- 1Department of Psychiatry, Faculty of Medicine, University Hospital in Pilsen, Charles University, Pilsen, Czechia
- 2Department of Psychology, Faculty of Social Studies, Masaryk University, Brno, Czechia
- 3Memory Clinic, Department of Neurology, Second Faculty of Medicine, Motol University Hospital, Charles University, Prague, Czechia
- 4International Clinical Research Center, St. Anne’s University Hospital Brno, Brno, Czechia
- 5Center of Physical Education and Sport, Faculty of Education, University of West Bohemia, Pilsen, Czechia
- 6Institute for Postgraduate Medical Education, Prague, Czechia
Understanding the predictors of the willingness to get vaccinated against COVID-19 may aid in the resolution of current and future pandemics. We investigate how the readiness to believe conspiracy theories and the three dimensions of health locus of control (HLOC) affect the attitude toward vaccination. A cross-sectional study was conducted based on the data from an online survey of a sample of Czech university students (n = 866) collected in January 2021, using the multivariate linear regression models and moderation analysis. The results found that 60% of Czech students wanted to get vaccinated against COVID-19. In addition, 40% of the variance of willingness to get vaccinated was explained by the belief in the COVID-19-related conspiracy theories and the powerful others dimension of HLOC. One-sixth of the variance of the willingness to get vaccinated was explained by HLOC, cognitive reflection, and digital health literacy [eHealth Literacy Scale (EHEALS)]. HLOC and conspiracy mentality (CM) and its predictors are valid predictors of a hesitancy to get vaccinated against COVID-19. The campaigns promoting vaccination should target the groups specifically vulnerable to the conspiracy theories and lacking HLOC related to powerful others.
Introduction
The vaccination campaign against COVID-19 was launched in December 2020 in the Czech Republic, with only half of the population willing to get vaccinated a month later (National Pandemic Alarm, 2021). Vaccination plays a major role in stopping the pandemics, while the cognitive, emotional, and social processes shape public compliance with protective measures, such as vaccination. The WHO (2020) highlights the importance of addressing the “infodemic” as a part of the pandemic response and scientists point to the importance of taking into consideration the social and behavioral factors (Van Bavel et al., 2020) and research that can “inform contextualized campaigns and information-sharing that will ultimately result in increased confidence in and uptake of available vaccines” (Machingaidze and Wiysonge, 2021, p. 1339). Such research needs to investigate how individuals gather and interpret information about and the reason for or against the vaccines, as the primary motivation to get vaccinated is related to the perceived costs and benefits for personal well-being (Solís Arce et al., 2021). Further, studying the predictors of vaccination intentions is important for understanding the reasons and beliefs behind vaccine refusal rather than blaming those who refuse them (refer to Williams, 2021). The intention to get vaccinated against COVID-19 (VAC) is, among other predictors, associated with the beliefs in the COVID-19-related conspiracy theories and about how human health is determined by health locus of control (HLOC), which are examined by the present study.
Health locus of control consists of three relatively independent dimensions: internal (the belief that health is determined by the internal factors and personal effort) and two external ones: the powerful others dimension summarizing the belief that health is determined by other persons, especially the medical personnel and family members, and last, the chance dimension, or the belief that health depends on chance, God, or destiny (Wallston et al., 1978). Internal dimension tends to be positively related to the health behavior, medication adherence, and self-reported health status and chance dimension to psychological distress and lack of adherence (Wallston, 2004; Grotz et al., 2011; Náfrádi et al., 2017; West et al., 2018). The role of the powerful others dimension is more complex, as it places health control in the hands of medical professionals and other people may yield different outcomes (Grotz et al., 2011; Náfrádi et al., 2017; West et al., 2018). Interaction of two dimensions or interaction of an HLOC dimension with another construct may play a crucial role (Wallston, 2004; O’Hea et al., 2005). With respect to vaccination, the chance dimension correlated with the vaccination intentions negatively (Chapman and Coups, 1999) and powerful others (Zhang et al., 2012; Kan et al., 2018) and internal HLOC (HLOC_I) (Tinsley and Holtgrave, 1989; Chapman and Coups, 1999) positively, although Kan et al. (2018) found opposite associations for the chance and internal HLOC, and the associations were not confirmed by Nexøe et al. (1999). In a recent model of the attitudes of parents toward child vaccination, the internal and powerful others HLOC is linked with pro-vaccination and chance HLOC is linked with the anti-vaccination attitudes (Aharon et al., 2018). Recently, the negative link between the chance of HLOC and the willingness to get vaccinated against COVID-19 was confirmed (Olagoke et al., 2021).
The intentions to vaccinate may be negatively affected by the conspiracy theories (Jolley and Douglas, 2014). In the case of COVID-19, a lack of willingness to get vaccinated was associated with the COVID-19-related conspiracy beliefs (Romer and Jamieson, 2020) and a gradual decrease in the vaccination intentions throughout 2020 was linked with the COVID-19-related misinformation (Robinson et al., 2021). Conspiracy theories are “attempts to explain the ultimate causes of significant social and political events and circumstances with claims of secret plots by two or more powerful actors” (Douglas et al., 2019, p. 4). The conspiracy claims, such as that COVID-19 is a hoax, or that it was spread intentionally, reduce compliance with protective measures and restrictions (Bierwiaczonek et al., 2020; Imhoff and Lamberty, 2020; Pummerer et al., 2021; as shown in Douglas, 2021 for an overview). Conspiracy mentality (CM) is studied as the individual predisposition to believe in conspiracy theories because beliefs in conspiracy theories from various domains are intercorrelated, even if the beliefs contradict each other (Wood et al., 2012; Imhoff and Bruder, 2013). CM is related to the external locus of control (Abalakina-Paap et al., 1999) and the belief in COVID-19-related conspiracy theories (Imhoff and Lamberty, 2020), and in those who perceive low support for the vaccination in their social environment, it predicts low vaccination intentions (Winter et al., 2021). CM is itself predicted by dissociation (Charlton, 2014) and cognitive reflection—the ability to reflect upon whether the result of an intuitive cognitive process is correct (Stoica and Umbreş, 2020). The COVID-19-related conspiracy theories are also associated with low digital health literacy (EHEALS) (Naeem and Boulos, 2021; Pickles et al., 2021), which is “the ability to seek, find, understand, and appraise health information from electronic sources and apply the knowledge gained to addressing or solving a health problem” (WHO, 2013, p. 61).
In our previous study on the same sample, we have shown that the COVID-19-related conspiracy theories were indeed predicted by digital health literacy, dissociation tendencies, and cognitive reflection and that the effect of the latter two was mediated by CM (Pisl et al., 2021). The present study further extends these results with respect to the vaccination intentions, studying the effects of HLOC and conspiracy theories and their predictors on the willingness to get vaccinated against COVID-19. Based on the model of Aharon et al. (2018), we hypothesize that the internal and powerful others HLOC is linked with higher and chance HLOC with the lower willingness of the university students of Czech to get vaccinated against COVID-19. With respect to the conspiracy theories, we examine how these conspiracy theories and their predictors influence the willingness to get vaccinated against COVID-19 in three steps. In the first model, we will test the effects of HLOC and belief in the COVID-19-related conspiracy theories on VAC. In the second model, we will test the effects of HLOC and the predictors of COVID-19-related conspiracy theories on VAC, expecting VAC to be related to the low CM and high digital health literacy. Further, we expect the effect of internal HLOC to interact with the CM and digital health literacy, indicating that the positive effect of internal HLOC on vaccination is higher in those who are well-informed and less susceptible to the conspiracy theories. In the third model, we will test the effects of HLOC, digital health literacy, and predictors of CM on VAC, expecting VAC to be related to low dissociation and high cognitive reflection.
Materials and Methods
Materials
Health locus of control was measured by the Multidimensional HLOC scale (MHLOC), version A (Wallston et al., 1978), a short instrument with acceptable reliability (Cronbach’s alpha usually hovers in the range 0.65–0.70) (Wallston, 2004), consisting of 18 items measuring three separate and only slightly intercorrelated dimensions: the belief that it is the subject who has control over their health (internal HLOC, HLOC_I), the belief that health of an individual is controlled by others (e.g., health professionals and family; powerful others HLOC, HLOC_P), and the belief that health is controlled by chance (HLOC_C). The answers were recorded on the 6-point Likert scales that were later converted to numbers ranging from 1 to 6 (6 meaning highest agreement), yielding three summary scores ranging from 6 to 36.
The vaccination intention (VAC) was measured by a single question: “How likely is it that you are going to get vaccinated against COVID-19” with 11 options ranging from 0 to 100%.
The measures of other variables were described previously by Pisl et al. (2021). Experience with dissociation was measured by the Dissociative Experience Scale (DES) (Ptáček and Bob, 2009), CM by the CM Questionnaire (CMQ) (Bruder et al., 2013), cognitive reflection by the cognitive reflection test (CRT) (Frederick, 2005), and digital health literacy (EHEALS) by the eHealth Literacy Scale (eHEALS) (Norman and Skinner, 2006). The belief in two COVID-19-related conspiracy theories, namely, that COVID-19 is a hoax, and that COVID-19 was created intentionally by humans, was measured by two scales, each consisting of three items, adopted from Imhoff and Lamberty (2020). The three items in the HOAX subscale are: “The virus is intentionally presented as dangerous in order to mislead the public,” “Experts intentionally mislead us for their benefit, even though the virus is not worse than a flu,” and “We should believe experts when they say that the virus is dangerous” (reverse-coded). The three items used in the CREATED subscale are: “Corona was intentionally brought into the world to reduce the population,” “Dark forces want to use the virus to rule the world,” and “I think it’s nonsense that the virus was created in a laboratory” (reverse-coded). The Czech translation of the original English scales was confirmed by a back translation.
Participants and Data Collection
The convenience sample consisted of 866 students (mean age 23.58 years; 621 women) of medicine, law, and pedagogy at the universities located in Pilsen, Czech Republic. Out of the original 914 responses, seven participants were excluded as they did not belong to the studied population and 40 submissions were excluded as duplicates (for details, refer to Pisl et al., 2021). The participants were delivered a link to an online questionnaire presented via Google Forms from their lecturers, consisting of the above-described scales. To avoid any possible effects of priming or self-stylization with respect to the COVID-19-related beliefs that might possibly influence the responses to the DES and CMQ, the questions regarding COVID-19 were placed at the end of the questionnaire, and coronavirus was not mentioned in the introduction of the aims of the research. The study was approved by the Ethics Committee of the University Hospital and Faculty of Medicine in Pilsen (No. 49/2021), Czech.
Settings
Data were collected between January 8 and January 21, 2021, during the second pandemic peak in the Czech Republic, shortly after vaccines were introduced and before they were made available to the general population. The first dose of the vaccine was given to a politician on December 27, 2020, and between then and January 21, 2021, 175,999 inhabitants, or 1.7% of the population received at least one dose (Mathieu et al., 2021). As of January 21, 2021, 15,445 persons died of coronavirus in the country of 10 million, according to government statistics (MZCR, 2021), with a mean of 164 daily deaths during the data collection period. According to a longitudinal panel survey with a sample representative of the Czech population above 15 years old, 78.4% of people of Czechs knew someone who was or had been ill with COVID-19 (National Pandemic Alarm, 2021). The pandemic-related concerns were rising since the previous November, together with the increasing perceived personal impact of the restrictions and dropping trust in the government (National Pandemic Alarm, 2021). The students were attending their lectures online and the national state of emergency was, except for 2 weeks before Christmas, in effect since October 2020, together with a night curfew, a general stay-at-home order, and the closure of many industries, such as hospitality, entertainment, and sport.
Statistical Analysis
The scores for each scale were calculated as the sums of all items for scales of HLOC and CRT and as means for DES, CM, EHEALS, and (converting the reverse-scored questions) CC_HOAX, and CC_CREATED. In CRT, the inputs not containing any answer were interpreted as lack of effort rather than lack of ability to solve the puzzle and labeled as the missing values rather than the incorrect answers. A forced entry multiple linear regression analysis was used to evaluate the effect of the independent variables on the vaccination intentions in three different models, using the function “lm()” with its predefined parameters. For testing the interactions, moderation analysis was used as described by Wu and Zumbo (2008). The analysis was conducted in R 3.6.3, using the packages tidyverse (Wickham et al., 2019), psych (Revelle, 2020), and QuantPsyc (Fletcher, 2012); the figures were created using sjPlot (Lüdecke, 2021).
Results
Descriptive Statistics
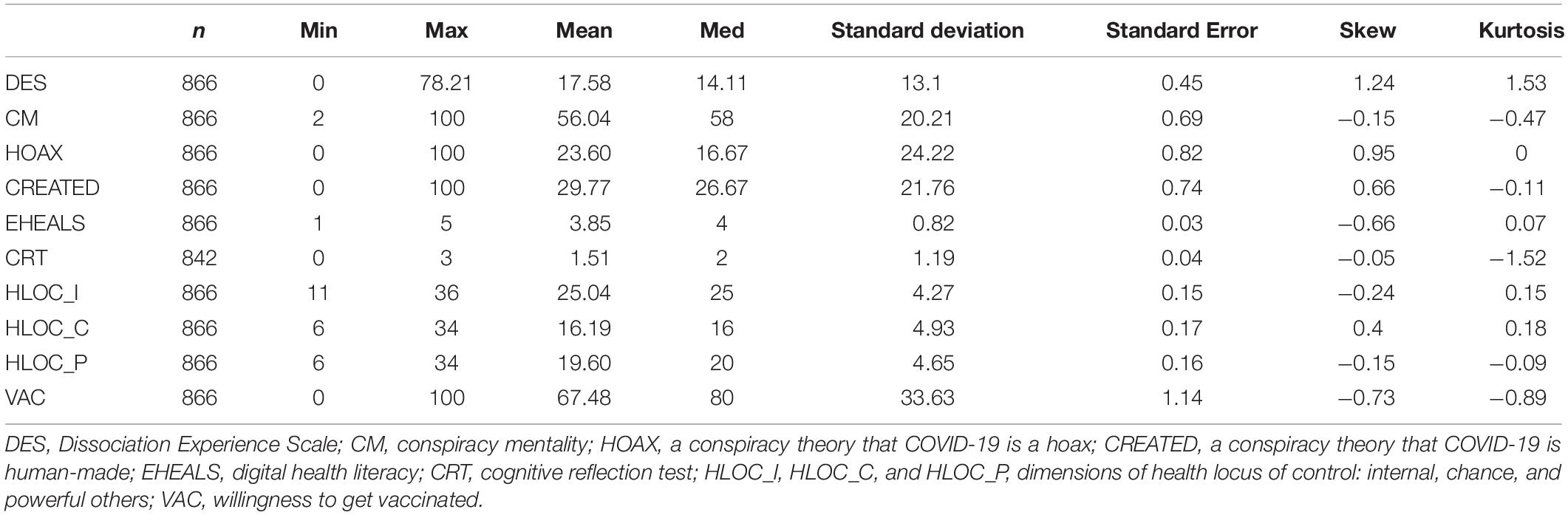
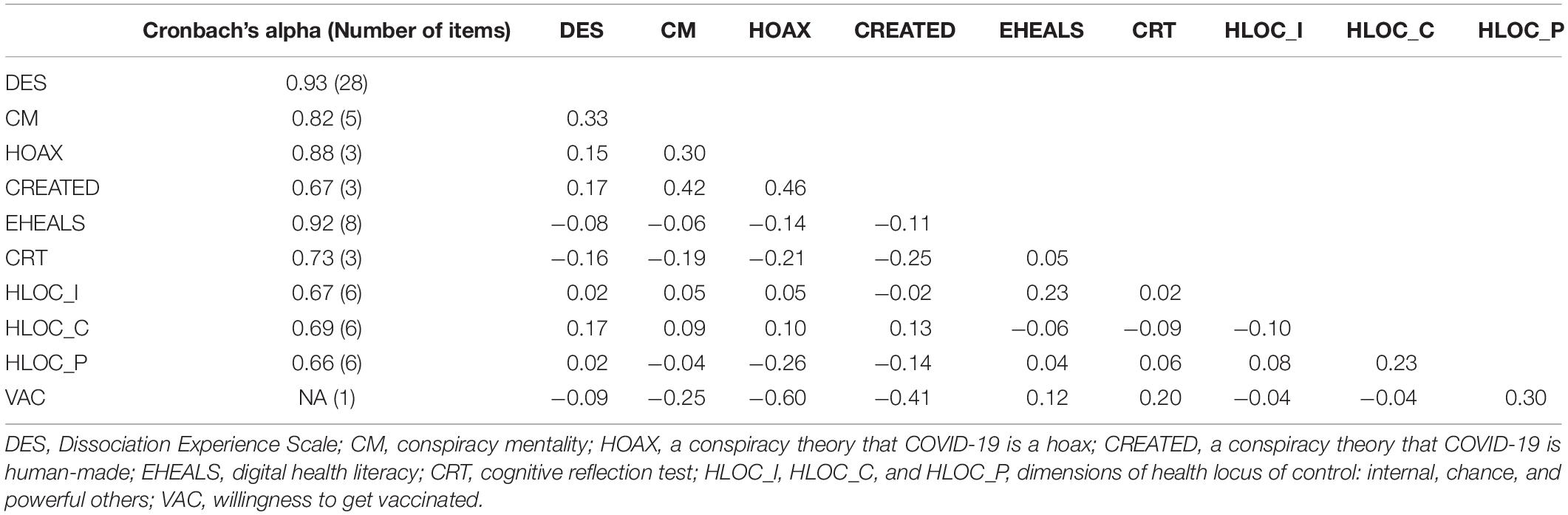
In the sample of 866 university students, 65.70% reported the probability that they would get vaccinated against COVID-19 as higher than 50%; the mean reported probability was 67.48%. Further descriptive values are depicted in Table 1. As shown in Table 2, all the scales used had at least acceptable reliability, especially taking into consideration the low number of items of some scales, and intercorrelations found elsewhere (refer to, for instance, Wallston, 2004).
Model 1
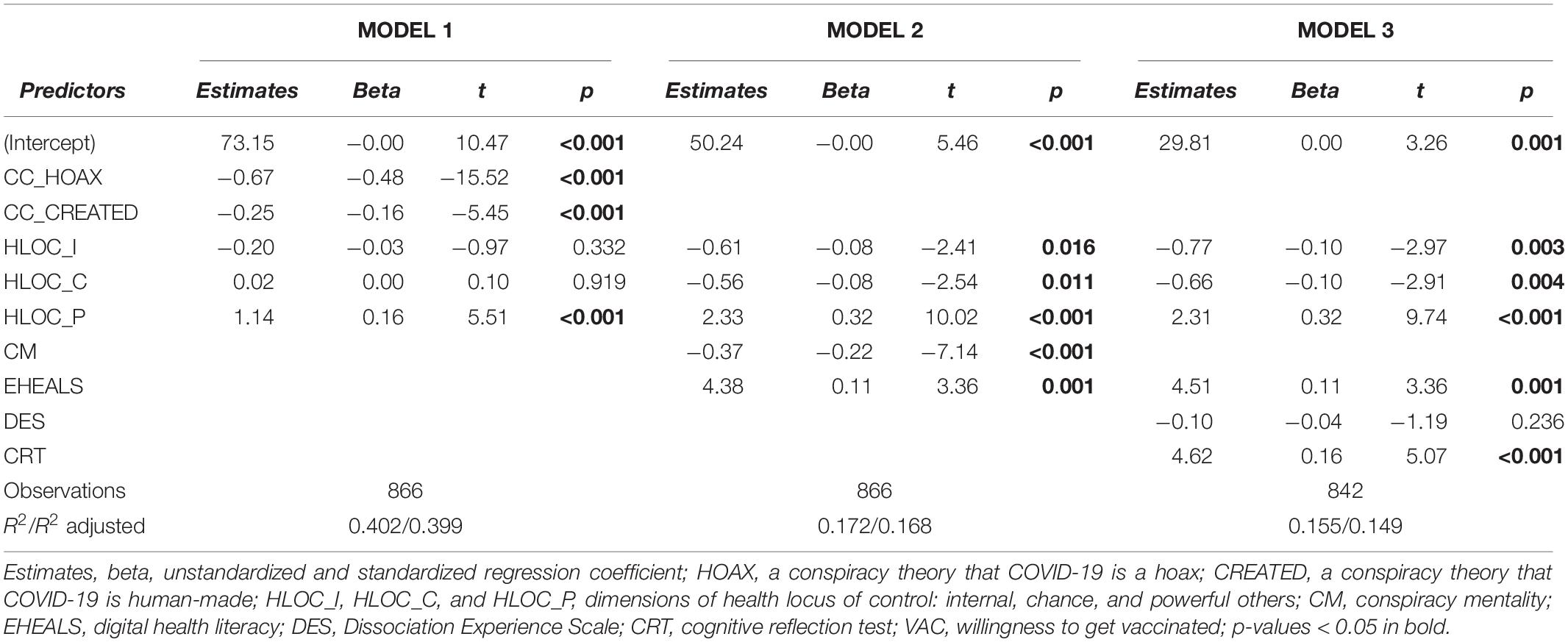
A multiple regression model using belief in COVID-19-related conspiracies and three dimensions of HLOC as predictors explained 40.21% of the variance of willingness to get vaccinated [R2 = 0.40, F(5,860) = 115.70, p < 0.001]. VAC was most strongly predicted by the belief that COVID-19 is a hoax (β = − 0.67, p < 0.001), followed by the belief that COVID-19 was created (β = − 0.16, p < 0.001), and powerful others HLOC (β = 0.16, p < 0.001), while the other two dimensions of HLOC had no effect (both the values of p > 0.3). The results summarized in Table 3 and visualized in Figure 1A support our hypothesis about VAC being predicted by the belief in the COVID-19-related conspiracy theories and reveal that when conspiracy theories about COVID-19 are taken into account, VAC is predicted by powerful others, but not internal or chance HLOC.

Figure 1. The effects of predictors on the willingness to get vaccinated. Beta coefficients of variables predicting willingness to get vaccinated in the linear regression model 1 (A), 2 (B), and 3 (C). CC_HOAX, a conspiracy theory that COVID-19 is a hoax; CC_CREATED, a conspiracy theory that COVID-19 is human-made; CM, conspiracy mentality; EHEALS, digital health literacy; DES, Dissociation Experience Scale; CRT, cognitive reflection test; HLOC_I, HLOC_C, and HLOC_P, internal, chance, and powerful others dimension of health locus of control. *p < 0.05, **p < 0.01, and ***p < 0.001.
Model 2
A multiple regression model using CM, digital health literacy, and three dimensions of HLOC as predictors explained 17.23% of the variance of willingness to get vaccinated [R2 = 0.17, F(5,860) = 35.81, p < 0.001]. VAC was most strongly predicted by powerful others HLOC (β = 0.32, p < 0.001), followed by CM (β = − 0.22, p < 0.001), digital health literacy (β = 0.11, p < 0.001), internal (β = − 0.08, p < 0.05), and chance (β = − 0.08, p < 0.05) HLOC. The results summarized in Table 3 and visualized in Figure 1B support our hypotheses about VAC being related to the CM and digital health literacy. Further, the results reveal that when CM and digital health literacy are taken into account, VAC is linked to low internal HLOC (contrary to our expectations), high powerful others HLOC, and low chance HLOC.
The moderation analysis was used to test whether the HLOC_I effect on the vaccination intentions may be moderated by the CM or digital health literacy (EHEALS). To test this, the HLOC_I and VAC scores were centered and scaled, and a regression model predicting CM (or EHEALS, respectively) based on the HLOC_I and VAC was compared with the same model containing the product of HLOC_I and VAC. The results of ANOVA revealed that the models did not differ significantly, indicating that there was no significant moderation effect of either EHEALS [F(1,862) = 1.85, p = 0.17] or CM [F(1,862) = 1.63, p = 0.20] on the link between HLOC_I on VAC. Therefore, our hypothesis that the effect of HLOC_I on vaccination intentions (VAC) may be moderated by CM and/or EHEALS is not supported by the data.
Model 3
A multiple regression model using experience with dissociation, cognitive reflection, digital health literacy, and three dimensions of HLOC as predictors explained 15.53% of the variance of the willingness to get vaccinated [R2 = 0.16, F(5,860) = 25.58, p < 0.001]. VAC was most strongly predicted by powerful others HLOC (β = 0.32, p < 0.001), followed by cognitive reflection (β = 0.22, p < 0.001), digital health literacy (β = 0.11, p < 0.001), internal (β = − 0.10, p < 0.01), and chance (β = − 0.10, p < 0.01) HLOC, while the effect of dissociation was not significant (p = 0.23). The results summarized in Table 3 and visualized in Figure 1C confirm the hypothesized effect of cognitive reflection on VAC but not the effect of dissociation on VAC. Further, they reveal that when dissociation and cognitive reflection are taken into account, VAC is linked to high powerful others HLOC, low chance HLOC, and low internal HLOC.
The results indicate that a one SD increase of powerful others dimension of HLOC was linked to an additional 10.76% of the subjectively estimated probability that the individual was going to get vaccinated against COVID-19. Similarly, a one SD increase in cognitive reflection and digital health literacy was linked to an additional 5.38% (CRT) and 3.70% (EHEALS) of the subjectively estimated probability that the individual was going to get vaccinated, and a decrease of one SD in internal or chance dimensions of HLOC was linked to an additional 3.36% of the subjectively estimated probability of getting vaccinated.
Discussion
The presented data support the hypotheses that the willingness to get vaccinated against COVID-19 is reduced by the belief in COVID-19-related conspiracy theories and its predictors: CM, low digital health literacy, and low cognitive reflection. Experience with dissociation had no effect on the willingness to get vaccinated. The vaccination intentions were strongly positively related to the powerful others dimension of HLOC and negatively to chance HLOC. Contrary to our expectations, internal HLOC also reduced the vaccination intentions and the effect of internal HLOC was not moderated by CM or digital health literacy.
The result showed that 66% of Czech university students participating in our study were willing to get vaccinated. Our result is consistent with the previous findings that 60–79% of the population was going to get vaccinated worldwide in the summer of 2020 and that the willingness to get vaccinated against COVID-19 was decreasing through the year 2020, with Eastern Europe (represented by Poland) showing the lowest vaccination intentions (Robinson et al., 2021). Considering the national representative survey with 50.3–50.4% of Czechs planning vaccination against COVID-19 (National Pandemic Alarm, 2021), our university student sample was showing above-average vaccination intentions, suggesting that the positive effect of higher education on the willingness to get vaccinated (Schwarzinger et al., 2021) was stronger than the negative effect of younger age (Neumann-Böhme et al., 2020; Robinson et al., 2021). It may also support the findings of some studies that the relationship between the vaccination intentions and age may be “U”-shaped rather than linear, with the middle-aged being least willing to get vaccinated (Kourlaba et al., 2021; Schwarzinger et al., 2021).
The vaccination intentions were predicted by COVID-19-related conspiracy theories. Further, they were predicted by digital health literacy, CM, and cognitive reflection. This is consistent with the previous research revealing a positive link between the vaccination intentions and cognitive reflection as a proxy of analytical cognitive style (Murphy et al., 2021). The observed effect of cognitive reflection on the vaccination intentions also mimics the results of an experimental study showing that promoting rational decision-making increases the intentions to wear a face mask (Capraro and Barcelo, 2021), indicating that our observations may be used to inspire interventions. Health literacy was also found to be predictive of higher vaccination intake under the conditions of a high risk of getting sick and complications in the short-term (Lorini et al., 2018)—conditions which are certainly satisfied with respect to the current pandemic. The experience with dissociation was not predictive of vaccination intention, even though it was predictive of CM (Pisl et al., 2021) which, in turn, predicted lower vaccination intentions. Given that the effect of paranormal thinking on belief in conspiracy theories is reduced by education (Douglas et al., 2016), the expected negative effect of dissociation experience on the vaccination intentions might possibly be present in the general population, although it was not reflected in our highly educated sample of university students. Alternatively, it is possible that while dissociation increases belief in the conspiracy theories, its effect does not translate into the changes in attitude toward vaccination.
The powerful others dimension of HLOC was strongly positively related to the intention of getting vaccinated, while the two other dimensions of HLOC (internal and chance) were related to vaccination weakly and negatively. A recent study found the same pattern of the effects of HLOC on the vaccine intentions in British, but not in an Irish representative sample of the general adult population (Murphy et al., 2021). Our data are also consistent with the previous findings that powerful others HLOC is positively related to pro-vaccination attitudes in parents (Tinsley and Holtgrave, 1989; Aharon et al., 2018) and nurses (Zhang et al., 2012; Kan et al., 2018), even though no effect of HLOC was found with respect to influenza vaccination in the elderly (Nexøe et al., 1999). Given that powerful others HLOC correlates with trust in the physicians (Brincks et al., 2010) and concerns related to side-effects and safety of vaccines are the top reasons for vaccine hesitation and refusal (Neumann-Böhme et al., 2020), the link between HLOC and willingness to get vaccinated may be mediated by trust in the medical professionals.
The chance HLOC was negatively related to the intention to get vaccinated in the latter two models, which is again consistent with the attitudes of parents toward vaccination (Aharon et al., 2018) as well as recent findings that the chance HLOC partly mediates the negative relationship between the religiosity and vaccination intentions (Olagoke et al., 2021). The absence of effect of chance HLOC in the first model, when two particular conspiracy theories were included, might reflect the correlation between the conspiracy beliefs and external HLOC in general (Abalakina-Paap et al., 1999).
The internal dimension of HLOC predicted the lower vaccination intentions in the latter two models. This is contrary to the model based on the attitudes of parents toward vaccination (Aharon et al., 2018) but consistent with the recent findings from Great Britain and Ireland (Murphy et al., 2021). The patients with higher internal HLOC might be more prone to follow their judgment rather than the advice of the professional community, as vaccine hesitancy may be an act of self-empowerment (Velan, 2016). In such cases, we would expect the link between the internal HLOC and vaccination intentions to be moderated by digital health literacy and/or CM, as it would be those individuals who lack health literacy and/or are prone to conspiracy thinking, for whom high internal HLOC would result in vaccine hesitancy. However, such moderation was not found in our data. Noticing that the findings of negative associations between internal HLOC and the willingness to get vaccinated come from highly informed samples, considering the medialization of COVID-19 in our study and in Murphy et al. (2021) and the medical background of the sample of Kan et al. (2018), we propose that internal HLOC may increase the vaccination intentions in the less-informed populations (perhaps increasing their awareness of the benefits or the mere existence of the vaccine) and decrease it in more informed ones (perhaps increasing the safety or efficacy concerns).
Our results may serve as a warning that promoting internal HLOC with respect to COVID-19 might come with an adverse effect on the willingness to get vaccinated. This is relevant, because the internal HLOC was previously found to be related to higher information seeking and lower depression, anxiety, and stress symptoms during the pandemic, and promoting it was suggested to reduce the psychiatric burden of COVID-19 (Sigurvinsdottir et al., 2020). This might be especially relevant for younger populations, as internal HLOC tends to decrease with age, together with a decreasing capacity to influence the health outcomes of an individual (Bailis et al., 2010). With respect to this age-specific pattern, the negative effect of internal HLOC on the willingness to get vaccinated might reflect overestimating the ability of an individual to cope with COVID-19 or reducing complacency in terms of the Confidence, Complacency, and Convenience Model of Vaccine Hesitancy (WHO, 2014). Such explanations would fit the finding that considering COVID-19 harmless is the third most popular reason for refusing vaccination in Europe (after concerns about vaccine side-effects and safety; Neumann-Böhme et al., 2020).
Altogether, 40% of the variance of vaccination intentions are explained by the belief in the COVID-19-related conspiracy theories and powerful others HLOC. Our final model then explained 16% of the variance of vaccination intentions based on cognitive reflection, digital health literacy, and HLOC. HLOC (the powerful others dimension in particular) was found to have the largest effect on the vaccination intentions, followed by the cognitive reflection, EHEALS, and the other two dimensions of HLOC. The effect of dissociation experience was not confirmed.
Recommendations
Reducing proneness to believing in the conspiracy theories by increasing analytical thinking and digital health literacy may increase the willingness to comply with the recommendations to get vaccinated in general. In the short-term, disproving the COVID-19-related conspiracy theories may have a positive effect on the willingness to get vaccinated against COVID-19. Furthermore, the positive link between powerful others HLOC and the willingness to get vaccinated suggests that the campaigns promoting vaccinations should target especially those not connecting their health with other persons. Because the persuasiveness of health-related promotion campaigns is increased when matching the prevailing HLOC of an audience (Williams-Piehota et al., 2004), the promotional messages should be created to appeal to audiences deriving their health from internal decisions (“Vaccination – your gift to yourself!”) or chance and destiny (“Destined to get vaccinated!”), rather than to those connecting their health with powerful others (“Scientists and doctors say: get vaccinated!”). Furthermore, the attempts to promote vaccination against COVID-19 should target those with intuitive rather than analytical cognitive style has given the lower vaccination intentions in those with low cognitive reflection.
Further Research
Possible mediators of the effect of powerful others HLOC on the vaccination intentions should be examined. To find ways to increase the intentions to get vaccinated, it would be beneficial to learn whether the effect of HLOC, which is relatively stable and developed in childhood (Lau, 1982), on the vaccination intentions may be mediated by something readier to change, such as the trust in health professionals. The effect of internal HLOC on the vaccination intentions and other health attitudes remains elusive and should be studied, especially with relation to how well subjects are informed about the scrutinized subject.
Limitations
The timing of the data collection in the weeks after the vaccination campaign was started limits the generalization of the absolute numbers. The immediate effect of pandemics on individual lives may strengthen the political and epistemic predictors of the conspiratorial explanations at the expense of the psychological ones (Hartman et al., 2020), which may have affected the attitudes toward vaccination. Further, the weekly number of persons met for at least 5 min in person was reduced to 17–18 in the respective period according to data on a representative Czech sample between 18 and 34 years of age (compared with up to 29.5 when the restrictions were loosened in summer 2020; Zivot behem pandemie, 2021). This might have affected our estimate of the relative importance of personal predictors and social factors with respect to the vaccination intentions. For instance, the personal willingness to get vaccinated is positively associated with the estimated vaccination intentions of peers and society (Agranov et al., 2021; Graupensperger et al., 2021). With peer interactions taking place online and offline (Luo et al., 2021), the effects of restricting personal contacts on social factors are complex, limiting the generalization of our findings beyond the end of the pandemic restrictions. Besides the restrictions, social processes tend to be affected by the experience of a disastrous event such as a pandemic (Sullivan, 2014; Townshend et al., 2015), which might have, again, affected the conspiracy beliefs as well as the willingness to comply with the recommendations to get vaccinated in a manner specific for a given time and place. Further, the survey answers of the participants about willingness to vaccinate might differ from their actual decision. For example, in a study of Dutch healthcare professionals, only 73.9% of those reporting high intention to get vaccinated against influenza in a survey were vaccinated a month later (compared with 1.3% of those with no intention; Lehmann et al., 2014).
The sample of university students may have influenced the effects of the scrutinized factors on the beliefs in conspiracy theories, via the above-mentioned effects of age and education on the willingness to get vaccinated and by the heterogeneity related to different fields of their studies. Also, our sample included predominantly (72%) female participants and women who have lower vaccination intentions and acceptance than men across the countries (Wang et al., 2021; Zintel et al., 2021), with the effect of gender being partly mediated by perceived behavioral control in the British and German samples (Sieverding et al., 2021). Because perceived behavioral control is conceptually related to HLOC, this might have affected the observed effects, although the link between both the constructs is weak, with HLOC explaining only 4% of the variance in the perceived behavioral control (Armitage, 2003). Only two COVID-19-related conspiracy theories were used for the analysis, limiting its generalizability to the whole scope of conspiracy beliefs about coronavirus.
Conclusion
In the study, two-thirds of our sample of Czech university students were willing to get vaccinated in January 2021, outpacing the national average of 50% of the population. About 40% of the variance of the willingness to get vaccinated was explained by powerful others HLOC and two conspiracy beliefs, indicating that a substantial part of vaccine refusal is a consequence of individual beliefs and characteristics rather than a moral decision one can be blamed for. One-sixth of the variance of vaccination intentions was explained by cognitive reflection, digital health literacy, and—especially—HLOC, showing that the psychological variables are relevant for the willingness to get vaccinated against COVID-19. The understanding of the predictors of vaccination intentions should be reflected in the campaigns promoting vaccination against COVID-19.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of the University Hospital and the Faculty of Medicine, Charles University in Pilsen (49/2021, 4th February 2021). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JVe, JVo, and VP: conceptualization. VP, JVe, and EC: methodology. VP and EC: formal analysis. VP, JVe, and GK: investigation. JVe, GK, KC, and VP: resources. VP: writing—original draft preparation. JVo, JVe, EC, GK, KC, and VP: writing—review and editing. JVe: supervision, project administration, and funding acquisition. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Research Center of Charles University, program number 9, and Ministry of the Interior of the Czech Republic, project VJ01010116.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Nicole Volavka, for editing this manuscript.
References
Abalakina-Paap, M., Stephan, W. G., Craig, T., and Gregory, W. L. (1999). Beliefs in conspiracies. Polit. Psychol. 20:3. doi: 10.1111/0162-895X.00160
Agranov, M., Elliott, M., and Ortoleva, P. (2021). The importance of Social Norms against strategic effects: the case of Covid-19 vaccine uptake. Econ. Lett. 206:109979. doi: 10.1016/j.econlet.2021.109979
Aharon, A. A., Nehama, H., Rishpon, S., and Baron-Epel, O. (2018). A path analysis model suggesting the association between health locus of control and compliance with childhood vaccinations. Hum. Vaccin. Immunother. 14, 1618–1625. doi: 10.1080/21645515.2018.1471305
Armitage, J. C. (2003). The relationship between multidimensional health locus of control and perceived behavioural control: how are distal perceptions of control related to proximal perceptions of control? Psychol. Health 18, 723–738.
Bailis, D. S., Segall, A., and Chipperfield, J. G. (2010). Age, relative autonomy and change in health locus of control beliefs: a longitudinal study of members of a health-promotion facility. J. Health Psychol. 15, 326–338. doi: 10.1177/1359105309342296
Bierwiaczonek, K., Kunst, J. R., and Pich, O. (2020). Belief in COVID-19 conspiracy theories reduces social distancing over time. Appl. Psychol. Health Well Being 12, 1270–1285. doi: 10.1111/aphw.12223
Brincks, A. M., Feaster, D. J., Burns, M. J., and Mitrani, V. B. (2010). The influence of health locus of control on the patient-provider relationship. Psychol. Health Med. 15, 720–728. doi: 10.1080/13548506.2010.498921
Bruder, M., Haffke, P., Neave, N., Nouripanah, N., and Imhoff, R. (2013). Measuring individual differences in generic beliefs in conspiracy theories across cultures: conspiracy mentality questionnaire. Front. Psychol. 4:225. doi: 10.3389/fpsyg.2013.00225
Capraro, V., and Barcelo, H. (2021). Telling people to “rely on their reasoning” increases intentions to wear a face covering to slow down COVID-19 transmission. Appl. Cogn. Psychol. 35, 693–699. doi: 10.1002/acp.3793
Chapman, G. B., and Coups, E. J. (1999). Predictors of influenza vaccine acceptance among healthy adults. Prev. Med. 29, 249–262.
Charlton, E. (2014). Conspiracy Theories and Dissociative Experiences: The Role of Personality and Paranormal Beliefs. Ph.D. thesis. London: Metropolitan University.
Douglas, K. M. (2021). COVID-19 conspiracy theories. Group Process. Intergroup Relat. 24, 270–275. doi: 10.1177/1368430220982068
Douglas, K. M., Sutton, R. M., Callan, M. J., Dawtry, R. J., and Harvey, A. J. (2016). Someone is pulling the strings: hypersensitive agency detection and belief in conspiracy theories. Think. Reason. 22, 57–77. doi: 10.1080/13546783.2015.1051586
Douglas, K. M., Uscinski, J. E., Sutton, R. M., and Deravi, F. (2019). Understanding conspiracy theories. Polit. Psychol. 40, 3–35. doi: 10.1111/pops.12568
Fletcher, T. D. (2012). QuantPsyc: Quantitative Psychology Tools. R Package. Available online at: https://cran.r-project.org/package=QuantPsyc. (accessed April 5, 2021).
Frederick, S. (2005). Cognitive reflection and decision making. J. Econ. Perspect. 19, 25–42. doi: 10.1257/089533005775196732
Graupensperger, S., Abdallah, D. A., and Lee, C. M. (2021). Social norms and vaccine uptake: college students’ COVID vaccination intentions, attitudes, and estimated peer norms and comparisons with influenza vaccine. Vaccine 39, 2060–2067. doi: 10.1016/j.vaccine.2021.03.018
Grotz, M., Hapke, U., Lampert, T., and Baumeister, H. (2011). Health locus of control and health behaviour: results from a nationally representative survey. Psychol. Health Med. 16, 129–140. doi: 10.1080/13548506.2010.521570
Hartman, T., Marshall, M., Stocks, T., McKay, R., and Bentall, R. (2020). Different conspiracy theories have different psychological and social determinants: comparison of three theories about the origins of the COVID-19 virus in a representative sample. PsyArXiv [Preprint]. doi: 10.31234/OSF.IO/MZ5SW
Imhoff, R., and Bruder, M. (2013). Speaking (Un-)truth to power: conspiracy mentality as a generalised political attitude. Eur. J. Pers. 20, 25–43. doi: 10.1002/per.1930
Imhoff, R., and Lamberty, P. (2020). A bioweapon or a hoax? the link between distinct conspiracy beliefs about the coronavirus disease (COVID-19) outbreak and pandemic behavior. Soc. Psychol. Pers. Sci. 11, 1110–1118. doi: 10.1177/1948550620934692
Jolley, D., and Douglas, K. M. (2014). The effects of anti-vaccine conspiracy theories on vaccination intentions. PLoS One 9:e89177. doi: 10.1371/journal.pone.0089177
Kan, T., Ai, J., Zhang, J., and Liu, X. (2018). Predictors of seasonal influenza vaccination behaviour among nurses and implications for interventions to increase vaccination uptake: a cross-sectional survey. Int. J. Nurs. Stud. 79, 137–144. doi: 10.1016/j.ijnurstu.2017.12.003
Kourlaba, G., Kourkouni, E., Maistreli, S., Tsopela, C.-G., Molocha, N.-M., Triantafyllou, C., et al. (2021). Willingness of Greek general population to get a COVID-19 vaccine. Glob. Health Res. Policy 6:3. doi: 10.1186/s41256-021-00188-1
Lau, R. R. (1982). Origins of health locus of control beliefs. J. Pers. Soc. Psychol. 42, 322–334. doi: 10.1037/0022-3514.42.2.322
Lehmann, B. A., Ruiter, R. A. C., Chapman, G., and Kok, G. (2014). The intention to get vaccinated against influenza and actual vaccination uptake of Dutch healthcare personnel. Vaccine 32, 6986–6991. doi: 10.1016/j.vaccine.2014.10.034
Lorini, C., Santomauro, F., Donzellini, M., Capecchi, L., Bechini, A., Boccalini, S., et al. (2018). Health literacy and vaccination: a systematic review. Hum. Vaccin. Immunother. 14, 478–488. doi: 10.1080/21645515.2017.1392423
Lüdecke, D. (2021). sjPlot: Data Visualization for Statistics in Social Science. Available online at: https://cran.r-project.org/package=sjPlot. (accessed April 5, 2021).
Luo, S., Xin, M., Wang, S., Zhao, J., Zhang, G., Li, L., et al. (2021). Behavioural intention of receiving COVID-19 vaccination, social media exposures and peer discussions in China. Epidemiol. Infect. 149:E158. doi: 10.1017/S0950268821000947
Machingaidze, S., and Wiysonge, C. S. (2021). Understanding COVID-19 vaccine hesitancy. Nat. Med. 27, 1338–1339. doi: 10.1038/s41591-021-01459-7
Mathieu, E., Ritchie, H., Ortiz-Ospina, E., Roser, M., Hasell, J., Appel, C., et al. (2021). A global database of COVID-19 vaccinations. Nat. Hum. Behav. 5, 947–953. doi: 10.1038/s41562-021-01122-8
Murphy, J., Vallières, F., Bentall, R. P., Shevlin, M., McBride, O., Hartman, T. K., et al. (2021). Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 12:29. doi: 10.1038/s41467-020-20226-9
MZCR (2021). COVID-19: Pøehled Aktuální Situace v ÈR. Available online at: https://onemocneni-aktualne.mzcr.cz/covid-19 (accessed August 29, 2021).
Naeem, B. S., and Boulos, K. M. N. (2021). COVID-19 misinformation online and health literacy: a brief overview. Int. J. Environ. Res. Public Health 2021:8091. doi: 10.3390/ijerph18158091
Náfrádi, L., Nakamoto, K., and Schulz, P. J. (2017). Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PLoS One 12:e0186458. doi: 10.1371/journal.pone.0186458
National Pandemic Alarm (2021). Representative Survey Monitoring Public Opinion, Emotions and Experience With Novelty Corona Virus Spread in Five Central European Countries. Available online at: https://www.nationalpandemicalarm.eu/en/2021-01-29?index=vaccination#global-timeline-index-wrapper. (accessed August 27, 2021).
Neumann-Böhme, S., Varghese, N. E., Sabat, I., Barros, P. P., Brouwer, W., van Exel, J., et al. (2020). Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur. J. Health Econ. 21, 977–982. doi: 10.1007/s10198-020-01208-6
Nexøe, J., Kragstrup, J., and Søgaard, J. (1999). Decision on influenza vaccination among the elderly: a questionnaire study based on the health belief model and the multidimensional locus of control theory. Scand. J. Prim. Health Care 17, 105–110. doi: 10.1080/028134399750002737
Norman, C. D., and Skinner, H. A. (2006). eHEALS: the eHealth literacy scale. J. Med. Internet Res. 8:e507. doi: 10.2196/jmir.8.4.e27
O’Hea, E. L., Grothe, K. B., Bodenlos, J. S., Boudreaux, E. D., White, M. A., and Brantley, P. J. (2005). Predicting medical regimen adherence: the interactions of health locus of control beliefs. J. Health Psychol. 10, 705–717. doi: 10.1177/1359105305055330
Olagoke, A. A., Olagoke, O. O., and Hughes, A. M. (2021). Intention to vaccinate against the Novel 2019 coronavirus disease: the role of health locus of control and religiosity. J. Relig. Health 60, 65–80. doi: 10.1007/s10943-020-01090-9
Pickles, K., Cvejic, E., Nickel, B., and McCaffery, K. J. (2021). COVID-19 misinformation trends in Australia: prospective longitudinal national survey. J. Med. Internet Res. 23:e23805. doi: 10.2196/23805
Pisl, V., Volavka, J., Chvojkova, E., Cechova, K., Kavalirova, G., and Vevera, J. (2021). Dissociation, cognitive reflection and health literacy have modest effect on belief in conspiracy theories about COVID-19. Int. J. Environ. Res. Public Health 18:5056. doi: 10.3390/ijerph18105065
Ptáček, R., and Bob, P. (2009). Metody diagnostiky disociativních symptomů. Czech Slovak Psychiatry 105, 163–172.
Pummerer, L., Böhm, R., Lilleholt, L., Winter, K., Zettler, I., and Sassenberg, K. (2021). Conspiracy theories and their societal effects during the COVID-19 pandemic. Soc. Psychol. Personal. Sci. doi: 10.1177/19485506211000217 [Epub ahead of print].
Revelle, W. (2020). psych: Procedures for Psychological, Psychometric, and Personality Research. R package. Available online at: https://cran.r-project.org/package=psych. (accessed April 5, 2021).
Robinson, E., Jones, A., Lesser, I., and Daly, M. (2021). International estimates of intended uptake and refusal of COVID-19 vaccines: a rapid systematic review and meta-analysis of large nationally representative samples. Vaccine 39, 2024–2034. doi: 10.1016/j.vaccine.2021.02.005
Romer, D., and Jamieson, K. H. (2020). Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc. Sci. Med. 263:113356. doi: 10.1016/j.socscimed.2020.113356
Schwarzinger, M., Watson, V., Arwidson, P., Alla, F., and Luchini, S. (2021). COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health 6, e210–e221. doi: 10.1016/s2468-2667(21)00012-8
Sieverding, M., Zintel, S., Schmidt, L. I., Arbogast, A. L., and von Wagner, C. (2021). Why do Women Report Lower Intentions to get Vaccinated Against COVID-19? The Mediating Role of Variables from the TPB and HBM. SSRN, 3826959. doi: 10.2139/ssrn.3826959
Sigurvinsdottir, R., Thorisdottir, I. E., and Gylfason, H. F. (2020). The impact of COVID-19 on mental health: the role of locus on control and internet use. Int. J. Environ. Res. Public Health 17:6985. doi: 10.3390/ijerph17196985
Solís Arce, S. A., Warren, S. S., Meriggi, N. F., Scacco, A., McMurry, N., and Omer, S. B. (2021). COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat. Med. 27, 1385–1394. doi: 10.1038/s41591-021-01454-y
Stoica, C. A., and Umbreş, R. (2020). Suspicious minds in times of crisis: determinants of Romanians’ beliefs in COVID-19 conspiracy theories. Eur. Soc. 23, S246–S261. doi: 10.1080/14616696.2020.1823450
Sullivan, G. (2014). “Disasters, overview,” in Encyclopedia of Critical Psychology, ed. T. Teo (New York, NY: Springer Science + Busines Media), 445–448.
Tinsley, B. J., and Holtgrave, D. R. (1989). Maternal health locus of control beliefs, utilization of childhood preventive health services, and infant health. J. Dev. Behav. Pediatr. 10, 236–241. doi: 10.1097/00004703-198910000-00003
Townshend, I., Awosoga, O., Kulig, J., and HaiYan, F. (2015). Social cohesion and resilience across communities that have experienced a disaster. Nat. Hazards 76, 913–938. doi: 10.1007/s11069-014-1526-4
Van Bavel, J. J., Baicker, K., Boggio, P. S., and Willer, R. (2020). Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 4, 460–471. doi: 10.1038/s41562-020-0884-z
Velan, B. (2016). Vaccine hesitancy as self-determination: an Israeli perspective. Isr. J. Health Policy Res. 5:13. doi: 10.1186/s13584-016-0071-x
Wallston, K. A. (2004). “Control and health,” in Encyclopedia of Health & Behavior, Vol. 1, ed. N. Anderson (Thousand Oaks, CA: Sage), 217–220.
Wallston, K. A., Wallston, B. S., and DeVellis, R. (1978). Development of the Multidimensional Health Locus of Control (MHLC) scales. Health Educ. Behav. 6, 160–170. doi: 10.1177/109019817800600107
Wang, Q., Yang, L., Jin, H., and Lin, L. (2021). Vaccination against COVID-19: a systematic review and meta-analysis of acceptability and its predictors. Prev. Med. 150:106694. doi: 10.1016/j.ypmed.2021.106694
West, L. M., Theuma, R. B., and Cordina, M. (2018). Health locus of control: its relationship with medication adherence and medication wastage. Res. Social Adm. Pharm. 14, 1015–1019. doi: 10.1016/j.sapharm.2017.12.003
Wickham, H., Averick, M., Bryan, J., Chang, W., McGowan, L., François, R., et al. (2019). Welcome to the Tidyverse. J. Open Source Softw. 4:1686. doi: 10.21105/joss.01686
Williams, S. (2021). The UK’s coronavirus policy still places too much responsibility–and blame–on the public. BMJ 373:1373. doi: 10.1136/bmj.n1373
Williams-Piehota, P., Schneider, T. R., Pizarro, J., Mowad, L., and Salovey, P. (2004). Matching health messages to health locus of control beliefs for promoting mammography utilization. Psychol. Health 19, 407–423. doi: 10.1080/08870440310001652678
Winter, K., Pummerer, L., Hornsey, M. J., and Sassenberg, K. (2021). Pro-vaccination subjective norms moderate the relationship between conspiracy mentality and vaccination intentions. Br. J. Health Psychol. doi: 10.1111/bjhp.12550 [Epub ahead of print].
Wood, M. J., Douglas, K. M., and Sutton, R. M. (2012). Dead and alive. Soc. Psychol. Person. Sci. 3, 767–773. doi: 10.1177/1948550611434786
WHO (2013). Health Literacy: The Solid Facts. Available online at: https://apps.who.int/iris/bitstream/handle/10665/128703/e96854.pdf. (accessed April 5, 2021).
WHO (2014). Report of the Sage Working Group on Vaccine Hesitancy. Available online at: https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf. (accessed April 5, 2021).
WHO (2020). Novel Coronavirus. Situation Report–13. 2020. Available online at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200202-sitrep-13-ncov-v3.pdf. (accessed April 5, 2021).
Wu, A. D., and Zumbo, B. D. (2008). Understanding and using mediators and moderators. Soc. Indic. Res. 87, 367–392. doi: 10.1007/s11205-007-9143-1
Zhang, J., While, A. E., and Norman, I. J. (2012). Seasonal influenza vaccination knowledge, risk perception, health beliefs and vaccination behaviours of nurses. Epidemiol. Infect. 140, 1569–1577. doi: 10.1017/S0950268811002214
Zintel, S., Flock, C., Arbogast, A. L., Forster, A., von Wagner, C., and Sieverding, M. (2021). Gender Differences in the Intention to get Vaccinated Against COVID-19-A Systematic Review and Meta-Analysis. SSRN, 3803323. doi: 10.2139/ssrn.3803323
Zivot behem pandemie (2021). S kolika lidmi byli respondenti v bližším kontaktu?. Available online at: https://zivotbehempandemie.cz/kontakty. (accessed August 27, 2021).
Keywords: COVID-19, pandemics, vaccination, willingness to get vaccinated, conspiracy theories, health locus of control, conspiracy mentality
Citation: Pisl V, Volavka J, Chvojkova E, Cechova K, Kavalirova G and Vevera J (2021) Willingness to Vaccinate Against COVID-19: The Role of Health Locus of Control and Conspiracy Theories. Front. Psychol. 12:717960. doi: 10.3389/fpsyg.2021.717960
Received: 31 May 2021; Accepted: 24 September 2021;
Published: 22 October 2021.
Edited by:
Victoria Team, Monash University, AustraliaReviewed by:
Catarina Samorinha, University of Sharjah, United Arab EmiratesValerio Capraro, Middlesex University, United Kingdom
Stephanie Rizio, University of Groningen, Netherlands
Copyright © 2021 Pisl, Volavka, Chvojkova, Cechova, Kavalirova and Vevera. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jan Vevera, dmV2ZXJhamFuQGdtYWlsLmNvbQ==
 Vojtech Pisl
Vojtech Pisl Jan Volavka1
Jan Volavka1 Katerina Cechova
Katerina Cechova Gabriela Kavalirova
Gabriela Kavalirova Jan Vevera
Jan Vevera