- Child, Family, and Population Health Nursing, University of Washington, Seattle, WA, United States
Mounting evidence that early life adversity (ELA) exposures confer risk for cardiometabolic disease over the lifespan motivated this narrative review to examine parenting quality as a potential intervention target to reduce ELA exposures or mitigate their impact as a way of reducing or preventing cardiometabolic disease. We describe findings from the limited number of family-based intervention studies in ELA-exposed children that have tested parenting impacts on cardiometabolic health outcomes. We then describe the implications of this work and make recommendations for future research that will move this field forward.
Introduction
Mounting evidence points to the toxic role of early life adversity (ELA) exposures such as family turmoil, stressful or traumatic events, and contextual stressors (i.e., poverty) in shaping cardiometabolic risk over the lifespan. In this context, it is imperative that we build our knowledge of potential interventions to either target the reduction of ELA exposures or to mitigate their impact as a means of reducing or preventing cardiometabolic disease. Given the large number of ELA exposures that have been identified as well as the intractable nature of their effects, much work remains to identify the type and delivery of interventions that would be most effective. In this narrative review, we examine the early emergence of cardiometabolic risk in childhood and the evidence relating ELA exposures to cardiometabolic health over the lifespan. We then provide a conceptual framework using attachment theory to highlight the potential role of parenting quality in mitigating ELA impacts on cardiometabolic health. Finally, we describe findings from the limited number of family-based intervention studies among ELA-exposed children that have tested parenting effects on cardiometabolic health outcomes and make recommendations for future research to move this field forward.
Early Life Adversity and the Origins of Adulthood Cardiometabolic Disease
Risk for adulthood cardiometabolic disease begins early in life (Olson et al., 2017). Elevated blood pressure and hypertension have been increasing in children (Din-Dzietham et al., 2007; Rosner et al., 2013; Flynn et al., 2017) as have overweight and obesity, with severe obesity in particular rising sharply in children ages 2–5 (Skinner et al., 2018). Type 2 diabetes increased 30% over an 8-year period in one study of almost 2 million children and by 7.1% annually in another study of 4.5 million children (Dabelea et al., 2014; Mayer-Davis et al., 2017). In a community sample, 5% of children ages 7–9 years met criteria for metabolic syndrome and 45% exhibited 1–2 metabolic syndrome components (Dubose et al., 2006). Moreover, insulin resistance and cardiovascular risk factors, including hypertensive status, low HDL cholesterol, and high triglycerides, have been reported in overweight or obese children as young as ages 3–5 years (Bocca et al., 2013). Evidence also shows that children of minority race/ethnic backgrounds exhibit disproportionate risk across these health indicators, including higher rates of hypertension, obesity, and type 2 diabetes compared to their non-Hispanic, white counterparts (Dabelea et al., 2014; Kit et al., 2015; Mayer-Davis et al., 2017; Skinner et al., 2018).
Taken together, the early emergence of risk for adulthood cardiometabolic disease highlights the need to identify modifiable risk factors early in life. ELA exposures are a subset of risk factors or social determinants of health that may be targeted to this end. These exposures encompass a range of experiences that threaten a child's physical or emotional security, such as family dysfunction, stressful or traumatic events, and contextual factors such as socioeconomic disadvantage. ELA exposures are hypothesized to become biologically embedded, possibly through stress-related physiological disruptions in neuroendocrine, immune, and metabolic systems that predispose children to preclinical disease processes and resulting poor cardiometabolic health (Berens et al., 2017). The link between ELA exposures and health was revealed in early findings from The Adverse Childhood Experiences (ACE) Study in which a graded relationship between the number of ELA exposure categories (e.g., physical abuse) and the occurrence of adulthood diseases was observed (Felitti et al., 1998).
To date, a robust and growing literature has substantiated strong and often prospective links between ELA exposures and adulthood health (Galobardes et al., 2008; Shonkoff and Garner, 2012; Su et al., 2015a; Basu et al., 2017; Elsenburg et al., 2017; Suglia et al., 2018), including all-cause and disease-specific mortality (Claussen et al., 2003; Lawlor et al., 2006; Naess et al., 2007), clinical and subclinical cardiovascular disease (CVD) (Roy et al., 2010; Rich-Edwards et al., 2012; Campbell et al., 2016; Hakulinen et al., 2016), CVD risk factors (Danese et al., 2007; Rich-Edwards et al., 2010; Alastalo et al., 2013; Midei et al., 2013; Su et al., 2015b), a worsening of CVD risk over time (Su et al., 2015b; Hakulinen et al., 2016), and negative health behaviors (e.g., cigarette smoking, poor diet) (Anda et al., 1999; Gavrieli et al., 2015). ELA exposures are common in the population, with 60% of adults reporting having experienced at least one type of adversity (CDC, 2010; Bethell et al., 2014). ELA exposures also disproportionately affect vulnerable groups (Slopen et al., 2016; Turney and Wildeman, 2017), suggesting they may contribute to pronounced socioeconomic- and race/ethnicity-based disparities in cardiometabolic health (Chen et al., 2006; Shonkoff et al., 2009).
Although studies of ELA exposures have primarily focused on adulthood health, emerging evidence supports links between ELA exposures and parallel health outcomes in children and adolescents. ELA exposures have been associated with higher systolic blood pressure in children age 5–6 (Smarius et al., 2018) and more rapid increases in blood pressure in young adults (Su et al., 2015b). ELA exposures have also been associated with obesity (Suglia et al., 2012), insulin resistance (Goodman et al., 2007), arterial stiffness (Klassen et al., 2016), and inflammation (Miller and Chen, 2007, 2010; Ehrlich et al., 2016) in children and adolescents, as well as a range of caregiver-reported health problems, including global ratings of the child's health status and medical problems serious enough to require medical attention or impacting functional outcomes such as missing school (Flaherty et al., 2006, 2013; Luby et al., 2017). Findings across the developmental spectrum suggest there is continuity in the role ELA exposures may play in conferring risk for poor cardiometabolic health over periods of childhood, adolescence, and adulthood.
Parenting Quality, Child Self-Regulation, and Child Cardiometabolic Health
The ELA-health literature is large in volume, but has several gaps outlined in recent publications, including a Scientific Statement from the American Heart Association and a report from an expert panel assembled as a part of an NHLBI workshop entitled “Social determinants of health: Early life adversity as a contributor to disparities in cardiovascular diseases” (Suglia et al., 2018, 2020). One gap concerns a lack of studies examining factors that modify ELA risk or that test interventions to lessen ELA impacts on cardiometabolic health. Recommendations for future research emphasize the need to test early life interventions which act on upstream ELA exposures, especially during vulnerable or sensitive developmental periods when intervention efforts may be most effective (Reynolds et al., 2011; Garner, 2013; McLaughlin et al., 2015; Michalopoulos et al., 2017). One potential target for intervention is parenting quality which is hypothesized to have protective effects on child cardiometabolic health by preventing or lessening the negative impacts of ELA exposures.
Attachment theory provides a potent conceptual framework for considering how parenting quality may “get into the body” to protect child health. Attachment theory posits that the ability of the primary caregiver to appropriately respond to the needs of the child, especially in times of distress, facilitates the development of self-regulatory processes in the child (Ainsworth et al., 1978; Coan, 2016). Self-regulatory processes represent key inter-related pathways through which parenting may operate to influence child health, including, but not limited to, self-regulation of socioemotional well-being (Cooke et al., 2019), stress responses systems (Gunnar, 2017), and emerging health behaviors (Bergmeier et al., 2020). In the context of ELA exposures, enhancing parenting quality may be especially important, potentially reducing the ELA exposures themselves, due to the parent's heighted awareness of their impact, or buffering the harmful impacts of ELA exposures. Moreover, effects of parenting-focused approaches may be far-reaching by generalizing to a broad array of family situations over time and by protecting children against a variety of ELA exposures, many of which are unavoidable.
The role of parenting quality, parent-child relationships, and self-regulatory child behaviors have generally been understudied in relation to physical health outcomes in children. This gap was noted in a recent review in which Bergmeier et al. (2020) urged that the quality of early parent-child relationships, well-studied in relation to areas of child socioemotional development, be examined in relation to childhood weight gain and obesity risk. In longitudinal studies, insecure mother-child attachment as well as a composite of insecure mother-child attachment and reduced maternal sensitivity predicted greater obesity risk in childhood (age 4.5 years) (Anderson and Whitaker, 2011) and adolescence (age 15 years) (Anderson et al., 2012), respectively. Insecure mother-child attachment among preadolescents also predicted changes in maladaptive eating behaviors, including increases in dietary constraint and body image concerns as well as increases in BMI over a 1-year period (Goossens et al., 2012). In one of the few studies with a broader health focus, insecure mother-child attachment assessed in infancy predicted an increased likelihood of having a physical illness in adulthood 30 years later, albeit as assessed by self-reports of health conditions (Puig et al., 2013).
Children with insecure (vs. secure) attachment relationships exhibit poor self-regulation, including maladaptive coping strategies in response to feelings of distress that paradoxically result in unresolved or further distress (Aldao et al., 2010; Cooke et al., 2019). This cyclical process may explain how self-regulatory behaviors, shaped by early parenting practices, influence emerging health behaviors and associated health outcomes. For example, poor self-regulation has been related to problematic eating behaviors (Stoeckel et al., 2017) such as emotional eating, decreased sensitivity to satiety (vs. external) food cues, and binge eating (Frankel et al., 2012; Braden et al., 2014; Dingemans et al., 2017). Emotional eating refers to the use of food as a way to manage negative emotions, potentially serving as a substitute for a lack of support in other areas, including parental support (Haedt-Matt and Keel, 2011). A separate literature shows adulthood attachment insecurity is also related to unhealthy eating behaviors (Faber et al., 2018) and eating disorders (Ringer and Crittenden, 2007), as well as to cardiometabolic risk, indexed by metabolic syndrome (Davis et al., 2014; Farrell et al., 2019).
In future studies, more work is necessary to extend these findings to consider physical health outcomes in children beyond those related to eating behaviors and to bridge the child and adulthood attachment literatures in relation to health by examining types of insecure childhood attachment strategies (both minimizing negative emotional expression, Type A, and maximizing negative emotional expression, Type C) (Ringer and Crittenden, 2007; Kozlowska et al., 2011; Crittenden, 2016; Cooke et al., 2019) in relation to parameters of cardiometabolic health in adulthood. In addition, although a significant role for fathers, apart from mothers, is supported by studies relating paternal sensitivity and attachment to child socioemotional and behavioral outcomes (Lucassen et al., 2011; Bureau et al., 2017; Fernandes et al., 2020), father-child attachment has not been examined in relation to child health. Consideration should also be given to the role of grandmothers who play an important role in supporting the parenting behaviors of young mothers and who often contribute to co-parenting efforts, especially in racial/ethnic minority families in whom multigenerational households are more common (Oberlander et al., 2007; Sellers et al., 2011; Cohn and Passel, 2018).
Conceptual Model: ELA, Parenting Quality, and Child Cardiometabolic Health
Based on the findings described above, a conceptual model is presented in Figure 1, depicting the hypothesized role of parenting quality as a protective factor in reducing ELA exposures or in mitigating their impact on child cardiometabolic health, in part, through child self-regulation in areas of socioemotional well-being, stress regulation, and the emergence of early feeding and sleep practices. In this framework, it is plausible that interventions to improve parenting quality among ELA-exposed children may reduce or even prevent cardiometabolic disease. Targeted areas for risk reduction may include chronic inflammation, individual cardiometabolic risk factors, and health behaviors. Although not an exhaustive list, these risk markers are important areas of focus as they are influenced by ELA exposures, show meaningful variation in children, and predict future clinical cardiometabolic disease.
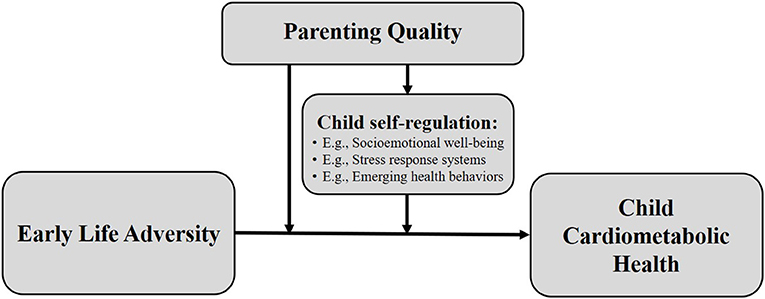
Figure 1. Conceptual model depicting hypothesized role of parenting quality as a protective factor in reducing early life adversity exposures or in mitigating their impact on child cardiometabolic health, in part, through child self-regulation mechanisms.
Specifically, levels of chronic inflammation are elevated in individuals with disadvantaged backgrounds including histories of poverty, child abuse, and family stress (Taylor et al., 2006; Danese et al., 2007; Baumeister et al., 2016). Chronic inflammation is itself correlated with obesity in children (Shashaj et al., 2014) and predicts the development of cardiometabolic diseases (e.g., type 2 diabetes) (Ridker et al., 2000a,b; Pradhan et al., 2001; Pradhan and Ridker, 2002)—some emerging even in early childhood (Hernandez et al., 1998; Weiss, 2007; Messiah et al., 2012; Bocca et al., 2013; Shashaj et al., 2014; Bornhorst et al., 2016; Perng et al., 2016). Likewise, cardiometabolic risk factors, risk factor composites such as metabolic syndrome, and relevant health behaviors are all negatively impacted by ELA exposures (Berens et al., 2017). The early emergence of cardiometabolic risk factors, including, for example, patterns of weight gain in the first years of life, predict trajectories of obesity and cardiometabolic risk over time (Stettler et al., 2003). Thus, there is strong support for the proposed conceptual model describing directional associations between ELA, parenting, and child cardiometabolic health that may ultimately lead to better understanding adulthood risk for cardiometabolic disease.
In future studies, important elaborations on this model will be necessary, including consideration of the developmental context of ELA exposures that might heighten risk for cardiometabolic disease. The Developmental Origins of Health and Disease Hypothesis, for example, focuses on exposures during the period of gestation in relation to adulthood cardiovascular risk (Barker et al., 1990; Barker, 1992). Another developmental period of interest is puberty during which time the occurrence of ELA exposures may also confer excess cardiovascular risk (Bleil et al., 2015). Furthermore, the pathway of pubertal development itself is of interest as ELA exposures appear to accelerate the onset of puberty (Belsky et al., 1991; Moffitt et al., 1992; Ellis, 2004; Bleil et al., 2013, 2021) and earlier pubertal timing, in turn, predicts post-pubertal weight gain, worsening CVD risk factor profiles, and incident cardiometabolic disease, and early mortality (Cooper et al., 1999; Frontini et al., 2003; Feng et al., 2008; Jacobsen et al., 2009; Lakshman et al., 2009).
Parenting Quality: Evidence From Observational and Intervention Studies
Parenting as a Moderator
A growing number of observational studies have examined the potential moderating role of parenting quality. Findings show responsive caregiving buffers impacts of ELA exposures on a range of health outcomes in adults and children (Evans et al., 2007; Chen et al., 2011; Miller et al., 2011; Asok et al., 2013; Carroll et al., 2013; Farrell et al., 2017; Bernard et al., 2019a). In one study, adults who were socioeconomically disadvantaged as children, but experienced high levels of maternal warmth, displayed fewer pro-inflammatory risk markers compared to their adult counterparts in whom maternal warmth was low (Chen et al., 2011). In another study, consistency in the quality and timing of parent-child interactions was linked prospectively to healthier in vitro inflammatory responses in adolescence (Manczak et al., 2018). Findings extend beyond the examination of inflammatory outcomes as well, showing responsive caregiving also buffers impacts of ELA exposures on metabolic syndrome, allostatic load, and BMI, as well as self-reports of physical symptoms and self-ratings of health (Evans et al., 2007; Miller et al., 2011; Carroll et al., 2013; Farrell et al., 2017).
Parenting Focused Interventions
With respect to randomized controlled trials, few studies have tested family-based interventions among ELA-exposed children to determine whether improvements in parenting may attenuate ELA impacts on cardiometabolic health. Findings among these studies, however, warrant special attention to evaluate evidence for the role of parenting, the ways in which parenting may be leveraged in future studies of child cardiometabolic health, and the broader implications for action in clinical and policy-making settings.
In the Strong African American Families (SAAF) study of vulnerable, low-income families, mothers and their children (11 years old) were randomized to a multifaceted family-based intervention versus control condition in which only the study assessments were administered (Brody et al., 2004). In secondary analyses of a subset of the mother-child dyads, children who received the intervention were found to have lower levels of inflammation 8 years later, as reflected by a composite of markers (IFN-γ, IL-10, IL-1β, IL-6, IL-8, and TNF-α) (Miller et al., 2014). Parenting quality, one of the multiple targets of the intervention, mediated this effect; intervention-related improvements in parenting, including both increases in nurturant-involved parenting and decreases in harsh-inconsistent parenting were associated with the lowest levels of inflammation. Moreover, improvements in parenting were greatest, and levels of inflammation the lowest, among the most at-risk families, suggesting the most vulnerable families experienced the most intervention benefit.
Additional secondary analyses in the SAAF study showed intervention effects extended to other cardiometabolic risk indicators as well, including metabolic syndrome and pre-diabetes (Brody et al., 2017, 2019; Chen et al., 2017, 2018). Randomization to the family-based intervention (vs. control condition) mitigated impacts of unsupportive parenting on metabolic syndrome assessed at age 25 with mediational analyses showing effects were attributable to changes in the intervention targets pertaining to parenting quality and parent-child relationships (Chen et al., 2018). Similarly, the family-based intervention (vs. control condition) was found to lessen risk for higher fasting glucose, a marker of pre-diabetes, at age 25 and to eliminate the association between the number of adversity exposures and pre-diabetes (Brody et al., 2017).
In another family-based intervention study, children and their parents who had a history of involvement with child protective services (CPS) due to an identified risk in the home (e.g., maltreatment, domestic violence) were randomized to receive the Attachment and Biobehavioral Catch-up (ABC) intervention vs. control condition in which educational materials about child development were delivered (Bernard et al., 2019a). The ABC intervention used parent coaching and feedback to promote parents' responsivity to child distress as a way of enhancing attachment security and child self-regulation. In the ABC intervention group, 52% of the children were classified as securely attached vs. 32% in the control condition, and attachment security predicted lower BMI at age 4 years and steeper declines in BMI between ages 2 and 4 years. While there was no direct effect of the ABC intervention on child BMI, the mediated or indirect effect of the intervention via attachment security reached marginal significance. In a separate analysis of a subset of children drawn from the same study, children with insecure (vs. secure) attachments exhibited higher levels of inflammation which predicted increases in BMI between ages 4 and 8 years, highlighting the potential mechanistic role of inflammation (Bernard et al., 2019b).
Implications and Future Directions
The studies reviewed above, describing effects of family-based interventions on health outcomes, highlight the important role of parenting as the “key ingredient” in such interventions. Findings indicate that the influence of parenting on these outcomes may even be causal as suggested by randomized control trials involving families randomized to receive parenting-focused training vs. control conditions. In this context, the use of parenting support interventions as a tool to improve cardiometabolic health in children is an exciting and promising new direction. Importantly, evidence also shows that intervention effects are stronger in families in greatest need (Miller et al., 2014), raising the possibility that such interventions may attenuate pronounced ELA-related health burdens in the most vulnerable families.
As a next step, it is important to move this literature forward by focusing on parenting quality directly as well as the potential mechanisms of its effects (e.g., improved child self-regulation). There is immense untapped potential in existing evidence-based parenting interventions that have already been developed to enhance outcomes in areas of child socioemotional well-being and parent-child relationships. These same interventions should be re-examined in relation to child health outcomes. Some examples of established parenting interventions include the ABC intervention mentioned above (Bernard et al., 2019a) and the Promoting First Relationships program, an attachment theory based program which focuses on enhancing positive parent-child relationships (Kelly et al., 2008). Another intervention, the New Beginnings Program, is a parenting-focused program designed to prevent problems in children who experience adversity such as parental divorce (Sandler et al., 2020). Thus, an urgent research question concerns whether existing parenting interventions that are effective in improving child socioemotional well-being and parent-child relationship outcomes, are also effective in reducing ELA impacts on child cardiometabolic health.
Existing parenting interventions are also uniquely positioned for large-scale dissemination through mechanisms such as the federally funded Maternal, Infant, and Early Childhood Home Visiting (MIECHV) program or other established home-visiting programs. MIECHV, described here to illustrate this potential, started in 2010 as a provision within the Affordable Care Act to provide states with resources for home visiting. Seventy-five percent of funds to the states are required to go to evidence-based home visiting programs. Currently, there are 18 programs listed as evidence-based (“US Department of Health and Human Services, Home Visiting Evidence of Effectiveness1,”). Although a few of these programs have reported at least some effects on “positive parenting” and “child health” defined broadly, none have tested the hypothesis presented here—that enhanced parenting quality may prevent or mitigate ELA impacts on child cardiometabolic health. It is plausible that if the benefits of one of these programs were found to extend to child health, there may be “shovel ready” treatment options available for dissemination on a large scale. Dissemination through a mechanism such as MIECHV would make it possible to reach thousands of mother-infant dyads during a sensitive developmental period that sets the stage for lifespan cardiometabolic risk.
Conclusions
In response to mounting evidence that ELA exposures confer risk for cardiometabolic disease, starting even in early childhood, we highlighted the role of parenting as a potential focus of intervention for the reduction of ELA exposures or their mitigation as a way of reducing or preventing cardiometabolic disease. Among the limited number of family-based intervention studies that examined cardiometabolic health outcomes in ELA-exposed children, significant intervention effects on health outcomes were mediated by improvements in parenting behaviors specifically, confirming the key role of parenting. These findings raise the profile of existing evidence-based parenting interventions that have primarily focused on child socioemotional and behavioral outcomes by identifying the opportunity to test these interventions in relation to child cardiometabolic health. Moreover, existing parenting interventions, if found to also benefit child health, have the potential for broad dissemination through home-visiting mechanisms such as the federally funded MIECHV program, making it plausible to reach the most vulnerable families in whom ELA exposures and cardiometabolic risk factors are disproportionately prevalent.
Author Contributions
MB developed the study concept and drafted the manuscript. SS and CB-L provided critical revisions. All authors read and approved the final version of the manuscript for submission.
Funding
The authors disclosed receipt of the following financial support for the preparation of this article. This work was supported by the National Institutes of Health/National Heart, Lung, and Blood Institute [R01HL130103 and R01HL153136] and the National Institutes of Health/Eunice Kennedy Shriver National Institute of Child Health and Human Development [R01HD091132, R01HD080851, and U54HD083091].
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to express our appreciation to members of the Study of Health in Early and Adult Health (SHINE) research team, Winnie Yeung, Alexis Thomas, and Rebecca Christopfel, for their thoughtful contributions to the research presented here, including efforts related to literature searches, referencing, and editorial review.
Abbreviations
ABC, Attachment and Biobehavioral Catch-up; BMI, body mass index; CVD, cardiovascular disease; ELA, early life adversity; MIECHV, Maternal, Infant, and Early Childhood Home Visiting; SAAF, Strong African American Families.
Footnote
1. ^US Department of Health and Human Services, Home Visiting Evidence of Effectiveness. Evidence-Based Models Eligible to Maternal, Infant, and Early Childhood Home Visiting (MIECHV) Grantees. Retrieved from: https://homvee.acf.hhs.gov/HRSA-Models-Eligible-MIECHV-Grantees.
References
Ainsworth, M., Blehar, M., Waters, E., and Wall, S. (1978). Patterns of Attachment. Hillsdale, NJ: Erlbaum.
Alastalo, H., Raikkonen, K., Pesonen, A. K., Osmond, C., Barker, D. J. P., Heinonen, K., et al. (2013). Early life stress and blood pressure levels in late adulthood. J. Hum. Hypertens. 27, 90–94. doi: 10.1038/jhh.2012.6
Aldao, A., Nolen-Hoeksema, S., and Schweizer, S. (2010). Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin. Psychol. Rev. 30, 217–237. doi: 10.1016/j.cpr.2009.11.004
Anda, R. F., Croft, J. B., Felitti, V. J., Nordenberg, D., Giles, W. H., Williamson, D. F., et al. (1999). Adverse childhood experiences and smoking during adolescence and adulthood. JAMA 282, 1652–1658. doi: 10.1001/jama.282.17.1652
Anderson, S. E., Gooze, R. A., Lemeshow, S., and Whitaker, R. C. (2012). Quality of early maternal-child relationship and risk of adolescent obesity. Pediatrics 129, 132–140. doi: 10.1542/peds.2011-0972
Anderson, S. E., and Whitaker, R. C. (2011). Attachment security and obesity in US preschool-aged children. Arch. Pediatr. Adolesc. Med. 165, 235–242. doi: 10.1001/archpediatrics.2010.292
Asok, A., Bernard, K., Roth, T. L., Rosen, J. B., and Dozier, M. (2013). Parental responsiveness moderates the association between early-life stress and reduced telomere length. Dev. Psychopathol. 25, 577–585. doi: 10.1017/S0954579413000011
Barker, D. J. P. (1992). The Fetal and Infant Origins of Adult Disease, 1st Edn. London: British Medical Journal Books.
Barker, D. J. P., Bull, A. R., Osmond, C., and Simmonds, S. J. (1990). Fetal and placental size and risk of hypertension in adult life. Brit. Med. J. 301, 259–262. doi: 10.1136/bmj.301.6746.259
Basu, A., McLaughlin, K. A., Misra, S., and Koenen, K. C. (2017). Childhood maltreatment and health impact: the examples of cardiovascular disease and Type 2 diabetes mellitus in adults. Clin. Psychol. 24, 125–139. doi: 10.1111/cpsp.12191
Baumeister, D., Akhtar, R., Ciufolini, S., Pariante, C. M., and Mondelli, V. (2016). Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-alpha. Mol. Psychiatry 21, 642–649. doi: 10.1038/mp.2015.67
Belsky, J., Steinberg, L., and Draper, P. (1991). Childhood experience, interpersonal development, and reproductive strategy - an evolutionary theory of socialization. Child Dev. 62, 647–670. doi: 10.2307/1131166
Berens, A. E., Jensen, S. K. G., and Nelson, C. A. (2017). Biological embedding of childhood adversity: from physiological mechanisms to clinical implications. BMC Med. 15:12. doi: 10.1186/s12916-017-0895-4
Bergmeier, H., Paxton, S. J., Milgrom, J., Anderson, S. E., Baur, L., Hill, B., et al. (2020). Early mother-child dyadic pathways to childhood obesity risk: a conceptual model. Appetite 144:7. doi: 10.1016/j.appet.2019.104459
Bernard, K., Frost, A., Jelinek, C., and Dozier, M. (2019a). Secure attachment predicts lower body mass index in young children with histories of child protective services involvement. Pediatr. Obes. 14:8. doi: 10.1111/ijpo.12510
Bernard, K., Hostinar, C. E., and Dozier, M. (2019b). Longitudinal associations between attachment quality in infancy, C-reactive protein in early childhood, and BMI in middle childhood: preliminary evidence from a CPS-referred sample. Attach. Hum. Dev. 21, 5–22. doi: 10.1080/14616734.2018.1541513
Bethell, C. D., Newacheck, P., Hawes, E., and Halfon, N. (2014). Adverse childhood experiences: Assessing the impact on health and school engagement and the mitigating role of resilience. Health Affairs 33, 2106–2115. doi: 10.1377/hlthaff.2014.0914
Bleil, M. E., Adler, N. E., Appelhans, B. M., Gregorich, S. E., Sternfeld, B., and Cedars, M. I. (2013). Childhood adversity and pubertal timing: understanding the origins of adulthood cardiovascular risk. Biol. Psychol. 93, 213–219. doi: 10.1016/j.biopsycho.2013.02.005
Bleil, M. E., Appelhans, B. M., Latham, M. D., Irving, M. A., Gregorich, S. E., Adler, N. E., et al. (2015). Neighborhood socioeconomic status during childhood versus puberty in relation to endogenous sex hormone levels in adult women. Nurs. Res. 64, 211–220. doi: 10.1097/NNR.0000000000000096
Bleil, M. E., Spieker, S. J., Gregorich, S. E., Thomas, A. S., Hiatt, R. A., Appelhans, B. M., et al. (2021). Early life adversity and pubertal timing: implications for cardiometabolic health. J. Pediatr. Psychol. 46, 36–48. doi: 10.1093/jpepsy/jsaa082
Bocca, G., Ongering, E. C., Stolk, R. P., and Sauer, P. J. (2013). Insulin resistance and cardiovascular risk factors in 3- to 5-year-old overweight or obese children. Horm. Res. Paediatr. 80, 201–206. doi: 10.1159/000354662
Bornhorst, C., Tilling, K., Russo, P., Kourides, Y., Michels, N., Molnar, D., et al. (2016). Associations between early body mass index trajectories and later metabolic risk factors in European children: the IDEFICS study. Eur. J. Epidemiol. 31, 513–525. doi: 10.1007/s10654-015-0080-z
Braden, A., Rhee, K., Peterson, C. B., Rydell, S. A., Zucker, N., and Boutelle, K. (2014). Associations between child emotional eating and general parenting style, feeding practices, and parent psychopathology. Appetite 80, 35–40. doi: 10.1016/j.appet.2014.04.017
Brody, G. H., Murry, V. M., Gerrard, M., Gibbons, F. X., Molgaard, V., McNair, L., et al. (2004). The Strong African American Families Program: Translating research into prevention programming. Child Dev. 75, 900–917. doi: 10.1111/j.1467-8624.2004.00713.x
Brody, G. H., Yu, T., Chen, E., and Miller, G. E. (2017). Family-centered prevention ameliorates the association between adverse childhood experiences and prediabetes status in young black adults. Prev. Med. 100, 117–122. doi: 10.1016/j.ypmed.2017.04.017
Brody, G. H., Yu, T. Y., Miller, G. E., Ehrlich, K. B., and Chen, E. (2019). Preventive parenting intervention during childhood and young black adults' unhealthful behaviors: a randomized controlled trial. J. Child Psychol. Psychiatry 60, 63–71. doi: 10.1111/jcpp.12968
Bureau, J. F., Martin, J., Yurkowski, K., Schmiedel, S., Quan, J., Moss, E., et al. (2017). Correlates of child-father and child-mother attachment in the preschool years. Attach. Hum. Dev. 19, 130–150. doi: 10.1080/14616734.2016.1263350
Campbell, J. A., Walker, R. J., and Egede, L. E. (2016). Associations between adverse childhood experiences, high-risk behaviors, and morbidity in adulthood. Am. J. Prevent. Med. 50, 344–352. doi: 10.1016/j.amepre.2015.07.022
Carroll, J. E., Gruenewald, T. L., Taylor, S. E., Janicki-Deverts, D., Matthews, K. A., and Seeman, T. E. (2013). Childhood abuse, parental warmth, and adult multisystem biological risk in the Coronary Artery Risk Development in Young Adults study. Proc. Natl. Acad. Sci. U.S.A. 110, 17149–17153. doi: 10.1073/pnas.1315458110
CDC (2010). Centers for Disease Control and Prevention. Adverse childhood experiences reported by adults: five states, 2009. MMWR Morb. Mortal. Weekly Rep. 59, 1609–1613. Available online at: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5949a1.htm
Chen, E., Martin, A. D., and Matthews, K. A. (2006). Understanding health disparities: the role of race and socioeconomic status in children's health. Am. J. Public Health 96, 702–708. doi: 10.2105/AJPH.2004.048124
Chen, E., Miller, G. E., Kobor, M. S., and Cole, S. W. (2011). Maternal warmth buffers the effects of low early-life socioeconomic status on pro-inflammatory signaling in adulthood. Mol. Psychiatry 16, 729–737. doi: 10.1038/mp.2010.53
Chen, E., Miller, G. E., Yu, T., and Brody, G. H. (2018). Unsupportive parenting moderates the effects of family psychosocial intervention on metabolic syndrome in African American youth. Int. J. Obes. 42, 634–640. doi: 10.1038/ijo.2017.246
Chen, Y. F., Yu, T. Y., and Brody, G. H. (2017). Parenting intervention at age 11 and cotinine levels at age 20 among African American youth. Pediatrics 140:8. doi: 10.1542/peds.2016-4162
Claussen, B., Smith, G. D., and Thelle, D. (2003). Impact of childhood and adulthood socioeconomic position on cause specific mortality: the Oslo Mortality Study. J. Epidemiol. Commun. Health 57, 40–45. doi: 10.1136/jech.57.1.40
Coan, J. A. (2016). “Toward a neuroscience of attachment,” in Handbook of Attachment: Theory, Research, and Clinical Applications, 3rd Edn., eds J. Cassidy and P. R. Shaver (New York, NY: Guilford), 242–269.
Cohn, D., and Passel, J. (2018). A Record 64 Million Americans Live in Multigenerational Households. Retrieved from: https://www.pewresearch.org/fact-tank/2018/04/05/a-record-64-million-americans-live-in-multigenerational-households/
Cooke, J. E., Kochendorfer, L. B., Stuart-Parrigon, K. L., Koehn, A. J., and Kerns, K. A. (2019). Parent-child attachment and children's experience and regulation of emotion: a meta-analytic review. Emotion 19, 1103–1126. doi: 10.1037/emo0000504
Cooper, G. S., Ephross, S. A., Weinberg, C. R., Baird, D. D., Whelan, E. A., and Sandler, D. P. (1999). Menstrual and reproductive risk factors for ischemic heart disease. Epidemiology 10, 255–259. doi: 10.1097/00001648-199905000-00011
Crittenden, P. M. (2016). Raising Parents: Attachment, Representation, and Treatment, 2nd Edn. London: Routledge.
Dabelea, D., Mayer-Davis, E. J., Saydah, S., Imperatore, G., Linder, B., Divers, J., et al. (2014). Prevalence of Type 1 and Type 2 diabetes among children and adolescents from 2001 to 2009. JAMA 311, 1778–1786. doi: 10.1001/jama.2014.3201
Danese, A., Pariante, C. M., Caspi, A., Taylor, A., and Poulton, R. (2007). Childhood maltreatment predicts adult inflammation in a life-course study. Proc. Natl. Acad. Sci. U.S.A. 104, 1319–1324. doi: 10.1073/pnas.0610362104
Davis, C. R., Usher, N., Dearing, E., Barkai, A. R., Crowell-Doom, C., Neupert, S. D., et al. (2014). Attachment and the metabolic syndrome in midlife: the role of interview-based discourse patterns. Psychosom. Med. 76, 611–621. doi: 10.1097/PSY.0000000000000107
Din-Dzietham, R., Liu, Y., Bielo, M. V., and Shamsa, F. (2007). High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation 116, 1488–1496. doi: 10.1161/CIRCULATIONAHA.106.683243
Dingemans, A., Danner, U., and Parks, M. (2017). Emotion regulation in binge eating disorder: a review. Nutrients 9:11. doi: 10.3390/nu9111274
Dubose, K. D., Stewart, E. E., Charbonneau, S. R., Mayo, M. S., and Donnelly, J. E. (2006). Prevalence of the metabolic syndrome in elementary school children. Acta Paediatr. 95, 1005–1011. doi: 10.1080/08035250600570553
Ehrlich, K. B., Ross, K. M., Chen, E., and Miller, G. E. (2016). Testing the biological embedding hypothesis: is early life adversity associated with a later proinflammatory phenotype? Dev. Psychopathol. 28, 1273–1283. doi: 10.1017/S0954579416000845
Ellis, B. J. (2004). Timing of pubertal maturation in girls: an integrated life history approach. Psychol. Bull. 130, 920–958. doi: 10.1037/0033-2909.130.6.920
Elsenburg, L. K., van Wijk, K. J. E., Liefbroer, A. C., and Smidt, N. (2017). Accumulation of adverse childhood events and overweight in children: a systematic review and meta-analysis. Obesity 25, 820–832. doi: 10.1002/oby.21797
Evans, G. W., Kim, P., Ting, A. H., Tesher, H. B., and Shannis, D. (2007). Cumulative risk, maternal responsiveness, and allostatic load among young adolescents. Dev. Psychol. 43, 341–351. doi: 10.1037/0012-1649.43.2.341
Faber, A., Dube, L., and Knauper, B. (2018). Attachment and eating: a meta-analytic review of the relevance of attachment for unhealthy and healthy eating behaviors in the general population. Appetite 123, 410–438. doi: 10.1016/j.appet.2017.10.043
Farrell, A. K., Simpson, J. A., Carlson, E. A., Englund, M. M., and Sung, S. (2017). The impact of stress at different life stages on physical health and the buffering effects of maternal sensitivity. Health Psychol. 36, 35–44. doi: 10.1037/hea0000424
Farrell, A. K., Waters, T. E. A., Young, E. S., Englund, M. M., Carlson, E. E., Roisman, G. I., et al. (2019). Early maternal sensitivity, attachment security in young adulthood, and cardiometabolic risk at midlife. Attach. Hum. Dev. 21, 70–86. doi: 10.1080/14616734.2018.1541517
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults - The adverse childhood experiences (ACE) study. Am. J. Prevent. Med. 14, 245–258. doi: 10.1016/S0749-3797(98)00017-8
Feng, Y., Hong, X. M., Wilker, E., Li, Z. P., Zhang, W. B., Jin, D. L., et al. (2008). Effects of age at menarche, reproductive years, and menopause on metabolic risk factors for cardiovascular diseases. Atherosclerosis 196, 590–597. doi: 10.1016/j.atherosclerosis.2007.06.016
Fernandes, C., Monteiro, L., Santos, A. J., Fernandes, M., Antunes, M., Vaughn, B. E., et al. (2020). Early father-child and mother-child attachment relationships: Contributions to preschoolers' social competence. Attach. Hum. Dev. 22, 687–704. doi: 10.1080/14616734.2019.1692045
Flaherty, E. G., Thompson, R., Dubowitz, H., Harvey, E. M., English, D. J., Proctor, L. J., et al. (2013). Adverse childhood experiences and child health in early adolescence. JAMA Pediatr. 167, 622–629. doi: 10.1001/jamapediatrics.2013.22
Flaherty, E. G., Thompson, R., Litrownik, A. J., Theodore, A., English, D. J., Black, M. M., et al. (2006). Effect of early childhood adversity on child health. Arch. Pediatr. Adolesc. Med. 160, 1232–1238. doi: 10.1001/archpedi.160.12.1232
Flynn, J. T., Kaelber, D. C., Baker-Smith, C. M., Blowey, D., Carroll, A. E., Daniels, S. R., et al. (2017). Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140(3). doi: 10.1542/peds.2017-1904
Frankel, L., Hughes, S., O'Connor, T., Power, T., Fisher, J., and Hazen, N. (2012). Parental influences on children's self-regulation of energy intake: insights from developmental literature on emotion regulation. J. Obes. 2012:327259. doi: 10.1155/2012/327259
Frontini, M. G., Srinivasan, S. R., and Berenson, G. S. (2003). Longitudinal changes in risk variables underlying metabolic Syndrome X from childhood to young adulthood in female subjects with a history of early menarche: the Bogalusa Heart Study. Int. J. Obes. 27, 1398–1404. doi: 10.1038/sj.ijo.0802422
Galobardes, B., Lynch, J. W., and Smith, G. D. (2008). Is the association between childhood socioeconomic circumstances and cause-specific mortality established? Update of a systematic review. J. Epidemiol. Commun. Health 62, 387–390. doi: 10.1136/jech.2007.065508
Garner, A. S. (2013). Home visiting and the biology of toxic stress: opportunities to address early childhood adversity. Pediatrics 132(Suppl 2), S65–S73. doi: 10.1542/peds.2013-1021D
Gavrieli, A., Farr, O. M., Davis, C. R., Crowell, J. A., and Mantzoros, C. S. (2015). Early life adversity and/or posttraumatic stress disorder severity are associated with poor diet quality, including consumption of trans fatty acids, and fewer hours of resting or sleeping in a US middle-aged population: a cross-sectional and prospective study. Metab. Clin. Exp. 64, 1597–1610. doi: 10.1016/j.metabol.2015.08.017
Goodman, E., Daniels, S. R., and Dolan, L. M. (2007). Socioeconomic disparities in insulin resistance: results from the Princeton School District Study. Psychosom. Med. 69, 61–67. doi: 10.1097/01.psy.0000249732.96753.8f
Goossens, L., Braet, C., Van Durme, K., Decaluwe, V., and Bosmans, G. (2012). The parent-child relationship as predictor of eating pathology and weight gain in preadolescents. J. Clin. Child Adolesc. Psychol. 41, 445–457. doi: 10.1080/15374416.2012.660690
Gunnar, M. R. (2017). Social buffering of stress in development: a career perspective. Perspect. Psychol. Sci. 12, 355–373. doi: 10.1177/1745691616680612
Haedt-Matt, A. A., and Keel, P. K. (2011). Revisiting the affect regulation model of binge eating: a meta-analysis of studies using ecological momentary assessment. Psychol. Bull. 137, 660–681. doi: 10.1037/a0023660
Hakulinen, C., Pulkki-Raback, L., Elovainio, M., Kubzansky, L. D., Jokela, M., Hintsanen, M., et al. (2016). Childhood psychosocial cumulative risks and carotid intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. Psychosom. Med. 78, 171–181. doi: 10.1097/PSY.0000000000000246
Hernandez, B., Uphold, C. R., Graham, M. V., and Singer, L. (1998). Prevalence and correlates of obesity in preschool children. J. Pediatr. Nurs. 13, 68–76. doi: 10.1016/S0882-5963(98)80033-X
Jacobsen, B. K., Oda, K., Knutsen, S. F., and Fraser, G. E. (2009). Age at menarche, total mortality and mortality from ischaemic heart disease and stroke: the Adventist Health Study, 1976-88. Int. J. Epidemiol. 38, 245–252. doi: 10.1093/ije/dyn251
Kelly, J., Sandoval, D., Zuckerman, T. G., and Buehlman, K. (2008). Promoting First Relationships: A Program for Service Providers to Help Parents and Other Caregivers Nurture Young Children's Social and Emotional Development, 2nd Edn. Seattle, WA: NCAST Programs.
Kit, B. K., Kuklina, E., Carroll, M. D., Ostchega, Y., Freedman, D. S., and Ogden, C. L. (2015). Prevalence of and trends in dyslipidemia and blood pressure among US children and adolescents, 1999-2012. JAMA Pediatr. 169, 272–279. doi: 10.1001/jamapediatrics.2014.3216
Klassen, S. A., Chirico, D., O'Leary, D. D., Cairney, J., and Wade, T. J. (2016). Linking systemic arterial stiffness among adolescents to adverse childhood experiences. Child Abuse Neglect, 56, 1–10. doi: 10.1016/j.chiabu.2016.04.002
Kozlowska, K., Scher, S., and Williams, L. M. (2011). Patterns of emotional-cognitive functioning in pediatric conversion patients: implications for the conceptualization of conversion disorders. Psychosom. Med. 73, 775–788. doi: 10.1097/PSY.0b013e3182361e12
Lakshman, R., Forouhi, N. G., Sharp, S. J., Luben, R., Bingham, S. A., Khaw, K. T., et al. (2009). Early age at menarche is associated with cardiovascular disease and mortality. J. Clin. Endocrinol. Metab. 94, 4953–4960. doi: 10.1210/jc.2009-1789
Lawlor, D. A., Sterne, J. A. C., Tynelius, P., Smith, G. D., and Rasmussen, F. (2006). Association of childhood socioeconomic position with cause-specific mortality in a prospective record linkage study of 1,839,384 individuals. Am. J. Epidemiol. 164, 907–915. doi: 10.1093/aje/kwj319
Luby, J. L., Barch, D., Whalen, D., Tillman, R., and Belden, A. (2017). Association between early life adversity and risk for poor emotional and physical health in adolescence: a putative mechanistic neurodevelopmental pathway. JAMA Pediatr. 171, 1168–1175. doi: 10.1001/jamapediatrics.2017.3009
Lucassen, N., Tharner, A., Van Ijzendoorn, M. H., Bakermans-Kranenburg, M. J., Volling, B. L., Verhulst, F. C., et al. (2011). The association between paternal sensitivity and infant-father attachment security: a meta-analysis of three decades of research. J. Fam. Psychol. 25, 986–992. doi: 10.1037/a0025855
Manczak, E. M., Leigh, A. K. K., Chin, C. P., and Chen, E. (2018). Consistency matters: Consistency in the timing and quality of daily interactions between parents and adolescents predicts production of proinflammatory cytokines in youths. Dev. Psychopathol. 30, 373–382. doi: 10.1017/S0954579417000918
Mayer-Davis, E. J., Lawrence, J. M., Dabelea, D., Divers, J., Isom, S., Dolan, L., et al. (2017). Incidence trends of Type 1 and Type 2 diabetes among youths, 2002-2012. N. Engl. J. Med. 376, 1419–1429. doi: 10.1056/NEJMoa1610187
McLaughlin, K. A., Sheridan, M. A., Tibu, F., Fox, N. A., Zeanah, C. H., and Nelson, C. A. III. (2015). Causal effects of the early caregiving environment on development of stress response systems in children. Proc. Natl. Acad. Sci. U.S.A. 112, 5637–5642. doi: 10.1073/pnas.1423363112
Messiah, S. E., Arheart, K. L., Natale, R. A., Hlaing, W. M., Lipshultz, S. E., and Miller, T. L. (2012). BMI, waist circumference, and selected cardiovascular disease risk factors among preschool-age children. Obesity 20, 1942–1949. doi: 10.1038/oby.2011.353
Michalopoulos, C., Faucetta, K., Warren, A., and Mitchell, R. (2017). Evidence on the Long-Term Effects of Home Visiting Programs: Laying the Groundwork for Long-Term Follow-Up in the Mother and Infant Home Visiting Program Evaluation (MIHOPE). OPRE Report 2017-73. Washington, DC; Office of Planning, Research and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services.
Midei, A. J., Matthews, K. A., Chang, Y. F., and Bromberger, J. T. (2013). Childhood physical abuse is associated with incident metabolic syndrome in mid-life women. Health Psychol. 32, 121–127. doi: 10.1037/a0027891
Miller, G., and Chen, E. (2007). Unfavorable socioeconomic conditions in early life presage expression of proinflammatory phenotype in adolescence. Psychosom. Med. 69, 402–409. doi: 10.1097/PSY.0b013e318068fcf9
Miller, G. E., Brody, G. H., Yu, T., and Chen, E. (2014). A family-oriented psychosocial intervention reduces inflammation in low-SES African American youth. Proc. Natl. Acad. Sci. U.S.A. 111, 11287–11292. doi: 10.1073/pnas.1406578111
Miller, G. E., and Chen, E. (2010). Harsh family climate in early life presages the emergence of a proinflammatory phenotype in adolescence. Psychol. Sci. 21, 848–856. doi: 10.1177/0956797610370161
Miller, G. E., Lachman, M. E., Chen, E., Gruenewald, T. L., Karlamangla, A. S., and Seeman, T. E. (2011). Pathways to resilience: maternal nurturance as a buffer against the effects of childhood poverty on metabolic syndrome at midlife. Psychol. Sci. 22, 1591–1599. doi: 10.1177/0956797611419170
Moffitt, T. E., Caspi, A., Belsky, J., and Silva, P. A. (1992). Childhood experience and the onset of menarche - a test of a sociobiological model. Child Dev. 63, 47–58. doi: 10.2307/1130900
Naess, O., Strand, B. H., and Smith, G. D. (2007). Childhood and adulthood socioeconomic position across 20 causes of death: a prospective cohort study of 800 000 Norwegian men and women. J. Epidemiol. Commun. Health 61, 1004–1009. doi: 10.1136/jech.2006.052811
Oberlander, S. E., Black, M. M., and Starr, R. H. Jr. (2007). African American adolescent mothers and grandmothers: a multigenerational approach to parenting. Am. J. Commun. Psychol. 39, 37–46. doi: 10.1007/s10464-007-9087-2
Olson, M., Chambers, M., and Shaibi, G. (2017). Pediatric markers of adult cardiovascular disease. Curr. Pediatr. Rev. 13, 255–259. doi: 10.2174/1573396314666180117092010
Perng, W., Rifas-Shiman, S. L., Kramer, M. S., Haugaard, L. K., Oken, E., Gillman, M. W., et al. (2016). Early weight gain, linear growth, and mid-childhood blood pressure: a prospective study in Project Viva. Hypertension 67, 301–308. doi: 10.1161/HYPERTENSIONAHA.115.06635
Pradhan, A. D., Manson, J. E., Rifai, N., Buring, J. E., and Ridker, P. M. (2001). C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. JAMA 286, 327–334. doi: 10.1001/jama.286.3.327
Pradhan, A. D., and Ridker, P. M. (2002). Do atherosclerosis and type 2 diabetes share a common inflammatory basis? Eur. Heart J. 23, 831–834. doi: 10.1053/euhj.2001.3052
Puig, J., Englund, M. M., Simpson, J. A., and Collins, W. A. (2013). Predicting adult physical illness from infant attachment: a prospective longitudinal study. Health Psychol. 32, 409–417. doi: 10.1037/a0028889
Reynolds, A. J., Temple, J. A., Ou, S. R., Arteaga, I. A., and White, B. A. B. (2011). School-based early childhood education and age-28 well-being: Effects by timing, dosage, and subgroups. Science 333, 360–364. doi: 10.1126/science.1203618
Rich-Edwards, J. W., Mason, S., Rexrode, K., Spiegelman, D., Hibert, E., Kawachi, I., et al. (2012). Physical and sexual abuse in childhood as predictors of early-onset cardiovascular events in women. Circulation 126, 920–927. doi: 10.1161/CIRCULATIONAHA.111.076877
Rich-Edwards, J. W., Spiegelman, D., Hibert, E. N. L., Jun, H. J., Todd, T. J., Kawachi, I., et al. (2010). Abuse in childhood and adolescence as a predictor of type 2 diabetes in adult women. Am. J. Prevent. Med. 39, 529–536. doi: 10.1016/j.amepre.2010.09.007
Ridker, P. M., Hennekens, C. H., Buring, J. E., and Rifai, N. (2000a). C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N. Engl. J. Med. 342, 836–843. doi: 10.1056/NEJM200003233421202
Ridker, P. M., Rifai, N., Stampfer, M. J., and Hennekens, C. H. (2000b). Plasma concentration of interleukin-6 and the risk of future myocardial infarction among apparently healthy men. Circulation 101, 1767–1772. doi: 10.1161/01.CIR.101.15.1767
Ringer, F., and Crittenden, P. M. (2007). Eating disorders and attachment: the effects of hidden family processes on eating disorders. Eur. Eat. Disord. Rev. 15, 119–130. doi: 10.1002/erv.761
Rosner, B., Cook, N. R., Daniels, S., and Falkner, B. (2013). Childhood blood pressure trends and risk factors for high blood pressure: the NHANES experience 1988-2008. Hypertension 62, 247–254. doi: 10.1161/HYPERTENSIONAHA.111.00831
Roy, A., Janal, M. N., and Roy, M. (2010). Childhood trauma and prevalence of cardiovascular disease in patients with Type 1 diabetes. Psychosom. Med. 72, 833–838. doi: 10.1097/PSY.0b013e3181eafc2d
Sandler, I., Wolchik, S., Mazza, G., Gunn, H., Tein, J. Y., Berkel, C., et al. (2020). Randomized effectiveness trial of the new beginnings program for divorced families with children and adolescents. J. Clin. Child Adolesc. Psychol. 49, 60–78. doi: 10.1080/15374416.2018.1540008
Sellers, K., Black, M. M., Boris, N. W., Oberlander, S. E., and Myers, L. (2011). Adolescent mothers' relationships with their own mothers: impact on parenting outcomes. J. Fam. Psychol. 25, 117–126. doi: 10.1037/a0021877
Shashaj, B., Bedogni, G., Graziani, M. P., Tozzi, A. E., DiCorpo, M. L., Morano, D., et al. (2014). Origin of cardiovascular risk in overweight preschool children: a cohort study of cardiometabolic risk factors at the onset of obesity. JAMA Pediatr. 168, 917–924. doi: 10.1001/jamapediatrics.2014.900
Shonkoff, J. P., Boyce, W. T., and McEwen, B. S. (2009). Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA 301, 2252–2259. doi: 10.1001/jama.2009.754
Shonkoff, J. P., and Garner, A. S. (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics 129, E232–E246. doi: 10.1542/peds.2011-2663
Skinner, A. C., Ravanbakht, S. N., Skelton, J. A., Perrin, E. M., and Armstrong, S. C. (2018). Prevalence of obesity and severe obesity in US children, 1999-2016. Pediatrics 141:9. doi: 10.1542/peds.2017-3459
Slopen, N., Shonkoff, J. P., Albert, M. A., Yoshikawa, H., Jacobs, A., Stoltz, R., et al. (2016). Racial disparities in child adversity in the U.S.: interactions with family immigration history and income. Am. J. Prev. Med. 50, 47–56. doi: 10.1016/j.amepre.2015.06.013
Smarius, L., Strieder, T. G. A., Doreleijers, T. A. H., Vrijkotte, T. G. M., and de Rooij, S. R. (2018). Maternal verbally aggressive behavior in early infancy is associated with blood pressure at age 5-6. J. Dev. Origins Health Dis. 9, 344–350. doi: 10.1017/S2040174418000041
Stettler, N., Kumanyika, S. K., Katz, S. H., Zemel, B. S., and Stallings, V. A. (2003). Rapid weight gain during infancy and obesity in young adulthood in a cohort of African Americans. Am. J. Clin. Nutr. 77, 1374–1378. doi: 10.1093/ajcn/77.6.1374
Stoeckel, L. E., Birch, L. L., Heatherton, T., Mann, T., Hunter, C., Czajkowski, S., et al. (2017). Psychological and neural contributions to appetite self-regulation. Obesity 25, S17–S25. doi: 10.1002/oby.21789
Su, S., Jimenez, M. P., Roberts, C. T., and Loucks, E. B. (2015a). The role of adverse childhood experiences in cardiovascular disease risk: a review with emphasis on plausible mechanisms. Curr. Cardiol. Rep. 17:88. doi: 10.1007/s11886-015-0645-1
Su, S., Wang, X., Pollock, J. S., Treiber, F. A., Xu, X., Snieder, H., et al. (2015b). Adverse childhood experiences and blood pressure trajectories from childhood to young adulthood: the Georgia stress and Heart study. Circulation 131, 1674–1681. doi: 10.1161/CIRCULATIONAHA.114.013104
Suglia, S. F., Brown, A. G. M., Campo, R. A., Boyce, S. A., Stoney, C., Appleton, A. A., et al. (2020). Social determinants of cardiovascular health: Early life adversity as a contributor to disparities in cardiovascular diseases. J. Pediatr. 219, 267–273. doi: 10.1016/j.jpeds.2019.12.063
Suglia, S. F., Duarte, C. S., Chambers, E. C., and Boynton-Jarrett, R. (2012). Cumulative social risk and obesity in early childhood. Pediatrics 129, e1173–e1179. doi: 10.1542/peds.2011-2456
Suglia, S. F., Koenen, K. C., Boynton-Jarrett, R., Chan, P. S., Clark, C. J., Danese, A., et al. (2018). Childhood and adolescent adversity and cardiometabolic outcomes: a Scientific Statement from the American Heart Association. Circulation 137, e15–e28. doi: 10.1161/CIR.0000000000000536
Taylor, S. E., Lehman, B. J., Kiefe, C. I., and Seeman, T. E. (2006). Relationship of early life stress and psychological functioning to adult C-reactive protein in the coronary artery risk development in young adults study. Biol. Psychiatry 60, 819–824. doi: 10.1016/j.biopsych.2006.03.016
Turney, K., and Wildeman, C. (2017). Adverse childhood experiences among children placed in and adopted from foster care: evidence from a nationally representative survey. Child Abuse Neglect 64, 117–129. doi: 10.1016/j.chiabu.2016.12.009
Keywords: early life adversity, parenting, parenting quality, parental sensitivity, attachment, cardiometabolic health, cardiometabolic risk factors, early life intervention
Citation: Bleil ME, Spieker SJ and Booth-LaForce C (2021) Targeting Parenting Quality to Reduce Early Life Adversity Impacts on Lifespan Cardiometabolic Risk. Front. Psychol. 12:678946. doi: 10.3389/fpsyg.2021.678946
Received: 10 March 2021; Accepted: 12 May 2021;
Published: 03 June 2021.
Edited by:
Neha John-Henderson, Montana State University, United StatesReviewed by:
Chioun Lee, University of California, Riverside, United StatesJunilla Kirsten Larsen, Radboud University Nijmegen, Netherlands
Copyright © 2021 Bleil, Spieker and Booth-LaForce. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria E. Bleil, bWJsZWlsQHV3LmVkdQ==
 Maria E. Bleil
Maria E. Bleil Susan J. Spieker
Susan J. Spieker