/fnhum.2013.00481
Robbins, T. W., James, M., Owen, A. M., Sahakian, B. J., Mc Innes, L., and Rabbitt, P. (1994). Cambridge neuropsychological test automated battery (CANTAB): a factor analytic study of a large sample of normal elderly volunteers. Dementia 5, 266–281. doi: 10.1159/000106735
Roberts, R. J., Hager, L. D., and Heron, C. (1994). Prefrontal cognitive processes: working memory and inhibition in the antisaccade task. Gen. J. Exp. Psychol. 123, 374–393. doi: 10.1037/0096-3445.123.4.374
Rodriguez-Jimenez, R., Aragües, M., Jiminez-Arriero, M. A., Ponce, G., Martinez, I., Hoenicka, J., et al. (2008). Psychopathology and Wisconsin card sorting test performance in male schizophrenic patients: influence of Dual Diagnosis. Psychopathology 41, 58–64. doi: 10.1159/000110627
Rodriguez-Jiminez, R., Bagney, A., Martinez-Gras, I., Ponce, G., Sanchez-Morla, E. M., Aragües, M., et al. (2010). Executive function in schizophrenia: influence of substance use disorder history. Schizophr. Res. 118, 34–40. doi: 10.1016/j.schres.2009.09.0259
Rogers, R. D., and Monsell, S. (1995). Costs of a predictable switch between simple cognitive tasks. Gen. J. Exp. Psychol. 124, 207–231. doi: 10.1037/0096-3445.124.2.207
Schnell, T., Koethe, D., Daumann, J., and Gouzoulis-Mayfrank, E. (2009). The role of cannabis in cognitive functioning of patients with schizophrenia. Psychopharmacology 205, 45–52. doi: 10.1007/s00213-009-1512-9
Sevy, S., Burdick, K. E., Visweswaraiah, H., Abdelmessih, S., Lukin, M., Yechiam, E., et al. (2007). Iowa gambling task in schizophrenia and co-occurring cannabis use disorders. Schizophr. Res. 92, 74–84. doi: 10.1016/j.schres.2007.01.005
Sharbanee, J. M., Hu, L., Stritzke, W. G., Wiers, R. W., Rinck, M., and MacLeod, C. (2014). The effect of approach/avoidance training on alcohol consumption is mediated by change in alcohol action tendency. PLoS ONE 9:e85855. doi: 10.1371/journal.pone.0085855
Smith, J. L., Mattick, R. P., Jamadar, S. D., and Iredale, J. M. (2014). Deficits in behavioural inhibition in substance abuse and addiction: a meta-analysis. Drug Alcohol Depend. 145, 1–33. doi: 10.1016/j.drugalcdep.2014.08.009
Snyder, H. R., Miyake, A., and Hankin, B. L. (2015). Advancing understanding of executive function impairments and psychopathology: bridging the gab between clinical and cognitive approaches. Front. Psychol. 6:328. doi: 10.3389/fpsyg.2015.00328
Stroop, J. R. (1935). Studies of interference in serial verbal reactions. J. Exp. Psychol. 18, 643–662. doi: 10.1037/0096-3445.121.1.15
Thoma, P., and Daum, I. (2013). Comorbid substance use disorder in schizophrenia: a selective overview of neurobiological and cognitive underpinnings. Psychiatry Clin. Neurosci. 67, 367–383. doi: 10.1111/pcn.12072
Van Gorp, W., Altshuler, L., Theberge, D. C., Wilkins, J., and Dixon, W. (1998). Cognitive impairment in euthymic bipolar patients with and without prior alcohol dependence: a preliminary study. Arch. Gen. Psychiatry 55, 41–66. doi: 10.1001/archpsyc.55.1.41
Verdejo-Garcia, A., Bechara, A., Recknor, E. C., and Perez-Garcia, M. (2006). Executive dysfunction in substance dependent individuals during drug use and abstinence: an examination of the behavioral, cognitive and emotional correlates of addiction. J. Int. Neuropsychol. Soc. 12, 405–415. doi: 10.1017/S1355617706060486
Verstraete, A. G. (2004). Detection times of drugs of abuse in blood, urine, and oral fluid. Ther. Drug Monit. 26, 200–205. doi: 10.1097/00007691-200404000-00020
Walvoort, S., Wester, A. J., and Egger, J. I. M. (2013). Neuropsychologische diagnostiek en cognitieve functies bij alcoholabstinentie. Tijdschr. Voor Psychiatr. 55, 101–111.
Weeda, M. R., Peters, B. D., De Haan, L., and Linszen, D. H. (2006). Blijvende neuropsychologische stoornissen en structurele en functionele hersenafwijkingen na langdurig cannabisgebruik. Tijdschr. Voor Psychiatr. 48, 185–193.
Wiers, R. W., Cousijn, J., Mors-Schulte, M., den Uijl, T., Goudriaan, A., Schilt, T., et al. (2012). State of the Art Neurocognitieve Effecten van Verslaving. Den Haag: ZonMW.
Wiers, R. W., Rinck, M., Dictus, M., and van den Wildenberg, E. (2009). Relatively strong automatic appetitive action-tendencies in male carriers of the OPRM1G-allele. Genes Brain Behav. 8, 101–106. doi: 10.1111/j.1601-183X.2008.00454.x
Wiers, R. W., Rinck, M., Kordts, R., Houben, K., and Strack, F. (2010). Retraining automatic action-tendencies to approach alcohol in hazardous drinkers. Addiction 105, 279–287. doi: 10.1111/j.1360-0443.2009.02775.x
World Health Organisation [WHO] (2011). Global Status Report on Alcohol and Health. Geneva: WHO Press.
Yntema, D. B. (1963). Keeping track of several things at once. Hum. Fact. 5, 7–17. doi: 10.1177/001872086300500102
Keywords: executive functioning, dual-diagnosis, comorbidity, substance use disorder, alcohol use disorder, addiction, schizophrenia, bipolar
Citation: Duijkers JCLM, Vissers CThWM and Egger JIM (2016) Unraveling Executive Functioning in Dual Diagnosis. Front. Psychol. 7:979. doi: 10.3389/fpsyg.2016.00979
Received: 31 January 2016; Accepted: 13 June 2016;
Published: 28 June 2016.
Edited by:
Leandro Fernandes Malloy-Diniz, Universidade Federal de Minas Gerais, BrazilReviewed by:
Charles W. Mathias, University of Texas Health Science Center San Antonio, USAEmmy Uehara, Universidade Federal Rural do Rio de Janeiro, Brazil
Copyright © 2016 Duijkers, Vissers and Egger. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Judith C. L. M. Duijkers, amR1aWprZXJzQHZ2Z2kubmw=; SnVkaXRob25kZXJ6b2VrQGhvdG1haWwuY29t
 Judith C. L. M. Duijkers
Judith C. L. M. Duijkers Constance Th. W. M. Vissers
Constance Th. W. M. Vissers Jos I. M. Egger
Jos I. M. Egger