- 1Department of Psychiatry and Neuropsychology, School for Mental Health and Neuroscience, Maastricht University Medical Centre, Maastricht, Netherlands
- 2Department of Educational Development and Research, Faculty of Health, Medicine and Life Sciences, Maastricht University, Maastricht, Netherlands
- 3King’s Health Partners, Department of Psychosis Studies, Institute of Psychiatry, King’s College London, London, United Kingdom
The world population is aging and the prevalence of dementia is increasing. By 2050, those aged 60 years and older are expected to make up a quarter of the population. With that, the number of people with dementia is increasing. Unfortunately, there is no cure for dementia. The progression of symptoms with no hope of improvement is difficult to cope with, both for patients and their caregivers. New and evidence-based strategies are needed to support the well-being of both caregiver and patient. Mindfulness training is a body-mind intervention that has shown to improve psychological well-being in a variety of mental health conditions. Mindfulness, a non-judgmental attention to one’s experience in the present moment, is a skill that can be developed with a standard 8-week training. Research has shown preliminary but promising results for mindfulness-based interventions to benefit people with dementia and caregivers. The aim of this review is (a) to provide a rationale for the application of mindfulness in the context of dementia care by giving an overview of studies on mindfulness for people with dementia and/or their caregivers and (b) to provide suggestions for future projects on mindfulness in the context of dementia and to give recommendations for future research.
Introduction
The world population is aging and the prevalence of dementia is increasing. By 2050, those aged 60 years and older are expected to make up almost a quarter of the world’s population (Prince et al., 2013). People who develop dementia mainly express concerns about memory loss, but also experience difficulties with communication, loss of control, and autonomy. Informal caregivers have an important role in the care for people with dementia (de Vugt and Verhey, 2013). Informal caregivers of people with dementia experience providing care as stressful, and show higher levels of psychological distress than caregivers of physically frail elderly people and non-caregivers (Pinquart and Sörensen, 2003). From the moment of the diagnosis of dementia, both the person with dementia and the caregiver will enter a time with stress and uncertainties.
Current interventions to support people with dementia and caregivers often focus on one or the other group, rather than the dyad (Schulz et al., 2007). New strategies are needed to support the well-being of both caregiver and person with dementia. Mindfulness training is an intervention that has shown to improve psychological well-being in both healthy and clinical populations (Fjorback et al., 2011; Hempel et al., 2014; Khoury et al., 2015). Mindfulness based interventions (MBIs) have received increasing empirical support, suggesting it increases well-being of older adults and caregivers in particular.
The aim of this review is (a) to provide a rationale for the application of mindfulness training in the context of dementia care by giving an overview of studies on mindfulness for people with dementia and/or their caregivers, and (b) to provide suggestions for future projects on mindfulness in the context of dementia and to give recommendations for future research.
Mindfulness-Based Interventions: General Overview
Although there is a wide variety of interventions that include components of mindfulness (e.g., Acceptance and Commitment Therapy), this review focuses on the two programs with the largest evidence base, the mindfulness-based stress reduction (MBSR) and mindfulness-based cognitive therapy (MBCT). These group-based programs have been studied in healthy populations and in those with mental or physical disorders, showing satisfactory to good efficacy (Chiesa and Serretti, 2009; Hofmann et al., 2010; Hempel et al., 2014).
The main characteristic of these standardized programs is the cultivation of mindfulness: being able to direct attention in the present moment, in a non-judgmental way, to allow one to act with awareness. Mindfulness is both a characteristic with a population distribution and a skill that can be trained by practicing mindfulness meditation (Brown and Ryan, 2003). The standard program consists of eight weekly group meetings with a duration of 2–2.5 h each plus a 1-day class during the sixth week, and homework for approximately 45 min a day. The programs incorporate meditative exercises such as the body scan, hatha yoga, sitting meditation, and walking meditation (Kabat-Zinn, 1990; Segal et al., 2002). As with any skill, it is important that participants continue the practice after the program has ended, so that they can continue to develop mindfulness and might use it in future difficult situations.
Mindfulness and Aging
Recent research on MBI and aging show positive effects on cognitive, emotional, and psychological domains. There is preliminary evidence that mindful meditation may improve attention, memory, executive function, processing speed, and general cognition (Gard et al., 2014; Marciniak et al., 2014). Moreover, studies show that meditation influences brain structure and function, particularly in areas involved in attentional control, self-awareness, and emotion-regulation (Luders, 2014; Boccia et al., 2015; Tang et al., 2015). Although more systematic research is needed, preliminary results indicate that meditation might reduce age-related cognitive decline (Kurth et al., 2017). These conclusions are drawn from both cross-sectional studies (e.g., comparing meditators versus controls) and longitudinal studies with differences in duration and type of meditation training.
Several mechanisms have been proposed by which mindfulness may promote healthy aging. These include enhanced attentional control, preserved neural functioning, improved psychological well-being, and reduced systemic inflammation (Larouche et al., 2014; Fountain-Zaragoza and Prakash, 2017).
The Mindfulness-to-Meaning Theory proposes a mechanism through which mindfulness increases psychological well-being (Garland et al., 2015b). Through mindfulness practice, participants develop a non-judgmental state of present-moment awareness, which has an effect on the interpretations of stressful life events. This developed broadened awareness, mental flexibility, and the ability to see distressing thoughts and emotions as events that will pass, instead of being the truth, reduces the negative impact of stressful events. Promoting positive reappraisal activates an upward spiral of positive psychological processes as specified in the broaden-and-build theory (Fredrickson, 1998), which increases psychological well-being (Garland et al., 2015a). Support for an upward spiral where state mindfulness and reappraisal enhance each other has been found in several studies such as a study using autoregressive latent trajectory modeling (Garland et al., 2017). Another study showed an upward spiral in which state mindfulness and positive affect enhanced each other (Gotink et al., 2016).
Moreover, the reduction of stress may result in increased telomerase activity, lower blood pressure, and heart rate (Innes and Selfe, 2014). Furthermore, a recent review suggests that mindfulness meditation may increase cognitive reserve capacity and may mitigate age-related cognitive decline (Malinowski and Shalamanova, 2017).
These mechanisms have been proposed as a general pathway to possibly reduce the risk of developing dementia and to slow the process of neurodegeneration. Although studies on improving cognition in older adults with MBI are inconclusive (Berk et al., 2016), there is preliminary evidence that MBI increases psychological well-being in older adults, although not without limitations (Geiger et al., 2016). The majority of this support comes from feasibility studies without a comparison group. These studies reported benefits on pain, attention, sleep, mood elevation, and global quality of life (Morone et al., 2008), emotional well-being (Splevins et al., 2009), anxiety, ruminative thoughts, sleep problems, depressive symptoms (Foulk et al., 2014), and emotional distress (Young and Baime, 2010). One of the two randomized controlled trials (RCT) in the area of aging reported greater reductions in loneliness in the MBSR participants than the wait-list group (Creswell et al., 2012). The other RCT reported improvement on disability, pain severity, and psychological functioning for both the MBSR and education group (Morone et al., 2009).
In the following sections, we provide a review of research on MBI for caregivers (section “Mindfulness and Caregivers”) and patient and caregiver dyads (see section “Mindfulness for Caregiver and Patient Dyads”). In the sections thereafter we focus on research involving people with dementia with a review of research on MBI for people with dementia (see section “Mindfulness for Persons with Dementia”), caregivers of people with dementia (see section “Mindfulness for Caregivers of Persons with Dementia”), and people with dementia and caregiver dyads [see section “Mindfulness for Dyads (Dementia and Caregivers Together”)]. Studies were identified by searches of PubMed, Web of Science, and PsychINFO using the following search terms: “(mindfulness OR MBCT OR MBSR)” AND “(dementia OR Alzheimer OR cognitive decline OR MCI OR caregivers).” Studies on mild cognitive impairment (MCI) and subjective cognitive decline (SCD) were included since individuals with these conditions have a high risk to develop dementia. Both qualitative and quantitative studies were included, and studies needed to include a standard MBI. In addition, additional relevant studies were identified from the reference lists of examined articles.
Mindfulness and Caregivers
Research on MBI to support informal caregivers suggests feasibility and potential benefit on mental health (Jaffray et al., 2016; Li et al., 2016). Most research involved uncontrolled trials for caregivers of a variety of conditions, ranging from terminally ill patients (e.g., patients with advanced-stage cancer) to chronic conditions (e.g., diabetes).
An uncontrolled pilot study with caregivers of elderly patients with cognitive or other functional impairment underwent an adjusted MBSR program (with shorter 90-min sessions) and showed improvements in depression symptoms, but no improvements in mindfulness (Epstein-Lubow et al., 2011). One RCT on caregivers of patients with chronic conditions showed an improvement on depression, which was the primary outcome, compared to an active control (Hou et al., 2014). Moreover, an improvement in anxiety, self-efficacy, and mindfulness were found. However, no effects were found on stress, quality of life, or self-compassion.
Mindfulness for Caregiver and Patient Dyads
Because the lives of caregivers and patients are closely related and MBI aims at being present without judgment with these (shared) life experiences, it may be that the beneficial effects of training could be enhanced by applying the intervention to the system of both patient and caregiver. There are several uncontrolled studies that recruited caregivers and patients to participate in the MBI together. In one pre-test and post-test design study, 21 patient-caregiver dyads completed an MBSR training and both caregiver and patients showed improvement in mood, stress, and mindfulness (Birnie et al., 2010a). A pilot study with an adapted MBSR (6 weeks: three in-person sessions, three audiotaped sessions) for caregivers of cancer patients included 26 dyads and reported improvement of stress and anxiety for patients, but no significant changes for the caregivers (Lengacher et al., 2012). A mixed-method study included 19 lung cancer patients and 16 partners (van den Hurk et al., 2015). Caregiver burden decreased among the partners. However, no significant changes were found in mental distress among all participants. The qualitative analysis of the semi-structured interviews showed that the MBSR training started a process in which both patients and partners became more aware of, and gained more insight into, their thoughts, feelings, and bodily sensations. Moreover, participants reported that it was helpful to participate together with their partner. They encouraged each other to perform the exercises, and it led to better mutual understanding.
Mindfulness and Dementia
Mindfulness for Persons With Dementia
Studies with persons with MCI or SCD have looked at the effect of MBI. This is informative for dementia research, since individuals with MCI have an increased annual conversion rate of 5–17% to Alzheimer’s disease (Cheng et al., 2017), and approximately 60% over a 15-year period of persons with SCD will continue to develop Alzheimer’s disease (Reisberg et al., 2008).
Studies with persons with MCI or subjective memory complaints have looked at the effect of MBI. One pilot study was a randomized trial with 14 people with MCI, which found a trend toward improvement of cognition, quality of life, and well-being for people in the mindfulness condition (Wells et al., 2013). An RCT with 22 people of MCI, showed that the participants in the MBI group showed less memory deterioration and greater decrease in depressive symptoms compared to the control group (Larouche et al., 2016).
Besides these studies on MCI, three other studies involved persons with SCD. One pilot study included 34 older adults with SCD and showed improved worry severity (Lenze et al., 2014). Another study on MBSR for people with SCD involved an RCT that included 14 older adults with and 22 without SCD (Smart et al., 2016). The participants with SCD reported a decrease in cognitive complaints and increase in memory self-efficacy. Attention regulation was improved in all MBSR participants. Recently, a feasibility mixed-methods study in middle-aged and older adults with SCD reported that participants after MBSR worried less about their memory complaints (Berk et al., 2017). Moreover, an RCT with older adults with stress disorders and subjective neurocognitive problems compared MBSR to health education, with the primary outcomes being memory and cognitive control (Wetherell et al., 2017). Participants receiving MBSR showed greater improvement in memory, but not cognitive control. Moreover, the MBSR group improved on measures of worry, depression, and anxiety, and decreased cortisol level for those with high baseline cortisol.
Although these studies demonstrate feasibility of MBSR with older adults with SCD and MCI, and preliminary evidence for memory improvement, more research is necessary to investigate whether MBI can influence cognitive decline. Such studies are beginning to be developed. Recently, a protocol mixed-methods longitudinal study for mindfulness with persons with MCI was published. This study will investigate whether a customized MBI will improve cognitive function, mental health, mindfulness, and functional abilities in daily life activities of persons with MCI, with a 1-year follow-up (Wong et al., 2016).
Mindfulness for Caregivers of Persons With Dementia
A recent systematic review reported that caregivers of persons with dementia show elevated stress, and poorer attention and executive function performance (Allen et al., 2017). Moreover, caregivers of persons with dementia show increased levels of anxiety and depression (Baumgarten et al., 1994; Mahoney et al., 2005). Studies have reported that caregiving for a person with dementia may be particularly stressful compared to other forms of caregiving (Ory et al., 1999; Kim and Schulz, 2008).
Three RCTs have investigated the effects of MBI in caregivers of persons with dementia (Oken et al., 2010; Whitebird et al., 2012; Brown et al., 2016). One study divided 31 caregivers between an adapted MBCT (90 min sessions, 7 weeks) and two control groups: education and respite only (Oken et al., 2010). Both MBCT and education improved the primary outcome of caregiver stress compared to the respite-only group. No effects were found on the secondary outcome measures of cognition and mindfulness. Another study randomized 78 caregivers of persons with dementia into a MBSR or active control group (Whitebird et al., 2012). Caregivers in the MBSR group showed greater improvement in overall mental health, stress, and depression. Both interventions improved anxiety, social support, and burden. In another RCT, 38 family caregivers of persons with dementia were randomized to MBSR or standard social support control condition (Brown et al., 2016). The caregivers in the MBSR group reported lower levels of perceived stress relative to active control group, but not at the 3-month follow-up.
Mindfulness for Dyads (Dementia and Caregivers Together)
To date, only two studies have investigated MBI including both persons with dementia as well as their caregivers. One study with single-group, pre-test and post-test design, involved an adjusted MBSR for persons with progressive cognitive decline (n = 17, majority with dementia) and 20 caregivers (Paller et al., 2014). This study showed improvement in quality of life and depressive symptoms, but no significant findings on cognitive functioning for both patients and caregivers. Another pilot study involved 12 persons with dementia and 8 caregivers with a standard MBSR (Leader et al., 2013). Interviews and observations indicated that some participants with dementia were able to learn mindfulness and experienced increases in quality of life. The caregivers were very positive in their evaluation in that it was helping them to cope better with life. Both groups showed improved quality of life after the intervention, but this was not maintained at the 3-month follow up.
These studies show that it is feasible and potentially beneficial to involve the person with dementia and their caregivers together in an MBI. Although the majority of studies have separated these groups, the well-being of a caregiver and the person with dementia should be considered in context because they influence each other. One study using both cross-sectional and longitudinal analyses investigated the role of suffering in 1222 persons with dementia and the well-being of their caregivers (Schulz et al., 2008). This study showed, in both cross-sectional and longitudinal analyses that perceived suffering of the person with dementia contributes to caregiver depression and burden. Importantly, this was after controlling for the effects of cognitive and physical disability, memory problems, disruptive behaviors, and time spent on caregiving.
Future Directions and Considerations
Although current research supports the rationale for MBI with persons with dementia and their caregivers, only few RCTs have been conducted and more research is necessary (see Table 1). There are several recommendations for future research.
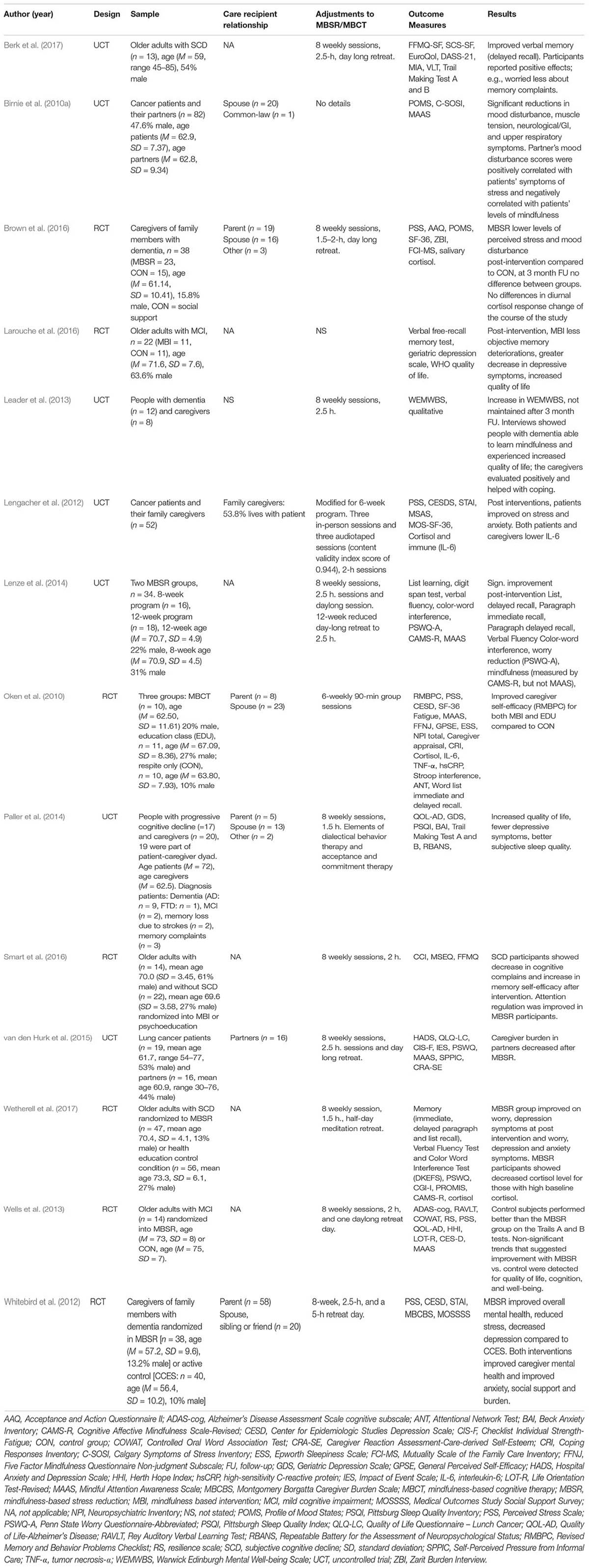
TABLE 1. Overview of MBI studies with caregiver and patient dyads, and MBI studies with persons with SCD, MCI or dementia.
First, more methodologically rigorous trials (RCT with active control) are recommended. The active control is a particularly important component given the strong evidence of the Dodo bird verdict; that all psychotherapies are equally effective (Luborsky et al., 2006; Cuijpers and Pim, 2017). However, this does not mean that the effects are realized by the same mechanisms. Since a mindfulness intervention is a complex process, research projects should not only consider the outcomes of a trial, but also address the mechanisms by which the effects are realized to gain more insight into applying mindfulness in the complex setting of a person with dementia and caregiver. Also, not much is known about the long-term effects, therefore follow-up measurements are recommended. Moreover, an active control for MBI should particularly control for the non-specific effect of “community” associated with mindfulness training. That is, the active control condition needs to provide the same degree of personal contact, being together with other people and feeling of “community.”
Second, it is unclear if and what kinds of adjustments are necessary for people with dementia and their caregivers. In several studies, adaptation of the MBSR or MBCT protocol to the context of a person with dementia and caregiver is frequently practiced, but it is unclear what the effects of specific adaptations are or what the rationale is. For example, many studies adjust the standard MBSR or MBCT protocol to reduce the duration of the sessions (e.g., Ernst et al., 2008), the duration of homework (e.g., Mallya and Fiocco, 2015), or do not include a silent day (e.g., Paller et al., 2014). Another study increased the duration by spreading out the 8 sessions over 8 months (Zellner Keller et al., 2014). However, one study compared an extended 12-week MBSR to an 8-week MBSR in older adults with worry symptoms and subjective cognitive dysfunction, and they found no difference in effects for the different duration of the MBSR (Lenze et al., 2014). Another study showed that a shorter 4-week MBSR with 1-h sessions improved caregiver burden (Hoppes et al., 2012). With different adjustments and different outcome measures it is difficult to tell which elements are crucial. Moreover, other programs that have major adaptations to an MBSR or MBCT protocol have been developed for people with dementia (Chan et al., 2017), and a pilot study showed its feasibility in care homes (Churcher Clarke et al., 2017). Other longer forms showed benefits on cognition in people with Alzheimer’s disease over a 2-year period, including three weekly sessions based on mindfulness, cognitive stimulation therapy, and progressive muscle relaxation (Quintana-Hernández et al., 2015).
Instead of general adjustments, there may be large inter-individual differences driving the need for adjustment within the training group. Therefore, it might be useful to approach the training with a certain amount of flexibility, both from the trainers and the participants. There might not be a “one size fits all” approach. Keeping that in mind, future research should investigate which modifications are beneficial. For example, practical strategies to support home practice and choice in personalized materials should be considered. Perhaps more exercises dedicated to compassion and self-compassion would be a valuable addition. This, however, is ideally investigated with a three-armed RCT (MBI with and without extra compassion, and an active control). Investigating components of the MBI have recently been a topic of discussion, not just for people with dementia and their caregivers. Recently, essential characteristics of MBI and teachers of MBI have been described (Crane et al., 2017). However, it does not touch upon the optimal amount of practice time in the sessions and time spent on homework assignments. Investigating home-practice could lead to different guidelines (i.e., less time) for homework, since the amount of time practiced seems to not be related to the positive outcomes of the program (Dobkin and Zhao, 2011). These and other studies measuring practice time, rely on self-report. However, similar results were found using objective electronic measurement in a 6-week MBCT-based program that showed that adherence to practice (length, frequency, and type of meditation chosen) did not relate to outcomes (Ribeiro et al., 2017). Recently, a first study to directly compare an 8-week with a 4-week MBI showed improvements compared to controls in mindfulness and positive affect, but not between the 4- and 8-week MBI (Demarzo et al., 2017). Thus, abbreviated MBI might be similar to a standard MBI. These studies on length of the program and practice might guide future research on adjustment of the program. A shorter program or shorter sessions might be just as effective, and would make it more accessible for a larger number of people. In particular, time investment could be a major obstacle for caregivers with people with dementia, and a shorter program could increase the likelihood of participation.
Third, future research could investigate whether it is desirable to have people with dementia and their caregiver participate in the MBI together. Although it seems feasible (e.g., Paller et al., 2014), caregivers may feel conflicted when they are invited to pay attention to themselves and focus on their own needs, preventing them from fully benefitting. For example, a few of participants in a study with MBSR for couples facing lung cancer indicated that they felt worried and distracted about the well-being of their partner (van den Hurk et al., 2015). Moreover, caregivers might be reluctant to discuss their fears. Perhaps a program that allows the dyad to separate at specific times could be investigated.
Fourth, future research should consider the following outcome measures to gain more insight into the effects of the MBI. Perhaps it is more fruitful to not only focus on cognition but also on other aspects, such as positive health (Huber et al., 2016). Measuring the influence of compassion on the relationship of the caregiver and person with dementia could be investigated since MBI can improve compassion and that, in turn, might improve couple functioning. One dyadic study with lung cancer patients and their partners showed that more self-compassion was related to less psychological distress in individuals with low levels of self-compassion (Schellekens et al., 2017). Unfortunately, compassion was not measured in most studies. However, research has shown self-reported increases in self-compassion after meditation, impacting mental health (Birnie et al., 2010b). Increasing self-compassion among persons with dementia and caregivers might be particularly valuable since it helps to buffer against anxiety and is associated with increased well-being (Neff et al., 2007). It thus may boost personal resources to supply care for others. In addition, meditation enhances compassionate responding; thus, acting to relieve a person’s suffering (Condon et al., 2013; Lim et al., 2015). Increased caregiver compassion could support the person with dementia. Measuring caregiver management strategies and the impact of MBI might also be interesting for future research since caregivers characterized by non-acceptance was associated with behavioral problems in people with dementia (De Vugt et al., 2004). MBI is thought to increase acceptance and therefore, it might also have an influence on the caregiver style. Future studies could investigate cost-effectiveness in order to make the training program more interesting for reimbursement (e.g., via health insurance). Another important direction of future research is to identify, understand, and develop strategies to overcome barriers to participation, such as time, finances and personal convictions; not only at the individual level, but also what the strategies and barriers are to deliver the program on a larger scale.
This review focuses on older adults since dementia is an age-related disease, however, the essential adjustments to the training are not particularly age-driven. That is, MBI would also be suitable for persons with early onset dementia. A major concern in this field of research is that there are many forms of meditation. Although this review is focused on MBSR/MBCT, other programs with a mindfulness component are developed and researched. It is important to investigate the potential mechanisms and carefully consider the reasons for adjustments.
Conclusion
In sum, current research supports the rationale for MBI with persons with dementia and their caregivers, shows that it is feasible with dyads, and shows preliminary support for improvement in their well-being. In applying interventions for people with dementia and caregivers, their well-being should be considered in context and how dyads influence each other. MBI may offer the couple a skill that they can both use in the future challenges that accompany the context of living with dementia, thus enhancing resilience and autonomy. However, more research is necessary, in particular with respect to what adjustments are beneficial and necessary, and the use of outcomes measures related to positive health.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Funding
LB was supported by a personal research grant (022.005.019) from the Netherlands Organisation for Scientific Research (NWO). This research was funded by Alzheimer Nederland (Grant No. WE.09-2016-4) and the Fred Foundation.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Allen, A. P., Curran, E. A., Duggan,Á., Cryan, J. F., Chorcoráin, A. N., Dinan, T. G., et al. (2017). A systematic review of the psychobiological burden of informal caregiving for patients with dementia: focus on cognitive and biological markers of chronic stress. Neurosci. Biobehav. Rev. 73, 123–164. doi: 10.1016/j.neubiorev.2016.12.006
Baumgarten, M., Hanley, J. A., Infante-Rivard, C., Battista, R. N., Becker, R., and Gauthier, S. (1994). Health of family members caring for elderly persons with dementia. A longitudinal study. Ann. Inter. Med. 120, 126–132. doi: 10.7326/0003-4819-120-2-199401150-00005
Berk, L., Hotterbeekx, R., van Os, J., and van Boxtel, M. (2017). Mindfulness-based stress reduction in middle-aged and older adults with memory complaints: a mixed-methods study. Aging Ment. Health 1–8. doi: 10.1080/13607863.2017.1347142 [Epub ahead of print].
Berk, L., van Boxtel, M., and van Os, J. (2016). Can mindfulness-based interventions influence cognitive functioning in older adults? A review and considerations for future research. Aging Ment. Health 21, 1113–1120. doi: 10.1080/13607863.2016.1247423
Birnie, K., Garland, S. N., and Carlson, L. E. (2010a). Psychological benefits for cancer patients and their partners participating in mindfulness-based stress reduction (MBSR). Psychooncology 19, 1004–1009. doi: 10.1002/pon.1651
Birnie, K., Speca, M., and Carlson, L. E. (2010b). Exploring self-compassion and empathy in the context of mindfulness-based stress reduction (MBSR). Stress Health 26, 359–371. doi: 10.1002/smi.1305
Boccia, M., Piccardi, L., and Guariglia, P. (2015). The meditative mind: a comprehensive meta-analysis of MRI studies. BioMed Res. Int. 2015:419808. doi: 10.1155/2015/419808
Brown, K. W., Coogle, C. L., and Wegelin, J. (2016). A pilot randomized controlled trial of mindfulness-based stress reduction for caregivers of family members with dementia. Aging Ment. Health 20, 1157–1166. doi: 10.1080/13607863.2015.1065790
Brown, K. W., and Ryan, R. M. (2003). The benefits of being present: mindfulness and its role in psychological well-being. J. Pers. Soc. Psychol. 84, 822–848. doi: 10.1037/0022-3514.84.4.822
Chan, J., Churcher Clarke, A., Royan, L., Stott, J., and Spector, A. (2017). A mindfulness program manual for people with dementia. Behav. Modif. 41, 764–787. doi: 10.1177/0145445517715872
Cheng, Y.-W., Chen, T.-F., and Chiu, M.-J. (2017). From mild cognitive impairment to subjective cognitive decline: conceptual and methodological evolution. Neuropsychiatr. Dis. Treat. 13, 491–498. doi: 10.2147/NDT.S123428
Chiesa, A., and Serretti, A. (2009). Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. J. Altern. Complement. Med. 15, 593–600. doi: 10.1089/acm.2008.0495
Churcher Clarke, A., Chan, J. M. Y., Stott, J., Royan, L., and Spector, A. (2017). An adapted mindfulness intervention for people with dementia in care homes: feasibility pilot study. Int. J. Geriatr. Psychiatry 32, e123–e131. doi: 10.1002/gps.4669
Condon, P., Desbordes, G., Miller, W. B., and DeSteno, D. (2013). Meditation increases compassionate responses to suffering. Psychol. Sci. 24, 2125–2127. doi: 10.1177/0956797613485603
Crane, R. S., Brewer, J., Feldman, C., Kabat-Zinn, J., Santorelli, S., Williams, J. M. G., et al. (2017). What defines mindfulness-based programs? The warp and the weft. Psychol. Med. 47, 990–999. doi: 10.1017/S0033291716003317
Creswell, J. D., Irwin, M. R., Burklund, L. J., Lieberman, M. D., Arevalo, J. M. G., Ma, J., et al. (2012). Mindfulness-Based Stress Reduction training reduces loneliness and pro-inflammatory gene expression in older adults: a small randomized controlled trial. Brain Behav. Immun. 26, 1095–1101. doi: 10.1016/j.bbi.2012.07.006
Cuijpers, P., and Pim. (2017). Four decades of outcome research on psychotherapies for adult depression: an overview of a series of meta-analyses. Can. Psychol. 58, 7–19. doi: 10.1037/cap0000096
De Vugt, M. E., Stevens, F., Aalten, P., Lousberg, R., Jaspers, N., Winkens, I., et al. (2004). Do caregiver management strategies influence patient behaviour in dementia? Int. J. Geriatr. Psychiatry 19, 85–92. doi: 10.1002/gps.1044
de Vugt, M. E., and Verhey, F. R. J. (2013). The impact of early dementia diagnosis and intervention on informal caregivers. Prog. Neurobiol. 110, 54–62.” doi: 10.1016/j.pneurobio.2013.04.005
Demarzo, M., Montero-Marin, J., Puebla-Guedea, M., Navarro-Gil, M., Herrera-Mercadal, P., Moreno-González, S., et al. (2017). Efficacy of 8- and 4-session mindfulness-based interventions in a non-clinical population: a controlled study. Front. Psychol. 8:1343. doi: 10.3389/fpsyg.2017.01343
Dobkin, P. L., and Zhao, Q. (2011). Increased mindfulness – the active component of the mindfulness-based stress reduction program? Complement. Ther. Clin. Pract. 17, 22–27. doi: 10.1016/j.ctcp.2010.03.002
Epstein-Lubow, G., McBee, L., Darling, E., Armey, M., and Miller, I. W. (2011). A pilot investigation of mindfulness-based stress reduction for caregivers of frail elderly. Mindfulness 2, 95–102. doi: 10.1007/s12671-011-0047-4
Ernst, S., Welke, J., Heintze, C., Gabriel, R., Zöllner, A., Kiehne, S., et al. (2008). Effects of mindfulness-based stress reduction on quality of life in nursing home residents: a feasibility study. Forsch. Komplementmed. 15, 74–81. doi: 10.1159/000121479
Fjorback, L. O., Arendt, M., Ornbøl, E., Fink, P., Walach, H., and Fjorback, M. (2011). Mindfulness-based stress reduction and mindfulness-based cognitive therapy - a systematic review of randomized controlled trials. Acta Psychiatr. Scand. 124, 102–119. doi: 10.1111/j.1600-0447.2011.01704.x
Foulk, M. A., Ingersoll-Dayton, B., Kavanagh, J., Robinson, E., and Kales, H. C. (2014). Mindfulness-based cognitive therapy with older adults: an exploratory study. J. Gerontol. Soc. Work 57, 498–520. doi: 10.1080/01634372.2013.869787
Fountain-Zaragoza, S., and Prakash, R. S. (2017). Mindfulness training for healthy aging: impact on attention, well-being, and inflammation. Front. Aging Neurosci. 9:11. doi: 10.3389/fnagi.2017.00011
Fredrickson, B. L. (1998). What good are positive emotions? Rev. Gen. Psychol. 2, 300–319. doi: 10.1037/1089-2680.2.3.300
Gard, T., Hölzel, B. K., and Lazar, S. W. (2014). The potential effects of meditation on age-related cognitive decline: a systematic review. Ann. N.Y. Acad. Sci. 1307, 89–103. doi: 10.1111/nyas.12348
Garland, E. L., Farb, N. A., Goldin, P., and Fredrickson, B. L. (2015a). Mindfulness broadens awareness and builds eudaimonic meaning: a process model of mindful positive emotion regulation. Psychol. Inq. 26, 293–314. doi: 10.1080/1047840X.2015.1064294
Garland, E. L., Farb, N. A., Goldin, P. R., and Fredrickson, B. L. (2015b). The mindfulness-to-meaning theory: extensions, applications, and challenges at the attention–appraisal–emotion interface. Psychol. Inq. 26, 377–387. doi: 10.1080/1047840X.2015.1092493
Garland, E. L., Kiken, L. G., Faurot, K., Palsson, O., and Gaylord, S. A. (2017). Upward spirals of mindfulness and reappraisal: testing the mindfulness-to-meaning theory with autoregressive latent trajectory modeling. Cognit. Ther. Res. 41, 381–392. doi: 10.1007/s10608-016-9768-y
Geiger, P. J., Boggero, I. A., Brake, C. A., Caldera, C. A., Combs, H. L., Peters, J. R., et al. (2016). Mindfulness-based interventions for older adults: a review of the effects on physical and emotional well-being. Mindfulness 7, 296–307. doi: 10.1007/s12671-015-0444-1
Gotink, R. A., Hermans, K. S. F. M., Geschwind, N., De Nooij, R., De Groot, W. T., and Speckens, A. E. M. (2016). Mindfulness and mood stimulate each other in an upward spiral: a mindful walking intervention using experience sampling. Mindfulness 7, 1114–1122. doi: 10.1007/s12671-016-0550-8
Hempel, S., Taylor, S. L., Marshall, N. J., Miake-Lye, I. M., Beroes, J. M., Shanman, R., et al. (2014). Evidence Map of Mindfulness. Washington, DC: Department of Veterans Affairs (US).
Hofmann, S. G., Sawyer, A. T., Witt, A. A., and Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J. Consult. Clin. Psychol. 78, 169–183. doi: 10.1037/a0018555
Hoppes, S., Bryce, H., Hellman, C., and Finlay, E. (2012). The effects of brief mindfulness training on caregivers’ well-being. Act. Adapt. Aging 36, 147–166. doi: 10.1037/a0018360
Hou, R. J., Wong, S. Y.-S., Yip, B. H.-K., Hung, A. T. F., Lo, H. H.-M., Chan, P. H. S., et al. (2014). The effects of mindfulness-based stress reduction program on the mental health of family caregivers: a randomized controlled trial. Psychother. Psychoso. 83, 45–53. doi: 10.1159/000353278
Huber, M., van Vliet, M., Giezenberg, M., Winkens, B., Heerkens, Y., Dagnelie, P. C., et al. (2016). Towards a “patient-centred” operationalisation of the new dynamic concept of health: a mixed methods study. Br. Med. J. Open 6:e010091. doi: 10.1136/bmjopen-2015-010091
Innes, K. E., and Selfe, T. K. (2014). Meditation as a therapeutic intervention for adults at risk for Alzheimer’s disease - potential benefits and underlying mechanisms. Front. Psychiatry 5:40. doi: 10.3389/fpsyt.2014.00040
Jaffray, L., Bridgman, H., Stephens, M., and Skinner, T. (2016). Evaluating the effects of mindfulness-based interventions for informal palliative caregivers: a systematic literature review. Palliat. Med. 30, 117–131. doi: 10.1177/0269216315600331
Kabat-Zinn, J. (1990). Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York, NY: Delacorte. doi: 10.1037/032287
Khoury, B., Sharma, M., Rush, S. E., and Fournier, C. (2015). Mindfulness-based stress reduction for healthy individuals: a meta-analysis. J. Psychosom. Res. 78, 519–528. doi: 10.1016/j.jpsychores.2015.03.009
Kim, Y., and Schulz, R. (2008). Family caregivers’ strains: comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. J. Aging Health 20, 483–503. doi: 10.1177/0898264308317533
Kurth, F., Cherbuin, N., and Luders, E. (2017). Aging mindfully to minimize cognitive decline. J. Cogn. Enhanc. 1, 108–114. doi: 10.1007/s41465-017-0027-2
Larouche, E., Chouinard, A.-M., Goulet, S., and Hudon, C. (2016). Mindfulness-based intervention prevents memory decline and improves mood and quality of life in older adults with mild cognitive impairment: preliminary findings. Alzheimers Dement. 12:310. doi: 10.1016/j.jalz.2016.06.562
Larouche, E., Hudon, C., and Goulet, S. (2014). Potential benefits of mindfulness-based interventions in mild cognitive impairment and Alzheimer’s disease: an interdisciplinary perspective. Behav. Brain Res. 276, 199-212. doi: 10.1016/j.bbr.2014.05.058
Leader, G., Litherland, R., Mason, T., Pilchick, T., Sansom, S., and Robertson, G. (2013). Mindfulness and Dementia: Report of a Pilot Study, Innovations in Dementia and Positive Ageing Associates. Available at: http://www.lifestorynetwork.org.uk/wp-content/uploads/downloads/2013/12/Mindfullness-and-Dementia-Report-of-a-Pilot-Study-Med-Dem-Briefingv2.pdf.
Lengacher, C. A., Kip, K. E., Barta, M., Post-white, J., Jacobsen, P. B., Groer, M., et al. (2012). A pilot study evaluating the effect of mindfulness-based stress reduction on psychological status, physical status, salivary cortisol, and interleukin-6 among advanced-stage cancer patients and their caregivers. J. Holist. Nurs. 30, 170–185. doi: 10.1177/0898010111435949
Lenze, E. J., Hickman, S., Hershey, T., Wendleton, L., Ly, K., Dixon, D., et al. (2014). Mindfulness-based stress reduction for older adults with worry symptoms and co-occurring cognitive dysfunction. Int. J. Geriatr. Psychiatry 29, 991–1000. doi: 10.1002/gps.4086
Li, G., Yuan, H., and Zhang, W. (2016). The effects of mindfulness-based stress reduction for family caregivers: systematic review. Arch. Psychiatr. Nurs. 30, 292–299. doi: 10.1016/j.apnu.2015.08.014
Lim, D., Condon, P., and De Steno, D. (2015). Mindfulness and compassion: an examination of mechanism and scalability. PLoS One 10:e0118221. doi: 10.1371/journal.pone.0118221
Luborsky, L., Rosenthal, R., Diguer, L., Andrusyna, T. P., Berman, J. S., Levitt, J. T., et al. (2006). The Dodo bird verdict is alive and well-mostly. Clin. Psychol. Sci. Pract. 9, 2–12. doi: 10.1093/clipsy.9.1.2
Luders, E. (2014). Exploring age-related brain degeneration in meditation practitioners. Ann. N.Y. Acad. Sci. 1307, 82–88. doi: 10.1111/nyas.12217
Mahoney, R., Regan, C., Katona, C., and Livingston, G. (2005). Anxiety and depression in family caregivers of people with Alzheimer disease: the LASER-AD study. Am. J. Geriatr. Psychiatry 13, 795–801. doi: 10.1097/00019442-200509000-00008
Malinowski, P., and Shalamanova, L. (2017). Meditation and cognitive ageing: the role of mindfulness meditation in building cognitive reserve. J. Cogn. Enhanc. 1:107. doi: 10.1007/s41465-017-0022-7
Mallya, S., and Fiocco, A. J. (2015). Effects of mindfulness training on cognition and well-being in healthy older adults. Mindfulness 7, 453–465. doi: 10.1007/s12671-015-0468-6
Marciniak, R., Sheardova, K., Cermáková, P., Hudeček, D., Sumec, R., and Hort, J. (2014). Effect of meditation on cognitive functions in context of aging and neurodegenerative diseases. Front. Behav. Neurosci. 8:17. doi: 10.3389/fnbeh.2014.00017
Morone, N. E., Lynch, C. S., Greco, C. M., Tindle, H. A., and Weiner, D. K. (2008). I felt like a new person.” The effects of mindfulness meditation on older adults with chronic pain: qualitative narrative analysis of diary entries. J. Pain 9, 841–848. doi: 10.1016/j.jpain.2008.04.003
Morone, N. E., Rollman, B. L., Moore, C. G., Li, Q., and Weiner, D. K. (2009). A mind-body program for older adults with chronic low back pain: results of a pilot study. Pain Med. 10, 1395–1407. doi: 10.1111/j.1526-4637.2009.00746.x
Neff, K. D., Kirkpatrick, K. L., and Rude, S. S. (2007). Self-compassion and adaptive psychological functioning. J. Res. Personal. 41, 139–154. doi: 10.1016/j.jrp.2006.03.004
Oken, B. S., Fonareva, I., Haas, M., Wahbeh, H., Lane, J. B., Zajdel, D., et al. (2010). Pilot controlled trial of mindfulness meditation and education for dementia caregivers. J. Altern. Complement. Med. 16, 1031–1038. doi: 10.1089/acm.2009.0733
Ory, M. G., Hoffman, R. R., Yee, J. L., Tennstedt, S., and Schulz, R. (1999). Prevalence and impact of caregiving: a detailed comparison between dementia and nondementia caregivers. Gerontologist 39, 177–185. doi: 10.1093/geront/39.2.177
Paller, K. A., Creery, J. D., Florczak, S. M., Weintraub, S., Mesulam, M.-M., Reber, P. J., et al. (2014). Benefits of mindfulness training for patients with progressive cognitive decline and their caregivers. Am. J. Alzheimer’s Dis. Other Demen. 30, 257-367. doi: 10.1177/1533317514545377
Pinquart, M., and Sörensen, S. (2003). Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychol. Aging 18, 250–267. doi: 10.1037/0882-7974.18.2.250
Prince, M., Bryce, R., Albanese, E., Wimo, A., Ribeiro, W., and Ferri, C. P. (2013). The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 9, 63.e–75.e. doi: 10.1016/j.jalz.2012.11.007
Quintana-Hernández, D. J., Miró-Barrachina, M. T., Ibáñez-Fernández, I. J., Pino, A. S., Quintana-Montesdeoca, M. P., Rodríguez-de Vera, B., et al. (2015). Mindfulness in the maintenance of cognitive capacities in Alzheimer’s disease: a randomized clinical trial. J. Alzheimer’s Dis. 50, 217–232. doi: 10.3233/JAD-143009
Reisberg, B., Prichep, L., Mosconi, L., John, E. R., Glodzik-Sobanska, L., Boksay, I., et al. (2008). The pre-mild cognitive impairment, subjective cognitive impairment stage of Alzheimer’s disease. Alzheimers Dement. 4(1 Suppl. 1), doi: 10.1016/j.jalz.2007.11.017
Ribeiro, L., Atchley, R. M., and Oken, B. S. (2017). Adherence to practice of mindfulness in novice meditators: practices chosen, amount of time practiced, and long-term effects following a mindfulness-based intervention. Mindfulness 9, 401–411. doi: 10.1007/s12671-017-0781-3
Schellekens, M. P. J., Karremans, J. C., van der Drift, M. A., Molema, J., van den Hurk, D. G. M., Prins, J. B., et al. (2017). Are mindfulness and self-compassion related to psychological distress and communication in couples facing lung cancer? A dyadic approach. Mindfulness 8, 325–336. doi: 10.1007/s12671-016-0602-0
Schulz, R., Hebert, R. S., Dew, M. A., Brown, S. L., Scheier, M. F., Beach, S. R., et al. (2007). Patient suffering and caregiver compassion: new opportunities for research, practice, and policy. Gerontologist 47, 4–13. doi: 10.1093/geront/47.1.4
Schulz, R., McGinnis, K. A., Zhang, S., Martire, L. M., Hebert, R. S., Beach, S. R., et al. (2008). Dementia patient suffering and caregiver depression. Alzheimer Dis. Assoc. Disord. 22, 170–176. doi: 10.1097/WAD.0b013e31816653cc
Segal, Z. V., Williams, J. M. G., and Teasdale, J. D. (2002). Mindfulness-Based Cognitive Therapy for Depression: a new approach to preventing relapse. New York, NY: Guilford.
Smart, C. M., Segalowitz, S. J., Mulligan, B. P., Koudys, J., and Gawryluk, J. R. (2016). Mindfulness training for older adults with subjective cognitive decline: Results from a pilot randomized controlled trial. J. Alzheimer’s Dis. 52, 757–774. doi: 10.3233/JAD-150992
Splevins, K., Smith, A., and Simpson, J. (2009). Do improvements in emotional distress correlate with becoming more mindful? A study of older adults. Aging Ment. Health 13, 328–335. doi: 10.1080/13607860802459807
Tang, Y.-Y., Hölzel, B. K., and Posner, M. I. (2015). The neuroscience of mindfulness meditation. Nat. Rev. Neurosci. 16, 213–225. doi: 10.1038/nrn3916
van den Hurk, D. G. M., Schellekens, M. P. J., Molema, J., Speckens, A. E. M., and van der Drift, M. A. (2015). Mindfulness-Based Stress Reduction for lung cancer patients and their partners: results of a mixed methods pilot study. Palliat. Med. 29, 652–660. doi: 10.1177/0269216315572720
Wells, R. E., Kerr, C. E., Wolkin, J., Dossett, M., Davis, R. B., Walsh, J., et al. (2013). Meditation for adults with mild cognitive impairment: a pilot randomized trial. J. Am. Geriatr. Soc. 61, 642–645. doi: 10.1111/jgs.12179
Wetherell, J. L., Hershey, T., Hickman, S., Tate, S. R., Dixon, D., Bower, E. S., et al. (2017). Mindfulness-based stress reduction for older adults with stress disorders and neurocognitive difficulties. J. Clini. Psychiatry 78, e734–e743. doi: 10.4088/JCP.16m10947
Whitebird, R. R., Kreitzer, M., Lauren Crain, A., Lewis, B. A., Hanson, L. R., and Enstad, C. J. (2012). Mindfulness-based stress reduction for family caregivers: a randomized controlled trial. Gerontologist 53, 676–686. doi: 10.1093/geront/gns126
Wong, W. P., Hassed, C., Chambers, R., and Coles, J. (2016). The effects of mindfulness on persons with mild cognitive impairment: protocol for a mixed-methods longitudinal study. Front. Aging Neurosci. 8:156. doi: 10.3389/fnagi.2016.00156
Young, L. A., and Baime, M. J. (2010). Mindfulness-based stress reduction: effect on emotional distress in older adults. Complement. Health Pract. Rev. 15, 59–64. doi: 10.1177/1533210110387687
Keywords: mindfulness, MBSR, older adults, dementia, caregivers
Citation: Berk L, Warmenhoven F, van Os J and van Boxtel M (2018) Mindfulness Training for People With Dementia and Their Caregivers: Rationale, Current Research, and Future Directions. Front. Psychol. 9:982. doi: 10.3389/fpsyg.2018.00982
Received: 22 February 2018; Accepted: 28 May 2018;
Published: 13 June 2018.
Edited by:
Francesco Pagnini, Università Cattolica del Sacro Cuore, ItalyReviewed by:
Suzie Xu Wang, Leeds Beckett University, United KingdomMaria A. Zayas, Brenau University, United States
Copyright © 2018 Berk, Warmenhoven, van Os and van Boxtel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lotte Berk, bG90dGUuYmVya0BtYWFzdHJpY2h0dW5pdmVyc2l0eS5ubA== Martin van Boxtel, bWFydGluLnZhbmJveHRlbEBtYWFzdHJpY2h0dW5pdmVyc2l0eS5ubA==
 Lotte Berk
Lotte Berk Franca Warmenhoven
Franca Warmenhoven Jim van Os
Jim van Os Martin van Boxtel
Martin van Boxtel